- 1South African Field Epidemiology Training Programme, National Institute for Communicable Diseases, Johannesburg, South Africa
- 2School of Public Health, Faculty of Health Sciences, University of Witwatersrand, Johannesburg, South Africa
- 3Centre for Emerging Zoonotic and Parasitic Diseases, National Institute for Communicable Diseases, a Division of the National Health Laboratory Service, Johannesburg, Gauteng, South Africa
- 4Communicable Disease and Control Directorate, KwaZulu-Natal Department of Health, Pietermaritzburg, South Africa
- 5Division of Public Health Surveillance and Response, National Institute for Communicable Diseases, Johannesburg, South Africa
Background: South Africa experiences approximately 10 human rabies deaths annually, despite the availability of effective post-exposure prophylaxis (PEP). In KwaZulu-Natal Province, one of the most rabies-affected provinces, many animal bite patients initially seek help from Traditional Health Practitioners (THPs) before considering conventional healthcare facilities. Prompt referral of animal bite patients for PEP initiation by THPs can be lifesaving. Our study aimed to assess the knowledge, attitudes, and referral practices regarding human rabies and the associated factors among THPs in eThekwini District, KwaZulu-Natal.
Methods: A cross-sectional study was conducted among registered THPs in eThekwini District, collecting data through a structured, standardized questionnaire. The questionnaire was administered through physical and telephone interviews. We described socio-demographic characteristics using summary statistics. Multivariable logistic regression was used to analyze factors associated with knowledge, attitudes, and referral practices. Odds ratios (OR) were used with 95% confidence intervals, and a probability (p)-value of ≤0.05 was considered statistically significant.
Results: The study involved 204 THPs, with 74% (150/204) being female. The median age was 43 years (inter-quartile range: 22–75 years) and 31% (64/204) had over 10 years of practicing experience. The majority of THPs had inadequate knowledge (80%, 163/204), and poor referral practices (73%, 149/204). However, 91% (186/204) had positive attitudes toward human rabies prevention. Having more experience was associated with adequate knowledge (p<0.01), and positive attitudes (p=0.02). THPs who had adequate knowledge (aOR:2.30 95% CI: 1.12-4.75) and positive attitudes (aOR:1.21 95% CI: 0.37-3.89), had higher odds of having good referral practices.
Conclusion: Despite THPs in the eThekwini District having positive attitudes towards rabies prevention, gaps exist in their knowledge and referral practices. The study highlights that improving their knowledge and attitudes might lead to better referral practices of animal bite patients for PEP initiation. A multidisciplinary approach that includes THPs is recommended to decrease human rabies deaths in eThekwini District and KwaZulu-Natal Province.
Introduction
Human rabies is a devastating neglected tropical disease that is reported to kill one person every nine minutes globally (1). The fatal viral infection commonly spreads to humans through contact with the saliva of infected animals (2, 3). Although all mammals can be infected with rabies, over 99% of human cases and deaths in developing countries are dog-mediated (1, 4). Despite being vaccine-preventable, human rabies remains a significant global public health issue, causing around 59–000 deaths annually (1). Approximately 80% of human rabies cases occur in rural areas of developing countries, with 40% of global deaths among children under 15 years old (1, 5). Low and middle-income subtropical African countries are significantly affected by human rabies, accounting for 44% (24 000) of annual global human rabies deaths (1, 6).
Poor preclinical animal bite management and lack of seeking post-exposure prophylaxis (PEP) in South Africa contribute to the ongoing public health issue of human rabies (7–10). Between 2018 and 2021, South Africa recorded 53 laboratory-confirmed human rabies cases (7–9). The majority of these cases were from the KwaZulu-Natal (KZN) Province (46%), followed by the Eastern Cape (37%) and Limpopo (15%) Province (8, 9). Although community rabies awareness and mass dog vaccination campaigns in the KZN Province have helped decrease human rabies cases, the province continues to report a disproportionate number of human rabies cases (11–13). The eThekwini District in KZN has been the primary location for most cases, accounting for 75% of laboratory-confirmed cases in South Africa in 2020 and 62% between January 2020 and July 2021 (7–9).
South Africa is among the member states committed to the goal of eliminating dog-mediated human rabies deaths by 2030, set by the World Health Organization (WHO), the World Organisation for Animal Health (WOAH), and other global partners (14). The strategic elimination plan aims to achieve this by enhancing affordability, access, and timely administration of PEP (1, 14). In exposed individuals, WHO’s preclinical guidelines recommend washing animal bite wounds with running water for 15 minutes, disinfecting with soap or disinfectants, and seeking immediate medical care for PEP (1, 15). Timely and appropriate administration of PEP is almost 100% effective in preventing human rabies mortality (16). Despite the availability of free PEP in South Africa, the country still experiences delays or no PEP initiation and records about 10 human rabies deaths every year (5, 8, 9).
Human rabies case reports in the KZN Province and the eThekwini District show frequent non or late presentation for PEP by animal bite patients (10). Similar to other African countries, animal bite patients especially in rural settings initially seek treatment from Traditional Health Practitioners (THPs) (17–19). They then consider conventional healthcare facilities as their last option, usually presenting with advanced clinical symptoms (18, 19). Seeking health-related care from THPs is one of the most common practices in South Africa and Sub-Saharan Africa (20, 21). Almost 80% of primary healthcare needs in Africa are met through traditional health practices (21). THPs are usually more accessible, less expensive, and trusted, and provide an explanation of the illness in a more relatable way using the local language (15, 17, 18). THPs are crucial in primary healthcare, particularly in rural areas, providing preclinical management, referrals, and rabies education if knowledgeable and willing (20, 22).
THPs in South Africa are recognized as vital stakeholders in primary healthcare and practice under one regulatory body, known as the Traditional Practitioners Council of South Africa (23, 24). The South African government through the National Department of Health (DoH) has also taken great strides in incorporating THPs into the healthcare system to improve healthcare access and resources (24). Local studies revealed their crucial role in managing HIV/AIDS, particularly in rural areas, through patient screening, referral, and education (20).
Formal educational interventions can significantly increase the referral rate between THPs and conventional healthcare facilities, ensuring a viable referral system between the two (25). A similar approach can be taken with human rabies through educating and incorporating THPs into primary healthcare for early PEP access and initiation. However, not much is known about their knowledge, attitudes, and referral practices regarding animal bites and rabies prevention.
There are currently no studies conducted in South Africa that assess the knowledge levels and perceptions of THPs regarding human rabies. Very little is known about how they manage animal bite wounds and if they are willing to refer patients to conventional health facilities for PEP. The study aimed to undertake a knowledge, attitudes, and referral practices (KAP) survey among THPs in eThekwini District. The assessment would help understand the educational needs of local THPs and their willingness to collaborate and refer animal bite patients. Understanding their knowledge levels and awareness will also allow educational interventions to be modified, tailored, and made more effective. A good referral relationship between conventional healthcare facilities and THPs who are knowledgeable on rabies and its prevention might help with early detection and referral of patients for prompt PEP initiation.
Methods
Study design
We conducted a primary study that employed an analytical cross-sectional study design.
Study setting
We conducted the study in eThekwini District, KZN Province, South Africa (Figure 1). KZN is an eastern coastal province with the 2nd biggest population in South Africa (26). It is divided into 11 districts and eThekwini is one of them. The district is roughly divided into four spatial regions (Central, North, South, and West) consisting of rural, semirural, and urban areas (26). The eThekwini District is the most populated in KZN, with an estimated population of 3 987–648 people, composed largely of the Zulu ethnic group (27).
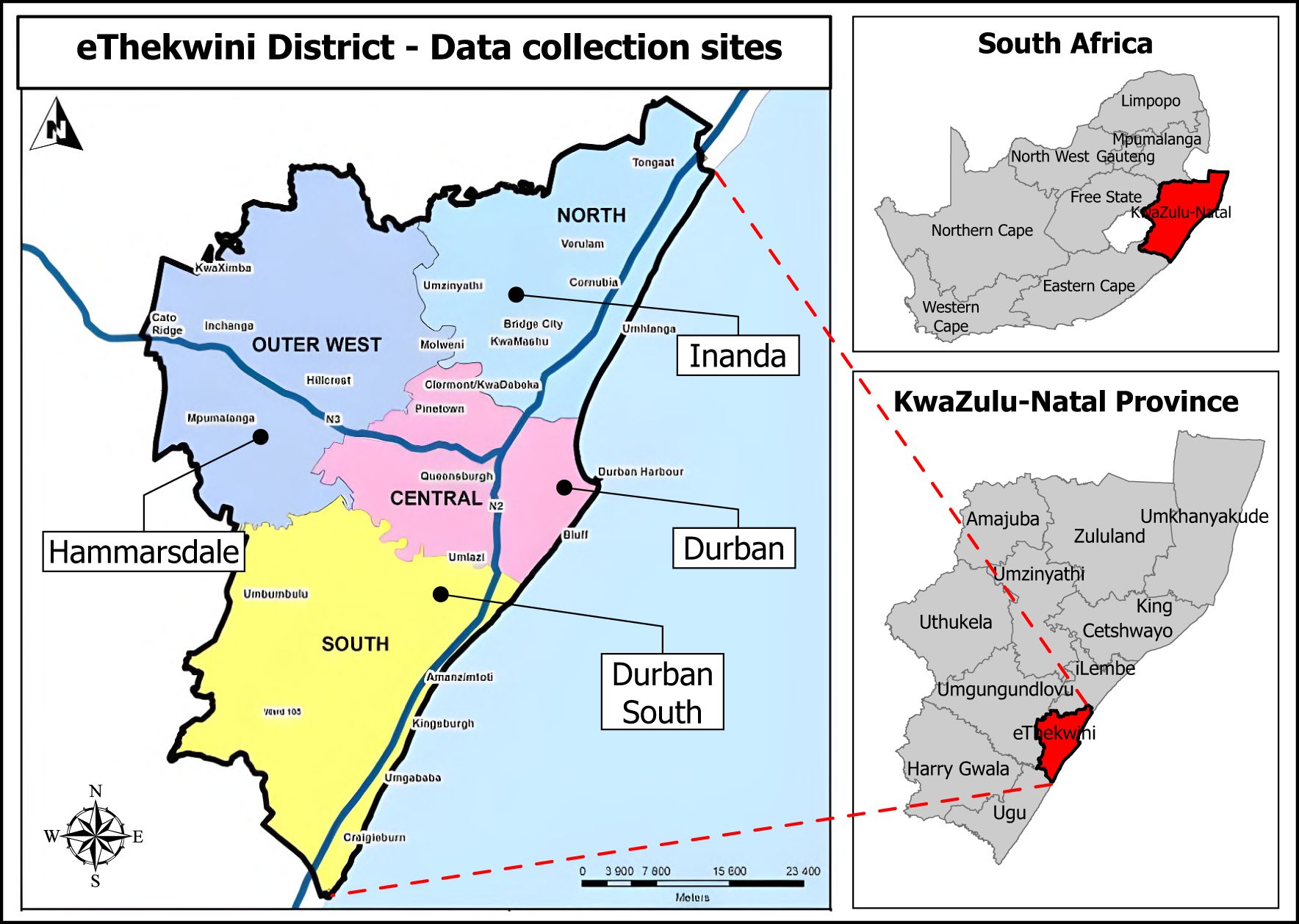
Figure 1. Map of eThekwini District, KwaZulu-Natal Province, South Africa, showing data collection sites where Traditional Health Practitioners gathered for physical interviews.
Study population
The study involved all THPs who consult patients in the eThekwini District, registered on the district’s THP association database. The database had approximately 2–000 registered THPs divided into four categories of practitioners which included herbalists (Izinyanga), diviners (Izangoma), traditional birth attendants (Ababelethisi), and faith healers (Abaprofethi or Abathandazi). All the THPs in the eThekwini’s THP association database were eligible for sampling.
Inclusion and exclusion criteria
The study included consenting THPs aged 18 years and above who were registered under eThekwini’s THPs association. The study also included THPs who are still being trained under experienced supervision (Amathwasa), and consulting patients, while traditional birth attendants (Ababelethisi) were excluded as they do not typically consult animal bite patients.
Sample size
The sample size was estimated by considering 50% of the THP population knowing about rabies since there was no previous study about rabies among THPs in the area. We used eThekwini’s registered THP population (1 500, approximately 500 traditional birth attendants (Ababelethisi) excluded), a 95% confidence interval, and a 5% margin of error to calculate the sample size. Our required minimum sample size was calculated using the modified Cochran’s Formula to be 307 THPs (28). Factoring in for a non-response rate of 20%, the study aimed to interview 384 THPs (Supplementary File 1).
Sampling strategy
Respondents were selected using the convenience sampling method. This was by including all THPs who were available during the data collection period (June to July 2022), and gave consent to respond to the questionnaire to maximize the response rate.
Data collection method
Before signing the consent form (Supplementary File 2), participants were provided and read a study information sheet (Supplementary File 3) to understand the study’s purpose and objectives. We collected data using a structured standardized questionnaire (Supplementary File 4). The questionnaire comprised socio-demographic, knowledge, attitude, and referral practice questions. The questionnaire was adapted from a tool previously used during a THP KAP study on rabies in Ethiopia and modified (29). The Research Electronic Data Capture (REDCap) web application was utilized for developing the questionnaire, collecting and storing data, allowing responses to be collected both online and offline (30). Tablets installed with REDCap were used by the researchers to record participants’ responses.
We administered the questionnaires through physical interviews conducted and led by the researcher. The THPs association assisted in convening data collection gatherings in four different sites in each of the four spatial regions (Figure 1). THPs were invited to the gatherings by THPs from the association responsible for each spatial region. THPs who could not attend the physical data collection gatherings were interviewed by telephone. The questionnaire, consent form, and information sheet were available in isiZulu (the local language) and English to ensure understanding. The isiZulu versions of the documents were validated by an independent isiZulu speaker, reader, and writer from the health department.
Data management and analysis
The responses were reviewed for errors, duplicate entries, and inconsistencies using REDCap’s unique anonymous participant identifiers. We then imported the data from the questionnaires into STATA statistical software (Version 17) for cleaning and analysis. Data cleaning and management on STATA statistical software included creating, labeling, and renaming variables, and looking for and dropping duplicates. We used STATA for data analysis per objective. Firstly, we performed descriptive analysis using summary statistics to describe the socio-demographic characteristics of the THPs.
Secondly, we allocated scores to the answers for the knowledge, attitude, and referral practice (KAP) section of the questionnaire. We calculated the KAP scores by giving a score of “0” for an incorrect and “1” for a correct answer. The highest possible score was 14 for knowledge, five for attitudes, and six for referral practice questions. We only assigned a score to respondents who answered all questions for that section. We used South Africa’s national guidelines for the prevention of rabies in humans to score knowledge, attitude, and referral practice answers as correct or incorrect. The scores were summarized using means with their standard deviations. To create binary variables, KAP scores equal to or above 60% were considered adequate knowledge, positive attitude, and good referral practices and otherwise for those less than 60%.
Thirdly, we categorized and considered the socio-demographic variables as explanatory variables against each of the binary outcomes of knowledge, attitude, and referral practice variables, respectively. The binary knowledge and attitude variables were also used as explanatory variables against the referral practice variable as an outcome. We used Pearson’s chi-square test to assess the association between socio-demographic factors and binary KAP variables. We also used Pearson’s chi-square test to assess for association between the binary knowledge and attitudes variables and the binary outcome of the referral practice variable.
The study employed an automatic backward elimination method to exclude non-significant predictor variables, ensuring only those with a p-value below 0.2 were included in the multivariable analysis. A multivariable logistic regression was conducted on knowledge, attitudes, and referral practices, adjusting for explanatory variables and all other variables simultaneously. Highly correlated variables were not entered in the multivariable model, a variation inflation factor (VIF) of > 10 was used to indicate multicollinearity. Variables with a probability (p)-value of ≤ 0.05 were considered statistically significant in the multivariable analyses. To display results, we used bar graphs and tables. The tables included odds ratios (OR) and adjusted OR, with their corresponding 95% confidence intervals (CI) and p-values.
Results
A total of 204 THPs were interviewed (66% of target sample size). The median age of THPs was 43 years (inter-quartile range (IQR): 22–75 years) and 74% (150/204) were females. The majority of the THPs categorized themselves as Izangoma (Diviners) (51%, 105/204), followed by Izinyanga (Herbalists) (28%, 57/204), and Abaprofethi or Abathandazi (Faith healers) (21%, 42/204). Most (78%, 160/204) of the THP’s practices were located in a rural/semi-rural area (underdeveloped countryside areas away from the city) (Table 1).
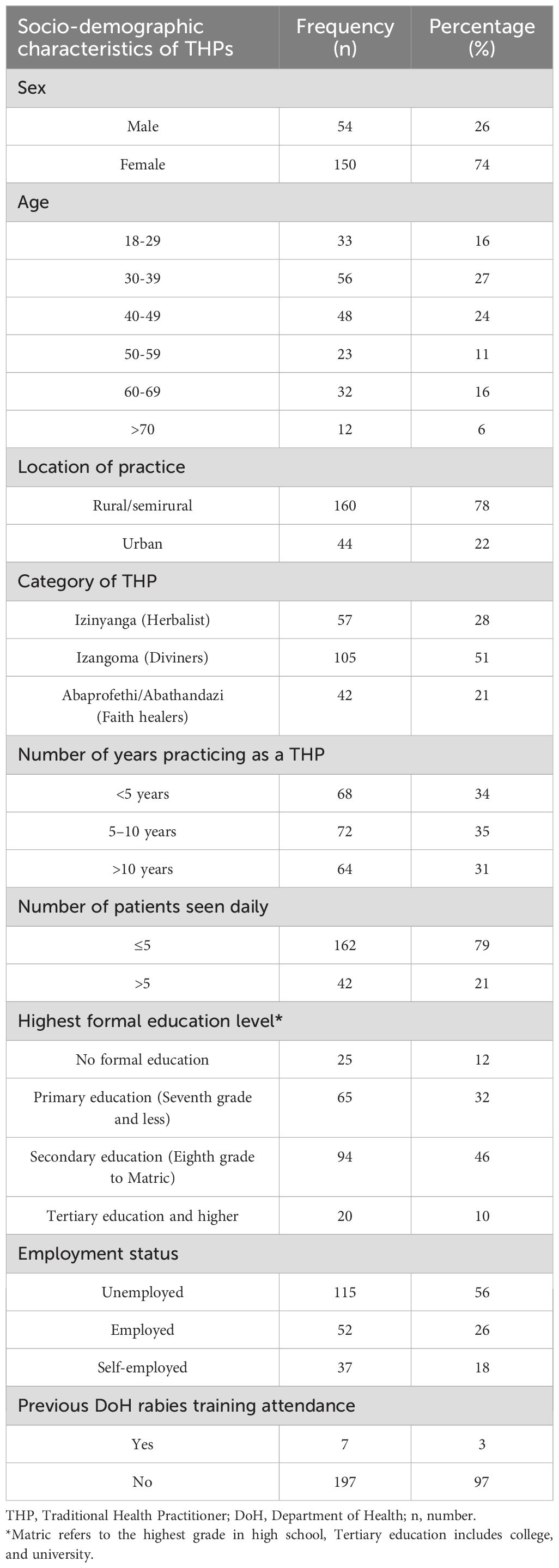
Table 1. Socio-demographic characteristics of Traditional Health Practitioners interviewed during the human rabies KAP study in eThekwini District, KwaZulu-Natal, 2022.
Slightly above a third (35%, 72/204) of the THPs had been practicing for 5–10 years. The median number of consultations done by the THPs was four patients (IQR: 2–5 patients) per day. The study found that 46% (94/204) of the THPs (94/204) had secondary schooling, followed by 32% (65/204) with primary schooling and 10% (20/204) with tertiary education. Over half of the respondents (56%, 115/204) were unemployed and solely reliant on income from their THP practices. Among the total interviewed, only seven (3%) previously attended a formal Department of Health rabies training.
Knowledge about rabies
The majority (92%, 187/204) of THPs had heard of rabies before, and 87% (178/204) of THPs were aware of the cause of rabies. Seventy-six percent (155/204) of THPs were able to give at least one sign or symptom of rabies in humans. The THPs scored a mean score of 2.80 (standard deviation (SD): 2.23) out of nine possible common signs and symptoms. Only 26% (53/204) of THPs correctly answered that rabies is not curable. More than three-quarters (76%, 156/204) knew that there is a vaccine to prevent illness after an animal bite, and 89% (182/204) knew that rabies is deadly. Overall, the interviewed THPs scored a mean knowledge score of 6.50 (SD: 2.61) out of a total of the 14 points possible (Table 2).
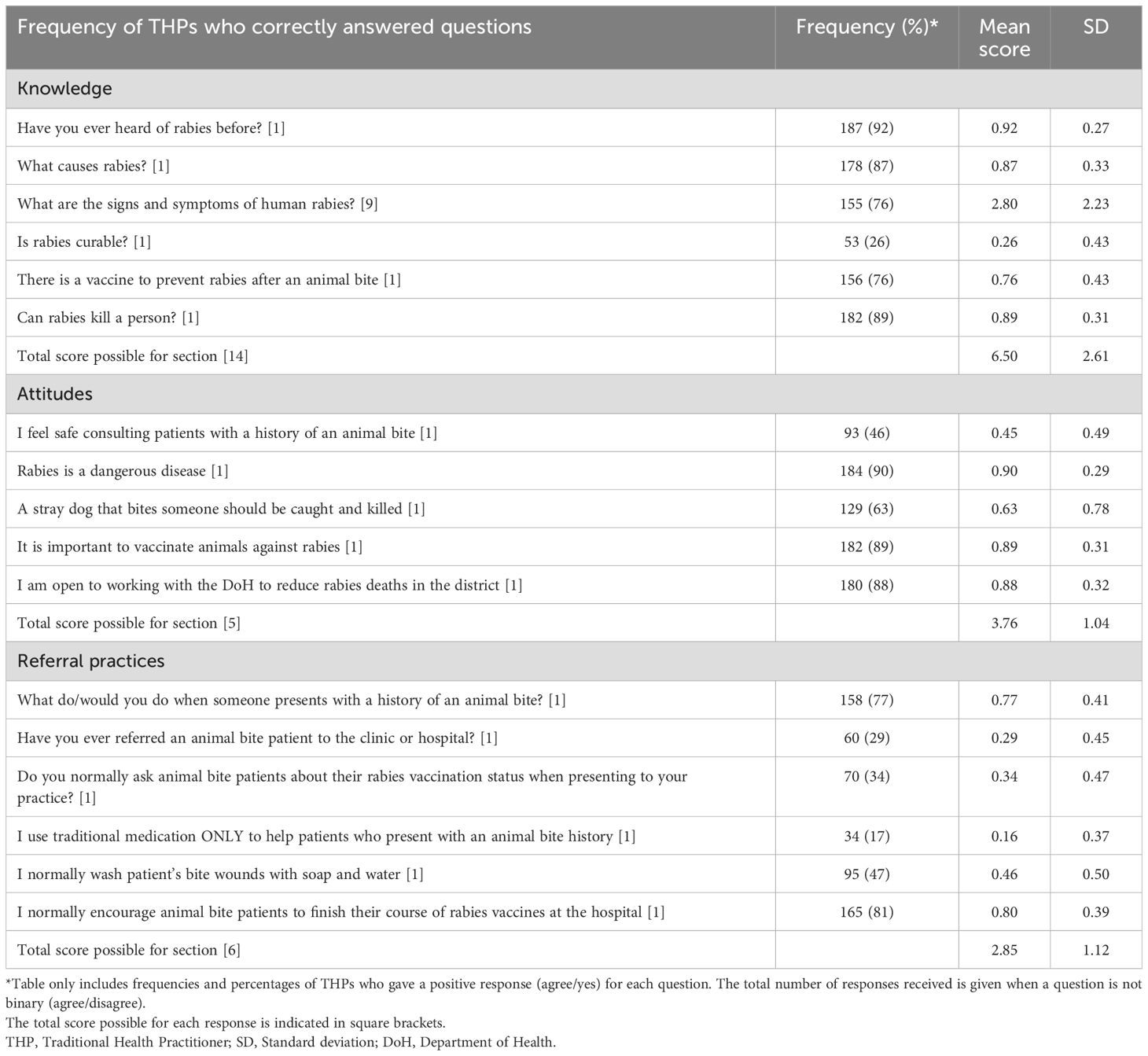
Table 2. Knowledge, attitudes and referral practice scores regarding human rabies among Traditional Health Practitioners in eThekwini District, KwaZulu-Natal, 2022.
Attitudes towards rabies
Only 46% (93/204) of the THPs responded that they felt safe when consulting patients with a history of an animal bite. The majority (90%, 184/204) deemed rabies a dangerous disease, but only 63% (129/204) supported the killing of a stray dog bitten by someone. Almost 90% (182/204) agreed that the vaccination of animals against rabies is important, and 88% (180/204) revealed that they are open to working with the DoH to reduce the incidence of human rabies in eThekwini District. Overall, the THPs scored a mean attitude score of 3.76 (SD: 1.04) out of a total of the five points possible (Table 2).
Rabies referral practices to conventional healthcare
When asked about what they do or would do when an animal bite patient presents to them, 77% (158/204) of THPs gave answers that included an urgent referral to a hospital/clinic. Amongst these answers, 92% (146/158) opted for exclusive urgent referral, and 8% (12/158) opted for treating the wound with traditional medicine (roots, herbs, seeds, flowers, animal products) before referring. The remaining (23%, 46/204) opted for treating with traditional medicine only (20% 40/204) or sending the animal bite patient to a nearby pharmacy (3%, 6/204).
Only 29% (60/204) of the THPs had ever referred an animal bite patient to a healthcare facility. Seventeen percent (34/204) reported that they only use traditional medicine to help the patients. Nearly half (47%, 95/204) reported normally washing bite wounds with soap and water, but more than two-thirds (81%, 165/204) reported encouraging patients to finish their course of PEP. Overall, the THPs scored a mean practice score of 2.85 (SD: 1.12) out of a total of six points possible (Table 2).
Overall status of knowledge, attitudes, and referral practices towards rabies
Figure 2 below shows the frequency distribution of THPs scores for each area the questionnaire assessed. The results show that most THPs (80%, 163/204) did not have adequate knowledge (scored below 60%) on rabies. Furthermore, most THPs (73%, 149/204) had poor (scored below 60%) rabies referral practices. However, the majority (91%, 186/204) had positive (scored above 60%) attitudes toward human rabies and its prevention.
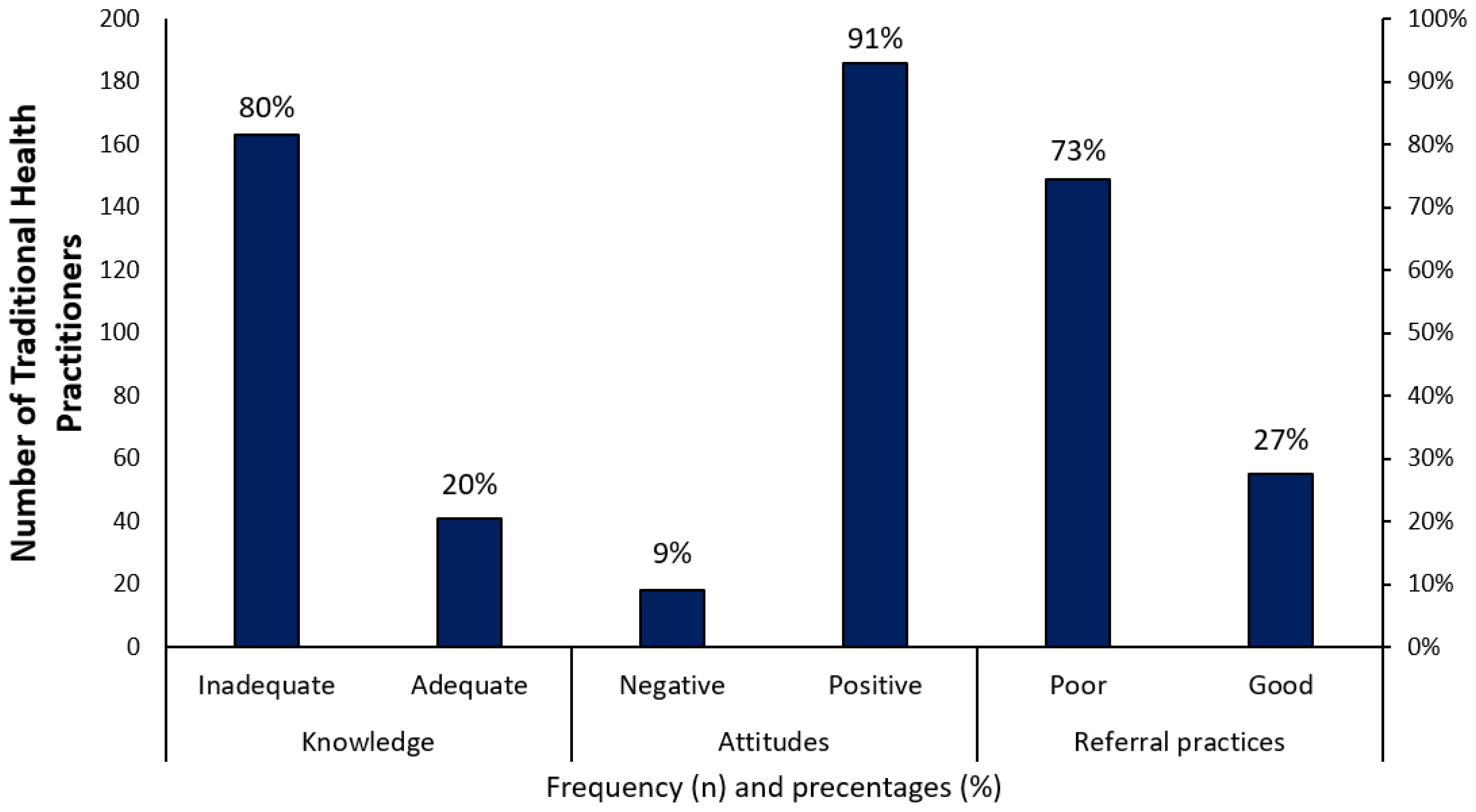
Figure 2. Overall scores indicating knowledge, attitudes, and referral practices among Traditional Health Practitioners in eThekwini District, KwaZulu-Natal, 2022.
Association between THP socio-demographic characteristics and knowledge, attitudes, and referral practices
This study found a significant association between THP’s sex and attitudes, with females having a positive attitude (94%) compared to males (83%). There was also a statistically significant (p=0.016) association between the category of the THP and their attitudes. Izangoma had more positive attitudes (96%) compared to Izinyanga (88%) and Abaprofethi or Abathandazi (83%). (Table 3).
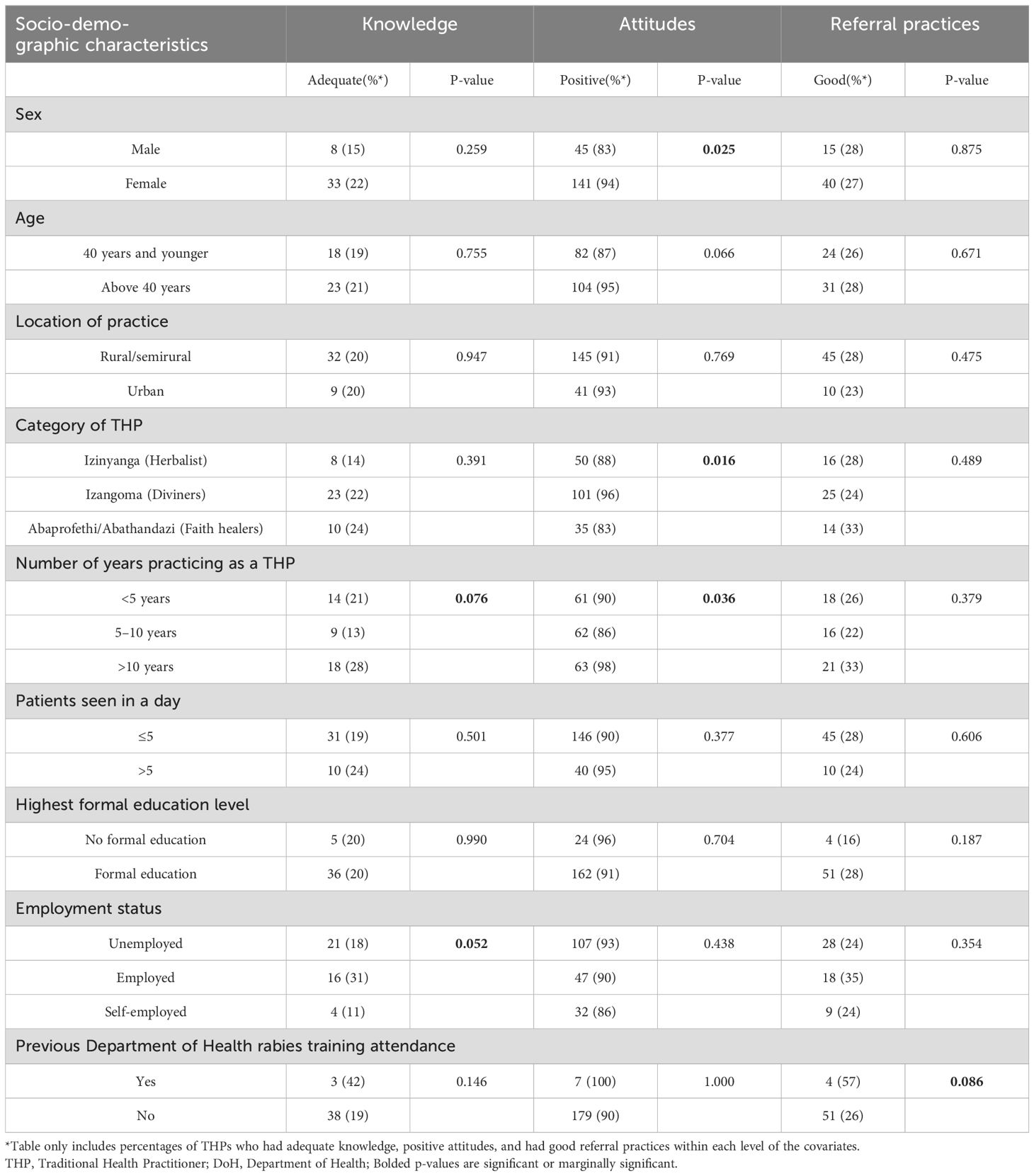
Table 3. Test of associations between Traditional Health Practitioners socio-demographic characteristics and knowledge, attitudes, and referral practices towards human rabies (n=204).
THPs with over 10 years (98%) of practicing experience had significantly more positive attitudes compared to those with less than five years (90%), and those with five to ten years of experience (86%) at a statistically significant (p=0.036) level. Similarly, the study found a marginal (p=0.076) association between the number of years in practice and rabies knowledge. THPs who practiced for more than 10 years (28%) had adequate knowledge compared to those who had practiced for less than five years (21%) and five to ten years (13%).
The employment status of THPs was associated with their knowledge with marginal significance (p=0.052). THPs who were employed (31%) had adequate knowledge compared to those who were unemployed (18%) or self-employed (11%). Lastly, this study found a marginal association between previous DoH rabies training attendance and referral practices, with 57% of THPs who have previously attended having good referral practices compared to 26% who had not attended.
Multivariable analysis
We included the category of THP, number of years practicing, and employment status in the final model as predictors of knowledge. Adjusting for the other variables, the multivariable analysis showed that the odds of having adequate rabies knowledge were 4.13 times higher for THPs who have practiced for more than 10 years than they were for THPs who practiced for five to 10 years (aOR: 4.13 95% CI: 1.52-11.21). THPs who were employed had almost four times higher odds of having adequate knowledge than those who were self-employed (aOR: 3.74 95% CI:1.03-13.57).
The variables; sex, category of THP, and number of years practicing were included in the final model as predictors of attitude. Adjusting for the other variables, a significant association was found between years of practice and attitude. Over 10 years of THP practice resulted in a 12.6 times higher likelihood of having a positive attitude towards rabies prevention compared to those who practiced for 5–10 years. (aOR:12.62 95% CI:1.49-106.61) (Table 4).
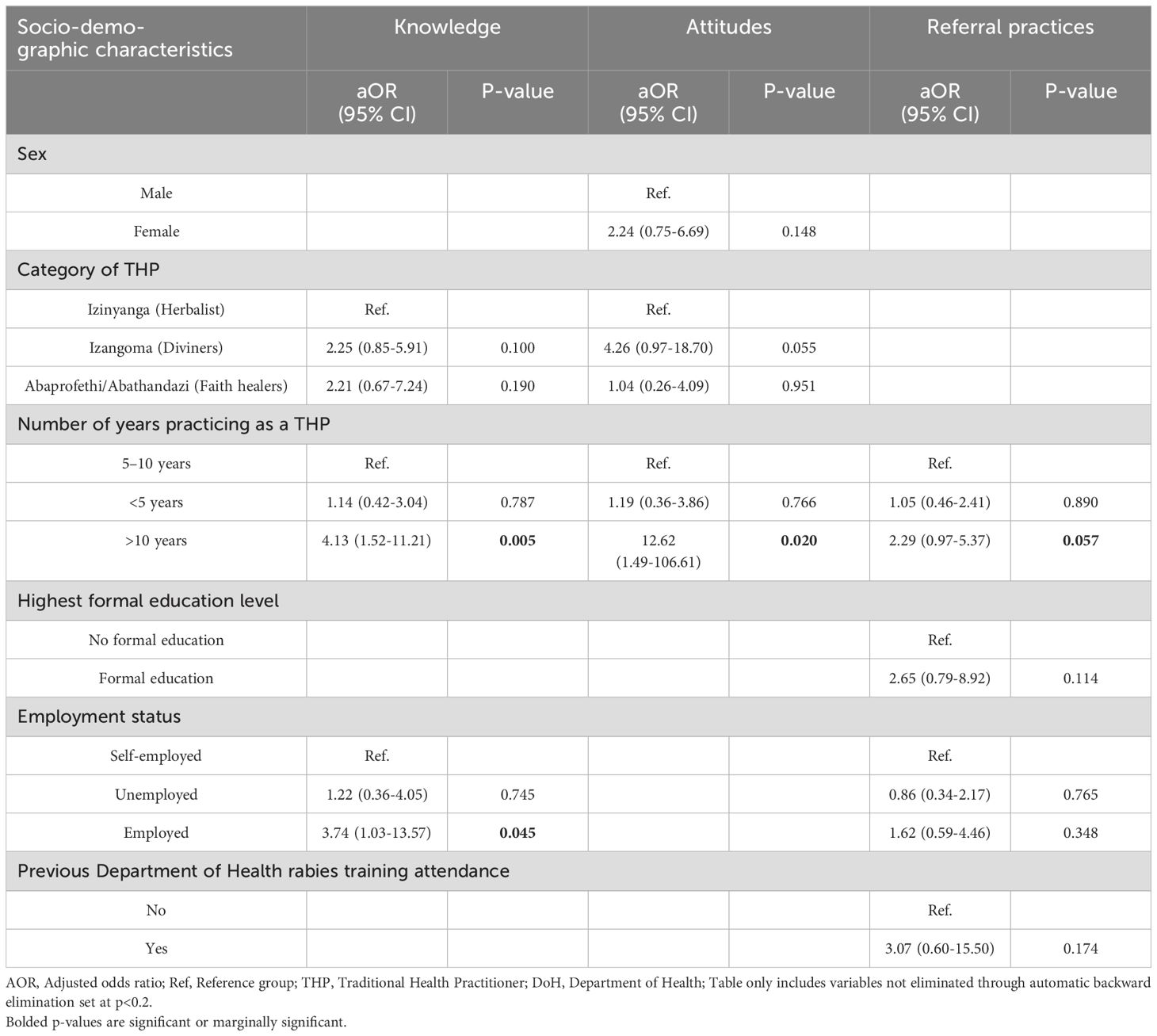
Table 4. Multivariable analysis of Traditional Health Practitioners’ socio-demographic characteristics and knowledge, attitudes, and referral practices towards human rabies (n=204).
The number of years practicing, highest formal education, employment status, and previous DoH rabies training attendance were the variables included in the final model to predict referral practices. Adjusting for the other variables, THPs who had practiced for more than 10 years also had 2.29 higher odds of having good referral practices than their counterparts (aOR:2.29 95% CI:0.97-5.37), although marginally significant (p=0.057).
Assessing the goodness of fit using the Hosmer-Lemeshow goodness of fit test showed that the knowledge and referral practice models were a good fit to data with p>0.05. However, the attitude model was not of good fit for data with p<0.01.
Association between THPs knowledge, attitudes and referral practices
THPs with sufficient knowledge of rabies had 2.33 times higher odds of good referral practices compared to those with inadequate knowledge (OR:2.33 95% CI: 1.13-4.78). Furthermore, a positive rabies attitude significantly increased referral practices compared to negative attitudes (OR:1.32 95% CI: 0.41-4.20), although not significant with a confidence interval that spanned one (Table 5).
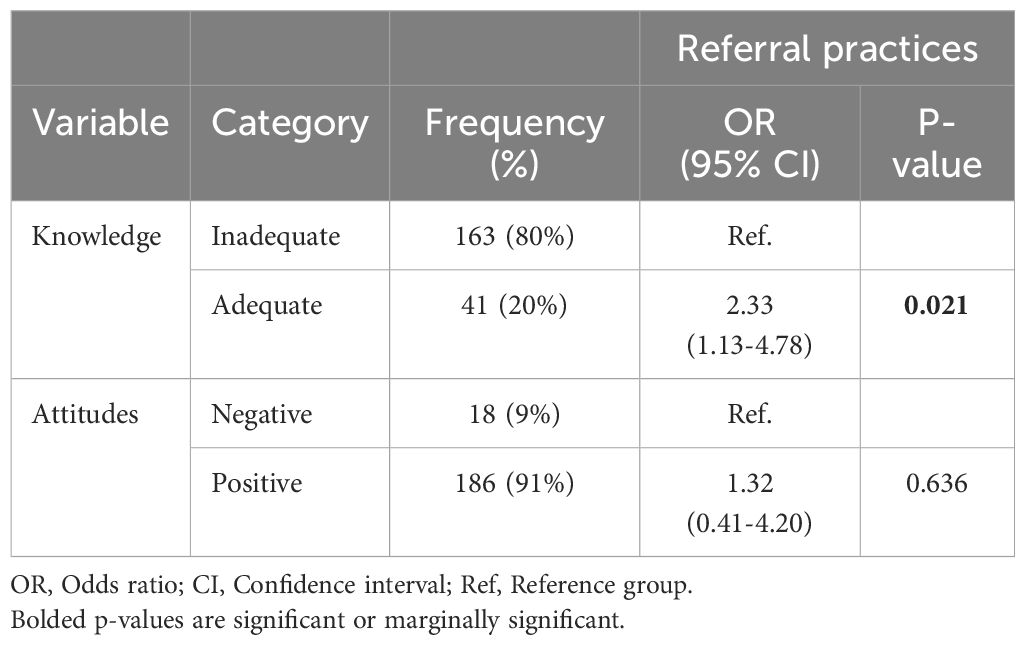
Table 5. Univariate analysis of Traditional Health Practitioners’ knowledge, and attitudes against referral practices towards human rabies (n=204).
Discussion
Our study assessed the knowledge, attitudes, and referral practices regarding animal bites and human rabies and the associated factors among THPs. The study found that most of the THPs had inadequate knowledge (80%) of human rabies and poor referral practices (73%) of animal bite patients. Most (91%) of the THPs had positive attitudes towards human rabies prevention. The study found that adequate knowledge, positive attitudes, and good referral practices were associated with longer experience as a THP and employment. Furthermore, good referral practices of animal bite patients to conventional healthcare facilities for PEP are linked to adequate knowledge and positive attitudes.
More than 87% of THPs in eThekwini were aware that dogs were common transmitters of rabies, however, they did not know that there is no treatment for human rabies after symptom onset. These findings were similar to studies done in Ethiopia and India (29, 31). The THPs in India believed that they can cure rabies or it can be cured by the rabies Goddess (31). The THPs included in the study on average were unable to list more than three signs and symptoms which remarkably lowered their knowledge scores. The inadequate knowledge of the clinical features of rabies was also observed among general community members, healthcare workers and students in South Africa and other African countries (4, 32–36). These findings might be due to the lack of training on rabies by health departments, proven by the finding that only three percent of the THPs in this study had previously attended a rabies training. Factors that were significantly associated with adequate knowledge were being employed and having practiced for more than ten years.
Most THPs (90%) had positive attitudes toward dog vaccinations as a method to prevent rabies. This is contrary to the Indian study amongst THPs who were against the vaccination of dogs against rabies (31). The objection against vaccination was based on the belief that vaccines contradict the natural protection of the Goddess against rabies (31). Most of the THPs in eThekwini were willing to collaborate with the health department to reduce rabies mortality. Three other studies done in South Africa show that most THPs have positive attitudes towards a collaborative relationship with conventional healthcare (23, 37, 38). These were also the findings of studies that interviewed THPs in Kenya and Ethiopia (21, 39, 40). The THPs in these two studies were also willing to work hand in hand with the health department (21, 39, 40). This study also found that having practiced for over ten years significantly predicts positive attitudes. Despite the positive attitudes and willingness to collaborate, the study THPs (73%) had poor overall referral practices of animal bite patients. Very few THPs reported having referred an animal bite patient to a healthcare facility for PEP. Additionally, less than half of them usually wash animal bite wounds with soap and running water, while washing and disinfecting wounds can prevent about one-third of rabies infections (16). Experience (more years of practice) as a THP is crucial for good referral practices, as experienced THPs have seen more cases over the years, leading to favorable practices. Although not statistically significant, the study showed that the odds of having good referral practices were increased amongst THPs with adequate knowledge or positive attitudes. This suggests that improving THP’s knowledge and attitudes towards human rabies may lead to better referral practices. This is congruent to previous rabies KAP studies that have demonstrated a direct correlation between knowledge, attitudes, and improved practices, which ultimately improves health outcomes (33, 41). Unlike socio-demographic characteristics that are not easily modifiable, educational interventions can significantly enhance the knowledge and attitudes of THPs.
The study was not without limitations. The total number of THPs interviewed did not meet the targeted sample size, potentially limiting the statistical power and contributing to some non-significant associations and wide confidence intervals. The cross-sectional study design chosen provided only a snapshot of THPs’ knowledge, attitudes, and referral practices. While this design allows for assessing associations between variables, it does not establish causality. The regression analysis also adjusted for confounding blindly (by using multivariate models). Lastly, since the study was only conducted in one of 11 districts of the province, the generalizability of the findings may be limited. Although these limitations may threaten the validity of the study findings, the study was not intended to be exhaustive but can rather be used as a preliminary investigation of the topic.
Conclusion
THPs are crucial in primary healthcare as animal bite patients usually seek healthcare from them before conventional healthcare facilities. Although they have good attitudes towards rabies, this study has shown that gaps exist in their knowledge, and referral practices in eThekwini District. It has also shown that improving their knowledge and attitudes might lead to better referral practices of animal bite patients for PEP. Lastly, this study indicates that THPs in the eThekwini District are open to collaborating with conventional health to decrease human rabies deaths. Continuous formal training on rabies and its prevention is necessary, in that way, THPs can also serve as trusted stakeholders that educate their patients about rabies, especially in rural areas. A multidisciplinary approach that includes THPs is needed to control and possibly eliminate dog-mediated rabies by 2030.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by University of the Witwatersrand Health Research Ethics Committee (M220123) (Supplementary File 5). The studies were conducted in accordance with the local legislation and institutional requirements (Supplementary Files 6-8). The participants provided their written informed consent to participate in this study.
Author contributions
MM: Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Visualization, Writing – original draft, Writing – review & editing. TZ: Data curation, Formal analysis, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. BM: Conceptualization, Funding acquisition, Investigation, Project administration, Resources, Writing – original draft, Writing – review & editing. LK: Conceptualization, Formal analysis, Funding acquisition, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing. PP: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by the South African Field Epidemiology Training Programme. Hence, the authors would like to thank the program for fully funding this study.
Acknowledgments
The authors would like to acknowledge Ms. Emelda Ramutshila, Dr. Alex De Voux, and Mrs. Hetani Mdose for their contributions to this research project. Sincere gratitude is also extended to Khulani Phoswa, Smiso Msani, Nhlakanipho Mbambo, Musa Cele, Zakhele Sibiya, and the eThekwini’s Traditional Health Practitioners Association who made data collection possible.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fitd.2025.1542614/full#supplementary-material
Abbreviations
WHO, World Health Organization; SA, South Africa; KZN, KwaZulu-Natal; KAP, Knowledge, Attitudes, and Practices; THP, Traditional Health Practitioners; PEP, Post-exposure Prophylaxis; DoH, Department of Health; VIF, Variation Inflation Factor; OR, Odds Ratios; aOR, Adjusted Odds Ratios; IQR, Interquartile Range; SD, Standard Deviation; CI, Confidence Interval; REDCap, Research Electronic Data Capture.
References
1. World Health Organization. ZERO BY 30 The Global Strategic Plan to end human deaths from dog-mediated rabies by 2030 Geneva, 2018–2018 (2022). Available online at: https://apps.who.int/iris/bitstream/handle/10665/272756/9789241513838-eng.pdf?ua1 (Accessed July 2, 2022).
2. Mshelbwala P, Ogunkoya A, Maikai B, and Atuman S. Knowledge, Attitude and Practice about Dog Bite and Rabies Exposure among Dog Meat Consumers and Processors in Abia State, Nigeria. J Veterinary Adv. (2014) 4. doi: 10.5455/jva.20140214105801
3. Liu C and Cahill JD. Epidemiology of rabies and current US vaccine guidelines. R I Med J (2013). (2020) 103:51–3.
4. Spargo RM, Coetzer A, Makuvadze FT, Chikerema SM, Chiwerere V, Bhara E, et al. Knowledge, attitudes and practices towards rabies: A survey of the general population residing in the Harare Metropolitan Province of Zimbabwe. PloS One. (2021) 16:e0246103. doi: 10.1371/journal.pone.0246103
5. Weyer J, Dermaux-Msimang V, Grobbelaar A, Le Roux C, Moolla N, Paweska J, et al. Epidemiology of human rabies in South Africa, 2008 - 2018. S Afr Med J. (2020) 110:877–81. doi: 10.7196/SAMJ.2020.v110i9.14324
6. Hampson K, Coudeville L, Lembo T, Sambo M, Kieffer A, Attlan M, et al. Estimating the global burden of endemic canine rabies. PloS Negl Trop Dis. (2015) 9:e0003709. doi: 10.1371/journal.pntd.0003709
7. Nel L, Roux K, and Atlas R. Meeting the rabies control challenge in South Africa. Microbe. (2009) 4:61–5.
8. National Institute for Communicable Diseases. An update on rabies in South Africa 2021–2021 (2022). Available online at: https://www.nicd.ac.za/wp-content/uploads/2021/12/An-update-on-rabies-in-South-Africa-2021.pdf (Accessed July 2, 2022).
9. National Institute for Communicable Diseases. An update on rabies in South Africa 2021–2021 (2021). Available online at: https://www.nicd.ac.za/wp-content/uploads/2021/01/An-update-on-rabies-in-South-Africa.pdf (Accessed July 2, 2022).
10. Bapela PM. Epidemiological report of human rabies cases in KwaZulu-Natal Province, June 2019-June 2021. (2021).
11. World Health Organization. The official launch of a rabies elimination programme funded by the Gates Foundation and coordinated by WHO will take place in the Richards Bay/Uthungulu area of KwaZulu-Natal province in South Africa on 22 April 2011–2011 (202). Available online at: https://www.who.int/news/item/01-04-2011-the-official-launch-of-a-rabies-elimination-programme-funded-by-the-gates-foundation-and-coordinated-by-who-will-take-place-in-KZN-on-22-april-2011 (Accessed July 2, 2022).
12. Kubheka V, Govender P, Margot B, and Kuonza L. Dog bites and human rabies in the Uthungulu District of KwaZulu-Natal province, 2008-2010: a review of surveillance data. South Afr J Epidemiol infection. (2013) 28:38–9. doi: 10.1080/10158782.2013.11441517
13. Hadebe JM and Sibiya MN. Experiences of people affected by rabies in Ethekwini district in the province of Kwazulu-Natal, South Africa. Afr Health Sci. (2020) 20:150–7. doi: 10.4314/ahs.v20i1.20
14. Development SANDoALRaR. National strategy for the elimination of canine mediated human rabies in South Africa 2019–2021 (2022). Available online at: https://www.dalrrd.gov.za/vetweb/pamphlets&Information/Policy/National%20Strategy%20for%20the%20Elimination%20of%20Canine%20Mediated%20Human%20Rabies%20in%20South%20Africa%202019.pdf (Accessed August 20, 2022).
15. Kisaka S, Makumbi FE, Majalija S, Bangirana A, and Thumbi SM. Epidemiology and preclinical management of dog bites among humans in Wakiso and Kampala districts, Uganda: Implications for prevention of dog bites and rabies. PloS One. (2020) 15:e0239090. doi: 10.1371/journal.pone.0239090
16. Liu Q, Wang X, Liu B, Gong Y, Mkandawire N, Li W, et al. Improper wound treatment and delay of rabies post-exposure prophylaxis of animal bite victims in China: Prevalence and determinants. PloS Negl Trop Dis. (2017) 11:e0005663. doi: 10.1371/journal.pntd.0005663
17. Beasley EA, Wallace RM, Coetzer A, Nel LH, and Pieracci EG. Roles of traditional medicine and traditional healers for rabies prevention and potential impacts on post-exposure prophylaxis: A literature review. PloS Negl Trop Dis. (2022) 16:e0010087. doi: 10.1371/journal.pntd.0010087
18. Rumana R, Sayeed AA, Basher A, Islam Z, Rahman MR, and Faiz MA. Perceptions and treatment seeking behavior for dog bites in rural Bangladesh. Southeast Asian J Trop Med Public Health. (2013) 44:244–8.
19. Salve H, Rizwan SA, Kant S, Rai SK, Kharya P, and Kumar S. Pre-treatment practices among patients attending an Animal Bite Management clinic at a primary health centre in Haryana, North India. Trop Doct. (2015) 45:123–5. doi: 10.1177/0049475514562492
20. Babb DA, Pemba L, Seatlanyane P, Charalambous S, Churchyard GJ, and Grant AD. Use of traditional medicine by HIV-infected individuals in South Africa in the era of antiretroviral therapy. Psychol Health Med. (2007) 12:314–20. doi: 10.1080/13548500600621511
21. Birhan W, Giday M, and Teklehaymanot T. The contribution of traditional healers’ clinics to public health care system in Addis Ababa, Ethiopia: a cross-sectional study. J Ethnobiol Ethnomed. (2011) 7:39. doi: 10.1186/1746-4269-7-39
22. Mulaudzi F. HIV/AIDS and TB knowledge and beliefs among rural traditional health practitioners in Limpopo Province, South Africa Simon M. Nemutandani1, Stephen J. H. Hendricks1 And F. Mavis Mulaudzi2. (2015). South Africa: African Journal for Physical, Health Education, Recreation and Dance(AJPHERD) (Sabinet African Journals).
23. Zuma T, Wight D, Rochat T, and Moshabela M. The role of traditional health practitioners in Rural KwaZulu-Natal, South Africa: generic or mode specific? BMC Complement Altern Med. (2016) 16:304. doi: 10.1186/s12906-016-1293-8
24. Moshabela M and Zuma T. Bridging the gap between biomedical and traditional health practitioners in South Africa. South Afr Health Review. (2016) 2016:83.
25. Audet CM, Salato J, Blevins M, Amsalem D, Vermund SH, and Gaspar F. Educational intervention increased referrals to conventional care by traditional healers in three high HIV-prevalence rural districts in Mozambique. PloS One. (2013) 8:e70326. doi: 10.1371/journal.pone.0070326
26. Britannica T. KwaZulu-natal province, South Africa 2020 (2022). Available online at: https://www.britannica.com/place/KwaZulu-Natal (Accessed July 2, 2022).
27. Statistics South Africa. Mid-year population estimates 2020–2020 (2022). Available online at: http://www.statssa.gov.za/publications/P0302/P03022020.pdf (Accessed July 2, 2022).
28. Barlett JE, Kotrlik JW, and Higgins CC. Organizational research: Determining appropriate sample size in survey research. Inf Technol Learning Performance Journal; Morehead. (2001) 19:44–8.
29. Gum B, Girma S, Mohamed H, Kerro dego O, and Chaka H. Assessment of retrospective rabies suspected cases registered at two hospitals, community and traditional healers’ knowledge, attitude and practices in south Ethiopian pastoralist. Ethiopian Veterinary J. (2019) 23:77. doi: 10.4314/evj.v23i2.6
30. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, and Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J BioMed Inform. (2009) 42:377–81. doi: 10.1016/j.jbi.2008.08.010
31. Nadal D, Hampson K, Lembo T, Rodrigues R, Vanak A, and Cleaveland S. where rabies is not a disease. bridging health worlds to improve mutual understanding and prevention of rabies. Front veterinary sci. (2022) 9:867266. doi: 10.3389/fvets.2022.867266
32. Mapatse M, Sabeta C, Fafetine J, and Abernethy D. Knowledge, attitudes, practices (KAP) and control of rabies among community households and health practitioners at the human-wildlife interface in Limpopo National Park, Massingir District, Mozambique. PloS Negl Trop Dis. (2022) 16:e0010202. doi: 10.1371/journal.pntd.0010202
33. Sambo M, Lembo T, Cleaveland S, Ferguson HM, Sikana L, Simon C, et al. Knowledge, attitudes and practices (kap) about rabies prevention and control: a community survey in Tanzania. PloS Neglected Trop Dis. (2014) 8:12–6. doi: 10.1371/journal.pntd.0003310
34. Ngobeni MF. Attitudes of community members toward human rabies in the Vhembe District of the Limpopo Province, South Africa. South Africa: University of South Africa (2018).
35. Savadogo M, Kanyala E, Traoré AK, Dahourou LD, Guigma HV, Ouandaogo SH, et al. Knowledge, attitudes and practices about rabies prevention and control: A community survey in five health districts of Burkina Faso. Int J Biol Chem Sci. (2022) 15:1800–16. doi: 10.4314/ijbcs.v15i5.9
36. Ba MF, Kane NM, Diallo MKK, Bassoum O, Boh OK, Mboup FZM, et al. Knowledge, Attitudes, and Practices on Rabies among human and animal health professionals in Senegal. Pathogens. (2021) 10:9–10. doi: 10.3390/pathogens10101282
37. Frimpong E and Nlooto M. Tswana traditional health practitioners’ perspectives on the management of diabetes and hypertension: a qualitative study using focus group discussions. Pan Afr Med J. (2019) 34:93. doi: 10.11604/pamj.2019.34.93.19112
38. van Rooyen D, Pretorius B, Tembani NM, and ten Ham W. Conventional and traditional health practitioners’ collaboration. Curationis. (2015) 38:1495. doi: 10.4102/curationis.v38i2.1495
39. Bitta MA, Kariuki SM, Gona J, Abubakar A, and Newton C. Priority mental, neurological and substance use disorders in rural Kenya: Traditional health practitioners’ and primary health care workers’ perspectives. PloS One. (2019) 14:e0220034. doi: 10.1371/journal.pone.0220034
40. Teklehaymanot T, Giday M, Medhin G, and Mekonnen Y. Knowledge and use of medicinal plants by people around Debre Libanos monastery in Ethiopia. J Ethnopharmacol. (2007) 111:271–83. doi: 10.1016/j.jep.2006.11.019
Keywords: animal bites, human rabies, Traditional Health Practitioners, post-exposure prophylaxis, KwaZulu-Natal
Citation: Mabona M, Zwane T, Mhlongo B, Kuonza L and Phafane P (2025) Knowledge, attitudes, and referral practices regarding animal bites and prevention of human rabies among Traditional Health Practitioners in the eThekwini District in KwaZulu-Natal Province, South Africa, 2022. Front. Trop. Dis. 6:1542614. doi: 10.3389/fitd.2025.1542614
Received: 10 December 2024; Accepted: 14 May 2025;
Published: 09 June 2025.
Edited by:
Teresa Elizabeth Leslie, Morgan State University, United StatesReviewed by:
April Davis, New York State Department of Health, United StatesWaqas Ahmad, University of Veterinary and Animal Sciences, Pakistan
Copyright © 2025 Mabona, Zwane, Mhlongo, Kuonza and Phafane. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maxwell Mabona, TWF4d2VsbG1AbmljZC5hYy56YQ==
 Maxwell Mabona
Maxwell Mabona Thembekile Zwane
Thembekile Zwane Babongile Mhlongo4
Babongile Mhlongo4 Poncho Phafane
Poncho Phafane