- 1Department of Cardiology, Fujian Provincial Hospital, Shengli Clinical Medical College of Fujian Medical University, Fuzhou, China
- 2Fujian Provincial Key Laboratory of Cardiovascular Disease, Fujian Cardiovascular Institute, Fujian Provincial Center for Geriatrics, Fujian Clinical Medical Research Center for Cardiovascular Diseases, Fuzhou, China
- 3Department of Hematology, Fujian Provincial Hospital, Shengli Clinical Medical College of Fujian Medical University, Fuzhou, China
- 4Department of Hematology, Fujian Heart Failure Center Alliance, Fuzhou, China
Extranodal NK/T-cell lymphoma (ENKTL) is a rare but aggressive subtype of non-Hodgkin lymphoma, which is derived from NK cells or T cells. There are very few cases of ENKTL invading the heart. Only 12 cases of ENKTL invading the heart have been reported in the English literature. Due to the rarity of this lymphoma, an effective therapeutic strategy has not been defined. Here, we present a case of a 51-year-old Chinese male with extranodal NK/T-cell lymphoma invading the heart and review the literature. The patient received a chemotherapy regimen of PD1 monoclonal antibody (Sintilimab) in combination with first-line P-Gemox. The patient survived for 2 months after diagnosis.
Introduction
Extranodal NK/T-cell lymphoma is a rare non-Hodgkin lymphoma with dismal outcomes and limited treatment options. According to anatomic origin and clinical manifestations, ENKTL can be divided into nasal, non-nasal, and aggressive/leukemia subtypes. Of the three types, the non-nasal type has much lower survival rate (1). The incidence of this disease is higher in China than in Western countries, and the prognosis is poor with traditional treatments (2, 3). Improving the treatment is an urgent requirement.
Here we report a patient having ENKTL invading the heart. Initially, the patient’s heart failure was thought to be due to pre-existing hypertrophic obstructive cardiomyopathy. Later, with the elevation of cardiac protein, rapid progression of heart failure and MODS, the patient was considered to have acute myocarditis, and finally ENKTL invading the heart was considered by biopsy of nodules found in the patient’s body and whole-body PET-CT.
Case persentation
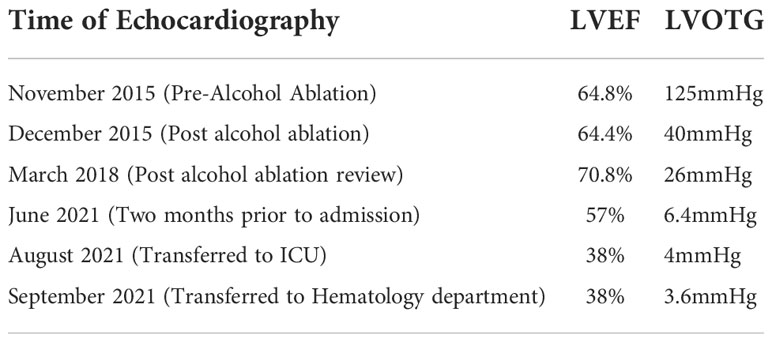
A 51-year-old man was admitted to our hospital with weakness and recurrent shortness of breath for almost a year, which was aggravated for two days. Two months prior to admission, a echocardiography showed left ventricular ejection fraction (LVEF) = 57% (Table 1). He was treated with alcohol ablation for hypertrophic obstructive cardiomyopathy 6 years ago. Laboratory tests after admission showed N-terminal pro-brain natriuretic peptide(NT-proBNP): 9077.00Pg/ml, Troponin T: 0.32ng/ml, ALT: 274U/L, AST: 432U/L, D dimer: 6.30mg/L. Therefore, acute heart failure is considered based on the patient’s condition and laboratory tests. The patient’s symptoms suddenly deteriorated two days after admission without any obvious cause, and laboratory tests found ALT: 1997U/L, AST: 2552U/L, D dimer:>35mg/L, LDH:2900U/L. The patient presenting acute heart failure combined with acute liver failure, MODS can be diagnosed. Thus, the patient was transferred to the ICU for further treatment.
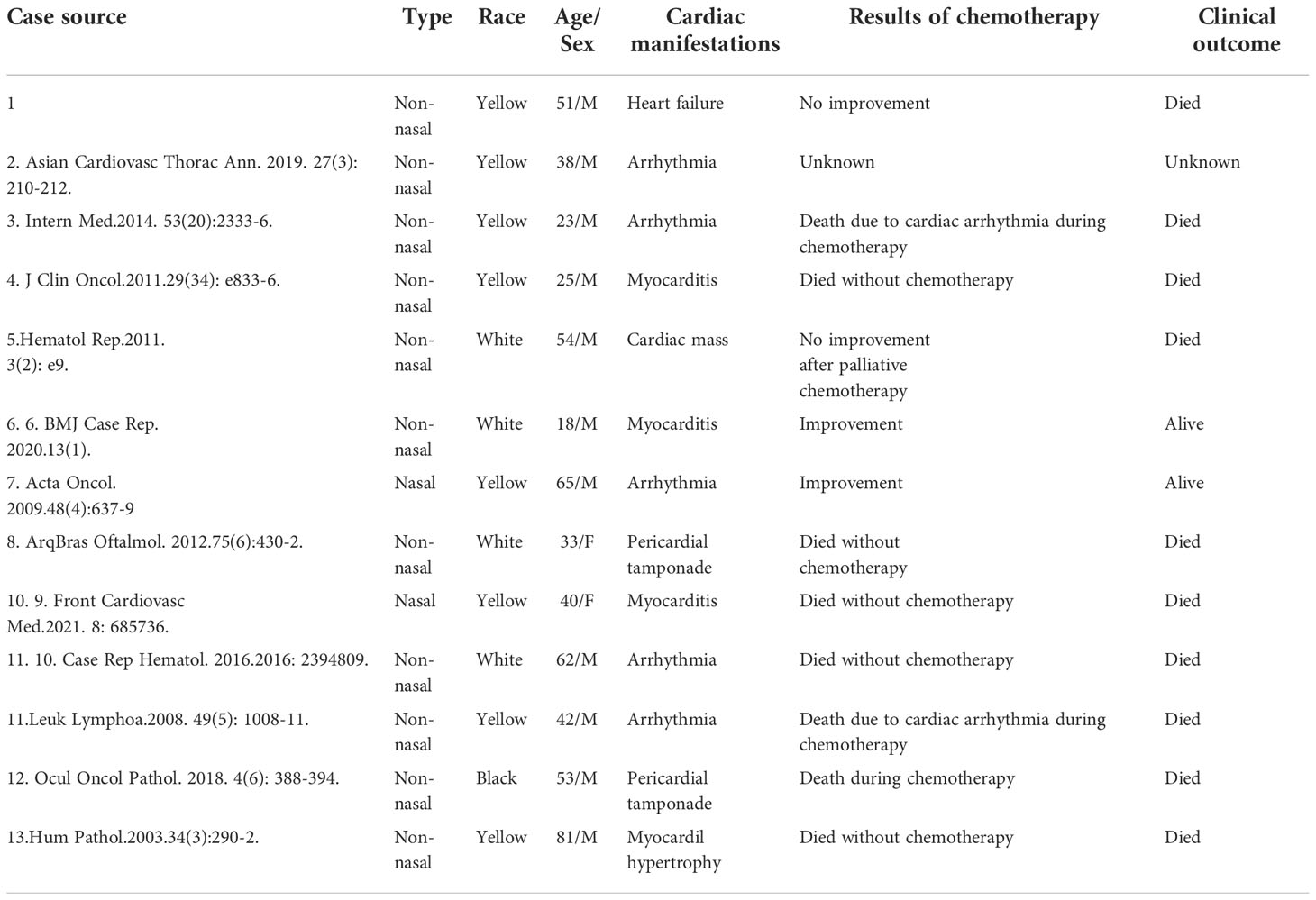
After transferred to ICU, the patient’s symptoms further deteriorate with oliguria and significantly increased NT-proBNP. Acute heart failure combined with acute kidney injury was taken into account. While in the ICU, a review of laboratory indicators indicated a rapid progression of NT-proBNP(25950Pg/ml), a sharp rise in troponin T(3.29ng/ml), and a progressive rise in ALT(2017U/L) and AST(2552U/L). By this time, the patient’s pre-existing hypertrophic obstructive cardiomyopathy could no longer explain the patient’s deteriorating condition. Consequently, fulminant myocarditis was taken into consideration. After administration of high dose methylprednisolone, the patient’s symptoms were relieved. Echocardiography revealed significant thickening of the septum and left ventricular wall, pericardial effusion with decreased left ventricular myocardial contractility(LVEF=38%) (Table 1). The patient was treated with pericardiocentesis to drain the pericardial fluid and sent it for examination to determine its nature. And the nature of the pericardial fluid returned showed lymphoma cells. Meanwhile, because of the progression of an inadvertently discovered groin swelling, excision of the inguinal mass was performed, post-operative pathological return: moderate-sized lymphoid tumor cells showing diffuse infiltration with multifocal map-like necrosis. Immunohistochemistry showed: Ki-67(70%+), CD20 (–), CD79a(Focal weak +), PAX5(-), CD3(++), CD5(++), CD43(++), CD4(-), CD8(++), CD56(-), TIA-1 (++), EBER(+), CD30(-), ALKp80(-), TdT(-), CD123(-), CD68(-), CD10(-), BCL6(-), MUMI(++). Combined with the above results, the diagnosis of extranodal NK/T-cell lymphoma(ENKTL) was confirmed (Figure 1). Furthermore, PET-CT of the whole body demonstrated that multiple involvement of the heart, skin, blood vessels and muscles without nasal involvement (Figure 2). Hence, the patient was regarded as having ENKTL invading the heart. The patient’s rapid progression of heart failure, myocardial injury and MODS were taken into account to be caused by the progressive myocardial infiltration of ENKTL. The palliative effect of glucocorticoids on the patient was considered to be due to the inhibition of the cytokine storm caused by ENKTL rather than inhibition of myocardial inflammation. The reason for this is that the effect of glucocorticosteroids on the patient is rapidly diminishing and the patient’s cardiac function is not improving significantly.
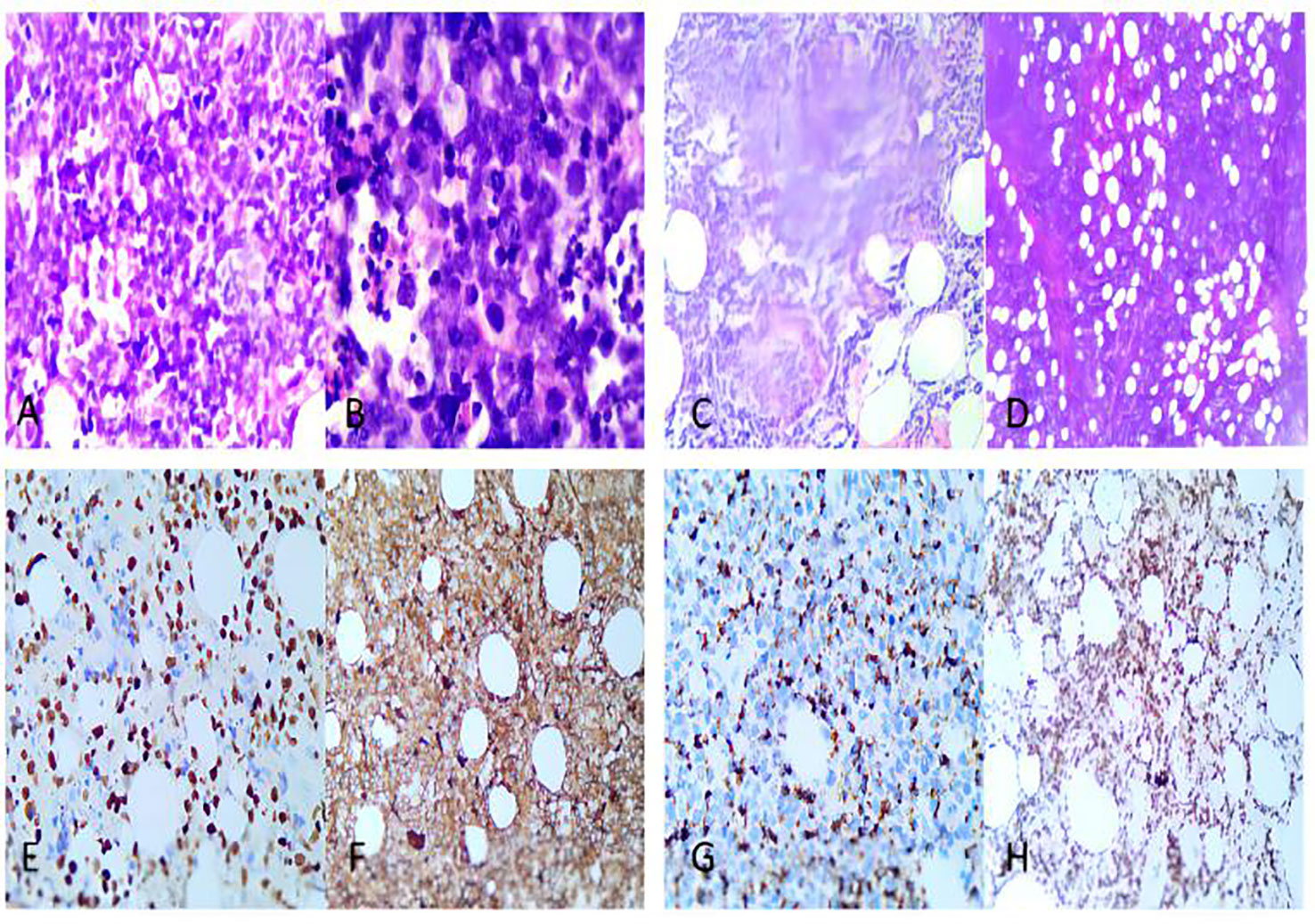
Figure 1 Pathological and immunohistochemical images of the patient. (A, B). Obviously heterogeneous medium-sized tumor cells with apoptotic nuclear fragmentation. (C). Tumor cells angiodestructive growth (D). Subcutaneous interfatty infiltration with extensive necrosis. (E). EBER positive. (F). CD3-positive. (G). TIA1-positive. (H). Ki-67 positive, shows high value-added index.
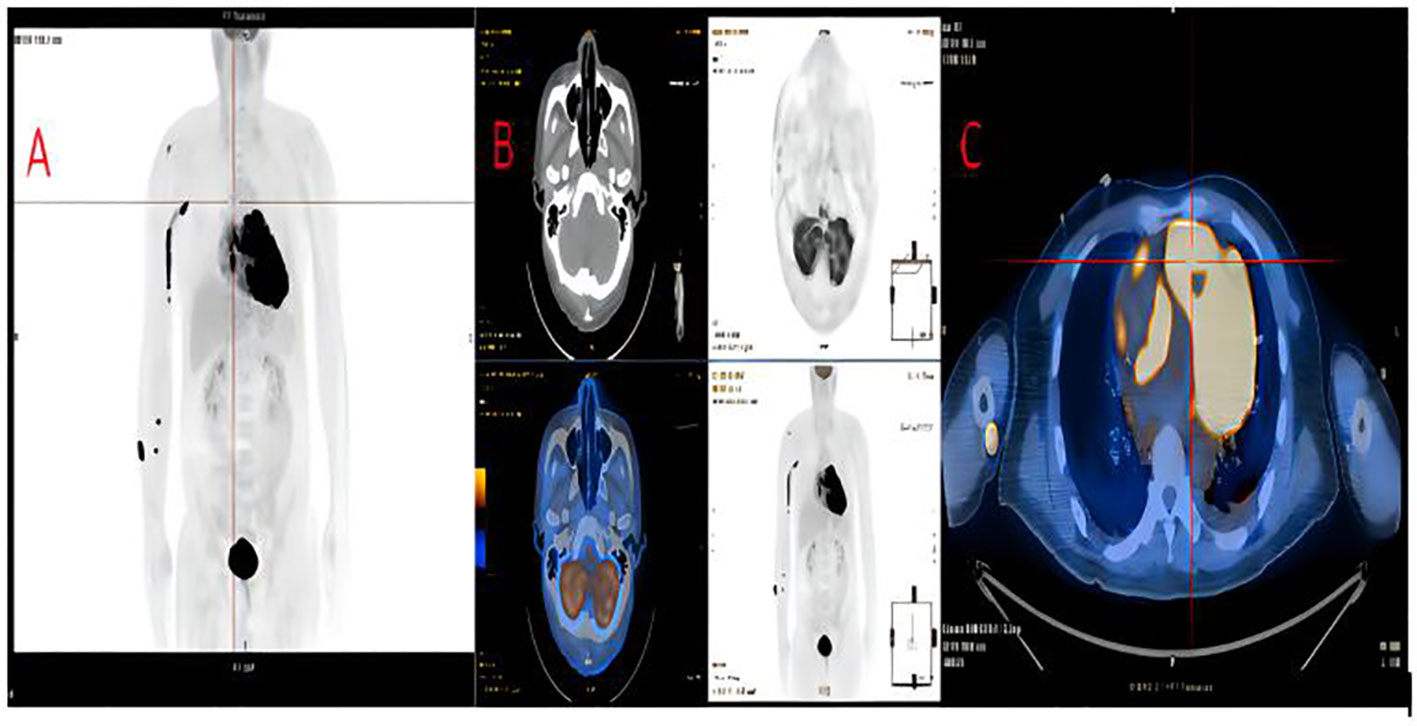
Figure 2 The whole pet-ct of this patient. (A). Multiple involvement throughout the body, including the heart, blood vessels, muscles, and skin. (B). No involvement of the nasal cavity. (C). Cardiac involvement: including the LV as well as the funnel of the RV.
After the patient’s condition stabilized and all laboratory indicators improved, he was transferred to the hematology department for chemotherapy. The results of echocardiography were similar to the previous results.(LVEF=38%) and laboratory tests showed NT-proBNP: 10246.00Pg/ml, Troponin T: 0.84ng/ml. Considering the severity of the patient’s disease, first-line P-Gemox regimen combined with PD-1 monoclonal antibody was administered. This regimen included sintilimab(200mg, day0), gemcitabine(1.8g, day1, day8), oxaliplatin(230mg, day1) and pegaspargase(3750U, day1). Taking into account the poor prognosis of ENKTL invasion of the heart combined with the patient’s physical condition at the time, the dose used in this patient’s chemotherapy regimen was adequate. During chemotherapy the patient’s nodules did not improve, and chidamide(30mg, BIW) was given to improve the efficacy of the treatment. At the end of the current chemotherapy course, the patient’s nodules did not improve and even new nodules appeared. In the meantime, the patient’s heart function also did not show improvement, and laboratory results showed NT-proBNP: 10648.00Pg/ml, Troponin T: 0.25ng/ml. Finally, the patients decided to be discharged automatically. After automatic discharge, the patient’s cardiac function deteriorated further, with symptoms of orthopnea, nocturnal paroxysmal dyspnea and edema of both lower limbs. Moreover, the patient’s skin nodules were larger and more numerous than previously, and they were breaking down. In the end, the patient died at home on October 4, 2021.
Discussion
ENKTL is a kind of aggressive Epstein‐Barr virus (EBV) infection‐related NHL stemmed from mature NK cells and NK‐Like T Cells, and shows highly‐aggressive progression. Nevertheless, to our knowledge, there are only few cases of ENKTL invading the heart, and the non-nasal type accounts for the majority of these cases. The non-nasal ENKTL, which originates in rare sites like the eyes and skin, are more likely to invade the heart than the nasal type, which may partly account for its poor prognosis.
Not only is the number of cases rare, but patients with ENKTL invading the heart are also prone to misdiagnosis of myocarditis, heart failure and arrhythmias. Whole-body PET-CT with echocardiography is indispensable in the diagnostic process of such diseases. Moreover, this type of patient has poor prognosis, often with death as the clinical outcome (Table 2) (1, 4–14).
These features were also seen in our reported cases. However, unlike the previously reported cases, our case has its own characteristics: history of hypertrophic obstructive cardiomyopathy. Because of this feature, the patient’s echocardiographic findings were not emphasized in the early stages. At the same time, because the history of heart disease was longer than the time of its nodal onset, it was thought to be a recurrence of hypertrophic obstructive cardiomyopathy triggering cardiac problems. These mislead clinicians about the diagnosis of the disease. In addition, to the best of our knowledge, this is the first case of ENKTL invading the heart in a patient with hypertrophic obstructive cardiomyopathy.
As ENKTL is one of the most difficult subtypes to treat and is associated with a poor prognosis, current treatment strategies have not been clear defined. Based on the only two surviving cases with successful chemotherapy, after successful chemotherapy for ENKTL invasion of the heart, significant improvements in various parameters such as echocardiography were observed, indicating that the results it caused could be reversed by chemotherapy (7, 8). Therefore, despite the adverse effects such as malignant arrhythmias that can occur in patients during chemotherapy, chemotherapy is still recommended as the preferred method once the diagnosis is confirmed. For the present, there is no standard chemotherapy regimen for ENKTL. In our case, we used the P-Gemox chemotherapy regimen, which has entered the National Comprehensive Cancer Network (NCCN) guidelines. In an oral presentation at ASH, the combination of Sintilimab and Chidamide was shown to have good antitumor activity in the treatment of patients with refractory or relapsed nasal ENKTL. In 36 refractory patients with evaluable efficacy, an overall efficacy rate of 58.3%, a complete remission rate of 44.4%, and an effective maintenance time of more than 9.2 months were achieved with a manageable safety profile (15). In contrast, the SMILE regimen used in successful cases has side effects that are so strong that patients may not tolerate them. Moreover, in a Japanese multicenter study, the SMILE regimen was reported to be ineffective in non-nasal type patients, with a 2-year overall survival of 34%, while it was more effective in nasal type patients, with a 2-year overall survival of 70% (16). Hence, the regimen we have adopted is already at the forefront of international regimens and is appropriate for the patient’s condition. Despite this, the patient’s skin nodules and heart failure continued to progress under this chemotherapy regimen. This makes us wonder about the refractory nature of ENKTL. Current considerations for the refractoriness and recurrence of ENKTL are due to immune evasion, some studies have shown that ENKTL cells avoid immune surveillance and the consequent killing of ENKTL, resulting in a poor outcome (17). This may be the reason why patients are resistant to Sintilimab. Such an outcome corresponds exactly to the poor prognosis of non-nasal ENKTL. This calls for further exploration of regimens for this disease.
Our case together with the summary of previous case reports illustrate (1). Non-nasal ENKTL is more likely to invade the heart and has a poorer prognosis than the nasal type (2). Our case is the first case of ENKTL invading the heart in a patient with hypertrophic obstructive cardiomyopathy (3). The regimen we used is already extremely cutting-edge clinically and has better efficacy and longer survival time for refractory recurrent ENKTL compared to the traditional SMILE regimen. Nonetheless, the results are still poor for our patients, which warrants for further exploration of chemotherapy regimens for this type of disease.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Fujian Provincial Hospital ethics committee. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
YX was responsible for the clinical design and conceptualization. YX and XL wrote the manuscript. XC was involved in the acquisition of the clinical data. SQ and K-YL conducted the clinical diagnosis. All authors discussed, read, and approved the submission of this manuscript to the journal.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
- ^ ENKTL, extranodal natural killer/T-cell lymphoma; MODS, multiple organ dysfunction syndrome; PET-CT, positron emission tomography - computed tomography; LVEF, left ventricular ejection fraction; LVOTG, left ventricular outflow tract gradient.
References
1. Farfán-Leal F, Esteban A, Hinojar R, García-Cosío M, Contreras F. Primary cardiac natural killer/T-cell lymphoma, a very rare form of lymphoma. Asian Cardiovasc Thorac Ann (2019) 27(3):210–2. doi: 10.1177/0218492318798230
2. Tse E, Kwong YL. How I treat NK/T-cell lymphomas. Blood (2013) 121:4997–5005. doi: 10.1182/blood-2013-01-453233
3. Lee J, Suh C, Park YH, Ko YH, Bang SM, Lee JH, et al. Extranodal natural killer T-cell lymphoma, nasal-type: a prognostic model from a retrospective multicenter study. J Clin Oncol (2006) 24:612–8. doi: 10.1200/JCO.2005.04.1384
4. Baek YS, Shin SH, Yi HG, Kim DH, Woo SI, Park KS, et al. Cardiac involvement in CD56 negative primary pancreatic extranodal NK/T-cell lymphoma, nasal type, presenting with ventricular tachycardia during the early stages of chemotherapy. Intern Med. (2014) 53(20):2333–6.
5. Huang SH, Hsieh SC, Ko BS, Liu YB. Cardiac involvement of natural killer/T-cell lymphoma presenting with electrical storm after cardioverter-defibrillator implantation. J Clin Oncol (2011) 29(34):e833–6. doi: 10.1200/JCO.2011.36.7276
6. Lepeak LM, Yang DT, Chang JE. Extranodal NK/T-cell lymphoma presenting with primary cardiac involvement. Hematol Rep (2011) 3(2):e9. doi: 10.4081/hr.2011.e9
7. Leonor Lopez GL, Chaparro SV, Brozzi N, Badiye A. Heart failure enigma in young man: the acute onset of a frequently encountered condition with an unexpected cause. BMJ Case Rep (2020) 13(1):e233190. doi: 10.1136/bcr-2019-233190
8. Kanesvaran R, Tao M, Huat IT, Weng DT, Eng DN, Thye LS. Malignant arrhythmia: a case report of nasal NK/T-cell lymphoma with cardiac involvement. Acta Oncol (2009) 48(4):637–9. doi: 10.1080/02841860902740923
9. Abe RY, Pinto RD, Bonfitto JF, Lira RP, Arieta CE. Ocular masquerade syndrome associated with extranodal nasal natural killer/T-cell lymphoma: case report. Arq Bras Oftalmol (2012) 75(6):430–2. doi: 10.1590/S0004-27492012000600013
10. Zhang Z, Wang S, Liang Q, Peng D. Progressive heart failure and death as the initial manifestation of NK/T-cell lymphoma: A case report and literature review. Front Cardiovasc Med (2021) 8:685736. doi: 10.3389/fcvm.2021.685736
11. Li Y, Damjanov I. Extranodal NK/T cell lymphoma causing cardiorespiratory failure. Case Rep Hematol (2016) 2016:2394809. doi: 10.1155/2016/2394809
12. Kawasaki H, Shigeno Ohnishi K, Tsuchida T, Miura K, Kato T. A case of primary cutaneous natural killer/T-cell lymphoma, nasal type, directly invading to the heart. Leuk Lymphoma (2008) 49:1008–11.
13. Thompson AC, McCall CM, Proia AD. Beneath the retinal pigment epithelium: Histopathologic findings in metastatic extranodal natural Killer/T-cell lymphoma, nasal type. Ocul Oncol Pathol (2018) 4:388–94. doi: 10.1159/000487268
14. Kuwabara H, Tsuji M, Yoshii Y, Kakuno Y, Akioka T, Kotani T, et al. Nasal-type NK/T cell lymphoma of the orbit with distant metastases. Hum Pathol (2003) 34:290–2.
15. Gao Y HHQ, Wang XX ea. Anti-PD-1 antibody (Sintilimab) plus histone deacetylase inhibitor (Chidamide) for the treatment of refractory or relapsed extranodal natural Killer/T cell lymphoma, nasal type (r/r-ENKTL): preliminary results from a prospective, multicenter,single arm, phase Ib/II trial (SCENT). Blood (2020) 136(Supplement 1):39–40. doi: 10.1182/blood-2020-134665
16. Yamaguchi M, Suzuki R, Miyazaki K, Amaki J, Takizawa J, Sekiguchi N, et al. Improved prognosis of extranodal NK/T cell lymphoma, nasal type of nasal origin but not extranasal origin. Ann Hematol. (2019) 98(7):1647–55.
Keywords: extranodal natural killer/T-cell lymphoma, heart failure, poor prognosis, targeted therapy, PET-CT
Citation: Xiang Y, Lin X, Cai X, Qu S and Lin K-Y (2022) Extranodal natural killer/T-cell lymphoma invading a patient’s heart: A rare case report and literature review. Front. Oncol. 12:1011894. doi: 10.3389/fonc.2022.1011894
Received: 04 August 2022; Accepted: 21 November 2022;
Published: 07 December 2022.
Edited by:
Carlo Gabriele Tocchetti, University of Naples Federico II, ItalyReviewed by:
Yuqin Song, Beijing Cancer Hospital, Peking University, ChinaXin Wang, Shandong Provincial Hospital, China
Copyright © 2022 Xiang, Lin, Cai, Qu and Lin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shuang Qu, c2h1YW5nZXJxdUAxNjMuY29t; Kai-Yang Lin, bGt5NzQxMUBzaW5hLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Yifei Xiang
Yifei Xiang Xueqin Lin
Xueqin Lin Xiaoling Cai1,2
Xiaoling Cai1,2 Kai-Yang Lin
Kai-Yang Lin