- 1Department of Gynecology, Liaoning Cancer Hospital and Institute, Cancer Hospital of China Medical University, Shenyang, China
- 2Department of Obstetrics and Gynecology, Shengjing Hospital of China Medical University, Shenyang, China
- 3Department of Neurosurgery, Liaoning Cancer Hospital and Institute, Cancer Hospital of China Medical University, Shenyang, China
Cervical cancer is the most common gynecological malignancy and screening for risk factors with early detection has been shown to reduce the mortality. In this study, we aimed to analyze the characteristics and risk factors of human papillomavirus (HPV) infection and precancerous lesions in women and provide clinical evidence for developing strategies to prevent cervical precancerous lesions and cancer in women. Furthermore, we evaluated the influencing factors for high-risk HPV infection. From April 2018 to December 2021, 10,628 women were recruited for cervical cancer screening at Liaoning Cancer Hospital, Shenyang Sujiatun District Women’s and Infants Hospital, Benxi Manchu Autonomous County People’s Hospital, and Shandong Affiliated Hospital of Qingdao University. The study participants were tested to determine if they were HPV-positive (HPV +) or underwent thinprep cytology test (TCT) for atypical squamous cells of undetermined significance (ASCUS) and above. Furthermore, colposcopies and biopsies were performed for the histopathological examination. Finally, 9991 cases were included in the statistical analysis, and the factors influencing HPV infection and those related to cervical cancer and precancerous lesions were analyzed. HPV + infection, high-grade squamous intraepithelial lesion-positive (CINII +) in cervical high-grade intraepithelial neoplasia, and early cervical cancer diagnosis rates were 12.45, 1.09, and 95.41%, respectively. The potential risk factors for HPV were education ≤ high school [odds ratio (OR) = 1.279 (1.129–1.449), P < 0.001], age at initial sexual activity ≤ 19 years [OR = 1.517 (1.080–2.129), P = 0.016], sexual partners > 1 [OR = 1.310 (1.044–1.644), P = 0.020], ASCUS and above [OR = 11.891 (10.105–13.993), P < 0.001], non-condom contraception [OR = 1.255 (1.059–1.487), P = 0.009], and HSIL and above [OR = 1.541 (1.430–1.662), P < 0.001]. Compared with women aged 56–65 and 35–45 years [OR = 0.810 (0.690–0.950), P = 0.010] the HPV infection rate was significantly lower in those aged 46–55 years [OR = 0.79 (0.683–0.915), P = 0.002]. Furthermore, ≤ high school age [OR = 1.577 (1.042–2.387), P = 0.031], not breastfeeding [OR = 1.763 (1.109–2.804), P = 0.017], ASCUS and above [OR = 42.396 (28.042–64.098), P < 0.001] were potential risk factors for cervical cancer and precancerous lesions. In women with HPV infection, ≤ high school education level, initial sexual activity at ≤ 19 years of age, number of sexual partners > 1, ASCUS and above, non-condom contraception, HSIL and above were risk factors for HPV infection. Compared with women aged 56–65 years, those aged 35–45 and 46–55 years had significantly lower HPV infection rates, and high school age and below, non-breastfeeding, and ASCUS and above were all potential risk factors for cervical cancer and precancerous lesions.
Introduction
Cervical cancer is the most common gynecological malignancy and in 2020, with 604,000 new cases worldwide, with approximately 342,000 related deaths (Sung et al., 2021). Cervical cancer has become the most common cancer in 23 countries and the leading cause of cancer-related deaths in 36 countries. The incidence rate of the disease in developing countries is significantly different from that in developed countries (Bray et al., 2018), with the highest occurring in sub Saharan Africa, South Polynesia, South America, and Southeast Asia (Sung et al., 2021). Inadequate living conditions and resources in developing regions, such as a lack of access to physical contraceptives and poor living and personal hygiene conditions, are considered factors that increase the burden of cervical cancer (Abulizi et al., 2017).
In contrast, developed countries have high coverage and availability of cancer screening and compliance by the target population (Thanapprapasr et al., 2012). The incidence of cervical cancer in China is not encouraging and the International Agency for Research on Cancer (IARC) reported 109,741 new cases in 2020. Furthermore, 59,060 patients died (Cao et al., 2021), accounting for 18.2 and 17.3% (Bray et al., 2018) of the cervical cancer incidence and death rate worldwide, respectively. According to the 2020 annual work report of the National Cancer Center, cervical cancer still has the sixth highest incidence of female cancers in China, and the mortality rate is still the eighth highest among female malignant tumors (Bray et al., 2018).
The incidence rate of cervical cancer at a younger age is showing an increasing trend (Zheng et al., 2019). Furthermore, cervical lesions are the most common diseases in women of childbearing age, and mainly include inflammation, injury, deformity, precancerous lesions, and tumors. Cervical cancer is usually caused by human papillomavirus (HPV) infection. HPV is a spherical DNA virus, which can cause proliferation of human skin mucosal squamous epithelium, and further reproduction may lead to various cervical diseases (McLaughlin-Drubin and Munger, 2008).
The German scholar Hausen first identified HPV infection as the main pathogenic factor of cervical cancer and precancerous lesions, which could be considered a milestone discovery in the prevention and treatment of this disease (Peter et al., 2010). A considerable amount of epidemiological and biological data have also proved that HPV infection is the main cause of cervical cancer and cervical intraepithelial neoplasia (Cordeiro et al., 2018). However, the HPV infection rate varies between regions because it is affected by numerous factors such as region, race, living habits, and HPV vaccination rate. Worldwide, economically developed regions such as South Korea, reported 18,170 women with HPV infection in 2014–2016, including 2,268 (12.5%) who were high-risk HPV positive (HPV +) (Ouh et al., 2018).
HPV E6/E7 mRNA detection is a new cervical cancer screening technology emerging in recent years. It is a screening method with E6/E7 as the detection target. Whether it has advantages in cervical cancer screening remains to be studied. The sensitivity of hpve6/E7 mRNA detection was lower than that of HR—HPV DNA detection, but the missed detection rate of hpve6/E7 mRNA detection was significantly lower than that of TCT and HR—HPV DNA detection (P < 0.05) (Giorgi Rossi et al., 2022).
The study of HPV prevalence and its subtype distribution may provide relevant information for routine vaccination and the types of HPV strains used in vaccination. HPV infection rates among women worldwide range from 11.70 to 7.20% (Lewandowska et al., 2021). The highest prevalence rates have been reported in Sub Saharan Africa (24.00%), Latin America and the Caribbean (16.10%), Eastern Europe (14.20%), and South East Asia (14.00%) (Bekmukhambetov et al., 2016). A study in the economically underdeveloped regions of West Africa showed that the high-risk HPV infection rate of 28.6% (Maria et al., 2018), whereas the overall HPV prevalence rate in Kazakhstan was reported to be as high as 43.8–55.8% (Aimagambetova and Azizan, 2018).
In China, significant differences were also reported in HPV infection rates in different regions, ranging from 13 to 31.9% (Zhong et al., 2017; Jiang et al., 2019). HPV also plays a vital role in the development of cervical lesions and cervical cancer, and the World Health Organization has confirmed that the mortality rate can effectively be reduced by screening. This study analyzed the characteristics and high-risk factors of HPV infection, cervical cancer, and high-grade precancerous lesions in a large-scale population screened for cervical cancer, to provide a reference for the prevention and treatment of these conditions.
Patients and Methods
Ethics Statement
This study was approved by the Ethics Committee of Liaoning Cancer Hospital and informed consent was obtain from all individual participants included in the study (No.: 20180106).
Research Participants
From April 2018 to December 2021, we recruited 10,628 women for cervical cancer screening in Liaoning Province at Liaoning Cancer Hospital, Shenyang Sujiatun District Women’s and Infant Hospital, Benxi Manchu Autonomous County People’s Hospital, and Shandong Affiliated Hospital of Qingdao University. The average and median ages of the selected research participants were 49.61 ± 7.195 years, and 49 years, respectively.
Methods
All women in the study underwent HPV testing and the thinprep cytology test (TCT). Community population and hospital outpatient opportunistic screenings were used to evaluate whether participants met the following inclusion criteria: (1) lived in Liaoning for > 3 years; (2) a history of sexual activity; (3) no sexual activity, vaginal medication, or drug flushing within 1 week before examination; (4) no serious organ dysfunction or mental illness; (5) voluntary participation and signed consent; and 5) willingness to complete the questionnaire survey. The exclusion criteria were: (1) women who were pregnant, lactating, or menstruating; (2) history of cervical surgery or hysterectomy; and (3) diagnosed with a tumor and being treated for other serious internal and external diseases. This study was approved by the ethics committee of Liaoning Cancer Hospital.
Sample Collection
Liquid-Based Cytology
TCT (Thinprep cytologic test purchased from Nanjing Xinbaishi Technology Co., Ltd.). The examination application forms of each patient was filled and their name and age and collection date was placed on the specimen bottle (liquid-based cytology preservation solution vial). The completely filled application form was checked to ensure the information was consistent with that on the preservation solution vial. The cervical brush was then placed in the preservation solution and rinsed by plunging it up and down 20 times, while spreading and rotating the bristles back and forth to make the cells fall into the solution.
Finally, the cervical brush was rapidly rotated to release the collected cells into the preservation solution, the sampler was discarded ensuring the brush head was not left in the bottle, and then it was sent to the pathology department for liquid-based analysis. The operating procedures of the system for the TCT, which is a liquid-based cytology production process, includes the following three steps, which were strictly adhered to: cell mixing, collection, and transfer. Briefly, the sample was placed into 95% alcohol for wet fixation, the production was completed, and then the next staining and diagnosis step was performed. The negative slides should be stored for 1 year, whereas the positive slides should be stored for a long time. Finally, the diagnosis was made by a full-time cytological diagnosis doctor in the pathology department.
Human Papillomavirus Detection Technology
The detection kit was purchased from Beijing Haolejie Healthcare Medical Equipment Company (Beijing). The E6/E7 mRNA detection kit was used to detect the following 14 high-risk HPV mRNAs known to cause cervical cancer (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68), and displayed the detection results of 16 and 18 to provide more clinical guidance information. The kit detects E6 and E7 mRNA of high-risk HPV to avoid missing the detection of high-level lesions and cancer, which could result from only detecting the L1 region. Furthermore, no cross reaction occurred with low-risk HPV and there were fewer false positives, which reduced unnecessary colposcopies and over diagnosis.
Questionnaire and Survey
The questionnaire used in this study adopts the principle of voluntariness and was designed professionally by the members of our research group. The questionnaire includes questions on the participants’ personal information; relevant medical, reproductive, sexual activity, smoking, contraceptive, and sports history; educational level; and economic income.
Standard of Referral Colposcopy
Cervical exfoliative cells were examined using cervical liquid-based thinprep cytology test (TCT). The diagnostic criteria are based on the Bethesda system (TBS) classification: atypical squamous cells of undetermined significance (ASCUS) without clear diagnostic significance, excluding ACS-cannot exclude high-grade squamous intraepithelial lesion (ASC-H), low-grade squamous intraepithelial lesion (LSIL), high-grade squamous epithelial lesion (HSIL), squamous cell carcinoma (SCC), and atypical glandular epithelial cells (AGCs) (Nayar and Wilbur, 2015).
For HPV+, TBS classified ASCUS or above, or both, or clinically suspicious abnormalities, a colposcopy is further recommended. The examination results suggested the need for a multipoint tissue biopsy of cervical lesions and bite the tissue for pathological examination. The pathological results were the gold standard, and the diagnostic criteria included normal or inflammatory reaction and cervical intraepithelial neoplasia-intraepithelial neoplasia (CIN) and cervical cancer. CIN is divided into CIN I, CIN II, and CIN III (Kclurman et al., 2014) according to the following three levels: light, medium, and heavy, respectively.
Technical Quality Control
The quality control evaluation of the cervical exfoliative cell examination was conducted using 20 and 5–10% of the randomly selected positive and negative smears, respectively. All smears were reviewed by experts in the field and the acceptable quality rate of the smear results was 80%. The quality control of the colposcopy examination involved a spot check of 10 and 20% of the normal and abnormal reports, respectively. The results were rechecked by experts in the field and the standard quality rate of the reported results was expected to reach 90%. The quality control of the histopathological examination was performed by spot checking 10% of the pathological sections and the results were recheck by experts. The coincidence rate of diagnostic results was expected to reach 90%.
Statistical Analysis
The statistical analysis of the relevant data was conducted using the statistical package for the social science (SPSS) version 19.0 software and the count data rate (%) was analyzed using the chi-square (χ2) test. The influencing factors were analyzed using univariate and multivariate logistic regression to evaluate the correlation between the relevant factors mentioned in the questionnaire and HPV infection, cervical cancer, and precancerous lesions.
Results
Characteristics of the Participants
Basic Information of Population
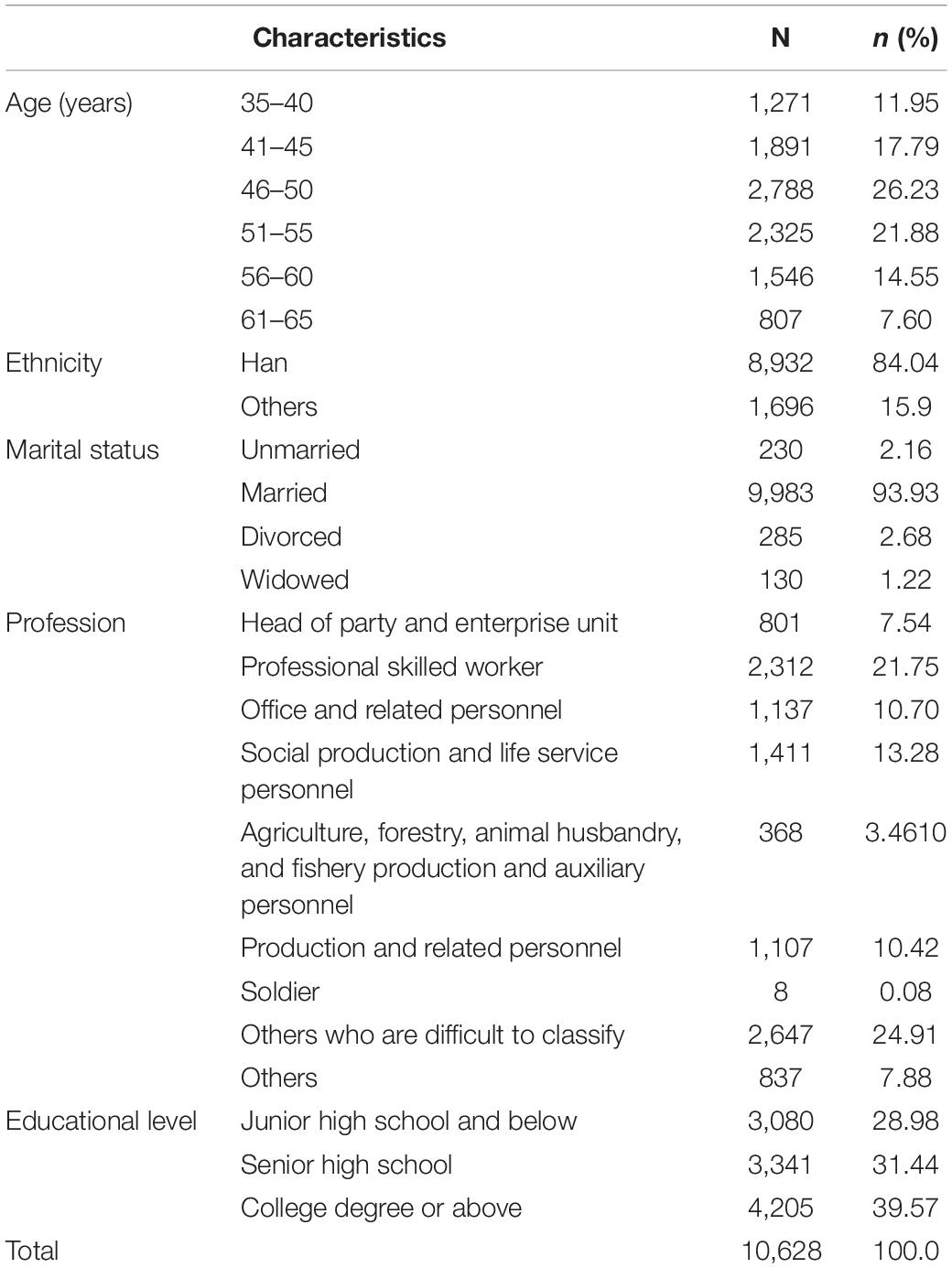
The patient age range was 35–65 years, and 1,271, 1,891, 2,788, 2,325, 1,536, and 807 were 35–40, 41–45, 46–50, 51–55, 56–60, and 61–65 year-old, respectively, corresponding to 11.95, 17.79, 21.88, 26.23, 21.88, 14.55, and 7.6% of the total population, respectively (Table 1).
Personal and Family History
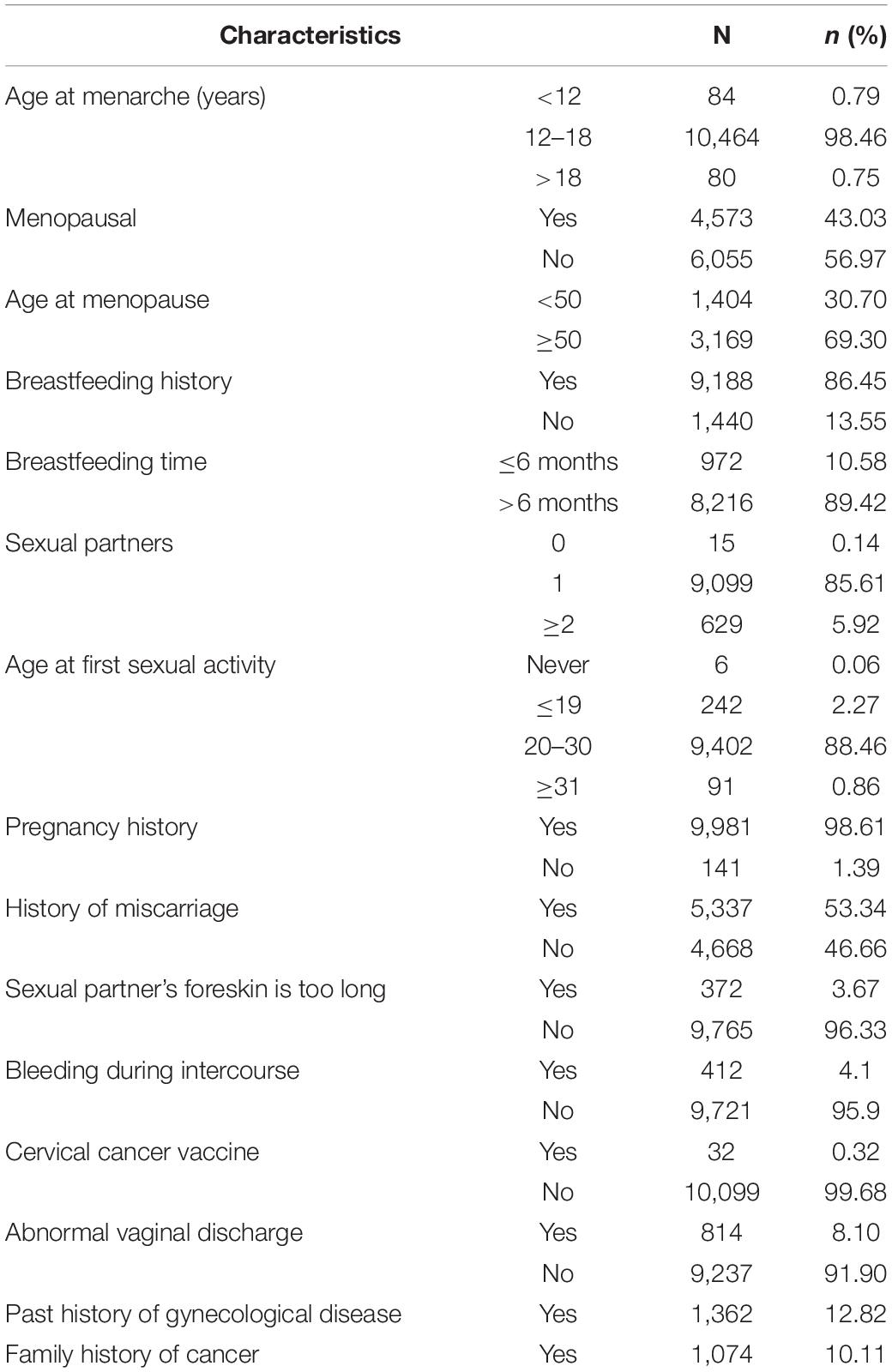
The age of menarche and menopause for most participants was 12–18 years and > 50 years, respectively, accounting for 98.46 and 43.03%, respectively. Furthermore, 86.45% of participants had a history of breastfeeding and 89.42% had a cumulative breastfeeding time > 6 months. In addition, 5.92% of participant had multiple sexual partners and 2.27% had sex for the first time under the age of 19. The results also showed that 53.34% of participants had a history of miscarriage, whereas 3.67 and 4.10% reported prepuce and bleeding during intercourse, respectively, and a history of gynecological diseases and family history of tumor accounted for 12.82 and 10.11%, respectively (Table 2).
Participant Living Habits
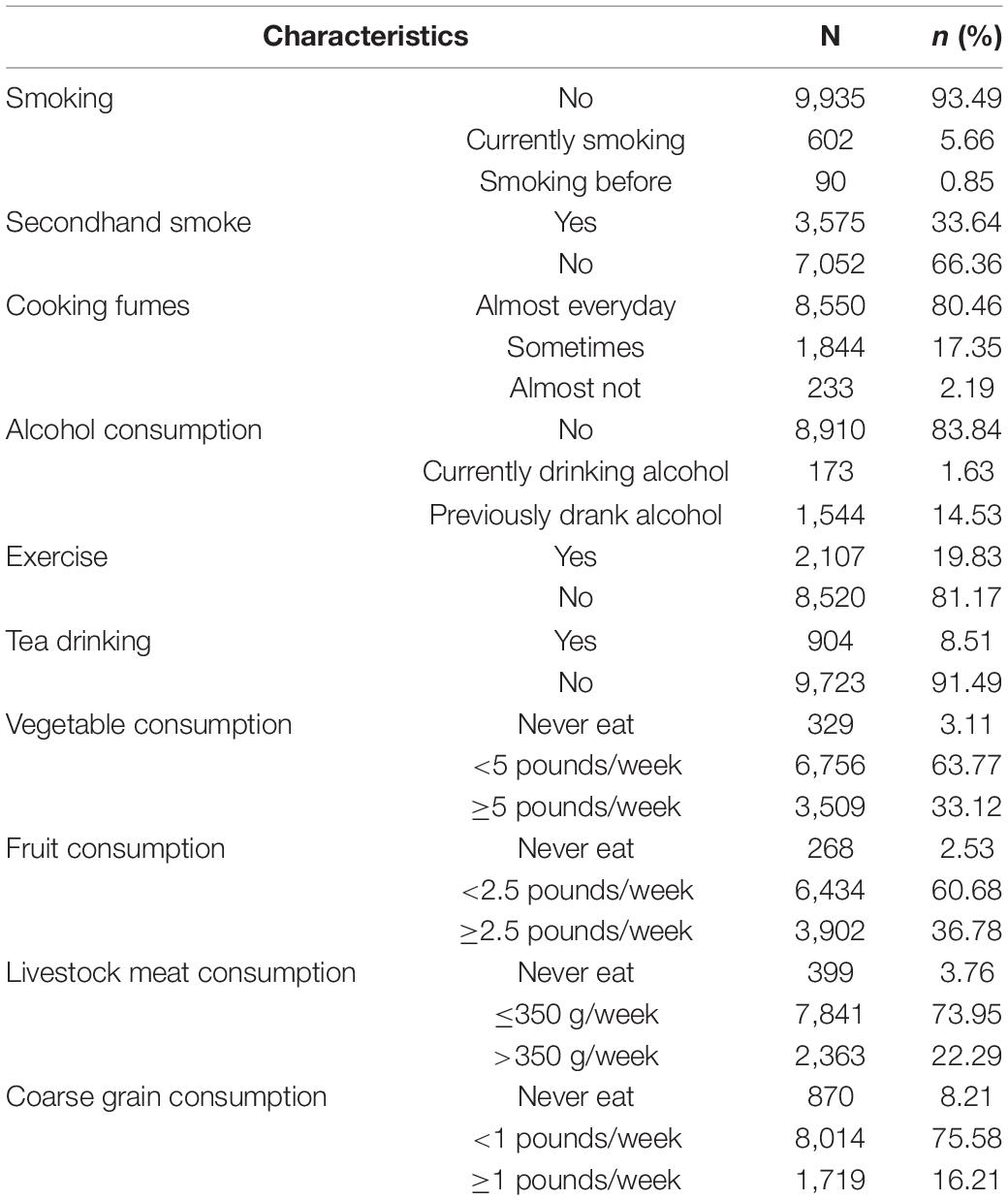
Among the cervical cancer screening population, 56% were current smokers, 0.85% had quit smoking, 33.64% were passive smokers, and 80.46% were exposed to cooking fumes almost daily. In addition, 14.53 and 1.63% of the participants had a history of drinking and were still drinking, respectively, whereas 81.17% did not often participate in outdoor physical exercise and 91.49% did not drink tea. More than 60% of the participants had an insufficient intake of fresh vegetables and fruits, consuming > 5 catties/week and > 2.5 catties/week, respectively. Approximately 75% of human and animal meat intake does not meet the 50–100 g daily requirements of the Dietary Guidelines for Chinese Residents, as shown in Table 3.
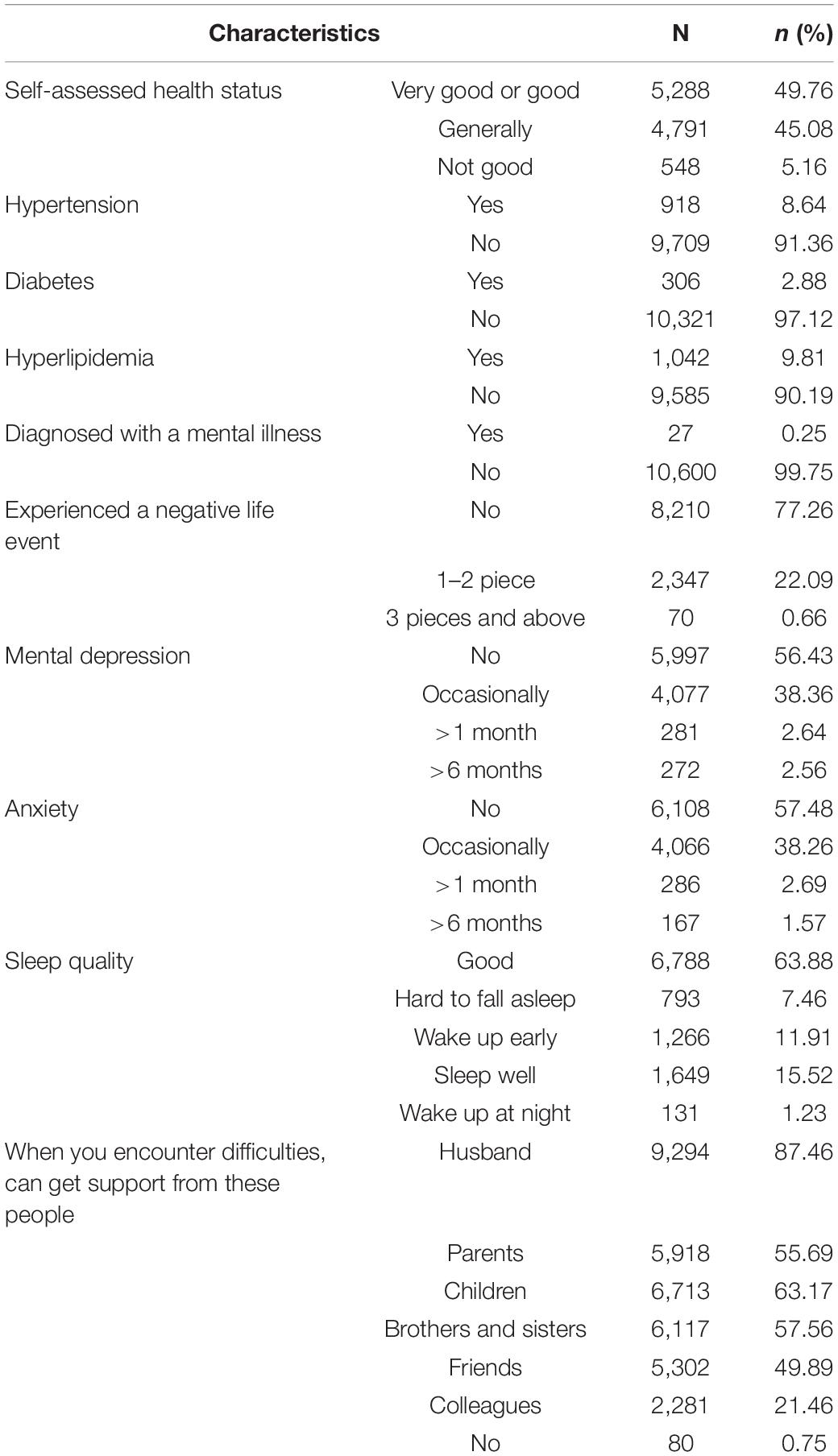
Health and Emotional Status of Study Population
Among the cervical cancer screening population, 49.76, 8.64, 2.88, and 9.81% had very good or good health status, a history of hypertension, a history of diabetes, hyperlipidemia, mental illness, respectively. Furthermore, 22.75, 43.57, and 36.12% of the study population experienced recent negative life events, mental depression or anxiety symptoms, and poor sleep quality, respectively (Table 4).
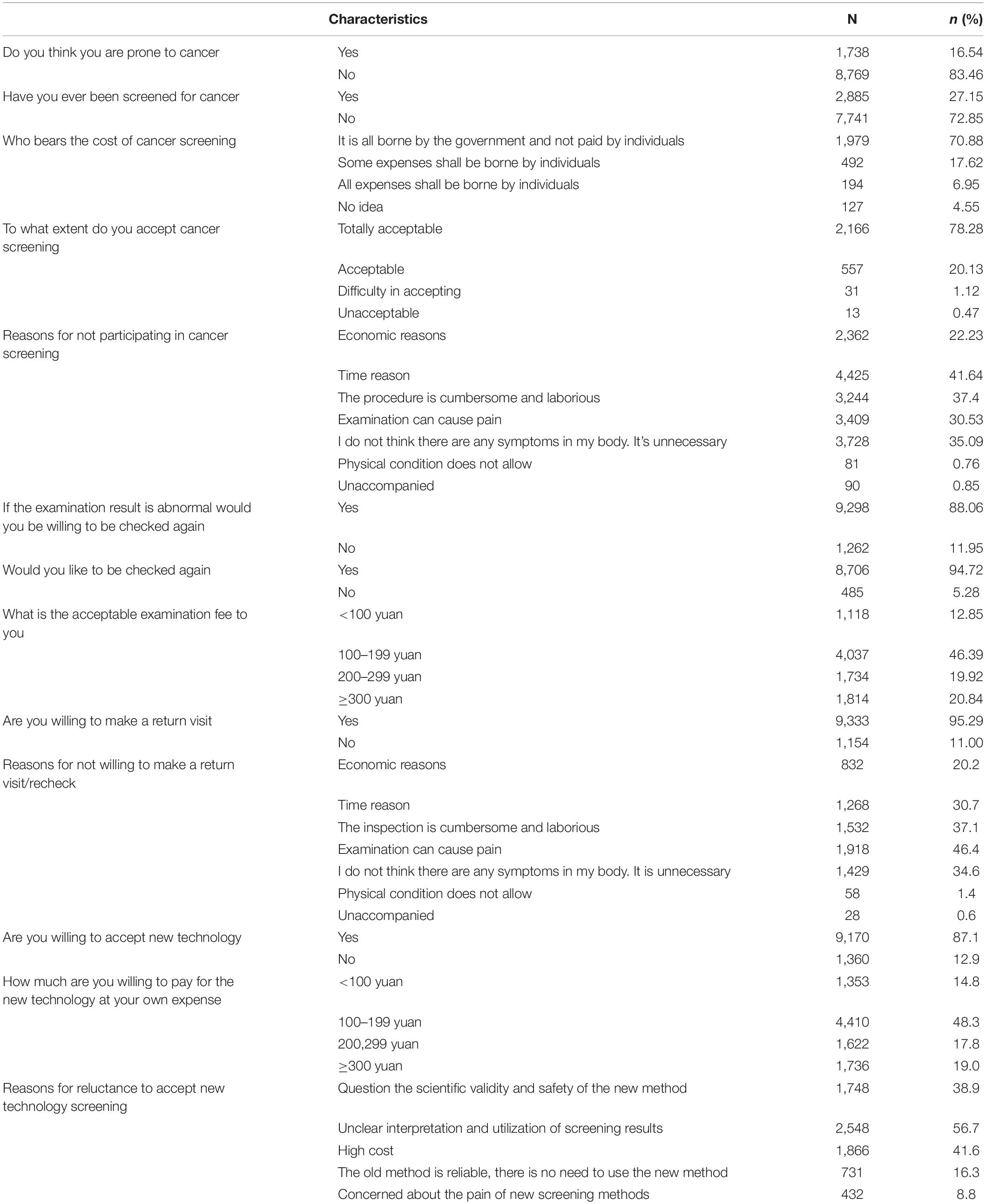
Population Screening Willingness
Among the cervical cancer screening population, 16.54% thought they could easily develop cancer, whereas 27.15% had received cancer screening, and the cancer screening cost was completely covered by the government for up to 70.88% of the individual participants. In addition, > 78.28% of the study population expressed the willingness to fully accept cancer screening and the main reasons for not accepting cancer screening were time and no obvious symptoms.
Most participants were willing to undergo subsequent screening and could bear the expenses. The acceptable proportion of the out-of-pocket expenses was < 200 yuan in most instances. The data showed that 95.29% of the study population reported a willingness to return for a visit in case of abnormal results, and the main reason for those who were unwilling to was concerns that the examination might be painful. Furthermore, 87.1% of participants expressed a willingness to try a more effective new screening technology, with an acceptable out-of-pocket cost of < 200 yuan. The unwillingness to undergo new technology-based screening was mainly attributable to concerns that the interpretation and utilization of the screening results were unclear, as shown in Table 5.
Human Papillomavirus and Thinprep Cytology Test Distribution
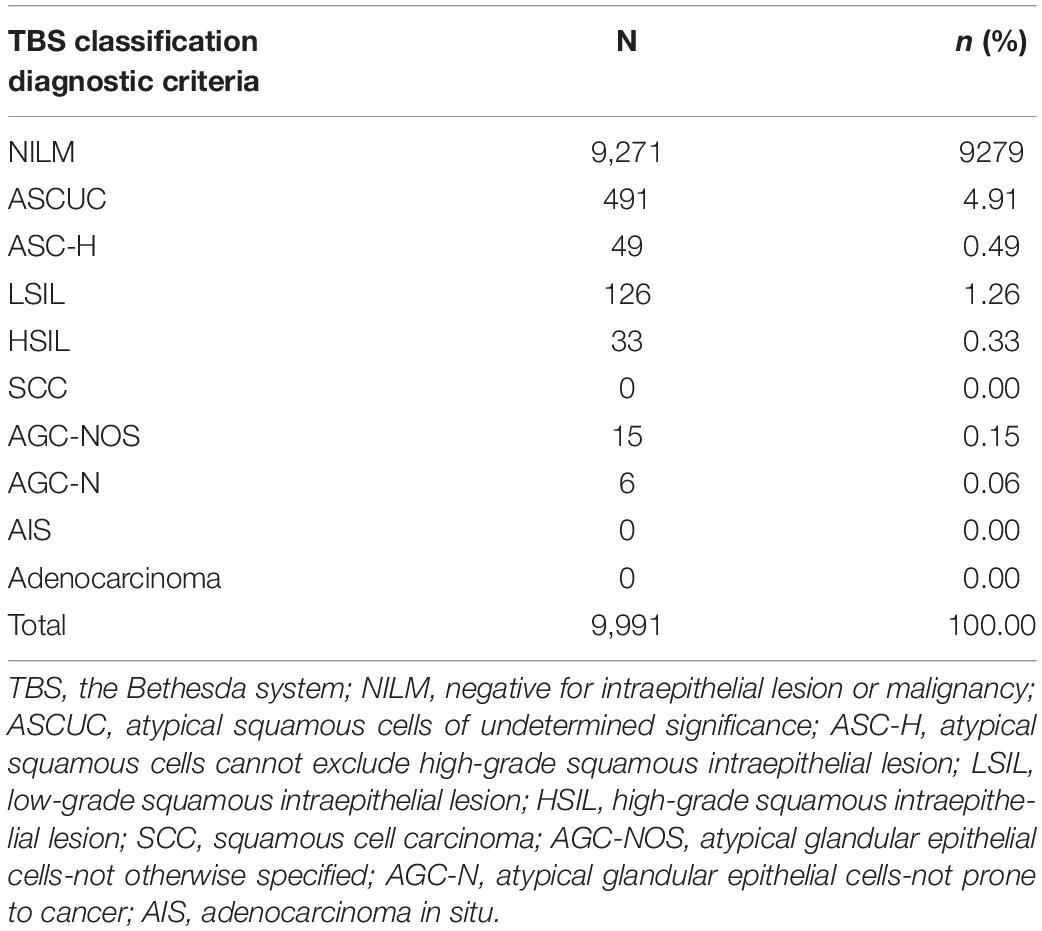
We recruited 10,628 women, aged 35–65 years, to participate in this study, including 626 who did not qualify and were subsequently excluded through the questionnaire survey results. Furthermore, 10,002 women were screened for cervical cancer, and 11 were subsequently excluded because they lacked a specimen and, thus, had no HPV examination results. Finally, 9991 participants were included in the statistical analysis, with an average and median age of 49.51 ± 7.188 and 49 years, respectively (Figure 1). The cytological examination result showed 721 TCT + cases, with 7.22% ASCUS + , which included 4.91% ASCUS, 0.49% ASC-H, 1.26% LSIL, 0.33% HSIL, 0.15% AGC-not otherwise specified (AGC-NOS), and 0.06% AGC-prone to cancer (AGC-N). In contrast, SCC, cervical carcinoma in situ, and adenocarcinoma were not detected (Table 6).
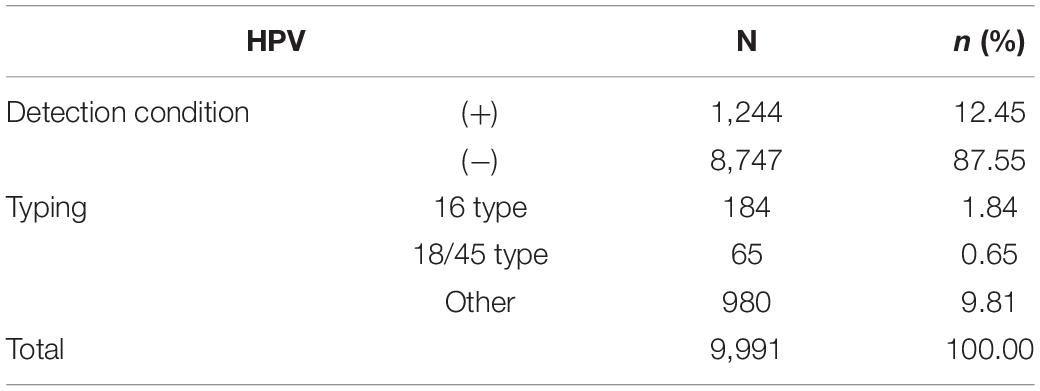
There were 1244 cases of HPV infection, and the positive detection rate was 12.45%. Among the HPV + women, 1213 were further tested for HPV typing, which showed that 184 (15.2%) and 65 (5.4%) were HPV 16 + and 18/45 + with detection rates of 1.84 and 0.65%, respectively. Furthermore, 980 (80.8%) patients were positive for other high-risk types of HPV, with a detection rate of 9.81%. Among the tested patients, 16 women had mixed HPV infections of the above three groups. The positive rate of HPV16 and HPV18/45 in the total screened population was 2.5% (247/9,991) (Table 7).
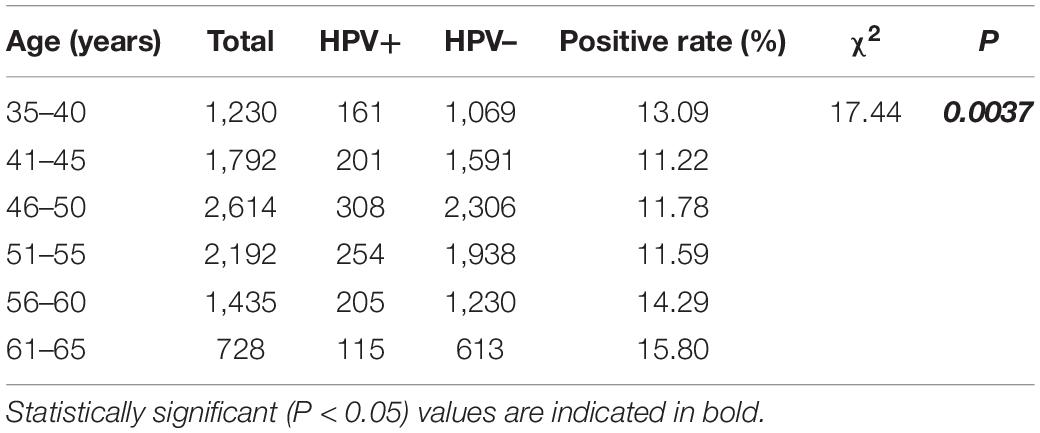
Age Specificity of High-Risk Human Papillomavirus Infection
In this study, 9,991 participants were recruited for high-risk HPV screening in 2018–2021, which included 1,244 (12.45%) that were positive for high-risk HPV. The average age of the women was 49.99 (35–65) years and they were all divided into the following five age groups: 35–40, 41–45, 46–50, 51–55, and 56–65 years old. The prevalence of high-risk HPV infection had two peaks at 35–40, 55–60/61–65 years with infection rates of 13.09, 14.29, and 15.80%, respectively (Table 8).
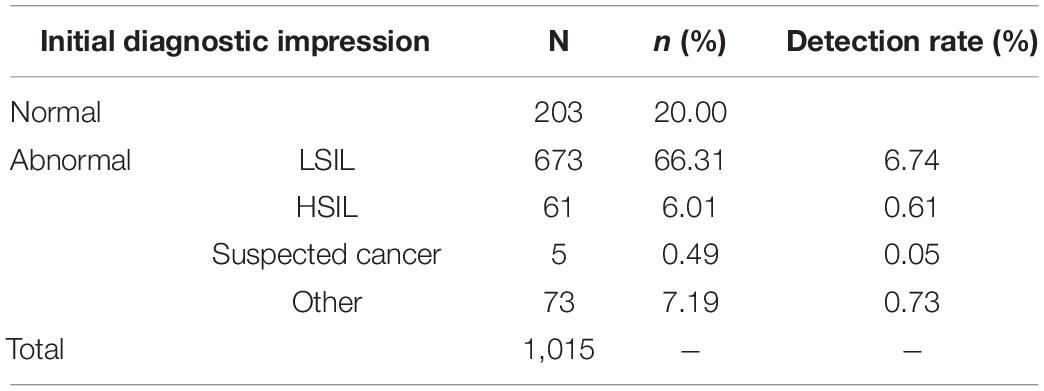
Colposcopy
Further colposcopy was performed in 1,571 cases. There were 1,015 cases with complete colposcopy report, and the referral rate was 64.61%. There were 812 abnormal cases suspected to be diagnosed by colposcopy, 673 cases of low-grade lesions, and 66 cases of high-grade lesions, with a detection rate of 0.66% (Table 9).
Single Factor Analysis of Risk Factors of Human Papillomavirus Infection
The results showed that 28 potential risk factors may be related to high-risk HPV infection. Univariate logistic analysis showed that HPV infection was correlated with different age groups, educational level, age of first sexual activity, number of sexual partners, contraceptive methods, and TCT positivity (P < 0.05) (Table 10).
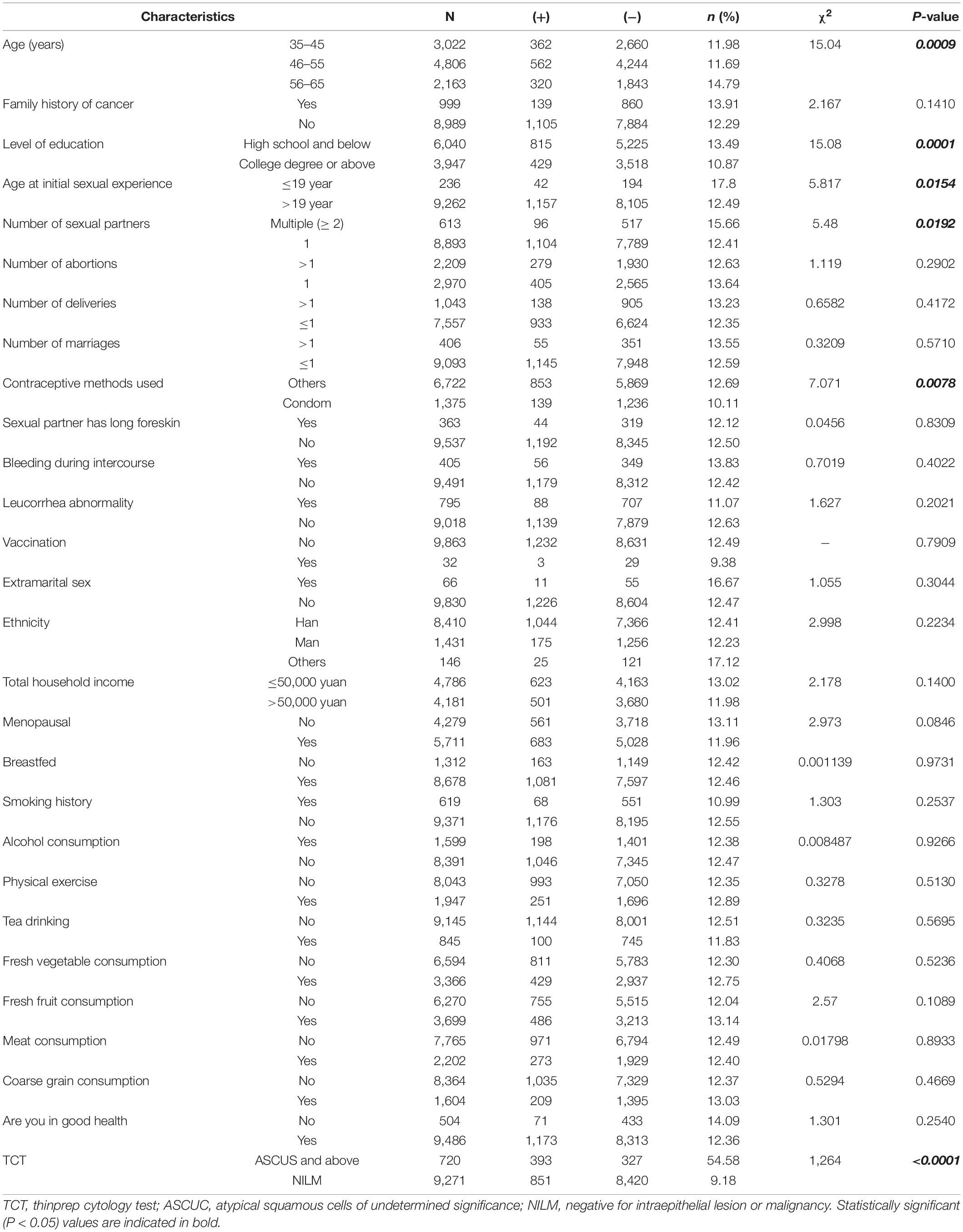
Table 10. Comparison of different information and living habits with human papillomavirus (HPV) positive detection rate.
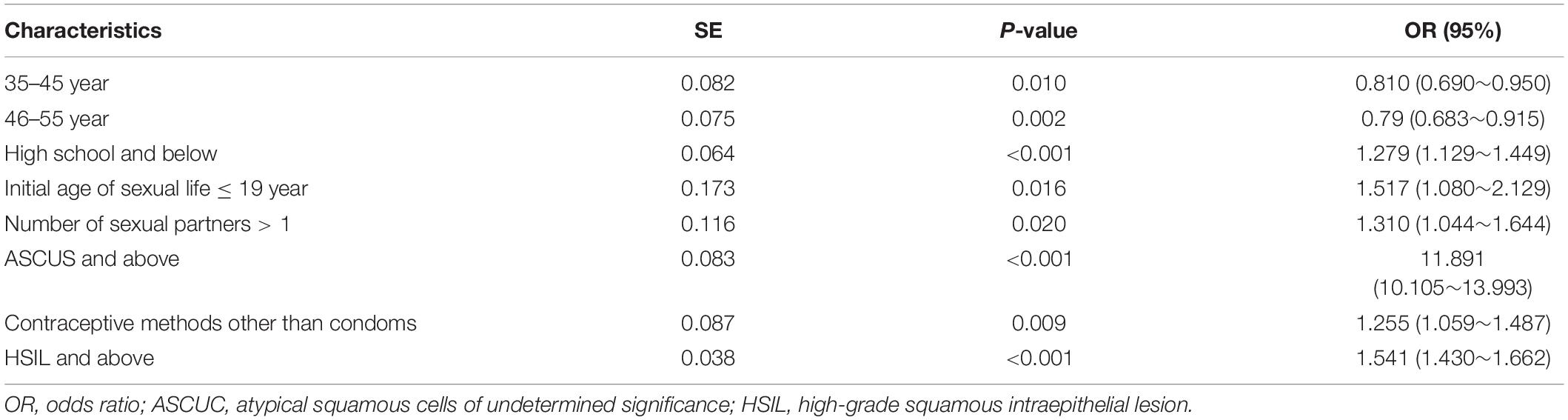
Logistic Regression Analysis of Risk Factors of Human Papillomavirus Infection
The results of the multivariate unconditional logistic regression analysis showed that high school and below [odds ratio (OR) = 1.279 (1.129–1.449), P < 0.001], initial sexual activity age ≤ 19 years old [OR = 1.517 (1.080–2.129), P = 0.016], number of sexual partners > 1 [OR = 1.310 (1.044–1.644), P = 0.020], ASCUS and above [OR = 11.891 (10.105–13.993), P < 0.001], non-condom contraception [OR = 1.255 (1.059–1.487), P = 0.009], and HSIL and above [OR = 1.541 (1.430–1.662), P < 0.001] were risk factors for HPV infection. Compared with women aged 56–65 years, the HPV infection rate of those 35–45 [OR = 0.810 (0.690–0.950), P = 0.010] and 46–55 [OR = 0.79 (0.683–0.915)] years old (P = 0.002) decreased significantly (Table 11).
Univariate Logistic Regression Analysis of Cervical Cancer and CIN II/III Univariate Analysis
Among the 9,991 patients included in the analysis, 1,004 had complete pathological results, including follow-up update, whereas 109 and 895 cases were CINII + and LSIL/inflammation, respectively. Furthermore, 136 and 1 patients were referred for a colposcopy because of TCT/HPV and clinically suspected abnormalities, respectively. The result of the colposcopy evaluation was negative and, therefore, no biopsy was performed. In addition, 137 patients were classified as LSIL and inflammation, and in the absence of pathological results, 8,210 women with double negative screening results (TCT-/HPV-) were regarded as having no cervical lesions. Therefore, 109 CINII + , 5 invasive carcinoma and 9, 242 LSIL/inflammation cases, respectively were included in the statistical analysis.
The detection rate of CINII + in cervical high-grade intraepithelial neoplasia was 1.09% (109/9,991), and the early diagnosis rate of cervical cancer was 95.41%(104/109). The results of the 28 logistic regression analyses using CINII + and diet as dependent variables showed a significant correlation between educational level, breastfeeding, and TCT positivity (P < 0.05). The detection rate of CINII + increased significantly with increasing age, early sexual activity, multiple sexual partners, total family income ≤ 50,000 yuan, bleeding during sexual intercourse and extramarital sex, but there was no significant difference (Table 12).
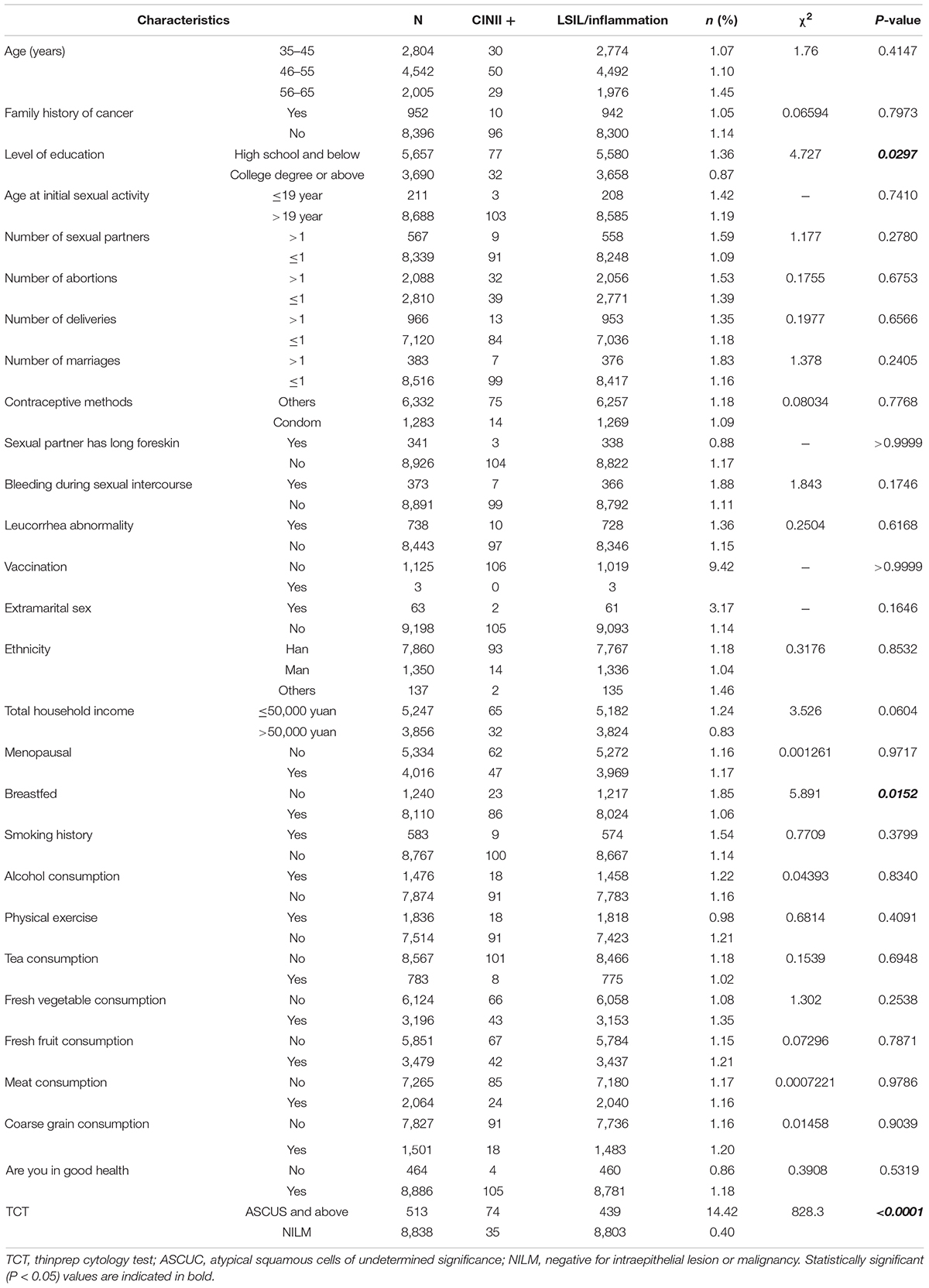
Table 12. Comparison of detection rates of high-grade squamous intraepithelial lesion positive (CINII +) in populations with different basic characteristics.
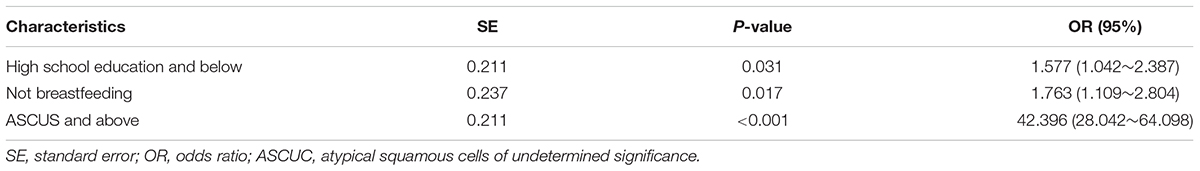
Multivariate Logistic Regression Analysis of Cervical Cancer and CIN2/3 Risk Factors
The factors that were statistically different in the univariate unconditional logistic regression analysis were further analyzed using multivariate unconditional logistic regression. The results showed that high school and below [OR = 1.577 (1.042–2.387), P = 0.031], not breastfeeding [OR = 1.763 (1.109–2.804), P = 0.017], ASCUS and above [OR = 42.396 (28.042–64.098), P < 0.001] were potential risk factors for cervical cancer and precancerous lesions (Table 13).
Discussion
In this multicenter, cross-sectional population study in women, we found that the overall prevalence of HR-HPV was 12.45%, which is lower than the national average. HPV infection can occur at any age and is related to age. In this study, the age-specific distribution showed a bimodal curve, and the first peak appeared in the 35–40-year-old age group, with the infection rate of middle-aged women showing a low trend. The second peak of high-risk HPV infection was observed in women aged 55–60 and 61–65 years, who were born in the 1960s–1970s and the economy of China has improved considerably since then. In addition, the education level of these age groups is significantly lower than that of the younger women, which contributes to their lack of knowledge about HPV infection. In addition, the low level of autoimmunity and hormones further impairs the resistance of the cervix to HPV infection, which may explain the significant increase in their HPV + rate.
Presently, there is no specific or effective drug treatment for HPV infection, and although a vaccine has been developed and listed in China, it is expensive and does not prevent all subtype infections (You et al., 2020). Therefore, the prevention of HPV infection is very important. Number studies have reported the following as some factors to be related to the incidence of cervical cancer: sexual activity, early first sexual activity, premature delivery, prolificacy, high-risk HPV infection, and smoking. The following are some of the factors related to cervical intraepithelial neoplasia: sexual activity, HPV infection, smoking, premature sexual activity, sexually transmitted diseases, low economic status, use of oral contraceptives, and immunosuppression (Shannon et al., 2017).
In this study, multicenter cervical screening was used to analyze the incidence of HPV infection, cervical cancer, and high-grade precancerous lesions in women. The results led us to conclude that high school and below, initial sexual life age ≤ 19 years old, number of sexual partners > 1, ASCUS and above, non-condom contraception, HSIL and above were all risk factors of HPV infection. The reason may be that women with a low educational level lack the awareness of cervical screening and prevention strategies (Williams et al., 2019). Women ≤ 19 years old who are sexually active are prone to HPV infection because of their immature cervical development and incompletely developed autoimmune function (Morris et al., 2019). Furthermore, a higher number of sexual partners increases the potential exposure to HPV infection, rendering an individual prone to HPV infection.
Numerous studies have shown that an active sex life is closely related to the occurrence and development of cervical cancer. Literature reports from countries other than China state that factors such as sexual partners and frequency are closely related to cervical cancer (Torres-Poveda et al., 2019). Condoms block pathogens from damaging the cervical mucosa and inhibiting the immune function, whereas cleaning the vulva reduces the probability of infection. Both processes reduce the stimulatory effects of semen on the cervical mucosa, which is consistent with the research results of Hariri and Warner (2013) on male condoms that indicates that they contribute to reducing the transmission of HPV. The incidence of CINII and above was positively correlated with HPV infection.
Cervical lesions mostly occur in married women and it is the most serious cervical disease, and shows higher occurrence in younger women (Arbyn et al., 2020). Cervical cancer, which is mainly caused by long-term cervical lesions, has a high mortality, which is gradually increasing (Arbyn et al., 2020). Therefore, preventing cervical lesions is extremely significant for women (Cree et al., 2021). HPV infection has always been considered an important factor in the development of cervical lesions, but most women can be protected by the autoimmune system. In addition, a few women will continue to be infected and develop cervical cancer over time. Therefore, the need to actively understand cervical lesions, HPV infection, and the influencing factors has been increasingly attracting clinical attention. Studies suggest that high-risk HPV infection was detected in 99.7% of cervical cancer patients (Crosbie et al., 2013).
HPV has been reported to be transmitted through direct or indirect skin or sexual contact (Wierzbicka et al., 2022). The infection occurs worldwide with approximately 4–20% of healthy individuals harboring the infection, and the cumulative lifetime infection rate is 60–70%. Sustained expression of the E6 and E7 HPV virus subtypes has been found to be closely related to the growth of HPV-infected cancer cells (Pinatti et al., 2017). HPV infection is the most important and definite cause of cervical cancer (Araldi et al., 2018). In this study, we found that an increasing histopathological grade of HR-HPV infection was associated with the incidence of cervical cancer. The results showed that a high school education and below, non-lactation, and TCT positivity were statistically significant (P < 0.05) risk factors of cervical cancer and CIN II/III.
The CINII + detection rate increased with increasing age, early sexual activity, multiple sexual partners, total family income ≤ 50,000 yuan, bleeding during sexual intercourse, and extramarital sex, but not significantly. This study has been compared with other similar related research data in the near future (see Supplementary Table 1 for details) (Kitamura et al., 2021; Tagne Simo et al., 2021; Niu et al., 2022). As a preventable malignant tumor, the occurrence and development of cervical cancer is a gradual process that takes several years to progress from intraepithelial lesions to invasive disease. Effective screening methods for cervical cancer could ensure early detection, diagnosis, and treatment of cervical precancerous lesions and, to a certain extent, reduce its incidence rate and mortality.
Conclusion
Cervical cancer is a prominent public health problem and proms focusing on its prevention and control should be strengthened. In this study, multicenter cervical screening of women to determine the HPV infection rate and incidence of cervical high-grade precancerous lesions, demonstrated a high school education and below, initial age of sexual activity ≤ 19 years old, more than one sexual partner, ASCUS and above, non-condom contraception, and HSIL and above as risk factors of HPV infection. Furthermore, a high school education and below, non-lactation, and a positive TCT result were identified as risk factors of cervical cancer and high-grade precancerous lesion infection. In conclusion, the investigation of risk factors for HPV infection and cervical high-grade precancerous lesions are of great significance for reducing the incidence rate of cervical cancer. Consequently, we recommend the establishment of strategies to enhance the awareness of the risk factors of high-risk HPV infection; to promote healthy sexual behavior, life, and health habits; and to improve immunity and strengthen physical exercise, which could effectively reduce the incidence rate of cervical cancer.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Liaoning Cancer Hospital (No. 20180106). The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
HP and CW designed and supervised the project. DY, JZ, and XC collected clinical data samples. DY collected and processed data and data analysis, and drafted the manuscript. JM translated and polished the manuscript. All authors reviewed, discussed, and edited versions of the final report manuscript.
Funding
This study was supported by the National Key Research and Development Program (2016YFC1303001).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank the staff from Cancer Hospital of China Medical University, who took part in the study. We would also like to thank JM for the great help offered in manuscript revision.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmicb.2022.914516/full#supplementary-material
References
Abulizi, G., Li, H., Mijiti, P., Abulimiti, T., Cai, J., Gao, J., et al. (2017). Risk factors for human papillomavirus infection prevalent among Uyghur women from Xinjiang. Chin. Oncotarget 8, 97955–97964.
Aimagambetova, G, and Azizan, A. (2018). Epidemiology of HPV Infection and HPV-related cancers in Kazakhstan:a review. Asian Pac. J. Cancer Prev. 19, 1175–1180.
Araldi, R. P., Sant’Ana, T. A., Módolo, D. G., Melo, T. C., Spadacci-Morena, D. D., de Cassia Stocco, R., et al. (2018). The human papillomavirus (HPV)-related cancer biology: an overview. Biomed. Pharmacother. 106, 1537–1556.
Arbyn, M., Weiderpass, E., Bruni, L., de Sanjosé, S., Saraiya, M., Ferlay, J., et al. (2020). Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob. Health 8:e191–e203.
Bekmukhambetov, Y. Z., Balmagambetova, S. K., Jarkenov, T. A., Nurtayeva, S. M., Mukashev, T. Z., and Koyshybaev, A. K. (2016). Distribution of high risk human papillomavirus types in Western Kazakhstan — retrospective analysis of PCR data. Asian Pac. J. Cancer Prev. 17, 2667–2672.
Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., and Jemal, A. (2018). Global cancer statistics 2018: gLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68, 394–424.
Cao, W., Chen, H. D., Yu, Y. W., Li, N., and Chen, W. Q. (2021). Changing profiles of cancer burden worldwide and in China: a secondary analysis of the global cancer statistics 2020. Chin. Med. J. 134, 783–791. doi: 10.1097/CM9.0000000000001474
Cordeiro, M. N., De Lima, R. C. P., Paolini, F., Melo, A. R. D. S., Campos, A. P. F., Venuti, A., et al. (2018). Current research into novel therapeutic vaccines against cervical cancer. Expert Rev. Anticancer Ther. Apr. 18, 365–376.
Cree, I. A., Indave Ruiz, B. I., Zavadil, J., McKay, J., Olivier, M., Kozlakidis, Z., et al. (2021). IC3R participants. The International Collaboration for Cancer Classification and Research. Int. J. Cancer. 148, 560-571. doi: 10.1002/ijc.33260
Crosbie, E. J., Einstein, M. H., Franceschi, S., and Kitchener, H. C. (2013). Human papillomavirus and cervical cancer. Lancet 382, 889–899.
Giorgi Rossi, P., Ronco, G., Mancuso, P., Carozzi, F., Allia, E., Bisanzi, S., et al. (2022). NTCC2 Working Group. Performance of HPV E6/E7 mRNA Assay as Primary Screening Test. Results from the NTCC2 Trial. Int. J. Cancer [Epub ahead of print]. doi: 10.1002/ijc.34120
Hariri, S., and Warner, L. (2013). Condom use and human papillomavirus in men. J. Infect. Dis. 208, 367–369.
Jiang, L., Tian, X., Peng, D., Zhang, L., Xie, F., Bi, C., et al. (2019). HPV prevalence and genotype distribution among women in Shandong Province, China:analysis of 94,489 HPV genotyping results from Shandong’s largest independent pathology laboratory. PLoS One 14, e0210311. doi: 10.1371/journal.pone.0210311
Kclurman, R. J., Carcangiu, M. L., Herrington, C. S., et al. (2014). WHO Classigication of Tumors of Female Reproductive organs [M] 4thed. Lyon: International Agency for Research on Cancer.
Kitamura, T., Suzuki, M., Shigehara, K., and Fukuda, K. (2021). Prevalence and Risk Factors of Human Papillomavirus Infection among Japanese Female People: a Nationwide Epidemiological Survey by Self-Sampling. Asian Pac. J. Cancer Prev. 22, 1843–1849. doi: 10.31557/APJCP.2021.22.6.1843
Lewandowska, A. M., Lewandowski, T., Rudzki, M., Rudzki, S., and Laskowska, B. (2021). Cancer prevention - review paper. Ann. Agric. Environ. Med. 2020:12.
Maria, H., Dana, H., Francoise, M., Michael, P., and Jurgen, W. (2018). Human papillomaviruses in Western Africa: prevalences and risk factors in Burkina Faso. Arch. Gynecol. Obstet. 298, 789–796.
McLaughlin-Drubin, M. E., and Munger, K. (2008). Viruses associated with human cancer. Biochim. Biophys. Acta Mol. Basis Dis. 1782, 127–150.
Morris, B. J., Hankins, C. A., Banerjee, J., Lumbers, E. R., Mindel, A., Klausner, J. D., et al. (2019). Does Male Circumcision Reduce Women’s Risk of Sexually Transmitted Infections, Cervical Cancer, and Associated Conditions? Front. Public Health 7, 4. doi: 10.3389/fpubh.2019.00004
Niu, J., Pan, S., Wei, Y., Hong, Z., Gu, L., Di, W., et al. (2022). Epidemiology and analysis of potential risk factors of high-risk human papillomavirus (HPV) in Shanghai China: a cross-sectional one-year study in non-vaccinated women. J. Med. Virol. 94, 761–770. doi: 10.1002/jmv.27453
Ouh, Y. T., Min, K. J., Cho, H. W., Ki, M, Oh, J. K, Shin, S. Y et al. (2018). Prevalence of human papillomavirus genotypes and precancerous cervical lesions in a screening population in the Republic of Korea, 2014–2016. J. Gynecol. Oncol. 29:e14. doi: 10.3802/jgo.2018.29.e14
Peter, M., Stransky, N., Couturier, J., Hupé, P., Barillot, E., de Cremoux, P., et al. (2010). Frequent genomic structural alterations at HPV insertion sites in cervical carcinoma. J. Pathol. 221, 320–330. doi: 10.1002/path.2713
Pinatti, L. M., Walline, H. M., and Carey, T. E. (2017). Human Papillomavirus Genome Integration and Head and Neck Cancer. J. Dent. Res. 97, 691–700.
Shannon, B., Yi, T. J., Perusini, S., Gajer, P., Ma, B., Humphrys, M. S., et al. (2017). Association of HPV infection and clearance with cervicovaginal immunology and the vaginal microbiota. Mucosal. Immunol. 10, 1310–1319.
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., et al. (2021). Global Cancer Statistics 2020: gLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 71, 209–249.
Tagne Simo, R., Djoko Nono, A. G., Fogang Dongmo, H. P., Seke Etet, P. F., Fonyuy, B. K., Kamdje, A. H. N., et al. (2021). Prevalence of precancerous cervical lesions and high-risk human papillomavirus types in Yaounde. Cameroon. J. Infect. Dev. Ctries. 15, 1339–1345.
Thanapprapasr, D., Deesamer, S., Sujintawong, S., Udomsubpayakul, U., and Wilailak, S. (2012). Cervical cancer screening behaviours among Thai women: results from a cross-sectional survey of 2112 healthcare providers at Ramathibodi Hospital. Thailand. Eur. J. Cancer Care 21, 542–547. doi: 10.1111/j.1365-2354.2012.01333.x
Torres-Poveda, K., Ruiz-Fraga, I., Madrid-Marina, V., Chavez, M., and Richardson, V. (2019). High risk HPV infection prevalence and associated cofactors: a population-based study in female ISSSTE beneficiaries attending the HPV screening and early detection of cervical cancer program. BMC Cancer. 19:1205. doi: 10.1186/s12885-019-6388-4
Wierzbicka, M., San Giorgi, M. R. M., and Dikkers, F. G. (2022). Transmission and clearance of human papillomavirus infection in the oral cavity and its role in oropharyngeal carcinoma - A review. Rev. Med. Virol. 22:e2337. doi: 10.1002/rmv.2337
Williams, M. S., Kenu, E., Adanu, A., Yalley, R. A., Lawoe, N. K., Dotse, A. S., et al. (2019). Awareness and beliefs about cervical cancer, the HPV vaccine, and cervical cancer screening among Ghanaian women with diverse education levels. J. Cancer Educ. 34, 897–903. doi: 10.1007/s13187-018-1392-y
You, D., Han, L., Li, L., Hu, J., Zimet, G. D., and Alias, H. (2020). Human Papillomavirus (HPV) Vaccine Uptake and the Willingness to Receive the HPV Vaccination among Female College Students in China: a Multicenter Study. Vaccines 8:31. doi: 10.3390/vaccines8010031
Zheng, R. S., Sun, K. X., Zhang, S. W., Zeng, H. M., Zou, X. N., Chen, R., et al. (2019). Report of cancer epidemiology in China, 2015. Zhonghua Zhong Liu Za Zhi 41, 19–28.
Keywords: cervical cancer, screening, high-risk factor, human papillomavirus infection, precancerous lesions
Citation: Yang D, Zhang J, Cui X, Ma J, Wang C and Piao H (2022) Risk Factors Associated With Human Papillomavirus Infection, Cervical Cancer, and Precancerous Lesions in Large-Scale Population Screening. Front. Microbiol. 13:914516. doi: 10.3389/fmicb.2022.914516
Received: 07 April 2022; Accepted: 10 June 2022;
Published: 30 June 2022.
Edited by:
Antoinette Van Der Kuyl, University of Amsterdam, NetherlandsReviewed by:
Suvankar Ghorai, Raiganj University, IndiaAna Afonso, University of São Paulo, Brazil
Komsun Suwannarurk, Thammasat University, Thailand
Copyright © 2022 Yang, Zhang, Cui, Ma, Wang and Piao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chunyan Wang, bG56bGd5bkAxNjMuY29t; Haozhe Piao, cHpweUAxNjMuY29t
 Di Yang1
Di Yang1 Chunyan Wang
Chunyan Wang