- 1Department of Biomedical Informatics, College of Medicine, The Ohio State University, Columbus, OH, United States
- 2Department of Strategic Communication, Edward R. Murrow College of Communication, Washington State University, Pullman, WA, United States
Introduction: Given the low patient portal adoption rates, the contradictory findings on the relationship between patient-provider communication and patient portal use, and the unclear mechanism of why doctor-patient communication might facilitate portal use as indicated in some existing studies, patient portal engagement warrants further examination.
Methods: Guided by the behavior change wheel framework and the channel expansion theory, this study examined the facilitators of patient portal engagement and tested the relationship between the facilitators (e.g., social opportunity and psychological capability) through analyzing the HINTS national survey data (N = 1251).
Results: We found that patient portal access (a physical opportunity) and physician advocacy (a social opportunity) were two significant predictors of portal engagement while educational attainment was not. We did not find any direct correlation between patient-centered communication (PCC) and patient portal engagement, but instead, found a significant indirect relationship between the two.
Discussion: To the best of our knowledge, this is the first study to employ the behavior change wheel and channel expansion theory to explain patient portal engagement. Theoretically, our study extended the behavior change theory by further explaining the relationship between the key components (e.g., capability, opportunity) of behavior change. Practical strategies to increase patient portal engagement were proposed.
Introduction
A patient portal is a secure online website that patients can use (e.g., to access personal health record) 24/7 from anywhere with Internet coverage (The Office of the National Coordinator for Health Information Technology, 2017). Despite the various potential benefits of patient portals (e.g., enhancing information sharing, improving patient safety, facilitating patient-provider communication, facilitating disease self-management, and empowering patients) (Miller et al., 2016; Rathert et al., 2017; Ammenwerth, 2018; Dendere et al., 2019), and despite the electronic health record (EHR) incentive programs to advocate and promote the meaningful use of EHRs to improve patient care (Ricciardi et al., 2013; Centers for Medicare and Medicaid Services, 2023), patient portal adoption rates have remained low, ranging from 37 to 54% (Anthony et al., 2018; Turner et al., 2020; Wright et al., 2022).
Among the empirical studies that have examined the facilitators of and barriers to online patient portal use, some conflicting results have been observed. For instance, some studies (e.g., Tieu et al., 2015) indicated that patient-provider communication is a facilitator while other studies (e.g., Zaidi et al., 2022) did not find such a significant relationship. The most prevalent barrier of portal use indicated by portal nonusers was the preference for in-person communication with providers (Anthony et al., 2018; Turner et al., 2020).
Even if patient-provider communication has a facilitating role, the mechanism of why the interpersonal communication (i.e., doctor-patient communication) can facilitate the computer- or technology-mediated communication (i.e., patient portal use) is unclear. Given the low patient portal adoption rates, the contradictory findings on the relationship between patient-provider communication and patient portal use, and the unclear mechanism of why doctor-patient communication might facilitate portal use as indicated in some existing studies, online patient portal use or engagement warrants further examination.
Guided by the behavior change wheel framework (Michie et al., 2011), the current research proposes that psychological capability (e.g., education attainment), physical opportunity (e.g., portal access), and social opportunity (e.g., physician advocacy) likely affect patients' levels of engagement in portal use. Also guided by the channel expansion theory (Carlson and Zmud, 1999), the current research proposes that patient-centered communication (PCC) likely affects portal engagement indirectly through levels of easiness in understanding the health information in patient portals. Therefore, the goals of the study are: (1) to test whether or not educational attainment, patient portal access, or physician advocacy predicts patient portal engagement, and (2) to find out the relationship between PCC and patient portal engagement.
Literature review
Functions of patient portals
Patient portals serve different functions. Basic functions include allowing patients to access their own medical information, such as medical history and records, immunizations, recent office visits. Other more advanced functions include enabling patients to schedule appointments, and exchange messages with healthcare their provider (Kruse et al., 2015). Some researchers have systematically reviewed the commonly shared functions among various patient portals. Bao et al. (2020) classified patient portal functions into two categories: clinical function and administrative function. Clinical function refers to outcomes that are directly related to patients' physical and mental health, such as viewing test results, messaging with health providers, scheduling an appointment. Administrative function is about how portal reduces the administrative burden on patients and health providers, such as updating insurance, resolving claims. Steitz et al. (2019) made a more detailed classification of patient portal's functions, which includes appointment, billing, document access, genetics, health results, immunization, medication, and messaging.
Patient portal engagement
Patient engagement is the process that patients themselves serve as an active member of the health care team and then build and maintain collaborative partnerships with health providers and provider organizations (Maurer et al., 2012). Patient portal engagement is a multi-step process, which goes from shallow to deep. Zhou et al. (2022) developed the patient portal engagement framework (PPEF) which summarized four levels of engagement: informing patients; involving patients; partnering with patients; and supporting ecology of care. Going through these four stages, a patient's role evolves from a passive information recipient to an active partner who collaborates with health providers. Portal engagement can generate some positive outcomes such as increasing medication adherence (Sarkar et al., 2014), empowering patients (Ammenwerth, 2018), reducing duplicate testing (Wakefield et al., 2020), significantly reducing patients' hospital visit times, and eventually decreasing hospitalization costs (Bao et al., 2020). However, though with various portal functions and the potential benefits, the adoption rates of patient portal, at least in the U.S., have remained low (Anthony et al., 2018; Turner et al., 2020). Given the low engagement rates, it is imperative to find out potential barriers to and facilitators of patient portal engagement.
The behavior change wheel and patient portal engagement
The behavior change wheel framework (Michie et al., 2011) can be used to systematically examine the facilitators of and barriers to patient portal engagement. According to the behavior change wheel (Michie et al., 2011, 2014), in order for the behavior of online patient portal engagement to happen, capability, opportunity, and motivation are necessary conditions (Michie et al., 2011). Capability includes physical capability (i.e., the physical skills or strength needed to perform a behavior) and psychological capability (i.e., the psychological skills or knowledge needed to engage in a behavior) (Michie et al., 2011). Patients with higher educational attainment will likely have more knowledge and skills needed for patient portal use. Studies indicated that education level (an example of psychological capability) (Sarkar et al., 2011; Osborn et al., 2013; Ancker et al., 2015; Sun et al., 2019) was a significant predictor of portal engagement. Therefore, we hypothesize that:
H1(a) educational attainment will predict patient portal engagement.
Motivation includes automatic motivation (i.e., automatic processes without much deliberate thoughts, such as wants and needs, impulses and emotions) and reflective motivation (i.e., reflective processes involving deliberate thoughts and mental processing, such as intentions and evaluations) (Michie et al., 2011). Lack of awareness or motivation (Goel et al., 2011; Turner et al., 2020) can inhibit a patient's portal use. Patients with stronger health emotions (an example of automatic motivation), and openness to new experiences (an example of reflective motivation) are more likely to use patient portals (Moqbel et al., 2020).
Opportunity includes physical opportunity (i.e., the physical environment external to an individual, such as resources, access) and social opportunity (i.e., the social environment and interpersonal relations that are supposed to influence people' perceptions of a behavior) (Michie et al., 2011). High income (an example of physical opportunity) was a facilitator of portal engagement (Ketterer et al., 2013; Osborn et al., 2013; Sun et al., 2019) while not having access to computer (another example of physical opportunity) is a barrier for patients' portal engagement (Osborn et al., 2013). Other factors related to physical opportunity were also mentioned in the existing literature. For instance, the levels of comprehensiveness of health data on patient portals (Fujioka et al., 2021) influence portal engagement whereas portal design features (Lazard et al., 2016) can influence portal acceptance by patients. Based on the definition, having access to online patient portal is a physical opportunity. Patients indicated that no patient portal access and lack of Internet access were barriers to patient portal use (Turner et al., 2020). Therefore, having access to online patient portal is likely to be a facilitator of portal engagement. We hypothesize that:
H1(b) patient portal access will predict patient portal engagement.
Provider advocacy of portal use is a social opportunity that has the potential to facilitate portal use. Some physicians do not hold a positive attitude toward a patient portal since they think it generates more workload (Miller et al., 2016). However, health providers' support can influence patients' trust on a portal (Goel et al., 2011). Providers can communicate the potential benefits of patient portals through interpersonal communication in a healthcare setting and promote the use of patient portals, which will in turn influence patients' perception of patient portals and facilitate portal engagement. The following hypothesis was proposed:
H1(c) physician advocacy of portal use will predict patient portal engagement.
Patient-provider communication and portal engagement
There are conflicting results regarding the relationship between patient-provider communication and patient portal engagement. Studies indicated that interest in the portal was predicted by dissatisfaction with the provider-patient relationship, and disinterest in the portal was predicted by satisfaction with the provider-patient relationship (Zickmund et al., 2008). National survey results indicated that preference for in-person communication with providers (Anthony et al., 2018; Turner et al., 2020) was one of the major barriers of patient portal use. While some studies (e.g., Zaidi et al., 2022) did not find a significant relationship between provider-patient communication and online portal use, some other studies (e.g., Lyles et al., 2013; Tieu et al., 2015) indicated that patient-provider communication is a facilitator of patients' online patient portal use. Patient-centered communication (PCC), a type of patient-provider communication, occurs when a provider takes a patient's needs, goals, and individual experience into consideration, gives the patient the opportunity to make decisions and participate in their care, and it will enhance doctor-patient relationship (Epstein and Street, 2007). Higher levels of PCC could make the patients feel that there is no motivation to use the portal (Zickmund et al., 2008) or could motivate patients to take care of their health by engaging in patient portal. Therefore, the following research question (RQ) was proposed:
RQ1: What is the relationship between PCC and patient portal engagement?
Portal-mediated communication vs. doctor-patient communication
Portal-mediated communication and interpersonal communication with providers have their distinctive characteristics, benefits or disadvantages, under different tasks or circumstances. First, we consider levels of synchronicity. According to media synchronicity theory (Dennis et al., 2008), it is better to use face to face communication which has the highest degree of synchronicity when a patient first sees a doctor to understand the diagnosis and discuss a treatment plan or when complex things need to be discussed. Some physicians hold that a portal was not able to handle complex communication (Laukka et al., 2020). The high immediate and interactive nature will facilitate the process to reach shared understanding of a patient's health conditions and disease management plans (Kashian and Mirzaei, 2019). Second, compared to face-to-face communication, patient portals, are mostly text based and lack of visual cues (An and Frick, 2006). Because of the lack of visual cues (e.g., body languages and gestures) that help facilitate understanding and convey emotions in patient portals, misunderstanding can happen (Slanetz et al., 2019) when patients use the portals. “Patients with advanced disease need the cues that come with direct interaction to help them along with their care” (Fuerst, 2017, para. 8). Third, portal-mediated communication lacks the ability to communicate empathy (Laukka et al., 2020). Fourth, the advantage of text-based communication is that it provides a written record of face-to-face communication (e.g., clinical notes), and information needed for patients to manage their health and coordinate healthcare (e.g., test results, patient education). Patients don't need to worry about forgetting important things in the interpersonal setting and later they have the opportunity to learn and reflect on the content provided in the portal (An and Frick, 2006). Fifth, another advantage of portal-mediated communication is that it is place and time independent (An and Frick, 2006). Patients can access their health information 24/7, with the access to the Internet and appropriate technology (e.g., smartphones).
Based on the previous discussion of the characteristics of the communication channels, according to media richness theory (Daft and Lengel, 1986), portal-mediated communication could be considered as a leaner medium, compared to face-to-face communication, because of the following four aspects: immediate feedback, multiple cues, language variety, and personal focus (Ishii et al., 2019). The perception that portal is a lean medium in medical context could be the reason of some peoples' preference of face-to-face communication and the low rates of portal adoption. However, according to the channel expansion theory (Carlson and Zmud, 1999), perceptions and attitudes of a medium and its characteristics vary across users because of a variety of factors, such as experience (Timmerman and Madhavapeddi, 2008). Experience can be specified into four categories: “(a) experience with a particular channel, (b) experience with a particular topic, (c) experience with a particular communicator, and (d) experience with particular organizational contexts” (Ishii et al., 2019, p. 125). Based on the channel expansion perspective (Carlson and Zmud, 1999), if a patient has more experience with their healthcare provider through PCC, the patient will be more familiar with the communicator (e.g., doctors) as well as the topic (e.g., health conditions). As the experience increases, their levels of the perception of the richness of the channel (i.e., patient portal) increase, and patients would likely feel easier to understand the health information on the patient portal. According to behavior change wheel (Michie et al., 2011), as patients feel easier to understand the health information on portal (i.e., the increase of psychological capability), they are more likely to engage in patient portals. Therefore, the following hypotheses were proposed:
H2. Higher levels of PCC will make patients feel easier to understand the health information on patient portal.
H3. If patients feel easier to understand health information on patient portals, they are more likely to engage in patient portals.
H4. There is a significant indirect relationship between PCC and patient portal engagement.
Methods
HINTS dataset and study population
The Health Information National Trends Survey (HINTS), developed by National Cancer Institute (n.d.), is used to collect nationally representative data to monitor and study health communication and health information technology. HINTS data are reliable and informative, and the items were carefully tested before the survey to ensure its validity (National Cancer Institute, n.d.). The data used in this study, HINTS 5 Cycle 4 (N = 3,865), were collected in 2020, and were available in 2022. HINTS data were used in this study because of its focus on patient portal use and because of its national representativeness. Patients (N = 1,251) who filled out the questions related to patient-centered communication and online patient portals were the focus of the analyses.
Instrumentation
The HINTS survey questions related to our hypotheses and research question were included in our investigation. Patient portal engagement can be measured by frequency of access (e.g., Wallace et al., 2016). Similarly, in our study, patient portal engagement was operationalized as the frequency of portal access (“How many times did you access your online medical record in the last 12 months?”). PCC was measure by seven items which have been used as PCC measures in previous studies (e.g., Totzkay et al., 2017). The questions asked how often the health professionals (e.g., doctors, nurses) did each of the processes, such as “give you the change to ask all the questions you had” and “involve you in decisions about your health care as much as you wanted.” Patient portal access was measured by asking participants: “Have you ever been offered online access to your medical records by your health care provider?” Physician advocacy was measured by the question: “Have any of your health care providers, including doctors, nurses, or office staff ever encouraged you to use an online medical record?” Educational attainment was measured by the question: “What is the highest grade or level of schooling you completed?” The level of easiness of understanding health information on patient portal was measured by the question: “How easy or difficult was it to understand the health information in your online medical record?”
Data analysis
In order to test hypotheses h1(a), h1(b), and h1(c), and answer the research question, multiple regression was used to analyze the data. Control variables included age, gender, health, race and ethnicity, household income. Gender, race, portal access, and physician advocacy were dummy coded. The mean score of the PCC items was used in the regression analysis. SPSS 27.0 (IBM Corp, 2020) was used for the regression analysis. Path analysis was used to test hypotheses 2, 3, and 4. In order to test the indirect effect, PCC was treated as a latent variable, and was the exogenous variable, the level of easiness of understanding health information on patient portal was a mediator, and portal engagement was the endogenous variable. Control variables included age, gender, health, race and ethnicity, household income. Bootstrapping technique, with the number of iterations being set to 5000, was used to obtain bias-corrected 95% confidence to test the indirect effect (Preacher and Hayes, 2008). Statistical software Mplus 8.0 (Muthén and Muthén, 2017) was employed to test the relationships.
Results
Participants' demographics
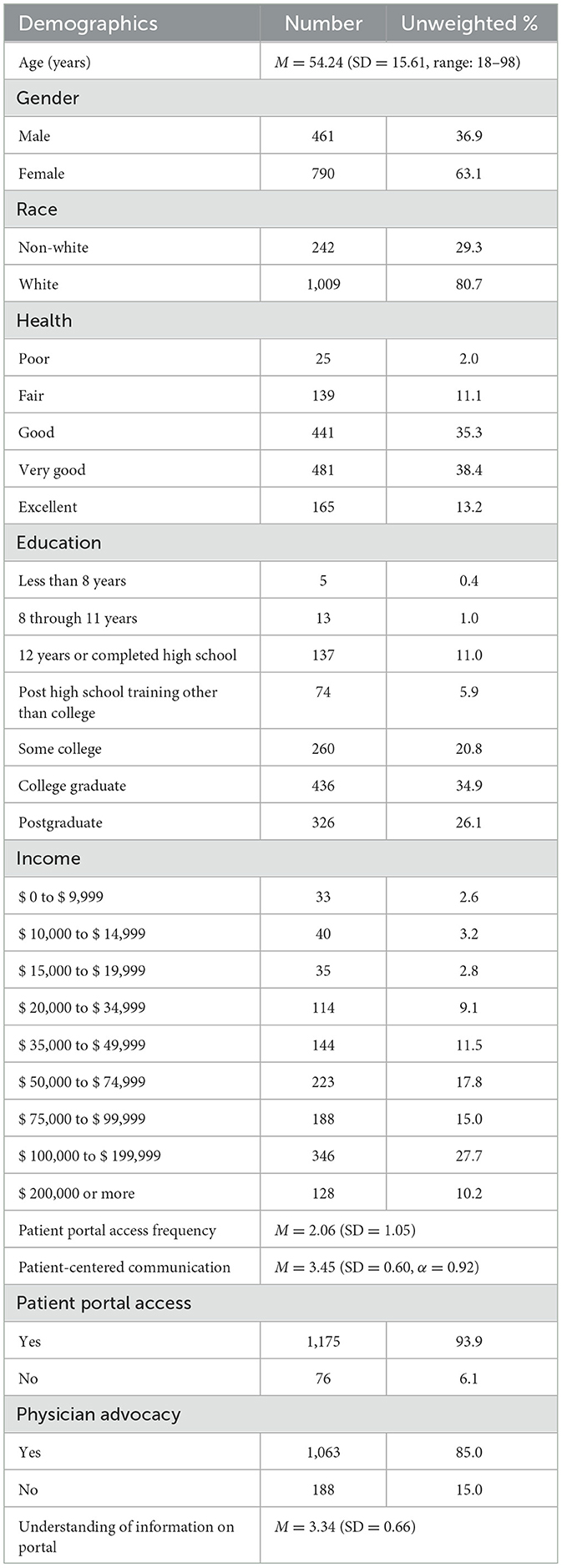
Participants' demographic characteristics were presented in Table 1. The mean age of the participants was 54.24. The majority of the participants were females (63.1%) and 80.7% of the participants were White. 38.4% of the participants reported to have very good health condition. 34.9% of the participants were college graduates.
Factors predicting patient portal engagement
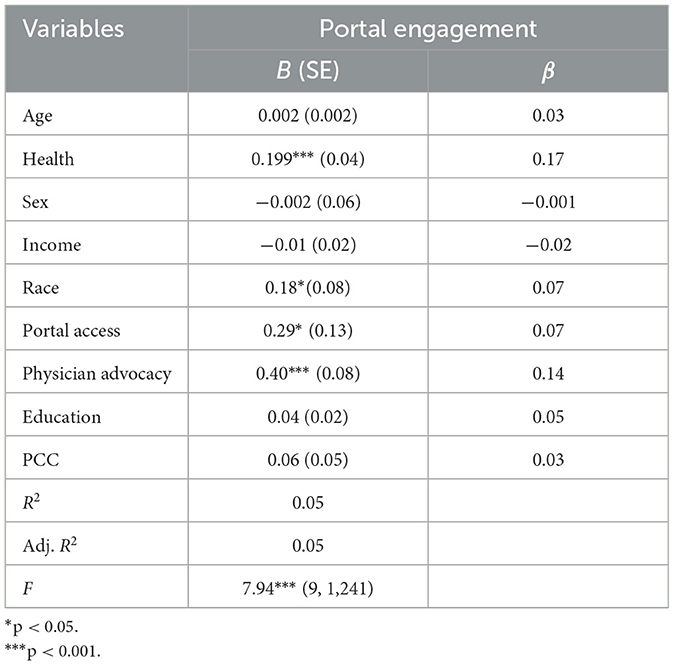
Hypotheses 1 posited that educational attainment (H1a), patient portal access (H1b), and physician advocacy (H1c) predicted patient portal engagement. As shown in Table 2, a significant proportion of variance was predicted in portal engagement, F (9,1,241) = 7.94, p < 0.001, R2 = 0.05. Patient portal access (β = 0.07, p < 0.05) and physician advocacy (β = 0.14, p < 0.001) were significant predictors of portal engagement, but educational attainment (β = 0.05, p = 0.10) was not a significant predictor of patient portal engagement. Therefore, hypotheses 1(b) and 1(c) were supported while hypothesis 1(a) was not supported. PCC was not a significant predictor (β = 0.03, p = 0.25) of portal engagement, meaning there was no direct relationship between PCC and portal engagement, and the research question was answered.
Indirect relationship between PCC and patient portal engagement
For the path analyses, the results for the overall fit of proposed model (χ2 = 411.93, df = 75, p < 0.01, RMSEA = 0.06, CFI = 0.93, TLI = 0.92, SRMR = 0.03) indicated acceptable fit to the data; although the p-value was significant. We used the following criteria to evaluate the model fit: values >0.90 for CFI and TLI, values smaller than 0.08 for RMSEA and SRMR (Browne and Cudeck, 1993; Hu and Bentler, 1998; McDonald and Ho, 2002). Higher levels of PCC (β = 0.24, p < 0.001) significantly predicted higher levels of easiness of understanding health information on patient portal. H2 was supported. Higher levels of easiness of understanding health information on patient portal (β = 0.16, p < 0.001) significantly predicted higher levels of patient portal engagement. H3 was supported. There was a significant indirect path from PCC to patient portal engagement [ES = 0.04, 95% CIs (0.02, 0.05)], and therefore, H4 was supported. The summary of the results is presented in Figure 1.
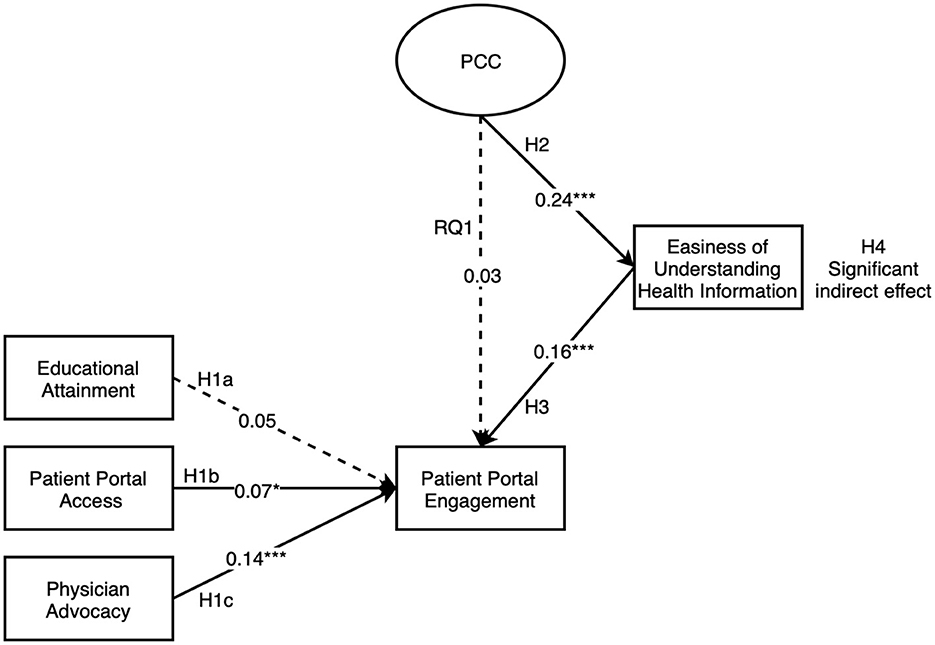
Figure 1. Summary of patient portal engagement results. *p < 0.05, ***p < 0.001; regression coefficients were standardized; dashed line represents non-significant result, solid line represents significant results.
Discussion
This study was guided by the behavior change wheel framework (Michie et al., 2011) and the channel expansion theory (Carlson and Zmud, 1999). In this study, we found that patient portal access and physician advocacy were two significant predictors of portal engagement while educational attainment was not. We did not find any direct correlation between PCC and patient portal engagement, but found a significant indirect relationship between the two.
We found that physician advocacy was a significant predictor of portal engagement. This finding is in agreement with existing studies (e.g., Amante et al., 2014; Irizarry et al., 2015; Powell, 2017). For instance, in the systematic review (Powell, 2017) on patient-perceived facilitators of and barriers to portal use, they found that provider encouragement was indicated as one of the patient-perceived facilitators. Another study (Dendere et al., 2019) indicated that a lack of provider advocacy was a barrier of portal engagement. We found that portal access was another significant predictor of portal engagement. This is in agreement with the existing studies (e.g., Ancker et al., 2017) which demonstrated that the rates of portal adoption increased as more patients were offered the portal accounts.
However, we did not find a significant relationship between education attainment and portal engagement. This was in agreement with some existing studies (e.g., Woods et al., 2017). The finding implies that people with higher education levels do not necessarily possess higher health literacy skills (Wright et al., 2022) or digital skills (Heponiemi et al., 2022) needed to understand the information on patient portals. Some studies demonstrated that low health literacy inhibits patient's portal use behavior (Baldwin et al., 2017; Hoogenbosch et al., 2018). Therefore, future studies may operationalize psychological capability necessary for patient portal engagement as health literacy and/or digital skills, rather than educational attainment.
Existing studies are not in agreement with regard to the relationship between provider patient relationship and patient portal engagement. While some studies (e.g., Zaidi et al., 2022) did not find a significant relationship between provider-patient communication and online portal use, some other studies (e.g., Tieu et al., 2015) indicated that patient-provider communication is a facilitator of patients' online patient portal use. Interestingly, we did not find a significant direct relationship between PCC and portal engagement, but found a significant indirect relationship between the two. We provided some evidence to explain how interpersonal doctor-patient communication could influence technology-mediated communication in an indirect way, using the channel expansion theory (Carlson and Zmud, 1999). Through patient-centered communication in the face-to-face setting, patients will gain a lot of experience (i.e., visual cues such as body language and gestures, ways of expressing things) that will help patients understand the physician (the communicator) and their health condition (the topic) better. This type of experience and understanding will serve as context of the subsequent portal-mediated communication to avoid potential misunderstanding. As the levels of experience increase, and as their levels of the perception of the richness of the channel (i.e., patient portal) increase, patients will find the health information on portal easier to understand, and they will be more likely to engage with the medium (i.e., portal). This implies that people's perception of a patient portal can be changed and their engagement with portal can also be changed through that mechanism; PCC will facilitate easier understanding of health information on portal which in turn promote portal engagement.
Implications for theory and practice
To the best of our knowledge, this is the first study to employ the behavior change wheel (Michie et al., 2011) and the channel expansion theory (Carlson and Zmud, 1999) to explain patient portal engagement. The two theories were employed to explain the mechanism of how interpersonal communication could influence technology-mediated communication. These findings indicated that the behavior change wheel framework (Michie et al., 2011) can be used as a guide to systematically examine the facilitators of and barriers of patient portal engagement. The three necessary components, capability, opportunity, and motivation, not only predict a behavior, but also interact with each other (Michie et al., 2011). For instance, capability and opportunity can influence motivation (Michie et al., 2011). Guided by the channel expansion theory (Carlson and Zmud, 1999), our study hypothesized the relationship between social opportunity (e.g., PCC) and psychological capability, and the indirect relationship between PCC and portal engagement. Our study provided some evidence to demonstrate that social opportunity (e.g., PCC) could influence psychological capability (e.g., perceived level of difficulty in understanding health information on patient portals) which predicts a behavior (e.g., portal engagement). In this sense, our study extended the theory by further explaining the relationship between the key components (e.g., capability, opportunity) of behavior change.
Practically, the behavior change wheel (Michie et al., 2011) has been applied as a framework to guide various interventions, for instance, mHealth interventions (Chiang et al., 2018). When it is used as a theoretical framework for designing interventions to promote portal adoption or engagement, the following dimensions can be considered: capability, motivation, and opportunity. Specifically, psychological capability, physical and social opportunity are important factors to be considered when designing an intervention to promote portal engagement. The behavior change wheel (Michie et al., 2011) also has provided strategies to facilitate capability, opportunity, and motivation, such as education, modeling, and enablement.
In our study, patient portal access was found to be a significant predictor of patient portal engagement, thus enhancing patients' digital access becomes an urgent and necessary effort. In the meantime, previous studies have revealed obvious disparities in digital healthcare service access, those with low socioeconomic status (SES) are less likely to use health technologies due to lack of access (e.g., Ahmed et al., 2020). Therefore, promoting patient portal access of people with low SES should be one focus of policy makers and healthcare providers' work in the future.
The results also provided important implications in terms of healthcare providers' key roles in facilitating patients' portal engagement. The following strategies can be used to facilitate portal engagement. First, during and/or after each doctor's office visit, healthcare providers can offer patient portal information (e.g., how to access portal online, how to use it) to patients who do not have access to patient portal to increase the rates of portal adoption and engagement. Second, physicians can briefly mention the benefits of a patient portal and encourage patients to use it. Moreover, the practice of PCC will potentially change patients' perception that a patient portal is a lean medium, and will also help patients understand better about the health information in the portal.
Limitation and future studies
There are several limitations of the study. One is that HINTS data did not have variables to measure channel perception. In future studies, we can conduct surveys to include participants' perceptions of the channel to test the relationships (i.e., from PCC to portal channel perception, to the level of difficulty in understanding health information on the patient portal, to patient portal engagement). Another limitation is that a limited number of variables representing limited categories of the behavior change model (Michie et al., 2011) were tested in this study. The model entails six categories (i.e., physical capability, psychological capability, social opportunity, physical opportunity, automatic motivation, and reflective motivation), and only three categories with one variable from each category were tested in this study. However, existing research has demonstrated a variety of variables (e.g., personal factors, health care delivery factors) influencing patient portal engagement (Irizarry et al., 2015). Future study could explore other categories of the behavior change model, such as reflective motivation. For instance, will including educational resources in patient portal (Johnson et al., 2023) promote reflective motivation, which then increases portal engagement? Another limitation is that because of the cross-sectional nature of the survey, no causal relationship can be demonstrated. Future research could use longitudinal surveys or experiments to test the relationships.
Conclusion
Guided by the behavior change wheel framework (Michie et al., 2011) and the channel expansion theory (Carlson and Zmud, 1999), this study examined the facilitators of patient portal engagement and tested the relationship between the facilitators. In order to test the relationships, HINTS national survey data (N = 1,251) were used. We found that patient portal access (an example of physical opportunity) and physician advocacy (an example of social opportunity) were two significant predictors of portal engagement while educational attainment was not. We did not find any direct correlation between PCC and patient portal engagement. However, we found a significant indirect relationship between PCC and portal engagement through levels of difficulty in understanding health information on the portals (an example of psychological capability). To the best of our knowledge, this is the first study to employ the behavior change wheel (Michie et al., 2011) and the channel expansion theory (Carlson and Zmud, 1999) to explain patient portal engagement, and to explain the mechanism of how interpersonal communication could influence portal-mediated communication. Theoretically, our study extended the behavior change wheel (Michie et al., 2011) by further explaining the relationship between the key components (e.g., capability, opportunity) of behavior change. Practical strategies have been proposed to increase patient portal engagement.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found at: https://hints.cancer.gov/.
Author contributions
WC: Conceptualization, Methodology, Writing—original draft, Writing—review & editing. XC: Writing—original draft, Writing—review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ahmed, T., Rizvi, S. J. R., Rasheed, S., Iqbal, M., Bhuiya, A., Standing, H., et al. (2020). Digital health and inequalities in access to health services in Bangladesh: mixed methods study. JMIR mHealth uHealth 8:e16473. doi: 10.2196/16473
Amante, D. J., Hogan, T. P., Pagoto, S. L., and English, T. M. (2014). A systematic review of electronic portal usage among patients with diabetes. Diabetes Technol. Ther. 16, 784–793. doi: 10.1089/dia.2014.0078
Ammenwerth, E. (2018). From eHealth to ePatient: the role of patient portals in fostering patient empowerment. Eur. J. Biomed. Inf. 14, 20–23. doi: 10.24105/ejbi.2018.14.2.4
An, Y. J., and Frick, T. (2006). Student perceptions of asynchronous computer-mediated communication in face-to-face courses. J. Comput-Mediat. Commun. 11, 485–499. doi: 10.1111/j.1083-6101.2006.00023.x
Ancker, J. S., Nosal, S., Hauser, D., Way, C., and Calman, N. (2017). Access policy and the digital divide in patient access to medical records. Health Policy Technol. 6, 3–11. doi: 10.1016/j.hlpt.2016.11.004
Ancker, J. S., Osorio, S. N., Cheriff, A., Cole, C. L., Silver, M., Kaushal, R., et al. (2015). Patient activation and use of an electronic patient portal. Inf. Health Soc. Care 40, 254–266. doi: 10.3109/17538157.2014.908200
Anthony, D. L., Campos-Castillo, C., and Lim, P. S. (2018). Who isn't using patient portals and why? Evidence and implications from a national sample of US adults. Health Aff. 37, 1948–1954. doi: 10.1377/hlthaff.2018.05117
Baldwin, J. L., Singh, H., Sittig, D. F., and Giardina, T. D. (2017). Patient portals and health apps: pitfalls, promises, and what one might learn from the other. Healthcare 5, 81–85. doi: 10.1016/j.hjdsi.2016.08.004
Bao, C., Singh, H., Meyer, B., Kirksey, K., and Bardhan, I. (2020). Patient-provider engagement and its impact on health outcomes: a longitudinal study of patient portal use. MIS Q. 44, 699–723. doi: 10.25300/MISQ/2020/14180
Browne, M. W., and Cudeck, R. (1993). “Alternative ways of assessing model fit,” in Testing Structural Equation Models, eds K. A. Bollen, and J. S. Long (London: Sage), 136–162.
Carlson, J. R., and Zmud, R. W. (1999). Channel expansion theory and the experiential nature of media richness perceptions. Acad. Manag. J. 42, 153–170. doi: 10.2307/257090
Centers for Medicare and Medicaid Services (2023). Promoting Interoperability Programs. Available online at: https://www.cms.gov/regulations-and-guidance/legislation/ehrincentiveprograms (accessed February 13, 2024).
Chiang, N., Guo, M., Amico, K. R., Atkins, L., and Lester, R. T. (2018). Interactive two-way mHealth interventions for improving medication adherence: an evaluation using the behaviour change wheel framework. JMIR mHealth uHealth 6:e9187. doi: 10.2196/mhealth.9187
Daft, R. L., and Lengel, R. H. (1986). Organizational information requirements, media richness and structural design. Manage. Sci. 32, 554–571. doi: 10.1287/mnsc.32.5.554
Dendere, R., Slade, C., Burton-Jones, A., Sullivan, C., Staib, A., Janda, M., et al. (2019). Patient portals facilitating engagement with inpatient electronic medical records: a systematic review. J. Med. Internet Res. 21:e12779. doi: 10.2196/12779
Dennis, A. R., Fuller, R. M., and Valacich, J. S. (2008). Media, tasks, and communication processes: a theory of media synchronicity. MIS Q. 32, 575–600. doi: 10.2307/25148857
Epstein, R. M., and Street, Jr R. L. (2007). Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering. Available online at: https://cancercontrol.cancer.gov/sites/default/files/2020-06/pcc_monograph.pdf (accessed February 13, 2024).
Fuerst, M. L. (2017). Patients prefer face-to-face communications with doctors. Oncol. Times 39:62. doi: 10.1097/01.COT.0000527379.44018.e1
Fujioka, J. K., Bickford, J., Gritke, J., Stamenova, V., Jamieson, T., Bhatia, R. S., et al. (2021). Implementation strategies to improve engagement with a multi-institutional patient portal: multimethod study. J. Med. Internet Res. 23:e28924. doi: 10.2196/28924
Goel, M. S., Brown, T. L., Williams, A., Hasnain-Wynia, R., Thompson, J. A., Baker, D. W., et al. (2011). Disparities in enrollment and use of an electronic patient portal. J. Gen. Intern. Med. 26, 1112–1116. doi: 10.1007/s11606-011-1728-3
Heponiemi, T., Kaihlanen, A. M., Kouvonen, A., Leemann, L., Taipale, S., Gluschkoff, K., et al. (2022). The role of age and digital competence on the use of online health and social care services: a cross-sectional population-based survey. Dig. Health 8:20552076221074485. doi: 10.1177/20552076221074485
Hoogenbosch, B., Postma, J., de Man-van Ginkel, J. M., Tiemessen, N. A., van Delden, J. J., and van Os-Medendorp, H. (2018). Use and the users of a patient portal: cross-sectional study. J. Med. Internet Res. 20:e262. doi: 10.2196/jmir.9418
Hu, L., and Bentler, P. M. (1998). Fit indices in covariance structure modeling: sensitivity to underparameterized model misspecification. Psychol. Methods 3, 424–453. doi: 10.1037/1082-989X.3.4.424
IBM Corp (2020). IBM SPSS Statistics for Windows (Version 27.0) [Computer software]. Armonk, NY: IBM Corp.
Irizarry, T., DeVito Dabbs, A., and Curran, C. R. (2015). Patient portals and patient engagement: a state of the science review. J. Med. Internet Res. 17:e148. doi: 10.2196/jmir.4255
Ishii, K., Lyons, M. M., and Carr, S. A. (2019). Revisiting media richness theory for today and future. Hum. Behav. Emerg. Technol. 1, 124–131. doi: 10.1002/hbe2.138
Johnson, A. M., Brimhall, A. S., Johnson, E. T., Hodgson, J., Didericksen, K., Pye, J., et al. (2023). A systematic review of the effectiveness of patient education through patient portals. JAMIA Open 6:ooac085. doi: 10.1093/jamiaopen/ooac085
Kashian, N., and Mirzaei, T. (2019). Understanding communication effectiveness, communication satisfaction, self-efficacy, and self-care management among patients with chronic disease. Sci. Commun. 41, 172–195. doi: 10.1177/1075547019834566
Ketterer, T., West, D. W., Sanders, V. P., Hossain, J., Kondo, M. C., Sharif, I., et al. (2013). Correlates of patient portal enrollment and activation in primary care pediatrics. Acad. Pediatr. 13, 264–271. doi: 10.1016/j.acap.2013.02.002
Kruse, C. S., Argueta, D. A., Lopez, L., and Nair, A. (2015). Patient and provider attitudes toward the use of patient portals for the management of chronic disease: a systematic review. J. Med. Internet Res. 17:e40. doi: 10.2196/jmir.3703
Laukka, E., Huhtakangas, M., Heponiemi, T., Kujala, S., Kaihlanen, A. M., Gluschkoff, K., et al. (2020). Health care professionals' experiences of patient-professional communication over patient portals: systematic review of qualitative studies. J. Med. Internet Res. 22:e21623. doi: 10.2196/21623
Lazard, A. J., Watkins, I., Mackert, M. S., Xie, B., Stephens, K. K., Shalev, H., et al. (2016). Design simplicity influences patient portal use: the role of aesthetic evaluations for technology acceptance. J. Am. Med. Inform. Assoc. 23, e157–e161. doi: 10.1093/jamia/ocv174
Lyles, C. R., Sarkar, U., Ralston, J. D., Adler, N., Schillinger, D., Moffet, H. H., et al. (2013). Patient–provider communication and trust in relation to use of an online patient portal among diabetes patients: the diabetes and aging study. J. Am. Med. Inform. Assoc. 20, 1128–1131. doi: 10.1136/amiajnl-2012-001567
Maurer, M., Dardess, P., Carman, K. L., Frazier, K., and Smeeding, L. (2012). Guide to Patient and Family Engagement: Environmental Scan Report. (Prepared by American Institutes for Research under contract HHSA 290-200-600019). AHRQ Publication No. 12-0042-EF. Rockville, MD: Agency for Healthcare Research and Quality.
McDonald, R. P., and Ho, M. H. R. (2002). Principles and practice in reporting structural equation analyses. Psychol. Methods 7, 64–82. doi: 10.1037/1082-989X.7.1.64
Michie, S., Atkins, L., and West, R. (2014). The Behaviour Change Wheel: A Guide to Designing Interventions, 1st ed. Great Britain: Silverback Publishing.
Michie, S., Van Stralen, M. M., and West, R. (2011). The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement. Sci. 6, 1–12. doi: 10.1186/1748-5908-6-42
Miller Jr, D. P., Latulipe, C., Melius, K. A., Quandt, S. A., and Arcury, T. A. (2016). Primary care providers' views of patient portals: interview study of perceived benefits and consequences. J. Med. Internet Res. 18:e8. doi: 10.2196/jmir.4953
Moqbel, M., Rahman, M. S., Cho, S., and Hewitt, B. (2020). Sustaining patient engagement: the role of health emotion and personality traits in patient portal continuous use decision. AIS Trans. Comput. Hum. Interact. 12, 179–205. doi: 10.17705/1thci.00135
Muthén, L. K., and Muthén, B. O. (2017). Mplus: Statistical Analysis with Latent Variables: User's Guide, 8th ed. Los Angeles, CA: Muthén and Muthén.
National Cancer Institute (n.d.). Frequently Asked Questions about HINTS. Available online at: https://hints.cancer.gov/about-hints/frequently-asked-questions.aspx (accessed February 13 2024).
Osborn, C. Y., Mayberry, L. S., Wallston, K. A., Johnson, K. B., and Elasy, T. A. (2013). Understanding patient portal use: implications for medication management. J. Med. Internet Res. 15:e2589. doi: 10.2196/jmir.2589
Powell, K. R. (2017). Patient-perceived facilitators of and barriers to electronic portal use: a systematic review. CIN: Comput. Inform. Nurs. 35, 565–573. doi: 10.1097/CIN.0000000000000377
Preacher, K. J., and Hayes, A. F. (2008). “Assessing mediation in communication research,” in The Sage Sourcebook of Advanced Data Analysis Methods for Communication Research, eds A. F. Hayes, M. D. Slater, and L. B. Snyder (London: Sage), 13–54. doi: 10.4135/9781452272054.n2
Rathert, C., Mittler, J. N., Banerjee, S., and McDaniel, J. (2017). Patient-centered communication in the era of electronic health records: what does the evidence say? Patient Educ. Couns. 100, 50–64. doi: 10.1016/j.pec.2016.07.031
Ricciardi, L., Mostashari, F., Murphy, J., Daniel, J. G., and Siminerio, E. P. (2013). A national action plan to support consumer engagement via e-health. Health Aff. 32, 376–384. doi: 10.1377/hlthaff.2012.1216
Sarkar, U., Karter, A. J., Liu, J. Y., Adler, N. E., Nguyen, R., López, A., et al. (2011). Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J. Am. Med. Inform. Assoc. 18, 318–321. doi: 10.1136/jamia.2010.006015
Sarkar, U., Lyles, C. R., Parker, M. M., Allen, J., Nguyen, R., Moffet, H. H., et al. (2014). Use of the refill function through an online patient portal is associated with improved adherence to statins in an integrated health system. Med. Care 52:194. doi: 10.1097/MLR.0000000000000069
Slanetz, P. J., Krishnaraj, A., Lee, C. I., and Lourenco, A. P. (2019). Patient portals and radiology: overcoming hurdles. J. Am. Coll. Radiol. 16, 1488–1490. doi: 10.1016/j.jacr.2019.02.036
Steitz, B. D., Wong, J. I. S., Cobb, J. G., Carlson, B., Smith, G., Rosenbloom, S. T., et al. (2019). Policies and procedures governing patient portal use at an Academic Medical Center. JAMIA Open 2, 479–488. doi: 10.1093/jamiaopen/ooz039
Sun, R., Burke, L. E., Saul, M. I., Korytkowski, M. T., Li, D., Sereika, S. M., et al. (2019). Use of a patient portal for engaging patients with type 2 diabetes: patterns and prediction. Diabetes Technol. Ther. 21, 546–556. doi: 10.1089/dia.2019.0074
The Office of the National Coordinator for Health Information Technology (2017). Frequently Asked Questions. Available online at: https://www.healthit.gov/faq/what-patient-portal (accessed February 13, 2024).
Tieu, L., Sarkar, U., Schillinger, D., Ralston, J. D., Ratanawongsa, N., Pasick, R., et al. (2015). Barriers and facilitators to online portal use among patients and caregivers in a safety net health care system: a qualitative study. J. Med. Internet Res. 17:e275. doi: 10.2196/jmir.4847
Timmerman, C. E., and Madhavapeddi, S. N. (2008). Perceptions of organizational media richness: channel expansion effects for electronic and traditional media across richness dimensions. IEEE Trans. Prof. Commun. 51, 18–32. doi: 10.1109/TPC.2007.2000058
Totzkay, D., Silk, K. J., and Sheff, S. E. (2017). The effect of electronic health record use and patient-centered communication on cancer screening behavior: an analysis of the Health Information National Trends Survey. J. Health Commun. 22, 554–561. doi: 10.1080/10810730.2017.1338801
Turner, K., Clary, A., Hong, Y. R., Tabriz, A. A., and Shea, C. M. (2020). Patient portal barriers and group differences: cross-sectional national survey study. J. Med. Internet Res. 22:e18870. doi: 10.2196/18870
Wakefield, B. J., Turvey, C., Hogan, T., Shimada, S., Nazi, K., Cao, L., et al. (2020). Impact of patient portal use on duplicate laboratory tests in diabetes management. Telemed. e-Health 26, 1211–1220. doi: 10.1089/tmj.2019.0237
Wallace, L. S., Angier, H., Huguet, N., Gaudino, J. A., Krist, A., Dearing, M., et al. (2016). Patterns of electronic portal use among vulnerable patients in a nationwide practice-based research network: from the OCHIN practice-based research network (PBRN). J. Am. Board Fam. Med. 29, 592–603. doi: 10.3122/jabfm.2016.05.160046
Woods, S. S., Forsberg, C. W., Schwartz, E. C., Nazi, K. M., Hibbard, J. H., Houston, T. K., et al. (2017). The association of patient factors, digital access, and online behavior on sustained patient portal use: a prospective cohort of enrolled users. J. Med. Internet Res. 19:e345. doi: 10.2196/jmir.7895
Wright, J. A., Volkman, J. E., Leveille, S. G., and Amante, D. J. (2022). Predictors of online patient portal use among a diverse sample of emerging adults: cross-sectional survey. JMIR Form. Res. 6:e33356. doi: 10.2196/33356
Zaidi, M., Amante, D. J., Anderson, E., Ito Fukunaga, M., Faro, J. M., Frisard, C., et al. (2022). Association between patient portal use and perceived patient-centered communication among adults with cancer: cross-sectional survey study. JMIR Cancer 8:e34745. doi: 10.2196/34745
Zhou, J., Arriaga, R. I., Liu, H., and Huang, M. (2022). “A tale of two perspectives: harvesting system views and user views to understand patient portal engagement,” in 2022 IEEE 10th International Conference on Healthcare Informatics (ICHI) (Rochester, MN: IEEE), 373–383. doi: 10.1109/ICHI54592.2022.00059
Keywords: patient portal engagement, the behavior change wheel, the channel expansion theory, patient-centered communication, patient portal access
Citation: Cao W and Cao X (2024) Facilitating patient portal engagement: a channel expansion and behavior change wheel perspective. Front. Commun. 9:1272825. doi: 10.3389/fcomm.2024.1272825
Received: 04 August 2023; Accepted: 06 February 2024;
Published: 21 February 2024.
Edited by:
Suleman Atique, Norwegian University of Life Sciences, NorwayReviewed by:
Iuliana Raluca Gheorghe, Carol Davila University of Medicine and Pharmacy, RomaniaHosna Salmani, Iran University of Medical Sciences, Iran
Raphael Oladeji Akangbe, Lagos State Government, Nigeria
Copyright © 2024 Cao and Cao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weidan Cao, bWFpbC53ZWlkYW5AZ21haWwuY29t
 Weidan Cao
Weidan Cao Xiaohui Cao
Xiaohui Cao