- 1Division of Urology, Taichung Tzu Chi General Hospital, The Buddhist Tzu Chi Medical Foundation, Taichung, Taiwan
- 2School of Post-Baccalaureate Chinese Medicine, Tzu Chi University, Hualien, Taiwan
- 3Graduate Institute of Chinese Medicine, China Medical University, Taichung, Taiwan
- 4Section of Infectious Disease, Hsinchu Mackay Memorial Hospital, Hsinchu, Taiwan
- 5Department of Microbiology and Immunology, Chung-Shan Medical University, Taichung, Taiwan
- 6School of Chinese Medicine, China Medical University, Taichung, Taiwan
In Klebsiella pneumoniae, we have previously shown that IscR, an Fe–S cluster-containing transcriptional factor, plays a dual role in controlling capsular polysaccharide biosynthesis and iron-acquisition systems by switching between its holo and apo forms. In this study, the effect of IscR on type 3 fimbriae expression and biofilm formation was investigated. We found that production of the major subunit of type 3 fimbriae, MrkA, was increased in the ΔiscR and iscR3CA strains, a strain expressing a mutant IscR that mimics apo-IscR, at both the translational and transcriptional levels. Based on the fact that type 3 fimbriae expression is the major factor affecting biofilm formation, increased biofilm formation was also found in ΔiscR or iscR3CA, suggesting that holo-IscR represses biofilm formation. However, the repression of type 3 fimbriae expression by IscR is indirect. To further understand the regulatory mechanism of IscR, the effect of IscR on the expression of mrkHIJ, which encodes cyclic di-GMP (c-di-GMP)-related regulatory proteins that control type 3 fimbriae expression, was studied. We found that holo-IscR could directly repress mrkHI transcription, indicating that MrkHI is required for IscR regulation of type 3 fimbriae expression. Finally, deletion of iscR attenuated K. pneumoniae virulence in a peritonitis model of mouse infection, while the absence of the [2Fe–2S] cluster of IscR had no effect on K. pneumoniae virulence during infection. Taken together, our results demonstrate the underlying mechanism of the [2Fe–2S] cluster of IscR in controlling type 3 fimbriae expression and its effect on K. pneumoniae pathogenesis.
Introduction
Iron is essential to most bacteria for growth and reproduction. It plays a key role as a cofactor in the electron transport chain and for various enzymes in the tricarboxylic acid (TCA) cycle and oxygen metabolism (Neilands, 1981). While limited iron concentrations abolish bacterial growth, high intracellular iron concentrations may damage bacteria owing to the formation of undesired reactive oxygen species (ROS) (Touati, 2000; Andrews et al., 2003). In addition, bacteria must alter the expression of various virulence genes to adapt to iron availability during infection, such as those involved in siderophore production, fimbriae expression, and biofilm formation (Lin et al., 2010; Rohmer et al., 2011; Wu et al., 2012; Porcheron and Dozois, 2015). Therefore, it is important for bacteria to develop a tight regulatory circuit in response to iron availability in order to perform infection processes successfully.
Klebsiella pneumoniae is a gram-negative facultative anaerobe that causes community-acquired diseases including pneumonia, bacteremia, septicemia, and urinary and respiratory tract infections in patients with underlying diseases (Podschun and Ullmann, 1998). In addition, hypervirulent K. pneumoniae is also a major pathogen for pyogenic liver abscesses in diabetic patients (Han, 1995; Lau et al., 2000; Yang et al., 2009). Heavy capsular polysaccharide (CPS) is a characteristic of isolates causing pyogenic liver abscesses, protecting the bacteria from serum killing (Sahly et al., 2000; Lin et al., 2004). Apart from CPS, fimbriae are considered another crucial virulence factor in K. pneumoniae pathogenesis (Livrelli et al., 1996). Type 3 fimbriae, which are encoded by the mrkABCDF operon, are often expressed in heavily encapsulated K. pneumoniae isolates and play an important role in biofilm formation (Di Martino et al., 2003; Jagnow and Clegg, 2003; Wu et al., 2012). Biofilm formation is considered to be a key factor in the development of nosocomial infections, increasing bacterial tolerance to antibiotics, which causes problems during medical treatment (Murphy and Clegg, 2012). Therefore, a majority of K. pneumoniae isolates from catheter-associated urinary tract or hospital-acquired respiratory tract infections can produce functional type 3 fimbriae (Ong et al., 2010). Furthermore, the ability of K. pneumoniae colonization and subsequent persistence in mice was reduced when the type 3 fimbriae expression was abolished (Murphy et al., 2013). In addition, immunization of mice with purified type 3 fimbriae confers protection against following challenge with virulent K. pneumoniae (Lavender et al., 2005; Wang et al., 2016). Even though these findings indicate the significance of type 3 fimbriae to the virulence of K. pneumoniae, the regulation of the type 3 fimbrial gene expression in K. pneumoniae still remains largely unknown (Murphy and Clegg, 2012).
In bacteria, c-di-GMP is a bacterial second messenger that modulates biofilm formation and controls expression of the virulence genes (Tamayo et al., 2007). In K. pneumoniae, several studies revealed that a gene cluster adjacent to the type 3 fimbriae, mrkHIJ, was involved in the modulation and sensing of cyclic di-GMP (c-di-GMP) and also regulated the type 3 fimbriae expression (Wilksch et al., 2011; Murphy and Clegg, 2012; Wu et al., 2012; Yang et al., 2013). MrkH is a PilZ-domain protein that is able to bind to c-di-GMP and is a central positive regulator in type 3 fimbriae expression (Wilksch et al., 2011; Yang et al., 2013). MrkI is a LuxR-type transcriptional regulator that activates type 3 fimbriae expression (Wu et al., 2012). MrkJ possesses an EAL domain that allows it to serve as a functional c-di-GMP phosphodiesterase (PDE) for hydrolysis of c-di-GMP to further repress type 3 fimbriae expression and biofilm formation (Johnson and Clegg, 2010). Similarly, YfiN and YjcC are also c-di-GMP PDE proteins and play a negative role in control of type 3 fimbriae expression in K. pneumoniae (Wilksch et al., 2011; Huang et al., 2013). In addition to c-di-GMP-related proteins, several transcriptional regulators have reported to be involved in control of type 3 fimbriae expression in K. pneumoniae, such as histone-like nucleoid-structuring protein (H-NS), CRP, and ferric uptake regulator (Fur) (Wu et al., 2012; Ares et al., 2016; Lin et al., 2016). Thus, the regulation of type 3 fimbriae in K. pneumoniae in response to different environmental stimulus is more complicated than previously expected.
During the infection, iron availability is an important environmental signal affecting bacterial pathogenesis. In K. pneumoniae, CPS biosynthesis, type 3 fimbriae expression, and bacterial biofilm formation in K. pneumoniae were controlled by Fur and iron availability (Lin et al., 2010; Wu et al., 2012). Like Fur, we found that IscR also affects the expression of genes involved in the iron-acquisition system and CPS biosynthesis in K. pneumoniae (Wu et al., 2014). IscR acts as a crucial transcriptional regulator that controls iron–sulfur (Fe–S) cluster biosynthesis in bacteria. Fe–S clusters are important cofactors of multiple proteins involved in various cellular processes in bacteria (Andrews et al., 2003; Outten et al., 2004). Switching between the [2Fe–2S] holo and apo forms of IscR can affect the regulatory specificity of IscR to target genes in response to iron availability and oxidative stress (Outten et al., 2004; Yeo et al., 2006; Pullan et al., 2007; Giel et al., 2013). In several bacteria, IscR has been demonstrated to be implicated in pathogenesis (Wu and Outten, 2009; Lim and Choi, 2013; Miller et al., 2014; Haines et al., 2015). In Escherichia coli, expression of type 1 fimbriae is inhibited by apo-IscR to further reduce biofilm formation (Wu and Outten, 2009). Furthermore, IscR can induce the production of CAF/I fimbriae in response to iron depletion in enterotoxigenic E. coli (Haines et al., 2015). In Vibrio vulnificus, the iscR mutant reduces the expression of multiple virulence factors to further affect mouse mortality (Lim and Choi, 2013). In Yersinia pseudotuberculosis, IscR plays a critical role in the control of type 3 secretion and virulence (Miller et al., 2014). However, the regulatory role of IscR in K. pneumoniae pathogenesis remains largely unknown.
In this study, we investigated if IscR regulates type 3 fimbriae expression, biofilm formation, and virulence in K. pneumoniae; the role of the [2Fe–2S] cluster in IscR regulation was also evaluated. Therefore, we found that holo-IscR is able to inhibit type 3 fimbriae expression to further reduce biofilm formation. Although IscR repression of type 3 fimbriae expression occurs indirectly, we demonstrated that holo-IscR directly represses mrkHI expression to further reduce type 3 fimbriae expression. Furthermore, we also found that deletion of iscR reduces the survival rate of mice, while the iscR3CA mutant maintains K. pneumoniae virulence. Taken together, our results show that IscR plays an important role in K. pneumoniae pathogenesis.
Materials and Methods
Bacterial Strains, Plasmids, and Media
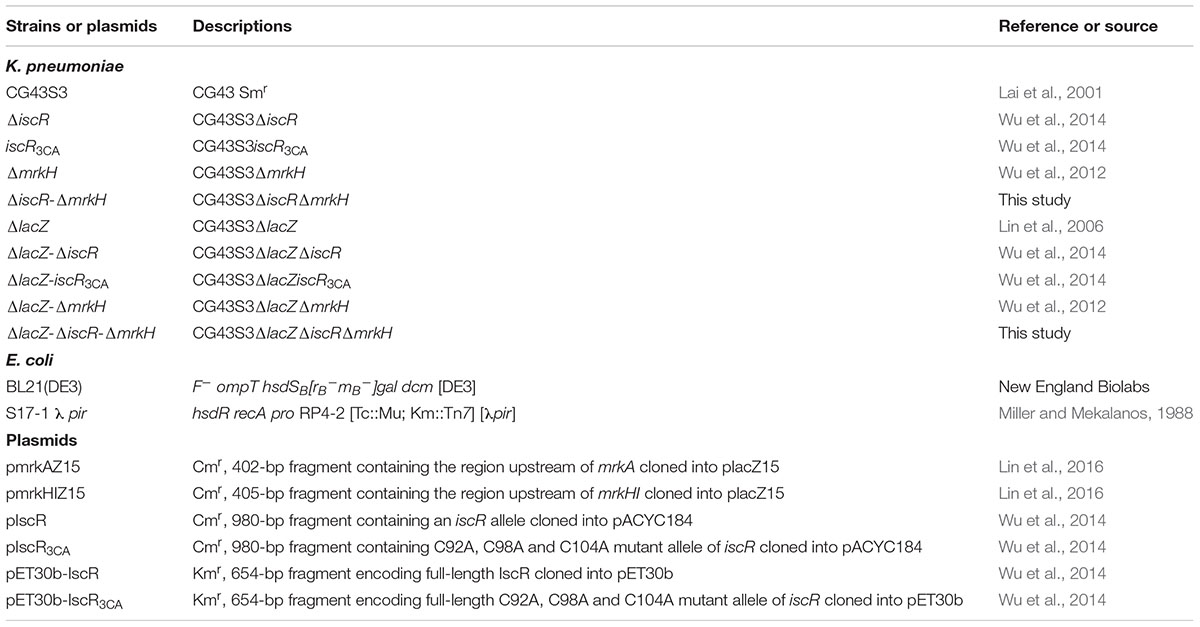
All bacterial strains and plasmids used in this study are listed in Table 1. Primers used in this study are list in Table 2. Bacterial were routinely cultured at 37°C in Luria-Bertani (LB) medium supplemented with appropriate antibiotics including ampicillin (100 μg/ml), kanamycin (25 μg/ml), and streptomycin (500 μg/ml).
Western Blotting
The total proteins of exponential phase K. pneumoniae cultures were separated by SDS-PAGE (approximately 5 μg per lane) and transferred to PVDF membrane. Western analysis was followed as previously described (Lin et al., 2016). Rabbit anti-MrkA antibody was used as the primary antibody. Goat anti-rabbit immunoglobulin G antibody conjugated to horseradish peroxidase (Abcam) was used as the secondary antibody. After incubation with corresponding antibody, the signal in the membranes was collected by ImageQuant LAS 4000 mini (GE Health, United States) after the visualization with an enhanced chemiluminescence ECL western blotting luminal reagent (PerkinElmer, Wellesley, MA, United States).
Quantitative Reverse-Transcription PCR (qRT-PCR)
Total RNA extraction, reverse transcription of isolated mRNA to cDNA, qRT-PCR, and data analysis were performed according to the previous study (Lin et al., 2013). Primers and probes were designed for selected target sequences using Universal ProbeLibrary Assay Design Center (Roche-applied science) and shown in Table 2. Relative gene expressions were quantified using the comparative threshold cycle 2-ΔΔCT method with 23S rRNA as the endogenous reference.
Measurement of Promoter Activity
To generate the promoter region of mrkHI that lacked #2 type 1 IscR box, the plasmid, pmrkHIZ15, was used as the template for the inverse-PCR with the primer pair GT342/GT345 to generate the DNA fragment of PmrkHIΔ2. Subsequently, the purified DNA fragment was treated with DpnI for 2 h, and then subject to T4 PNK treatment and self-ligation. The ligation product was transformed into E. coli DH5α and confirmed by DNA sequencing. Then, the DNA fragment containing PmrkHIΔ2 was subcloned into placZ15 to generate pmrkHIZ15Δ2. The DNA fragment of PmrkHIΔ1, which lacked #1 type 1 IscR box, was also generated by PCR-amplified with primer pair GT348/GT289 and the amplicon was then cloned into placZ15 to generate pmrkHIZ15Δ1. Finally, the promoter-reporter plasmids, pmrkAZ15, pmrkHIZ15, pmrkHIZ15Δ2, and pmrkHIZ15Δ1, were mobilized into K. pneumoniae strains by electroporation, respectively. The β-galactosidase activity of logarithmic phase bacteria was measured as previously described (Lin et al., 2006).
Biofilm Formation
Biofilm formation was assessed by the ability of the cells to adhere to the walls of 96-well microtitre dishes made of PVC (TPP 96 flat) with some modification of the reported protocol (Lembke et al., 2006). The plate contained an aliquot of 1:10 diluted overnight bacteria culture and then was incubated at 37°C statically for 24 h for biofilm formation. The un-adherent bacteria was washed triply with 200 μl PBS and then adherent bacteria was stained with 200 μl of 0.1% safranin solution at room temperature for 30 min. The plates was rinsed twice with deionised water to remove excess stain. Finally, the safranin stained biofilm was solubilized in 200 μl of 95% ethanol and the absorbance determined at a wavelength of 492 nm.
Purification of IscR::His6 and IscR3CA::His6
The plasmids, pET30b-IscR and pET30b-IscR3CA, in E. coli BL21(DE3)[pLysS] (Invitrogen, United States) was used to overexpress the recombinant proteins IscR::His6 and IscR3CA::His6, respectively. The detail of expression and purification of the recombinant proteins was followed as previously described (Wu et al., 2014).
Electrophoretic Mobility Shift Assay (EMSA)
DNA fragments of the putative promoter region of mrkHI were amplified with Pfu polymerase using the indicated primer sets to generate DNA probes for EMSA (PmrkHI-1 and PmrkHI-3). To obtain DNA fragment of PmrkHI-2, the plasmid pmrkHIZ15Δ2 was as a template to be amplified with GT349/GT290 for DNA probe in EMSA. EMSA was performed as previously described (Wu et al., 2014). The assay was repeated in at least 3 independent experiments.
The Peritonitis Model of Mouse Infection
To evaluate the role of iscR in K. pneumoniae virulence, the 8-weeks male BALB/c mice (National Laboratory Animal Center, Taiwan) were injected intraperitoneally with 100 μl of bacterial suspension containing 5 × 104 CFU of mid-log K. pneumoniae strains. The survival rate of the infected mice was monitored daily for 10 days.
Ethics Statement
All the animal experiments were followed as the recommendation in the Guide for the Care and Use of Laboratory Animals of the National Laboratory Animal Center (NLAC, Taiwan). The animal protocols were approved by China Medical University Experimental Animal Center (Permit number: 2016-212).
Statistical Method
The results of qRT-PCR analysis and promoter activity were performed at least triplicate. The results are showed as the mean and standard deviation. Differences between groups were evaluated by an unpaired t-test. The survival rate was determined by log-rank test using GraphPad Prism 5.0. Values of P < 0.05 and P < 0.01 were considered statistically significant difference.
Results
Effect of the State of the Fe-S Cluster in IscR on Type 3 Fimbriae Expression
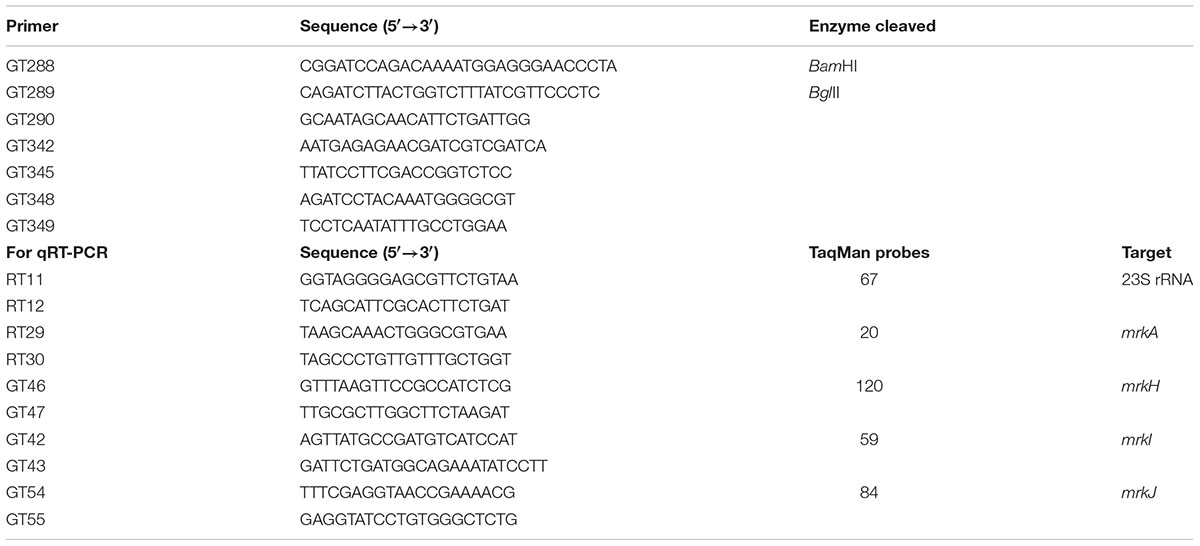
To study whether IscR regulates K. pneumoniae type 3 fimbriae expression, we determined the levels of MrkA (the major subunit of type 3 fimbriae) in CG43S3 (WT) and ΔiscR strains. Compared with the levels in the WT, ΔiscR produced higher amounts of MrkA (Figure 1A), suggesting that IscR represses type 3 fimbriae expression. To further investigate the role of the [2Fe–2S] cluster in the IscR regulation of type 3 fimbriae, an iscR mutant (named iscR3CA), created by replacing three cysteines with alanines to mimic apo-IscR, was used to observe type 3 fimbriae expression. Likewise, we also found that levels of MrkA were higher in the iscR3CA strain than in the WT strain, suggesting that the [2Fe–2S] cluster is required for the repression of type 3 fimbriae expression by IscR. However, we noted that higher levels of MrkA production were found in the iscR3CA strain than in the ΔiscR mutant, implying that apo-IscR acts as an activator in controlling type 3 fimbriae expression. To further confirm the role of the [2Fe–2S] cluster in IscR regulation of fimbriae expression, the empty vector (pACYC184) and complement plasmids pIscR and pIscR3CA were introduced into the ΔiscR strain to observe MrkA production. Compared to the MrkA expression in ΔiscR [pACYC184], the introduction of the complement plasmid pIscR into ΔiscR repressed the MrkA production level, whereas a slight increase in MrkA production was found in ΔiscR [pIscR3CA]. These results suggest that IscR plays a dual role in the regulation of type 3 fimbriae expression and that the status of the [2Fe–2S] cluster in IscR is critical for this regulation. Furthermore, to further study the activity of IscR as a transcriptional regulator in control of type 3 fimbriae expression, mRNA levels of mrkA were measured in the WT, ΔiscR, and iscR3CA strains by qRT-PCR. As shown in Figure 1B, the mRNA levels of mrkA were higher in the ΔiscR and iscR3CA strains than in the WT strain. In addition, the mRNA levels of mrkA in the iscR3CA strain were higher than those in the ΔiscR strain. Furthermore, to further identify IscR could affect the promoter activity of mrkA, a plasmid carrying PmrkA fused with the lacZ reporter gene was constructed and introduced into the ΔlacZ, ΔlacZ-ΔiscR, and ΔlacZ-iscR3CA strains, respectively. As shown in Figure 1C, PmrkA activity was higher in the ΔlacZ-ΔiscR strain than in the ΔlacZ strain. In addition, PmrkA activity was significantly higher in the ΔlacZ-iscR3CA strain than in the ΔlacZ-ΔiscR strain. Taken together, this confirms that the status of the [2Fe–2S] cluster in IscR is critical for regulating type 3 fimbriae expression at the transcriptional level.
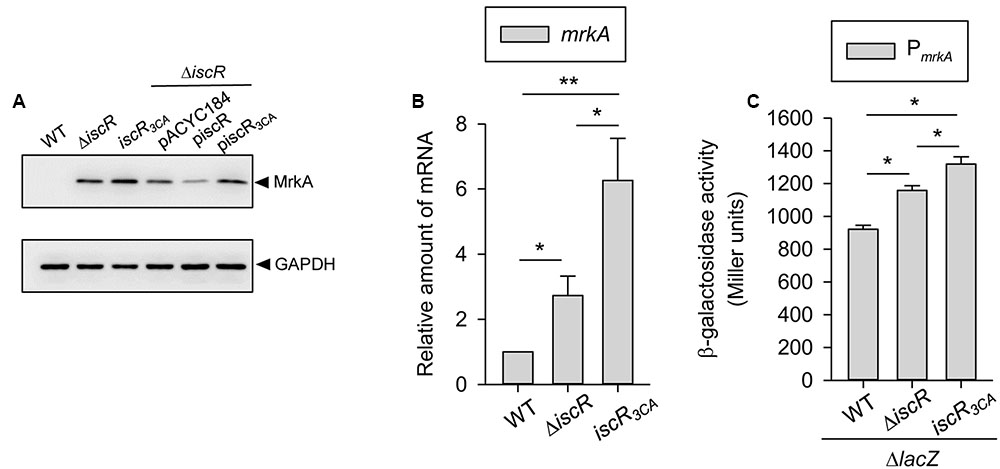
FIGURE 1. IscR affects the type 3 fimbriae expression in K. pneumoniae. K. pneumoniae CG43S3 WT, ΔiscR, and iscR3CA strains was grown to mid-log phase at 37°C in LB broth to observe the type 3 fimbriae expression by (A) western blot analysis against MrkA (the upper panel) and GAPDH antiserum (the lower panel, for internal control). The MrkA and GAPDH proteins are indicated by an arrow, respectively, and (B) qRT-PCR analyses of mrkA gene expression. (C) β-galactosidase activities of K. pneumoniae CG43S3 ΔlacZ and the isogenic strains (ΔlacZ-ΔiscR and ΔlacZ-iscR3CA) carrying the reporter plasmid pmrkAZ15 (PmrkA::lacZ) were determined using log-phase cultures grown in LB medium. The results are representative of three independent experiments. Error bars indicate standard deviations. ∗P < 0.05 and ∗∗P < 0.01 compared to the indicated group.
IscR Represses Biofilm Formation
Based on the fact that type 3 fimbriae are a major mediator of biofilm formation, we further speculated that IscR could affect K. pneumoniae biofilm formation. As shown in Figure 2, we found that the ΔiscR [pACYC184] strain resulted in a slight increase in biofilm formation compared with that in theWT [pACYC184] strain, confirming that the repression of type 3 fimbriae activity by IscR was also reflected in biofilm formation. To further investigate the role of the [2Fe–2S] cluster in the IscR regulation of type 3 fimbriae, iscR3CA [pACYC184] was used to observe biofilm formation. Biofilm formation activity was elevated in the iscR3CA strain compared with that in the WT [pACYC184] strain. This indicates that the [2Fe–2S] cluster of IscR is required for the repression of biofilm formation. Furthermore, the introduction of the complement plasmid pIscR into the ΔiscR strain repressed biofilm formation as compared with that in ΔiscR [pACYC184] and ΔiscR [pIscR3CA], confirming that holo-IscR acts as a negative regulator in controlling biofilm formation. In addition, we noted that biofilm formation was stronger in ΔiscR [pIscR3CA] than in ΔiscR [pACYC184], implying that apo-IscR plays a positive role in biofilm formation.
FIGURE 2. Effect of IscR on biofilm formation. K. pneumoniae strains, WT [pACYC184], ΔiscR [pACYC184], iscR3CA [pACYC184], ΔiscR [piscR], and ΔiscR [piscR3CA], were grown at 37°C for 24 h in LB, and bacterial biofilm formation was quantified as described in “Materials and Methods.” The results are representative of three independent experiments. Error bars indicate standard deviations. ∗P < 0.05 and ∗∗P < 0.01 compared to the indicated group.
No Binding Activity of IscR in the Promoter of mrkA
For further investigation of the mechanism of IscR regulation of mrkA transcription, sequences of putative IscR binding sites were manually analyzed in the promoter region of mrkA. We found a putative type 1 IscR box (5′-ATAACTTAATGAAACGTGAACAAAT-3′) with 60% (15/25 bp) homology to the consensus sequence of E. coli located between -15 and -39 bp relative to the transcriptional start codon of mrkABCDF (type 3 fimbriae gene cluster). Therefore, an electrophoretic mobility shift assay (EMSA) was performed to demonstrate whether IscR could directly bind to the promoter region of mrkABCDF. We found that the purified recombinant IscR::His6 protein was unable to bind to the promoter region of mrkABCDF (data not shown). In addition, we also noted a putative type 2 IscR box (5′-ACCACCCTCGCGTTTTCATCTATCAA-3′) with about 69% (18/26 bp) homology to the consensus sequence of E. coli located between -75 and –100 bp relative to the transcriptional start codon of mrkABCDF. However, the purified recombinant IscR3CA::His6 protein did not bind to this sequence in the promoter region of mrkABCDF either (data not shown). Therefore, these results indicate that IscR represses type 3 fimbriae expression indirectly.
MrkH and MrkI Are Involved in IscR Regulation of Type 3 Fimbriae
A c-di-GMP-related gene cluster (mrkHIJ) adjacent to the type 3 fimbriae operon has been demonstrated to regulate type 3 fimbriae expression (Murphy and Clegg, 2012; Wu et al., 2012). To further investigate whether mrkHIJ are involved in the IscR regulon, the effect of iscR deletion on the mRNA levels of these genes was determined by qRT-PCR. Compared with levels in the WT strain, the mRNA levels of mrkH and mrkI were markedly increased in the ΔiscR and iscR3CA strains, while no apparent effect was found on the mRNA level of mrkJ (Figure 3A). This indicates that the [2Fe-2S] cluster of IscR is required for repressing the expression of mrkH and mrkI. Furthermore, we also noted that the expression levels of mrkH and mrkI in the iscR3CA strain were higher than those in the ΔiscR strain. This implies that apo-IscR activates mrkH and mrkI expression. Likewise, the activities of PmrkHI were also higher in the ΔlacZ-ΔiscR and ΔlacZ-iscR3CA strains than in the ΔlacZ strain (Figure 3B), but no apparent difference was found between the ΔlacZ-ΔiscR and ΔlacZ-iscR3CA strains, indicating that holo-IscR acts a transcriptional repressor of mrkHI expression.
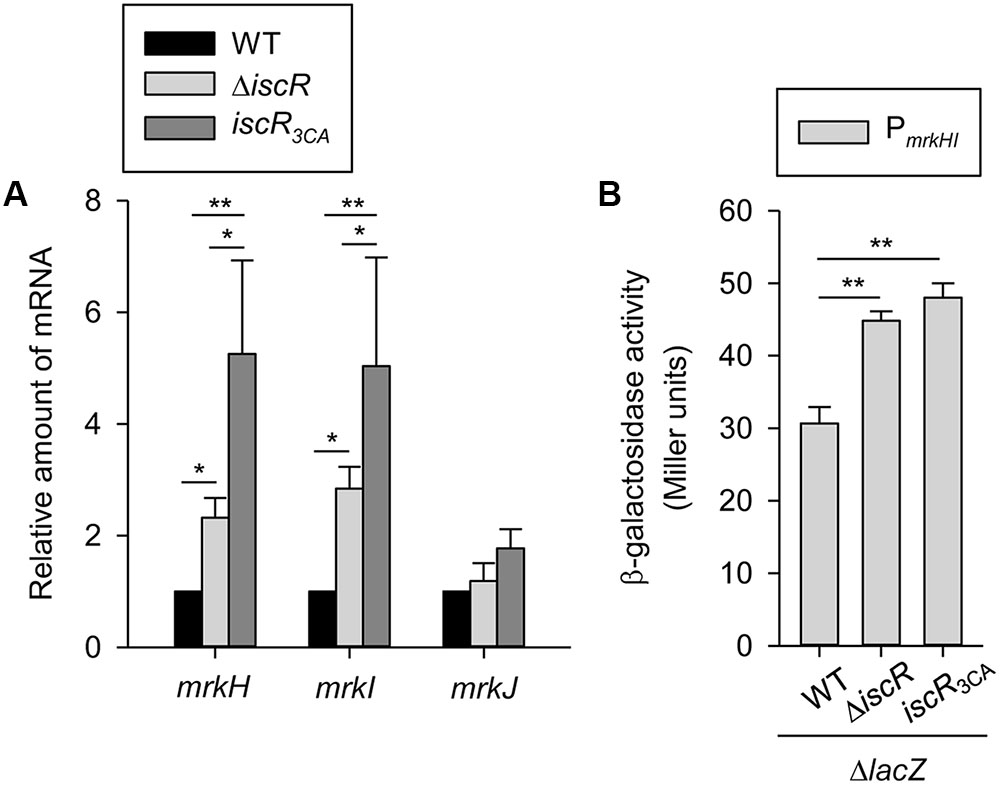
FIGURE 3. Effect of IscR on mrkH, mrkI, and mrkJ expression. (A) qRT-PCR analyses of the mrkH, mrkI, and mrkJ expressions for WT, ΔiscR, and iscR3CA strains in LB medium. (B) β-galactosidase activities of K. pneumoniae CG43S3 ΔlacZ and the isogenic strains (ΔlacZ-ΔiscR and ΔlacZ-iscR3CA) carrying the reporter plasmid pmrkHZ15 (PmrkHI::lacZ) were determined using log-phase cultures grown in LB medium. The results are representative of three independent experiments. Error bars indicate standard deviations. ∗P < 0.05 and ∗∗P < 0.01 compared to the indicated group.
IscR Directly Binds the Promoter of mrkHI
For further investigation of the mechanism of IscR regulation of mrkHI transcription, sequences of putative IscR binding sites were manually analyzed in the promoter region of mrkHI. As shown in Figure 4A, we found two predicted type 1 IscR boxes (#1 and #2) located at -277 to -254 and -211 to -187 relative to the translation start site of mrkHI, respectively. The #1 and #2 sites are 76% (19/25 bp) and 68% (17/25 bp) homologous, respectively, with the consensus sequence of E. coli. We hypothesized that IscR would bind directly to the #1 or #2 site in the promoter region of mrkHI to repress gene transcription, and we confirmed this by performing an EMSA. As shown in Figure 4B, we found that IscR::His6 could directly bind to PmrkHI-1, PmrkHI-2, and PgalF-1 (as a positive control), whereas no specific binding between IscR::His6, and PmrkH-3 or PgalF-2 (as a negative control) was found. Although the binding activity of IscR::His6 to PmrkHI-1 and PmrkHI-2 seemed to be weaker than that to PgalF-1, the intensity of the shifted bands slightly increased when the protein concentration was increased (Figure 4B). This result supports that IscR could specifically bind to the #1 site in the promoter region of mrkHI to control mrkHI expression. In addition, compared with that of IscR::His6, the recombinant [2Fe–2S]-clusterless IscR, IscR3CA::His6, was unable to bind PmrkHI-1 (Data not shown). These results indicate a direct interaction between IscR and the #1 site of the type 1 IscR box in the mrkHI promoter and confirm that the [2Fe–2S] cluster of IscR plays a crucial role in this interaction.
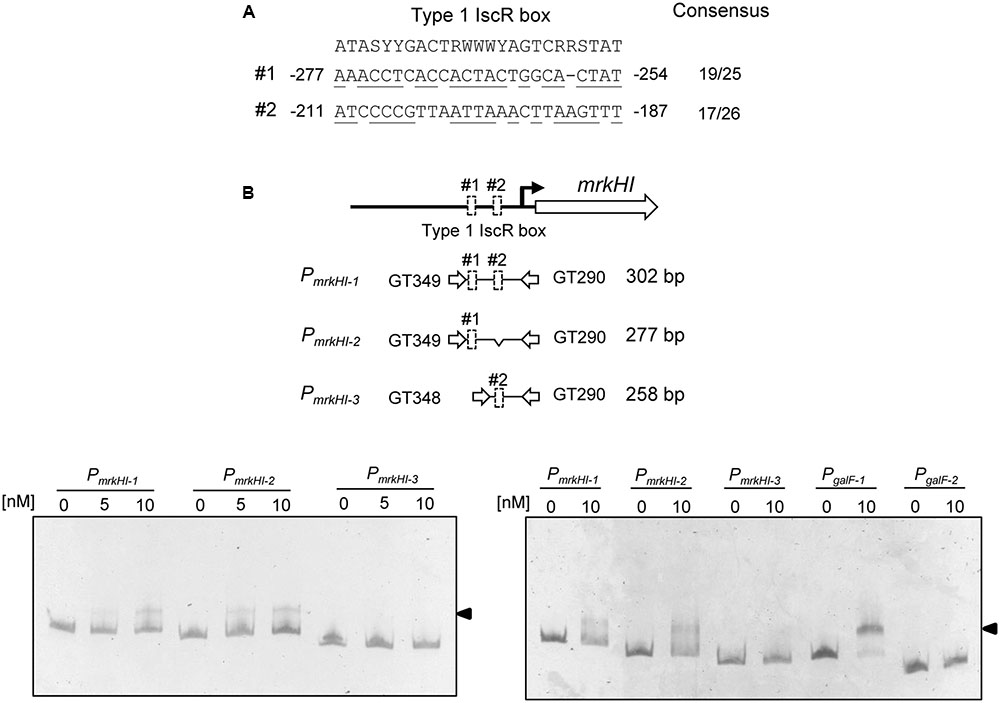
FIGURE 4. IscR represses directly the mrkHI expression. (A) DNA sequence alignment between the E. coli type 1 IscR box and the putative IscR binding sequence in the upstream region of mrkH. Positions identical to the consensus sequences are underlined. (B) Diagrammatic representation of the upstream of mrkH (the upper panel). The large arrows represent the open reading frames. The primer sets used in PCR amplification of the DNA probes are indicated, and the numbers denote the DNA amplified length. The predicted type 1 IscR boxes are deleted and indicated by an open box. Different concentrations of purified IscR::His6 were incubated with 5 ng of various DNA fragments of the upstream regions of mrkH. Following incubation at room temperature for 30 min, the mixtures were analyzed on a 5% non-denaturing polyacrylamide gel. The gel was stained with SYBR Green I dye and photographed.
IscR Regulates the Expression of Type 3 Fimbriae through MrkH and an Unknown Factor
Although MrkH is a well-known regulator of type 3 fimbriae (Wilksch et al., 2011; Yang et al., 2013), we wanted to identify whether MrkH is the sole transcriptional regulator in the regulation of type 3 fimbriae expression by IscR. An ΔiscRΔmrkH strain was generated, and the mRNA expression of mrkA was analyzed in the ΔiscR, ΔiscRΔmrkH, and ΔmrkH strains. As shown in Figure 5A, the mRNA expression of mrkA in the ΔiscRΔmrkH strain was significantly higher than that in the ΔmrkH strain. Similarly, the promoter activity of mrkA also confirmed this finding; although the effect was weak, it was still significant (Figure 5B). This suggests that in addition to MrkH, another transcriptional factor is also involved in the repression of type 3 fimbriae expression by IscR.
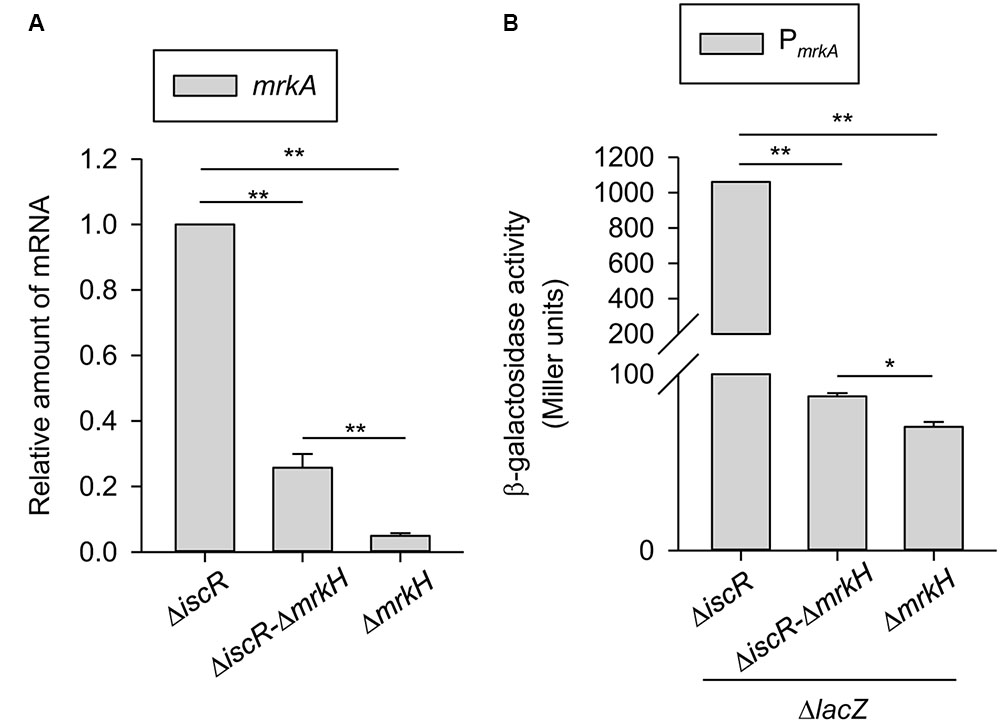
FIGURE 5. Role of MrkH in IscR regulation of type 3 fimbriae expression. (A) qRT-PCR analyses of mrkA expression in ΔiscR, ΔiscR-ΔmrkH, and ΔmrkH strains which was grown in LB medium. (B) β-galactosidase activities of K. pneumoniae CG43S3 ΔlacZ-ΔiscR, ΔlacZ-ΔiscR-ΔmrkH, and ΔlacZ-ΔmrkH carrying the reporter plasmid pmrkAZ15 (PmrkA::lacZ) were determined using log-phase cultures grown in LB medium. The results are representative of three independent experiments. Error bars indicate standard deviations. ∗P < 0.05 and ∗∗P < 0.01 compared to the indicated group.
Role of IscR in K. pneumoniae Virulence
To understand the effect of the deletion of iscR on K. pneumoniae virulence, the survival of mice that were intraperitoneally inoculated with the WT, ΔiscR, or iscR3CA strains was monitored for 10 days. As shown in Figure 6A, when mice were inoculated with the WT, ΔiscR, and iscR3CA strains, survival decreased to 16.7, 66.7, and 16.7% by day 10, respectively. The deletion of iscR showed a trend to attenuate the bacterial virulence; however, the difference did not reach statistical significance. In addition, this result also implied that the absence of the [2Fe–2S] cluster of IscR did not eliminate K. pneumoniae virulence during infection. To further confirm the result, the mice were intraperitoneally inoculated with ΔiscR [pACYC184], ΔiscR [pIscR], and ΔiscR [pIscR3CA] to monitor the survival rate. As shown in Figure 6B, we found that mice inoculated with ΔiscR [pACYC184], ΔiscR [pIscR], or ΔiscR [pIscR3CA] exhibited survivals of 100, 33.3, and 50% by day 10, respectively. The complementation of iscR significantly decreased the survival of mice, suggesting that IscR is involved in the K. pneumoniae virulence. Besides, the complementation of iscR3CA appeared to partly restore the bacterial virulence; however, the difference is not statistically different.
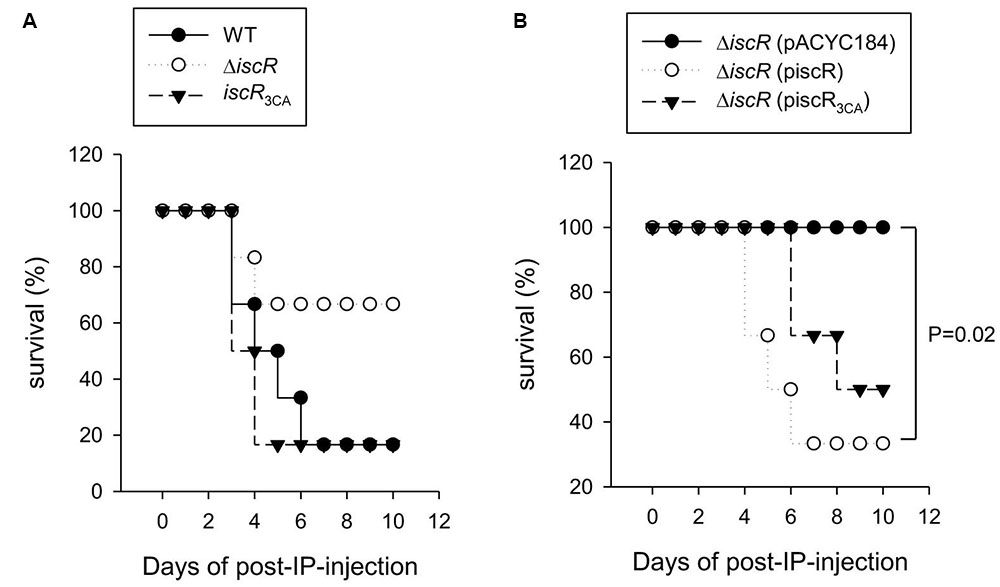
FIGURE 6. Analysis of iscR on K. pneumoniae virulence to survival rate of mice. The survival rate of K. pneumoniae CG43S3 (A) WT (dark spot), ΔiscR (open spot), or iscR3CA (dark triangle) and (B) the complement strains, ΔiscR [pACYC184] (dark spot), ΔiscR [pIscR] (open spot), or ΔiscR [pIscR3CA] (dark triangle) infected mice (n = 6 per group) was monitored daily for 10 days and determined by log-rank test using GraphPad Prism 5.0; P-value of <0.05 was considered statistically significant.
Discussion
In many bacteria, iron-responsive regulators play important roles in controlling the expression of several virulence factors according to iron availability (Wu and Outten, 2009; Wu et al., 2012; Lim and Choi, 2013; Miller et al., 2014). Previously, we demonstrated that iron availability affects CPS, iron acquisition systems, type 3 fimbriae expression, and biofilm formation in K. pneumoniae (Lin et al., 2010; Wu et al., 2012, 2014). In addition, while the regulatory role of IscR in CPS biosynthesis and the iron-acquisition system have been demonstrated (Wu et al., 2014), the role of IscR in K. pneumoniae pathogenesis had not been entirely elucidate. In this study, we found that type 3 fimbriae expression and biofilm formation were also affected by the status of [2Fe–2S] cluster of IscR, playing a critical role in mediating the expression of virulence factors for successful infection.
In K. pneumoniae, Fur has been demonstrated to play a central role in directly activating mrkA and mrkH expression to increase biofilm formation (Wu et al., 2012). In this study, we found that, compared to the WT strain, both the K. pneumoniae ΔiscR and iscR3CA strains harbored increased the type 3 fimbriae expression and biofilm-forming activities, which could be reversed by the complementation of pIscR, but not pIscR3CA into the ΔiscR strain (Figures 1, 2). Likewise, overexpression of pIscR in K. pneumoniae CG43S3 also repressed the mRNA expression of mrkA, while pIscR3CA in K. pneumoniae CG43S3 activated the mrkA expression (Supplementary Figure S1). These results suggest that IscR represses type 3 fimbriae expression and biofilm formation in a Fe–S-cluster-dependent manner. Although Fur and IscR exert positive and negative regulatory effects, respectively, on K. pneumoniae biofilm formation under iron-repleted conditions, we speculated that Fur played a major role, since iscR expression is repressed in response to environmental iron (Wu et al., 2014). Furthermore, although type 3 fimbriae are critical in K. pneumoniae biofilm formation, it has also been demonstrated that the function of fimbriae is hindered by the concomitant expression of a thick capsule on the bacterial surface (Schembri et al., 2005; Goncalves Mdos et al., 2014). Previously, we found that holo-IscR but not apo-IscR could activate CPS production (Wu et al., 2014). In Figure 1, the repressive effect of IscR on MrkA production at the translational level was more apparent than that at the transcriptional level. We hypothesized that the reduced CPS production in the ΔiscR strain would promote the assembly of type 3 fimbriae on the bacterial surface. Moreover, we also found that type 3 fimbriae expression is slightly increased in the iscR3CA strain as compared to that in the WT strain (Figure 1). In contrast to pIscR, the introduction of pIscR3CA into the ΔiscR strain increased K. pneumoniae biofilm formation (Figure 2B). It implies that apo-IscR acts as an activator to increase biofilm formation. However, the recombinant protein IscR3CA::His6 did not bind to the promoter regions of mrkA or mrkH, suggesting that apo-IscR indirectly regulates the expression of type 3 fimbriae. In K. pneumoniae, c-di-GMP is a critical second messenger that influences biofilm formation and type 3 fimbriae expression (Johnson and Clegg, 2010; Wilksch et al., 2011; Wu et al., 2012). To identify possible IscR-regulated genes that are involve in c-di-GMP signaling, we analyzed the upstream sequences of c-di-GMP-related genes in K. pneumoniae CG43, (Lin et al., 2016). We found a typical type 2 IscR box exhibiting more than 73% homology with the E. coli consensus sequence upstream of the c-di-GMP-related genes D364_06025 and D364_22720 in K. pneumoniae CG43 (data not shown). Apo-IscR may affect biofilm formation and type 3 fimbriae expression via the regulation of c-di-GMP-related gene expression, which awaits further investigation.
Holo-IscR directly repressed mrkHI expression to affect type 3 fimbriae expression, while apo-IscR appeared to indirectly activate mrkHI expression (Figures 3, 4). In many bacteria, small non-coding RNAs play a critical role in post-transcriptional regulation, allowing bacteria to adapt to various environmental stimuli (Waters and Storz, 2009). RyhB is a well-known iron-responsive small RNA in bacteria (Oglesby-Sherrouse and Murphy, 2013), and we previously demonstrated that apo-IscR can directly activate several iron uptake systems that affect intracellular iron homeostasis (Wu et al., 2014). In K. pneumoniae, RyhB is involved in the regulation of CPS biosynthesis and the iron-acquisition system (Huang et al., 2012). Because small RNA regulates its target mRNAs via base pairing (Masse et al., 2003; Geissmann and Touati, 2004), the 5′ untranslated region (5′ UTR) of mrkHI mRNA was analyzed for sequences complementary to the RyhB sequence. No apparent potential interacting site was found by using RNAhybrid in BiBiServ (Rehmsmeier et al., 2004). Therefore, whether other small RNAs are involved in IscR regulation of type 3 fimbriae expression requires further investigation. Recently, H-NS was also reported as an activator in control of type 3 fimbriae expression and biofilm formation in K. pneumoniae (Ares et al., 2016). Deletion of hns increased the mRNA expression of mrkH, mrkI, and mrkJ. Thus, H-NS may affect the c-di-GMP concentration, through activation of mrkJ expression, to further influence MrkH and MrkI activity and type 3 fimbriae expression (Ares et al., 2016). As shown in Figure 3A, deletion of iscR increased the mRNA levels of mrkH and mrkI but not mrkJ; thus, IscR and H-NS seemed to regulate the expression of type 3 fimbriae in different manners.
To further analyze the DNA sequence of PmrkH to observe whether other transcriptional regulator is also involved in mrkH regulation, we found a putative binding site of phosphorylated ArcA is overlapped with the #2 site that displays 80% (12/15 bp) homology with the consensus sequence of E. coli (Liu and De Wulf, 2004). ArcA acts as the transcriptional regulator in the ArcA/B two-component system, regulating gene expression to adapt to aerobic and microaerobic conditions (Iuchi and Weiner, 1996; Alexeeva et al., 2003). Oxygen-limited conditions may trigger the kinase activity of ArcB, which then phosphorylates and activates the DNA binding activity of ArcA (Carpenter and Payne, 2014). Therefore, we suggest that the expression of mrkH and type 3 fimbriae could be affected by phosphorylated ArcA in response to redox growth conditions. This possibility should be further investigated. Furthermore, a slightly higher expression level of mrkA was found in ΔiscRΔmrkH as compared with that in ΔmrkH (Figure 5). This indicates that IscR may affect other transcriptional regulator(s) besides MrkH in order to influence type 3 fimbriae expression. In addition to MrkH, MrkI is a LuxR-type transcriptional regulator containing a conserved aspartate residue (D56) able to receive a phosphorylated group for affecting its regulatory activity. In our previous study, we have demonstrated that a D56A site-directed MrkI mutant, which loss the phosphorylated state in MrkI, exhibited to decrease MrkA production as compared to that in a D56E site-directed MrkI mutant, which mimic the phosphorylate state of MrkI (Wu et al., 2012). Therefore, whether IscR could also affect the phosphorylation of MrkI to further influence type 3 fimbriae expression remains to be studied.
During infection, Fe–S cluster homeostasis in bacteria is deeply affected by iron starvation and oxidative stress conditions (Miller and Britigan, 1997; Wilks and Burkhard, 2007; Py et al., 2011). These stimuli may affect the functions of IscR in controlling gene expression during infection. In Figure 6A, we found that IscR is required for regulating the virulence of K. pneumoniae during infection in a mouse peritonitis model. Furthermore, the iscR3CA mutant exhibited a similar virulence to that of the WT strain. In K. pneumoniae, CPS and iron-acquisition systems are critical and important virulence factors for successful infection (Lin et al., 2004; Regueiro et al., 2006; Russo et al., 2015). We have previously demonstrated that CPS can be activated by holo-IscR, while the three iron-acquisition systems (fhuA, sitA, and iucA) are directly activated by apo-IscR (Wu et al., 2014). It may be described that the deletion of iscR in K. pneumoniae reduces CPS production and iron-acquisition system expression to further diminish virulence during infection, while the introduction of pIscR into the ΔiscR strain increases virulence compared with that of the vector alone or pIscR3CA in the ΔiscR strain. Furthermore, aerobactin (iuc) plays a critical role in the growth and survival of highly virulent K. pneumoniae strains (Russo et al., 2015). It may be that high expression of aerobactin biosynthesis is one of the factors used by the iscR3CA mutant for maintaining a similar virulence to that of the WT strain. In addition, overexpression of suf, which is another Fe-S assembly gene cluster, in the iscR3CA mutant leads to a defect in the proton motive force in E. coli and Y. pseudotuberculosis (Ezraty et al., 2013; Miller et al., 2014). Such a defect could influence the expression of multiple virulence factors, such as antibiotic resistance, the type 3 secretion pathway, and bacterial mobility (Ezraty et al., 2013; Miller et al., 2014). In K. pneumoniae CG43S3, we also found that the mRNA level of sufA was apparently increased in the iscR3CA mutant as compared to that in the WT and ΔiscR strains (Supplementary Figure S2A). This means that apo-IscR could activate the suf operon, as it does in E. coli and Y. pseudotuberculosis. However, compared to the WT strain, no apparent effect on growth rate was found in the ΔiscR and iscR3CA strains grown in LB medium (Supplementary Figure S2B). Therefore, whether overexpression of suf in the iscR3CA mutant affects the proton motive force in K. pneumoniae remains to be investigated.
Aside from the role of the CPS and iron-acquisition systems during infection, type 3 fimbriae play crucial roles in adhesion to host cells, persistence, and biofilm formation (Hornick et al., 1992; Tarkkanen et al., 1997; Sebghati and Clegg, 1999; Jagnow and Clegg, 2003). Furthermore, type 3 fimbriae are key factors that affect the ability of K. pneumoniae to colonize and subsequently persist in mice (Murphy et al., 2013). Therefore, we suggest that IscR is also involved in K. pneumoniae colonization and adherence with eukaryotic cells and catheters through the regulation on the type 3 fimbriae expression and the bacterial biofilm forming activity. The role of IscR in K. pneumoniae virulence according to different infectious routes and host interactions needs to be further evaluated. In addition, IscR also plays an important role in mediating proper levels of Fe–S cluster biosynthesis in bacteria via transcriptional repression of the iscRSUA operon (Yeo et al., 2006; Giel et al., 2013), indicating that the manner in which IscR impacts K. pneumoniae virulence is dependent on the conditions that K. pneumoniae encounters during the course of infection.
Taken together, our results show that IscR can directly repress mrkHI expression to affect type 3 fimbriae expression and biofilm formation. Furthermore, the deletion of iscR decreases K. pneumoniae virulence during infection, demonstrating that IscR is implicated in K. pneumoniae pathogenesis.
Author Contributions
Conceived and designed the experiments: T-HL, CY-T, and C-TL. Performed the experiments: T-HL, Y-CL, C-CW, and C-TL. Analyzed the data: C-YT, Y-CL, and CL. Contributed reagents/materials/analysis tools: C-YT, Y-CL, C-CW, and C-FH. Wrote the paper: T-HL and C-TL. All authors read and approved the final manuscript.
Funding
The work is supported by the grant from Ministry of Science and Technology (MOST 105-2320-B-039-051-) and Taichung Tzuchi Hospital, The Buddhist Tzu Chi Medical Foundation (TTCRD103-10 and TTCRD104-11). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We are grateful to Mr. Jing-Ciao Lin and Miss. Yi-Min Hong for their technical assistance during the study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmicb.2017.01984/full#supplementary-material
References
Alexeeva, S., Hellingwerf, K. J., and Teixeira De Mattos, M. J. (2003). Requirement of ArcA for redox regulation in Escherichia coli under microaerobic but not anaerobic or aerobic conditions. J. Bacteriol. 185, 204–209. doi: 10.1128/JB.185.1.204-209.2003
Andrews, S. C., Robinson, A. K., and Rodriguez-Quinones, F. (2003). Bacterial iron homeostasis. FEMS Microbiol. Rev. 27, 215–237. doi: 10.1016/S0168-6445(03)00055-X
Ares, M. A., Fernandez-Vazquez, J. L., Rosales-Reyes, R., Jarillo-Quijada, M. D., Von Bargen, K., Torres, J., et al. (2016). H-NS nucleoid protein controls virulence features of Klebsiella pneumoniae by regulating the expression of Type 3 pili and the capsule polysaccharide. Front. Cell. Infect. Microbiol. 6:13. doi: 10.3389/fcimb.2016.00013
Carpenter, C., and Payne, S. M. (2014). Regulation of iron transport systems in Enterobacteriaceae in response to oxygen and iron availability. J. Inorg. Biochem. 133, 110–117. doi: 10.1016/j.jinorgbio.2014.01.007
Di Martino, P., Cafferini, N., Joly, B., and Darfeuille-Michaud, A. (2003). Klebsiella pneumoniae type 3 pili facilitate adherence and biofilm formation on abiotic surfaces. Res. Microbiol. 154, 9–16. doi: 10.1016/S0923-2508(02)00004-9
Ezraty, B., Vergnes, A., Banzhaf, M., Duverger, Y., Huguenot, A., Brochado, A. R., et al. (2013). Fe-S cluster biosynthesis controls uptake of aminoglycosides in a ROS-less death pathway. Science 340, 1583–1587. doi: 10.1126/science.1238328
Geissmann, T. A., and Touati, D. (2004). Hfq, a new chaperoning role: binding to messenger RNA determines access for small RNA regulator. EMBO J. 23, 396–405. doi: 10.1038/sj.emboj.7600058
Giel, J. L., Nesbit, A. D., Mettert, E. L., Fleischhacker, A. S., Wanta, B. T., and Kiley, P. J. (2013). Regulation of iron-sulphur cluster homeostasis through transcriptional control of the Isc pathway by [2Fe-2S]-IscR in Escherichia coli. Mol. Microbiol. 87, 478–492. doi: 10.1111/mmi.12052
Goncalves Mdos, S., Delattre, C., Balestrino, D., Charbonnel, N., Elboutachfaiti, R., Wadouachi, A., et al. (2014). Anti-biofilm activity: a function of Klebsiella pneumoniae capsular polysaccharide. PLOS ONE 9:e99995. doi: 10.1371/journal.pone.0099995
Haines, S., Arnaud-Barbe, N., Poncet, D., Reverchon, S., Wawrzyniak, J., Nasser, W., et al. (2015). IscR regulates synthesis of colonization factor antigen I fimbriae in response to iron starvation in enterotoxigenic Escherichia coli. J. Bacteriol. 197, 2896–2907. doi: 10.1128/JB.00214-15
Han, S. H. (1995). Review of hepatic abscess from Klebsiella pneumoniae. An association with diabetes mellitus and septic endophthalmitis. West. J. Med. 162, 220–224.
Hornick, D. B., Allen, B. L., Horn, M. A., and Clegg, S. (1992). Adherence to respiratory epithelia by recombinant Escherichia coli expressing Klebsiella pneumoniae type 3 fimbrial gene products. Infect. Immun. 60, 1577–1588.
Huang, C. J., Wang, Z. C., Huang, H. Y., Huang, H. D., and Peng, H. L. (2013). YjcC, a c-di-GMP phosphodiesterase protein, regulates the oxidative stress response and virulence of Klebsiella pneumoniae CG43. PLOS ONE 8:e66740. doi: 10.1371/journal.pone.0066740
Huang, S. H., Wang, C. K., Peng, H. L., Wu, C. C., Chen, Y. T., Hong, Y. M., et al. (2012). Role of the small RNA RyhB in the Fur regulon in mediating the capsular polysaccharide biosynthesis and iron acquisition systems in Klebsiella pneumoniae. BMC Microbiol. 12:148. doi: 10.1186/1471-2180-12-148
Iuchi, S., and Weiner, L. (1996). Cellular and molecular physiology of Escherichia coli in the adaptation to aerobic environments. J. Biochem. 120, 1055–1063. doi: 10.1093/oxfordjournals.jbchem.a021519
Jagnow, J., and Clegg, S. (2003). Klebsiella pneumoniae MrkD-mediated biofilm formation on extracellular matrix- and collagen-coated surfaces. Microbiology 149, 2397–2405. doi: 10.1099/mic.0.26434-0
Johnson, J. G., and Clegg, S. (2010). Role of MrkJ, a phosphodiesterase, in type 3 fimbrial expression and biofilm formation in Klebsiella pneumoniae. J. Bacteriol. 192, 3944–3950. doi: 10.1128/JB.00304-10
Lai, Y. C., Peng, H. L., and Chang, H. Y. (2001). Identification of genes induced in vivo during Klebsiella pneumoniae CG43 infection. Infect. Immun. 69, 7140–7145. doi: 10.1128/IAI.69.11.7140-7145.2001
Lau, Y. J., Hu, B. S., Wu, W. L., Lin, Y. H., Chang, H. Y., and Shi, Z. Y. (2000). Identification of a major cluster of Klebsiella pneumoniae isolates from patients with liver abscess in Taiwan. J. Clin. Microbiol. 38, 412–414.
Lavender, H., Jagnow, J. J., and Clegg, S. (2005). Klebsiella pneumoniae type 3 fimbria-mediated immunity to infection in the murine model of respiratory disease. Int. J. Med. Microbiol. 295, 153–159. doi: 10.1016/j.ijmm.2005.04.001
Lembke, C., Podbielski, A., Hidalgo-Grass, C., Jonas, L., Hanski, E., and Kreikemeyer, B. (2006). Characterization of biofilm formation by clinically relevant serotypes of group A streptococci. Appl. Environ. Microbiol. 72, 2864–2875. doi: 10.1128/AEM.72.4.2864-2875.2006
Lim, J. G., and Choi, S. H. (2013). IscR is a global regulator essential for pathogenesis of Vibrio vulnificus and induced by host cells. Infect. Immun. 82, 569–578. doi: 10.1128/IAI.01141-13
Lin, C. T., Chen, Y. C., Jinn, T. R., Wu, C. C., Hong, Y. M., and Wu, W. H. (2013). Role of the cAMP-dependent carbon catabolite repression in capsular polysaccharide biosynthesis in Klebsiella pneumoniae. PLOS ONE 8:e54430. doi: 10.1371/journal.pone.0054430
Lin, C. T., Huang, T. Y., Liang, W. C., and Peng, H. L. (2006). Homologous response regulators KvgA, KvhA and KvhR regulate the synthesis of capsular polysaccharide in Klebsiella pneumoniae CG43 in a coordinated manner. J. Biochem. 140, 429–438. doi: 10.1093/jb/mvj168
Lin, C. T., Lin, T. H., Wu, C. C., Wan, L., Huang, C. F., and Peng, H. L. (2016). CRP-Cyclic AMP regulates the expression of Type 3 fimbriae via cyclic di-GMP in Klebsiella pneumoniae. PLOS ONE 11:e0162884. doi: 10.1371/journal.pone.0162884
Lin, C. T., Wu, C. C., Chen, Y. S., Lai, Y. C., Chi, C., Lin, J. C., et al. (2010). Fur regulation of the capsular polysaccharide biosynthesis and iron-acquisition systems in Klebsiella pneumoniae CG43. Microbiology 157, 419–429. doi: 10.1099/mic.0.044065-0
Lin, J. C., Chang, F. Y., Fung, C. P., Xu, J. Z., Cheng, H. P., Wang, J. J., et al. (2004). High prevalence of phagocytic-resistant capsular serotypes of Klebsiella pneumoniae in liver abscess. Microbes Infect. 6, 1191–1198. doi: 10.1016/j.micinf.2004.06.003
Liu, X., and De Wulf, P. (2004). Probing the ArcA-P modulon of Escherichia coli by whole genome transcriptional analysis and sequence recognition profiling. J. Biol. Chem. 279, 12588–12597. doi: 10.1074/jbc.M313454200
Livrelli, V., De Champs, C., Di Martino, P., Darfeuille-Michaud, A., Forestier, C., and Joly, B. (1996). Adhesive properties and antibiotic resistance of Klebsiella, Enterobacter, and Serratia clinical isolates involved in nosocomial infections. J. Clin. Microbiol. 34, 1963–1969.
Masse, E., Escorcia, F. E., and Gottesman, S. (2003). Coupled degradation of a small regulatory RNA and its mRNA targets in Escherichia coli. Genes Dev. 17, 2374–2383. doi: 10.1101/gad.1127103
Miller, H. K., Kwuan, L., Schwiesow, L., Bernick, D. L., Mettert, E., Ramirez, H. A., et al. (2014). IscR is essential for Yersinia pseudotuberculosis type III secretion and virulence. PLOS Pathog. 10:e1004194. doi: 10.1371/journal.ppat.1004194
Miller, R. A., and Britigan, B. E. (1997). Role of oxidants in microbial pathophysiology. Clin. Microbiol. Rev. 10, 1–18.
Miller, V. L., and Mekalanos, J. J. (1988). A novel suicide vector and its use in construction of insertion mutations: osmoregulation of outer membrane proteins and virulence determinants in Vibrio cholerae requires toxR. J. Bacteriol. 170, 2575–2583. doi: 10.1128/jb.170.6.2575-2583.1988
Murphy, C. N., and Clegg, S. (2012). Klebsiella pneumoniae and type 3 fimbriae: nosocomial infection, regulation and biofilm formation. Future Microbiol. 7, 991–1002. doi: 10.2217/fmb.12.74
Murphy, C. N., Mortensen, M. S., Krogfelt, K. A., and Clegg, S. (2013). Role of Klebsiella pneumoniae type 1 and type 3 fimbriae in colonizing silicone tubes implanted into the bladders of mice as a model of catheter-associated urinary tract infections. Infect. Immun. 81, 3009–3017. doi: 10.1128/IAI.00348-13
Neilands, J. B. (1981). Microbial iron compounds. Annu. Rev. Biochem. 50, 715–731. doi: 10.1146/annurev.bi.50.070181.003435
Oglesby-Sherrouse, A. G., and Murphy, E. R. (2013). Iron-responsive bacterial small RNAs: variations on a theme. Metallomics 5, 276–286. doi: 10.1039/c3mt20224k
Ong, C. L., Beatson, S. A., Totsika, M., Forestier, C., Mcewan, A. G., and Schembri, M. A. (2010). Molecular analysis of type 3 fimbrial genes from Escherichia coli, Klebsiella and Citrobacter species. BMC Microbiol. 10:183. doi: 10.1186/1471-2180-10-183
Outten, F. W., Djaman, O., and Storz, G. (2004). A suf operon requirement for Fe-S cluster assembly during iron starvation in Escherichia coli. Mol. Microbiol. 52, 861–872. doi: 10.1111/j.1365-2958.2004.04025.x
Podschun, R., and Ullmann, U. (1998). Klebsiella spp. as nosocomial pathogens: epidemiology, taxonomy, typing methods, and pathogenicity factors. Clin. Microbiol. Rev. 11, 589–603.
Porcheron, G., and Dozois, C. M. (2015). Interplay between iron homeostasis and virulence: Fur and RyhB as major regulators of bacterial pathogenicity. Vet. Microbiol. 179, 2–14. doi: 10.1016/j.vetmic.2015.03.024
Pullan, S. T., Gidley, M. D., Jones, R. A., Barrett, J., Stevanin, T. M., Read, R. C., et al. (2007). Nitric oxide in chemostat-cultured Escherichia coli is sensed by Fnr and other global regulators: unaltered methionine biosynthesis indicates lack of S nitrosation. J. Bacteriol. 189, 1845–1855. doi: 10.1128/JB.01354-06
Py, B., Moreau, P. L., and Barras, F. (2011). Fe-S clusters, fragile sentinels of the cell. Curr. Opin. Microbiol. 14, 218–223. doi: 10.1016/j.mib.2011.01.004
Regueiro, V., Campos, M. A., Pons, J., Alberti, S., and Bengoechea, J. A. (2006). The uptake of a Klebsiella pneumoniae capsule polysaccharide mutant triggers an inflammatory response by human airway epithelial cells. Microbiology 152, 555–566. doi: 10.1099/mic.0.28285-0
Rehmsmeier, M., Steffen, P., Hochsmann, M., and Giegerich, R. (2004). Fast and effective prediction of microRNA/target duplexes. RNA 10, 1507–1517. doi: 10.1261/rna.5248604
Rohmer, L., Hocquet, D., and Miller, S. I. (2011). Are pathogenic bacteria just looking for food? Metabolism and microbial pathogenesis. Trends Microbiol. 19, 341–348. doi: 10.1016/j.tim.2011.04.003
Russo, T. A., Olson, R., Macdonald, U., Beanan, J., and Davidson, B. A. (2015). Aerobactin, but not yersiniabactin, salmochelin, or enterobactin, enables the growth/survival of hypervirulent (hypermucoviscous) Klebsiella pneumoniae ex vivo and in vivo. Infect. Immun. 83, 3325–3333. doi: 10.1128/IAI.00430-15
Sahly, H., Podschun, R., Oelschlaeger, T. A., Greiwe, M., Parolis, H., Hasty, D., et al. (2000). Capsule impedes adhesion to and invasion of epithelial cells by Klebsiella pneumoniae. Infect. Immun. 68, 6744–6749. doi: 10.1128/IAI.68.12.6744-6749.2000
Schembri, M. A., Blom, J., Krogfelt, K. A., and Klemm, P. (2005). Capsule and fimbria interaction in Klebsiella pneumoniae. Infect. Immun. 73, 4626–4633. doi: 10.1128/IAI.73.8.4626-4633.2005
Sebghati, T. A., and Clegg, S. (1999). Construction and characterization of mutations within the Klebsiella mrkD1P gene that affect binding to collagen type V. Infect. Immun. 67, 1672–1676.
Tamayo, R., Pratt, J. T., and Camilli, A. (2007). Roles of cyclic diguanylate in the regulation of bacterial pathogenesis. Annu. Rev. Microbiol. 61, 131–148. doi: 10.1146/annurev.micro.61.080706.093426
Tarkkanen, A. M., Virkola, R., Clegg, S., and Korhonen, T. K. (1997). Binding of the type 3 fimbriae of Klebsiella pneumoniae to human endothelial and urinary bladder cells. Infect. Immun. 65, 1546–1549.
Touati, D. (2000). Iron and oxidative stress in bacteria. Arch. Biochem. Biophys. 373, 1–6. doi: 10.1006/abbi.1999.1518
Wang, Q., Chang, C. S., Pennini, M., Pelletier, M., Rajan, S., Zha, J., et al. (2016). Target-agnostic identification of functional monoclonal antibodies against Klebsiella pneumoniae multimeric MrkA fimbrial subunit. J. Infect. Dis. 213, 1800–1808. doi: 10.1093/infdis/jiw021
Waters, L. S., and Storz, G. (2009). Regulatory RNAs in bacteria. Cell 136, 615–628. doi: 10.1016/j.cell.2009.01.043
Wilks, A., and Burkhard, K. A. (2007). Heme and virulence: how bacterial pathogens regulate, transport and utilize heme. Nat. Prod. Rep. 24, 511–522. doi: 10.1039/b604193k
Wilksch, J. J., Yang, J., Clements, A., Gabbe, J. L., Short, K. R., Cao, H., et al. (2011). MrkH, a novel c-di-GMP-dependent transcriptional activator, controls Klebsiella pneumoniae biofilm formation by regulating type 3 fimbriae expression. PLOS Pathog. 7:e1002204. doi: 10.1371/journal.ppat.1002204
Wu, C. C., Lin, C. T., Cheng, W. Y., Huang, C. J., Wang, Z. C., and Peng, H. L. (2012). Fur-dependent MrkHI regulation of type 3 fimbriae in Klebsiella pneumoniae CG43. Microbiology 158, 1045–1056. doi: 10.1099/mic.0.053801-0
Wu, C. C., Wang, C. K., Chen, Y. C., Lin, T. H., Jinn, T. R., and Lin, C. T. (2014). IscR regulation of capsular polysaccharide biosynthesis and iron-acquisition systems in Klebsiella pneumoniae CG43. PLOS ONE 9:e107812. doi: 10.1371/journal.pone.0107812
Wu, Y., and Outten, F. W. (2009). IscR controls iron-dependent biofilm formation in Escherichia coli by regulating type I fimbria expression. J. Bacteriol. 191, 1248–1257. doi: 10.1128/JB.01086-08
Yang, J., Wilksch, J. J., Tan, J. W., Hocking, D. M., Webb, C. T., Lithgow, T., et al. (2013). Transcriptional activation of the mrkA promoter of the Klebsiella pneumoniae type 3 fimbrial operon by the c-di-GMP-dependent MrkH protein. PLOS ONE 8:e79038. doi: 10.1371/journal.pone.0079038
Yang, Y. S., Siu, L. K., Yeh, K. M., Fung, C. P., Huang, S. J., Hung, H. C., et al. (2009). Recurrent Klebsiella pneumoniae liver abscess: clinical and microbiological characteristics. J. Clin. Microbiol. 47, 3336–3339. doi: 10.1128/JCM.00918-09
Keywords: Klebsiella pneumoniae, IscR, type 3 fimbriae, biofilm formation, MrkHI
Citation: Lin T-H, Tseng C-Y, Lai Y-C, Wu C-C, Huang C-F and Lin C-T (2017) IscR Regulation of Type 3 Fimbriae Expression in Klebsiella pneumoniae CG43. Front. Microbiol. 8:1984. doi: 10.3389/fmicb.2017.01984
Received: 01 June 2017; Accepted: 26 September 2017;
Published: 16 October 2017.
Edited by:
Xihui Shen, Northwest A&F University, ChinaReviewed by:
Victoria Auerbuch, University of California, Santa Cruz, United StatesMiguel A. De la Cruz, Instituto Mexicano de Seguridad Social, Mexico
Copyright © 2017 Lin, Tseng, Lai, Wu, Huang and Lin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ching-Ting Lin, Z2luZ3RpbmdAbWFpbC5jbXUuZWR1LnR3
†These authors have contributed equally to this work.
 Tien-Huang Lin
Tien-Huang Lin Cheng-Yin Tseng
Cheng-Yin Tseng Yi-Chyi Lai
Yi-Chyi Lai Chien-Chen Wu
Chien-Chen Wu Chun-Fa Huang
Chun-Fa Huang Ching-Ting Lin
Ching-Ting Lin