- 1Department of Rehabilitation, Xinhua Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
- 2Chongming Hospital, Shanghai University of Medicine and Health Sciences, Shanghai, China
Objective: Traditional Chinese Medicine (TCM) has considerable experience in the treatment of cerebral palsy (CP), but little evidence shows the effect of a combination of TCM and modern rehabilitation therapies on CP. This systematic review aims to evaluate the effect of integrated TCM and modern rehabilitation therapies on motor development in children with CP.
Methods: We systematically searched five databases up to June 2022, including PubMed, the Cumulative Index to Nursing and Allied Health, Cochrane Library, Embase, and Web of Science. Gross motor function measure (GMFM) and Peabody Development Motor Scales-II were the primary outcomes to evaluate motor development. Secondary outcomes included the joint range of motion, the Modified Ashworth scale (MAS), the Berg balance scale, and Activities of Daily living (ADL). Weighted mean differences (WMD) and 95% confidence intervals (CIs) were used to determine intergroup differences.
Results: A total of 2,211 participants from 22 trials were enrolled in this study. Among these, one study was at a low risk of bias and seven studies showed a high risk of bias. Significant improvements were found in GMFM-66 (WMD 9.33; 95% CI 0.14–18.52, P < 0.05, I2 = 92.1%), GMFM-88 (WMD 8.24; 95% CI 3.25–13.24, P < 0.01, I2 = 0.0%), Berg balance scale (WMD 4.42; 95% CI 1.21–7.63, P < 0.01, I2 = 96.7%), and ADL (WMD 3.78; 95% CI 2.12–5.43, P < 0.01, I2 = 58.8%). No adverse events were reported during the TCM intervention in the included studies. The quality of evidence was high to low.
Conclusion: Integrated TCM and modern rehabilitation therapies may be an effective and safe intervention protocol to improve gross motor function, muscle tone, and the functional independence of children with CP. However, our results should be interpreted carefully because of the heterogeneity between the included studies.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/, identifier CRD42022345470.
1. Introduction
Cerebral palsy (CP) is a group of persistent motor and postural development disorders with participation limitations caused by non-progressive brain lesions (Michael-Asalu et al., 2019). CP is mainly divided into seven types: spastic quadriplegia, spastic diplegia, spastic hemiplegia, dyskinesia, ataxia, Worster-Drought syndrome, and mixed types (Chinese Association of Rehabilitation Medicine Pediatric Rehabilitation Committee et al., 2022a). Most children with CP are spastic (85–91%), with symptoms of muscle stiffness (Novak et al., 2017).
Cerebral palsy is a frequent cause of physical disability in children. Functional independence and social participation may be influenced by motor dysfunction, pain, and cognitive impairment in children with CP (Lindsay, 2016). Because of the irreversible brain damage in CP, comprehensive rehabilitation therapies for motor function, cognition, language, and daily living ability are widely used in children with CP (Vargus-Adams and Martin, 2011). Evidence showed that exercise interventions significantly improved gait speed and muscle strength in children with CP (Liang et al., 2021). Invasive therapies, such as selective dorsal rhizotomy, botulinum toxin-A therapy, and intrathecal baclofen therapy, were effective in reducing muscle tone, which can be employed in children with spastic CP (Damiano et al., 2021).
Traditional Chinese medicine (TCM) has been reported as an alternative therapy to CP treatment. CP is described as “congenital deficiencies,” “retardation,” and “weakness” in the view of TCM. Congenital deficiencies lead to loss of nutrients in the meridians and musculoskeletal system, which prevents the meridians from mobilizing the bones, causing joint stiffness. The spleen and stomach promote the development of the children via nutrient absorption, and weakness of the spleen and stomach are associated with a deficiency of kidney essence, which results in developmental delay. The treatment strategy is to stretch and dredge the meridian, and warm and nourish the spleen and kidney to condition the poor state of the congenial deficiencies and the acquired weakness of the spleen and kidney. At the same time, treatment should also focus on mind refreshing and wisdom increasing, because of the lesions of the brain in children with CP. TCM treatments, which include massage, acupuncture, herbs, and Qigong, have been practiced in the treatment of CP for a long time. One study showed that TCM may improve the posture balance and cognition of rats with CP (Niu et al., 2021). Increased secretion of dopamine, brain-derived neurotrophic factor, and nerve growth factor were discovered after stimulations on the meridian in rats, which helped repair neuronal damage (Chuang et al., 2007; Tao et al., 2016). Studies suggested that massage and acupuncture dilate blood vessels and increase blood flow and oxygen supply by stimulating acupoints in children with CP, which may improve the function and metabolism of brain cells and muscles (Wang and Wu, 2005; Wu et al., 2008).
Although modern rehabilitation therapies were widely recommended by the guidelines as the first-line treatment for children with CP (Castelli and Fazzi, 2016; Verschuren et al., 2016; Damiano et al., 2021), there was a paucity of evidence on whether TCM is a beneficial supplement to modern rehabilitation therapy to improve the motor development in children with CP. This systematic review aims to clarify the effectiveness of integrated TCM and modern rehabilitation therapies on motor development compared to modern rehabilitation therapies only in children with CP, and we hypothesize that the combination of TCM and modern rehabilitation therapies may be better in the improvement of motor development than modern rehabilitation therapies only.
2. Materials and methods
This systematic review was conducted under the guidance of the Cochrane Handbook for Systematic Reviews of Interventions (Cumpston et al., 2019). To find relevant studies published until June 2022, we systematically searched PubMed, the Cumulative Index to Nursing and Allied Health, Cochrane Library, Embase, and Web of Science. Search terms, such as “traditional Chinese medicine,” “TCM,” “cerebral palsy,” and “motor function,” were used, and the full search strategy was listed in the Supplementary material. The references of enrolled studies were screened to find additional eligible articles. The protocol of this systematic review has been registered in PROSPERO (No. CRD42022345470).
2.1. Eligibility criteria
The enrolled studies should meet the following conditions: (1) Participants: infants or children under 18 years old with a clear diagnosis of CP and with abnormalities in motor function or postural development. (2) Interventions: TCM treatments combine with conventional modern rehabilitation therapies. (3) Comparisons: conventional modern rehabilitation like physical therapy, occupational therapy, or speech therapy. (4) Outcome measures: primary outcome measures: ➀ Gross motor function measure (GMFM)-66 and GMFM-88 (Te Velde and Morgan, 2022): measurement of motor function of decubitus position, turn-over, sitting position, creeping, and kneeling, erect position, walking, running, and jumping. ➁ Fine motor function measure: 2 subscales (grasping and visual-motor integration) of Peabody Development Motor Scales-II (Fay et al., 2019). Secondary outcome measures: ➀ Muscle tone: Joint range of motion and modified Ashworth scale (MAS) (Bohannon and Smith, 1987). ➁ Balance function: the Berg balance scale (Downs, 2015). ➂ Activities of daily living (ADL): cerebral palsy specified ADL scale to measure functional independence (Deng et al., 2005; Zhang and Hu, 2012). (5) Study design: Randomized Controlled Trial (RCT). (6) Language: English and Chinese.
2.2. Exclusion criteria
(1) Patients with serious heart, lung, or nerve diseases. (2) Concomitant invasive treatments in the intervention group or the control group, including surgery and botulinum toxin injecting. (3) Any TCM treatment that was used in control groups.
2.3. Data extraction
Two reviewers (Z.C. and Z.H.) independently screened the enrolled articles through title and abstract screening and full-text reading. Data were extracted under the guidance of Cochrane Collaboration by Z.C. and Z.H. Extracted data included: publication year, author name, demographics, the severity of CP, data on outcome measures, and adverse events. A third reviewer (Q.D.) would participate in the discussion when disagreements arise.
2.4. Quality assessment
The Cochrane risk of bias tool was used to assess the methodological quality of the included studies. The evidence quality was measured by Grading of Recommendation Assessment, Development, and Evaluation (GRADE). The quality appraisal was done by Z.H.
2.5. Statistical analysis
Stata version 16.0 (StataCorp, College Station, TX, USA) was used for data analysis. The fixed effects model would be chosen for quantitative analysis if there was no significant heterogeneity, otherwise random effects model would be used. The results would be presented as weighted mean difference (WMD) and 95% confidence interval (CI) with a significance value set as 0.05. Data would be synthesized if there were over two TCM intervention groups in one research. Heterogeneity was determined by I2 statistics with a significant value set as 50%. A sensitivity test was used to identify the outlying studies that may influence the between-study heterogeneity. Review Manager 5.0 (The Cochrane Collaboration, Copenhagen, Denmark) was used to generate the bias chart of risk of bias evaluation.
3. Results
We obtained 485 relevant papers from the five databases, and 205 articles were removed as duplicates. The remind 280 articles were evaluated based on the relevance and publication type, and 233 articles with obvious irrelevant topics or non-RCTs were ruled out. After the full-text reading, 22 RCTs inclusion met the eligibility criteria. The screening flow diagram is described in Figure 1.
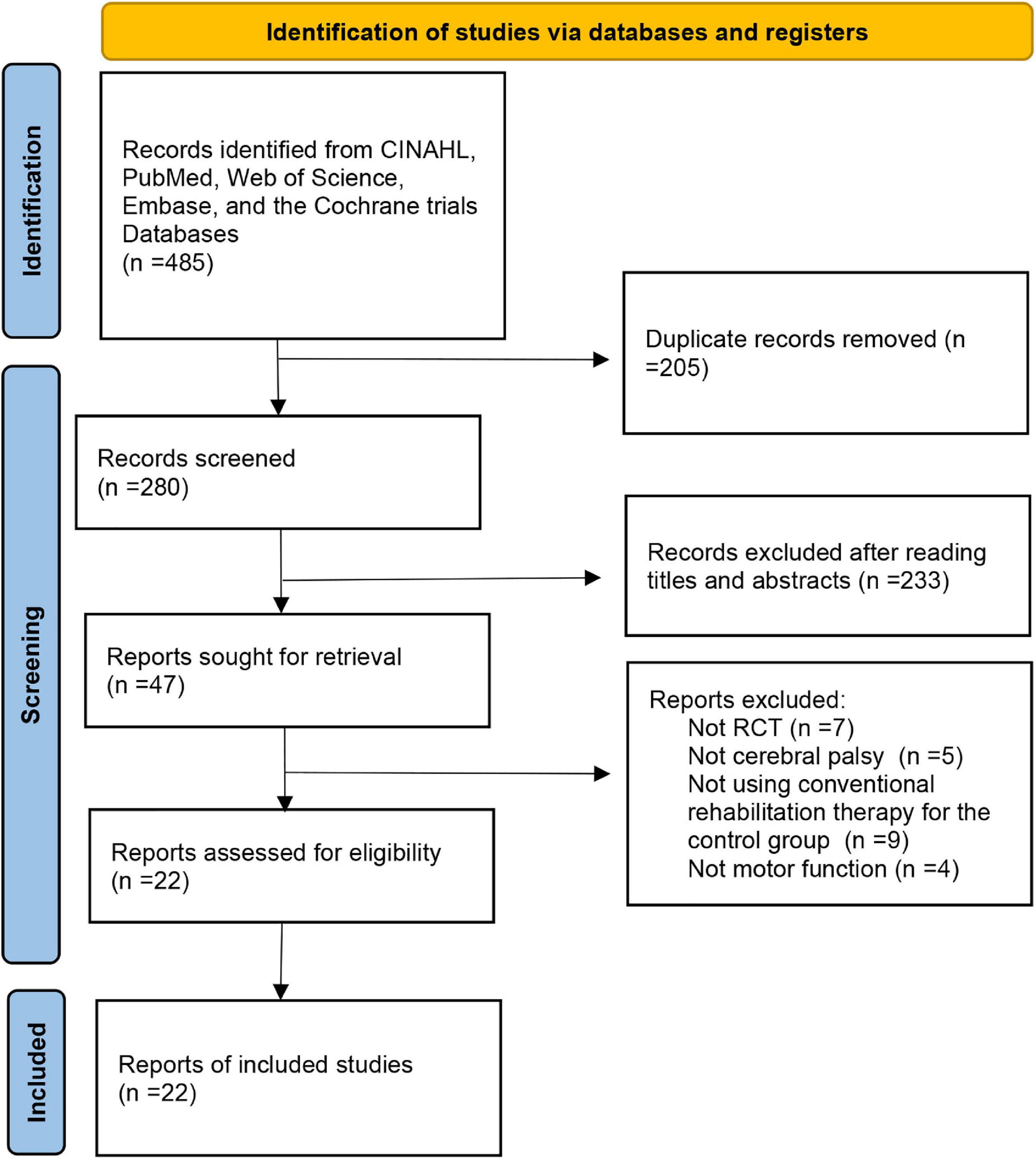
Figure 1. Flowchart of the process of literature search and extraction of studies meeting the inclusion criteria.
3.1. Studies’ characteristics
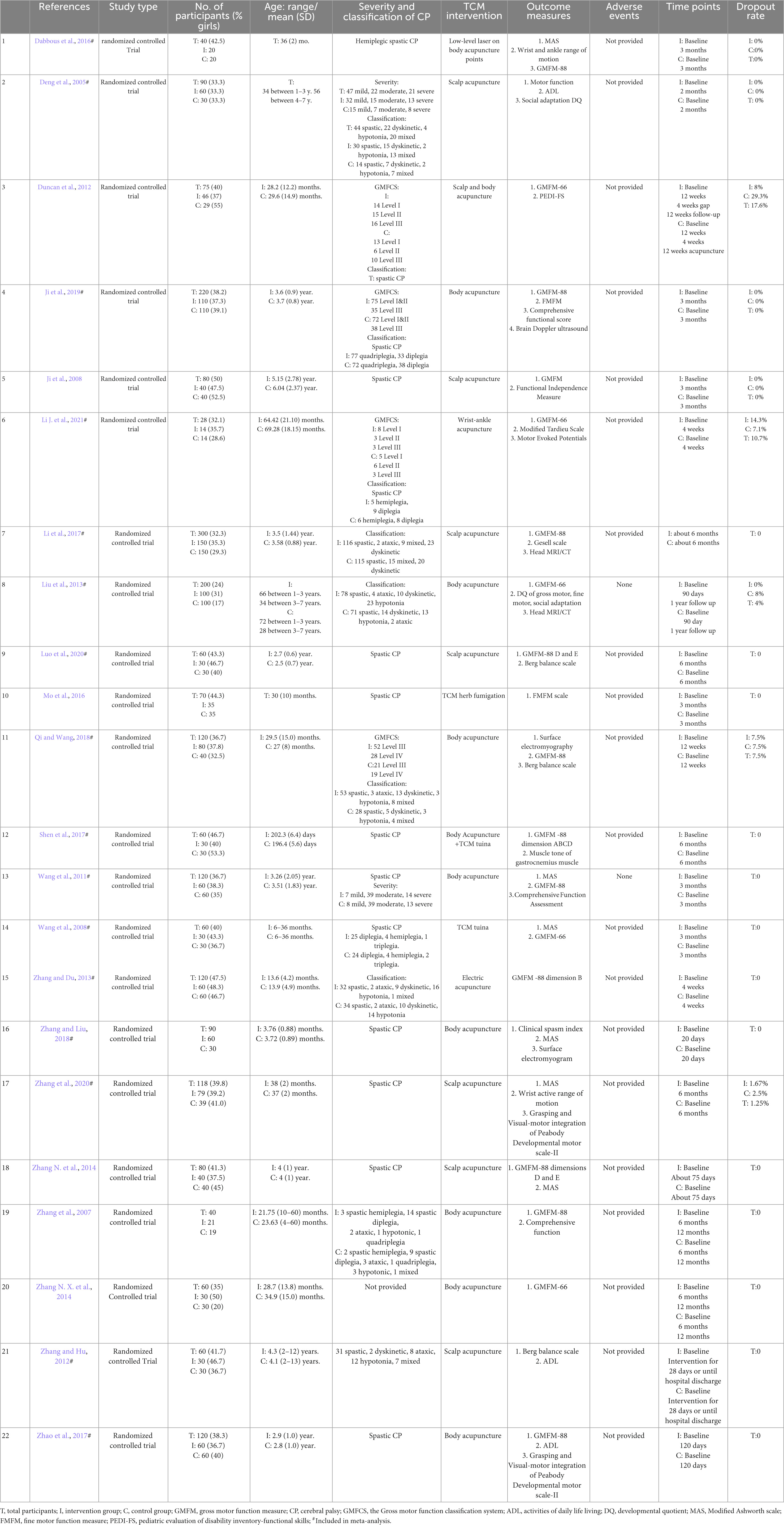
The demographics of the included studies, consisting of author year, number of participants, age, type of CP, outcome measures, significant results, and loss to follow-up, are shown in a customized Table 1. The intervention method, treatment frequency, and treatment duration of the intervention group and the control group are shown in Table 2.
Table 2. Traditional Chinese medicine combined with rehabilitation and control interventions in the included trials.
This review includes 22 articles published from 2005 to 2021, and data from 15 studies were included in the meta-analysis. This systematic review included 2,211 children aged 4 months to 13 years old. The participants in both the intervention group and control group were diagnosed with spasticity, dyskinesia, ataxia, or mixed types of CP depending on the types of motor abnormalities. Hemiplegia, diplegia, or quadriplegia is further diagnosed according to the affected body parts in children with spasticity CP (Sellier et al., 2016; Novak et al., 2017). All included studies were RCTs in English and Chinese language.
The duration of intervention for children with CP ranged from 20 days to 6 months, and the frequency of treatment ranged from 2 to 7 days per week. The duration of TCM treatments was 10–240 min with a median of 45 min. The duration of modern rehabilitation therapies ranged from 30 min to 240 min, and the median duration was 55 min. All participants received conventional modern rehabilitation therapy, and the intervention group was additionally treated with TCM. Modern rehabilitation therapy includes physiotherapy (Zhang et al., 2007; Duncan et al., 2012; Liu et al., 2013; Li et al., 2017), occupational therapy (Zhang et al., 2007; Wang et al., 2011; Duncan et al., 2012; Liu et al., 2013; Zhang and Liu, 2018), speech therapy (Zhang et al., 2007; Wang et al., 2011; Liu et al., 2013; Li et al., 2017; Zhang and Liu, 2018), and hydrotherapy (Dabbous et al., 2016). Fifteen studies explicitly used Bobath therapy (Zhang et al., 2007, 2020; Ji et al., 2008, 2019; Wang et al., 2008, 2011; Zhang and Hu, 2012; Liu et al., 2013; Zhang N. X. et al., 2014; Mo et al., 2016; Li et al., 2017; Shen et al., 2017; Zhao et al., 2017; Qi and Wang, 2018; Zhang and Liu, 2018), and 5 conducted ADL training (Deng et al., 2005; Zhang et al., 2007, 2020; Duncan et al., 2012; Mo et al., 2016). Zhang et al. (2020) used biofeedback therapy, and Zhang N. et al. (2014) added virtual reality games for treatment. In the TCM treatment of the intervention group, 21 studies applied acupuncture treatment, 2 studies used massage therapy (Wang et al., 2008; Shen et al., 2017), and 1 study applied TCM fumigation (Mo et al., 2016). Particularly, 10 studies applied scalp acupuncture (Deng et al., 2005; Zhang et al., 2007, 2020; Ji et al., 2008; Duncan et al., 2012; Zhang and Hu, 2012; Liu et al., 2013; Zhang N. X. et al., 2014; Li et al., 2017; Luo et al., 2020).
3.2. Primary outcomes
3.2.1. Gross motor function measure
Four studies evaluated gross motor function according to GMFM-66 (Wang et al., 2008; Duncan et al., 2012; Liu et al., 2013; Li J. et al., 2021). One study provided average GMFM-66 scores without standard deviation, which was excluded from the meta-analysis (Duncan et al., 2012). The pooled analysis reported a significantly better improvement in GMFM-66 in intervention groups than in control groups (WMD 9.33; 95% CI 0.14–18.52, P = 0.047, I2 = 92.1%) (Figure 2A). When Liu et al. (2013) was excluded from the pooled results according to the sensitivity analysis, there were still significant differences between the two groups without significant heterogeneity (WMD 3.30; 95% CI 1.62–4.97, P < 0.001, I2 = 47.4%).
Figure 2. Forest plot of pooled results for gross motor function measure (GMFM) (A) GMFM–66. (B) GMFM–88. (C) GMFM–88–Dimension A. (D) GMFM–88–Dimension B. (E) GMFM–88–Dimension C. (F) GMFM–88–Dimension D. (G) GMFM–88–Dimension E.
GMFM-88 consists of 88 items in five dimensions: dimension A (lying and rolling), dimension B (sitting), dimension C (crawling and kneeling), dimension D (standing), and dimension E (walking, running, and jumping). Twelve studies applied GMFM-88 or part of GMFM-88 to measure gross motor function. We analyzed each of the five dimensions and the total score of GMFM-88.
The sum of five dimension scores of GMFM-88: Pooled data from 2 studies (Zhang et al., 2007; Zhao et al., 2017) showed a significant result (WMD 8.24; 95% CI 3.25–13.24, P = 0.001, I2 = 0.0%) (Figure 2B).
Dimension A: Pooled data from 3 studies (Li et al., 2017; Shen et al., 2017; Ji et al., 2019) showed a significant result (WMD 6.63; 95% CI 5.36–7.91, P < 0.001, I2 = 0.0%) (Figure 2C).
Dimension B: Pooled data from 5 studies (Zhang and Du, 2013; Li et al., 2017; Shen et al., 2017; Qi and Wang, 2018; Ji et al., 2019) showed a significant result (WMD 5.76; 95% CI 3.20–8.31, P < 0.001, I2 = 84.6%) (Figure 2D). After removing Zhang and Du (2013) based on sensitivity analysis, the pooled results still showed significant differences between the intervention group and the control group while there was no significant heterogeneity (WMD 7.07; 95% CI 5.90–8.23, P < 0.001, I2 = 27.4%).
Dimension C: Pooled data from 4 studies (Li et al., 2017; Shen et al., 2017; Qi and Wang, 2018; Ji et al., 2019) showed a significant result (WMD 4.83; 95% CI 2.62–7.04, P < 0.001, I2 = 79.6%) (Figure 2E). After removing Qi and Wang (2018), there were still significant differences between the intervention group and the control group without significant heterogeneity (WMD 5.49; 95% CI 4.60–6.38, P < 0.001, I2 = 47.7%).
Dimension D: Pooled data from 5 studies (Li et al., 2017; Shen et al., 2017; Qi and Wang, 2018; Ji et al., 2019; Luo et al., 2020) showed a significant result (WMD 2.88; 95% CI 1.33–4.43, P < 0.001, I2 = 82.6%) (Figure 2F). After removing Ji et al. (2019) from the pooled data based on sensitivity analysis, there was no significant statistical heterogeneity, but the intervention group still showed a significantly better effect than the control group (WMD 3.18; 95% CI 2.39–3.97, P < 0.001, I2 = 0.0%).
Dimension E: Pooled data from 4 studies (Li et al., 2017; Qi and Wang, 2018; Ji et al., 2019; Luo et al., 2020) showed no significant result (WMD 4.49; 95% CI −0.82 to 9.79, P = 0.097, I2 = 95.9%) (Figure 2G). After removing Luo et al. (2020) from the pooled results based on the sensitivity analysis, no significant results were found (WMD 0.39; 95% CI −0.27 to 1.05, P = 0.248, I2 = 37.7%).
3.2.2. Fine motor function measure
Two studies, respectively measured fine motor development using the grasping and visual-motor subscales of the Peabody Development Motor Scales-II (Zhao et al., 2017; Zhang et al., 2020). No significant changes were found in neither grasping part (WMD 3.46; 95% CI −1.77 to 8.70, P = 0.195, I2 = 91.8%) nor visual-motor integration part (WMD 3.08; 95% CI −2.78 to 8.93, P = 0.303, I2 = 82.2%) (Figures 3A, B).
Figure 3. Forest plot of pooled results for Peabody Development Motor Scales-II (A) Peabody Developmental Motor Scales–Grasping. (B) Peabody Developmental Motor Scales–Visual motor integration.
3.3. Secondary outcomes
3.3.1. Joint range of motion
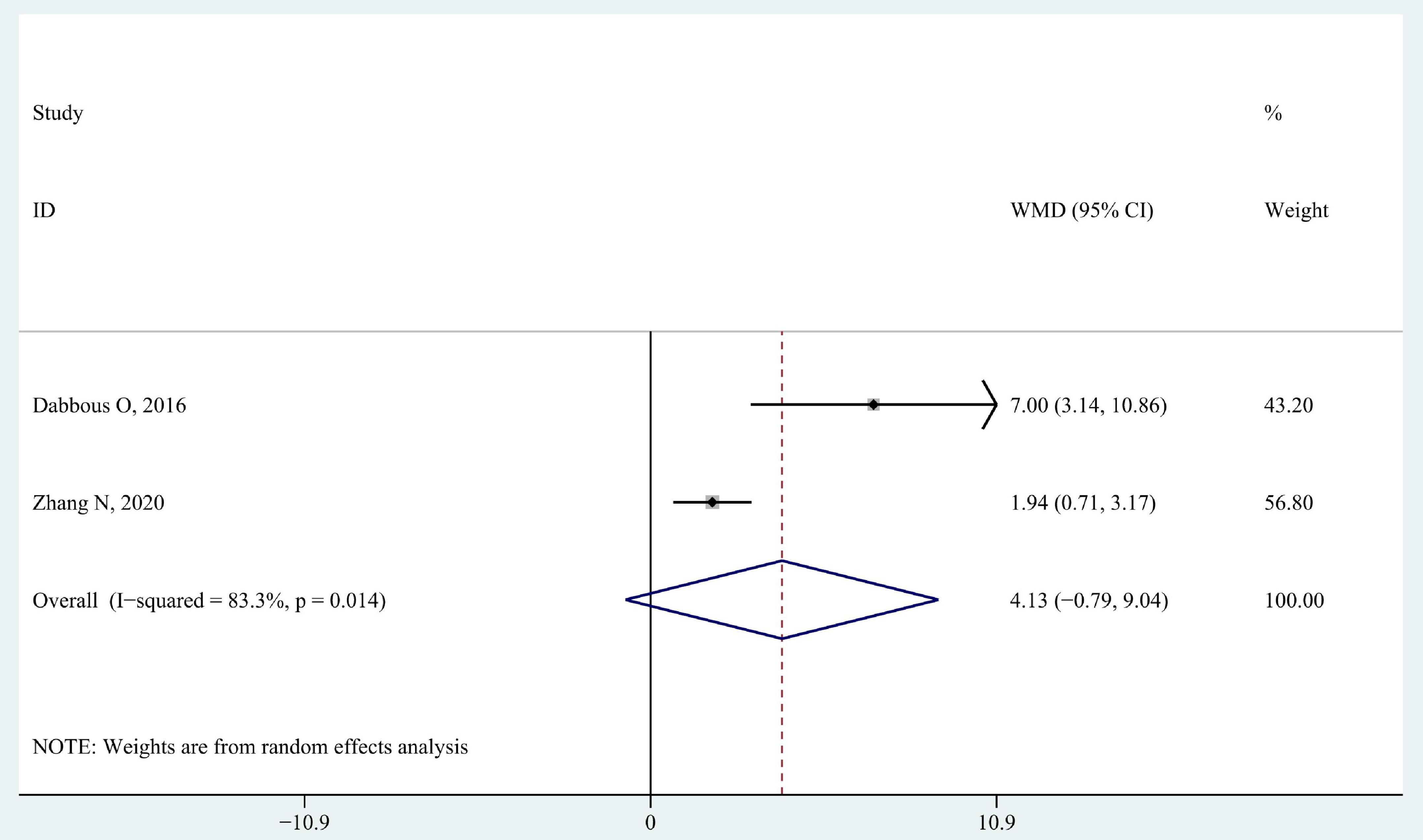
Two studies that recruited children with hemiplegia spastic CP used the joint range of motion to measure the changes in spasticity. Dabbous et al. (2016) described flexion, and extension of the wrist and ankle while Zhang et al. (2020) measured the wrist active extension. It showed no significant differences in wrist extension range of motion when data were pooled (WMD 4.13; 95% CI −0.79 to 9.04, P = 0.100, I2 = 83.3%) (Figure 4).
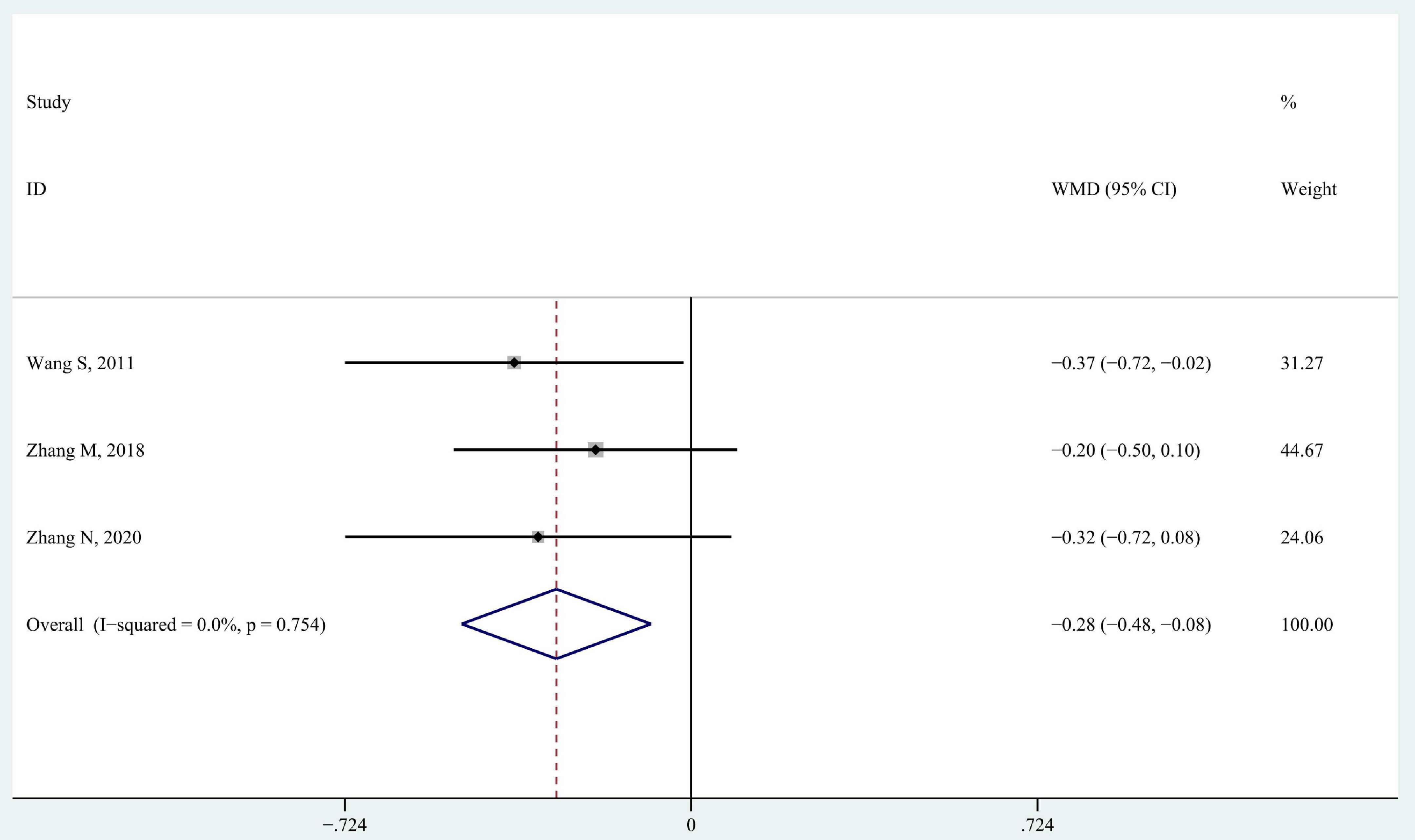
3.3.2. Modified Ashworth scale
Modified Ashworth scale includes six levels to describe muscular tone (0, 1, 1+, 2, 3, 4, from normal to high). We replaced these six levels with scores ranging from 0 to 5 from low to high in data analysis. Three studies recruited children with spastic CP and used MAS to measure the changes in spasticity (Wang et al., 2011; Zhang and Liu, 2018; Zhang et al., 2020). The results showed that the MAS level decreased more in intervention groups than in control groups when data from the three studies were pooled together (WMD −0.28; 95% CI −0.48 to −0.08, P = 0.005, I2 = 0%) (Figure 5).
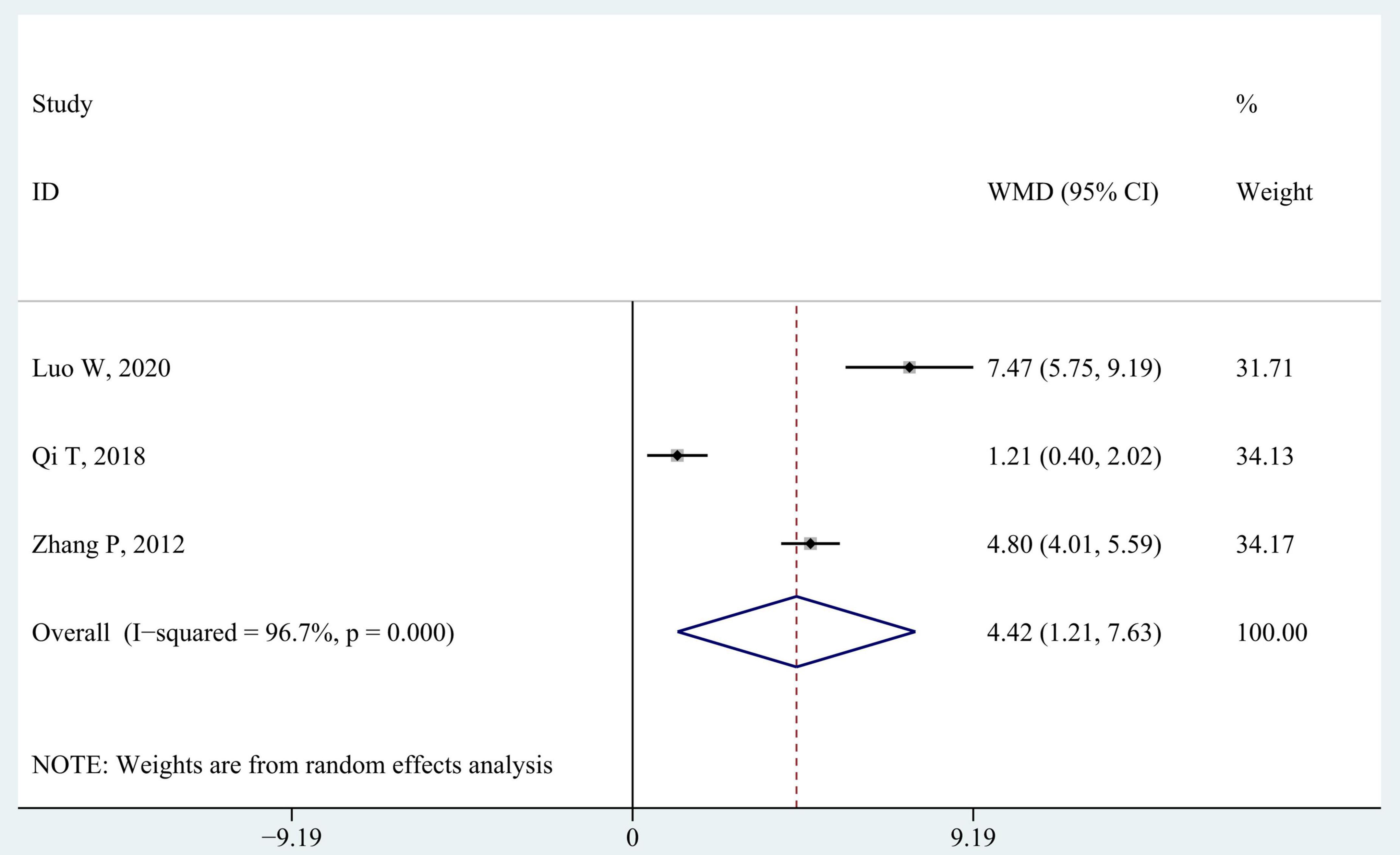
3.3.3. Berg balance scale
Berg balance scale is used in three studies to evaluate static and dynamic balance (Zhang and Hu, 2012; Qi and Wang, 2018; Luo et al., 2020). As shown in Figure 6, children in intervention groups achieved significantly better improvement in balance ability than those in control groups (WMD 4.42; 95% CI 1.21–7.63, P = 0.007, I2 = 96.7%). There was still significant heterogeneity between studies (all I2 > 80%) when the three studies were eliminated from the pooled data gradually through the sensitivity analysis.
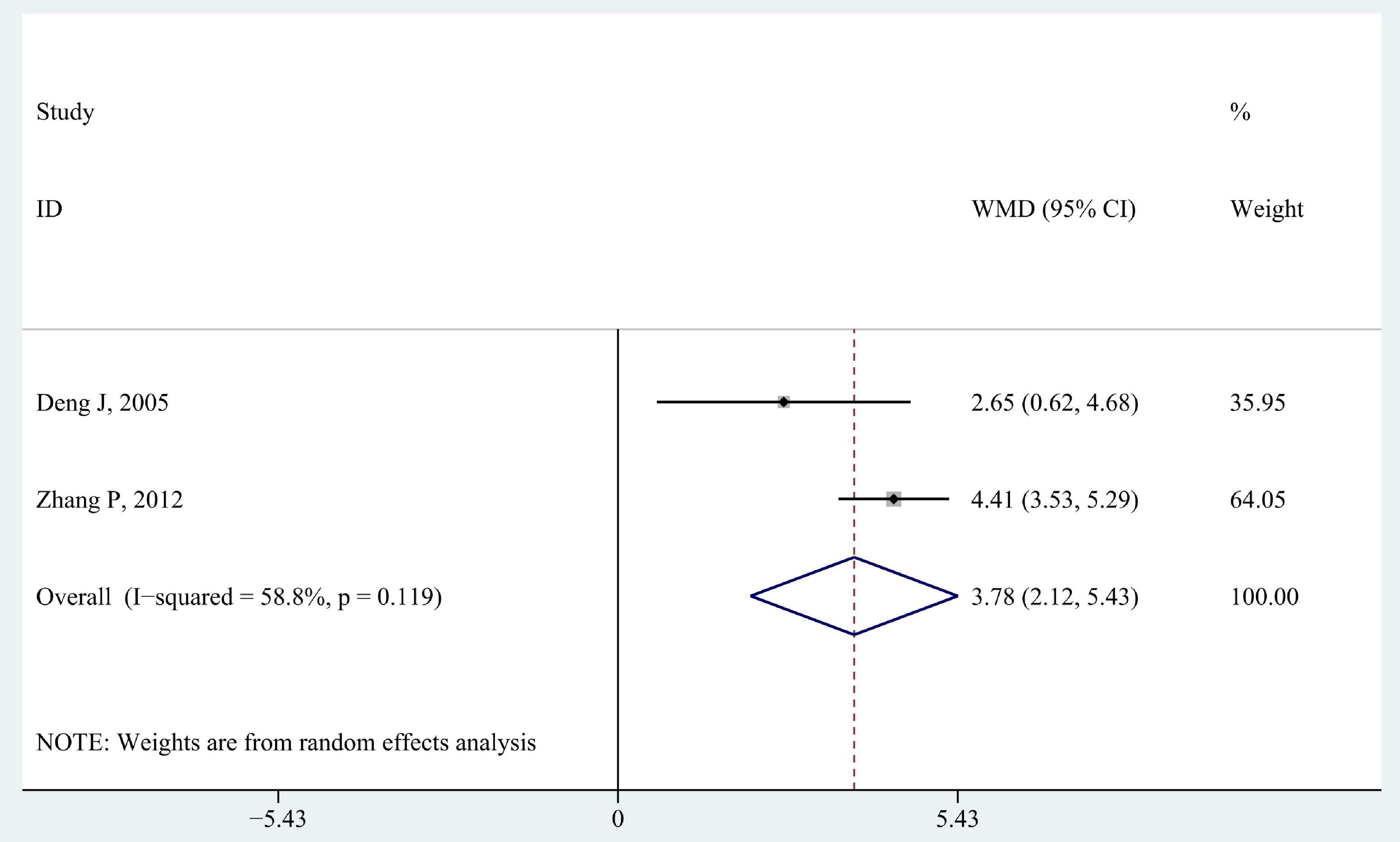
3.3.4. Activities of daily living
Two studies reported ADL scores (Figure 7; Deng et al., 2005; Zhang and Hu, 2012). The pooled analysis reported a significantly better improvement in ADL scores in intervention groups than that in control groups (WMD 3.78; 95% CI 2.12–5.43, P < 0.001, I2 = 58.8%).
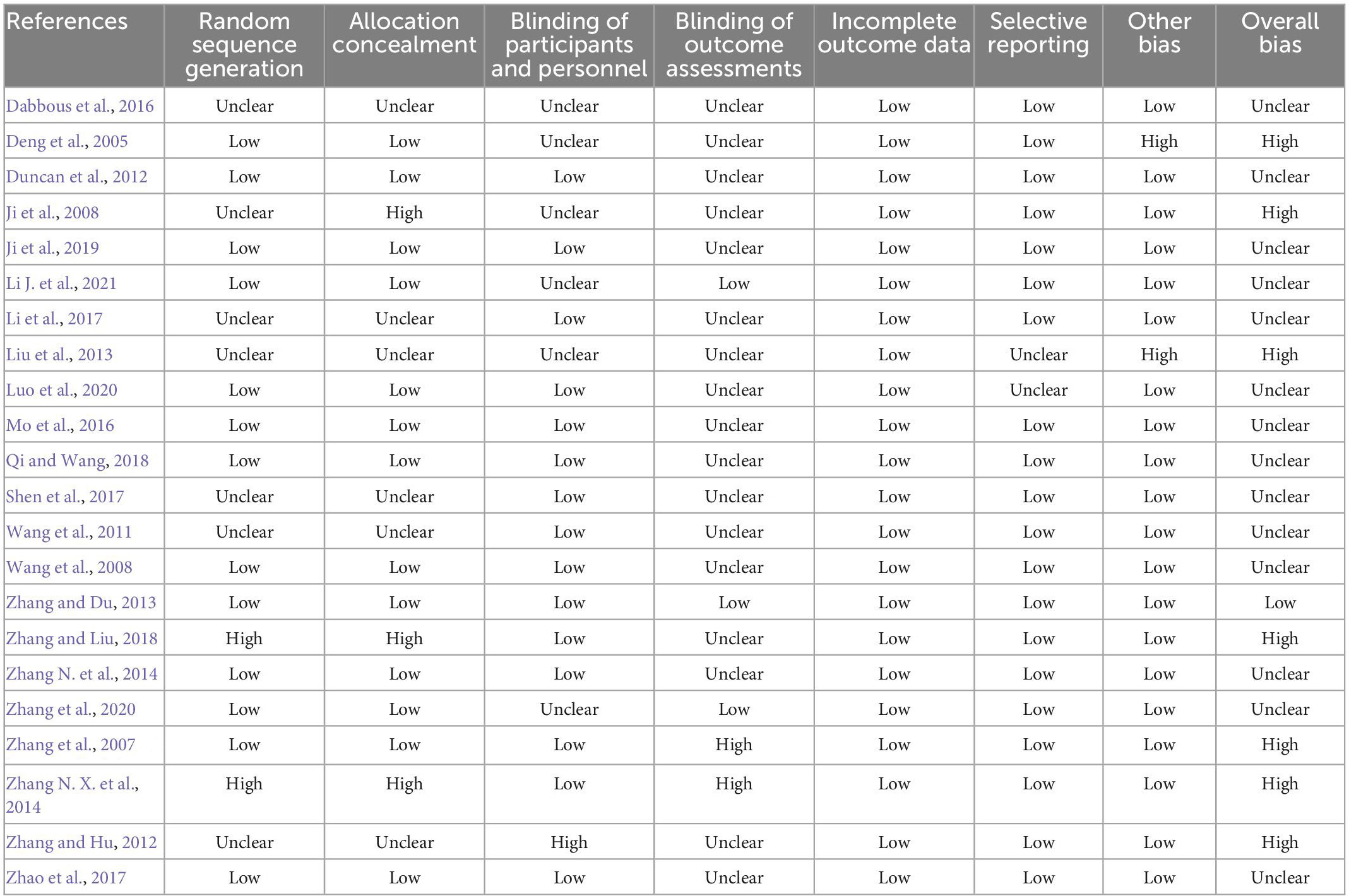
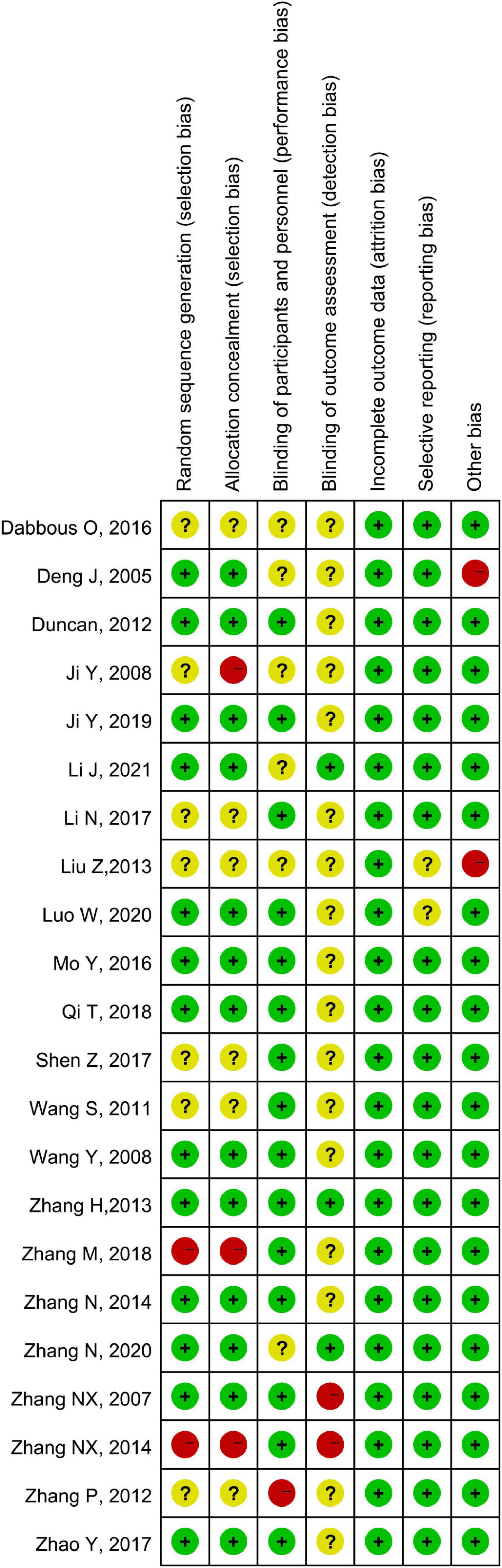
3.4. Quality appraisal
According to the Cochrane risk of bias tool, seven studies had a high risk of bias, while 14 studies showed an unclear risk of bias, with only one study having a low risk of bias (Table 3 and Figure 8). The quality of evidence of the included outcome measures is shown in Table 4, with only one outcome measure (GMFM-88–Dimension A) showing high quality, while five of the thirteen outcome measures, including GMFM-88 Dimension B, C, D, and E, and MAS, have moderate quality.
Table 4. Quality of evidence measured by grading of recommendation assessment, development, and evaluation.
4. Discussion
Our study found that integrated TCM and modern rehabilitation therapies significantly improved motor development in children with CP (ΔGMFM-66 score: 9.33, ΔGMFM-88 score: 8.24, ΔBerg balance scale score: 4.42), reduced muscle tone (ΔMAS score: −0.28), and increased the functional independence (ΔADL score: 3.78). These results suggested that TCM treatments combined with modern rehabilitation therapies may be an effective package of intervention for children with CP, compared to modern rehabilitation therapies only.
Developmental delay, especially motor development, is a symptom of widespread concern for children with CP. The brain remodeling theory is the basis of modern rehabilitation to improve motor development in children with CP (Aisen et al., 2011). Brain remodeling refers to the plasticity and modifiability of the brain. The neurons in the brain may reconnect by external stimuli, thus compensating for the dysfunction caused by brain damage (Gulyaeva, 2017). Modern rehabilitation therapy may help children with CP via neuroplasticity that reshapes the brain and compensates for the development delay (Dancause and Nudo, 2011). For example, the contralateral movement evoked field and ipsilateral motor field of the cortex were activated and reorganization in children with CP after constraint-induced movement therapy (Sutcliffe et al., 2007). Different from the brain remodeling theory of modern rehabilitation therapy, the mechanism of TCM improving motor development may be the blood flow regulation for the brain, which might promote the development of neurons and synaptic interconnection (Shepherd et al., 2018; Niu et al., 2019). Especially in scalp acupuncture, some special acupoints, such as DU-20 and X-HN1, may expand the blood vessels of the corresponding brain areas or promote collateral circulation (Chinese Association of Rehabilitation Medicine Pediatric Rehabilitation Committee et al., 2022b). Expression of endothelin receptor type A, which was associated with vasoconstriction, decreased in mice after being treated with acupuncture (Li J. et al., 2021). Some studies demonstrated that another mechanism of TCM in improving motor development might be the mediation of neurotransmitters, such as gamma-aminobutyric acid, an inhibitory neurotransmitter for motoneurons to improve motor development (Shorter and Segesser, 2013).
Our systematic review showed that the spasticity was improved by the integrated TCM and modern rehabilitation therapies, compared to modern rehabilitation therapy only. In the theory of TCM, children with spastic CP may have a constitution with Yin-deficiency (Zhang et al., 2016). The kidney stores the essence of life and is responsible for body development. The liver is the organ that stores blood. The spleen-stomach is responsible for digestion and nutrient absorption, which is then converted into Qi-blood-body fluid for brain and body development. Therefore, the treatment for spastic CP should aim at brain recovery and start with the Yin deficiency. Acupuncture, massage, or herbal fumigation should consider tonifying Yin deficiency via the acupoints on Yin meridians (such as spleen, liver, and kidney meridians) based on the dialectical diagnosis. With regard to the mechanism related to the effect of the TCM treatments on spasticity, one study suggested that scalp acupuncture may increase and disentangle the white matter fiber bundles in rats with CP (Wang et al., 2021), which may be the anatomical evidence for improving spasticity. A neuroimaging study showed that acupuncture on LR3 may relieve the spasticity of children with CP by reducing the activation of the frontal lobe cortex, an important brain region that controls muscle tone and active movement (Wu et al., 2008).
However, no significant improvement was found in fine motor development in the integrated TCM and modern rehabilitation therapies group, compared to the control group. The possible explanation might be that fine motor improvement requires targeted training. Evidence supported that task-oriented motor training based on the requirements of daily routines may be effective in the improvement of fine motor development (Baker et al., 2022). With regard to unilateral hand function, constraint-induced movement therapy may be effective in children who were diagnosed with unilateral CP (Tinderholt Myrhaug et al., 2014). However, few included studies in our systematic review employed targeted training for fine motor in the conservative rehabilitation protocol. Massage and acupuncture were also recommended for fine motor development delay in children with CP, but individualized treatment should be considered because children with CP vary in the syndrome classifications based on the TCM theory (Chinese Association of Rehabilitation Medicine Pediatric Rehabilitation Committee et al., 2022b). Our results suggest that targeted and individualized therapy should be added to promote fine motor development in children with CP.
Seventeen studies declared that none of the participants withdrew from the studies and no severe adverse event was reported in any of the enrolled studies, indicating that TCM treatments are safe in the clinical setting for children with CP. The duration of intervention for children with CP ranged from 20 days to 6 months with a median intervention time of 3 months. Future studies should focus on the long-term effects of TCM treatments on CP.
4.1. Limitations
There were some limitations of our systematic review, which should be interpreted with caution. First, methodological heterogeneity in the included should not be ignored. Due to the differences in the age and CP severity of the participants, TCM treatments varied among the included studies, such as acupuncture, massage, and herbal fumigation. Subgroup analysis of different intervention protocols could not be conducted because of the insufficient number of included studies. Future studies should consider standardized TCM diagnosis and treatment for children with CP. Second, the pooled results of our systematic review may suffer from methodological quality. Seven of the included studies showed a high risk of bias, while only two studies specified the blinding of the assessors. Third, 21 of the 22 included studies are from China, which indicates that the integrated TCM and modern rehabilitation therapies for CP are not widely used in the world. In the future, the promotion of TCM needs to be strengthened, such as the training of international TCM practitioners. Fourth, it is difficult to quantitatively divide the proportion of TCM treatments and modern rehabilitation therapies because of the differences in basic theory between TCM and modern rehabilitation.
4.2. Implications for clinical practice and research
This systematic review with meta-analysis suggests that TCM may be integrated into the traditional rehabilitation treatment of children with cerebral palsy to improve gross motor development and regulate muscle tone. With regard to fine motor improvement, further studies on the targeted and individualized treatment protocol for children with CP should be noticed. For example, meridians and acupoints should be selected based on syndrome differentiation.
Children with CP also showed a significant increase in functional independence after the treatment of integrated TCM and modern rehabilitation therapies compared to modern rehabilitation therapies only. More studies will be needed in the future to explore the long-term effect of integrated therapies on activities of daily living, given that long-term application of the integrated therapies to children with CP may help them to return to school in adolescence and return to society in adulthood.
Traditional Chinese medicine therapies included in this systematic review consist of body and scalp acupuncture, massage, and fumigation. The methodological heterogeneity needs attention in this systematic review, which may be due to the diversity of TCM treatments. Future studies should focus on the standardization of TCM diagnosis and treatment for children with CP. To promote the application of TCM worldwide, an international training program of TCM should be established to increase the accreditation of TCM practitioners.
5. Conclusion
This systematic review indicated that integrated TCM and modern rehabilitation therapies may be recognized as an effective and safe therapy to improve gross motor function, reduce muscle tone, and improve the functional independence of children with CP, compared to modern rehabilitation therapy only. Due to the methodological heterogeneity and the potential risk of bias in the included studies, our results should be interpreted with caution. Future studies should focus on the standardization of TCM treatments, and training of international TCM practitioners may be considered for TCM promotions.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
ZC and ZH contributed to the studies retrieval and data extraction. QD and XZ designed and developed the framework for the manuscript. All authors contributed to the article’s writing, read the manuscript, and agreed to submit this version.
Funding
This study was funded by the Shanghai Three-Year Action Plan to Further Accelerate the Development of Chinese Medicine Inheritance and Innovation (2021–2023) Project, No. ZY(2021-2023)-0201-05.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnins.2023.1097477/full#supplementary-material
Abbreviations
CP, cerebral palsy; TCM, traditional Chinese medicine; GMFM, gross motor function measure; MAS, Modified Ashworth scale; ADL, activities of daily living; RCT, randomized controlled trial; GRADE, grading of recommendation assessment, development, and evaluation; WMD, weighted mean difference; CI, confidence interval.
References
Aisen, M. L., Kerkovich, D., Mast, J., Mulroy, S., Wren, T. A., Kay, R. M., et al. (2011). Cerebral palsy: Clinical care and neurological rehabilitation. Lancet Neurol. 10, 844–852. doi: 10.1016/s1474-4422(11)70176-4
Baker, A., Niles, N., Kysh, L., and Sargent, B. (2022). Effect of motor intervention for infants and toddlers with cerebral palsy: A systematic review and meta-analysis. Pediatr. Phys. Ther. 34, 297–307. doi: 10.1097/pep.0000000000000914
Bohannon, R. W., and Smith, M. B. (1987). Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys. Ther. 67, 206–207. doi: 10.1093/ptj/67.2.206
Castelli, E., and Fazzi, E. (2016). Recommendations for the rehabilitation of children with cerebral palsy. Eur. J. Phys. Rehabil. Med. 52, 691–703.
Chinese Association of Rehabilitation Medicine Pediatric Rehabilitation Committee, Chinese Association of Rehabilitation of Disabled Persons Rehabilitation Committee for Cerebral Palsy, Chinese Medical Doctor Association Pediatric Rehabilitation Committee, and Chinese Rehabilitation Guidelines for Cerebral Palsy Editorial Board (2022a). Chinese rehabilitation guidelines for cerebral palsy (2022) part 1: Overview. Chin. J. Appl. Clin. Pediatr. 37, 887–892.
Chinese Association of Rehabilitation Medicine Pediatric Rehabilitation Committee, Chinese Association of Rehabilitation of Disabled Persons Rehabilitation Committee for Cerebral Palsy, Chinese Medical Doctor Association Pediatric Rehabilitation Committee, and Chinese Rehabilitation Guidelines for Cerebral Palsy Editorial Board (2022b). Chinese rehabilitation guidelines for cerebral palsy (2022) part 5: Traditional Chinese Medicine rehabilitation therapy. Chin. J. Appl. Clin. Pediatr. 37, 1365–1376.
Chuang, C. M., Hsieh, C. L., Li, T. C., and Lin, J. G. (2007). Acupuncture stimulation at Baihui acupoint reduced cerebral infarct and increased dopamine levels in chronic cerebral hypoperfusion and ischemia-reperfusion injured sprague-dawley rats. Am. J. Chin. Med. 35, 779–791. doi: 10.1142/s0192415x07005260
Cumpston, M., Li, T., Page, M. J., Chandler, J., Welch, V. A., Higgins, J. P., et al. (2019). Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochr. Database Syst. Rev. 10:Ed000142. doi: 10.1002/14651858.Ed000142
Dabbous, O. A., Mostafa, Y. M., El Noamany, H. A., El Shennawy, S. A., and El Bagoury, M. A. (2016). Laser acupuncture as an adjunctive therapy for spastic cerebral palsy in children. Lasers Med. Sci. 31, 1061–1067. doi: 10.1007/s10103-016-1951-6
Damiano, D. L., Longo, E., Carolina de Campos, A., Forssberg, H., and Rauch, A. (2021). Systematic review of clinical guidelines related to care of individuals with cerebral palsy as part of the world health organization efforts to develop a global package of interventions for rehabilitation. Arch. Phys. Med. Rehabil. 102, 1764–1774. doi: 10.1016/j.apmr.2020.11.015
Dancause, N., and Nudo, R. J. (2011). Shaping plasticity to enhance recovery after injury. Prog. Brain Res. 192, 273–295. doi: 10.1016/b978-0-444-53355-5.00015-4
Deng, J. E., Pan, Q. L., and Zhang, L. M. (2005). Influence of scalp acupuncture combined with modern rehabilitation on the treatment of infantile cerebral palsy. Chin. J. Clin. Rehabil. 9, 120–121. doi: 10.3969/j.issn.16721349.2015.02.018
Duncan, B., Shen, K. L., Zou, L. P., Han, T. L., Lu, Z. L., Zheng, H., et al. (2012). Evaluating intense rehabilitative therapies with and without acupuncture for children with cerebral palsy: A randomized controlled trial. Arch. Phys. Med. Rehabil. 93, 808–815. doi: 10.1016/j.apmr.2011.12.009
Fay, D., Wilkinson, T., Anderson, A. D., Hanyzewski, M., Hellwig, K., Meador, C., et al. (2019). Effects of modified instructions on Peabody developmental motor scales, second edition, gross motor scores in children with typical development. Phys. Occup. Ther. Pediatr. 39, 433–445. doi: 10.1080/01942638.2018.1534921
Gulyaeva, N. V. (2017). Molecular mechanisms of neuroplasticity: An expanding universe. Biochemistry (Mosc) 82, 237–242. doi: 10.1134/s0006297917030014
Ji, Y. H., Ji, Y. H., and Sun, B. D. (2019). Effect of acupuncture combined with repetitive transcranial magnetic stimulation on motor function and cerebral hemodynamics in children with spastic cerebral palsy with spleen-kidney deficiency. Acupunct. Res. 44, 757–761. doi: 10.13702/j.1000-0607.190154
Ji, Y. H., Sun, B. D., Zhang, J., Zhang, R., and Ji, Y. H. (2008). Therapeutic effect of scalp-acupuncture combined with exercise therapy on spastic cerebral palsy of the child. Chin. Acupunct. Moxibustion 28, 723–726.
Li, J. M., Chen, C., Zhu, S. Y., Niu, X. L., Yu, X. D., Ren, J., et al. (2021). Evaluating the effects of 5-Hz repetitive transcranial magnetic stimulation with and without wrist-ankle acupuncture on improving spasticity and motor function in children with cerebral palsy: A randomized controlled trial. Front. Neurosci. 15:771064. doi: 10.3389/fnins.2021.771064
Li, J., Peng, C., Lai, D., Fang, Y., Luo, D., Zhou, Z., et al. (2021). PET-CT and RNA sequencing reveal novel targets for acupuncture-induced lowering of blood pressure in spontaneously hypertensive rats. Sci. Rep. 11:10973. doi: 10.1038/s41598-021-90467-1
Li, N., Liu, Z. H., Li, J. L., Jin, B. X., Zhao, Y., Fu, W. J., et al. (2017). Clinical observation on Governor Vessel-unblocking and brain-refreshing scalp acupuncture for cerebral palsy complicated with intellectual disabilities. J. Acupunct. Tuina Sci. 15, 131–135. doi: 10.1007/s11726-017-0989-8
Liang, X., Tan, Z., Yun, G., Cao, J., Wang, J., Liu, Q., et al. (2021). Effectiveness of exercise interventions for children with cerebral palsy: A systematic review and meta-analysis of randomized controlled trials. J. Rehabil. Med. 53:jrm00176. doi: 10.2340/16501977-2772
Lindsay, S. (2016). Child and youth experiences and perspectives of cerebral palsy: A qualitative systematic review. Child Care Health Dev. 42, 153–175. doi: 10.1111/cch.12309
Liu, Z.-h., Qi, Y.-c., Pan, P.-g., Ma, M.-m., Qian, X.-g., and Fu, W.-j. (2013). Clinical observation on treatment of clearing the governor vessel and refreshing the mind needling in neural development and remediation of children with cerebral palsy. Chin. J. Integr. Med. 19, 505–509. doi: 10.1007/s11655-013-1504-9
Luo, W., Wang, P. Q., Liu, C. L., Huang, C., Yang, Y., and Wang, Y. M. (2020). Therapeutic effect of scalp acupuncture combined with rehabilitation training on balance dysfunction in children with spastic hemiplegia. Acupunct. Res. 45, 662–666. doi: 10.13702/j.1000-0607.190461
Michael-Asalu, A., Taylor, G., Campbell, H., Lelea, L. L., and Kirby, R. S. (2019). Cerebral palsy: Diagnosis, epidemiology, genetics, and clinical update. Adv. Pediatr. 66, 189–208. doi: 10.1016/j.yapd.2019.04.002
Mo, Y. L., Yang, J. M., Wu, B. Y., and Nie, J. (2016). Clinical research on the effect of Chinese herbal fumigation combined with occupational therapy for improving the fine motor function of children with spastic cerebral palsy. Clin. Med. Eng. 23, 105–106. doi: 10.3969/j.issn.1674-4659.2016.01.0105
Niu, F., Wang, C., Zhong, H., Ren, N., Wang, X., and Li, B. (2021). Spinal tuina improves cognitive impairment in cerebral palsy rats through inhibiting pyroptosis induced by NLRP3 and caspase-1. Evid. Based Complement. Alternat. Med. 2021:1028909. doi: 10.1155/2021/1028909
Niu, J. F., Zhao, X. F., Hu, H. T., Wang, J. J., Liu, Y. L., and Lu, D. H. (2019). Should acupuncture, biofeedback, massage, Qi gong, relaxation therapy, device-guided breathing, yoga and tai chi be used to reduce blood pressure?: Recommendations based on high-quality systematic reviews. Complement. Ther. Med. 42, 322–331. doi: 10.1016/j.ctim.2018.10.017
Novak, I., Morgan, C., Adde, L., Blackman, J., Boyd, R. N., Brunstrom-Hernandez, J., et al. (2017). Early, accurate diagnosis and early intervention in cerebral palsy: Advances in diagnosis and treatment. JAMA Pediatr. 171, 897–907. doi: 10.1001/jamapediatrics.2017.1689
Qi, T., and Wang, C. (2018). Effects of intradermal needling on core muscle stability in children with cerebral palsy: A clinical comparative study. Chin. Acupunct. Moxibustion 38, 597–601. doi: 10.13703/j.0255-2930.2018.06.007
Sellier, E., Platt, M. J., Andersen, G. L., Krägeloh-Mann, I., De La Cruz, J., and Cans, C. (2016). Decreasing prevalence in cerebral palsy: A multi-site European population-based study, 1980 to 2003. Dev. Med. Child Neurol. 58, 85–92. doi: 10.1111/dmcn.12865
Shen, Z.-f, Luo, K.-t, and Yan, Y.-q (2017). Effect of acupuncture and tuina plus rehabilitative therapy on lower limb motor dysfunction in infants with spastic cerebral palsy. J. Acupunct. Tuina Sci. 15, 31–35. doi: 10.1007/s11726-017-0971-5
Shepherd, E., Salam, R. A., Middleton, P., Han, S., Makrides, M., McIntyre, S., et al. (2018). Neonatal interventions for preventing cerebral palsy: An overview of Cochrane Systematic Reviews. Cochr. Database Syst. Rev. 6:Cd012409. doi: 10.1002/14651858.CD012409.pub2
Shorter, E., and Segesser, K. (2013). Traditional Chinese medicine and Western psychopharmacology: Building bridges. Phytother. Res. 27, 1739–1744. doi: 10.1002/ptr.4940
Sutcliffe, T. L., Gaetz, W. C., Logan, W. J., Cheyne, D. O., and Fehlings, D. L. (2007). Cortical reorganization after modified constraint-induced movement therapy in pediatric hemiplegic cerebral palsy. J. Child Neurol. 22, 1281–1287. doi: 10.1177/0883073807307084
Tao, J., Zheng, Y., Liu, W., Yang, S., Huang, J., Xue, X., et al. (2016). Electro-acupuncture at LI11 and ST36 acupoints exerts neuroprotective effects via reactive astrocyte proliferation after ischemia and reperfusion injury in rats. Brain Res. Bull. 120, 14–24. doi: 10.1016/j.brainresbull.2015.10.011
Te Velde, A., and Morgan, C. (2022). Gross motor function measure (GMFM-66 & GMFM-88) user’s manual, 3rd Edition. Book Review. Pediatr. Phys. Ther. 34, 88–89. doi: 10.1097/pep.0000000000000858
Tinderholt Myrhaug, H., Østensjø, S., Larun, L., Odgaard-Jensen, J., and Jahnsen, R. (2014). Intensive training of motor function and functional skills among young children with cerebral palsy: A systematic review and meta-analysis. BMC Pediatr. 14:292. doi: 10.1186/s12887-014-0292-5
Vargus-Adams, J. N., and Martin, L. K. (2011). Domains of importance for parents, medical professionals and youth with cerebral palsy considering treatment outcomes. Child Care Health Dev. 37, 276–281. doi: 10.1111/j.1365-2214.2010.01121.x
Verschuren, O., Peterson, M. D., Balemans, A. C., and Hurvitz, E. A. (2016). Exercise and physical activity recommendations for people with cerebral palsy. Dev. Med. Child Neurol. 58, 798–808. doi: 10.1111/dmcn.13053
Wang, H. L., and Wu, J. W. (2005). Lin Xue-Jian’s experience on treatment of a part of cerebral diseases with scalp acupuncture. Chin. Acupunct. Moxibustion 25, 729–732. doi: 10.3321/j.issn:0255-2930.2005.10.018
Wang, S. Q., Liang, W. X., Huang, G. H., and Wu, P. C. (2011). Randomized controlled clinical trials for acupuncture treatment of spastic cerebral palsy children by bilateral horizontal puncturing from Yuzhen (BL 9) to Tianzhu (BL 10). Acupunct. Res. 36, 215–219.
Wang, Y., Zhu, W. L., and Dong, Y. F. (2008). Massage manipulation of supplementing marrow and kneading tendon in treating 30 children with spastic cerebral palsy. Chin. J. Integr. Tradit. Western Med. 28, 363–365. doi: 10.3321/j.issn:1003-5370.2008.04.021
Wang, Z., Fan, X., Chen, K., Yu, X., and Gao, J. (2021). Effects of three kinds of head acupuncture therapies on regulation of brain microenvironment and rehabilitation of nerve function in rats with cerebral palsy. J. Tradit. Chin. Med. 41, 276–283.
Wu, Y., Jin, Z., Li, K., Lu, Z. L., Wong, V., Han, T. L., et al. (2008). Effect of acupuncture on the brain in children with spastic cerebral palsy using functional neuroimaging (FMRI). J. Child Neurol. 23, 1267–1274. doi: 10.1177/0883073808318049
Zhang, H. Y., and Du, F. (2013). Clinical trials of acupuncture intervention combined with sitting training for cerebral palsy children with parafunctional sitting position. Acupunct. Res. 38, 403–406,410.
Zhang, M., and Liu, Z. (2018). Effects of acupuncture on muscle tension of lower limb in children with spastic cerebral palsy. Chin. Acupunct. Moxibustion 38, 591–595. doi: 10.13703/j.0255-2930.2018.06.006
Zhang, N. X., Liu, G. Z., Sun, K. X., and Hao, J. D. (2007). Clinical study of the treatment of infant cerebral palsy with warm-reinforcing needling combined with rehabilitation training. Acupunct. Res. 32, 260–263. doi: 10.3969/j.issn.1000-0607.2007.04.010
Zhang, N. X., Wang, X. Y., Li, Y. B., Liu, G. Z., and Zhang, H. Y. (2014). Effects of individualized therapeutic porgram with heat-reinforcing needling in combination with Bobath therapy on gross motor dysfunction in children with cerebral palsy: A randomized controlled trial. World J. Acupunct. Moxibustion 24, 21–31.
Zhang, N., He, X. H., Liu, Y. M., and Lu, Y. (2020). Effect of Jin’s three-needle combined with MyoTrac biostimulation therapy on upper limb function in children with spastic hemiplegia. Chin. Acupunct. Moxibustion 40, 1314–1318. doi: 10.13703/j.0255-2930.20191119-k0002
Zhang, N., Tang, Q. P., and Xiong, Y. H. (2014). Impacts on the lower limb motor function in children with spastic cerebral palsy treated by Jin three-needle therapy combined with MOTOmed intelligent motor training. Chin. Acupunct. Moxibustion 34, 657–660.
Zhang, P. Y., and Hu, F. F. (2012). Influence of cluster needling at scalp acupoints combined with rehabilitation training on balance functions of children with cerebral palsy. World J. Acupunct. Moxibustion 22, 23–26. doi: 10.1016/S1003-5257(13)60023-9
Zhang, Z., Zhang, J., Guan, L., and Mu, Y. (2016). Characteristics of TCM Constitution in children with cerebral palsy. Chin. J. Integr. Tradit. Western Med. 36, 494–496.
Keywords: cerebral palsy, traditional Chinese medicine, acupuncture, motor function, systematic review
Citation: Chen Z, Huang Z, Li X, Deng W, Gao M, Jin M, Zhou X and Du Q (2023) Effects of traditional Chinese medicine combined with modern rehabilitation therapies on motor function in children with cerebral palsy: A systematic review and meta-analysis. Front. Neurosci. 17:1097477. doi: 10.3389/fnins.2023.1097477
Received: 13 November 2022; Accepted: 19 January 2023;
Published: 08 February 2023.
Edited by:
Min Fang, Shanghai University of Traditional Chinese Medicine, ChinaReviewed by:
Dengna Zhu, The Third Affiliated Hospital of Zhengzhou University, ChinaYing Fang, Northern Arizona University, United States
Copyright © 2023 Chen, Huang, Li, Deng, Gao, Jin, Zhou and Du. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xuan Zhou,  emhvdXh1YW5AeGluaHVhbWVkLmNvbS5jbg==; Qing Du,
emhvdXh1YW5AeGluaHVhbWVkLmNvbS5jbg==; Qing Du,  ZHVxaW5nQHhpbmh1YW1lZC5jb20uY24=
ZHVxaW5nQHhpbmh1YW1lZC5jb20uY24=
†These authors have contributed equally to this work and share first authorship
 Zhengquan Chen1†
Zhengquan Chen1† Xin Li
Xin Li Xuan Zhou
Xuan Zhou Qing Du
Qing Du