- 1Department of Radiology, Hospital of the University of Pennsylvania, Philadelphia, PA, United States
- 2Department of Surgery, Hospital of the University of Pennsylvania, Philadelphia, PA, United States
Purpose: Millions of contrast-enhanced CTs are performed every year, resulting in thousands of contrast reactions that require prompt assessment. Radiologists tasked with responding to these patients must develop and maintain appropriate skills, which can be difficult in the absence of consistent exposure or practice. The aim of this study was to evaluate the efficacy of virtual reality (VR) for teaching radiology residents how to manage contrast reactions.
Approach: A custom VR application was developed to simulate contrast reaction scenarios. First-year radiology residents were asked to complete the VR simulation in parallel with an in-person, instructor-led workshop. After completing the VR simulation, an anonymous survey was used to assess views towards and experience of the simulator via components of previously validated instruments including motion sickness, realism, task load, and technology access and awareness.
Results: A total of 11 participants completed the VR contrast reaction simulation and survey. Post-simulation survey results found that 91% thought VR could be useful for radiology education, 82% reported an intent to use the technology again in the future, and 73% thought the VR simulation would be useful for maintaining their skills. 54% reported some level of general discomfort and 18% reported severe headache. A Fisher exact test found no correlation between perceived usefulness and discomfort (p = 1).
Conclusion: Initial findings of this pilot study suggest radiology residents are open to utilizing VR tools, despite moderate levels of discomfort, but view these tools as education adjuncts. However, given the small sample size, continued investigation is needed to better understand the role of VR for primary education versus maintenance of skills.
1 Introduction
Simulation for mastery of medical learning is an established paradigm (Elendu et al., 2024; Rosen, 2008; Le, 2023). Although simulation is an established tool in medical education, implementation remains difficult as manakin simulators are expensive, space for simulation is at a premium, and physicians have limited time. Virtual reality via head mounted displays such as the Oculus Rift and HTC Vibe are a new technology that hold the promise to improve medical simulation by decreasing the price and improving accessibility (Pottle, 2019; Jallad and Işık, 2021). VR achieves these benefits by abstracting simulation by an extra degree. Rather than practicing CPR through a simulated cardiac arrest on a physical manakin in a room designed to look like an emergency department, VR enables the user to practice within a fully virtual world, eliminating the need for a manakin or a physical room. Through VR, users can train in simulations on demand, on their schedule, and in their own space, reducing or eliminating the footprint for dedicated simulation space and hardware. In addition, a single VR device can be used for an expanding list of possible tasks including physical tasks (e.g., suturing) and knowledge-based tasks (e.g., running a code).
A prime example of the benefits of medical simulation is contrast reactions. Every year, hospitals perform millions of contrast-enhanced CT exams. With an aggregate allergic reaction rate to iodinated CT contrast of up to 0.6% (Wang et al., 2008), this equates to thousands of patients who will need to be assessed by a physician. In addition, a small minority of these events will be severe (less than 0.04% (Katayama et al., 1990)), requiring advanced therapies and have a high risk of patient mortality. Given the high mortality potential, it is important that the responding physician be well trained. However, much of medical training occurs “on the job” and through repetition, which is at odds with the low incidence of these events (Donoghue et al., 2021). Most medical trainees will never see a severe reaction. While these low prevalence-high morbidity events are difficult to train through real-life experience, they can be recreated through simulation. This gives trainees a chance to learn and physicians a chance to maintain their skills. The cost and complexity of running an in-person medical simulation limits the ability to learn by repetition (Kurrek and Devitt, 1997). The absence of a feeling of immersion from book or 2D computer-based education modules limits the ability to test for less tangible skills such as communication or presence under pressure. VR-based medical simulation has the potential to provide a nice balance between cost and ease (Farra et al., 2019).
VR itself has its own set of implementation barriers. The foremost of which is the lack of an open cost-effective high fidelity medical simulator. The stated benefits of VR are minimized or lost due to high licensing costs of commercially available products, requirements to tether headsets to computers with powerful GPUs, and requirement of medical content experts to have computer science expertise to develop simulation scenarios (Goh et al., 2021). The development of custom simulations is especially important as every institution has their own unique set of operating procedures and environmental challenges, and one size fits all simulation scenarios will have limited benefit in these situations. To address this issue, a VR medical simulator that can be used to create custom medical scenarios was developed. In this study, we describe the development, of a VR platform that enables creation of a custom simulation for practicing how to handle a patient experiencing a contrast allergy and subsequently conduct a pilot validation study of the developed scenarios.
2 Materials and methods
2.1 Immersive VR platform
A platform for developing VR scenarios was created on a computer with an Intel i9-11900 @ 2.50 GHz processor using 32 GB of RAM, NVIDIA GeForce RTX 3060 Ti graphics processor, and Windows 11 Home (Microsoft Corporation, Redmond, WA, United States). The application was developed using a cross platform game engine (Unity v2019.2; Unity Technologies, San Francisco, CA, United States) to create the VR environment and an open source 3D modeling tool (Blender v3.5.0; Blender Foundation, Amsterdam, Netherlands) to create the 3D world. A head mounted display (Oculus Quest 2; Meta, Menlo Park, CA) was used to interact with the final VR scenarios.
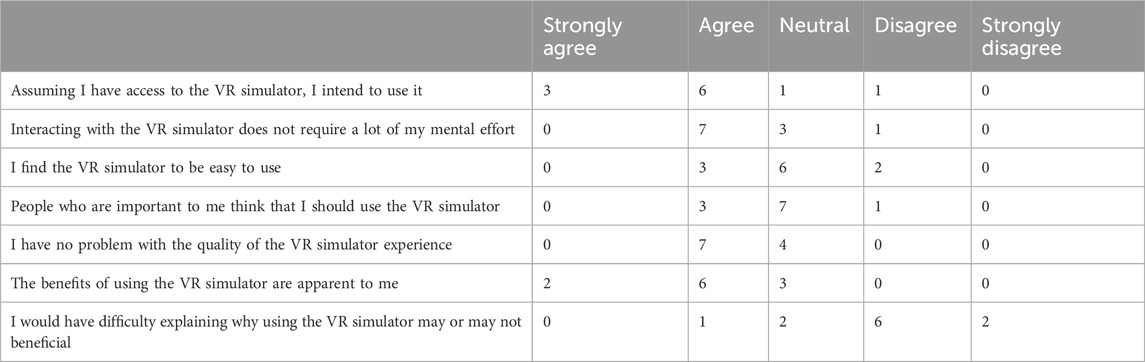
The VR program is made up of several systems that interact to allow a non-linear, problem-solving, open-ended approach to completing each module. There are a few main core systems that allow this level of interaction (Figure 1).
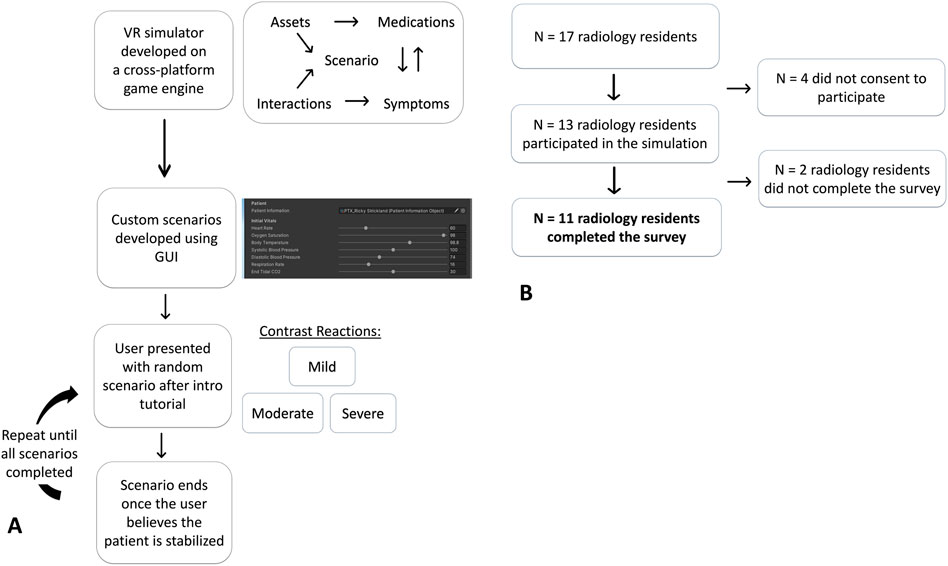
Figure 1. Flowchart describing the VR contrast software platform pathway (A). Participant selection workflow (B).
2.1.1 Asset library
A collection of virtual objects including 3D models of the environment, medication, equipment, and avatars are stored in a common asset location allowing them to be used within and across simulations.
2.1.2 Interaction system
Base API features available within the gaming engine are used to handle user navigation and object interaction. User movement through the environment, interaction with objects in the environment, and menu creation and interaction are tracked and handled by the game engine without the need for additional custom code.
2.1.3 Symptoms module
This system represents the patient and their symptoms and is added on top of a base patient model asset. Symptoms are additive, allowing conditions like hypoxia, hypotension, and tachycardia to be represented together. In addition, the system handles symptom display including quantitatively via charts or vital readings, qualitatively through visual clues like rashes or coughs, and through patient dialogue. Symptoms can be static or dynamic, and can be triggered in response to elements in the scenario. For example, an urticaria symptom can be set to turn off upon application of antihistamine and a tachycardia symptom can be set to increase the heart rate by 0.12 bpm over 5 min, up to a max of 170 bpm until IV fluids are given.
2.1.4 Medication module
This system handles medication effects. Medications are specified via a YAML file format with fields for declaring what symptoms are affected, how medications interact with each other, and drug dosing/units. A drug dispensary within the simulation enables the user to retrieve the medication. As medication is given, this system keeps track and interacts with the symptoms module to update the patient state.
2.1.5 Scenario module
This system handles scenario timeline. The simulation is set up as a base state followed by a series of triggered events. The base state which includes items such as the location (e.g., CT scanner room), equipment in the environment, the patient, nonplayable characters (NPC), and available medications. The scenario progresses based on how subsequent events are triggered. Any number of actions can trigger an event such as user action, time, or symptom. When an event is triggered, it updates the necessary modules. A set of default values are included so that every possible scenario combination does not need to be explicitly specified. Scenarios are completed when a user activates an “end state” event. Finally, the system includes a front-end GUI for setting events and triggers. This then generates a YAML file which is interpreted by the simulation in real time. All these systems were developed in house with modularity and future use in mind. In addition, the aim was to create a system that would allow content experts (i.e., physicians) to create scenarios without having to be technical experts (i.e., computer programmers). Creation of a new simulation is therefore as easy as adjusting a few sliders.
2.1.6 Tutorial module
For many users, this will be their first experience with VR. To overcome potential hesitancy with the technology a VR Introduction Tutorial module was developed. This module is a short 5-min interactive tutorial which teaches users the basics of moving and interacting in VR in general and within the simulation environment in specific. Topics including moving, grabbing objects, navigating menus, and starting and ending scenarios are covered. This module can be customized to an institution’s needs.
2.2 Contrast reaction scenario
Utilizing the VR platform described above, three contrast reaction scenarios were developed corresponding to a mild, moderate, and severe reaction (Figure 2). The scenarios were developed utilizing national society American College of Radiology contrast manual best practices (American College of Radiology ACR, 2024), and our own health system best practices. The signs and symptoms needed to determine the severity of the reaction (mild vs. moderate vs. severe) were taken directly from the manual and no additional standardization of validation was performed. The scenario begins with a tutorial introducing the user to the platform. This is followed by a scenario specific introduction. The scenario takes place in a replica of a CT scanner room within our hospital and was designed to be open-ended; the user can perform any of the tasks, in any other order, with success depending on the final outcome (e.g., patient stabilized, or sent to a higher level of care) rather than any specific path. Certain events do require a specific order. For example, donning personal protective equipment (PPE) must occur before interacting with the patient. Certain events can also trigger a fail, such as allow the patient to be hypotensive for greater than 20 min. Users are given access to equipment that would be reasonably expected within a CT scanner room such as blood pressure cuff, pulse oximetry, and ECG. Medications are accessed via a medication dispensing cabinet which requires the user to specify the medication and dosing they need to administer. Extraneous medications can be added to the cabinet to prevent the user from simply guessing the correct medication. As an example, in the mild scenario, the user is presented with a patient with patches of red skin who is endorsing “itching” on their arms. A general path to a successful completion includes donning PPE, obtaining a set of vitals, asking the patient more about their symptoms, administering oral anti-histamine if the blood pressure is appropriate, and then discharging after 30 min of observation (Figure 2).
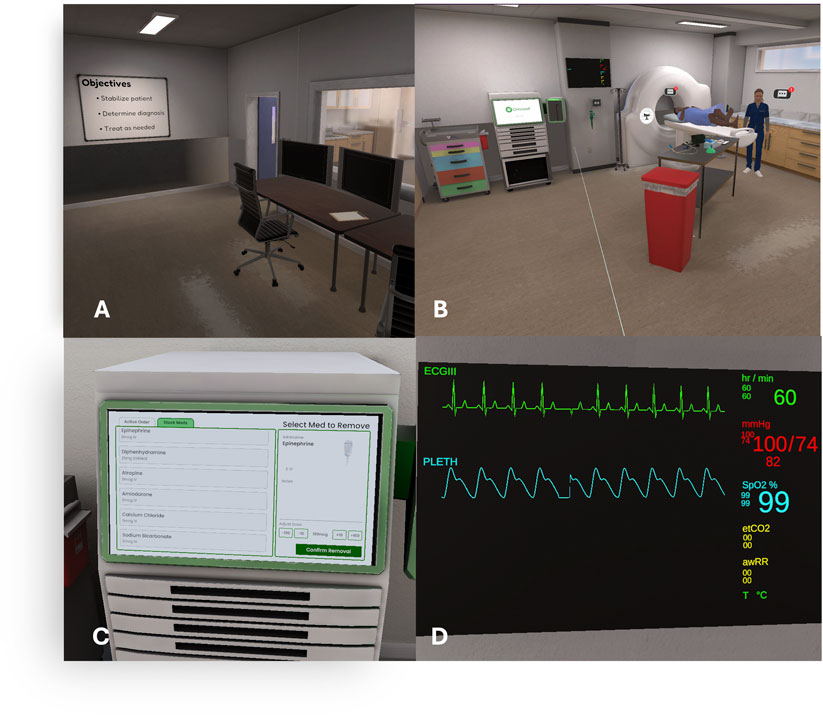
Figure 2. Example snapshots of a contrast simulation scenario. (A) Introduction room briefly describing the task. (B) The computed tomography room in which the simulation takes place with the patient, nurse, vitals monitor, and medication machine. (C) The machine where users obtain the requested medication(s). (D) The vitals monitor which varies with time and/or medication administration.
2.3 Trial design
The study was approved by our local institutional review board (IRB) who provided a waiver for written informed consent as no protect health information (PHI) or other identifying information (user name, location) was obtained and the study was deemed minimal risk. In addition, the first question of the survey re-verified that the participant was voluntarily participating in the study and provided the option to withdraw. The survey was administered via an online survey platform (Qualtrics, Silver Lake). Individual questions from the survey were collated into a single survey. In addition to questions scored on a 1-5 Likert scale from Strongly disagree to strongly agree, symptoms were scored from none to severe while usability was scored from not at all to high. First-year radiology residents at a large urban academic institution were targeted for recruitment as they had the least experience with handling contrast reactions. Residents who agreed were given a VR headset and were asked to complete the scenarios at their convenience in the location of their choosing. The residents were instructed before use on how to safely use VR and selecting a space of at least 1 m × 1 m to allow them to walk around within the VR scenario. Participants were also informed to immediately remove the headset if they experienced any ill effects such as vertigo. The scenarios were presented in random order. Immediately following the completion of the VR scenarios, the users were asked to complete an anonymous survey assessing various aspects of the VR simulation experience (Table 1). The survey was designed to include components of previously validated instruments to assess for motion sickness (Kim et al., 2018), realism (Ralston et al., 2021) difficulty (Hart, 2006), accessibility (Khatkar et al., 2022) and the user’s awareness of technology (Venkatesh and Davis, 2000), (Supplemental 1). To maintain anonymity, the VR headsets were placed in kiosk mode allowing usage without a sign in and no data was collected from the VR headset. In addition, no personal information was collected at the time of the survey including any electronic information such as location.
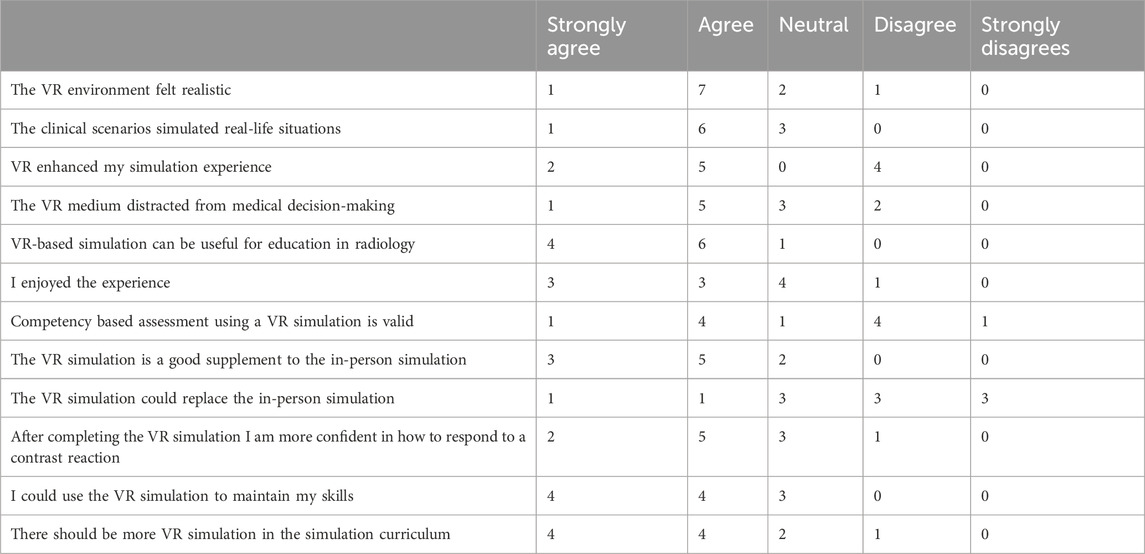
Table 1. Participants views on the VR scenarios for simulation. Note, not all rows add to total participants as participants were allowed to skip questions.
2.4 Statistical methods
Data was analyzed using Excel (v.16.100, Microsoft) and GNU Octave (Eaton et al., 2025). Demographics are summarized with descriptive statistics. Results from the survey are reported as percentages. A Fisher exact test was used to assess for associations between the survey results. No additional statistical testing was attempted as the small sample size with limit interpretation of any result.
3 Results
Thirteen of the 17 eligible radiology residents consented to participate in the study of which 11 completed the survey. Of those that agreed to participate, average age was 31 ± 3.29, 35% were female, and 12% completed a surgical intern year. Within the study group, 36% (4/11) had never used VR and none of the participants who had prior exposure had used it for simulation, training, education. 73% (8/11) found the pre-scenario tutorial helpful but would have liked more training on how to use the VR simulator. The majority of participants agreed that VR-based simulation could be useful for radiology education 91% (10/11) and that VR could be used to maintain skills 73% (8/11) (Table 1). Of the participants who had never used VR 75% (3/4) reported VR to be useful. However, this relationship was not found to be statistically significant (p = 1).
A third of participants 36% (4/11) were moderately uncomfortable wearing the headsets but the majority reported no fatigue 64% (7/11), no headache 64% (7/11) and no eye strain 64% (7/11) (Table 2). Of participants who reported discomfort, 45% (5/11) identified VR as useful, however, this relationship was not found to be statistically significant (p = 1).
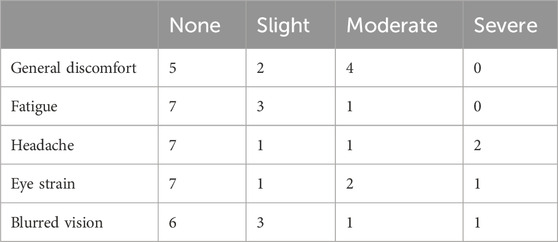
Table 2. Symptoms queried to evaluate for discomfort with values representing number of participants.
Evaluation of the NASA task load index demonstrated effort, physical and mental demand to be the main driving factors for task load resulting in a medium self-assessment of performance (Table 3). No correlation was identified between mental demand task load and perceived usefulness (p = 1).
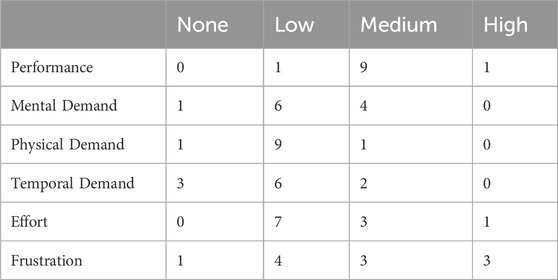
Table 3. NASA task load index. Note, for ‘Performance’, a score of ‘High’ means the participant felt like they performed well while ‘Low’ equates to the perception of performing poorly. For the remaining categories, a low task load score means the task was easy while high means difficult. Values represent number of participants.
Finally, under the technology acceptance model, participants rated an intention to use the technology 82% (9/11), they would receive a benefit 73% (8/11) and that the technology requires low effort to use 64% (7/11) (Table 4).
4 Discussion
A VR simulation platform was developed to address the need for increased cost effective access to medical simulation. As a test of the platform, a set of training simulations on how to handle allergic reactions following intravenous iodinated contrast injection within a CT scanner room were created. A majority of the participants found the VR simulations useful and agreed that VR would be beneficial as a tool for medical simulation.
VR continues to be recognized as a powerful platform for simulation learning. Recent scoping reviews of VR in medical education (Dhar et al., 2023), surgical training (Mao et al., 2021) and interventional radiology (Gelmini et al., 2021) demonstrate a vast but heterogeneous collection of studies investigating VR as a potential education tool. In addition, an increasing number of commercial VR simulation packages are available. Given the breadth of medical knowledge that must be learned and can be simulated, there is little overlap between studies. No similar studies investigating VR for contrast reaction training were identified, making direct comparison difficult.
Our data is overall consistent with the current body of literature which demonstrates that users are generally enthusiastic about this technology and that the majority do not have issues with VR motion sickness while using these tools. A recent systemic review (Shetty et al., 2024) described positive perceptions of VR simulation training for skill development of radiology trainees. However, our study suggests that users may not be ready to use VR as a primary learning and assessment tool, but rather would prefer to use is as an adjunct to in person learning or a refresher for previously learned material and thus better suited for upper level residents or attendings for maintenance of skills. We hypothesize that unfamiliarity with VR technology remains a strong confounding factor. Within our cohort, a third had never used VR and of the users, none had used VR for education. In addition, a third of the cohort reported moderate discomfort, which may be due to a general unease, or unfamiliarity, with the technology as no specific symptom–fatigue, headache, eye strain–was subsequently reported. Absence of prior use makes it inherently more difficult for a user to be comfortable with a technology (Hamilton et al., 2021). 2D screen technology such as desktop computers and smartphones are prolific and most people interact with them multiple times a day. Users are comfortable with the technology thus viewing it as “easy to use.” Users who have grown up with the technology will likely be comfortable with it in a way current users are not. Just as initial users had trouble using personal computers whereas now few tasks can be completed without them.
A major strength of the study is the custom VR platform that was developed. Access to the full software stack allowed the simulation scenario to be custom tailored to the local environment and local practice patterns. In addition, the modularity of the code simplified the creation of the scenario variants. The major limitations of this pilot study are the small sample size and the difficulty measuring true benefit. Sample size was limited by the population size of residents who had not received prior training at our single hospital site. Despite this we believe that the diverse resident group and the location at a large urban academic institute provides generalizability and is consistent with other sample sizes from similar studies evaluating residents training with VR (Lombardo et al., 2022; Lorenz et al., 2025; Kuhn et al., 2024). However, as with all pilot studies, results should be interpreted with caution. In addition, we found recruitment difficult due to an absence of an explicit requirement. American college of graduate medical education (ACGME) maintains a list of requirements that residents must complete to graduate. However, to date, VR simulations are not considered an accepted method for completing these objectives, thus limiting the incentive for users to utilize this learning method. Furthermore, to limit potential bias and enable evaluation of the potential for VR for primary education, we limited recruitment to first year residents who had not received any formal education in contrast reactions. Although this limited the size of the recruitable population, it limited the extent of participant exposure to other potential sources of education which could confound the data. Clinical benefit remains difficult to evaluate due to the low number of truly severe contrast reactions. The low incidence makes it difficult to capture true quantitative outcome data to assess causation between a good (or bad) outcome and quality (and quantity) of medical simulation training due to the large required sample size.
As this is a pilot study several potential avenues for future work are suggested. First, strategies to mitigate discomfort could be performed including optimizing natural changes in visual and locomotion stimuli, decreased session lengths, and novel head mounted display software such as movement blurring to mitigate discomfort (Saredakis et al., 2020). Next, institutional implementation strategies should be performed to educate and promote the technology by purchasing headsets for all incoming residents, identify and address barriers by conducting institution wide anonymous electronics surveys and smaller in person focus groups with key institution stakeholders, and collaborate with the IT department to enable maintenance of these devices (Gupta et al., 2023). Finally, additional studies evaluating the potential role of VR primary learning and maintenance of skills for upper level residents and board certified physicians should be conducted. Important for all these will be the recruitment of larger sample sizes with diverse populations to achieve statistical power but will likely require enterprise-wide adoption of VR simulation technology to achieve these numbers.
5 Conclusion
VR simulation is feasible and well-tolerated for realistic contrast reaction scenarios in its current form and is felt to be beneficial for skills maintenance of radiology residents.
However, in this pilot study, learners do not believe VR simulation should replace in person learning, suggesting that VR simulation should perhaps be developed as a means to maintain knowledge rather than a method of primary knowledge acquisition.
6 Key takeaways
• 91% of participants agreed that VR-based simulation could be useful for radiology education
• VR simulation is feasible and well-tolerated for realistic contrast reaction scenarios in its current form and is felt to be beneficial for skills maintenance by radiology residents.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the University of Pennsylvania Human Research Protections Program. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JK: Writing – original draft, Resources, Writing – review and editing. DW: Resources, Visualization, Investigation, Software, Writing – review and editing, Writing – original draft. MS: Formal Analysis, Writing – original draft, Supervision, Conceptualization, Writing – review and editing. NH: Supervision, Conceptualization, Formal Analysis, Writing – review and editing, Writing – original draft. TG: Writing – review and editing, Writing – original draft. NW: Writing – original draft, Writing – review and editing. KD: Writing – original draft, Formal Analysis, Investigation, Supervision, Conceptualization, Writing – review and editing. AD: Investigation, Resources, Writing – original draft, Conceptualization, Project administration, Writing – review and editing, Methodology, Visualization, Supervision, Validation, Data curation, Formal Analysis.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
Published SPIE Proceedings abstract in Volume13411 - https://doi.org/10.1117/12.3046834.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frvir.2025.1615849/full#supplementary-material
References
American College of Radiology (ACR) (2024). “ACR manual on contrast media,” in Patient selection and preparation strategies before contrast medium administration, 5.
Dhar, E., Upadhyay, U., Huang, Y., Uddin, M., Manias, G., Kyriazis, D., et al. (2023). A scoping review to assess the effects of virtual reality in medical education and clinical care. Digit. Health 9. doi:10.1177/20552076231158022PubMed Abstract | CrossRef Full Text | Google Scholar
Donoghue, A., Heard, D., Griffin, R., Abbadessa, M. K., Gaines, S., Je, S., et al. (2021). Longitudinal effect of high frequency training on CPR performance during simulated and actual pediatric cardiac arrest. Resusc. Plus 6, 100117. doi:10.1016/j.resplu.2021.100117PubMed Abstract | CrossRef Full Text | Google Scholar
Eaton, J. W., Bateman, D., Hauberg, S., and Wehbring, R. (2025). GNU Octave version 10.2.0 manual: a high-level interactive language for numerical computations. Available online at: https://www.gnu.org/software/octave/doc/v10.2.0/.
Elendu, C., Amaechi, D. C., Okatta, A. U., Amaechi, E. C., Elendu, T. C., Ezeh, C. P., et al. (2024). The impact of simulation-based training in medical education: a review. Med. Baltim. 103 (27), e38813. doi:10.1097/MD.0000000000038813PubMed Abstract | CrossRef Full Text | Google Scholar
Farra, S. L., Gneuhs, M., Hodgson, E., Kawosa, B., Miller, E. T., Simon, A., et al. (2019). Comparative cost of virtual reality training and live Exercises for training hospital Workers for Evacuation. Comput. Inf. Nurs. 37 (9), 446–454. doi:10.1097/CIN.0000000000000540PubMed Abstract | CrossRef Full Text | Google Scholar
Gelmini, A. Y., Duarte, M. L., Assis, A. M., Guimarães Junior, J. B., and Carnevale, F. C. (2021). Virtual reality in interventional radiology education: a systematic review. Radiol. Bras. 54 (4), 254–260. doi:10.1590/0100-3984.2020.0162PubMed Abstract | CrossRef Full Text | Google Scholar
Goh, G. S., Lohre, R., Parvizi, J., and Goel, D. P. (2021). Virtual and augmented reality for surgical training and simulation in knee arthroplasty. Arch. Orthop. Trauma Surg. 141, 2303–2312. doi:10.1007/s00402-021-04037-1PubMed Abstract | CrossRef Full Text | Google Scholar
Gupta, S., Wilcocks, K., Matava, C., Wiegelmann, J., Kaustov, L., and Alam, F. (2023). Creating a successful virtual reality-based medical simulation environment: tutorial. JMIR Med. Educ. 9, e41090. doi:10.2196/41090PubMed Abstract | CrossRef Full Text | Google Scholar
Hamilton, D., McKechnie, J., Edgerton, E., and Wilson, C. (2021). Immersive virtual reality as a pedagogical tool in education: a systematic literature review of quantitative learning outcomes and experimental design. J. Comput. Educ. 8, 1–32. doi:10.1007/s40692-020-00169-2CrossRef Full Text | Google Scholar
Hart, S. G. (2006). NASA-task load index (NASA-TLX); 20 years later. Proc. Hum. Factors Ergonomics Soc. Annu. Meet. 50 (9), 904–908. doi:10.1177/154193120605000909CrossRef Full Text | Google Scholar
Jallad, S. T., and Işık, B. (2021). The effectiveness of virtual reality simulation as learning strategy in the acquisition of Medical Skills in Nursing Education: a systematic review. Ir. J. Med. Sci. (1971 -) 191 (3), 1407–1426. doi:10.1007/s11845-021-02695-zPubMed Abstract | CrossRef Full Text | Google Scholar
Katayama, H., Yamaguchi, K., Kozuka, T., Takashima, T., Seez, P., and Matsuura, K. (1990). Adverse reactions to ionic and nonionic contrast media. A report from the Japanese Committee on the Safety of Contrast Media. Radiology 175, 621–628. doi:10.1148/radiology.175.3.2343107PubMed Abstract | CrossRef Full Text | Google Scholar
Khatkar, H., Ferro, A., Kotecha, S., Prokopenko, M., Evans, A., Kyriakides, J., et al. (2022). Assessing the attitude of surgical trainees towards virtual reality simulation: a national cross-sectional questionnaire study. Scott. Med. J. 67 (3), 87–92. doi:10.1177/00369330221103279PubMed Abstract | CrossRef Full Text | Google Scholar
Kim, H. K., Park, J., Choi, Y., and Choe, M. (2018). Virtual reality sickness questionnaire (VRSQ): motion sickness measurement index in a virtual reality environment. Appl. Ergon. 69, 66–73. doi:10.1016/j.apergo.2017.12.016PubMed Abstract | CrossRef Full Text | Google Scholar
Kuhn, A. W., Yu, J. K., Gerull, K. M., Silverman, R. M., and Aleem, A. W. (2024). Virtual reality and surgical simulation training for Orthopaedic Surgery residents: a qualitative assessment of trainee Perspectives. JB JS Open Access 9 (1), e23.00142. doi:10.2106/JBJS.OA.23.00142PubMed Abstract | CrossRef Full Text | Google Scholar
Kurrek, M. M., and Devitt, J. H. (1997). The cost for construction and operation of a simulation centre. Can. J. Anaesth. 44 (11), 1191–1195. doi:10.1007/BF03013344PubMed Abstract | CrossRef Full Text | Google Scholar
Le, K. D. R. (2023). Principles of effective simulation-based teaching sessions in medical education: a Narrative review. Cureus 15 (11), e49159. doi:10.7759/cureus.49159PubMed Abstract | CrossRef Full Text | Google Scholar
Lombardo, R., Walther, N., Young, S., Gorbatkin, C., Sletten, Z., Kang, C., et al. (2022). Ready medic one: a Feasibility study of a Semi-Autonomous virtual reality Trauma simulator. Front. Virtual Real 2, 719656. doi:10.3389/frvir.2021.719656CrossRef Full Text | Google Scholar
Lorenz, M., Knopp, S., Pillen, N., Sanrow, M., Hoffmann, A., Stoiser, V., et al. (2025). HIPS: evaluating a virtual reality training simulation for total hip arthroplasty (THA) and insights into qualitative assessment of surgical training simulations. Front. Virtual Real 6, 1620135. doi:10.3389/frvir.2025.1620135CrossRef Full Text | Google Scholar
Mao, R. Q., Lan, L., Kay, J., Lohre, R., Ayeni, O. R., Goel, D. P., et al. (2021). Immersive virtual reality for Surgical Training: a systematic review. J. Surg. 268, 40–58. doi:10.1016/j.jss.2021.06.045PubMed Abstract | CrossRef Full Text | Google Scholar
Pottle, J. (2019). Virtual reality and the transformation of medical education. Future Healthc. J. 6 (3), 181–185. doi:10.7861/fhj.2019-0036PubMed Abstract | CrossRef Full Text | Google Scholar
Ralston, B. H., Willett, R. C., Namperumal, S., Brown, N. M., Walsh, H., Muñoz, R. A., et al. (2021). Use of virtual reality for pediatric cardiac critical care simulation. Cureus 13, e15856. doi:10.7759/cureus.15856PubMed Abstract | CrossRef Full Text | Google Scholar
Rosen, K. R. (2008). The history of medical simulation. J. Crit. Care 23 (2), 157–166. doi:10.1016/j.jcrc.2007.12.004PubMed Abstract | CrossRef Full Text | Google Scholar
Saredakis, D., Szpak, A., Birckhead, B., Keage, H. A. D., Rizzo, A., and Loetscher, T. (2020). Factors associated with virtual reality sickness in head-mounted displays: a systematic review and Meta-Analysis. Front. Hum. Neurosci. 14, 96. doi:10.3389/fnhum.2020.00096PubMed Abstract | CrossRef Full Text | Google Scholar
Shetty, S., Bhat, S., Al Bayatti, S., Al Kawas, S., Talaat, W., El-Kishawi, M., et al. (2024). The Scope of virtual reality simulators in radiology education: systematic literature review. Med. Educ. 10, e52953. doi:10.2196/52953PubMed Abstract | CrossRef Full Text | Google Scholar
Venkatesh, V., and Davis, F. D. (2000). A theoretical extension of the technology acceptance model: Four longitudinal field studies. Manag. Sci. 46 (2), 186–204. doi:10.1287/mnsc.46.2.186.11926CrossRef Full Text | Google Scholar
Wang, C. L., Cohan, R. H., Ellis, J. H., Caoili, E. M., Wang, G., and Francis, I. R. (2008). Frequency, outcome, and appropriateness of treatment of nonionic iodinated contrast media reactions. AJR Am. J. Roentgenol. 191, 409–415. doi:10.2214/ajr.07.3421PubMed Abstract | CrossRef Full Text | Google Scholar
Keywords: virtual reality, simulation, resident education, radiology, contrast reactions
Citation: Karp JD, Weber D, Sheng M, Harrison NE, Gade TP, Williams N, Dumon K and Dhanaliwala AH (2025) Feasibility and perceived utility of immersive virtual reality for training radiology residents in contrast reaction management: a pilot study. Front. Virtual Real. 6:1615849. doi: 10.3389/frvir.2025.1615849
Received: 22 April 2025; Accepted: 08 September 2025;
Published: 18 September 2025.
Edited by:
Chukwuka Elendu, American College of Cardiology, United StatesReviewed by:
Mark Anthony Torio, University of Perpetual Help System DALTA- Molino, PhilippinesShishir Shetty, University of Sharjah, United Arab Emirates
Copyright © 2025 Karp, Weber, Sheng, Harrison, Gade, Williams, Dumon and Dhanaliwala. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: John D. Karp, a2FycGpAcGVubm1lZGljaW5lLnVwZW5uLmVkdQ==
 John D. Karp
John D. Karp Daniel Weber2
Daniel Weber2 Ali H. Dhanaliwala
Ali H. Dhanaliwala