- 1Department of Nephrology, Kidney Research Institute, West China Hospital of Sichuan University, Chengdu, China
- 2Department of Thyroid and Parathyroid Surgery, West China Hospital, Sichuan University, Chengdu, Sichuan, China
- 3Department of Thoracic Oncology, Cancer Center, and State Key Laboratory of Biotherapy, West China Hospital, Sichuan University, Chengdu, China
Background: The incidence and risk factors of acute kidney injury (AKI) in patients with malignancies receiving immune checkpoint inhibitors (ICIs) are being extensively reported with their widespread application.
Objective: This study aimed to quantify the incidence and identify risk factors of AKI in cancer patients treated with ICIs.
Methods: We searched the electronic databases of PubMed/Medline, Web of Science, Cochrane and Embase before 1 February 2023 on the incidence and risk factors of AKI in patients receiving ICIs and registered the protocol in PROSPERO (CRD42023391939). A random-effect meta-analysis was performed to quantify the pooled incidence estimate of AKI, identify risk factors with pooled odds ratios (ORs) and 95% confidence intervals (95% CIs) and investigate the median latency period of ICI-AKI in patients treated with ICIs. Assessment of study quality, meta-regression, and sensitivity and publication bias analyses were conducted.
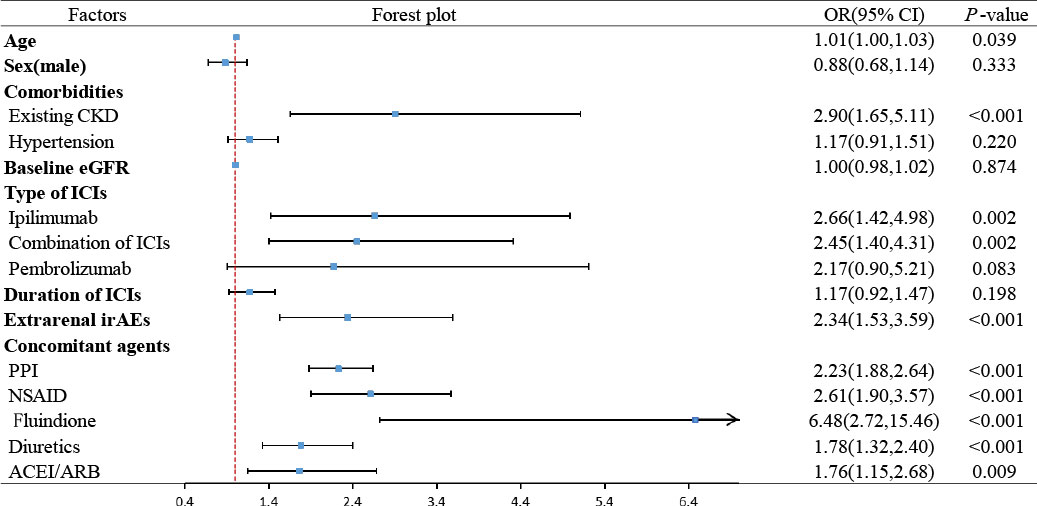
Results: In total, 27 studies consisting of 24048 participants were included in this systematic review and meta-analysis. The overall pooled incidence of AKI secondary to ICIs was 5.7% (95% CI: 3.7%-8.2%). Significant risk factors were older age (OR: 1.01, 95% CI: 1.00–1.03), preexisting chronic kidney disease (CKD) (OR: 2.90, 95% CI: 1.65–5.11), ipilimumab (OR: 2.66, 95% CI: 1.42–4.98), combination of ICIs (OR: 2.45, 95% CI: 1.40–4.31), extrarenal immune-related adverse events (irAEs) (OR: 2.34, 95% CI: 1.53-3.59), and proton pump inhibitor (PPI) (OR: 2.23, 95% CI: 1.88–2.64), nonsteroidal anti-inflammatory drug (NSAID) (OR: 2.61, 95% CI: 1.90–3.57), fluindione (OR: 6.48, 95% CI: 2.72–15.46), diuretic (OR: 1.78, 95% CI: 1.32–2.40) and angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin-receptor blockers (ARBs) (pooled OR: 1.76, 95% CI: 1.15–2.68) use. Median time from ICIs initiation to AKI was 108.07 days. Sensitivity and publication bias analyses indicated robust results for this study.
Conclusion: The occurrence of AKI following ICIs was not uncommon, with an incidence of 5.7% and a median time interval of 108.07 days after ICIs initiation. Older age, preexisting chronic kidney disease (CKD), ipilimumab, combined use of ICIs, extrarenal irAEs, and PPI, NSAID, fluindione, diuretics and ACEI/ARB use are risk factors for AKI in patients receiving ICIs.
Systematic review registration: https://www.crd.york.ac.uk/prospero/, identifier CRD42023391939.
1 Introduction
Cancer is the leading cause of death worldwide (1). Oncologists urgently need to develop novel remedies that effectively target tumor cells to break new ground on this universal conundrum. The human immune system is the superior force in killing cancer cells, whose activation can be inhibited by the combination of two transmembrane proteins located in T cells known as immune checkpoints, cytotoxic T lymphocyte-associated antigen 4 (CTLA-4) and programmed cell death protein 1 (PD-1), and their corresponding ligand proteins B7, PD-L1/PD-L2, respectively (2, 3). Tumor cells cunningly take advantage of this negative regulation beneficial for immune tolerance to evade the body’s immune attack (4). Immune checkpoint inhibitors (ICIs), as monoclonal antibodies of immunotherapy to interrupt the binding of CTLA-4 and B7, PD-1 and PD-L1/PD-L2, have revolutionized the treatment paradigm of a variety of advanced malignancies with surprising results, especially melanoma and lung cancer (5).
Along with the wide application of ICIs in cancer treatment, multisystem autoimmune phenomena termed immune-related adverse events (irAEs) have markedly emerged into our vision for their nonselective role on immune checkpoints. The overall incidences of irAEs in patients treated with ICIs range from 15% to 90%, of which the most frequently observed are dermal, gastrointestinal tract, endocrine system and liver (6, 7). Although renal-associated irAEs are relatively rare, fatal complications such as acute kidney injury (AKI) should be seriously considered. In total, the use of ICIs was linked to an increased risk of all-grade AKI (RR = 1.37, 95% CI: 1.14–1.65), as indicated by a pharmacovigilance study (8). However, high inconsistency of the incidence of AKI after ICI use, ranging from 0. 4% to 28.1%, brings about a challenge for clinicians to determine evidence-based therapy strategies (9, 10). Simultaneously, a growing body of studies has pioneered efforts to investigate risk factors of AKI occurring with ICIs. The first study performed by Seethapathy et al. in 2019 found that exposure to PPIs was associated with a significantly increased risk for sustained ICI-AKI (11). Both similar and opposite results were detected in a series of later works but lacked consensus (12, 13). In addition, differential diagnoses and renal biopsy of ICI-AKI are challenging in clinical practice. In light of this, we regard median onset time AKI after ICIs initiation as a valuable implication for clinicians. Knowledge of the overall incidence and risk factors of AKI following ICIs, involving sex, older age, comorbidities, concomitant agents and so on, is controversial and not comprehensive to date. To address this gap, this systematic review and meta-analysis is aimed at providing an updated result of the quantified incidence and risk factors of AKI in patients treated with ICIs, as well as median time from ICIs initiation to the occurrence of AKI.
2 Methods
2.1 Protocol and guidance
The study protocol has already been registered in PROSPERO (CRD42023391939) and in accordance with the Cochrane handbook and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (14).
2.2 Search strategy
Electronic databases of English language publications, PubMed/Medline, Web of Science, Cochrane and Embase were searched to collect studies dated to 1 February 2023 in terms of the incidence and risk factors of AKI in patients treated with ICIs. We retrieved relevant articles through the combination of Medical Subject Headings (MeSH) terms comprising “immune checkpoint inhibitors”, “acute kidney injury”, “risk factor” or “incidence” and all the corresponding free words. Complete and detailed search strategies of each database are provided in Supplementary Appendix S1 for incidence and Supplementary Appendix S2 for risk factors. Searches were limited to English but with no date, sex, or ethnicity restrictions.
2.3 Inclusion and exclusion criteria
The inclusion criteria were as follows: (a) the study sample consisted of patients with malignancy and treated with ICIs aged 18 years or above; (b) the study reported the incidence or risk factors of AKI in patients receiving ICIs. AKI is defined as an increase in serum creatinine to≥1.5 times the baseline level, which is known or presumed to have occurred within the prior 7 days; or an increase in serum creatinine by ≥26.5 µmol/L within 48 hours; or oliguria (urine volume <0.5 ml/kg per hour for 6 hours; and (c) sufficient data were provided on the event number or effect size, the odds ratios (OR) or hazard ratio (HR), and 95% confidence intervals (95% CI) with full texts.
Studies were excluded for the following reasons: (a) they were reviews, meta-analyses, case reports, conference abstracts and guidelines; and (b) the study was conducted based on animals.
2.4 Study selection
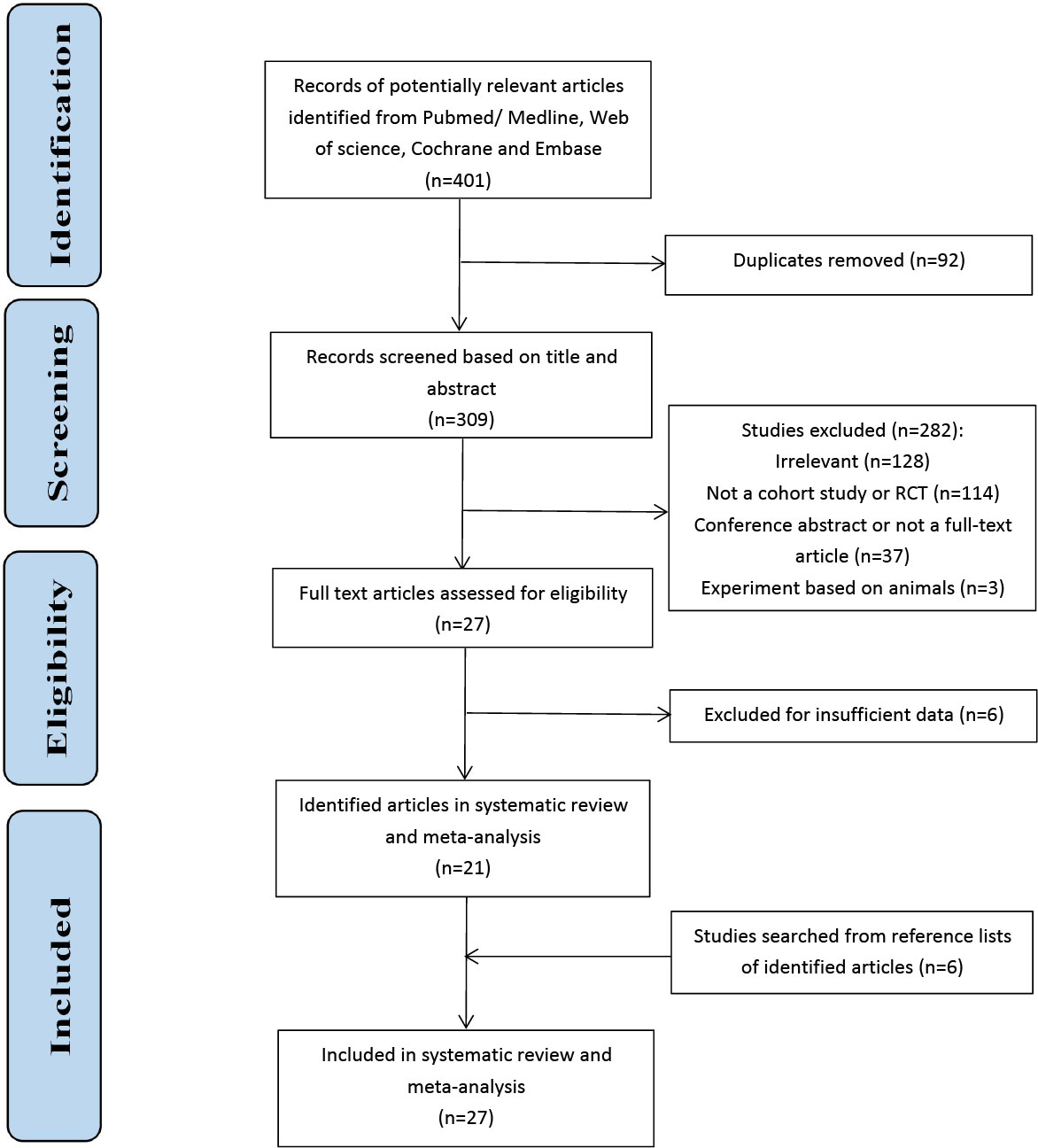
After excluding duplicates, two researchers independently screened the titles and abstracts of all identified records to remove irrelevant documents. Then, a full-text review was conducted to determine the eligibility for inclusion. Any disagreement on study selection was resolved by discussion with the third researcher (LC, ZY, and WW). The study selection process is shown in Figure 1.
2.5 Data extraction and quality assessment
The following data were extracted from the included studies: (a) the basic information, including first author, publication year, region, data source, data, study design, study type, and enrollment period; (b) characteristics of the participants, including sample size, number of AKI cases, sex ratio (male), and median age; and (c) the incidence, median time and interquartile ranges and effect size (OR or HR) and 95% CI of potential risk factors in each study, encompassing sex, older age, comorbidities, baseline eGFR, ICIs, extrarenal irAEs, and concomitant agents. We prioritized the extraction of multivariate analysis data from the adjustment model. According to the Newcastle−Ottawa Scale (NOS) designed for cohort studies and case−control studies and the Cochrane Handbook designed for randomized clinical trial, two researchers (LC and ZY) independently assessed the risk of bias. For 23 observational studies, selection (0-4 scores), comparability (0-2 scores) and outcome or exposure (0-3 scores) are the three evaluation domains containing an eight-item checklist ranging from 0 to 9 scores. The scores of the included articles ranged from 6 to 9 and were classified as high quality. Among the three domains, the outcome of the included records performed the worst due to scant time for the occurrence of potential ICI-AKI. For 4 randomized clinical trials, 2 studies that did not adopt blinding methods for participants and outcome were evaluated as ‘‘High risk.” A study failing to elaborate specific method of allocation concealment was classified as ‘‘Unclear”. Other evaluation items were mostly ‘‘Low risk.” Generally, the included studies had low methodological bias. Detailed information is illustrated in Supplementary Table S1 and Supplementary Figures S1, S2. Any disagreement was discussed with another reviewer (LC, ZY and WW).
2.6 Statistical analysis
In this meta-analysis, the incidence, median time from ICIs initiation and risk factors of AKI encompassing sex, older age, comorbidities, baseline eGFR, ICIs, extrarenal irAEs, and concomitant agents in cancer patients receiving ICIs were pooled and compared between patients with AKI and without AKI using random effects and I2 statistics for between-study heterogeneity (I2>50%, P<0.05 implied potential heterogeneity). Meta-regression was conducted to explore the contributor of substantial heterogeneity. OR and 95% CI were employed as pooled effects, and P<0.05 was considered to be statistically significant. We regarded HR as a good estimate of OR only if HR was represented in original studies. IBM SPSS Statistics 20 was used to calculate ORs and 95% CIs if neither ORs nor HRs were provided in the primary texts. All statistical analyses were performed using Stata Statistical Software, version 16.0. Moreover, sensitivity analyses by sequentially omitting studies and publication bias analyses by funnel plots, Begg’s and Egger’s statistical tests were shown to evaluate the robustness of the results.
3 Results
3.1 Eligible studies
A total of 401 documents were initially searched for incidence and risk factors. After removing 92 duplicates, we screened the title and abstract of each study and found that 128 citations were apparently irrelevant. In the remaining records, 3 studies based on animals, 15 meta-analyses, 80 reviews, 19 identified as case reports and guidelines were deleted. Besides, 19 conference abstracts and 18 without full articles were also excluded. Then, 27 full texts were scrutinized, and 6 studies were excluded for insufficient data on risk factors. In addition, 6 studies were added by searching from reference lists of 21 identified articles. Finally, 27 literatures were carried out in this systematic review and meta-analysis, with 22 for incidence, 17 for risk factors and 12 shared (9–13, 15–36).
3.2 Study characteristics
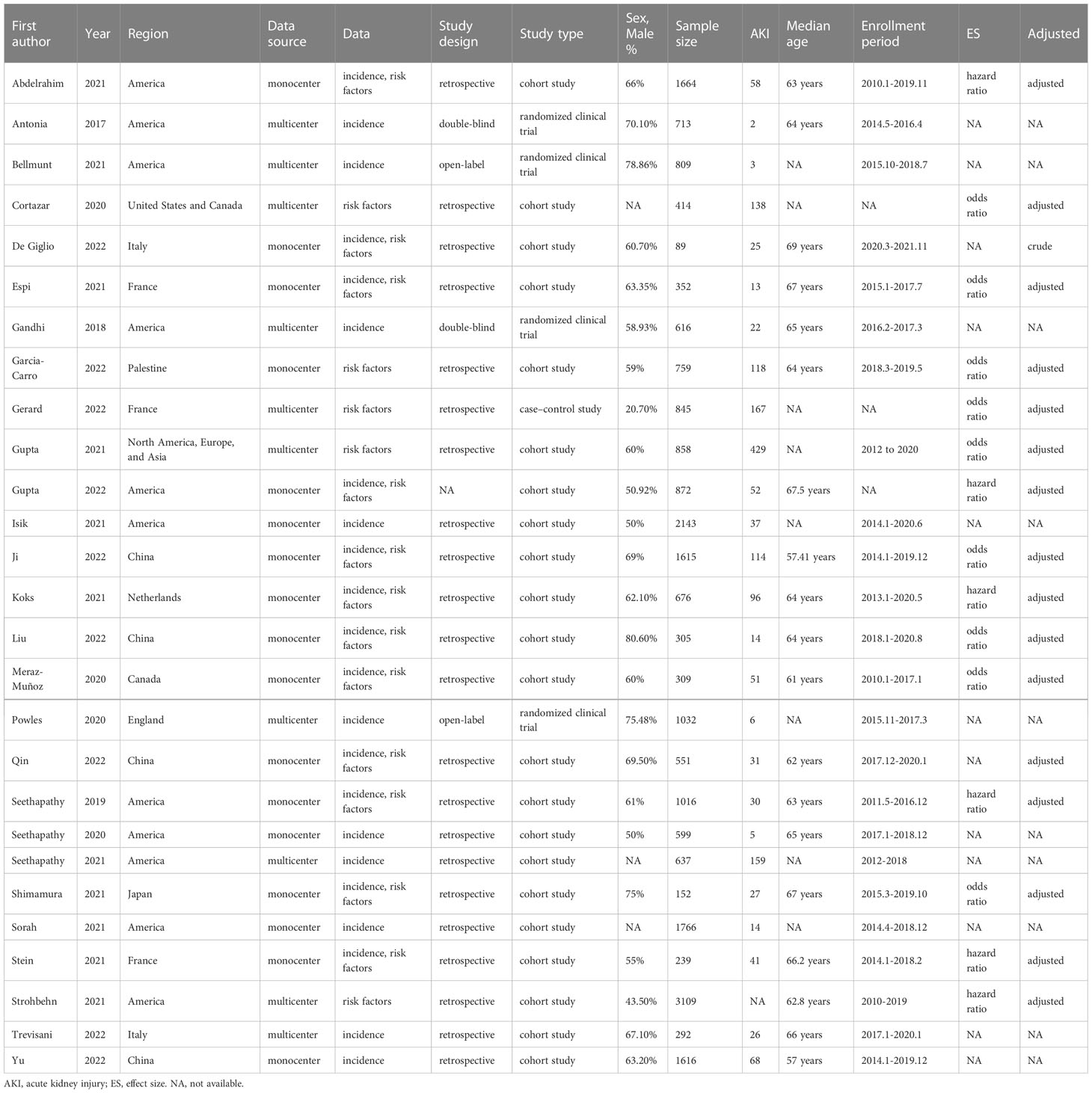
A total of 24048 participants receiving different types of ICIs due to malignancies from 27 studies were investigated in our systematic review and meta-analysis. The sample size varied between 89 and 3109, and the median age of recorded patients ranged from a minimum of 57 years to a maximum of 69 years. The majority were native to America and Asia. These articles were all published between 2017 and 2022, and studies were performed from 2010 to 2021. Despite 4 randomized clinical trials and a case-control study, the remaining 22 were cohort studies (Table 1).
3.3 The incidence of AKI following ICIs
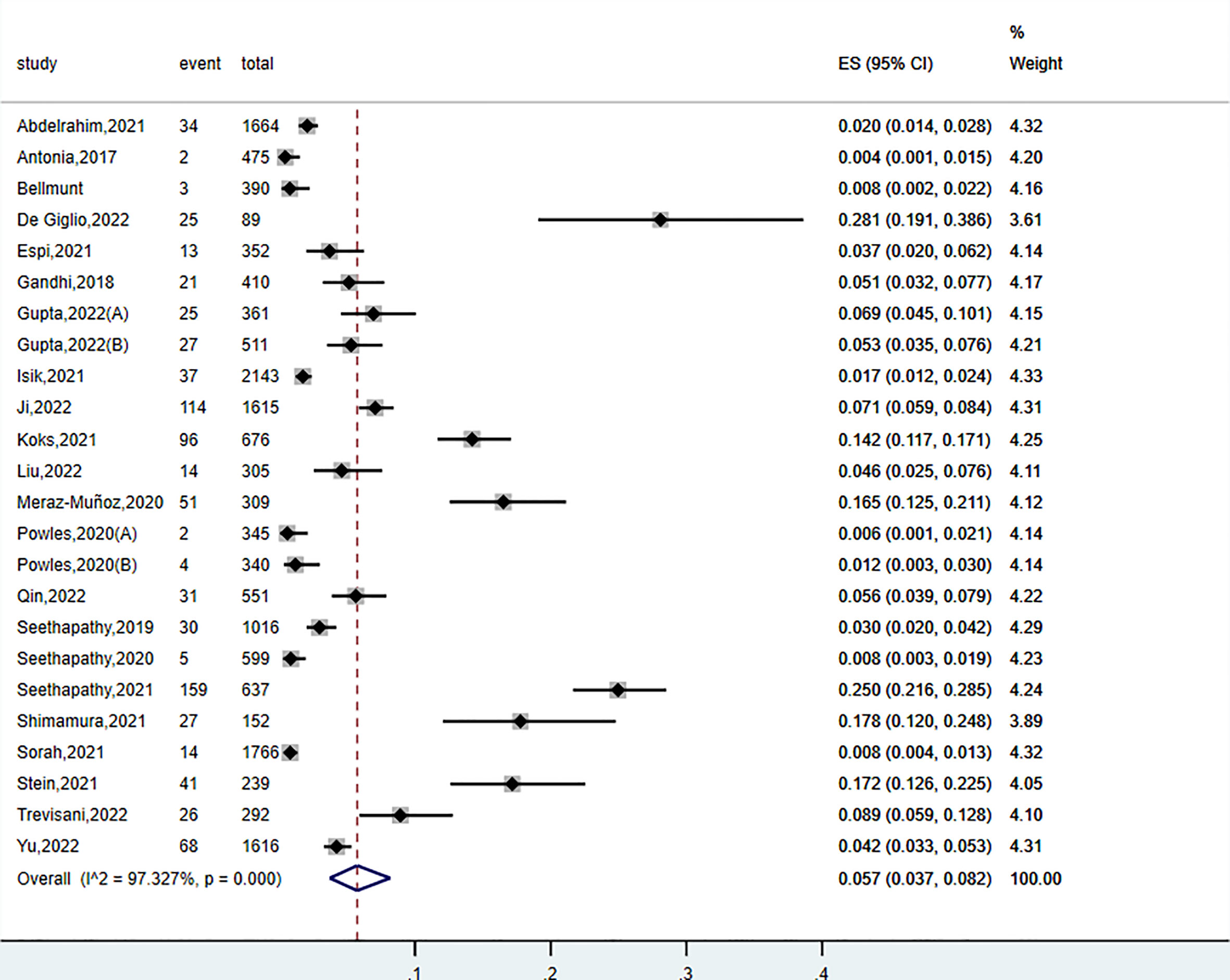
The incidence of AKI secondary to ICIs in patients with malignancies was available from 22 articles. Morbidity ranging from 0.4% to 28.1% was relatively low compared with other irAEs, such as colitis and rash (37). The overall pooled incidence of AKI following ICIs was 5.7% (95% CI: 3.7%-8.2%, P< 0.001, I2 = 97.3%) (Figure 2). Meta-regression was performed to explore the source of noted heterogeneity. We analyzed seven covariates, including region, publication year, sample size, follow-up time, male ratio, malignancy type, and ICI type. Nevertheless, none of them was acknowledged as a potential contributor to heterogeneity.
3.4 Risk factors for AKI following ICIs
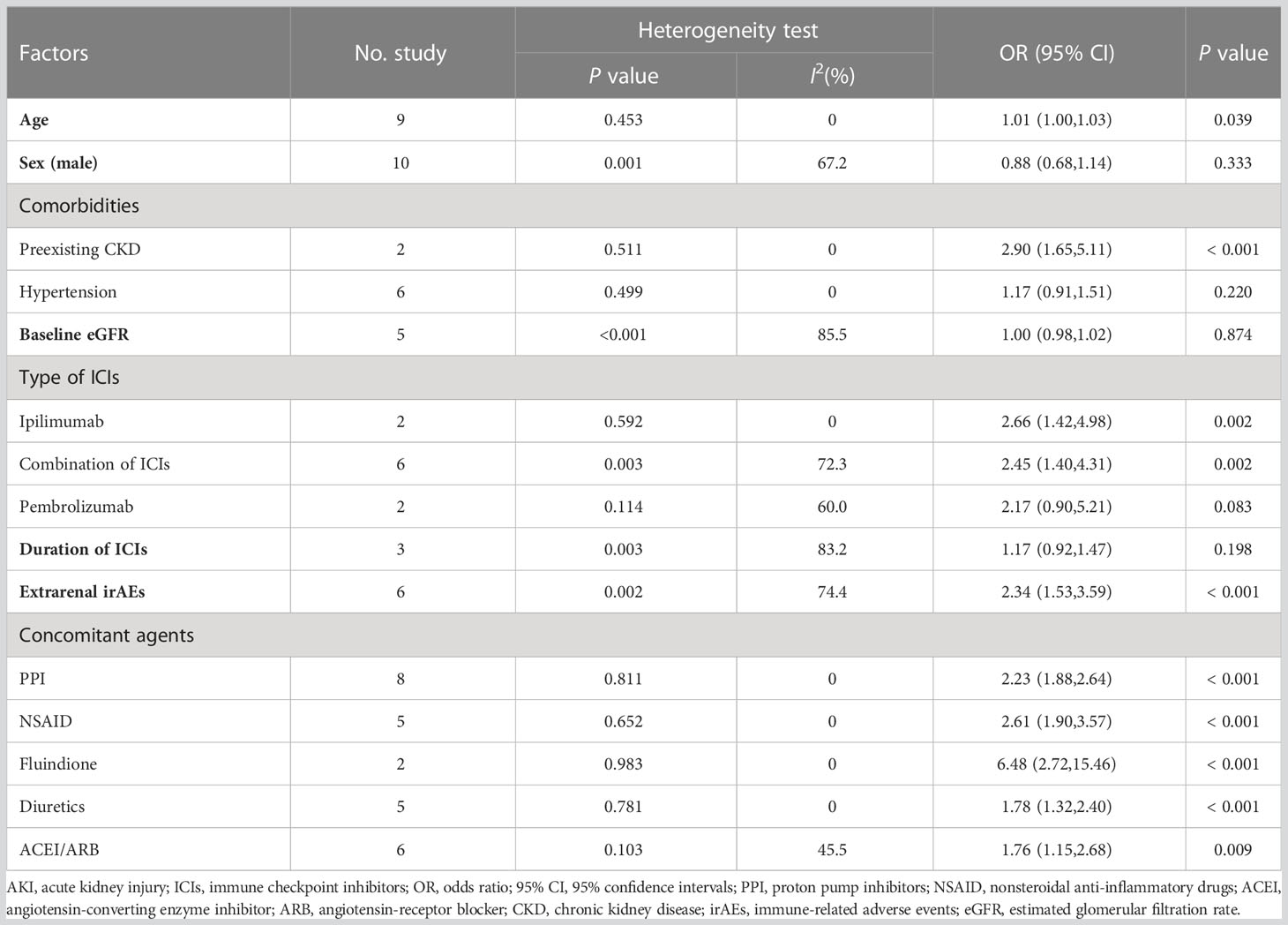
Data on risk factors for AKI in patients suffering from cancer during ICI treatment were reported by 17 papers. In most articles, comparisons were made between participants in the AKI group and the no AKI group. The summary statistics of potential risk factors are shown in Table 2 and Figure 3.
3.4.1 Age, sex and comorbidities
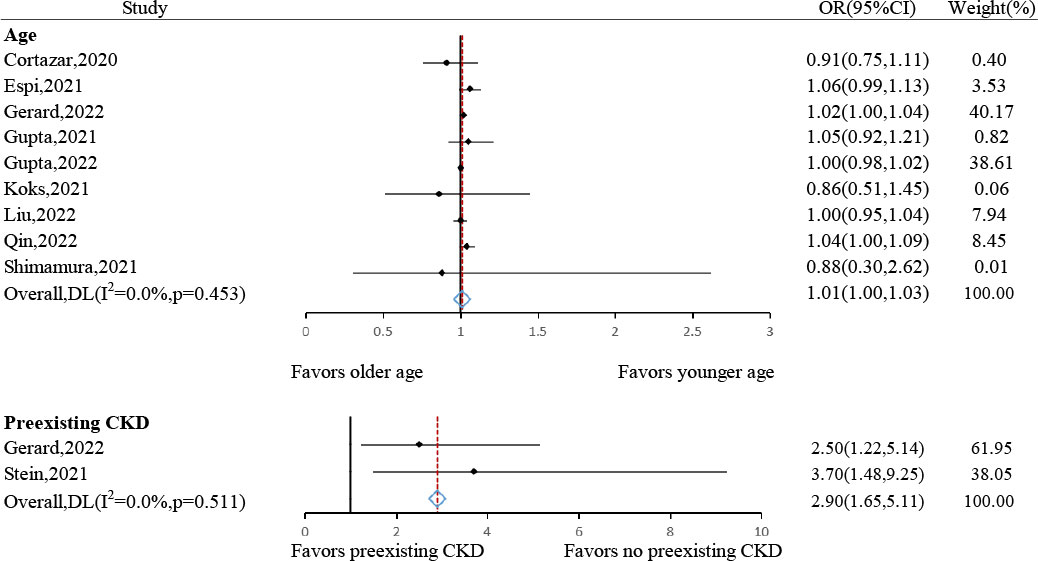
The risk of AKI following ICIs generally increased with advancing age (pooled OR: 1.01, 95% CI: 1.00–1.03, P= 0.039, I2 = 0.0%, n= 9 studies) (Figure 4). However, sex gap was not proven to be associated with AKI (male: pooled OR: 0.88, 95% CI: 0.68-1.14, P= 0.333, I2 = 67.2%, n= 10 studies) (Supplementary Figure S3)
The risk of contracting AKI after ICIs was significantly higher in patients with preexisting CKD (pooled OR: 2.90, 95% CI: 1.65–5.11, P< 0.001, I2 = 0.0%, n= 2 studies) (Figure 4), but not in those with hypertension (pooled OR: 1.17, 95% CI: 0.91–1.51, P= 0.220, I2 = 0.0%, n= 6 studies) (Supplementary Figure S4). Regarding eGFR, no statistically significant relationship with AKI was showed by our results (pooled OR: 1.00, 95% CI: 0.98–1.02, P= 0.874, I2 = 85.5%, n= 5 studies) (Supplementary Figure S5).
3.4.2 Type of ICIs and extrarenal irAEs
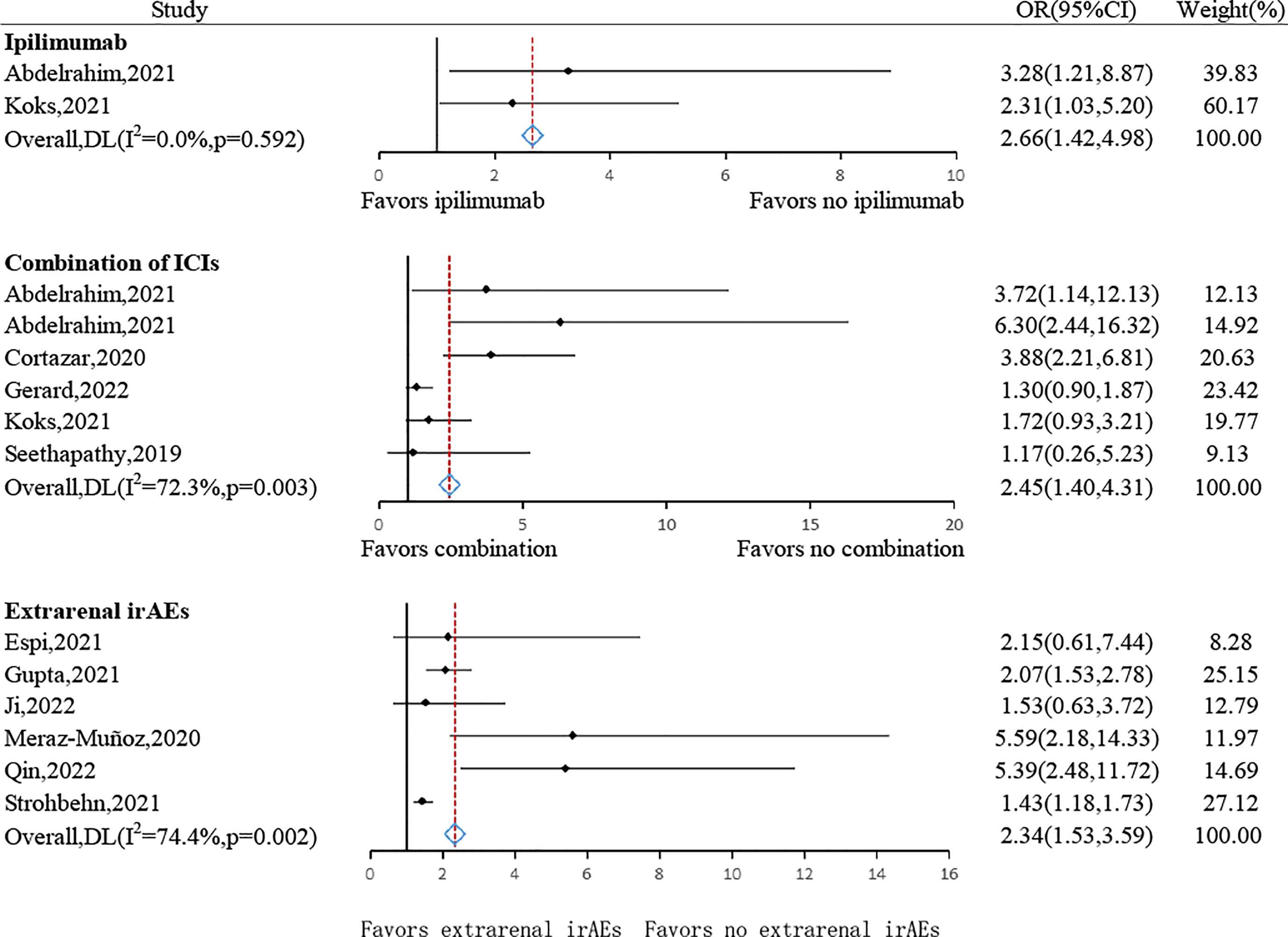
The risk of AKI following ICIs was significantly higher in cancerous individuals receiving ipilimumab (pooled OR: 2.66, 95% CI: 1.42–4.98, P= 0.002, I2 = 0.0%, n= 2 studies) or who received combined treatment with two or more kinds of ICIs (pooled OR: 2.45, 95% CI: 1.40–4.31, P= 0.002, I2 = 72.3%, n= 6 studies) (Figure 5). The risk of patients receiving pembrolizumab was not statistically different (pooled OR: 2.17, 95% CI: 0.90–5.21, P= 0.083, I2 = 60.0%, n= 2 studies) (Supplementary Figure S7). In addition, no substantial difference between the duration or cycle of ICI treatment and the risk of ICI-AKI was found (pooled OR: 1.17, 95% CI: 0.92-1.47, P= 0.198, I2 = 83.2%, n= 3 studies) (Supplementary Figure S6).
The presence of extrarenal irAEs such as colitis, hypophysitis, rash, and pneumonitis was strongly suggested as an important risk factor for AKI (pooled OR: 2.34, 95% CI: 1.53–3.59, P<0.001, I2 = 74.4%, n= 6 studies) (Figure 5) (33).
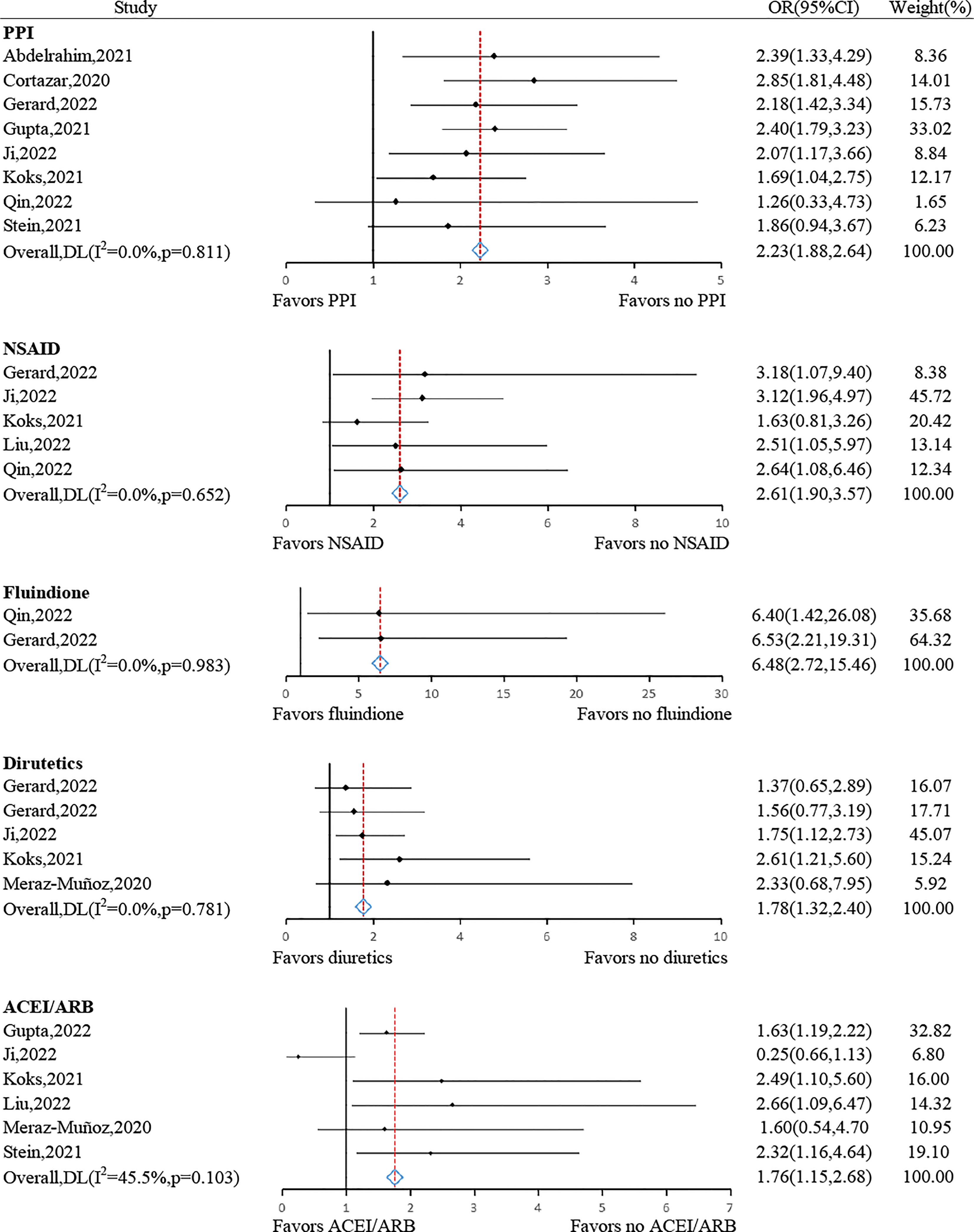
3.4.3 Concomitant agents
Various concomitant agents administered accompanied by ICIs were associated with a significantly greater risk of developing AKI, including PPIs (pooled OR: 2.23, 95% CI: 1.88–2.64, P< 0.001, I2 = 0.0%, n= 8 studies), NSAID (pooled OR: 2.61, 95% CI: 1.90–3.57, P< 0.001, I2 = 0.0%, n = 5 studies), fluindione (pooled OR: 6.48, 95% CI: 2.72–15.46, P< 0.001, I2 = 0.0%, n = 2 studies), diuretics (pooled OR: 1.78, 95% CI: 1.32–2.40, P< 0.001, I2 = 0.0%, n= 5 studies) and ACEI/ARB (pooled OR: 1.76, 95% CI: 1.15–2.68, P= 0.009, I2 = 45.5%, n= 6 studies) (Figure 6).
3.4.4 Sensitivity analysis and publication bias
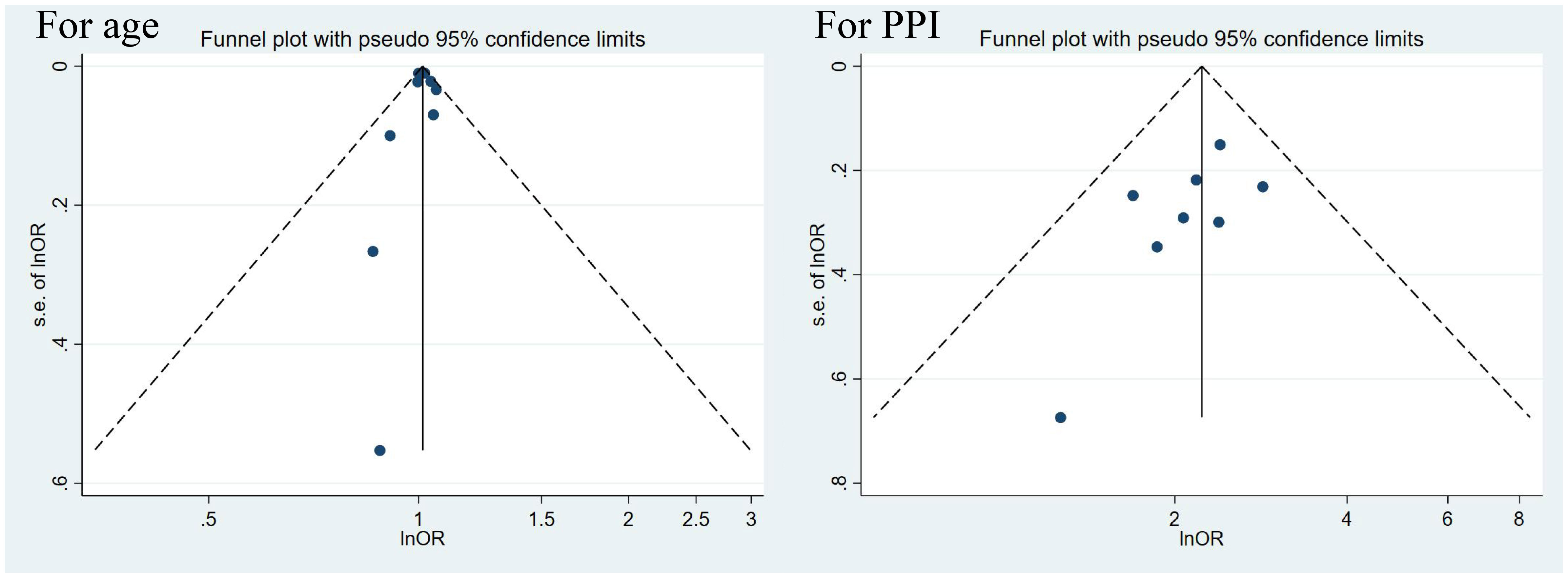
In consideration of adequate studies on age and PPI as risk factors, sensitivity and publication bias analyses were performed to verify the stability of their results. We conducted sensitivity analyses by omitting 1 study at a time and recalculating the estimates on the remaining studies. No single study was observed to influence the overall estimates (Supplementary Table S2). According to the publication bias analyses, graphical symmetry presented by the funnel plot was satisfied, and P was more than 0.05 for both Begg’s test and Egger’s test, confirming robust results (Figure 7 and Supplementary Table 3).
3.5 Time from ICIs initiation to ICI-AKI
Among the selected studies, there were 4 studies investigating median time from first ICI administration to the occurrence of ICI-AKI, ranging from 88.9 days to 112 days. The overall pooled median time was 108.07 days (Supplementary Figure S8).
4 Discussion
4.1 Principal findings and clinical interpretation
This systematic review and meta-analysis is one of the first to comprehensively reveal the incidence and substantial risk factors of AKI secondary to ICIs in patients suffering from cancer. The overall estimated pooled incidence was 5.7% based on 22 included studies. The therapeutic effects of ICIs for malignances are often accompanied by unavoidable damage to innocent organs such as the kidney due to imprecise strikes in the body (38, 39). In contrast to the previous recognition that AKI secondary to ICIs was relatively rare, with a morbidity of 1.3% in a meta-analysis conducted in 2022 (40), the overall pooled incidence of AKI was as high as 5.7% in our meta-analysis, demonstrating a greatly underrated result in the past. This inconsistency could be due to the expanding use of ICI in the latest years among vulnerable patient group, the growing awareness of ICI-related adverse effects, as well as the ambiguous definition of ICI-AKI. Only severe and fatal AKI was detected when it was reported initially, leading to an underestimation of the overall incidence at early ages. In addition, the occurrences of AKI were all attributed to ICIs in some of the included studies regardless of any other potential reason, largely responsible for uncertainties in the incidence of ICI-AKI. Given these considerations, a unified conception and early diagnosis of ICI-AKI in cancer patients are imperative for accurate estimation of the incidence. Effort to address the scarcity of representative estimates has been made by Gupta et al., who introduced a relatively clear definition of ICI-AKI based on at least one of the following: acute tubulointerstitial nephritis on kidney biopsy, received ICI therapy for at least one cycle, but this definition has not been applied widely (20). Respecting the noted incidence and high mortality rate of 15.9% for AKI after ICIs (8), proper diagnosis and refined management of this anticancer treatment-induced AKI is a challenge for both oncologists and nephrologists due to their limited clinical skills and knowledge. However, compared with other therapies against tumors with renal-associated adverse outcomes, such as small-molecule protein kinase inhibitors (PKIs), whose incidence of secondary AKI is 2.16% and corresponding mortality is 26% (41), ICIs are advantageous in terms of ultimate survival outcomes. Hence, risk factors for secondary AKI due to ICIs need to be comprehensively analyzed and applied to make individualized decisions for patients with potential risk factors and predict the development of AKI. In this random-effect meta-analysis, we extracted 15 potential risk factors investigated by at least 2 studies to be statistically analyzed. Patients with older age and preexisting CKD were at increased risk of AKI during ICI treatment. In addition, ipilimumab, the combined use of 2 or more ICIs and extrarenal irAEs were also contributors to ICI-AKI. Seethapathy et al. found that patients receiving CTLA-4, such as ipilimumab, showed a higher risk of developing AKI than those receiving PD-1 like pembrolizumab, and patients treated with PD-L1 had a similar tendency to PD-1 but have not been fully proven statistically, which was not included in this meta-analysis because no other studies have emphasized it (11). The most frequent organs affected by ICIs are skin, liver, heart, lungs and so on (42), whose impairments are significant indicators of the occurrence of ICI-AKI as extrarenal irAEs are associated with ICI-AKI. Concomitant agents are of great importance to the occurrence of AKI, among which PPI, NSAID, fluindione, diuretics and ACEI/ARB use were proven to be common risk factors. Therefore, clinicians are supposed to be cautious and evaluate the pros and cons when treating cancer patients who are receiving those therapies with ICIs. In addition to the key risk factors listed hereinbefore, other potential risk factors not included in this meta-analysis due to limited data available are displayed in Supplementary Table S4. The median time of the occurrence AKI after ICIs initiation was found to be 108.07 days by our study, in contrast to a 2022 pharmacovigilance study reporting a time interval of 48 days which however, did not clearly point out whether it was calculated from the first dose or last dose of ICIs (8).
With regard to the underlying pathogenesis of ICI-AKI, we have learned that ICIs such as anti-PD-1 and anti-CTLA-4 could activate the immune system by detecting and combining with immune checkpoints on the surface of immune cells such as T cells, B cells, and dendritic cells to prevent inhibited activation by B7 and PD-L1/PD-L2, which function as regulators of immune tolerance. AKI induced by ICIs stands a good chance of being deprived of this protective mechanism in the kidney caused by reprogramming of the immune system. Abnormally activated T cells have a tendency to attack renal cells when provoked by exogenous or endogenous factors, which also explains the result of this meta-analysis that patients with concomitant PPIs, NSAIDs and other drugs that could induce acute interstitial nephritis (AIN) are at greater risk of AKI (43). PPIs and NSAIDs can bind to renal tubules and stimulate immune responses that are suppressed under normal conditions. Interestingly, even kidney tissue can be recognized as a natural antigen (44). Therefore, renal cells are attacked by T cells activated by ICIs and the stimulation of the immune system by concomitant agents or the kidney, resulting in AKI (45). AIN was the most common lesion on kidney biopsy of ICI-AKI, demonstrating that inflammation may be an important contributor to the development of AKI in cancer patients treated with ICIs (19). Elevated levels of serum pro-inflammatory cytokines/chemokines, such as IL-1Ra and TNF-α, were detected during pharmacological treatment with ICIs (46), which may result in AKI when they immigrate to renal tissue. Extrarenal irAEs as risk factors for AKI might be explained by the multisystemic responses brought about by inflammatory factors, although this hypothesis has not yet been confirmed. The potential reason for the higher risk of AKI observed in patients receiving ipilimumab compared with other ICI drugs of anti-PD-L1 is likely due to its identity as an anti-CTLA-4 agent. In contrast, PD-L1 is expressed on renal tubular epithelial cells and may play an inhibitory role in immunopathogenesis in the kidney, although its understanding remains poor (47).
4.2 Strengths and limitations
This systematic review and meta-analysis filled the gap of insufficient and not comprehensive data on AKI following ICIs with regard to incidence and risk factors, as well as latency period of ICI-AKI. Several limitations should be noted when interpreting the results of this study. First, publications enrolled in this meta-analysis were mostly retrospective cohort studies. Potential bias is unavoidable due to the nature of source studies. Second, the definition of ICI-AKI varied across studies. A universal diagnostic criterium of ICI-AKI is needed. Third, the number of studies included in the analysis of certain risk factors was limited, which might hamper the robustness of the study findings, especially for preexisting CKD, ipilimumab and fluindione investigated by only 2 studies. In addition, as only a small fraction of the primary studies reported tumor-type specific data of AKI following ICI use, we were unable to perform subgroup analysis stratified by type of tumor.
4.3 Future directions
Some potential risk factors were not included in this meta-analysis due to the limited number of primary studies. For example, Asian participants were found by Abdelrahim et al. to have a stronger tendency to contract AKI secondary to ICIs (12). In terms of comorbidities, anemia, Alb<30 g/L or liver disease, gynecologic cancer and ICI-induced thyroiditis were reported as risk factors by only one study (19) (20) (46). More future studies are warranted to verify these candidate risk factors. Apart from them, the influence of tumor type on the occurrence of ICI-AKI also deserves further investigation. More importantly, a clear and universal definition of ICI-AKI would be helpful to standardize future research and optimize patient management.
5 Conclusions
This systematic review and meta-analysis demonstrated a substantial incidence (5.7%) of AKI in cancer patients receiving ICIs with a median latency period of 108.07 days. Older age, preexisting CKD, ipilimumab, joint use of more than one ICI, extrarenal irAEs, and use of PPI, NSAID, fluindione, diuretics and ACEI/ARB were all identified as risk factors for ICI-AKI. These findings may provide insights into the optimization of the management of patients who receive ICI treatment.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
Conceptualization: YZ, LZ and PF. Data Curation: YZ, CL, WW, LY, and CY. Formal analysis: YZ, CL, WW, YP, TY, and FN. Funding Acquisition: YZ. Supervision: YZ and PF. Writing-original draft: CL and YZ. Writing review/editing: all co-authors.
Funding
This study was supported by the Science and Technology Department of Sichuan Province (2021YJ0423) and 135 Project for Disciplines of Excellence, West China Hospital, Sichuan University (2020HXFH014). The funding sources had no involvement in carrying out the study.
Acknowledgments
We thank Dr. Lijun Zeng for giving constructive suggestions on this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2023.1173952/full#supplementary-material
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin (2018) 68:394–424. doi: 10.3322/caac.21492
2. Rowshanravan B, Halliday N, Sansom DM. CTLA-4: a moving target in immunotherapy. Blood (2018) 131:58–67. doi: 10.1182/blood-2017-06-741033
3. Sun C, Mezzadra R, Schumacher TN. Regulation and function of the PD-L1 checkpoint. Immunity (2018) 48:434–52. doi: 10.1016/j.immuni.2018.03.014
4. Zhang H, Dai Z, Wu W, Wang Z, Zhang N, Zhang L, et al. Regulatory mechanisms of immune checkpoints PD-L1 and CTLA-4 in cancer. J Exp Clin Cancer Res (2021) 40:184. doi: 10.1186/s13046-021-01987-7
5. Seidel JA, Otsuka A, Kabashima K. Anti-PD-1 and anti-CTLA-4 therapies in cancer: mechanisms of action, efficacy, and limitations. Front Oncol (2018) 8:86. doi: 10.3389/fonc.2018.00086
6. Champiat S, Lambotte O, Barreau E, Belkhir R, Berdelou A, Carbonnel F, et al. Management of immune checkpoint blockade dysimmune toxicities: a collaborative position paper. Ann Oncol (2016) 27:559–74. doi: 10.1093/annonc/mdv623
7. Postow MA, Sidlow R, Hellmann MD. Immune-related adverse events associated with immune checkpoint blockade. N Engl J Med (2018) 378:158–68. doi: 10.1056/NEJMra1703481
8. Zhu J, Wu J, Chen P, You K, Su J, Gao Z, et al. Acute kidney injury associated with immune checkpoint inhibitors: a pharmacovigilance study. Int Immunopharmacol (2022) 113:109350. doi: 10.1016/j.intimp.2022.109350
9. De Giglio A, Grandinetti V, Aprile M, Borelli G, Campus A, Croci Chiocchini AL, et al. Patterns of renal toxicity from the combination of pemetrexed and pembrolizumab for advanced nonsquamous non-small-cell lung cancer (NSCLC): a single-center experience. Lung Cancer (2022) 174:91–6. doi: 10.1016/j.lungcan.2022.10.007
10. Yu X, Wu R, Ji Y, Huang M, Feng Z. Identifying patients at risk of acute kidney injury among patients receiving immune checkpoint inhibitors: a machine learning approach. Diagnostics (Basel) (2022) 12:3157. doi: 10.3390/diagnostics12123157
11. Seethapathy H, Zhao S, Chute DF, Zubiri L, Oppong Y, Strohbehn I, et al. The incidence, causes, and risk factors of acute kidney injury in patients receiving immune checkpoint inhibitors. Clin J Am Soc Nephrol (2019) 14:1692–700. doi: 10.2215/cjn.00990119
12. Abdelrahim M, Mamlouk O, Lin H, Lin J, Page V, Abdel-Wahab N, et al. Incidence, predictors, and survival impact of acute kidney injury in patients with melanoma treated with immune checkpoint inhibitors: a 10-year single-institution analysis. Oncoimmunology (2021) 10:1927313. doi: 10.1080/2162402x.2021.1927313
13. Qin Z, Liu K, Xu X, Li T, Ge Y, Wu B, et al. Incidence, predictors and 6-month overall outcome of acute kidney injury in Chinese patients receiving PD-1 inhibitors. Future Oncol (2022) 18:1951–62. doi: 10.2217/fon-2021-1004
14. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PloS Med (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
15. Antonia SJ, Villegas A, Daniel D, Vicente D, Murakami S, Hui R, et al. Durvalumab after chemoradiotherapy in stage III non-Small-Cell lung cancer. N Engl J Med (2017) 377:1919–29. doi: 10.1056/NEJMoa1709937
16. Bellmunt J, Hussain M, Gschwend JE, Albers P, Oudard S, Castellano D, et al. Adjuvant atezolizumab versus observation in muscle-invasive urothelial carcinoma (IMvigor010): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol (2021) 22:525–37. doi: 10.1016/S1470-2045(21)00004-8
17. Cortazar FB, Kibbelaar ZA, Glezerman IG, Abudayyeh A, Mamlouk O, Motwani SS, et al. Clinical features and outcomes of immune checkpoint inhibitor-associated AKI: a multicenter study. J Am Soc Nephrol (2020) 31:435–46. doi: 10.1681/asn.2019070676
18. Gandhi L, Rodriguez-Abreu D, Gadgeel S, Esteban E, Felip E, De Angelis F, et al. Pembrolizumab plus chemotherapy in metastatic non-Small-Cell lung cancer. N Engl J Med (2018) 378:2078–92. doi: 10.1056/NEJMoa1801005
19. Gérard AO, Barbosa S, Parassol N, Andreani M, Merino D, Cremoni M, et al. Risk factors associated with immune checkpoint inhibitor-induced acute kidney injury compared with other immune-related adverse events: a case-control study. Clin Kidney J (2022) 15:1881–7. doi: 10.1093/ckj/sfac109
20. Gupta S, Short SAP, Sise ME, Prosek JM, Madhavan SM, Soler MJ, et al. Acute kidney injury in patients treated with immune checkpoint inhibitors. J Immunother Cancer (2021) 9:e003467. doi: 10.1136/jitc-2021-003467
21. Gupta S, Strohbehn IA, Wang Q, Hanna PE, Seethapathy R, Prosek JM, et al. Acute kidney injury in patients receiving pembrolizumab combination therapy versus pembrolizumab monotherapy for advanced lung cancer. Kidney Int (2022) 102:930–5. doi: 10.1016/j.kint.2022.07.019
22. Ji MS, Wu R, Feng Z, Wang YD, Wang Y, Zhang L, et al. Incidence, risk factors and prognosis of acute kidney injury in patients treated with immune checkpoint inhibitors: a retrospective study. Sci Rep (2022) 12:18752. doi: 10.1038/s41598-022-21912-y
23. Koks MS, Ocak G, Suelmann BBM, Hulsbergen-Veelken CAR, Haitjema S, Vianen ME, et al. Immune checkpoint inhibitor-associated acute kidney injury and mortality: an observational study. PloS One (2021) 16:e0252978. doi: 10.1371/journal.pone.0252978
24. Powles T, van der Heijden MS, Castellano D, Galsky MD, Loriot Y, Petrylak DP, et al. Durvalumab alone and durvalumab plus tremelimumab versus chemotherapy in previously untreated patients with unresectable, locally advanced or metastatic urothelial carcinoma (DANUBE): a randomised, open-label, multicentre, phase 3 trial. Lancet Oncol (2020) 21:1574–88. doi: 10.1016/S1470-2045(20)30541-6
25. Stein C, Burtey S, Mancini J, Pelletier M, Sallee M, Brunet P, et al. Acute kidney injury in patients treated with anti-programmed death receptor-1 for advanced melanoma: a real-life study in a single-centre cohort. Nephrol Dialysis Transplant (2021) 36:1664–74. doi: 10.1093/ndt/gfaa137
26. Espi M, Teuma C, Novel-Catin E, Maillet D, Souquet PJ, Dalle S, et al. Renal adverse effects of immune checkpoints inhibitors in clinical practice: ImmuNoTox study. Eur J Cancer (2021) 147:29–39. doi: 10.1016/j.ejca.2021.01.005
27. Garcia-Carro C, Bolufer M, Bury R, Cataneda Z, Munoz E, Felip E, et al. Acute kidney injury as a risk factor for mortality in oncological patients receiving checkpoint inhibitors. Nephrol Dialysis Transplant (2022) 37:887–94. doi: 10.1093/ndt/gfab034
28. Isik B, Alexander MP, Manohar S, Vaughan L, Kottschade L, Markovic S, et al. Biomarkers, clinical features, and rechallenge for immune checkpoint inhibitor renal immune-related adverse events. Kidney Int Rep (2021) 6:1022–31. doi: 10.1016/j.ekir.2021.01.013
29. Liu K, Qin Z, Ge Y, Bian A, Xu X, Wu B, et al. Acute kidney injury in advanced lung cancer patients treated with PD-1 inhibitors: a single center observational study. J Cancer Res Clin Oncol (2022) 18:1951-1962. doi: 10.1007/s00432-022-04437-9
30. Meraz-Muñoz A, Amir E, Ng P, Avila-Casado C, Ragobar C, Chan C, et al. Acute kidney injury associated with immune checkpoint inhibitor therapy: incidence, risk factors and outcomes. J Immunother Cancer (2020) 8:e000467. doi: 10.1136/jitc-2019-000467
31. Seethapathy H, Zhao S, Strohbehn IA, Lee M, Chute DF, Bates H, et al. Incidence and clinical features of immune-related acute kidney injury in patients receiving programmed cell death ligand-1 inhibitors. Kidney Int Rep (2020) 5:1700–5. doi: 10.1016/j.ekir.2020.07.011
32. Seethapathy H, Street S, Strohbehn I, Lee M, Zhao SH, Rusibamayila N, et al. Immune-related adverse events and kidney function decline in patients with genitourinary cancers treated with immune checkpoint inhibitors. Eur J Cancer (2021) 157:50–8. doi: 10.1016/j.ejca.2021.07.031
33. Shimamura Y, Watanabe S, Maeda T, Abe K, Ogawa Y, Takizawa H. Incidence and risk factors of acute kidney injury, and its effect on mortality among Japanese patients receiving immune check point inhibitors: a single-center observational study. Clin Exp Nephrol (2021) 25:479–87. doi: 10.1007/s10157-020-02008-1
34. Sorah JD, Rose TL, Radhakrishna R, Derebail VK, Milowsky MI. Incidence and prediction of immune checkpoint inhibitor-related nephrotoxicity. J Immunother (2021) 44:127–31. doi: 10.1097/cji.0000000000000338
35. Strohbehn IA, Street S, Chute D, Seethapathy H, Lee M, Seethapathy R, et al. Immune checkpoint inhibitor-induced thyroiditis is a risk factor for acute and chronic kidney dysfunction. Nephrol Dialysis Transplant (2022) 37:187–9. doi: 10.1093/ndt/gfab240
36. Trevisani F, Di Marco F, Floris M, Pani A, Minnei R, Scartozzi M, et al. Renal function outcomes in metastatic non-Small-Cell lung carcinoma patients treated with chemotherapy or immune checkpoint inhibitors: an unexpected scenario. Vaccines (2022) 10:679. doi: 10.3390/vaccines10050679
37. Khoja L, Day D, Wei-Wu Chen T, Siu LL, Hansen AR. Tumour- and class-specific patterns of immune-related adverse events of immune checkpoint inhibitors: a systematic review. Ann Oncol (2017) 28:2377–85. doi: 10.1093/annonc/mdx286
38. Ramos-Casals M, Brahmer JR, Callahan MK, Flores-Chávez A, Keegan N, Khamashta MA, et al. Immune-related adverse events of checkpoint inhibitors. Nat Rev Dis Primers (2020) 6:38. doi: 10.1038/s41572-020-0160-6
39. Das S, Johnson DB. Immune-related adverse events and anti-tumor efficacy of immune checkpoint inhibitors. J Immunother Cancer (2019) 7:306. doi: 10.1186/s40425-019-0805-8
40. Righini M, Mollica V, Rizzo A, La Manna G, Massari F. Renal toxicities in cancer patients receiving immune-checkpoint inhibitors: a meta-analysis. J Clin Med (2022) 11:4373. doi: 10.3390/jcm11154373
41. Fan Q, Ma J, Zhang B, Li Q, Liu F, Zhao B. Assessment of acute kidney injury related to small-molecule protein kinase inhibitors using the FDA adverse event reporting system. Cancer Chemother Pharmacol (2020) 86:655–62. doi: 10.1007/s00280-020-04151-8
42. Esfahani K, Elkrief A, Calabrese C, Lapointe R, Hudson M, Routy B, et al. Moving towards personalized treatments of immune-related adverse events. Nat Rev Clin Oncol (2020) 17:504–15. doi: 10.1038/s41571-020-0352-8
43. Koda R, Watanabe H, Tsuchida M, Iino N, Suzuki K, Hasegawa G, et al. Immune checkpoint inhibitor (nivolumab)-associated kidney injury and the importance of recognizing concomitant medications known to cause acute tubulointerstitial nephritis: a case report. BMC Nephrol (2018) 19:48. doi: 10.1186/s12882-018-0848-y
44. Marco T, Anna P, Annalisa T, Francesco M, Stefania SL, Stella D, et al. The mechanisms of acute interstitial nephritis in the era of immune checkpoint inhibitors in melanoma. Ther Adv Med Oncol (2019) 11:1758835919875549. doi: 10.1177/1758835919875549
45. Perazella MA, Shirali AC. Nephrotoxicity of cancer immunotherapies: past, present and future. J Am Soc Nephrol (2018) 29:2039–52. doi: 10.1681/asn.2018050488
46. Murakami N, Motwani S, Riella LV. Renal complications of immune checkpoint blockade. Curr Probl Cancer (2017) 41:100–10. doi: 10.1016/j.currproblcancer.2016.12.004
Keywords: immune checkpoint inhibitors, acute kidney injury, cancer, incidence, risk factors
Citation: Liu C, Wei W, Yang L, Li J, Yi C, Pu Y, Yin T, Na F, Zhang L, Fu P and Zhao Y (2023) Incidence and risk factors of acute kidney injury in cancer patients treated with immune checkpoint inhibitors: a systematic review and meta-analysis. Front. Immunol. 14:1173952. doi: 10.3389/fimmu.2023.1173952
Received: 25 February 2023; Accepted: 10 May 2023;
Published: 29 May 2023.
Edited by:
Xuyao Zhang, Fudan University, ChinaReviewed by:
Idris Boudhabhay, Assistance Publique Hopitaux De Paris, FranceQiong Bai, Peking University Third Hospital, China
Fausta Catapano, Sant’Orsola-Malpighi Polyclinic, Italy
Copyright © 2023 Liu, Wei, Yang, Li, Yi, Pu, Yin, Na, Zhang, Fu and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuliang Zhao, emhhb3l1bGlhbmdAc2N1LmVkdS5jbg==
†These authors have contributed equally to this work
 Caihong Liu1†
Caihong Liu1† Letian Yang
Letian Yang Yuliang Zhao
Yuliang Zhao