- 1Department of Pain, The Third Xiangya Hospital and Institute of Pain Medicine, Central South University, Changsha, China
- 2Department of Orthopedics, The Third Xiangya Hospital, Central South University, Changsha, China
- 3Hunan Key Laboratory of Brain Homeostasis, Central South University, Changsha, China
Background: Lumbosacral radicular pain (LSRP) can be caused by disc herniation, spinal stenosis, and failed back surgery syndrome. The clinical effect of pulsed-radiofrequency (PRF) combined with transforaminal epidural steroid injection (TESI) for radiating pain in different population remains unclear.
Methods: We retrospectively reviewed the medical recordings of patients with LSRP caused by different etiologies, who underwent PRF and TESI treatment. The primary clinical outcome was assessed by a 10-point Visual Analog Scale (VAS) pre- and post-treatment.
Results: A total of 34 LSRP patients were identified and classified into 3 subgroups (disc herniation, spinal stenosis, and failed back surgery syndrome). The overall immediate pain reduction was 4.4 ± 1.1 after procedure. After a median follow-up of 9.5 months, the VAS decreased from 6.5 ± 1.0 to 2.4 ± 1.9 at the last follow-up.
Conclusion: PRF combined with TESI is an effective approach to treat persistent LSRP in distinct population.
Introduction
Lumbosacral radicular pain (LSRP) is defined as a radiating pain affected one or more lumbar or sacral dermatomes (Van Boxem et al., 2010). LSRP is commonly accompanied with disc herniation (DH), spinal stenosis (SS), and failed back surgery syndrome (FBSS) (Abejón et al., 2007; Park and Lee, 2019; Clingan et al., 2020). Conservative therapy remains the first option for the initial management of LSRP, including oral NSAIDs and/or anticonvulsants, exercise, and physiotherapy. In addition, epidural corticosteroid injections may provide supplementary relief from pain at short-term follow-up (Oliveira et al., 2020). The principal goal of surgical intervention is to remove the compression of nerve root. However, no significant improvement of pain or physical function was achieved through the discectomy compared with conservative care up to 2 years follow-up (Weinstein et al., 2006). Thus, alternative option of LSRP management is further needed.
A complex interplay between mechanical, inflammatory, immune and neurophysiologic mechanism of dorsal root ganglion (DRG) attributes to the chronicity of radicular pain (Dower et al., 2019). Thus, it is essential to normalize the dysfunction of DRG to achieve sustained pain relief in patient with or without mechanical compression. Pulsed-radiofrequency (PRF) is the most widely used technique of neuromodulation in pain management. Recently, PRF adjacent to the DRG has been increasingly used to treat cervical, thoracic, lumbar, and sacral radicular pain (Koh et al., 2015; Hetta et al., 2020; Lee et al., 2020). After administration of PRF, more than three quarters of patients with lumbar radicular pain rejected to undertake spinal surgery (Trinidad et al., 2015).
Despite PRF therapy, spinal injection is another important technique to treat radicular pain when conservative therapy is ineffective. To treat chronic LSRP, different approach of epidural injections, including transforaminal epidural steroid injection (TESI) and interlaminar epidural steroid injections, can be considered. The overall percentage of the patients with significant functional improvement and pain relief receiving TESI treatment was higher than interlaminar routine (Rados et al., 2011). Given the anti-inflammatory effect, TESI may provide a supplementary analgesic effect to PRF. The aim of this study was to retrospectively evaluate the clinical efficiency of PRF combined with TESI to treat LSRP with different etiologies.
Materials and Methods
Study Design
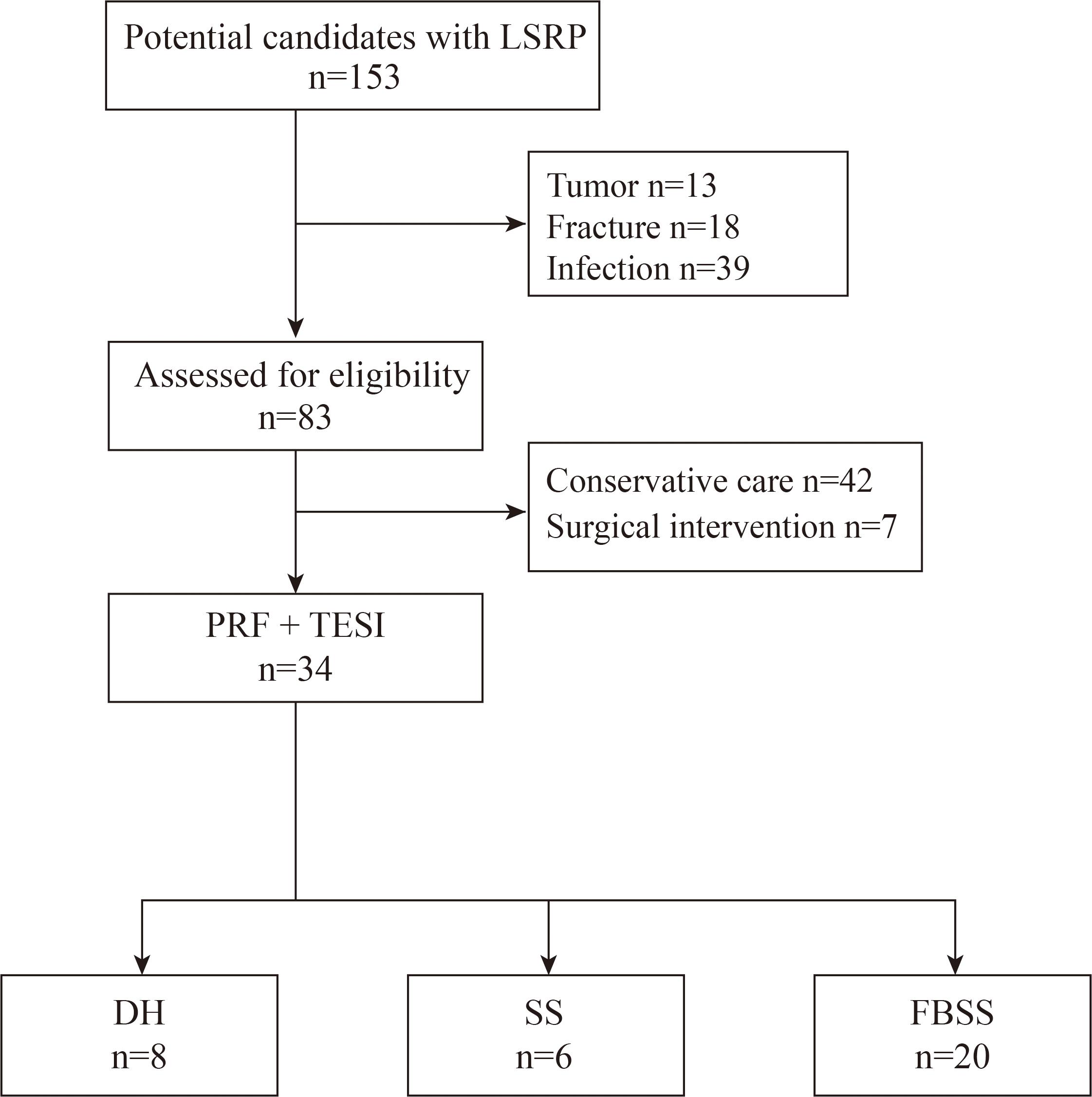
We conducted a retrospective analysis of medical recordings in the Department of Pain, the Third Xiangya Hospital between August 2019 and February 2021. All participants presented unilateral or bilateral LSRP. DH or SS was confirmed with either computed tomography or magnetic resonance imaging. We also enrolled patients present with sustained radiating pain after back surgery. One or more oral analgesic medication, or nerve block was administrated prior to surgery. This study was approved by the local ethics committee of the Third Xiangya Hospital (No. 21035) and conducted in accordance with the Declaration of Helsinki. Patients with pathologic history were excluded for further study, including tumor, fractures, and infection. The enrolled patients were subsequently divided into three subgroups according to the etiology (DH, SS, and FBSS), as shown in Figure 1. Most patients (20 out of 34) had a history of back surgery. There were 8 patients diagnosed with DH, and six for SS cohort, respectively.
Surgical Detail
All interventional procedures were performed under the guidance of C-arm fluoroscopy (TOSHIBA). Patients were placed prone position, and kept awake during the procedure to respond the test of sensory stimulation. Local anesthesia was administrated to the skin entry with 1% lidocaine in a total volume of 5 mL.
To perform PRF therapy, a 22-G curved-tip cannula was applied to place adjacent to the DRG (Figure 2). One catheter needle with active tip electrode was then inserted though the cannula, and the distal ending of electrode was connected to the radiofrequency generator (Beiqi, R-2000BA1, Beijing, China). Sensory test was conducted to induce a tingling sensation and/or dysesthesia at a voltage less than 0.5 V. PRF treatment was set at 2 Hz (20 ms pulse width) three times for 240 s. During the procedure, the temperature of electrode tip did not exceed 42°C (Tortora et al., 2021). After PRF treatment, a mixture of ropivacaine 0.2% 5 mL and betamethasone 2.5 mg was injected to the DRG site. When multiple DRGs were targeted in one procedure, the total amount of betamethasone was no more than 5 mg.
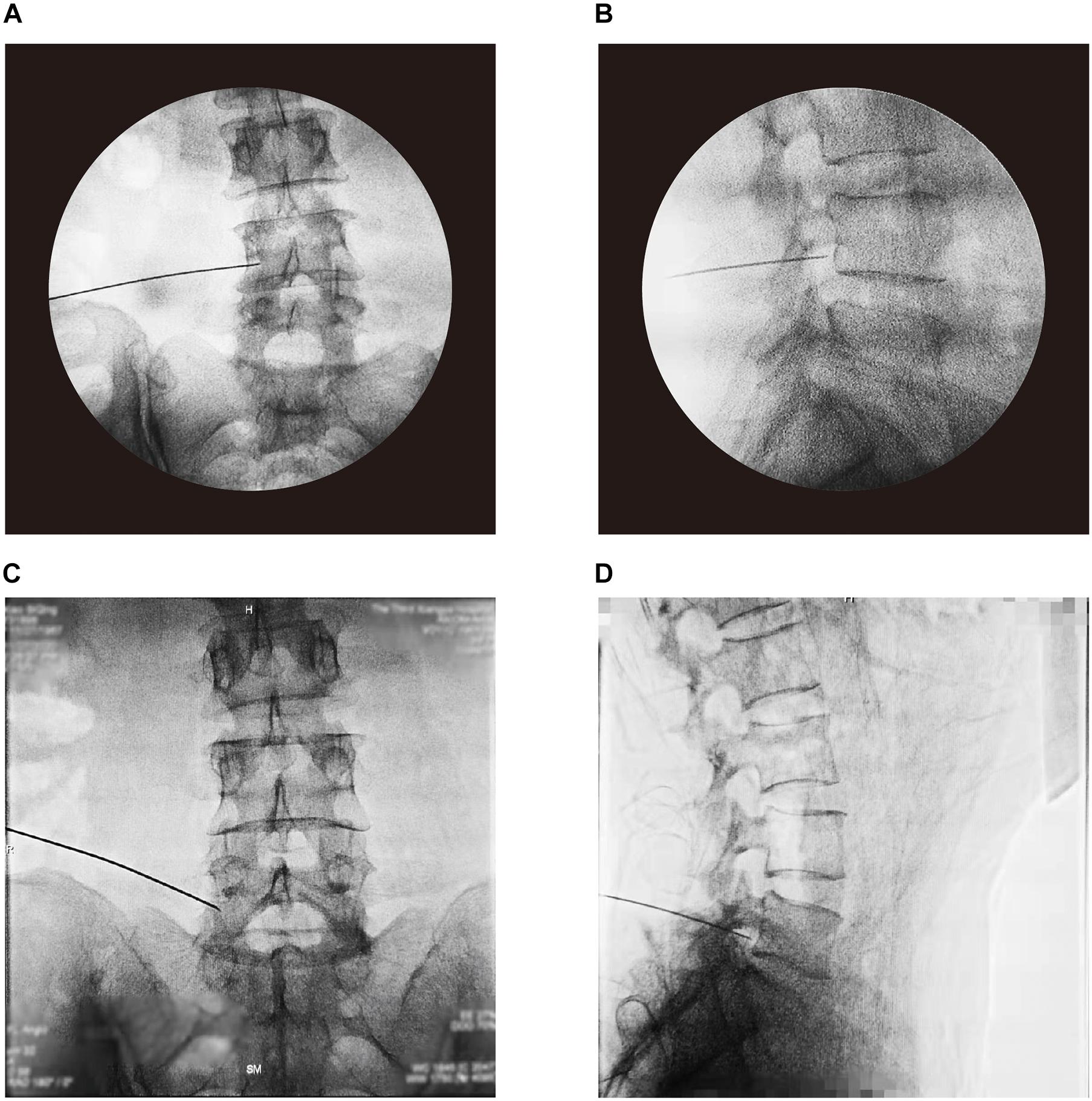
Figure 2. Placement of PRF cannula confirmed by the guidance of C-arm fluoroscopy. Anterior-posterior and lateral view at L4 level (A,B), and L5 level (C,D).
Measurement and Follow-up
The primary outcome was the pain scores in LSRP patients. Visual analog scale (VAS) was used to evaluate the pain intensity, ranging from 0 (“pain free”) to 10 (“worst pain imaginable”). Patients who achieved reduction of pain over 50% compared with baseline were considered as “responder.” Patients were assessed pre- and post-treatment. To identify the long-term therapeutic effect, a telephone interview was conducted after discharge from hospital.
Statistical Analyses
Statistical analysis was performed with GraphPad Prism 8 (GraphPad, San Diego, CA, United States). Variables are presented as the mean ± standard deviation. The pain score changes were assessed pre- and post-therapy with paired Student’s t-test. P < 0.05 was considered significant.
Results
General Demographics
We identified 34 patients (16 males and 18 females) with LSRP who underwent 57 PRF procedures combined with TESI from August 2019 until February 2021. The average age of participants was 65 ± 11.8 years. The L4-5 spinal nerve accounted for the most common lesion, affected 49 of 73 (67.1%) painful dermatomes. Patients presented moderate to severe radiating pain at admission, with a mean baseline VAS of 6.5 ± 1.0. In this study, about 76.4% patients (26 out of 34) underwent one or twice procedures during hospitalization. The general demographics of enrolled patients is given in Table 1.
Follow-Up
All patients were evaluated pre- and post-surgery. We performed one routine follow-up 1 month after discharge from hospital for all participants. The median time of the last follow-up was 9.5 months, ranging from 1 to 18 months.
Clinical Outcome
The initial relief from pain is given in Figure 3. The immediate reduction of pain scores was 4.4 ± 1.1 across different etiologies. All SS patients achieved significant improvement of pain symptom, with pain scores reduction over 50%. The response rate before discharge was 87.5% for DH cohort, and 90% for FBSS, respectively.
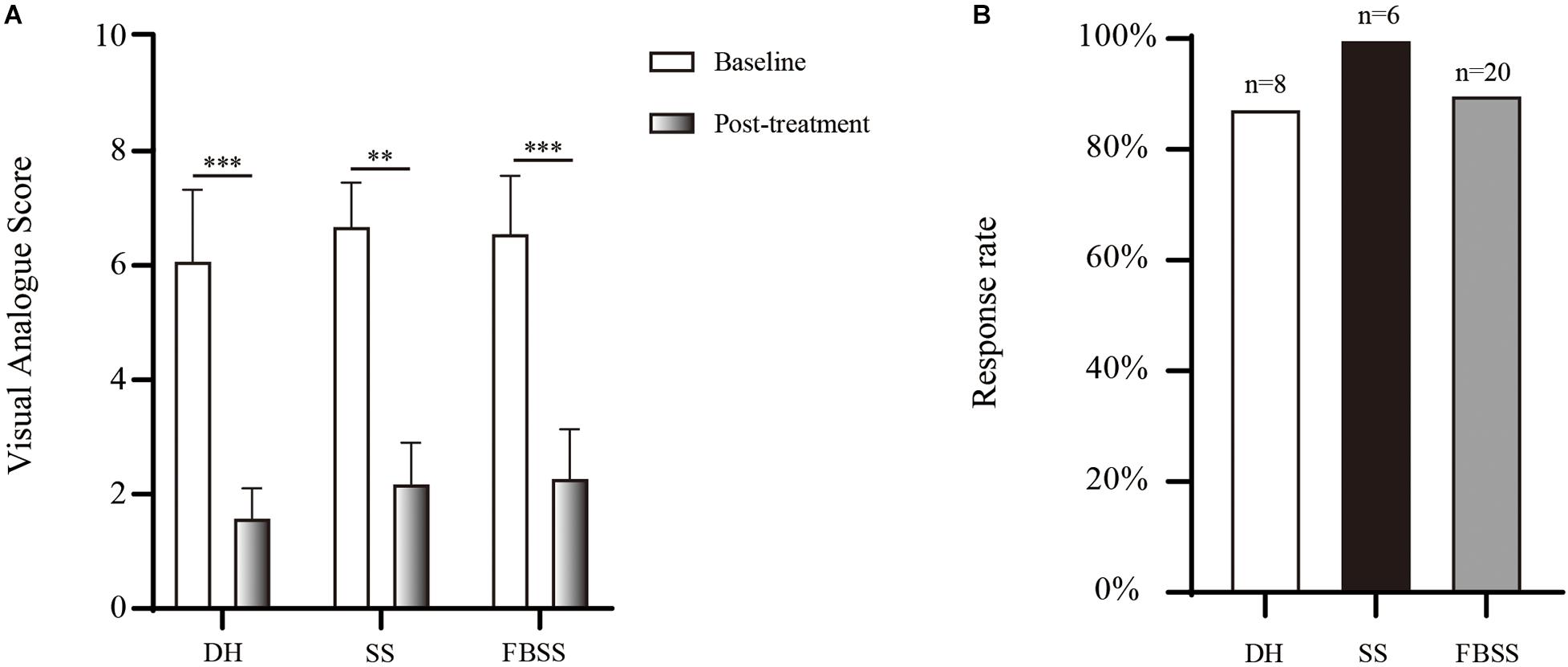
Figure 3. The initial analgesic effect provided by PRF and TESI. (A) Changes of pain score between pre- and post-treatment. (B) The initial response rate of each group. ∗∗p < 0.01, ∗∗∗p < 0.001.
Next, we compared the effect of PRF and TESI on pain scores between different groups at 1-month after discharge and the last follow-up (Figure 4). In general, the VAS decreased from 6.5 ± 1.0 to 2.4 ± 1.9 at the last follow-up. No significant difference of pain scores was observed between 1-month and the last follow-up across all etiologies. At the last follow-up, the long-term response rate was only 66.7% for SS population, and 70% for FBSS, respectively. The combination of PRF and TESI therapy provided an enduring pain relief up to the last follow-up in DH subgroup, with 87.5% of patients presented over 50% pain relief compared with baseline.
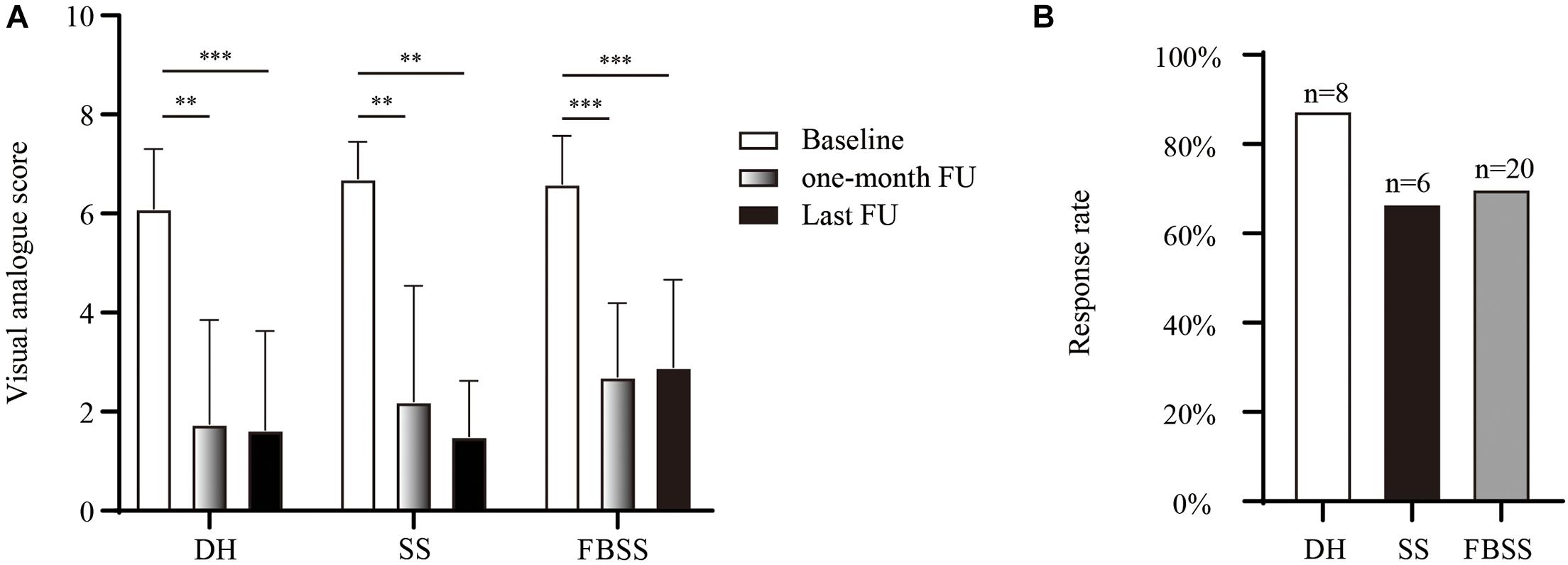
Figure 4. The long-term therapeutic effect. (A) Comparison of pain degree assessed by visual analog scores. (B) The long-term response rate of the last follow-up. ∗∗p < 0.01, ∗∗∗p < 0.001.
Discussion
LSRP is common and results from diverse etiologies, including DH, SS, and FBSS. One general feature of LSRP is sensitization of spinal nerve root or DRG, caused by mechanical, inflammatory, immune and neurophysiologic factors. Thus, novel neuromodulation therapy targeted DRG may provide an alternative option to treat LSRP.
The most common cause of LSRP is DH (Dydyk et al., 2021). However, only 24% (8/34) of patients were diagnosed with DH in this study. Majority of patients were those still presented radiating pain after spinal surgery. Similarly, the high incidence of longstanding pain with or without radicular pain ranged 20–40% in FBSS population (Thomson, 2013; Baber and Erdek, 2016). In addition, we found that over half of the participants experienced radicular pain associated with L4-5 distribution, which is consistent with previous data (DeFroda et al., 2016).
In recent years, radiofrequency therapy has evolved as a promising neuromodulatory technique for the management of various chronic pain syndromes, like radicular pain, trigeminal neuralgia, occipital pain, shoulder and knee pain (Vanneste et al., 2017; Huang et al., 2020). In current study, we applied PRF adjacent to the DRG to achieve relief from radicular pain caused by different etiologies. To our knowledge, only one study compared the clinical outcome of pulsed-radiofrequency for LSRP across different etiologies. Previous data indicated that PRF treatment was significantly more efficacious in DH and SS population than those with FBSS (Abejón et al., 2007). However, we did not observe any superior therapeutic effect in DH or SS cohort compared with FBSS in this study. One possible reason is the additional analgesic effect provided by TESI. Similarly, previous data has demonstrated that PRF combined with TESI achieved better clinical outcome of lumbar DH than PRF alone 1 month after procedure (Ding et al., 2018). Despite relief from pain, PRF can achieve significant functional improvement, demonstrated by the reduction of Oswestry Disability Index scores (Sansone et al., 2020). One significant limitation of this study was that we did not perform functional evaluation pre- and post-treatment systematically.
TESI is more specific and selected nerves can be targeted during treatment, compared with interlaminar or caudal route access. The degree of nerve root compression is the key factor to predict the long-term therapeutic effect (Ghahreman and Bogduk, 2011). Thus, one principle of our treatment is to initially identify and remove the severe compression responsible for the painful distribution. As a result, we recommended 7 patients for decompressive surgery (Figure 1) and none presented sustained radiating pain after procedure. One key factor of therapeutic effect is the ingredients present in the TESI, we administrated betamethasone during surgery based on our clinical routine. However, previous data has demonstrated that patient responded better to triamcinolone compared with betamethasone with TESI for LSRP (McCormick et al., 2015). It is essential to examine the superiority of different agents for TESI combined with PRF in the future study.
Meanwhile, patient who underwent spinal surgery may still experience pain due to previous sensitization of the nerve root (Dower et al., 2019). TESI may attenuate the pain symptom of FBSS patient by reducing the inflammatory process and desensitizing the inflamed nerve root, namely the “battered” root syndrome (Waisbrod and Gerbershagen, 1985; Ragab and Deshazo, 2008). Thus, we propose that the battered sensory nerve (nerve root and/or DRG) syndrome (BSNS) is the common pathological condition of LRSP, caused by distinct etiology. The chronicity of neuropathic pain caused by central or peripheral sensitization is the characteristic feature of BSNS.
One novel strategy of neuromodulation for LRSP is electrical DRG or spinal cord stimulation, which is most widely applied in patients with FBSS (Atallah et al., 2008; Kallewaard et al., 2019). Unlike PRF, functional electrical stimulator generates currents flow between the cathode and anode to interrupt the abnormal processing of pain signal. However, few patients can afford an expensive permanent stimulation device, and the risk of complication (e.g., lead migration, infection, and tolerance) increases with implantation duration (Eldabe et al., 2016). The mean total health care costs for the spinal cord stimulation treatment were almost 5 times more than those with conventional medical management (Manca et al., 2008). An obvious advantage of PRF or TESI is that the therapy can be repeated at low cost if necessary.
Current study has several main limitations. Firstly, the clinical data were collected retrospectively and the number of DH, and SS subgroup was smaller than FBSS. Actually, we found more patients presented intractable radicular pain with previous back surgery, compared with non-surgical population. Further study with larger cohort is needed to confirm the incidence of LRSP for individual etiology. Second, the uncontrolled nature of study design. Previous study has demonstrated the clinical efficacy was changed in different therapies (TESI vs. PRF vs. TESI combined PRF) (Ding et al., 2018). However, the superiority of each method in management of LRSP with distinct etiology remains unclear. It is essential to perform prospective, controlled study in the future to confirm the optimal indication of neuromodulation therapy.
Conclusion
In summary, PRF combined with TESI is an effective approach to treat LSRP in patients, providing considerable sustained relief from pain with distinct etiology.
Data Availability Statement
The data are not publicly available due to privacy and ethical reasons. The data presented in this study are available on reasonable request from the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by the ethics board of The Third Xiangya Hospital, Central South University (No. 21035). The patients/participants provided their written or verbal informed consent to participate in this study.
Author Contributions
HZ and DH: conceptualization, investigation, supervision, project administration, and funding acquisition. LY, YH, RHa, GG, YN, RHu, XY, DH, and HZ: methodology. LY, YH, and ZL: formal analysis. LY, ZL, and HZ: data curation. YH and HZ: writing—original draft preparation. HZ: writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by National Natural Science Foundation of China (81901146 to HZ and 81771101 to HZ and DH), the Key Laboratory of Hunan Province grants (2018TP1009 to HZ and DH), and the Huizhiyucai Project of The Third Xiangya Hospital, Central South University.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abejón, D., Garciadel-Valle, S., Fuentes, M. L., Gómez-Arnau, J. I., Reig, E., and van Zundert, J. (2007). Pulsed radiofrequency in lumbar radicular pain: clinical effects in various etiological groups. Pain Pract. 7, 21–26. doi: 10.1111/j.1533-2500.2007.00105.x
Atallah, J., Armah, F., Wong, D., Weis, P., and Fahy, B. (2008). Use of spinal cord stimulator for treatment of lumbar radiculopathy in a patient with severe kyphoscoliosis. Pain Physician 11, 555–559. doi: 10.36076/ppj.2008/11/555
Baber, Z., and Erdek, M. A. (2016). Failed back surgery syndrome: current perspectives. J. Pain Res. 9, 979–987. doi: 10.2147/jpr.s92776
Clingan, J. A., Patel, A., and Maher, D. P. (2020). Survey of spinal cord stimulation hardware currently available for the treatment of chronic pain in the United States. Front. Pain Res. 1:572907. doi: 10.3389/fpain.2020.572907
DeFroda, S., Daniels, A., and Deren, M. (2016). Differentiating radiculopathy from lower extremity arthropathy. Am. J. Med. 129:1124.e1-7.
Ding, Y., Li, H., Zhu, Y., Yao, P., and Zhao, G. (2018). Transforaminal epidural steroid injection combined with pulsed radio frequency on spinal nerve root for the treatment of lumbar disc herniation. J. Pain Res. 11, 1531–1539. doi: 10.2147/jpr.s174318
Dower, A., Davies, M. A., and Ghahreman, A. (2019). Pathologic basis of lumbar radicular pain. World Neurosurg 128, 114–121. doi: 10.1016/j.wneu.2019.04.147
Dydyk, A. M., Khan, M. Z., and Das, J. M. (2021). Radicular Back Pain. In: StatPearls. Treasure Island, FL: StatPearls Publishing.
Eldabe, S., Buchser, E., and Duarte, R. (2016). Complications of spinal cord stimulation and peripheral nerve stimulation techniques: a review of the literature. Pain Med. 17, 325–336.
Ghahreman, A., and Bogduk, N. (2011). Predictors of a favorable response to transforaminal injection of steroids in patients with lumbar radicular pain due to disc herniation. Pain Med. 12, 871–879. doi: 10.1111/j.1526-4637.2011.01116.x
Hetta, D. F., Mohamed, S. A. B., Mohamed, K. H., Mahmoud, T. A. E., and Eltyb, H. A. (2020). Pulsed radiofrequency on thoracic dorsal root ganglion versus thoracic paravertebral nerve for chronic postmastectomy pain, a randomized trial: 6-month results. Pain Physician 23, 23–35.
Huang, Y., Deng, Q., Yang, L., Ma, J., Wang, Z., Huang, D., et al. (2020). Efficacy and safety of ultrasound-guided radiofrequency treatment for chronic pain in patients with knee osteoarthritis: a systematic review and meta-analysis. Pain Res. Manag. 2020:2537075.
Kallewaard, J., Nijhuis, H., Huygen, F., Wille, F., Zuidema, X., van de Minkelis, J., et al. (2019). Prospective cohort analysis of DRG stimulation for failed back surgery syndrome pain following lumbar discectomy. Pain Pract. 19, 204–210.
Koh, W., Choi, S.-S., Karm, M. H., Suh, J. H., Leem, J. G., Lee, J. D., et al. (2015). Treatment of chronic lumbosacral radicular pain using adjuvant pulsed radiofrequency: a randomized controlled study. Pain Med. 16, 432–441. doi: 10.1111/pme.12624
Lee, S. H., Choi, H. H., Roh, E. Y., and Chang, M. C. (2020). Effectiveness of ultrasound-guided pulsed radiofrequency treatment in patients with refractory chronic cervical radicular pain. Pain Physician 23, E265–E272.
Manca, A., Kumar, K., Taylor, R. S., Jacques, L., Eldabe, S., Meglio, M., et al. (2008). Quality of life, resource consumption and costs of spinal cord stimulation versus conventional medical management in neuropathic pain patients with failed back surgery syndrome (PROCESS trial). Eur. J. Pain 12, 1047–1058. doi: 10.1016/j.ejpain.2008.01.014
McCormick, Z., Kennedy, D. J., Garvan, C., Rivers, E., Temme, K., Margolis, S., et al. (2015). Comparison of pain score reduction using triamcinolone vs. betamethasone in transforaminal epidural steroid injections for lumbosacral radicular pain. Am. J. Phys. Med. Rehabil. 94, 1058–1064. doi: 10.1097/phm.0000000000000296
Oliveira, C. B., Maher, C. G., Ferreira, M. L., Hancock, M. J., Oliveira, V. C., McLachlan, A. J., et al. (2020). Epidural corticosteroid injections for lumbosacral radicular pain. Cochrane Database Syst. Rev. 4:CD013577.
Park, C. H., and Lee, S. H. (2019). The outcome of pulsed radiofrequency treatment according to electodiagnosis in patients with intractable lumbosacral radicular pain. Pain Med. 20, 1697–1701. doi: 10.1093/pm/pnz028
Rados, I., Sakic, K., Fingler, M., and Kapural, L. (2011). Efficacy of interlaminar vs transforaminal epidural steroid injection for the treatment of chronic unilateral radicular pain: prospective, randomized study. Pain Med. 12, 1316–1321. doi: 10.1111/j.1526-4637.2011.01213.x
Ragab, A., and Deshazo, R. D. (2008). Management of back pain in patients with previous back surgery. Am. J. Med. 121, 272–278. doi: 10.1016/j.amjmed.2008.01.004
Sansone, P., Giaccari, L. G., Lippiello, A., Aurilio, C., Paladini, A., Passavanti, M. B., et al. (2020). Pulsed radiofrequency for lumbar facet joint pain: a viable therapeutic option? a retrospective observational study. Pain Ther. 9, 573–582. doi: 10.1007/s40122-020-00187-z
Thomson, S. (2013). Failed back surgery syndrome–definition, epidemiology and demographics. Br. J. Pain 7, 56–59. doi: 10.1177/2049463713479096
Tortora, F., Negro, A., Russo, C., Cirillo, S., and Caranci, F. (2021). Chronic intractable lumbosacral radicular pain, is there a remedy? Pulsed radiofrequency treatment and volumetric modifications of the lumbar dorsal root ganglia. Radiol. Med. 126, 124–132. doi: 10.1007/s11547-020-01212-z
Trinidad, J. M., Carnota, A. I., Failde, I., and Torres, L. M. (2015). Radiofrequency for the treatment of lumbar radicular pain: impact on surgical indications. Pain Res. Treat. 2015:392856.
Van Boxem, K., Cheng, J., Patijn, J., van Kleef, M., Lataster, A., Mekhail, N., et al. (2010). 11. Lumbosacral radicular pain. Pain Pract. 10, 339–358. doi: 10.1111/j.1533-2500.2010.00370.x
Vanneste, T., Van Lantschoot, A., Van Boxem, K., and Van Zundert, J. (2017). Pulsed radiofrequency in chronic pain. Curr. Opin. Anaesthesiol. 30, 577–582.
Waisbrod, H., and Gerbershagen, H. (1985). Spinal cord stimulation in patients with a battered root syndrome. Arch. Orthop. Trauma Surg. 104, 62–64. doi: 10.1007/bf00449960
Keywords: neuromodulation, pulsed radiofrequency, transforaminal epidural steroid injection, disc herniation, spinal stenosis, failed back surgery syndrome, radicular pain, chronic pain
Citation: Yang L, Huang Y, Ma J, Li Z, Han R, Guo G, Ni Y, Hu R, Yan X, Zhou H and Huang D (2021) Clinical Outcome of Pulsed-Radiofrequency Combined With Transforaminal Epidural Steroid Injection for Lumbosacral Radicular Pain Caused by Distinct Etiology. Front. Neurosci. 15:683298. doi: 10.3389/fnins.2021.683298
Received: 20 March 2021; Accepted: 28 June 2021;
Published: 28 July 2021.
Edited by:
Hari S. Sharma, Uppsala University, SwedenReviewed by:
Aritra Kundu, University of Texas at Austin, United StatesSeaab Imad Sahib, University of Arkansas, United States
Copyright © 2021 Yang, Huang, Ma, Li, Han, Guo, Ni, Hu, Yan, Zhou and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dong Huang, SHVhbmdkb25nNjYxOUB2aXAuMTYzLmNvbQ==; Haocheng Zhou, SGFvY2hlbmcuemhvdUBjc3UuZWR1LmNu
†These authors have contributed equally to this work
 Liuqing Yang
Liuqing Yang Yuzhao Huang
Yuzhao Huang Jiahui Ma1
Jiahui Ma1 Rui Han
Rui Han Haocheng Zhou
Haocheng Zhou