- 1Department of Pharmacy, Fuda Cancer Hospital, Guangzhou, Guangdong, China
- 2Department of Pharmacy, Ganzhou People’s Hospital, Ganzhou, China
Introduction: Minocycline can induce a rare but serious adverse drug reaction known as drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome. We explored the clinical features of minocycline-associated DRESS to aid in early diagnosis and risk mitigation.
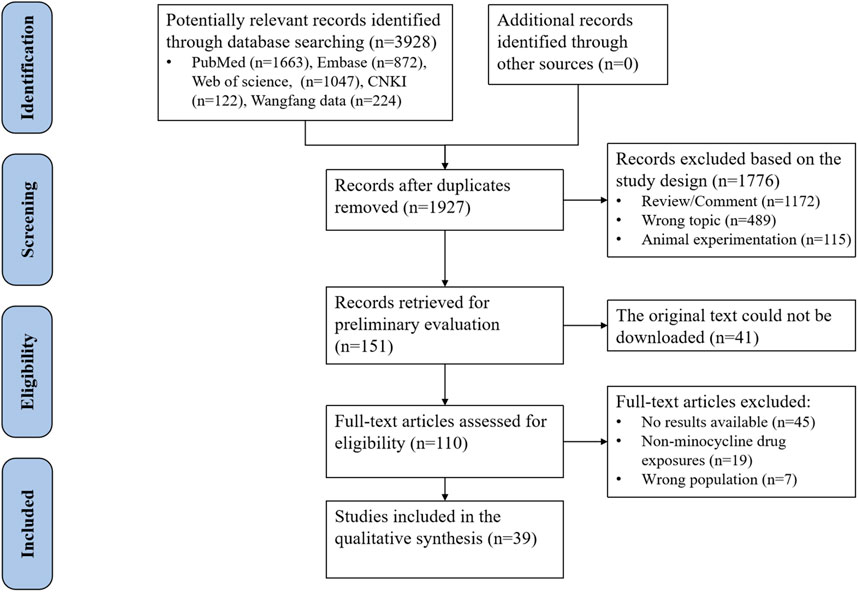
Methods: A comprehensive exploration of published cases from the start of electronic databases (PubMed, Embase, Web of Science, CNKI, Wanfang Data) to December 1, 2024. Cases were screened using RegiSCAR criteria.
Results: A total of 3,928 citations were identified through database searches, and after screening, 39 case reports (comprising 57 patients) were included. Fifty-seven patients (mean age 37.1 years) exhibited median DRESS onset at 17.5 days. Respiratory symptoms (87.7%, n = 50) dominated, including non-productive cough, dyspnea, pharyngitis, and wheezing. Fever occurred in 45 (78.9%) patients. Median eosinophilia peaked at 4.09 × 109/L. Symptom improvement median time was 10.5 days. Overall, forty-five patients (93.8% of 48 with outcome data) recovered post-minocycline discontinuation. Four deaths occurred (hepatic failure, refractory hypotension, unknown causes).
Conclusion: Minocycline-associated DRESS syndrome is characterized by diverse clinical manifestations, including prominent respiratory symptoms. Timely drug cessation, corticosteroid therapy, and vigilant monitoring are critical to optimize outcomes. These findings underscore the need for enhanced pharmacovigilance in high-risk populations.
Introduction
Minocycline is a semi-synthetic tetracycline antimicrobial drug that binds to the A position of the bacterial ribosome 30S subunit, preventing the elongation of the peptide chain and inhibiting the protein synthesis of bacteria or other pathogenic microorganisms, thereby exerting an antibacterial or bactericidal effect (Allen, 1976; Hellmann-Regen et al., 2022). The antibacterial spectrum of minocycline is similar to that of tetracycline, and it is effective against Gram-positive bacteria (including Staphylococcus aureus, Streptococcus, and Pneumococcus), Gram-negative bacteria (including Neisseria gonorrhoeae, Shigella dysenteriae, Escherichia coli, Klebsiella), Treponema pallidum, Chlamydia trachomatis, and Ureaplasma urealyticum (Asadi et al., 2020; Yang et al., 2022; Wu et al., 2021; Mojica et al., 2023). While in vitro activity has been reported against Proteus and Pseudomonas aeruginosa, minocycline is not considered clinically effective for infections caused by these organisms. Recent evidence highlights its classification as an antimicrobial agent implicated in antimicrobial-associated DRESS syndrome, particularly through mechanisms involving drug metabolism and immune dysregulation (Sharifzadeh et al., 2021). Data collected from the regulatory approval of minocycline showed that minocycline was generally well tolerated, with the most common adverse events including gastrointestinal symptoms (e.g., abdominal pain, nausea, anorexia, and gastrointestinal disorders) and dizziness (Chow et al., 1975; Martins et al., 2021; Garner et al., 2000). Twenty-nine previous randomized controlled trials (RCTs) reported adverse events attributed to minocycline treatment: 332 of 1906 treated participants (17.4%) experienced one or more adverse events (Garner et al., 2000). Systemic use of minocycline is associated with some serious autoimmune adverse events, including shock and allergic reactions, worsening of systemic lupus erythematosus-like symptoms, nodular arteritis, autoimmune hepatitis, toxic epidermal necrolysis, idiopathic intracranial hypertension, and eosinophilia and systemic symptoms (DRESS) syndrome (Hung and Chung, 2022; Dominic, 2021; Elkayam et al., 1999). Recent studies highlight that systemic use of minocycline is associated with severe hypersensitivity reactions, including DRESS syndrome, which manifests not only as cutaneous eruptions but also profound visceral organ involvement. Pulmonary manifestations (e.g., interstitial pneumonia, pleural effusion, and acute respiratory distress syndrome) occur in up to 50% of cases (Chen et al., 2013), while renal impairment (e.g., acute tubular necrosis, interstitial nephritis) has been reported in 20%–30% of patients (Mori et al., 2019). Cardiac involvement, though less frequent, includes myocarditis and pericardial effusion, contributing to increased mortality risk (Kardaun et al., 2013).
DRESS is a rare but serious adverse event. Rash is commonly observed in DRESS and can progress to involve most parts of the body. It may be associated with systemic involvement of major organs such as the liver or kidneys, leading to elevated liver enzymes, renal dysfunction, and other inflammatory manifestations. Hepatic involvement, manifested by hepatitis, cholestasis, or even fulminant liver failure, represents one of the most frequent and potentially severe organ manifestations. Severe cases may lead to death (Krantz and Phillips, 2023; Hama et al., 2022). Existing studies have shown that DRESS is typically drug-induced, with common causative agents including anti-epileptic drugs (such as lamotrigine, phenytoin, carbamazepine) and antimicrobial drugs (such as vancomycin, trimethoprim-sulfamethoxazole). Studies have shown that minocycline is associated with DRESS (Cardones, 2020; Shiohara and Mizukawa, 2019; Wei et al., 2024), but most of the research on eosinophilia and DRESS is based on case reports, and there is limited understanding of its clinical features and prognosis (Kardaun et al., 2013; Brüggen et al., 2024). The purpose of this study is to explore the clinical characteristics of minocycline-related DRESS. By identifying early diagnostic indicators and understanding the typical progression of the syndrome, clinicians can more promptly recognize and manage DRESS.
Methods
Ethical approval and patient consent statements
The study did not require approval from the institutional ethics committee because it was a retrospective analysis of case reports published in a public database and did not involve sensitive personal information.
Search strategy
Both international (PubMed, Embase, Web of Science) and Chinese (China National Knowledge Infrastructure, Wanfang data) databases were searched independently from their inception to 1 December 2024 with no restriction on the search language. We identified the literature regarding minocycline-induced DRESS via the search terms ‘minocycline’ AND ‘eosinophilia’ OR ‘systemic symptoms syndrome’ OR ‘Hypersensitivity’ OR ‘DRESS’. Additional sources, including reference lists of included studies and conference proceedings, were manually reviewed.
Inclusion and exclusion criteria
Case reports and case analysis of patients with eosinophilia and systemic symptoms syndrome induced by minocycline were included as a preliminary study. Reviews, animal experimentation, mechanism studies, preclinical studies, repeated cases, and studies with insufficient data, non-minocycline drug exposures, or the wrong population were excluded.
Diagnostic criteria for DRESS
The most widely used diagnostic criteria of DRESS are contained in the Registry of Severe Cutaneous Adverse Reactions (RegiSCAR) scoring system (Kardaun et al., 2007; Calle et al., 2023), based on the following key clinical manifestations: (1) Fever with a core temperature >101.3°F (38.5°C), or an axillary temperature >100.4°F (38°C), (2) Enlarged lymph nodes in at least 2 different body sites, (3) Patients with eosinophilia and heterogeneous lymphocytes. Heterogeneous lymphocytes refer to a mixed population of lymphocyte subsets (including reactive/atypical forms), as defined by RegiSCAR criteria. (4) Skin involvement (extent of rash, whether suggestive of DRESS, biopsy), (5) Organ damage, e.g., elevated liver enzymes defined as either: Alanine transaminase (ALT) or conjugated bilirubin at least two-fold over the upper normal limit on at least two separate dates, or Aspartate transaminase (AST), total bilirubin, and alkaline phosphatase (AP) all at least two-fold over the upper normal limit at least once (Kardaun et al., 2014), (6) Duration of illness >15 days. Each clinical manifestation was scored from −1 to 2 points based on severity, with total scores categorizing diagnostic certainty as negative case (<2 points), possible case (2-3 points), probable case (4-5 points), or definitive case (>5 points). To ensure diagnostic consistency, two independent reviewers applied the RegiSCAR criteria to all included cases. Discrepancies were resolved via consensus or referral to a senior dermatologist with expertise in hypersensitivity reactions. Studies reporting incomplete diagnostic data were excluded.
Data extraction
Based on inclusion and exclusion criteria, studies were selected independently according to the diagnostic criteria by two researchers. Disagreements were resolved through consensus or referral to a senior researcher when needed. A specially designed data extraction table was used to extract the following information of the patients: nationality, sex, age, primary disease, primary indications, time of symptom onset, clinical symptoms, laboratory investigation, imaging examination, therapy, time of symptom improvement, clinical outcome, hospitalization days, and follow-up time.
Statistical analysis
Statistical analyses were processed using IBM SPSS Statistics for Windows, Version 26.0. For continuous variables, if they conformed to a normal distribution, the variables were presented as means ± standard deviation (SD), otherwise, they were presented in the form of median and interquartile ranges (IQR). Categorical variables were reported in the form of counts and percentages.
Results
Demographic information
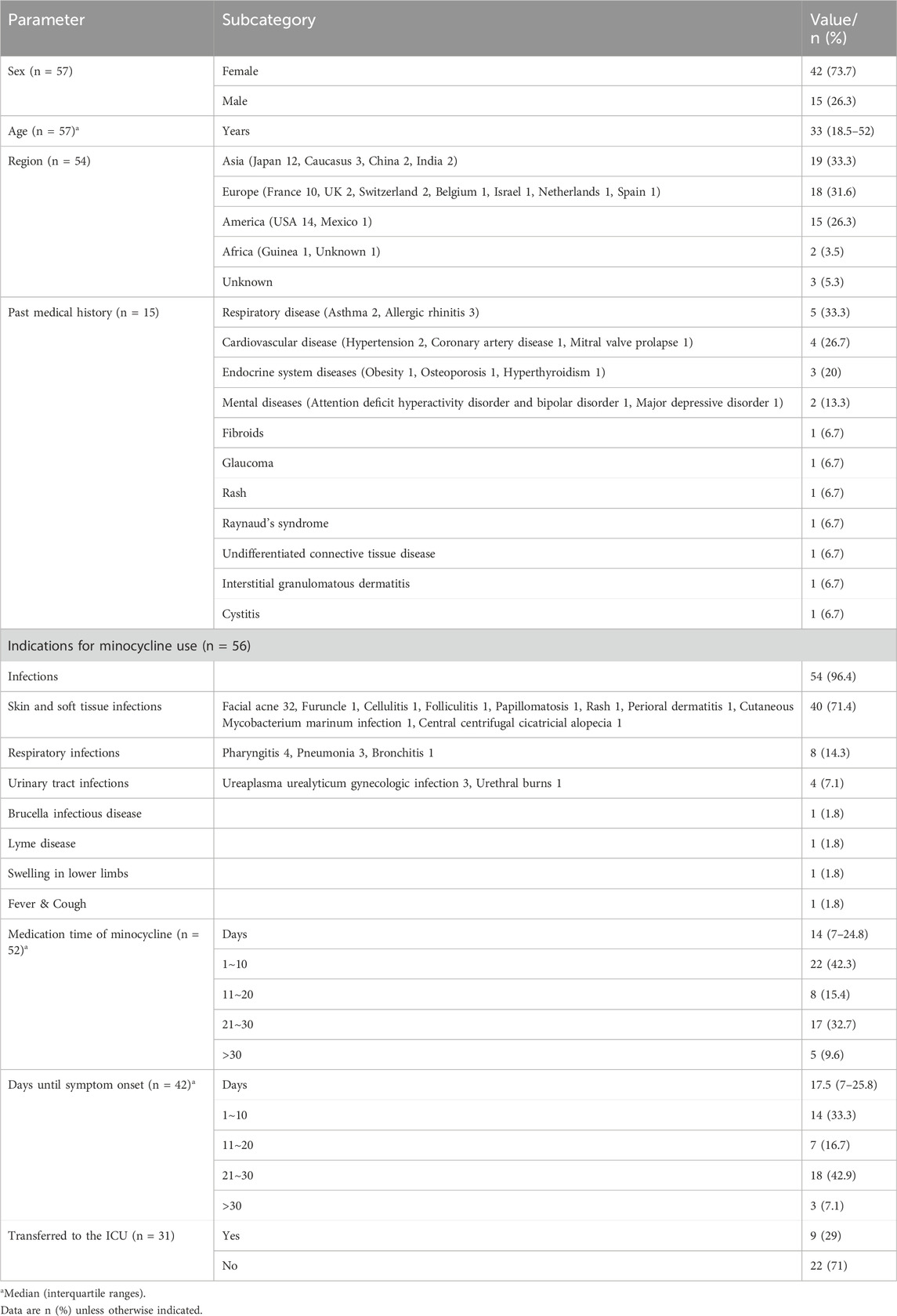
In total, 3,928 citations were identified through a database search. After duplicate records and records that were not meeting the eligibility criteria were removed, a total of 39 case reports (comprising 57 patients), with a median age of 33 years, were included (Figure 1). Supplementary Table S1 systematically summarizes the clinical and diagnostic findings of the included DRESS cases, aligned with the RegiSCAR criteria. Table 1 shows detailed characteristics of the included individuals. The patients were mainly from Asia (19 cases, 33%), Europe (18 cases, 31.6%), America (15 cases, 26.3%), and Africa (two cases, 3.5%). Minocycline was mainly used to treat skin and soft tissue infections (40 cases, 71.4%) and respiratory infections (eight cases, 14.3%). Daily doses of minocycline ranged from 100 to 250 mg/day. The median medication time was 14 days (range, 7–24.8). The median days until symptom onset was 17.5 days (range, 7–25.8). Nine patients (29%) were transferred to the ICU. In the past medical history, 33.3% of 15 patients had respiratory disease. 26.7% of 15 patients had cardiovascular disease.
Clinical manifestations of drug reactions
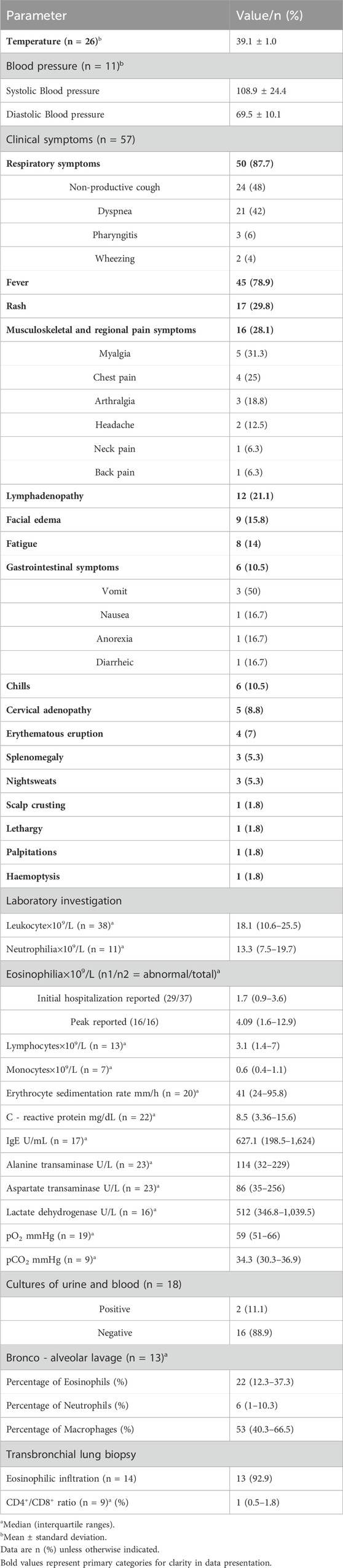
The clinical manifestations are summarized in Table 2. Vital signs included a mean temperature of 39.1°C in 26 patients. Symptoms (50 cases, 87.7%) included non-productive cough, dyspnea, pharyngitis, and wheezing were prevalent. Forty-five (78.9%) patients had the symptom of fever, and rash was observed in 17 patients (29.8%). Musculoskeletal and regional pain symptoms were reported in 16 patients (28.1%), including myalgia (31.3%), chest pain (25%), arthralgia (18.8%), headache (12.5%), neck pain (6.3%), and back pain (6.3%). Lymphadenopathy was present in 12 patients (21.1%), with cervical adenopathy specifically noted in five patients (8.8%). Fatigue was reported in eight patients (14%), and gastrointestinal symptoms (vomiting, nausea, anorexia, diarrhea) were observed in six patients (10.5%). In terms of organ-specific involvement, we counted 23 patients with hepatic involvement and 6 patients with gastrointestinal involvement based on clinical symptoms and laboratory investigation results. To highlight the distinct clinical patterns of minocycline-induced DRESS, we compared its features with those of DRESS caused by anticonvulsants, sulfonamides, and allopurinol (Supplementary Table S2).
Laboratory investigation
The laboratory test results are summarized in Table 2. Leukocytes were elevated in 38 (66.7%) of 57 patients, with a median value of 18.1*109/L (range, 10.6–25.5). Neutrophilia occurred in 11 patients, with a median value of 13.3*109/L (range, 7.5–19.7). Thirty-seven patients reported eosinophil results on the first day of admission, with a median value of 1.7*109/L (range 0.9–3.6). Eosinophilia (>0.7*109/L) was present in 78.4% (29/37) of patients at admission. The 16 patients who reported peak eosinophils during hospitalisation all had abnormal values with a median of 4.09*109/L (range 1.6–12.9). Lymphocyte values ranged from 1.4 to 7 *109/L, with a median of 3.1*109/L. Seven patients reported monocytes value with a median value of 0.6*109/L (range, 0.4–1.1). Urine and blood cultures were provided by 18 patients to rule out concurrent infections, particularly in febrile patients. Positive cultures were identified in 2 cases (11.1%). These results guided adjunctive antimicrobial therapy but did not alter the primary diagnosis of DRESS, which was confirmed by RegiSCAR criteria and histopathology. The erythrocyte sedimentation rate (ESR) was elevated in 20 patients (35.1%), with a median value of 41 mm/h (range, 24–95.8). The median C-reactive protein level was 8.5 mg/dL (range, 3.36–15.6). IgE was reported in 17 patients, with a median value of 627.1U/mL (range, 198.5–1,624). Twenty-three patients provided alanine transaminase and aspartate transaminase, with a median value of 114U/L (range, 32–229) and 86U/L (range, 35–256), respectively. Lactate dehydrogenase was elevated in 16 patients (28.1%), with a median value of 512U/L (range, 346.8–1,039.5). The broncho-alveolar lavage results from 13 patients showed that the percentage of eosinophils was 22% (interquartile range 12.3%–37.3%), the percentage of neutrophils was 6% (interquartile range 1%–10.3%), and the percentage of macrophages was 53% (interquartile range 40.3%–66.5%). Additionally, transbronchial lung biopsy results from 14 patients revealed eosinophilic infiltration in 13 cases (92.9%). These findings highlight a significant presence of eosinophils in both broncho-alveolar lavage fluid and lung tissue, indicating a potential eosinophilic inflammatory process in the included patients.
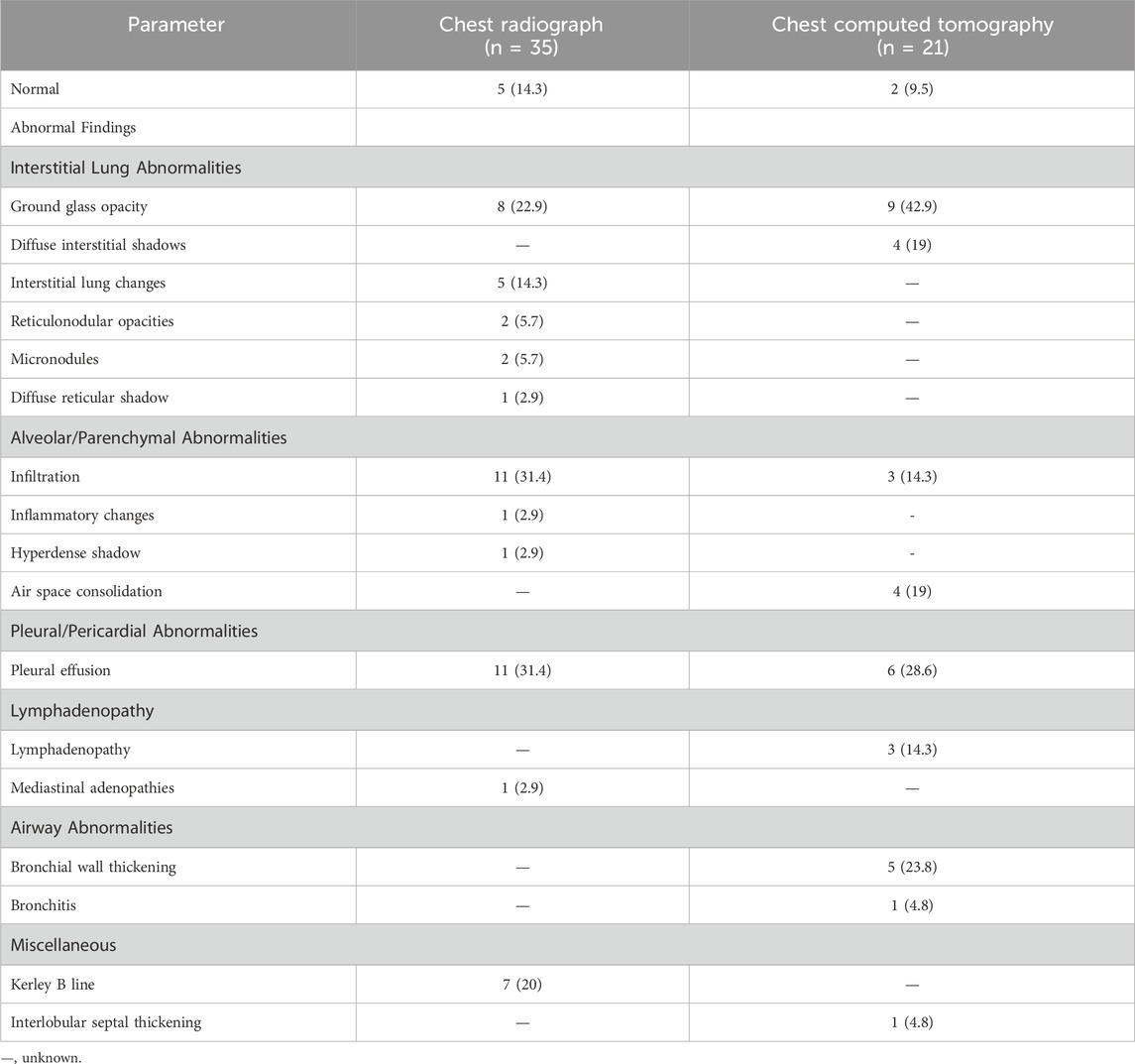
Imaging examination
The imaging examination results are summarized in Table 3. The imaging examination results of the 57 included patients showed that among chest radiograph findings (n = 35), 14.3% were normal, while abnormal findings included interstitial lung changes (14.3%), ground glass opacity (22.9%), pleural effusion (31.4%), reticulonodular opacities (5.7%), micronodules (5.7%), diffuse reticular shadow (2.9%), infiltration (31.4%), inflammatory changes (2.9%), hyperdense shadow (2.9%), and mediastinal adenopathies (2.9%). Among chest computed tomography findings (n = 21), 9.5% were normal, while abnormal findings included ground glass opacity (42.9%), diffuse interstitial shadows (19%), air space consolidation (19%), pleural effusion (28.6%), lymphadenopathy (14.3%), bronchial wall thickening (23.8%), bronchitis (4.8%), and interlobular septal thickening (4.8%).
Treatment and outcomes
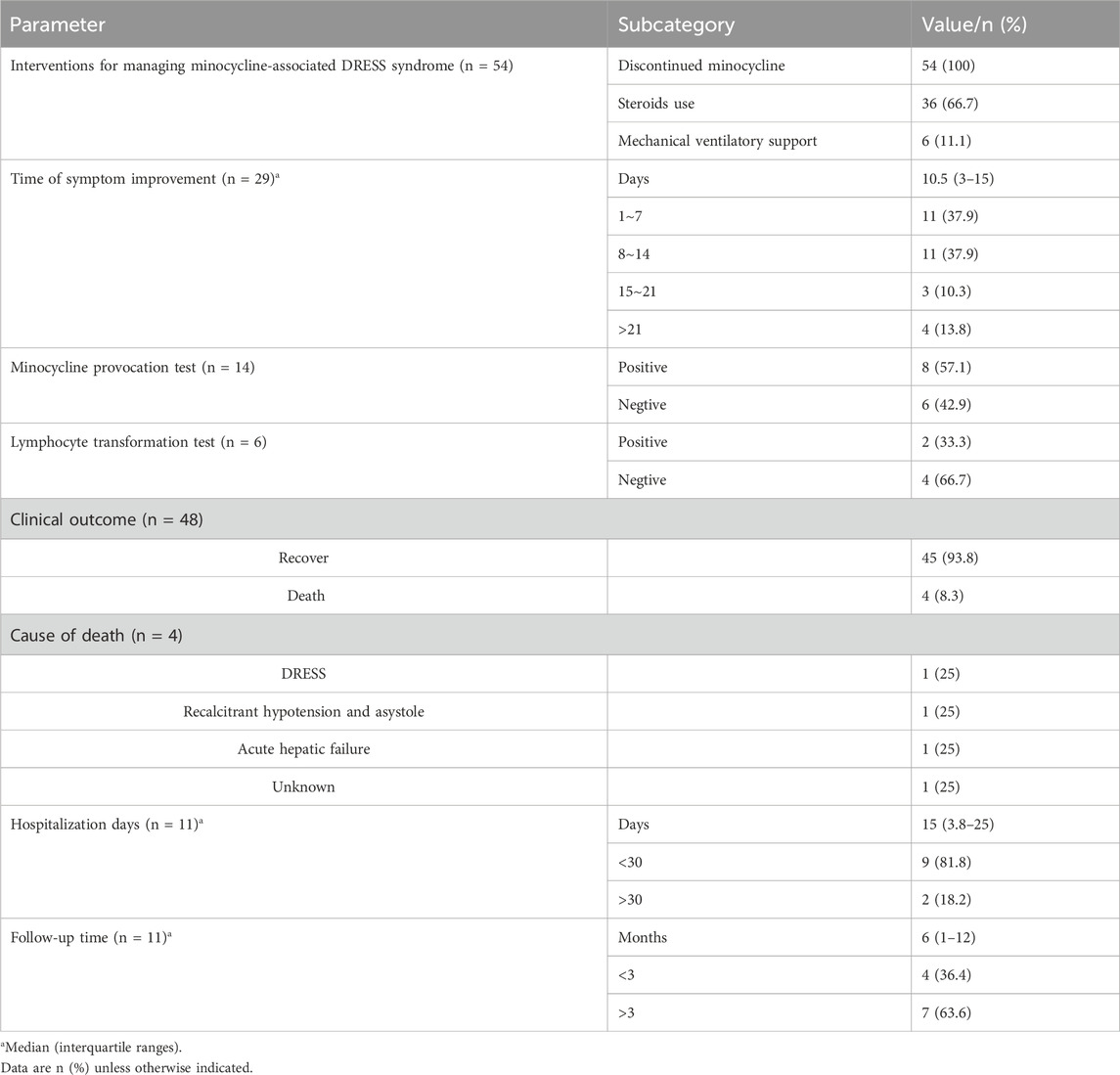
The results are summarized in Table 4. After patients developed DRESS, 54 patients reported treatment outcomes, and all discontinued minocycline. Thirty-six patients (66.7%) received steroid treatment, including intravenous or oral methylprednisolone, dexamethasone, or prednisone. Six (11.1%) patients needed mechanical ventilatory support. The median time of symptom improvement was 10.5 days (range, 3–15), and 11 (37.9%) cases had improvement in clinical symptoms in 1–7 days, 11 (37.9%) cases in 8–14 days, 3 (10.3%) cases in 15–21 days, and 4 (13.8%) cases in more than 21 days. Minocycline provocation test was done in 14 patients after discontinuation of minocycline, of which 57.1% (8 cases) came back positive and 42.9% (6 cases) negative. Six patients reported undergoing lymphocyte transformation testing, of which 2 (33.3%) tested positive and four (66.7%) tested negative. Eventually, a total of 45 patients (93.8%) recovered after treatment. Unfortunately, 4 patients died due to recalcitrant hypotension and asystole (1 case), hepatic failure (1 case), DRESS (1 case), and unknown cause (1 case). Hospitalization days were recorded in 11 patients: 9 (81.8%) within 30 days, 2 (18.2%) more than 30 days, and the median time of hospitalization days was 15 days (range, 3.8–25). Follow-up data were available for 11 patients, with a median follow-up duration of 6 months (range: 1–12 months). Among these, 4 patients (36.4%) were followed for less than 3 months, and seven patients (63.6%) were followed for more than 3 months.
Discussion
Drug reaction with eosinophilia and systemic symptoms (DRESS) is a syndrome of drug-induced hypersensitivity reactions, characterized primarily by rash, fever, hematologic and visceral organ involvement (Wei et al., 2024). First reported to be triggered by aromatic anticonvulsants, it has been successively reported that antibiotics and allopurinol also cause DRESS (Husain et al., 2013). The lack of reliable epidemiologic information on disease incidence and associated etiology has resulted in the absence of definitive studies counting the incidence of DRESS. Minocycline is a semi-synthetic tetracycline broad-spectrum antibiotic mainly used for pneumonia, acute bronchitis, urinary tract infections, respiratory tract infections, and acne due to staphylococcus, streptococcus, pneumococcus, and other pathogenic bacteria (Baldwin and Ward, 2021). Several adverse reactions, including life-threatening ones, have been reported in association with minocycline (Dominic, 2021). According to the French Pharmacovigilance Database (FPD), based on marketing authorization holders (MAH) data and published reports, minocycline-associated ADRs were more serious and were reported more frequently than for the other tetracyclines, especially autoimmune disorders, DRESS, and other hypersensitivity reactions (Lebrun-Vignes et al., 2012). This can prolong a patient’s medication regimen and hospitalization, increase medical costs, and even endanger a patient’s life. Therefore, we conducted this study to summarize the clinical features and outcomes of DRESS caused by minocycline.
The clinical manifestations of DRESS are not limited to eosinophilia, but also fever, cough, and pleurisy. Our finding that respiratory symptoms were the most common clinical manifestation (87.7%) aligns with the focused analysis by Taweesedt et al. which reported pulmonary involvement in 72% of definitive DRESS cases with lung involvement (Taweesedt et al., 2019). Notably, their study highlighted that pulmonary manifestations are less frequent in DRESS overall, underscoring that our higher prevalence may reflect minocycline-specific mechanisms (e.g., tissue accumulation) or a selection bias toward severe cases captured in published reports. However, our study observed a higher proportion of respiratory symptoms compared to the 50% interstitial infiltrates and 31% acute respiratory distress syndrome (ARDS) reported in that review. This discrepancy may be attributed to differences in study populations (pediatric vs. adult focus) or diagnostic criteria (RegiSCAR score ≥6 vs. clinical diagnosis). These similarities underscore the importance of maintaining a high index of suspicion for DRESS in patients presenting with unexplained respiratory symptoms and peripheral eosinophilia. Some patients are also accompanied by abnormally elevated CRP and ESR, and are therefore easily misdiagnosed. Therefore, it needs to be differentiated from other severe skin rashes, viral or bacterial infections, eosinophilia, lymphomas, and connective tissue diseases. Histopathology can specifically diagnose DRESS and monitor disease progression and response to treatment. Histopathology can support the differential diagnosis of DRESS by excluding alternative diseases, such as infections, lymphomas, or connective tissue disorders. However, it cannot definitively diagnose DRESS, as no pathognomonic histological features have been described for DRESS in skin or lung biopsies. In this study, transbronchial lung biopsy revealed eosinophilic infiltration in 13 of 14 cases (92.9%), suggesting a significant eosinophilic inflammatory process in the lungs of these individuals. While nonspecific, it aligns with the immune-mediated eosinophilic inflammation characteristic of DRESS and helps corroborate the clinical diagnosis when combined with other RegiSCAR criteria. The high prevalence of pulmonary involvement may reflect both the systemic distribution of minocycline and the immune-mediated eosinophilic infiltration observed in lung tissue (92.9% of biopsies). This aligns with the broader pathophysiology of DRESS, where drug-specific immune responses contribute to multi-organ inflammation, including the respiratory system.
The exact pathogenesis of DRESS is unknown. It is currently proposed that drug metabolism, immune dysregulation, and genetic susceptibility interact to trigger a systemic hypersensitivity response, which may be exacerbated by viral reactivation (e.g., herpesviruses) in susceptible individuals. However, drug exposure remains the primary and essential trigger for DRESS (Kardaun et al., 2013; Yamada et al., 2019). Minocycline is mainly metabolized by the liver and kidneys, with a plasma half-life of about 18 h (Saivin and Houin, 1988; Nelis and De Leenheer, 1982). Due to its high lipid solubility, minocycline easily penetrates into lipophilic tissues and body fluids, and is widely distributed in the body, especially prone to cause thyroid pigmentation and skin pigmentation (Jonas and Cunha, 1982). Eve Maubec et al. showed that minocycline accumulation in patients, especially in the skin, is associated with a prolonged course of DRESS (Maubec et al., 2008). This may mediate an autoimmune response that is ultimately a key factor in the poor clinical outcomes of DRESS. The median time to symptom improvement was 10.5 days, with 24.1% of patients (10.3% in 15–21 days and 13.8% in >21 days) requiring more than 2 weeks to achieve clinical recovery. Some studies have already shown, by positive patch tests and in vitro lymphocyte proliferation assays, that a strong drug-specific immune response is a key factor in the pathogenesis of DRESS (Genin et al., 2014; Barbaud et al., 2013). In our study, we reported two cases with positive results of the minocycline lymphocyte transformation test. Fourteen additional patients reported results of the minocycline provocation test, of which 57.1% were positive. We retained 6 cases with negative drug provocation tests results. This is because all 6 cases met the RegiSCAR criteria for a definite or probable diagnosis of DRESS based on clinical presentation, laboratory findings, and temporal association with minocycline exposure. In addition, we performed a sensitivity analysis to exclude these cases and found no substantial changes in our main findings regarding clinical features or prognosis. Our study reported below-normal CD4+/CD8+ ratios in nine patients. It has been shown that during the acute phase of DRESS, activated cytotoxic T cells (CD8+ T cells) and helper T cells (CD4+ T cells) expand, and the CD4+/CD8+ ratio usually decreases, which corroborates our results (Miyagawa et al., 2020). It has been established that individuals carrying specific mutations in genes that encode drug detoxification enzymes have a higher risk of DRESS (Tas and Simonart, 1999). Unlike other cyclines, for example, minocycline is metabolized in the liver, and the patients included in our study generally had abnormal liver function. Liver function tests (ALT/AST) were measured after DRESS symptom onset and showed median elevations of 114 U/L and 86 U/L, respectively. The observed transaminase elevations may result from a combination of minocycline’s hepatotoxic potential and immune-mediated liver injury, a hallmark of DRESS. While hepatic detoxification pathways could play a role, our study lacks direct evidence to confirm this mechanism. Unfortunately, our study did not report results regarding pharmacogenetic susceptibility.
Discontinuation of minocycline is an imperative step in managing suspected DRESS, as ongoing exposure risks exacerbating organ damage and mortality, as stipulated in the RegiSCAR diagnostic framework. The patients included in this study were treated with timely interventions to discontinue the drug. Treatment requires different interventions depending on the patient’s symptoms, including, but not limited to, antipyretic, cough suppression, rehydration, maintenance of electrolyte balance, nutritional support, and liver protection. Prioritize the use of highly effective topical corticosteroids when necessary. Although only one death was due to DRESS, and 93.8% of patients had a favorable outcome, there were still two cases of death due to severe involvement of vital organs. This demonstrates the critical importance of frequent monitoring and follow-up for patients with severe or rapidly progressing disease. Two patients in our study had relapses after improvement on initial treatment, and the duration of relapse was 6 weeks. Therefore, it cannot be ruled out that patients may develop autoimmune diseases and related sequelae months or years after the end of the drug response (Chen et al., 2013).
Several limitations of this study should be mentioned. This is insufficient for a comprehensive assessment of the clinical features of minocycline-induced DRESS, especially the assessment of risk factors. Subsequent analysis of relevant risk factors and predictive modeling based on a large data platform is required. This was a retrospective study, and parameters such as time to onset of adverse reactions and time to improvement of the patient’s symptoms may bias the results due to factors such as the reporting person’s recording preferences. As the included studies were from different regions, the test indicator eligibility ranges and indicator units varied, which may cause some bias to the results after standardization and harmonization.
Conclusion
In conclusion, we comprehensively delineated the clinical characteristics, diagnostic challenges, and treatment outcomes of minocycline-associated DRESS syndrome. The study underscores the importance of recognizing the diverse clinical manifestations, particularly respiratory symptoms, and the necessity of timely intervention through drug cessation and corticosteroid therapy. Despite the favorable prognosis in most cases, the potential for severe organ involvement and the risk of prolonged hospitalization highlights the critical need for vigilant monitoring and follow-up. Future research should focus on expanding the sample size and addressing the limitations of retrospective studies to further enhance our understanding of this complex syndrome and improve patient care.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors upon reasonable request.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
YP: Writing – review and editing. QW: Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2025.1515000/full#supplementary-material
References
Asadi, A., Abdi, M., Kouhsari, E., Panahi, P., Sholeh, M., Sadeghifard, N., et al. (2020). Minocycline, focus on mechanisms of resistance, antibacterial activity, and clinical effectiveness: back to the future. J. Glob. Antimicrob. Resist. 22, 161–174. doi:10.1016/j.jgar.2020.01.022
Baldwin, H. E., and Ward, D. B. (2021). Fifty years of minocycline and its evolution: a dermatological perspective. J. drugs dermatology JDD 20 (10), 1031–1036. doi:10.36849/JDD.6370
Barbaud, A., Collet, E., Milpied, B., Assier, H., Staumont, D., Avenel-Audran, M., et al. (2013). A multicentre study to determine the value and safety of drug patch tests for the three main classes of severe cutaneous adverse drug reactions. Br. J. dermatology 168 (3), 555–562. doi:10.1111/bjd.12125
Brüggen, M. C., Walsh, S., Ameri, M. M., Anasiewicz, N., Maverakis, E., French, L. E., et al. (2024). Management of adult patients with drug reaction with eosinophilia and systemic symptoms: a delphi-based international consensus. JAMA dermatol. 160 (1), 37–44. doi:10.1001/jamadermatol.2023.4450
Calle, A. M., Aguirre, N., Ardila, J. C., and Cardona Villa, R. (2023). DRESS syndrome: a literature review and treatment algorithm. World Allergy Organ. J. 16 (3), 100673. doi:10.1016/j.waojou.2022.100673
Cardones, A. R. (2020). Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome. Clin. dermatology 38 (6), 702–711. doi:10.1016/j.clindermatol.2020.06.008
Chen, Y. C., Chang, C. Y., Cho, Y. T., Chiu, H. C., and Chu, C. Y. (2013). Long-term sequelae of drug reaction with eosinophilia and systemic symptoms: a retrospective cohort study from Taiwan. J. Am. Acad. Dermatology 68 (3), 459–465. doi:10.1016/j.jaad.2012.08.009
Chow, A. W., Patten, V., and Guze, L. B. (1975). Comparative susceptibility of anaerobic bacteria to minocycline, doxycycline, and tetracycline. Antimicrob. agents Chemother. 7 (1), 46–49. doi:10.1128/aac.7.1.46
Dominic, M. R. (2021). Adverse reactions induced by minocycline: a review of literature. Curr. drug Saf. 16 (3), 309–321. doi:10.2174/1574886316666210120090446
Elkayam, O., Yaron, M., and Caspi, D. (1999). Minocycline-induced autoimmune syndromes: an overview. Seminars arthritis rheumatism 28 (6), 392–397. doi:10.1016/s0049-0172(99)80004-3
Garner, S. E., Eady, E. A., Popescu, C., Newton, J., and Li Wan Po, A. (2000). Minocycline for acne vulgaris: efficacy and safety. Cochrane database Syst. Rev. (2), Cd002086. doi:10.1002/14651858.CD002086
Genin, E., Chen, D. P., Hung, S. I., Sekula, P., Schumacher, M., Chang, P. Y., et al. (2014). HLA-A*31:01 and different types of carbamazepine-induced severe cutaneous adverse reactions: an international study and meta-analysis. pharmacogenomics J. 14 (3), 281–288. doi:10.1038/tpj.2013.40
Hama, N., Abe, R., Gibson, A., and Phillips, E. J. (2022). Drug-induced hypersensitivity syndrome (DIHS)/drug reaction with eosinophilia and systemic symptoms (DRESS): clinical features and pathogenesis. J. allergy Clin. Immunol. Pract. 10 (5), 1155–1167.e5. doi:10.1016/j.jaip.2022.02.004
Hellmann-Regen, J., Clemens, V., Grözinger, M., Kornhuber, J., Reif, A., Prvulovic, D., et al. (2022). Effect of minocycline on depressive symptoms in patients with treatment-resistant depression: a randomized clinical trial. JAMA Netw. open 5 (9), e2230367. doi:10.1001/jamanetworkopen.2022.30367
Hung, W. K., and Chung, W. H. (2022). Drug reaction with eosinophilia and systemic symptoms. N. Engl. J. Med. 387 (2), 167. doi:10.1056/NEJMicm2116076
Husain, Z., Reddy, B. Y., and Schwartz, R. A. (2013). DRESS syndrome: part I. Clinical perspectives. J. Am. Acad. Dermatology 68 (5), e1–e14. doi:10.1016/j.jaad.2013.01.033
Jonas, M., and Cunha, B. A. (1982). Minocycline. Ther. drug Monit. 4 (2), 115–146. doi:10.1097/00007691-198206000-00002
Kardaun, S. H., Mockenhaupt, M., and Roujeau, J. C. (2014). Comments on: DRESS syndrome. J. Am. Acad. Dermatology 71 (5), 1000–1000.e2. doi:10.1016/j.jaad.2013.11.053
Kardaun, S. H., Sekula, P., Valeyrie-Allanore, L., Liss, Y., Chu, C. Y., Creamer, D., et al. (2013). Drug reaction with eosinophilia and systemic symptoms (DRESS): an original multisystem adverse drug reaction. Results from the prospective RegiSCAR study. Br. J. dermatology 169 (5), 1071–1080. doi:10.1111/bjd.12501
Kardaun, S. H., Sidoroff, A., Valeyrie-Allanore, L., Halevy, S., Davidovici, B. B., Mockenhaupt, M., et al. (2007). Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br. J. dermatology 156 (3), 609–611. doi:10.1111/j.1365-2133.2006.07704.x
Krantz, M. S., and Phillips, E. J. (2023). Drug reaction with eosinophilia and systemic symptoms. JAMA dermatol. 159 (3), 348. doi:10.1001/jamadermatol.2022.4519
Lebrun-Vignes, B., Kreft-Jais, C., Castot, A., and Chosidow, O.French Network of Regional Centers of Pharmacovigilance (2012). Comparative analysis of adverse drug reactions to tetracyclines: results of a French national survey and review of the literature. Br. J. dermatology 166 (6), 1333–1341. doi:10.1111/j.1365-2133.2012.10845.x
Martins, A. M., Marto, J. M., Johnson, J. L., and Graber, E. M. (2021). A review of systemic minocycline side effects and topical minocycline as a safer alternative for treating acne and rosacea. Antibiot. Basel, Switz. 10 (7), 757. doi:10.3390/antibiotics10070757
Maubec, E., Wolkenstein, P., Loriot, M. A., Wechsler, J., Mulot, C., Beaune, P., et al. (2008). Minocycline-induced DRESS: evidence for accumulation of the culprit drug. Dermatol. Basel, Switz. 216 (3), 200–204. doi:10.1159/000112926
Miyagawa, F., Nakamura-Nishimura, Y., Kanatani, Y., and Asada, H. (2020). Correlation between expression of CD134, a human herpesvirus 6 cellular receptor, on CD4+ T cells and Th2-type immune responses in drug-induced hypersensitivity syndrome/drug reaction with eosinophilia and systemic symptoms. Acta dermato-venereologica 100 (6), adv00102. doi:10.2340/00015555-3465
Mojica, M. F., Bonomo, R. A., and van Duin, D. (2023). Treatment approaches for severe Stenotrophomonas maltophilia infections. Curr. Opin. Infect. Dis. 36 (6), 572–584. doi:10.1097/QCO.0000000000000975
Mori, F., Caffarelli, C., Caimmi, S., Bottau, P., Liotti, L., Franceschini, F., et al. (2019). Drug reaction with eosinophilia and systemic symptoms (DRESS) in children. Acta bio-medica Atenei Parm. 90 (3-s), 66–79. doi:10.23750/abm.v90i3-S.8167
Nelis, H. J., and De Leenheer, A. P. (1982). Metabolism of minocycline in humans. Drug metabolism Dispos. Biol. fate Chem. 10 (2), 142–146. doi:10.1016/s0090-9556(25)07851-1
Saivin, S., and Houin, G. (1988). Clinical pharmacokinetics of doxycycline and minocycline. Clin. Pharmacokinet. 15 (6), 355–366. doi:10.2165/00003088-198815060-00001
Sharifzadeh, S., Mohammadpour, A. H., Tavanaee, A., and Elyasi, S. (2021). Antibacterial antibiotic-induced drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome: a literature review. Eur. J. Clin. Pharmacol. 77 (3), 275–289. doi:10.1007/s00228-020-03005-9
Shiohara, T., and Mizukawa, Y. (2019). Drug-induced hypersensitivity syndrome (DiHS)/drug reaction with eosinophilia and systemic symptoms (DRESS): an update in 2019. Allergology Int. official J. Jpn. Soc. Allergology 68 (3), 301–308. doi:10.1016/j.alit.2019.03.006
Tas, S., and Simonart, T. (1999). Drug rash with eosinophilia and systemic symptoms (DRESS syndrome). Acta Clin. Belg. 54 (4), 197–200. doi:10.1080/17843286.1999.11754231
Taweesedt, P. T., Nordstrom, C. W., Stoeckel, J., and Dumic, I. (2019). Pulmonary manifestations of drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome: a systematic review. BioMed Res. Int. 2019, 7863815. doi:10.1155/2019/7863815
Wei, B. M., Fox, L. P., Kaffenberger, B. H., Korman, A. M., Micheletti, R. G., Mostaghimi, A., et al. (2024). Drug-induced hypersensitivity syndrome/drug reaction with eosinophilia and systemic symptoms. Part I. Epidemiology, pathogenesis, clinicopathological features, and prognosis. J. Am. Acad. Dermatology 90 (5), 885–908. doi:10.1016/j.jaad.2023.02.072
Wu, L., Morrow, B. R., Jefferson, M. M., Li, F., and Hong, L. (2021). Antibacterial collagen composite membranes containing minocycline. J. Pharm. Sci. 110 (5), 2177–2184. doi:10.1016/j.xphs.2020.12.026
Yamada, H., Hida, N., Kurashima, Y., Satoh, H., Saito, T., and Hizawa, N. (2019). A case of severe eosinophilic asthma and refractory rheumatoid arthritis well controlled by combination of IL-5Rα antibody and TNFα inhibitor. Allergology Int. official J. Jpn. Soc. Allergology 68 (4), 536–538. doi:10.1016/j.alit.2019.04.003
Yang, Y. S., Huang, T. W., Huang, Y. C., Huang, W. C., Hsu, S. Y., Wu, H. C., et al. (2022). In vitro and in vivo efficacy of minocycline-based therapy for Elizabethkingia anophelis and the impact of reduced minocycline susceptibility. Int. J. Antimicrob. agents 60 (5-6), 106678. doi:10.1016/j.ijantimicag.2022.106678
Keywords: minocycline, eosinophilia, hypersensitivity, dress, adverse event
Citation: Pan Y and Wu Q (2025) Clinical manifestations, diagnostic criteria, and treatment outcomes of minocycline-associated DRESS syndrome: a comprehensive exploration of published cases. Front. Pharmacol. 16:1515000. doi: 10.3389/fphar.2025.1515000
Received: 22 October 2024; Accepted: 09 July 2025;
Published: 22 July 2025.
Edited by:
Rannakoe Lehloenya, University of Cape Town, South AfricaReviewed by:
Teresa Bellon, University Hospital La Paz Research Institute (IdiPAZ), SpainGenevieve Elizabeth Martin, The University of Melbourne, Australia
Mireille Porter, University of Cape Town, South Africa
Copyright © 2025 Pan and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiquan Wu, NzkxODE4MTUxQHFxLmNvbQ==
 Yan Pan
Yan Pan Qiquan Wu
Qiquan Wu