- 1Department of Infectious Diseases, University of Georgia, Athens, GA, United States
- 2Virology Branch, Veterinary Sciences Division, Agri-Food and Biosciences Institute, Belfast, United Kingdom
- 3Wellcome Wolfson Institute for Experimental Medicine, School of Medicine, Dentistry and Biomedical Sciences, Queen’s University Belfast, Belfast, United Kingdom
Respiratory syncytial virus (RSV) or measles virus (MeV) infection modifies host responses through small non-coding RNA (sncRNA) expression. We show that RSV or MeV infection of neuronal cells induces sncRNAs including various microRNAs and transfer RNA fragments (tRFs). We show that these tRFs originate from select tRNAs (GCC and CAC for glycine, CTT and AAC for Valine, and CCC and TTT for Lysine). Some of the tRNAs are rarely used by RSV or MeV as indicated by relative synonymous codon usage indices suggesting selective cleavage of the tRNAs occurs in infected neuronal cells. The data implies that differentially expressed sncRNAs may regulate host gene expression via multiple mechanisms in neuronal cells.
Introduction
Small non-coding RNAs (sncRNAs) are <200 nucleotides and include microRNAs (miRs), PIWI-interacting RNAs (piRs), and transfer RNA fragments (tRNA)-derived RNA fragments (tRFs) (Petrov et al., 2017). The expression of sncRNAs differs in their biogenesis and functional activity (Bartel, 2009; Bakre et al., 2019). Most sncRNAs induced by viral infection involve regulatory mechanisms affecting virus replication, persistence, or latency (Grassmann and Jeang, 2008; Roizman et al., 2011), and immune evasion (Cullen, 2013; Bernier and Sagan, 2018). RSV typically infects ciliated respiratory epithelial cells, while MeV may infect dendritic cells and subsequently infect the epithelia for virus release from the respiratory tract (Lay et al., 2016; Lin and Richardson, 2016; Singh et al., 2016; Taniguchi et al., 2019). These viruses cause a spectrum of diseases and may infect a spectrum of people, i.e., the very young to the elderly (Griffin, 2018; Mazur et al., 2018). RSV is a major cause of serious lower respiratory tract infections in childhood (Mirra et al., 2018; Paes, 2018), but also affects the elderly and immune-compromised (Haber, 2018). MeV causes acute viral infection with respiratory involvement leading to symptoms of rash and more serious complications, and in some cases to mortality (Bohmwald et al., 2018; Leung et al., 2018). Both RSV and MeV are paramyxoviruses with non-segmented negative-sense single-stranded RNA genomes (Russell et al., 2018). Unfortunately, there are no approved RSV vaccines and anti-viral treatments are limited. Although there is an effective MeV vaccine, incidences of MeV infection are increasing worldwide due to vaccine complacency.
Respiratory syncytial virus and MeV can infect neuronal cells, and MeV may cause persistent infection (Rota et al., 2017; Griffin et al., 2018). Compromised immunity may facilitate neuronal infection (Rima and Duprex, 2005; Omar et al., 2017; Ganesan et al., 2018; Ferren et al., 2019). MeV infection of neuronal cells may lead to subacute sclerosing panencephalitis (SSPE), and measles inclusion body encephalitis (MIBE) in immunocompromised individuals. In MIBE, MeV replicates in the central nervous system usually because of an inadequate immune response (McQuaid et al., 1998; Hardie et al., 2013; Rota et al., 2017). RSV infection in mice has been associated with exaggerated neurogenic inflammation in the airways, and studies have shown that the neuropeptide, substance P (SP) is a mediator of neurogenic inflammation (King et al., 2001; Tan et al., 2008).
Expression of the RSV G protein is associated with increased pulmonary expression of SP, and lung neurons express CX3CR1 (Tripp et al., 2000, 2002, 2003; Haynes et al., 2003). CX3CR1 is the receptor for fractalkine (aka neurotactin) and CX3CR1 has been shown to bind RSV G protein (Tripp et al., 2001; Harcourt et al., 2004; Choi et al., 2012; Bakre et al., 2017; Bergeron et al., 2021).
Studies in mice suggest that RSV may cause lasting infection (Dakhama et al., 1997; Li et al., 2006). RSV has been shown to infect mouse primary cortical neuronal cells as shown by co-localization of the RSV N protein and neuronal markers (Li et al., 2006). These findings support how RSV may cause neurological irregularities in patients (Eisenhut, 2006; Li et al., 2006; Morichi et al., 2017). Several studies have described an association between lower respiratory tract RSV infection in infancy and the subsequent development of persistent wheezing in children (Zhou N. et al., 2017; Zhong et al., 2018). In mice, RSV induces long-term airway disease characterized by chronic airway inflammation and airway hyperreactivity (Long et al., 2016; Zhou N. et al., 2017), and RSV antigens have been detected in the lungs >100 days (Schwarze et al., 2004). However, RSV persistence does not appear in the bronchial epithelium (the primary site of viral replication) but in deeper lung structures (Long et al., 2016; Zhou N. et al., 2017).
Respiratory syncytial virus and MeV infection modulate sncRNA expression inducing mRNA degradation or translation inhibition and have a role in determining the level of protein expression of host cells (Munday et al., 2012). It has been shown that tRNAs are cleaved during cellular stress, and that cleavage results in tRFs that contain the 5′ end (5′tRFs) or the 3′ end (3′tRFs) of the parent tRNA molecule (Sofos et al., 2015; Advani and Ivanov, 2019). Although the specific activity of tRFs is not well-understood, tRFs can behave as small interfering RNA leading to the degradation of transcripts (Ivanov et al., 2011) which can regulate ribosomal loading and protein chain elongation (Sobala and Hutvagner, 2013).
Accumulating data have shown that both coding and non-coding transcriptomes are modified during RSV infection. We have shown that RSV infection of human A549 lung cells modifies sncRNA expression and that the RSV G protein and NS1/NS2 proteins modulate miR expression (Bakre et al., 2012, 2015, 2017). Other studies have shown that the pattern of miR expression is modified following RSV infection of nasal epithelial cells (Inchley et al., 2015; Hasegawa et al., 2018), and PBMCs from children (Wang et al., 2017). Deregulated miR expression occurs in MeV-infected human neuroblastoma cells and PBMCs (Inchley et al., 2015; Yis et al., 2015; Naaman et al., 2017; Hasegawa et al., 2018), as well as in PBMCs from RSV-infected children (Wang et al., 2017). It is known that MeV persistence in neuroblastoma cells is assisted by the downregulation of CDK6, a component of cell cycle progression regulated by miRNA-124 (Riddell et al., 2007; Naaman et al., 2017; Griffin et al., 2018).
In this study, we examined sncRNA responses in neuronal SHSY5Y (SHS) cells infected with RSV or MeV and show that infection with either of these viruses modifies miRs and tRF expression in a temporal and virus-specific manner. Anti-microbial peptides (AMPs) are generated in the response to pathogens, and arginine and glycine are especially abundant in AMPs (Mishra and Wang, 2012). In this study, we show that RSV or MeV infection modifies the extent of transfer RNA fragments (tRFs), and the finding of decreased full-length tRNAs after infection indicates decreased translation rates possibly indicative of a lessened anti-viral state. Together, these findings strengthen the notion that sncRNAs have a key role in regulating the host cell response to infection and viral replication.
Materials and Methods
Cells and Viruses
Human SHSY5Y (SHS) neuroblastoma cells (ATCC CRL 2266) were grown in DMEM (Sigma, St. Louis, MO, United States) containing 10% FBS (Atlanta Biologicals, Atlanta, GA, United States). SHS cells were maintained at 37°C, 5% CO2. RSV strain A2 (ATCC CCL 81) was propagated in Vero cells (Oshansky et al., 2009; Dahiya and Atreya, 2014). Briefly, 80% confluent Vero cells were infected (MOI = 1.0) for 1 h at 37°C, 5% CO2. After infection, 2% FBS was added to the DMEM, and the cells were incubated for 3 days until syncytia were evident. On the day of harvest, the cells were removed and centrifuged at 500 × g for 15 min at 4°C. RSV strain A2 was used for the infection in SHS cells and rgRSV224 GFP (Hallak et al., 2000, 2007; Techaarpornkul et al., 2002) (a kind gift from Dr. Michael Teng, University of South Florida) for microscopy studies. The WT strain Dublin-3267 of MeV was grown in Vero cells expressing human CD150 (SLAM), a high-affinity receptor for MeV (Tatsuo et al., 2000).
RNA Isolation and Library Construction
Total RNA from mock-treated or virus-infected SHS cells was isolated using RNAzol RT (MRC, Cincinnati, OH, United States) per the manufacturer’s instructions and divided into small and large RNA fractions and quantified using a Qubit fluorimeter-based RNA assay (Invitrogen Life Tech, Carlsbad, CA, United States). Illumina next-generation sequencing (NGS) libraries were constructed using a TruSeq® small RNA library (Illumina, San Diego, CA, United States). Briefly, small RNA from mock-treated SHS cells (n = 2/group), or RSV- or MeV-infected SHS cells (n = 3/group) was isolated at 12 or 24 hpi and ligated with 3′ and 5′ RNA adaptors using T4 RNA ligase 2 (Epicenter Biotechnologies, Madison, WI, United States) at 28°C for 60 min. Ligated RNA was reverse transcribed using proprietary reverse primers and the first-strand cDNA was amplified with a combination of a proprietary forward primer and reverse primers containing unique index bar codes per the manufacturer’s instructions. Amplicons were run on a Tapestation 2200 (Agilent, Santa Clara, CA, United States) high-sensitivity DNA chip to visualize products. Indexed samples were pooled per the manufacturer’s protocol and electrophoresed on a 6% TBE-urea PAGE gel. Bands corresponding to 147 and 157 bp corresponding to adaptor-ligated mature miRNA and other non-coding RNAs were cut out and cDNAs were precipitated. Libraries were validated on a Tapestation 2200 (Agilent) using a high-sensitivity DNA chip. Libraries were denatured for 5 min using 5 M NaOH and loaded onto a MiSeq (Agilent) for sequencing by synthesis. Reads were trimmed to remove adaptor sequences and then analyzed for miRNA differential expression using Chimira (Vitsios and Enright, 2015) and OASIS 2.0 (Rahman et al., 2018a). Read counts were normalized to a total number of reads per sample and then differential expression was calculated using DESeq2 (Love et al., 2014). All reads used for analysis had quality scores (Q_ > 30. This represents less than or equal to 1 error per 1,000 nts corresponding to a 99.99% accuracy.
miR Analysis
The host genes and pathways predicted to be regulated by miRs were determined by DIANA miRPath analysis (Vlachos et al., 2015). miRs were examined using the DIANA-miRPath server and targets extracted from the Tarbase database (Karagkouni et al., 2018). Enriched KEGG pathway analysis was used to determine intersections (Kanehisa et al., 2016, 2017). We applied a p-value threshold of ≤0.05 along with a false-discovery rate correction.
Virus Quantitation
QRT-PCR of RSV M, or MeV M, and N gene primer-probes were examined for each replicate to confirm infection of SHS cells. Sequences of the primers/probes used were RSV M forward 5′- ACACCCAAGGGACCTTCACTAAGA, RSV M reverse 5′-GCCTTGATTTCACAGGGTGTGGTT-3′, RSV M probe/56-FAM/AAG TGC AGT GCT AGC ACA AAT GCC CA/3BHQ_1. For MeV, primer sequences were forward primer MeVEdNPF-5′-CAAGACCCTGAGGGATTCAA-3′ and reverse primer MeVEdNPR-5′-CTCTCGCATCACTTGCTCTG-3. For both viruses, 100 ng of RNA was reverse transcribed using Lunascript RT Supermix (New England Biolabs, Ipswitch, MA, United States) using the following conditions: primer annealing at 25°C for 2 min, reverse transcription at 55°C for 30 min followed by heat-inactivation of reverse transcriptase at 95°C for 1 min. Undiluted cDNA was used for PCR. PCR reactions contained cDNA, 0.4 μM of forward and reverse oligomers, 0.8 μM of the probe, 2X Luna Universal probe master mix (New England Biolabs) and were amplified as follows: initial denaturation at 95°C for 60 s, 40 cycles of denaturation at 95°C for 10 s, and combined annealing and extension at 60°C for 30 s. For MeV NP amplification, PCR reactions contained cDNA, 10 μM of forward and reverse primers, Q5 2X High-Fidelity master mix (New England Biolabs), and was amplified using the conditions: initial denaturation at 98°C for 30 s, 25 cycles of 98°C for 10 s, annealing at 65°C for 30 s and extension at 72°C for 2 min, and a final extension at 72°C for 2 min. MeV NP amplicons were resolved on a 1% agarose gel in low osmolality buffer at 5 V/cm and imaged using a Protein Simple imager (Invitrogen).
Results
sncRNAs and Virus-Infected SHS Cells
Previous studies from our laboratory have shown that RSV infection of A549 cells modifies miR expression (Bakre et al., 2012, 2015, 2017) however, information regarding miR expression in RSV- or MeV-infected neuronal SHS cells is inadequate (Naaman et al., 2017; Cakmak Genc et al., 2018; Haralambieva et al., 2018). Neuronal cells are not the primary cell type infected by RSV, but they can be infected and may act as a reservoir of infection. Mechanisms that contribute to this are poorly understood. Thus, we examined SHS cells that were RSV- or MeV-infected (MOI = 1.0), or mock-treated and sncRNA expression determined at 12 and 24 hpi by Illumina NGS. We confirmed RSV infection of SHS neuronal cells using RSV-GFP. SHS cells were infected with RSV-GFP at a MOI = 0.1 (Supplementary Figure 1). At 48 h and 72 hpi, virus replication was evident using combined dark field and fluorescence microscopy (UV Eclipse Ti2000-U microscope, Nikon).
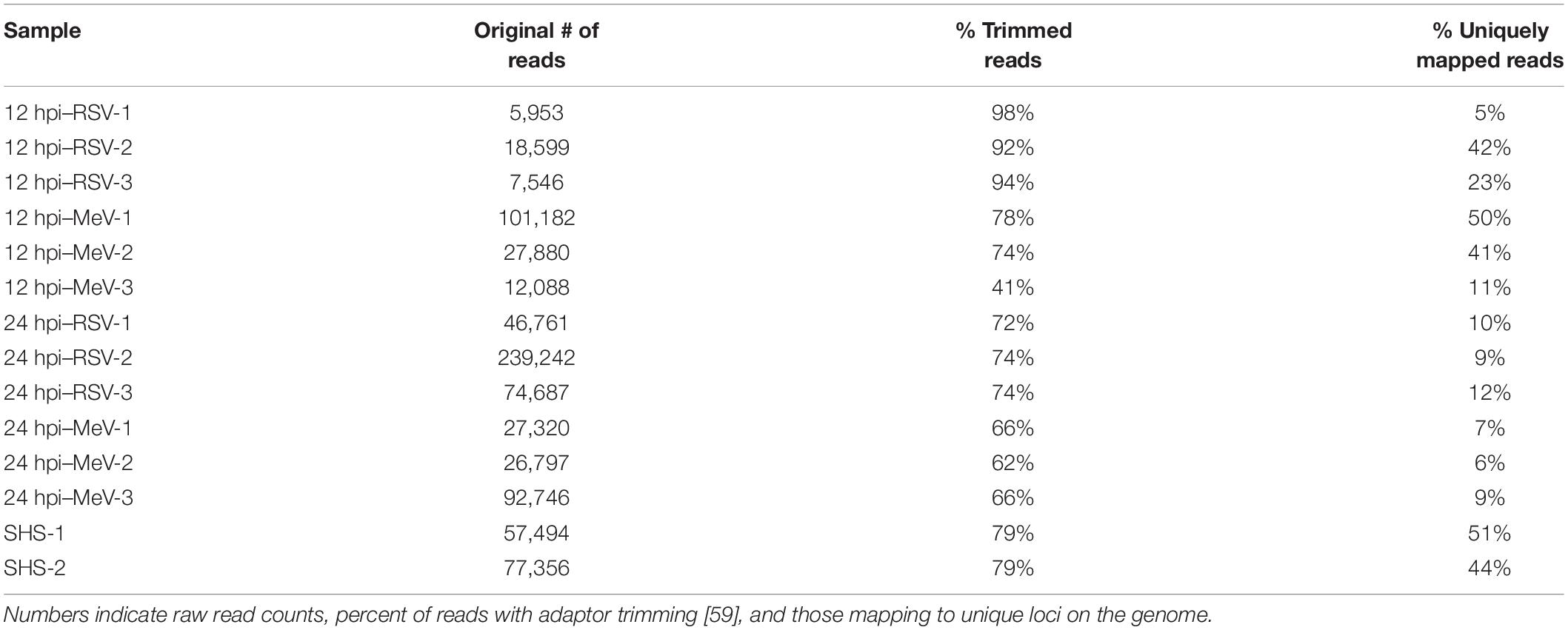
It is important to note that production of infectious viral particles is restricted in the neuronal environment and viral spread is mediated by fusogenic events leading to syncytia formation that are common to both MeV and RSV infection (Sato et al., 2018). Total reads expressed in a text-based format (fastq) were used and the corresponding reads passing quality scores (Q > 30) are listed in Table 1. Raw fastq reads were mapped to the human genome, and miRs using Chimira (Vitsios and Enright, 2015) and Oasis 2.0 (Rahman et al., 2018a) were normalized to the total read counts and used to calculate differential expression using DESeq 2.0 (Love et al., 2014) relative to mock-treated cells. We used principal component analysis (PCA) to determine sample clustering based on similarity for miR expression profiling. PCA is a method of taking combinations of measured variables and lowering the dimensionality of the data to find the principal source of variance. As the human genome encodes > 2,300 miRs and we examined RSV and MeV and two time points, the dataset had > 9,200 variables. PCA identified two major component dimensions—PC1 consists of the time component in addition to virus and miRNA expression, and PC2 is the infection state. PC1 and PC2 are principal components and organized by the percent of variability they explain. Being derived from combinations of variables, PCs do not have labels/units. Samples 1–3 (12 h MeV), 4–6 (12 h RSV), 7–9 (24 h MeV), and 10–12 (24 h RSV) clustered together and away from mock infected cells (samples 13–14) suggesting that the sncRNA response to MeV or RSV infection is distinct from mock infected cells. In addition, clustering of 12 and 24 h MeV and RSV datasets suggests that infections elicit temporal responses. The PCA results indicate that the time post infection is a major component driving differential miRNA expression as shown on PC1 (x-axis with 54% variance) compared to pathogen (PC2 y-axis 13% variance). This is evident in the clustering among mock-treated vs. virus-infected cells (Figure 1). Similarly, miR expression profiles in RSV- or MeV-infected SHS cells at 12 and 24 hpi revealed distinct clustering. Most RSV samples clustered separately from MeV at each time-point (Figure 1).
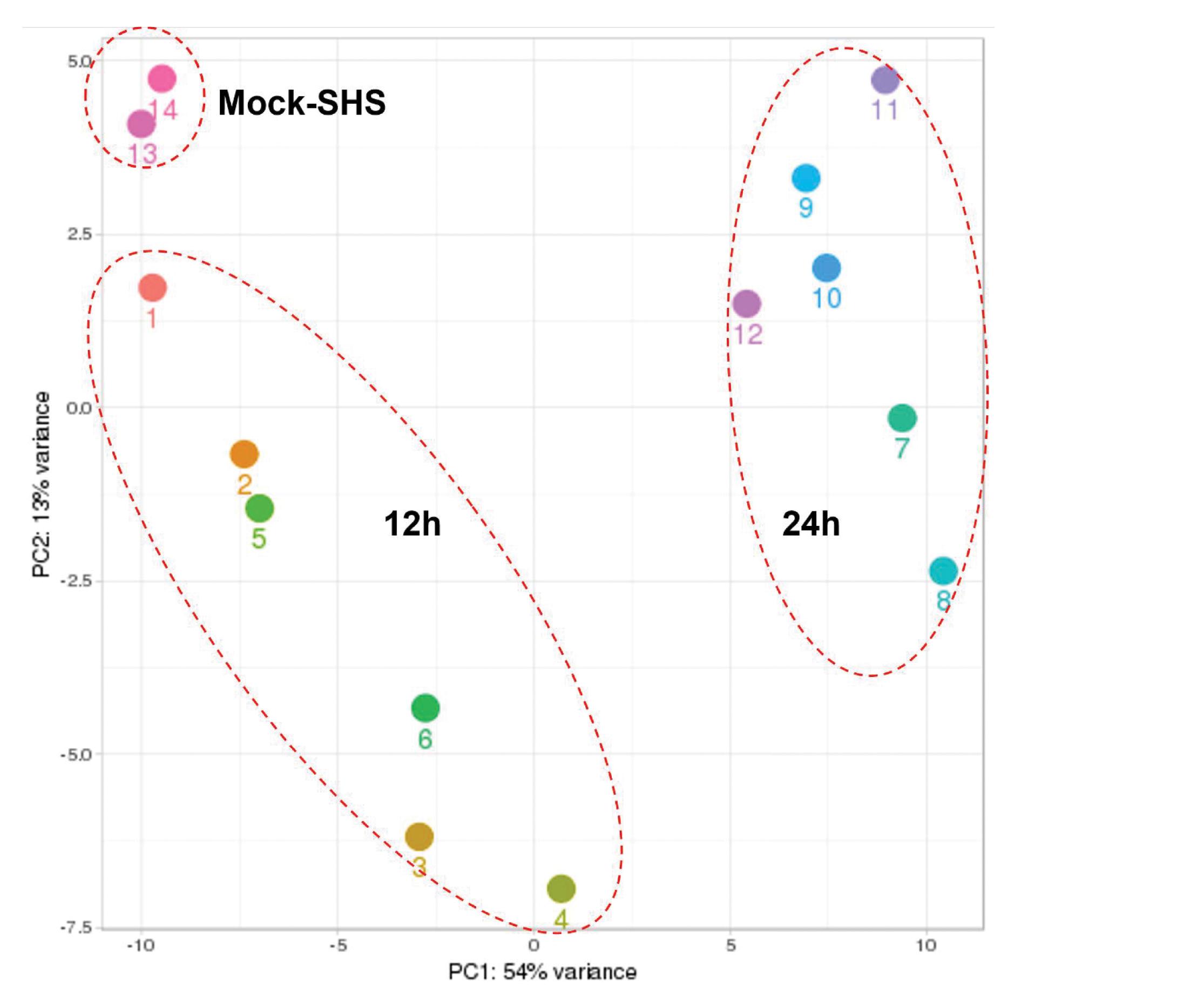
Figure 1. Hierarchical clustering of miR expression. Analysis of overall read composition following RSV- or MeV-infection of SHS cells. Clustering is indicated by dashed circles. 12 h = 12 hpi; 24 h = 24 hpi. Samples 1–3 are 12 h MeV infection, samples 4–6 are 12 h RSV infection, samples 7–9 are 24 h MeV infection, samples 10–12 are 24 h RSV infected SHS cells and mock infected samples are samples 13 and 14. PCA involved all miR, differential expression profiles, and RSV and MeV time points (12 h vs. 24 h) to determine the derived variables known as principal components (PCs). Principal component 1 (PC1) was separated by time (hpi) while principal component 2 (PC2) was separated by infected vs. non-infected.
The data were filtered to contain only read numbers > 5 (Table 1), and those having p-values ≤0.05, and fold-change ≤1.5 or ≥1.5 were used to help identify downregulated vs. upregulated miRs. RSV or MeV infection was confirmed by qPCR. The chief deregulated miRs expressed in SHS cells following RSV- or MeV-infection are shown in Table 2. Compared to mock-infection, expression of miR-10b-5p, miR-181c-5p, and miR-125b-5p were strikingly downregulated in SHS cells at 12 or 24 hpi following RSV or MeV infection. In contrast, expression of p-miR-330, p-miR-338, p-miR-317, p-miR-106, p-miR-113, p-miR-256, p-miR-232, p-miR-103 and miR-182-5p, miR-4532, miR-1273g-3p, miR-483-3p, miR-3141, miR-1246 miR-3196, miR-4516, and miR-4488 were substantially upregulated in SHS cells.
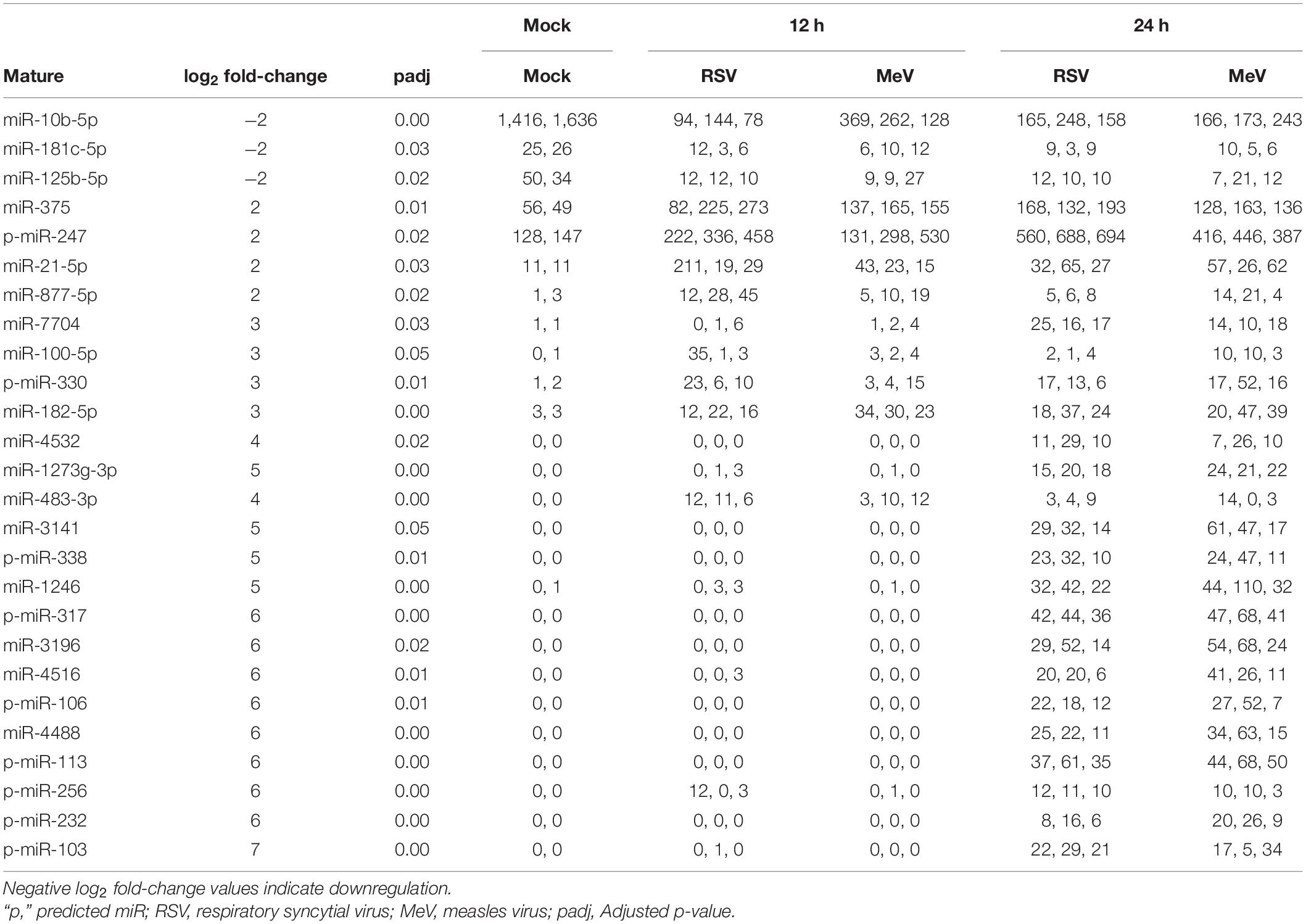
Table 2. Normalized read counts between mock, RSV- and MeV-infected samples as analyzed by OASIS 2.0 (Rahman et al., 2018a).
Studies suggest that modifications involving Adenosine to Inosine (A- > I) or Cytosine to Uracil (C- > U) within miRs, N6 methylation, and oxidation affect miR stability, maturation and target specificity (Alarcon et al., 2015; Wang et al., 2015; Correia De Sousa et al., 2019). Post-transcriptional modifications to miRNAs have been shown to alter their binding and function (Pirouz et al., 2019; Briand et al., 2020; Cheray et al., 2020). We therefore examined epitranscriptional modifications of the deregulated miRs using Chimira (Figure 2; Vitsios and Enright, 2015). Most modifications were located on the 3p arms of the deregulated miRs. RSV infection in SHS cells decreased the abundance of 3p modifications at 12 hpi (Figure 2 and Supplementary Table 1).
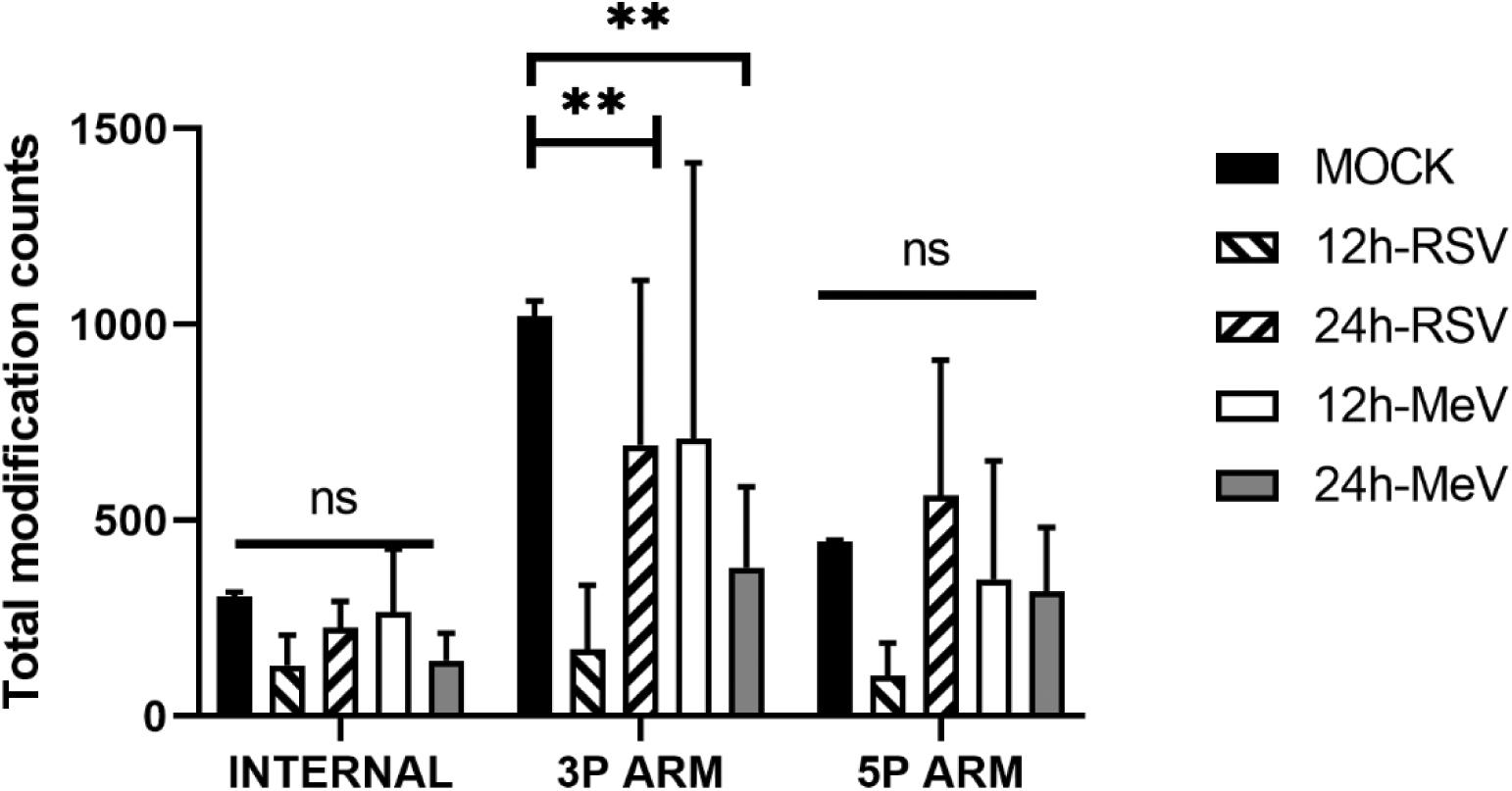
Figure 2. Raw miR reads from RSV- or MeV-infected SHS cells were analyzed for post-transcriptional modifications using Chimira (Vitsios and Enright, 2015). Total counts of internal, 3′ arm and 5′ arm modifications per sample type are shown. Differences in the number of modifications were analyzed by 2-way ANOVA with post hoc Dunnet’s test. p-values are indicated by ∗∗<0.01; ns, not significant. Error bars represent ± SD from three replicate measurements. 3p ARM, 3′ end of miRNA; 5P ARM, 5′ arm of miRNA.
RSV or MeV Infection Induces tRNA Fragments
Cellular stress triggers the degradation of tRNA to tRFs (Shen et al., 2018). tRFs may encompass the 5′, 3′, or internal anti-codon loop and are classified as 5′-, 3-, or class I tRFs (Shen et al., 2018). Functions of tRFs are poorly understood, but tRFs can perform as siRNAs degrading target transcripts (Maute et al., 2013), and regulate ribosomal loading and protein chain elongation (Sobala and Hutvagner, 2013). The biosynthesis of tRFs involves degradation of pre-tRNA molecules via the nuclear TRAMP pathway (Anderson, 2005; Maraia and Lamichhane, 2011) or cytosolic degradation of mature tRNAs via the rapid tRNA decay pathway. Analysis of the small RNA sequencing dataset in this study showed a differing abundance of tRFs following RSV or MeV infection. Analysis of tRFs showed that among the most abundant were 5′tRFs derived from tRNAs for glycine and valine (Figure 3), suggesting that tRNAs for these two amino acids were targeted during RSV and MeV infection. Levels of 5′tRFs for glycine and valine were substantially increased at 24 hpi following RSV or MeV infection. Frequencies of glycine and valine 5′tRFs increased with time, i.e., from 12 to 24 hpi in RSV- and MeV-infected SHS cells. Analysis of the anti-codon sequence for these tRFs showed that GCC, AAC, and CAC anticodons are enriched in 5′tRFs in SHS cells following RSV or MeV infection (Figure 4). A previous report showed that 5′tRF-Glu-CTC produced during RSV infection of A549 cells interacted with apolipoprotein E receptor 2 (APOER2) mRNA to inhibit translation of the gene, favoring RSV replication (Deng et al., 2015).
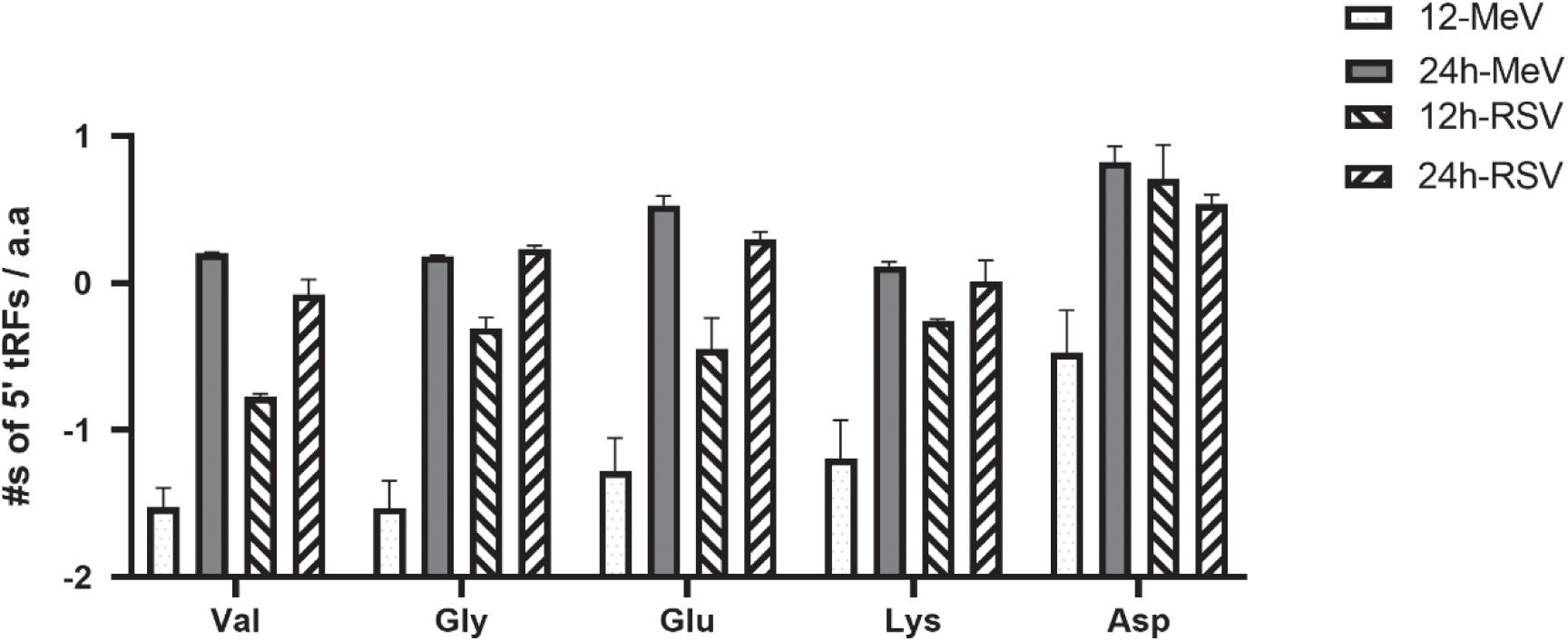
Figure 3. RSV- and MeV -infection influence tRF expression in SHS cells. Total counts for the principal 5′tRFs in MeV- or RSV- infected SHS cells are shown. Error bars represent ± SD from three replicate data. Val, valine; Gly, glycine; Glu, glutamate; Lys, lysine; Asp, aspartate.
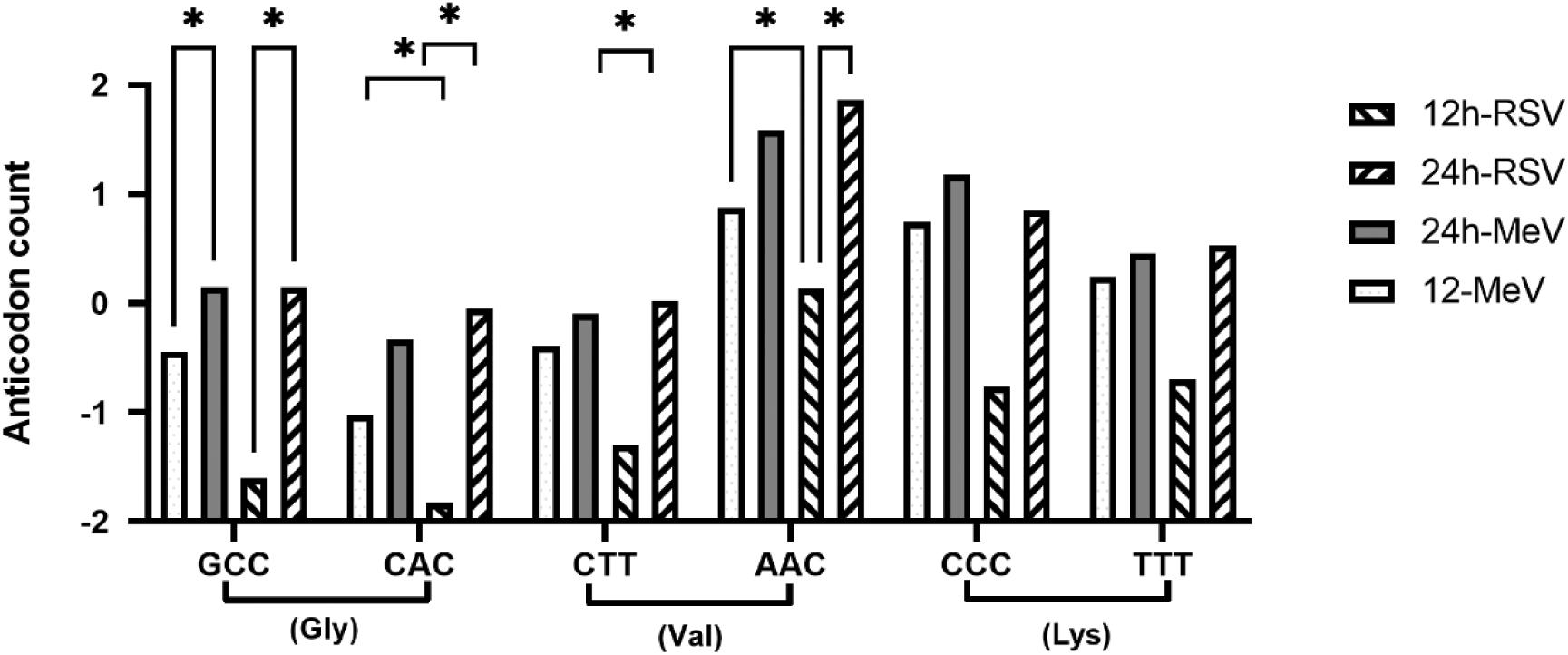
Figure 4. Anti-codons for foremost 5′tRFs during RSV- and MeV-infection. Anti-codon sequence for the top 5′tRFs deregulated in mock, RSV-, or MeV-infected SHS cells. Error bars represent ± SD from three replicate data. Comparisons were done using 2-way ANOVA with a mixed model (to account for outliers) and two replicates for mock followed by post hoc Tukey’s correction for multiple comparisons. ∗Indicate comparisons with significance p ≤ 0.05. Triplets on the x-axis indicate codon sequence.
We postulated that tRFs had a direct effect on translation and compared tRF profiles in RSV- or MeV-infected SHS cells with synonymous codon usage. Our analysis compared how frequently each codon in the RSV or MeV genome is utilized relative to the standard genetic code frequencies that are given as a codon adaptation index (CAI). CAI ranges from 0 to 1.0, with 0 representing least used, and 1.0 representing most common codons. A comparison of RSCU profiles for RSV and MeV genomes using Mega X (Kumar et al., 2018) showed the codon usage to be considerably different than standard human codon usage frequencies (Figures 5A,B). The assessment showed that of the four possible codons that encode glycine (GGU, GGC, GGA, GGG), three codons (GGC, GGU, GGG) are under-utilized for RSV genes, and valine, RSV uses the GUC codon less frequently. For MeV, two of the four codons for glycine (GGU, GGC) and GUA for valine are under-utilized. The consequence of these findings is unknown but suggests that the tRNAs used during RSV or MeV infection are selectively processed to produce these tRNAs potentially for two reasons—to reduce host translation (Kim et al., 2017, 2019; Mesitov et al., 2017), and/or to function as siRNAs and silence host genes (Emara et al., 2010; Wang et al., 2013; Kuscu et al., 2018; Jehn et al., 2020). For valine, and the increased abundance of valine 5′tRFs (AAC and CAC), the corresponding codon usage was not low suggesting that valine tRFs might have functions other than reducing translation rates. RSCU analysis of individual RSV and MeV genes showed that glycine and valine tRNAs were under-utilized following RSV or MeV infection in SHS cells (Table 3). Together these findings suggest that tRNA cleavage is linked with codon usage. The sncRNA results show that the expression profiles for small RNAs differ in kinetics of expression for RSV and MeV infection of SHS cells.
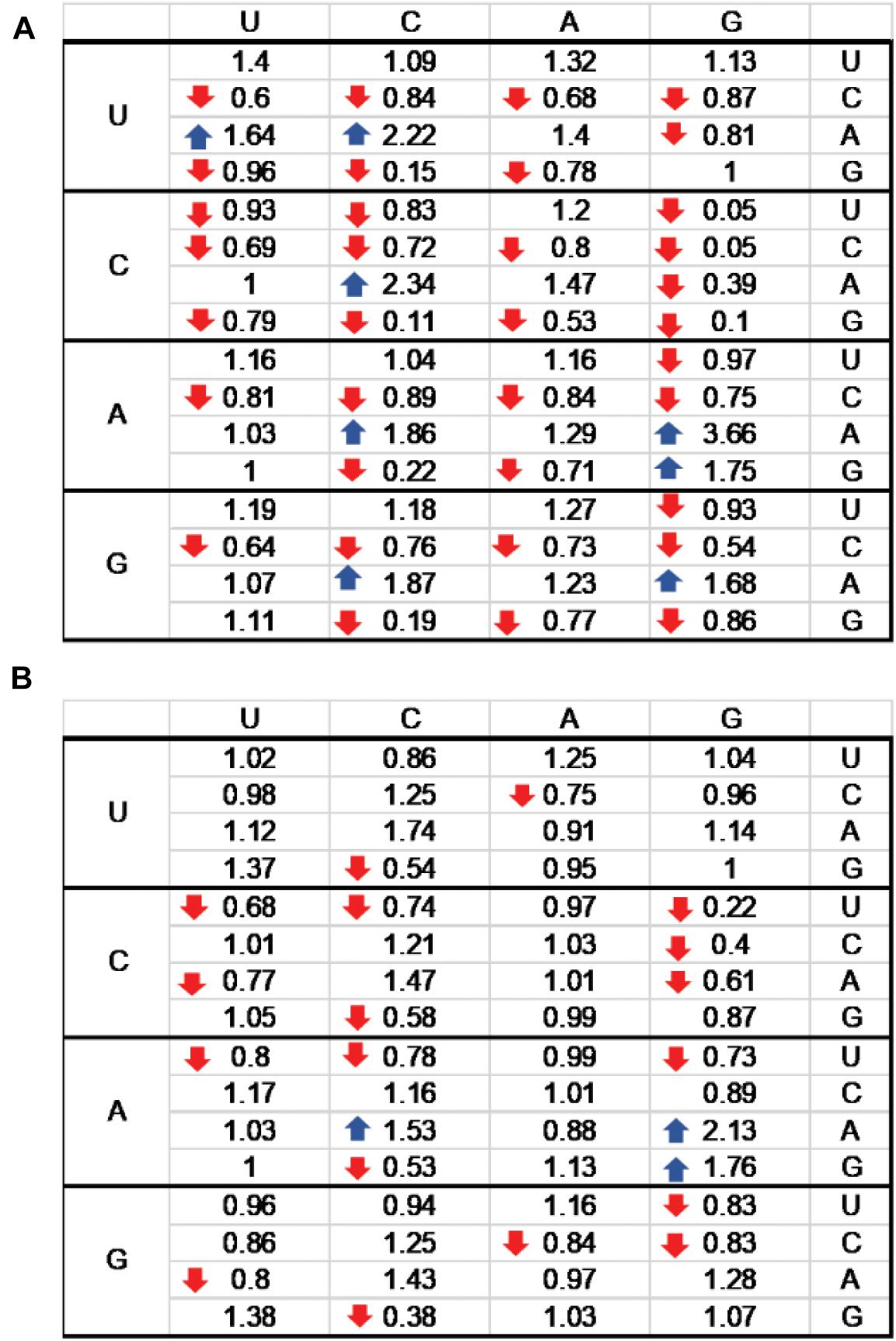
Figure 5. Relative synonymous codon usage (RSCU) index for RSV (A) and MeV (B) genomes. The standard genetic code table with RSCUs for RSV (A) and MeV (B) is shown. RSCU indices < 1.0 are indicated by downward arrow icons; RSCU indices > 1.5 are indicated by upward arrows. U, C, A, and G indicate uracil, cytosine, adenosine, and guanosine, respectively.
Discussion
In this study, we examined differentially expressed sncRNAs following RSV or MeV infection of SHS cells at 12 and 24 hpi using NGS. NGS showed unique miR expression profiles following RSV or MeV infection (Figure 1 and Table 2). We identified that (1) miR-10b-5p was expressed in mock-treated cells but showed reduced expression in RSV- or MeV-infected cells, (2) p-miR-247 and miR-375 had robust expression in RSV- or MeV-infected cells, (3) miRs had no/low expression in mock-treated cells, but were increased by RSV or MeV infection, and (4) miRs were not expressed in mock-infected cells at 12 hpi but showed robust copy numbers at 24 hpi. These findings show that RSV or MeV infection induces distinct miR expression in SHS cells that is virus-type and time-point specific. While the sequencing data from our study has identified these deregulated miRNAs, the mechanisms contributing to their biogenesis remains unknown and is out of the scope of this manuscript.
Evidence suggests that epitranscriptomics (or post-transcriptional modification of cellular RNAs) especially 3′ end uridylation and adenylation of miRs can alter both miRNA stability and target repertoire (Vitsios and Enright, 2015). We explored the nature of epitranscriptional miR modifications following RSV or MeV infection. The findings suggest that RSV and MeV induce sncRNA modifications affecting target cell specificity. The results showed extensive 3′ modifications (mostly uridylation and adenylation) in the miRs following RSV or MeV infection that may alter host mRNA or miRNA transcript stability. Further studies are needed to elucidate the function of these epitranscriptional modifications on miRNA function.
Post-transcriptional regulatory mechanisms control translation of >60% of the human transcriptome (Friedman et al., 2009). The identification of cleaved tRNAs during RSV or MeV infection of SHS cells is novel. The tRFs identified contained exclusively of 5′tRFs during later stages of RSV or MeV infection, and of these tRNAs, glycine, and valine were the primary targets for 5′tRF formation. Other studies showed that RSV infection can induce angiogenin (ANG)-mediated cleavage of tRNAs to produce tRFs (Deng et al., 2015; Zhou J. et al., 2017). These studies identified a pro-viral role for 5′tRF-GlyCCC, 5′tRF-LysCTT, and 5′tRF-GluCTC by depression of APOER2 mRNA. We postulate that tRNA cleavage to tRFs may have a broader anti-viral role. Degradation of host tRNAs may reduce the anti-viral protein response, and recent findings from proteomic studies in RSV-infected A549 cells have shown that the host nuclear proteins are considerably reduced following RSV infection (Munday et al., 2012, 2015). Similar results have also been shown for MeV, an attribute linked to the N protein (Sato et al., 2007; Okonski and Samuel, 2013). It is important to investigate why RSV or MeV infection induces selective cleavage of glycine and valine tRNAs as glycine, and valine tRNAs are selectively under-utilized by most RSV and MeV genes (Table 3). Transfer RNA fragments operate in mucosal immunity (Chen and Shen, 2021) regulating retrotransposon expression (Schorn et al., 2017) and viral adaptation to the host (Lauring et al., 2012; Pavon-Eternod et al., 2013; Rahman et al., 2018b; Le Nouën et al., 2020; Nunes et al., 2020).
The degradation of tRNAs may be a host stress response to viral infection, however, the increases in tRNA for glycine and valine hint that MeV and RSV may potentially target these tRNAs. The mechanisms that cause are unknown and are difficult to resolve in the context of this study. Currently, we do not understand the mechanisms involved in sncRNA deregulation, nor the functional outcome, thus further studies are necessary. Translation of mRNAs linked to the anti-viral response is key to control of virus infection and clearance. The findings show that RSV or MeV infection induces several classes of sncRNAs that regulate post-transcriptional gene expression and emphasizes the need to better understand the host-virus interface.
Data Availability Statement
The data presented in the study are deposited in Gene Expression Omnibus (GEO) with accession numbers GSE167724 and GSM5112024–GSM-5112037.
Author Contributions
AB contributed to conception, execution, and data analysis, and wrote manuscript drafts and revisions. CD contributed to execution. SC and RT contributed to study design, funding, data interpretation, manuscript writing, and review. HA contributed to validating infection using dark field fluorescence microscopy. All authors have seen the draft of the manuscript.
Funding
The studies were supported by a grant awarded to SC and RT (IE140652) to study “Paramyxovirus miRNA biogenesis and implications for host and viral gene expression” and the Georgia Research Alliance Foundation for RT.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to acknowledge the kind gift of rgRSV224GFP from Michael Teng at University of South Florida (USF).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmicb.2021.671852/full#supplementary-material
Supplementary Figure 1 | RSV infects SHS neuronal cells. SHS cells were infected with rgRSV-GFP at MOI = 0.1 for indicated time points. Viral replication was visualized by dark field fluorescence microscopy on a Nikon UV Eclipse TE2000-U microscope at 10X magnification.
Supplementary Table 1 | MiRNA modification data patterns in RSV and MeV infected neuronal cells. Table lists samples, microRNAs, type of modifications, modification site, pattern, modification position, internal modification type, internal modification position, repeat modifications and counts of modifications for all deregulated miRNAs identified in the study.
References
Advani, V. M., and Ivanov, P. (2019). Translational Control under Stress: Reshaping the Translatome. Bioessays 41:e1900009.
Alarcon, C. R., Lee, H., Goodarzi, H., Halberg, N., and Tavazoie, S. F. (2015). N6-methyladenosine marks primary microRNAs for processing. Nature 519, 482–485. doi: 10.1038/nature14281
Anderson, J. T. (2005). RNA turnover: unexpected consequences of being tailed. Curr. Biol. 15, R635–R638.
Bakre, A. A., Harcourt, J. L., Haynes, L. M., Anderson, L. J., and Tripp, R. A. (2017). The Central Conserved Region (CCR) of Respiratory Syncytial Virus (RSV) G Protein Modulates Host miRNA Expression and Alters the Cellular Response to Infection. Vaccines 5:16. doi: 10.3390/vaccines5030016
Bakre, A. A., Maleki, A., and Tripp, R. A. (2019). MicroRNA and Nonsense Transcripts as Putative Viral Evasion Mechanisms. Front. Cell Infect. Microbiol. 9:152. doi: 10.3389/fcimb.2019.00152
Bakre, A., Mitchell, P., Coleman, J. K., Jones, L. P., Saavedra, G., Teng, M., et al. (2012). Respiratory syncytial virus modifies microRNAs regulating host genes that affect virus replication. J. Gen. Virol. 93, 2346–2356. doi: 10.1099/vir.0.044255-0
Bakre, A., Wu, W., Hiscox, J., Spann, K., Teng, M. N., and Tripp, R. A. (2015). Human respiratory syncytial virus non-structural protein NS1 modifies miR-24 expression via transforming growth factor-beta. J. Gen. Virol. 96, 3179–3191. doi: 10.1099/jgv.0.000261
Bartel, D. P. (2009). MicroRNAs: Target Recognition and Regulatory Functions. Cell 136, 215–233. doi: 10.1016/j.cell.2009.01.002
Bergeron, H. C., Murray, J., Nunez Castrejon, A. M., Dubois, R. M., and Tripp, R. A. (2021). Respiratory Syncytial Virus (RSV) G Protein Vaccines With Central Conserved Domain Mutations Induce CX3C-CX3CR1 Blocking Antibodies. Viruses 13:352. doi: 10.3390/v13020352
Bernier, A., and Sagan, S. M. (2018). The Diverse Roles of microRNAs at the Host(-)Virus Interface. Viruses 10:440. doi: 10.3390/v10080440
Bohmwald, K., Galvez, N. M. S., Rios, M., and Kalergis, A. M. (2018). Neurologic Alterations Due to Respiratory Virus Infections. Front. Cell Neurosci. 12:386. doi: 10.3389/fncel.2018.00386
Briand, J., Sérandour, A. A., Nadaradjane, A., Bougras-Cartron, G., Heymann, D., Ory, B., et al. (2020). N6-Adenosine Methylation of miRNA-200b-3p Influences Its Functionality and Is a Theranostic Tool. Mol. Ther. Nucleic Acids 22, 72–83. doi: 10.1016/j.omtn.2020.08.010
Cakmak Genc, G., Dursun, A., Karakas Celik, S., Calik, M., Kokturk, F., and Piskin, I. E. (2018). IL28B, IL29 and micro-RNA 548 in subacute sclerosing panencephalitis as a rare disease. Gene 678, 73–78. doi: 10.1016/j.gene.2018.07.062
Chen, Y., and Shen, J. (2021). Mucosal immunity and tRNA, tRF, and tiRNA. J. Mol. Med. 99, 47–56. doi: 10.1007/s00109-020-02008-4
Cheray, M., Etcheverry, A., Jacques, C., Pacaud, R., Bougras-Cartron, G., Aubry, M., et al. (2020). Cytosine methylation of mature microRNAs inhibits their functions and is associated with poor prognosis in glioblastoma multiforme. Mol. Cancer 19:36.
Choi, Y., Mason, C. S., Jones, L. P., Crabtree, J., Jorquera, P. A., and Tripp, R. A. (2012). Antibodies to the central conserved region of respiratory syncytial virus (RSV) G protein block RSV G protein CX3C-CX3CR1 binding and cross-neutralize RSV A and B strains. Viral Immunol. 25, 193–203.
Correia De Sousa, M., Gjorgjieva, M., Dolicka, D., Sobolewski, C., and Foti, M. (2019). Deciphering miRNAs’ Action through miRNA Editing. Int. J. Mol. Sci. 20:6249. doi: 10.3390/ijms20246249
Cullen, B. R. (2013). MicroRNAs as mediators of viral evasion of the immune system. Nat. Immunol. 14, 205–210. doi: 10.1038/ni.2537
Dahiya, N., and Atreya, C. D. (2014). MicroRNAs and Major Blood-borne Infectious Viral Diseases. Microrna 2, 212–218. doi: 10.2174/2211536602666131118224225
Dakhama, A., Vitalis, T. Z., and Hegele, R. G. (1997). Persistence of respiratory syncytial virus (RSV) infection and development of RSV-specific IgG1 response in a guinea-pig model of acute bronchiolitis. Eur. Respir. J. 10, 20–26. doi: 10.1183/09031936.97.10010020
Deng, J., Ptashkin, R. N., Chen, Y., Cheng, Z., Liu, G., Phan, T., et al. (2015). Respiratory Syncytial Virus Utilizes a tRNA Fragment to Suppress Antiviral Responses Through a Novel Targeting Mechanism. Mol. Ther. 23, 1622–1629. doi: 10.1038/mt.2015.124
Eisenhut, M. (2006). Extrapulmonary manifestations of severe respiratory syncytial virus infection–a systematic review. Crit. Care 10:R107.
Emara, M. M., Ivanov, P., Hickman, T., Dawra, N., Tisdale, S., Kedersha, N., et al. (2010). Angiogenin-induced tRNA-derived stress-induced RNAs promote stress-induced stress granule assembly. J. Biol. Chem. 285, 10959–10968. doi: 10.1074/jbc.m109.077560
Ferren, M., Horvat, B., and Mathieu, C. (2019). Measles Encephalitis: Towards New Therapeutics. Viruses 11:1017. doi: 10.3390/v11111017
Friedman, R. C., Farh, K. K., Burge, C. B., and Bartel, D. P. (2009). Most mammalian mRNAs are conserved targets of microRNAs. Genome Res. 19, 92–105. doi: 10.1101/gr.082701.108
Ganesan, P., Chandwani, M. N., Creisher, P. S., Bohn, L., and O’donnell, L. A. (2018). The neonatal anti-viral response fails to control measles virus spread in neurons despite interferon-gamma expression and a Th1-like cytokine profile. J. Neuroimmunol. 316, 80–97. doi: 10.1016/j.jneuroim.2017.12.018
Grassmann, R., and Jeang, K. T. (2008). The roles of microRNAs in mammalian virus infection. Biochim. Biophys. Acta 1779, 706–711. doi: 10.1016/j.bbagrm.2008.05.005
Griffin, D. E., Lin, W. W., and Nelson, A. N. (2018). Understanding the causes and consequences of measles virus persistence. F1000Res 7:237. doi: 10.12688/f1000research.12094.1
Haber, N. (2018). Respiratory syncytial virus infection in elderly adults. Med. Mal. Infect. 48, 377–382. doi: 10.1016/j.medmal.2018.01.008
Hallak, L. K., Kwilas, S. A., and Peeples, M. E. (2007). Interaction between respiratory syncytial virus and glycosaminoglycans, including heparan sulfate. Methods Mol. Biol. 379, 15–34. doi: 10.1385/1-59745-393-5:15
Hallak, L. K., Spillmann, D., Collins, P. L., and Peeples, M. E. (2000). Glycosaminoglycan sulfation requirements for respiratory syncytial virus infection. J. Virol. 74, 10508–10513. doi: 10.1128/jvi.74.22.10508-10513.2000
Haralambieva, I. H., Kennedy, R. B., Simon, W. L., Goergen, K. M., Grill, D. E., Ovsyannikova, I. G., et al. (2018). Differential miRNA expression in B cells is associated with inter-individual differences in humoral immune response to measles vaccination. PLoS One 13:e0191812. doi: 10.1371/journal.pone.0191812
Harcourt, J. L., Karron, R. A., and Tripp, R. A. (2004). Anti-G protein antibody responses to respiratory syncytial virus infection or vaccination are associated with inhibition of G protein CX3C-CX3CR1 binding and leukocyte chemotaxis. J. Infect. Dis. 190, 1936–1940. doi: 10.1086/425516
Hardie, D. R., Albertyn, C., Heckmann, J. M., and Smuts, H. E. (2013). Molecular characterisation of virus in the brains of patients with measles inclusion body encephalitis (MIBE). Virol J. 10:283.
Hasegawa, K., Perez-Losada, M., Hoptay, C. E., Epstein, S., Mansbach, J. M., Teach, S. J., et al. (2018). RSV vs. rhinovirus bronchiolitis: difference in nasal airway microRNA profiles and NFkappaB signaling. Pediatr. Res. 83, 606–614. doi: 10.1038/pr.2017.309
Haynes, L. M., Jones, L. P., Barskey, A., Anderson, L. J., and Tripp, R. A. (2003). Enhanced disease and pulmonary eosinophilia associated with formalin-inactivated respiratory syncytial virus vaccination are linked to G glycoprotein CX3C-CX3CR1 interaction and expression of substance P. J. Virol. 77, 9831–9844. doi: 10.1128/jvi.77.18.9831-9844.2003
Inchley, C. S., Sonerud, T., Fjaerli, H. O., and Nakstad, B. (2015). Nasal mucosal microRNA expression in children with respiratory syncytial virus infection. BMC Infect. Dis. 15:150. doi: 10.1186/s12879-015-0878-z
Ivanov, P., Emara, M. M., Villen, J., Gygi, S. P., and Anderson, P. (2011). Angiogenin-induced tRNA fragments inhibit translation initiation. Mol. Cell 43, 613–623. doi: 10.1016/j.molcel.2011.06.022
Jehn, J., Treml, J., Wulsch, S., Ottum, B., Erb, V., Hewel, C., et al. (2020). 5’ tRNA halves are highly expressed in the primate hippocampus and might sequence-specifically regulate gene expression. RNA 26, 694–707. doi: 10.1261/rna.073395.119
Kanehisa, M., Furumichi, M., Tanabe, M., Sato, Y., and Morishima, K. (2017). KEGG: new perspectives on genomes, pathways, diseases and drugs. Nucleic Acids Res. 45, D353–D361.
Kanehisa, M., Sato, Y., Kawashima, M., Furumichi, M., and Tanabe, M. (2016). KEGG as a reference resource for gene and protein annotation. Nucleic Acids Res. 44, D457–D462.
Karagkouni, D., Paraskevopoulou, M. D., Chatzopoulos, S., Vlachos, I. S., Tastsoglou, S., Kanellos, I., et al. (2018). DIANA-TarBase v8: a decade-long collection of experimentally supported miRNA-gene interactions. Nucleic Acids Res. 46, D239–D245.
Kim, H. K., Fuchs, G., Wang, S., Wei, W., Zhang, Y., Park, H., et al. (2017). A transfer-RNA-derived small RNA regulates ribosome biogenesis. Nature 552, 57–62. doi: 10.1038/nature25005
Kim, H. K., Xu, J., Chu, K., Park, H., Jang, H., Li, P., et al. (2019). A tRNA-Derived Small RNA Regulates Ribosomal Protein S28 Protein Levels after Translation Initiation in Humans and Mice. Cell Rep. 29, 3816.e–3824.e.
King, K. A., Hu, C., Rodriguez, M. M., Romaguera, R., Jiang, X., and Piedimonte, G. (2001). Exaggerated neurogenic inflammation and substance P receptor upregulation in RSV-infected weanling rats. Am. J. Respir. Cell Mol. Biol. 24, 101–107. doi: 10.1165/ajrcmb.24.2.4264
Kumar, S., Stecher, G., Li, M., Knyaz, C., and Tamura, K. (2018). MEGA X: Molecular Evolutionary Genetics Analysis across Computing Platforms. Mol. Biol. Evol. 35, 1547–1549. doi: 10.1093/molbev/msy096
Kuscu, C., Kumar, P., Kiran, M., Su, Z., Malik, A., and Dutta, A. (2018). tRNA fragments (tRFs) guide Ago to regulate gene expression post-transcriptionally in a Dicer-independent manner. RNA 24, 1093–1105. doi: 10.1261/rna.066126.118
Lauring, A. S., Acevedo, A., Cooper, S. B., and Andino, R. (2012). Codon usage determines the mutational robustness, evolutionary capacity, and virulence of an RNA virus. Cell Host Microbe 12, 623–632. doi: 10.1016/j.chom.2012.10.008
Lay, M. K., Bueno, S. M., Galvez, N., Riedel, C. A., and Kalergis, A. M. (2016). New insights on the viral and host factors contributing to the airway pathogenesis caused by the respiratory syncytial virus. Crit. Rev. Microbiol. 42, 800–812.
Le Nouën, C., Luongo, C. L., Yang, L., Mueller, S., Wimmer, E., Dinapoli, J. M., et al. (2020). Optimization of the Codon Pair Usage of Human Respiratory Syncytial Virus Paradoxically Resulted in Reduced Viral Replication In Vivo and Reduced Immunogenicity. J. Virol. 94, e1296–e1219.
Leung, A. K., Hon, K. L., Leong, K. F., and Sergi, C. M. (2018). Measles: a disease often forgotten but not gone. Hong Kong Med. J. 24, 512–520.
Li, X. Q., Fu, Z. F., Alvarez, R., Henderson, C., and Tripp, R. A. (2006). Respiratory syncytial virus (RSV) infects neuronal cells and processes that innervate the lung by a process involving RSV G protein. J. Virol. 80, 537–540. doi: 10.1128/jvi.80.1.537-540.2006
Lin, L. T., and Richardson, C. D. (2016). The Host Cell Receptors for Measles Virus and Their Interaction with the Viral Hemagglutinin (H) Protein. Viruses 8:250. doi: 10.3390/v8090250
Long, X., Xie, J., Zhao, K., Li, W., Tang, W., Chen, S., et al. (2016). NK cells contribute to persistent airway inflammation and AHR during the later stage of RSV infection in mice. Med. Microbiol. Immunol. 205, 459–470. doi: 10.1007/s00430-016-0459-9
Love, M. I., Huber, W., and Anders, S. (2014). Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15:550.
Maraia, R. J., and Lamichhane, T. N. (2011). 3’ processing of eukaryotic precursor tRNAs. Wiley Interdiscip. Rev. RNA 2, 362–375. doi: 10.1002/wrna.64
Maute, R. L., Schneider, C., Sumazin, P., Holmes, A., Califano, A., Basso, K., et al. (2013). tRNA-derived microRNA modulates proliferation and the DNA damage response and is down-regulated in B cell lymphoma. Proc. Natl. Acad. Sci. U S A. 110, 1404–1409. doi: 10.1073/pnas.1206761110
Mazur, N. I., Higgins, D., Nunes, M. C., Melero, J. A., Langedijk, A. C., Horsley, N., et al. (2018). The respiratory syncytial virus vaccine landscape: lessons from the graveyard and promising candidates. Lancet Infect. Dis. 18, e295–e311.
McQuaid, S., Cosby, S. L., Koffi, K., Honde, M., Kirk, J., and Lucas, S. B. (1998). Distribution of measles virus in the central nervous system of HIV-seropositive children. Acta Neuropathol. 96, 637–642. doi: 10.1007/s004010050945
Mesitov, M. V., Soldatov, R. A., Zaichenko, D. M., Malakho, S. G., Klementyeva, T. S., Sokolovskaya, A. A., et al. (2017). Differential processing of small RNAs during endoplasmic reticulum stress. Sci. Rep. 7:46080.
Mirra, V., Ullmann, N., Cherchi, C., Onofri, A., Paglietti, M. G., and Cutrera, R. (2018). Respiratory syncytial virus prophylaxis and the “special population”. Minerva Pediatr. 70, 589–599.
Mishra, B., and Wang, G. (2012). The Importance of Amino Acid Composition in Natural AMPs: An Evolutional, Structural, and Functional Perspective. Front. Immunol. 3:221. doi: 10.3389/fimmu.2012.00221
Morichi, S., Morishita, N., Ishida, Y., Oana, S., Yamanaka, G., Kashiwagi, Y., et al. (2017). Examination of neurological prognostic markers in patients with respiratory syncytial virus-associated encephalopathy. Int. J. Neurosci. 127, 44–50. doi: 10.3109/00207454.2016.1138951
Munday, D. C., Howell, G., Barr, J. N., and Hiscox, J. A. (2015). Proteomic analysis of mitochondria in respiratory epithelial cells infected with human respiratory syncytial virus and functional implications for virus and cell biology. J. Pharm. Pharmacol. 67, 300–318.
Munday, D. C., Surtees, R., Emmott, E., Dove, B. K., Digard, P., Barr, J. N., et al. (2012). Using SILAC and quantitative proteomics to investigate the interactions between viral and host proteomes. Proteomics 12, 666–672. doi: 10.1002/pmic.201100488
Naaman, H., Rall, G., Matullo, C., Veksler-Lublinsky, I., Shemer-Avni, Y., and Gopas, J. (2017). MiRNA-124 is a link between measles virus persistent infection and cell division of human neuroblastoma cells. PLoS One 12:e0187077. doi: 10.1371/journal.pone.0187077
Nunes, A., Ribeiro, D. R., Marques, M., Santos, M. A. S., Ribeiro, D., and Soares, A. R. (2020). Emerging Roles of tRNAs in RNA Virus Infections. Trends Biochem. Sci. 45, 794–805. doi: 10.1016/j.tibs.2020.05.007
Okonski, K. M., and Samuel, C. E. (2013). Stress granule formation induced by measles virus is protein kinase PKR dependent and impaired by RNA adenosine deaminase ADAR1. J. Virol. 87, 756–766. doi: 10.1128/jvi.02270-12
Omar, S., Clarke, R., Abdullah, H., Brady, C., Corry, J., Winter, H., et al. (2017). Respiratory virus infection up-regulates TRPV1, TRPA1 and ASICS3 receptors on airway cells. PLoS One 12:e0171681. doi: 10.1371/journal.pone.0171681
Oshansky, C. M., Krunkosky, T. M., Barber, J., Jones, L. P., and Tripp, R. A. (2009). Respiratory syncytial virus proteins modulate suppressors of cytokine signaling 1 and 3 and the type I interferon response to infection by a toll-like receptor pathway. Viral Immunol. 22, 147–161. doi: 10.1089/vim.2008.0098
Paes, B. (2018). Respiratory Syncytial Virus in Otherwise Healthy Prematurely Born Infants: A Forgotten Majority. Am. J. Perinatol. 35, 541–544. doi: 10.1055/s-0038-1637762
Pavon-Eternod, M., David, A., Dittmar, K., Berglund, P., Pan, T., Bennink, J. R., et al. (2013). Vaccinia and influenza A viruses select rather than adjust tRNAs to optimize translation. Nucleic Acids Res. 41, 1914–1921. doi: 10.1093/nar/gks986
Petrov, A. I., Kay, S. J. E., Kalvari, I., Howe, K. L., Gray, K. A., Bruford, E. A., et al. (2017). RNAcentral: a comprehensive database of non-coding RNA sequences. Nucleic Acids Res. 45, D128–D134.
Pirouz, M., Ebrahimi, A. G., and Gregory, R. I. (2019). Unraveling 3’-end RNA uridylation at nucleotide resolution. Methods 155, 10–19. doi: 10.1016/j.ymeth.2018.10.024
Rahman, R.-U., Gautam, A., Bethune, J., Sattar, A., Fiosins, M., Magruder, D. S., et al. (2018a). Oasis 2: improved online analysis of small RNA-seq data. BMC Bioinformatics 19:54. doi: 10.1186/s12859-018-2047-z
Rahman, S. U., Yao, X., Li, X., Chen, D., and Tao, S. (2018b). Analysis of codon usage bias of Crimean-Congo hemorrhagic fever virus and its adaptation to hosts. Infect. Genet. Evol. 58, 1–16. doi: 10.1016/j.meegid.2017.11.027
Riddell, M. A., Moss, W. J., Hauer, D., Monze, M., and Griffin, D. E. (2007). Slow clearance of measles virus RNA after acute infection. J. Clin. Virol. 39, 312–317. doi: 10.1016/j.jcv.2007.05.006
Rima, B. K., and Duprex, W. P. (2005). Molecular mechanisms of measles virus persistence. Virus Res. 111, 132–147. doi: 10.1016/j.virusres.2005.04.005
Roizman, B., Zhou, G., and Du, T. (2011). Checkpoints in productive and latent infections with herpes simplex virus 1: conceptualization of the issues. J. Neurovirol. 17, 512–517. doi: 10.1007/s13365-011-0058-x
Rota, P. A., Rota, J. S., and Goodson, J. L. (2017). Subacute Sclerosing Panencephalitis. Clin. Infect. Dis. 65, 233–234.
Russell, C. J., Simoes, E. A. F., and Hurwitz, J. L. (2018). Vaccines for the Paramyxoviruses and Pneumoviruses: Successes, Candidates, and Hurdles. Viral Immunol. 31, 133–141. doi: 10.1089/vim.2017.0137
Sato, H., Masuda, M., Kanai, M., Tsukiyama-Kohara, K., Yoneda, M., and Kai, C. (2007). Measles virus N protein inhibits host translation by binding to eIF3-p40. J. Virol. 81, 11569–11576. doi: 10.1128/jvi.00570-07
Sato, Y., Watanabe, S., Fukuda, Y., Hashiguchi, T., Yanagi, Y., and Ohno, S. (2018). Cell-to-Cell Measles Virus Spread between Human Neurons Is Dependent on Hemagglutinin and Hyperfusogenic Fusion Protein. J. Virol. 92, e2166–e2117.
Schorn, A. J., Gutbrod, M. J., Leblanc, C., and Martienssen, R. (2017). LTR-Retrotransposon Control by tRNA-Derived Small RNAs. Cell 170, 61.e–71.e.
Schwarze, J., O’donnell, D. R., Rohwedder, A., and Openshaw, P. J. (2004). Latency and persistence of respiratory syncytial virus despite T cell immunity. Am. J. Respir. Crit. Care Med. 169, 801–805. doi: 10.1164/rccm.200308-1203oc
Shen, Y., Yu, X., Zhu, L., Li, T., Yan, Z., and Guo, J. (2018). Transfer RNA-derived fragments and tRNA halves: biogenesis, biological functions and their roles in diseases. J. Mol. Med. 96, 1167–1176. doi: 10.1007/s00109-018-1693-y
Singh, B. K., Li, N., Mark, A. C., Mateo, M., Cattaneo, R., and Sinn, P. L. (2016). Cell-to-Cell Contact and Nectin-4 Govern Spread of Measles Virus from Primary Human Myeloid Cells to Primary Human Airway Epithelial Cells. J. Virol. 90, 6808–6817.
Sobala, A., and Hutvagner, G. (2013). Small RNAs derived from the 5’ end of tRNA can inhibit protein translation in human cells. RNA Biol. 10, 553–563. doi: 10.4161/rna.24285
Sofos, N., Xu, K., Dedic, E., and Brodersen, D. E. (2015). Cut to the chase–Regulating translation through RNA cleavage. Biochimie 114, 10–17. doi: 10.1016/j.biochi.2015.01.009
Tan, Y. R., Yang, T., Liu, S. P., Xiang, Y., Qu, F., Liu, H. J., et al. (2008). Pulmonary peptidergic innervation remodeling and development of airway hyperresponsiveness induced by RSV persistent infection. Peptides 29, 47–56. doi: 10.1016/j.peptides.2007.10.020
Taniguchi, M., Yanagi, Y., and Ohno, S. (2019). Both type I and type III interferons are required to restrict measles virus growth in lung epithelial cells. Arch. Virol. 164, 439–446. doi: 10.1007/s00705-018-4087-0
Tatsuo, H., Ono, N., Tanaka, K., and Yanagi, Y. (2000). SLAM (CDw150) is a cellular receptor for measles virus. Nature 406, 893–897. doi: 10.1038/35022579
Techaarpornkul, S., Collins, P. L., and Peeples, M. E. (2002). Respiratory syncytial virus with the fusion protein as its only viral glycoprotein is less dependent on cellular glycosaminoglycans for attachment than complete virus. Virology 294, 296–304. doi: 10.1006/viro.2001.1340
Tripp, R. A., Barskey, A., Goss, L., and Anderson, L. J. (2002). Substance P receptor expression on lymphocytes is associated with the immune response to respiratory syncytial virus infection. J. Neuroimmunol. 129, 141–153. doi: 10.1016/s0165-5728(02)00169-8
Tripp, R. A., Dakhama, A., Jones, L. P., Barskey, A., Gelfand, E. W., and Anderson, L. J. (2003). The G glycoprotein of respiratory syncytial virus depresses respiratory rates through the CX3C motif and substance P. J. Virol. 77, 6580–6584. doi: 10.1128/jvi.77.11.6580-6584.2003
Tripp, R. A., Jones, L. P., Haynes, L. M., Zheng, H., Murphy, P. M., and Anderson, L. J. (2001). CX3C chemokine mimicry by respiratory syncytial virus G glycoprotein. Nat. Immunol. 2, 732–738. doi: 10.1038/90675
Tripp, R. A., Moore, D., Winter, J., and Anderson, L. J. (2000). Respiratory syncytial virus infection and G and/or SH protein expression contribute to substance P, which mediates inflammation and enhanced pulmonary disease in BALB/c mice. J. Virol. 74, 1614–1622. doi: 10.1128/jvi.74.4.1614-1622.2000
Vitsios, D. M., and Enright, A. J. (2015). Chimira: analysis of small RNA sequencing data and microRNA modifications. Bioinformatics 31, 3365–3367. doi: 10.1093/bioinformatics/btv380
Vlachos, I. S., Zagganas, K., Paraskevopoulou, M. D., Georgakilas, G., Karagkouni, D., Vergoulis, T., et al. (2015). DIANA-miRPath v3.0: deciphering microRNA function with experimental support. Nucleic Acids Res. 43, W460–W466.
Wang, J. X., Gao, J., Ding, S. L., Wang, K., Jiao, J. Q., Wang, Y., et al. (2015). Oxidative Modification of miR-184 Enables It to Target Bcl-xL and Bcl-w. Mol. Cell 59, 50–61. doi: 10.1016/j.molcel.2015.05.003
Wang, Q., Lee, I., Ren, J., Ajay, S. S., Lee, Y. S., and Bao, X. (2013). Identification and functional characterization of tRNA-derived RNA fragments (tRFs) in respiratory syncytial virus infection. Mol. Ther. 21, 368–379. doi: 10.1038/mt.2012.237
Wang, S., Liu, P., Yang, P., Zheng, J., and Zhao, D. (2017). Peripheral blood microRNAs expression is associated with infant respiratory syncytial virus infection. Oncotarget 8, 96627–96635. doi: 10.18632/oncotarget.19364
Yis, U., Tufekci, U. K., Genc, S., Carman, K. B., Bayram, E., Topcu, Y., et al. (2015). Expression patterns of micro-RNAs 146a, 181a, and 155 in subacute sclerosing panencephalitis. J. Child Neurol. 30, 69–74. doi: 10.1177/0883073814531329
Zhong, Q., Feng, H., Lu, Q., Liu, X., Zhao, Q., Du, Y., et al. (2018). Recurrent wheezing in neonatal pneumonia is associated with combined infection with Respiratory Syncytial Virus and Staphylococcus aureus or Klebsiella pneumoniae. Sci. Rep. 8:995.
Zhou, J., Liu, S., Chen, Y., Fu, Y., Silver, A. J., Hill, M. S., et al. (2017). Identification of two novel functional tRNA-derived fragments induced in response to respiratory syncytial virus infection. J. Gen. Virol. 98, 1600–1610. doi: 10.1099/jgv.0.000852
Keywords: respiratory syncytial virus, measles virus, neuronal cells, microRNAs, piwi-associated RNAs, transfer RNAs
Citation: Bakre AA, Duffy C, Abdullah H, Cosby SL and Tripp RA (2021) Small Non-coding RNA Expression Following Respiratory Syncytial Virus or Measles Virus Infection of Neuronal Cells. Front. Microbiol. 12:671852. doi: 10.3389/fmicb.2021.671852
Received: 24 February 2021; Accepted: 03 August 2021;
Published: 03 September 2021.
Edited by:
Jianrong Li, The Ohio State University, United StatesReviewed by:
Qiyun Zhu, Lanzhou Veterinary Research Institute, Chinese Academy of Agricultural Sciences (CAS), ChinaMark Peeples, The Ohio State University, United States
Copyright © 2021 Bakre, Duffy, Abdullah, Cosby and Tripp. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abhijeet A. Bakre, YmFrcmVAdWdhLmVkdQ==; Ralph A. Tripp, cmF0cmlwcEB1Z2EuZWR1
 Abhijeet A. Bakre
Abhijeet A. Bakre Catherine Duffy2
Catherine Duffy2 S. Louise Cosby
S. Louise Cosby Ralph A. Tripp
Ralph A. Tripp