Abstract
Venomous animal envenomation remains a significant but neglected public health problem worldwide, with an estimated 5.4 million cases and up to 138,000 deaths annually. The burden is particularly acute in tropical and subtropical regions, especially sub-Saharan Africa, where rural and vulnerable populations face limited access to effective antivenoms and healthcare. Despite this, comprehensive data on envenomation incidence, clinical management, and outcomes remain scarce, hampering efforts to develop effective prevention and treatment strategies. This review synthesizes current knowledge on venomous animal diversity, epidemiology, and clinical manifestations globally, with a focus on Africa’s unique challenges. We examine critical gaps in antivenom production, distribution, and affordability, and highlight international initiatives, including the World Health Organization’s 2019 roadmap for snakebite envenoming control. Recent advances in diagnostics, therapeutics, and community engagement are discussed alongside persistent barriers to implementation. Finally, we propose strategic recommendations to strengthen surveillance, improve antivenom accessibility, and foster regional collaborations to reduce envenomation morbidity and mortality in Africa. Addressing these challenges requires coordinated global and local efforts to translate scientific advances into sustainable health outcomes for affected populations.
1 Introduction
Venomous animals represent a remarkable and diverse component of global biodiversity, encompassing over 540,000 species distributed across terrestrial, aerial, and aquatic ecosystems (Figure 1) (1). These species, including snakes, scorpions, spiders, and marine animals, have evolved complex venom systems over millions of years, enabling them to capture prey, deter predators, and protect against microbial threats. Venoms are complex mixtures of proteins, peptides, and other bioactive molecules with potent biological effects, some of which have been harnessed for therapeutic purposes.
Figure 1

Diversity of venomous animals across terrestrial, aerial, and aquatic ecosystems.
Despite their ecological importance, venomous animals pose a significant threat to human health worldwide. Snakebite envenoming alone is recognized by the World Health Organization (WHO) as a neglected tropical disease, responsible for an estimated 5.4 million bites, 81,000 to 138,000 deaths, and numerous disabilities annually (2). Beyond snakes, scorpion and spider envenomation contribute substantially to morbidity, particularly in tropical regions.
The burden of envenomation is especially pronounced in sub-Saharan Africa, where a combination of high biodiversity of venomous species, environmental factors, and socio-economic vulnerabilities converge to create a major public health challenge (3). Rural populations, agricultural workers, and children are disproportionately affected due to increased exposure and limited access to timely and adequate medical care. In many African countries, reliable epidemiological data are lacking due to underreporting, insufficient surveillance systems, (2) and barriers to healthcare access, which complicate resource allocation and intervention planning.
Treatment of envenomation in Africa faces critical obstacles. The supply of safe and effective antivenoms is frequently insufficient and unevenly distributed, reflecting challenges in global antivenom production, economic constraints, cold chain logistics, and regulatory hurdles (4, 5). The high cost of antivenoms often places them out of reach for impoverished populations, leading to delayed or inappropriate treatment, which exacerbates morbidity and mortality. Furthermore, clinical management is complicated by the diversity of venomous species, each requiring specific or polyvalent antivenoms, and by frequent adverse reactions to some antivenom formulations.
Recognizing these challenges, the WHO released a global roadmap in 2019 aimed at halving snakebite mortality and morbidity by 2030 through a multipronged approach including improved epidemiological data collection, strengthened antivenom availability and quality, enhanced healthcare worker training, and community education (2). This strategy acknowledges the urgent need for regional collaborations and investment in local production capacities to ensure sustainable access to effective treatments.
This review synthesizes the current global understanding of venomous animal envenomation with a focus on Africa’s unique epidemiological patterns, clinical challenges, and treatment gaps. It further examines recent scientific and technological advances in venom diagnostics and antivenom development, as well as international efforts addressing these issues. Finally, it outlines strategic recommendations to improve surveillance, healthcare delivery, and research, emphasizing the critical need for coordinated actions to reduce the burden of envenomation and improve health outcomes across the African continent.
2 Data synthesis methodology
This work is a narrative review of the literature aiming to provide an overview of current knowledge on envenomations in Africa, with a particular focus on snakebites and scorpion stings. The selection criteria included studies published between 2015 and 2024, with priority given to those addressing prevalence, morbidity, mortality, and access to treatment in sub-Saharan Africa.
Data sources comprised major scientific databases such as PubMed, Scopus, and Google Scholar, as well as reports from international organizations, including the World Health Organization and the World Bank. Information was synthesized using a thematic approach, which allowed for the identification of the main challenges and proposed solutions, while taking into account the specific socio-economic and health contexts of each region.
To illustrate this approach, several representative studies were considered. For instance, 32, in Nature, highlighted the persistent neglect of snakebite management in Africa, despite its recognition by the WHO as a neglected tropical disease. Similarly, 33, in PLOS, emphasized the severe cardiac complications associated with scorpion stings, particularly myocarditis, and underscored the importance of rapid clinical management. 34, in ScienceDirect, analyzed the availability and accessibility of antivenoms in Africa, identifying key barriers and proposing strategies to improve their distribution and use.
This methodological clarification strengthens the transparency and rigor of our synthesis, while maintaining the objective of providing a comprehensive overview of envenomations and their management in Africa.
3 Global overview of venomous animals and envenomation burden
Venomous animals are taxonomically diverse, distributed across multiple phyla including Arthropoda, Mollusca, Chordata, and others, and occupy varied ecological niches worldwide. Their venoms have evolved as adaptive tools primarily for prey immobilization and defense, composed of complex cocktails of proteins, peptides, enzymes, and other bioactive compounds with diverse physiological targets (1). Among the most medically significant groups are snakes, scorpions, spiders, and certain marine animals, each contributing variably to the global envenomation burden.
3.1 Diversity and medical importance of animals
Snakes (Order Squamata, Suborder Serpentes) represent the majority of envenomation cases globally. Families of particular medical relevance include Elapidae (cobras, mambas, kraits, taipans), Viperidae (vipers, rattlesnakes, lanceheads), and Atractaspididae. The geographical distribution of venomous snakes spans all continents except Antarctica (Figure 2), with the highest diversity and incidence of bites in tropical and subtropical regions (2). Snake venoms typically contain neurotoxins, hemotoxins, cytotoxins, or combinations thereof, leading to a spectrum of clinical manifestations from neuroparalysis to hemorrhage and tissue necrosis.
Figure 2
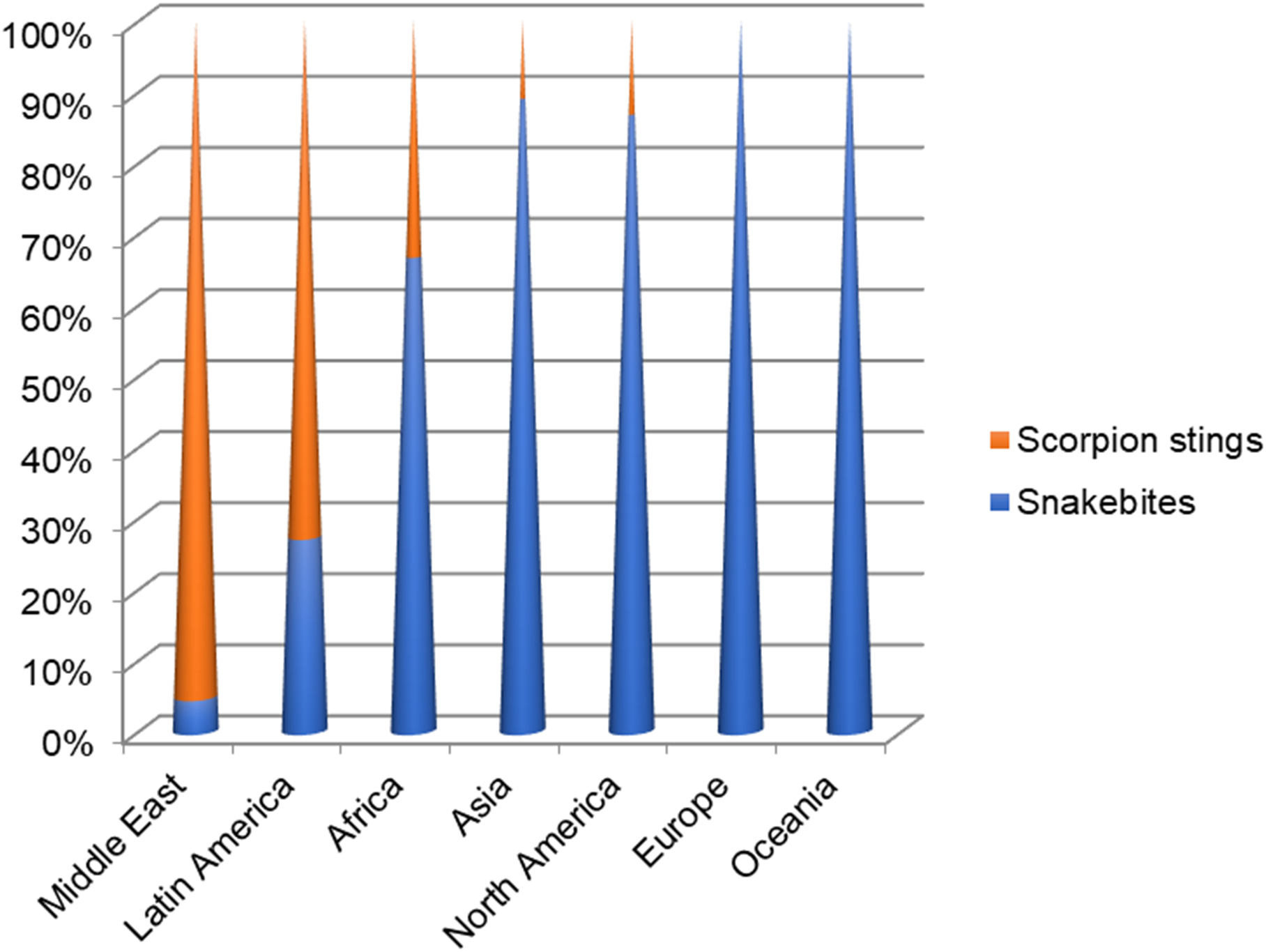
Normalized comparison of snakebites versus scorpion stings incidences by geographic region. Scorpion stings represent the major threat in the Middle East and Latin America.
Scorpions (Order Scorpiones) are responsible for a significant number of envenomation cases, especially in arid and semi-arid regions such as North Africa, the Middle East, and Latin America (Figure 3). Species of medical importance include Androctonus, Leiurus, Tityus, and Centruroides, whose venoms predominantly induce neurotoxic and cardiotoxic effects (6). Scorpion envenomation can lead to severe systemic symptoms and even death, particularly in children.
Figure 3
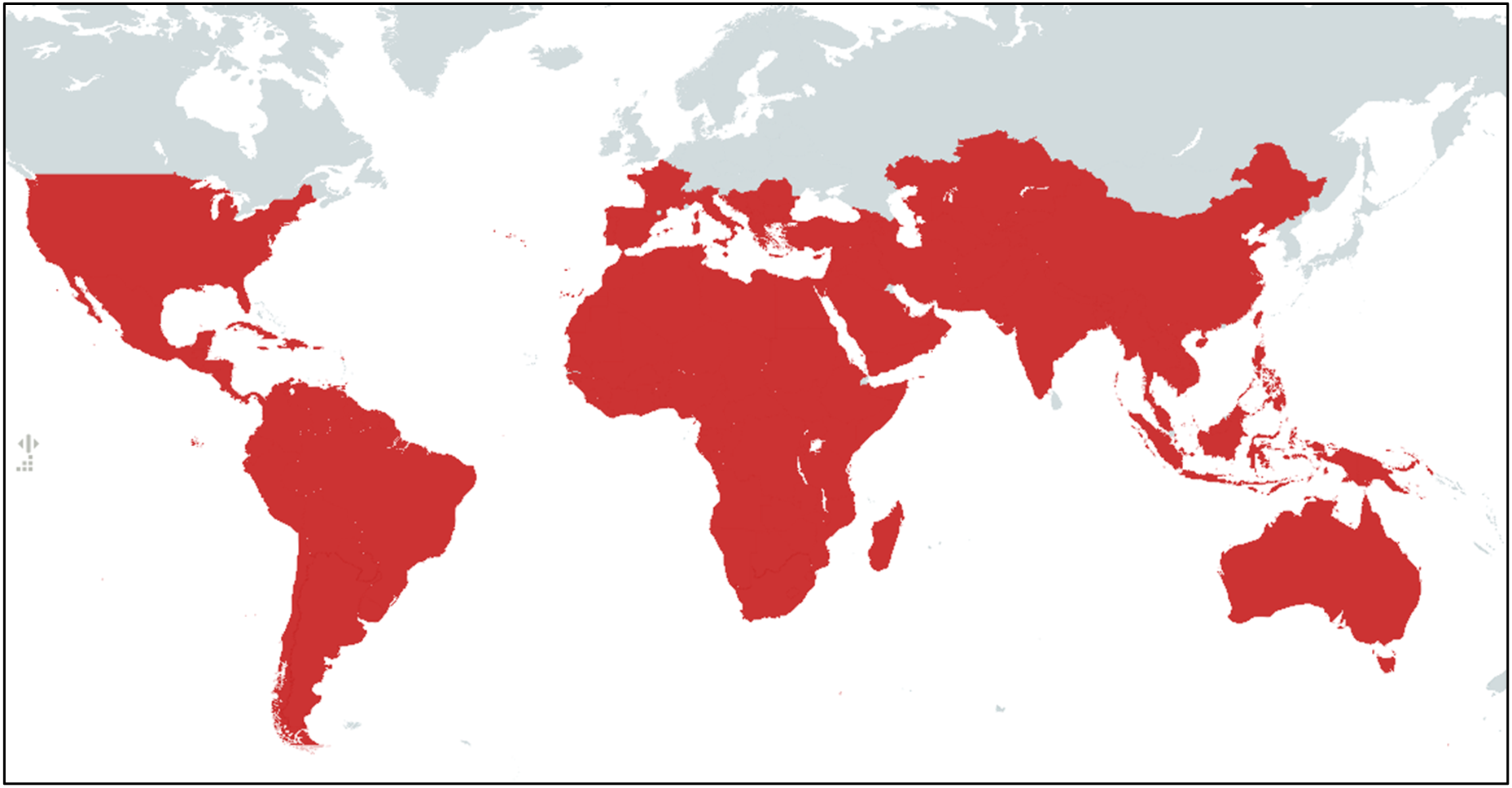
Geographical distribution of scorpions.
Spiders (Order Araneae), while diverse, are less frequently implicated in medically severe envenomation. However, genera such as Latrodectus (black widows) and Loxosceles (recluse spiders) produce venoms capable of causing neurotoxic and dermonecrotic syndromes respectively (7). Envenomation by these spiders is geographically restricted but clinically significant in endemic regions.
Marine venomous animals, including cone snails, jellyfish, stonefish, and certain fish species, also contribute to envenomation, particularly in coastal communities and recreational users. While often less frequent, these incidents can result in severe systemic reactions and fatalities (8).
3.2 Epidemiology of envenomation: global incidence and impact
The global burden of venomous animal envenomation is substantial yet underestimated due to limited surveillance and reporting. The WHO estimates that approximately 5.4 million snakebites occur each year, resulting in 81,000 to 138,000 deaths and numerous cases of permanent disability (2). Scorpion stings are estimated to cause over 1.2 million envenomations and approximately 3,250 deaths annually (9). The burden is disproportionately borne by rural, impoverished populations in low- and middle-income countries (LMICs), where healthcare access is limited and exposure risk is high.
Geographical patterns reveal that South Asia, Southeast Asia, sub-Saharan Africa, and Latin America bear the greatest burden of snakebite envenoming, with incidence rates reaching up to 500 bites per 100,000 people per year in some regions (10). Scorpion envenomation similarly shows hotspots in North Africa, the Middle East, and parts of Latin America (Table 1, Figure 2). Variability in incidence is influenced by ecological factors such as climate and habitat, as well as socio-economic determinants including housing quality, occupation, and education.
Table 1
| Envenomation | Asia | Africa | Europe | Latin America | Middle East | North America | Oceania |
|---|---|---|---|---|---|---|---|
| Snakebites | 2’000’000 | 500’000 | 8’000 | 150’000 | 15’000 | 6’500 | 3’000 |
| Scorpion stings | 250’000 | 250’000 | 1’000 | 400’000 | 300’000 | 16’000 | 0 |
Estimated annual number of reported snakebites and scorpion stings by geographic region.
3.3 Clinical manifestations and envenomation syndromes
The clinical presentation of envenomation depends on the species involved and the composition of their venom. Snakebite symptoms vary from local effects such as pain, swelling, and tissue necrosis, to systemic complications including coagulopathy, neurotoxicity, acute kidney injury, and shock (5). Scorpion venom typically affects the autonomic nervous system, producing symptoms such as severe pain, hypertension or hypotension, cardiac arrhythmias, and pulmonary edema (6). Spider envenomations may cause local dermonecrosis or systemic neurotoxic effects, albeit less commonly than snake or scorpion envenomations (11).
3.4 Data gaps and surveillance challenges
Accurate data collection on envenomation incidence and outcomes remains a critical challenge globally. Many regions lack standardized reporting systems, and cultural, economic, and logistical barriers result in significant underreporting, especially in remote and underserved areas (4). This data gap hampers effective resource allocation, antivenom production planning, and policy development.
Moreover, the available studies are often fragmented, outdated, and restricted to specific regions, while information on scorpion stings remains particularly scarce. Variability in case reporting, lack of standardized data collection methods, and regional disparities further complicate precise assessment of the envenomation burden. These limitations underscore the urgent need for systematic and updated epidemiological studies, particularly in rural areas, to better inform prevention, diagnostic, and treatment strategies.
4 The African context: epidemiology and clinical features
Africa bears one of the heaviest burdens of venomous animal envenomation globally, particularly from snakes and scorpions. With vast ecological diversity ranging from savannas and deserts to tropical forests, the continent is home to a high diversity of medically significant venomous species. However, the true scale of envenomation-related morbidity and mortality in Africa is obscured by substantial data gaps, underreporting, and weak health information systems (12, 13).
4.1 Epidemiological overview
Each year, sub-Saharan Africa records nearly one million snakebites, resulting in an estimated 30,000 to 50,000 deaths and tens of thousands of cases of amputations or disabling sequelae (2, 4). The incidence is particularly high in rural and agricultural areas, where close contact between human populations and snake habitats increases the likelihood of accidental encounters. The species responsible for the most severe envenomations in West and Central Africa mainly include Echis ocellatus, Bitis arietans, Naja nigricollis, and Dendroaspis polylepis.
Echis ocellatus (West African carpet viper), widely distributed across West Africa (Ghana, Burkina Faso, Togo, Benin), is responsible for a large number of fatal bites. Its hemotoxic venom induces severe hemorrhage, extensive edema, and multiorgan failure. Bitis arietans (puff adder), one of the most widespread species in sub-Saharan Africa, particularly in savanna and semi-arid regions, is also a frequent cause of envenomation (14). Its cytotoxic venom leads to local necrosis, edema, and intense pain. Although its bites are rarely fatal, they represent a major cause of morbidity. Naja nigricollis (black-necked spitting cobra), found in West and Central Africa (Senegal, Guinea, Mali, Nigeria) (31), produces a potent neurotoxic venom capable of causing rapid respiratory and cardiac paralysis in the absence of antivenom treatment. Finally, Dendroaspis polylepis (black mamba), mainly distributed in East Africa (Kenya, Tanzania, Uganda, South Africa), delivers an extremely neurotoxic venom. The clinical course is often fulminant, with early paralysis and a high likelihood of fatal outcome if antivenom is not administered urgently (15).
Scorpion stings also represent a major public health problem, particularly in North Africa, where species of the family Buthidae predominate. In Algeria, Tunisia, and Morocco, species such as Androctonus australis, Leiurus quinquestriatus, and Buthus occitanus are responsible for most severe envenomations (6). In Morocco alone, more than 30,000 cases are reported annually, with case fatality rates reaching up to 1.5% in certain regions, due to delays in access to care and the lack of effective antivenom in rural areas (16).
Androctonus australis, widely distributed across North Africa (Morocco, Algeria, Tunisia, Libya), secretes a neurotoxic venom capable of inducing severe respiratory and cardiovascular complications (17). Leiurus quinquestriatus (deathstalker scorpion), found in North Africa and some desert areas of the Sahel, is notorious for its highly virulent venom, which can cause seizures, paralysis, and cardiac disturbances (35). Buthus occitanus, present throughout the Maghreb, usually induces local pain and edema but can also lead to severe systemic manifestations (18).
Despite the magnitude of the problem, centralized and real-time surveillance systems remain absent in many African countries. Mortality associated with envenomations is often underestimated, particularly in rural settings where deaths frequently occur at home or during transport to healthcare facilities (19). Moreover, available data from Central Africa remain limited, representing a potential source of bias in assessing the overall burden. This underrepresentation, acknowledged in the discussion and conclusion, highlights the urgent need for additional epidemiological studies to refine estimates of the health impact and to guide prevention and management strategies (5, 12).
4.2 Risk factors and vulnerable populations
The populations most affected by envenomations—particularly farmers, herders, women, and children—are exposed during daily activities and face heightened vulnerability. The absence of protective footwear, walking barefoot at night, and precarious housing conditions constitute major risk factors (3). In many communities, cultural beliefs and reliance on traditional healers strongly influence health-seeking behaviors, leading to delays in accessing medical care and thereby worsening the severity and mortality of envenomations. Gender and occupational roles further modulate both exposure and access to treatment, with children and rural workers being especially at risk.
To overcome these cultural and traditional barriers, several integrated approaches have proven effective. Collaboration with traditional healers—particularly by training them to recognize danger signs and provide basic first aid—helps reduce treatment delays. The involvement of community leaders in awareness campaigns promotes acceptance of biomedical care, while context-specific educational initiatives inform rural populations about the risks of bites and stings and emphasize the importance of early medical consultation. These strategies, already recommended by the World Health Organization for snakebite envenomation, should also be extended to scorpion stings, which have long been neglected yet remain frequent in rural settings (2, 36).
Children represent a particularly vulnerable group due to their low body mass, which increases the venom-to-body weight ratio and predisposes them to severe systemic effects, especially following scorpion stings. Pediatric mortality associated with envenomations remains a critical issue in North Africa and the Sahel, reflecting both the intensity of the biological hazard and persistent limitations in timely and adequate access to care (20).
4.3 Clinical features and syndromes
In Africa, the clinical spectrum of envenomations varies considerably depending on the species involved. Vipers of the genus Echis (E. ocellatus, E. leucogaster) produce highly hemotoxic venoms that cause coagulopathies, internal hemorrhages, edema, and tissue necrosis. Without the rapid administration of an appropriate antivenom, victims face a high risk of amputation or death from massive hemorrhage. Elapids, such as Naja spp. and Dendroaspis spp., induce severe neurotoxic effects, including descending paralysis and respiratory failure, sometimes combined with local cytotoxic lesions. Mixed syndromes, combining neurotoxic and cytotoxic effects, represent a major therapeutic challenge since they require polyvalent or species-specific antivenoms.
Scorpion envenomations are characterized by a severe “autonomic storm,” manifested by hypersalivation, vomiting, hypertension, arrhythmias, and pulmonary edema, with particularly rapid progression in children. Venoms from Androctonus and Leiurus species contain potent neurotoxins that act on sodium channels, causing life-threatening cardiopulmonary complications (21). Clinical management is frequently hampered by the absence of precise species identification, the clinical similarity between different envenomations, the lack of access to diagnostic tools, and the persistence of inappropriate first-aid practices such as the use of tourniquets or traditional remedies, which often aggravate the initial lesions.
To address these challenges, several recent innovations offer promising perspectives for improving diagnosis and treatment. Rapid diagnostic tools, including immunochromatographic tests and ELISA-based assays, enable the identification of species or venom profiles and guide therapeutic decisions. Antivenomics, based on ex vivo assays, assesses the ability of antivenoms to neutralize different toxins and thus supports the development of formulations better adapted to the complexity of African venoms. Biotechnological advances, particularly recombinant antivenoms and monoclonal antibodies, provide targeted neutralization of specific toxins with enhanced efficacy and improved safety compared with conventional products. In addition, the development of adjunctive therapies targeting critical manifestations—such as hemorrhage, necrosis, or paralysis—may improve survival and reduce morbidity, especially when antivenom administration is delayed.
While these diagnostic and therapeutic advances hold considerable potential, their feasibility, cost-effectiveness, and implementation strategies must be carefully tailored to African health systems. Integrated approaches combining rapid diagnostics, antivenomics, advanced biotechnologies, and adjunctive symptomatic treatments represent major opportunities to strengthen the management of snakebite and scorpion envenomations across the continent. These advances align with the priorities emphasized by the World Health Organization and several experts (2; Chippaux, 2018), underlining the need to adapt therapeutic strategies to the specific epidemiological and toxinological contexts of Africa.
4.4 Gaps in clinical management and reporting
Despite the severity of envenomation syndromes, many health facilities across Africa lack trained personnel, standardized protocols, or sufficient stocks of high-quality antivenoms. Several countries depend entirely on imported antivenoms, which are not always adapted to the local snake species, further compromising efficacy (2).
Recent studies have also shown that clinical guidelines are inconsistently applied across facilities, and that health workers often lack training in recognizing and managing envenomation syndromes (4). In addition, the absence of functional pharmacovigilance systems prevents adequate tracking of treatment effectiveness and adverse effects.
5 Antivenom production, access, and affordability challenges
Despite the existence of antivenoms as the only specific treatment for venomous bites and stings, significant challenges related to their production, distribution, and affordability continue to impede their effectiveness in reducing envenomation-related mortality and morbidity particularly in Africa.
5.1 Global and African antivenom production landscape
Antivenom production is a complex, resource-intensive process involving venom collection, immunization of host animals (usually horses or sheep), plasma harvesting, antibody purification, and formulation. This multi-step process requires high biosafety standards and technological expertise (5).
Globally, the number of antivenom producers has declined dramatically since the 1980s, with most current producers based in Latin America (e.g., Instituto Clodomiro Picado, Instituto Butantan), India, and Southeast Asia. In Africa, local production is extremely limited. Notably, Nigeria and South Africa host some production capacities (e.g., SAVP in South Africa), but they are insufficient to meet the continent’s demand (22).
As a result, many African countries depend on imported antivenoms, which may not be effective against local snake or scorpion species. The lack of region-specific venoms used in immunization is a major reason for reduced therapeutic efficacy and poor clinical outcomes (2, 23).
5.2 Decline of manufacturers and supply chain fragility
Since the 1990s and early 2000s, several historical pharmaceutical companies, including Sanofi Pasteur, have ceased antivenom production for economic reasons, citing insufficient profitability and increasing regulatory constraints. This discontinuation created a supply gap that has never been fully addressed (2). The current antivenom market remains characterized by low production volumes, high manufacturing costs, and limited purchasing power in the most affected regions. This configuration generates a vicious cycle: reduced demand discourages industrial investment, which further decreases supply, raises prices, and undermines accessibility.
According to the World Health Organization, current global production covers only about 50% of actual needs, with the deficit being particularly severe in Africa (2). As illustrated in Figure 4, the entire supply chain is affected by bottlenecks, ranging from venom collection and the standardization of production processes to formulation, quality control, distribution, and ultimately economic accessibility. These constraints exacerbate geographic and socioeconomic inequities in access to antivenoms, thereby worsening the health burden of envenomations.
Figure 4
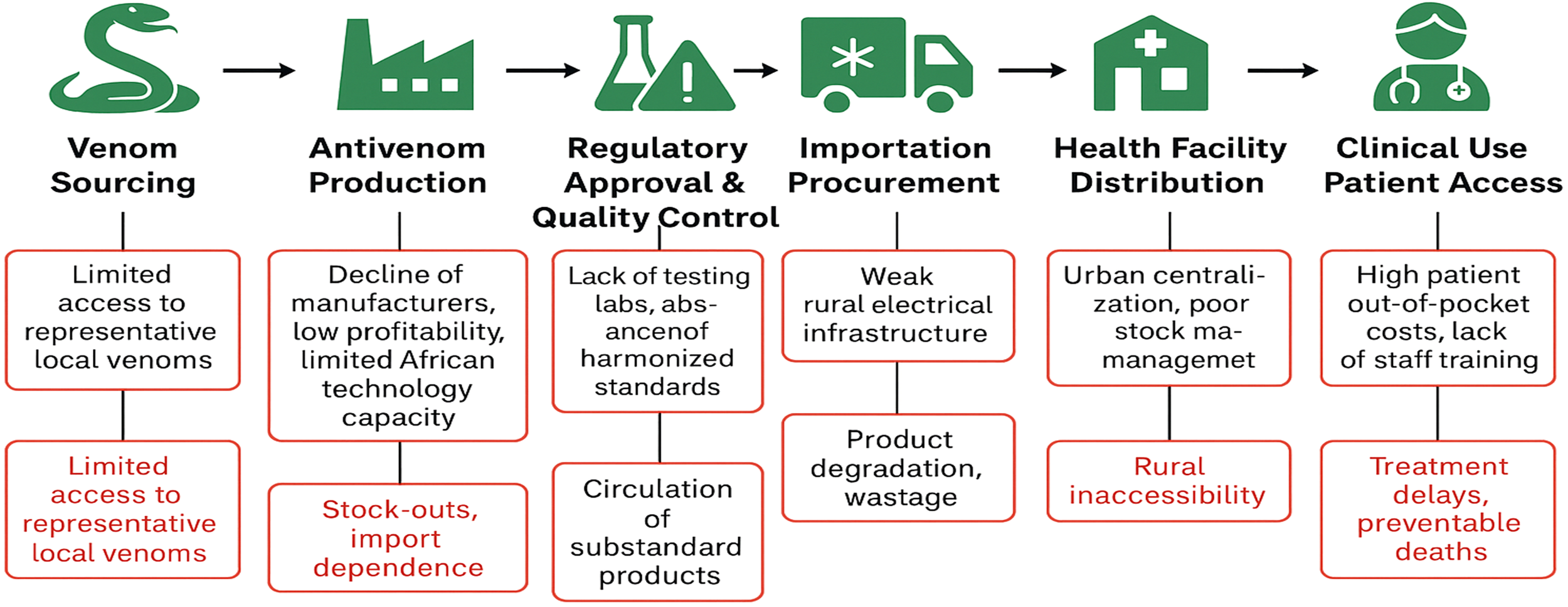
Schematic of the antivenom supply chain and barriers along the antivenoms supply chain in African Health systems.
To overcome these obstacles, it is essential to strengthen public–private partnerships, implement innovative financing mechanisms such as pooled procurement or subsidies, and integrate antivenoms into national essential medicines lists to stimulate demand and ensure the economic viability of the market. Logistical optimization through reinforced distribution infrastructures—particularly by leveraging vaccine supply chains—along with the development of technological innovations such as thermostable formulations or more efficient production processes, also represent critical levers to reduce costs and improve availability. Such an integrated approach is indispensable to transform this fragile market into a sustainable system capable of effectively meeting global health needs.
5.3 Distribution inequities and cold chain constraints
Even when effective antivenoms are available, distribution challenges severely restrict access. Antivenoms require cold chain logistics (2–8°C), yet many rural health facilities in Africa lack reliable electricity or refrigeration infrastructure (24). This leads to centralized stockpiling in urban hospitals, leaving rural communities—the most affected—underserved.
Additionally, lack of national coordination and forecasting systems often results in expired stocks in some regions and acute shortages in others. Emergency procurement is rarely possible due to procurement delays and customs regulations (25).
5.4 Financial barriers and health system limitations
Antivenoms are often prohibitively expensive for both governments and patients. The cost of a single vial ranges from $100 to $500, and treatment may require multiple vials. In many countries, patients are forced to pay out-of-pocket, which results in treatment delays or abandonment (22, 24).
National health systems frequently do not prioritize antivenom in essential drug budgets, and donor support remains fragmented and insufficient. Moreover, training gaps among healthcare professionals lead to poor recognition of envenomation syndromes and underutilization of antivenom even when available (26).
5.5 Case studies: disruptions and impact
Several African countries have faced critical shortages of antivenoms in recent years, revealing systemic weaknesses in envenomation management programs. In Nigeria, the national snakebite response infrastructure almost collapsed in 2016 after supply from a major Indian manufacturer was interrupted (25). Similarly, in Morocco, despite relatively robust surveillance systems for scorpion stings, access to effective and species-specific antivenoms remains severely restricted in peripheral and remote provinces (37). These episodes underscore profound structural deficiencies in the antivenom market and highlight the urgent need for local and regional production hubs, coordinated pooled procurement mechanisms, and strengthened South–South collaborations to ensure sustainable supply, context-specific adaptation, and equitable accessibility of antivenoms.
The antivenom supply chain, schematically represented in Figure 4, spans six critical stages—from venom collection and product formulation to regulatory approval, distribution, and patient access—each characterized by distinct systemic bottlenecks. Collectively, these constraints compromise availability, affordability, and timely access to antivenoms, thereby perpetuating morbidity and mortality associated with snakebite and scorpion envenomations. Addressing these multifactorial barriers requires an integrated strategy combining capacity building in production, regulatory harmonization, supply chain optimization, and innovative financial mechanisms. Such an approach is critical to overcoming market fragility and ensuring equitable, timely, and sustainable access to life-saving antivenoms across the continent.
6 Strategic recommendations for addressing envenomation in Africa
Despite growing global attention to snakebite and other envenomations, Africa remains disproportionately affected and under-resourced in addressing this public health threat. The following recommendations are aimed at guiding African countries, regional organizations, and their international partners toward sustainable, context-specific solutions.
6.1 Strengthening surveillance and epidemiological data
Accurate, real-time data are essential for planning and resource allocation. Yet in many African countries, snakebite and scorpion stings remain under-reported due to weak health information systems and stigma around traditional treatments. To address these challenges, national envenomation registries should be established and integrated into existing disease surveillance platforms. Community-based reporting mechanisms, leveraging digital tools and mobile health applications, can further enhance data collection. Collaboration with traditional healers, who often serve as the first point of contact, should be encouraged to improve referral and documentation. For example, in Benin and Togo, pilot projects using SMS-based reporting have successfully increased real-time documentation of bites and treatment gaps (4).
6.2 Improving local antivenom production and quality assurance
Africa imports the vast majority of its antivenoms, which are often ineffective due to poor species coverage, inadequate regulation, or cold-chain disruptions. Investment in local production capacity is therefore critical. To address this, the development of regional production hubs with validated quality control should be supported, as exemplified by the Institut Pasteur network in Algeria, Tunisia, and Morocco, and the EchiTAb project in Nigeria. Public-private partnerships and South–South cooperation should be encouraged to facilitate technology transfer, improve formulations, and ensure compliance with Good Manufacturing Practices (GMP). In parallel, regulatory frameworks must be strengthened to guarantee product safety and efficacy, with regional harmonization promoted through institutions such as the African Medicines Agency (AMA) (5, 25).
6.3 Enhancing access and affordability
Even where antivenoms are available, they remain largely inaccessible, unaffordable, or poorly distributed, particularly in rural areas. To address these challenges, antivenoms should be subsidized through national essential medicines lists and pooled procurement mechanisms. Their delivery should be integrated into universal health coverage (UHC) strategies and emergency care packages. Furthermore, cold-chain infrastructure and last-mile distribution systems must be expanded through collaborations with vaccine programs or humanitarian supply chains, such as GAVI or Médecins Sans Frontières (MSF). For instance, in Burkina Faso, subsidized procurement combined with decentralized storage reduced antivenom stock-out rates by half within two years (27).
6.4 Training and retention of healthcare providers
A lack of trained personnel in snakebite treatment contributes to inappropriate use of antivenoms, high case fatality rates, and community distrust. To address this, standardized curricula on the management of venomous animals should be introduced in medical, pharmacy, and nursing schools. National workshops and simulation-based training programs should be organized for rural clinicians and emergency responders. Additionally, incentives and career development opportunities should be offered to health workers managing envenomation cases in rural areas. For instance, in Kenya, the implementation of decentralized training combined with pocket protocols improved patient outcomes and reduced inappropriate antivenom use (28).
6.5 Community engagement and behavior change
Cultural beliefs and misinformation often delay care-seeking or promote reliance on ineffective traditional remedies. To address these challenges, targeted education campaigns should be implemented using local languages and trusted community figures, such as teachers, radio hosts, and religious leaders. Interactive media and theater can be employed to modify risk perceptions in high-incidence areas. In addition, school-based education on venomous animals and envenomation prevention should be supported to promote safe practices and first aid knowledge (29).
6.6 Research and innovation
Africa must develop and lead its own strategies for venom and antivenom innovation. Achieving this requires substantial investment in venomics and antivenomics platforms to characterize regional venom profiles and guide the development of effective antivenoms. The establishment of biobanks and venom repositories, initiatives already underway in North and Southern Africa, provides essential infrastructure to support research, standardization, and production. Strategic measures to ensure financial sustainability and enhance the effectiveness of envenomation management include the local production of antivenoms, which not only reduces costs and dependence on imports but also enables the development of products specifically tailored to local species, thereby minimizing variability and inefficacy commonly associated with imported antivenoms. Additionally, coordinated pooled procurement mechanisms and regional partnerships can optimize purchasing volumes and resource sharing among multiple countries, improving access and stabilizing supply. Integrating antivenom programs into national health systems, including budgetary planning and sustainable financing strategies, is crucial to maintain these initiatives beyond the lifespan of temporary subsidies. Collectively, these approaches aim to ensure that the prevention, management, and treatment of envenomations are both locally appropriate and economically sustainable (2).
7 Recent advances in research, diagnostics, and therapeutics
Snakebite, scorpion stings and other envenomations remain critical public health challenges across Africa, contributing to significant morbidity and mortality. Recent advances in research and clinical management hold promise for improving outcomes in this resource-limited context.
7.1 Rapid diagnostic assays
Innovative rapid diagnostic tools, including immunochromatographic and molecular assays, have been developed to enable timely and accurate identification of envenoming species. These point- of-care tests are particularly valuable in rural African settings, facilitating prompt clinical decision- making where laboratory infrastructure is scarce.
7.2 Recombinant and monoclonal antibody antivenoms
Biotechnological breakthroughs have ushered in a new generation of antivenoms based on recombinant proteins and monoclonal antibodies (30). These agents offer enhanced specificity and reduced immunogenicity, with the potential for scalable and standardized production tailored to African venomous species.
7.3 Polyvalent antivenoms and next-generation therapeutics
Given the extensive venom diversity across Africa, polyvalent antivenoms targeting multiple species remain essential. Concurrently, emerging therapeutic strategies, including enzymatic inhibitors, venom-neutralizing peptides, and adjunctive pharmacological agents, are under investigation to augment or replace conventional antivenom therapy.
7.4 Supportive care and adjunct therapies
Optimized supportive care—such as targeted management of coagulopathies with anticoagulants and modulation of immune responses—has proven crucial in mitigating severe complications. Integration of these adjunct therapies enhances patient prognosis in clinical settings with limited resources.
7.5 Challenges in clinical trials, regulatory approval, and market incentives
Despite these promising developments, clinical implementation faces substantial hurdles. Conducting rigorous clinical trials in remote areas remains difficult, regulatory frameworks often lack harmonization, and market incentives for producing affordable, region-specific antivenoms are insufficient. Addressing these barriers requires coordinated efforts among researchers, health authorities, and industry stakeholders to ensure equitable access to improved therapies across the continent.
8 Strategic recommendations and future directions
To effectively reduce the burden of envenomation across Africa, a multi-pronged strategic approach is essential, addressing gaps in surveillance, healthcare delivery, local capacity, and community engagement.
8.1 Strengthening epidemiological data systems
Robust, standardized data collection and reporting frameworks are crucial to accurately assess the incidence, geographic distribution, and clinical outcomes of envenomation. Improved surveillance will inform resource allocation, identify high-risk regions, and guide targeted interventions.
8.2 Enhancing healthcare infrastructure and decentralized antivenom access
Upgrading healthcare facilities, particularly in rural and underserved areas, is vital to enable timely diagnosis and treatment. Decentralized distribution networks for antivenoms should be established to ensure rapid availability, reducing delays that contribute to morbidity and mortality.
8.3 Promoting local production and technology transfer
Developing indigenous manufacturing capacity for antivenoms and related biotherapeutics within Africa will enhance sustainability, affordability, and adaptability to local venomous species. Technology transfer partnerships and capacity-building initiatives are key to achieving this goal.
8.4 Integrating community education, prevention, and first aid training
Community-level programs focused on awareness, prevention strategies, and basic first aid can substantially reduce the incidence and severity of envenomation. Empowering local populations through education promotes early healthcare seeking and appropriate initial management.
8.5 Fostering regional and international collaboration and funding support
Envenomation is a transboundary health issue that requires coordinated efforts across countries and sectors. Strengthening regional networks, sharing data and best practices, and mobilizing sustained international funding are critical to support research, surveillance, and implementation of effective interventions.
9 Conclusion
In conclusion, envenomation remains a significant public health challenge across Africa, compounded by persistent gaps in surveillance, healthcare access, and the availability of regionally appropriate antivenoms. Nonetheless, recent advances in rapid diagnostics, recombinant antivenoms, and adjunctive therapies offer promising avenues to improve clinical outcomes. To translate these innovations into meaningful impact, it is critical to strengthen epidemiological data systems, enhance healthcare infrastructure with decentralized antivenom distribution, and promote local manufacturing and technology transfer. Furthermore, community education and regional collaboration are pivotal for effective prevention and management. Only through a comprehensive, coordinated approach supported by sustained partnerships and funding can the morbidity and mortality associated with envenomation in Africa be substantially reduced.
Statements
Author contributions
KA: Writing – original draft, Writing – review & editing, Formal Analysis, Data curation, Methodology, Visualization, Conceptualization. NM: Writing – review & editing. NH: Writing – review & editing. RS: Writing – review & editing, Supervision. JG: Supervision, Writing – review & editing. AM: Supervision, Writing – review & editing. NO: Writing – review & editing, Project administration, Funding acquisition, Validation, Supervision, Methodology, Resources.
Funding
The author(s) declare that no financial support was received for the research, and/or publication of this article.
Conflict of interest
Author RS was employed by company Atheris Laboratories, Switzerland.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1
Oldrati V Arrell M Violette A Perret F Sprüngli X Wolfender J-L et al . Advances in venomics. Mol Biosyst. (2016) 12:35303543. doi: 10.1039/C6MB00516K
2
World Health Organization . Snakebite envenoming: WHO strategy for prevention and control(2019). Available online at: https://policycommons.net/artifacts/540654/snakebite-envenoming/1517483/ (Accessed June 18, 2023).
3
Harrison RA Hargreaves A Wagstaff SC Faragher B Lalloo DG . Snake envenoming: A disease of poverty. PloS Negl Trop Dis. (2009) 3:e569. doi: 10.1371/journal.pntd.0000569
4
Chippaux J-P . Snakebite envenomation turns again into a neglected tropical disease! J Venomous Anim Toxins Including Trop Dis. (2017) 23:38. doi: 10.1186/s40409-017-0127-6
5
Gutiérrez JM Solano G Pla D Herrera M Segura Á Vargas M et al . Preclinical evaluation of the efficacy of antivenoms for snakebite envenoming: state-of-the-art and challenges ahead. Toxins. (2017) 9:Article 5. doi: 10.3390/toxins9050163
6
Isbister GK Bawaskar HS . Scorpion envenomation. New Engl J Med. (2014) 371:457463. doi: 10.1056/NEJMra1401108
7
Vetter RS Isbister GK . Medical aspects of spider bites. Annu Rev Entomol. (2008) 53:409429. doi: 10.1146/annurev.ento.53.103106.093503
8
Fenner P . Venomous marine animals. South Pacif Underwater Med Soc J. (2004) 34, 196–202.
9
Chippaux J-P . Emerging options for the management of scorpion stings. Drug Design Dev Ther. (2012) 6, 165–73. doi: 10.2147/DDDT.S24754
10
Kasturiratne A Wickremasinghe AR Silva N Gunawardena NK Pathmeswaran A Premaratna R et al . The global burden of snakebite: A literature analysis and modelling based on regional estimates of envenoming and deaths. PloS Med. (2008) 5:e218. doi: 10.1371/journal.pmed.0050218
11
Isbister GK Fan HW . Spider bite. Lancet. (2011) 378:20392047. doi: 10.1016/S0140-6736(10)62230-1
12
Chippaux J-P . Estimate of the burden of snakebites in sub-Saharan Africa: A meta- analytic approach. Toxicon. (2011) 57:586599. doi: 10.1016/j.toxicon.2010.12.022
13
Longbottom J Shearer FM Devine M Alcoba G Chappuis F Weiss DJ et al . Vulnerability to snakebite envenoming: A global mapping of hotspots. Lancet. (2018) 392:673684. doi: 10.1016/S0140-6736(18)31224-8
14
Dajel TB Abubakar SB Dan-Amarya NM Azi NA Mu’azu S Hamza M et al . A prospective observational phase IV study on effectiveness of animal derived polyclonal antibody antivenoms against West African carpet viper (Echis romani) induced coagulopathy and mortality. Toxicon. (2023) 232:107211. doi: 10.1016/j.toxicon.2023.107211
15
Alfa-Ibrahim Adio A Malami I Lawal N Jega AY Abubakar B Bello MB et al . Neurotoxic snakebites in Africa: Clinical implications, therapeutic strategies, and antivenom efficacy. Toxicon. (2024) 247:107811. doi: 10.1016/j.toxicon.2024.107811
16
Hilal I Khourcha S Safi A Hmyene A Stöcklin R Oukkache N . Exploring the inter- and intra-specific variability of androctonus scorpion venoms. Biol Life Sci Forum. (2023) 24:Article 1. doi: 10.3390/IECT2023-14797
17
Bouaziz M Bahloul M Kallel H Samet M Ksibi H Dammak H et al . Epidemiological, clinical characteristics and outcome of severe scorpion envenomation in South Tunisia: Multivariate analysis of 951 cases. Toxicon. (2008) 52:918−926. doi: 10.1016/j.toxicon.2008.09.004
18
Darkaoui B Lafnoune A Chgoury F Daoudi K Chakir S Mounaji K et al . Induced pathophysiological alterations by the venoms of the most dangerous Moroccan scorpions Androctonus mauretanicus and Buthus occitanus: A comparative pathophysiological and toxic-symptoms study. Hum Exp Toxicol. (2022) 41, 09603271211072872. doi: 10.1177/09603271211072872
19
Habib AG Brown NI . The snakebite problem and antivenom crisis from a health-economic perspective. Toxicon. (2018) 150:115−123. doi: 10.1016/j.toxicon.2018.05.009
20
Rebahi H Ba-M’hamed S Still ME Mouaffak Y Younous S Bennis M . Clinical features and prognosis of severe scorpion envenomation in children. Pediatr International: Off J Japan Pediatr Soc. (2022) 64:e14687. doi: 10.1111/ped.14687
21
Ismail M . The scorpion envenoming syndrome. Toxicon. (1995) 33:825858. doi: 10.1016/0041-0101(95)00005-7
22
Gutiérrez JM Maduwage K Iliyasu G Habib A . Snakebite envenoming in different national contexts: Costa Rica, Sri Lanka, and Nigeria. Toxicon: X. (2021) 910:100066. doi: 10.1016/j.toxcx.2021.100066
23
Harrison RA Oluoch GO Ainsworth S Alsolaiss J Bolton F Arias A-S et al . Preclinical antivenom- efficacy testing reveals potentially disturbing deficiencies of snakebite treatment capability in East Africa. PloS Negl Trop Dis. (2017) 11:e0005969. doi: 10.1371/journal.pntd.0005969
24
Alirol E Sharma SK Bawaskar HS Kuch U Chappuis F . Snake bite in South Asia: A review. PloS Negl Trop Dis. (2010) 4:e603. doi: 10.1371/journal.pntd.0000603
25
Habib AG Musa BM Iliyasu G Hamza M Kuznik A Chippaux J-P . Challenges and prospects of snake antivenom supply in sub-Saharan Africa. PloS Negl Trop Dis. (2020) 14:e0008374. doi: 10.1371/journal.pntd.0008374
26
Brown NI . Consequences of neglect: analysis of the sub-saharan African snake antivenom market and the global context. PloS Negl Trop Dis. (2012) 6:e1670. doi: 10.1371/journal.pntd.0001670
27
Ahmed S Koudou GB Bagot M Drabo F Bougma WR Pulford C et al . Health and economic burden estimates of snakebite management upon health facilities in three regions of southern Burkina Faso. PloS Negl Trop Dis. (2021) 15:e0009464. doi: 10.1371/journal.pntd.0009464
28
Birte B-M . Evidence, Education, Empowerment: Health Action International Snakebite Programme – Kenya. Amsterdam, Netherlands: Health Action International (HAI) (2017).
29
Williams HF Layfield HJ Vallance T Patel K Bicknell AB Trim SA et al . The urgent need to develop novel strategies for the diagnosis and treatment of snakebites. Toxins. (2019) 11:Article 6. doi: 10.3390/toxins11060363
30
Laustsen AH . Antivenom in the age of recombinant DNA technology. In: Handbook of Venoms and Toxins of Reptiles, 2e éd. Boca Raton, Florida, USA: CRC Press (2021).
31
Habib AG . Venomous snakes and snake envenomation in Nigeria. In: Clinical Toxinology in Asia Pacific and Africa. Springer, Dordrecht (2015). p. 275298. doi: 10.1007/978-94-007-6386-9_32
32
Berg P Theart F van Driel M Saaiman EL Mavoungou L-B . Snakebite envenoming in Africa remains widely neglected and demands multidisciplinary attention. Nat Commun. (2024) 15:9598. doi: 10.1038/s41467-024-54070-y
33
Fereidooni R Shirzadi S Ayatizadeh SH Bahloul M Tavangar A Zomorodian SA et al . Scorpion envenomation-associated myocarditis : A systematic review. PLoS Negl Trop Dis. (2023) 17:e0011219. doi: 10.1371/journal.pntd.0011219
34
Dalhat MM Potet J Mohammed A Chotun N Tesfahunei HA Habib AG et al . Availability, accessibility and use of antivenom for snakebite envenomation in Africa with proposed strategies to overcome the limitations. Toxicon: X, (2023) 18, 100152. doi: 10.1016/j.toxcx.2023.100152
35
Omran MaA . Cytotoxic and apoptotic effects of scorpion Leiurus quinquestriatus venom on 293T and C2C12 eukaryotic cell lines. Journal of Venomous Animals and Toxins Including Tropical Diseases, (2003) 9, 255–76. doi: 10.1590/S1678-91992003000200008
36
Chippaux J-P . (2018). Snakebite envenomation turns again into a neglected tropical disease! Journal of Venomous Animals and Toxins Including Tropical Diseases, 23:38. doi: 10.1186/s40409-017-0127-6
37
Ministère de la Santé, Maroc . (2020). Available online at: https://www.sante.gov.ma/Pages/actualites.aspx?IDActu=371 (Accessed November 3, 2023)
Summary
Keywords
venomous animal, envenomation, public health, antivenom access, treatment strategies
Citation
Ammouch K, Mesmoudi N, Hammani N, Galan J, Moustaghfir A, Stöcklin R and Oukkache N (2025) Tackling the burden of envenomation in Africa: advances, challenges, and strategic priorities for enhanced diagnosis and treatment. Front. Trop. Dis. 6:1653213. doi: 10.3389/fitd.2025.1653213
Received
24 June 2025
Accepted
06 October 2025
Published
11 November 2025
Volume
6 - 2025
Edited by
Lucas Sousa Magalhães, Federal University of Alagoas, Brazil
Reviewed by
Michelle Yap, Monash University Malaysia, Malaysia
Sewbert Rodrigues Jati, Fundação de Medicina Tropical Doutor Heitor Vieira Dourado (FMT-HVD), Brazil
Updates
Copyright
© 2025 Ammouch, Mesmoudi, Hammani, Galan, Moustaghfir, Stöcklin and Oukkache.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Khawla Ammouch, khawla_ammouch@um5.ac.ma; Naoual Oukkache, naoual.oukkache@pasteur.ma
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.