- 1Division of General Surgery, Department of Surgery, Taipei Veterans General Hospital, Taipei, Taiwan
- 2School of Medicine, National Yang Ming Chiao Tung University, Taipei, Taiwan
- 3Center of Immuno-Oncology, Department of Oncology, Taipei Veterans General Hospital, Taipei, Taiwan
- 4Department of Surgery, National Yang Ming Chiao Tung University Hospital, Yilan, Taiwan
- 5Department of Pathology, Taipei Veterans General Hospital, Taipei, Taiwan
Background: To date, few reports have investigated genetic alterations and clinicopathological features in cardia and noncardia gastric cancer (GC).
Methods: In total, 435 GC patients receiving curative surgery were included. The clinicopathological features, recurrence patterns, prognoses and genetic alterations were compared between cardia and noncardia GC patients.
Results: Among the 435 enrolled patients, 47 (10.8%) had cardia GC. Compared with noncardia GC, cardia GC was associated with more intestinal-type tumors and similar initial recurrence patterns and 5-year overall survival (OS; 50.8% vs. 50.5%, P = 0.480) and disease-free survival (DFS; 48.6% vs. 48.9%, P = 0.392) rates. For both intestinal-type GC and diffuse-type GC, the clinicopathological features and 5-year OS and DFS rates were not significantly different between the cardia and noncardia GC patients. Multivariable analysis showed that cardia GC was not an independent prognostic factor. Compared with noncardia GC, cardia GC was associated with increased PIK3CA amplification than in patients with intestinal-type GC and was associated with increased HER2 expression in patients with diffuse-type GC.
Conclusions: Cardia GC is not an independent prognostic factor. In cardia GC patients with intestinal-type GC, PIK3CA amplification was more common, and in those with diffuse-type GC, HER2 expression was more common. Targeted therapy may be beneficial for these patient subgroups.
Introduction
Gastric cancer (GC) is the sixth most common cancer and ranks second in terms of cancer-related death worldwide (1). The incidence of cardia GC has shown an increasing trend over time, while that of noncardia GC has shown a decreasing trend.
According to the 8th edition of the American Joint Committee on Cancer (AJCC)/Union for International Cancer Control (UICC) tumor, node, metastasis (TNM) classification system (2), Siewert type 2 cardia cancer with esophagogasric junction invasion is classified as esophageal cancer, and Siewert type 3 cardia cancer is classified as GC. It was reported that cardia GC was associated with more advanced staging and unfavorable clinicopathological features at diagnosis than noncardia GC (3).
In terms of molecular analyses, some reports have investigated genetic alterations in cardia and noncardia GC (4, 5). Genome-wide association studies have revealed that some single nucleotide polymorphisms (SNPs) are associated with noncardia GC only (4), while others have shown no difference in the SNPs between cardia and noncardia GC (5). In addition, HER2 expression has been reported to be higher in cardia GC than in noncardia GC (6). The correlation between HER2 expression and histologic types in GC is controversial; HER2 expression has been reported to be associated with intestinal-type GC in some studies (7), whereas other studies have indicated that HER2 expression was more common in diffuse-type GC (8). Consequently, there is a need to investigate the correlation between genetic alterations and histologic type in cardia and noncardia GC.
The aim of the current study was to compare the clinicopathological characteristics, recurrence patterns, and prognoses between cardia and noncardia GC after curative surgery. As in a previous study (9), a nine-gene mutation panel was used to perform genetic analysis with the MassARRAY method; in addition, Helicobacter pylori (HP) infection, Epstein–Barr virus (EBV) infection, and PIK3CA amplification were compared between cardia and noncardia GC patients.
Materials and Methods
Between 2005 and 2014, a total of 435 GC patients with adenocarcinoma who underwent curative surgery were included in the present study. According to the 8th edition of the AJCC/UICC TNM classification system, among the 435 GC patients, 47 (10.8%) patients were classified as having cardia GC. Tumor and normal gastric mucosa tissues were collected, and genetic alterations were analyzed for all 435 GC patients. The Institutional Review Board of Taipei Veterans General Hospital approved the present study (2020-09-017CC). All samples used in this study had been previously collected from the biobank of Taipei Veterans General Hospital and were anonymized. All enrolled patients signed an informed consent form before sample collection from the biobank.
Regarding the extent of lymphadenectomy, at least D1+ dissection was performed for early GC, while D2 dissection was performed for advanced GC (10).
The follow-up examinations were the same as those performed in a previous study (11) and were conducted every 3 months during the first 3 years after surgery and every 6 months thereafter. Patients with tumor recurrence could receive 5-fluorouracil (FU)-based chemotherapy. No patients enrolled in the present study received preoperative chemotherapy. Adjuvant therapy, such as S-1, has been prescribed for stage II or III disease after curative surgery at our institute since 2008 due to its proven survival benefit (12). Approximately 62% of the enrolled patients underwent surgery before 2008. Consequently, the number of patients who received adjuvant chemotherapy was low in the present study.
Analysis of Microsatellite Instability and Genetic Mutations
As reported in a previous study (13), five reference microsatellite markers were used to determine microsatellite instability (MSI), namely, D5S345, D2S123, D17S250, BAT25 and BAT26. MSI-high (MSI-H) was defined as ≥2 loci of instability, while MSI-low/stable (MSI-L/S) was defined as one locus or no MSI loci of instability (13).
As demonstrated in a previous study (9), a MassARRAY system (Agena, San Diego, CA) was used to identify 76 mutation hotspots in nine GC-related genes: PIK3CA, AKT1, AKT2, AKT3, PTEN, ARID1A, TP53, BRAF, and KRAS. Mutations in PTEN, PIK3CA, AKT1, AKT2, or AKT3 were defined as PI3K/AKT pathway genetic mutations.
HP and EBV Detection
As mentioned in a previous study, HP infection was identified using polymerase chain reaction (PCR) assays (14).
EBV infection was identified using the in situ hybridization (ISH) technique for the detection of EBV-encoded small RNAs in formalin-fixed paraffin-embedded tissue samples (15).
Immunohistochemical (IHC) Staining for HER2
HER2 IHC staining was performed with anti-human c-erbB-2 A0485 polyclonal antibody (dilution 1:500; Dako) (16). An IHC score of 3+ or an IHC score of 2+ with a positive fluorescence in situ hybridization result was defined as positive HER2 IHC staining.
Statistical Analysis
IBM SPSS Statistics 25.0 (IBM Corp., Armonk, NY, USA) was used for statistical analyses. Categorical data were compared between groups using the χ2 test with Yate’s correction or Fisher’s exact test. Overall survival (OS) was defined from the date of surgery to the date of death or the last follow-up. Disease-free survival (DFS) was defined as the length of time after surgery during which the patient was alive without GC recurrence. The Kaplan–Meier method was applied for the survival analysis of OS and DFS. Multivariable analysis with Cox proportional hazards models was applied to analyze the independent prognostic factors of OS. Statistical significance was defined as a P value less than 0.05.
Results
Clinicopathological Features
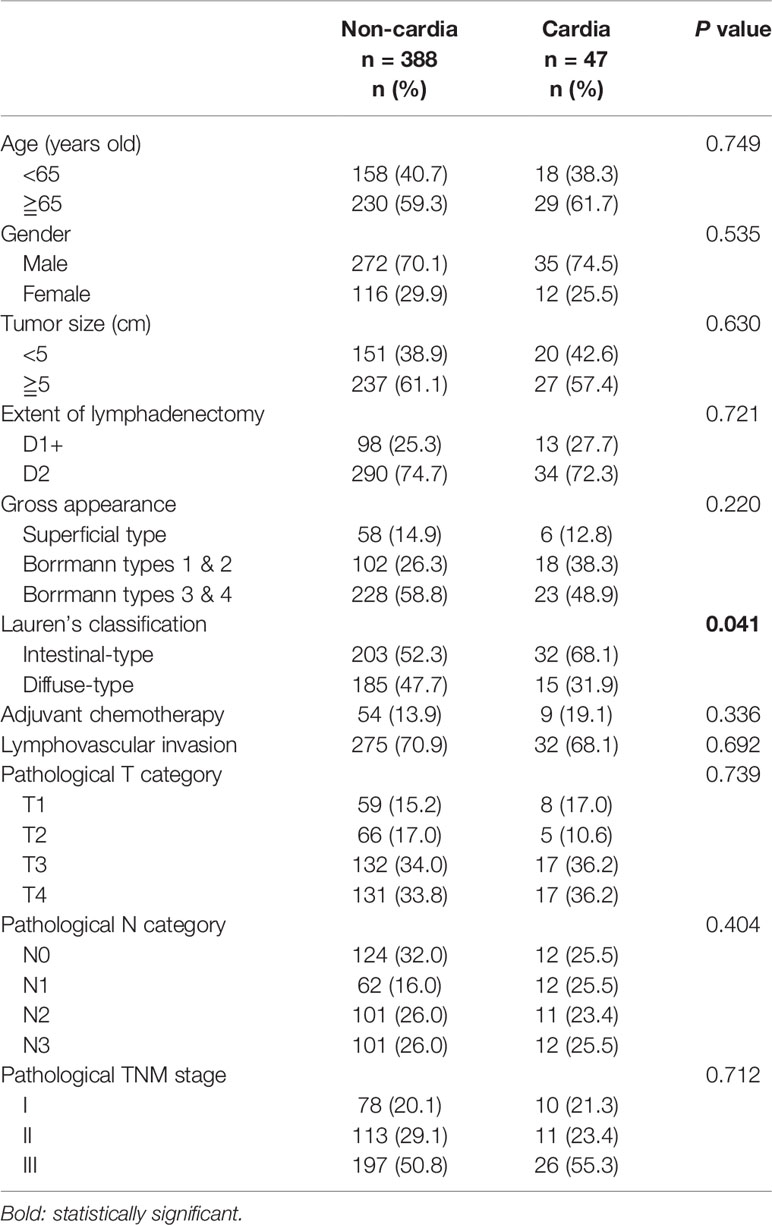
Among the 435 GC patients, 47 (10.8%) had cardia GC. Regarding the clinicopathological characteristics, as shown in Table 1, patients with cardia GC had more intestinal-type tumors than those with noncardia GC.
As shown in Table 2, for both intestinal-type and diffuse-type GC, there was no significant difference between patients with cardia GC and those with noncardia GC in terms of clinicopathological features.
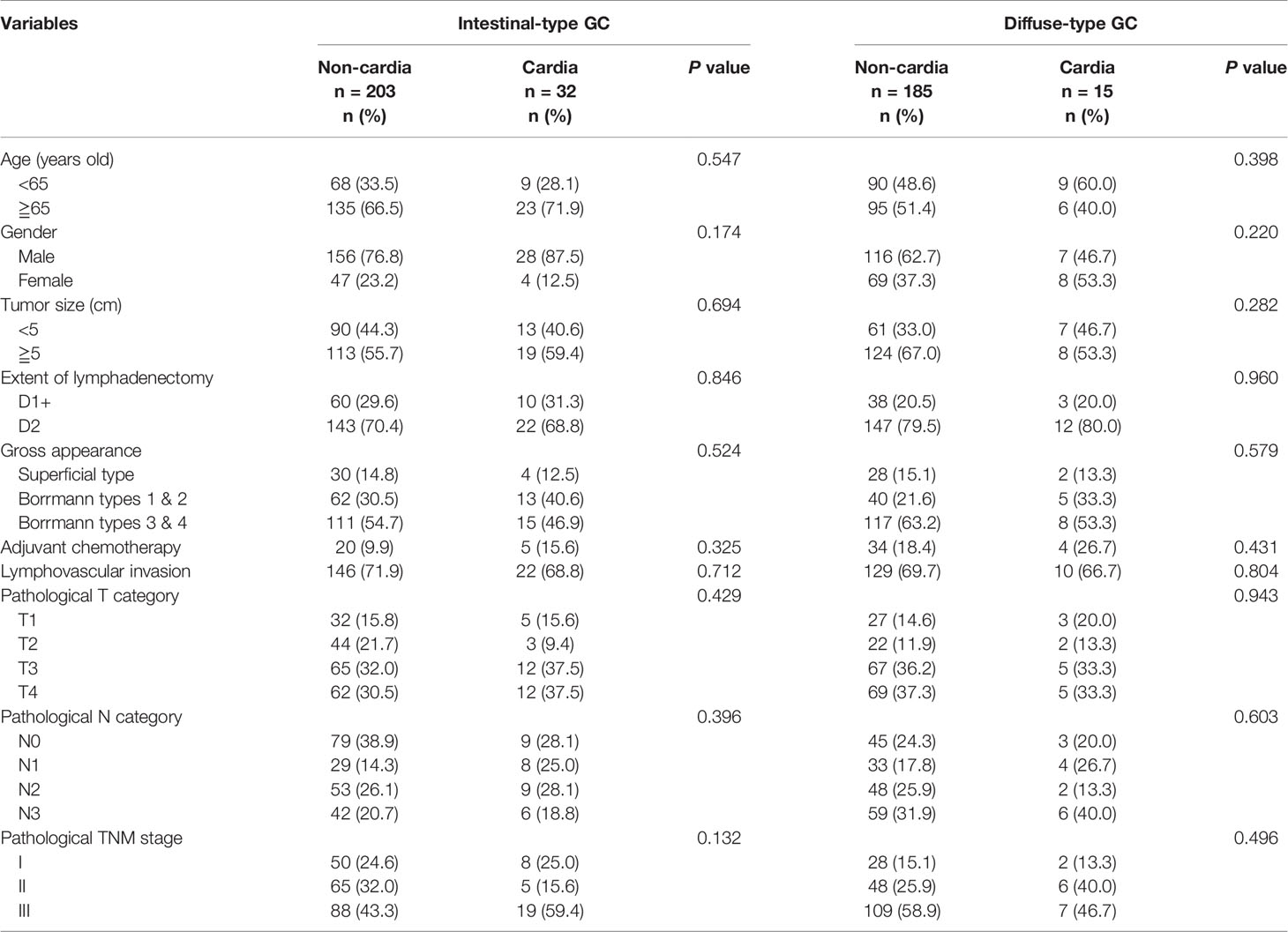
Table 2 Clinical profile between cardia and non-cardia GC patients in intestinal-type and diffuse-type GC.
Initial Recurrence Patterns
Among the 435 patients, 145 (33.3%) experienced tumor recurrence. As shown in Table 3, no significant difference was observed in the initial recurrence pattern between cardia and noncardia GC or between intestinal-type GC and diffuse-type GC.
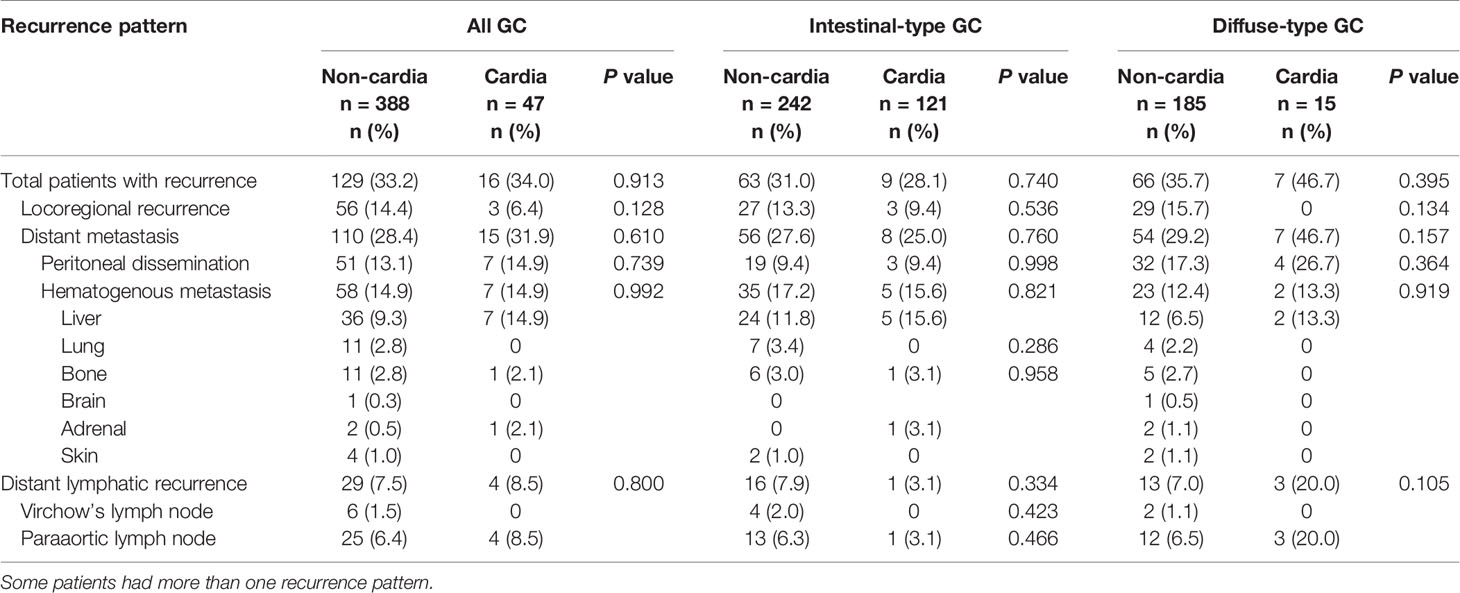
Table 3 The initial recurrence pattern between cardia and non-cardia GC patients in intestinal-type and diffuse-type GC.
Survival Analysis
As shown in Figure 1, there was no significant difference in the 5-year OS (50.8% vs. 50.5%, P = 0.480, Figure 1A) or DFS (48.6% vs. 48.9%, P = 0.392, Figure 1B) between cardia and noncardia GC patients. For intestinal-type GC, the 5-year OS (53.8% vs. 52.5%, P = 0.440, Figure 1C) and DFS (49.3% vs. 51.9%, P = 0.356, Figure 1D) rates were not significantly different between cardia and noncardia GC patients. For diffuse-type GC, the same trends were observed for 5-year OS (46.7% vs. 46.8%, P = 0.759, Figure 1E) and DFS (46.7% vs. 45.4%, P = 0.688, Figure 1F) between cardia and noncardia GC patients.
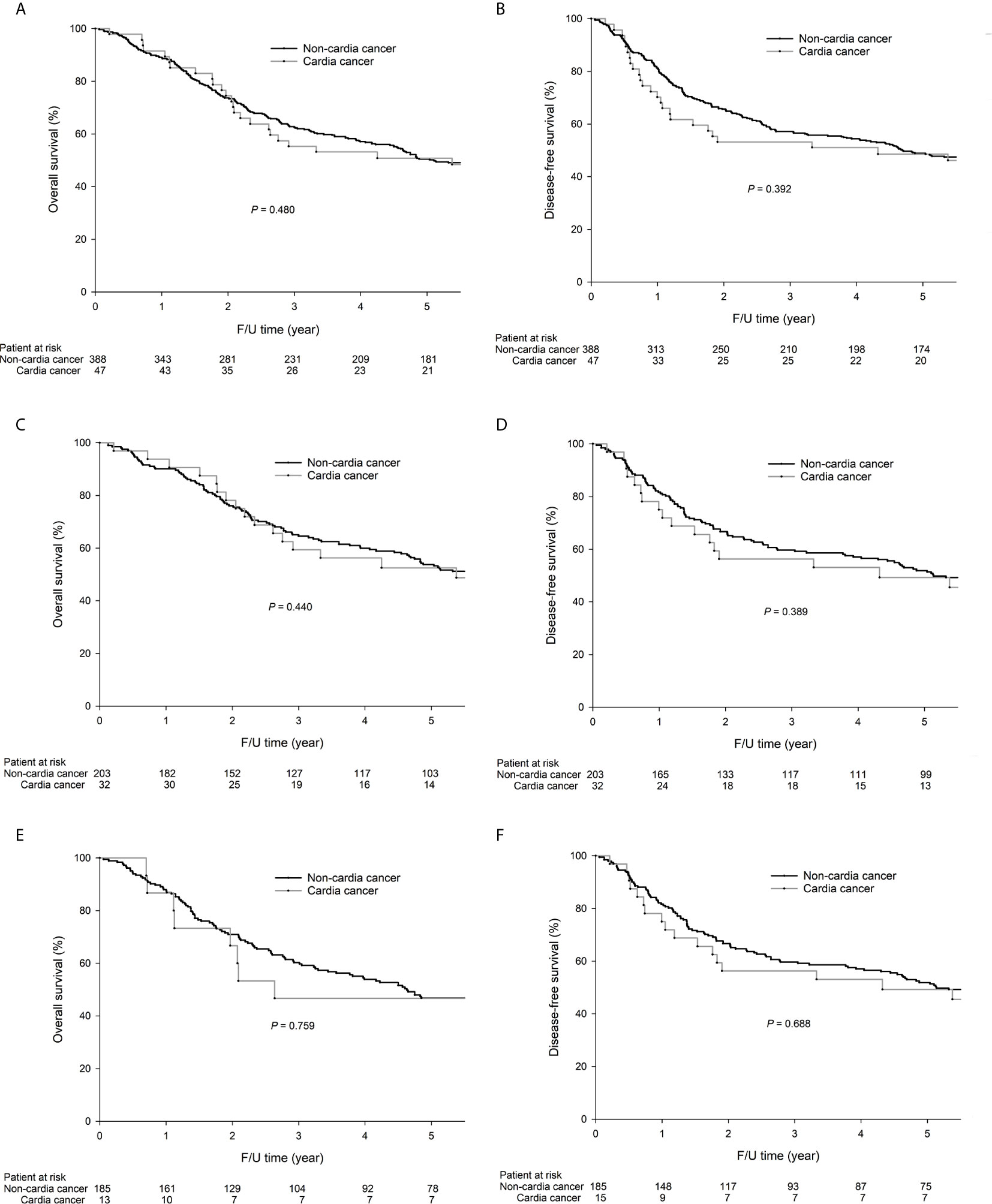
Figure 1 The 5-year OS (50.8% vs. 50.5%, P = 0.480) and DFS (48.6% vs. 48.9%, P = 0.392) rates were not significantly different between cardia and noncardia GC. For intestinal-type GC patients, the 5-year OS (53.8% vs. 52.5%, P = 0.440) and DFS (49.3% vs. 51.9%, P = 0.389) rates were not significantly different between cardia and noncardia GC. For diffuse-type GC patients, the 5-year OS (46.7% vs. 46.8%, P = 0.759) and DFS (46.7% vs. 45.4%, P = 0.688) rates were not significantly different between cardia and noncardia GC. The survival curves are shown as follows: (A) OS curves of all GC patients; (B) DFS curves of all patients; (C) OS curves of intestinal-type GC patients; (D) DFS curves of intestinal-type GC patients; (E) OS curves of diffuse-type GC patients; (F) DFS curves of diffuse-type GC patients.
Univariable analysis demonstrated that age, sex, gross appearance, lymphovascular invasion, pathological T and N categories, and PIK3CA amplification were significantly associated with OS. The seven factors mentioned above, as well as tumor location (cardia GC vs noncardia GC), were included in the multivariable analysis. The Cox proportional hazard model demonstrated that age, gross appearance, and pathological T and N categories were independent prognostic factors of OS (Table 4).
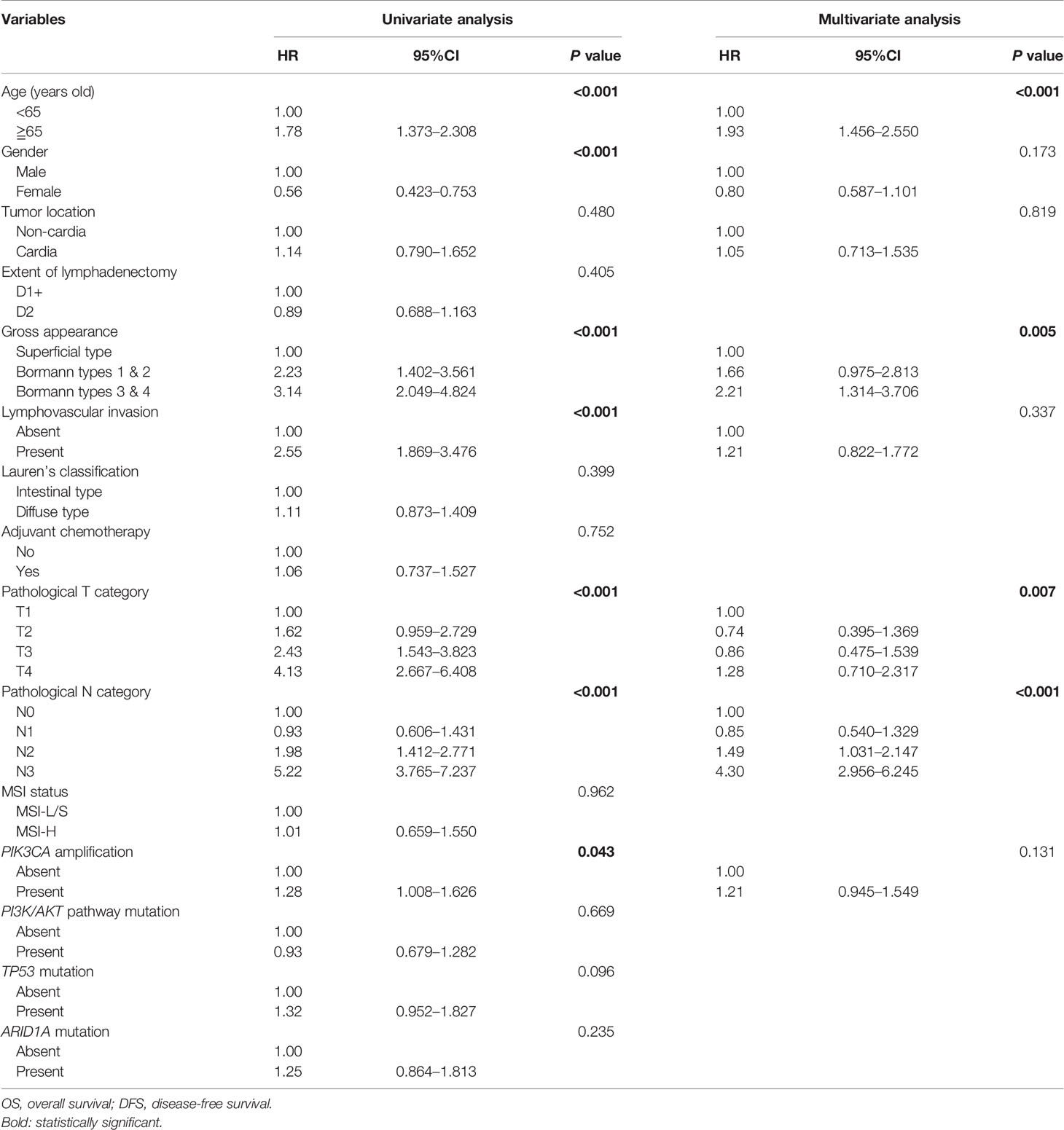
Table 4 Univariate and multivariate analysis of factors affecting OS of GC patients after curative surgery.
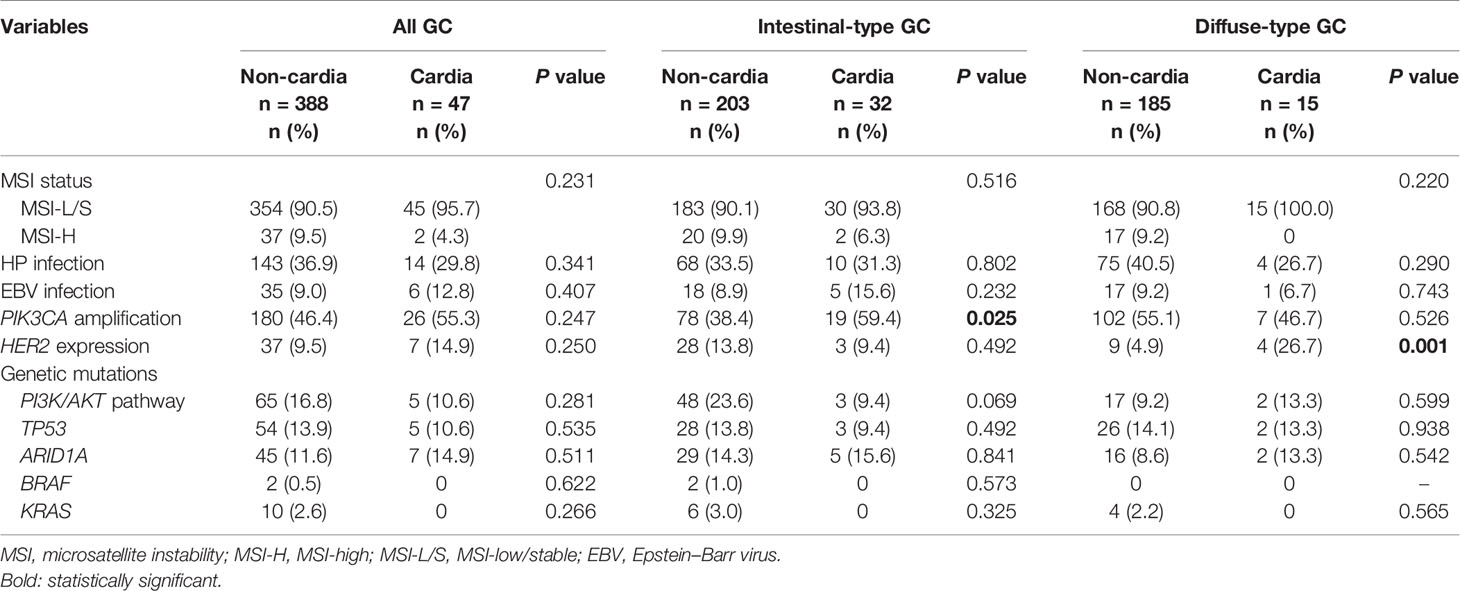
Genetic Analysis
As shown in Table 5, for intestinal-type GC, patients with cardia GC had increased PIK3CA amplification (59.4% vs. 38.4%, P = 0.025) compared to patients with noncardia GC. For diffuse-type GC, patients with cardia GC had increased HER2 expression (26.7% vs. 4.9%) compared to patients with noncardia GC.
Discussion
Cardia GC patients have been reported to have a more advanced tumor stage and unfavorable clinicopathological features at diagnosis than noncardia GC patients (3). However, the 5-year OS was shown to be similar between cardia and noncardia GC patients at each TNM stage (3). In the present study, the clinicopathological features, recurrence patterns, and prognoses were similar between cardia and noncardia GC patients; however, more intestinal-type tumors were observed in cardia GC patients. The multivariable analysis also demonstrated that cardia GC itself is not an independent prognostic factor. According to our results and those of other studies (3), late-stage diagnosis is the main cause of the poorer patient prognosis for cardia GC than noncardia GC.
HER2 expression is higher in the gastric cardia than in other locations of the stomach (6). The correlation between HER2 expression and Lauren’s histologic types remains controversial. Some studies have reported that HER2 expression was associated with intestinal-type GC (7); however, others have reported that HER2 expression was correlated with diffuse-type GC (8). In addition, the presence of HP infection may induce HER2 overexpression (17). Consequently, the discrepancy among studies might be due to the small sample sizes and differences in racial and environmental factors. One of the novel findings of the present study is that HER2 expression is significantly higher in cardia GC patients than in noncardia GC patients among those with diffuse-type GC but not intestinal-type GC. A randomized controlled trial demonstrated that trastuzumab in combination with chemotherapy improved survival in patients with advanced gastric or gastroesophageal junction cancer compared with chemotherapy alone (16). The frequency of HER2 expression in the GC patients enrolled in the present study was 10.1%, which was considered the cutoff percentage for targeted therapy benefits. According to our results, we recommend performing IHC staining for HER2 in patients with diffuse-type GC, as targeted therapy may be beneficial for this subtype.
It has been reported that PIK3CA amplification was associated with GC-related death (18); in addition, patients with PIK3CA amplification had worse survival than patients without PIK3CA amplification, which is similar to our results. In the present study, cardia GC was associated with higher PIK3CA amplification than noncardia GC but only among intestinal-type GC patients, not diffuse-type GC patients. In vivo and in vitro studies demonstrated the significance of proapoptotic and antiproliferative inhibition of PI3K. Therapeutic agents targeting PI3K have been applied in phase 1 and phase 2 clinical trials among patients with gastrointestinal cancer. In addition, combination therapy with PI3K inhibitors and other targeted therapies are under investigation (19). The frequency of PIK3CA amplifications in the enrolled GC patients in the present study was 47.4%, which was considered the cutoff percentage for targeted therapy benefits. According to our results, we recommend testing for PIK3CA amplification in intestinal-type cardia cancer patients, as they may benefit from targeted therapy.
Four molecular subtypes of GC using the database of The Cancer Genome Atlas (TCGA) have been reported (20); however, the etiology and genetic alterations of cardia GC are still not well known. Our results demonstrated that cardia GC presented with more intestinal-type tumors than noncardia GC, which was also reported in a TCGA analysis (20). The differences between cardia GC and noncardia GC are multifactorial, involving etiology, biological behaviors, lifestyle, HP infection, EBV infection, gastroesophageal reflux disease, environment, and genetic and epigenetics (21). For economic reasons, we used the MassARRAY method to analyze genetic mutations. Despite the high cost, we believe that next-generation sequencing could provide additional information on differences in the genetic alterations between cardia and noncardia GC; we plan to implement this technique in future research on this topic.
In the present study, the top three genetic mutations in gastric cardia and noncardia cancer were in the PI3K/AKT pathway, TP53 and ARID1A. In the present study, the frequency of PI3K/AKT pathway mutations was not significantly different between patients with cardia and noncardia GC. It has been reported that only tumors located in the middle third of the stomach show an increase in PIK3CA mutations (22). EBV infection was associated with PIK3CA mutation, especially in the body of the stomach (20). EBV infection and PIK3CA mutation are more likely to induce carcinogenesis in the middle third of the stomach. TP53 mutations can upregulate the transcription of vascular endothelial growth factor receptor-2 (VEGFR2) by promoter remodeling (23). A significant increase in VEGF expression was observed in cancer patients with TP53 mutations (24). The anti-VEGFR2 inhibitor ramucirumab combined with paclitaxel has been approved as the standard second-line systemic therapy (25); however, the survival benefit is limited and novel combination therapies with other targeted therapies and immunotherapy may be beneficial for patient outcome (26). ARID1A, a tumor suppressor gene, has been identified as the second most mutated gene after TP53 in GC (19), and ARID1A deficiency is associated with poor prognosis and lymph node metastasis in GC patients (27). Loss of ARID1A expression correlated with increased PD-L1 expression (28), and ARID1A mutation was associated with MSI and EBV infection (29). Consequently, immunotherapy might be beneficial for GC patients with ARID1A alterations.
One of the limitations of this study is its retrospective and single-center nature. In addition, the number of cardia GC patients in the molecular analysis was small, which may have caused selection bias. In the future, more patients from different countries and races are needed to validate our results, which may provide convincing evidence for GC treatment in the future.
Conclusion
In conclusion, cardia GC is not an independent prognostic factor. For intestinal-type GC, PIK3CA amplification was more common in cardia GC patients than in noncardia GC patients. For diffuse-type GC, HER2 expression was more common in cardia GC patients than in noncardia GC patients. Targeted therapy may be beneficial for these patient subgroups.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by The Institutional Review Board of Taipei Veterans General Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
Conceptualization: S-MP, K-HH, M-HC, W-LF, YC, S-SL, AF-Y, C-WW, and Y-MS. Data curation: S-MP and W-LF. Formal analysis: S-MP and W-LF. Funding acquisition: W-LF. Investigation: K-HH, and W-LF. Methodology: K-HH, and W-LF. Writing—original draft: S-MP and W-LF. Writing—review and editing: W-LF. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by research grants from the Ministry of Science and Technology, Taiwan (107-2314-B-075-007, 107-2314-B-075-005-MY2) and Taipei Veterans General Hospital (V107C-040, V109C-105). The funding sources had no role in the study design, data analysis, or writing and submission of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
AJCC, American Joint Committee on Cancer; DFS, Disease-free survival; EBV, Epstein–Barr virus; FU, Fluorouracil; GC, Gastric cancer; HP, Helicobacter pylori; IHC, Immunohistochemical; ISH, In situ hybridization; MSI, Microsatellite instability; MSI-H, Microsatellite instability-high; MSI-L/S, Microsatellite instability-low/stable; OS, Overall survival; PCR, Polymerase chain reaction; SNP, Single nucleotide polymorphism; TCGA, The Cancer Genome Atlas; TNM, Tumor, node, metastasis; UICC, Union for International Cancer Control; VEGFR2, Vascular endothelial growth factor receptor-2.
References
1. Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, et al. Estimating the Global Cancer Incidence and Mortality in 2018: GLOBOCAN Sources and Methods. Int J Cancer (2019) 144:1941–53. doi: 10.1002/ijc.31937
2. American Joint Committee on Cancer. AJCC Cancer Staging Manual. 8th ed. New York: Springer (2017).
3. An JY, Baik YH, Choi MG, Noh JH, Sohn TS, Bae JM, et al. The Prognosis of Gastric Cardia Cancer After R0 Resection. Am J Surg (2010) 199:725–9. doi: 10.1016/j.amjsurg.2009.04.012
4. Shi Y, Hu Z, Wu C, Dai J, Li H, Dong J, et al. A Genome-Wide Association Study Identifies New Susceptibility Loci for non-Cardia Gastric Cancer At 3q13.31 and 5p13.1. Nat Genet (2011) 43:1215–8. doi: 10.1038/ng.978
5. Hu N, Wang Z, Song X, Wei L, Kim BS, Freedman ND, et al. Genome-Wide Association Study of Gastric Adenocarcinoma in Asia: A Comparison of Associations Between Cardia and non-Cardia Tumours. Gut (2016) 65:1611–8. doi: 10.1136/gutjnl-2015-309340
6. Li GC, Jia XC, Zhao QC, Zhang HW, Yang P, Xu LL, et al. The Expression of Epidermal Growth Factor Receptor 1 and Human Epidermal Growth Factor Receptor 2 Based on Tumor Location Affect Survival in Gastric Cancer. Med (Baltimore) (2020) 99:e20460. doi: 10.1097/MD.0000000000020460
7. He C, Bian XY, Ni XZ, Shen DP, Shen YY, Liu H, et al. Correlation of Human Epidermal Growth Factor Receptor 2 Expression With Clinicopathological Characteristics and Prognosis in Gastric Cancer. World J Gastroenterol (2013) 19:2171–8. doi: 10.3748/wjg.v19.i14.2171
8. Rajadurai P, Fatt HK, Ching FY. Prevalence of HER2 Positivity and Its Clinicopathological Correlation in Locally Advanced/Metastatic Gastric Cancer Patients in Malaysia. J Gastrointest Cancer (2018) 49:150–7. doi: 10.1007/s12029-017-9921-1
9. Fang WL, Lan YT, Huang KH, Liu CA, Hung YP, Lin CH, et al. Clinical Significance of Circulating Plasma DNA in Gastric Cancer. Int J Cancer (2016) 138:2974–83. doi: 10.1002/ijc.30018
10. Japanese Gastric Cancer Association. Japanese Gastric Cancer Treatment Guidelines 2014 (Ver. 4). Gastric Cancer (2017) 20:1–19. doi: 10.1007/s10120-016-0622-4
11. Wu CW, Chen MH, Huang KH, Chang SC, Fang WL, Lin CH, et al. The Clinicopathological Characteristics and Genetic Alterations Between Younger and Older Gastric Cancer Patients With Curative Surgery. Aging (Albany NY) (2020) 12:18137–50. doi: 10.18632/aging.103627
12. Sakuramoto S, Sasako M, Yamaguchi T, Kinoshita T, Fujii M, Nashimoto A, et al. Adjuvant Chemotherapy for Gastric Cancer With S-1, an Oral Fluoropyrimidine. N Engl J Med (2007) 357:1810–20. doi: 10.1056/NEJMoa072252
13. Fang WL, Chang SC, Lan YT, Huang KH, Chen JH, Lo SS, et al. Microsatellite Instability is Associated With a Better Prognosis for Gastric Cancer Patients After Curative Surgery. World J Surg (2012) 36:2131–8. doi: 10.1007/s00268-012-1652-7
14. Fang WL, Huang KH, Chang SC, Lin CH, Chen MH, Chao Y, et al. Comparison of the Clinicopathological Characteristics and Genetic Alterations Between Patients With Gastric Cancer With or Without Helicobacter Pylori Infection. Oncologist (2019) 24:e845–53. doi: 10.1634/theoncologist.2018-0742
15. Ribeiro J, Oliveira A, Malta M, Oliveira C, Silva F, Galaghar A, et al. Clinical and Pathological Chaterization of Epstein-Barr Virus-Associated Gastric Carcinoma in Portugal. World J Gastroenterol (2017) 23:7292–302. doi: 10.3748/wjg.v23.i40.7292
16. Bang YJ, Cutsem EV, Feyereislova A, Chung HC, Shen L, Sawaki A, et al. Trastuzumab in Combination With Chemotherapy Versus Chemotherapy Alone for Treatment of HER2-positive Advanced Gastric or Gastro-Oesophageal Junction Cancer (ToGA): A Phase 3, Open-Label, Randomised Controlled Trial. Lancet (2010) 376:687–97. doi: 10.1016/S0140-6736(10)61121-X
17. Yoo MW, Han HS, Kim SY, Cho YH, Lee HG, Kim JH, et al. Is Helicobacter Pylori Associated With Her2/neu Overexpression in Gastric Cancer Patients Who Underwent Curative Resection? Hepatogastroenterology (2014) 61:858–62.
18. Shi J, Yao D, Liu W, Wang N, Lv H, Zhang G, et al. Highly Frequent PIK3CA Amplification is Associated With Poor Prognosis in Gastric Cancer. BMC Cancer (2012) 12:50. doi: 10.1186/1471-2407-12-50
19. Hashemzadeh K, Jokar MH, Sedighi S, Moradzadeh M. Therapeutic Potency of PI3K Pharmacological Inhibitors of Gastrointestinal Cancer. Middle East J Dig Dis (2019) 11:5–16. doi: 10.15171/mejdd.2018.122
20. Cancer Genome Atlas Research Network. Comprehensive Molecular Characterization of Gastric Adenocarcinoma. Nature (2014) 513:202–9. doi: 10.1038/nature13480
21. Abdi E, Latifi-Navid S, Zahri S, Yazdanbod A, Pourfarzi F. Risk Factors Predisposing to Cardia Gastric Adenocarcinoma: Insights and New Perspectives. Cancer Med (2019) 8:6114–26. doi: 10.1002/cam4.2497
22. Fang WL, Huang KH, Lan YT, Lin CH, Chang SC, Chen MH, et al. Mutations in PI3K/AKT Pathway Genes and Amplifications of PIK3CA are Associated With Patterns of Recurrence in Gastric Cancers. Oncotarget (2016) 7:6201–20. doi: 10.18632/oncotarget.6641
23. Pfister NT, Fomin V, Regunath K, Zhou JY, Zhou W, Silwal-Pandit L, et al. Mutant p53 Cooperates With the SWI/SNF Chromatin Remodeling Complex to Regulate VEGFR2 in Breast Cancer Cells. Genes Dev (2015) 29:1298–315. doi: 10.1101/gad.263202.115
24. Li AM, Boichard A, Kurzrock R. Mutated TP53 is a Marker of Increased VEGF Expression: Analysis of 7,525 Pan-Cancer Tissues. Cancer Biol Ther (2020) 21:95–100. doi: 10.1080/15384047.2019.1665956
25. Casak SJ, Fashoyin-Aje I, Lemery SJ, Zhang L, Jin R, Li H, et al. Fda Approval Summary: Ramucirumab for Gastric Cancer. Clin Cancer Res (2015) 21:3372–6. doi: 10.1158/1078-0432.CCR-15-0600
26. Khan U, Shah MA. Ramucirumab for the Treatment of Gastric or Gastro-Esophageal Junction Cancer. Expert Opin Biol Ther (2019) 19:1135–41. doi: 10.1080/14712598.2019.1656715
27. Yang L, Wei S, Zhao R, Wu Y, Qiu H, Xiong H. Loss of ARID1A Expression Predicts Poor Survival Prognosis in Gastric Cancer: A Systematic Meta-Analysis From 14 Studies. Sci Rep (2016) 6:28919. doi: 10.1038/srep28919
28. Tober JM, Halske C, Behrens HM, Krüger S, Röcken C. Intratumoral Heterogeneity and Loss of ARID1A Expression in Gastric Cancer Correlates With Increased PD-L1 Expression in Western Patients. Hum Pathol (2019) 94:98–109. doi: 10.1016/j.humpath.2019.09.016
Keywords: gastric cancer, cardia, noncardia, genetic alteration, PIK3CA amplification, HER2 expression
Citation: Pai S-M, Huang K-H, Chen M-H, Fang W-L, Chao Y, Lo S-S, Li AF-Y, Wu C-W and Shyr Y-M (2021) Cardia Gastric Cancer Is Associated With Increased PIK3CA Amplifications and HER2 Expression Than Noncardia Gastric Cancer According to Lauren Classification. Front. Oncol. 11:632609. doi: 10.3389/fonc.2021.632609
Received: 23 November 2020; Accepted: 17 May 2021;
Published: 08 June 2021.
Edited by:
Kecheng Zhang, People’s Liberation Army General Hospital, ChinaReviewed by:
Paulo Kassab, Santa Casa of Sao Paulo, BrazilPo-Jen Yang, National Taiwan University Hospital, Taiwan
Po-Chu Lee, National Taiwan University Hospital, Taiwan
Copyright © 2021 Pai, Huang, Chen, Fang, Chao, Lo, Li, Wu and Shyr. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wen-Liang Fang, d2xmYW5nQHZnaHRwZS5nb3YudHc=
 Shih-Min Pai1,2
Shih-Min Pai1,2 Wen-Liang Fang
Wen-Liang Fang