- 1Policlinico Veterinario Roma Sud AniCura, Rome, Italy
- 2Centro Veterinario Fossanese, Cuneo, Italy
Introduction: This prospective randomized study (protocol number 0156185) aims to evaluate the perioperative analgesic efficacy of quadratus lumborum block (QLB) versus transversus abdominis plane block (TAPB) in dogs undergoing elective laparoscopic ovariectomy.
Materials and methods: Dogs premedicated with methadone (0.2 mg/kg IV), inducted with propofol and maintained under general anesthesia with isoflurane were randomized into 3 groups. In the QLB group, 0.5 mL/kg of ropivacaine 0.35% was administered at L1–L2 bilaterally; in the TAPB group, 0.25 mL/kg of ropivacaine 0.35% per injection was administered in four sites; the third group, named P, was a control group where dogs did not receive any block. Heart rate (HR), invasive mean arterial pressure (MAP) and end-tidal concentration of isoflurane (etISO) were recorded at surgical timepoints: pre-stimulus baseline (T0), skin and abdominal wall incision (T1), induction of capnoperitoneum (T2), traction and ligation of the right (T3) and left ovaries (T4). Intraoperative data collection and adjustment of the hypnotic plan were performed by an operator blinded to the used technique. Cardiovascular response (CR) was defined as a 20% increase in MAP and/or HR from T0. Dogs with MAP greater than 30% of baseline received an infusion of remifentanil (0.5 mcg/kg/min) and were recorded as intraoperative rescue analgesia (iRA) events. Postoperative analgesia was assessed with Glasgow Composite Measure Pain Scale short form (GCMPS-SF) at 2 and 4 h after extubating.
Results: Thirty-two dogs were included and analyzed (12 in TAPB, 10 in QLB, 10 in P). In all groups MAP was higher than baseline at T2-T3-T4 time points (p < 0.05), in P group MAP also increased at T1 (p < 0.05). The incidence of CR at T1 was higher in P (70%) compared to TAPB (0%) and QLB (20%) (p = 0.001). No patient received postoperative rescue analgesia.
Conclusion: Both TAPB and QLB guaranteed adequate analgesia regarding the somatic stimulus (T1) compared to P whereas all groups were not able to prevent a cardiovascular response during the induction of capnoperitoneum (T2) and ovarian traction (T3–T4). Analgesia in the early postoperative period (up to 4 h) was adequate in all groups.
Introduction
Interfascial plane blocks, such as transverse abdominis plane block (TAPB) and quadratus lumborum block (QLB), have gained increasing attention in veterinary anesthesia over the past decades (1–3) as effective techniques for minimizing perioperative pain during abdominal surgical procedures (4). They consist in administering a local anesthetic solution (LA) into interfascial planes under the guidance of ultrasonography (5).
The TAPB consists in injecting the LA between the transversus abdominis and the internal oblique muscles of the abdominal wall targeting the intercostal, costoabdominal, cranial and caudal iliohypogastric, and ilioinguinal nerves. They innervate the anterior and lateral abdominal wall and the parietal peritoneum, theoretically providing only somatic analgesia of the abdominal wall (1, 6–8), even though a visceral involvement is still debated (9, 10).
The QLB consists in administering the LA solution in the interfascial plane adjacent to the quadratus lumborum muscle, where thoracolumbar ventral branches from T12 to L3 run; the LA can spread into the paravertebral space and reconnect with the sympathetic trunk, providing somatic and visceral abdominal analgesia (11, 12). Although further studies need to be accomplished, data in human medicine suggest that QLB might provide better abdominal pain control than TAPB (11, 13, 14).
Recently, several cadaveric studies regarding TAPB and QLB in the canine species have been published. They investigated the relationship between injected volume and its longitudinal distribution, the number of nervous branches involved, the site and number of injections necessary (15–21). Furthermore, several ultrasound approaches and fascial points of injection have been described (22–27). Recently, a growing number of clinical studies also evaluated the distribution of LA and its possible implications (28–30). Some have shown that TAPB can provide adequate postoperative analgesia for ovariectomy (31), ovariohysterectomy (32) and laparoscopic ovariectomy (33, 34). Regarding intraoperative rescue analgesia with TAPB, Paolini et al. (33) reported less evidence of nociception compared to the control group, whereas Espadas-González et al. (34) found no statistical difference. Regarding QLB, Degani et al. (35) reported a perioperative reduction of opioid consumption in patients undergoing laparoscopic ovariectomy (LO). However, to the authors’ knowledge, no comparative studies of clinical efficacy between TAP and QLB in dogs have been reported in literature.
The aim of this study was to compare the intraoperative and postoperative analgesic efficacy between TAPB and QLB using laparoscopic ovariectomy as a model to test somatic and visceral nociceptive stimuli. We hypothesized that: (1) TAPB and QLB would trigger less cardiovascular response (CR) during LO compared to the control group, named P; (2) CR during visceral manipulation would be minor in QLB group in comparison with TAP group; (3) TAPB and QLB would provide comparable postoperative analgesic effect.
Materials and methods
This clinical, randomized, blinded, prospective study was approved by the Scientifics Ethics Committee of the University of Turin (protocol number 0156185). Thirty-seven female mixed-breed dogs scheduled for elective laparoscopic ovariectomy at Policlinico Veterinario Roma Sud AniCura (Rome, Italy) and Centro Veterinario Fossanese (Cuneo, Italy) entered this prospective study. Written informed consent was obtained from the animals’ owners before the starting of procedures.
Animals
Dogs were at least 1 year of age and classified as ASA status I according to physical examination and blood test results. Dogs considered uncooperative, presenting infection on the site of injection of local anesthetic or undergoing pseudocyesis, pregnancy or heat were excluded from the study. Dogs receiving antimuscarinic or vasoactive drugs in the perioperative period, having body temperature below 35°C during recovery, or undergoing surgery within 20 min of the loco-regional block or within 90 min following the administration of methadone were also excluded from the study.
Anesthetic procedure
After admission, dogs were premedicated with 0.2 mg/kg of methadone (Semfortan, 10 mg/mL, Dechra, Turin, Italy) intramuscularly, 15 min later a 18–22 G intravenous catheter (Delta Ven 1, Delta Med, Milano, Italy) was inserted and general anesthesia was induced with propofol (Propomitor, 10 mg/mL, Orion Pharma, Ecuphar Italia S.r.l., Milano, Italy) administered intravenously with a median dose of 4 mg/kg, titrated to effect. They were intubated, connected to a rebreathing system and maintained on general anesthesia with isoflurane (Isoflo fl 250 mL, Zoetis, Milan, Italy) in a mixture of oxygen and medical air with an inspiration fraction (FiO2) of 0.6. They were connected to an anesthetic workstation (GE Aespire View, Datex-Ohmeda Inc., Madison WI, United States) and mechanically ventilated with a pressure-controlled ventilation technique with a starting peak pressure of 9 cm H2O, that would subsequently be adjusted to maintain normocapnia (end-tidal carbon dioxide between 35 and 45 mmHg). The hair of the abdomen and flanks was shaved alike in all dogs, and a peripheral catheter 18–22 G (Delta Ven 1, Delta Med, Milano, Italy) was placed in the metatarsal artery and connected to an arterial line transducer set.
During the anesthetic procedure, dogs were monitored with a multiparametric monitor (Datex AS3, GE Healthcare Finland Oy, Helsinki, Finland) continuously with the assessment of heart rate (HR), electrocardiogram (ECG), peripheral capillary oxygen saturation (SpO2), end-tidal isoflurane concentration (etISO), end-tidal carbon dioxide (etCO2), respiratory rate (f R), spirometry, invasive arterial blood pressure (IBP). Such parameters were recorded every 5 s1 and post hoc analyzed.
Experimental groups
Dogs were randomly assigned to group TAPB, QLB, or P.2 Anesthesiologists with at least 2 years of experience with TAP and QL block performed the locoregional technique using a HS-50 Samsung ultrasound machine and a linear array probe (Samsung LA3-16A).
Group TAPB
TAP block was performed with the patient in lateral position, with the technique previously described by Romano et al. (21) administering the LA in four sites, bilaterally caudally the last rib and cranially the iliac crest. The probe was placed perpendicularly the spine, once abdominal external oblique, internal oblique and transversus abdominis muscles were identified, a 20–22 G spinal needle (BD Quincke spinal needle, BD, Milan, Italy) connected to a syringe was introduced “in-plane” with a ventro-lateral to dorso-medial direction until the interfascial plane between the transversus abdominis and internal oblique muscles was reached, aspiration for preventing intravascular administration was executed and 0.25 mL/kg of ropivacaine 0.35% (Ropivacaina 10 mg/mL, Fresenius Kabi s.r.l., Verona, Italy) per site of injection was administered. The block was considered adequate if hydro dissection between the two muscles was observed.
Group QLB
QLB was executed with the dogs in lateral position, with the technique described by Garbin et al. (23), administering the LA in two specular sites. The linear array was positioned dorsally perpendicularly to the spine, caudally the last rib, the second lumbar vertebra was recognized, and a 18–22 G spinal needle was introduced in-plane with a ventrolateral to dorsomedial direction and 0.5 mL/kg of ropivacaine 0.35% was injected either between the QL and psoas muscle or the QL muscle and lateral thoracolumbar fascia. The block was considered adequate whether hydro dissection between the two muscles, together with ventral movement of the thoracolumbar fascia, was observed. Were it not to happen, the needle was retreated and redirected until hydro dissection was observed. Once the correct needle position was confirmed, the entire volume of local anesthetic was administered.
Group P
In group P, dogs did not receive a locoregional block.
Intraoperative period
Dogs were subsequently taken to the operating room by a second anesthesiologist, blinded to the locoregional technique performed. A surgical anesthetic plane with etISO 1.1% was maintained (36), assessing palpebral reflex, voluntary movements and jaw tone, with adjustment of etISO during the procedure when necessary. The laparoscopic ovariectomy adopted technique was two-port with a transabdominal suspension suture for the ovarian traction (37). The anesthetic plan was considered adequate in all dogs before the beginning of surgery, and average HR and MAP 5 min before the starting of surgery were recorded as T0 values. Subsequently, maximal HR and MAP were recorded at the incision of skin (T1), the insufflation of capnoperitoneum (T2), ligation and excision of right (T3) and left ovaries (T4). An increase by 20% of HR or MAP relative to T0 was considered a cardiovascular response (CR). Any increase by 30% of HR or MAP was considered a nociceptive stimulus and was treated with a constant rate infusion of remifentanil at the dose of 0.5 mcg/kg/min as intraoperative rescue analgesia (iRA) until the end of surgery.
Postoperative period
During recovery a third anesthesiologist, not informed of the loco-regional technique performed and eventual iRA treatment, assessed the postoperative pain using the short form Glasgow Composite Pain Scale (SF-GCPS) (38) at 2 and 4 h after extubating. In case of a score ≥6/24 methadone 0.2 mg/kg intramuscularly as postoperative rescue analgesia (pRA) was administered. Meloxicam 0.1 mg/kg (Metacam 5 mg/mL, Boehringer Ingelheim Vetmedica GmbH, Terrassa, Spain) was administered subcutaneously prior hospital discharge, approximately 4 h after extubating.
Statistical analysis
Statistical analysis was performed using MedCalc Software for Windows version 12.5 (MedCalcSoftware, Ltd., Belgium). Shapiro–Wilk test and visual inspection of histograms were used to analyze the distribution of data. Categorical variables were reported as frequency and percentage; Fisher’s exact test was used to evaluate frequency distribution between the groups.
Two-way repeated-measures ANOVA was used to evaluate changes in HR and MAP over time and compare them among the groups with Bonferroni post-hoc analysis. Statistical significance was set at p < 0.05.
The minimum sample size of at least 10 dogs per group was calculated for repeated measures between factors with an effect size of 0.5 with a power 80% and setting significance level at 5% (G*Power 3.1.9.6).
Results
Thirty-seven dogs were enrolled in the study. Five dogs were excluded: two in group TAPB for hemodynamic instability requiring antimuscarinic treatment and three in group QLB, two of whom for procedural difficulty in performing the block and one for hemodynamic instability requiring vasoactive treatment. Thirty-two dogs were analyzed, divided as follows: 12 cases in group TAPB, 10 in group QLB, 10 in group P. The dogs were a mixture of breeds, reported in Table 1. All dogs were ASA status I. Groups did not differ for age, body mass, end-tidal concentrations of isoflurane and duration of surgery (Table 1).
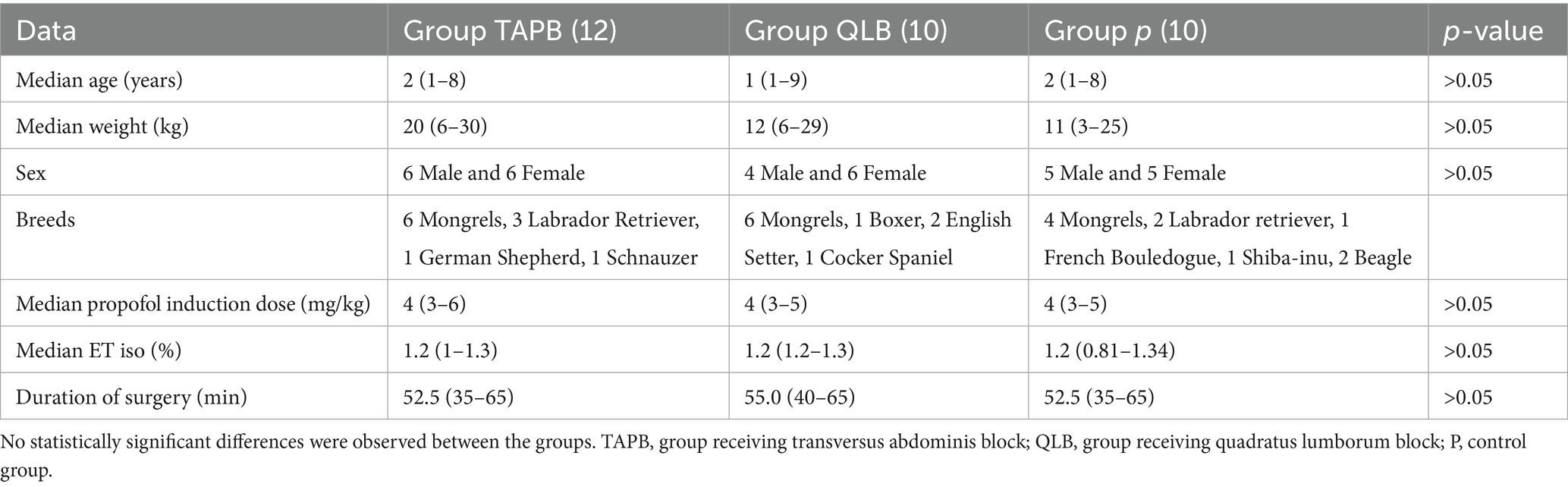
Table 1. Demographic data (age, weight, sex), end-tidal isoflurane concentration (ET iso), and duration of surgery for the TAPB, QLB, and P groups.
The incidence of CR and iRA during surgery was reported in Table 2. The incidence of CR at T1 was different in P compared to TAP and QLB groups (p = 0.001).
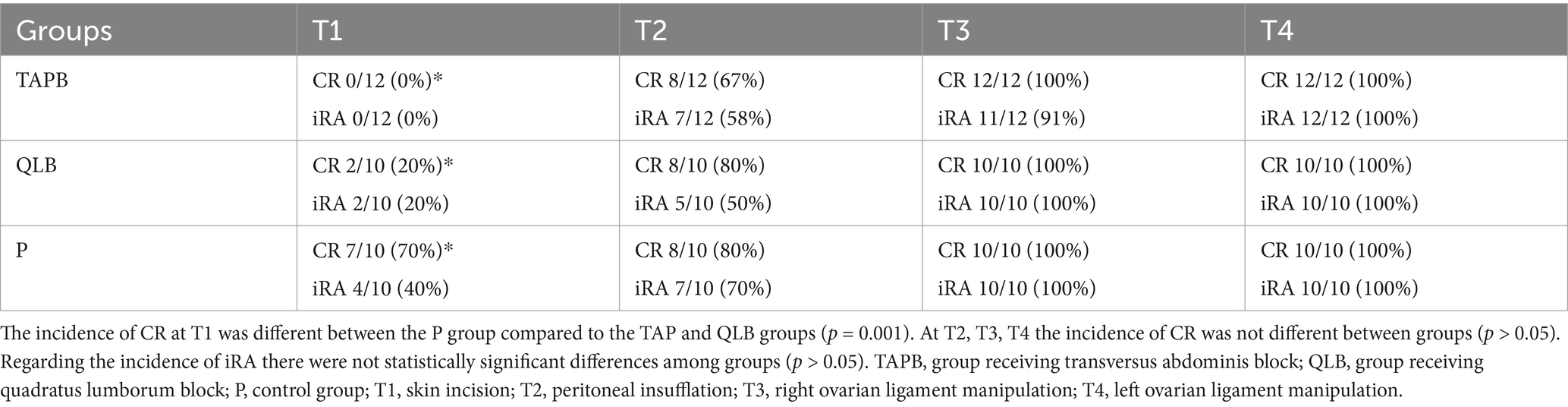
Table 2. Incidence of cardiovascular response (CR) and intraoperative rescue analgesia (iRA) between group TAPB, QLB, and P.
In QLB and TAPB group, MAP was greater than baseline at T2-T3-T4 (p < 0.05), whereas in P group MAP increased at T1-T2-T3-T4 (p < 0.05) (Figure 1).
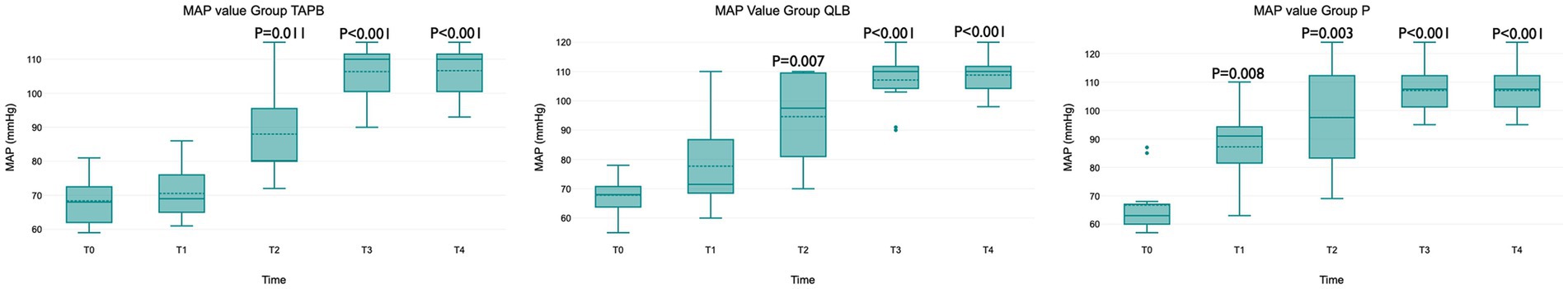
Figure 1. MAP values for group TAPB, QLB and P at each timepoint. The central box represents the values from the lower to upper quartile, the middle solid line the median, the spotted line the mean, spots the outliers, and whiskers the range values. In QLB and TAPB group, MAP was greater than baseline at T2-T3-T4 (p < 0.05), whereas in P group MAP increased at T1-T2-T3-T4 (p < 0.05).
In all groups HR did not increase during surgery compared to T0 at any time point (p > 0.05) (Figure 2).
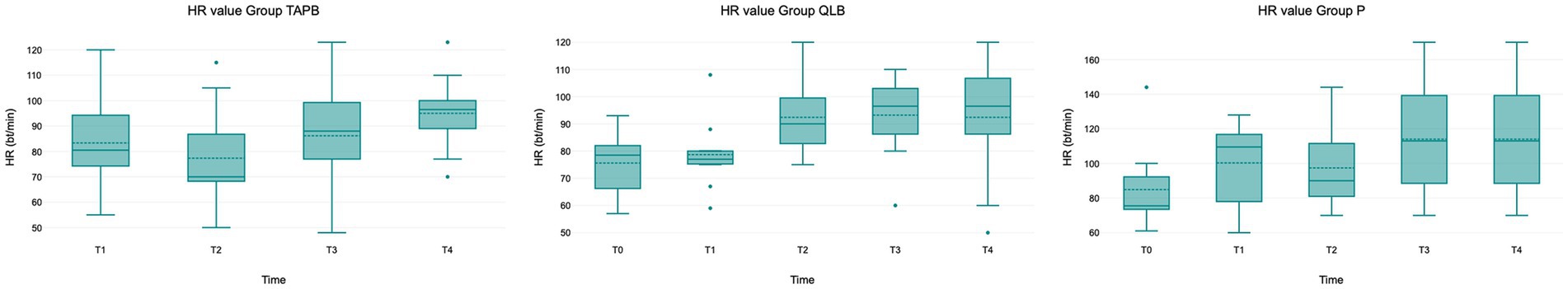
Figure 2. HR values for group TAPB, QLB and P at each timepoint. The central box represents the values from the lower to upper quartile, the middle solid line the median, the spotted line the mean, spots the outliers, and whiskers the range values. In all groups HR did not increase during surgery compared to T0 at any time point (p > 0.05).
No patient received pRA during the postoperative observation period. Results of GCMPS-SF at 2 and 4 h showed no difference between groups (p > 0.05) (Figure 3).
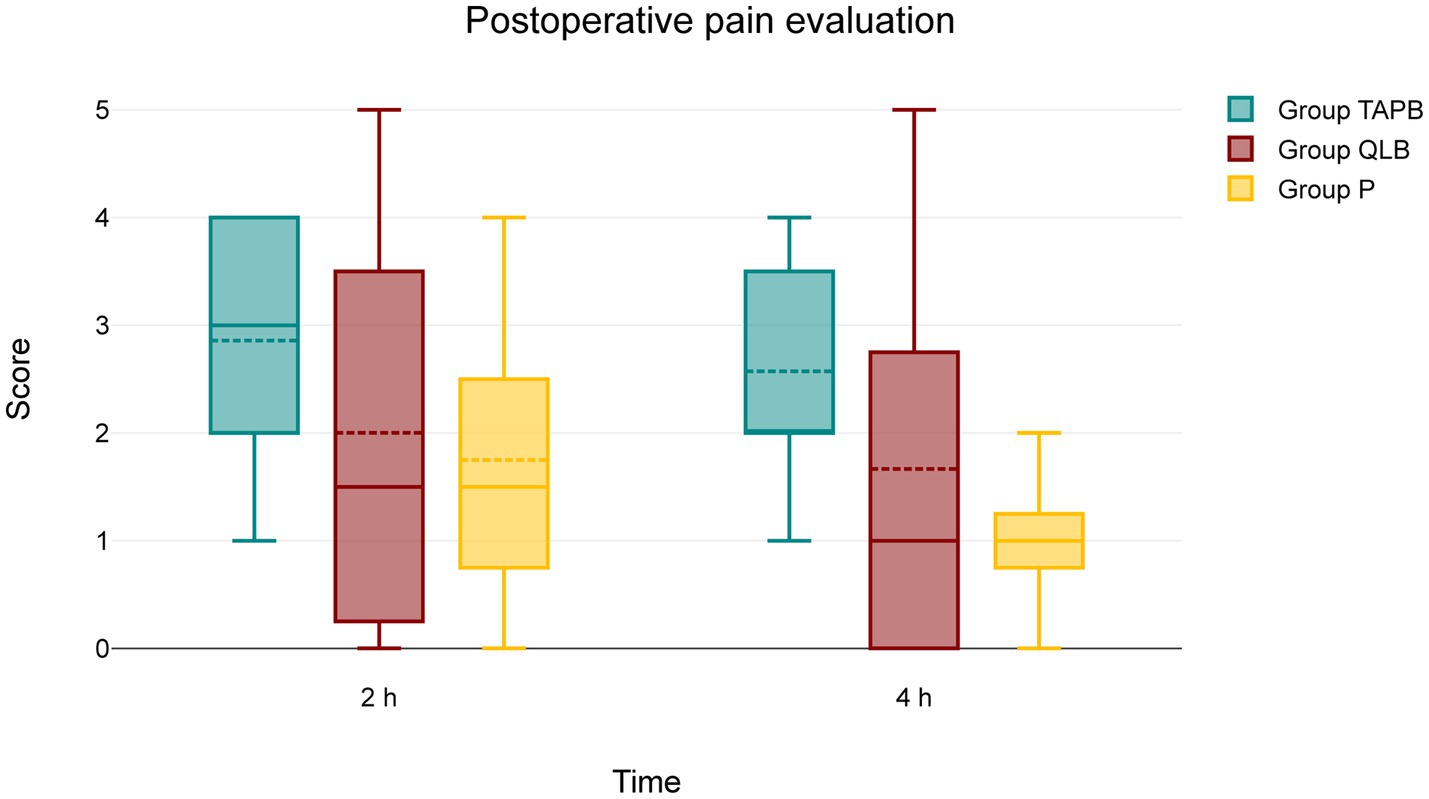
Figure 3. Values of GCPS-SF at 2 and 4 h. The central box represents the values from the lower to upper quartile, the middle solid line the median, the spotted line the mean, spots the outliers, and whiskers the range values. No patient received postoperative rescue analgesia during the postoperative observation period. Results showed no difference between groups (p > 0.05).
In the post-operative period no adverse effects, including nausea, vomiting, or excessive salivation, were observed in any of the dogs involved in the study.
Discussion
This study showed that TAPB and QLB provided similar perioperative analgesia in dogs undergoing laparoscopic ovariectomy. Both blocks provided excellent somatic pain control but failed to control visceral intraoperative stimulation (specifically peritoneal insufflation and ovarian manipulation).
During intraoperative monitoring, no statistically significant increase in MAP at T1 was observed in the TAPB and QLB groups, yet it was registered in P group. The efficacy of TAPB and QLB in preventing CR during skin-muscle abdominal incision was very high (100 and 80% respectively) and statistically higher compared to the control group (30%). This finding is in line with the results of Degani et al. (35), who reported an 80% success rate in preventing CR with QLB in a similar setting at T1.
Interestingly, these findings are not entirely in line with the findings of the referenced cadaveric studies, which describe different longitudinal distributions of injectate. The canine abdominal wall is innervated by the ventral branches of nerves T10 to L3, with anatomical variations regarding the presence of T7 to T9 (18). Romano et al. (21), using the same technique and administering a comparable volume as our study, reported a distribution of injectate from T11 to L2, whereas the QLB technique of Garbin et al. (23) described a shorter spread, from T13 to L3. According to these findings, we would have expected TAPB to be superior to QLB in terms of somatic coverage. However, the dye distribution may not accurately reflect the actual spread of local anesthetics in clinical cases, as the physiochemical properties of different contrast agents, dye and LA mixtures may influence the distribution in the interfascial planes (39).
At time point T2 (abdominal insufflation), both the TAPB and QLB groups showed an increase in MAP compared to baseline. The incidence of CR at T2 was similar among groups, with 63, 82, and 80% of cases, respectively, in TAPB, QLB, and P group. The visceral sensitivity of abdominal organs is regulated by the sympathetic trunk between T11 and L4 (40, 50). TAPB was expected not to be able to prevent CR during visceral stimulation, as it has not been described to stain the sympathetic trunk in cadaveric studies, although Freitag et al. (10) reported pain relief in patients with severe pancreatitis and it is commonly used in humans to treat postoperative abdominal pain (41).
In our study, QLB was also unable to prevent CR. This finding is in contrast with the evidence of the cadaveric study of Garbin et al. (23) where a high percentage of stain on spinal nerves and sympathetic trunk was observed. Additionally, we cannot rule out the possibility that the intraoperative failure of the QL block may have been due to the technical limitations related to the difficulty of execution. In the QLB group, the local anesthetic was injected either between the QL and psoas muscles or between the QL muscle and thoracolumbar fascia, depending on the depth of the QL muscle and on the confidence of the operator. Even though the technique was performed by expert anesthesiologists and considered adequate in the presence of hydro dissection, the accuracy of execution and potential variability in the spreading of local anesthetic were not further investigated.
Our results also did not confirm our initial hypothesis that QLB would reduce CR during ovarian manipulation (T3 and T4) compared to TAPB. In both TAPB and QLB, CR was recorded during ovarian stimulation in 100% of cases.
In terms of cardiovascular variables, a 20% increase in either HR or MAP at T0 was considered CR, in line with previous studies (24). However, in our study, unlike others, iRA was administered with an increase of 30%, in order to increase the power of the study evaluating the analgesic efficacy and to explore a time window usually not taken into consideration when RC and iRA are corresponding. In the majority of cases MAP kept on increasing and required treatment, however in few cases it returned to baseline values and a minority reached a MAP lower than T0.
Regarding the drug chosen for iRA, remifentanil was selected for its pharmacokinetic properties and not to interfere with postoperative pain assessment (42). Also, patients requiring antimuscarinic or vasoactive treatment were automatically excluded from the study in order not to bias CR recognition.
Interestingly, the increase in MAP was not associated with a significant change in HR. This may be explained by two opposing effects: halogenated compounds, specifically isoflurane in this study, may decrease baroreflex sensitivity (43), whereas opioids, specifically methadone, may exert a potentiating agonist effect on it (44). Therefore, HR cannot be considered a useful predictor of nociceptive response to surgical stimulation in dogs undergoing LO.
The type of surgical stimulation and the drugs chosen in premedication may significantly influence the incidence of CR, as supported by the results of several studies. For example, in Espadas-González et al. (34) dogs receiving dexmedetomidine and methadone as premedication showed low incidence of CR during LO both in the TAP block and in the control group (3/26 and 7/26 respectively). Two studies of Degani et al. (35, 45) regarding intraoperative QLB efficacy also found different CR rates probably depending on premedication: 2/7 in dogs receiving dexmedetomidine and methadone (45) and 13/16 in dogs only receiving fentanyl (35). Taking this into account, group P, acting as control group, played a crucial role in validating our study model, confirming the evocation of CR in dogs only receiving opioid premedication and undergoing minimally invasive laparoscopic surgery.
Postoperative analgesia at 2 and 4 h after extubating was adequate in all groups and none of the dogs received pRA. These data are consistent with the current veterinary literature (46, 47), where no pRA within the 8 postoperative hours is reported in dogs undergoing LO. Meloxicam was administered immediately prior to hospital discharge in order not to bias the pain scale, unlike other clinical trials: Viscasillas et al. (28) administered meloxicam as premedication, Espadas-González et al. (34) intraoperatively, and Paolini et al. (33) immediately at the end of surgery, potentially influencing pain assessment. This study mainly focused on intraoperative efficacy and, for organizational reasons, dogs were postoperatively monitored only for 4 h before hospital discharge. It cannot be excluded that a longer period of postoperative pain monitoring would have shown different results between the groups.
This study presents limits that need to be addressed. Firstly, in the QLB group LA was injected either between QL and psoas muscles or between QL muscle and thoracolumbar fascia and the distribution of LA was not furtherly investigated, as dogs did not undergo advanced diagnostic imaging. Per contra, studies report that the distribution of radiological contrast does not correlate with distribution of LA (28, 48). Also, this study is focusing on clinical efficacy and prolonging anesthesia duration was not considered necessary.
Secondly, once administered, the constant rate infusion of remifentanil was continued until the end of surgery and the further surgical timepoints were categorized as iRA events for the inability to evaluate them. This could have influenced total iRA, however this is a common limit in this type of clinical studies, as rescue analgesia needs to be administered for ethical reasons.
Finally, dogs were postoperatively monitored only for 4 h before hospital discharge for organizational reasons. However, no dog was brought back the following day nor needed to be re-examined for collateral effects.
This study did not report any complication during the locoregional procedures, nor postoperative side effects such as nausea, vomiting or sialorrhea. In recent veterinary literature, no complications have been described for TAPB (24, 33), while a QLB study reported two cases of retroperitoneal hematoma in dogs (49). Due to the limited number of cases in our study, it is not possible to draw any conclusive comparisons regarding the safety of these two techniques in dogs.
In conclusion, to the authors’ knowledge, this is the first study comparing clinical efficacy of TAPB and QLB during intraoperative analgesia while carefully monitoring cardiovascular variables at different surgical time points. TAPB and QLB provide effective somatic analgesia in dogs undergoing laparoscopic ovariectomy. However, the clinical efficacy of QLB and TAPB on abdominal visceral innervation remains uncertain. Since QLB does not show any advantage in comparison to TAPB in our findings, future studies are needed to establish whether QLB might grant a more extensive pain relief and should be preferred in specific scenarios.
Data availability statement
The data will be made available on request at discretion of the authors. Requests to access the datasets should be directed to Eleonora Fumanelli, ZWxlb25vcmEuZnVtYW5lbGxpQGdtYWlsLmNvbQ==.
Ethics statement
The animal studies were approved by Scientific Ethics Committee of the University of Turin. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent was obtained from the owners for the participation of their animals in this study.
Author contributions
EF: Investigation, Visualization, Writing – original draft, Writing – review & editing. GC: Data curation, Investigation, Writing – original draft. GG: Investigation, Writing – original draft. MP: Supervision, Writing – original draft. RR: Conceptualization, Methodology, Validation, Writing – review & editing. DS: Conceptualization, Formal Analysis, Methodology, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Chin, KJ, McDonnell, JG, Carvalho, B, Sharkey, A, Pawa, A, and Gadsden, J. Essentials of our current understanding: abdominal wall blocks. Reg Anesth Pain Med. (2017) 42:133–83. doi: 10.1097/AAP.0000000000000545
2. Elsharkawy, H, Pawa, A, and Mariano, ER. Interfascial plane blocks: back to basics. Reg Anesth Pain Med. (2018) 43:341–6. doi: 10.1097/AAP.0000000000000750
3. Fischer, BL. Introduction to fascial plane blocks. In: M Read, L Campoy, and B Fischer, editors. Small animal regional anesthesia and analgesia [internet]. 1 Wiley; (2024). p. 117–125. Available online at: https://onlinelibrary.wiley.com/doi/10.1002/9781119514183.ch12 (Accessed May 15, 2025).
4. Campoy, L. Development of enhanced recovery after surgery (ERAS) protocols in veterinary medicine through a one-health approach: the role of anesthesia and locoregional techniques. J Am Vet Med Assoc. (2022) 260:1751–9. doi: 10.2460/javma.22.08.0354
5. Jones, J, and Aldwinckle, R. Interfascial plane blocks and laparoscopic abdominal surgery: a narrative review. Local Reg Anesth. (2020) 13:159–69. doi: 10.2147/LRA.S272694
6. Schroeder, CA, Snyder, LBC, Tearney, CC, Baker-Herman, TL, and Schroeder, KM. Ultrasound-guided transversus abdominis plane block in the dog: an anatomical evaluation. Vet Anaesth Analg. (2011) 38:267–71. doi: 10.1111/j.1467-2995.2011.00612.x
7. Garbin, M, Marangoni, S, Finck, C, and Steagall, PV. An anatomical, sonographic, and computed tomography study of the transversus abdominis plane block in cat cadavers. Animals. (2022) 12:2674. doi: 10.3390/ani12192674
8. Mavarez, AC, Hendrix, JM, and Ahmed, AA. Transabdominal plane block. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; (2025). Available online at: http://www.ncbi.nlm.nih.gov/books/NBK560527/ (Accessed April 5, 2025).
9. Smith, DI, Hawson, A, and Correll, L. Transversus abdominis plane block and treatment of viscerosomatic abdominal pain. Reg Anesth Pain Med. (2015) 40:731–2. doi: 10.1097/AAP.0000000000000321
10. Freitag, FA, Bozak, VL, Do Carmo, MP, Froes, TR, and Duque, JC. Continuous transversus abdominis plane block for analgesia in three dogs with abdominal pain. Vet Anaesth Analg. (2018) 45:581–3. doi: 10.1016/j.vaa.2018.02.003
11. Blanco, R, Ansari, T, Riad, W, and Shetty, N. Quadratus Lumborum block versus transversus abdominis plane block for postoperative pain after cesarean delivery: a randomized controlled trial. Reg Anesth Pain Med. (2016) 41:757–62. doi: 10.1097/AAP.0000000000000495
12. Elsharkawy, H, El-Boghdadly, K, and Barrington, M. Quadratus lumborum block: anatomical concepts, mechanisms, and techniques. Anesthesiology. (2019) 130:322–35. doi: 10.1097/ALN.0000000000002524
13. Murouchi, T, Iwasaki, S, and Yamakage, M. Quadratus lumborum block: analgesic effects and chronological ropivacaine concentrations after laparoscopic surgery. Reg Anesth Pain Med. (2016) 41:146–50. doi: 10.1097/AAP.0000000000000349
14. Öksüz, G, Bilal, B, Gürkan, Y, Urfalioğlu, A, Arslan, M, Gişi, G, et al. Quadratus Lumborum block versus transversus abdominis plane block in children undergoing low abdominal surgery: a randomized controlled trial. Reg Anesth Pain Med. (2017) 42:674–9. doi: 10.1097/AAP.0000000000000645
15. Johnson, EK, Bauquier, SH, Carter, JE, Whittem, T, and Beths, T. Two-point ultrasound-guided transversus abdominis plane injection in canine cadavers – a pilot study. Vet Anaesth Analg. (2018) 45:871–5. doi: 10.1016/j.vaa.2018.06.014
16. Bruggink, SM, Schroeder, KM, Baker-Herman, TL, and Schroeder, CA. Weight-based volume of injection influences cranial to caudal spread of local anesthetic solution in ultrasound-guided transversus abdominis plane blocks in canine cadavers. Vet Surg. (2012) 41:455–7. doi: 10.1111/j.1532-950X.2012.00972.x
17. Drożdżyńska, M, Monticelli, P, Neilson, D, and Viscasillas, J. Ultrasound-guided subcostal oblique transversus abdominis plane block in canine cadavers. Vet Anaesth Analg. (2017) 44:183–6. doi: 10.1111/vaa.12391
18. Castañeda-Herrera, FE, Buriticá-Gaviria, EF, and Echeverry-Bonilla, DF. Anatomical evaluation of the thoracolumbar nerves related to the transversus abdominis plane block technique in the dog. Anat Histol Embryol. (2017) 46:373–7. doi: 10.1111/ahe.12279
19. Zoff, A, Laborda-Vidal, P, Mortier, J, Amengual, M, and Rioja, E. Comparison of the spread of two different volumes of contrast medium when performing ultrasound-guided transversus abdominis plane injection in dog cadavers. J Small Anim Pract. (2017) 58:269–75. doi: 10.1111/jsap.12639
20. Freitag, FAV, Muehlbauer, E, Gaio, T dS, Dos Santos, AAM, Machado, M, Sanchez, A, et al. Evaluation of injection volumes for the transversus abdominis plane block in dog cadavers: a preliminary trial. Vet Anaesth Analg. (2021) 48:142–6. doi: 10.1016/j.vaa.2020.10.001
21. Romano, M, Portela, DA, Thomson, A, and Otero, PE. Comparison between two approaches for the transversus abdominis plane block in canine cadavers. Vet Anaesth Analg. (2021) 48:101–6. doi: 10.1016/j.vaa.2020.09.005
22. Alaman, M, Bonastre, C, De Blas, I, Gomez-Alvarez, CM, and Laborda, A. Description of a novel ultrasound-guided approach for a dorsal quadratus lumborum block: a canine cadaver study. Vet Anaesth Analg. (2022) 49:118–25. doi: 10.1016/j.vaa.2021.09.002
23. Garbin, M, Portela, DA, Bertolizio, G, Garcia-Pereira, F, Gallastegui, A, and Otero, PE. Description of ultrasound-guided quadratus lumborum block technique and evaluation of injectate spread in canine cadavers. Vet Anaesth Analg. (2020) 47:249–58. doi: 10.1016/j.vaa.2019.12.005
24. Garbin, M, Portela, DA, Bertolizio, G, Gallastegui, A, and Otero, PE. A novel ultrasound-guided lateral quadratus lumborum block in dogs: a comparative cadaveric study of two approaches. Vet Anaesth Analg. (2020) 47:810–8. doi: 10.1016/j.vaa.2020.08.003
25. Viscasillas, J, Terrado, J, Marti-Scharfhausen, R, Castiñeiras, D, Esteve, V, Clancy, N, et al. A modified approach for the ultrasound-guided Quadratus Lumborum block in dogs: a cadaveric study. Animals. (2021) 11:2945. doi: 10.3390/ani11102945
26. Marchina-Gonçalves, A, Laredo, FG, Gil, F, Soler, M, Agut, A, Redondo, JI, et al. An ultrasound-guided Latero-ventral approach to perform the Quadratus Lumborum block in dog cadavers. Animals. (2023) 13:2214. doi: 10.3390/ani13132214
27. Marchina-Gonçalves, A, Gil, F, Laredo, FG, Soler, M, Agut, A, and Belda, E. Evaluation of high-volume injections using a modified dorsal quadratus lumborum block approach in canine cadavers. Animals. (2021) 12:18. doi: 10.3390/ani12010018
28. Viscasillas, J, Sanchis-Mora, S, Burillo, P, Esteve, V, Del Romero, A, Lafuente, P, et al. Evaluation of Quadratus Lumborum block as part of an opioid-free Anaesthesia for canine ovariohysterectomy. Animals. (2021) 11:3424. doi: 10.3390/ani11123424
29. Swanton, WE, Christensen, N, and Schroeder, C. Rectus sheath block results in greater cranial-caudal spread whereas transversus abdominis plane block results in greater lateral spread as assessed by computed tomography in dogs. Am J Vet Res. (2024) 85:ajvr.24.04.0106. doi: 10.2460/ajvr.24.04.0106
30. Degani, M, Bolen, G, Talarico, C, Noël, S, Gommeren, K, Di Franco, C, et al. Description and outcomes of an ultrasound-guided technique for catheter placement in the canine Quadratus Lumborum plane: a cadaveric tomographic study and clinical case series. Vet Sci. (2024) 11:472. doi: 10.3390/vetsci11100472
31. Cavaco, JS, Otero, PE, Ambrósio, AM, Neves, ICB, Perencin, FM, Pereira, MAA, et al. Analgesic efficacy of ultrasound-guided transversus abdominis plane block in dogs undergoing ovariectomy. Front Vet Sci. (2022) 9:1031345. doi: 10.3389/fvets.2022.1031345
32. Campoy, L, Martin-Flores, M, Boesch, JM, Moyal, MN, Gleed, RD, Radhakrishman, S, et al. Transverse abdominis plane injection of bupivacaine with dexmedetomidine or a bupivacaine liposomal suspension yielded lower pain scores and requirement for rescue analgesia in a controlled, randomized trial in dogs undergoing elective ovariohysterectomy. Am J Vet Res. (2022) 83:ajvr.22.03.0037. doi: 10.2460/ajvr.22.03.0037
33. Paolini, A, Santoro, F, Bianchi, A, Collivignarelli, F, Vignoli, M, Scialanca, S, et al. Use of transversus abdominis plane and intercostal blocks in bitches undergoing laparoscopic Ovariectomy: a randomized controlled trial. Vet Sci. (2022) 9:604. doi: 10.3390/vetsci9110604
34. Espadas-González, L, Usón-Casaús, JM, Pastor-Sirvent, N, Santella, M, Ezquerra-Calvo, J, and Pérez-Merino, EM. Evaluation of the two-point ultrasound-guided transversus abdominis plane block for laparoscopic canine Ovariectomy. Animals. (2022) 12:3556. doi: 10.3390/ani12243556
35. Degani, M, Di Franco, C, Tayari, H, Fages Carcéles, A, Figà Talamanca, G, Sandersen, C, et al. Postoperative analgesic effect of bilateral Quadratus Lumborum block (QLB) for canine laparoscopic Ovariectomy: comparison of two concentrations of Ropivacaine. Animals. (2023) 13:3604. doi: 10.3390/ani13233604
36. Grubb, T, Sager, J, Gaynor, JS, Montgomery, E, Parker, JA, Shafford, H, et al. 2020 AAHA anesthesia and monitoring guidelines for dogs and cats*. J Am Anim Hosp Assoc. (2020) 56:59–82. doi: 10.5326/JAAHA-MS-7055
37. Devitt, CM, Cox, RE, and Hailey, JJ. Duration, complications, stress, and pain of open ovariohysterectomy versus a simple method of laparoscopic-assisted ovariohysterectomy in dogs. J Am Vet Med Assoc. (2005) 227:921–7. doi: 10.2460/javma.2005.227.921
38. Reid, J, Nolan, A, Hughes, J, Lascelles, D, Pawson, P, and Scott, E. Development of the short-form Glasgow composite measure pain scale (CMPS-SF) and derivation of an analgesic intervention score. Anim Welf. (2007) 16:97–104. doi: 10.1017/S096272860003178X
39. De Miguel Garcia, C, Whyte, M, St James, M, and Ferreira, TH. Effect of contrast and local anesthetic on dye spread following transversus abdominis plane injection in dog cadavers. Vet Anaesth Analg. (2020) 47:391–5. doi: 10.1016/j.vaa.2020.01.003
40. Struller, F, Weinreich, FJ, Horvath, P, Kokkalis, MK, Beckert, S, Königsrainer, A, et al. Peritoneal innervation: embryology and functional anatomy. Pleura Peritoneum. (2017) 2:153–61. doi: 10.1515/pp-2017-0024
41. Kim, AJ, Yong, RJ, and Urman, RD. The role of transversus abdominis plane blocks in enhanced recovery after surgery pathways for open and laparoscopic colorectal surgery. J Laparoendosc Adv Surg Tech A. (2017) 27:909–14. doi: 10.1089/lap.2017.0337
42. Chism, JP, and Rickert, DE. The pharmacokinetics and extra-hepatic clearance of remifentanil, a short acting opioid agonist, in male beagle dogs during constant rate infusions. Drug Metab Dispos. (1996) 24:34–40. doi: 10.1016/S0090-9556(25)07242-3
43. Seagard, JL, Elegbe, EO, Hopp, FA, Bosnjak, ZJ, von Colditz, JH, Kalbfleisch, JH, et al. Effects of isoflurane on the baroreceptor reflex. Anesthesiology. (1983) 59:511–20. doi: 10.1097/00000542-198312000-00005
44. Szilagyi, JE. Opioid modulation of baroreceptor reflex sensitivity in dogs. Am J Phys. (1987) 252:H733–7. doi: 10.1152/ajpheart.1987.252.4.H733
45. Degani, M, Paolini, A, Bianchi, A, Tamburro, R, Di Matteo, L, Sandersen, C, et al. Comparative study between lateral versus latero-ventral quadratus lumborum block for perioperative analgesia in canine laparoscopic ovariectomy. Vet Anaesth Analg. (2024) 51:738–45. doi: 10.1016/j.vaa.2024.09.001
46. Fuertes-Recuero, M, de Segura, IAG, López, AS, Suárez-Redondo, M, Arrabé, SC, Hidalgo, SP, et al. Postoperative pain in dogs undergoing either laparoscopic or open ovariectomy. Vet J. (2024) 306:106156. doi: 10.1016/j.tvjl.2024.106156
47. Lazzarini, E, Gioeni, D, Del Prete, G, Sala, G, Baio, M, and Carotenuto, AM. A comparative analysis of opioid-free and opioid-sparing anaesthesia techniques for laparoscopic ovariectomy in healthy dogs. Vet Anaesth Analg. (2024) 51:288–97. doi: 10.1016/j.vaa.2024.02.005
48. Marhofer, D, Marhofer, P, Kettner, SC, Fleischmann, E, Prayer, D, Schernthaner, M, et al. Magnetic resonance imaging analysis of the spread of local anesthetic solution after ultrasound-guided lateral thoracic paravertebral blockade: a volunteer study. Anesthesiology. (2013) 118:1106–12. doi: 10.1097/ALN.0b013e318289465f
49. Chiavaccini, L, Solari, FP, Ham, KM, Regier, PJ, Vettorato, E, and Portela, DA. Retroperitoneal hematoma after dorsal quadratus lumborum block in two dogs. Vet Anaesth Analg. (2024) 51:112–4. doi: 10.1016/j.vaa.2023.11.002
50. Breuer, M, Wittenborn, J, Rossaint, R, Van Waesberghe, J, Kowark, A, Mathei, D, et al. Warm and humidified insufflation gas during gynecologic laparoscopic surgery reduces postoperative pain in predisposed patients-a randomized, controlled multi-arm trial. Surg Endosc. (2022) 36:4154–70. doi: 10.1007/s00464-021-08742-1
Keywords: analgesia, canine, laparoscopic surgery, ultrasound-guided locoregional anesthesia, interfascial block, TAP block, QL block
Citation: Fumanelli E, Cocca G, Giannetti G, Parabella M, Rabozzi R and Sarotti D (2025) Perioperative analgesic efficacy of quadratus lumborum block versus transversus abdominis plane block in dogs undergoing laparoscopic ovariectomy: a prospective randomized clinical trial. Front. Vet. Sci. 12:1613741. doi: 10.3389/fvets.2025.1613741
Edited by:
Angela Briganti, University of Pisa, ItalyReviewed by:
Eliseo Belda Mellado, University of Murcia, SpainAndrea Paolini, University of Teramo, Italy
Copyright © 2025 Fumanelli, Cocca, Giannetti, Parabella, Rabozzi and Sarotti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eleonora Fumanelli, ZWxlb25vcmEuZnVtYW5lbGxpQGdtYWlsLmNvbQ==
 Eleonora Fumanelli
Eleonora Fumanelli Giorgia Cocca
Giorgia Cocca Giorgia Giannetti
Giorgia Giannetti Marianna Parabella
Marianna Parabella Roberto Rabozzi
Roberto Rabozzi Diego Sarotti
Diego Sarotti