- 1Department of Pharmacy Practice, College of Clinical Pharmacy, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia
- 2College of Clinical Pharmacy, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia
- 3Department of Clinical Pharmacy, College of Pharmacy, Umm Al Qura University, Makkah, Saudi Arabia
- 4Department of Clinical Pharmacy, College of Pharmacy, Prince Sattam bin Abdulaziz University, Alkharj, Saudi Arabia
- 5Pharmaceutical Research Center, Deanship of Scientific Research, Umm Al Qura University, Makkah, Saudi Arabia
- 6Department of Pharmacy, King Abdulaziz Hospital, National Guard Health Authority, Alahsa, Saudi Arabia
- 7Department of Clinical and Hospital Pharmacy, College of Pharmacy, Taibah University, Al-Madinah Al-Munawarah, Saudi Arabia
- 8Department of Clinical Pharmacy, School of Pharmaceutical Sciences, University Sains Malaysia, Penang, Malaysia
- 9Department of Pharmacy Practice, Kulliyah of Pharmacy, International Islamic University Malaysia, Kuantan, Malaysia
- 10Qualitative Research-Methodological Application in Health Sciences Research Group, Kulliyyah of Pharmacy, International Islamic University Malaysia, Kuantan, Malaysia
Objective: The study aimed to evaluate the association between disease knowledge and medication adherence in patients with type 2 diabetes mellitus.
Methods: A cross-sectional study was conducted for three months, in patients with type 2 diabetes who visited three community pharmacies located in Khobar, Saudi Arabia. Patients’ disease knowledge and their adherence to medications were documented using Arabic versions of the Michigan Diabetes Knowledge Test and the General Medication Adherence Scale respectively. Data were analyzed through SPSS version 23. Chi-square test was used to report association of demographics with adherence. Spearman’s rank correlation was employed to report the relationship among HbA1c values, disease knowledge and adherence. Logistic regression model was utilized to report the determinants of medication adherence and their corresponding adjusted odds ratio. Study was approved by concerned ethical committee (IRB-UGS-2019-05-001).
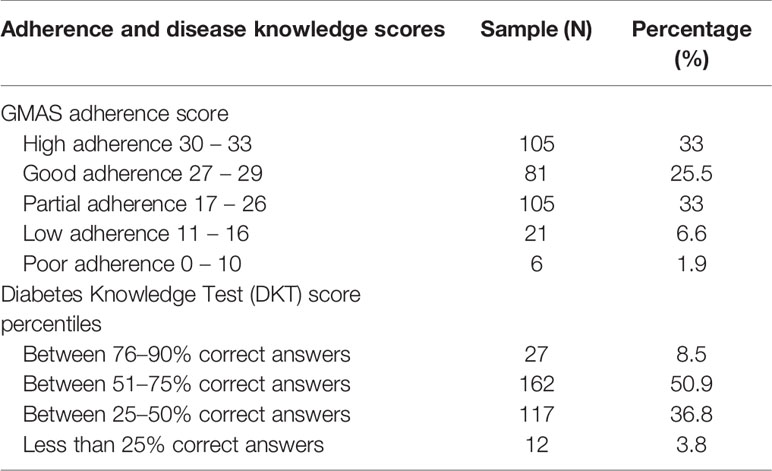
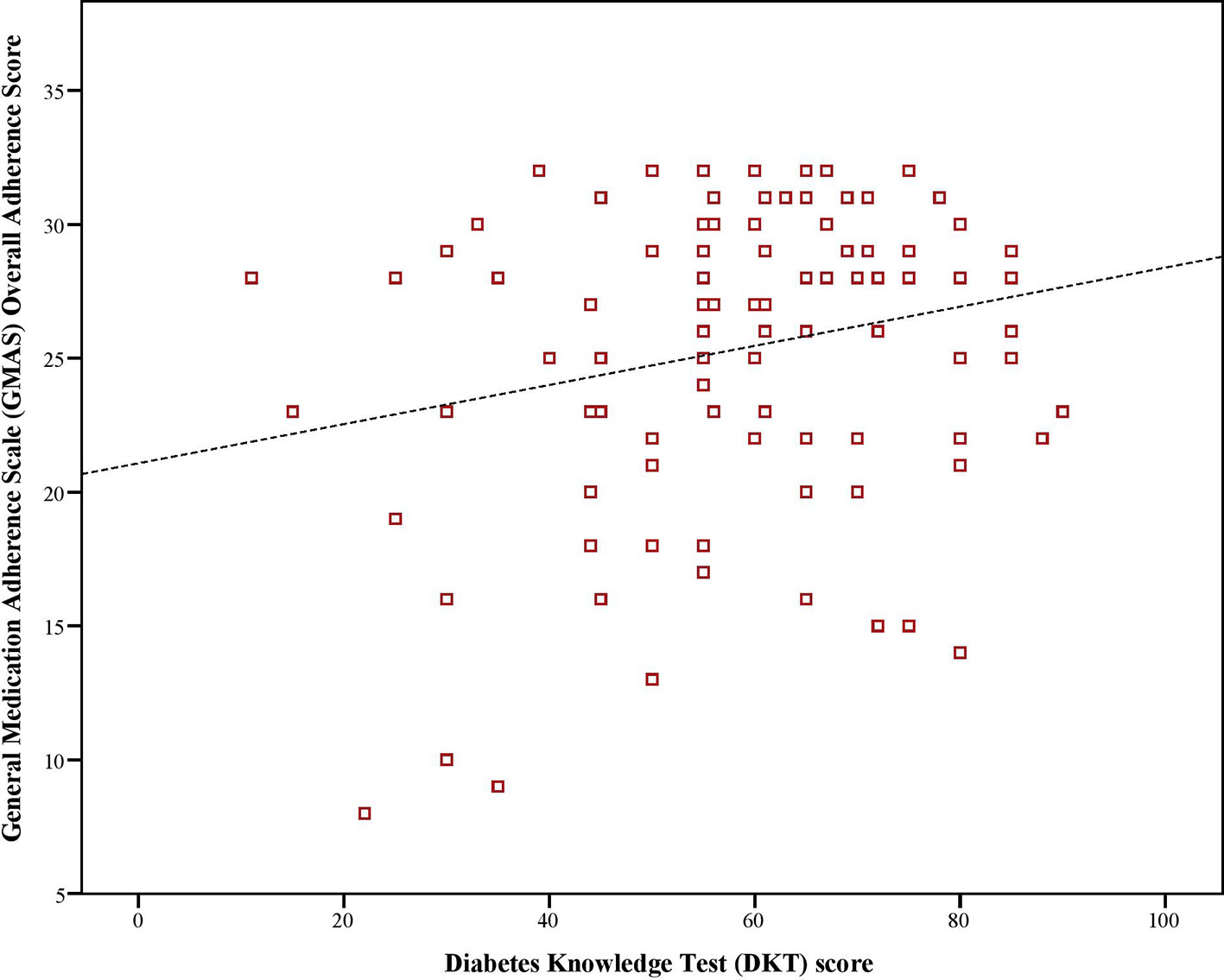
Results: A total of 318 patients consented to participate in the study. Mean HbA1c value was 8.1%. A third of patients (N = 105, 33%) had high adherence and half of patients (N = 162, 50.9%) had disease knowledge between 51% - 75%. A significantly weak-to-moderate and positive correlation (ρ = 0.221, p < 0.01) between medication adherence and disease knowledge was reported. Patients with >50% correct answers in the diabetes knowledge test questionnaire were more likely to be adherent to their medications (AOR 4.46, p < 0.01).
Conclusion: Disease knowledge in most patients was average and half of patients had high-to-good adherence. Patients with better knowledge were 4 to 5 times more likely to have high adherence. This highlights the importance of patient education and awareness regarding medication adherence in managing diabetes.
Introduction
Diabetes mellitus (DM) is a type of chronic illness that requires careful management with medications to keep blood glucose level in recommended range (Abahussain and El-Zubier, 2005; World Health Organization, 2010; Abbas et al., 2015). The disease could result in micro and macro vascular complications that have serious short and long-term repercussions. Estimation of glycated hemoglobin (HbA1c) is done to monitor the disease and forms the basis of treatment recommendations (Nazir et al., 2016). Patient adherence to anti diabetic medication therapy results in better control of disease and may help to keep HbA1c in recommended range (Al Dawish et al., 2016). There is a plethora of studies that highlight the importance of adhering to medications in type 2 diabetes mellitus (Al-Nozha et al., 2004; Abahussain and El-Zubier, 2005; Abbas et al., 2015; Al Dawish et al., 2016). However, it is imperative to improve patients’ disease knowledge to achieve high adherence to therapy (Yeh et al., 2018).
Patient education with an emphasis on adherence to anti diabetic medications and how it contributes positively to disease, would empower them to become compliant to prescribed therapy and, recognize and self-manage disease symptoms at home. Conversely, low literacy regarding disease is associated with poor treatment outcomes and a higher cost of therapy (Al-Nozha et al., 2004). Therefore, assessment of disease knowledge might be helpful in uncovering one of the determinants of poor disease outcome. Moreover, its relationship with adherence also provides an estimate of the extent to which knowledge translates into patients’ efforts for achieving treatment goals (Fawad et al., 2014; Abbas et al., 2015). Medication adherence in diabetic patients may be defined as the extent to which a patient remains committed to taking anti diabetic medications in right dose and frequency (Al Dawish et al., 2016). Patients and healthcare providers have a role to play in improving medication adherence (Brown and Bussell, 2011). Studies have emphasized that improvement in disease knowledge go hand-in-hand with improved medication adherence (Zullig et al., 2015).
Figures from International Diabetes Federation (IDF) report that globally there were more the 400 million patients living with diabetes in 2015. The World Health Organization estimates that there will be over 592 million patients with type 2 DM in 2035 (World Health Organization, 2016). The prevalence of type 2 DM in Saudi Arabia was 18.5% and has increased during the past decade (International Diabetes Federation, 2019). It remains as one of the main causes of death and disability in the country (Hussain et al., 2014; Sami et al., 2017). Saudi Arabia has the second largest diabetic population in the Gulf region and seventh largest in the world (Al Dawish et al., 2016). Evidence indicates that DM is more prevalent in urban areas and in males (Al-Nozha et al., 2004). The crude death rate is estimated to be 2.25% (95% CI: 2.02–2.5%) and accounts for 4.78% of total years lived with disability (95% CI: 3.86–5.7%) (Institute for Health Metrics and Evaluation, 2017) Ministry of Health KSA (2014).
Previous researches have highlighted a low adherence to medication therapy, poor self-management and an unsatisfactory disease knowledge in Saudi patients with diabetes. However, none of the studies investigated the relationship between disease knowledge and medication adherence (Abahussain and El-Zubier, 2005; Al-Aboudi et al., 2016; Alanazi et al., 2017).
Methods
Objective
The study examined the association between disease knowledge and medication adherence in patients with type 2 diabetes. The study also analyzed relationship between HbA1c (%) as a proxy for disease control, with adherence and disease knowledge.
Duration and Venue of Study
A cross-sectional study was conducted for three months in three community pharmacies located in Khobar city of Saudi Arabia. Community pharmacies from three districts of the city were randomly selected.
Target Population and Eligibility Criteria
All adult male and female out-patients, with or without comorbidities, who had established diagnosis of type 2 diabetes mellitus at least three months before the study, were identified as target population for this study. Patients not fulfilling the above criteria and those with an acute illness, diabetes complication and/or planned surgery were considered ineligible.
Participants’ Recruitment
There were three types of patients who visited pharmacies for their medication needs; patients who obtained medicines through government supply, patients with corporate insurance and, patients who paid out-of-pocket cost. All patients had a medical record number (MRN). This MRN was obtained from patients and entered into the pharmacy software to retrieve electronic prescriptions. In addition to being used to check patients’ eligibility, the electronic patient records provided Hb1Ac related data. Following confirmation of diabetes, they were briefed about the study. Those who agreed to participate were handed a written informed consent form. Patients who signed the consent were included in the study.
Sampling Procedure and Sample Size
Convenience sampling procedure was employed to obtain information from patients who visited the community pharmacies. Data collection was done at a time of convenience, i.e., on weekends during evening hours. This time was selected based on peak visiting hours. The sample size was calculated based on disease prevalence with help of an online sample size calculator (Sampsize, 2019). The prevalence of DM according to IDF Report was 18.5% (International Diabetes Federation, 2019). This figure was entered in the calculator keeping a two-tailed alpha error rate of 0.05%, confidence level was kept at 95% and precision was set at 5%. The required sample size was 232 patients. A drop-out of 30% was added and final sample size required was 302. Post hoc power was calculated and was reported >85% (Cohen, 1988; Hertzog, 2008; Zhang et al., 2019).
Research Instrument
The research instruments used for evaluation of patient’ disease knowledge and medication adherence were the Arabic versions of the Revised Diabetes Knowledge Questionnaire (DKT) and, the General Medication Adherence Scale (GMAS) respectively (Collins et al., 2011; Alhaiti et al., 2016; Fitzgerald et al., 2016; Naqvi et al., 2018; Naqvi and Hassali, 2019; Naqvi et al., 2019a; Naqvi et al., 2019b). The Arabic version of the Revised Diabetes Knowledge Questionnaire (DKT-2) is a 23-item questionnaire containing multiple choice questions (MCQs) to assess the knowledge of diabetes mellitus. It is a validated tool to measure disease knowledge with good internal consistency. The scale assesses a patient’s knowledge regarding the disease, complication, diet, treatment and monitoring, etc. (Alhaiti et al., 2016). The General Medication Adherence Scale (GMAS) was recently developed and validated in Saudi patients with chronic diseases. It contains 11 items and each item have 4 options (Naqvi et al., 2019a). The scale measures adherence to medications considering patient’s behaviors, comorbidities and out-of-pocket expenditures. Each option awards a score and sum of all individual scores yields a patient’s adherence to medication (Naqvi et al., 2018; Naqvi et al., 2019a; Naqvi et al., 2019b).
Data Analyses
The data obtained were analyzed through SPSS version 23 and expressed as sample counts (N) and percentages (%). The data were checked for distribution and outliers by informal methods (Dunn and Clark, 1987; Islam et al., 2016). Based on data distribution, descriptive statistics as mean (X) and standard deviation (SD) were used for normally distributed data while median (M) and interquartile range (IQR) were used to report non-normally distributed data. Percentiles were used to report categorical data. Chi-square (χ2) test and cross tabulation was used to examine the association between patient demographics and medication adherence. Spearman’s rank correlation (r) was employed to report the relationship between disease knowledge and medication adherence. Adherence was assessed using multivariable logistic regression models, adjusting for patient baseline characteristics by using significant variables obtained from the Chi-Square (χ2) tests. The reliabilities of the GMAS and DKT questionnaires were analyzed using Cronbach alpha (α) (Cronbach, 1951; Cohen, 1988).
Ethical Approval and Consent
The study was approved from the Institutional Review Board of Imam Abdulrahman Bin Faisal University (IRB-UGS-2019-05-001). Permission was also obtained from the pharmacies. A written informed consent was obtained from patients before participation.
Results
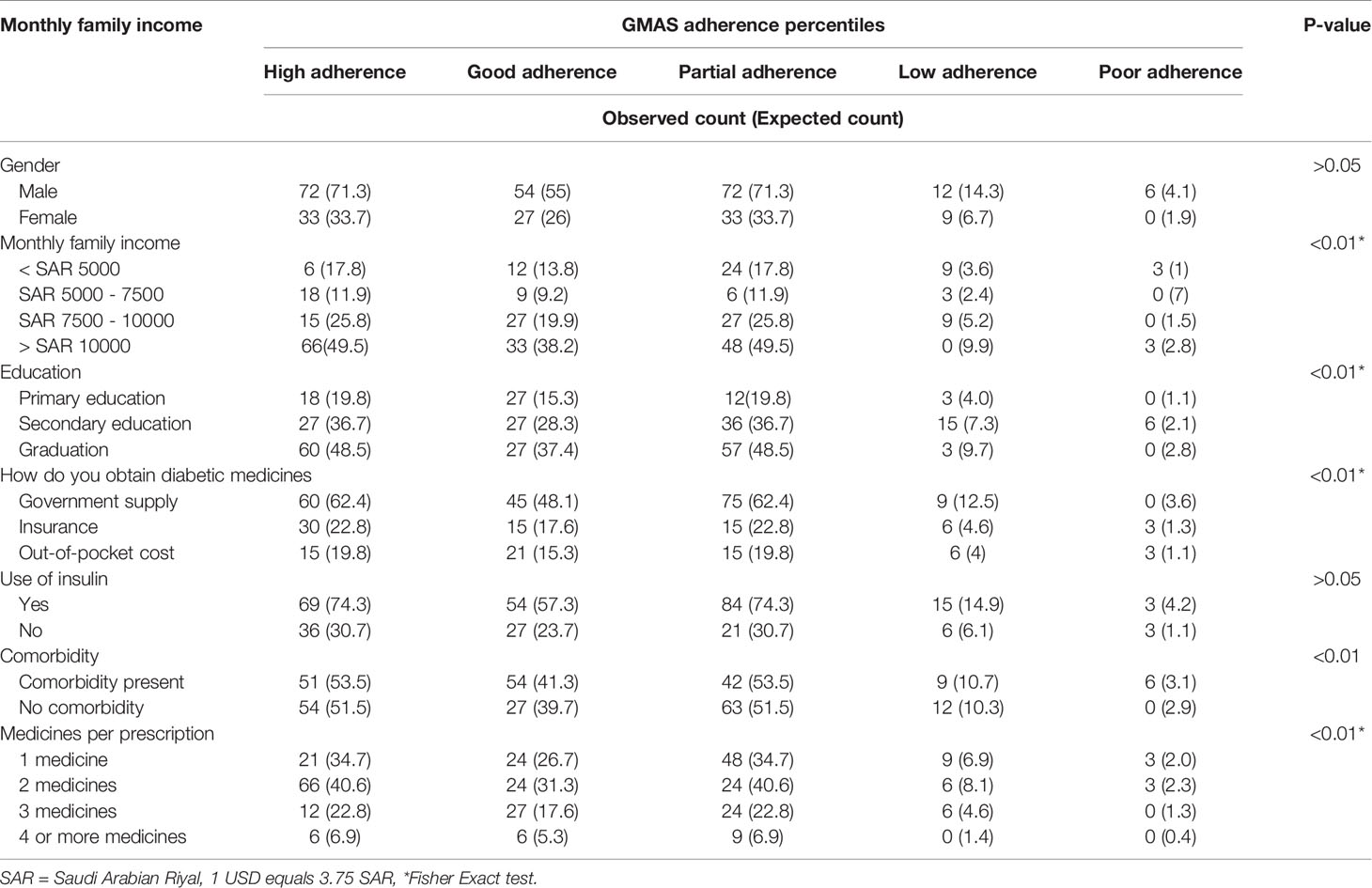
A total of 318 patients consented to participate in the study. The reliabilities of GMAS and DKT questionnaires were reported at 0.81 and 0.75 respectively, i.e., satisfactory. The mean age of patients was 44 ± 15.5 years. The majority was male (N = 216, 67.9%), married (N = 231, 72.7%) with an income above SAR 10,000 (N = 150, 47.2%). Slightly less than half (N = 147, 46.2%) were university graduates. More than a third of patients had 1 – 3 comorbidities (N = 147, 46.2%). More than a third of patients (N = 123, 38.7%) were prescribed at least two medicines. Most patients were on insulin therapy (N = 225, 70.8%). More than half of patients had government insurance (N = 189, 59.4%) (Table 1).
Out of total 147 patients with comorbidities, 30.6% had one comorbidity (N = 45), 60.5% had 2 comorbidities (N = 89) and 8.9% had three comorbidities (N = 13). Those who had one comorbidity (N = 45, 30.6%) mainly had a disease of cardiovascular origin along with DM. Those who had two comorbidities (N = 89, 60.5%), had cardiovascular + other endocrine diseases for most part and, to some extent, cardiovascular + pulmonary diseases, cardiovascular + musculoskeletal diseases, and, cardiovascular + liver/kidney diseases. Those who had 3 comorbidities (N = 13, 8.9%), had a combination of either cardiovascular + other endocrine diseases + liver/kidney disease or, cardiovascular + other endocrine diseases + musculoskeletal diseases, etc.
The average adherence score was 25.3 out of total 33 [median 27, IQR 7]. A third of patients (N = 105, 33%) had high adherence followed by same number of patients who were partially adherent. The average score for DKT-2 was 56.46 ± 16.7 out of 100. Most patients (N = 162, 50.9%) had disease knowledge score between 51–75%. (Table 2).
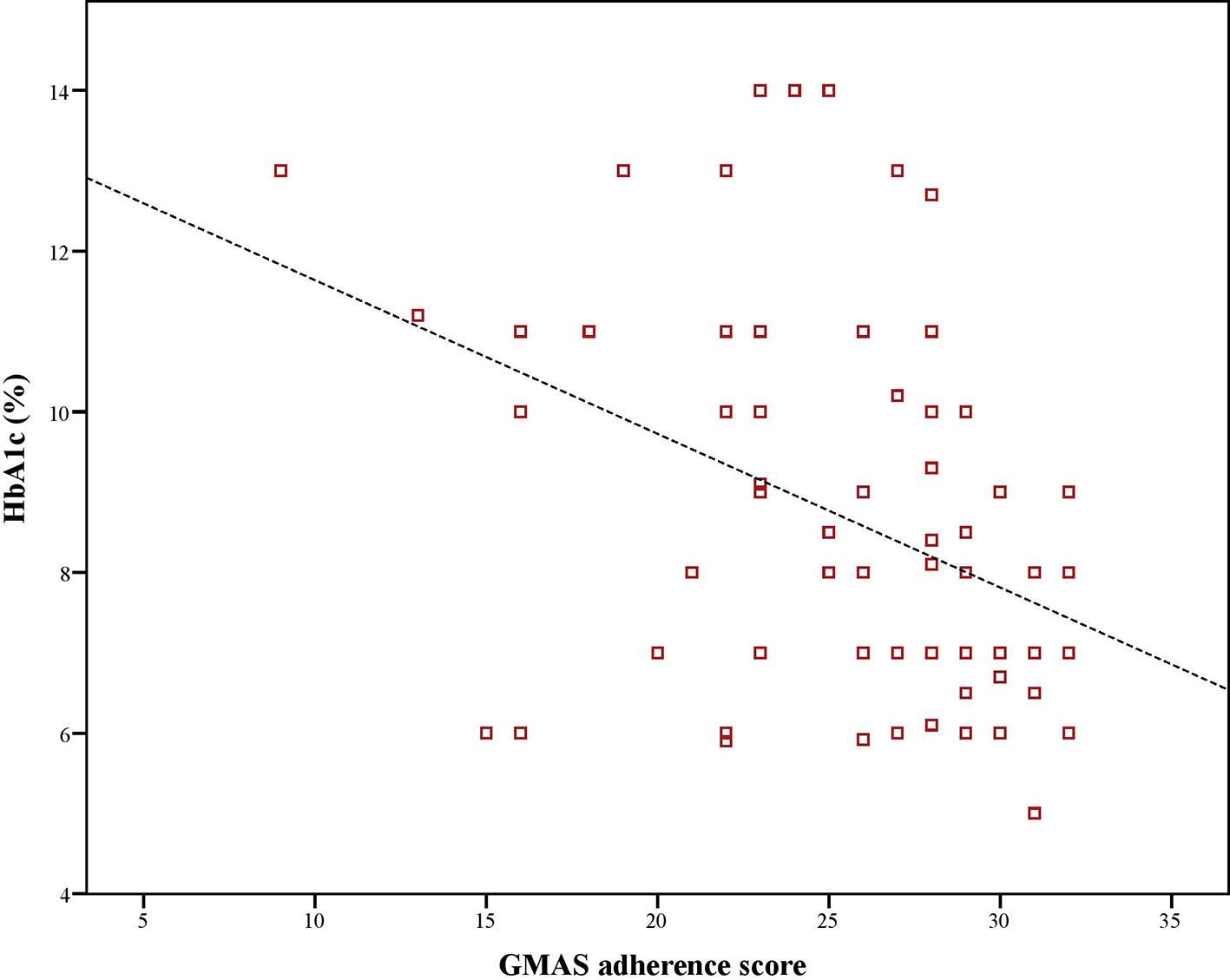
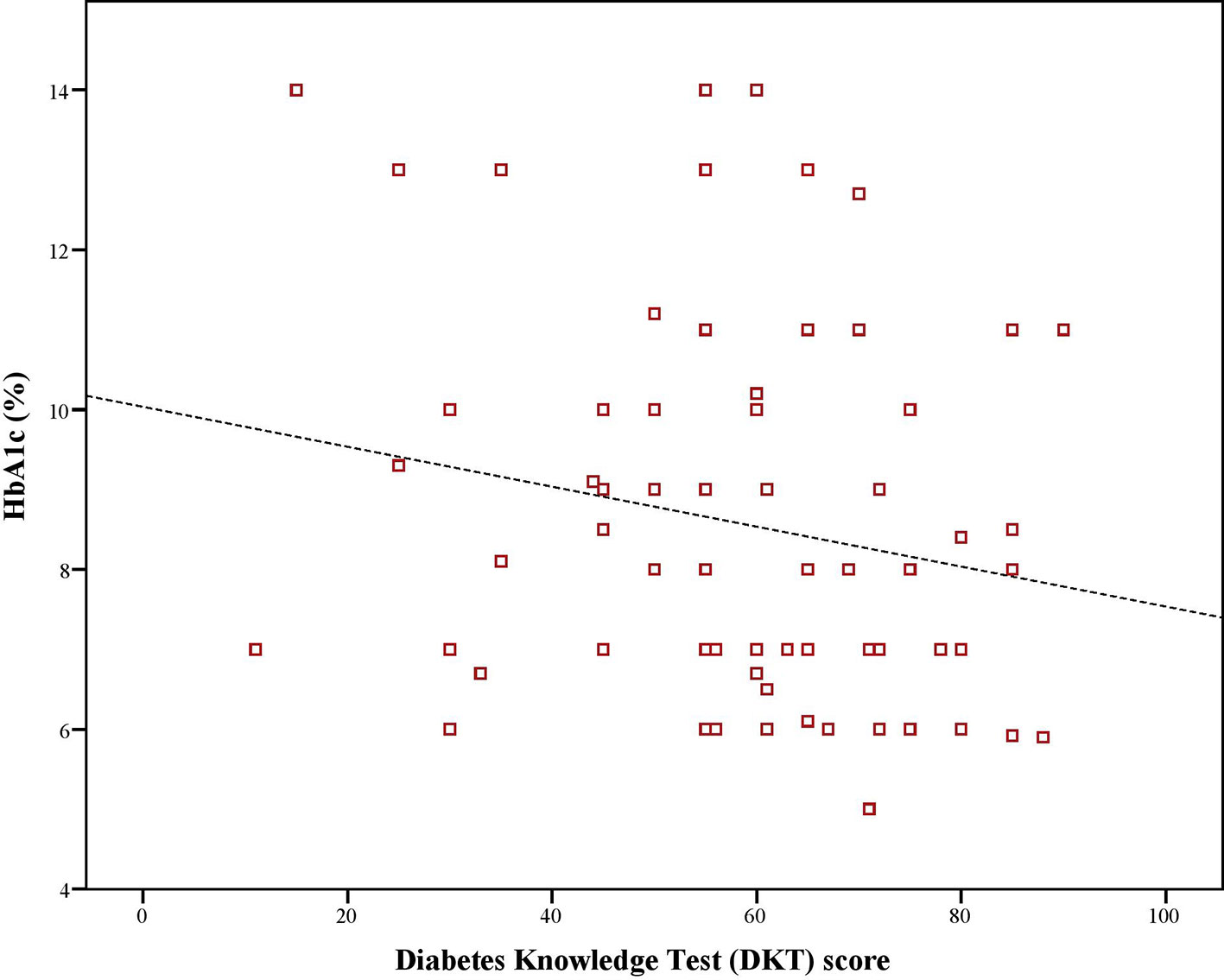
Mean HbA1c value was 8.1%. There was a significant, negative, moderate-to-strong relationship between adherence score and, HbA1c values (ρ = –0.423, p < 0.01). Similarly, there was a significant, negative and weak-to-moderate relationship between HbA1c values and disease knowledge (ρ = –0.199, p < 0.01). Moreover, there was a significant, positive, weak-to-moderate correlation (ρ = 0.221, p < 0.01) between adherence and disease knowledge scores of diabetic patients (Figures 1–3).
There was a significant association between GMAS adherence percentiles and monthly family income (χ2 = 56.85, p < 0.01). The patients with a monthly family income less than SAR 5000 were observed in higher numbers in partial, low and poor adherence percentiles as compared to patients with higher income. Similarly, a significant association existed between adherence and education level (χ2 = 46.02, p < 0.01) as graduates were mostly observed to have a high adherence compared to patients who had primary or secondary education. Besides, a significant association was observed between adherence and mode of obtaining medicines (χ2 = 23.97, p < 0.01) as patients who obtained their medications by out-of-pocket expenditure were mostly seen in lower adherence percentiles.
There was a significant association between adherence and comorbidity (χ2 = 19.6, p < 0.01) as patients with comorbidity were mostly observed in high and good adherence percentiles. A significant association was reported between adherence and number of medicines per prescription (χ2 = 51.65, p < 0.01) as most patients prescribed with 2 medicines were mostly in high adherence percentile. Statistical significance was not achieved for association between adherence percentiles and; gender as well as, use of insulin (Table 3).
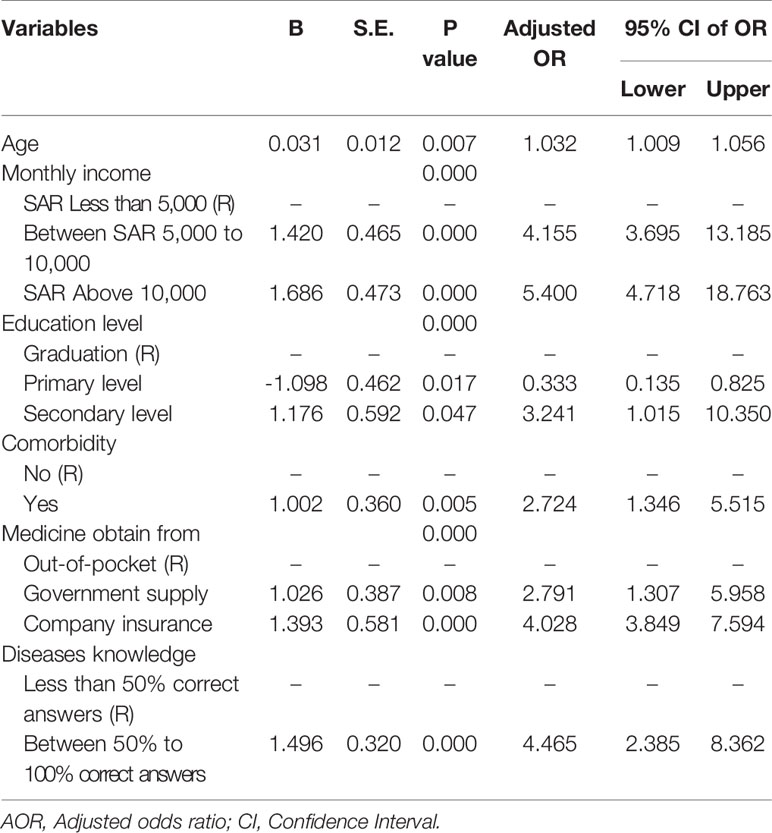
Further analysis using multiple logistic regression revealed that patients who had a monthly family income above SAR 10,000 were five times more likely to be adherent (AOR = 5.4, p < 0.01) compared to patients with income lower than SAR 5,000. Besides, patients with comorbidity were two to three times more likely to be adherent to their medications (AOR = 2.7, p < 0.01). Moreover, patients who obtained their medications from insurance were four times more likely to be adherent as compared to those patients who paid out-of-pocket. On the negative side, patients with primary education were less likely to be adherent (AOR = 0.3, p < 0.01) compared to patients who were graduates. Finally, patients who answered more than 50% correct answers in the diabetes knowledge test questionnaire were observed to be 4–5 times more likely to be adherent to their medications (AOR 4.46, p < 0.01). The model was adjusted for age, income, education comorbidity and method of obtaining medicines, to amend for potential confounder of the relationship between disease knowledge and medication adherence. The model for medication adherence is tabulated in Table 4. In multiple logistic regression, “Enter” method was applied, multicollinearity was checked and was not found. Hosmer-Lemeshow test value was reported at χ2 = 11.334, p = 0.183 while Nagelkerke R Square value was 0.497.
Discussion
Several studies have been conducted on measuring adherence to medications as well as knowledge regarding disease in Saudi patients with diabetes however, studies that examine the link between adherence and disease knowledge are lacking. This study was novel in this aspect and reported a weak-to-moderate positive relationship between the two. Moreover, it further revealed a moderate-to-strong negative relationship between adherence score and glycated haemoglobin A1c value as well between disease knowledge and same. HbA1c was considered as a proxy for disease control as the American Diabetes Association (ADA) mentions a better HbA1c value as an indicator for adequate glycemic control over 4 months (Sherwani et al., 2016). This approach has been previously used by AlQarni et al. (2019) in Saudi patients with T2DM. All correlations were statistically significant. This implied that patients who had better adherence and disease knowledge demonstrated better glycemic control. Moreover, it further highlighted that knowledge about the disease and adherence to therapy were related. Better knowledge contributes to better adherence. This finding was in line with previously reported literature that mentions disease literacy as a determinant of achieving positive treatment outcomes (Yeh et al., 2018; AlQarni et al., 2019). Our findings are in line with the results of Nazir et al. (2016) as there was a negative relationship between HbA1c value and, adherence and disease knowledge in patients with diabetes in Pakistan. Moreover, we also found disease knowledge as a determinant of adherence as patients with more than average knowledge of diabetes were 4 to 5 times more likely to be adherent to medications. In another study, patients with HbA1c values less than 6.5% had better disease knowledge and adherence (Al-Qazaz et al., 2011). In a systematic review, Kardas et al. (2013) reported that disease knowledge was a determinant of persistence. Better disease knowledge results in improved symptom recognition and self-management. It empowers patients to understand the importance of adherence and consequences of non-adherence (Zullig et al., 2015). Based on health behavior theory, patients would choose a behavioral option that helps them achieve a healthy status which in this case would be adhering to prescribed therapy that improves glycemic control (Becker, 1974; Nazir et al., 2016).
The scores for disease knowledge and adherence reported for Saudi patients were not satisfactory as less than 60% had high-to-good adherence and majority had average disease knowledge. This increases the likelihood of negative disease outcomes such as micro and macro vascular complications namely cardiovascular diseases, eyes and kidney damage, etc. Besides, it could also result in cerebrovascular events such as stroke. All these outcomes contribute to disability, morbidity, increase economic burden and lost productivity. These outcomes could worsen the health-related quality of life of diabetic patients and may increase likelihood of mortality in severe cases. Moreover, psychological impact of such outcomes may result in the form of depression. In this context, a study in Pakistan reported undiagnosed depression in diabetic patients (Abbas et al., 2015). Hence, this knowledge barrier could be a reason that diabetes remains as one of the main causes of death and disability in Saudi Arabia (Institute for Health Metrics and Evaluation, 2017).
Increasing health literacy remains a challenge in Saudi population. Recently, a large sample size study highlighted that more than half of Saudi population had low health literacy. The study stressed on the need to design and execute health literacy programs and campaigns (Abdel-Latif and Saad, 2019). Quite the reverse, Mashi et al. (2019) reported that there was high health literacy that was not associated with glycemic control, in Saudi patients with type 2 diabetes. Our study results contradict the findings of Mashi et al. (2019). This was evident in this study as most patients were graduates but had unsatisfactory disease awareness. An average HbA1c value of 8.1% explains that despite being educated, the patients’ diabetes were not adequately controlled. Moreover, most patients were on insulin therapy which further strengthen this proposition. This finding was in line with the work of Rabba et al. (2017). The study further highlighted that individual patient characteristics such as education, income, insurance and comorbidities may act as determinants of medication adherence. This occurrence was in line with previous study by AlQarni et al. (2019). However, the fact that education does not act as a determinant of disease awareness in this population uncovers the need to initiate diabetes awareness campaigns to educate patients about the disease, its symptoms and self-management that includes adherence to treatment. All healthcare professionals need to play a role in patient education.
Pharmacists fill prescriptions for patients after consultations. They are last healthcare professional patients see before leaving the hospitals. Pharmacist provide routine drug information service in Saudi hospitals (Alamri et al., 2017). Therefore, educational interventions by pharmacist could be more beneficial as compared to interventions by other HCPs. Moreover, pharmacists provide pharmaceutical care in which one of the core areas is patient education (Shah et al., 2016; Naqvi et al., 2019c). Studies that evaluate the benefits of an educational intervention by pharmacists to improve disease knowledge and adherence are recommended. The use of convenience sampling might have made it difficult to generalize the findings however, the demographics obtained in the current study were quite similar to the results of study by AlQarni et al. (2019) that used random sampling. Nonetheless, the results should be interpreted with caution.
Conclusion
The disease knowledge in most patients was average and half of patients had high-to-good adherence. A significant weak-to-moderate correlation between disease knowledge and medication adherence was present. Moreover, there was a significantly moderate-to-strong, negative relationship between HbA1c and, disease knowledge as well as adherence. This revealed that glycemic control was better in patients with good knowledge of diabetes and high adherence to anti diabetic medications. A positive relationship between disease knowledge and adherence score was observed that highlights the impact of disease awareness on treatment concordance. This may result in better control of disease. These results highlight the importance of patient education and awareness regarding medication adherence in managing diabetes.
Author’s Note
This manuscript is based on undergraduate research thesis submitted by AA and OA; students of Pharm.D 5th Year for partial fulfillment of the degree of Doctor of Pharmacy (Pharm.D) at College of Clinical Pharmacy, Imam Abdulrahman Bin Faisal University, Dammam 31441, Saudi Arabia. No funding was sought for the study. The work was a collaborative assignment of Evidence Based Improvement (EBI) initiative team and supervisors from Saudi and Malaysian universities (Abbas, 2014; Naqvi, 2016).
Data Availability Statement
All datasets generated for this study are included in the article/supplementary material.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Review Board, IAU (IRB-UGS-2019-05-001). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
DA, AN, OA, and AA conceived the idea and designed the study. AA and OA formulated initial draft of introduction and DA and AN finalized it. SG, AH, MA, MSI, ME, and AI conducted literature review and added their part in the introduction. The methodology was jointly written by all authors as they were involved in data collection. Data was entered by DA, AN, OA, AA, and SG. Data analyses was carried out by AN, SG, MM, IK, and SJ. The re-analysis of data in the revised version was done by MAI. The results section were written by OA, AA, MM, and IK and were re-checked by SJ. The results section in revised version was modified by AN and MAI. The discussion and conclusion was written by MM, IK, AN, MA, AH, MSI, ME, and AI. During revision of manuscript all authors provided their insights. The whole process was supervised by SJ.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Abahussain, N. A., El-Zubier, A. G. (2005). Diabetes knowledge among self reported diabetic female teachers: Al-Khobar, Saudi Arabia. J. Family Community Med. 12, 43–48.
Abbas, A., Nasir, H., Zehra, A., Noor, A., Jabbar, F. A., Siddqui, B. (2015). Assessment of depression as comorbidity in diabetes mellitus patients using beck depression inventory II (BDI II) scale. J. Young Pharm. 7, 206–216. doi: 10.5530/jyp.2015.3.11
Abbas, A. (2014). Evidence based improvements in clinical pharmacy clerkship program in undergraduate pharmacy education: the evidence based improvement (EBI) initiative. Pharmacy 2, 270–275. doi: 10.3390/pharmacy2040270
Abdel-Latif, M. M. M., Saad, S. Y. (2019). Health literacy among Saudi population: a cross-sectional study. Health Promotion Int. 34, 60–70. doi: 10.1093/heapro/dax043
Al Dawish, M. A., Robert, A. A., Braham, R., Al Hayek, A. A., Al Saeed, A., Ahmed, R. A., et al. (2016). Diabetes Mellitus in Saudi Arabia: a review of the recent literature. Curr. Diabetes Rev. 12, 359–368. doi: 10.2174/1573399811666150724095130
Al-Aboudi, I. S., Hassali, M. A., Shafie, A. A. (2016). Knowledge, attitudes, and quality of life of type 2 diabetes patients in Riyadh, Saudi Arabia. J. Pharm. Bioall. Sci. 8, 195–202. doi: 10.4103/0975-7406.171683
Alamri, S. A., Ali Jaizani, R., Naqvi, A. A., Al Ghamdi, M. S. (2017). Assessment of drug information service in public and private sector tertiary care hospitals in the eastern province of Saudi Arabia. Pharm. (Basel.) 5, 37. doi: 10.3390/pharmacy5030037
Alanazi, A. M., Abo El-Fetoh, N. M., Alotaibi, H. K., Alanazi, K. A., Alotaibi, B. K., Alshammari, S. M., et al. (2017). Survey of awareness of diabetes mellitus among the Arar population, Northern Border Region of Saudi Arabia. Electron. Physician 9, 5369–5374. doi: 10.19082/5369
Alhaiti, A. H., Alotaibi, A. R., Jones, L. K., DaCosta, C., Lenon, G. B. (2016). Psychometric evaluation of the revised michigan diabetes knowledge test (V.2016) in Arabic: translation and validation. J. Diabetes Res. doi: 10.1155/2016/9643714
Al-Nozha, M. M., Al-Maatouq, M. A., Al-Mazrou, Y. Y., Al-Harthi, S. S., Arafah, M. R., Khalil, M. Z., et al. (2004). Diabetes mellitus in Saudi Arabia. Saudi. Med. J. 25, 1603–1610.
AlQarni, K., AlQarni, E. A., Naqvi, A. A., AlShayban, D. M., Ghori, S. A., Haseeb, A., et al. (2019). Assessment of medication adherence in saudi patients with type II diabetes mellitus in Khobar City, Saudi Arabia. Front. Pharmacol. 10, 1306. doi: 10.3389/fphar.2019.01306
Al-Qazaz, H. K., Sulaiman, S. A., Hassali, M. A., Shafie, A. A., Sundram, S., Al-Nuri, R., et al. (2011). Diabetes knowledge, medication adherence and glycemic control among patients with type 2 diabetes. Int. J. Clin. Pharm. 33, 1028–1035. doi: 10.1007/s11096-011-9582-2
Becker, M. H. (1974). The health belief model and personal health behavior. vol. 2 (Thorofare, NJ: Slack, Inc).
Brown, M. T., Bussell, J. K. (2011). Medication adherence: WHO cares? Mayo. Clin. Proc. 86, 304–314. doi: 10.4065/mcp.2010.0575
Cohen, J. (1988). Statistical power analysis for the behavioral sciences. 2nd ed. (Mahwah, NJ: LEA).
Collins, G. S., Mughal, S., Barnett, A. H., Fitzgerald, J., Lloyd, C. E. (2011). Short report: education and psychological aspects modification and validation of the revised diabetes knowledge scale. Diabet. Med. 28, 306–310. doi: 10.1111/j.1464-5491.2010.03190.x
Cronbach, L. J. (1951). Coefficient alpha and the internal structure of tests. Psychometrika 16, 297–334. doi: 10.1007/BF02310555
Dunn, O. J., Clark, V. A. (1987). Applied statistics: analysis of variance and regression (New York: Wiley), 214–235.
Fawad, H., Maqsood, M., Abbas, A. (2014). The association between type-II diabetes mellitus and hypertension: a case report. Int. J. Allied. Med. Sci. Clin. Res. 2, 182–185.
Fitzgerald, J. T., Funnell, M. M., Anderson, R. M., Nwankwo, R., Stansfield, R. B., Piatt, G. A. (2016). Validation of the revised brief diabetes knowledge test (DKT2). Diabetes Educ. 42, 178–187. doi: 10.1177/0145721715624968
Hertzog, M. A. (2008). Considerations in determining sample size for pilot studies. Res. Nurs. Health 31, 180–191. doi: 10.1002/nur.20247
Hussain, M., Naqvi, S. B. S., Khan, M. A., Rizvi, M., Alam, S., Abbas, A., et al. (2014) Direct cost of treatment of diabetes mellitus type 2 in Pakistan. Int. J. Pharm. Pharm. Sci. 6, 261–264.
Institute for Health Metrics and Evaluation. GBD (2017). 2019. https://vizhub.healthdata.org/gbd-compare/.
Internation Diabetes Federation (IDF). MENA Members (2019). https://www.idf.org/our-network/regions-members/middle-east-and-north-africa/members/46-saudi-arabia.html.
Islam, A., Islam, N., Bharati, P., Aik, S., Hossain, G. (2016). Socio-economic and demographic factors influencing nutritional status among early childbearing young mothers in Bangladesh. BMC Womens Health 16, 58. doi: 10.1186/s12905-016-0338-y
Kardas, P., Lewek, P., Matyjaszczyk, M. (2013). Determinants of patient adherence: a review of systematic reviews. Front. Pharmacol. 4, 91. doi: 10.3389/fphar.2013.00091
Mashi, A. H., Aleid, D., Almutairi, S., Khattab, F., AlMuqawed, A. N., Khan, S., et al. (2019). The association of health literacy with glycemic control in Saudi patients with type 2 diabetes. Saudi. Med. J. 40, 675–680. doi: 10.15537/smj.2019.7.24277
Ministry of Health KSA. Diabetes at-a-glance (2014). Available from: https://www.moh.gov.sa/Ministry/Statistics/Documents/diabetes.pdf.
Naqvi, A. A., Hassali, M. A. (2019a). Limitations in contemporary self-reported medication adherence questionnaires: the concept and design of the General Medication Adherence Scale (GMAS) originating from a developing country. Curr. Med. Res. Opin. 35, 1–2. doi: 10.1080/03007995.2018.1526169
Naqvi, A. A., Hassali, M. A., Rizvi, M., Zehra, A., Iffat, W., Haseeb, A., et al. (2018b). Development and validation of a novel general medication adherence scale (GMAS) for chronic illness patients in Pakistan. Front. Pharmacol. 9, 1124. doi: 10.3389/fphar.2018.011
Naqvi, A. A., AlShayban, D. M., Ghori, S. A., Mahmoud, M. A., Haseeb, A., Faidah, H. S., et al. (2019b). Validation of the general medication adherence scale in saudi patients with chronic diseases. Front. Pharmacol. 10, 633. doi: 10.3389/fphar.2019.00633
Naqvi, A. A., Hassali, M. A., Jahangir, A., Nadir, M. N., Kachela, B. (2019c). Translation and validation of the English version of the general medication adherence scale (GMAS) in patients with chronic illnesses. J. Drug Assess. 8, 36–42. doi: 10.1080/21556660.2019.1579729
Naqvi, A. A., Hassali, M. A., Naqvi, S. B. S., Aftab, M. T., Zehra, F., Nadir, M. N., et al. (2019d). Assessment of patient satisfaction following pharmacist counselling session by a novel patient satisfaction feedback on counselling questionnaire. JPHSR 10, 243–254. doi: 10.1111/jphs.12294
Naqvi, A. A. (2016). Evolution of clinical pharmacy teaching practices in Pakistan. Arch. Pharma. Pract. 7, 26–27. doi: 10.4103/2045-080X.174939
Nazir, S. U. R., Hassali, M. A., Saleem, F., Bashir, S., Aljadhay, H. (2016). Disease related knowledge, medication adherence and glycaemic control among patients. Primary Care Diabetes 10, 136–141. doi: 10.1016/j.pcd.2015.09.004
Rabba, A. K., Aljiris, W. S., Ahmed, N. J., AlKkarfy, K. M. (2017). Medication adherence in type 2 diabetic patients: a study in Saudi Arabia. Int. J. Pharm. Pharm. Sci. 9, 247–250. doi: 10.22159/ijpps.2017v9i11.16963
Sami, W., Ansari, T., Butt, N. S., Ab Hamid, M. S. (2017). Effect of diet on type 2 diabetes mellitus: a review. Int. J. Health Sci. (Qassim) 11, 65–71.
Sampsize (2019). http://sampsize.sourceforge.net/iface/.
Shah, A., Naqvi, A. A., Ahmad, R. (2016) The need for providing pharmaceutical care in geriatrics: a case study of diagnostic errors leading to medication-related problems in a patient treatment plan. Arch. Pharma. Pract. 7, 87–94. doi: 10.4103/2045-080X.186173
Sherwani, S. I., Khan, H. A., Ekhzaimy, A., Masood, A., Sakharkar, M. K. (2016). Significance of HbA1c test in diagnosis and prognosis of diabetic patients. Biomarker Insights 11, 95–104. doi: 10.4137/BMI.S38440
World Health Organization (WHO) (2010). Diabetes. Available from: http://www.who.int/nmh/publications/fact_sheet_diabetes_en.pdf.
World Health Organization (WHO) (2016). Global Report on Diabetes. Available from: http://apps.who.int/iris/bitstream/handle/10665/204871/9789241565257_eng.pdf;jsessionid=918821FC88B9F4697792D707C49AE514?sequence=1.
Yeh, J. Z., Wei, C. J., Weng, S. F., Tsai, C. Y., Shih, J. H., Shih, C. L., et al. (2018). Disease-specific health literacy, disease knowledge, and adherence behavior among patients with type 2 diabetes in Taiwan. BMC Public Health 18, 1062. doi: 10.1186/s12889-018-5972-x
Zhang, Y., Hedo, R., Rivera, A., Rull, R., Richardson, S., Tu, X. M. (2019). Post hoc power analysis: is it an informative and meaningful analysis? BMJ 32, 4. doi: 10.1136/gpsych-2019-100069
Keywords: disease knowledge, medication adherence, patient compliance, concordance, diabetes mellitus, out-patients, Saudi Arabia
Citation: AlShayban DM, Naqvi AA, Alhumaid O, AlQahtani AS, Islam MA, Ghori SA, Haseeb A, Ali M, Iqbal MS, Elrggal ME, Ishaqui AA, Mahmoud MA, Khan I and Jamshed S (2020) Association of Disease Knowledge and Medication Adherence Among Out-Patients With Type 2 Diabetes Mellitus in Khobar, Saudi Arabia. Front. Pharmacol. 11:60. doi: 10.3389/fphar.2020.00060
Received: 12 October 2019; Accepted: 22 January 2020;
Published: 20 February 2020.
Edited by:
Maria Dimitrova, Medical University-Sofia, BulgariaReviewed by:
Anthony Kar Hsing Chan, Pfizer, IrelandTanja Mueller, University of Strathclyde, United Kingdom
Copyright © 2020 AlShayban, Naqvi, Alhumaid, AlQahtani, Islam, Ghori, Haseeb, Ali, Iqbal, Elrggal, Ishaqui, Mahmoud, Khan and Jamshed. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Atta Abbas Naqvi, bmFxdmlhdHRhYWJiYXNAZ21haWwuY29t
 Dhfer Mahdi AlShayban
Dhfer Mahdi AlShayban Atta Abbas Naqvi
Atta Abbas Naqvi Othman Alhumaid2
Othman Alhumaid2 Syed Azizullah Ghori
Syed Azizullah Ghori Abdul Haseeb
Abdul Haseeb Muhammad Shahid Iqbal
Muhammad Shahid Iqbal Mahmoud E. Elrggal
Mahmoud E. Elrggal Azfar Athar Ishaqui
Azfar Athar Ishaqui Mansour Adam Mahmoud
Mansour Adam Mahmoud Irfanullah Khan
Irfanullah Khan Shazia Jamshed
Shazia Jamshed