- 1Eastern and Southern Africa Centre of International Parasite Control (ESACIPAC), Kenya Medical Research Institute (KEMRI), Nairobi, Kenya
- 2School of Public Health, Jomo Kenyatta University of Agriculture and Technology (JKUAT), Nairobi, Kenya
- 3Washington State University Global Health Program, Washington State University, Nairobi, Kenya
- 4Paul G, Allen School of Global Health, Washington State University, Pullman, WA, United States
- 5Department of Research and Programmes, African Institute for Health and Development (AIHD), Nairobi, Kenya
- 6Division of Vector Borne and Neglected Tropical Diseases (DVB/NTDs), Ministry of Health (MoH), Nairobi, Kenya
- 7Center for Global Health, Department of Neurology, Technical University of Munich (TUM), Munich, Germany
- 8Department of Infectious Disease Epidemiology and International Health, London School of Hygiene and Tropical Medicine, London, United Kingdom
- 9Department of Community Medicine and Global Health, Institute of Health and Society, University of Oslo, Oslo, Norway
- 10Department of Global Health and Social Medicine, Harvard Medical School, Boston, MA, United States
Background: Over 50 million preschool-age children (PSAC) in Africa need treatment for schistosomiasis but are excluded due to lack of a suitable child-friendly medication. The Paediatric Praziquantel Consortium has developed a novel paediatric formulation for PSAC. In advance of its roll-out, we conducted a social science study to draw lessons to inform implementation.
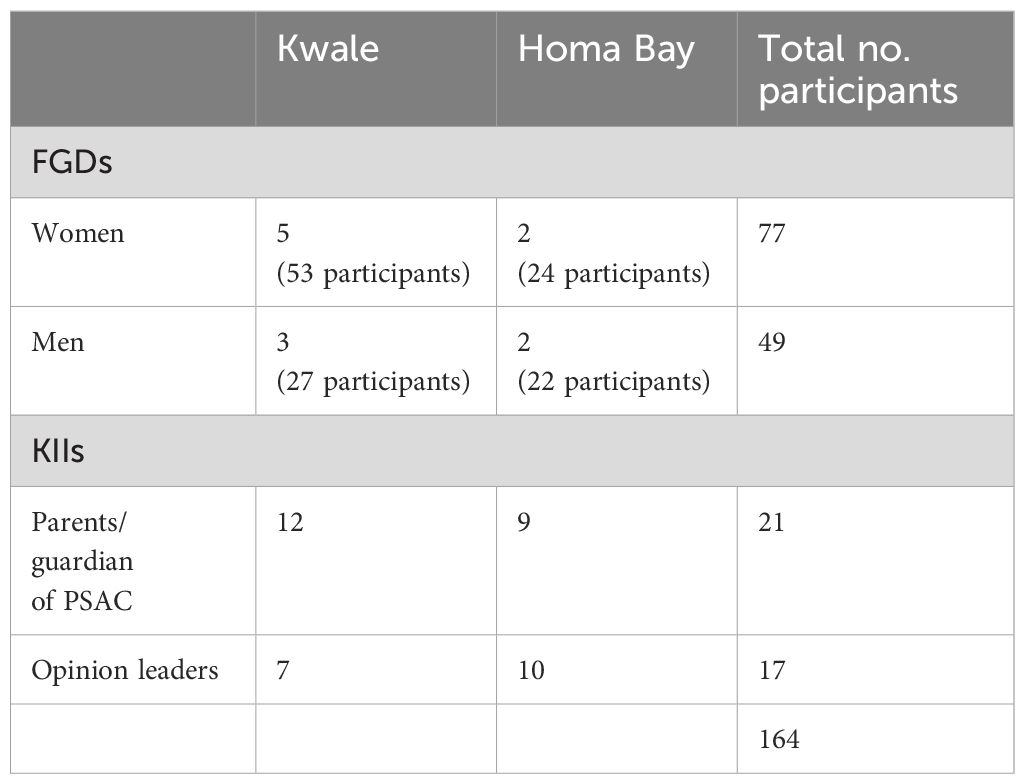
Methods: We conducted a cross-sectional study in eight villages in two purposively selected highly endemic Kenyan counties (Homa Bay and Kwale). We conducted 17 in-depth interviews with community opinion leaders and 21 with parents/guardians of PSAC. Twelve focus group discussions with parents/guardians of PSAC were also held. The aim was to assess their knowledge, perceptions, practices and willingness to participate in the medication’s roll-out for schistosomiasis. Thematic data analysis was performed.
Results: Most participants had heard of schistosomiasis and perceived it to be a serious disease whose treatment should be prioritised. Others felt it was a common disease that should not cause concern. Some people believed schistosomiasis was caused by witchcraft while others regarded it as a sexually transmitted infection. In addition, some practices like poor human waste disposal and water contact were thought to contribute to continued transmission of the disease.
Conclusion: Community members know and perceive schistosomiasis to be serious, but misinformation about its cause is prevalent. The study suggests the need for increased awareness creation to change the perceptions of communities in relation to schistosomiasis prevention and control. Community sensitisation should be prioritised in advance of medication roll-out.
Introduction
Schistosomiasis leads to chronic illness as well as significant health and economic burden to affected persons in large parts of the world (1). It is one of the twenty neglected tropical diseases (NTDs), affecting the world’s poorest people (2). Globally, an estimated 779 million people are at risk of schistosomiasis (3). More than 230 million are infected. Of the 230 total infected, the following are either symptomatic or severely affected respectively (120 million and 20 million) (4, 5). The parasitic disease occurs mainly among rural dwellers in tropical and subtropical countries where limited health awareness, poverty and inadequate sanitation favour the disease transmission (6). Transmission occurs mainly due to contact with cercariae-contaminated water bodies (7). Over the last fifty years, schistosomiasis distribution has reduced in some areas due to successful control but increased in others due to population growth and increased contact with unsafe water (4). In Kenya, over five million school age children (SAC) are estimated to be at risk of either urinary or intestinal schistosomiasis infection with the disease mainly occurring in Coastal and Western Regions (8).
Several studies have assessed knowledge and awareness of schistosomiasis among adults and SAC populations living in endemic areas. There has been high level of familiarity with the name of the parasitic infection, however, awareness has often been limited to hearing about the disease name (9, 10). In addition, many studies have reported poor knowledge of disease transmission, treatment, prevention and control measures (9, 11). The most common misconceptions and misinformation held are that schistosomiasis is acquired by drinking or eating contaminated food and water (12, 13).
Previously, pre-school age children (PSAC) (≤5 years) and infants were perceived to be at low risk of infection with schistosomiasis based on the assumption that young children have little direct contact with schistosome cercariae-infested water (14–16). In many cases, children from endemic areas are often infected by the age of two years and most of them remain chronically infected throughout their school-age years unless there is mass drug administration (MDA) intervention (17). Hence, in 2010, the World Health Organization (WHO) recommended inclusion of PSAC in large scale treatment programmes (18). In the absence of an appropriate paediatric formulation, broken or crushed praziquantel (PZQ) tablets have been recommended (19).
Treatment with PZQ has shown to be safe and efficacious in children aged 1 to 5 years, but dosing and administration is challenged by the standard 600 mg tablet dose, for its large size and bitter taste (19). The overall lack of paediatric formulation for schistosomiasis poses several operational challenges in regard to individual drug dosage determination (weighing, measuring length/height), drug manipulation (crushing, splitting, suspending) and administration (dissolving and mixing) (20). These practices are, however, not considered feasible in the context of large-scale MDA programmes. The residual bitterness of PZQ has seen children spitting out the drug, raising questions around actual intake, drug efficacy and potential need for repeated administration (20).
Acknowledging the unmet need to treat PSAC, the Paediatric Praziquantel Consortium has developed a novel child-friendly ar-Praziquantel (arPZQ) 150 mg orodispersible tablet (ar-PZQ-ODT) (21). Successful clinical trials in Kenya and Côte d’Ivoire established that the new arPZQ tablet is suitable for use by PSAC. A pilot programmatic rollout is expected to be conducted in two endemic counties of Kenya (22). However, the inclusion of PSAC into MDA programmes may cause implementation challenges among various stakeholders. Previous studies have shown that MDA programmes for NTDs in Sub-Saharan Africa do not always meet their projected goals and may be less effective for the targeted communities than expected (23, 24). The aim of this study was to gather information on knowledge, perceptions and practices of schistosomiasis among parents/guardians of PSAC and other key stakeholders to reveal possible misinformation, concerns, or hesitation that prevent communities from accepting deworming drugs.
Methods
Study design and site
We conducted a cross-sectional study using qualitative methods in two purposively selected counties of Kenya (Homa Bay and Kwale) owing to previous studies which had shown high prevalence of schistosomiasis in these areas (8, 25). One sub-county was purposely sampled in each county and four villages were randomly selected for the study.
Kwale County is located along the coast of the Indian ocean, 40 kilometres (kms) south of Mombasa, the second largest city in Kenya. The County has an area of 8360 km2 with an estimated population of 866,829 persons (26). The County is endemic for S. haematobium (8). Homa Bay County is situated in the western part of Kenya and borders Lake Victoria, which is endemic for both schistosomiasis species (25). The County has an approximate population of 1,131,950, spread over 262,036 households, in an area of 3,154.7 km2 (26).
Study population and data collection
Data was collected by conducting in-depth interviews (IDIs) and focus group discussions (FGDs) (Table 1). We conducted 12 FGDs with parents/guardians of PSAC in both counties segregated by age and gender. Each FGD contained a minimum of eight and a maximum of 12 participants and standard procedures were adhered to (27). In addition, IDIs were conducted with 17 opinion leaders (community leaders, village heads and chiefs) and 21 parents/guardians of PSAC in both counties. All the study participants were purposively selected. The saturation model was used to determine the number of FGDs and KIIs to be conducted in each study area (28). Meetings were held with the county and subcounty health management teams to sensitize them on the study and get permission to conduct the study. In addition, community level meetings were held with chiefs, village heads and community health volunteers (CHVs), working in their respective villages to support community mobilization.
Data collection was done using interview and discussion guides for each category by trained research assistants as moderators and note takers using digital voice recorders. The purpose was to gather information on the participants on the research questions and ask for their recommendations for the planned pilot MDA of the new drug. Data were audio recorded, transcribed verbatim and coded by the lead author according to study themes. The notes of all the transcripts were typed and saved in MS Word format.
Data analysis
All notes were imported to Nvivo version 12 software for further processing and analysis. The software enabled distinguishing of themes and sub-themes by running queries to allow identification of patterns within the coded data. This involved reviewing the data to identify emerging themes and sub-themes by generating a coding framework and applying it to the data to identify synergies between themes. For specific analyses, simple and advanced coding queries were used to search for words, and phrases in the notes. A thematic analysis was used where responses were categorised into themes and then ideas formulated by examining the patterns of responses (27).
Results
Knowledge about schistosomiasis/bilharzia infection
Most study participants in both counties indicated that they know and have heard about schistosomiasis, also referred to as bilharzia. The local names mentioned for the disease in Homa Bay and Kwale were “Layo remo” and ‘Kishonono”, respectively. The participants opined as follows.
“I know it’s a disease of urinating blood (Layo Remo) and it is transmitted when we urinate in water (Ka walayo e pii)” (Male FGD Homa Bay).
“We know that bilharzia penetrates through the feet by stepping in water, already one may contract this disease, or can even stay longer but not contract this disease. People should be warned not to urinate inside the water be it lake or river. Bilharzia has a cycle it follows, from a snail and then it continues up to us” (Male FGD Homa Bay).
Nevertheless, two of the parents/guardians from Kwale study site indicated that they had not heard of the disease infecting adults. They reported that they thought the disease affects children only. On the same note, there were a few parents/guardians from the Homa Bay site who felt that there was general poor knowledge of bilharzia infection among community members, saying that most of them did not know about the signs and symptoms.
“I thought it is a disease that affects children, that’s why I wanted to know more about it and get the drugs so that my kid will not be affected” (KII parent, Kwale).
“In real sense I cannot explain much because I don’t know much about the disease” (KII, parent Kwale).
“What I know is that the community has a lot of problems in terms of knowledge of bilharzia. Most people do not know the signs and symptoms of the disease. They know that when urine has traces of blood is when they assume to be having bilharzia, but what I know is that bilharzia can be transmitted through the foot when somebody steps on water infested with snails” (Male FGD, Homa Bay).
Gender and age at risk of getting infected by bilharzia
When asked which gender and age were most at risk of getting infected by bilharzia, those participants who had heard about bilharzia felt that everyone, including children aged above five years, were at risk of getting infected if they came into contact with infested waters. Most of the study participants felt that children and women were at higher risk of becoming infected than men. The reasons given included children swimming in water bodies infested with bilharzia. This notwithstanding, a couple of the parents/guardians felt that men are also prone to infection since they like bathing in the rivers. Below are some statements from the study participants.
“It cuts across all ages. It does not choose so long as you are exposed to the causative agents” (Male FGD Homa Bay).
“I would say the disease affects mostly women and children, because children above five years of age play and swims in water and women who do their washing in water, may get these parasites in the water” (Female FGD Homa Bay).
However, not all respondents felt that women are more at risk than men, like a female parent from Kwale study site who reported that the male gender is also at risk of getting infected because they like bathing in the rivers.
“The male gender is mostly affected by bilharzia because men are notorious. They have a habit of bathing and even swimming in the rivers where they can easily get bilharzia if the parasite is in the water” (Female FGD, Kwale).
Nevertheless, there was a diversity of knowledge among the parents/guardians of PSAC in both counties about the disease infecting children below five years. In each site, there were a couple parents/guardians who had not heard of the disease infects children below five years of age while others felt they are not infected, probably because it is a disease associated with contact with bilharzia infested water bodies, considering that this age group is rarely allowed to play/swim in the water for safety reasons.
“It affects children from two years and above, for the children below two years they are not easy to be infected by the disease since the mode of play is totally different from the others” (Female FGD Kwale).
“I have never heard about this disease in children between 1–5 years” (KII parent, Homa Bay).
Signs and symptoms of bilharzia
The majority of the study participants knew the signs and symptoms of bilharzia infection. Some of the mentioned symptoms were blood in urine, abdominal pain, blood in stool, diarrhoea, stomach-ache, pain while passing urine, loss of body weight, pale skin, itchiness, irritation at the time of urinating and general body weakness.
“I would say urinating blood, you feel much pain when urinating (Male FGD, Homa Bay).
“As the name suggests, “Alaa Remo”: presence of blood both in stool and urine” (KII Opinion Leader, Homa Bay).
“The child feels itchy in the private parts before urinating and he also feels much pain” (Female FGD, Kwale).
Perception about bilharzia infection
When asked how they perceived the parasitic disease, the parents/guardians in each site who had heard about it, felt that it is a bad and a serious disease which scares people. Male opinion leaders from Homa Bay County felt that the parasitic disease should be given priority in treatment and control, as they believed that it causes a person to lose blood.
“Bilharzia is a bad disease. People take it seriously because if you are urinating blood, do you know where the blood is coming from? So, it’s a must you get help by seeking treatment quickly so that the situation goes away” (KII parent, Kwale).
“The community members perceive the disease to be very dangerous therefore they try their best to take care of their children” (KII parent, Kwale).
“Bilharzia should also be considered among serious diseases such as malaria. It should also be given same priority along the lake region” (KII opinion leader, Homa Bay).
On the contrary, a few parents/guardians drawn from the FGD category we interviewed in Homa Bay County indicated that the disease was viewed like any other disease, and it was common to be infected and urinate blood especially in children.
“I really can’t tell what causes the disease since even our grandfathers had it … it is normal for us to see someone urinate blood” (Male FGD, Homa Bay).
“I think our community views it like any other normal disease because you find a person with the disease going to a traditional healer for herbs claiming something is eating their stomach. So, I feel our community members view it as any other disease that anyone can get, and I don’t see them giving it some special attention” (Female FGD, Homa Bay).
Misinformation on bilharzia transmission
It was evident that a few of the respondents had misinformation on how the disease is transmitted. Some of these included consuming too much sugar, drinking dirty water, drinking water that an infected person has urinated in, playing in murky water and eating cold and undercooked food.
“What I know is that bilharzia is brought about by drinking dirty water. Considering that we don’t always treat water, our children might drink this water and get bilharzia” (Female FGD, Homa Bay).
“When an infected person urinates in water then a healthy person drinks the same water from the lake, they get infected by bilharzia. Also, when an infected person defecates in the water and then there is some water splashing back to skin they too get infected” (Female FGD, Homa Bay).
“When I was a little boy, I liked eating sugar, but my grandmother told me not to do this because my uncle used to consume too much sugar. I followed him and saw him urinate blood” (Male FGD, Kwale).
Transmission of bilharzia
It was clear that apart from the few misinformation about the disease transmission reported, majority of the study participants had knowledge on how bilharzia is transmitted. Many of the participants reported that the disease is transmitted through having contact with bilharzia infested water. However, a handful of participants felt that some community members might not be knowledgeable about the disease transmission.
“During my childhood when I was in school, our teacher used to tell us not to play in dirty water because that is where students get bilharzia from. And indeed, most of us who used to play in the contaminated water used to urinate blood” (Male FGD, Kwale).
“We know that bilharzia penetrates through the feet, by stepping in water, one may contract this disease, or you can step in the water but you do not contracting this disease. People should be warned not to urinate inside the water be it in the lake or river. Bilharzia has a cycle it follows, from the snail until it infects us” (Female FGD, Kwale).
“The community members do not know how this disease is transmitted from one person to another. So, if they can know how it is transmitted, they can easily see a way of preventing it” (Female FGD, Kwale).
Myths and misconceptions about bilharzia infection
Some of the parents/guardians of PSAC in both counties considered bilharzia to be a sexually transmitted infection (STI), and that they would not like to be associated with it. They mentioned that it felt like a curse and humiliation for adults to be found infected with the disease which could expose them as being promiscuous. Indeed, they feared being stigmatised by the community if diagnosed with the disease and would rather seek treatment from native doctors or traditional healers rather than from conventional medicine. On the same note, two male participants said that they would like to be taught the difference between bilharzia and syphilis since they present with similar symptoms of bloody urine and lower abdominal pain, as opined below.
“We are afraid of going to the hospital and being found with the disease upon testing that you have it, you get stigmatised” (Male FGD, Homa Bay).
“Our people believe that it’s like a trap, a curse to adult people but not to children. For us, it is a children’s disease, and we will take them to the hospital. But for the adults, they will run to witchdoctors to seek traditional/herbal medicines locally known as miti shamba” (FGD female participant, Kwale).
“We also have syphilis that also presents with blood in urine and you can have lower abdominal pain and puss in the urine. Bilharzia also comes with the same symptoms, but you now urinate blood and not puss. So, we would wish to know clarity on the two” (Male FGD Homa Bay).
Prevention of schistosomiasis/bilharzia
Study participants suggested methods of disease prevention include wearing shoes, seeking treatment at health facilities, controlling snails, health promotion on the importance of proper human waste disposal, and owning and utilising toilets.
“Some of the ways of preventing bilharzia infection are like wearing shoes, boiling drinking water and provision of treatment centres when one is diagnosed with the disease” (KII opinion leader, Homa Bay).
“Other than controlling the snails, draining of stagnant water also helps in controlling other vectors like mosquito. In addition, the snails can be removed physically from the water” (Male, FGD Homa Bay).
“I think supporting the community members in latrine construction can be another way. We can also encourage and motivate people to have latrines” (KII opinion leader, Kwale).
Practices that promote continued schistosomiasis infection
The study participants felt that there are practices that promote continued infection with bilharzia like poor human waste disposal and open defecation. The reason mentioned for not owning and using toilets by majority of the opinion leaders in Homa Bay County were poor soil type that affects the construction of pit latrines. While for participants in Kwale County, cultural beliefs and practices were mentioned as a major hindrance towards owning and utilising a pit latrine. The participants indicated that their cultural beliefs do not allow certain household members to share a toilet like a father and his daughter in-law.
“Disposal of human waste is not properly managed because most of us don’t have toilets and if we build toilets, they easily collapse because of the type of soil in this area. The church only has one toilet that the villagers use to relieve themselves, but their preferred places are the bushes and gardens” (KII Opinion leader Homa Bay).
“Some people here still do not have latrines. There is a cultural belief that defecating in an enclosed toilet is like defecating inside the house, so some people choose to defecate in the open instead” (KII opinion leader Kwale).
“Some of the community members refuse to adhere to the preventive guidelines given. Some refuse to construct latrines to ensure human waste is disposed properly. Community cultural beliefs that one cannot use the same toilet with his daughters-in-law have also contributed in people refusing to use latrines” (KII, opinion leader, Kwale).
Willingness of the community to participate in treatment programme
Community members expressed their willingness to participate in the upcoming treatment pilot roll-out of the new drug if proper sensitisation and awareness is done.
“I would like to participate because my children participated in the previous mass drug administration, and I did not see any side effects in them” (KII, opinion leader, Kwale).
“As long as you explain to them the benefit of the drug, mothers who have children 1–5years will allow their children to take the drug and also the work of CHVs will be made easier since the parents will be aware of the drug given to their children and the benefit of that drug” (KII, opinion leader, Homabay).
Reasons for hesitancy
A few of the participants were reluctant for their children to participate in the planned pilot roll-out stating that the PSAC children are being given many drugs, religious/cultural beliefs, and lack of food to be eaten by the children before taking the drugs.
“I have never taken a polio vaccine in my lifetime and I am okay, why do you give these young children too many drugs, yet they are not sick. During our time, the children were left to develop their own immunity against diseases … nowadays its polio … malaria … etc.” (KII, Parent PSAC, Kwale).
“Some churches do not allow their members to take drugs due to their doctrines” (KII, Religious leader, Homabay).
“Some people refuse to take the drugs because of their cultural beliefs, they claim that such programmes are associated with devil worshiping” (KII, Parent, Kwale).
Recommendation given to improve the uptake of the medicine
Study participants recommended on the importance of involving and educating the parents/guardians of PSAC and all the relevant stakeholders in order to increase the uptake of the medicine in the planned pilot roll -out. Other recommendations given were that proper planning and involvement of local administrative structures.
“If proper mobilization and sensitisation is done, then we will have a good turn up. This mobilization should not be a one-day thing, it should be for some weeks. Using door to door approach and gatherings” (KII, opinion leader, Homa Bay)
“It is good to educate the parents on the side effects. I once saw a child collapse because they were given the deworming drugs in school with the parents knowing” (KII, opinion leader Homa Bay).
“Proper planning and active involvement of local structures such as chiefs, elders and religious leaders so that they can organize on the best place the activity can take place” (KII, opinion leader, Kwale).
Discussion
This study used qualitative methods to assess community knowledge and perceptions of schistosomiasis in preparation of the planned pilot MDA of the novel child friendly treatment. Immense efforts are being made by the MOH in prevention and control of morbidity caused by schistosomiasis. However, it is important to note that the perceptions and practices of the communities play a major role in the uptake and sustainable control of interventions.
Knowledge of schistosomiasis
Our results show that community members know about schistosomiasis, which is commonly referred to as bilharzia, as a disease that leads to bloody stool and haematuria. However, a minority of the parents/guardians we interviewed indicated that they had not heard about the disease. A similar study done elsewhere in Kenya has shown that there was moderate knowledge about schistosomiasis among community members (11). Another study done in Philippines by Inobaya et al., 2018 showed that community members had poor awareness of the signs and symptoms of schistosomiasis, disease prevention, and available treatment options (29). For improved prevention and control, it would be good for the concerned health ministries and NTD programmes to include health promotion packages in the ongoing community strategy MDAs for effective outcomes, as the country moves towards elimination of schistosomiasis or the interruption of transmission.
Schistosomiasis transmission, myths and misconceptions
Most of the community members had knowledge on disease transmission, which they said it was through having contact with bilharzia infested freshwater bodies while bathing in the rivers or doing domestic chores. Nevertheless, some community members had misconceptions and were misinformed about the transmission of the disease. Some of the misconceptions and misinformation were that schistosomiasis is acquired by eating sugar, drinking or eating contaminated food and water. Previous studies have also found similar results (30, 31). People also believe that bilharzia is transmitted through sexual contact probably because of blood in urine for S. haematobium specifically which also causes genital ulcers in both males and females or they may have heard the association between genital schistosomiasis and STI, HIV (human immunodeficiency virus) in particular (32, 33). Previous studies done in Western Kenya and Mozambique have also shown that community members confuse bilharzia infection with STI (11, 30, 31). Hence, there is need for continued health education to the community members on the disease transmission for effective control.
This notwithstanding, it was perceived normal for children to be infected with bilharzia and urinate blood, but a curse when adults are infected since it exposes those who are promiscuous and have extramarital affairs (34, 35). Similar studies have shown that community members may not seek treatment for bilharzia since it is sometimes confused as being an STI and brings stigma to those infected and fear of their partners (36–38). In this study, community members indicated that for the above reasons, they would not seek healthcare services through conventional treatment but rather go to a traditional healer for fear of stigmatization. Studies by Kabeterine et al., 2014 and Acka et al., 2010 have shown that schistosomiasis health seeking behaviour was poor among fisher folk and this could be influenced by several factors, such as perceived seriousness of the disease (12, 13). It is worth to note that a few studies have conducted research on schistosomiasis treatment using herbal medication in communities where the disease is prevalent. However, it is not yet scientifically proven whether the herbs can treat the parasitic disease, which can be a cause for concern due to continued transmission and hindering control efforts (39–41). Similar studies have shown that social and cultural factors are important in schistosomiasis control by focal communities because they are a source of myths and misconceptions about the disease (36, 42). This calls for enhanced awareness creation from the relevant ministries in order to educate the communities on the signs and symptoms, risks of acquiring the disease and the need for seeking treatment once infected, for effective control efforts.
Practices
In the current study, children and women were mentioned to be at high risk of infection with schistosomiasis because of their water contact practices as a result of their play habits and doing domestic chores, respectively. In addition, poor human waste disposal because of lack of access and use of toilets due to cultural practices and poor soil types were also mentioned as contributors to continued transmission of the disease. Similar studies conducted elsewhere have shown poor human waste disposal to be contributing to infection with schistosomiasis (43–45). Hence the need for continued sensitisation of community members on the importance of owning and utilising toilets to influence their practices in prevention and control. Understanding community perceptions of disease along with the enablers and barriers to risk reduction behaviours can inform health promotion activities, and programmes for prevention and control of schistosomiasis (46).
Willingness to participate in the upcoming pilot roll-out
Most of the community members including parents/guardians of PSAC indicated that they will be willing to allow their children to participate in the planned pilot roll-out of the new drug since the drug will benefit their children. However, they suggested the need for awareness creation and sensitisation before the pilot roll-out. A similar study conducted by Roll et al., 2022, in Benin, Malawi and India with policy stakeholders in preparation for community MDA on helminths, indicated that the effective launch with high coverage relies on community sensitisation that dispels rumours, addresses myths, and mobilizes community members through training and education. The study also indicated that without proper sensitisation, community MDA could fail to achieve the coverage needed to stop helminths transmission, potentially delegitimizing the programme early in its implementation (47).
Reasons for hesitancy and community recommendations to the programme
A few of the study participants indicated that they would be hesitant to allow their children to take the drugs to fear of the unknown and possible side effects. A study conducted by Carlos et al., 2021 showed that uptake of most schistosomiasis related MDAs in Sub-Saharan Africa are influenced by several factors which include; knowledge and attitudes towards schistosomiasis and MDAs, fears of side effects, gender values, community and health systems support, alongside programme design features like training, sensitisation, and provision of incentives for drug-distributors among others (48). Community members gave suggestions on how they felt the programme can effectively implement the pilot roll-out. Some of the suggestions given were adequate awareness creation, involvement of the local leadership structures and give incentives to those who will be actively involved in the programme. A study done in Uganda by Parker and Tim 2011 found that there are specific reasons why MDA succeeds in some areas or locations and falters in others relates to local dynamics such as changing food supply, relations between drug distributors and targeted groups, rumours and conspiracy theories about the real purpose of treatment, subjective experiences of side effects from previous treatment among others (49). The current study suggests the need to adapt to the local circumstances and ensure adequate health education, good training to all those who will be involved while incorporating exiting public health legislative.
Study limitation
There may have been responses bias during IDIs and FGDs as study participants may have provided answers that they believed the interviewers expected or wanted to hear, and observations were not carried out to substantiate the interviews. Additionally, bias may have been introduced due to only having a single coder during analysis and data interpretations by the study team even though language translations were substantiated with local research assistants.
Conclusion
Community members know and perceive schistosomiasis to be a serious disease, but there are gaps about its causes. In addition, some of the practices such as water contact and human waste disposal contribute to continued transmission. This study recommends increased knowledge through awareness creation to change the perceptions of communities in relation to schistosomiasis prevention and control. This can be done through contextual health promotion activities encouraging behavioural change. This notwithstanding, studies focusing on schistosomiasis among PSAC should not overlook the role which can be played by parents/guardian in protecting children from infection if they are adequately empowered to do so. The study emphasises the need to prioritise health promotion regarding communities’ perception about the disease transmission and the long-term effects in advance of medication roll-out.
Data availability statement
The datasets presented in this article are not readily available because: All data for this paper are within the manuscript. Requests to access the datasets should be directed toam1hc2FrdUBrZW1yaS5nby5rZQ==.
Ethics statement
The studies involving humans were approved by the Kenya Medical Research Institute (KEMRI), Scientific and Ethics Review Unit (SERU No. 4992) and the Ethical Committee at the Technical University of Munich (TUM) (731/21 S). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing, Funding acquisition, Resources. JG: Data curation, Investigation, Methodology, Supervision, Validation, Visualization, Writing – review & editing, Conceptualization. AS: Conceptualization, Data curation, Investigation, Methodology, Project administration, Software, Supervision, Validation, Writing – review & editing, Resources. MM: Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Writing – review & editing. FW: Investigation, Methodology, Resources, Supervision, Validation, Writing – review & editing, Conceptualization, Funding acquisition, Project administration. WO: Conceptualization, Funding acquisition, Investigation, Resources, Supervision, Validation, Visualization, Writing – review & editing, Project administration. LR: Conceptualization, Data curation, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing, Resources. IL: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing. AW: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Supervision, Validation, Visualization, Writing – review & editing. SN: Conceptualization, Funding acquisition, Investigation, Methodology, Resources, Supervision, Validation, Writing – review & editing, Project administration, Visualization. MA-N: Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study received funding from Merck KGaA, Darmstadt, Germany (RIA2019IR-2895); https://www.edctp.org/. The funders had no role in the study design, data collection and analysis, preparation of the manuscript or the decision to publish.
Acknowledgments
We are grateful to the communities of Homa Bay and Kwale Counties for participation in the study. We also express appreciation to the respective County governments, especially the Directors of Health for their support in conducting the study. Special thanks to all the Public Health Officers (PHOs) and County NTD coordinators in the two counties for their effort in supporting data collection. In addition, we are grateful to the research assistants for the hard work and commitment during the data collection period. Finally, thank you to the entire research team for coordinating study implementation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
PSAC, Pre-School-Age Children; NTDs, Neglected Tropical Diseases; PZQ, Praziquantel; WHO, World Health Organization; MDA, Mass Drug Administration; MoH, Ministry of Health; CHVs, Community Health Volunteers; FGDs, Focus Group Discussions; KIIs, Key Informant Interviews; SERU, Scientific and Ethics Review Unit; ESACIPAC, Eastern and Southern Africa Centre of International Parasite Control; KEMRI, Kenya Medical Research Institute; JKUAT, Jomo Kenyatta University of Agriculture and Technology; AIHD, African Institute for Health and Development; DVB/NTDs, Division of Vector Borne and Neglected Tropical Diseases; TUM, Technical University of Munich.
References
1. Hotez PJ, Alvarado M, Basáñez MG, Bolliger I, Bourne R, Boussinesq M, et al. The global burden of disease study 2010: interpretation and implications for the neglected tropical diseases. PloS Negl Trop Dis. (2014) 8(7):e2865. doi: 10.1371/journal.pntd.0002496
2. Brooker S, Kabatereine NB, Gyapong JO, Stothard JR, Utzinger J. Rapid mapping of schistosomiasis and other neglected tropical diseases in the context of integrated control programmes in Africa. Parasitology. (2009) 136:1707–18. doi: 10.1017/S0031182009005940
3. Colley DG. Morbidity control of schistosomiasis by mass drug administration: how can we do it best and what will it take to move on to elimination? Trop Med Health. (2014) 42:S25–32. doi: 10.2149/TMH.2014-S04
4. Colley DG, Bustinduy AL, Secor WE, King CH. Human schistosomiasis. Lancet. (2014) 383:2253–64. doi: 10.1016/S0140-6736(13)61949-2
5. Vos T, Flaxman A, Naghavi M, Lozano R, lancet CM-T. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010 (2012). Elsevier. Available online at: https://www.sciencedirect.com/science/article/pii/S0140673612617292 (Accessed 3 Feb 2022).
6. WHO.Working to Overcome the Global Impact of Neglected Tropical Diseases Annexe I First WHO report on neglected tropical diseasesMeissner WHO, Denis (2010). Geneva, Switzerland. Available online at: https://apps.who.int/iris/bitstream/handle/10665/44440/9789241564090_eng.pdf;jsessionid=5B765050D323372A1FAEBCD5E8D81762?sequence=1 (Accessed 24 Jun 2019).
7. Waite RC, Velleman Y, Woods G, Chitty A, Freeman MC. Integration of water, sanitation and hygiene for the control of neglected tropical diseases: A review of progress and the way forward. Int Health. (2015) 8:i22–7. doi: 10.1093/inthealth/ihw003
8. Mwandawiro C, Okoyo C, Kihara J, Simiyu E, Kepha S, Campbell SJ, et al. Results of a national school-based deworming programme on soil-transmitted helminths infections and schistosomiasis in Kenya: 2012–2017. Parasites Vectors. (2019) 12:76. doi: 10.1186/s13071–019-3322–1
9. Sady H, Al-Mekhlafi HM, Atroosh WM, Al-Delaimy AK, Nasr NA, Dawaki S, et al. Knowledge, attitude, and practices towards schistosomiasis among rural population in Yemen. Parasites Vectors. (2015) 8:1–13. doi: 10.1186/s13071-015-1050-8
10. Maseko TSB, Mkhonta NR, Masuku SKS, Dlamini SV, Fan CK. Schistosomiasis knowledge, attitude, practices, and associated factors among primary school children in the Siphofaneni area in the Lowveld of Swaziland. J Microbiol Immunol Infect. (2018) 51:103–9. doi: 10.1016/j.jmii.2015.12.003
11. Masaku J, Mwende F, Odhiambo G, Musuva R, Matey E, Kihara JH, et al. Knowledge, practices and perceptions of geo-helminthes infection among parents of pre-school age children of coastal region, Kenya. Glob Heal Res. (2017) 11(3): e0005514. doi: 10.1371/journal.pntd.0005514
12. Kabatereine N, Fleming F, Thuo W, Tinkitina B, Tukahebwa EM, Fenwick A. Community perceptions, attitude, practices and treatment seeking behaviour for schistosomiasis in L. Victoria islands Uganda. BMC Res Notes. (2014) 7:900. doi: 10.1186/1756–0500-7–900
13. Acka CA, Raso G, N’Goran EK, Tschannen AB, Bogoch II, Séraphin E, et al. Parasitic worms: knowledge, attitudes, and practices in western côte d’Ivoire with implications for integrated control. PloS Negl Trop Dis. (2010) 4:e910. doi: 10.1371/JOURNAL.PNTD.0000910
14. Sousa-Figueiredo JC, Betson M, Atuhaire A, Arinaitwe M, Navaratnam AMD, Kabatereine NB, et al. Performance and safety of praziquantel for treatment of intestinal schistosomiasis in infants and preschool children. PloS Negl Trop Dis. (2012) 6:e1864. doi: 10.1371/JOURNAL.PNTD.0001864
15. Stothard JR, Sousa-Figueiredo JC, Betson M, Green HK, Seto EYW, Garba A, et al. Closing the praziquantel treatment gap: new steps in epidemiological monitoring and control of schistosomiasis in African infants and preschool-aged children. Parasitology. (2011) 138:1593–606. doi: 10.1017/S0031182011001235
16. Stothard JR, Sousa-Figueiredo JC, Betson M, Bustinduy A, Reinhard-Rupp J. Schistosomiasis in African infants and preschool children: Let them now be treated! Trends Parasitol. (2013) 29:197–205. doi: 10.1016/j.pt.2013.02.001
17. Nalugwa A, Nuwaha F, Tukahebwa EM, Olsen A. Single versus double dose praziquantel comparison on efficacy and schistosoma mansoni re-infection in preschool-age children in Uganda: A randomized controlled trial. PloS Negl Trop Dis. (2015) 9:e0003796. doi: 10.1371/JOURNAL.PNTD.0003796
18. World Heath Organization. REPORT OF A MEETING TO REVIEW THE RESULTS OF STUDIES ON THE TREATMENT OF SCHISTOSOMIASIS IN PRESCHOOL-AGE CHILDREN (2010). Available online at: http://www.who.int/neglected_diseases/en (Accessed 17 Mar 2021).
19. Coulibaly JT, N’Gbesso YK, Knopp S, Keiser J, N’Goran EK, Utzinger J. Efficacy and safety of praziquantel in preschool-aged children in an area co-endemic for schistosoma mansoni and S. haematobium. PloS Negl Trop Dis. (2012) 6:e1917. doi: 10.1371/journal.pntd.0001917
20. Abdel-Rahman SM, Ridgen A, Kearnsn GL. Estimation of body weight in children in the absence of scales: a necessary measurement to insure accurate drug dosing. Arch Dis Child. (2014) 99:570–4. doi: 10.1136/ARCHDISCHILD-2013–305211
21. Richey RH, Hughes C, Craig JV, Shah UU, Ford JL, Barker CE, et al. A systematic review of the use of dosage form manipulation to obtain required doses to inform use of manipulation in paediatric practice. Int J Pharm. (2017) 518:155–66. doi: 10.1016/j.ijpharm.2016.12.032
22. N’Goran EK, Odiere MR, Assandé Aka R, Ouattara M, Aka NAD, Ogutu B, et al. Efficacy, safety, and palatability of arpraziquantel (L-praziquantel) orodispersible tablets in children aged 3 months to 6 years infected with Schistosoma in Côte d’Ivoire and Kenya: an open-label, partly randomised, phase 3 trial. Lancet Infect Dis. (2023) 23:867–76. doi: 10.1016/S1473–3099(23)00048–8
23. Kabatereine NB, Malecela M, Lado M, Zaramba S, Amiel O, Kolaczinski JH. How to (or not to) integrate vertical programmes for the control of major neglected tropical diseases in Sub-Saharan Africa. PloS Negl Trop Dis. (2010) 4(6): e755. doi: 10.1371/journal.pntd.0000755
24. Tchuem Tchuenté LA, Rollinson D, Stothard JR, Molyneux D. Moving from control to elimination of schistosomiasis in sub-Saharan Africa: Time to change and adapt strategies. Infect Dis Poverty. (2017) 6: 1–101. doi: 10.1186/s40249-017-0256-8
25. Odiere MR, Rawago FO, Ombok M, Secor WE, Karanja DM, Mwinzi PN, et al. High prevalence of schistosomiasis in Mbita and its adjacent islands of Lake Victoria, western Kenya. Parasites & Vectors. (2012) 5, 278. doi: 10.1186/1756–3305-5–278
26. Kenya National Bureu of statisticics. 2019 Kenya Population and Housing Census Reports (2019). Available online at: https://housingfinanceafrica.org/documents/2019-Kenya-population-and-housing-census-reports/ (Accessed 25 Jan 2022).
27. Onwuegbuzie AJ, et al. Toward a Broader Understanding of Stress and Coping: Mixed Methods Approaches - Google Books (2010). Information Age Publishing. Available online at: https://books.google.co.ke/books?hl=en&lr=&id=2vcnDwAAQBAJ&oi=fnd&pg=PA243&dq=24.%09Onwuegbuzie+AJ,+Dickinson+WB,+Leech+NL+and+Zoran+AG+(2010a).+Towards+more+rigor+in+focus+group+research+in+stress+and+coping+and+beyond:+A+new+mixed+research+framework+for (Accessed 7 Nov 2022).
28. Onwuegbuzie A, WD-T a broader. Toward more rigor in focus group research in stress and coping and beyond (2010). Available online at: https://books.google.com/books?hl=en&lr=&id=2vcnDwAAQBAJ&oi=fnd&pg=PA243&dq=Onwuegbuzie+AJ,+Dickinson+WB,+Leech+NL+and+Zoran+AG.+Towards+more+rigor+in+focus+group+research+in+stress+and+coping+and+beyond:+A+new+mixed+research+framework+for+collecting+and+analyzing+focus+group+data.+Charlotte,+NC:+Information+Age+Publishing.+2010a%3B&ots=FYJLifkHvF&sig=Dq3DFX_pbI86lh05eggFAoloiGo (Accessed 19 Jul 2022).
29. Inobaya MT, Chau TN, Ng S-K, Macdougall C, Olveda RM, Tallo VL, et al. Mass drug administration and the sustainable control of schistosomiasis: Community health workers are vital for global elimination efforts. Int J Infect Dis (2017) 66, 14–21. doi: 10.1016/j.ijid.2017.10.023
30. Musuva RM, Awiti A, Omedo M, Ogutu M, Secor WE, Montgomery SP, et al. Community knowledge, attitudes and practices on schistosomiasis in western Kenya-the SCORE project. Am J Trop Med Hyg. (2014) 90:646–52. doi: 10.4269/ajtmh.13-0488
31. Rassi Id C, Martin S, Graham K, Anna De Cola Id M, Christiansen-Jucht C, Smith Id LE, et al. Knowledge, attitudes and practices with regard to schistosomiasis prevention and control: Two cross-sectional household surveys before and after a Community Dialogue intervention in Nampula province, Mozambique. PLoS ONE (2019) 16(8): e0255647. doi: 10.1371/journal.pone.0255647
32. Patel P, Rose CE, Kjetland EF, Downs JA, Mbabazi PS, Sabin K, et al. Association of schistosomiasis and HIV infections: A systematic review and meta-analysis. Int J Infect Dis. (2021) 102:544–53. doi: 10.1016/j.ijid.2020.10.088
33. Bustinduy AL, Randriansolo B, Sturt AS, Kayuni SA, Leustcher PDC, Webster BL, et al. An update on female and male genital schistosomiasis and a call to integrate efforts to escalate diagnosis, treatment and awareness in endemic and non-endemic settings: The time is now. Adv Parasitol. (2022) 115:1–44. doi: 10.1016/bs.apar.2021.12.003
34. Mbabazi PS, Andan O, Fitzgerald DW, Chitsulo L, Engels D, Downs JA. Examining the relationship between urogenital schistosomiasis and hiv infection. PloS Negl Trop Dis. (2011) 5(12): e1396. doi: 10.1371/journal.pntd.0001396
35. Kjetland EF, Hegertun IE, Baay MF, Onsrud M, Ndhlovu PD, Taylor M. Genital schistosomiasis and its unacknowledged role on HIV transmission in the STD intervention studies. Int J STD AIDS. (2014) 25:705–15. doi: 10.1177/0956462414523743
36. Dawaki S, Al-Mekhlafi HM, Ithoi I, Ibrahim J, Abdulsalam AM, Ahmed A, et al. The menace of schistosomiasis in Nigeria: knowledge, attitude, and practices regarding schistosomiasis among rural communities in kano state. PLoS ONE (2015) 10(11): e0143667. doi: 10.1371/journal.pone.0143667
37. Masaku J, Mwende F, Odhiambo G, Musuva R, Matey E, Kihara JH, et al. Knowledge, practices and perceptions of geo-helminthes infection among parents of pre-school age children of coastal region, Kenya. PloS Negl Trop Dis. (2017) 11:e0005514. doi: 10.1371/journal.pntd.0005514
38. Musuva RM, Matey E, Masaku J, Odhiambo G, Mwende F, Thuita I, et al. Lessons from implementing mass drug administration for soil transmitted helminths among pre-school aged children during school based deworming program at the Kenyan coast. BMC Public Health. (2017) 17:575. doi: 10.1186/s12889–017-4481–7
39. Ndegwa FK, Kondam C, Aboagye SY, Esan TE, Waxali ZS, Miller ME, et al. Traditional Kenyan herbal medicine: exploring natural products’ therapeutics against schistosomiasis. J Helminthol. (2022) 96:e16. doi: 10.1017/S0022149X22000074
40. Anibogwu R, De Jesus K, Pradhan S, Pashikanti S, Mateen S, Sharma K. Extraction, isolation and characterization of bioactive compounds from Artemisia and their biological significance: a review. Molecules. (2021) 26:6995. doi: 10.3390/molecules26226995
41. Williams DL, Hagen TJ, Ndegwa FK, Kondam C, Aboagye SY, Esan TE, et al. Traditional Kenyan herbal medicine: exploring natural products’ therapeutics against schistosomiasis. J Helminthol. (2022) 96:e16. doi: 10.1017/S0022149X22000074
42. Dejon-Agobé JC, Zinsou JF, Honkpehedji YJ, Edoa JR, Adegbité BR, Beh-Mba R, et al. Knowledge, attitudes and practices pertaining to urogenital schistosomiasis in Lambaréné and surrounding areas, Gabon. Parasites Vectors. (2021) 14:1–12. doi: 10.1186/S13071–021-04905–0/TABLES/5
43. Njambi E, Magu D, Masaku J, Okoyo C, Njenga SM. Prevalence of intestinal parasitic infections and associated water, sanitation, and hygiene risk factors among school children in mwea irrigation scheme, kirinyaga county, Kenya. J Trop Med. (2020) 2020. doi: 10.1155/2020/3974156
44. Masaku J, Njomo DW, Njoka A, Okoyo C, Mutungi FM, Njenga SM. Soil-transmitted helminths and schistosomiasis among pre-school age children in a rural setting of Busia County, Western Kenya: A cross-sectional study of prevalence, and associated exposures. BMC Public Health. (2020) 20:1–11. doi: 10.1186/s12889-020-08485-z
45. Onasanya A, Bengtson M, Oladepo O, Van Engelen J, Diehl JC. Rethinking the top-down approach to schistosomiasis control and elimination in sub-saharan africa. Front Public Heal. (2021) 9:622809/FULL. doi: 10.3389/fpubh.2021.622809
46. Person B, Ali SM, A’Kadir FM, Ali JN, Mohammed UA, Mohammed KA, et al. Community knowledge, perceptions, and practices associated with urogenital schistosomiasis among school-aged children in zanzibar, united republic of Tanzania. PloS Negl Trop Dis. (2016) 10:e0004814. doi: 10.1371/JOURNAL.PNTD.0004814
47. Roll A, Saxena M, Orlan E, Titus A, Juvekar SK, Gwayi-Chore MC, et al. Policy stakeholder perspectives on barriers and facilitators to launching a community-wide mass drug administration program for soil-transmitted helminths. Glob Heal Res Policy. (2022) 7(47). doi: 10.1186/s41256-022-00281-z
48. Torres-Vitolas CA, Dhanani N, Fleming FM. Factors affecting the uptake of preventive chemotherapy treatment for schistosomiasis in Sub-Saharan Africa: A systematic review. PloS Negl Trop Dis. (2021) 15:e0009017. doi: 10.1371/JOURNAL.PNTD.0009017
Keywords: knowledge, schistosomiasis, preschool-age children (PSAC), praziquantel, paediatric
Citation: Masaku J, Gachohi JM, Sinkeet A, Maghanga M, Wakesho F, Omondi W, Reigl LS, Lange IL, Winkler AS, Njenga SM and Amuyunzu-Nyamongo M (2024) A qualitative assessment of community perceptions and practices towards schistosomiasis prior to introduction of a potential novel treatment option for preschool-age children in Kenya. Front. Trop. Dis 5:1404634. doi: 10.3389/fitd.2024.1404634
Received: 21 March 2024; Accepted: 06 May 2024;
Published: 24 May 2024.
Edited by:
Alfonso J. Rodriguez-Morales, Fundacion Universitaria Autónoma de las Américas, ColombiaReviewed by:
Housseini Dolo, Université des Sciences, des Techniques et des Technologies de Bamako, MaliLisette Van Lieshout, Leiden University Medical Center (LUMC), Netherlands
Copyright © 2024 Masaku, Gachohi, Sinkeet, Maghanga, Wakesho, Omondi, Reigl, Lange, Winkler, Njenga and Amuyunzu-Nyamongo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Janet Masaku, bWJpbnlhbWFzYWt1QGdtYWlsLmNvbQ==; Sm1hc2FrdUBrZW1yaS5nby5rZQ==
 Janet Masaku
Janet Masaku John M. Gachohi
John M. Gachohi Alice Sinkeet5
Alice Sinkeet5 Lisa Sophie Reigl
Lisa Sophie Reigl