- 1Department of Acupuncture and Rehabilitation, Jiangsu Province Hospital of Chinese Medicine, Affiliated Hospital of Nanjing University of Chinese Medicine, Nanjing, China
- 2Department of Acupuncture and Rehabilitation, Nanjing Traditional Chinese Medicine Hospital, Affiliated Hospital of Nanjing University of Chinese Medicine, Nanjing, China
- 3The Second Clinical Medical College, Nanjing University of Chinese Medicine, Nanjing, China
- 4Department of Oncology, Jiangsu Cancer Hospital, Affiliated Cancer Hospital of Nanjing Medical University, Nanjing, China
Background: Studies on the efficacy of acupuncture and auricular acupressure on sleep disturbances in cancer patients have been growing, but there is no specific and comprehensive systematic review and meta-analysis. This review aims to evaluate the efficacy and safety of acupuncture and auricular acupressure on sleep disturbances in cancer survivors based on existing randomized clinical trials (RCTs).
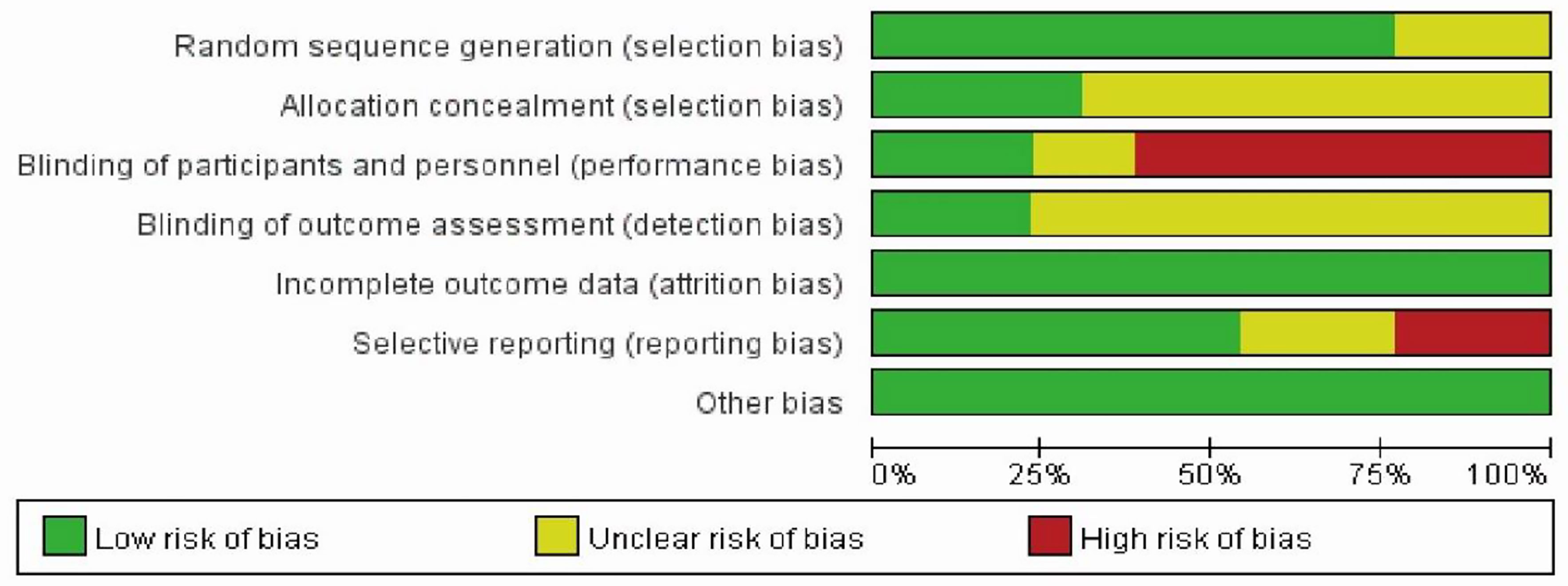
Methods: Four English-language and four Chinese-language biomedical databases were searched for RCTs published from database inception to July 30, 2021. RCTs comparing acupuncture and auricular acupressure with sham control, drug therapy, behavior therapy, or usual care for managing cancer were included. The quality of RCTs was appraised with the Cochrane Collaboration risk of bias (ROB) tool. Mean differences (MDs) and 95% confidence intervals (CIs) were calculated for the effect sizes.
Results: Thirteen RCTs with 961 patients were included. The risk of performance bias or reporting bias for most of the included trials was high or unclear. Evidence was not found for short-term effects on sleep scales compared to sham control (MD, 1.98; 95% CI, 0.33–3.64; p = 0.02; I2 = 36%), wait list control (MD, 0.40; 95% CI, −0.87–1.68; p = 0.54; I2 = 49%), drug therapy (MD, 1.18; 95% CI, −3.09–5.46; p = 0.59; I2 = 98%). For long-term effect, two sham-controlled RCTs showed no significance of acupuncture on insomnia scale scores (MD, 1.71; 95% CI, −2.38–5.81; p = 0.41; I2 = 89%). Subgroup analyses suggested no evidence that auricular acupressure (MD, 3.14; 95% CI=1.52, 4.76; p = 0.0001; I2 = 0%) or acupuncture (MD, 0.54; 95% CI=−1.27, 2.34; p = 0.56; I2 = 0%) was associated with the reduction in insomnia scale scores.
Conclusions: This systematic review and meta-analysis found no evidence about acupuncture or auricular acupressure in the improvement of sleep disturbances in cancer survivors in terms of short- or long-term effect. Adverse events were minor. The finding was inconsistent with previous research and suggested that more well-designed and large-scale randomized controlled trials are needed to identify the efficacy of acupuncture and auricular acupressure for sleep disturbances in cancer survivors.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/, CRD42020171612.
1 Introduction
Sleep disorder is one of the most prevalent symptoms in patients with cancer (1, 2). It is reported that the prevalence of insomnia in cancer ranges from 30% to 50%, nearly three times higher than that in the general population (3). Although symptoms may slightly improve with time, most of the patients still suffer from insomnia years after cancer treatment (4, 5). Side effects of cancer treatment like depression and pain led to insomnia (6); meanwhile, insomnia would affect cancer treatment effects and result in a decreased quality of life with daytime fatigue, poor cognition, emotion disorder, and other health problems (7, 8). Unfortunately, sleep disturbances in cancer surviovrs are often underrecognized and poorly managed (9).
Pharmacological therapy is the typical options for chronic insomnia, but many cancer survivors refuse to take these drugs taking into account the side effects and drug-to-drug interactions in case of polypharmacy and dependency (10, 11). Instead, cognitive-behavioral therapy (CBT) is the first-line treatment for chronic insomnia yet can be difficult to access, which may require trained therapists to address survivorship-specific barriers to sleep (12). Thus, it is urgent to find a widely used, relatively safe, and well-accepted intervention. Both acupuncture and auricular acupressure (AA), as complementary and alternative treatment, might be promising treatment options, which appear to be effective in improving cancer-related insomnia (13, 14). Acupuncture has been defined as the insertion of fine needles into specific acupuncture points (acupoints) in the human body to relieve certain symptoms, and AA is a non-invasive therapy of treating physical and psychosomatic diseases by stimulating specific points of ears with something (15). Studies on acupuncture and AA for cancer-related insomnia have been growing. There were two systematic reviews discussing the association of acupuncture with cancer-related insomnia. One was published in 2013 and only included three studies (16), and the other one was published in 2016 and included six trials. However, two trials (17, 18) included in the review were conducted by one team, and data were repeated (19). Meanwhile, there were four new trials conducted in the years since 2016 (20–23). Thus, we pooled data from previous RCTs and conducted a systematic review and meta-analysis to investigate the efficacy and safety of acupuncture and AA on sleep in patients with cancer.
2 Methods
This systematic review and meta-analysis was registered in PROSPERO (No. CRD42020171612) and followed a pre-specified analysis plan.
2.1.Eligibility Criteria
Study eligibility was assessed according to five aspects of PICOS.
Participants. Patients who were diagnosed with cancer with or without sleep disturbances were included, but sleep quality was estimated pre- and post-treatment with records of sleep.
Interventions. Interventions included acupuncture and/or AA regardless of specific needling techniques such as manual acupuncture, electroacupuncture, or a combination of acupuncture or AA with other therapies for sleep disturbances.
Comparisons. Sham acupuncture or acupressure, usual care for managing cancer symptoms, drug therapy, or cognitive behavioral therapy were compared. Studies comparing different acupuncture techniques (i.e., warming needle acupuncture vs. manual acupuncture) or different acupoint combinations (i.e., scalp acupuncture vs. body acupuncture) were excluded.
Outcomes. Outcome measures were as follows: first, scales or parameters for sleep evaluation, such as Pittsburgh Sleep Quality Index (PSQI), Insomnia Severity Index (ISI), and other scales including items reflecting the severity of insomnia such as cancer quality of life questionnaire-core 30 (QLQ-C30), M.D. Anderson symptom inventory (MDASI), quality of life (QOL); second, logbook or sleep diary with records of sleep assessment; and third, adverse events. Studies that did not test the efficacy of acupuncture or AA on sleep disorder in cancer patients were excluded.
Studies. Studies that were included were randomized controlled trials.
2.2 Search Strategy
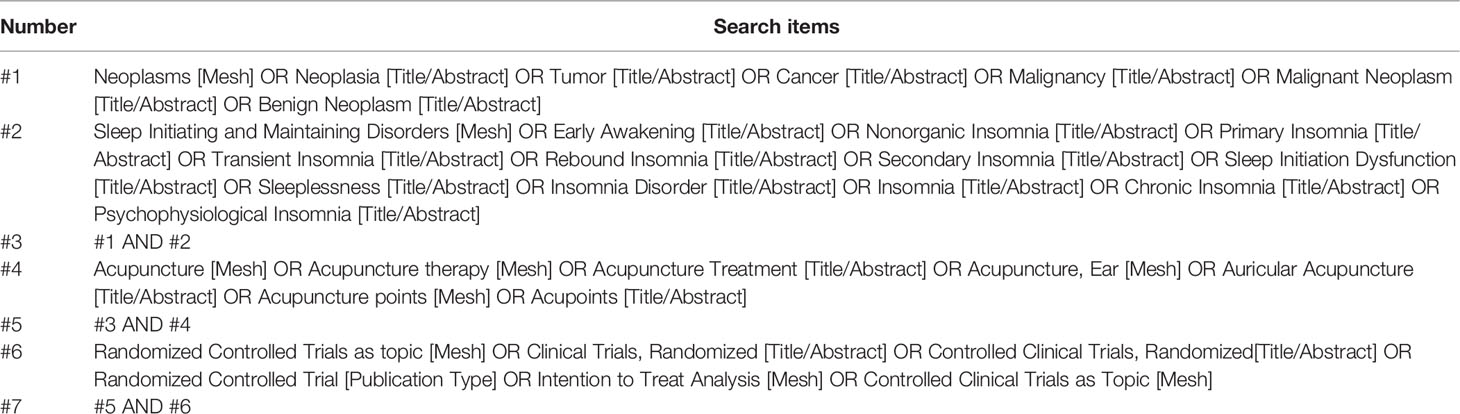
Four English databases (PubMed, Embase, Cochrane Library, and Web of Science) and four Chinese databases (China National Knowledge Infrastructure, Wanfang Database, VIP Database for Chinese Technical Periodicals, and Chinese Biomedical Literature Database) were searched for RCTs published from the database inception to July 30, 2021. The search terms included (acupuncture OR acupuncture therapy OR auricular acupressure) AND (cancer OR tumor OR neoplasms OR carcinoma OR malignancy) AND (sleep initiating and maintaining disorders, insomnia OR sleep disturbance OR sleep disorder OR wakefulness OR waking) AND (randomized controlled trial OR controlled clinical trial) in Chinese and English. The details of the search strategy are shown in Table 1.
2.3 Study Selection
Two of the authors (HX and QF) independently identified articles by scanning titles and abstracts and full text as needed. A third reviewer (QT) would be involved to resolve disagreements between two reviewers by consensus. Articles meeting criteria would be included in the systematic review and, if applicable, included in the meta-analysis.
2.4 Data Extraction
All data extraction was independently performed by two reviewers (HX and QF) using a predetermined protocol according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines (24). These variables included details of trials (year of publication, country, study design, and number of participants), participants (age, sex, cancer type, cancer treatment, and treatment status), intervention (acupoints, frequency, and course), comparisons, and outcomes (sleep measures and adverse event).
For the insomnia scores, the results measured by other scales were converted to the corresponding grade in the 21-point PSQI (higher points indicating more severe insomnia). For example, the result of a 3-score on the 10-score version of the MDASI sleep item was recorded as 6.3 points for data synthesis. The results of the PSQI, the converted QLQ-C30, MDASI, and QOL were used in the meta-analysis. Data in other forms (i.e., mean [95% CI], median, and interquartile range) were converted to means (SDs) according to the Cochrane Handbook for Systematic Reviews of Interventions (25). Corresponding authors would be contacted if data (i.e., SDs) acquisition failed in the original article.
2.5 Quality Assessment
The quality of RCTs included was appraised with the Cochrane Collaboration risk of bias tool (25). Each RCT was assigned a low, high, or unclear risk of bias (ROB) for six specific domains (sequence generation, allocation concealment, blinding of participants and outcome assessment, incomplete outcome data, selective outcome reporting, and other potential threats), with information originating from the published articles.
2.6 Data Synthesis and Analysis
Meta-analysis of RCTs with data was performed by calculating the effect size and 95% CI using the random-effects model. When the number of studies was less than five or studies were substantially heterogeneous, the random-effects model was according to Cochrane Handbook for Systematic Reviews of Interventions (25). Statistical heterogeneity across trials was assessed and quantified by the I2 statistic using forest plots. I2 value >50% was substantially heterogeneous. Statistical analysis was performed with RevMan, version 5.3. Two-sided p < 0.05 was considered statistically significant.
Studies were grouped according to the comparators including sham therapy, drug therapy, behavior therapy, and usual care for managing cancer insomnia. For studies with over one control group, such as real acupuncture vs. sham acupuncture vs. wait-list control, the results were split into corresponding comparison groups.
We conducted subgroup sensitivity analysis to explore potential sources of heterogeneity. Planned subgroup analysis was the type of intervention including manual acupuncture and AA.
3 Results
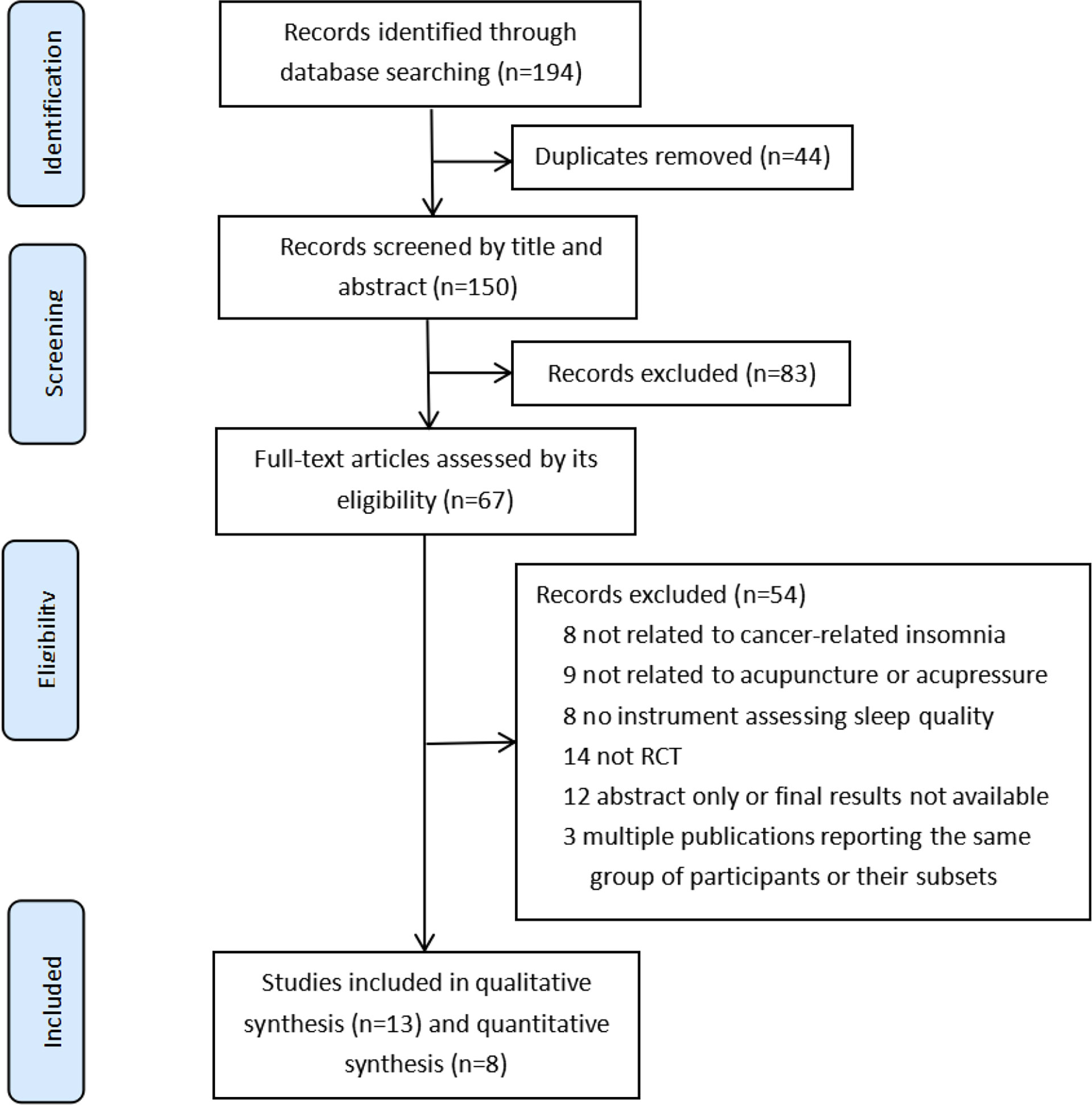
A total of 194 studies were identified by database search. Of those, 44 duplicates and 83 records were filtered and discarded through titles and abstracts; 54 records were excluded for other reasons (Figure 1). At last, 13 RCTs (20–23, 26–34) met our inclusion criteria and were included in this review, only 8 RCTs (20, 27–31, 33, 34) with sufficient data were included in the meta-analysis.
3.1 Study Characteristics
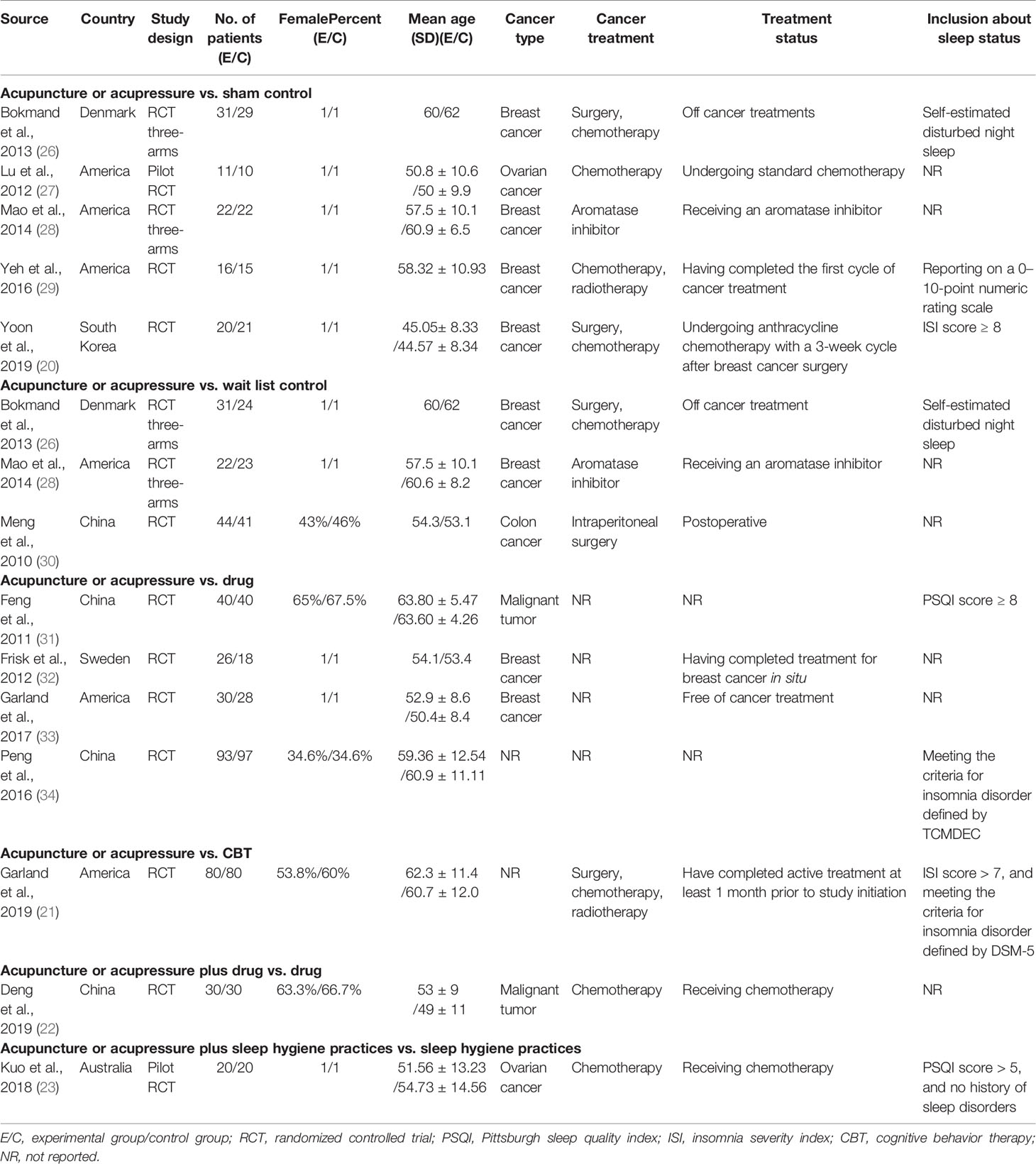
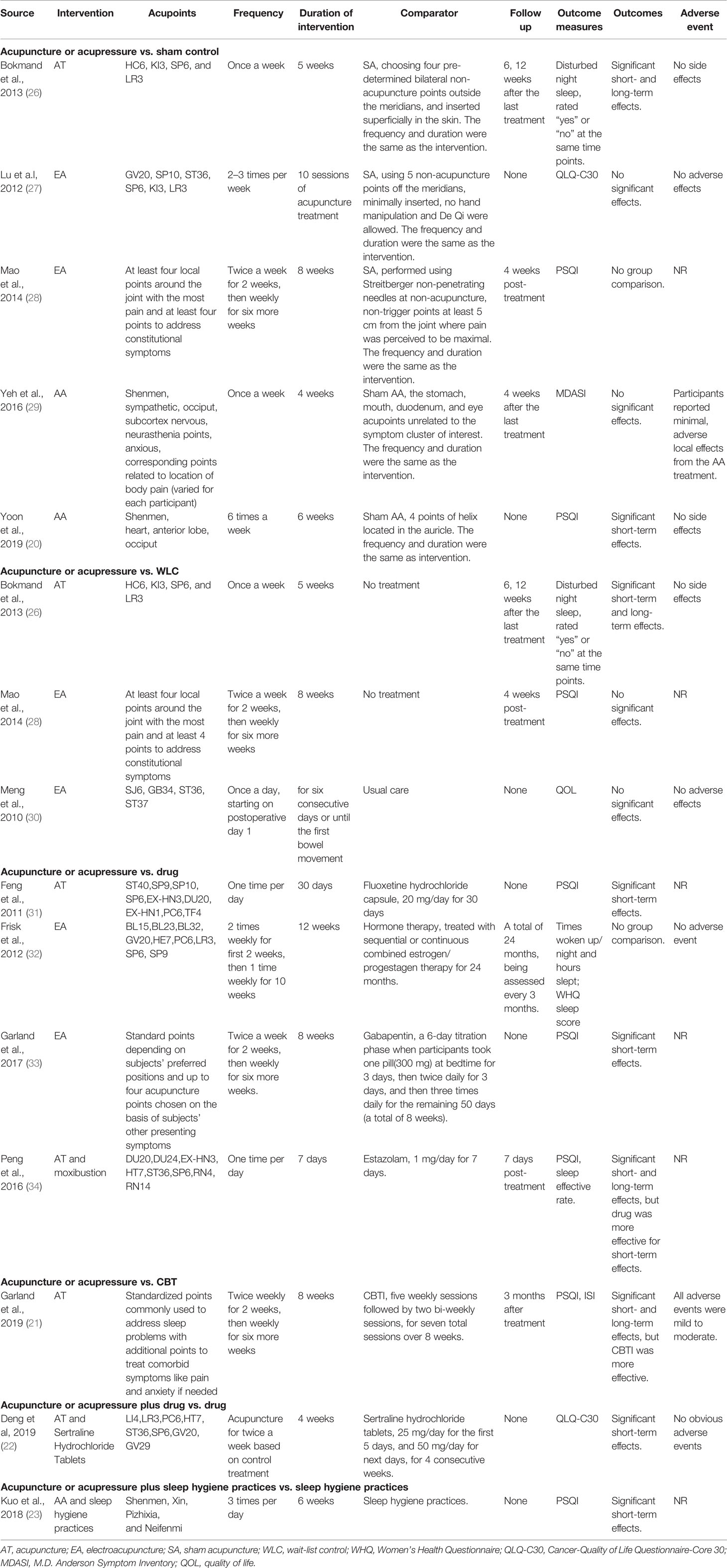
Characteristics of trials, patients, interventions, comparators, and outcomes are shown in Tables 2, 3.
Studies were conducted in six countries: five studies (21, 27–29, 33) in America, four studies (22, 30, 31, 34) in China, and one each in South Korea (20), Denmark (26), Sweden (32), and Australia (23). Among the included studies, only two of them (15%) were three-arms RCTs (26, 28) with two comparators of sham control and wait-list control.
The sample size of patients ranged from 21 to 190, and we included 961 patients with 463 in the experimental group and 498 in the comparator group. The mean age of participants varied from 44 to 63 years old. The types of cancer involved breast cancer (46%) (20, 26, 28, 29, 32, 33), ovarian cancer (15%) (23, 27), malignant tumor (15%) (22, 31), colon cancer (15%) (30), and unspecific cancer (15%) (21, 34). Five of the retrieved studies (52%) included patients undergoing cancer treatments (chemotherapy, radiotherapy, surgery, and cancer-related therapies) at the time of the study (20, 22, 23, 27, 28), while four studies were conducted after treatment (26, 28, 30, 33); three other studies (30%) investigated only patients having completed at least one cycle of cancer treatment (21, 29, 32). Four studies (30%) gave clear scaled inclusion criteria for sleep disturbances with the lowest scores of PSQI or ISI ranging from 5 to 10 (20, 21, 23, 31). There were six trials (46%) that assessed the sleep quality of cancer patients before and after treatment without inclusion criteria for insomnia (22, 27, 28, 30, 32, 33).
Interventions among the included studies were shown as single forms (acupuncture, electro-acupuncture, auricular acupressure) or combinations (acupuncture and sertraline hydrochloride tablets, auricular acupressure, and sleep hygiene practices), only with clear disparities in acupoints, frequency, and duration. All studies were divided into six groups according to the intervention and comparator: five studies in the sham-controlled group (20, 26–29), three studies in the wait-list control group (26, 28, 30), four studies in the comparator group of drug (31–34), and one each in the group of acupuncture compared to CBT (21), acupuncture plus drug compared to the drug (22), and auricular acupressure plus sleep hygiene practices compared to sleep hygiene practices (23).
Outcome measures were the use of logbook, where disturbed night sleep or times woken at night were recorded in one RCT (26, 32), and sleep scales (i.e., PSQI, ISI, and QLQ-C30). PSQI was applied in seven trials (20, 21, 23, 28, 31, 33, 34). QLQ-C30 was used in two RCTs (22, 27); MADSI (29) and QOL (30) were used in one study, respectively.
3.2 Risk of Bias in Individual Studies
The risk of bias in 13 RCTs is shown in Figure 2. Ten trials (20–22, 27, 28, 30–34) had a low ROB regarding random sequence generation, whereas the remaining RCTs (20, 29, 30) did not report the methods. Four RCTs (21, 26, 28, 33) had a low risk of allocation concealment with opaque envelopes. The highest risk of bias in eight studies (21–23, 30–34) was due to the absent masking of participants and personnel. Only two trials (26, 27) demonstrated blinding for outcome assessment. Three RCTs (32–34) had high ROBs with selective reporting of outcomes for incomplete baseline characteristics of cancer survivors and results of trials.
3.3 Analysis of Overall Effects
3.3.1 Short-Term Effect
Four RCTs with a total of 137 patients provided adequate data on the insomnia scale scores and were included in the meta-analysis (20, 27–29). Unsurprisingly, it reported that sham controls was superior to acupuncture and AA groups in the improvement of sleep quality, with mean differences of 1.98 (95% CI = 0.33, 3.64; p = 0.02; I2 = 36%; Figure 3A). Compared to the wait-list control, the pooled results of two RCTs (130 patients) suggested no significant reduction in acupuncture on the score of sleep scales (MD, 0.40; 95% CI=−0.87, 1.68; p = 0.54; I2 = 49%; Figure 3B). Meta-analysis of three studies (328 patients) showed equivalent effects of acupuncture therapy as drug therapy on the score of sleep scales with substantial heterogeneity (MD, 1.18; 95% CI=−3.09, 5.46; p = 0.59; I2 = 98%; Figure 3C).
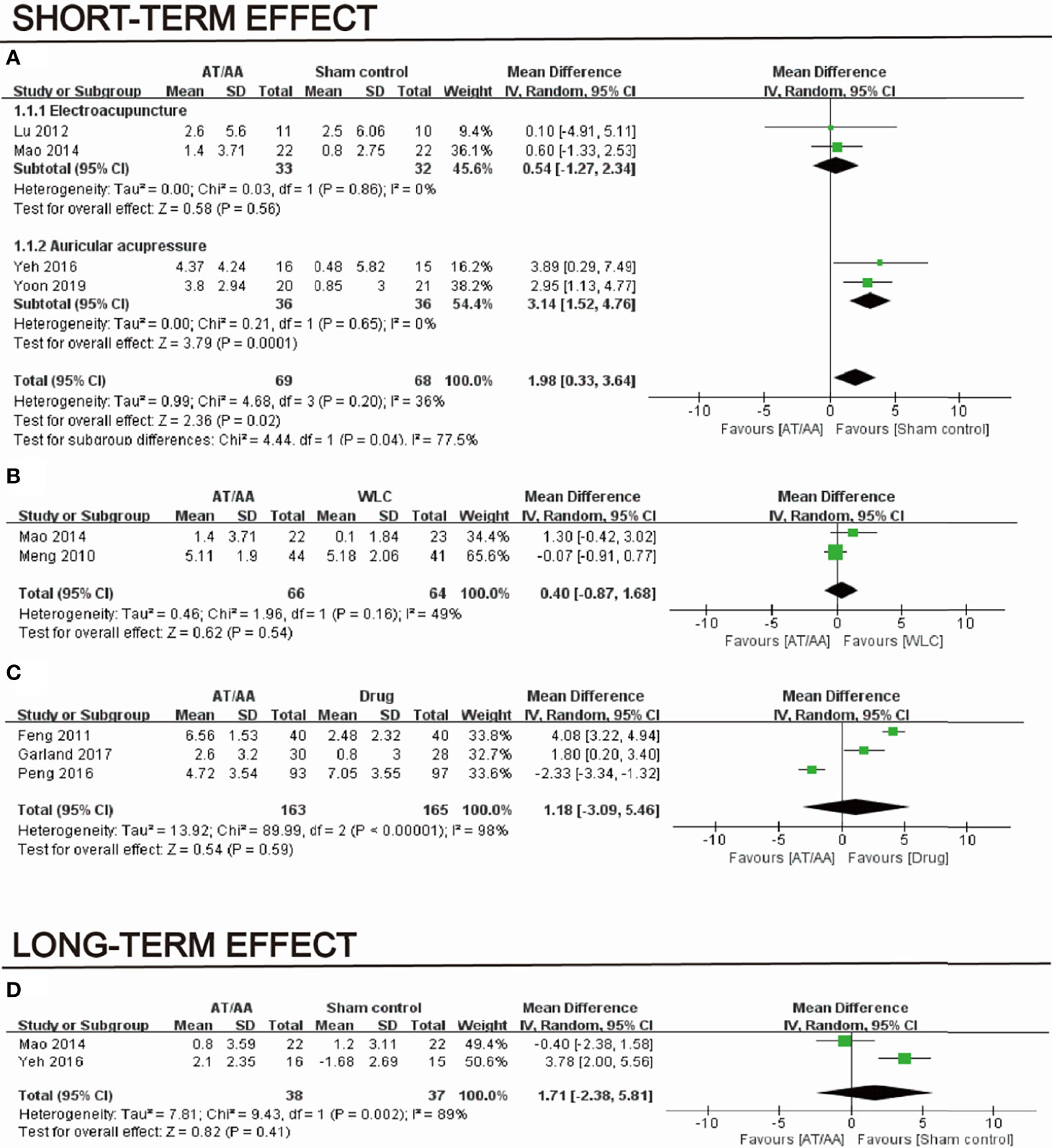
Figure 3 Short-term effect of acupuncture and auricular acupressure groups vs. (A) sham, (B) wait-list, and (C) drug and (D) long-term effect of acupuncture and auricular acupressure groups vs drug.
3.3.2 Long-Term Effect
Two sham-controlled RCTs showed no significance of acupuncture or AA on insomnia scale scores (MD, 1.71; 95% CI=−2.38, 5.81; p = 0.41; I2 = 89%; Figure 3D).
3.3.3.Subgroup Analyses
When compared to sham control, subgroup analyses suggested no evidence that AA (MD, 3.14; 95% CI=1.52, 4.76; p = 0.0001; I2 = 0%) and acupuncture (MD, 0.54; 95% CI=-1.27, 2.34; p = 0.56; I2 = 0%) were associated with the reduction in insomnia scale scores. The heterogeneity degraded from 36% to 0%.
3.3.4 Sensitivity Analysis
Sensitivity analysis was realized by subgroup analysis; drug-controlled RCTs demonstrated no significance for short-term effect but showed long-term effect on sleep scales in studies with unclear or low risk of selection bias (MD, 3.04; 95% CI=0.82, 5.27; p = 0.007; I2 = 84%; Figures 4A, B).
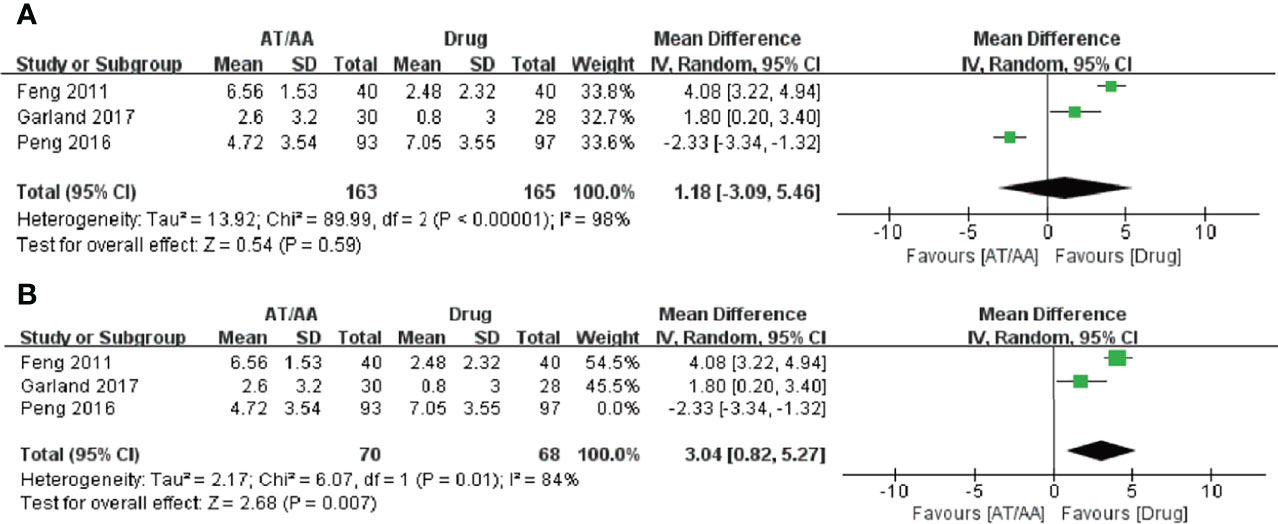
Figure 4 Forest plots of the (A) short-term effect and (B) long-term effect of acupuncture or auricular acupressure for cancer-related insomnia.
3.3.5 Publication Bias
Funnel plots were not analyzed due to the small number of eligible studies.
3.3.6 Safety of Acupuncture and Acupressure
Minor adverse events were reported in one study (21, 29) (Table 3), in which patients complained about minimal, adverse effects from the AA. All adverse events were mild to moderate. Seven RCTs reported no adverse effects (20, 22, 23, 26, 27, 30, 32), while adverse events were not mentioned in other studies (28, 31, 33, 34).
4 Discussion
This is the first review and meta-analysis to investigate the efficacy and safety of acupuncture and AA in sleep disturbances of cancer survivors. The results of the meta-analysis indicated that cancer survivors treated with acupuncture and AA might not experience a positive effect on sleep quality when compared to sham control, wait-list control, or drug therapy, which is inconsistent with the previous studies (16, 19). The difference might be owing to the following aspects: first, recent high-quality studies enrolled and strict inclusion criteria applied. Data of two trials (17, 18) included in the research (19) were from the same team, and they were replaced by a recent study (34) of their team in this research. Second is the generally high ROBs for methodological limitations of acupuncture and AA trials. Lastly is the high heterogeneity of using various acupoints, frequency, and duration.
Although 13 studies had a total sample of 961 participants and were conducted in six countries, which included United States, China, South Korea, Denmark, Sweden, and Australia, acupuncture and AA with few adverse effects were poor persuasion for cancer survivors (35). There was a study suggesting that lack of related knowledge was a major barrier in the use of acupuncture on common cancer symptoms (36); cancer survivors generally were confused about what symptoms or medical conditions that acupuncture could be used to treat, how acupuncture works, and how long the effects of acupuncture lasts (37). To address misconceptions above, we need to provide appropriate and timely education and communication in the treatment of insomnia for cancer survivors (37, 38). Certainly, robust evidence is the key factor based on evidence-informed patients, as participants preferred the treatment perceived as having stronger evidence (35). Thus, more high-quality clinical studies and detailed guideline of cancer survivors management should be promoted.
We found that the combination of acupuncture or AA with drug or sleep hygiene practices could significantly improve sleep quality of cancer surviors, and it was reported that participants responded to acupuncture effectively with responsible sleep hygiene practices and persistence of a durable therapy (39). Besides, there were studies showing that the combination of drug with sleep hygiene practices helped alleviate the patients’ depression (22, 23). Therefore, acupuncture or AA should be combined with sleep hygiene practices for the sleep management of cancer survivors, which might be more effective. Furthermore, the persistence of acupuncture contributes to a long-term effect (39, 40).
The negative results from sham-controlled RCTs suggested the potential efficacy of true and sham acupuncture or acupressure in improving sleep quality in cancer patients. The points of sham acupuncture employed in a number of included trials were not associated with improving sleep, so it was not physiologically inserted. In some sham control, needles were even retractable, but they could still elicit effects in participants. In reality, psychological effect was inevitable in the course of sham acupuncture for insomnia in cancer patients, while psychology was strongly linked with insomnia disorder (41). This might be another contributing factor in the review findings showing no significance between the two groups on improvement of sleep disturbance in cancer patients.
Subgroup analyses suggested the potential efficacy of AA in improving sleep quality for cancer survivors. The possible mechanism reported was that auricular reflective points were connected to the internal organs of the body (20, 42). Meanwhile, auricular therapy has been widely used to relieve symptoms like pain with few side effects (20, 43). However, we need more RCTs to illustrate the efficacy of AA on insomnia due to a paucity of related literature so far.
The drug-controlled RCTs had high heterogeneity in the study. The result of the sensitivity analysis suggested that acupuncture had superior short-term effects in studies with unclear or low risk of selection bias, and the statistical heterogeneity just fell from 99% to 84%. The fluoxetine- and gabapentin-controlled trials showed that they could improve insomnia by alleviating other symptoms causing insomnia in cancer survivors (31, 33), and it is well-known that fluoxetine and gabapentin were used for cancer-related depression and pain, respectively (44, 45). Besides, differences among drug comparators (i.e., manufacturers, dose, frequency, and course) were also factors leading to heterogeneity. Thus, studies on the specific drug-controlled group would be necessary to provide robust evidence of the acupuncture effects.
There were some other surprising findings in the study. A majority of the trials included were conducted in women, which might be closely related with characteristics of cancer survivors who are suffering from sleep disturbances (46, 47); for example, the prevelance of insomnia was lower in men with prostate cancer (25%–39%) but higher in women with breast (42%–69%) and gynecological (33%–68%) cancer (46). In addition, there was a study confirming that breast cancer survivors had higher prevelance of insomnia during chemotherapy (47). To the best of our knowledge, cancer treatments are also one of the predisposing causes of insomnia (48). Subgroup analysis about patients’ features was not conducted due to a limitation of included trials in each group. Further research could focus on the relationship of the treatments with specific cancer patients’ insomnia.
This review and meta-analysis is not without limitations. First, given the limited number of CBT-controlled RCTs in each group, it was not possible to compare the efficacy of acupuncture and AA when compared to comparators like CBT. Second, the study used subjective scales (e.g., PSQI) instead of polysomnogram as outcome measure due to few relevant literature, which reduced the credibility of this conclusion. Lastly, funnel plots evaluating publication bias was not feasible owing to the small number of included studies. In short, future RCTs are needed to provide robust evidence of the association of acupuncture or AA with the improvement of sleep disturbances of cancer survivors.
5 Conclusions
The findings of this systematic review and meta-analysis suggest that acupuncture or AA is irrelevant to the improvement of sleep disturbances in cancer survivors for short- or long-term effects. Adverse events were minor. To further understand the potential role of acupuncture and AA on cancer-related insomnia, well-designed and large-scale randomized controlled trials are needed.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author Contributions
QW and SL handled conception, design of the review, data analysis, and drafting of the manuscript. XW, QT, HX, and SZ carried out data extraction and assessment of risk of bias. QF and HC were responsible for administrative support and supervision. RP and WW performed critical revision of the manuscript for important intellectual content and participated in conception and design. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors thank all the authors of the original studies included in this meta-analysis. The research, authorship, and publication of this article were funded by Nanjing University of Chinese Medicine (grant number 2019YSHL091) and Key Research & Development Social Development Program of Jiangsu Province (grant number BE2021751).
Abbreviations
RCTs, randomized controlled trials; AT, acupuncture; EA, electroacupuncture; SA, sham acupuncture; AA, auricular acupressure; WLC, wait-list control; CBT, cognitive behavior therapy; PSQI, Pittsburgh Sleep Quality Index; WHQ, Women’s Health Questionnaire; QLQ-C30, cancer-quality of life questionnaire-core 30; MDASI, M.D. Anderson symptom inventory; QOL, quality of life. E/C, Experimental group/control group; ISI, insomnia severity index; NR,not reported; RevMan, Review Manager Software; CI, confidence interval; MD, mean difference.
References
1. Santoso AMM, Jansen F, de Vries R, Leemans CR, van Straten A, Verdonck-de Leeuw IM. Prevalence of Sleep Disturbances Among Head and Neck Cancer Patients: A Systematic Review and Meta-Analysis. Sleep Med Rev (2019) 47:62–73. doi: 10.1016/j.smrv.2019.06.003
2. Voiss P, Höxtermann MD, Dobos G, Cramer H. Cancer, Sleep Problems, and Mind-Body Medicine Use: Results of the 2017 National Health Interview Survey. Cancer (2019) 125(24):4490–7. doi: 10.1002/cncr.32469
3. Savard J, Ivers H, Villa J, Caplette-Gingras A, Morin CM. Natural Course of Insomnia Comorbid With Cancer: An 18-Month Longitudinal Study. J Clin Oncol (2011) 29(26):3580–6. doi: 10.1200/JCO.2010.33.2247
4. Lowery-Allison AE, Passik SD, Cribbet MR, Reinsel RA, O'Sullivan B, Norton L, et al. Sleep Problems in Breast Cancer Survivors 1-10 Years Posttreatment. Palliat Support Care (2018) 16(3):325–34. doi: 10.1017/S1478951517000311
5. Pachman DR, Barton DL, Swetz KM, Loprinzi CL. Troublesome Symptoms in Cancer Survivors: Fatigue, Insomnia, Neuropathy, and Pain. J Clin Oncol (2012) 30(30):3687–96. doi: 10.1200/JCO.2012.41.7238
6. Devlin EJ, Denson LA, Whitford HS. Cancer Treatment Side Effects: A Meta-Analysis of the Relationship Between Response Expectancies and Experience. J Pain Symptom Manage (2017) 54(2):245–58.e2. doi: 10.1016/j.jpainsymman.2017.03.017
7. Ruel S, Ivers H, Savard MH, Gouin JP, Lemieux J, Provencher L, et al. Insomnia, Immunity, and Infections in Cancer Patients: Results From a Longitudinal Study. Health Psychol (2020) 39(5):358–69. doi: 10.1037/hea0000811
8. Loh KP, Zittel J, Kadambi S, Pandya C, Xu H, Flannery M, et al. Elucidating the Associations Between Sleep Disturbance and Depression, Fatigue, and Pain in Older Adults With Cancer. J Geriatr Oncol (2018) 9(5):464–8. doi: 10.1016/j.jgo.2018.02.006
9. Howell D, Oliver TK, Keller-Olaman S, Davidson JR, Garland S, Samuels C, et al. Sleep Disturbance in Adults With Cancer: A Systematic Review of Evidence for Best Practices in Assessment and Management for Clinical Practice. Ann Oncol (2014) 25(4):791–800. doi: 10.1093/annonc/mdt506
10. Krystal AD, Ashbrook LH, Prather AA. What Is Insomnia? JAMA (2021) 326(23):2444. doi: 10.1001/jama.2021.19283
11. Matthews E, Carter P, Page M, Dean G, Berger A. Sleep-Wake Disturbance: A Systematic Review of Evidence-Based Interventions for Management in Patients With Cancer. Clin J Oncol Nursing (2018) 22(1):37–52. doi: 10.1188/18.CJON.37-52
12. Koffel E, Bramoweth AD, Ulmer CS. Increasing Access to and Utilization of Cognitive Behavioral Therapy for Insomnia (CBT-I): A Narrative Review. J Gen Internal Med (2018) 33(6):955–62. doi: 10.1007/s11606-018-4390-1
13. Zhang Y, Sun Y, Li D, Liu X, Fang C, Yang C. Acupuncture for Breast Cancer: A Systematic Review and Meta-Analysis of Patient-Reported Outcomes. Front Oncol (2021) 1(10):646315. doi: 10.3389/fonc.2021.646315
14. Hxtermann MD, Buner K, Haller H, Kohl W, Dobos G, Reinisch M, et al. Efficacy and Safety of Auricular Acupuncture for the Treatment of Insomnia in Breast Cancer Survivors: A Randomized Controlled Trial. Cancers (2021) 13(16):4082. doi: 10.3390/cancers13164082
15. Gao H, Zhang L, Liu J. Auricular Acupressure for Myopia in Children and Adolescents: A Systematic Review. Complement Ther Clin Pract (2020) 2(38):101067. doi: 10.1016/j.ctcp.2019.101067
16. Garcia MK, Mcquade J, Haddad R, Patel S, Lee R, Yang P, et al. Systematic Review of Acupuncture in Cancer Care: A Synthesis of the Evidence. J Clin Oncol (2013) 31(7):952–60. doi: 10.1200/JCO.2012.43.5818
17. Song JR, Zhao YL, Peng XH, Hu YP. Clinical Randomized Controlled Study of Using Acupuncture to Treat Tumor Patients With Insomnia. J Sichuan Tradit Chin Med (2015) 33(4):163–64. doi: CNKI:SUN:SCZY.0.2015-04-080
18. Dan ZJ. A Randomized Controlled Clinical Study of Acupuncture Intervention for Cancer Patients With Insomnia [Master’s Thesis]. Chengdu, China: Chengdu University of Traditional Chinese Medicine (2013).
19. Choi TY, Kim JI, Lim HJ, Lee MS. Acupuncture for Managing Cancer-Related Insomnia: A Systematic Review of Randomized Clinical Trials. Integr Cancer Therapies (2016) 16(2):135–46. doi: 10.1177/1534735416664172
20. Yoon HG, Park H. The Effect of Auricular Acupressure on Sleep in Breast Cancer Patients Undergoing Chemotherapy: A Single-Blind, Randomized Controlled Trial. Appl Nurs Res (2019) 48:45–51. doi: 10.1016/j.apnr.2019.05.009
21. Garland SN, Xie SX, DuHamel K, Bao T, Li Q, Barg FK, et al. Acupuncture Versus Cognitive Behavioral Therapy for Insomnia in Cancer Survivors: A Randomized Clinical Trial. J Natl Cancer Inst (2019) 111(12):1323–31. doi: 10.1093/jnci/djz050
22. Deng XY, Xu TS. Clinical Observation of Acupuncture Combined With Sertraline Hydrochloride Tablets on Tumor-Related Depression. Zhongguo Zhen Jiu (2019) 39(4):379–83. doi: 10.13703/j.0255-2930.2019.04.009
23. Kuo HC, Tsao Y, Tu HY, Dai ZH, Creedy DK. Pilot Randomized Controlled Trial of Auricular Point Acupressure for Sleep Disturbances in Women With Ovarian Cancer. Res Nurs Health (2018) 41(5):469–79. doi: 10.1002/nur.21885
24. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann Intern Med (2009) 151(4):264–69. doi: 10.7326/0003-4819-151-4-200908180-00135
25. Higgins JPT, Altman DG. Assessing Risk of Bias in Included Studies. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions, vol. chap 8 . Chichester, UK: John Wiley & Sons (2008).
26. Bokmand S, Flyger H. Acupuncture Relieves Menopausal Discomfort in Breast Cancer Patients: A Prospective, Double Blinded, Randomized Study. Breast (2013) 22(3):320–3. doi: 10.1016/j.breast.2012.07.015
27. Lu W, Matulonis UA, Dunn JE, Lee H, Doherty-Gilman A, Dean-Clower E, et al. The Feasibility and Effects of Acupuncture on Quality of Life Scores During Chemotherapy in Ovarian Cancer: Results From a Pilot, Randomized Sham-Controlled Trial. Med Acupuncture (2012) 24(4):233–40. doi: 10.1089/acu.2012.0904
28. Mao JJ, Farrar JT, Bruner D, Zee J, Bowman M, Seluzicki C, et al. Electroacupuncture for Fatigue, Sleep, and Psychological Distress in Breast Cancer Patients With Aromatase Inhibitor-Related Arthralgia: A Randomized Trial. Cancer (2014) 120(23):3744–51. doi: 10.1002/cncr.28917
29. Yeh CH, Chien LC, Lin WC, Bovbjerg DH, van Londen GJ, et al. Pilot Randomized Controlled Trial of Auricular Point Acupressure to Manage Symptom Clusters of Pain, Fatigue, and Disturbed Sleep in Breast Cancer Patients. Cancer Nursing (2016) 39(5):402–10. doi: 10.1097/NCC.0000000000000303
30. Meng ZQ, Garcia MK, Chiang JS, Peng HT, Shi YQ, Fu J, et al. Electro-Acupuncture to Prevent Prolonged Postoperative Ileus: A Randomized Clinical Trial. World J Gastroenterol (2010) 16(1):104–11. doi: 10.3748/wjg.v16.i1.104
31. Feng Y, Wang XY, Shao-Dan LI, Zhang Y, Wang HM, Li M, et al. Clinical Research of Acupuncture on Malignant Tumor Patients for Improving Depression and Sleep Quality. J Traditional Chin Med (2011) 31(3):199–202. doi: 10.1016/S0254-6272(11)60042-3
32. Frisk J, Källström A, Wall N, Fredrikson M, Hammar M. Acupuncture Improves Health-Related Quality-of-Life (HRQoL) and Sleep in Women With Breast Cancer and Hot Flushes. Supportive Care Cancer (2012) 20(4):715–24. doi: 10.1007/s00520-011-1134-8
33. Garland SN, Xie SX, Li Q, Seluzicki C, Basal C, Mao JJ. Comparative Effectiveness of Electro-Acupuncture Versus Gabapentin for Sleep Disturbances in Breast Cancer Survivors With Hot Flashes. Menopause (2017) 24(5):517–23. doi: 10.1097/GME.0000000000000779
34. Peng XH, Zhang JL, Song JR, Liu DY, Zhao YL, Chan ZJ, et al. Clinical Observation of Acupuncture Treatment of Insomnia in Tumor Patients. Chin J Traditional Chin Med (2016) 31(6):2409–11. doi: CNKI:SUN:BXYY.0.2016-06-106
35. Garland SN, Eriksen W, Song S, Dearing J, Barg FK, Gehrman P, et al. Factors That Shape Preference for Acupuncture or Cognitive Behavioral Therapy for the Treatment of Insomnia in Cancer Patients. Support Care Cancer (2018) 26(7):2407–15. doi: 10.1007/s00520-018-4086-4
36. Eriksen WT, Singerman L, Romero SAD, Bussell J, Barg FK, Mao JJ. Understanding the Use of Acupuncture for Insomnia Among Cancer Survivors: A Qualitative Study. J Altern Complement Med (2018) 24(9-10):962–7. doi: 10.1089/acm.2018.0156
37. Bao T, Li Q, DeRito JL, Seluzicki C, Im EO, Mao J. Barriers to Acupuncture Use Among Breast Cancer Survivors: A Cross-Sectional Analysis. Integr Cancer Ther (2018) 17(3):854–9. doi: 10.1177/1534735418754309
38. Frenkel M, Ben-Arye E, Cohen L. Communication in Cancer Care: Discussing Complementary and Alternative Medicine. Integr Cancer Ther (2010) 9(2):177–85. doi: 10.1177/1534735410363706
39. Romero SAD, Jiang E, Bussell J, Eriksen W, Duhamel KN, Barg FK, et al. What Makes One Respond to Acupuncture for Insomnia? Perspectives of Cancer Survivors. Palliat Support Care (2020) 18(3):301–6. doi: 10.1017/S1478951519000762
40. MacPherson H, Vertosick EA, Foster NE, Lewith G, Linde K, Sherman KJ, et al. The Persistence of the Effects of Acupuncture After a Course of Treatment: A Meta-Analysis of Patients With Chronic Pain. Pain (2017) 158(5):784–93. doi: 10.1097/j.pain.0000000000000747
41. Liu C, Xi H, Wu W, Wang X, Qin S, Zhao Y, et al. Placebo Effect of Acupuncture on Insomnia: A Systematic Review and Meta-Analysis. Ann Palliat Med (2020) 9(1):19–29. doi: 10.21037/apm.2019.11.15
42. Oleson T. Auriculotherapy Manual. In: Chinese and Western Systems of Ear Acupuncture(4th Ed.). Los Angeles: Elsevier Health Sciences (2013).
43. Moura CC, Chaves ECL, Chianca TCM, Ruginsk SG, Nogueira DA, Souza VHS, et al. Contribution of Chinese and French Ear Acupuncture for the Management of Chronic Back Pain: A Randomised Controlled Trial. J Clin Nurs (2019) 28(21-22):3796–806. doi: 10.1111/jocn.14983
44. Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y, et al. Comparative Efficacy and Acceptability of 21 Antidepressant Drugs for the Acute Treatment of Adults With Major Depressive Disorder: A Systematic Review and Network Meta-Analysis. Lancet (2018) 391(10128):1357–66. doi: 10.1016/S0140-6736(17)32802-7
45. Verret M, Lauzier F, Zarychanski R, Perron C, Savard X, Pinard AM, et al. Perioperative Use of Gabapentinoids for the Management of Postoperative Acute Pain: A Systematic Review and Meta-Analysis. Anesthesiology (2020) 133(2):265–79. doi: 10.1097/ALN.0000000000003428
46. Savard J, Ivers H, Villa J, Caplette-Gingras A, Morin CM. Natural Course of Insomnia Comorbid With Cancer: An 18-Month Longitudinal Study. J Clin Oncol (2011) 29(26):3580–6. doi: 10.1200/JCO.2010.33.2247
47. Bower JE, Ganz PA, Irwin MR, Kwan L, Breen EC, Cole SW, et al. Inflammation and Behavioral Symptoms After Breast Cancer Treatment: Do Fatigue, Depression, and Sleep Disturbances Share a Common Underlying Mechanism? J Clin Oncol (2011) 29(26):3517–22. doi: 10.1200/JCO.2011.36.1154
Keywords: sleep disturbances in cancer survivors, acupuncture, auricular acupressure, systematic review, meta-analysis
Citation: Wan Q, Luo S, Wang X, Tian Q, Xi H, Zheng S, Fang Q, Chen H, Wu W and Pan R (2022) Association of Acupuncture and Auricular Acupressure With the Improvement of Sleep Disturbances in Cancer Survivors: A Systematic Review and Meta-Analysis. Front. Oncol. 12:856093. doi: 10.3389/fonc.2022.856093
Received: 16 January 2022; Accepted: 30 March 2022;
Published: 18 May 2022.
Edited by:
Hannah Arem, George Washington University, United StatesReviewed by:
Elizabeth Ann Salerno, Washington University in St. Louis, United StatesEleonora Anna Mess, Wroclaw Medical University, Poland
John Hughes, Royal London Hospital for Integrated Medicine, United Kingdom
Copyright © 2022 Wan, Luo, Wang, Tian, Xi, Zheng, Fang, Chen, Wu and Pan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenzhong Wu, bWFlcnRhX3pob25nYWN1QDE2My5jb20=
†These authors share first authorship
 Qingyun Wan1†
Qingyun Wan1† Shuting Luo
Shuting Luo