- 1The College of Traditional Chinese Medicine, Hunan University of Chinese Medicine, Changsha, China
- 2Provincial Key Laboratory of Traditional Chinese Medicine (TCM) Diagnostics, Hunan University of Chinese Medicine, Changsha, China
- 3Institute of Chinese Medicine Diagnosis, Hunan University of Chinese Medicine, Changsha, China
- 4School of Physical Education and Health, Hunan University of Technology and Business, Changsha, China
Objective: To investigate the effect of multiple eHealth-delivered lifestyle interventions on obesity-related anthropometric outcomes in children and adolescents.
Methods: The Medline (via PubMed), Embase, Cochrane Library, Web of Science, CBM, VIP, CNKI, and Wanfang electronic databases were systematically searched from their inception to March 18, 2022, for randomized controlled trials (RCTs). Meta-analyses were performed to investigate the effect of multiple eHealth-delivered lifestyle interventions on obesity-related anthropometric outcomes (body mass index [BMI], BMI Z-score, waist circumference, body weight, and body fat%). Two independent investigators reviewed the studies for accuracy and completeness. All included studies were evaluated using the Cochrane Risk-of-Bias (ROB) Tool.
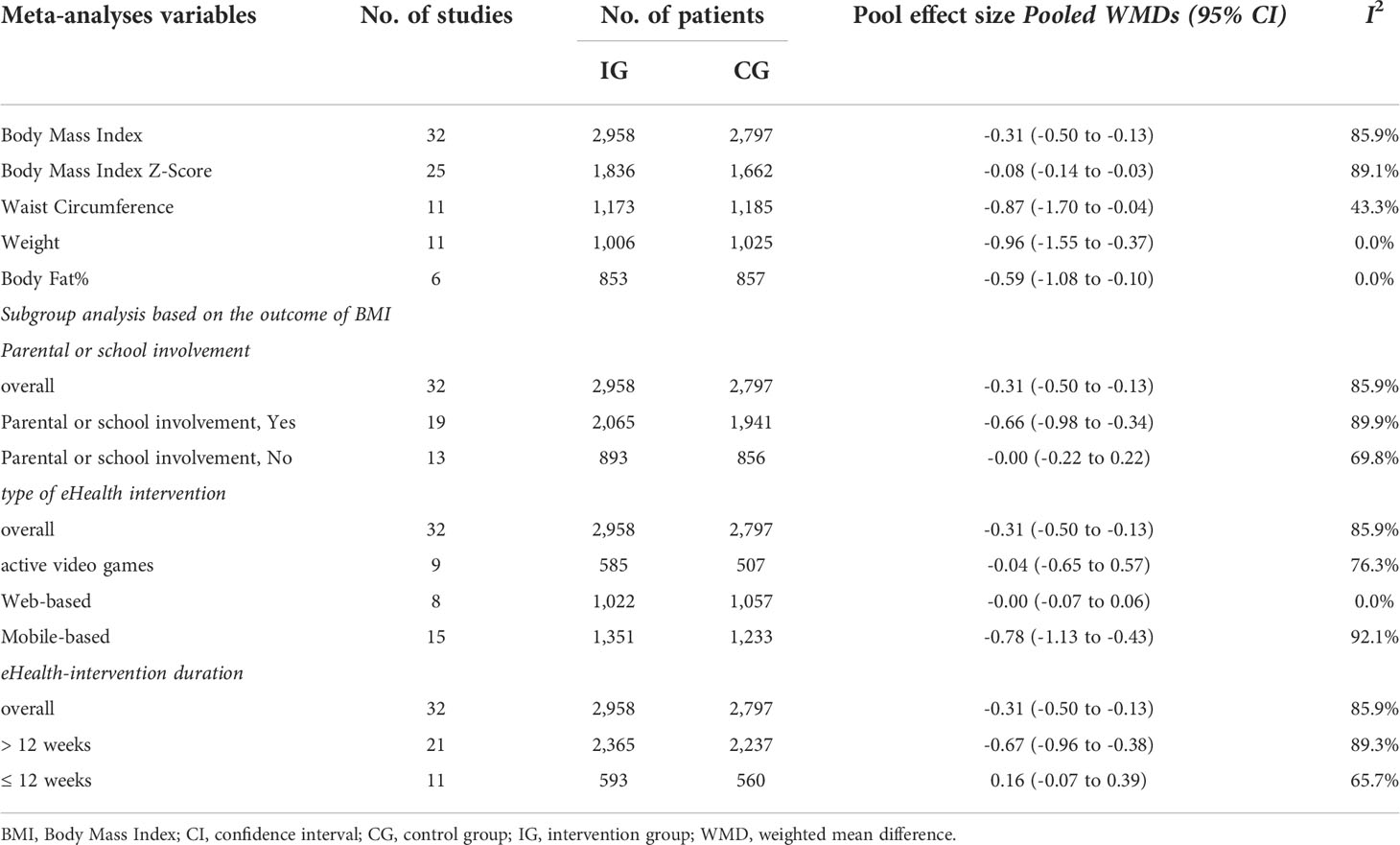
Results: Forty trials comprising 6,403 patients were selected for the meta-analysis. The eligible trials were published from 2006 to 2022. Compared with the control group, the eHealth-intervention group was more effective in reducing BMI (weighted mean difference [WMD] = −0.32, 95% confidence interval [CI]: −0.50 to −0.13, I2 = 85.9%), BMI Z-score (WMD = −0.08, 95% CI: −0.14 to −0.03, I2 = 89.1%), waist circumference (WMD = −0.87, 95% CI: −1.70 to −0.04, I2 = 43.3%), body weight (WMD = −0.96, 95% CI: −1.55 to −0.37, I2 = 0.0%), and body fat% (WMD = −0.59, 95% CI: −1.08 to −0.10, I2 = 0.0%). The subgroup analysis showed that parental or school involvement (WMD = −0.66, 95% CI: −0.98 to −0.34), eHealth-intervention duration of >12 weeks (WMD = −0.67, 95% CI: −0.96 to −0.38), and mobile-based interventions (WMD = −0.78, 95% CI: −1.13 to −0.43) had a significantly greater intervention effect size on BMI.
Conclusions: This review recommends that multiple eHealth-delivered lifestyle strategies may be useful for preventing or treating overweight and obesity among children and adolescents. However, our results should be cautiously interpreted due to certain limitations in our study.
Introduction
Obesity in children and adolescents has become one of the most serious public health problems of the 21st century. A population-based survey from 1975 to 2016 revealed that the number of children and adolescents with obesity has rapidly increased from 11 million to 124 million, with an additional 213 million in the overweight category (1). Obesity in children and adolescents increases the incidence of chronic diseases, such as cardiovascular disease, type 2 diabetes mellitus, and cancer (2, 3). A meta-analysis suggested that obesity in children and adolescents contributes to psychological problems (4). Furthermore, children and adolescents with overweight or obesity often have a higher risk of becoming adults with obesity than those with normal weight (5), and those with a higher body mass index (BMI) have a significantly higher risk of developing a wide range of diseases in adulthood (e.g., cardiomyopathy and cancers) than those with a lower BMI (3, 6). Moreover, such conditions will increase lifetime direct healthcare and indirect productivity costs, posing a substantial financial burden worldwide (7). In this situation, implementing an effective intervention to prevent and reduce overweight/obesity among children and adolescents becomes even more important.
At present, lifestyle interventions are the mainstay for the prevention and treatment of obesity among children and adolescents. In this article, we discuss lifestyle interventions, including dietary changes (nutritional education and provision of balanced meals), physical activity (exercise promotion and reduced sedentary behaviors), behavioral therapy (cognitive behavioral therapy), or any combination of these interventions; evidence shows that single and multiple lifestyle interventions are effective in weight loss (8). However, traditional lifestyle intervention methods (e.g., hospital-based weight management (9) may not be suitable for everyone, especially those with limited time, money, or mobility. With the development of electronic, information, and communication technologies, the internet and smart devices (e.g., smartphones and tablets) provide an alternative means to engage in healthy lifestyles, thereby overcoming time, funding, and geographical barriers. Digitally delivered interventions, commonly referred to as eHealth—the use of electronic tools in delivering healthcare (10)—provide a practical and reliable method to access health information and assess, prevent, and manage health conditions. eHealth technologies, such as web-based services and mobile phone applications, can stimulate a healthy lifestyle among individuals through self-monitoring, goal setting, evaluation, and feedback or recommendation generation (11). Studies have shown that the use of internet is almost universal among teenagers (12), and it has become a major resource for the repertory of health information (13). To date, electronic-delivered health interventions are increasingly being developed and evaluated. Digital health interventions for children and adolescents have indicated significant improvements in health behaviors and self-efficacy (14); thus, eHealth technologies are a feasible channel for providing health information.
Several review studies have attempted to evaluate the effect of eHealth interventions in preventing or treating overweight and obesity among children and adolescents (15–19); however, these studies have reported inconsistent evidence and several limitations that should be considered. First, these reviews were generally limited to only one form of eHealth technology, such as web-based (15), mobile-based (16), or digital game-based interventions (17); thus, the question of whether multiple eHealth interventions (i.e., an eHealth intervention delivered in any modality focused on any particular behavior) can be considered to improve overweight and obesity in children and adolescents remains unanswered. However, only two meta-analyses have evaluated eHealth interventions involving the weight control of children and adolescents; one of these reviews (18) was limited to a few selected trials (n = 8). As the results of that review were based on limited evidence, it may not be a suitable reference, and the inclusion criteria only focused on parent-focused interventions; parents are an agent of change in improving overweight and obesity in children and adolescents. Thus, it is difficult to draw robust conclusions. Another review (19) of the inclusion criteria only included trials published in English, and the intervention duration was limited to a minimum of 6 months, during which some relevant key trials may have been missed, possibly resulting in bias. Moreover, these reviews typically focused only on a single intervention [self-monitoring (15) and physical activity promotion (16, 17)]; therefore, there is insufficient evidence on the efficacy of multiple interventions. Nevertheless, as more studies are published, the literature should be further updated. Therefore, this review aims to determine the efficacy of multiple eHealth-delivered lifestyle interventions for the prevention or treatment of overweight and obesity in children and adolescents.
Methods
This review was developed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020 updated version) guidelines (20) and the Cochrane Collaboration Handbook recommendations (21). Ethical approval or patient consent was not required as all analyses were performed using the previously published studies.
We performed a comprehensive literature search in several databases, such as Medline (via PubMed), Embase, Cochrane Library, Web of Science, Chinese Biomedical Literature Database, Chinese Scientific Journal Database, Wanfang Data, and Chinese National Knowledge Infrastructure, to obtain all potentially eligible articles on multiple eHealth-delivered lifestyle interventions in children and adolescents with overweight or obesity from their inception to March 18, 2022. Moreover, searches were not restricted to the language or publication time.
Our search strategy was based on the Boolean logical operators by combining the Medical Subject Headings (MeSH) terms and free text-word terms. We used the following search terms: “Obesity,” “Overweight,” “Pediatric obesity,” “Telemedicine,” “eHealth,” “Children,” “Adolescents,” and “Randomized controlled trial.” Furthermore, we screened the top international journals (e.g., Nature Reviews Endocrinology, Lancet Diabetes & Endocrinology, and JAMA Pediatrics), famous publishers, major international conference proceedings, and gray literature (e.g., published noncommercial bibliography of doctors and masters as well as government reports) to reduce the unexpected omission of suitable lost studies that met our inclusion criterion. Reference lists of retrieved studies including these systematic reviews and meta-analyses were hand-searched to identify whether other relevant publications would meet our selection criteria. The exhaustive search strategies for each database are described in Supplement Materials.
Two independent investigators reviewed the studies for accuracy and completeness. The citation manager EndNote X9 (Thomson ISI Research Soft, Philadelphia, Pennsylvania, USA) was used to evaluate and filter all records. Following the assessment of titles and abstracts, the researchers obtained and reviewed the full texts of all articles. Any discrepancies between the two authors were addressed via discussion or consultation with a third author.
Eligibility criteria and selection process
Inclusion criteria were defined in terms of participants, interventions, comparisons, outcomes, and study design (PICOS) criteria reporting structure as follows:
Participants
Participants in this review were primarily children and adolescents aged 6–18 years with different body weights (underweight, healthy weight, overweight, and obese), BMI, and body composition.
Interventions
Acceptable treatments must involve the use of eHealth (e.g., internet, computers, tablets, telehealth, mobile applications, phone calls, text messages, and emails) for delivering lifestyle interventions (e.g., dietary changes, physical activity, or behavioral therapy for weight management, such as self-monitoring, goal setting, or providing feedback), but these interventions did not have to be solely delivered through eHealth.
Comparison
Studies were included if the control groups were treated according to standard or usual care, without any intervention, wait-list intervention, or another delivery mode (e.g., face-to-face), whereas studies were excluded if the control group used an eHealth intervention.
Outcomes
The obesity-related anthropometric outcomes were determined (e.g., BMI, BMI Z-score, waist circumference, body weight, and body fat%).
Study design
Only two-arm randomized controlled trials were included.
After removing the duplicates from our search, two authors independently screened titles and abstracts of the studies, and then the same two authors independently screened full manuscripts to finalize eligibility. Disagreements were resolved by discussion between the authors.
Data collection and quality assessment
Following the Cochrane Consumers and Communication Review Group’s data extraction template guideline (21), two reviewers independently verified studies for data extraction. Based on the aims of the pre-elaborated study, we collected information on the following items: first name, year of publication, study region, study design, total, population characteristics (age and sex), intervention method, intervention duration, and study outcomes.
The overall quality of evidence for each included RCT was assessed using the Cochrane Collaboration Risk-of-Bias Tool (21). The ROB tool has several domains: sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete outcome data, selective outcome data, and other sources of bias. Based on the established criteria, each domain was rated as “low,” “unclear,” or “high.” Emerging inconsistencies were resolved by consensus through discussion.
Statistical analyses
Data were analyzed according to the Cochrane Collaboration Handbook recommendations using a statistical software program (Stata, version 15.0; StataCorp, College Station, TX) (22). First, we measured heterogeneity within the meta-analysis using the I2 statistic and p-value for heterogeneity (Cochran’s Q statistic). A Cochran’s Q test result with p-value of <0.1 indicated statistically significant heterogeneity. The I2 values between 0% and 100% was used to measure the degree of heterogeneity, with threshold values of 0%–25%, 25%–50%, 50%–75%, and 75%–100% representing low, moderate, large, and extreme heterogeneity, respectively (23). Second, for dichotomous variables, the effect size was the odds ratio, whereas for continuous variables, the effect size was WMD, which were both reported with their 95% CI (24). Third, we visually evaluated the presence of publication bias using funnel plot and Egger test, with p < 0.05 indicating the presence of bias for funnel plot asymmetry. Finally, to further evaluate the heterogeneity and robustness of the results, additional subgroup analyses (parental or school involvement, type of eHealth intervention, and eHealth-intervention duration) were performed.
Results
Study selection and characteristics of included studies
In the initial target databases and manual search, 51,678 articles were collected. After comparing the retrieved titles, 13,601 articles were repeated and eliminated, and 38,077 remained. After screening the titles and abstracts, 393 potentially eligible articles for full-text screening were identified. Subsequently, the following articles were excluded: 16 articles with no full text or containing only the abstract, 110 studies that did not report appropriate outcomes, 25 studies that included electronic technology intervention in the control group, 90 studies where participants’ age was not within the range of 6–18 years, 108 articles with study design that did not meet the inclusion criteria (i.e., studies that were not RCTs or were 3/4-arm RCTs), and 4 studies that did not use electronic technology interventions. Finally, 40 (25–63) double-arm RCT studies were included for further meta-analysis (see Figure 1 for details).
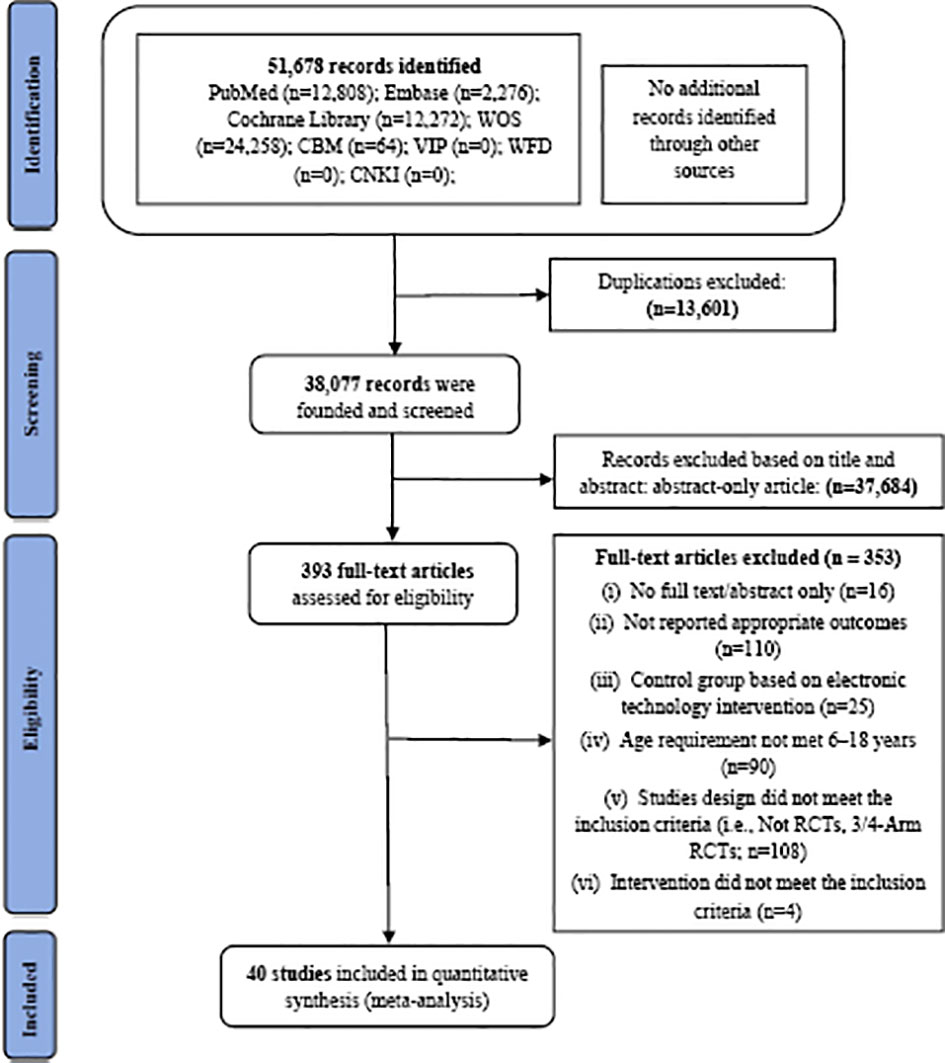
Figure 1 Literature review flowchart. CBM, Chinese Biomedical Literature Database; CNKI, China National Knowledge Infrastructure database; VIP, Chinese Scientific Journal Database; WFD, Wanfang database; WOS, Web of Science; RCT, randomized controlled trial.
The eligible trials were published from 2006 to 2022. These studies were most commonly performed in the USA (16 trials). Participants were randomized to the intervention and control groups, which included 3,283 and 3,120 participants, respectively. This study comprised 3,122 males and 2,808 females (some studies did not report sex), with a mean age of 12.38 years. The duration of interventions ranged from 6 weeks to 24 months. Table 1 presents the demographic characteristics of 40 studies.
Quality of included studies
Seventeen of these trials (26, 28, 29, 31, 32, 37, 39, 41, 42, 44, 51, 52, 54, 55, 57–59) applied random sequence generation and allocation concealment. Based on the design, blinding of the participants and personnel in interventions was difficult to achieve in any of these studies. In 14 trials (26, 28, 31, 32, 37, 41–43, 45, 46, 48, 51, 61, 62), the outcome assessments were blinded. Finally, none of these trials showed incomplete outcome data, and 8 trials (31, 33, 34, 41, 42, 55, 57, 59) reported intention-to-treat analyses. Further details of the overall and individual quality are summarized in Supplemental Figures S1, S2.
Meta-analyses
Body mass index
The meta-analysis included 32 trials evaluating the effect of intervention group and control group, and the pooled effect size estimate was based on a random-effects model, indicating that the eHealth-intervention group showed more clinical effect compared with the control group, with a statistically significant WMD of −0.32 (95% CI: −0.50 to −0.13, I2 = 85.9%) (Table 2). The funnel plot examination showed the presence of publication bias (Supplemental Figure S3), and the Egger test confirmed this outcome (p < 0.05).
Body mass index Z-score
A total of 25 studies focused on BMI Z-score. The results of these studies showed that patients who had received eHealth interventions showed more significant changes than the control group (WMD = −0.08, 95% CI: −0.14 to −0.03, I2 = 89.1%) (Table 2). The funnel plot did not reveal asymmetry (Supplemental Figure S4), and egger test suggested no publication bias (p > 0.05).
Waist circumference
Of the 11 studies that assessed waist circumference, pooled study results indicated that waist circumference significantly differed between the intervention and control groups (WMD = −0.87, 95% CI: −1.70 to −0.04, I2 = 43.3%) (Table 2). The funnel plot did not identify the asymmetry (Supplemental Figure S5).
Body weight
Overall, 11 studies recorded the endpoints of body weight. High-quality evidence showed that the group with eHealth interventions was more efficient in reducing body weight than the control group (WMD = −0.96, 95% CI: −1.55 to −0.37, I2 = 0.0%) (Table 2). The funnel plot suggested no publication bias (Supplemental Figure S6).
Body fat%
A total of six studies reported outcomes in terms of body fat%, and the body fat% was measured by bioelectrical impedance analysis (BIA) in all six studies. The results presented remarkable improvement in the intervention group compared with the control group (WMD = −0.59, 95% CI: −1.08 to −0.10, I2 = 0.0%) (Table 2).
Subgroup analyses
We performed several prespecified subgroup analyses (Table 2). A subgroup analysis revealed a significant difference in BMI in studies with parental or school involvement (WMD = −0.66, 95% CI: −0.98 to −0.34) and no statistically significant difference in trials without parental or school involvement (WMD = −0.00, 95% CI: −0.22 to 0.22). Another subgroup analysis found that the mobile-based intervention group showed a significant effect on BMI compared with the control group (WMD = −0.78, 95% CI: −1.13 to −0.43). No statistically significant differences were noted between the active video game (AVG)-based (WMD = −0.04, 95% CI: −0.65 to 0.57) and web-based (WMD = −0.00, 95% CI: −0.07 to 0.06) interventions. Further subgroup analysis demonstrated that an eHealth-intervention duration of >12 weeks (WMD = −0.67, 95% CI: −0.96 to −0.38) significantly reduced BMI, whereas that of ≤12 weeks did not have a significant effect on BMI (WMD = 0.16, 95% CI: −0.07 to 0.39).
Discussion
This review provides the existing evidence regarding the effect of eHealth interventions through the assessment of obesity-related outcomes. Overall, the meta-analysis demonstrated the use of eHealth-delivered lifestyle interventions, which could be an effective method to improve health-related outcomes in children and adolescents and is probably more effective than the standard or usual care. The subgroup analysis indicated that parental or school involvement, eHealth-intervention duration of >12 weeks, and mobile-based interventions had significant positive intervention effects on BMI.
This meta-analysis revealed that the use of eHealth-delivered lifestyle interventions can effectively improve the BMI, BMI Z-score, waist circumference, body weight, and body fat% of children and adolescents. Our findings were consistent with those of previous systematic reviews. To date, two reviews have evaluated the effect of eHealth interventions in children/adolescents (19) and adults (64) with overweight and obesity and showed significant reductions in obesity-related outcomes, such as BMI or BMI Z-score; however, the control group in these reviews included eHealth interventions. In contrast, the control group in our review excluded any eHealth intervention. Our method may draw more meaningful and reliable conclusions to support the benefits of eHealth-delivered lifestyle intervention for children and adolescents. Lifestyle interventions through caloric restriction increased physical activity and behavior strategies, which may contribute to a negative energy balance, resulting in weight loss; this is the most popular approach to combat obesity (8). The health benefits of weight loss can reduce the risk factors for type 2 diabetes and cardiovascular diseases and improve the quality of life and mental health (65). Achieving weight control requires sustained lifestyle changes; in other words, after individuals follow a healthy lifestyle and maintain their weight loss for 2–5 years, the chances of success increase dramatically (66). However, due to the complex interaction among biological, behavioral, environmental, and cognitive factors, individuals fail to maintain weight loss over time (67). eHealth technologies provide a unique opportunity for the implementation of self-management and lifestyle modification processes for continued weight control. Based on the design of eHealth interventions, combining the persuasive system design principles and behavioral change techniques applied in eHealth-intervention design can stimulate motivation and adherence and promote healthy lifestyles and weight loss maintenance (68). Moreover, children and adolescents with overweight and obesity are desired to lose weight to improve body image, and they enjoy using technology as part of the intervention (69). A previous review demonstrated that digital health interventions improved the dietary habits, physical activity level, screen time, and psychological well-being outcomes in children and adolescents and revealed an overall significant decrease in BMI-related metrics (e.g., BMI or BMI z-score) (14). These conclusions further suggest that eHealth-delivered lifestyle interventions can enhance weight loss by promoting healthy lifestyles, which plays an important role in preventing and treating overweight and obesity. Further, a previous study reported that the eHealth intervention was effective in maintaining the relative stability of children’s weight and BMI z-score and could control the increasing prevalence of being overweight/obesity in children (70). These findings further demonstrate the important role of eHealth interventions in maintaining normal weight. However, it is worth noting that body fat% in all included studies was measured using BIA. BIA is an inexpensive, simple, and safe method to estimate body composition, which is generally considered as a portable alternative to whole-body imaging (71). However, the accuracy of BIA may easily be affected by fluid retention and general health status (71). Therefore, the results of body fat% should be interpreted with caution.
A subgroup analysis found that eHealth interventions with parental or school involvement had significantly decreased the BMI compared with those without parental or school involvement. Data from several studies indicate that parental or school involvement in obesity-related health interventions is effective in weight control among children and adolescents (72–75). Parents are usually the main influence in shaping their children’s health habits, and schools are important institutions to help children develop healthy lifestyles. The benefits of parental involvement in obesity-related eHealth interventions may be attributed to parents determining the structure of their child’s home environment (such as providing healthy foods and identifying opportunities for activity) as well as supporting and encouraging healthy behaviors (74), and the benefits of school involvement are realized in schools’ infrastructure, curriculum, policies, environment, and staff having the potential to promote health-related behaviors among children (75).Another subgroup analysis revealed that mobile-based intervention had a more significant impact on BMI than the relevant active video game (AVG) intervention and web-based intervention. The results of this analysis are differ from those of other meta-analyses (14, 17). The discrepancy in these results may be due to the study design. For instance, in our study, the participants were selected without any weight criteria, whereas a previous study only included patients with overweight or obesity (14); our study analyzed the AVG effect size on BMI, whereas a previous study assessed the BMI/zBMI data (17). Therefore, some caution is needed to interpret our results. Further subgroup analysis showed that interventions with a duration of >12 weeks significantly decreased the BMI compared with those with a duration of ≤12 weeks. This result is consistent with those of other meta-analyses (76, 77). Lifestyle intervention effects would be greater if the duration of intervention is ≥3 months (78). To prevent weight regain, a 1-year weight loss maintenance program is also recommended (79). However, it has long been recognized that children and adolescents were prone to losing interest and had poor compliance (80). Therefore, when using eHealth for long-term interventions, targeted strategies [such as sustained monitoring and goal setting, home environment support, and peer interactions (81)] should be applied to maintain long-term interest and compliance in children and adolescents; thus, children and adolescents can successfully develop healthy lifestyle habits to maintain long-term behavioral changes.
This meta-analysis has several advantages. First, our meta-analysis is the first to provide evidence for the effect of multiple eHealth-delivered lifestyle strategies in preventing and treating overweight and obesity among children and adolescents. Second, we selected an intervention tool focusing on multiple eHealth technologies (electronic communication, telephone, web, and AVGs), which provides a comprehensive outcome that determined the efficacy of the latest health technology through an approach of quantitative analysis and a reference for future research designs or practical use. Third, our review focused on comprehensive lifestyle strategies (increasing physical activity and promoting healthy eating habits, education, and guidance), providing a comprehensive overview of lifestyle interventions to prevent and treat overweight and obesity in children and adolescents. This systematic review updated the evidence from the current literature on the effect of eHealth-delivered lifestyle strategies in preventing and treating overweight and obesity among children and adolescents.
A few uncontrollable limitations must be clarified. First, it is difficult to blind the participants due to the nature of intervention; thus, the rigor of double-blind RCTs may be nonexistent in this research area, and it cannot be excluded that intervention may have an impact on the clinical evaluation. Second, although 40 individually published trials were included in this meta-analysis, some of these were obtained from the same research group (26, 28, 36, 37, 47, 54) and often used similar populations, which may directly affect the generalizability of our evidence. The third limitation is the heterogeneity ranging from mild to high, which cannot be ignored in this meta-analysis. Furthermore, we included studies with different body weights of participants (including underweight, healthy-weight, overweight, and obese) in this review, which may affect the stability of our results. Finally, a lack of evaluation and oversight have resulted in some potential quality issues related to health information available on the Internet, including inaccurate or out-of-date information, and children and adolescents may refer to inaccurate health information. To address this problem, relevant guidelines should be considered for obtaining medical information.
Conclusion
The results of this review show a possible positive impact of eHealth-delivered lifestyle interventions on obesity-related outcomes in children and adolescents with overweight and obesity. Moreover, we found that parental or school involvement and sustained intervention over a long period significantly improved the BMI. Therefore, we cautiously suggest that practitioners, clinicians, and policymakers should consider eHealth as a model for preventing or intervening overweight and obesity in children and adolescents. More appropriate and high-quality relevant RCTs are needed in the future to determine the most effective obesity-related outcomes of eHealth interventions in preventing and treating obesity in children and adolescents.
Author contributions
L-TQ served as principal author and had full access to all the data in the study, takes responsibility for the accuracy of the data analysis, and the integrity of the data. L-TQ, G-XS and LL contributed to the conception and design. L-TQ, J-DZ and DW contributed to data acquisition and interpretation. L-TQ, G-XS and B-YF contributed to draft of the manuscript. G-XS and LL contributed to revise of the article and final approval.
Funding
This study was supported by the National Natural Science Foundation of China (81973670), the Natural Science Foundation of Hunan Province (2020JJ5418).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2022.999702/full#supplementary-material
Supplementary 1 | Search strategies.
Supplementary Figure 1 | Risk-of-bias graph.
Supplementary Figure 2 | Risk-of-bias summary.
Supplementary Figure 3 | Funnel plots of body mass index.
Supplementary Figure 4 | Funnel plots of body mass index Z-score.
Supplementary Figure 5 | Funnel plots of the waist circumference.
Supplementary Figure 6 | Funnel plots of body weight.
References
1. NCD Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet (2017) 390(10113):2627–42. doi: 10.1016/S0140-6736(17)32129-3
2. Zhao M, López-Bermejo A, Caserta CA, Medeiros CCM, Kollias A, Bassols J, et al. Metabolically healthy obesity and high carotid intima-media thickness in children and adolescents: International childhood vascular structure evaluation consortium. Diabetes Care (2019) 42(1):119–25. doi: 10.2337/dc18-1536
3. Bendor CD, Bardugo A, Pinhas-Hamiel O, Afek A, Twig G. Cardiovascular morbidity, diabetes and cancer risk among children and adolescents with severe obesity. Cardiovasc Diabetol (2020) 19(1):020–01052. doi: 10.1186/s12933-020-01052-1
4. Quek YH, Tam WWS, Zhang MWB, Ho RCM. Exploring the association between childhood and adolescent obesity and depression: a meta-analysis. Obes Rev (2017) 18(7):742–54. doi: 10.1111/obr.12535
5. Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev (2008) 9(5):474–88. doi: 10.1111/j.1467-789X.2008.00475.x
6. Robertson J, Schaufelberger M, Lindgren M, Adiels M, Schiöler L, Torén K, et al. Higher body mass index in adolescence predicts cardiomyopathy risk in midlife. Circulation (2019) 140(2):117–25. doi: 10.1161/CIRCULATIONAHA.118.039132
7. Hamilton D, Dee A, Perry IJ. The lifetime costs of overweight and obesity in childhood and adolescence: a systematic review. Obes Rev (2018) 19(4):452–63. doi: 10.1111/obr.12649
8. Salam RA, Padhani ZA, Das JK, Shaikh AY, Hoodbhoy Z, Jeelani SM, et al. Effects of lifestyle modification interventions to prevent and manage child and adolescent obesity: A systematic review and meta-analysis. Nutrients (2020) 12(8):2208. doi: 10.3390/nu12082208
9. Hampl S, Odar Stough C, Poppert Cordts K, Best C, Blackburn K, Dreyer Gillette ML. Effectiveness of a hospital-based multidisciplinary pediatric weight management program: Two-year outcomes of PHIT kids. Child Obes (2016) 12(1):20–5. doi: 10.1089/chi.2014.0119
10. Catwell L, Sheikh A. Evaluating eHealth interventions: the need for continuous systemic evaluation. PLoS Med (2009) 6(8):e1000126. doi: 10.1371/journal.pmed.1000126
11. Chatterjee A, Prinz A, Gerdes M, Martinez S. Digital interventions on healthy lifestyle management: Systematic review. J Med Internet Res (2021) 23(11):26931. doi: 10.2196/26931
12. Royant-Parola S, Londe V, Tréhout S, Hartley S. The use of social media modifies teenagers' sleep-related behavior. Encephale (2018) 44(4):321–8. doi: 10.1016/j.encep.2017.03.009
13. Gray NJ, Klein JD, Noyce PR, Sesselberg TS, Cantrill JA. Health information-seeking behaviour in adolescence: the place of the internet. Soc Sci Med (2005) 60(7):1467–78. doi: 10.1016/j.socscimed.2004.08.010
14. Kouvari M, Karipidou M, Tsiampalis T, Mamalaki E, Poulimeneas D, Bathrellou E, et al. Digital health interventions for weight management in children and adolescents: Systematic review and meta-analysis. J Med Internet Res (2022) 24(2):30675. doi: 10.2196/30675
15. Ho TJH, Lee CCS, Wong SN, Lau Y. Internet-Based self-monitoring interventions for overweight and obese adolescents: A systematic review and meta-analysis. Int J Med Inform (2018) 120:20–30. doi: 10.1016/j.ijmedinf.2018.09.019
16. He Z, Wu H, Yu F, Fu J, Sun S, Huang T, et al. Effects of smartphone-based interventions on physical activity in children and adolescents: Systematic review and meta-analysis. JMIR Mhealth Uhealth (2021) 9(2):22601. doi: 10.2196/22601
17. Oliveira CB, Pinto RZ, Saraiva BTC, Tebar WR, Delfino LD, Franco MR, et al. Effects of active video games on children and adolescents: A systematic review with meta-analysis. Scand J Med Sci Sports (2020) 30(1):4–12. doi: 10.1111/sms.13539
18. Hammersley ML, Jones RA, Okely AD. Parent-focused childhood and adolescent overweight and obesity eHealth interventions: A systematic review and meta-analysis. J Med Internet Res (2016) 18(7):e203. doi: 10.2196/jmir.5893
19. Azevedo LB, Stephenson J, Ells L, Adu-Ntiamoah S, DeSmet A, Giles EL, et al. The effectiveness of e-health interventions for the treatment of overweight or obesity in children and adolescents: A systematic review and meta-analysis. Obes Rev (2022) 23(2):7. doi: 10.1111/obr.13373
20. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj (2021) 29(372):n71. doi: 10.1136/bmj.n71
21. Higgins J, Green S. Cochrane handbook for systematic reviews of interventions, version 5.1.0. The Cochrane Collaboration (2013).
22. Higgins J, Green S. Cochrane handbook for systematic reviews for interventions, version 5.1.0. (2011).
23. Higgins J, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med (2002) 21(11):1539–58. doi: 10.1002/sim.1186
24. Larry V. Advances in statistical methods for meta-analysis. New Directions for Program Evaluation (1984) 1984(24):25–42. doi: 10.1002/ev.1376
25. Comeras-Chueca C, Villalba-Heredia L, Perez-Lasierra JL, Marín-Puyalto J, Lozano-Berges G, Matute-Llorente Á, et al. Active video games improve muscular fitness and motor skills in children with overweight or obesity. Int J Environ Res Public Health (2022) 19(5):2642. doi: 10.3390/ijerph19052642
26. Likhitweerawong N, Boonchooduang N, Kittisakmontri K, Chonchaiya W, Louthrenoo O. Effectiveness of mobile application on changing weight, healthy eating habits, and quality of life in children and adolescents with obesity: A randomized controlled trial. BMC Pediatr (2021) 21(1):499. doi: 10.1186/s12887-021-02980-x
27. Delli Bovi AP, Manco Cesari G, Rocco MC, Di Michele L, Rimauro I, Lugiero A, et al. Healthy Lifestyle Management of Pediatric Obesity with a Hybrid System of Customized Mobile Technology: The PediaFit Pilot Project. Nutrients (2021) 13(2):631. doi: 10.3390/nu13020631
28. Maddison R, Foley L, Ni Mhurchu C, Jiang Y, Jull A, Prapavessis H, et al. Effects of active video games on body composition: A randomized controlled trial. Am J Clin Nutr (2011) 94(1):156–63. doi: 10.3945/ajcn.110.009142
29. Graves LE, Ridgers ND, Atkinson G, Stratton G. The effect of active video gaming on children's physical activity, behavior preferences and body composition. Pediatr Exerc Sci (2010) 22(4):535–46. doi: 10.1123/pes.22.4.535
30. Maloney AE, Bethea TC, Kelsey KS, Marks JT, Paez S, Rosenberg AM, et al. A pilot of a video game (DDR) to promote physical activity and decrease sedentary screen time. Obesity (2008) 16(9):2074–80. doi: 10.1038/oby.2008.295
31. Jones M, Luce KH, Osborne MI, Taylor K, Cunning D, Doyle AC, et al. Randomized, controlled trial of an internet-facilitated intervention for reducing binge eating and overweight in adolescents. Pediatrics (2008) 121(3):453–62. doi: 10.1542/peds.2007-1173
32. Doyle AC, Goldschmidt A, Huang C, Winzelberg AJ, Taylor CB, Wilfley DE. Reduction of overweight and eating disorder symptoms via the Internet in adolescents: a randomized controlled trial. J Adolesc Health (2008) 43(2):172–9. doi: 10.1016/j.jadohealth.2008.01.011
33. Heinicke BE, Paxton SJ, McLean SA, Wertheim EH. Internet-delivered targeted group intervention for body dissatisfaction and disordered eating in adolescent girls: a randomized controlled trial. J Abnorm Child Psychol (2007) 35(3):379–91. doi: 10.1007/s10802-006-9097-9
34. Schiel R, Vahl T, Bieber G. InterLearn - Interactive Learning and Telemedical Follow-Up for Children and Adolescents with Overweight and Obesity. Diabetologie und Stoffwechsel (2015) 10(6):314–21. doi: 10.1055/s-0041-108741
35. Nollen NL, Mayo MS, Carlson SE, Rapoff MA, Goggin KJ, Ellerbeck EF. Mobile technology for obesity prevention: a randomized pilot study in racial- and ethnic-minority girls. Am J Prev Med (2014) 46(4):404–8. doi: 10.1016/j.amepre.2013.12.011
36. Maddison R, Mhurchu CN, Jull A, Prapavessis H, Foley LS, Jiang Y. Active video games: the mediating effect of aerobic fitness on body composition. Int J Behav Nutr Phys Act (2012) 9(1):54. doi: 10.1186/1479-5868-9-54
37. Likhitweerawong N, Boonchooduang N, Kittisakmontri K, Chonchaiya W, Louthrenoo. O. Short-Term Outcomes of Tablet/Smartphone-Based (OBEST) Application Among Obese Thai School-Aged Children and Adolescents: A Randomized Controlled Trial. Obes Med (2020), 100287. doi: 10.1016/j.obmed.2020.100287
38. Lau PW, Wang JJ, Maddison R. A Randomized-Controlled Trial of School-Based Active Video game Intervention on Chinese Children's Aerobic Fitness, Physical Activity Level, and Psychological Correlates. Games Health J (2016) 5(6):405–12. doi: 10.1089/g4h.2016.0057
39. Chen JL, Guedes CM, Lung AE. Smartphone-based Healthy Weight Management Intervention for Chinese American Adolescents: Short-term Efficacy and Factors Associated With Decreased Weight. J Adolesc Health (2019) 64(4):443–9. doi: 10.1016/j.jadohealth.2018.08.022
40. Baños RM, Oliver E, Navarro J, Vara MD, Cebolla A, Lurbe E, et al. Efficacy of a cognitive and behavioral treatment for childhood obesity supported by the ETIOBE web platform. Psychol Health Med (2019) 24(6):703–13. doi: 10.1080/13548506.2019.1566622
41. Staiano AE, Beyl RA, Guan W, Hendrick CA, Hsia DS, Newton RL Jr.. Home-based exergaming among children with overweight and obesity: A randomized clinical trial. Pediatr Obes (2018) 13(11):724–33. doi: 10.1111/ijpo.12438
42. Staiano AE, Marker AM, Beyl RA, Hsia DS, Katzmarzyk PT, Newton RL. A randomized controlled trial of dance exergaming for exercise training in overweight and obese adolescent girls. Pediatr Obes (2017) 12(2):120–8. doi: 10.1111/ijpo.12117
43. Fleischman A, Hourigan SE, Lyon HN, Landry MG, Reynolds J, Steltz SK, et al. Creating an integrated care model for childhood obesity: a randomized pilot study utilizing telehealth in a community primary care setting. Clin Obes (2016) 6(6):380–8. doi: 10.1111/cob.12166
44. Babic MJ, Smith JJ, Morgan PJ, Lonsdale C, Plotnikoff RC, Eather N, et al. Intervention to reduce recreational screen-time in adolescents: Outcomes and mediators from the 'Switch-Off 4 Healthy Minds' (S4HM) cluster randomized controlled trial. Prev Med (2016) 91:50–7. doi: 10.1016/j.ypmed.2016.07.014
45. Nguyen B, Shrewsbury VA, O' Connor J, Steinbeck KS, Hill AJ, Shah S, et al. Two-year outcomes of an adjunctive telephone coaching and electronic contact intervention for adolescent weight-loss maintenance: the Loozit randomized controlled trial. Int J Obes (2013) 37(3):468–72. doi: 10.1038/ijo.2012.74
46. Lubans DR, Morgan PJ, Okely AD, Dewar D, Collins CE, Batterham M, et al. Preventing Obesity Among Adolescent Girls: One-Year Outcomes of the Nutrition and Enjoyable Activity for Teen Girls (NEAT Girls) Cluster Randomized Controlled Trial. Arch Pediatr Adolesc Med (2012) 166(9):821–7. doi: 10.1001/archpediatrics.2012.41
47. Smith JJ, Morgan PJ, Plotnikoff RC, Dally KA, Salmon J, Okely AD, et al. Smart-phone obesity prevention trial for adolescent boys in low-income communities: the ATLAS RCT. Pediatrics (2014) 134(3):e723–31. doi: 10.1542/peds.2014-1012
48. Murphy EC, Carson L, Neal W, Baylis C, Donley D, Yeater R. Effects of an exercise intervention using Dance Dance Revolution on endothelial function and other risk factors in overweight children. Int J Pediatr Obes (2009) 4(4):205–14. doi: 10.3109/17477160902846187
49. Wright JA, Phillips BD, Watson BL, Newby PK, Norman GJ, Adams WG. Randomized trial of a family-based, automated, conversational obesity treatment program for underserved populations. Obesity (2013) 21(9):E369–78. doi: 10.1002/oby.20388
50. Mohammed Nawi A, Che Jamaludin FI. Effect of Internet-based Intervention on Obesity among Adolescents in Kuala Lumpur: A School-based Cluster Randomised Trial. Malays J Med Sci (2015) 22(4):47–56.
51. Bagherniya M, Mostafavi Darani F, Sharma M, Maracy MR, Allipour Birgani R, Ranjbar G, et al. Assessment of the Efficacy of Physical Activity Level and Lifestyle Behavior Interventions Applying Social Cognitive Theory for Overweight and Obese Girl Adolescents. J Res Health Sci (2018) 18(2):e00409.
52. Christison AL, Evans TA, Bleess BB, Wang H, Aldag JC, Binns HJ. Exergaming for Health: A Randomized Study of Community-Based Exergaming Curriculum in Pediatric Weight Management. Games Health J (2016) 5(6):413–21. doi: 10.1089/g4h.2015.0097
53. Coknaz D, Mirzeoglu AD, Atasoy HI, Orcid Id, Alkoy S, Coknaz H, et al. A digital movement in the world of inactive children: favourable outcomes of playing active video games in a pilot randomized trial. Eur J Pediatr (2019) 178(10):1567–76. doi: 10.1007/s00431-019-03457-x
54. Lubans DR, Smith JJ, Plotnikoff RC, Dally KA, Okely AD, Salmon J, et al. Assessing the sustained impact of a school-based obesity prevention program for adolescent boys: the ATLAS cluster randomized controlled trial. Int J Behav Nutr Phys Act (2016) 13(1):92. doi: 10.1186/s12966-016-0420-8
55. Currie J, Collier D, Raedeke TD, Lutes LD, Kemble CD, DuBose KD. The effects of a low-dose physical activity intervention on physical activity and body mass index in severely obese adolescents. Int J Adolesc Med Health (2017). doi: 10.1515/ijamh-2016-0121
56. Brito Beck da Silva K, Ortelan N, Giardini Murta S, Sartori I, Couto RD, Leovigildo Fiaccone R, et al. Evaluation of the Computer-Based Intervention Program Stayingfit Brazil to Promote Healthy Eating Habits: The Results from a School Cluster-Randomized Controlled Trial. Int J Environ Res Public Health (2019) 16(10):1674. doi: 10.3390/ijerph16101674
57. Kennedy SG, Smith JJ, Morgan PJ, Peralta LR, Hilland TA, Eather N, et al. Implementing Resistance Training in Secondary Schools: A Cluster Randomized Controlled Trial. Med Sci Sports Exerc (2018) 50(1):62–72. doi: 10.1249/MSS.0000000000001410
58. Maddison R, Marsh S, Foley L, Epstein LH, Olds T, Dewes O, et al. Screen-Time Weight-loss Intervention Targeting Children at Home (SWITCH): a randomized controlled trial. Int J Behav Nutr Phys Act (2014) 11(1):1–11. doi: 10.1186/s12966-014-0111-2
59. Trost SG, Sundal D, Foster GD, Lent MR, Vojta D. Effects of a pediatric weight management program with and without active video games a randomized trial. JAMA Pediatr (2014) 168(5):407–13. doi: 10.1001/jamapediatrics.2013.343637
60. Jago R, Baranowski T, Baranowski JC, Thompson D, Cullen KW, Watson K, et al. Fit for Life Boy Scout badge: outcome evaluation of a troop and Internet intervention. Prev Med (2006) 42(3):181–7. doi: 10.1016/j.ypmed.2005.12.010
61. Wagener TL, Fedele DA, Mignogna MR, Hester CN, Gillaspy SR. Psychological effects of dance-based group exergaming in obese adolescents. Pediatr Obes (2012) 7(5):e68–74. doi: 10.1111/j.2047-6310.2012.00065.x
62. Jones. Reducing binge eating M. and overweight in adolescents via the Internet. Dissertations Theses - Gradworks (2010).
63. Li C, Zhao H, Yang H, Lu J. Effects of remote exercise support on weight loss and maintenance in obese adolescents. Chin J Modern Nurs (2020) 26(20):5. doi: 10.3760/cma.j.cn115682-20191211-04545
64. Hutchesson MJ, Rollo ME, Krukowski R, Ells L, Harvey J, Morgan PJ, et al. eHealth interventions for the prevention and treatment of overweight and obesity in adults: a systematic review with meta-analysis. Obes Rev (2015) 16(5):376–92. doi: 10.1111/obr.12268
65. Wadden TA, Tronieri JS, Butryn ML. Lifestyle modification approaches for the treatment of obesity in adults. Am Psychol (2020) 75(2):235–51. doi: 10.1037/amp0000517
66. Christiansen T, Bruun JM, Madsen EL, Richelsen B. Weight loss maintenance in severely obese adults after an intensive lifestyle intervention: 2- to 4-year follow-up. Obesity (2007) 15(2):413–20. doi: 10.1038/oby.2007.530
67. MacLean PS, Wing RR, Davidson T, Epstein L, Goodpaster B, Hall KD, et al. NIH Working group report: Innovative research to improve maintenance of weight loss. Obesity (2015) 23(1):7–15. doi: 10.1002/oby.20967
68. Asbjørnsen RA, Wentzel J, Smedsrød ML, Hjelmesæth J, Clark MM, Solberg Nes L, et al. Identifying persuasive design principles and behavior change techniques supporting end user values and needs in eHealth interventions for long-term weight loss maintenance: Qualitative study. J Med Internet Res (2020) 22(11):22598. doi: 10.2196/22598
69. Jones HM, Al-Khudairy L, Melendez-Torres GJ, Oyebode O. Viewpoints of adolescents with overweight and obesity attending lifestyle obesity treatment interventions: a qualitative systematic review. Obes Rev (2019) 20(1):156–69. doi: 10.1111/obr.12771
70. Rerksuppaphol L, Rerksuppaphol S. Internet Based obesity prevention program for Thai school children- a randomized control trial. J Clin Diagn Res (2017) 11(3):SC07–11. doi: 10.7860/JCDR/2017/21423.9368
71. Tosato M, Marzetti E, Cesari M, Savera G, Miller RR, Bernabei R, et al. Measurement of muscle mass in sarcopenia: from imaging to biochemical markers. Aging Clin Exp Res (2017) 29(1):19–27. doi: 10.1007/s40520-016-0717-0
72. Gittelsohn J, Kumar MB. Preventing childhood obesity and diabetes: is it time to move out of the school? Pediatr Diabetes (2007) 9:55–69. doi: 10.1111/j.1399-5448.2007.00333.x
73. Niemeier BS, Hektner JM, Enger KB. Parent participation in weight-related health interventions for children and adolescents: a systematic review and meta-analysis. Prev Med (2012) 55(1):3–13. doi: 10.1016/j.ypmed.2012.04.021
74. Young KM, Northern JJ, Lister KM, Drummond JA, O' Brien WH. A meta-analysis of family-behavioral weight-loss treatments for children. Clin Psychol Rev (2007) 27(2):240–9. doi: 10.1016/j.cpr.2006.08.003
75. Brown T, Summerbell C. Systematic review of school-based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: an update to the obesity guidance produced by the national institute for health and clinical excellence. Obes Rev (2009) 10(1):110–41. doi: 10.1111/j.1467-789X.2008.00515.x
76. Yen HY, HL C. The effectiveness of wearable technologies as physical activity interventions in weight control: A systematic review and meta-analysis of randomized controlled trials. Obes Rev (2019) 20(10):1485–93. doi: 10.1111/obr.12909
77. Cavero-Redondo I, Martinez-Vizcaino V, Fernandez-Rodriguez R, Saz-Lara A, Pascual-Morena C, Álvarez-Bueno C. Effect of behavioral weight management interventions using lifestyle mHealth self-monitoring on weight loss: A systematic review and meta-analysis. Nutrients (2020) 12(7):1977. doi: 10.3390/nu12071977
78. Hebden L, Chey T, Allman-Farinelli M. Lifestyle intervention for preventing weight gain in young adults: a systematic review and meta-analysis of RCTs. Obes Rev (2012) 13(8):692–710. doi: 10.1111/j.1467-789X.2012.00990.x
79. Webb VL, Wadden TA. Intensive lifestyle intervention for obesity: Principles, practices, and results. Gastroenterology (2017) 152(7):1752–64. doi: 10.1053/j.gastro.2017.01.045
80. Schaefer SE, Ching CC, Breen H, Bruce German J. Wearing, thinking, and moving: Testing the feasibility of fitness tracking with urban youth. Am J Health Educ (2016) 47(1):8–16. doi: 10.1080/19325037.2015.1111174
Keywords: eHealth, lifestyle interventions, overweight and obesity, children and adolescents, meta-analysis
Citation: Qiu L-T, Sun G-X, Li L, Zhang J-D, Wang D and Fan B-Y (2022) Effectiveness of multiple eHealth-delivered lifestyle strategies for preventing or intervening overweight/obesity among children and adolescents: A systematic review and meta-analysis. Front. Endocrinol. 13:999702. doi: 10.3389/fendo.2022.999702
Received: 21 July 2022; Accepted: 16 August 2022;
Published: 05 September 2022.
Edited by:
Evan P. Nadler, Children’s National Hospital, United StatesReviewed by:
Eleanor Mackey, Children’s National Hospital, United StatesDominique R. Williams, College of Medicine, The Ohio State University, United States
Copyright © 2022 Qiu, Sun, Li, Zhang, Wang and Fan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gui-Xiang Sun, ODQ2NjM0MjNAcXEuY29t; Ling Li, bGlsaW5nMTA0OUBobnVjbS5lZHUuY24=
 Li-Ting Qiu
Li-Ting Qiu Gui-Xiang Sun1,2,3*
Gui-Xiang Sun1,2,3* Ling Li
Ling Li Ji-Dong Zhang
Ji-Dong Zhang