- 1First Clinical Medical College, Shandong University of Traditional Chinese Medicine, Jinan, China
- 2Department of Traditional Chinese Medicine, Qilu Hospital, Cheeloo College of Medicine, Shandong University, Jinan, China
- 3Department of Ophthalmology, Qilu Hospital, Cheeloo College of Medicine, Shandong University, Jinan, China
- 4Department of Nursing, Qilu Hospital, Cheeloo College of Medicine, Shandong University, Jinan, China
- 5Department of Neurosurgery, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, Jinan, China
Objective: To evaluate the efficacy and safety of combined traditional Chinese medicine in the adjuvant treatment of proliferative diabetic retinopathy (PDR) by Meta-analysis.
Methods: PubMed, Embase, Web of Science, Cochrane Library, China National Knowledge Infrastructure (CNKI), Wanfang databases were searched by computer. Random controlled clinical trials (RCTS) using traditional Chinese medicine as adjuvant therapy for proliferative diabetic retinopathy were screened, and Stata16.0 software was used to perform meta-analysis on the final included literatures.
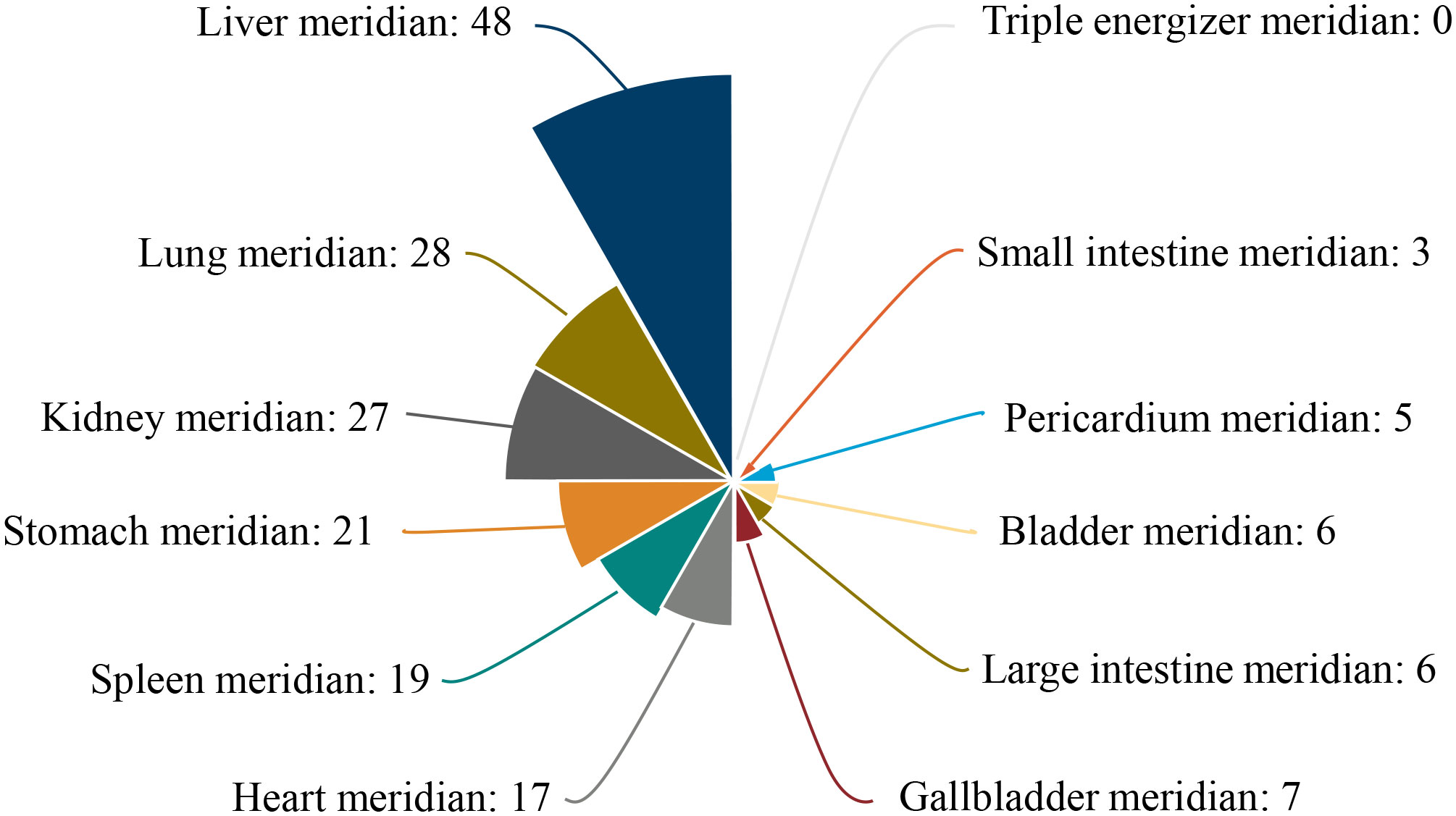
Results: A total of 18 studies involving 1392 patients were included. Meta-analysis showed that the clinical effective rate OR=2.99 (CI: 2.18-4.10, I2 = 42.7%, P<0.05); Visual acuity MD=0.10(CI: 0.06-0.13, I2 = 0%, P<0.05); Fundus efficacy OR=5.47 (CI: 1.33-22.51, I2 = 71.4%, P<0.05); Neovascularisation regression rate OR=8 (CI: 3.83-16.71, I2 = 30.1%, P<0.05); Macular foveal thickness MD=-44.24 (CI: -84.55–3.93, I2 = 95.6%, P<0.05); Absorption of vitreous hemorrhage OR=4.7 (CI: 2.26-9.77, I2 = 0%, P<0.05); Fasting blood glucose MD=-0.23, (CI: -0.38–0.07, I2 = 0%, P<0.05); 2h postprandial blood glucose MD=-0.19 (CI: -0.52-0.14, I2 = 0%, P=0.25). From the results, the combined Chinese medicine adjuvant therapy showed better efficacy than the control group. A total of 69 kinds of traditional Chinese medicine were involved in 18 studies, among which the top four applied frequencies were Panax notoginseng, Rehmannia rehmannii, Astragalus membranaceus and Poria cocos. Most of the medicines were sweet and bitter in taste, the qi tended to be slight cold and cold, and the meridian tropism belongs to the liver meridian.
Conclusion: The combination of traditional Chinese medicine adjuvant therapy has a good curative effect on PDR patients. However, the relevant clinical trials are few and more high-quality clinical trials are still needed, what’s more the attention should be paid to the exploration of its safety.
1 Introduction
Diabetic retinopathy (DR) is one of the most common clinical complications of diabetes mellitus (DM). Of the 537 million diabetic patients worldwide, DR accounts for about 22.27% and has become the leading cause of blindness in middle-aged and older adults (1). As a disease with a large potential patient population base and a high probability of blindness and disability, DR brings serious life hindrances and mental suffering to patients while adding heavy economic pressure and burden to society. As the world’s largest diabetes population, China has a staggering 140.9 million people with diabetes, with the number of diabetic retinopathy patients estimated to be between 34 and 53 million (2). The search for clinical drugs that can effectively treat diabetic retinopathy is an urgent problem worldwide, especially in China.
Chinese medicine has been handed down in China for thousands of years. A large amount of research evidence shows that it has excellent therapeutic effects on diabetes and its complications by reducing blood glucose, lipid profile and improving other metabolic indicators (3). At the same time, many studies have also proved that Chinese herbal therapy has a better intervention effect on DR (4, 5). In China’s extensive clinical practice, not only traditional Chinese medicine practitioners commonly utilize herbal remedies to treat DR, while Western medical practitioners also frequently incorporate certain Chinese patent medicines to complement their treatment regimens for DR.
However, it is worth noting that DR can be divided into two types: Non-proliferative diabetic retinopathy (NPDR) and Proliferative diabetic retinopathy (PDR) based on the presence of neovascularization, and the two have distinct pathological features (6). Currently, research on TCM treatment for DR in China focuses mostly on the NPDR stage, where clinical manifestations include blood stasis lesions such as retinal microaneurysms and venous beading, and herbal remedies are often used to improve retinal microcirculation, with their efficacy widely recognized (7). However, the effectiveness and safety of TCM treatment for PDR, in which new blood vessels grow in the retina, are still debated. High-level research evidence is urgently needed to determine whether TCM treatment can help improve clinical symptoms in PDR patients and whether it is safe to use in this stage. To this end, we conducted this study with the aim of addressing this controversy. Additionally, to better guide the selection and subsequent research of TCM treatments, we summarized the frequency, four natures and five flavors, and meridian tropism of the herbal medicines included in the studies, aiming to explore the laws of TCM treatment for PDR.
2 Methods
2.1 Literature search
This study searched PubMed, Web of Science, Cochrane Library, Embase database, China Knowledge Network, Wanfang to include randomized clinical controlled trials of combination treatment of PDR with Chinese herbs since the establishment of the database until October 8, 2022.
2.2 Inclusion criteria
(1) Study type: a randomized controlled trial of Chinese herbal medicine for treating PDR, language not limited.
(2) Study subjects: all included cases must meet the pathological diagnostic criteria for PDR.
(3) Interventions: The interventions in the control group can be conventional Western medical treatment, such as drugs, photocoagulation or surgery, or blank; the interventions in the trial group should be based on conventional Western medical treatment combined with the use of Chinese herbal medicine as an adjunct, which can be herbal medicine, compound prescriptions, Chinese patent medicines, injections, ion introduction.
(4) Outcome indicators: Assess post-treatment outcomes involving at least one clinical efficacy, visual acuity, blood glucose, fundus efficacy, regression of neovascularisation, macular central recess thickness, and absorption of vitreous blood accumulation.
2.3 Exclusion criteria
(1) Type of literature is a review, animal test, or another non-clinical trial article.
(2) Non-simultaneous randomized controlled clinical trials, lack of randomization of groupings.
(3) The treatment method does not include herbal medicine as an adjunctive treatment.
(4) Lack of observation on relevant indicators.
(5) Inappropriate statistical methods or severe errors in the data.
2.4 Data extraction
Two researchers (Baogeng Huai and Baosha Huai) independently screened the literature according to the above criteria using EndNote X9 software, cross-checked, and controversial literature was decided by a third party (Changling Li) in consultation. Judgments were made based on whether the study population belonged to PDR patients, whether the intervention method involved TCM treatment, and whether there were any logical loopholes or data errors in the research. An Excel sheet was used to prepare an information extraction form based on the study content, and the data were extracted as follows.
(1) Basic information about the literature: first author, date of publication.
(2) Trial subjects: sample size of the trial and control groups.
(3) Interventions: type, dosage form, a dose of Chinese herbal medicine and control drugs, and duration of intervention.
(4) Outcome indicators: clinical efficacy, visual acuity, fundus efficacy criteria, neovascularization regression rate, central macular recess thickness.
2.5 Evaluation of literature quality and risk of bias
The risk of bias assessment tool of the Cochrane Systematic Reviews was used to evaluate the included studies, including randomization, allocation concealment, whether blinding was used, completeness of outcome indicators, whether study results were reported selectively, and other biases. The evaluation results were categorized into three risk levels: “high risk,” “low risk,” and “uncertain.”
2.6 Statistical methods
The study was analyzed using Stata16.0 software. The mean difference (MD) was selected for the analysis of the effect of measures, and the odds ratio (OR) was selected as the effect size for dichotomous variables, both using a 95% confidence interval (CI). P-values and I2 were calculated to determine whether heterogeneity existed among the included studies, and if heterogeneity was observed (P<0.05, or I2>50%), a random-effects model was selected; if no heterogeneity was observed (P>0.05, and I2≤50%), a fixed-effects model was selected. α = 0.05 was used as the meta-analysis test level. Publication bias was evaluated using the funnel plot, Begg’s test, and Egger’s test.
3 Results
3.1 Basic process for inclusion in the literature
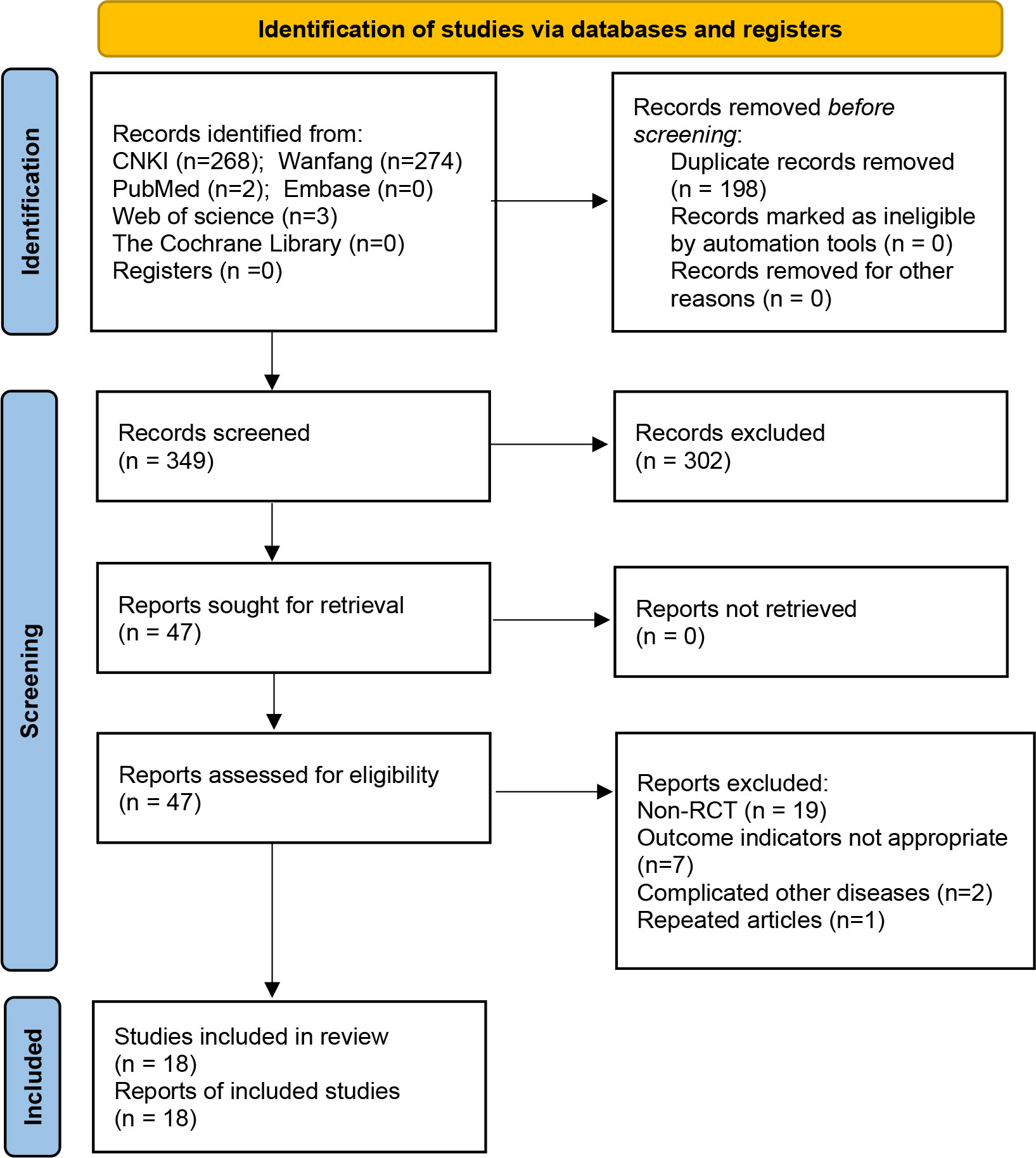
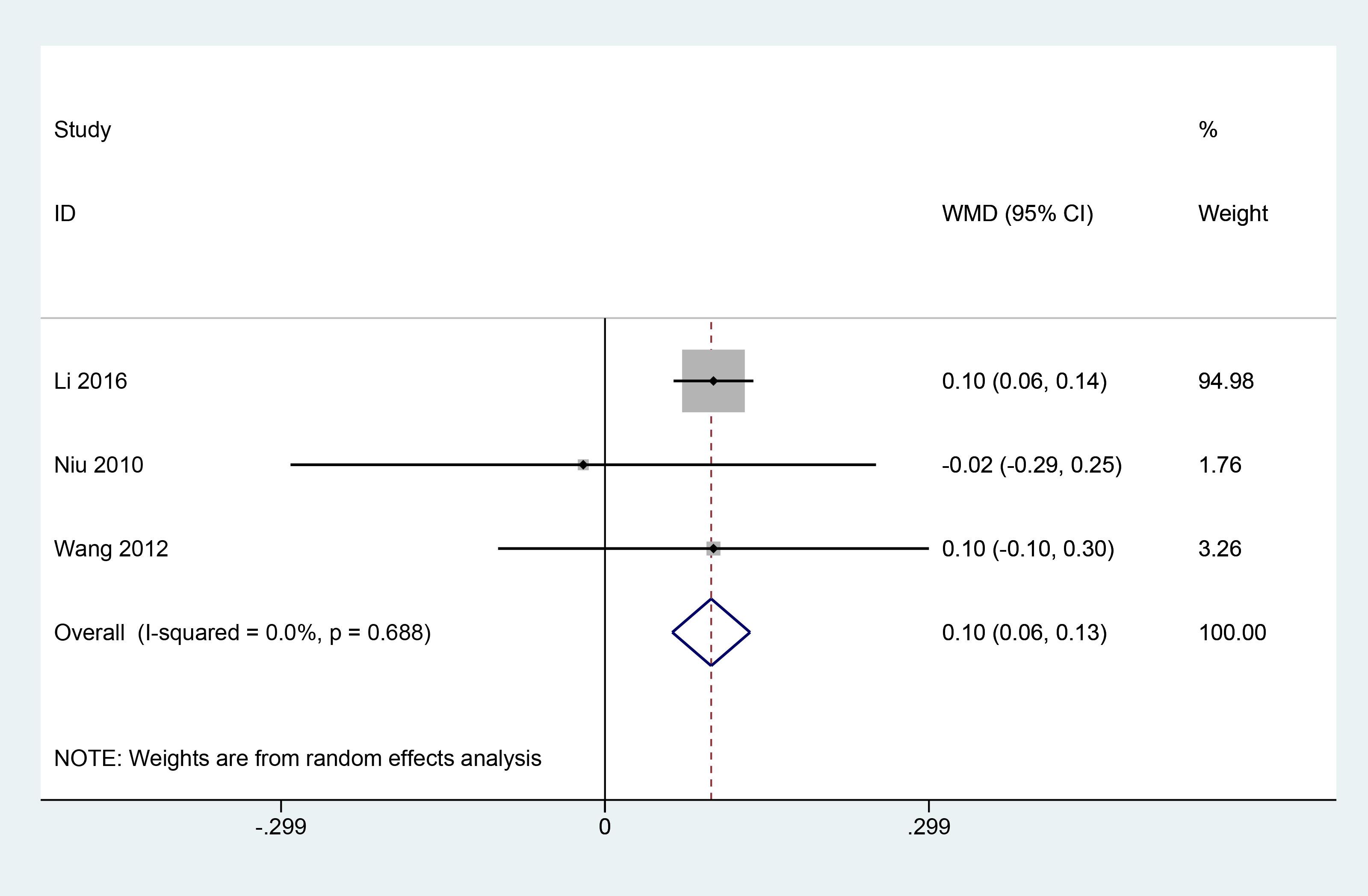
As of October 2022, a total of 547 studies in the literature that could be potentially relevant were retrieved. After title and abstract screening, 47 articles were reviewed in total, and 18 RCT studies (8–25) were finally included for Meta-analysis based on the inclusion criteria (Figure 1). There are 1392 patients altogether in the sample size of the 18 studies. The intervention group and the control group had equivalent pre-treatment data (Table 1).
3.2 Evaluation of the quality of the included literature
The 18 pieces of literature were divided into six items to explore the quality of the studies. All 18 papers were organized for randomized sequence generation using the randomized order principle. 11 datasets (9–11, 13–16, 19, 20, 23, 25) used either the random number table or the coin flip method, so the bias judgment was assessed as low risk. Only one study (10) used a single-blind design, and the remaining studies did not involve blinding, so the risk of bias was assessed as high. While the remaining four were not mentioned. (There was no mention of concealment of assignment order, insufficient result data, selective reporting, or other biases.)
3.3 Results of meta-analysis
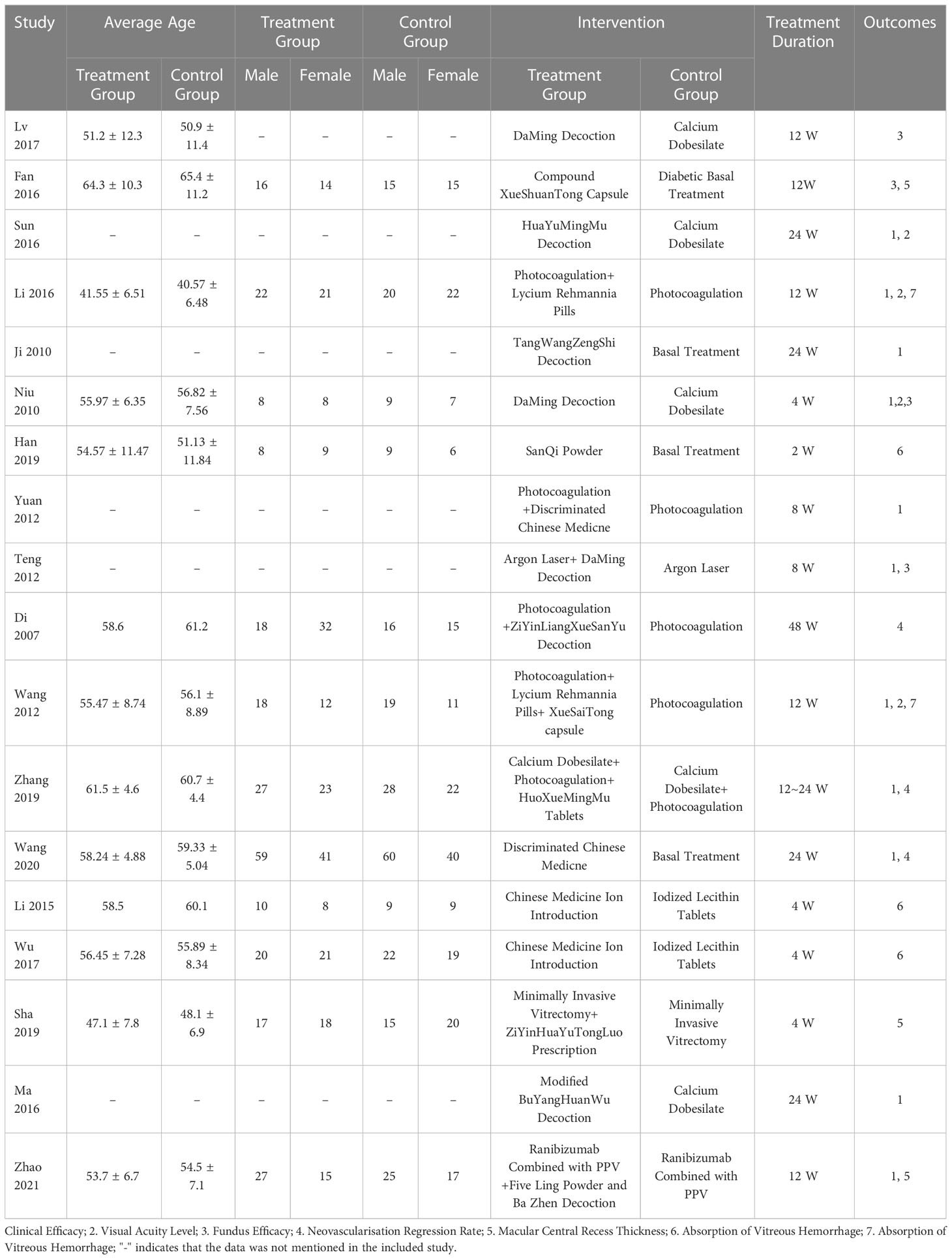
3.3.1 Clinical efficacy
A total of 9 articles (10–13, 15, 18–20, 25) reported the clinical efficacy of combined herbal treatments for patients with PDR, including 827 patients. The meta results showed that combined herbal treatments effectively improved the clinical outcomes of patients with PDR (9 studies, 827 patients, OR=2.99, CI: 2.18-4.10, I2 = 42.7%, P<0.05) (Figure 2).
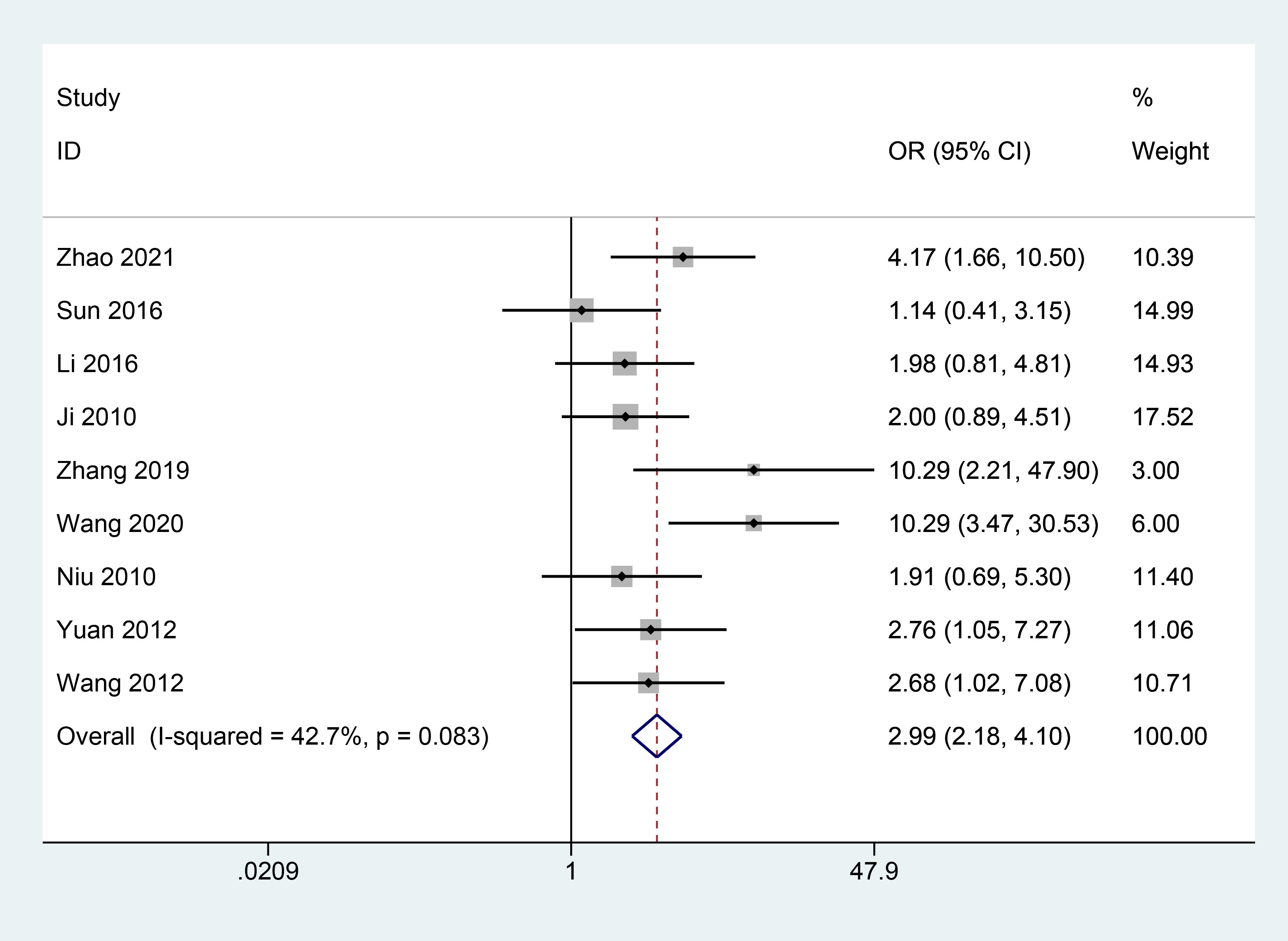
3.3.2 Visual acuity level
A total of 3 articles (11, 13, 18) reported the effect of combined herbal treatment on visual acuity in patients with PDR. 177 patients were included, and the meta results showed that combined herbal treatment could improve the visual acuity level of patients to some extent (3 studies, 177 patients, MD=0.10, CI: 0.06-0.13, I2 = 0%, P<0.05) (Figure 3).
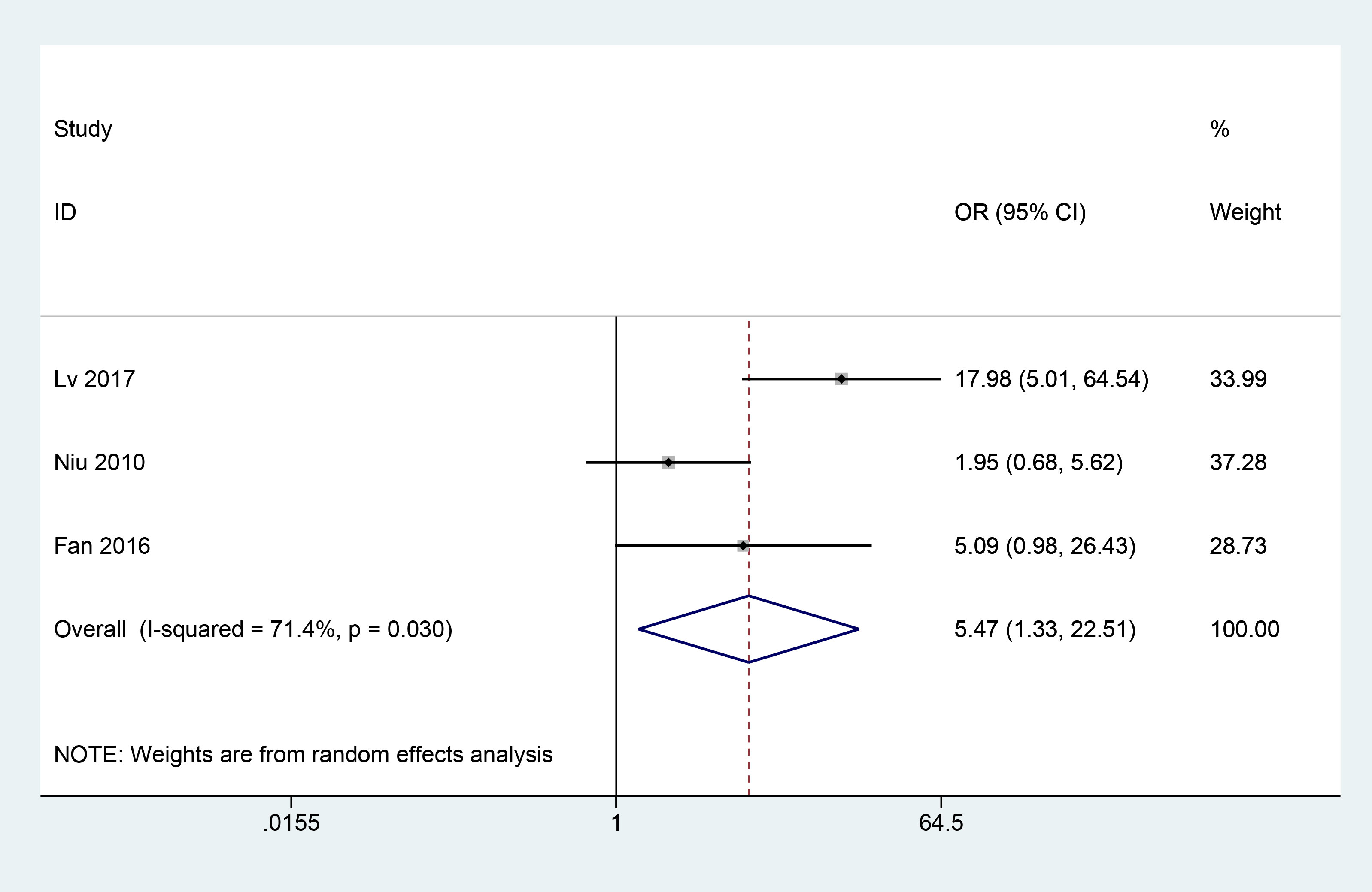
3.3.3 Fundus efficacy
A total of 3 articles (8, 9, 13) reported the fundus efficacy of combined herbal treatment in patients with PDR. 202 patients were included, and the meta results showed that combined herbal treatment significantly improved the fundus efficacy in patients with PDR (3 studies, 202 patients, OR=5.47, CI: 1.33-22.51, I2 = 71.4%, p<0.05) (Figure 4).
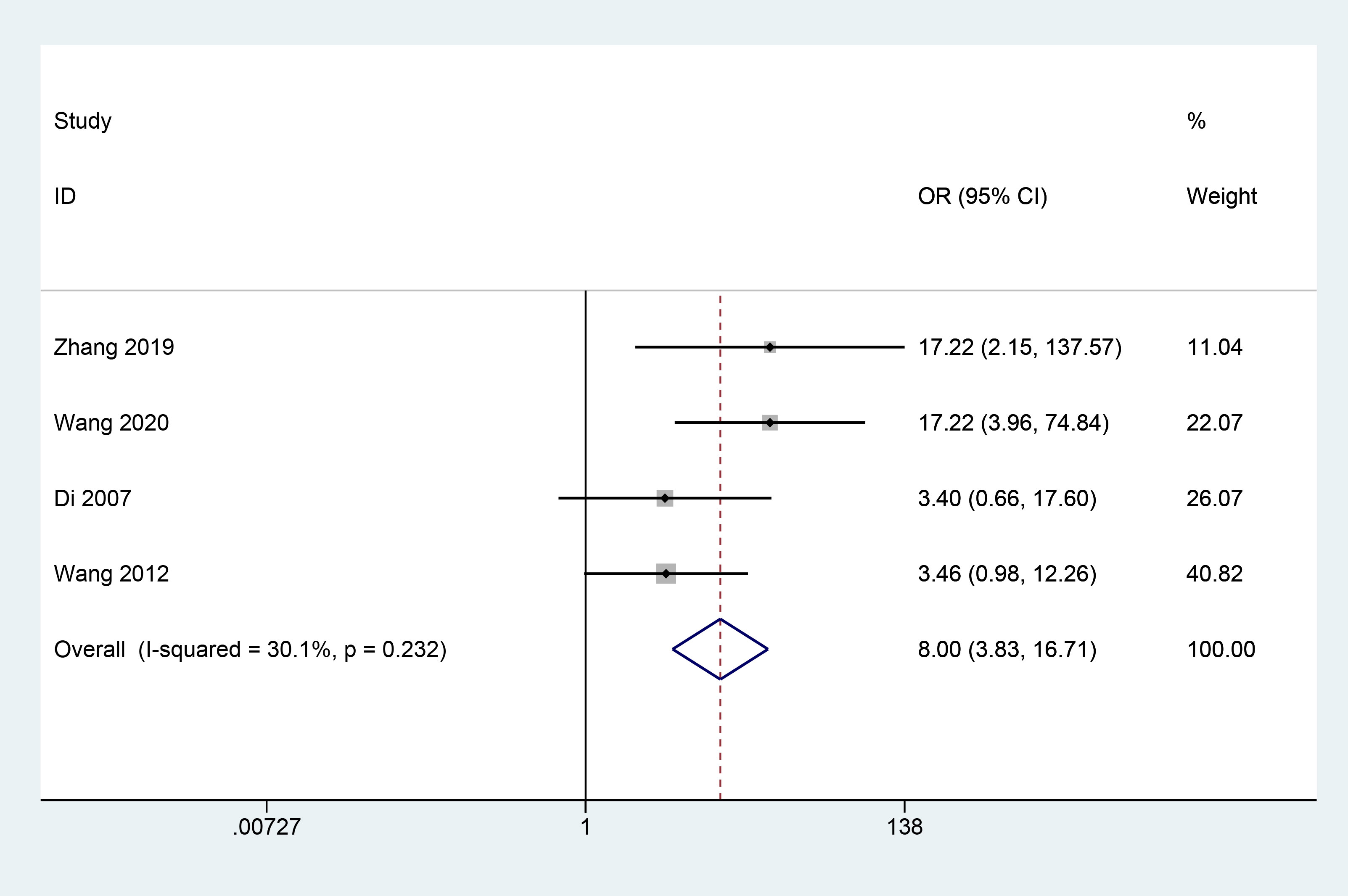
3.3.4 Neovascularisation regression rate
A total of 4 articles (17–20) reported the effect of herbal combination therapy on the regression of neovascularisation. 424 patients were included and the meta results showed that herbal combination therapy was effective in helping the regression of retinal neovascularisation in patients with PDR (4 studies, 424 cases, OR=8, CI: 3.83-16.71, I2 = 30.1%, P<0.05) (Figure 5).
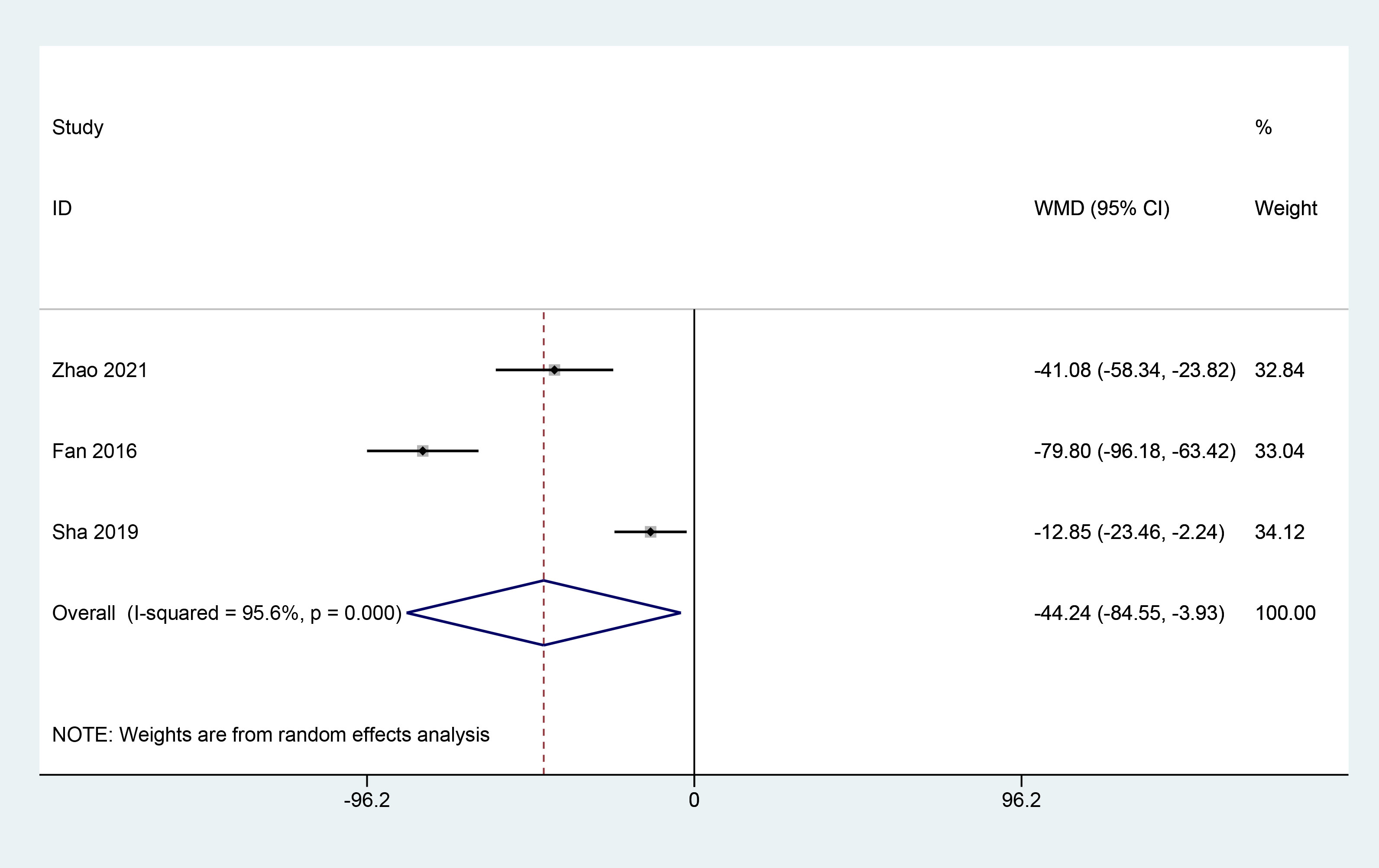
3.3.5 Macular central recess thickness
A total of 3 articles (9, 23, 25) reported on the effect of herbal combination therapy on macular central recess thickness, including 214 patients, and the meta results showed that herbal combination therapy was effective in reducing macular central recess thickness in patients with PDR (3 studies, 214 patients, MD=-44.24, CI:-84.55–3.93, I2 = 95.6%, p<0.05) (Figure 6).
3.3.6 Absorption of vitreous hemorrhage
A total of 3 articles (14, 21, 22) reported the effect of herbal combination therapy on vitreous blood accumulation in patients with PDR. 183 patients were included and the meta results showed that herbal combination therapy was effective in helping vitreous blood accumulation absorption in patients with PDR (3 studies, 183 cases, OR=4.7, CI: 2.26-9.77, I2 = 0%, P<0.05) (Figure 7).
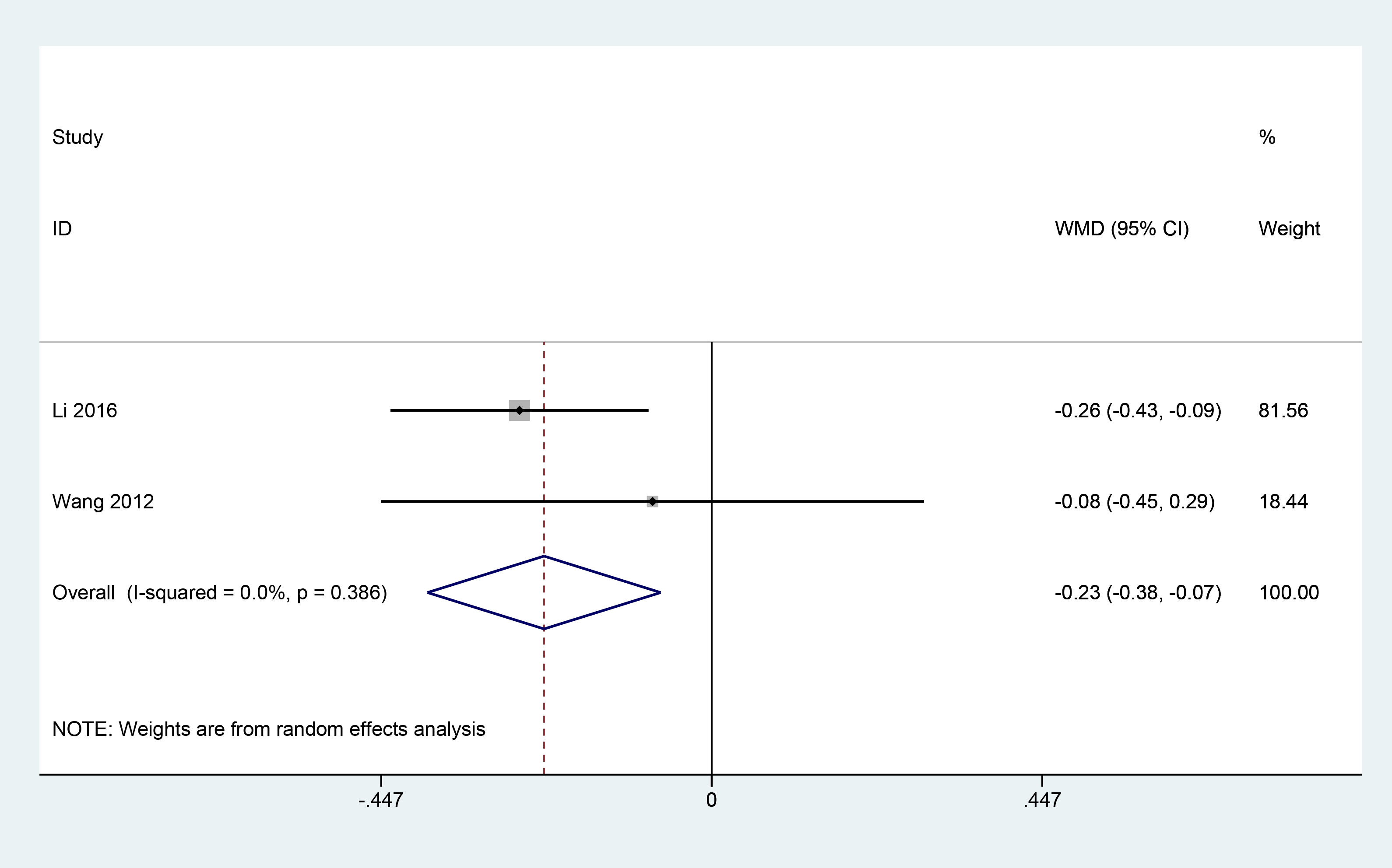
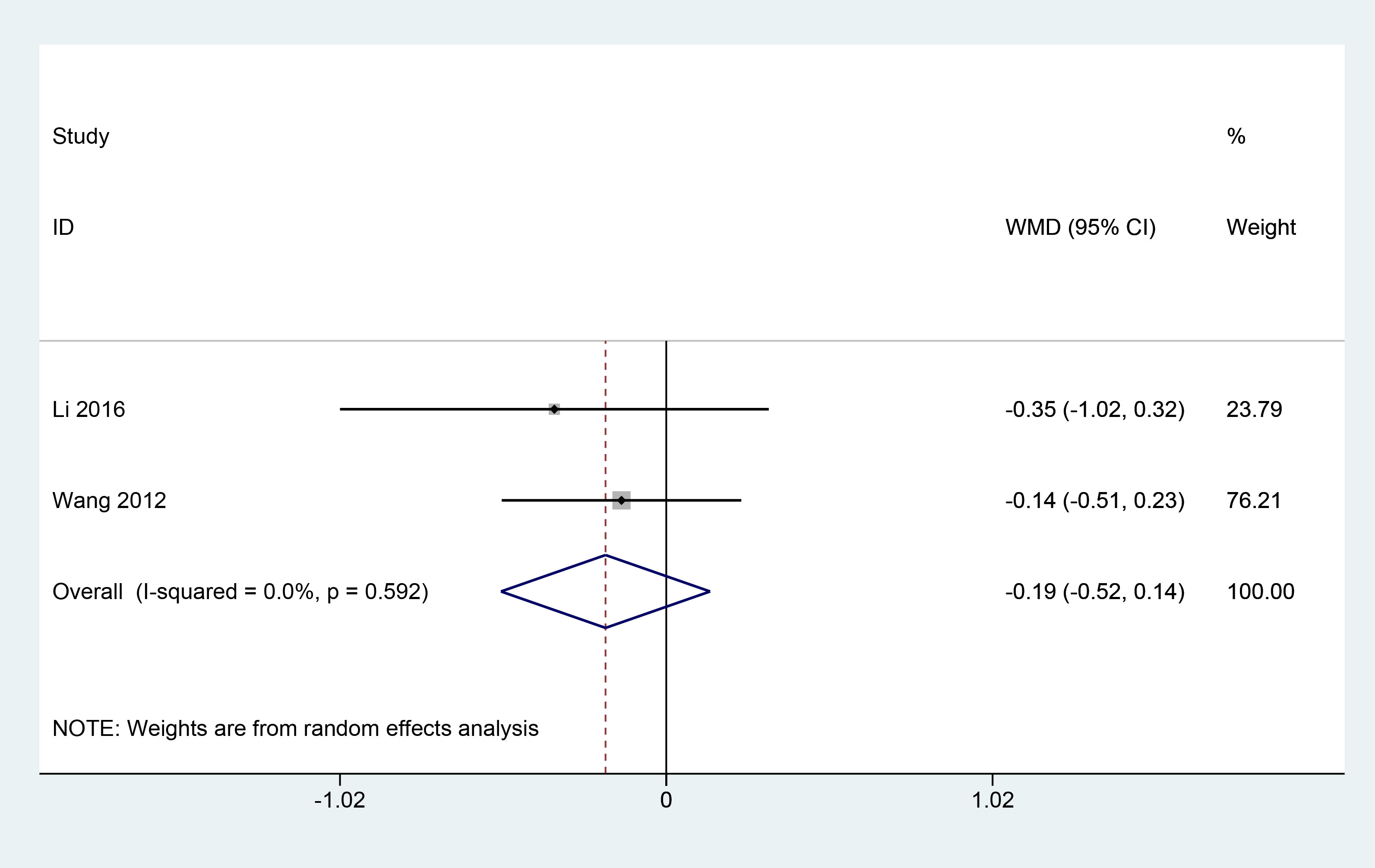
3.3.7 Fasting blood glucose and postprandial 2h blood glucose levels
A total of 2 articles (11, 18) reported the effect of herbal combination therapy on fasting blood glucose and postprandial 2h blood glucose in patients with PDR. 145 patients were included, and the meta results showed that herbal combination therapy was effective in reducing fasting blood glucose in patients with PDR (2 studies, 145 patients, fasting blood glucose: MD=-0.23, CI: -0.38-0.07, I2 = 0%. P<0.05; postprandial 2h glucose, MD=-0.19, CI: -0.52-0.14, I2 = 0%, P=0.25) (Figures 8, 9).
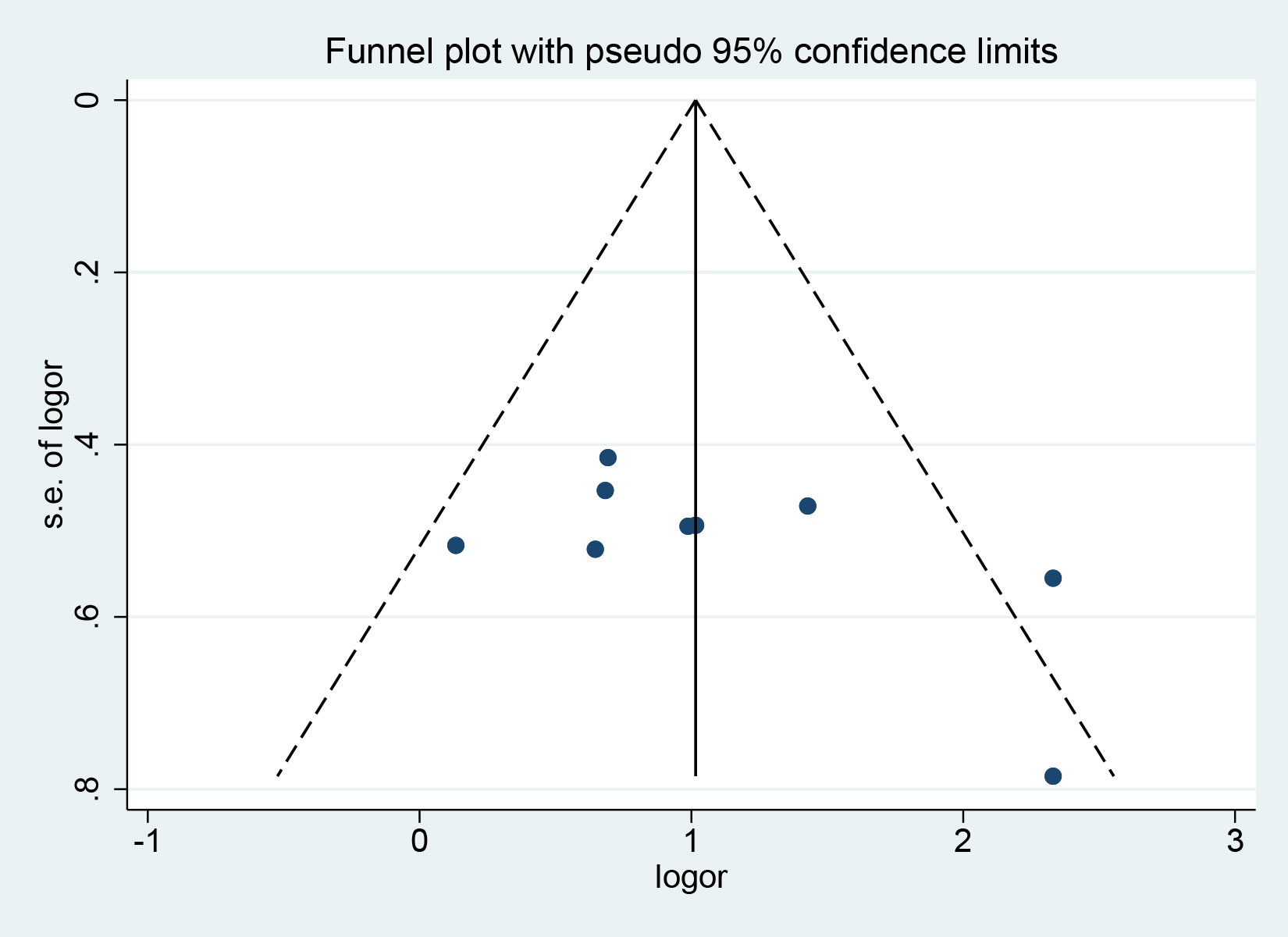
3.4 Publication bias
The clinical efficiency was tested for publication bias. The funnel plot showed that the symmetry was acceptable. Further quantitative analysis was performed using Begg ‘s and Egger ‘s tests. The results showed that there was no publication bias in the outcome index (P = 0.251, P = 0.112, respectively) (Figure 10).
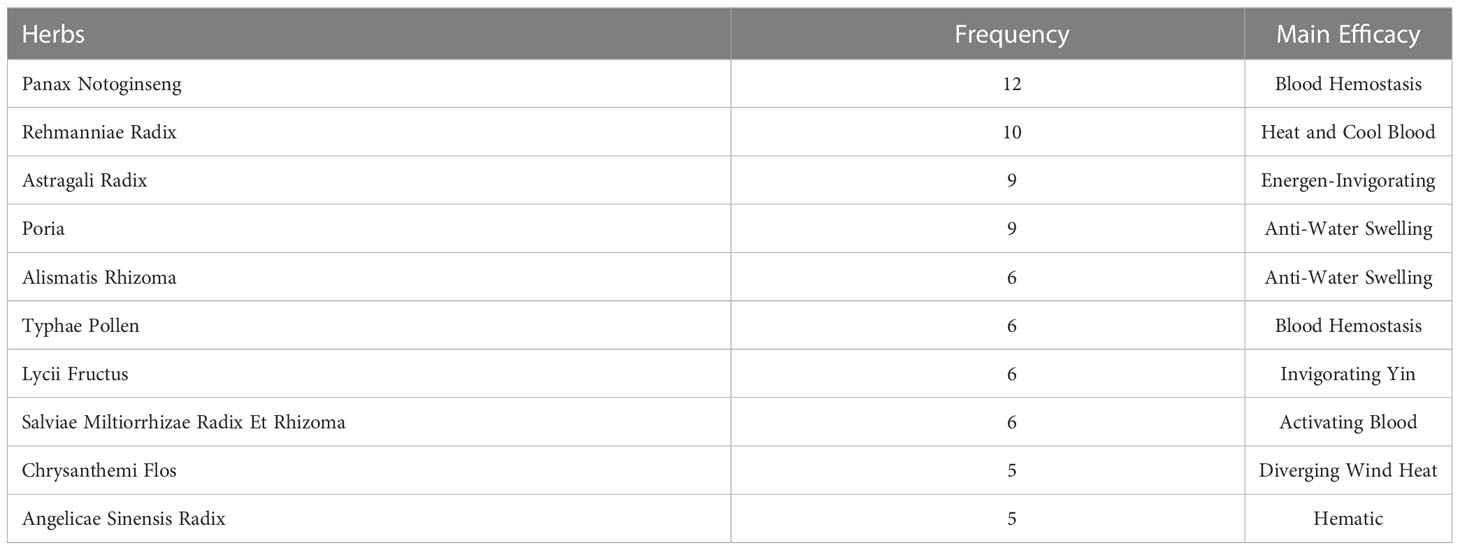
3.5 Inclusion of Chinese herbal medicines
In all 18 studies, a total of 69 herbal medicines were applied. After counting the frequency of repetition, it was found that the top four herbal medicines in terms of frequency were Panax notoginseng, Rehmanniae Radix, Astragali Radix and Poria, with their efficacy categories of resolving blood stasis and stopping bleeding, clearing heat and cooling the blood, tonifying Qi, promoting water retention and reducing swelling, respectively (Table 2).
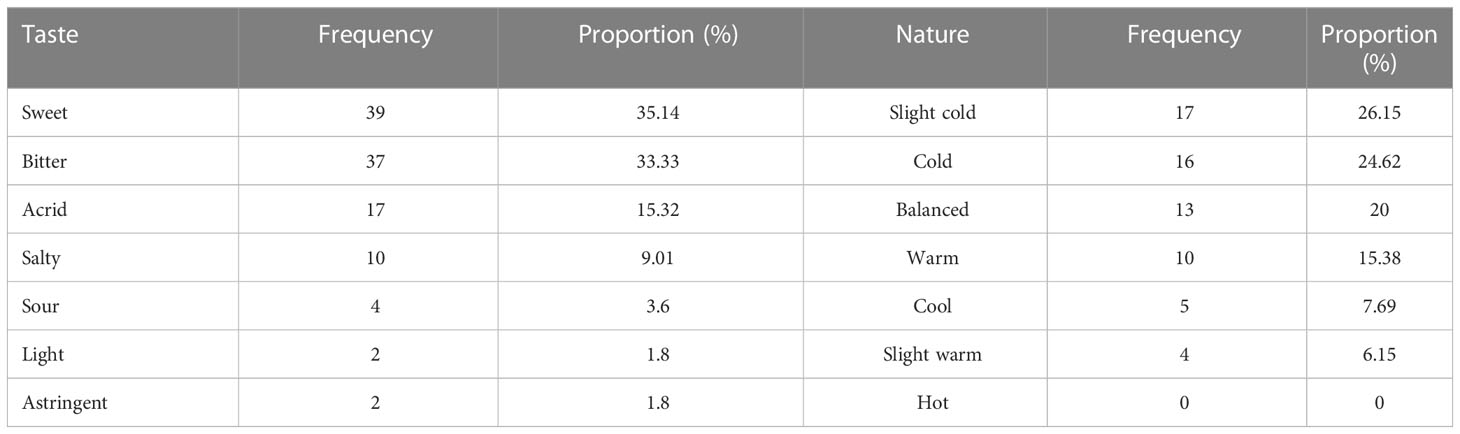
3.6 Analysis of the odour and meridian orientation of the included herbs
By analysing the nature, taste and meridian orientation information of the 69 herbs intervening in the PDR, the results showed that sweet and bitter herbs accounted for the highest frequency, with the two together accounting for 68.47%; most herbs were on the cold side. In terms of meridian orientation, herbs belonging to the liver meridian accounted for the highest proportion of the 69 species, at 69.57%, which may be related to the theory that the liver opening into the eye in traditional Chinese medicine thinking (Table 3) (Figure 11).
4 Discussion
4.1 Summary of main results
Our study included a total of 18 research articles, involving 1,392 patients with PDR. The results show that TCM therapy as an adjunctive treatment effectively improves the clinical outcome and visual acuity of PDR patients and the extent of their fundus lesions. It also has multiple therapeutic effects, such as lowering blood glucose, promoting capillary regression, and accelerating absorption of vitreous hemorrhage, which has multiple positive clinical implications for PDR. The results of publication bias test showed that there was no publication bias in the main indicator, which proved that the results were reliable.
4.2 Advantages and limitations of research
The main advantage of this meta-analysis is that it is the first systematic evaluation of the effectiveness of traditional Chinese medicine (TCM) in treating PDR, which preliminary answer the controversial issue of whether TCM is appropriate for PDR treatment. This is of great significance for guiding clinical PDR treatment. Throughout the study, we strictly followed the systematic review method, included almost all relevant and standard RCT studies available online, and the conclusions drawn were comprehensive and robust. Additionally, we conducted bias tests to confirm the reliability of our findings.
However, our study also has some limitations. Firstly, only one of the included studies mentioned the absence of complications and adverse reactions, while the remaining studies did not explore the safety of Chinese herbal medicine in treating PDR. Moreover, most of the studies did not use allocation concealment and blinding methods, nor did they design a placebo group, which may lead to bias in the study results. Finally, as all the literature included in our study came from China, the results we obtained may be more applicable to Chinese PDR patients, and whether TCM is effective for PDR patients in other countries still requires further research.
4.3 Analysis of Chinese herbal medicine
The study counted the Chinese medicines used in each study, and the results showed that the top four in terms of replication rate were Panax notoginseng, Rehmanniae Radix, Astragali Radix, and Poria. Panax notoginseng, the root and rhizome of Panax notoginseng, is usually used as a powder in amounts of 1.5-6 g. It is considered by Chinese medicine practitioners to be a critical medicine in the treatment of blood disorders, with the characteristics of “stopping bleeding and activating blood, stopping bleeding without leaving stasis.” Studies have shown that Panax notoginseng can effectively increase the concentration of thrombin and the number of platelets to shorten the clotting time and play a hemostatic role (26). Panax notoginseng contains various types of compounds such as cyclic terpenes and their glycosides, phenolic compounds, sugars, amino acids, and organic acids. These drugs have a variety of pharmacological effects including anti-ageing, hypoglycaemic, anti-inflammatory and immune system boosting (27).
There are relatively few studies on treating DR and PDR with Rehmanniae Radix. However, interestingly, a study from China showed that when the cases of effective treatment of diabetic retinopathy with Chinese herbs in the Chinese Journal Full Text Database (CNKI) were aggregated, Rehmanniae Radix ranked first in the frequency of administration, with 48 times (28), suggesting that Rehmanniae Radix has excellent potential for the treatment of DR and PDR. Its specific mechanisms need to be further explored. Astragalus is the dried root of Astragalus mongolica or Astragalus membranaceus, a leguminous plant, first published in Shen nong Ben Cao Jing and used medicinally in China for more than 2,000 years. It is a sacred tonic for the qi and is one of the most widely used Chinese herbs in China today. Studies have shown that the main anti-diabetic chemicals contained in Astragalus are astragalus polysaccharides, astragalosides, and astragalus flavonoids (29). These drug components can alleviate structural damage and apoptosis of retinal cells caused by the high glucose environment through multiple mechanisms such as hypoglycaemia, anti-oxidative stress, increased free radical scavenging activity, anti-inflammatory response, and inhibition of endoplasmic reticulum stress (30–32). Poria cocos, the dried nucleus of a porous fungus, is a particular herbal medicine that can be used for both medicinal and food purposes. In ancient times, Chinese medicine practitioners believed that regular Poria cocos could strengthen the spleen, promote hydration, tonify the qi and calm the mind, and prolong life, placing it alongside nine other drugs such as ginseng and Ganoderma lucidum as “immortal herbs”. However, there are relatively few records and studies on the use of Poria as a treatment for DR. It ranks highly among the therapeutic drugs for PDR due to its unique effect of promoting the body’s water metabolism (33). In addition to retinal microaneurysms, haemorrhages, and neovascularization, DR often results in diabetic macular oedema (DME) due to the disruption of the blood-retinal barrier and altered hemodynamics, causing extracellular fluid accumulation (34). PDR patients whose disease has progressed to the late stages of DR are usually associated with severe DME with exudative symptoms. Unfortunately, similar to Rehmanniae Radix, there is almost a gap in research exploring Poria alone for treating DME. However, a computer search of the Chinese Journal Full Text Database (CNKI) and Wanfang database for clinical cases related to the treatment of macular oedema ranked Poria first with a frequency of 60 recurrences (35), suggesting that TCM community generally recognizes the efficacy of Poria in the treatment of DME. At the same time, its specific mechanism of action needs to be further explored.
5 Conclusion
In summary, our study preliminarily proved that Chinese herbal medicine can effectively improve the clinical outcomes, visual acuity, and degree of retinopathy in patients with proliferative diabetic retinopathy (PDR), as well as reducing blood glucose levels, aiding capillary regression, and alleviating vitreous hemorrhage. These conclusions have significant implications for resolving controversies surrounding the application of traditional Chinese medicine (TCM) in the field of PDR. In addition, data mining of herbal medicines included in the literature reveals that researchers prefer to use herbs with sweet or bitter taste and slight cold or cold properties that belong to the liver meridian to treat PDR. In future studies, we need a larger sample of high-quality, multi-centre RCT studies to provide evidence for treating PDR with Chinese herbs. These studies should also focus on exploring safety.
Author contributions
This review was created by BGH, BSH, ZS, MS, DL, TX, CL and YC. The First drafts of the article were written by BGH and BSH, and further revisions were contributed to by the other co-authors. The final version of the work was approved by all authors. DL obtained funding for this study. All authors contributed to the article and approved the submitted version.
Funding
Project of National Natural Science Foundation of China: Construction and Empirical Study of Rural Elderly Type 2 Diabetes Mellitus with MCI Management Model Based on Complex Adaptive System Theory (72274110). Project of Shandong Provincial Natural Science Foundation: Study on the Role and Mechanism of Salvianolic Acid in Promoting IGFBP3 Methylation to Regulate Microcirculation Disorder in Diabetic Cardiomyopathy (ZR2022QH163). Qilu Geriatric Diseases Chinese and Western Academic School Inheritance Workshop Project (No.2022-93-1-10).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Teo ZL, Tham Y, Yu M, Chee ML, Rim TH, Cheung N, et al. Global prevalence of diabetic retinopathy and projection of burden through 2045. Ophthalmology (2021) 128:1580–91. doi: 10.1016/j.ophtha.2021.04.027
2. Group NATG. Technical scheme of grading diagnosis and treatment service for diabetic retinopathy. Chin J Gen Practitioners (2017) 16:589–93. doi: 10.3760/cma.j.issn.1671-7368.2017.08.005
3. Tian J, Jin D, Bao Q, Ding Q, Zhang H, Gao Z, et al. Evidence and potential mechanisms of traditional Chinese medicine for the treatment of type 2 diabetes: a systematic review and meta-analysis. Diabet Obes Metab (2019) 21:1801–16. doi: 10.1111/dom.13760
4. Ai X, Yu P, Hou Y, Song X, Luo J, Li N, et al. A review of traditional Chinese medicine on treatment of diabetic retinopathy and involved mechanisms. BioMed Pharmacother (2020) 132:110852. doi: 10.1016/j.biopha.2020.110852
5. Chen Q, Ni Q, Liu Y. Guidelines for diagnosis and treatment of diabetic retinopathy ( 2021-09-24 ). World Tradition Chin Med (2021) 16:3270–77. doi: 10.3969/j.issn.1673-7202.2021.22.002
6. Wilkinson CP, Ferris FL, Klein RE, Lee PP, Agardh CD, Davis M, et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology (2003) 110:1677–82. doi: 10.1016/S0161-6420(03)00475-5
7. Chen Z, Xie L, Hao X. Research progress of traditional Chinese medicine in the treatment of diabetic retinopathy. J Tradition Chin Ophthalmol (2023) 33:84–7. doi: 10.13444/j.cnki.zgzyykzz.2023.01.021
8. Lu XD, Cao J. Study on the mechanism of PD1 /PDL1 signaling pathway in proliferative diabetic retinopathy treated by Chinese traditional study on the mechanism of PD1 /PDL1 signaling pathway in proliferative diabetic retinopathy treated by Chinese traditional medicine. Pharmacol Clinics Chin Materia Med (2017) 33:136–40. doi: 10.13412/j.cnki.zyyl.2017.06.035
9. Fan XJ, Zhang GF. Effect of compound xueshuantong capsule in treatment patients of cataract with proliferative diabetic retinopathy. Chin J Biochem Pharm (2016) 36:121–23. doi: 10.3969/j.issn.1005-1678.2016.12.034
10. Sun R, Hui SY. In different periods of diabetic retinopathy in the observation of the curative effect of treatment of HuaYuMingMu decoction and its influence on VEGF. World Chin Med (2016) 11:75–8. doi: 10.3969/j.issn.1673-7202.2016.01.018
11. Li JL, Dong JG. Effect of qiju dihuang pill combined with photocoagulation on proliferative stage of diabetic retinopathy. J Pract Diabetol (2016) 12:18–20. doi: CNKI:SUN:LNSY.0.2016-06-013
12. Ji LP. Tangwang zengshi decoction in the treatment of 126 cases of diabetic retinopathy. Chin Med Mod Dis Educ China (2010) 8:27–8. doi: 10.3969/j.issn.1672-2779.2010.13.020
13. Niu SY. The clinical study on proiferative diabetic retinopathy with chinses traditional medicine-DaMingYin. Heilongjiang University of Chinese Medicine (2010). Available at: https://kns.cnki.net/kcms/detail/detail.aspx?FileName=1011037812.nh&DbName=CMFD2012.
14. Han MY. Clinical observation and mechanism study of sanqi combined with vitrectomy on patients with proliferative diabetic retinopathy. Beijing University of Chinese Medicine (2018). Available at: https://kns.cnki.net/kcms/detail/detail.aspx?FileName=1018205351.nh&DbName=CMFD2018.
15. Yuan CY. Efficiency of Chinese herbal medicine combined with laser photocoagulation on proliferation diabetic retinopathy. Clin Med Eng (2012) 19:819–20. doi: 10.3969/j.issn.1674-4659.2012.05.0819
16. Teng XM, Sun H. Clinical experience of traditional Chinese medicine combined with retinal laser in treatment of proliferative diabetic retinopathy. Heilongjiang Univ Chin Med (2009) 38:22–3. doi: 10.3969/j.issn.1000-9906.2012.04.013
17. Di PH, Zhao N, Sun RX, Wang JC. The effect of Chinese traditional medicine combine with laser on the treatment of new vessels of diabetic retinopathy. Hebei J Tradition Chin Med (2007), 29:543–45. doi: 10.3969/j.issn.1002-2619.2007.06.044
18. Wang RJ. Traditional Chinese medicine combined with retinal photocoagulation in treatment of diabetic retinopathy(gan shen yin xu and xue yu xing) clinical study abstract. Yunnan University of Chinese Medicine (2012). Available at: https://kns.cnki.net/kcms/detail/detail.aspx?FileName=1013132859.nh&DbName=CMFD2013.
19. Zhang L. Clinical observation of Chinese and Western medicine combined with retinal laser treatment in proliferative diabetic retinopathy complicated with vitreous hemorrhage. Diabetes New World (2019) 22:189–91. doi: 10.16658/j.cnki.1672-4062.2019.11.189
20. Wang SJ. Data from: the effect of combined treatment of Chinese and Western medicine in proliferative diabetic retinopathy complicated with vitreous hemorrhage. CNKI (2020). Available at: https://kns.cnki.net/kcms/detail/detail.aspx?FileName=CXCM202004003033&DbName=CPFD2020.
21. Li J, Li XH, Wang Q. Clinical observation on treating stage IV vitreous hemorrhage of diabetic retinopathy by Chinese medicine combined with iontophoresis. J Sichuan Tradition Chin Med (2015) 33:141–42. doi: CNKI:SUN:SCZY.0.2015-10-067
22. Wu YY. Clinical observation on Chinese herbs combined with iontophoresis in the treatment of stage IV vitreous hemorrhage of diabetic retinopathy. Guangming J Chin Med (2017) 32:1482–84. doi: 10.3969/j.issn.1003-8914.2017.10.048
23. Sha YF, Duan SL, Du DJ. Clinical study on ziyin huayu tongluo prescription in adjuvant treatment for proliferative diabetic retinopathy. New Chin Med (2019) 51:166–68. doi: 10.13457/j.cnki.jncm.2019.06.049
24. Ma WQ, Li ZH, Jiang WL. The observation of efficacy of traditional Chinese medicine combined with vitrectomy in the treatment of; proliferative diabetic retinopathy. J Chin Ophthalmol Otorhinolaryngol (2016) 6:5. doi: 10.3969/j.issn.1674-9006.2016.02.011
25. Zhao YX, Wang S, Ju JJ. Influence of addition and subtraction of bazhen decoction and five drugs with poria combined with leizhumab on conscious symptoms and retinal function recovery in patients with proliferative diabet-ic retinopathy after vitrectomy. J Aerospace Med (2021) 32:385–88. doi: 10.3969/j.issn.2095-1434.2021.04.002
26. Xie Y, Wang C. Herb–drug interactions between panax notoginseng or its biologically active compounds and therapeutic drugs: a comprehensive pharmacodynamic and pharmacokinetic review. J Ethnopharmacol (2023) 307:116156. doi: 10.1016/j.jep.2023.116156
27. Wang T, Guo R, Zhou G, Zhou X, Kou Z, Sui F, et al. Traditional uses, botany, phytochemistry, pharmacology and toxicology of panax notoginseng (Burk.) F.H. Chen: a review. J Ethnopharmacol (2016) 188:234–58. doi: 10.1016/j.jep.2016.05.005
28. Gu Z, Yang Y, Shi Y. Analysis of the medication rule of contemporary medical doctors for treating diabetic retinitis based on the TCM inheritance auxiliary platform. J Liaoning Univ Tradition Chin Med (2022) 24:130–34. doi: 10.13194/j.issn.1673-842x.2022.01.029
29. Salehi B, Carneiro JNP, Rocha JE, Coutinho HDM, Morais Braga MFB, Sharifi Rad J, et al. Astragalus species: insights on its chemical composition toward pharmacological applications. Phytother Res (2021) 35:2445–76. doi: 10.1002/ptr.6974
30. Peng Q, Tong P, Gu L, Li W. Astragalus polysaccharide attenuates metabolic memory-triggered ER stress and apoptosis via regulation of miR-204/SIRT1 axis in retinal pigment epithelial cells. Biosci Rep (2020) 40(1):BSR20192121. doi: 10.1042/BSR20192121
31. You L, Lin Y, Fang Z, Shen G, Zhao J, Wang T. Research advances on astragaloside-IV in treatment of diabetes mellitus and its complications pharmacological effects. Zhongguo zhongyao zazhi (2017) 42:4700–06. doi: 10.19540/j.cnki.cjcmm.20171010.007
32. Zhang K, Pugliese M, Pugliese A, Passantino A. Biological active ingredients of traditional Chinese herb astragalus membranaceus on treatment of diabetes: a systematic review. Mini Rev medicinal Chem (2015) 15:315. doi: 10.2174/1389557515666150227113431
33. Hu G, Huang C, Zhang Y, Xiao W, Jia J. Accumulation of biomass and four triterpenoids in two-stage cultured poria cocos mycelia and diuretic activity in rats. Chin J Nat Med (2017) 15:265–70. doi: 10.1016/S1875-5364(17)30043-2
34. Zhang J, Zhang J, Zhang C, Zhang J, Gu L, Luo D, et al. Diabetic macular edema: current understanding, molecular mechanisms and therapeutic implications. Cells (2022) 11:3362. doi: 10.3390/cells11213362
Keywords: traditional Chinese medicine, proliferative diabetic retinopathy, meta analysis, diabetic complications, Chinese medicinal herb
Citation: Huai B, Huai B, Su Z, Song M, Li C, Cao Y, Xin T and Liu D (2023) Systematic evaluation of combined herbal adjuvant therapy for proliferative diabetic retinopathy. Front. Endocrinol. 14:1157189. doi: 10.3389/fendo.2023.1157189
Received: 02 February 2023; Accepted: 04 May 2023;
Published: 18 May 2023.
Edited by:
Mohd Imtiaz Nawaz, King Saud University, Saudi ArabiaReviewed by:
Haiping Duan, Qingdao Municipal Center for Disease Control and Prevention, ChinaMashhood Uz Zafar Farooq, Karachi Institute of Medical Sciences, Pakistan
Copyright © 2023 Huai, Huai, Su, Song, Li, Cao, Xin and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tao Xin, eGludGFvQHNkZm11LmVkdS5jbg==; Deshan Liu, bGl1ZGVzaGFuQHNkdS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
 Baogeng Huai
Baogeng Huai Baosha Huai3†
Baosha Huai3† Deshan Liu
Deshan Liu