Abstract
Africa continues to face numerous public health and humanitarian crises, including infectious disease epidemics and pandemics. These shocks have major impacts on health systems and socio-economic development. While countries have made progress in implementing the International Health Regulations (2005), the COVID-19 pandemic and the 2014-2016, West Africa Ebola Virus Disease epidemic revealed major inadequacies in containing major public health emergencies effectively and promptly. In an instant, these shocks brought the world to a standstill– tragically costing many lives with a severe toll on communities, societies, and economies. In this perspective, we urge African countries to accelerate integrating health security reforms into broader health systems strengthening. We propose a logical, system-wide approach, including a comprehensive gap assessment and analysis, followed by holistic planning and comprehensive reforms for improving key dimensions, including, service delivery, organizational and management processes; governance, leadership and coordination; predictable, scalable, and sustainable financing; surveillance and health information systems; quantity, quality and distribution of the health and care workforce; resilient health infrastructure; and finally local/regional manufacturing and procurement and supply chain management systems for health products and technologies. Positioning health security reforms as part of overall health systems strengthening will advance the primary health care approach, promote health security, and accelerate the achievement of universal health coverage (UHC). The latter will lead to equitable access to essential health services; better provision of efficient emergency response; and ultimately improved population health. Integrating investment in health security and UHC is a “double-win” and a pathway to achieve resilience.
Introduction
The emergence and re-emergence of infectious diseases of epidemic and pandemic potential along with other public health and humanitarian emergencies threatens the health of populations worldwide, with the highest burden in Africa (1). According to the International Health Regulations (IHR, 2005), as amended in 2024, “ a pandemic emergency is a public health emergency of international concern that is caused by a communicable disease and: (i) has, or is at high risk of having, wide geographical spread to and within multiple states; and (ii) is exceeding, or is at high risk of exceeding the capacity of health systems to respond in those states; and (iii) is causing, or is at high risk of causing substantial social and or economic disruption, including disruption to international traffic and trade; and (iv) requires rapid, equitable, and enhanced coordinated international action, with whole-of-government and whole-of-society approaches (2). While African countries have made progress in the IHR implementation, the COVID-19 pandemic, and West Africa Ebola Virus Disease (EVD) epidemic revealed inadequacies, similar in other regions, in preparedness and health systems resilience (3, 4). It is crucial therefore to identify and apply fundamental lessons learnt in responding to the COVID-19 pandemic and the West Africa EVD epidemic to build resilience to tackle current and future shocks in Africa.
Advancing global health security and resilient health systems
Global health security (GHS) concerns the activities required (proactively and reactively) to minimize the vulnerability to any public health emergencies that endanger the collective health of populations, across geographical regions and international boundaries (5). Health security becomes a general security and development concern when it threatens a nation’s ability to function and safeguard its citizens’ welfare, including provision of basic services. COVID-19 showed the critical need to develop a holistic approach to health, emphasizing both health security-controlling health emergencies, and health development-tackling upstream causes and determinants (6). Inevitably, we need resilient health systems with the capacity to proactively foresee, absorb, recover from, and adapt to shocks, including epidemics, pandemics, climate change related disasters, geopolitical conflicts, and cyberthreats (7). A resilient system that ensures the continuity of essential health services during shock events, is a necessity for health security and universal health coverage (UHC) goals (6, 7).
Public health emergencies affect all four interconnected health system outputs, namely, access, quality, demand, and resilience (8). Recent major shock events have highlighted the vulnerability of health systems across the world, and the need for an integrated approach to health system strengthening, bringing together health security, disease-specific and life course-specific programmes to make progress towards UHC and health security goals. These shocks not only introduce new threats, but also draw existing health system resources away from routine essential services, undermining progress towards health goals (9).
As countries embrace the current fiscal constraints, bolstering the overall capacity of health systems is more critical than ever. Health system resilience must be prioritized as a requirement for health systems that deliver efficient, equitable and quality essential health and related services that people need for their health and wellbeing, even during shock events (8). During policy formulation, planning and budgeting, promoting health security has to be an intended outcome of health systems strengthening.
Learning from COVID-19, the World Health Organisation (WHO), in 2024, formulated its fourteenth general programme of work (GPW-14) to guide technical and other support to countries over the period 2025-2028 (10). The overarching goal of the WHO-GPW-14 is to promote, provide and protect health for all people in the world (10). The WHO-GPW-14 calls upon all countries to accelerate efforts to build and sustain resilient health systems capable of preventing, preparing for, timely detecting, and effectively and promptly responding to all public health and humanitarian emergencies.
In this perspective, we urge all African countries to urgently adapt the proposals in the WHO-GPW-14 to foster integrated approaches to health systems strengthening with the ultimate goal of improving population health, ensure equitable access, and provide responsive care.
A logical health system-wide approach
Individual health programmes typically provide a time-bound results-orientation for a particular intervention or disease. However, even when specific programmes are well-run, if they duplicate or misalign responsibilities with one another or with the rest of the health system, they can impose high costs when viewed from a wider perspective (11). As countries seek to expand and sustain coverage in the current reduced fiscal space, a holistic perspective that embeds health programmes within the overall health system can identify areas to improve efficiency in how resources are allocated and deployed.
System-wide gap identification and analysis
First, gaps in the availability and functionality of the IHR (2005) core capacities should be periodically assessed using the IHR monitoring and evaluation framework (IHR-MEF) (Table 1) (12). Importantly, hazard specific readiness assessments should be conducted. Similarly, gaps in the availability and functionality of essential public health functions (EPHFs) should be identified and analyzed through periodic health system assessments (covering health financing, Health and care workforce, medicines, and supply chains (13–15). Furthermore, health systems resilience gap analysis and testing should be institutionalized using standardized tools (16, 17). Data from the system wide assessments should be consolidated and synthesized to form the basis for the formulation of integrated policies and plans.
Table 1
| States Parties Self-Assessment Annual Reporting (SPAR) | Voluntary Joint External Evaluation (JEE) | After Action Reviews (AAR) and Intra-Actions Reviews (IAR) | Simulation and Exercises (SimEx) | |
|---|---|---|---|---|
| Purpose | Monitoring progress in the implementation of the IHR | Objectively evaluates IHR contribution to health security | Assesses the functionality of capacities during real events | Assesses potential functionality of capacities in the absence of real events |
| Mandate | Mandatory | Voluntary | Voluntary | Voluntary |
| Focus | Availability of capacities | Availability of Capacities | Functionality of capacities | Functionality of Capacities |
| Periodicity | Annually | Every 4–5 years | Within 3 months after end of event for AAR OR During a real event for IAR |
Regularly as required to test capacities |
| Type | Quantitative | Quantitative | Qualitative | Qualitative |
The four components of the international health regulations (2005) monitoring and evaluation framework (IHRMEF).
Holistic policy formulation, planning and budgeting
Countries should formulate integrated policies and develop costed health sector strategic and development plans (HSSDPs), providing scope to facilitate transition and integration of various disease specific and other vertical plans. The WHO-GPW-14 (10), and health emergency prevention, preparedness, response, and resilience (HEPPR) framework endorsed by the 75th World Health Assembly should serve as guiding references (Figures 1, 2) (18). Importantly, the plans should align with country financing cycles and should be funded more from domestic financing. Moreover, both the HSSDPs and the national action plans for health security (NAPHS) should be better synergized, aligned and coordinated to ensure that IHR (2005) core capacities build health systems resilience, strengthen essential public health functions, and are underpinned on the - “One-Health approach” - (19–22). We urge countries to ensure that NAPHS activities and budgets are fully integrated into the HSSDPs which should be incorporated into national budget development cycles. This synergy is likely to improve overall health sector planning, investment in primary health care and essential public health functions, while addressing gaps in health security and health systems foundations.
Figure 1
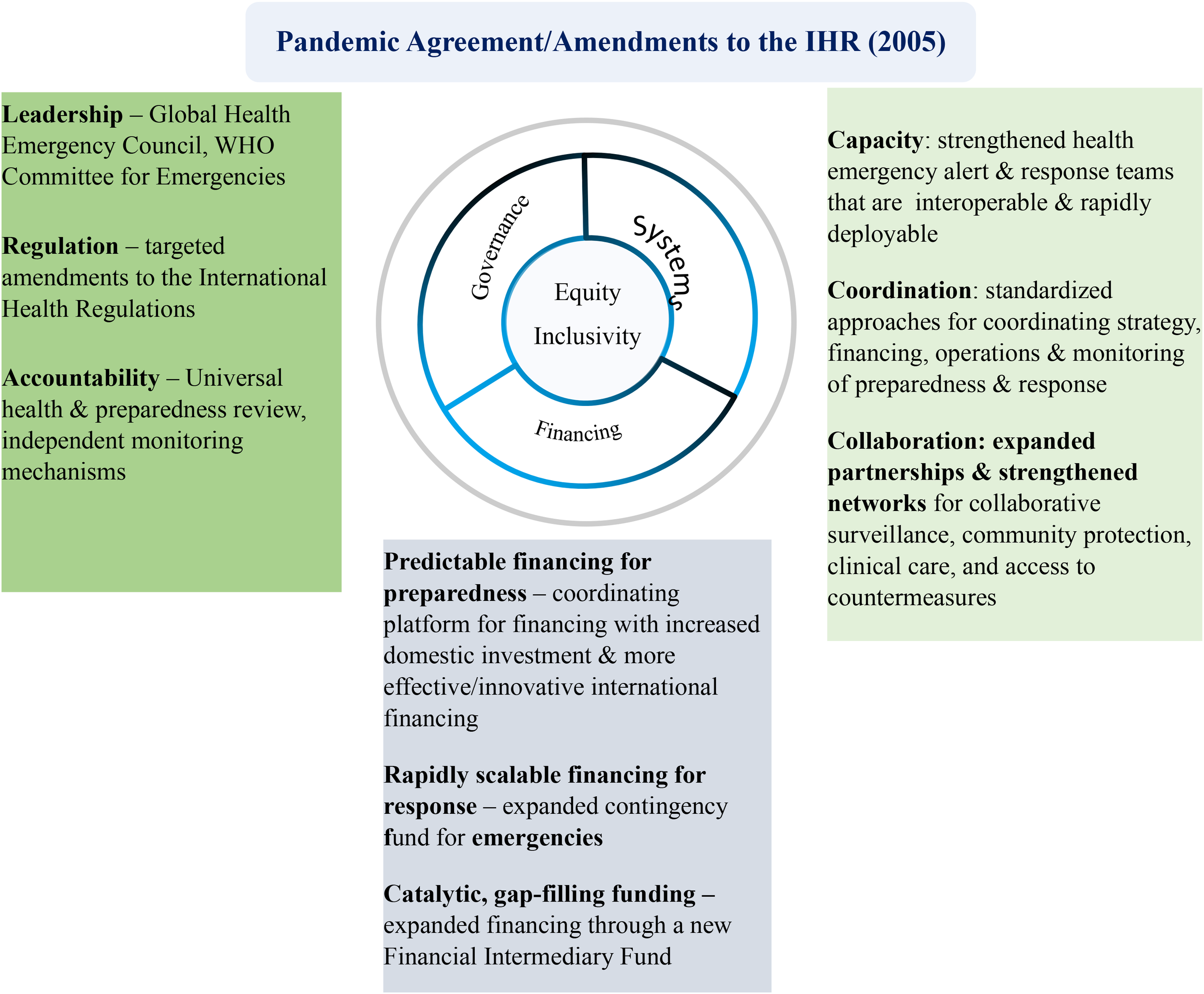
Learning from COVID-19: Ten WHO proposals to strengthen the global architecture for health emergency prevention, preparedness, response, and resilience. (Adapted from reference 18).
Figure 2
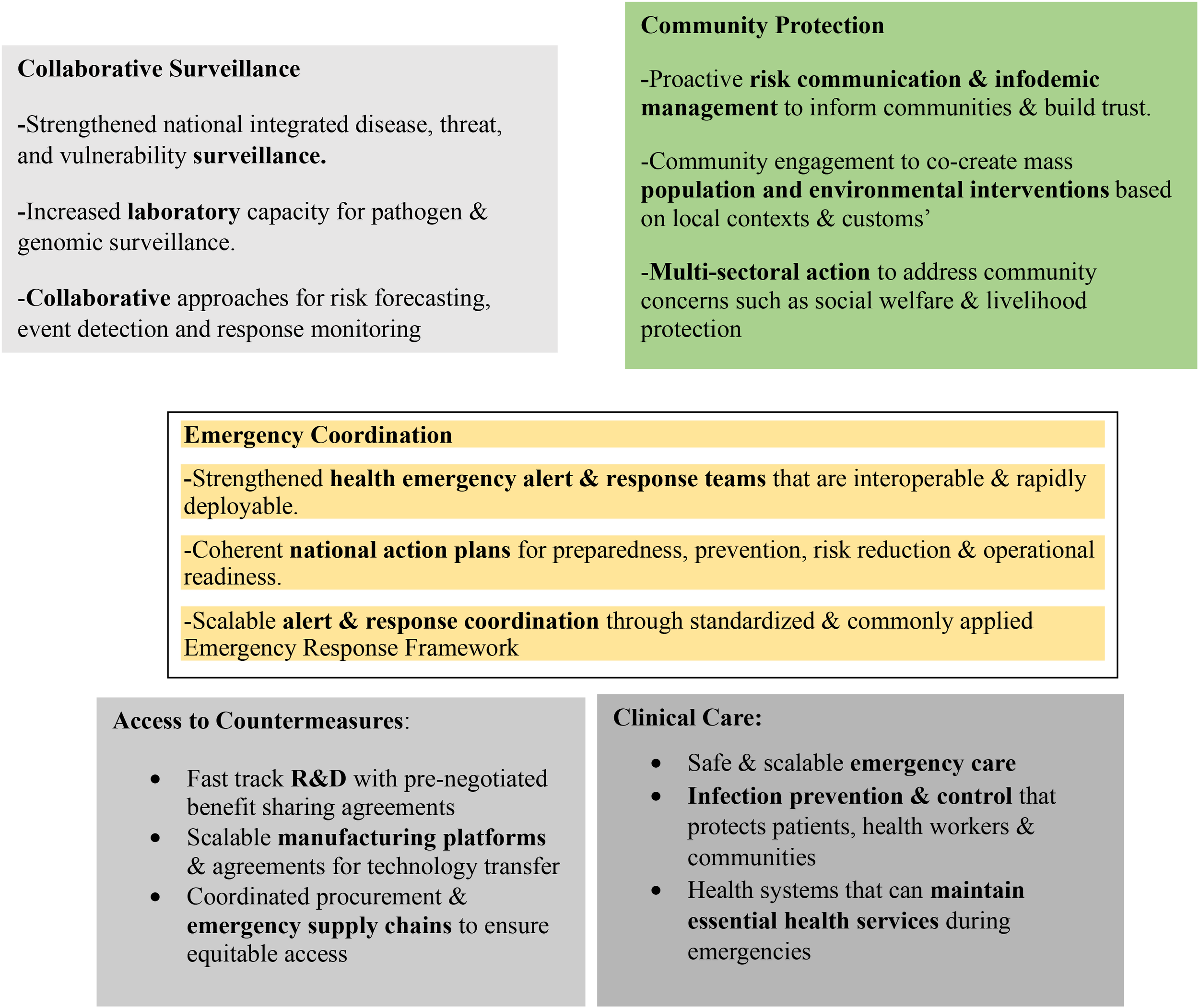
Five interconnected systems of core capabilities and solutions-the 5Cs. (Adapted from reference 18).
Positioning health security reforms as part of overall health systems reforms
Following West Africa EVD outbreak, in 2016 the WHO health emergencies (WHE) programme was established to consolidate and strengthen emergency preparedness and response. It integrated all WHO’s emergency-related activities under a unified structure, aiming at enhancing operational capacity and coordination; strengthening financial and human resource processes; improving preparedness; addressing gaps in response; and ensuring accountability and transparency (23). Determined to change the status quo, the health security, and emergencies (HSE) cluster in the WHO African region also undertook reforms to transform its response to multiple health emergencies including significant strides to support countries to better manage and respond to shock events. The support came in forms such as strategy formulation for health security and emergencies and revising the integrated disease surveillance and response (IDSR) strategy (24, 25). As of December 2024, the reforms had resulted in 17 out of 18 outbreaks of either EVD or Marburg Virus Disease (MVD), that occurred between 2016 and 2023, being brought under control with no cross-border spread (26). There was a 50% improvement in the timeliness of outbreak detection and the overall time to contain outbreaks reduced by 60% (156 days in 2017 to 63 days in 2023). Additionally, similar achievements were witnessed in the response to vector-borne diseases such as yellow fever, dengue and leishmaniasis, whose containment time decreased from 234 days to just 16 days; vaccine-preventable diseases such as diphtheria, from 308 days to 56 days; and viral hemorrhagic diseases, from 106 days to 48 days (26). Underpinning the response to all emergencies is a standardized three-level emergency response framework (27).
While these reforms have led to a positive impact, the current decline in development assistance necessitates positioning health security reforms as part of comprehensive health systems reforms to improve overall functionality and performance. Hereunder, we propose comprehensive reforms for improving key health dimensions (Figure 3).
Figure 3
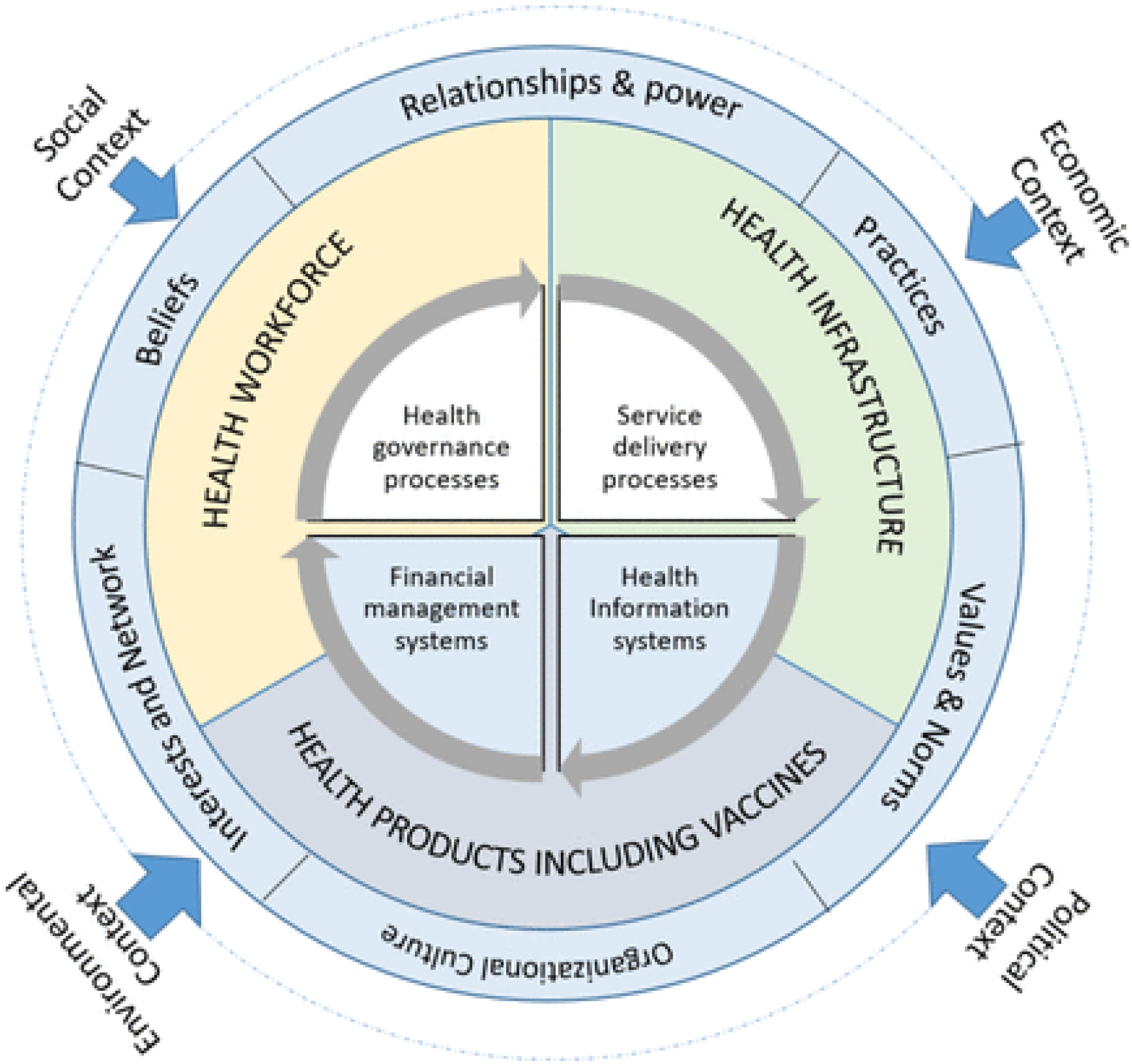
Functional health system components and building inputs. (Adapted from reference 8).
Service delivery organizational and management processes
Sustaining the provision of essential health services should be a major consideration for all health systems. Although the development of essential health service packages (EHSP) is an established tradition in countries, outbreak response experiences teach us lessons that sharpen our understanding to anticipate and mitigate their impacts. The design of EHSP must therefore reflect such awareness. First, countries should define their EHSP that should be available by level of the heath system from primary to tertiary care. Second, in periods of normalcy, countries should strengthen the organizational and management processes to deliver the EHSP based on past experiences (Table 2). Third, countries should invest in staff, infrastructure and supplies needed to sustain the EHSP. Fourth, during shock events, there should be robust tracking of the disruption of essential services, along with tracking emergency response metrics. Importantly, countries need to model and plan for different scenarios of EHSP and models of care that ensure continuity in provision of essential services in contexts of different emergencies (Table 2). Finally, lessons need to be documented and used to further strengthen health system resilience to withstand future shocks.
Table 2
| Targeted system resilience | Inherent system resilience | |
|---|---|---|
| Potential shocks | • Contagion-Viral Hemorrhagic Disease Outbreak. • Severe Respiratory Disease Outbreak- Influenza, COVID-19, SARs. • Vaccine Preventable Diseases-VPDs-Measles, Poliomyelitis. • Waterborne Disease Outbreak-Diarrheal Syndromes’-Cholera, Shigellosis, Typhoid, E-Coli. • Vector Borne Disease Outbreak- Malaria, Yellow Fever, Dengue, Crimean Congo Hemorrhagic Fever (CCHF). • Food Poisoning Disease Outbreak-Salmonella, • Zoonotic Disease Outbreaks- Rift Valley Fever, Marburg Virus Disease, Anthrax. • Natural disasters- Mudslides, Drought, Floods, Cyclones) • Mass Causalities (Human made non-intentional-Road Traffic Injuries, Plane and Train crashes. • Human-made-intentional-Bomb Blasts. • Antimicrobial Resistance (AMR)-MDR and XDR TB • Chemical events • Radio-nuclear emergencies |
• Prediction and forecasting systems. • Sound routine vaccination programmes. • Sound surveillance and response systems for each syndrome. • Sound Laboratory systems. • Risk communication and community engagement. • Sound infection prevention and Control systems. • Robust border health and point of entry capacities. • Safe and scalable emergency care infrastructure to deal with the first 10–15 patients for each syndrome at district level-clinical management pathways, case management treatment centers (CTUs), intensive care units (ICUs), high-dependency care units (HDCUs). • Adequately trained human resources (HR) for each syndrome. • Adequate operational supplies and logistics (OSL) systems for each syndrome by level. • Prediction capacity in animal and environmental health sectors. • Ambulance referral systems. • Blood transfusion services. • Decontamination capacities. • Negative pressure rooms. |
| Desired situation | Mitigate: Avoid / ensure shock event does not occur in the coming 12 months. Prevent: Appropriate capacity to know if shock event is imminent (prediction and forecasting), pre-exposure vaccination. Detect: Sound surveillance and laboratory systems. Respond: Availability of the required infrastructure, staff, and products to avoid any deaths due to shock event. Recover: Document and learn lessons that can be used to better prepare for shock event in the future. |
Anticipate: Have the ability to pick up on time, any disruptions to provision of essential services Absorb: Know how we can boost the existing capacity to ensure it can sustain routine services as it responds to shocks Adapt: Know how to quickly modify the system organization to make it appropriate for changing needs during a shock event Transform: How to institutionalize system modifications that allow better response to shocks |
Example of mapping the situation for targeted and inherent system resilience building based on known shock event syndromes.
Governance, leadership, and coordination
Governance, leadership, and coordination processes are critical for a well-functioning health system and for promoting health security. Governance provides the framework for decision-making and accountability, while leadership provides the vision and direction for achieving goals (28). Effective coordination ensures that all parts of the system work together efficiently. There is therefore a need for countries to have an enabling legislative, regulatory and policy environment to advance the integration of strategies for health systems strengthening and promoting health security. This will facilitate, for example, the implementation of the IHR (2005) as amended in 2024, including the designation of the IHR national focal points and the national IHR authorities, as well as supporting the implementation of the pandemic agreement, when it comes into force (2, 29, 30). The governance and coordination mechanisms proposed in recent global and regional frameworks need to be domesticated at the country level. For example, the Pandemic Agreement adopted in 2025 and the amendments to the IHR, such as the designation or establishment of national IHR authorities are likely to improve coordination of the implementation of the IHR (2005) within and between countries. However, the main challenge at country level is where to situate the IHR national authority to ensure it is functional and operational and underpinned on the One health approach”.
Importantly, it will be critical to set up standardized, integrated, and multi-sectoral mechanisms for coordinating strategy, resource mobilization, financing, operations, and monitoring and evaluation. At the regional/continental level, there will be a need for frameworks, guidance, and standards; coordination mechanisms for external technical and financial support; expanded strategic partnerships and collaboration for the provision of knowledge, skills, resources, and finally, continental/regional mechanisms for regulatory harmonization and research governance.
Enhancing sub-national programmes-”district”-led programming
“District” in the context of this paper is the administrative level below the national level. In some federal systems this may be a state, a province, or a region. We urge countries to strengthen “district”-led programming and planning. This will entail strengthening the performance of the health system inputs in each “district” while mainstreaming emergency preparedness and response capacities into each health system building input and service delivery platforms. In Africa, it is important to strengthen the “district” as the operational unit for primary healthcare, and is generally the first point of entry for epidemics. Information from the private sector should be made available to the public sector when managing epidemics. The private sector must no longer operate in silos but must also report to the “district” health authorities in which they operate, with a referral and counter-referral system and using the same information system and tools (case notification, contact tracing, etc.).
In addition, the DLP can facilitate the functionality of district public health emergency operation centers (PHEOCs), district incident management systems (D-IMS), task forces/committees and multi-sectoral and multi- disciplinary district rapid response teams (D-RRTs). D-RRTs, which are often composed of a single sector, must follow a One Health approach. Districts should have funding for transporting samples from remote rural areas to reference laboratories. Finally, it is important that there is a multisectoral coordination mechanism at the decentralized levels in order to operationalize “One Health Approach”, which has very often remained at the central level.
For border districts the DLP can support capacity building at designated points of entry (PoE) in line with the guidance for the assessment of the availability and functionality of PoE capacities, contingency planning under the IHR (2005), and implementing routine and emergency border health interventions. Barriers to institutionalization should be identified from the outset to ensure success, including stewardship from national levels, availability of guidelines, and clear key performance indicators (KPIs) for the integration (31).
Strengthening community systems and tools for community protection
Countries should strengthen community systems and primary care as well as their linkages, to prevent, detect and respond to outbreaks, including proactive risk communication and community engagement (RCCE) and infodemic management to inform communities and build trust. Community engagement to co-create mass population and environmental interventions based on local contexts and customs; and multi-sectoral action to address community concerns such as social welfare and livelihood protection.
Sustainable financing systems
Countries should develop financing strategies to ensure predictable financing for health security as core to building resilient health systems. This will require coordinating platforms for financing with increased domestic investment and more effective and innovative private and external financing. We urge countries to conduct resource mapping exercises for the implementation of the HSSDPs and NAPHS. These exercises should not be duplicated by donor partners and should be conducted in an integrated manner. A key challenge at country level is inefficiencies in health sector budget execution, with often unspent funds returned to the Ministry of Finance and redirected to other sectors.
To increase domestic financing, there is a need to engage legislators and local governments to advocate for increased domestic financing for health in line with the 2001 Abuja declaration (32). Further, countries could scale up social health insurance (SHI) schemes, a form of financing and managing health care based on risk pooling (33). To facilitate rapid response, countries need to set up rapidly scalable financing for response – a contingency fund for emergencies. However, to avoid fragmenting health financing systems in terms of managing multiple funds, the contingency fund for emergencies should be part of a unified health financing system governed by a robust and efficient public financial management (PFM) framework. Such systems must be adaptable and responsive, while ensuring value for money and safeguarding against fraud and corruption. African countries can implement several immediate measures to strengthen their PFM systems in support of emergency response efforts. The flexibility of country budgets has enabled many countries to increase budget transfers to sub-national entities and health purchasers during emergency periods (https://blogs.worldbank.org/en/governance/getting-government-financial-management-systems-covid-19-ready).
Importantly, African countries should leverage existing fiscal space for integrated health sector planning, consistent with the Lusaka Agenda (34), and global aid effectiveness commitments including the Paris declaration, the Accra agenda for Action, and the Busan partnership for effective development cooperation (35–37). This will require to increasingly align with the Lusaka agenda encompassing relevant external support, consistent with their economic and development priorities. Programmatic actions are more likely to achieve high coverage and sustainability when they are integrated into national mechanisms-from policy to strategic planning, budgeting, and resource allocation. Finally, prioritizing domestic financing for core health system interventions, with external partners playing a complementary and catalytic role.
Health information systems and innovative technologies
There is a need to strengthen national integrated disease, event, and conditions surveillance, but also risk, threat, and vulnerability surveillance, including mortality surveillance. Importantly, there is a need to increase access to laboratory capacity for serology, pathogen, and genomic surveillance. For some countries this may be possible in-country, while for others like the small island developing states (SIDs) there may be a need to set up sample transport systems to reference laboratories outside the country. Importantly, collaborative approaches for risk forecasting, event detection and response monitoring are needed at continental, regional, sub-regional and national level. This necessitates a paradigm shift from information management to outbreak intelligence, where the emphasis is on understanding risk patterns and response impact to guide resilience and system investments.
We urge all countries to leverage the opportunities offered by digital technology and artificial intelligence to scale up digital transformation, including inter-operable and interconnected electronic information systems linking human, animal and environmental surveillance and laboratory data systems; improving surveillance data quality, reporting rates, analysis, and use for real-time decision making; strengthening laboratory information management systems and institutionalizing simulations and exercises to test the functionality of the IHR and health systems core capacities, underpinned on multisectoral accountability.
Health and care workforce
COVID-19 unraveled major gaps in the availability and distribution of the HWF. There are some “orphan cadres” that urgently need affirmative action, including mental health and psychosocial support (MHPSS) experts, anthropologists and social scientists, logisticians, and severe respiratory disease care experts. Countries need to review and assess their HWF status and their distribution to develop or update their strategies to strengthen the HWF by focusing on quality education and training, recruitment, deployment, morale, retention, and career pathways. This should include addressing shortages and improving training quality and accessibility. Importantly, the HWF strategies should be informed by “One Health” mapping of human resources, training needs assessments and health labor market analysis (HLMA) to streamline recruitment processes within the public sector to ensure timely and efficient hiring of healthcare professionals. Countries are urged to use a comprehensive health labor market framework to analyze and develop policy options in the following four main areas: production, inflows and outflows, maldistribution and inefficiencies, and regulation (38).
Where necessary countries should scale up and strengthen the capacity of community health workers (CHWs), including standardizing their training and investment in their retention and integration within the overall HWF. In addition, there is a need to review and formulate employment policies that provide for quick repurposing and national service. Finally, it will be crucial to train and keep a database of multi-disciplinary health emergency preparedness and response surge teams that are interoperable, scalable, and rapidly deployable as and where needed, depending on the shock syndrome (Table 2).
Resilience in health infrastructure
Appropriate and resilient health infrastructure is the foundation for GHS and UHC and assures local communities’ confidence in access and supply. The right facility structure is also necessary to optimize patient and health and care worker flows, including adequate spaces for patient cohorting, triage and isolation for infection prevention and control (IPC) purposes. However, health service infrastructure is sadly insufficient or inadequate in Africa and thus requires improvement (39). Infrastructure needs to be designed with a possibility of being repurposed for different emergencies. This will require leveraging on emergency resources to put in place permanent infrastructure and equipment that strengthen the system “building back better after each emergency”.
Investing in health infrastructure today can support systems transformation and create sustainable health services. During the peak of the COVID-19 first wave, the Ghana COVID-19 Private Sector -led initiative provided a prompt response to COVID-19 by mobilizing a combination of public sector, private sector, and philanthropy partners and instead of setting up a “makeshift” COVID-19 treatment center, built the Ghana Infectious Disease Centre (GIDC) (40). The GIDC (100-bed hospital in Accra), the first infectious disease center in Ghana now provides the needed health services to the city. We urge countries to develop comprehensive and balanced approaches across the entire scope of PHC service delivery infrastructure. Nationally owned health infrastructure plans should be aligned with national health plans and be included as key components of social and economic development strategies. Countries should build fit-for-purpose health facilities now and in the future that are safe, functional, scalable, climate and disaster resilient and with dedicated budget for environmental impact assessments and maintenance (Table 2).
Continental, regional, and national manufacturing, procurement, and supply management systems for health products and commodities
In collaboration with relevant partners, African countries need to advance research and development (R&D) for vaccines, therapeutics, and diagnostics, with pre-negotiated benefit-sharing frameworks where the terms as to how benefits will be shared from R and D activities, particularly those involving biological resources, are agreed upon in advance (41). Africa also needs to leverage on emergencies to catalyze local manufacturing capacity, harmonization of regulation, market shaping including pooling of procurements. Countries should use the opportunities offered by the Africa Continental Free Trade Area (AfCFTA) and regional economic communities RECs) free trading treaties and protocols to develop regional scalable manufacturing platforms for new technologies and health products, with consistent quality across different manufacturing sites. It will be critical to establish and strengthen coordinated procurement and emergency supply chains to ensure equitable access to essential goods, considering vulnerable and hard to reach communities. We advocate for advancing models that support pooling resources and demand to negotiate better prices, optimize logistics, and ensure a more reliable supply of essential health commodities and equipment. Finally there is a need to support countries to review/update the procurement supply chain management systems for health commodities; update guidelines and lists of essential items needed during emergencies to allow for faster procurement and distribution; ensure effective coordination between governments, international organizations, and the private sector. Finally, we call upon countries to utilize technology for tracking supplies, forecasting demand, and optimizing logistics to improve efficiency and transparency.
“Parting shots”
To effectively respond to and mitigate the cross-sectoral impacts of public health emergencies, health security efforts are crucial. However, health security efforts alone are likely to be insufficient if they overlook broader health systems strengthening, which are underfunded, fragmented, under resourced and inequitable (42). There can’t be sustainable health security capacities without resilient health systems with EPHFs and adequate resources at all levels. Strong health systems are the foundation for effective health security, but health security interventions also enhance the overall health system functions. Building strong primary healthcare networks and strengthening essential public health functions (like disease surveillance, laboratory capacity, emergency preparedness and enabling IHR implementation) are crucial for both UHC and health security. Collaboration across different sectors (Human and animal health, environment, finance) is essential for addressing the complex factors that affect health security and building a resilient system.
Conclusion
During COVID-19, most countries faced challenges in sustaining an effective response over the course of the pandemic. Health systems that were more resilient with health security preparedness and services continuity performed better to protect their citizens against the social and economic impacts of the pandemic (43). It is therefore imperative that we simultaneously accelerate the achievement of UHC and advancing health security. Mobilizing investments in an integrated health system approach represents a “double-win”.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
AT: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. HK: Writing – original draft, Writing – review & editing. SS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. BD: Writing – original draft, Writing – review & editing. GB: Writing – original draft, Writing – review & editing. JN-O: Writing – original draft, Writing – review & editing. DC: Writing – original draft, Writing – review & editing. AG: Writing – original draft, Writing – review & editing. FK: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1
Talisuna AO Okiro EA Yahaya AA Stephen M Bonkoungou B Musa EO et al . Spatial and temporal distribution of infectious disease epidemics, disasters, and other potential public health emergencies in the World Health Organisation Africa. Globalization Health. (2020) 16. doi: 10.1186/s12992-019-0540-4
2
World health Oranisation (WHO) . International Health Regulations (2005) as amended (2024). Available online at: https://apps.who.int/gb/ebwha/pdf_files/WHA77/A77_ACONF14-en.pdf (Accessed August 12, 2025).
3
United Nations . Impact of COVID-19 and responses in landlocked developing countries (2021). Available online at: https://www.un.org/ohrlls/sites/www.un.org.ohrlls/files/impact_of_covid19_and_responses_in_lldcs.pdf (Accessed August 12, 2025).
4
Kyobe Bosa H Kamara N Aragaw M Wayengera M Talisuna A James Bangura J et al . The west Africa Ebola virus disease outbreak: 10 years on. Lancet Glob Health. (2024) 12:7e1081–e1083. doi: 10.1016/S2214-109X(24)00129-3
5
World Health Organisation (WHO) . Health Security . Available online at: https://www.who.int/health-topics/health-securitytab=tab_1 (Accessed August 12, 2025).
6
McInnes C Roemer-Mahler A . From security to risk: reframing global health threats. Int Affairs. (2017) 93:1313–37. doi: 10.1093/ia/iix187
7
World Health Organisation . Building health system resilience to public health challenges: guidance for implementation in countries (2024). Available online at: https://www.who.int/publications/i/item/9789240094321 (Accessed August 12, 2025).
8
Karamagi HC Tumusiime P Titi- Ofei R Droti B Kipruto H Nabyonga-Orem J et al . Towards universal health coverage in the WHO African Region: assessing health system functionality, incorporating lessons from COVID-19. BMJ Global Health. (2021) 6:e004618. doi: 10.1136/bmjgh-2020-004618
9
Karamagi HC Titi-Ofei R Kipruto HK Benitou A Seydi AB-W Droti B Talisuna A et al . On the resilience of health systems: A methodological exploration across countries in the WHO African Region. PLoS ONE (2022) 17:e0261904. doi: 10.1371/journal.pone.0261904
10
World Health Organisation . Global Health Strategy and Fourteenth General Programme of Work 2025–2028 (2024). Available online at: https://www.who.int/about/general-programme-of-work/fourteenth (Accessed August 12, 2025).
11
World Health Organisation . A System Wide Approach To Assessing Efficiency Across Programmes (2017). Available online at: https://www.scribd.com/document/770448427/A-system-wide-approach-to-assessing-efficiency-across-programmes (Accessed August 12, 2025).
12
World Health Organisation . International Health Regulations Monitoring and Evaluation Framework (IHR MEF) (2016). Available online at: https://www.who.int/emergencies/operations/international-health-regulations-monitoring-evaluation-framework (Accessed August 12, 2025).
13
World Health Organisation . Health Equity Assessment Toolkit . Available online at: https://www.who.int/data/inequality-monitor/assessment_toolkit (Accessed August 12, 2025).
14
Herold KR . UHC 2030 Technical Working Group on Health Systems Assessments, review of health system assessment tools and approaches (2017). Available online at: https://www.uhc2030.org/fileadmin/uploads/uhc2030/1_Who_we_are/1.3_Governance/UHC2030_Working_Groups/2017_Health_Systems_Assess_Working_Group/First_face_to_face_meeting_2017/D1_Rohrer_Consultant.pdf (Accessed August 12, 2025).
15
World Health Organisation . Health systems resilience toolkit: a WHO global public health good to support building and strengthening of sustainable health systems resilience in countries with various contexts (2022). Available online at: https://www.who.int/publications/i/item/9789240048751 (Accessed August 12, 2025).
16
World Bank Group . Strategic Investment for Health System Resilience: A Three-Layer Framework (2024). Available online at: https://documents1.worldbank.org/curated/en/099623011052446919/pdf/IDU122ce063d1da0c14d271b08d18d75d51511e4.pdf (Accessed August 12, 2025).
17
World Health Organization . Health Systems Resilience Simulation Exercises (2021). Available online at: https://www.who.int/teams/primary-health-care/health-systems-resilience/integrated-health-system-strengthening/health-systems-resilience-simulation-exercises (Accessed August 12, 2025).
18
World Health Organisation . Strengthening health emergency prevention, preparedness, response and resilience (2023). Available online at: https://cdn.who.int/media/docs/default-source/emergency-preparedness/who_hepr_wha2023-21051248b.pdf (Accessed August 12, 2025).
19
World Health Organisation . NAPHS for all: A country implementation guide for national action plan for health security (NAPHS) (2025). Available online at: https://iris.who.int/bitstream/handle/10665/380231/9789240104983-eng.pdf?sequence=1 (Accessed August 12, 2025).
20
World Health Organisation . WHO benchmarks for strengthening health emergency capacities (2023). Available online at: https://iris.who.int/bitstream/handle/10665/375815/9789240086760-eng.pdf?sequence=1 (Accessed August 12, 2025).
21
World Health Organisation . NAPHS Planning and Costing Tool (2024). Available online at: https://extranet.who.int/sph/naphs-planning-and-costing-tool (Accessed August 12, 2025).
22
World Health Organisation . REMAP Online Tool – User Manual, Version June 2025 (2025). Available online at: https://extranet.who.int/sph/sites/default/files/2025-06/REMAP%20Online%20Tool_User%20Manual_200625_0.pdf (Accessed August 12, 2025).
23
World Health Organisation . Ebola Interim Assessment Panel: Report by the Secretariat (2015). Available online at: https://www.who.int/publications/i/item/ebola-interim-assessment-panel-report-by-the-secretariat (Accessed August 12, 2025).
24
World Health Organisation, Regional Committee for Africa . Regional Strategy for Health Security and Emergencies 2016–2020, Report of the Secretariat (2016). Available online at: https://www.afro.who.int/sites/default/files/2017-07/afr-rc66-6-en-2107.pdf (Accessed August 12, 2025).
25
World Health Organisation, Regional Committee for Africa . Regional Strategy for Integrated Disease Surveillance and Response: 2020–2030, Report of the Secretariat. Brazzavile, Republic of Congo (2019).
26
World Health Organisation, Regional Office for Africa . A Decade of Transformation 2015–2024: Improving the Health of the People of Africa (2025). Available online at: https://www.afro.who.int/sites/default/files/2025-02/WHO-AFRO_RD-Legacy-Book_DIGITAL_EN_0.pdf (Accessed August 12, 2025).
27
World Health Organisation . Emergency response framework (ERF), Edition 2.1 (2024). Available online at: https://iris.who.int/bitstream/handle/10665/375964/9789240058064-eng.pdf?sequence=1 (Accessed August 12, 2025).
28
World Health Organisation . Leadership and Governance (2010). Available online at: https://cdn.who.int/media/docs/default-source/service-availability-and-readinessassessment(sara)/related-links-(sara)/who_mbhss_2010_section6_web.pdf?sfvrsn=71928980_3 (Accessed August 12, 2025).
29
World Health Organisation (WHO) . Health systems for health security: a framework for developing capacities for international health regulations, and components in health systems and other sectors that work in synergy to meet the demands imposed by health emergencies (2021). Available online at: https://iris.who.int/bitstream/handle/10665/342006/9789240029682-eng.pdf?sequence=1 (Accessed August 12, 2025).
30
World Health Organisation . World Health Assembly adopts historic Pandemic Agreement to make the world more equitable and safer from future pandemics (2025). Available online at: https://www.who.int/news/item/20-05-2025-world-health-assembly-adopts-historic-pandemic-agreement-to-make-the-world-more-equitable-and-safer-from-future-pandemics (Accessed August 12, 2025).
31
Nanyonjo A Kertho E Tibenderana J Källander K . District health teams’ Readiness to institutionalize integrated community case management in the Uganda local health systems: A repeated qualitative study. Global Health: Sci Pract. (2020) 8:190–204. doi: 10.9745/GHSP-D-19-00318
32
World Health Organisation . The Abuja Declaration: Ten Years On (2011). Available online at: https://iris.who.int/bitstream/handle/10665/341162/WHO-HSS-HSF-2010.01-eng.pdf (Accessed August 12, 2025).
33
Acharya A Vellakkal S Taylor F Masset E Satija A Burke M et al . The Impact of Health Insurance Schemes for the Informal Sector in Low- and Middle-Income Countries: A Systematic Review. World Bank Research Observer (2012). doi: 10.1093/wbro/lks009
34
Future of Global Health Initiatives (FGHI) . The Lusaka agenda: conclusions of the future of global health initiatives process (2023). Available online at: https://d2nhv1us8wflpq.cloudfront.net/prod/uploads/2023/12/Lusaka-Agenda.pdf (Accessed August 12, 2025).
35
Organisation for Economic Co-operation and Development (OECD) . Paris Declaration on Aid Effectiveness (2005). Available online at: https://www.oecd.org/en/publications/2005/03/paris-declaration-on-aid-effectiveness_g1g12949.html (Accessed August 12, 2025).
36
Global Partnership for Effective Development Cooperation . The Accra agenda for action (AAA) (2008). Available online at: https://www.effectivecooperation.org/system/files/2020-09/Accra%20Agenda%20for%20Action.pdf (Accessed August 12, 2025).
37
The Busan Partnership for Effective Development Cooperation . (2012). Available online at: https://www.dev-practitioners.eu/media/key_documents/Busan_partnership.pdf (Accessed August 12, 2025).
38
Sousa A Scheffler RM Nyoni J Boerma T . A comprehensive health labour market framework for universal health coverage. Bull World Health Organ. (2013) 91:892–894. doi: 10.2471/BLT.13.118927
39
The World Bank . Resilient, Green, and Inclusive Health Facilities: Guidance on Planning, Design, and Operation (2025). Available online at: https://documents1.worldbank.org/curated/en/099032725113028865/pdf/P178556-4158cc18-04a0-4127-a787-79810ee19264.pdf (Accessed August 12, 2025).
40
Ghana Infectious Disease Centre (GIDC) . IDC . Available online at: https://edgebuildings.com/project-studies/Ghana-infectious-disease-center/ (Accessed August 12, 2025).
41
Zhai Y Hong G Jiang M Wei Q . Access and benefit-sharing of the pathogenic microorganisms such as SARS-CoV-2. Biosaf Health. (2022) 4:414–20. doi: 10.1016/j.bsheal.2022.05.003
42
El-Jardalil F Fadlallah R . No Global Health Security without Strong and Resilient Health Systems in the Mediterranean (2022). Available online at: https://www.iemed.org/wp-content/uploads/2022/12/Focus-9-Fadi.pdf (Accessed August 12, 2025).
43
World Bank . Protecting Essential Services for Women, Children and Adolescents during COVID-19 (2021). Available online at: https://www.globalfinancingfacility.org/sites/gff_new/files/documents/GFF-IG11-3-Protecting-Essential-Services-in-Times-of-COVID19.pdf (Accessed August 12, 2025).
Summary
Keywords
climate change, detect, epidemic, health security, health systems, resilience, humanitarian emergency, integration
Citation
Talisuna AO, Karamagi HC, Saikat S, Droti B, Bisoborwa GK, Nabyonga-Orem J, Chamla D, Gueye AS and Kasolo FC (2025) Strengthening health systems for health emergency preparedness and response in Africa: integrating building system resilience to achieve universal health coverage and promote health security is a “double win”. Front. Trop. Dis. 6:1685122. doi: 10.3389/fitd.2025.1685122
Received
13 August 2025
Accepted
30 September 2025
Published
21 October 2025
Volume
6 - 2025
Edited by
Jeffrey Mecaskey, Consultant, Berlin, Germany
Reviewed by
Aristide Rondouba Dionkounda, Africa One Health University Network (AFROHUN), Côte d’Ivoire
Updates
Copyright
© 2025 Talisuna, Karamagi, Saikat, Droti, Bisoborwa, Nabyonga-Orem, Chamla, Gueye and Kasolo.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ambrose Otau Talisuna, talisunaa@who.int
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.