- 1Center for Infectious Diseases, Beijing Youan Hospital, Capital Medical University, Beijing, China
- 2Beijing Key Laboratory for HIV/AIDS Research, Beijing, China
- 3Institute of Psychology, Chinese Academy of Sciences, Beijing, China
- 4School of Public Health, Yale University, New Haven, CT, United States
Background: Posttraumatic stress disorder (PTSD) is a commonly reported and serious complication among people living with HIV (PLWH). PTSD may significantly increase unintentional non-adherence to antiretroviral therapy. In this systematic review and meta-analysis, we aimed to pool the observational studies exploring the association between PTSD and medication adherence among PLWH.
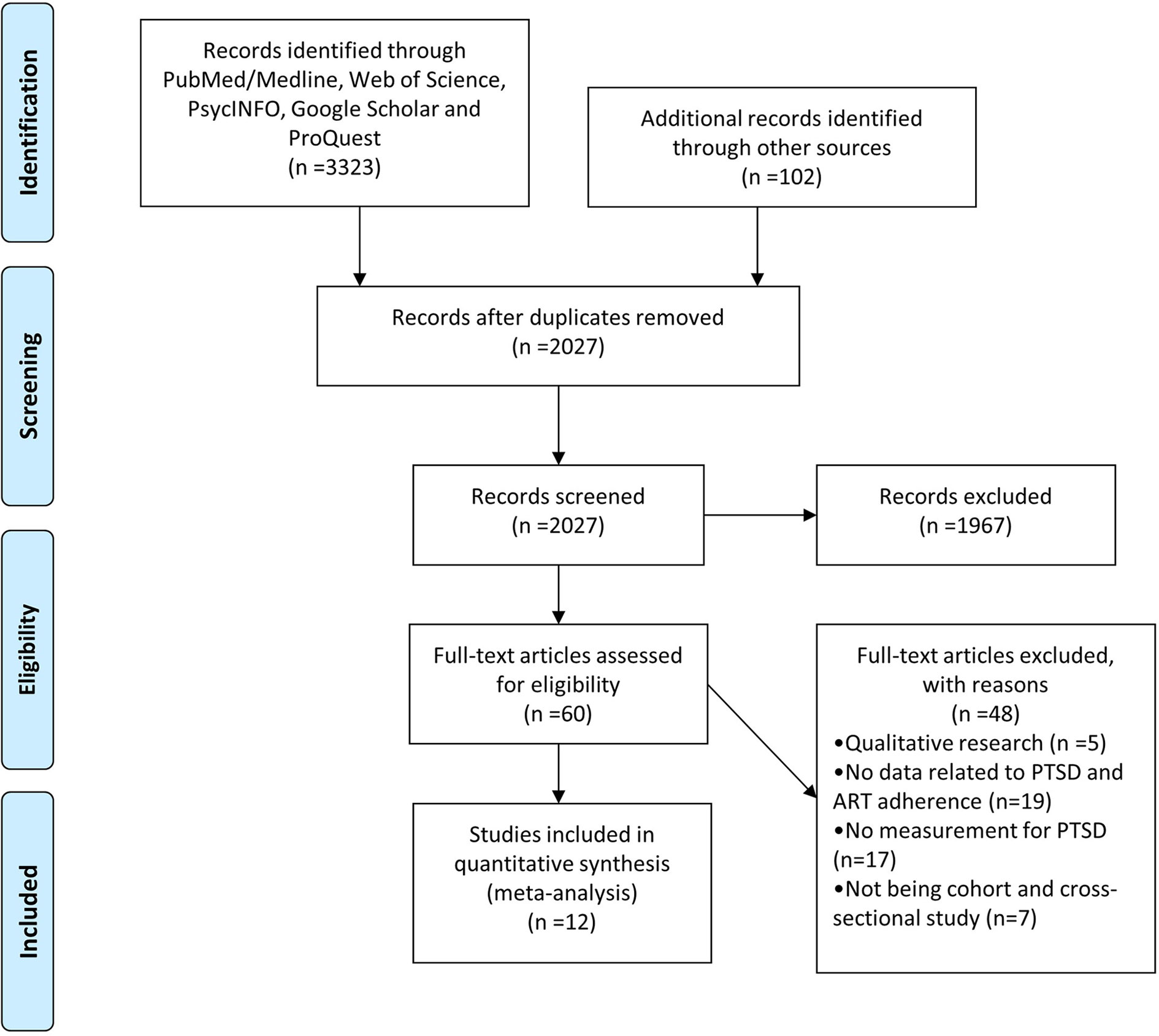
Methods: Comprehensive searches were conducted in PubMed/Medline, Web of Science, PsycINFO, Google Scholar, and ProQuest to identify relevant articles and dissertations. A random effects meta-analysis with inverse variance weighting was used to summarize the odds ratio (OR) across studies. Meta-regression and subgroup analyses were also carried out to assess the moderation effects for potential factors.
Results: By synthesizing 12 studies comprising 2489 participants, the pooled odd ratio of non-adherence to antiretroviral therapy was 1.19 (95% confidential interval (CI), 1.03–1.37, p = 0.02). No significant publication bias was detected by Egger’s test (Intercept = 0.842, p = 0.284). Factors moderating the association were mean age of participants, depression adjustment, and depression (all p < 0.05).
Conclusions: This meta-analysis supports that PTSD is related to adherence in PLWH. The hypothesized mechanisms (avoidant behavior and cognitive impairment) underlying this association need further investigation. Overall, this study highlights that clinicians should thoughtfully integrate timely mental health intervention into routine care.
Introduction
Compared with the general population, posttraumatic stress disorder (PTSD) is a commonly reported psychiatric disease among people living with HIV (PLWH) (1–4). The estimated prevalence of PTSD in PLWH was 28% worldwide, and PTSD is a frequent encountered psychiatric comorbidity in HIV primary care setting (5). PLWH with PTSD symptoms may be tremendously affected by unaffordable public health cost, disabling psychological distress, worsened quality of life, and even increased odds of suicide (6, 7). Moreover, an increasing amount of evidence suggests that PTSD like other commonly reported mental health disorders, may accelerate HIV disease progression characterized by significant CD4 decline (8, 9). Although the mechanism underlying PTSD and HIV disease progress remains far from understood, non-adherence to antiretroviral therapy (ART) may represent one such mechanism (9).
One previously published systematic review has summarized the impact of different mental health disorders including PTSD on ART non-adherence (10). No quantitative analysis was adopted in that review. As far as we know, no previous meta-analytic study has assessed the relationship between PTSD and ART adherence for PLWH. Moreover the mixed results of original articles also necessitate the quantitative analyses (9, 11–21). Such a quantitative method also enables us to clarify whether the association is moderated by different population- and study- based factors.
Previous studies exploring the association between PTSD and ART nonadherence adjusted several demographic and psychological confounders. A large number of studies reported that depression and substance were associated with lower level of ART adherence in PLWH (22–27). We thus hypothesized that depression and substance use might be added risk factors for PLWH with PTSD. Age, a commonly reported demographic confounder, is associated with cognitive impairment, especially the worsened prospective memory which is related to higher missing doses of medication among the participants with chronic disease (28–31). Gender disparity may also exist. Brown et al. (19) found significant gender disparity in the association between trauma experience and ART adherence (19). Thus we tried to figure out the moderator effects of the commonly reported confounders in previous original studies and interpret the potential mechanism.
In summary, we conducted a systematic review and meta-analysis to quantitatively pool the observational studies exploring the association between PTSD and ART adherence among PLWH. We hypothesized PLWH with PTSD would be more likely to be non-adherent to their ART. We also tried to figure out potential moderators that influence the association.
Methods
This meta-analysis complied with the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) checklist (32).
Search Strategy
Comprehensive searches were conducted in PubMed/Medline, Web of Science, PsycINFO, Google Scholar, and ProQuest to identify relevant articles and dissertations. The search terms included an intersection of PTSD- and participant- terms. PTSD terms included “Posttraumatic stress disorder,” “PTSD,” and “trauma.” Participant terms included “HIV,” “AIDS,” and “human immunodeficiency virus.” All searches were restricted to English articles and dissertations. Additional searches were conducted in the reference lists of included articles. The detailed information for searching process is attached in Supplementary Table 1.
Selection Criteria
Studies were considered as eligible if they met all of the following inclusion criteria:
P: people living with HIV;
I: not available;
C: PTSD vs no PTSD;
O: the association of PTSD and ART adherence (coefficient or odd ratio);
S: cohort or cross-sectional study
Study Selection and Data Coding
We used Endnote version 7 to assist the process of study selection. First, titles and abstracts were preliminarily screened to exclude irrelevant studies by JHH and TYJ. Second, full-text versions were assessed independently to ensure that all inclusion criteria were met by JHH and TYJ. Disagreement in the process of study selection was resolved by discussion with TZ. The two researchers used standardized Microsoft Excel spreadsheets to extract the following information: authors, year of publication, country of study, number of participants, study design, age, gender, education level, PTSD assessment, and adherence assessment.
Data Analyses
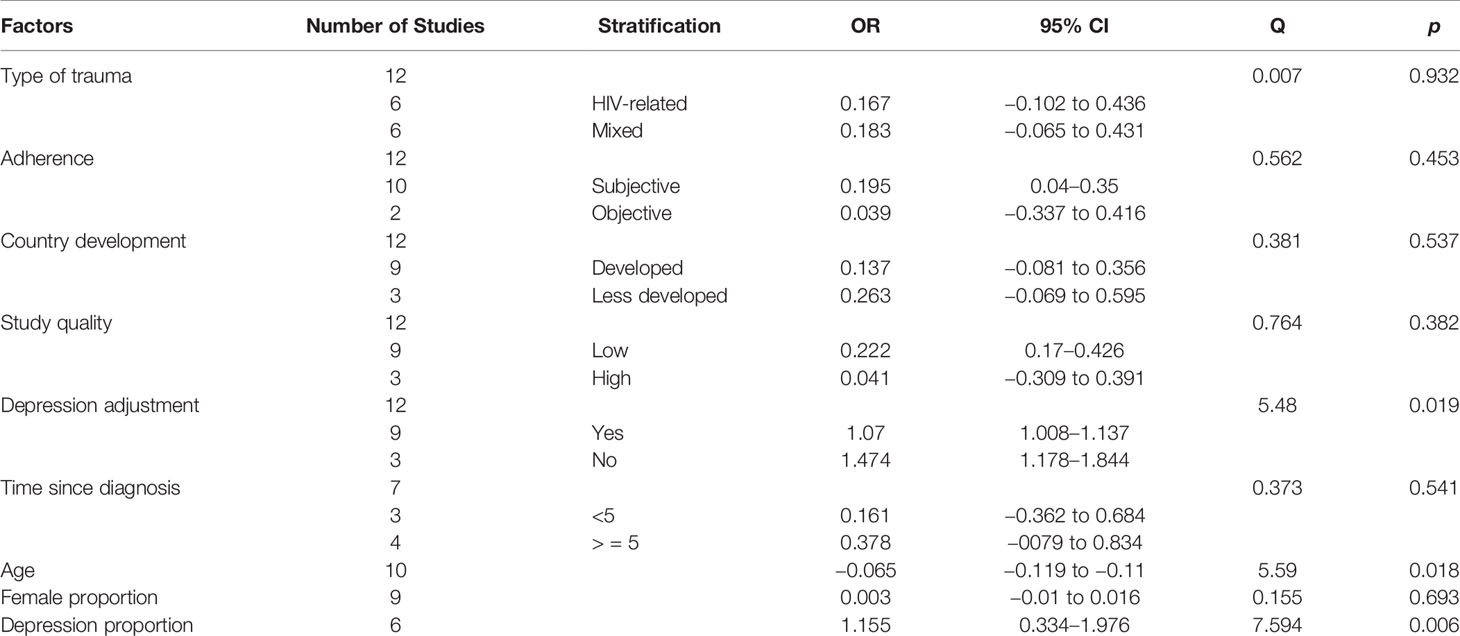
The primary outcome of interest was the association between PTSD and ART adherence among PLWH. Risk estimates were standardized to express odds ratios of non-adherence. A random effects meta-analysis with inverse variance weighting was used to summarize the odds ratio (OR) in CMA 2 (Comprehensive Meta-Analysis version 2, Biostat, Englewood, NJ). The extent and significance of between-study heterogeneity was assessed by I-square and Cochrane Q test, respectively (33). Egger’s linear regression test were used to assess the potential publication bias (34). For categorical moderators, sub-group analyses were adopted to compare different stratifications. The categorical moderators included type of trauma (HIV-related vs. mixed), adherence measurement (objective vs. subjective), study quality (low vs. high), years since HIV diagnosis (fewer than or equal to five years vs. more than five years) and depression adjustment (Yes vs. No). For continuous moderators, meta-regression analyses were used to explore linear association. The continuous moderators included age, female proportion, proportion of depression, and substance use. All analyses with p<0.05 were considered as statistical significance.
Quality Assessment
We used the Agency for Healthcare Research and Quality (AHRQ) checklist with a maximum score of 11 to assess the study quality for observational studies (35). Each item is worth one point. The original categorization for this checklist were 0–4 (high-risk), 5–8(moderate), and 9–11(low-risk). We used stricter criteria for study quality categorization in this meta-analysis. Studies were considered as low-risk if they scored more than 8 while other studies with a score lower than or equal to 8 were considered as high-risk. We also calculated the pooled results stratified by study quality to check the robustness of our results.
Results
Characteristic of Included Studies
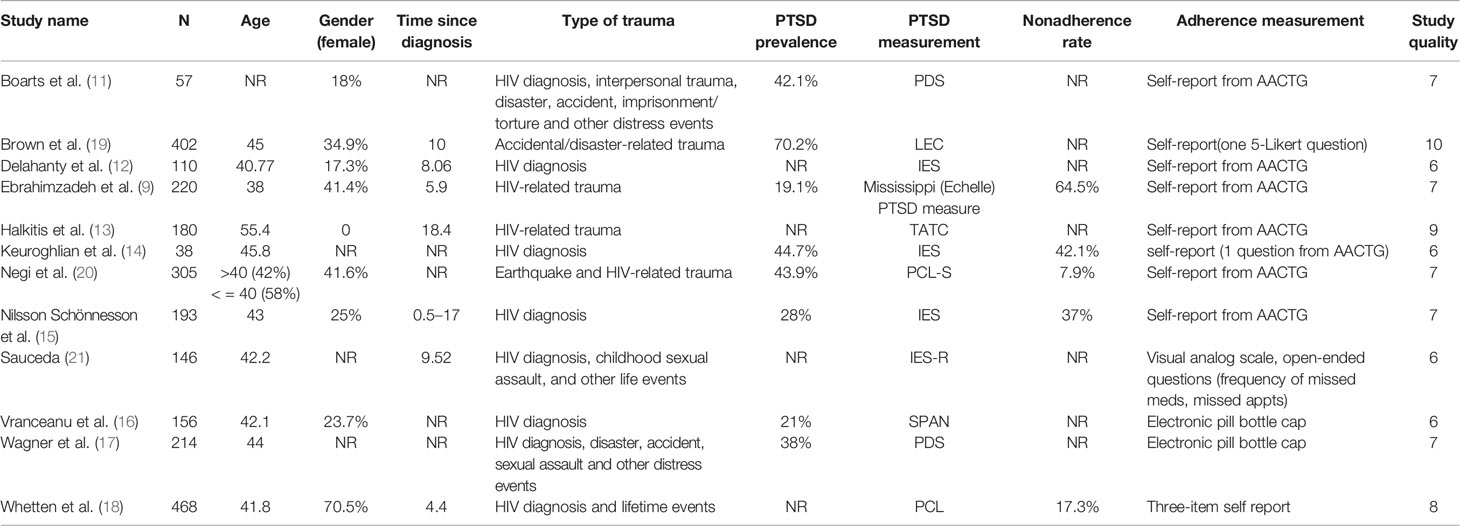
The comprehensive search yielded 3425 items (Figure 1). Twelve studies comprising 2489 participants met the inclusive criteria (Table 1). The mean age ranged from 38 to 55 (n = 10) and the female proportion ranged from 0 to 70.5% (n = 9). Three studies (3/12, 25%) were categorized as high-quality. The detailed information for quality assessment is shown in Supplementary Table 2.
Assessments of PTSD and ART Adherence
All studies adopted self-report scales. The self-report scales and questionnaires included Impact of Event Scale (IES) or its revised version (IES-R); the PTSD Checklist (PCL) or its Stressor Specific (PCL-S); the Trauma Awareness and Treatment Center (TATC) PTSD Scale; the Posttraumatic Diagnostic Scale (PDS); the Startle, Physiological arousal to reminders, Anger, and Numbness (SPAN) and Mississippi (Echelle) PTSD measure.
Ten studies (10/12, 83.3%) used self-report, and four articles (2/12, 16.7%) used various objective adherence measurement. Seven studies adopted Medication Adherence Questionnaire of AIDS Clinical Test Group (ACTG). Two studies adopted a three-item self-report questionnaire or a five-point Likert scale, respectively. Sauceda’s team systematically assessed the missing doses in past 7 days and past month, due medication doses, frequency of taking all scheduled doses for one month, ability to take all medicine in five questions. Two studies used the pill-counting method by the following formula: Medication adherence=number of pills actually used by the patient/number of pills that the patient should have used*100%.
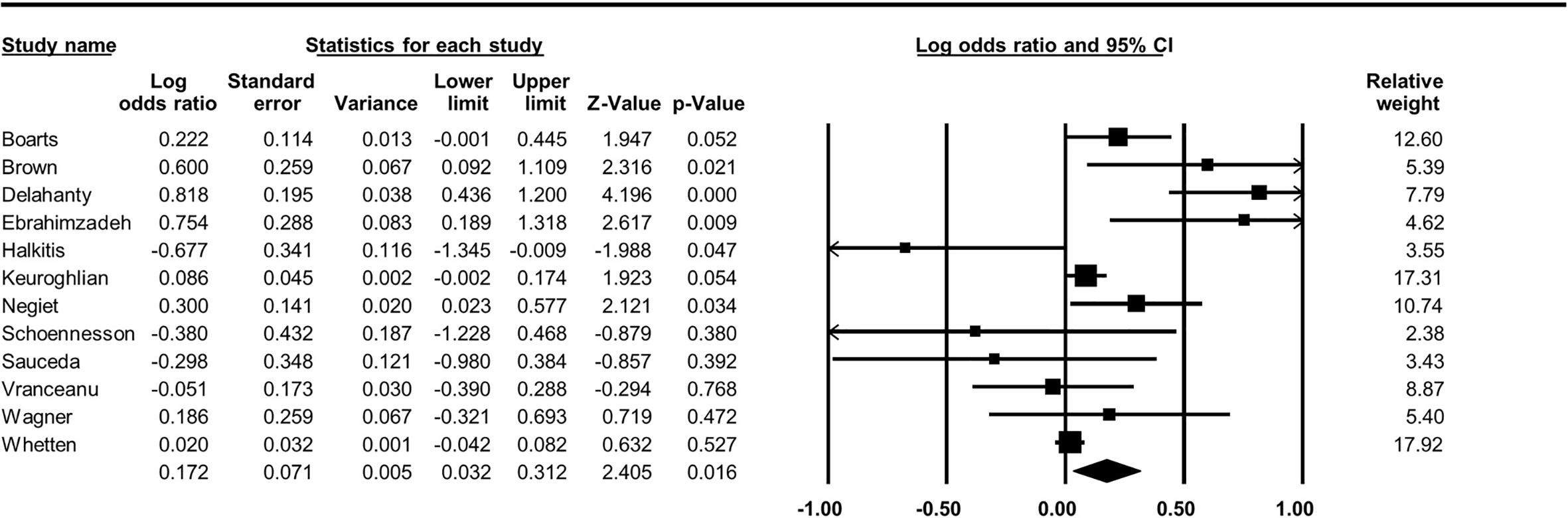
Overall Association Between PTSD and ART Adherence
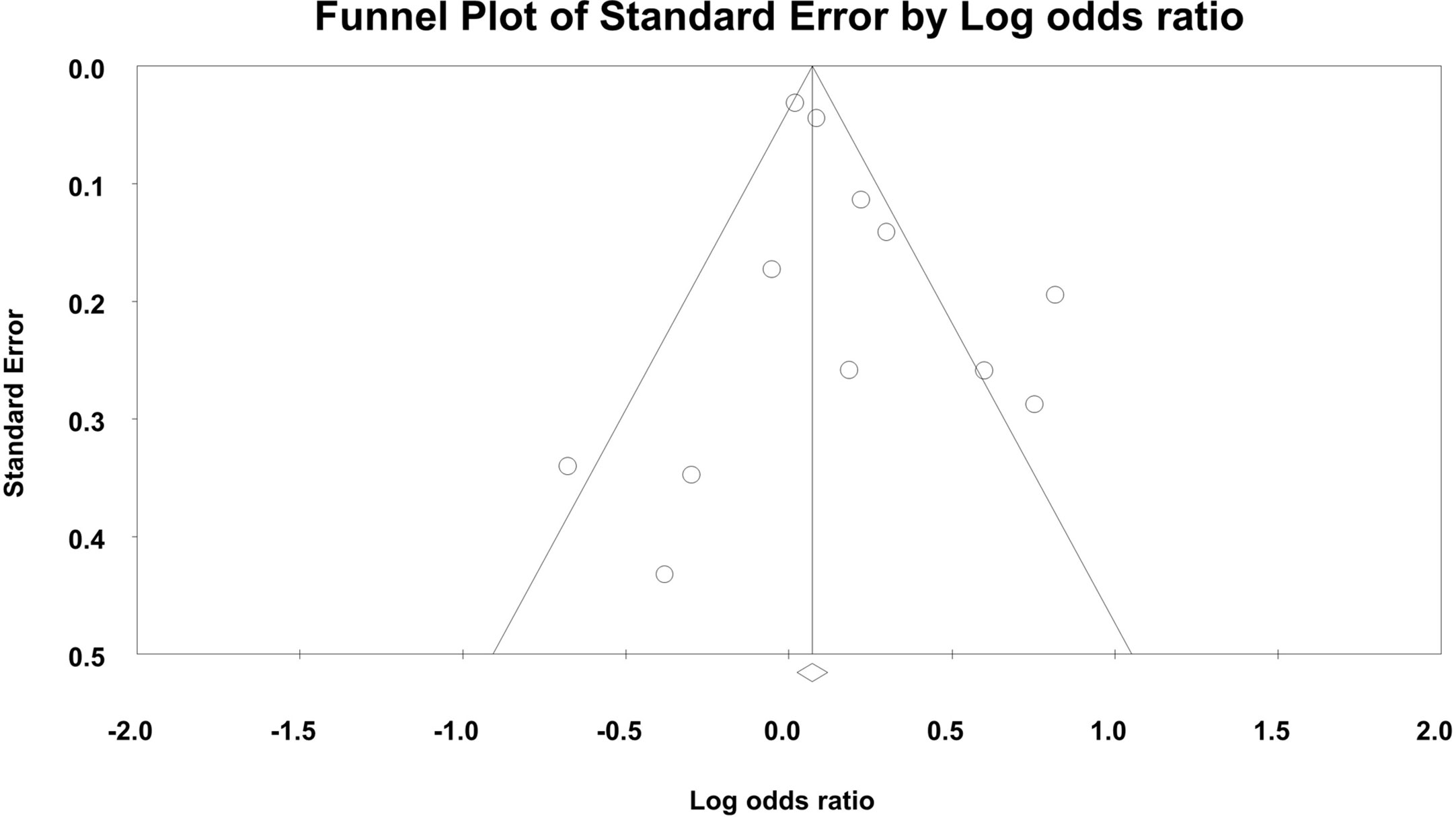
By synthesizing 12 studies, the pooled odds ratio was 1.19 (95% CI, 1.03–1.37, p = 0.02, Figure 2), indicating increased odds of non-adherence to ART for participants with PTSD. The between-study heterogeneity was significant and large (Q(11) = 39.29, I-square = 72.01, p<0.01). No significant asymmetry was detected by Egger’s test (Intercept = 0.842, p = 0.284, Figure 3).
Factors Related to the PTSD-Adherence Association
Mean age of participants was significantly related to the PTSD-adherence association (Q(1) = 5.59, p = 0.018), indicating that compared to younger participants, older PLWH was associated with lower odds of non-adherence for individuals with PTSD. Adjustment of depression status was also significantly related to PTSD-adherence association (Q(1) = 5.48, p = 0.019), indicating that compared to depression-unadjusted studies, PLWH was associated with lower odds of non-adherence for individuals with PTSD in depression-adjusted studies. The level of depression was associated with higher odds of non-adherence among participants with PTSD (Q(1) = 7.594, p = 0.006). Other factors did not significantly moderate this association. Only three studies reported substance use proportion, and we thus did not carry out moderator analysis for this variable (15–17). The detailed information for moderator analyses is shown in Table 2.
Discussion
As far as we know, this is the first systematic review and meta-analysis that explores the PTSD-ART adherence association among PLWH. The present meta-analysis of 12 studies found that there was elevated odds of ART non-adherence amongst HIV-infected participants with PTSD. Although the effect size for this association was small, from the perspective of public health, the result is still meaningful in making public health policy in terms of high prevalence (28%) of PTSD among PLWH worldwide (5). Moreover, there was a significant effect toward this association among younger participants and depression-unadjusted studies.
Underlying the relationship between PTSD and ART adherence in PLWH relates to cognitive impairments and PTSD symptoms. PLWH may already have potential impairment in multi-cognitive domains that have been linked to ART non-adherence (36). Specifically, PLWH is profoundly associated with prospective memory deficit which is a strong risk of concurrent problems ranging from medication non-adherence to employment (31). PTSD-caused cognitive decline may also lead to regular forgetting of medication in many chronic diseases (such as cardio-vascular diseases) (37, 38) and may further lead to treatment failure. Future prospective cohort studies are thus needed to verify the interaction of HIV and PTSD on non-adherence among PLWH and to explore the mediation effect of cognitive impairment in PTSD-adherence association.
Additionally, avoidance, a specific PTSD symptom, may lead to intentional non-adherence (39). HIV-related medication may remind participants may bring back memories of the traumatic life event, and re-experience illness belief and death fear (40, 41). In the other hand, PTSD may also lead to low trauma coping self-efficacy and self-control (42). Thus, PLWH with PTSD may skip the medication by avoidance of traumatic memories and a sense of futility.
As aforementioned, our moderator analyses also shed lights on roles of participants’ age and depression. Within this narrow age range in this meta-analysis (38–55.4), older participants may develop more systematic coping strategies to confront the traumatic events. Conversely, biological ageing process and HIV infection are associated with severe prospective memory deficit which may lead to medication nonadherence (31, 43). We are not sure whether the association pattern between PTSD and adherence is consistent throughout the whole life span. Future longitudinal studies should verify the association in different age groups. Depression significantly moderated the association, indicating depression may act as an added risk factor associated with non-adherence. A recent meta-analysis comprising nine studies demonstrated that PLWH with depression were 14% less likely (pooled odds ratio [OR], 0.86; 95% CI, 0.71–1.05) to use ART than those without depression (44). In the meanwhile, though there are not enough studies exploring other psycho-social factors in PTSD-adherence literatures, these factors (anxiety, stigma, and substance use) may also be related to ART adherence (27, 45–47). As a result of the complexity of the influential path, the association will require further clarification by structural equational modeling (SEM).
Several limitations should be mentioned. First, limited articles in potential moderators (for instance, anxiety and substance use) make it hard to draw conclusion on all related factors. In addition, the reported association in this study should also interpreted in cautious due to limited studies. Second, the interactive effects between all these factors necessitate more complicated mathematical modeling methods (such as SEM). Third, only ¼ articles were categorized as high quality, which may result in potential bias. Furthermore, there was a high between-study heterogeneity. However, no group difference was detected between high vs. low quality studies. Next, we cannot draw causal relationship from this meta-analysis and exclude potential confounding effects due to the cross-sectional nature of included studies. Future studies adopting randomized controlled trials are also needed to verify the causal relationship between PTSD and ART nonadherence. Furthermore, only studies in English were accepted. And the cutoff for the p-value was not corrected for multiple comparisons, which increases the risk of false positive.
Conclusion
In conclusion, this is the very first meta-analysis suggesting that PTSD is related to ART nonadherence among PLWH. The age of participants and depression adjustment our statistical models moderated this association. Some hypothesized mechanisms (avoidant behavior and cognitive impairment) underlying this association need further investigation. PTSD is one of the most commonly reported mental disorders among PLWH, so clinicians should thoughtfully integrate timely mental health intervention into routine care.
Data Availability Statement
The data supporting this meta-analysis are from previously reported studies and datasets, which have been cited. The processed data are available from the corresponding author Dr. Tong Zhang (enRfZG9jQGNjbXUuZWR1LmNu) upon request.
Author Contributions
JH conceptualized the study. JH and TJ searched the literature, selected studies, and extracted the data. JH and JF contributed to the analysis and interpretation of the data and provided important scientific input. JH analyzed the findings and wrote the first draft of the manuscript with input from BS. SM, and CG revised the first draft with concrete contribution. HW and TZ supervised the study. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Science and Technology Major Project: the National 13th Five-Year Grand Program on Key Infectious Disease Control (2017ZX10202102-005-003 to BS, 2018ZX10301-407-005 and 2018ZX10302103-001-003 to TJ, 2018ZX10715-005-002-002 to CG, and 2017ZX10202101-004-001 to TZ); the Beijing Municipal of Science and Technology Major Project (D161100000416003 to HW, and D161100000416005 to CG); and the Beijing Key Laboratory for HIV/AIDS Research (BZ0089). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.00834/full#supplementary-material
References
1. Verhey R, Gibson L, Brakarsh J, Chibanda D, Seedat S. Prevalence and correlates of probable post-traumatic stress disorder and common mental disorders in a population with a high prevalence of HIV in Zimbabwe. Eur J Psychotraumatol (2018) 9:9. doi: 10.1080/20008198.2018.1536286
2. Luo ST, Lin CQ, Ji GP, Li L. Post-traumatic Stress Disorder Symptoms Among People Living with HIV/AIDS in Rural China. AIDS Behav (2017) 21:3202–8. doi: 10.1007/s10461-016-1641-1
3. Devieux JG, Malow RM, Attonito JM, Jean-Gilles M, Rosenberg R, Gaston S, et al. Post-traumatic stress disorder symptomatology and alcohol use among HIV-seropositive adults in Haiti. AIDS Care-Psychol Socio-Med Asp Aids-Hiv (2013) 25:1210–8. doi: 10.1080/09540121.2013.763894
4. Sherr L, Nagra N, Kulubya G, Catalan J, Clucas C, Harding R. HIV infection associated post-traumatic stress disorder and post-traumatic growth - A systematic review. Psychol Health Med (2011) 16:612–29. doi: 10.1080/13548506.2011.579991
5. Tang C, Goldsamt L, Meng J, Xiao X, Zhang L, Williams AB, et al. Global estimate of the prevalence of post-traumatic stress disorder among adults living with HIV: a systematic review and meta-analysis. BMJ Open (2020) 10:e032435. doi: 10.1136/bmjopen-2019-032435
6. Gard TL, Hoover DR, Shi QH, Cohen MH, Mutimura E, Adedimeji AA, et al. The impact of HIV status, HIV disease progression, and post-traumatic stress symptoms on the health-related quality of life of Rwandan women genocide survivors. Qual Life Res (2013) 22:2073–84. doi: 10.1007/s11136-012-0328-y
7. Adewuya AO, Afolabi MO, Ola BA, Ogundele OA, Ajibare AO, Oladipo BF, et al. Post-traumatic stress disorder (PTSD) after stigma related events in HIV infected individuals in Nigeria. Soc Psychiatry Psychiatr Epidemiol (2009) 44:761–6. doi: 10.1007/s00127-009-0493-7
8. Reilly KH, Clark RA, Schmidt N, Benight CC, Kissinger P. The effect of post-traumatic stress disorder on HIV disease progression following hurricane Katrina. AIDS Care (2009) 21:1298–305. doi: 10.1080/09540120902732027
9. Ebrahimzadeh Z, Goodarzi MA, Joulaei H, et al. Predicting the Antiretroviral Medication Adherence and CD4 Measure in Patients with HIV/AIDS Based on the Post Traumatic Stress Disorder and Depression. Iranian J Public Health (2019) 48:139–46. doi: 10.18502/ijph.v48i1.802
10. Springer SA, Dushaj A, Azar MM. The impact of DSM-IV mental disorders on adherence to combination antiretroviral therapy among adult persons living with HIV/AIDS: a systematic review. AIDS Behav (2012) 16:2119–43. doi: 10.1007/s10461-012-0212-3
11. Boarts JM, Sledjeski EM, Bogart LM, Delahanty DL. The differential impact of PTSD and depression on HIV disease markers and adherence to HAART in people living with HIV. AIDS Behav (2006) 10:253–61. doi: 10.1007/s10461-006-9069-7
12. Delahanty DL, Bogart LM, Figler JL. Posttraumatic stress disorder symptoms, salivary cortisol, medication adherence, and CD4 levels in HIV-positive individuals. AIDS Care (2004) 16:247–60. doi: 10.1080/09540120410001641084
13. Halkitis PN, Perez-Figueroa RE, Carreiro T, Kingdon MJ, Kupprat SA, Eddy J. Psychosocial burdens negatively impact HIV antiretroviral adherence in gay, bisexual, and other men who have sex with men aged 50 and older. AIDS Care (2014) 26:1426–34. doi: 10.1080/09540121.2014.921276
14. Keuroghlian AS, Kamen CS, Neri E, Lee S, Liu R, Gore-Felton C. Trauma, dissociation, and antiretroviral adherence among persons living with HIV/AIDS. J Psychiatr Res (2011) 45:942–8. doi: 10.1016/j.jpsychires.2011.05.003
15. Nilsson Schonnesson L, Williams ML, Ross MW, Bratt G, Keel B. Factors associated with suboptimal antiretroviral therapy adherence to dose, schedule, and dietary instructions. AIDS Behav (2007) 11:175–83. doi: 10.1007/s10461-006-9160-0
16. Vranceanu AM, Safren SA, Lu M, Coady WM, Skolnik PR, Rogers WH, et al. The relationship of post-traumatic stress disorder and depression to antiretroviral medication adherence in persons with HIV. AIDS Patient Care STDS (2008) 22:313–21. doi: 10.1089/apc.2007.0069
17. Wagner GJ, Bogart LM, Galvan FH, Banks D, Klein DJ. Discrimination as a key mediator of the relationship between posttraumatic stress and HIV treatment adherence among African American men. J Behav Med (2012) 35:8–18. doi: 10.1007/s10865-011-9320-1
18. Whetten K, Shirey K, Pence BW, Yao J, Thielman N, Whetten R, et al. Trauma history and depression predict incomplete adherence to antiretroviral therapies in a low income country. PloS One (2013) 8:e74771. doi: 10.1371/journal.pone.0074771
19. Brown MJ, Harrison SE, Li X. Gender Disparities in Traumatic Life Experiences and Antiretroviral Therapy Adherence Among People Living with HIV in South Carolina. AIDS Behav (2019) 23:2904–15. doi: 10.1007/s10461-019-02440-9
20. Negi BS, Joshi SK, Nakazawa M, Kotaki T, Bastola A, Kameoka M, et al. Impact of a massive earthquake on adherence to antiretroviral therapy, mental health, and treatment failure among people living with HIV in Nepal. PloS One (2018) 13:e0198071. doi: 10.1371/journal.pone.0198071
21. Sauceda JA. A diathesis-stress approach to post-traumatic stress disorder symptoms associated with an HIV diagnosis: Implications for medication non-adherence. (Texas, United States: The University of Texas at El Paso) (2013). p. 195.
22. Cruess DG, Kalichman SC, Christine A, Connie S, Chauncey C, Kalichman MO. Benefits of Adherence to Psychotropic Medications on Depressive Symptoms and Antiretroviral Medication Adherence Among Men and Women Living with HIV/AIDS. Ann Behav Med A Publ Soc Behav Med (2011) 2:189–97. doi: 10.1007/s12160-011-9322-9
23. Jiang M, Yang J, Song, Zheng J, Li X, Guang. Social support, stigma, and the mediating roles of depression on self-reported medication adherence of HAART recipients in China. AIDS Care (2019) 31:942–50. doi: 10.1080/09540121.2019.1587360
24. M. Investigators. A Closer Look at Depression and Its Relationship to HIV Antiretroviral Adherence. Ann Behav Med (2011) 3:352–60. doi: 0.1007/s12160-011-9295-8
25. Mao Y, Qiao S, Li X, Zhao Q, Zhou Y, Shen Z. Depression, Social Support, and Adherence to Antiretroviral Therapy Among People Living With HIV in Guangxi, China: A Longitudinal Study. AIDS Educ Prev (2019) 31:38–50. doi: 10.1521/aeap.2019.31.1.38
26. Shim EJ, Hahm BJ, Lee SH, Kim NJ. The relationships among fear of disease progression, anxiety, depression and medication adherence in persons with HIV/AIDS. J Psychosomatic Res (2018) 109:135–. doi: 10.1016/j.jpsychores.2018.03.143
27. Carra G, Scioli R, Monti MC, Marinoni A. Severity profiles of substance-abusing patients in Italian community addiction facilities: influence of psychiatric concurrent disorders. Eur Addict Res (2006) 12:96–101. doi: 10.1159/000090429
28. Poquette AJ, Moore DJ, Gouaux B, Morgan EE, Woods SP. Prospective Memory and Antiretroviral Medication Non-Adherence in HIV: An Analysis of Ongoing Task Delay Length Using the Memory for Intentions Screening Test. J Int Neuropsychol Soc Jins (2012) 19:1–7. doi: 10.1017/S1355617712001051
29. Weber E, Morgan EE, Rooney AS, Grant I, Woods SP, T.H.N.R.P.H. Group. Longer ongoing task delay intervals exacerbate prospective memory deficits in HIV-associated neurocognitive disorders (HAND). J Clin Exp Neuropsychol (2012) 34:416–27. doi: 10.1080/13803395.2012.654764
30. Casaletto KB, Doyle K, Weber E, Woods SP. Self-predictions of prospective memory in HIV-associated neurocognitive disorders: evidence of a metamemory deficit. Arch Clin Neuropsychol Off J Natl Acad Neuropsychol (2014). 29:818–27. doi: 10.1093/arclin/acu061
31. Avci G, Sheppard DP, Tierney SM, Kordovski VM, Sullivan KL, Woods SP. A systematic review of prospective memory in HIV disease: from the laboratory to daily life. Clin Neuropsychol (2018) 32:858–90. doi: 10.1080/13854046.2017.1373860
32. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. Jama (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
33. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med (2002) 21:1539–58. doi: 10.1002/sim.1186
34. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clin Res ed) (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
35. Bindman AB. The Agency for Healthcare Research and Quality and the Development of a Learning Health Care System. JAMA Internal Med (2017) 177:909–10. doi: 10.1001/jamainternmed.2017.2589
36. Awori V, Mativo P, Yonga G, Shah R. The association between asymptomatic and mild neurocognitive impairment and adherence to antiretroviral therapy among people living with human immunodeficiency virus. South Afr J HIV Med (2018) 19:674. doi: 10.4102/sajhivmed.v19i1.674
37. Edmondson D. An Enduring Somatic Threat Model of Posttraumatic Stress Disorder Due to Acute Life-Threatening Medical Events. Soc Pers Psychol Compass (2014) 8:118–34. doi: 10.1111/spc3.12089
38. Favaro A, Gerosa G, Caforio AL, Volpe B, Rupolo G, Zarneri D, et al. Posttraumatic stress disorder and depression in heart transplantation recipients: the relationship with outcome and adherence to medical treatment. Gen Hosp Psychiatry (2011) 33:1–7. doi: 10.1016/j.genhosppsych.2010.10.001
39. Shemesh E, Yehuda R, Milo O, Dinur I, Rudnick A, Vered Z, et al. Posttraumatic stress, nonadherence, and adverse outcome in survivors of a myocardial infarction. Psychosomatic Med (2004) 66:521–6. doi: 10.1097/01.psy.0000126199.05189.86
40. Stafford L, Jackson HJ, Berk M. Illness beliefs about heart disease and adherence to secondary prevention regimens. Psychosomatic Med (2008) 70:942–8. doi: 10.1097/PSY.0b013e318187e22e
41. Psarros C, Theleritis C, Economou M, Tzavara C, Kioulos KT, Mantonakis L, et al. Insomnia and PTSD one month after wildfires: evidence for an independent role of the “fear of imminent death”. Int J Psychiatry Clin Pract (2017) 21:137–41. doi: 10.1080/13651501.2016.1276192
42. Samuelson KW, Bartel A, Valadez R, Jordan JT. PTSD symptoms and perception of cognitive problems: The roles of posttraumatic cognitions and trauma coping self-efficacy. psychol Trauma Theory Res Pract Policy (2017) 9:537–44. doi: 10.1037/tra0000210
43. Lee SD, Ong B, Pike KE, Kinsella GJ. Prospective memory and subjective memory decline: A neuropsychological indicator of memory difficulties in community-dwelling older people. J Clin Exp Neuropsychol (2018) 40:183–97. doi: 10.1080/13803395.2017.1326465
44. Tao J, Vermund SH, Qian HZ. Association Between Depression and Antiretroviral Therapy Use Among People Living with HIV: A Meta-analysis. AIDS Behav (2018) 22:1542–50. doi: 10.1007/s10461-017-1776-8
45. Rueda S, Mitra S, Chen S, Gogolishvili D, Globerman J, Chambers L, et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: a series of meta-analyses. BMJ Open (2016) 6:e011453. doi: 10.1136/bmjopen-2016-011453
46. Wykowski J, Kemp CG, Velloza J, Rao D, Drain PK. Associations Between Anxiety and Adherence to Antiretroviral Medications in Low- and Middle-Income Countries: A Systematic Review and Meta-analysis. AIDS Behav (2019) 23:2059–71. doi: 10.1007/s10461-018-02390-8
47. Carra G, Crocamo C, Borrelli P, Popa I, Ornaghi A, Montomoli C, et al. Correlates of dependence and treatment for substance use among people with comorbid severe mental and substance use disorders: findings from the “Psychiatric and Addictive Dual Disorder in Italy (PADDI)” Study. Compr Psychiatry (2015) 58:152–9. doi: 10.1016/j.comppsych.2014.11.021
Keywords: posttraumatic stress disorder, people living with HIV, meta-analysis, antiretroviral therapy adherence, systematic review
Citation: Hou J, Fu J, Meng S, Jiang T, Guo C, Wu H, Su B and Zhang T (2020) Posttraumatic Stress Disorder and Nonadherence to Treatment in People Living With HIV: A Systematic Review and Meta-analysis. Front. Psychiatry 11:834. doi: 10.3389/fpsyt.2020.00834
Received: 23 February 2020; Accepted: 31 July 2020;
Published: 19 August 2020.
Edited by:
Leandro Da Costa Lane Valiengo, University of São Paulo, BrazilReviewed by:
Lucas Borrione, Fundação Faculdade de Medicina, BrazilGiuseppe Carrà, University of Milano-Bicocca, Italy
Copyright © 2020 Hou, Fu, Meng, Jiang, Guo, Wu, Su and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tong Zhang, enRfZG9jQGNjbXUuZWR1LmNu
 Jianhua Hou
Jianhua Hou Jiangning Fu
Jiangning Fu Siyan Meng4
Siyan Meng4 Hao Wu
Hao Wu Bin Su
Bin Su Tong Zhang
Tong Zhang