- 1Department of Radiology, Saint Louis University, Saint Louis, MO, USA
- 2Division of Nuclear Medicine, Department of Radiology, Saint Louis University, Saint Louis, MO, USA
- 3Division of Nuclear Medicine, Department of Radiology, Saint Louis VA Medical Center, Saint Louis, MO, USA
We present the case of a 77-year-old male with a history of prostate cancer. Follow up PET-CT and contrast-enhanced CT demonstrated a small peritoneal loose body or “mouse” in the pelvis. This is an uncommon, benign, asymptomatic finding which is usually incidentally discovered. The significance of being aware of this entity is to distinguish it from metastasis, especially in patients with known abdominal and pelvic malignancies.
Case Presentation
A 77-year-old male with a remote history of prostate cancer was referred to our imaging facility after undergoing a prostatectomy at an outside facility. He presented to the emergency department with non-specific abdominal pain. A contrast-enhanced CT abdomen and pelvis was performed which showed no acute findings to explain his symptoms. However, a well circumscribed round soft tissue density measuring 1.7 cm was seen in the right hemipelvis adjacent to the sigmoid colon (Figure 1). The lesion was not contiguous with bowel. Given the patient’s history of prostate cancer, a peritoneal metastasis or necrotic lymph node was suggested. On the coronal image, a surgical clip inferior to the lesion was from prior prostatectomy. 18F-FDG PET-CT was performed 3 days following the contrast-enhanced CT. The low dose CT showed that the lesion had moved from the right to the left and was located near the urinary bladder (Figure 2). The lesion demonstrated no FDG uptake on PET. Based on the mobility of the lesion, a diagnosis of a peritoneal loose body or “mouse” was made.
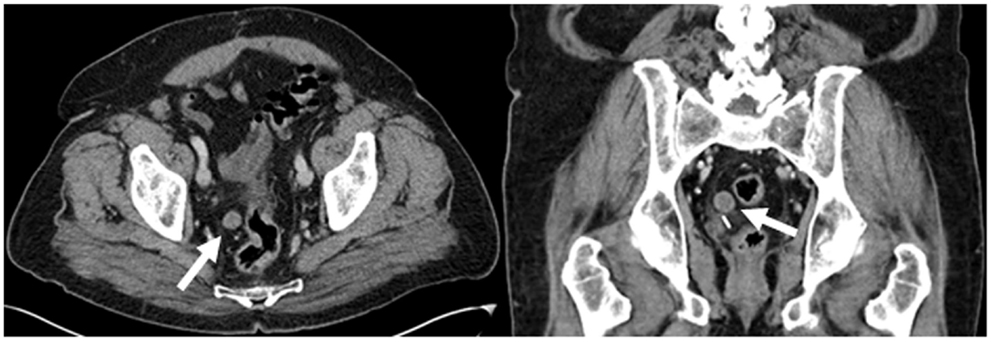
Figure 1. Contrast-enhanced CT demonstrates a well circumscribed round soft tissue density measuring 1.7 cm in the right hemipelvis adjacent to the sigmoid colon (white arrows).
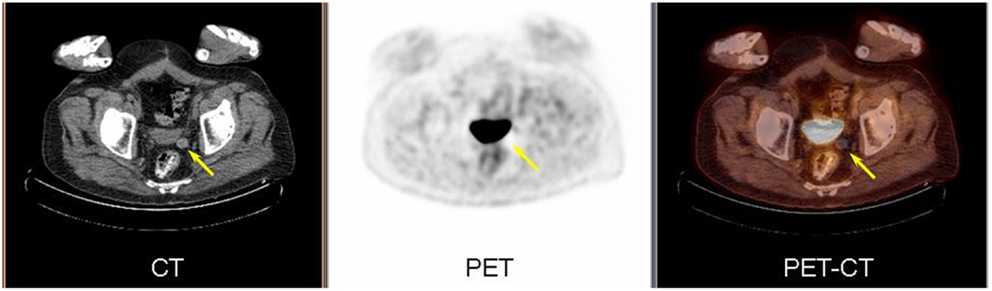
Figure 2. PET/CT images demonstrate the soft tissue lesion has moved from the right to left hemipelvis (arrow) on low dose CT (left). The lesion demonstrated no metabolic activity on PET (center) and fused image (right).
Background
Peritoneal loose bodies or “mice” are commonly small mobile lesions falling into the category of an incidentaloma. They are found within the peritoneum during surgery or radiographically and have little clinical significance. However, in patients with a history of malignancy they can lead to altered patient management if perceived as a site of metastasis. We report a case of a peritoneal mouse in a patient with prostate cancer and differentiating it from a metastatic lesion.
Discussion
Peritoneal mice have not been previously reported in nuclear medicine literature. There are a few surgical case reports describing this uncommon entity (Nomura et al., 2003; Asabe et al., 2005; Mohri et al., 2007; Kavanagh et al., 2010). Two radiology case reports have described this finding on CT (Ohgitani et al., 2004; Gayer and Petrovitch, 2011). The most commonly accepted hypothesis suggests that peritoneal mice arise from the colonic epiploic appendages. Epiploic appendages are fat containing structures along the antimesenteric tenia of the colon. An epiploic appendage may torse on its axis resulting in infarction and fat necrosis. In the acute setting, the torsion may present as acute abdominal pain and could mimic appendicitis. In cases of chronic torsion, ischemia leads to saponification and calcification of the fat contents and atrophy of the pedicle (Kavanagh et al., 2010). The epiploic appendage detaches from the colon and becomes a peritoneal mouse. Since they are avascular and no longer connected to bowel, they can freely move in the peritoneum as loose bodies. On CT a peritoneal mouse manifests as a well circumscribed round soft tissue density which may have thick or calcified rims. The most common location is adjacent to the colon, particularly the sigmoid colon. It does not enhance with contrast and shows no FDG uptake on PET. Most peritoneal mice are asymptomatic incidentalomas which are usually 0.5–2.5 cm in diameter. Rare giant peritoneal mice measuring 5–10 cm in diameter may cause symptoms due to mass effect. Cases of urinary and intestinal obstruction have been reported due to giant peritoneal mice (Bhandarwar et al., 1996; Ghosh et al., 2006). A case of a peritoneal mouse mimicking a rectal leiomyoma has been reported (Takada et al., 1998).
Conclusion
A peritoneal loose body or mouse is a benign finding. The significance of being aware of this entity is to distinguish it from metastasis, especially in patients with known abdominal or pelvic malignancies.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Asabe, K., Maekawa, T., Yamashita, Y., and Shirakusa, T. (2005). Endoscopic extraction of a peritoneal loose body: a case report of an infant. Pediatr. Surg. Int. 21, 388–389.
Bhandarwar, A. M., Desai, V. V., Gajbhiye, R. N., and Deshraj, B. P. (1996). Acute retention of urine due to a loose peritoneal body. Br. J. Urol. 78, 951–952.
Gayer, G., and Petrovitch, I. (2011). CT diagnosis of a large peritoneal loose body: a case report and review of literature. Br. J. Radiol. 84, e83–e85.
Ghosh, P., Strong, C., Naugler, W., Haghighi, P., and Carethers, J. M. (2006). Peritoneal mice implicated in intestinal obstruction: report of a case and review of the literature. J. Clin. Gastroenterol. 40, 427–430.
Kavanagh, D. O., Moran, D., Flynn, R., and Neary, P. C. (2010). Laproscopic Retrieval of A Peritoneal Mouse. Case Report Medicine. [pii:624825]. New York: Hindawi Publishing Corporation.
Mohri, T., Kato, T., and Suzuki, H. (2007). A giant peritoneal loose body: report of a case. Am. Surg. 73, 895–896.
Nomura, H., Hata, F., Yasoshima, T., Kuwahar, S., Naohara, T., Nishimori, H., et al. (2003). Giant peritoneal loose body in the pelvic cavity: report of a case. Surg. Today 33, 791–793.
Ohgitani, D., Kani, H., Matsuki, M., Kanazawa, S., and Narabayashi, I. (2004). A case of a giant peritoneal loose body: usefulness of a wide window width CT. Nihon Igaku Hoshasen Gakkai Zasshi 64, 223–224.
Keywords: peritoneal mouse, loose body, epiploic appendage, PET-CT, colon cancer
Citation: Allam T, Muzaffar R, Nguyen NC and Osman MM (2013) Peritoneal mouse as detected on 18F-FDG PET-CT. Front. Oncol. 3:83. doi: 10.3389/fonc.2013.00083
Received: 28 January 2013; Accepted: 29 March 2013;
Published online: 10 April 2013.
Edited by:
Georgios Limouris, Athens University Medical Faculty, GreeceReviewed by:
Abdulaziz S. Al Sugair, King Faisal Specialist Hospital and Research Center, Saudi ArabiaVikram R. Lele, Jaslok Hospital and Research Centre, India
Copyright: © 2013 Allam, Muzaffar, Nguyen and Osman. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in other forums, provided the original authors and source are credited and subject to any copyright notices concerning any third-party graphics etc.
*Correspondence: Medhat M. Osman, Division of Nuclear Medicine, Department of Radiology, Saint Louis University, 3635 Vista Avenue, 2-DT, St. Louis, MO 63110, USA. e-mail:bW9zbWFuQHNsdS5lZHU=



