- 1The Affiliated Stomatological Hospital of Chongqing Medical University, Chongqing, China
- 2Chongqing Key Laboratory of Oral Diseases, Chongqing, China
- 3Chongqing Municipal Key Laboratory of Oral Biomedical Engineering of Higher Education, Chongqing, China
- 4Chongqing Municipal Health Commission Key Laboratory of Oral Biomedical Engineering, Chongqing, China
- 5The Fifth People’s Hospital of Chongqing, Chongqing, China
Introduction: This study aimed to evaluate the biomechanical effects of varying sagittal root position (SRP), root length (RL), and cortical bone thickness (CBT) on tooth movement and stress distribution during clear aligner therapy (CAT) in extraction cases, using finite element analysis.
Methods: Three-dimensional finite element models, including the maxillary alveolar bone, periodontal ligament (PDL), dentition, and clear aligner, were constructed. Groups with varying SRP (labial, middle, and palatal), RL (long, normal, short) and CBT (1 mm, 2 mm) were established. Tooth movement and stress distribution were analyzed for each group after 0.2 mm anterior tooth retraction.
Results: Without attachments or additional forces, clear aligners (CAs) resulted in lingual tipping, extrusion, and distal movement of the central incisor in extraction cases. A labially positioned root amplified lingual tipping and torque loss, whereas a palatally positioned root preserved torque but increased posterior anchorage loss; moreover, shorter roots accentuated tipping and generated peak PDL stresses at the cervical and apical regions, while thinner cortical bone resulted in higher stress.
Conclusion: SRP and RL significantly affect tooth movement and stress distribution during anterior tooth retraction with CAs in extraction cases, while CBT has minimal impact in tooth movement. The optimal pre-retraction state involves a crown-to-root ratio not exceeding 1.1, with the root positioned upright in the cancellous bone, preventing contact with the labial or palatal cortical bone.
1 Introduction
Clear aligner therapy (CAT), initially limited to minor crowding or spacing, has expanded to extraction cases through advancements in 3D digital modeling and biomechanical refinement. (Adel et al., 2023). Nonetheless, undesirable tooth movements, such as deepened overbite, lingual inclination of anterior teeth, or mesial tilting of posterior teeth, are unavoidable during extraction space closure. (Dai et al., 2021). Qian et al. observed that, in premolar extraction cases, clear aligners (CAs) demonstrate a more pronounced “roller-coaster effect” compared to fixed orthodontic appliances. (Qian et al., 2024). Control of anterior labiolingual inclination remains challenging, as Dai et al.'s clinical research revealed that central incisors displayed reduced retraction, greater lingual inclination and extrusion than anticipated (Dai et al., 2019). Significant changes in incisor inclination may lead to orthodontic complications, such as dehiscence and fenestration. (Chambrone and Avila-Ortiz, 2021; Bae et al., 2018). Miyama et al. noted that lingual and extrusive incisor movements contribute to a reduction in alveolar bone height, (Miyama et al., 2018), potentially compromising periodontal health and treatment stability. (Yagci et al., 2011).
Finite Element Analysis (FEA) is a noninvasive virtual modeling tool that simulates oral conditions to analyze force dynamics. (Singh et al., 2024). In orthodontics, FEA is widely used to assess tooth movement and stress distribution under various loading conditions. (Knop et al., 2015). Studies using FEA have provided key insights into the biomechanical optimization of extraction cases in CAT. Meng et al. reported that varying power ridge depths had little effect on tooth displacement patterns, but displacement magnitude increased with deeper ridges. (Meng et al., 2023). According to Lyu’s FEA, optimized aligners with differential margin designs and varied thermoplastic thicknesses improved tooth movement efficiency and control during extraction space closure. (Lyu et al., 2023). Mao et al. found that increasing shape designs at extraction space height enhances anterior teeth retraction, while lowering CAES height aids controlled root movement during extraction space closure. (Mao et al., 2024). Semi-ellipsoid attachments proved uperior for labiolingual inclination control, while power ridges enhanced root control, as noted by Hong (2024).
Prior studies have primarily concentrated on enhancing tooth movement efficiency in CAT by refining aligner designs, attachments, and tooth movement strategies. However, patient-specific factors, such as alveolar bone thickness, tooth root morphology, and sagittal skeletal pattern, significantly influence efficiency and constrain movement range. (Coşkun and Kaya, 2019; Rodrigues et al., 2023). For instance, Zhou et al. found that teeth with longer clinical crowns exhibit reduced torque loss during translational movement, whereas shorter crowns are more prone to bodily movement. (Zhou et al., 2025). Similarly, Sun’s FEA of models with varying alveolar bone resorption highlighted the need to minimize stress on periodontal tissues in patients with bone loss to prevent irreversible damage. (Sun et al., 2019). Despite these findings, FEA studies examining how root/cortical bone relation—like root length (RL), cortical bone thickness (CBT), and sagittal root position (SRP) of maxillary anterior teeth—influence tooth movement efficiency and safety are limited. In addition, deformation of the aligner leads to inconsistent contact points with the crown, causing uncertainty in the force’s magnitude, direction, and application point. (Barone et al., 2017; Liu, 2023). The complex biomechanics of clear aligners further complicates predicting anterior tooth retraction in extraction cases across diverse patients.
Therefore, this study aims to evaluate the effects of different root/cortical bone relation (with varying RL, CBT, and SRP) on tooth movement and stress distribution in CAT for extraction cases using finite element analysis.
2 Materials and methods
One healthy female volunteer aged 26 years was selected based on the following criteria: (1) Bilateral maxillary first premolars extracted with aligned and leveled maxillary dentition, (2) normal tooth morphology with harmonious crown-root ratio, no root resorption, (3) SRP of the maxillary central incisors in the alveolar bone middle, (3) no significant periodontal soft or hard tissue recession with normal Alveolar bone thickness, (4) no temporomandibular joint disorders. Cone-beam computed tomography (CBCT) data were acquired using a KaVo Dental GmbH scanner (KaVo, United States) under these settings: 120 kVp, 0.4 mm voxel size; scanning time, 8.9 s. Data were saved in “.dicom” format. This study was approved by the Ethics Committee of the Affiliated Stomatological Hospital of Chongqing Medical University [CQHS -REC-2025 (LSNo.083)].
A 3-dimensional preliminary model of the maxillary dentition and maxilla was established with CBCT data using Mimics 21.0 (Materialise, Belgium) by adjusting thresholds based on grayscale differences. The model was adjusted and symmetrically aligned along the midsagittal plane to develop a complete maxillary dentition and maxilla model using Geomagic Wrap 2017 (Geomagic, United States) and SolidWorks 2022 (SolidWorks, United States). To create models with varying root lengths for anterior teeth, the root apices of maxillary anterior teeth were reduced by 2 mm and 4 mm, respectively, resulting in three maxillary dentition models. (Figure 1E). After calculation, the crown-to-root ratios, from smallest to largest, were 1.3(long root), 1.1(normal root), and 0.8 (short root). PDL was generated by offsetting each tooth’s surface outward by 0.2 mm using Geomagic Wrap 2017, followed by Boolean operations using SolidWorks 2022 (Figure 1D). The anterior maxillary teeth were retracted sagittally by 0.2 mm, and the updated maxillary dentition was shelled outward to a thickness of 0.75 mm to generate the aligner model using Boolean operations (Figure 1F). The maxilla model was hollowed outward by 1 mm and both outward and inward by 1 mm each (keeping the outer surface dimensions of the cortical bone model consistent, with thicknesses of 1 mm and 2 mm respectively), producing two cortical bone models (Figure 1B). Through Boolean operations, two cancellous bone models were generated from these cortical bone models (Figure 1A). To acquire the alveolar fossa of the maxilla, dentition, and PDL were subtracted from the maxilla by Boolean operation (Figure 1C). Three different SRPs of maxillary anterior teeth were established: (1) created by translating the teeth labially by 2.5 mm from their original position; (2) the original position; and (3) lingually by 2.5 mm. These resulted in three distinct alveolar socket morphologies. All components were assembled to form the final assembly (Figure 1G).

Figure 1. Finite element model: (A) cancellous bone; (B) Cortical bone; (C) Alveolar bone; (D) PDL; (E) Maxillary dentition; (F) CA; (G) Final assembly.
Eighteen model groups were established based on SRP, RL and CBT (Figure 2). The SRP is denoted as La for the labial side, M for the middle, and P for the palatal side. RL is represented as LR for long root, NR for normal root, and SR for short root. CBT is indicated as CBT1 for 1 mm and CBT2 for 2 mm. For example, the group characterized by a sagittal root position on the labial side, long root, and cortical bone thickness of 1 mm is denoted as La-LR-CBT1, and so forth.
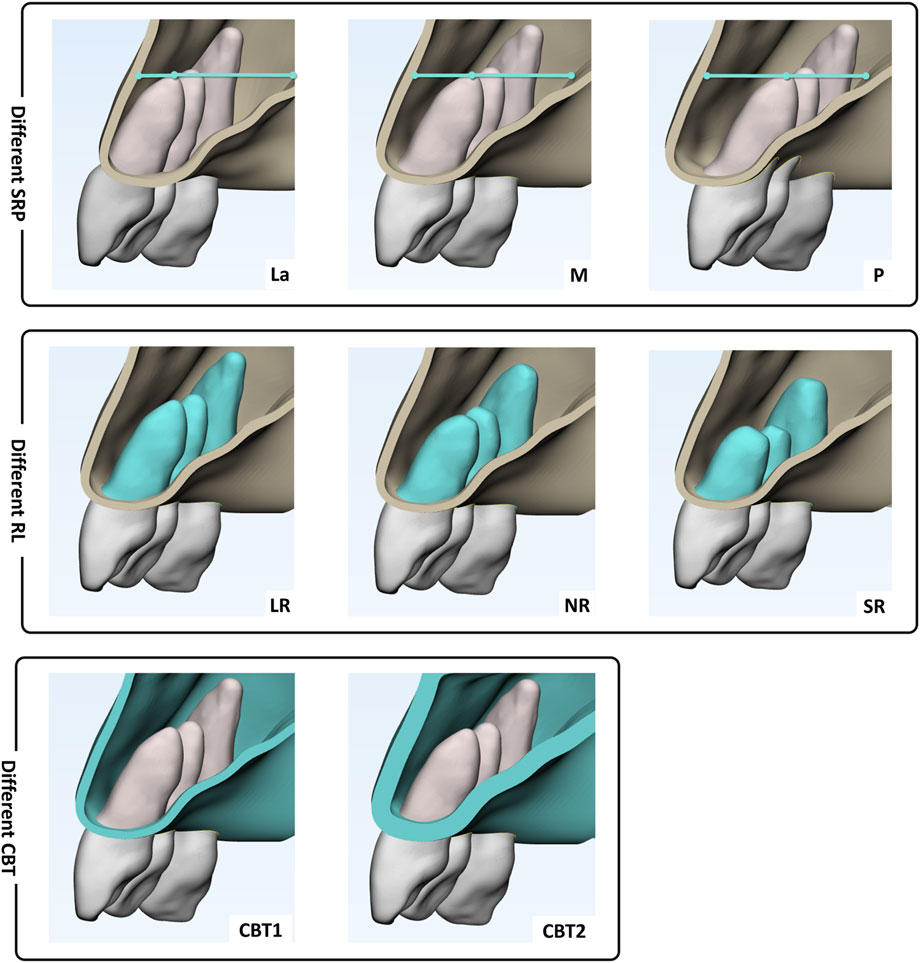
Figure 2. Grouping: Sagittal root position (SRP): on the labial side (La), in the middle (M), on the palatal side (P); Root length (RL): long root (LR), normal root (NR)and short root (SR); Cortical bone thickness of 1 mm (CBT1) and 2 mm (CBT2).
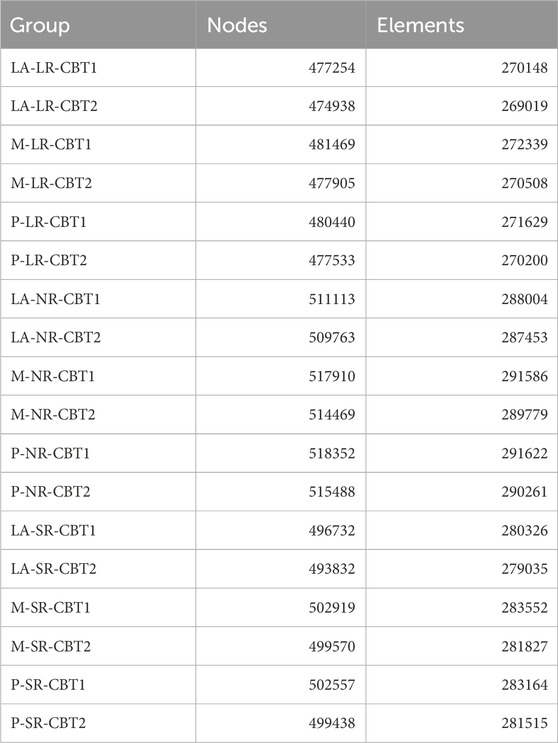
The material properties of each component were assumed to be linear elastic, isotropic, and homogeneous. The Young’s moduli and Poisson’s ratios for teeth, alveolar bone (composed of cortical and cancellous bone), the PDL, and the aligner are presented in Table 1. (Davy et al., 1981; Tanne et al., 1987; Liang et al., 2009; Gomez et al., 2015; Wang et al., 2024). Meshing was conducted with mesh sizes of 1.0 mm for teeth, 2.0 mm for alveolar bone (cortical and cancellous), 0.5 mm for the PDL, and 0.6 mm for the aligner (Davy et al., 1981). Node and element counts for the teeth, alveolar bone, PDL, and aligner models in each group are presented in Table 2.
Contact settings and boundary conditions were implemented. The maxillary alveolar bone base was fixed, with bonded contacts set between teeth and PDL, PDL and alveolar bone, and cortical and cancellous bone. Frictional contact, with a 0.2 friction coefficient, was defined between the outer crown surface and the inner aligner surface. No further constraints or loads were applied to the teeth or aligner.
A global coordinate system was established: the X-axis (coronal direction) aligned parallel to the plane, directed toward the patient’s right (positive) or left (negative); the Y-axis (sagittal direction) set perpendicular to the X-axis, oriented toward the central incisor (positive) or opposite (negative); and the Z-axis (vertical direction), perpendicular to both X and Y-axes, directed apically (positive) or coronally (negative).
Finite element analysis (FEA) was conducted using Ansys 2024 (Ansys, United States) for calculations. The analysis included: (1) initial tooth movement tendencies and displacement in the X-, Y-, and Z-axes.; (2) maximum von Mises stresses in the PDL and alveolar bone.
3 Result
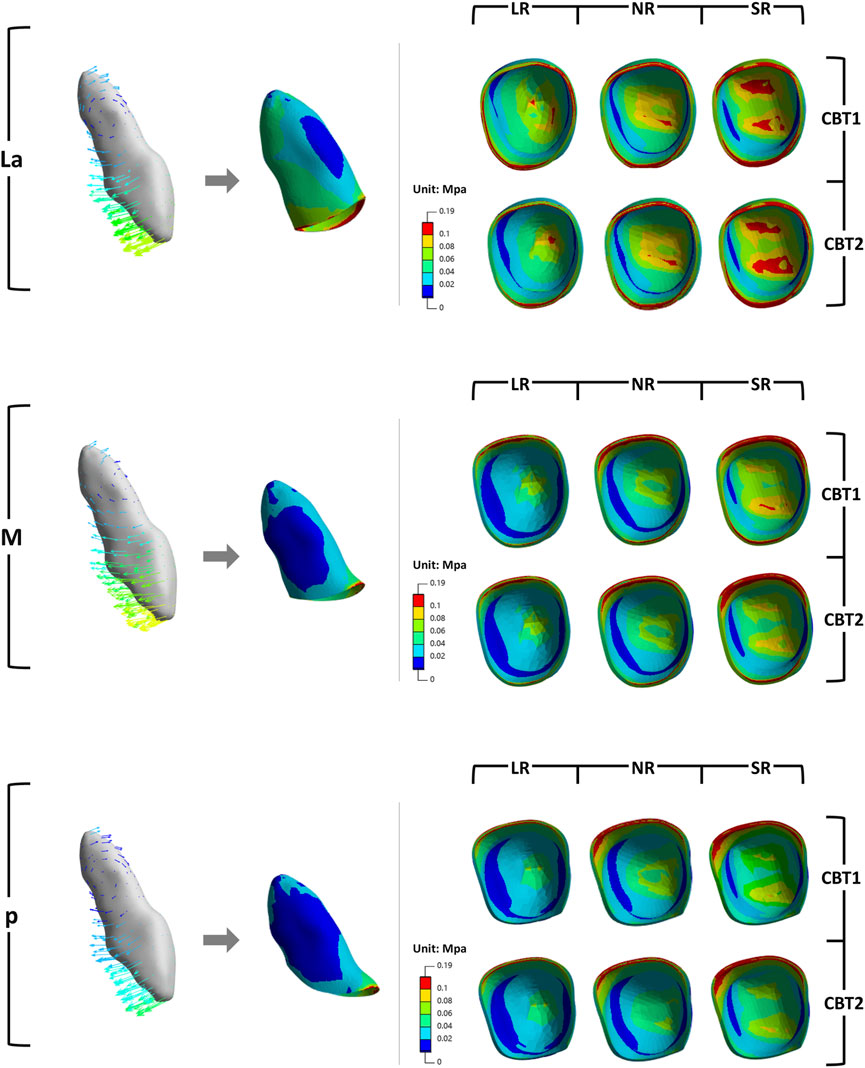
In all groups, the maxillary central incisors exhibited opposing crown and root movements. The crowns moved distally and lingually with extrusion and slight distal-lingual torsion, while the roots moved mesially and labially with intrusion (Figure 3). SRP and LR significantly influenced tooth movement, whereas CBT had no notable effect (P > 0.05).
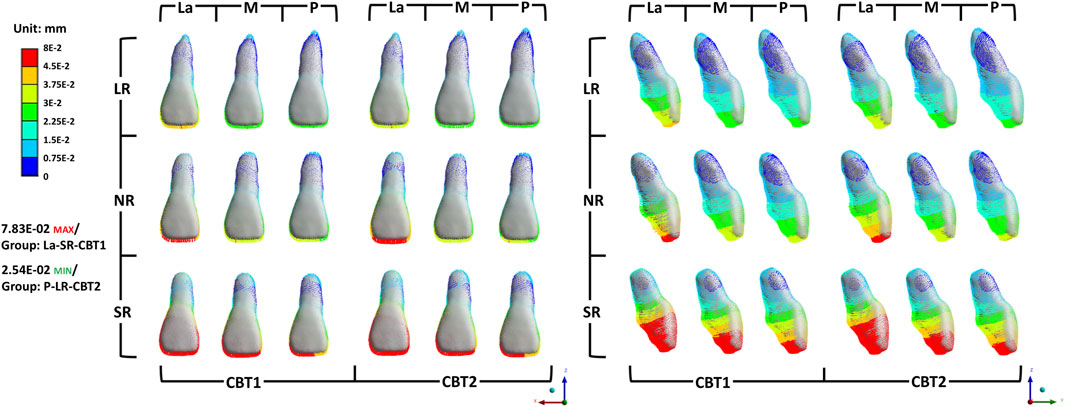
Figure 3. The initial tooth movement tendencies of maxillary central incisor with varying SRP/RL/CBT in coronal and sagittal directions.
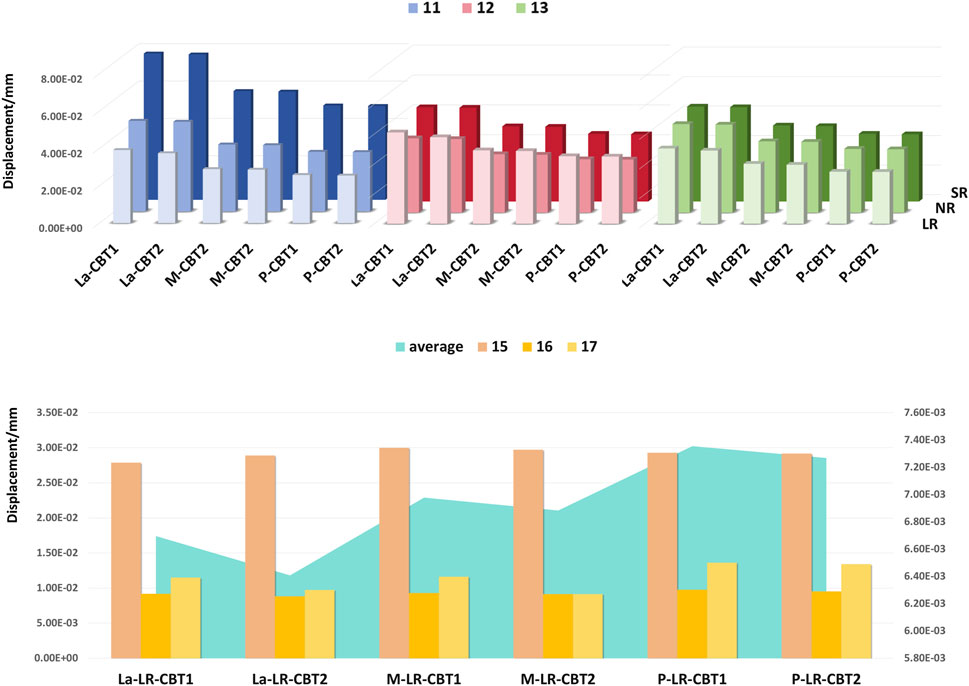
Changes in the three-dimensional direction were predominantly sagittal (Figure 4). When SRP varied, the La groups demonstrated the poorest torque control, with greater sagittal and vertical displacement of the root and apex in the opposite direction (Figures 4, 5). In the coronal direction, the P groups showed the largest axial inclination change. As RL decreased, torque control deteriorated, leading to a more pronounced lingual tipping of the maxillary central incisors (Figure 5). For groups with different CBTs, differences between 1 mm and 2 mm were minimal (Figure 3).
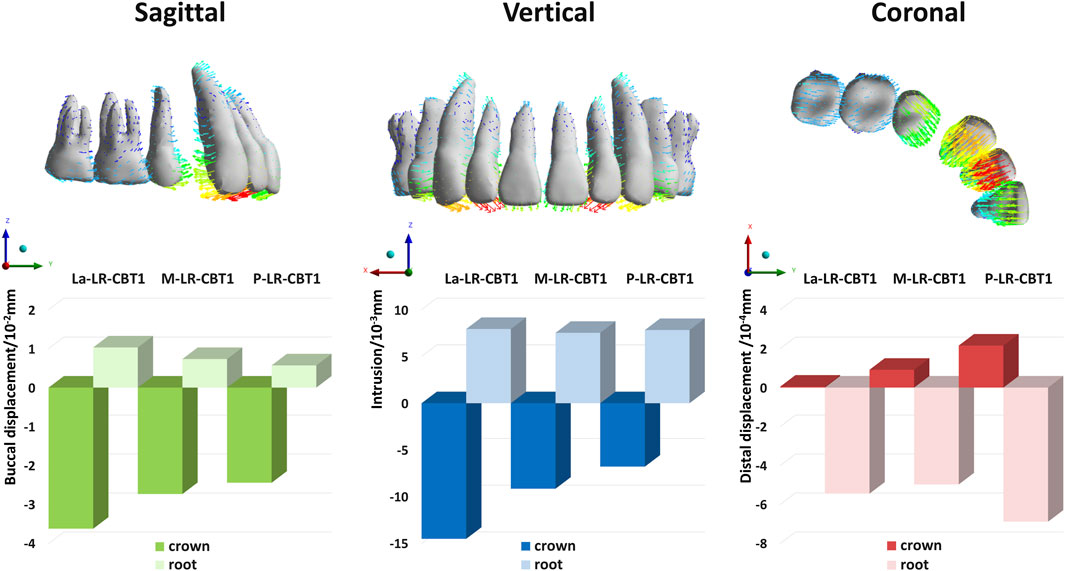
Figure 4. Bar charts: Three-dimensional displacement of the crown and root of maxillary central incisors under different SRP (with LR, CBT1).
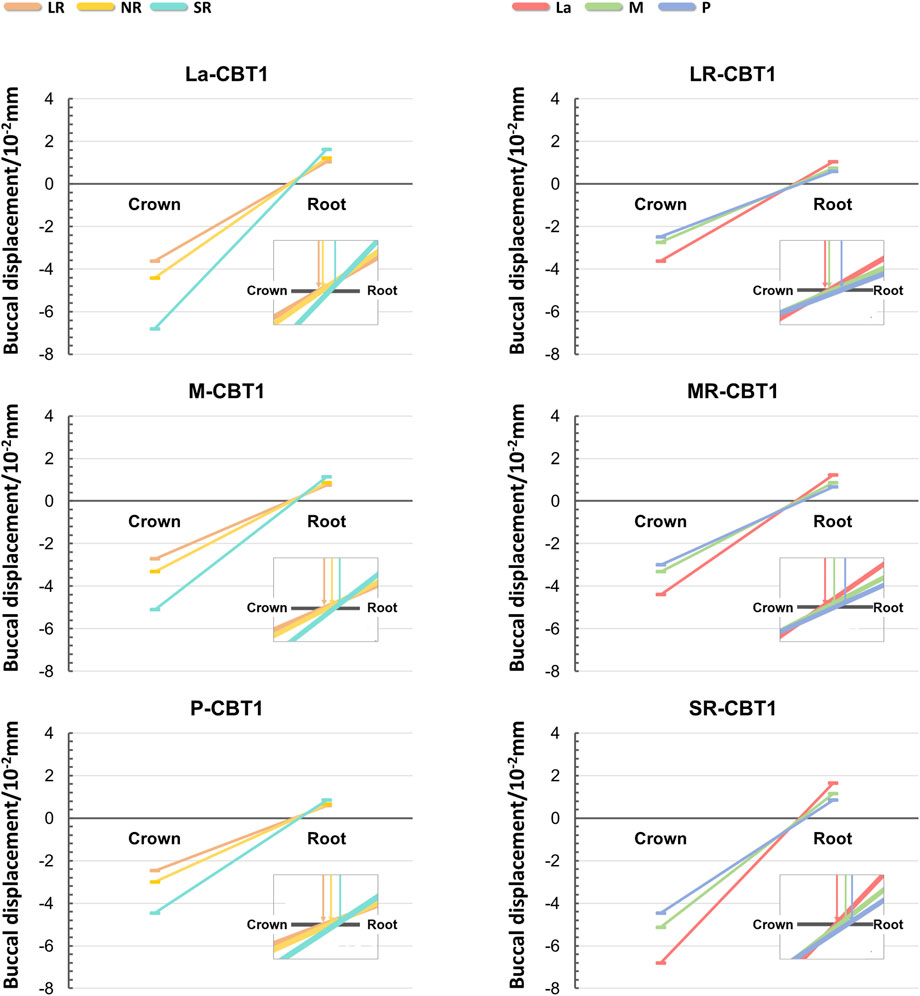
Figure 5. Line charts: Displacement of the crown and root of the maxillary central incisor under different SRP and RL (with CBT1). The point where the line intersected the x-axis marked the center of rotation, and the slope reflected the shift in labiolingual tilt.
Lateral incisors and canines exhibited similar movement tendencies to central incisors (Figure 6). Using M-LR-CBT1 as the control group, the effects of varying SRP, RL, and CBT on anterior teeth movement are illustrated in Figure 6.
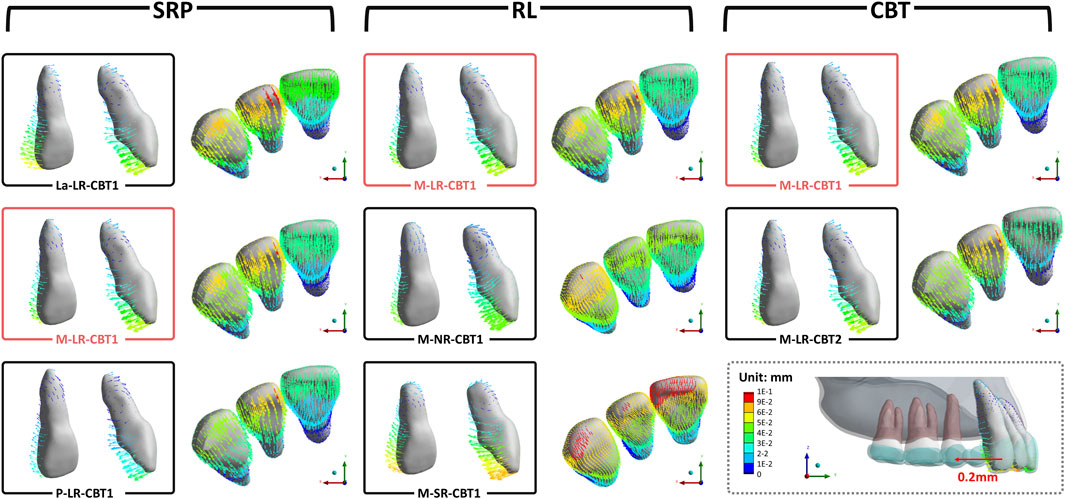
Figure 6. The initial tooth movement tendencies of anterior teeth with varying SRP/RL/CBT in occlusal directions. (M-LR-CBT1 as the control group).
Although the posterior teeth were not designed to move, they all exhibited a tendency for the crowns to move mesially and the roots to move distally in all groups (Figure 7)
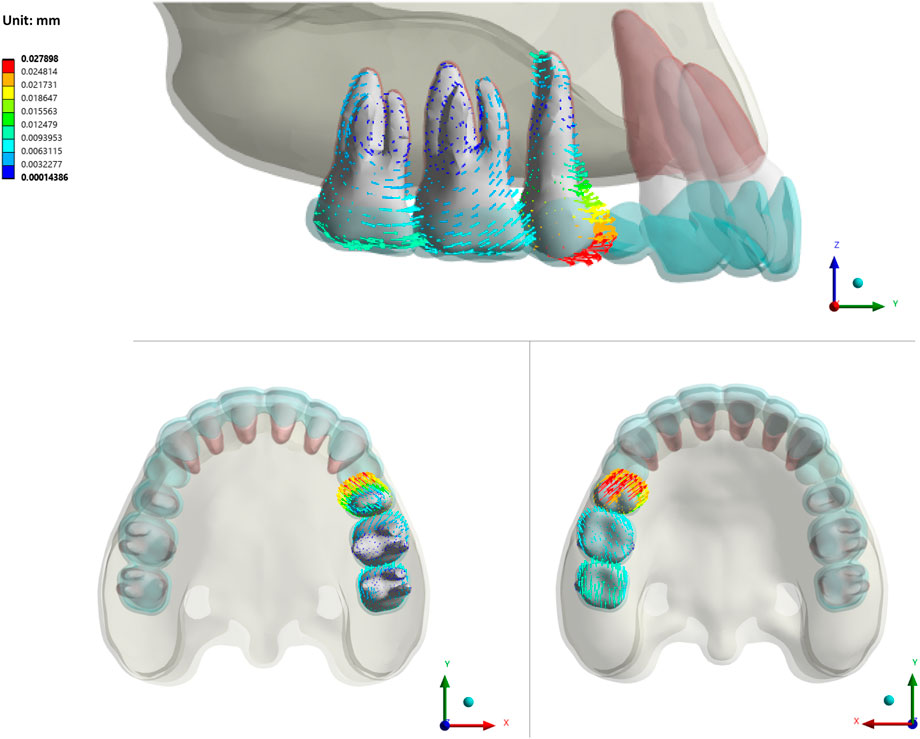
Figure 7. The initial tooth movement tendencies of posterior teeth with varying SRP/RL/CBT in sagittal/apex/occlusal directions (La-LR-CBT1).
The maximum displacement of each tooth is presented in Figure 8. Among anterior teeth, lateral incisors exhibited the greatest displacement, while central incisors showed the least. Among posterior teeth, second premolars showed the greatest mesial crown inclination, while first molars showed the least. Using average posterior tooth displacement to represent posterior anchorage loss, the P groups exhibited the greatest anchorage loss. Overall, anterior teeth displayed greater displacement than posterior teeth.
Von Mises stress concentrations were observed in the cervical areas and root apices of the periodontal ligament (PDL) of all central incisors, aligning with tooth movement patterns (Figure 9). The M groups exhibited the lowest stress, followed by the P groups, with the La groups showing the highest. Within each group, shorter roots were associated with progressively higher Von Mises stress, while increased cortical bone thickness significantly reduced stress (P < 0.05).
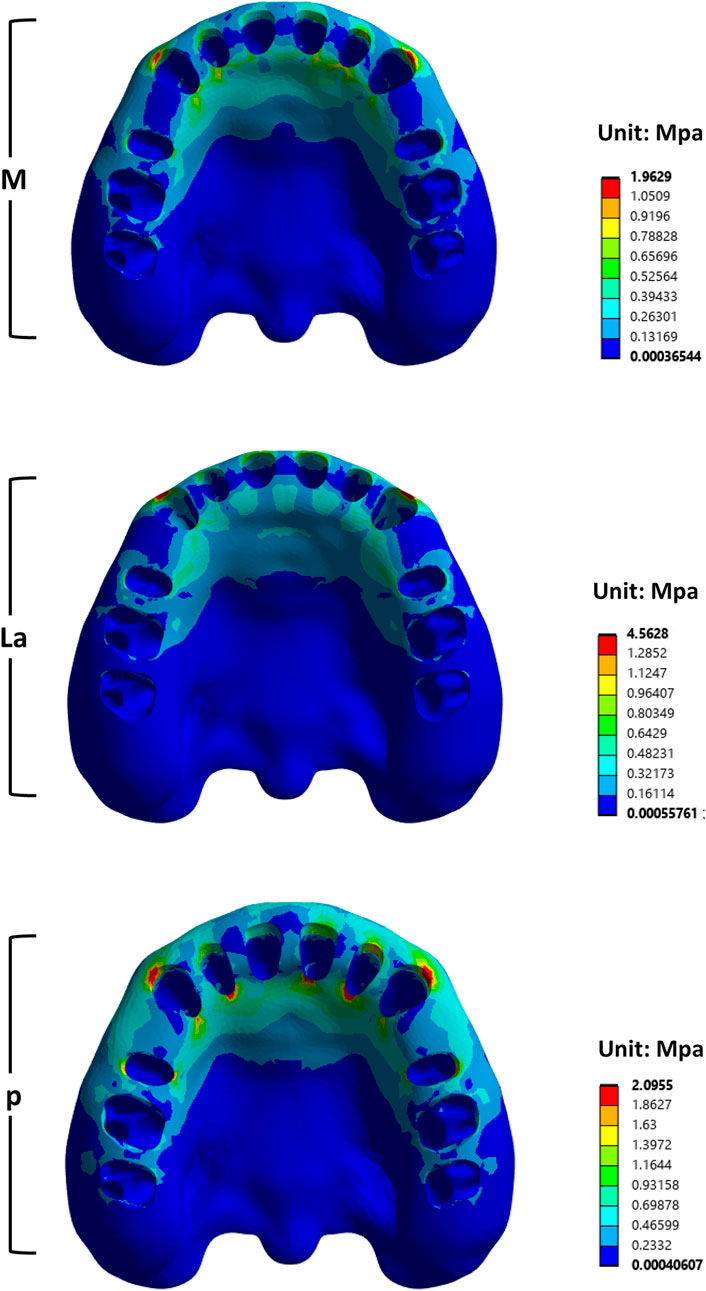
For the alveolar bone, stress was significantly concentrated on the labial alveolar wall of the canine (Figure 10). The La groups showed the highest stress among the three.
4 Discussion
This FEA found that during anterior tooth retraction using CAs without attachments or additional forces, teeth exhibited tilting with opposing crown and root movements. Maxillary central incisors demonstrated lingual tipping, extrusion, and slight distal movement, with lateral incisors and canines showing similar patterns. The inclination of anterior teeth results from the resultant force of CAs missing the center of resistance (CR), generating rotational moments. (Theodorou et al., 2019; Geramy et al., 2022; Jacob et al., 2024). The CR of maxillary central incisors is located approximately 6–8 mm apical to the crest along the tooth’s long axis, as confirmed by Viecilli et al. through 3D analysis. (Viecilli et al., 2013). However, CAs envelop the crown, applying forces far from the CR, generating moments. (Elshazly et al., 2022; Li et al., 2024; Aminian et al., 2024). Consequently, bodily retraction of anterior teeth in extraction cases is nearly unachievable using CAs. (Kang et al., 2023). Previous FEA studies identified a roller-coaster effect in the maxillary and mandibular arches during extraction space closure and reported significant lingual inclination and extrusion of anterior teeth without power ridge designs. (Liu, 2023; Meng et al., 2023).
Furthermore, among groups with different sagittal root positions (SRPs), the La groups exhibited the most pronounced anterior tooth tilting. Due to minimal labial bone resistance, labial crown movement exceeded root apex movement, resulting in greater retraction (Figure 11). The P groups showed minimal anterior tooth movement and optimal torque control, due to palatal cortical bone anchorage. Ricketts notes that dense cortical bone provides robust anchorage, with root contact against cortical bone enhancing stability. (Ricketts, 1976). The M groups displayed tilting similar to the P groups but with slightly inferior anterior anchorage control, both outperforming the La groups. Variations in SRP ultimately altered the rotation axis, causing variable displacement. A more labial SRP shifts the sagittal rotation center closer to the palatal side, as shown in Figure 11.
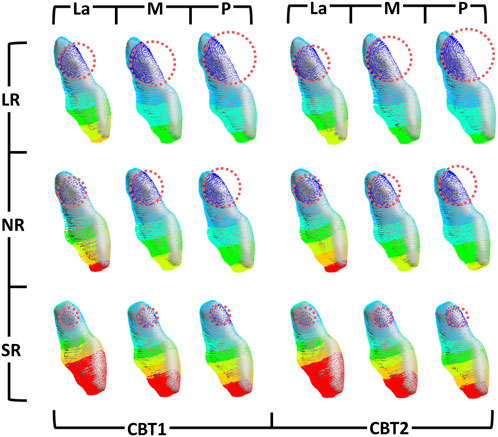
Figure 11. Mesial view of the initial tooth movement tendencies of the maxillary central incisor with varying SRP/RL/CBT. Rotation centers were approximated by visual best-fit.
Posterior teeth, although not intended to move, displayed mesial crown tipping and distal root tipping. Mesial movement in posterior teeth was less than distal movement in anterior teeth due to larger root surface area, indicating moderate molar anchorage in extraction cases. Among posterior teeth, the second premolar exhibited the most pronounced mesial crown tipping, while the first molar showed the least. This was due to inadequate aligner rigidity at the extraction site, which compromised force transmission and shape retention during retraction. (Dai et al., 2021; Upadhyay and Arqub, 2022). Among groups with different SRPs, the P groups experienced the greatest posterior anchorage loss, characterized by mesial movement and crown tipping. This was consistent with the finding that the P groups showed minimal anterior tooth displacement.
Shorter root led to greater tilting. Figure 11 illustrates vertical changes in the rotation center of maxillary central incisors with varying RLs across groups. Similarly, Figure 5 shows the SR group’s rotation axis line intersecting the horizontal axis closest to the root, indicating a rotation axis nearest the apex. Prior research has shown that in short-rooted teeth, the center of resistance is nearer to the crown, increasing the likelihood of uncontrolled moments from applied forces (Jinrui et al., 2023). With the center of resistance closer to the crown in short-rooted teeth, the rotation axis shifts toward the apex, heightening the risk of lingual tipping and crown extrusion during retraction.
This study modeled CBTs of 1 mm and 2 mm, controlling for consistent alveolar bone thickness. Although CBT did not significantly affect the magnitude of initial tooth displacement in this model, it functioned as a critical mechanical boundary condition. A trend was observed whereby thinner cortical bone (1 mm) increased periodontal ligament stress. However, our positive findings were derived from anterior retraction under two CBT conditions. Consequently, these results should not be extrapolated to other tooth movements—such as extrusion, intrusion, or torque correction—where root-to-cortex proximity may exert a far greater influence. At present, the effect of CBT on these unexplored types of tooth movement remains essentially unknown and must be investigated under dynamic or prolonged loading.
Von Mises stress quantifies PDL stress distribution, revealing stress concentrations. Excessive stress may cause PDL ischemia and root resorption, while insufficient stress reduces movement efficiency. (Li et al., 2021). This study found stress concentrations at the root apices and cervical regions of anterior teeth in all groups, most notably in the La groups. The La groups exhibited the highest von Mises stress due to greater root displacement compared to other groups. The P groups showed high PDL stress due to resistance from palatal cortical bone, restricting movement. Movement within cancellous bone, the M groups’ pattern, reduced root resorption risk. Shorter roots increased von Mises stress, as shown in Figure 8. In short-rooted teeth, a 1:0.8 crown-root ratio increases tipping and root resorption risk compared to 1:1.1 and 1:1.3 ratios, requiring slower retraction and intrusion to prevent bone fenestration or dehiscence.
In clinical practice, to effectively close extraction spaces, orthodontists must maintain proper incisor torque and molar anchorage control to achieve an optimal cusp-fossa relationship. (Zhu et al., 2023). Molar anchorage requirements vary among orthodontic patients, based on both the ideal sagittal positions of the incisors and the patient’s dental and periodontal conditions.
Cases requiring substantial retraction typically necessitate strong molar anchorage designs to prevent anterior torque loss and maintain the sagittal position of posterior teeth. This study found that the optimal pre-retraction state is a crown-root ratio not exceeding 1.1 (the NR group), with roots upright in cancellous bone and not contacting labial or palatal cortical bone. While this ideal condition may not be achievable in all patients, orthodontists can optimize outcomes through personalized designs. For patients with a labial SRP, maintaining anterior torque is the primary challenge during retraction. These cases often show poor predictability, particularly with pre-existing lingual tipping or deep overbite. Clinical strategies include applying additional torque, stepwise and overcorrected intrusion designs, or using retention attachments may prevent lingual tipping and deep overbite during extraction space closure. (Zhang et al., 2024; Kang et al., 2023; Liu, 2023). However, reduced labial alveolar bone resistance may increase the risk of bone fenestration or dehiscence, necessitating precise force control. (Li et al., 2025; Sun et al., 2021). Excessive initial stress in aligners should be managed cautiously to avoid exceeding cortical bone limits. (Jacob et al., 2024; Upadhyay and Arqub, 2022). For patients with a palatal SRP, strong posterior anchorage designs are unsuitable, as maintaining the sagittal position of posterior teeth is challenging. Anterior cortical bone anchorage increases periodontal ligament stress on anterior teeth when posterior anchorage is excessively enhanced, elevating root resorption risk.
In cases with minimal or moderate anchorage, posterior teeth may move mesially, but mesial tipping should be prevented. Strategies to prevent posterior mesial tipping include Class II traction, power arms, or proactive anchorage preparation. (Qiang et al., 2025; Ahmed et al., 2019; Wang et al., 2022). If significant posterior tipping occurs, auxiliary techniques such as sectional arches may be necessary. (Caldas et al., 2014). The primary focus in these cases is to prevent anterior tooth fenestration, dehiscence, and root resorption. Contact between anterior roots and palatal cortical bone should be avoided, especially when the SRP is palatally located. Using palatal cortical bone as anchorage is not recommended, even in cases with minimal or moderate anchorage.
For patients with shorter roots, orthodontists should evaluate baseline conditions such as SRP. This helps determine whether extraction treatment is suitable, minimizing risks of torque loss, anchorage failure, and further root resorption. Although PDL stress in short-rooted teeth remains below clinical limits in this study, orthodontists should reduce step distances, or adjust power ridge depth to minimize resorption.
Moreover, Patients with thinner cortical bone may experience more pronounced undesired tooth movement and higher periodontal-ligament stresses; consequently, smaller step distances are required to prevent torque loss, bone fenestration, or dehiscence.
It should be noted that in clinical practice, the condition of patients’ tooth roots and alveolar bone may change between initial diagnosis and after the stage of alignment and leveling. To ensure safe tooth movement within the alveolar bone, the position of tooth roots within the alveolar bone must be evaluated before anterior retraction. (Barootchi et al., 2020; Rekhi et al., 2020). Clinical examination can confirm the sagittal root position, alveolar bone thickness, and presence of root resorption, with cone-beam computed tomography (CBCT) imaging employed when necessary.
Limitations: This FEA study has limitations. The complexity of tooth geometry and periodontal tissues makes simulating aligner-tooth interactions challenging, with variations across individuals and teeth. The model does not address biological processes like PDL changes or bone and gingival remodeling This static FEA captures only immediate stress, not the cumulative, time-dependent root-resorption risk that arises from prolonged loading and individual biology. Validation through animal or clinical studies is necessary, as FEA alone is insufficient. Future research should develop optimized FEA models and conduct clinical validations.
5 Conclusion
In this finite element analysis study, the effects of different root/cortical bone relation (with varying RL, CBT, and SRP) on anterior tooth retraction in clear aligner therapy (CAT) with premolar extraction were evaluated. The following conclusions were drawn:
1. Premolar extraction space closure via CAT caused distal and lingual movement with extrusion of maxillary central incisors.
2. SRP and RL significantly affect tooth movement and stress distribution during anterior tooth retraction with CAs in extraction cases, while CBT has minimal impact in tooth movement.
3. The ideal pre-retraction condition is a crown-to-root ratio no more than 1.1, with the root upright in the cancellous bone, avoiding contact with the labial or palatal cortical bone.
4. For patients with SRP on the labial side, additional labial torque on anterior teeth is required to prevent bone fenestration or dehiscence.
5. For patients with SRP on the palatal side, care should be taken to prevent root resorption due to excessive stress on PDL of anterior teeth.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author contributions
YD: Data curation, Formal Analysis, Methodology, Writing – original draft. YaW: Investigation, Validation, Visualization, Writing – review and editing. ZY: Investigation, Writing – review and editing. WG: Formal Analysis, Software, Writing – original draft. MG: Formal Analysis, Software, Validation, Writing – original draft. YoW: Data curation, Software, Writing – original draft. YH: Project administration, Supervision, Writing – review and editing. LZ: Conceptualization, Funding acquisition, Resources, Writing – review and editing.
Funding
The authors declare that financial support was received for the research and/or publication of this article. This study is supported by Chongqing Medical Scientific Research Project (CSTB2023NSCQ-MSX0233); Chongqing Talent Program: Innovative leading talents (Medical field, CQYC20210303384); Chongqing Medical Scientific Research Project (2018ZDXM020).
Acknowledgements
Authors would like to thank LZ’s team for its assistance in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fbioe.2025.1717813/full#supplementary-material
Abbreviations
CBCT, Cone-beam computed tomography; CAT, clear aligner treatment; CA, clear aligner; PDL, periodontal ligament; FEA, Finite Element Analysis; SRP, sagittal root position, RL, root length, CBT, cortical bone thickness.
References
Adel, S. M., Hansa, I., and Vaid, N. R. (2023). “Clear Aligner Therapy in Contemporary Orthodontics: a Scoping Review of Scholarly Literature.”. APOS Trends Orthod. 14 (April), 3–27. doi:10.25259/apos_215_2022
Ahmed, N., Megalan, P., Suryavanshi, S., Sidiqha, N., and Neelakantappa, K. K. (2019). Effect of Bracket Slot and Archwire Dimension on Posterior Tooth Movement in Sliding Mechanics: a Three-Dimensional Finite Element Analysis. Cureus 11 (9), e5756. doi:10.7759/cureus.5756
Aminian, A., Garino, F., Castroflorio, T., and Younessian, F. (2024). Biomechanics of Tooth Rotation in Clear Aligner Therapy. seminars in orthodontics, ahead of print doi:10.1053/j.sodo.2024.10.005
Bae, S.-M., Kim, H.-J., and Kyung, H.-M. (2018). Long-term changes of the anterior palatal alveolar bone after treatment with bialveolar protrusion, evaluated with computed tomography. Eval. Comput. Tomogr. Am. J. Orthod. Dentofac. Orthop. 153 (1), 108–117. doi:10.1016/j.ajodo.2016.09.034
Barone, S., Paoli, A., Razionale, A. V., and Savignano, R. (2017). Computational design and engineering of polymeric orthodontic aligners. Int. J. Numer. Methods Biomed. Eng. 33 (8), e2839. doi:10.1002/cnm.2839
Barootchi, S., Lorenzo, T., Giovanni, Z., Giannobile, W. V., and Wang, H.-L. (2020). Gingival phenotype modification therapies on natural teeth: a network meta-analysis. J. Periodontology 91 (11), 1386–1399. doi:10.1002/JPER.19-0715
Caldas, G. F. R. S., Antonio Ribeiro, A., Simplício, H., and Machado, A. W. (2014). Segmented arch or continuous arch technique? A rational approach. Dent. Press J. Orthod. 19 (2), 126–141. doi:10.1590/2176-9451.19.2.126-141.sar
Chambrone, L., and Avila-Ortiz, G. (2021). An evidence-based system for the classification and clinical management of non-proximal gingival recession defects. J. Periodontology 92 (3), 327–335. doi:10.1002/JPER.20-0149
Coşkun, İ., and Kaya, B. (2019). Relationship between Alveolar Bone Thickness, Tooth Root Morphology, and Sagittal Skeletal Pattern: a Cone Beam Computed Tomography Study. J. Orofac. Orthop. 80 (3), 144–158. doi:10.1007/s00056-019-00175-9
Dai, F.-F., Xu, T.-M., and Shu, G. (2019). Comparison of achieved and predicted tooth movement of maxillary first molars and central incisors: first premolar extraction treatment with Invisalign. Angle Orthod. 89 (5), 679–687. doi:10.2319/090418-646.1
Dai, F.-F., Xu, T.-M., and Shu, G. (2021). Comparison of achieved and predicted crown movement in adults after 4 first premolar extraction treatment with invisalign. Am. J. Orthod. Dentofac. Orthop. 160 (6), 805–813. doi:10.1016/j.ajodo.2020.06.041
Davy, D. T., Dilley, G. L., and Krejci, R. F. (1981). Determination of stress patterns in root-filled teeth incorporating various dowel designs. J. Dent. Res. 60 (7), 1301–1310. doi:10.1177/00220345810600070301
Elshazly, T. M., Keilig, L., Salvatori, D., Chavanne, P., Aldesoki, M., and Bourauel, C. (2022). Effect of trimming line design and edge extension of orthodontic aligners on force transmission: an in vitro study. J. Dent. 125 (October), 104276. doi:10.1016/j.jdent.2022.104276
Geramy, A., Reza Geramy, A., and Fazli, B. (2022). An expansion to the Nägerl’s theory of proportionality in reduced alveolar bone height models: a 3D finite element analysis. BMC Oral Health 22 22, 434. doi:10.1186/s12903-022-02476-9
Gomez, J. P., Peña, F. M., Martínez, V., Giraldo, D. C., and Cardona, C. I. (2015). Initial force systems during bodily tooth movement with plastic aligners and composite attachments: a three-dimensional finite element analysis. Angle Orthod. 85 (3), 454–460. doi:10.2319/050714-330.1
Hong, Y.-Ya, Kang, T., Zhou, M. Q., Zhong, J. Y., and Chen, X. P. (2024). Effect of varying auxiliaries on maxillary incisor torque control with clear aligners: a finite element analysis. Am. J. Orthod. Dentofac. Orthop. 166 (1), 50–60. doi:10.1016/j.ajodo.2024.02.012
Jacob, B. H., Gonçalves Azeredo, R., and Spreafico, C. S. (2024). Biomechanical considerations for tooth movement and strategies to avoid undesirable side seminars in orthodontics. Manag. Complex Malocclusions 30 (5), 557–571. doi:10.1053/j.sodo.2024.02.006
Jinrui, Xu, Zihan, W., and Jing, N. (2023). 2023. Research progress of crown -Root ratio in orthodontics. Front. Med. Sci. Res. 5 (1). doi:10.25236/FMSR.050116
Kang, F., Wu, Y., Cui, Y., Yuan, J., Hu, Z., and Zhu, X. (2023). The displacement of teeth and stress distribution on periodontal ligament under different upper incisors proclination with clear aligner in cases of extraction: a finite element study. Prog. Orthod. 24 (1), 38. doi:10.1186/s40510-023-00491-2
Knop, L., Gonzaga Gandini, L., Lima Shintcovsk, R., and Regina, M. (2015). Scientific use of the finite element method in orthodontics. Sci. Use Finite Elem. Method Orthod. Dent. Press J. Orthod. 20 (2), 119–125. doi:10.1590/2176-9451.20.2.119-125.sar
Li, Y., Zhan, Qi, Bao, M., Yi, J., and Li, Yu (2021). Biomechanical and biological responses of periodontium in orthodontic tooth movement: Up-Date in a new decade. Int. J. Oral Sci. 13 (1), 20. doi:10.1038/s41368-021-00125-5
Li, J., Si, J., Xue, C., and Xu, H. (2024). Seeking orderness out of the orderless movements: an up-to-date review of the biomechanics in clear aligners. Prog. Orthod. 25 (1), 44. doi:10.1186/s40510-024-00543-1
Li, Y., Huang, J., Fan, Z., Han, M., Gu, Y., Li, D., et al. (2025). Changes in alveolar bone remodeling after maxillary anterior retraction using fixed appliances with different periodontal conditions: a retrospective study based on cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 168 (1), 99–109. doi:10.1016/j.ajodo.2025.02.013
Liang, W., Rong, Q., Lin, J., and Xu, B. (2009). Torque control of the maxillary incisors in lingual and labial orthodontics: a 3-Dimensional finite element analysis. Am. J. Orthod. Dentofac. Orthop. 135 (3), 316–322. doi:10.1016/j.ajodo.2007.03.039
Liu, J.-qi, Zhu, G. y., Wang, Y. g., Zhang, B., Yao, K., and Zhao, Z. h. (2023). Different biomechanical effects of clear aligners in closing maxillary and mandibular extraction spaces: finite element analysis. Am. J. Orthod. Dentofac. Orthop. 163 (6), 811–824.e2. doi:10.1016/j.ajodo.2022.07.021
Lyu, X., Cao, X., Yan, J., Zeng, R., and Tan, J. (2023). Biomechanical effects of clear aligners with different thicknesses and gingival-margin morphology for appliance design optimization. Am. J. Orthod. Dentofac. Orthop. 164 (2), 239–252. doi:10.1016/j.ajodo.2022.12.014
Mao, B., Tian, Y., Xiao, Y., Liu, J., Liu, D., Li, J., et al. (2024). Biomechanical effects of clear aligner with different shape design at extraction space area during anterior teeth retraction. Orthod. and Craniofacial Res. 27 (5), 740–749. doi:10.1111/ocr.12795
Meng, X., Wang, C., Xu, W., Wang, R., Zheng, L., Wang, C., et al. (2023). Effects of different designs of orthodontic clear aligners on the maxillary central incisors in the tooth extraction cases: a biomechanical study. BMC Oral Health 23, 416. doi:10.1186/s12903-023-03106-8
Miyama, W., Uchida, Y., Motoyoshi, M., Motozawa, K., Kato, M., and Shimizu, N. (2018). Cone-beam computed tomographic evaluation of changes in maxillary alveolar bone after orthodontic treatment. J. Oral Sci. 60 (1), 147–153. doi:10.2334/josnusd.17-0151
Qian, Y., Tang, Z., Chen, Y., Song, W., Zhao, Z., Zheng, W., et al. (2024). The ‘roller Coaster Effect’ in premolar extraction cases: clear aligners vs. straight-wire appliance. Eur. J. Orthod. 47 (1), cjae072. doi:10.1093/ejo/cjae072
Qiang, R., Wu, J., Gao, J., Chen, H., Xu, J., Jin, Z., et al. (2025). An integrated approach to posterior Anchorage preparation and incisor torque compensation in premolar extraction cases using clear aligners. BMC Oral Health 25 (1), 558. doi:10.1186/s12903-025-05945-z
Rekhi, U., Queiroz Catunda, R., and Gibson, M. P. (2020). Surgically accelerated orthodontic techniques and periodontal response: a systematic review. Eur. J. Orthod. 42 (6), 635–642. doi:10.1093/ejo/cjz103
Ricketts, R. M. (1976). Bioprogressive therapy as an answer to orthodontic needs part II. Part II. Am. J. Orthod. 70 (4), 359–397. doi:10.1016/0002-9416(76)90111-1
Rodrigues, D. M., Petersen, R. L., Montez, C., JoséDe Moraes, R., Ferreira, V., and Barboza, E. P. (2023). The relationship between tomographic sagittal root position of maxillary anterior teeth and the bone housing. J. Prosthet. Dent. 130 (5), 705–714. doi:10.1016/j.prosdent.2021.10.006
Singh, D., Fatima, K., Gandhi, A., Tripathi, T., and Rai, P. (2024). Finite element Analysis-A biomechanical tool in orthodontics. IP Indian J. Orthod. Dentofac. Res. 10 (1), 11–15. doi:10.18231/j.ijodr.2024.003
Sun, Z.-T., Wang, Y.-C., Cui, Y.-M., and Sun, Y. (2019). Finite element analysis of maxillary anterior teeth retraction of posterior teeth with different alveolar bone absorption heights under orthodontic force. Hua Xi Kou Qiang Yi Xue Za Zhi = Huaxi Kouqiang Yixue Zazhi = West China J. Stomatology 37 (3), 265–269. doi:10.7518/hxkq.2019.03.007
Sun, Q., Lu, W., Zhang, Y., Peng, L., Chen, Si, and Han, B. (2021). Morphological changes of the anterior alveolar bone due to retraction of anterior teeth: a retrospective study. Head and Face Med. 17 (July), 30. doi:10.1186/s13005-021-00277-z
Tanne, K., Sakuda, M., and Burstone, C. (1987). Three-dimensional finite element analysis for stress in the periodontal tissue by orthodontic forces. Am. J. Orthod. Dentofac. Orthop. 92, 499–505. doi:10.1016/0889-5406(87)90232-0
Theodorou, C. I., Anne Marie Kuijpers-JagtmanBronkhorst, E. M., FrankWagener, A. D. T. G., and Wagener, F. A. (2019). Optimal force magnitude for bodily orthodontic tooth movement with fixed appliances: a systematic review. Am. J. Orthod. Dentofac. Orthop. 156 (5), 582–592. doi:10.1016/j.ajodo.2019.05.011
Upadhyay, M., and Arqub, S. A. (2022). Biomechanics of clear aligners: Hidden truths and first principles. J. World Fed. Orthod. 11 (1), 12–21. doi:10.1016/j.ejwf.2021.11.002
Viecilli, R. F., Budiman, A., and Burstone, C. J. (2013). Axes of resistance for tooth movement: does the center of resistance exist in 3-Dimensional space. Am. J. Orthod. Dentofac. Orthop. 143 (2), 163–172. doi:10.1016/j.ajodo.2012.09.010
Wang, Q., Dai, D., Wang, J., Chen, Y., and Zhang, C. (2022). Biomechanical analysis of effective mandibular En-Masse retraction using class II elastics with a clear aligner: a finite element study. Prog. Orthod. 23 (July), 23. doi:10.1186/s40510-022-00417-4
Wang, Ya, Daraqel, B., Wang, Y., Yang, D., Dong, Y., Hu, Y., et al. (2024). Biomechanical effects of different mandibular movements and torque compensations during mandibular advancement with clear aligners: a finite element analysis. Front. Bioeng. Biotechnol. 12, 1496517. doi:10.3389/fbioe.2024.1496517
Yagci, A., İlknur, V., Uysal, T., Izzet Ucar, F., Ozer, T., and Enhos, S. (2011). Dehiscence and fenestration in skeletal class I, II, and III malocclusions assessed with cone-beam computed tomography. Angle Orthod. 82 (1), 67–74. doi:10.2319/040811-250.1
Zhang, Y., Wang, K., Li, M., Liu, C., Tang, L., Wan, C., et al. (2024). Effects of different intrusion patterns during anterior teeth retraction using clear aligners in extraction cases: an iterative finite element analysis. Front. Bioeng. Biotechnol. 12, 1388876. doi:10.3389/fbioe.2024.1388876
Zhou, C., Feng, Z., Ren, J., Luo, H., Ieong, H. C., Li, R., et al. (2025). The effects of clinical crown length on the sagittal movement of maxillary central incisor in clear aligner treatment: a finite element exploration. BMC Oral Health 25 (1), 357. doi:10.1186/s12903-025-05726-8
Zhu, G.-yin, Zhang, Bo, Yao, Ke, Lu, W. x., Peng, J. j., Shen, Y., et al. (2023). Finite element analysis of the biomechanical effect of clear aligners in extraction space closure under different Anchorage controls. Am. J. Orthod. Dentofac. Orthop. 163 (5), 628–644.e11. doi:10.1016/j.ajodo.2022.02.018
Keywords: finite element study, clear aligner, root/cortical bone relation, sagittal rootposition, tooth movement, space closure
Citation: Dong Y, Wang Y, Yang Z, Gong W, Guo M, Wu Y, Hu Y and Zheng L (2025) Biomechanical effects of root/cortical bone relation on tooth movement during premolar-extraction space closure with clear aligners: a finite element study. Front. Bioeng. Biotechnol. 13:1717813. doi: 10.3389/fbioe.2025.1717813
Received: 02 October 2025; Accepted: 07 November 2025;
Published: 19 November 2025.
Edited by:
Alessandro Ruggiero, University of Salerno, ItalyCopyright © 2025 Dong, Wang, Yang, Gong, Guo, Wu, Hu and Zheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yun Hu, NTAwMTg4QGhvc3BpdGFsLmNxbXUuZWR1LmNu; Leilei Zheng, emhlbmdsZWlsZWljcW11QGhvc3BpdGFsLmNxbXUuZWR1LmNu
 Yihan Dong1,2,3,4
Yihan Dong1,2,3,4 Yun Hu
Yun Hu Leilei Zheng
Leilei Zheng