- 1Mayo Clinic Graduate School of Biomedical Sciences, Mayo Clinic, Rochester, MN, United States
- 2Mayo Clinic College of Medicine and Science, Mayo Clinic, Rochester, MN, United States
- 3Human Resources, Leadership and Organizational Development, Mayo Clinic, Rochester, MN, United States
- 4Office of Applied Scholarship and Education Science, Mayo Clinic College of Medicine and Science, Mayo Clinic, Rochester, MN, United States
- 5Department of Biochemistry and Molecular Biology, Mayo Clinic, Rochester, MN, United States
- 6Department of Anatomy, Cell Biology, and Physiology, Indiana University School of Medicine, Indianapolis, IN, United States
- 7Indiana Center for Musculoskeletal Health, Indianapolis, IN, United States
- 8IU Simon Comprehensive Cancer Center, Indianapolis, IN, United States
Increasing diversity in the biomedical research workforce is a critical national issue. Particularly concerning is the lack of representation at more advanced career stages/in leadership positions. While there are numerous institutional initiatives promoting professional research skills (i.e., grant writing, presenting, networking) for underrepresented (UR) PhD trainees, there are comparatively fewer opportunities for leadership development. We present a blueprint for Leadership in PhD (LeaP), a cohort-based program aiming to equip UR biomedical research trainees with skills to succeed as academic, industry, and community leaders. In contrast to intensive short-term programs or workshops, LeaP is a longitudinal 4-year experience with an blend of didactic, self-directed, and experiential learning. First year trainees receive foundational didactic instruction on core leadership concepts coupled with facilitated peer discussions and one-on-one coaching support. We outline a program evaluation framework that assesses student learning, satisfaction, and program efficacy. Evaluation data from the inaugural year is presented and discussed.
Introduction
Despite efforts to diversify the composition of the scientific workforce, stark disparities remain (Woolston, 2021). A recent analysis conducted by the Pew Research Center in 2021 found that Black and Hispanic workers remain underrepresented in the science, technology, engineering, and math (STEM) workforce compared with their share of all jobs (Fry et al., 2021). This disparity is acutely evident in the life sciences where Black and Hispanic workers comprise 6 and 8%, respectively, of the workforce despite overall representation across all jobs being 11 and 17%. Representation of women in the life sciences has fared better—in 2019 women comprised 48% of the life sciences workforce compared to 34% in 1990. Intersectional inequalities, however, compound individual deficits in representation. These inequalities are evident when considering the number of minority women in science, and further, when examining performance-based metrics including sub-discipline funding rates and scholarly impact (Kozlowski et al., 2022). Perdurance in academic science also lags in minoritized groups. A recent study by Lambert and colleagues surveying postdoctoral fellow career choices found that academia-bound UR postdocs have significantly lower confidence in securing funding, feelings of self-worth, and research career self-efficacy. Exit rates of minoritized postdocs from research/academia were also significantly higher than their white/majority counterparts (Lambert et al., 2020).
Representational diversity and equity concerns persist for those fortunate to secure research intensive faculty-level positions (Rosenbloom et al., 2017; Chance, 2021). Bias within the promotion and tenure process coupled with a lack of cultural sensitivity and social awareness regarding the professional and personal needs of UR faculty has resulted in substantial attrition. Women, for example, reached a remarkable milestone in 2003 when rates of medical school matriculation first hit the 50% mark. Despite that achievement, the proportions of women associate professors (37%) and professors (25%) in medicine in 2020 indicate that academia is not capitalizing on those gains in student interest in pursuing medical and science-based careers (Brown, 2020). Due to numerous individual and systemic roadblocks hindering progress through academic rank, the number of women and underrepresented faculty in leadership positions remains low. According to a 2017 overview of university presidents reported by the American Council on Education, women comprised 30% of all University president positions. Further, within the already slim proportion of women presidents, only 9% identify as Black women, and only 4% as Hispanic women—compared to the roughly 83% who identify as White (ACE, 2017). A closer look at these numbers further reveals another disturbing trend in that minority women who do attain senior leadership are often serving at lower-ranked, less prestigious schools with small endowments, and limited resources for research and advanced scholarship (ACE, 2017). These intersectional inequities are not limited to the University presidents. Across all research and health sciences jobs, women hold 52% of reported leadership positions, while racial/ethnic minorities represent 11% of leadership, and Black/Hispanic women only 3% (CUPA-HR, 2020).
Addressing representational inequities in biomedical and senior academic leadership promotes individual fairness and justice, and if done in conjunction with rigorous training and support, could tackle a much larger issue of culture and climate concerns in academia. Many from minoritized groups report difficulties penetrating, enduring, and thriving within the privileged (i.e., older, white, and male) academic ecosystem. Diversifying leadership would inherently promote and foster professional networking and development of underrepresented trainees/junior fellows/faculty who have shared life experiences and seek role models/inspiration. Indeed, representational diversity is known to be a strong catalyst for career progression within underrepresented communities, which further yields benefits for the overall enterprise (Hunt et al., 2018). Another benefit of leadership training is tackling the pervasive culture of ineffective leadership and poor mentoring in academia (Rockey, 2014; Choi et al., 2019; Bond et al., 2020; Canti et al., 2021; Gutierrez et al., 2021)—a state largely resulting from inadequate training, inconsistent continuous professional development, and little accountability. Racism, xenophobia, and microaggressions present additional barriers for UR trainees and contribute to heightened stress, demotivation, and feelings of exclusion. LeaP supports students as they navigate these and other issues as a cohort, while honing critical resiliency skills.
Leadership development at academic research centers is not new. Many institutions, centers, and scientific societies have stepped up and begun addressing this critical societal need. Key programmatic activities include robust mentor training initiatives, resilience and wellness support for diverse trainees, networking opportunities, and targeted leadership development opportunities. Notable leadership from the National Institute for General Medical Sciences, the National Science Foundation and cross-institutional networks/alliances including the National Research Mentoring Network (NRMN) (Ahmed et al., 2021) and the Leadership Alliance (Ghee et al., 2014, 2016) has seeded a movement of academics dedicated to improving culture/climate and fostering the development of diverse leaders (Tucker Edmonds et al., 2022). That said, significant gaps and opportunities remain. First, many (if not most) leadership initiatives target individuals at an advanced career stage—typical requirements include holding an advanced degree and/or an active or pending faculty appointment. Second, many programs employ an intensive, immersion-based approach—excellent for building knowledge and seeding skills but limited in the ability to support longitudinal skill perdurance and further development. Third, programs targeted to early-stage trainees, such as advanced degree candidates, tend to feature a defined curriculum that prioritizes knowledge building and group skills while providing fewer opportunities for individual skills exploration and development.
With the Leadership in PhD (LeaP) program, we aimed to create a supportive and flexible learning environment for underrepresented PhD trainees to discover, explore, and refine leadership skills essential for leading an inclusive workplace. While LeaP does not have the ability to singlehandedly address systemic issues hindering UR advancement in academia, we contend that it does have significant value as it provides UR trainees with foundational skills to succeed and thrive as leaders in the biomedical sciences. Here, we outline a conceptual framework for LeaP, describe key programmatic features, present a summary and evaluation of year one, and discuss future directions for this work.
Program overview
Conceptual framework
The core mission of the LeaP program is to facilitate the development of knowledge, skills, and abilities essential for future biomedical research leaders in academia, industry, and society. The cohort-based model is intended to provide a safe and encouraging environment in which to engage in active self-discovery and peer-to-peer support. LeaP takes a student-centered learning approach, whereby programmatic components are designed to meet the needs of individual students. Characteristics of a student-centered learning model include competency-based progression, student engagement in knowledge construction, shared-decision making, choice, and continuous reassessment/reevaluation of student needs (Neumann, 2013; Cornelius-White, 2016; Starkey, 2017; Bremner et al., 2022). Indeed, student-centered pedagogy is gaining world-wide traction as an approach to improve learning outcomes (Burner et al., 2016; Connell et al., 2016; Cheng and Ding, 2020).
Within the framework of the student-centered learning approach, we sought to include elements of self-directed learning via one-on-one coaching sessions. Self-directed learning involves an intentional process of identifying wants and needs, setting goals, planning, experimentation, and evaluation (Knowles, 1975; Goleman et al., 2009; Taylor and Hamdy, 2013). This term has shown up regularly in the adult education literature since the 1970s, often defined in a context-specific manner. One constant, however, is the emphasis on learner autonomy (i.e., the ability to drive their own learning), which we achieved via coaching (Loeng, 2020). Indeed, according to Losch et al. (2016), “coaching can be defined as a collaborative helping relationship, where coach and client (‘coachee’) engage in a systematic process of setting goals and developing solutions with the aim of facilitating goal attainment, self-directed learning, and personal growth of the coachee”. Coaching sessions included support around identifying strengths and areas for growth as well as desires and motivations; all with a focus on goal setting and crafting a plan for experimentation and real-world skill practice. Monthly coaching sessions gave students the opportunity to evaluate progress and to expand or create new goals to support their individual skill development. This repeated (monthly) cycle built in support for self-directed learning during students’ first year in LeaP, and ultimately taught students a life-long process for engaging in continued learning and growth (an essential skill for leaders).
Finally, considering that scholars engaged with LeaP are biomedical PhD trainees, concerted efforts were made to (1) provide scholars with experiences complementary to but distinct from thesis advisory committees or workshop-based professional development opportunities, (2) tailor contact hours to fit within the constraints of a rigorous PhD curriculum, and (3) support progressive leadership development throughout their biomedical PhD training.
Cohort selection
One of our primary objectives was to foster development of leadership skills in trainees historically underrepresented in biomedical research. Here we defined underrepresented (UR) in accordance with National Institutes of Health (NIH) NOT-OD-20-031. In order to be as inclusive as possible, we did extend program participation/nomination to include allies (i.e., those who do not identify as UR but who demonstrate a commitment to diversity and inclusion). A modified version of the PhD application rubric was used—one that equally prioritized the following four areas: (1) leadership potential, (2) research potential, (3) industry, persistence and commitment to education/personal growth, and (4) academic performance/research experience. With applicant permission, LeaP candidacy was evaluated in parallel to the PhD admissions process. Eight students were selected for the inaugural LeaP cohort, the majority of whom self-identified as female, and all of whom self-identified as meeting the NIH UR definition.
Leadership competencies
The four-year LeaP experience centers around leadership competencies described in and assessed by the Occupational Personality Questionnaire (OPQ) developed by SHL Group Limited (Joubert and Venter, 2013; Furnham et al., 2014). While the OPQ is broadly used in the context of talent acquisition and management, Mayo Clinic has long partnered with SHL to leverage the OPQ for upper-level leadership preparation. Here, the OPQ identifies strengths, working styles, and opportunities to develop capability and unlock potential—thus setting the stage for individualized leadership coaching. We aimed to adapt and streamline this approach for LeaP participants. Ultimately, ten core leadership competencies were selected from the OPQ that served as the foundation for the didactic and discussion-based material covered in Year 1: (1) leading and deciding, (2) working with people, (3) adhering to principles/values, (4) presenting and communicating, (5) persuading and influencing, (6) creating and innovating, (7) planning and organizing, (8) adapting and responding to change, (9) coping with pressures and setbacks, and (10) relating and networking (Joubert and Venter, 2013; Furnham et al., 2014). These ten competencies were selected (a) based on their broad applicability to diverse potential biomedical careers and (b) to complement, synergize with, and reinforce competencies addressed by career development programs such as the NIH-sponsored Initiative for Maximizing Student Development (IMSD). LeaP program activities were aligned to these ten competencies and are described in more detail below.
Programmatic components
The overarching structure of the LeaP curriculum involves iterative and progressive cycles of didactic learning, facilitated peer discussions, and coaching (self-reflection, goal setting, experimentation, and skill-practice). In discussions, LeaP facilitators joined learners as they discussed, processed, and applied information, strategies, and skills covered in the previous week’s seminar (Burgess et al., 2020). Coaching sessions followed these discussions and further enhanced learning by inviting students to self-reflect, set goals, and create an action plan (Deiorio et al., 2016). This structure is reflected in the year-to-year plan; year one focuses on concept assimilation, cohort building, self-discovery, goal setting, and skill practice, year two on continued self-directed learning and skill implementation/practice (e.g., choosing study topics and materials, leading discussions, mentoring first year LeaP scholars, pursuing community projects, etc.), year three on individual or small group-based intramural (institutional) leadership experiences, and year four on tailored extramural (e.g., community-based, scientific society, etc.) leadership experiences. Opportunities in years three and four represent a partnership with the Mayo Clinic Graduate School of Biomedical Sciences (MCGSBS) Career Development Internship (CDI) program, whereby career exploration will be coupled with leadership skills building/practice. With this plan, students can progressively apply skills learned in year 1 in peer-based settings, within the institution, and finally, in the community. A summary of planned activities is depicted in Figure 1. Year one activities are described in more detail below.
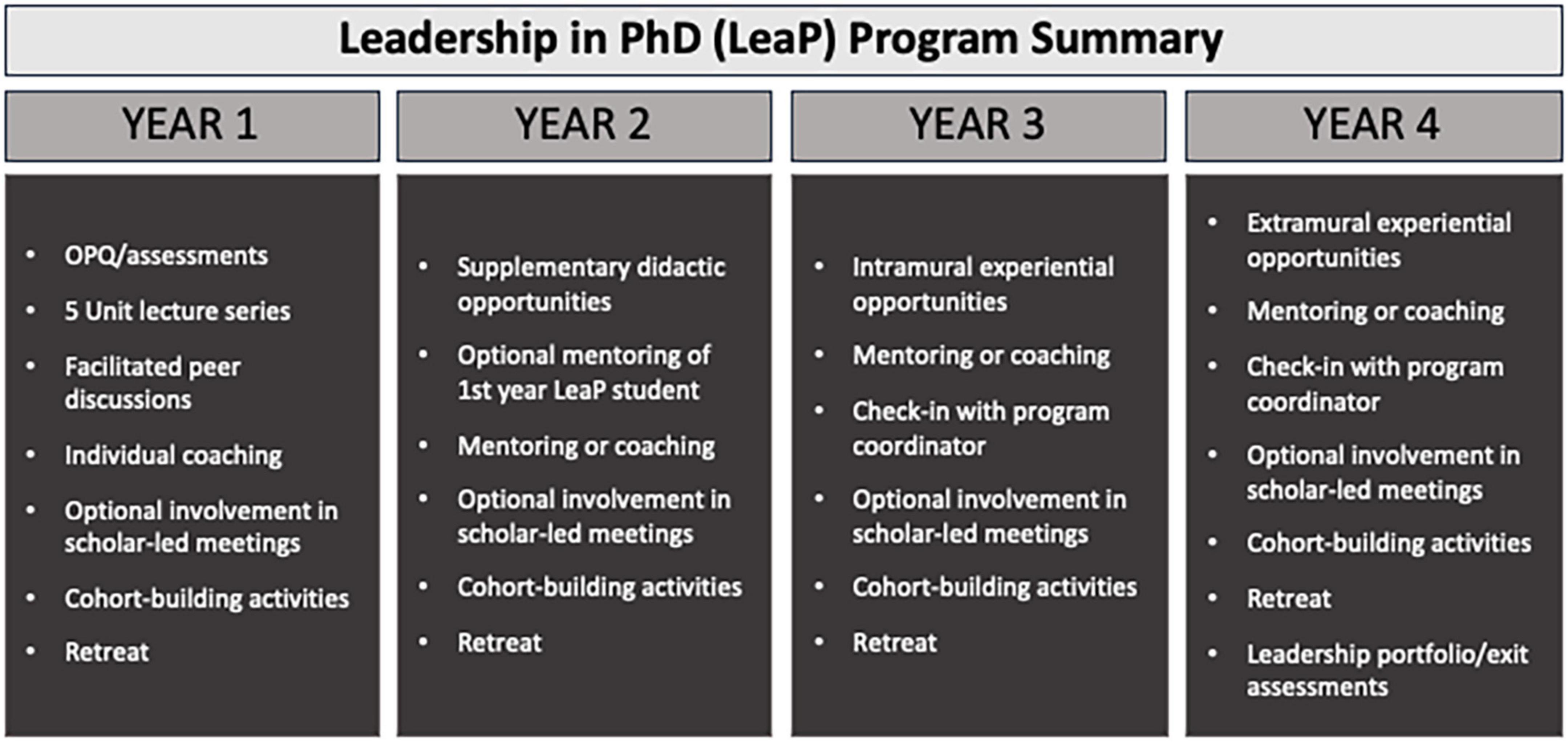
Figure 1. Program summary. Shown (L to R) are summaries of key activities proposed for each year in the program.
The first year was presented over 9 months during the 2021–2022 academic year, with a staggered start with PhD coursework to give time for students to acclimate to their home campus, classes, and laboratory rotations. Prior to official program launch, an introductory session was held where program mission, motivation, and structure were shared and discussed. Five units were outlined each with sub-themes that were intentionally designed to address the ten leadership competencies described above (see competency map in Figure 2). Units were structured as monthly modules each containing a seminar (open to all graduate students), a facilitated discussion, and an individual coaching session. Modules were structured in order to (1) provide foundational information (as some students may not have had prior exposure to certain leadership concepts/terminology), (2) permit deeper, group-based exploration of key concepts covered in a given seminar, and (3) facilitate individual reflection with a coach and to set relevant goals for that would reinforce learned concepts. Two units (emotional intelligence and communication) were presented as two-month modules with six touchpoints instead of three. Most meetings were held virtually given that LeaP included MCGSBS students from all three Mayo Clinic campuses (Rochester, MN, USA; Scottsdale, AZ, USA; Jacksonville, FL, USA). Brief unit descriptions are as follows:
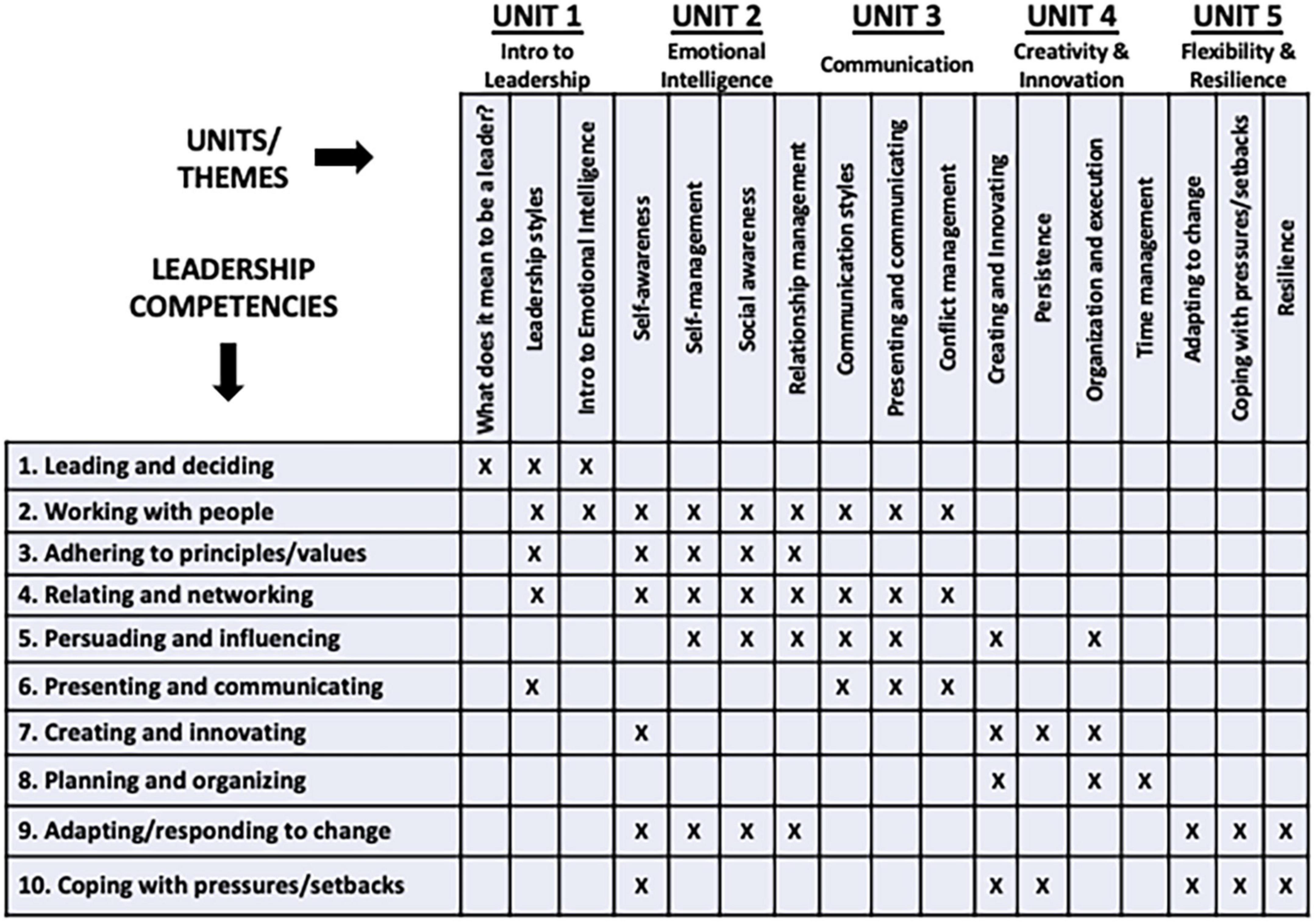
Figure 2. Competency map. Shown (across) are the five year one units and associated sub-themes. Rows indicate specific leadership competencies derived from the OPQ. An “X” indicates, at minimum, the competency coverage addressed by a given unit sub-theme. Note that most competencies were covered by more units than indicated above.
Unit One: Introduction to Leadership. Sub-themes: (1) meaning of leadership, (2) leadership styles, and (3) introduction to emotional intelligence. Discussion highlights: Students were asked to (a) identify their go-to leadership styles, (b) consider when/why it may be beneficial to adapt their leadership style, and (c) reflect on how to go about navigating leadership styles while maintaining an inclusive and equitable environment.
Unit Two: Emotional Intelligence (EI). Sub-themes: (1) self-awareness, (2) self-management, (3) social awareness, and (4) relationship management. Discussion highlights: (a) the importance of (and strategies to develop) self-awareness and social awareness, (b) ways to practice self-management and relationship management, and (c) scenarios to prompt discussion around how to apply EI skills in the workplace.
Unit Three: Communication. Sub-themes: (1) presenting and communicating, (2) communication styles, and (3) conflict management. Discussion highlights: (a) communicating for impact, (b) the importance of relationships, (c) communication styles and how they relate to EI, and (d) prompts to discuss real-life applicability (e.g., how does understanding of our own and others’ communication styles help us manage conflict?).
Unit Four: Creativity and Innovation. Sub-themes: (1) creating and innovating, (2) planning and time management, (3) organization and execution, and (4) persistence. Discussion highlights: (a) brainstorming techniques, (b) the importance and impact of creativity and innovation, and (c) conversation around how to create a safe and supportive environment that encourages different points of view, experimentation, failure, and persistence.
Unit Five: Flexibility and Resilience. Sub-themes: (1) adapting to change, (2) flexibility, (3) dealing with pressures and setbacks, and (4) resilience. Discussion highlights: flexibility and resilience strategies were shared during an integrated in-person two-day retreat held on the Rochester campus.
Evaluation plan and results
Evaluation plan
Leadership in PhD program evaluation was developed collaboratively with the co-program directors and the OASES Director of Evaluation prior to the start of the program in Fall 2021. Being a new program, evaluation design focused on gathering both qualitative and quantitative data that would be useful for ensuring program quality and for identifying improvements for future years. Qualitative data gathered included post-session suggestions for session and program improvements, as well as post-program narrative feedback about the program and its impacts, described later in this paper. Understanding participant views on the value of the sessions, as well as on the impact of the educational components and the program overall were top priorities.
After each of the five units, a survey was sent asking scholars to: (a) rate the effectiveness of the session and coaching, (b) describe 1-2 main take-aways from the discussions, (c) rate the role of the lecture, discussion, and coaching in supporting those take-aways, and (d) make suggestions for session and program improvements. This survey approach parallels other surveys at the institution to evaluate participant satisfaction with the programming. The survey questions were uniform across all units but referenced unit-specific content. At the close of the program, qualitative data were gathered from participants in a focus group setting to query the value of the program and its various components, as well as opportunities for improvements.
The evaluation for years 2–4 is designed to: (a) gauge participants’ reaction to the programming (Kirkpatrick, 1998); (b) identify components of the program that were working as intended (Stufflebeam et al., 2000), and assess short-term outcomes of the components on the participants (Van Velsor et al., 2010). Evaluation instruments will include post-session reaction surveys, periodic touchpoint surveys, year-end focus groups, peer assessments, PhD mid-program and exit surveys, and a final portfolio encompassing summaries and reflections on experiential (years 3 and 4) projects. A final OPQ will be administered and results discussed at individual exit meetings/coaching sessions. LeaP alumni will be encouraged to visit and periodically present to/serve on panels for current scholars. Following graduation, LeaP program directors will partner with MCGSBS alumni relations staff to maintain communication with and track career progression of former scholars.
Results
Overall, the unit survey results were highly positive. Between 4 and 5 participants responded to each survey for a general response rate of between 50 and 63%. Participants were asked to rate their level of agreement (5-point Likert scale from strongly disagree to strongly agree) with various statements about the lecture, discussion, and coaching, as well as whether they were likely to use the information they learned in the session. Sessions were highly rated with all respondents across all topics either strongly agreeing or somewhat agreeing that: (a) the lectures broadened their understanding of various leadership styles, (b) the post-lecture discussions were effective in deepening their knowledge about the topic, (c) coaching supported their personal understanding of their strengths and areas for growth, and (d) they were likely to use the information they learned in the unit. In those ratings, most participants strongly agreed with those statements (Figure 3A). Notably, for all sessions, all respondents strongly agreed that the coaching was supporting their personal understanding of their strengths and areas for growth.

Figure 3. Aggregate unit survey data. (A) A heatmap depicting participant level of agreement with survey statements. (B) A heatmap depicting participant opinions regarding the three main teaching modalities. Data for both panels (A,B) are shown as a percentage of total responses across all five units.
For each unit, participants were asked about their main take-aways, as well as the extent to which the lecture, the discussion, and the coaching supported those take-aways. Participants all indicated that the lecture, discussion, and coaching supported their take-aways either “somewhat” or “a lot” with most checking “a lot” (Figure 3B). Participants had relatively few suggestions for improving the teaching modalities; however, suggestions that did surface tended to be related to creating more opportunities for participation and discussion.
In order to gather qualitative data on the value and impact of the program, a focus group was held in early June 2022 following completion of Year 1 of the program. Six of the eight participants attended the focus group. The two participants who were unable to attend the focus group provided feedback separately, one in an individual interview and the other with written responses. The same set of guiding evaluation questions was used for all participants:
1. Strengths: What were the strengths of the program in your opinion?
2. Group dynamics: Describe the group dynamics of the participants in the LeaP program. Was the size of the group good (or too small or too large)? How important was it that all the participants come from groups underrepresented in biomedical research?
3. Facilitation: Tell me about how the co-program directors facilitated the group. To what extent did the way they facilitated work for you? Is there anything that could have been done to improve the facilitation?
4. Coaching: Tell me about the coaching. Was the coaching valuable to you? If yes, in what ways? Is there anything that could have been done to improve the coaching?
5. Impact: What impact has participation in the program had on you? Do you feel that you are able to apply what you learned in the program? What impact do you think participation in the program will have on you as you go through the rest of your PhD program?
6. Changes and recommendations: Were the session topics the right ones? Are there any other topics that could or should have been included? What suggestions do you have for improving the program for the participants who start this upcoming academic year?
7. Other comments: What other suggestions or comments do you have about the program that have not been covered in the questions above.
Participants were overwhelmingly positive about the LeaP program, its value, and its impact. Summarized, representative findings included:
• The size of the cohort was just right. A significantly larger cohort would have made it more difficult for participants to share openly and freely. That openness and ability to be vulnerable with the group helped participants reflect on and make sense of their experiences through the year without judgment and led to a greater sense of belonging.
• Participants in the program developed long-lasting bonds with each other over the year and with the program leads. Having come to the program with shared lived experiences, they were able to gain validation for their experiences as first-year PhD students.
• The coaching was clearly a critical component of the program. Participants described tailored experiences to their individual needs and styles. Participants appreciated session flexibility and the lack of a rigid agenda or approach. All described how they had changed over the year and been impacted by the experience.
• Participants all thought that the topics chosen were important, and the format of the units—with a presentation by a speaker on Tuesdays, a follow-up discussion among the participants, along with the coaching—helped them reflect on and think deeper about the topic and how it applied to their graduate school experience. The separation between the presentation and the follow-up discussion was appreciated, as it left time for participants to “marinate” on the topic.
• Participants noted repeatedly that the program co-directors did an excellent job facilitating the discussions, being prepared with probing questions, helping moderate when discussions got intense, and avoiding judgment. They also attributed the sense of belonging that they gained, in part, to their facilitation.
• Some suggested that it would be better if the individuals who present on Tuesday do not attend the discussion session on Thursday because their presence sometimes changed and restricted open discussion among the participants. Although the speakers only attended the discussion sessions once during the year, the participants noticed the difference in the quality of the discussion.
• Some longer-term impacts described by the participants included: (a) having a cohort they could rely on throughout their PhD program, (b) finding a sense of belonging, (c) feeling validated through cohort discussions, (d) building their communication skills so they could advocate for themselves and others, including about physical and mental well-being, (e) gaining clarity about their personal and professional goals, (f) learning to be assertive and intentional about those goals, and (g) coming to see themselves as leaders and feeling empowered to lead.
• A few suggestions were made for improvements to the program: (a) ensuring that the discussions held on the Thursday following the presentation are specifically for open discussion among the participants (without the presence of the speakers), (b) getting the cohort together as early as possible in the academic year so that connections could be nurtured sooner, (c) having the program be in person, (d) developing a cohort mission statement within each group, (e) ensuring a better gender balance among the cohort, (f) expanding the program with additional cohorts, and (g) keeping quality coaching as a central aspect of the program for future cohorts.
• Participants would like the program to continue for their cohort, with Year 2 involving the development of a project proposal that could impact their communities and with Year 3 being used to implement that project. They noted that the format of Year 1—with a focus on reflection and gaining great knowledge of their strengths and areas for growth—was an important stepping stone enabling them to have a broader impact in future years.
Discussion
Persistent concerns with representational diversity, equity and fairness, and feelings of inclusion/belonging in biomedical research underscore the need to diversify research leadership and support leadership skills development (Elmassian, 2014; Onyura et al., 2019; True et al., 2020; Wang et al., 2021). LeaP tackles these issues by providing a space for underrepresented biomedical research trainees to build community, self-reflect, learn new leadership skills, and to progressively practice and refine those skills in a safe and supportive environment. To that end, LeaP joins a growing number of programs aiming to modernize biomedical education and training by providing early-stage leadership development opportunities (Byington et al., 2016; Meador et al., 2016; Blanchard et al., 2019; Spector and Overholser, 2019; Kumar et al., 2020; Wang et al., 2021). What sets LeaP apart from many of these programs, however, is that LeaP (1) promotes skills development early on in biomedical training, (2) intentionally weaves diversity, equity and inclusion topics into the curriculum, (3) cultivates social interactions via a cohort model that supports trainee persistence and retention (Estrada et al., 2019), and (4) promotes not only the acquisition of new skills, but skill perdurance via coaching and longitudinal (four year) engagement. The value of LeaP derives from the intentional combination of these component parts.
Despite participant feedback being largely positive, LeaP is not without limitations. One limitation was the unit survey response rate of 50–63%. Reflecting upon this underwhelming response rate, we acknowledge that we should have provided time during individual sessions to complete surveys. That said, with intentional planning and scheduling, final focus group participation was 100%. Given that the unit survey feedback elicited less robust/complete data, greater weight was placed on the final focus group qualitative data due to 100% participation. A second limitation was the gender imbalance (majority female) of this inaugural cohort. Gender was not considered in LeaP selection and the initial cohort did not have balanced gender representation. This can, in part, be explained by an overall imbalance in the entire PhD matriculating class (∼75% identifying as female).
Based on promising early returns, it is tempting to propose rapid program growth/scaling to make the program accessible to anyone who wants to participate. While this is an admirable goal, it will be important to carefully reflect on what made the program meaningful to participants in the first place. Two themes stood out in the evaluations: trust/the cohort effect and the value of coaching. Indeed, most participants cited a strong culture of trust—between each other as well as with the program directors—as critically important. So how could/can growth occur while maintaining a safe and supportive environment? Parallel cohorts is one idea, although issues of cohort variability would have to be addressed. This includes careful selection and onboarding of any new facilitators and coaches. A team/task-based approach may help alleviate this concern, whereby curricular components (facilitation, coaching, etc.) could be split into teams guided by a lead facilitator or coach that could help set and maintain standards. Scaling LeaP effectively will take time, thoughtful consideration, and input from/consultation with education and leadership experts.
It is important to note that we do not yet know the long-term impact of LeaP. How effective are such student-centered leadership programs? This question is difficult to answer given often inadequate long-term follow-up and widely varying definitions of what it means to be “successful” (Onyura et al., 2019; Price et al., 2020). That said, with LeaP, we are anticipating lasting impact by leveraging a two-pronged approach consisting of (1) coaching to enhance self-reflection and accountability and (2) experiential/service-learning opportunities to reinforce and amplify self-efficacy and personal growth (Long et al., 2011; Boehmer et al., 2021). Both tactics are evidence-based leadership development strategies that we believe could be implemented as a component of formal PhD/advanced degree training, particularly for historically marginalized and underrepresented trainees.
What opportunities lie ahead for LeaP? Certainly, there is potential to adapt the model to other health professional programs at Mayo Clinic. To that end, there are numerous leadership development initiatives at other medical institutions (Long et al., 2011; Blumenthal et al., 2014; Meador et al., 2016; Mokshagundam et al., 2019; Brown, 2020; Coe et al., 2020; Kumar et al., 2020; Daaleman et al., 2021; James et al., 2021) that could integrate core LeaP concepts/approaches to tailor the experience to medical students, clinical fellows, or other professional degree seekers. Additionally, while trainee-focused initiatives are highly valuable and critically important, efforts to “train the trainer” to best support UR trainees (Norman et al., 2021) are needed and could be an interesting expansion of/addition to LeaP offerings. Another version of this approach is the concept of reverse mentoring (Garg and Singh, 2019; Gadomska-Lila, 2020). This experience could be particularly beneficial for LeaP participants as it would show them that learning and leadership are bi-directional and that while established faculty/leaders may have expertise in many areas, many are willing to seek out and engage in continued personal growth.
Finally, should a program like LeaP be available to both minority and majority trainees? While thinking about the answer to this question, it is important to remember and consider historical disparities in biomedical leadership as well as obstacles and challenges that underrepresented trainees continue to face today. Equity and fairness do not equate with equality and some disparities may need to be addressed with specialized programs such as LeaP, where a culture of trust and safety is paramount and may be compromised in open settings where “outsider” feelings persist. We opted to open some activities—notably the didactic seminars—to all graduate students, while the majority were targeted to LeaP scholars. Striking a balance of targeted and untargeted activities will require continuous feedback and reflection from all stakeholders moving forward. Ultimately, our hope is that the initial success of LeaP is recognized as a viable model of UR trainee leadership development, such that similar approaches are initiated, adapted, and sustained at biomedical institutions worldwide.
Data availability statement
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
MD and JD: conceptualization and manuscript preparation. MD and LS: data collection. All authors: program design and manuscript editing.
Acknowledgments
We thank the Kern National Network for Caring and Character in Medicine (KNN)/Mayo Clinic for generous financial support of this pilot initiative. We also thank Mayo Clinic Graduate School of Biomedical Sciences leaders, faculty, students, and staff who participated in and served on planning/advisory committees. We further wish to acknowledge the content expertise provided by individuals within Mayo Clinic Workforce Learning and Leadership Development.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ahmed, T., Johnson, J., Latif, Z., Kennedy, N., Javier, D., Stinson, K., et al. (2021). MyNRMN: a national mentoring and networking platform to enhance connectivity and diversity in the biomedical sciences. FASEB Bioadv. 3, 497–509. doi: 10.1096/fba.2020-00102
Blanchard, S. A., Rivers, R., Martinez, W., and Agodoa, L. (2019). Building the network of minority health research investigators: a novel program to enhance leadership and success of underrepresented minorities in biomedical research. Ethn. Dis. 29, 119–122. doi: 10.18865/ed.29.S1.119
Blumenthal, D. M., Bernard, K., Fraser, T. N., Bohnen, J., Zeidman, J., Stone, V. E., et al. (2014). Implementing a pilot leadership course for internal medicine residents: design considerations, participant impressions, and lessons learned. BMC Med. Educ. 14:257. doi: 10.1186/s12909-014-0257-2
Boehmer, K. R., Lucio Boschen, B., Doles, J. D., Lachman, N., Mays, D., Hedin, K. E., et al. (2021). Motivating self-efficacy in diverse biomedical science post-baccalaureate and graduate students through scientific conference implementation. Front. Educ. 6:774070. doi: 10.3389/feduc.2021.774070
Bond, M. R., Gammie, A. E., Lorsch, J. R., and Welch, M. (2020). Developing a culture of safety in biomedical research training. Mol. Biol. Cell 31, 2409–2414. doi: 10.1091/mbc.E20-03-0167
Bremner, N., Sakata, N., and Cameron, L. (2022). The outcomes of learner-centred pedagogy: a systematic review. Int. J. Educ. Dev. 94:102649. doi: 10.1016/j.ijedudev.2022.102649
Brown, N. J. (2020). Promoting the success of women and minority physician-scientists in academic medicine: a dean’s perspective. J. Clin. Invest. 130, 6201–6203. doi: 10.1172/JCI144526
Burgess, A., van Diggele, C., Roberts, C., and Mellis, C. (2020). Facilitating small group learning in the health professions. BMC Med. Educ. 20:457. doi: 10.1186/s12909-020-02282-3
Burner, T., Madsen, J., Zako, N., and Ismail, A. (2016). Three secondary school teachers implementing student-centred learning in Iraqi Kurdistan. Educ. Action Res. 25, 402–419. doi: 10.1080/09650792.2016.1162186
Byington, L., Keenan, H., Phillips, J. D., Childs, R., Wachs, E., Berzins, M. A., et al. (2016). A matrix mentoring model that effectively supports clinical and translational scientists and increases inclusion in biomedical research: lessons from the university of Utah. Acad. Med. 91, 497–502. doi: 10.1097/ACM.0000000000001021
Canti, L., Chrzanowska, A., Doglio, M. G., Martina, L., and Van Den Bossche, T. (2021). Research culture: science from bench to society. Biol. Open 10:bio058919. doi: 10.1242/bio.058919
Chance, N. (2021). Exploring the disparity of minority women in senior leadership positions in higher education in the United States and Peru. J. Compar. Int. Higher Educ. 13, 206–225. doi: 10.32674/jcihe.v13iSummer.3107
Cheng, H.-Y., and Ding, Q.-T. (2020). Examining the behavioral features of Chinese teachers and students in the learner-centered instruction. Eur. J. Psychol. Educ. 36, 169–186. doi: 10.1007/s10212-020-00469-2
Choi, M. K., Moon, J. E., Steinecke, A., and Prescott, J. E. (2019). Developing a culture of mentorship to strengthen academic medical centers. Acad. Med. 94, 630–633. doi: 10.1097/ACM.0000000000002498
Coe, C., Piggott, C., Davis, A., Hall, M. N., Goodell, K., Joo, P., et al. (2020). Leadership pathways in academic family medicine: focus on underrepresented minorities and women. Fam. Med. 52, 104–111. doi: 10.22454/FamMed.2020.545847
Connell, G. L., Donovan, D. A., Chambers, T. G., and Smith, M. (2016). Increasing the use of student-centered pedagogies from moderate to high improves student learning and attitudes about biology. CBE Life Sci. Educ. 15:ar3. doi: 10.1187/cbe.15-03-0062
Cornelius-White, J. (2016). Learner-centered teacher-student relationships are effective: a meta-analysis. Rev. Educ. Res. 77, 113–143. doi: 10.3102/003465430298563
CUPA-HR (2020). 2020 Professionals in Higher Education Annual Report. Knoxville, TN: College and University Professional Association for Human Resources.
Daaleman, T. P., Storrie, M., Beck Dallaghan, G., Smithson, S., Gilliland, K. O., Byerley, J. S., et al. (2021). Medical student leadership development through a business school partnership model: a case study and implementation strategy. J. Med. Educ. Curricular Dev. 8. doi: 10.1177/23821205211010479
Deiorio, N. M., Carney, P. A., Kahl, L. E., Bonura, E. M., and Juve, A. M. (2016). Coaching: a new model for academic and career achievement. Med. Educ. Online 21. doi: 10.3402/meo.v21.33480
Elmassian, K. (2014). The growing void of leadership training in medical education. Mich. Med. 113:28.
Estrada, M., Zhi, Q., Nwankwo, E., and Gershon, R. (2019). The influence of social supports on graduate student persistence in biomedical fields. CBE Life Sci. Educ. 18:ar39. doi: 10.1187/cbe.19-01-0029
Fry, R. K., Brian, K., and Funk, C. (2021). STEM Jobs See Uneven Progress in Increasing Gender, Racial and Ethnic Diversity. Washington, DC: Pew Research Center.
Furnham, A., Race, M.-C., and Rosen, A. (2014). Emotional intelligence and the Occupational Personality Questionnaire (OPQ). Front. Psychol. 5:935. doi: 10.3389/fpsyg.2014.00935
Gadomska-Lila, K. (2020). Effectiveness of reverse mentoring in creating intergenerational relationships. J. Organ. Change Manag. 33, 1313–1328. doi: 10.1108/JOCM-10-2019-0326
Garg, N., and Singh, P. (2019). Reverse mentoring: a review of extant literature and recent trends. Dev. Learn. Organ. Int. J. 34, 5–8. doi: 10.1108/DLO-05-2019-0103
Ghee, M., Collins, D., Wilson, V., and Pearson, W. (2014). The leadership alliance: twenty years of developing a diverse research workforce. Peabody J. Educ. 89, 347–367. doi: 10.1080/0161956X.2014.913448
Ghee, M., Keels, M., Collins, D., Neal-Spence, C., and Baker, E. (2016). Fine-tuning summer research programs to promote underrepresented students’ persistence in the STEM pathway. CBE Life Sci. Educ. 15:ar28. doi: 10.1187/cbe.16-01-0046
Goleman, D., Boyatzis, R., and McKee, A. (2009). Primal leadership. IEEE Eng. Manag. Rev. 37, 75–84. doi: 10.1109/EMR.2009.5235507
Gutierrez, A., Guerrero, L. R., McCreath, H. E., and Wallace, S. P. (2021). Mentoring experiences and publication productivity among early career biomedical investigators and trainees. Ethn. Dis. 31, 273–282. doi: 10.18865/ed.31.2.273
Hunt, V., Lareina, Y., Sara, P., and Sundiatu, D. F. (2018). Delivering Through Diversity. New York: McKinsey and Company.
James, M., Evans, M., and Mi, M. (2021). Leadership training and undergraduate medical education: a scoping review. Med. Sci. Educ. 31, 1501–1509. doi: 10.1007/s40670-021-01308-9
Joubert T., and Venter, N. (2013). “The occupational personality questionnaire,” in Psychological Assessment in South Africa, eds S. Laher and K. Cockcroft (New York, NY: NYU Press), 277–291. doi: 10.18772/22013015782.25
Kirkpatrick, D. L. (1998). Evaluating Training Programs: the Four Levels. San Francisco, CA: Berrett-Koehler Publishers.
Knowles, M. S. (1975). Self-Directed Learning: a Guide for Learners and Teachers. Chicago: Association Press.
Kozlowski, D., Larivière, V., Sugimoto, C. R., and Monroe-White, T. (2022). Intersectional inequalities in science. Proc. Natl. Acad. Sci. 119:e2113067119. doi: 10.1073/pnas.2113067119
Kumar, B., Swee, M. L., and Suneja, M. (2020). Leadership training programs in graduate medical education: a systematic review. BMC Med. Educ. 20:175. doi: 10.1186/s12909-020-02089-2
Lambert, W. M., Wells, M. T., Cipriano, M. F., Sneva, J. N., Morris, J. A., Golightly, L. M., et al. (2020). Career choices of underrepresented and female postdocs in the biomedical sciences. eLife 9:e48774. doi: 10.7554/eLife.48774
Loeng, S. (2020). Self-directed learning: a core concept in adult education. Educ. Res. Int. 2020, 1–12. doi: 10.1155/2020/3816132
Long, J. A., Lee, R. S., Federico, S., Battaglia, C., Wong, S., Earnest, M., et al. (2011). Developing leadership and advocacy skills in medical students through service learning. J. Public Health Manag. Pract. 17, 369–372. doi: 10.1097/PHH.0b013e3182140c47
Losch, S., Mühlberger, M. D., and Jonas, E. (2016). Comparing the effectiveness of individual coaching, self-coaching, and group training: how leadership makes the difference. Front. Psychol. 7:629. doi: 10.3389/fpsyg.2016.00629
Meador, B., Parang, B., Musser, M. A., Haliyur, R., Owens, D. A., Dermody, T. S., et al. (2016). A workshop on leadership for senior MD-PhD students. Med. Educ. Online 21:31534. doi: 10.3402/meo.v21.31534
Mokshagundam, S., Pitkin, J., Dekhtyar, M., Santen, S., Hammoud, M., Skochelak, S. E., et al. (2019). Engaging medical students in leadership development. Med. Sci. Educ. 29, 849–853. doi: 10.1007/s40670-019-00754-w
Neumann, J. W. (2013). Developing a new framework for conceptualizing “student-centered learning”. Educ. Forum 77, 161–175. doi: 10.1080/00131725.2012.761313
Norman, M. K., Mayowski, C. A., Wendell, S. K., Forlenza, M. J., Proulx, C. N., Rubio, D. M., et al. (2021). Delivering what we promised: outcomes of a coaching and leadership fellowship for mentors of underrepresented mentees. Int. J. Environ. Res. Public Health 18:4973. doi: 10.3390/ijerph18094793
Onyura, B., Crann, S., Tannenbaum, D., Whittaker, M. K., Murdoch, S., Freeman, R., et al. (2019). Is postgraduate leadership education a match for the wicked problems of health systems leadership? a critical systematic review. Perspect. Med. Educ. 8, 133–142. doi: 10.1007/S40037-019-0517-2
Price, T., Coverley, C. R., Arrington, A. K., Nfonsam, V. N., Morris-Wiseman, L., Riall, T. S., et al. (2020). Are we making an impact? a qualitative program assessment of the resident leadership, well-being, and resiliency program for general surgery residents. J. Surg. Educ. 77, 508–519. doi: 10.1016/j.jsurg.2019.12.003
Rockey, S. J. (2014). Mentorship matters for the biomedical workforce. Nat. Med. 20, 575–575. doi: 10.1038/nm0614-575
Rosenbloom, J. L., Gumpertz, M., Durodoye, R., Griffith, E., and Wilson, A. (2017). Retention and promotion of women and underrepresented minority faculty in science and engineering at four large land grant institutions. PLoS One 12:e0187285. doi: 10.1371/journal.pone.0187285
Spector, N. D., and Overholser, B. (2019). Leadership and professional development: sponsored; catapulting underrepresented talent off the cusp and into the game. J. Hosp. Med. 14:415. doi: 10.12788/jhm.3214
Starkey, L. (2017). Three dimensions of student-centred education: a framework for policy and practice. Crit. Stud. Educ. 60, 375–390. doi: 10.1080/17508487.2017.1281829
Stufflebeam, D. L., Madaus, G. F., and Kellaghan, T. (2000). Evaluation Models : Viewpoints on Educational and Human Services Evaluation, Evaluation in Education and Human Services. New York, NY: Kluwer Academic Publishers.
Taylor, D. C. M., and Hamdy, H. (2013). Adult learning theories: implications for learning and teaching in medical education: AMEE Guide No. 83. Med. Teacher 35, e1561–e1572. doi: 10.3109/0142159X.2013.828153
True, M. W., Folaron, I., Colburn, J. A., Wardian, J. L., Hawley-Molloy, J. S., Hartzell, J. D., et al. (2020). Leadership training in graduate medical education: time for a requirement? Mil. Med. 185, e11–e16. doi: 10.1093/milmed/usz140
Tucker Edmonds, B., Tori, A. J., Ribera, A. K., Allen, M. R., Dankoski, M. E., Rucker, S. Y., et al. (2022). Diversifying faculty leadership in academic medicine. Acad. Med. 97, 1459–1466. doi: 10.1097/ACM.0000000000004611
Van Velsor, E., McCauley, C. D., and Ruderman, M. N. (2010). The Center for Creative Leadership Handbook of Leadership Development. San Francisco, CA: Jossey-Bass.
Wang, Y. C., Brondolo, E., Monane, R., Kiernan, M., Davidson, K. W., The, M. A. V. E. N., et al. (2021). Introducing the MAVEN leadership training Initiative to diversify the scientific workforce. eLife 10:e69063. doi: 10.7554/eLife.69063
Keywords: leadership, diversity, equity, inclusion, stem education, professional development
Citation: Doles MD, Kang JY, Scholl LM and Doles JD (2023) Leadership in PhD (LeaP): A longitudinal leadership skill building program for underrepresented biomedical research trainees. Front. Educ. 8:1063075. doi: 10.3389/feduc.2023.1063075
Received: 06 October 2022; Accepted: 21 March 2023;
Published: 04 April 2023.
Edited by:
Margaret Grogan, Chapman University, United StatesReviewed by:
Carol Nash, University of Toronto, CanadaSunny Stout-Rostron, Stellenbosch University, South Africa
Copyright © 2023 Doles, Kang, Scholl and Doles. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mali D. Doles, ZG9sZXMubWFsaUBtYXlvLmVkdQ==; Jason D. Doles, amFkb2xlc0BpdS5lZHU=
 Mali D. Doles
Mali D. Doles Ji Yun Kang3
Ji Yun Kang3 Linda M. Scholl
Linda M. Scholl Jason D. Doles
Jason D. Doles