- 1Department of Public Health Pharmacy and Management, School of Pharmacy, Sefako Makgatho Health Sciences University, Garankuwa, Pretoria, South Africa
- 2Saselamani Pharmacy, Saselamani, South Africa
- 3Department of Pharmacy, Faculty of Medicine, University of Banja Luka, Banja Luka, Bosnia and Herzegovina
- 4School of Health Sciences, University of Manchester, Manchester, United Kingdom
- 5Department of Pharmacology, Faculty of Health Sciences, University of Pretoria, Pretoria, South Africa
- 6Centre for Neonatal and Paediatric Infection, Institute for Infection and Immunity, City St. George’s University of London, London, United Kingdom
- 7Health Economics Research Centre, Nuffield Department of Population Health, University of Oxford, Oxford, United Kingdom
- 8Department of Pharmacoepidemiology, Strathclyde Institute of Pharmacy and Biomedical Sciences, University of Strathclyde, Glasgow, United Kingdom
- 9South African Vaccination and Immunisation Centre, Sefako Makgatho Health Sciences University, Pretoria, South Africa
Background: Antimicrobial resistance is a considerable global health threat especially among low- and middle-income countries, exacerbated by considerable inappropriate dispensing of antibiotics. There have though been concerns with variable levels of dispensing of antibiotics without a prescription in South Africa. Consequently, a need to comprehensively estimate current levels of dispensing of antibiotics without a prescription, which was the aim of this study.
Methods: Administer a previously piloted questionnaire to all currently operating community pharmacies in a rural province, where dispensing of antibiotics without a prescription is likely to be greatest. The questionnaire included data on the estimated prevalence of antibiotics dispensed, their class and indication, and whether dispensed without a prescription. Community pharmacies were categorized into three: Independent, Chain and Franchise.
Results: 128/169 (75.7%) operational pharmacies participated, with independent pharmacies representing the majority (60.9%). There was a 78.3% response rate from 400 distributed questionnaires, including 106 pharmacists (33.9%) and 207 pharmacist assistants (66.1%) from 128 pharmacies. Antibiotics accounted for 47.9% (95% CI: 47.2%-48.6%) of all medicines dispensed. Penicillins were the most prevalent antibiotic dispensed (41.1%). Almost half (47.2%) of the antibiotics dispensed included macrolides, fluoroquinolones and cephalosporins, which are typically antibiotics from the Watch group. Sexually transmitted infections (33.5%) and upper respiratory tract infections (25.8%) were the most frequent indications for antibiotic dispensing. Overall, 69.3% of 128 participating pharmacies in this rural province in South Africa admitted to dispensing antibiotics without a prescription in the past 14 days, principally among independent pharmacies (98.7%). However, estimates suggest only 8.6% of the total volume of antibiotics being dispensed were dispensed without a prescription among the 88 community pharmacies admitting to this practice in the past 3 days. Encouragingly, 98.1% of community pharmacists and 97.6% of pharmacist assistants indicated they always or mostly offered symptomatic relief before dispensing antibiotics without a prescription to patients with self-limiting conditions.
Conclusion: There were considerable concerns regarding the prescribing and dispensing of antibiotics in this rural province including Watch antibiotics. This included the number of community pharmacies, especially independent pharmacies, where patients could purchase antibiotics without a prescription. Multiple strategies involving all key stakeholder groups are need to improve future antibiotic use across South Africa and reduce AMR.
1 Introduction
Antimicrobial resistance (AMR) is a growing global public health threat, contributing to significant morbidity and mortality worldwide (1–3). If left unaddressed, AMR could become the next pandemic, necessitating urgent interventions (4, 5). Beyond its appreciable public health impact, AMR is also associated with substantial economic costs (6, 7). The financial burden stems from increased hospital stays, more expensive treatments and productivity losses due to prolonged illness and premature death (7, 8). The greatest burden of AMR is currently in low- and middle-income countries (LMICs), which includes sub-Saharan African countries (9–12). AMR is driven by the overuse of antibiotics, which is unlike the situation seen with other medicines (13–15). This includes considerable purchasing of antibiotics without a prescription for essentially self-limiting infections, particularly prevalent in LMICs including Sub-Saharan Africa, and enhanced by socioeconomic and cultural issues (11–13, 16–23).
Key global activities to reduce AMR include the launch of the Global Action Plan (GAP) by the World Health Organization (WHO) in 2015 (24), followed by the AWaRe classification of antibiotics into three groups (Access, Watch and Reserve) in 2017 based on their resistance profile followed by the launch of the WHO AWaRe antibiotic guidance book in 2022 (25–27). Across Africa, the GAP was subsequently translated into National Action Plans (NAPs) (28–31). There are though concerns with the implementation of NAPs among African countries in view of available personnel and resource challenges (28, 32–35).
In South Africa despite the launch of their NAP to combat AMR in 2017 (36), recent evidence suggests that antibiotics continue to be dispensed without prescriptions in some community pharmacies, across both rural and urban areas (37–40). However, the findings have been inconsistent, and little is known about the current extent of this practice, the types and classes of antibiotics dispensed, or the knowledge and attitudes of pharmacy personnel in these settings, with key potential developments including improved monitoring of current antibiotic utilization patterns (41).
Overall, there are a number of identified areas of concern with current antibiotic use among LMICs including among African countries. These include current high levels of inappropriate prescribing and dispensing of antibiotics particularly in ambulatory care including high levels of antibiotics from the WHO Watch list, with ambulatory care accounting for up to 95% of total human antibiotic use in LMICs (42–44) as well as challenges with supply chains and high rates of substandard and falsified medicines including antibiotics (45, 46). In some LMICs, there are also an appreciable number of available branded generic Watch and Reserve antibiotics adding to AMR with their manufacturers pushing their use among community pharmacies (47).
Ongoing activities in South Africa to reduce AMR include regularly monitoring the goals and objectives of the NAP alongside active surveillance of AMR, initiatives to improve infection prevention and control, implementation and monitoring of antimicrobial stewardship (AMS) activities including antimicrobial stewardship programs (ASPs), and promoting antibiotic guardians (48–54). This is important, given appreciably increasing utilization of antibiotics in recent years in the public sector in South Africa, with rising use of antibiotics from the WHO Watch list which has a greater resistance potential and accounting for 52% of total antibiotic use in 2022 (55–57).
In many LMICs, certain perceptions surrounding antibiotics contribute to their widespread use without a prescription, with both prescribers and patients believing that antibiotics are a ‘quick fix’ for common infections including many viral infections (43). Known factors which drive patients to seek antibiotics directly from pharmacies rather than consulting healthcare professionals (HCPs) in LMICs, incorporating Sub-Saharan African countries, include long waiting times to see healthcare professionals (HCPs) in primary healthcare clinics (PHCs) and/or limited access to primary care facilities, travel costs and time to visit HCPs in PHCs, high patient co-payments for both visiting HCPs and medicines in LMICs without universal health coverage (UHC), concerns with the limited knowledge of both dispensers and patients regarding antibiotics and AMR, lack of communication skills among dispensers, as well as shortages of antibiotics in PHC settings due to inaccurate forecasting and limited resources (12, 17, 19, 38, 58–61). These experiences with public sector PHC facilities, alongside issues of knowledge, contrast with the convenience and ready availability of antibiotics among community pharmacists and drug sellers, which is an important consideration especially in rural areas in LMICs (17, 19, 62–68).
Health literacy gaps also play a significant role in the appropriate use of antibiotics whereby patients lack knowledge and awareness regarding the risks associated with self-medication, coupled with their misconceptions about antibiotic efficacy for viral infections, increases this practice (43, 45, 62). The business model of community pharmacies in LMICs also contributes to over-the-counter (OTC) antibiotic sales, as profit motives and competition can encourage dispensers to meet patient demands, rather than strictly adhering to current regulations (43, 45, 63).
As a result, we have seen high rates of purchasing of antibiotics without a prescription among Sub-Saharan African countries, up to 100% of community pharmacies in some African countries (17, 69–71). However, this is not always the case with limited or no self-purchasing of antibiotics in Botswana, enhanced by UHC as well as strictly enforced regulations to ensure that antibiotics are only dispensed to patients presenting with a prescription (17, 72). There is a similar situation in Namibia with the instigation of strict regulations among community pharmacies, coupled with their monitoring and training concerning key issues surrounding antibiotics and AMR, even during the COVID-19 pandemic (17, 73–75). This demonstrates the impact of strong governance and economic stability, alongside UHC, which results in better access to healthcare, reducing the need to purchase antibiotics from community outlets without a prescription. We have also seen limited or no self-purchasing of antibiotics for viral infections, including patients with COVID-19, among community pharmacies linked with the University of Nairobi in Kenya (17, 76, 77).
As mentioned, there has been variable purchasing of antibiotics without a prescription in South Africa with limited or no purchasing seen in the studies of Anstey Watkins et al. (2016) and Do et al. (2021) in rural South Africa (37, 38). This contrasts with the findings of Mokwele et al. (39) who found that antibiotics were being sold without a prescription among privately-owned but not corporate (franchised) pharmacies (39). Sono et al. (40) had similar findings to Mokwele et al. (2020) when surveying both community pharmacies and patients in recent pilot studies (39, 40, 78). This is despite current legislation prohibiting the dispensing and sale of antibiotics without a prescription in South Africa to enhance patient safety as well as promote the responsible use of antibiotics (17, 40). Rural areas in South Africa face unique challenges that can contribute to the sale of antibiotics without a prescription. These include limited healthcare infrastructure, long travel distances to clinics, and waiting times when at public sector PHC facilities. These challenges, alongside financial constraints, make community pharmacies a more accessible and pertinent option for patients. However, this is not always the case especially with high levels of unemployment versus free healthcare, including medicines, in PHC facilities (38). Additionally, pharmacists’ perspectives on antibiotic dispensing are shaped by their knowledge, attitudes, financial gain and prioritizing patient convenience over strict adherence to legal requirements of obtaining antibiotics. These findings mirror concerns with the current prescribing of antibiotics among HCPs in PHC facilities in South Africa, with high rates of prescribing of antibiotics seen for essentially self-limiting conditions (79–81). In an ongoing study, Chigome et al. (82) found that when surveying 615 patients visiting PHC clinics in South Africa, at least one antibiotic was prescribed to 87.0% of attending patients, 53.4% being Access antibiotics and 46.6% Watch antibiotics. The most common symptoms where antibiotics were prescribed included genital discharge (21.8%) and painful urination (18.4%) as well as acute cough (17.7%) and a sore throat (13.5%) (82). This mirrors generally the increasing use of Watch antibiotics in the public healthcare system in South Africa in recent years (55, 56).
In view of conflicting evidence regarding the extent of dispensing of antibiotics without a prescription in South Africa, coupled with ongoing concerns with AMR in the country, there is a need to extend our pilot study among pharmacists and pharmacist assistants in rural South Africa (40). This includes documenting the extent of the problem in a larger sample as well as appraising community pharmacy personnel’s knowledge of antibiotics and AMR. Subsequently using the findings to propose potential activities among all key stakeholder groups to reduce AMR in South Africa. The first step in this process is to comprehensively assess current dispensing patterns for antibiotics among community pharmacists in South Africa, especially in rural areas where problems with accessing PHCs are likely to be greatest. This incorporates assessing the prevalence and type of antibiotics typically dispensed in rural pharmacies, their indications and the extent of any self-purchasing of antibiotics. Alongside this, common approaches undertaken by pharmacists and pharmacist assistants when they are consulted by patients with self-limiting conditions such as upper respiratory tract infections (URTIs). Subsequently, assessing their knowledge regarding key aspects of antibiotics, AMR and AMS as well as the risks associated with dispensing antibiotics without a prescription. The findings can be used to suggest potential activities in South Africa to reduce inappropriate dispensing of antibiotics, building on recent suggestions among LMICs (21, 43, 45).
We are also aware that patients play a key role across LMICs, including South Africa, with influencing both the prescribing and dispensing of antibiotics in ambulatory care for essentially self-limiting conditions such as URTIs (43, 83). This is exacerbated by their limited knowledge of antibiotics, AMR and AMS, as well as similarly among pharmacists and their assistants, alongside any profit motive (43, 78, 79, 84–87). However, in this paper, the principal focus will be on the perceived nature and extent of antibiotic prescriptions, including indications, and the perceived extent of dispensing of antibiotics without a prescription among community pharmacies in rural South Africa. Follow-up papers will explore in more detail community pharmacists’ and their assistants’ knowledge, attitude and practices towards antibiotics, as well as similar issues among patients, to provide further guidance on suggested educational and other activities among key stakeholder groups to reduce AMR in South Africa.
2 Materials and methods
2.1 Study setting and design
Community pharmacies in a rural province were used for the study setting since, as mentioned, the extent of any self-purchasing of antibiotics in South Africa is likely to be greatest in this setting (21, 40). Community pharmacies in South Africa are principally divided into three categories: chain pharmacies, franchise pharmacies and independent pharmacies. Chain pharmacies include ‘Clicks’, ‘Dischem’ and ‘Medirite’ at Checkers (supermarket), which are owned by corporate entities. Franchise pharmacies are independently owned by the franchisee but operate under a brand name and include ‘The Local Choice’, ‘Link’ and ‘Van Heerden’. Independent pharmacies are standalone pharmacies with no ties to a particular brand or group.
We utilized a descriptive self-administered survey method to collect data directly from community pharmacists and pharmacist assistants thereby avoiding the introduction of interviewer bias.
The 11 pharmacies who participated in the pilot study, described previously (40), were not included in the main study. All the remaining 186 pharmacies that were identified at the time of the study across this rural South African Province were the target population for this study. A comprehensive census approach was employed, ensuring that all eligible pharmacies within the Province were included in the study, thereby maximizing representation and minimizing selection bias. This method allowed for a thorough assessment of dispensing practices across the different community pharmacy settings, particularly in rural areas where healthcare access challenges are mostly experienced.
2.2 Data collection instrument and pilot study
The data collection instrument (Supplementary Table 1) (40) was designed to capture key variables related to antibiotic dispensing patterns, management of self-limiting conditions as well as participants’ knowledge of antibiotics and AMR. A pilot study was previously conducted with the aim of evaluating the suitability of the initial data collection instrument and subsequently recommending necessary modifications (40). The pilot study focused on the clarity, relevance, and effectiveness of the survey questions and methodologies used. The goal was to ensure that the final instrument could successfully elicit the information needed to address the research questions and achieve the objectives of the main study.
Through analysis of participant feedback and responses, we identified potential shortcomings and challenges encountered during the pilot phase. These insights guided the refinement and optimization of the data collection instrument, ensuring its appropriateness for broader application in the main study. The data collection instrument was subsequently revised to ensure the final questionnaire was comprehensive, appropriately structured, and could be completed within 10 minutes to enhance likely participation in the study (40). The pilot study confirmed that the length of the questionnaire was optimal for maintaining engagement while collecting meaningful data. This approach was undertaken to enhance the validity of the data and the robustness of the findings (40).
The finalized questionnaire collected information on the type of community pharmacy, numbers and types of staff, as well as participants’ basic sociodemographic information. Key variables on estimated antibiotic use included the number of items (medicines including antibiotics) typically dispensed in a day among participating community pharmacies over a typical recent week (7 days). Furthermore, the estimated percentage that antibiotics represented of the estimated total number of items typically dispensed over the identified period. To reduce recall bias, estimates were based on broad therapeutic categories and reported as either daily means or categorized ranges. The nature of antibiotics dispensed, whether dispensed following a prescription or purchased without a prescription, were grouped by their Anatomical, Therapeutic and Chemical (ATC) classification, i.e. penicillins, macrolides, fluoroquinolones, cephalosporins and others (88). Respondents who were unable to confidently classify specific antibiotics into the major ATC classes were permitted to group them under “Other”. Antibiotics were not categorized further according to their WHO AWaRe classification of Access, Watch, or Reserve, as there could be greater recall difficulties with this approach (27, 89). However, the penicillins are typically Access antibiotics with macrolides, fluoroquinolones, and cephalosporins typically from the WHO Watch group (27, 89). Antibiotics classified as “Other” may include those not falling within the major Access or Watch categories. All estimates were self-reported; consequently, should be interpreted with caution with recognition of potential recall limitations.
Potential indications for antibiotic dispensing, which were based on previous publications, included URTIs, lower respiratory tract infections (LRTIs), sexually transmitted infections (STIs), urinary tract infections (UTIs), skin and soft tissue infections (SSTIs) and others (16, 17). Similar indications were collected for any self-purchasing of antibiotics. Alongside this, whether OTC medicines were offered first to patients who presented with self-limiting infectious disease symptoms, including coughs, colds or influenza, before antibiotics were sold without a prescription.
2.3 Data collection and study participants
Four trained data collectors, including two of the co-authors (TMM and MTM), approached the pharmacist in charge of each community pharmacy they visited, with an invitation for all pharmacists and pharmacist assistants present in the pharmacy on the day of data collection to participate in the study. The rationale for the study was explained to those present to encourage their participation; however, emphasizing that participation was entirely voluntary and that their replies would remain confidential. Participants were subsequently requested to complete the questionnaire independently, providing insights into their current practices and knowledge regarding infectious diseases, antibiotics and AMR. If no pharmacist was present at the time of data collection, the questionnaire was completed by pharmacist assistants only.
Each questionnaire had a consent form attached, which participants were requested to sign prior to completion of the questionnaire and subsequently place this in a sealed box in the pharmacy. Pharmacists and pharmacist assistants were subsequently requested to place their completed anonymized questionnaires into a sealed envelope that was provided and subsequently place these in a separate sealed box in the pharmacy. Two separate sealed boxes were provided to ensure that the questionnaire responses could not be linked back to signed consent forms. The sealed boxes were collected at the end of the day or the next day depending on what was practically feasible during data collection. This approach allowed participants to respond to the questionnaire at their own pace while maintaining anonymity.
2.4 Data management and analysis
The data entry process was conducted using Microsoft Excel™, where TMM initially entered all the data. A second individual subsequently performed a double-check of the data entry to ensure the accuracy of the entered data. Before analysis, the data were cleaned and coded to standardize responses and eliminate inconsistencies. In cases where discrepancies were observed in the estimated number of items and antibiotics dispensed within a particular pharmacy, the response from the participating pharmacist, as opposed to their assistants, was prioritized as the primary source, as they typically have direct oversight of pharmacy operations. In cases where only pharmacist assistants from a particular pharmacy responded to the questionnaire, their responses were utilized accordingly. This occurred when no pharmacist in charge was available at the time of data collection. Similarly, when only pharmacists were present at participating community pharmacies, their responses were used.
Once finalized, the cleaned and coded data was imported into jamovi (version 2.6) (https://www.jamovi.org/) for descriptive statistical analysis. Frequencies and percentages were calculated to summarize categorical variables. The Wilson score interval method was used for calculating 95% confidence intervals (CI) for proportions where appropriate. Means with standard deviation and medians with quartiles were calculated for continuous variables.
2.5 Ethical considerations
Ethical approval for the study was obtained from the Sefako Makgatho University Research Ethics Committee. The National Department of Health was not contacted for permission to collect data as no public sector facilities were surveyed. Participation in the study was completely voluntary, with potential participants being informed that they could withdraw from the study at any time without providing a reason for their decision. All participants were required to provide written informed consent for participation, with signed consent forms placed in a separate sealed box to keep the replies anonymous.
All responses were kept confidential, with data stored securely in a password-protected computer and backed up in a cloud with access to the principal investigator (TMM) only. Data will be securely stored for a period of 5 years after the results have been published, after which it will be safely destroyed in compliance with university policies.
3 Results
3.1 Response rates and the characteristics of participants
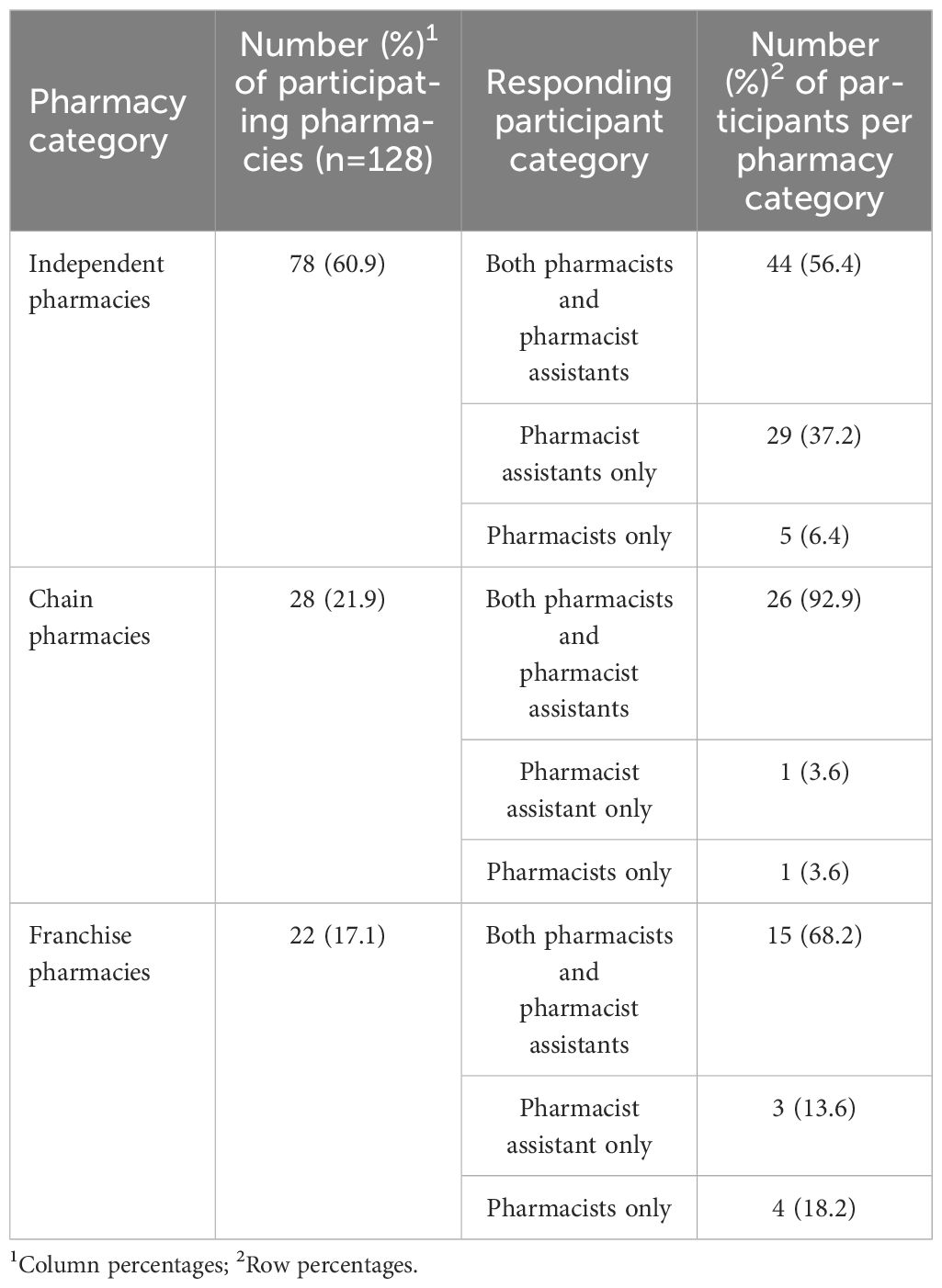
Of the 186 pharmacies targeted across this rural province for this study, 17 pharmacies (9.1%) were found to be non-operational, meaning they could not be invited to participate in the survey. Among the 169 operational pharmacies, 41 (24.3%) declined participation due to a number of reasons. These included time constraints, the need for owner approval before participation and the absence of qualified personnel to complete the questionnaire. Ultimately, 128 pharmacies participated, resulting in a participation rate of 75.7% at the pharmacy level (128/169 operational pharmacies). Among participating pharmacies, independent pharmacies accounted for almost two thirds (60.9%; n=78), while chain pharmacies and franchise pharmacies accounted for 21.9% (n=28) and 17.1% (n=22) respectively of all pharmacies surveyed (Table 1).
A total of 400 questionnaires were distributed among participating pharmacies, of which 313 completed questionnaires were returned, resulting in a response rate of 78.3% at the individual questionnaire level. Participants included 106 pharmacists (33.9%) and 207 pharmacist assistants (66.1%). Pharmacist assistants were the sole participants in a minority of chain (3.6%) and franchise (13.6%) pharmacies, however, the sole participant in 37.2% of independent pharmacies (Table 1).
All participants were registered with the South African Pharmacy Council as either pharmacists, post-basic pharmacist assistants or learner pharmacist assistants following basic training (90).
3.2 Pharmacy operational hours
All participating community pharmacies operated for a minimum of 8 hours during weekdays and maintained a minimum 5-hour operation on Saturdays.
Overall, 38 (29.7%) of the pharmacies surveyed remained closed on Sundays, while 26 (20.3%) pharmacies were not operational on public holidays.
3.3 Details of antibiotics dispensed among participating community pharmacies
Table 2 contains details of the consolidated estimated number of items dispensed per day among the different community pharmacy categories, the proportion (%) of antibiotics this represents and their nature. Overall, antibiotics represent an estimated 47.9% (95% CI: 47.2%-48.6%) of the medicines being dispensed per day among surveyed community pharmacies, greatest among chain pharmacies (48.9%; 95% CI: 47.6%-50.2%) and least among independent pharmacies (47.5%; 95% CI: 46.5%-48.5%).
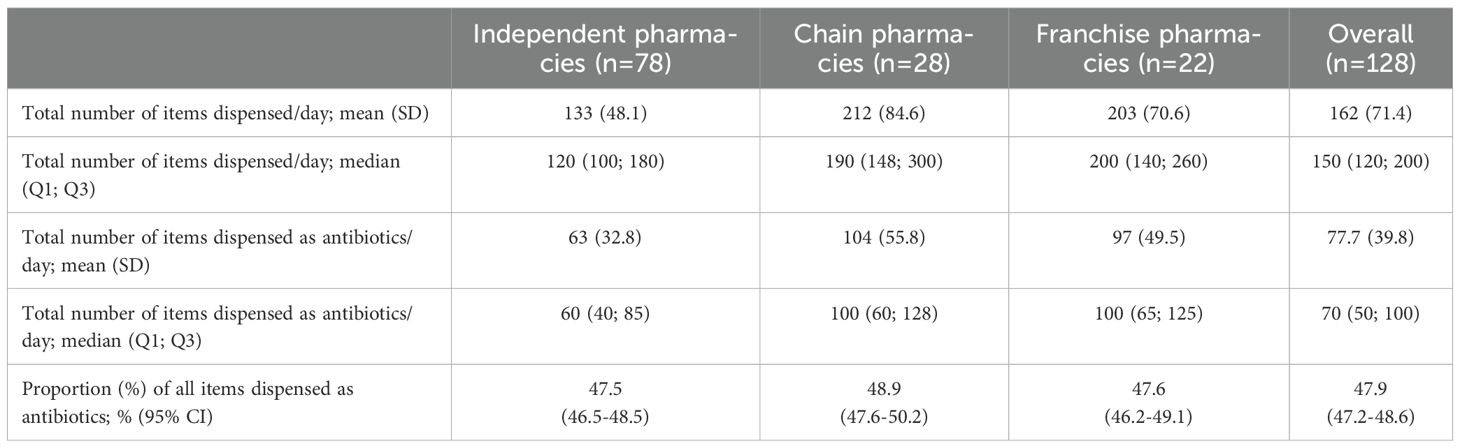
Table 2. Estimates of items (medicines including antibiotics) dispensed on a typical day among surveyed pharmacies considering the past week.
Overall, penicillins were the most frequently dispensed class of antibiotics, accounting for 41.1% of all antibiotics dispensed (Figure 1). Penicillins accounted for the highest proportion of antibiotics dispensed in chain pharmacies, comprising 45.7% of all antibiotics dispensed. The combined percentage of antibiotics dispensed as macrolides, fluoroquinolones and cephalosporins, which as mentioned, are typically from the WHO Watch group, represented 47.2% of the antibiotics dispensed, with the other antibiotics contributing the remainder (Figure 1). Other antibiotics classified under the WHO Access group contributed to the remaining percentage, though their specific breakdown is not detailed in this analysis. Future studies may further categorize the Access and Watch antibiotics to provide a more comprehensive overview.
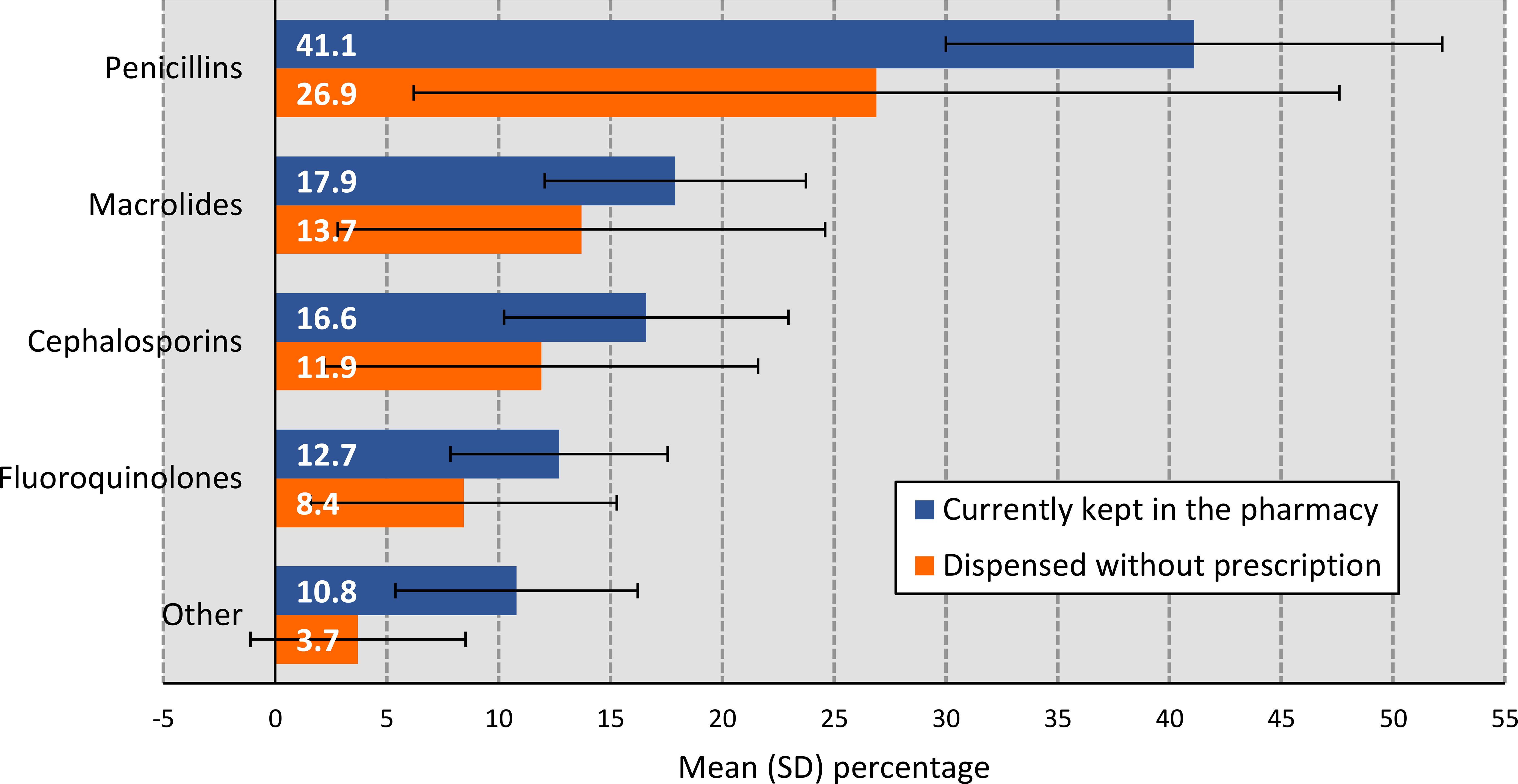
Figure 1. Estimated percentage of antibiotics kept in surveyed pharmacies and dispensed without a prescription distributed by ATC class. NB: Percentages may not necessarily add up to exactly 100% as they were calculated as an average % based on estimates from the participants.
Overall, antibiotics were dispensed most frequently for STIs (33.5%), followed by URTIs (25.8%), UTIs (12.6%), SSTIs (11.3%), LRTIs (8.8%) and pediatric diarrhea (8.4%). Figure 2 illustrates variations in the typical indications for which antibiotics are dispensed among the different pharmacy categories.
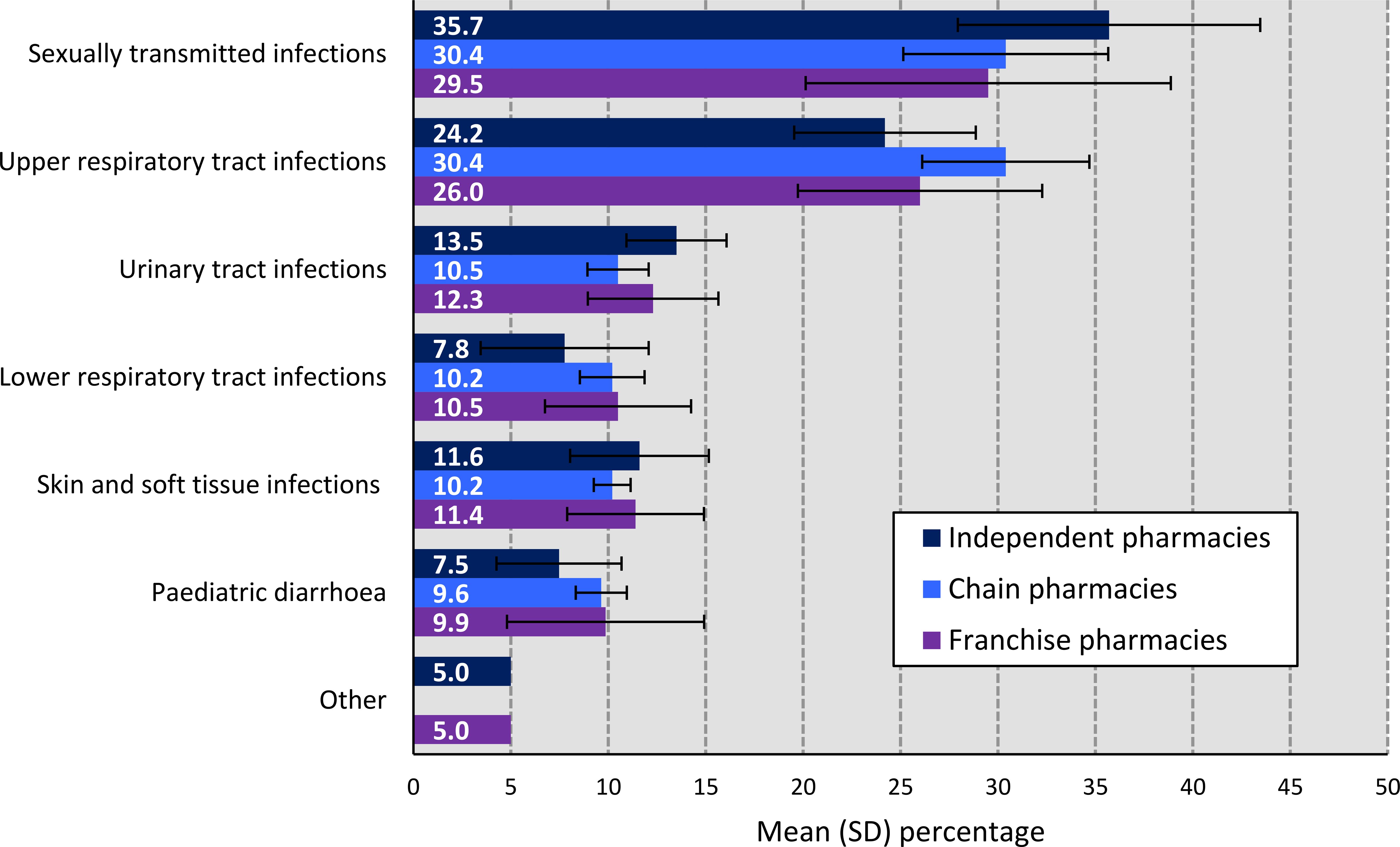
Figure 2. Estimated percentage of common infectious diseases for which antibiotics are dispensed in surveyed pharmacies, distributed by pharmacy category. NB: Percentages may not necessarily add up to exactly 100% as they were calculated as an average % based on estimates from the participants.
3.4 Antibiotics being dispensed without a prescription
When questioned about dispensing of antibiotics without a prescription, at least one respondent from 68.8% (88/128) of the pharmacies surveyed acknowledged that they had dispensed antibiotics without a prescription over the past 14 days. At an individual level, 56.9% (178/313) of respondents within the community pharmacies surveyed reported engaging in this practice over the past 14 days (Table 3). Overall, a slightly higher proportion of pharmacist assistants (57.5%) admitted to dispensing antibiotics without a prescription in the last 14 days compared with pharmacists (55.7%) (Table 3).
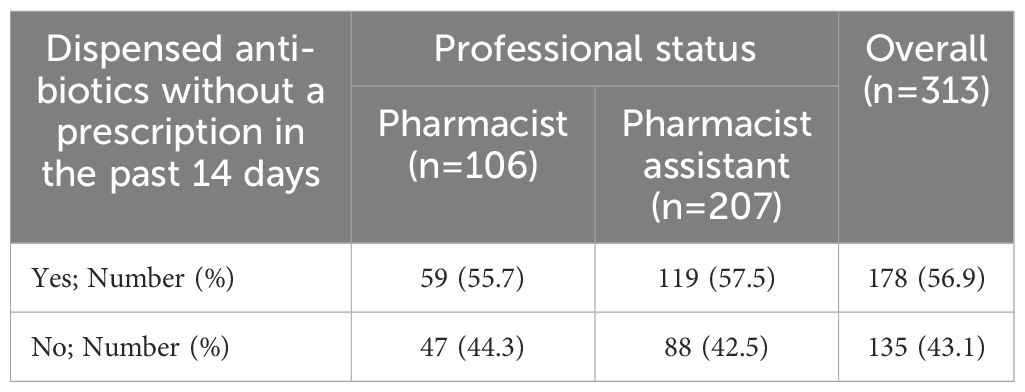
Table 3. Dispensing of antibiotics without a prescription in the last 14 days stratified by professional status among respondents from surveyed pharmacies.
However, when asked about dispensing of antibiotics in a typical day in the pharmacy, considering the past 3 days, the proportion of antibiotics dispensed without a prescription in the 88 pharmacies, accounted on average of only 8.6% of total antibiotic volumes dispensed, which was higher for adults than for children. This was principally among independent pharmacies where pharmacy personnel from 77 of the 78 (98.7%) community pharmacies surveyed admitted to this practice. Pharmacy personnel from only 9 of the franchise pharmacies and 2 of the chain pharmacies admitted to this practice. This suggests that although this behavior was relatively common among personnel and outlets, the volume of such dispensing appeared comparatively low. Consequently, according to respondents’ estimates, over 90% of antibiotics were dispensed with a prescription among the 88 pharmacies admitting to this practice.
Encouragingly, penicillins were the most dispensed antibiotics without a prescription when this occurred (Figure 1). However, an appreciable number (34.0%) of antibiotics principally from the antibiotic classes containing Watch antibiotics were also being dispensed without a prescription among the 88 pharmacies admitting to this practice. Overall, a greater proportion of antibiotics from the ATC classes including Watch antibiotics were dispensed with a prescription than without a prescription (Figure 1).
3.5 Dispensing approaches when patients consulted for treatment of self-limiting conditions
Among the community pharmacists (n=104), the majority indicated that they always (57.7%) or mostly (41.3%) offer symptomatic OTC medicines before dispensing antibiotics without a prescription to patients presenting with self-limiting infectious disease symptoms, including coughs, colds or influenza. Pharmacist assistants (n=203) responded similarly, indicating that they always (51.7%) or mostly (47.8%) follow this practice. In each of the respective groups, only one respondent (0.5%) indicated that they sometimes follow this practice.
Alongside this, 57.7% of pharmacists and 52.2% of pharmacist assistants indicated that they never suggest antibiotics for self-limiting infectious diseases, while 42.3% of pharmacists and 47.8% of pharmacist assistants admitted to sometimes suggesting antibiotics for self-limiting infectious diseases.
4 Discussion and suggested activities
We believe this is the most extensive study to date undertaken in a rural province of South Africa on the prevalence of antibiotics being dispensed, as estimated by pharmacy personnel, versus other medicines as well as the classes of antibiotics dispensed. In addition, estimate the extent to which antibiotics are being dispensed without a prescription given previous conflicting findings (37–40), the class of antibiotics being dispensed without a prescription and the indications.
The study identified that on average antibiotics were estimated to account for 47.9% of the medicines dispensed per day among community pharmacies in this rural South African province. This is consistent with high rates of infectious diseases across Africa coupled with antibiotic use in the community accounting for an appreciable proportion of total antibiotic use within LMICs (13, 42, 61, 91–93). However, lower than a recent study in Zimbabwe where antibiotics were being prescribed in 70.6% of patients in ambulatory care (94).
There are concerns though with the appropriateness of antibiotics being dispensed, which were principally being dispensed with a prescription, and with a relatively low prevalence overall of antibiotics being dispensed without a prescription. This included high rates of antibiotics being dispensed from classes containing Watch antibiotics, with antibiotics principally being dispensed for patients with respiratory tract infections. This is similar to other studies in South Africa as well as other African countries (43, 81, 82, 95). Future interventions and activities should include the instigation of ASPs, incorporating the potential instigation of quality indicators based on the AWaRe system and guidance, with these discussed further in the study of Chigome et al. (82) (43, 96, 97). This is important to attain the recent goals of the United Nations that at least 70% of antibiotic utilization across sectors should be from the Access group of antibiotics (98), especially given rising use of Watch antibiotics in South Africa in recent years (56).
The observed discrepancy between the proportion of pharmacy personnel or outlets acknowledging non-prescription antibiotic dispensing and the reported antibiotic volume dispensed without a prescription warrants consideration. While 69.3% of pharmacies and 56.9% of individual respondents reported engaging in this practice within the past 14 days, this accounted for only 8.6% of total antibiotics dispensed in the past 3 days among these outlets based on the feedback provided. This suggests that, although widespread, the behavior may occur infrequently at each site or in limited quantities. Apart from the difference in the period covered by the questions (past 14 days versus the past 3 days), social desirability bias or regulatory concerns may have influenced self-reported rates, potentially leading to an underestimation of the extent and volume of antibiotics being dispensed without a prescription in this rural province (99). Higher figures for self-purchasing were reported in the two recent pilot patient surveys in this rural province (78, 100), which have now been taken further, underscoring the value of triangulating data sources to more accurately capture antibiotic use patterns at the community level. Having said this, 98.1% of the community pharmacists surveyed, alongside 97.6% of pharmacist assistants surveyed, stated that they always or mostly offered symptomatic OTC medicines before dispensing antibiotics without a prescription to patients presenting with self-limiting infectious disease symptoms including coughs, colds or influenza. Alongside this, an appreciable number of community pharmacists and pharmacist assistants stated that they never suggested antibiotics for self-limiting infectious diseases when patients presented with these conditions.
Furthermore, the finding that 98% of respondents prioritized recommending OTC medicines does not necessarily contradict the observed antibiotic usage rate (47.9% of all medicines dispensed). OTC prioritization may reflect initial consultation approaches, but does not exclude subsequent decisions to dispense antibiotics especially with patient expectations, symptom severity or limited access to formal healthcare services influencing HCP and patient behavior. These insights underline the complex interplay between intent, professional judgment and community-level factors in driving antimicrobial dispensing behaviors (43, 45). The higher levels of purchasing of antibiotics without a prescription seen in the two pilot studies with patients exiting community pharmacies in this rural province could have been driven by pressure from patients combined with concerns with their knowledge regarding antibiotics and AMR (78, 100). These key issues will be explored further in ongoing research projects surveying patients exiting community pharmacies in this rural province.
Despite existing regulations prohibiting the dispensing of antibiotics without a prescription in South Africa, enforcement remains inconsistent, particularly in rural areas. Overall, any inappropriate dispensing of antibiotics without a prescription where antibiotics are not warranted needs to be addressed at various levels. This is particularly important in countries such as South Africa with multiple official languages, with some of these languages containing no direct words for terminology such as antibiotics and AMR (100). ASPs have been successfully undertaken across LMICs, including among African countries, to reduce inappropriate dispensing of antibiotics without a prescription (Table 4). Other suggested activities include improving electronic monitoring of antibiotic dispensing practices among community pharmacies through mobile telephone and other technologies (17, 43, 101). In addition, training programs for community pharmacists and pharmacist assistants on the AWaRe system and guidance, as well as AMR, during undergraduate training and post qualification (25, 27, 43). The recent instigation of an AMR Awareness Module by the Department of Health in South Africa should also help in this regard (102). Alongside this, the implementation of targeted public awareness campaigns, combined with collaboration with professional pharmacy associations to improve future activities (84, 103). The second phase of this multifaceted study involving ascertaining patients’ perspectives and attitudes on antibiotic use and AMR should provide further insights from a patient perspective assisting in this regard.
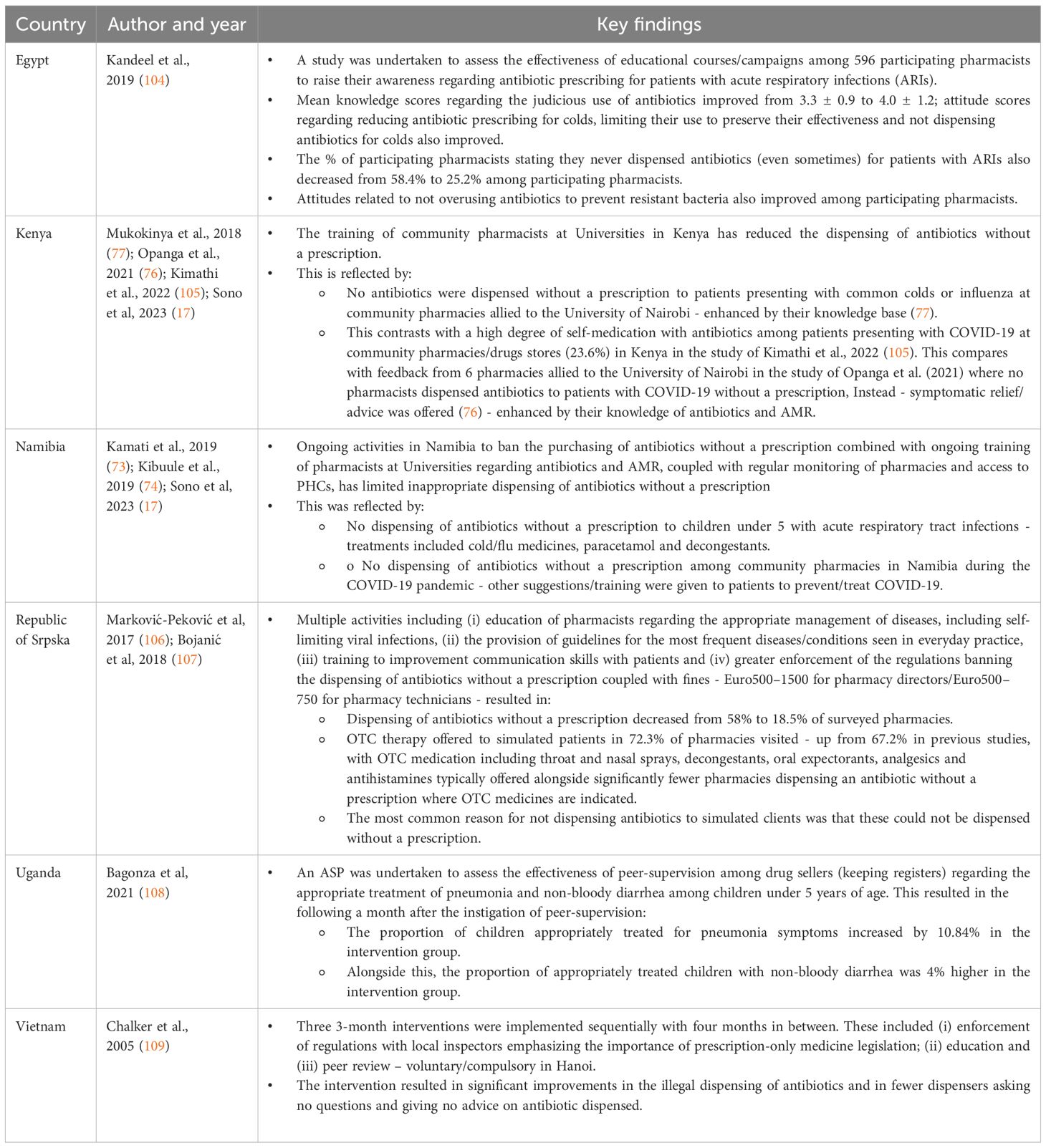
Table 4. ASPs and other activities among community pharmacies and drug stores across LMICs to improve dispensing of antibiotics.
We are aware though that the introduction of extensive penalties among community pharmacies for contravening the law have been successful in high-income countries (110). In addition, as seen, extensive fines for both pharmacy directors and personnel, combined with guidelines and education of pharmacists, appreciably reduced the dispensing of antibiotics without a prescription in the Republic of Srpska, which is a middle-income country (Table 4) (106, 107). This contrasts with the more limited impact when appreciably lower levels of fines were introduced for breaking the law in Vietnam when community pharmacists or their staff dispense antibiotics without a prescription (111). Consequently, careful consideration is needed before introducing fines.
Overall, the targeting of appropriate interventions including ASPs will depend on the current knowledge, attitudes and practices of community pharmacists and pharmacist assistants towards these key terms, as well as patients’ understanding if community pharmacists or assistants are not speaking to them in their first language. These key issues are being explored further in the second part of this project, alongside a separate project with assessing the knowledge and attitudes of patients towards antibiotics, AMR and AMS activities. The combined findings from community pharmacists and assistants, as well as patients, will be used to guide future activities among these key stakeholder groups. The findings from patients leaving community pharmacies in this rural province are also important to guide future activities as we are aware that there can be discrepancies between the rate of actual dispensing of antibiotics without a prescription and the extent stated by community pharmacists, who may downplay the situation (112). This was the case in the pilot studies with patients in this rural province, which is now being followed up (40, 78, 100). We are also aware that fining pharmacists for dispensing of antibiotics without a prescription in LMICs may be counterproductive in terms of pushing patients towards the informal sector among African countries if the reasons still remain as to why they approached community pharmacies in the first place with their infectious disease symptoms. In addition, we are aware that in South Africa in the public sector healthcare system that there are considerable concerns with excessive antibiotic prescribing, including Watch antibiotics (56, 81, 82). Consequently, a combined comprehensive approach is needed to address AMR in LMICs including South Africa (113). We will be exploring this further in future research projects.
We do acknowledge a number of limitations with this study. Firstly, not all community pharmacists and pharmacist assistants in this rural province participated in the study. However, 65.1% of approached community pharmacies participated. Consequently, we are confident that our findings can represent the province as a whole. Secondly, we were unable to verify the replies from the pharmacists or pharmacist assistants for their accuracy. This though is common for self-administered questionnaires. However, we did not question pharmacists or pharmacist assistants directly which may also have introduced additional response bias. Several measures though were implemented to reduce bias and improve data reliability. These included anonymous responses, with participants being assured of confidentiality, encouraging honest responses. The questionnaire was also carefully designed to avoid leading questions, ensuring responses reflected actual practices rather than perceived expectations. However, as mentioned, to supplement these findings, we have undertaken surveys with patients leaving community pharmacies in this rural province to further verify the robustness of some of the replies, alongside the knowledge and attitudes of patients towards antibiotics and AMR. Overall, we are confident of the findings and some of the implications going forward to improve antibiotic utilization in this rural province and throughout South Africa. These though will be explored further in additional research projects.
5 Conclusion
This study highlighted concerns regarding the prescribing and dispensing of antibiotics in this rural province in South Africa, especially Watch antibiotics. Concerns included the number of community pharmacies, especially independent pharmacies, where patients could purchase antibiotics without a prescription for self-limiting conditions, including before OTC medicines. As a result, confirming concerns raised during the pilot study. Multiple strategies involving pharmacists, pharmacist assistants as well as prescribers and patients are need to improve future antibiotic use in this province, and across South Africa. We will be exploring this further in future research projects.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Sefako Makgatho University Research Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
TM: Investigation, Data curation, Methodology, Writing – review & editing, Conceptualization, Validation, Formal analysis, Visualization, Writing – original draft. MM: Writing – review & editing, Validation, Investigation, Formal analysis, Methodology, Data curation. AG: Conceptualization, Validation, Formal analysis, Methodology, Data curation, Writing – review & editing. SC: Data curation, Validation, Methodology, Conceptualization, Formal analysis, Writing – review & editing. VM: Investigation, Methodology, Writing – review & editing, Validation, Formal analysis, Conceptualization, Data curation. NS: Data curation, Investigation, Conceptualization, Validation, Methodology, Writing – review & editing, Formal analysis. AC: Conceptualization, Validation, Writing – review & editing, Investigation, Methodology. AC: Conceptualization, Validation, Writing – review & editing, Methodology, Investigation, Formal analysis. BG: Methodology, Supervision, Investigation, Validation, Data curation, Conceptualization, Writing – review & editing, Writing – original draft, Formal analysis, Visualization. JM: Writing – review & editing, Formal analysis, Resources, Data curation, Visualization, Conceptualization, Methodology, Supervision, Investigation, Validation.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This study was supported by South African National Research Foundation (NRF) (Grant reference: MND210917640292UID; Grant reference: SRUG200509520910, Grant No: 129365).
Acknowledgments
We sincerely thank Veronica Mboweni and Ntwanano Eulander Sono for their assistance with the data collection for this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fitd.2025.1637362/full#supplementary-material
References
1. Naghavi M, Vollset SE, Ikuta KS, Swetschinski LR, Gray AP, Wool EE, et al. Global burden of bacterial antimicrobial resistance 1990-2021: a systematic analysis with forecasts to 2050. Lancet. (2024) 404:1199–226. doi: 10.1016/S0140-6736(24)01867-1
2. Murray CJ, Ikuta KS, Sharara F, Swetschinski L, Aguilar GR, Gray A, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. (2022) 399:629–55. doi: 10.1016/S0140-6736(21)02724-0
3. Cassini A, Högberg LD, Plachouras D, Quattrocchi A, Hoxha A, Simonsen GS, et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: a population-level modelling analysis. Lancet Infect Dis. (2019) 19:56–66. doi: 10.1016/S1473-3099(18)30605-4
4. Gautam A. Antimicrobial resistance: the next probable pandemic. JNMA. (2022) 60:225–8. doi: 10.31729/jnma.7174
5. Laxminarayan R. The overlooked pandemic of antimicrobial resistance. Lancet. (2022) 399:606–7. doi: 10.1016/S0140-6736(22)00087-3
6. Dadgostar P. Antimicrobial resistance: implications and costs. Infect Drug Resist. (2019) 12:3903–10. doi: 10.2147/IDR.S234610
7. World Bank and the World Health Organization. Sustaining action against antimicrobial resistance: A case series of country experiences(2022). Available online at: https://openknowledge.worldbank.org/server/api/core/bitstreams/624f5193-99c0-5a28-adfe-0191a8c40d04/content (Accessed May 3, 2025).
8. OECD. Stemming the superbug tide - just A few dollars more(2018). Available online at: https://www.oecd.org/en/publications/stemming-the-superbug-tide_9789264307599-en.html (Accessed May 4, 2025).
9. Lewnard JA, Charani E, Gleason A, Hsu LY, Khan WA, Karkey A, et al. Burden of bacterial antimicrobial resistance in low-income and middle-income countries avertible by existing interventions: an evidence review and modelling analysis. Lancet. (2024) 403:2439–54. doi: 10.1016/S0140-6736(24)00862-6
10. Antimicrobial Resistance Collaborators. The burden of bacterial antimicrobial resistance in the WHO African region in 2019: a cross-country systematic analysis. Lancet Glob Health. (2024) 12:e201–e16. doi: 10.1016/S2214-109X(23)00539-9
11. Totaro V, Guido G, Cotugno S, De Vita E, Asaduzzaman M, Patti G, et al. Antimicrobial resistance in Sub-Saharan Africa: A comprehensive landscape review. Am J Trop Med hygiene. (2025) 1–11:tpmd250035. doi: 10.4269/ajtmh.25-0035
12. Melaku T and Assegid L. Prescription in peril: the sociology of antibiotics and antimicrobial resistance in low resource settings. Discover Soc Sci Health. (2025) 5:71. doi: 10.1007/s44155-025-00225-1
13. Godman B, Egwuenu A, Haque M, Malande OO, Schellack N, Kumar S, et al. Strategies to improve antimicrobial utilization with a special focus on developing countries. Life. (2021) 11:528. doi: 10.3390/life11060528
14. Laxminarayan R, Impalli I, Rangarajan R, Cohn J, Ramjeet K, Trainor BW, et al. Expanding antibiotic, vaccine, and diagnostics development and access to tackle antimicrobial resistance. Lancet. (2024) 403:2534–50. doi: 10.1016/S0140-6736(24)00878-X
15. Atif M, Scahill S, Azeem M, Sarwar MR, and Babar Z-U-D. Drug utilization patterns in the global context: A systematic review. Health Policy Technol. (2017) 6:457–70. doi: 10.1016/j.hlpt.2017.11.001
16. Godman B, Haque M, McKimm J, Abu Bakar M, Sneddon J, Wale J, et al. Ongoing strategies to improve the management of upper respiratory tract infections and reduce inappropriate antibiotic use particularly among lower and middle-income countries: findings and implications for the future. Curr Med Res Opin. (2020) 36:301–27. doi: 10.1080/03007995.2019.1700947
17. Sono TM, Yeika E, Cook A, Kalungia A, Opanga SA, Acolatse JEE, et al. Current rates of purchasing of antibiotics without a prescription across sub-Saharan Africa; rationale and potential programmes to reduce inappropriate dispensing and resistance. Expert Rev Anti Infect Ther. (2023) 21:1025–55. doi: 10.1080/14787210.2023.2259106
18. Llor C and Bjerrum L. Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Ther Adv Drug Saf. (2014) 5:229–41. doi: 10.1177/2042098614554919
19. Torres NF, Chibi B, Kuupiel D, Solomon VP, Mashamba-Thompson TP, and Middleton LE. The use of non-prescribed antibiotics; prevalence estimates in low-and-middle-income countries. A systematic review and meta-analysis. Arch Public Health. (2021) 79:2. doi: 10.1186/s13690-020-00517-9
20. Auta A, Hadi MA, Oga E, Adewuyi EO, Abdu-Aguye SN, Adeloye D, et al. Global access to antibiotics without prescription in community pharmacies: A systematic review and meta-analysis. J Infect. (2019) 78:8–18. doi: 10.1016/j.jinf.2018.07.001
21. Sono TM, Markovic-Pekovic V, and Godman B. Effective programmes to reduce inappropriate dispensing of antibiotics in community pharmacies especially in developing countries. Adv Hum Biol. (2024) 14:1–4. doi: 10.4103/aihb.aihb_128_23
22. Yeika EV, Ingelbeen B, Kemah BL, Wirsiy FS, Fomengia JN, and van der Sande MAB. Comparative assessment of the prevalence, practices and factors associated with self-medication with antibiotics in Africa. Trop Med Int Health. (2021) 26:862–81. doi: 10.1111/tmi.13600
23. Gajdács M and Jamshed S. Editorial: Knowledge, attitude and practices of the public and healthcare-professionals towards sustainable use of antimicrobials: the intersection of pharmacology and social medicine. Front Antibiot. (2024) 3:1374463. doi: 10.3389/frabi.2024.1374463
24. WHO. Global action plan on antimicrobial resistance(2016). Available online at: https://www.who.int/publications/i/item/9789241509763 (Accessed May 3, 2025).
25. Sharland M, Zanichelli V, Ombajo LA, Bazira J, Cappello B, Chitatanga R, et al. The WHO essential medicines list AWaRe book: from a list to a quality improvement system. Clin Microbiol Infect. (2022) 28:1533–5. doi: 10.1016/j.cmi.2022.08.009
26. Zanichelli V, Sharland M, Cappello B, Moja L, Getahun H, Pessoa-Silva C, et al. The WHO AWaRe (Access, Watch, Reserve) antibiotic book and prevention of antimicrobial resistance. Bull World Health Organ. (2023) 101:290–6. doi: 10.2471/BLT.22.288614
27. Sharland M, Gandra S, Huttner B, Moja L, Pulcini C, Zeng M, et al. Encouraging AWaRe-ness and discouraging inappropriate antibiotic use-the new 2019 Essential Medicines List becomes a global antibiotic stewardship tool. Lancet Infect Dis. (2019) 19:1278–80. doi: 10.1016/S1473-3099(19)30532-8
28. Godman B, Egwuenu A, Wesangula E, Schellack N, Kalungia AC, Tiroyakgosi C, et al. Tackling antimicrobial resistance across sub-Saharan Africa: current challenges and implications for the future. Expert Opin Drug Safety. (2022) 21:1089–111. doi: 10.1080/14740338.2022.2106368
29. Sariola S, Butcher A, Cañada JA, Aïkpé M, and Compaore A. Closing the GAP in antimicrobial resistance policy in Benin and Burkina Faso. mSystems. (2022) 7:e0015022. doi: 10.1128/msystems.00150-22
30. Pallett SJ, Charani E, Hawkins L, Mazzella A, Anton-Vazquez V, Banerjee R, et al. National action plans for antimicrobial resistance and variations in surveillance data platforms. Bull World Health Organ. (2023) 101:501–12f. doi: 10.2471/BLT.22.289403
31. Mukoko J, Wesangula E, Gitonga N, Kusu N, Odhiambo C, Tanui E, et al. Kenya’s National Action Plan on antimicrobial resistance: measuring implementation progress. Front Trop Dis. (2025) 6. doi: 10.3389/fitd.2025.1540713
32. Harant A. Assessing transparency and accountability of national action plans on antimicrobial resistance in 15 African countries. Antimicrob Resist Infect Control. (2022) 11:15. doi: 10.1186/s13756-021-01040-4
33. Frumence G, Mboera LEG, Sindato C, Katale BZ, Kimera S, Metta E, et al. The governance and implementation of the national action plan on antimicrobial resistance in Tanzania: A qualitative study. Antibiotics. (2021) 10:273. doi: 10.3390/antibiotics10030273
34. Shabangu K, Essack SY, and Duma SE. Barriers to implementing National Action Plans on antimicrobial resistance using a One Health Approach: policymakers’ perspectives from South Africa and Eswatini. J Glob Antimicrob Resist. (2023) 33:130–6. doi: 10.1016/j.jgar.2023.02.007
35. Patel J, Harant A, Fernandes G, Mwamelo AJ, Hein W, Dekker D, et al. Measuring the global response to antimicrobial resistance, 2020-21: a systematic governance analysis of 114 countries. Lancet Infect Dis. (2023) 23:706–18. doi: 10.1016/S1473-3099(22)00796-4
36. Department of Health Republic of South Africa. South African antimicrobial resistance national strategy framework; A one health approach - 2017 – 2024 2017. Available online at: https://www.knowledgehub.org.za/system/files/elibdownloads/2020-03/AMR%20National%20Action%20Plan%202018%20-%202024.pdf (Accessed May 4, 2025).
37. Anstey Watkins J, Wagner F, Xavier Gómez-Olivé F, Wertheim H, Sankoh O, and Kinsman J. Rural South African community perceptions of antibiotic access and use: qualitative evidence from a health and demographic surveillance system site. Am J Trop Med Hyg. (2019) 100:1378–90. doi: 10.4269/ajtmh.18-0171
38. Do NTT, Vu HTL, Nguyen CTK, Punpuing S, Khan WA, Gyapong M, et al. Community-based antibiotic access and use in six low-income and middle-income countries: a mixed-method approach. Lancet Glob Health. (2021) 9:e610–e9. doi: 10.1016/S2214-109X(21)00024-3
39. Mokwele RN, Schellack N, Bronkhorst E, Brink AJ, Schweickerdt L, and Godman B. Using mystery shoppers to determine practices pertaining to antibiotic dispensing without a prescription among community pharmacies in South Africa—a pilot survey. JAC-Antimicrobial Resistance. (2022) 4. doi: 10.1093/jacamr/dlab196
40. Sono TM, Maluleke MT, Jelić AG, Campbell S, Marković-Peković V, Schellack N, et al. Potential strategies to limit inappropriate purchasing of antibiotics without a prescription in a rural province in South Africa: pilot study and the implications. Adv Hum Biol. (2024) 14:60–7. doi: 10.4103/aihb.aihb_127_23
41. WHO implementation handbook for national action plans on antimicrobial resistance: guidance for the human health sector(2022). Available online at: https://www.who.int/publications/i/item/9789240041981.
42. Duffy E, Ritchie S, Metcalfe S, Van Bakel B, and Thomas MG. Antibacterials dispensed in the community comprise 85%-95% of total human antibacterial consumption. J Clin Pharm Ther. (2018) 43:59–64. doi: 10.1111/jcpt.12610
43. Saleem Z, Moore CE, Kalungia AC, Schellack N, Ogunleye O, Chigome A, et al. Status and implications of the knowledge, attitudes and practices towards AWaRe antibiotic use, resistance and stewardship among low- and middle-income countries. JAC-Antimicrobial Resistance. (2025) 7. doi: 10.1093/jacamr/dlaf033
44. Saleem Z, Hassali MA, Godman B, Fatima M, Ahmad Z, Sajid A, et al. Sale of WHO AWaRe groups antibiotics without a prescription in Pakistan: a simulated client study. J Pharm Policy Pract. (2020) 13:26. doi: 10.1186/s40545-020-00233-3
45. Saleem Z, Mekonnen BA, Orubu ES, Islam MA, Nguyen TTP, Ubaka CM, et al. Current access, availability and use of antibiotics in primary care among key low- and middle-income countries and the policy implications. Expert Rev Anti Infect Ther. (2025), 1–42. doi: 10.1080/14787210.2025.2477198
46. Asrade Mekonnen B, Getie Yizengaw M, and Chanie Worku M. Prevalence of substandard, falsified, unlicensed and unregistered medicine and its associated factors in Africa: a systematic review. J Pharm Policy Pract. (2024) 17:2375267. doi: 10.1080/20523211.2024.2375267
47. Abdullah S, Zikria S, Brian G, Khurshid HF, Abdul H, A. ALRMB, et al. Surge of branded generics and antimicrobial resistance: analyzing the antibiotic market dynamics in Pakistan through the WHO essential medicines and AWaRe lens. Expert Rev Anti-infective Ther. (2025) 23:513–21. doi: 10.1080/14787210.2025.2511958
48. Mendelson M, Brink A, Gouws J, Mbelle N, Naidoo V, Pople T, et al. The One Health stewardship of colistin as an antibiotic of last resort for human health in South Africa. Lancet Infect Dis. (2018) 18:e288–e94. doi: 10.1016/S1473-3099(18)30119-1
49. Department of Health Republic of South Africa. Surveillance for antimicrobial resistance(2020). Available online at: https://www.knowledgehub.org.za/system/files/elibdownloads/2020-03/Guide%20to%20access%20the%20National%20AMR%20Surveillance%20Dashboard.pdf (Accessed May 4, 2025).
50. Departments of Health and Agriculture. Forestry and fisheries for the republic of South Africa: antimicrobial resistance national strategy framework 2017 – 2024. Available online at: https://www.knowledgehub.org.za/system/files/elibdownloads/2020-03/AMR%20National%20Action%20Plan%202018%20-%202024.pdf (Accessed May 10, 2025).
51. Engler D, Meyer JC, Schellack N, Kurdi A, and Godman B. Compliance with South Africa’s Antimicrobial Resistance National Strategy Framework: are we there yet? J Chemother. (2021) 33:21–31. doi: 10.1080/1120009X.2020.1789389
52. Department of Health Republic of South Africa. Practical manual for implementation of the national infection prevention and control strategic framework(2020). Available online at: https://www.knowledgehub.org.za/system/files/elibdownloads/2020-04/Practical%20Manual%20for%20implementation%20of%20the%20National%20IPC%20Strategic%20Framework%20March%202020.pdf (Accessed May 3, 2025).
53. Engler D, Meyer JC, Schellack N, Kurdi A, and Godman B. Antimicrobial stewardship activities in public healthcare facilities in South Africa: A baseline for future direction. Antibiotics (Basel). (2021) 10:996. doi: 10.3390/antibiotics10080996
54. Department of Health Republic of South Africa. Become an antibiotic guardian(2022). Available online at: https://antibioticguardian.com/south-africa/ (Accessed May 4, 2025).
55. Finlayson H, Chibabhai V, Jeena P, Kolman S, Lowman W, Manzini TC, et al. The changing landscape of antimicrobial resistance and use in South Africa: The need for access to new antibiotics: A position paper. S Afr Med J. (2024) 114:e2348. doi: 10.7196/SAMJ.2024.v114i10.2348
56. Department of Health, Republic of South Africa. Surveillance for antimicrobial resistance and consumption of antibiotics in South Africa 2018-2022(2024). Available online at: https://www.nicd.ac.za/wp-content/uploads/2024/04/South-African-AMR-Surveillance-Report-2022.pdf (Accessed May 5, 2025).
57. Sulis G, Sayood S, Katukoori S, Bollam N, George I, Yaeger LH, et al. Exposure to World Health Organization’s AWaRe antibiotics and isolation of multidrug resistant bacteria: a systematic review and meta-analysis. Clin Microbiol Infect. (2022) 28:1193–202. doi: 10.1016/j.cmi.2022.03.014
58. Li J, Zhou P, Wang J, Li H, Xu H, Meng Y, et al. Worldwide dispensing of non-prescription antibiotics in community pharmacies and associated factors: a mixed-methods systematic review. Lancet Infect Dis. (2023) 23:e361–e70. doi: 10.1016/S1473-3099(23)00130-5
59. Wang T, Wu J, Li J, Zhou P, Li Q, Xu X, et al. Is self-medication with antibiotics among the public a global concern: a mixed-methods systematic review. Expert Rev Anti-infective Ther. (2024) 22:1199–208. doi: 10.1080/14787210.2024.2419607
60. Baldeh AO, Millard C, Pollock AM, and Brhlikova P. Bridging the gap? Local production of medicines on the national essential medicine lists of Kenya, Tanzania and Uganda. J Pharm Policy Pract. (2023) 16:18. doi: 10.1186/s40545-022-00497-x
61. Ogaji DS, Nwaejike D, and Ebiekuraju O. Quality of drug prescribing and dispensing practices in primary healthcare centres in an urban local government area in Nigeria. West Afr J Med. (2023) 40:925–34.
62. Kotwani A, Joshi J, Lamkang AS, Sharma A, and Kaloni D. Knowledge and behavior of consumers towards the non-prescription purchase of antibiotics: An insight from a qualitative study from New Delhi, India. Pharm Pract. (2021) 19:2206. doi: 10.18549/PharmPract.2021.1.2206
63. Torres NF, Solomon VP, and Middleton LE. Pharmacists’ practices for non-prescribed antibiotic dispensing in Mozambique. Pharm Pract. (2020) 18:1965. doi: 10.18549/PharmPract.2020.3.1965
64. Nepal G and Bhatta S. Self-medication with antibiotics in WHO Southeast Asian region: A systematic review. Cureus. (2018) 10:e2428. doi: 10.7759/cureus.2428
65. Simon B and Kazaura M. Prevalence and factors associated with parents self-medicating under-fives with antibiotics in Bagamoyo district council, Tanzania: a cross-sectional study. Patient Prefer Adherence. (2020) 14:1445–53. doi: 10.2147/PPA.S263517
66. Loosli K, Davis A, Muwonge A, and Lembo T. Addressing antimicrobial resistance by improving access and quality of care-A review of the literature from East Africa. PloS Negl Trop Dis. (2021) 15:e0009529. doi: 10.1371/journal.pntd.0009529
67. Waseem H, Ali J, Sarwar F, Khan A, Rehman HSU, Choudri M, et al. Assessment of knowledge and attitude trends towards antimicrobial resistance (AMR) among the community members, pharmacists/pharmacy owners and physicians in district Sialkot, Pakistan. Antimicrob Resist Infect Control. (2019) 8:67. doi: 10.1186/s13756-019-0517-3
68. Kumar KS, Saranya S, and Rani NV. Community pharmacists’ Knowledge, attitude, and nonprescription dispensing practices of antibiotics: an explorative study in a selected city of south India. J Res Pharm Pract. (2022) 11:51–8. doi: 10.4103/jrpp.jrpp_48_21
69. Kalungia AC, Burger J, Godman B, Costa JO, and Simuwelu C. Non-prescription sale and dispensing of antibiotics in community pharmacies in Zambia. Expert Rev Anti Infect Ther. (2016) 14:1215–23. doi: 10.1080/14787210.2016.1227702
70. Torres NF, Solomon VP, and Middleton LE. Identifying the commonly used antibiotics for self-medication in urban Mozambique: a qualitative study. BMJ Open. (2020) 10:e041323. doi: 10.1136/bmjopen-2020-041323
71. Ndaki PM, Mushi MF, Mwanga JR, Konje ET, Mugassa S, Manyiri MW, et al. Non-prescribed antibiotic dispensing practices for symptoms of urinary tract infection in community pharmacies and accredited drug dispensing outlets in Tanzania: a simulated clients approach. BMC Prim Care. (2022) 23:287. doi: 10.1186/s12875-022-01905-6
72. BOMRA. Licensing and enforcement(2024). Available online at: https://www.bomra.co.bw/licensing-and-enforcement/ (Accessed May 8, 2025).
73. Kamati M, Godman B, and Kibuule D. Prevalence of self-medication for acute respiratory infections in young children in Namibia: findings and implications. J Res Pharm Pract. (2019) 8:220–4. doi: 10.4103/jrpp.JRPP_19_121
74. Kibuule D, Nambahu L, Sefah IA, Kurdi A, Phuong TNT, Kwon H-Y, et al. Activities in Namibia to limit the prevalence and mortality from COVID-19 including community pharmacy activities and the implications. Sch Acad J Pharm. (2021) 5:82–92. doi: 10.36347/sajp.2021.v10i05.001
75. Pereko DD, Lubbe MS, and Essack SY. Public knowledge, attitudes and behaviour towards antibiotic usage in Windhoek, Namibia. South Afr J Infect Diseases. (2015) 30:134–7. doi: 10.1080/23120053.2015.1107290
76. Opanga S, Rizvi N, Wamaitha A, Abebrese Sefah I, and Godman BB. Availability of medicines in community pharmacy to manage patients with COVID-19 in Kenya; pilot study and implications. Sch Acad J Pharm. (2021) 3:36–42. doi: 10.36347/sajp.2021.v10i03.001
77. Mukokinya MMA, Opanga S, Oluka M, and Godman B. Dispensing of antimicrobials in Kenya: A cross-sectional pilot study and its implications. J Res Pharm Pract. (2018) 7:77–82. doi: 10.4103/jrpp.JRPP_17_88
78. Sono TM, Maluleke MT, Ramdas N, Jelic AG, Campbell S, Markovic-Pekovic V, et al. Pilot study to evaluate the feasibility of a patient questionnaire for the purpose of investigating the extent of purchasing antibiotics without a prescription in a rural province in South Africa: rationale and implications. Adv Hum Biol. (2024) 14:138–47. doi: 10.4103/aihb.aihb_140_23
79. Farley E, Stewart A, Davies MA, Govind M, Van den Bergh D, and Boyles TH. Antibiotic use and resistance: Knowledge, attitudes and perceptions among primary care prescribers in South Africa. S Afr Med J. (2018) 108:763–71. doi: 10.7196/SAMJ.2018.v108i9.12933
80. Gasson J, Blockman M, and Willems B. Antibiotic prescribing practice and adherence to guidelines in primary care in the Cape Town Metro District, South Africa. S Afr Med J. (2018) 108:304–10. doi: 10.7196/SAMJ.2018.v108i4.12564
81. Chigome A, Ramdas N, Skosana P, Cook A, Schellack N, Campbell S, et al. A narrative review of antibiotic prescribing practices in primary care settings in South Africa and potential ways forward to reduce antimicrobial resistance. Antibiotics. (2023) 12:1540. doi: 10.3390/antibiotics12101540
82. Chigome MA, Vambe MS, Kganyago MK, Meyer PJ, Campbell PS, Godman PB, et al. Point prevalence surveys of acute infection presentation and antibiotic prescribing in selected primary healthcare facilities in North-West and Gauteng provinces of South Africa. Int J Infect Diseases. (2025) 152:107689. doi: 10.1016/j.ijid.2024.107689
83. Ramdas N, Meyer JC, Schellack N, Godman B, Turawa EB, and Campbell SM. Knowledge, attitudes, motivations and expectations regarding antimicrobial use among community members seeking care at the primary healthcare level: a scoping review protocol. BMJ Open. (2025) 15:e088769. doi: 10.1136/bmjopen-2024-088769
84. Ramdas N, Meyer JC, Schellack N, Godman B, Turawa E, and Campbell SM. Knowledge, attitudes, motivations, expectations, and systemic factors regarding antimicrobial use amongst community members seeking care at the primary healthcare level: A scoping review. Antibiotics. (2025) 14:78. doi: 10.3390/antibiotics14010078
85. Khan FU, Khan FU, Hayat K, Chang J, Saeed A, Khan Z, et al. Knowledge, attitude and practices among consumers toward antibiotics use and antibiotic resistance in Swat, Khyber-Pakhtunkhwa, Pakistan. Expert Rev Anti Infect Ther. (2020) 18:937–46. doi: 10.1080/14787210.2020.1769477
86. Mitchell J, Cooke P, Ahorlu C, Arjyal A, Baral S, Carter L, et al. Community engagement: The key to tackling Antimicrobial Resistance (AMR) across a One Health context? Glob Public Health. (2022) 17:2647–64. doi: 10.1080/17441692.2021.2003839
87. Lubanga AF, Bwanali AN, Kambiri F, Harawa G, Mudenda S, Mpinganjira SL, et al. Tackling antimicrobial resistance in sub-Saharan Africa: challenges and opportunities for implementing the new people-centered WHO guidelines. Expert Rev Anti Infect Ther. (2024) 22:379–86. doi: 10.1080/14787210.2024.2362270
88. WHO. ATC/DDD toolkit - introduction to DDD indicators. Available online at: https://www.who.int/tools/atc-ddd-toolkit/indicators (Accessed May 3, 2025).
89. Sharland M, Pulcini C, Harbarth S, Zeng M, Gandra S, Mathur S, et al. Classifying antibiotics in the WHO Essential Medicines List for optimal use-be AWaRe. Lancet Infect Dis. (2018) 18:18–20. doi: 10.1016/S1473-3099(17)30724-7
90. Dakarai K. Top 3 pharmacy assistant courses in South Africa(2024). Available online at: https://coursesouthafrica.co.za/pharmacy-assistant-courses-in-south-africa/ (Accessed May 10, 2025).
91. Kakumba JM, Kindenge JM, Kapepula PM, Iyamba JL, Mashi ML, Mulwahali JW, et al. Evaluation of antibiotic prescribing pattern using WHO access, watch and reserve classification in Kinshasa, Democratic Republic of Congo. Antibiotics. (2023) 12:1239. doi: 10.3390/antibiotics12081239
92. Abebe RB, Ayal BM, Alemu MA, and Zeleke TK. Antibiotic appropriateness at outpatient settings in Ethiopia: the need for an antibiotic stewardship programme. Drugs Context. (2024) 13:2023-12-2. doi: 10.7573/dic.2023-12-2
93. Igirikwayo ZK, Migisha R, Mukaga H, and Kabakyenga J. Prescription patterns of antibiotics and associated factors among outpatients diagnosed with respiratory tract infections in Jinja city, Uganda, June 2022-May 2023. BMC Pulm Med. (2024) 24:446. doi: 10.1186/s12890-024-03246-9
94. Olaru ID, Chingono RMS, Mhino F, Gregson C, Bottomley C, Bandason T, et al. Infectious diseases burden and antibiotic prescribing patterns among primary care patients in Harare, Zimbabwe - a cross-sectional analysis. PloS Glob Public Health. (2025) 5:e0004442. doi: 10.1371/journal.pgph.0004442
95. Maksane N, Langfeld K, Bhaskar JP, Sadhu S, and van Hasselt J. Attitudes and practices for antibiotic prescription and antimicrobial resistance among general physicians -Findings from a multi-country survey. PloS Glob Public Health. (2025) 5:e0004558. doi: 10.1371/journal.pgph.0004558
96. Funiciello E, Lorenzetti G, Cook A, Goelen J, Moore CE, Campbell SM, et al. Identifying AWaRe indicators for appropriate antibiotic use: a narrative review. J Antimicrob Chemother. (2024) 79:3063–77. doi: 10.1093/jac/dkae370
97. Chigome A, Ramdas N, Campbell S, Gajdacs M, Sefah IA, Hango E, et al. Potential activities to improve primary care prescribing of antibiotics across Africa. Front Trop Dis. Available online at: https://reviewfrontiersinorg/review/1634182/16/14310/tab/History.
98. United Nations. Political declaration of the high-level meeting on antimicrobial resistance(2024). Available online at: https://www.un.org/pga/wp-content/uploads/sites/108/2024/09/FINAL-Text-AMR-to-PGA.pdf (Accessed May 3, 2025).
99. Edessa D, Sisay M, Hagos B, and Amare F. Antimicrobial use and management of childhood diarrhea at community drug retail outlets in eastern Ethiopia: A matched questionnaire-based and simulated patient-case study. Pediatr Health Med Ther. (2022) 13:63–79. doi: 10.2147/PHMT.S348204
100. Sono TM, Mboweni V, Jelić AG, Campbell SM, Marković-Peković V, Ramdas N, et al. Pilot study to evaluate patients’ Understanding of key terms and aspects of antimicrobial use in a rural province in South Africa findings and implications. Adv Hum Biol. (2025) 15:108–12. doi: 10.4103/aihb.aihb_119_24
101. Kalungia A and Godman B. Implications of non-prescription antibiotic sales in China. Lancet Infect Dis. (2019) 19:1272–3. doi: 10.1016/S1473-3099(19)30408-6
102. Department of Health Republic of South Africa. Antimicrobial resistance (AMR) awareness module(2024). Available online at: https://knowledgehub.health.gov.za/course/antimicrobial-resistance-amr-awareness-module (Accessed May 10, 2025).
103. Ramdas N, Biyela T, Thema M, Sibanda M, Sono TM, Campbell SM, et al. Patient knowledge, attitudes and behaviors related to antimicrobial use in South African primary healthcare settings: development and testing of the CAMUS and its implications. Front Trop Dis. (2025) 6. doi: 10.3389/fitd.2025.1569076
104. Kandeel A, Palms DL, Afifi S, Kandeel Y, Etman A, Hicks LA, et al. An educational intervention to promote appropriate antibiotic use for acute respiratory infections in a district in Egypt- pilot study. BMC Public Health. (2019) 19:498. doi: 10.1186/s12889-019-6779-0
105. Kimathi G, Kiarie J, Njarambah L, Onditi J, and Ojakaa D. A cross-sectional study of antimicrobial use among self-medicating COVID-19 cases in Nyeri County, Kenya. Antimicrob Resist Infect Control. (2022) 11:111. doi: 10.1186/s13756-022-01150-7
106. Marković-Peković V, Grubiša N, Burger J, Bojanić L, and Godman B. Initiatives to reduce nonprescription sales and dispensing of antibiotics: findings and implications. J Res Pharm Pract. (2017) 6:120–5. doi: 10.4103/jrpp.JRPP_17_12
107. Bojanić L, Marković-Peković V, Škrbić R, Stojaković N, Ðermanović M, Bojanić J, et al. Recent initiatives in the republic of Srpska to enhance appropriate use of antibiotics in ambulatory care; their influence and implications. Front Pharmacol. (2018) 9:442. doi: 10.3389/fphar.2018.00442
108. Bagonza A, Kitutu FE, Peterson S, Mårtensson A, Mutto M, Awor P, et al. Effectiveness of peer-supervision on pediatric fever illness treatment among registered private drug sellers in East-Central Uganda: An interrupted time series analysis. Health Sci Rep. (2021) 4:e284. doi: 10.1002/hsr2.284
109. Chalker J, Ratanawijitrasin S, Chuc NT, Petzold M, and Tomson G. Effectiveness of a multi-component intervention on dispensing practices at private pharmacies in Vietnam and Thailand–a randomized controlled trial. Soc Sci Med. (2005) 60:131–41. doi: 10.1016/j.socscimed.2004.04.019
110. Alrasheedy AA, Alsalloum MA, Almuqbil FA, Almuzaini MA, Aba Alkhayl BS, Albishri AS, et al. The impact of law enforcement on dispensing antibiotics without prescription: a multi-methods study from Saudi Arabia. Expert Rev Anti Infect Ther. (2020) 18:87–97. doi: 10.1080/14787210.2020.1705156
111. Nguyen TTP, Do TX, Nguyen HA, Nguyen CTT, Meyer JC, Godman B, et al. A national survey of dispensing practice and customer knowledge on antibiotic use in Vietnam and the implications. Antibiotics. (2022) 11:1091. doi: 10.3390/antibiotics11081091
112. Edessa D, Assefa N, Dessie Y, Asefa F, Dinsa G, and Oljira L. Non-prescribed antibiotic use for children at community levels in low- and middle-income countries: a systematic review and meta-analysis. J Pharm Policy Pract. (2022) 15:57. doi: 10.1186/s40545-022-00454-8
Keywords: community pharmacists, antibiotic prescribing, prevalence, self-purchasing antibiotics, indications, antimicrobial resistance, antimicrobial stewardship, South Africa
Citation: Maluleke TM, Maluleke MT, Jelic AG, Campbell SM, Marković-Peković V, Schellack N, Chigome A, Cook A, Godman B and Meyer JC (2025) Estimated extent of purchasing of antibiotics without a prescription from community pharmacies in a rural province in South Africa and the implications. Front. Trop. Dis. 6:1637362. doi: 10.3389/fitd.2025.1637362
Received: 29 May 2025; Accepted: 18 July 2025;
Published: 28 August 2025.
Edited by:
Sylvia Opanga, University of Nairobi, KenyaReviewed by:
Feng Zhou, Henan Institute of Science and Technology, ChinaGayathri Govindaraju, Rutgers, The State University of New Jersey, United States
Copyright © 2025 Maluleke, Maluleke, Jelic, Campbell, Marković-Peković, Schellack, Chigome, Cook, Godman and Meyer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Brian Godman, QnJpYW4uR29kbWFuQHN0cmF0aC5hYy51aw==
†ORCID: Tiyani Milta Maluleke, orcid.org/0000-0001-6437-7198
Ana Golić Jelić, orcid.org/0000-0001-6883-4739
Stephen Campbell, orcid.org/0000-0002-2328-4136
Vanda Marković-Peković, orcid.org/0000-0001-8963-5720
Natalie Schellack, orcid.org/0000-0001-9690-6285
Brian Godman, orcid.org/0000-0001-6539-6972
Johanna C. Meyer, orcid.org/0000-0003-0462-5713
Aislinn Cook, orcid.org/0000-0002-9189-7815
 Tiyani Milta Maluleke1,2†
Tiyani Milta Maluleke1,2† Ana Golić Jelic
Ana Golić Jelic Vanda Marković-Peković
Vanda Marković-Peković Natalie Schellack
Natalie Schellack Brian Godman
Brian Godman Johanna C. Meyer
Johanna C. Meyer