- Department of Anesthesiology, Peking Union Medical College Hospital, Beijing, China
Background: Perioperative complications are higher in patients with pheochromocytoma and/or paraganglioma. The aim of this study was to identify the risk factors of postoperative complications after pheochromocytoma and/or paraganglioma resection surgery.
Method: We retrospectively reviewed 438 patients who underwent laparoscopic or open surgery for pheochromocytoma and/or paraganglioma at our center between January 2014 and December 2019. Demographic characteristics and intraoperative and postoperative data were recorded. Complications were defined as deviations from the normal postoperative course and Clavien–Dindo classification was used to grade the severity of postoperative complication. Patients with complications of grade II or above were included for analysis. Binary logistic regression was used to determine the risk factors for postoperative complications.
Results: The median age of the patients was 47 years old. There were 295 cases (67.4%) of phepchromocytoma and 143 cases (32.6%) of paraganglioma. Three hundred sixty-seven (87.8%) patients had laparoscopic approach, and 55 (12.6%) patients had laparotomy; the conversion rate from laparoscopy to laparotomy was 3.7%. Eighty-seven complications occurred in 65 patients (14.8%). No death occurred in our study and transfusion (36, 8.2%) was the most common complication. The mean follow-up length was 14 months. Independent risk factors for postoperative complications included a tumor size larger than 5.6 cm (OR = 2.427, 95% CI 1.284–4.587, P = 0.006), laparotomy (OR 2.590, 95% CI 1.230–5.453, P = 0.012), conversion to laparotomy (OR = 8.384, 95% CI 2.247–31.285, P = 0.002), and the operation time longer than 188 min (OR = 3.709, 95% CI 1.847–7.450, P < 0.001).
Conclusion: Complications were not uncommon after pheochromocytoma and/or paraganglioma surgery. Tumor size, surgical type, and operation time were determined as the risk factors for postoperative complications. These factors should be considered to improve perioperative management.
Introduction
Pheochromocytoma and/or paraganglioma are rare neuroendocrine tumors. Due to the excessive secretion of catecholamines, the main clinical symptoms include hypertension, palpitation, tachycardia, headache, and palpitations. Comprehensive preoperative evaluation and adequate anti-hypertensive treatment to restore blood volume are essential to decrease intraoperative hemodynamic instability and perioperative mortality and morbidity.
Surgical resection is still the primary strategy for the treatment of pheochromocytoma and/or paraganglioma. The surgical mortality rate had been reported as high as 50% in the past, and this rate had significantly decreased since the improvement in perioperative management and surgical techniques (1). However, pheochromocytoma and/or paraganglioma are still potential challenges to anesthesiologists.
Previous reports had focused on the incidence and risk factors of intraoperative hemodynamic instability and cardiovascular related complications (2–4). The incidence of postoperative complications after pheochromocytoma surgery ranged from 11.4 to 29.8%, and comorbidities, tumor size, catecholamine level, and surgical approach had been reported to be associated with higher risk of postoperative complications (3–5). However, few studies had evaluated the severity of postoperative complications, and the results were inconsistent. Identifying risk factors for complications may lead to improved perioperative management.
The aim of this study was to explore the relationship between patients’, tumor’s, and surgical factors and postoperative complications in patients with pheochromocytoma and/or paraganglioma.
Materials and methods
After the approval of the Institutional Review Board, a retrospective, observational, and single-center study was conducted at Peking Union Medical College Hospital. All medical records (which included patients progress note and nurse log) of patients who had pheochromocytoma and/or paraganglioma resection at Peking Union Medical College Hospital from January 2014 to December 2019 were reviewed.
The exclusion criteria included incidental pheochromocytoma or paraganglioma without anti-hypertension medication preoperatively, pregnancy, incomplete perioperative data, patients with bilateral pheochromocytoma, paraganglioma outside abdominal (e.g., carotid body tumor, Glomus Jugular tumor, paraganglioma in the bladder, and cardiac paraganglioma), and those who had previous history of abdominal operations.
Preoperative management included selective or non-selective alpha blocker for at least 2 weeks and beta blocker for tachycardia if necessary. Perioperative target blood pressure was defined as blood pressure less than 130/80 mmHg while seated and systolic blood pressure no less than 90 mmHg while standing. All patients had operations under general anesthesia with the insertion of arterial line before induction. All operations and anesthesia were performed by qualified surgeons and anesthesiologists. Bolus infusion of phentolamine or continuous infusion of nitroprusside were administered to maintain systolic blood pressure less than 160 mmHg or no more than 30% above baseline. Continuous infusion of norepinephrine or epinephrine was administrated when systolic blood pressure less than 90 mmHg or 30% below baseline. Patients were all transferred to intensive care unit (ICU) postoperatively for further hemodynamic monitoring. Genetic analysis was performed in the majority of patients, but the results were not available for this study.
The following data were collected, which included age, sex, body mass index (BMI), comorbidities, tumor size, the level of urine catecholamine, duration of operation, intraoperative hemodynamic instability, perioperative blood product infusion, length of stay in ICU and hospital, and postoperative complications.
Deviations from the normal postoperative course recorded in medical records during hospitalization was considered as postoperative complications (6). The Clavien–Dindo classification was used to grade the severity of postoperative complication (6). Furthermore, patients who had complications with grade II or above were included in our analysis (4, 7). For patients with multiple complications, the grade was based on the most severe complication. Hemodynamic instability was defined as previously reported (8, 9). Postoperative hypotension episode was defined as SBP < 90 mmHg and/or DBP < 60 mmHg with typical clinical symptom of hypotension despite continuous infusion of norepinephrine or epinephrine.
SPSS 22.0 was used for statistical analysis. Continuous variables were presented as means ± standard deviations or medians and interquartile ranges. Category variables were presented as numbers and percentages. Student t-test or Mann–Whitney U-test was used to compare variables between two groups. Receiver Operating Characteristic Curve (ROC) was used to define cutoff point of age, tumor size, and length of operation. In addition, variables with a P < 0.1 were entered in binary logistic regression analysis. P < 0.05 was considered statistic significant.
Results
Four hundred thirty-eight patients were included for our analysis. The median age of the patients was 47 years old [IQR 36,55], and the mean BMI was 23.9 ± 3.2. 237 patients were male (54.1%) and 201 patients were female (45.9%). Three hundred forty-five (78.8%) were ASA II, 66 (15.1%) were ASA III, and 27 (6.2%) were ASA IV at the time of the operation (see Table 1). There were 295 (67.1%) cases of pheochromocytoma and 143 (32.9%) cases of paraganglioma.
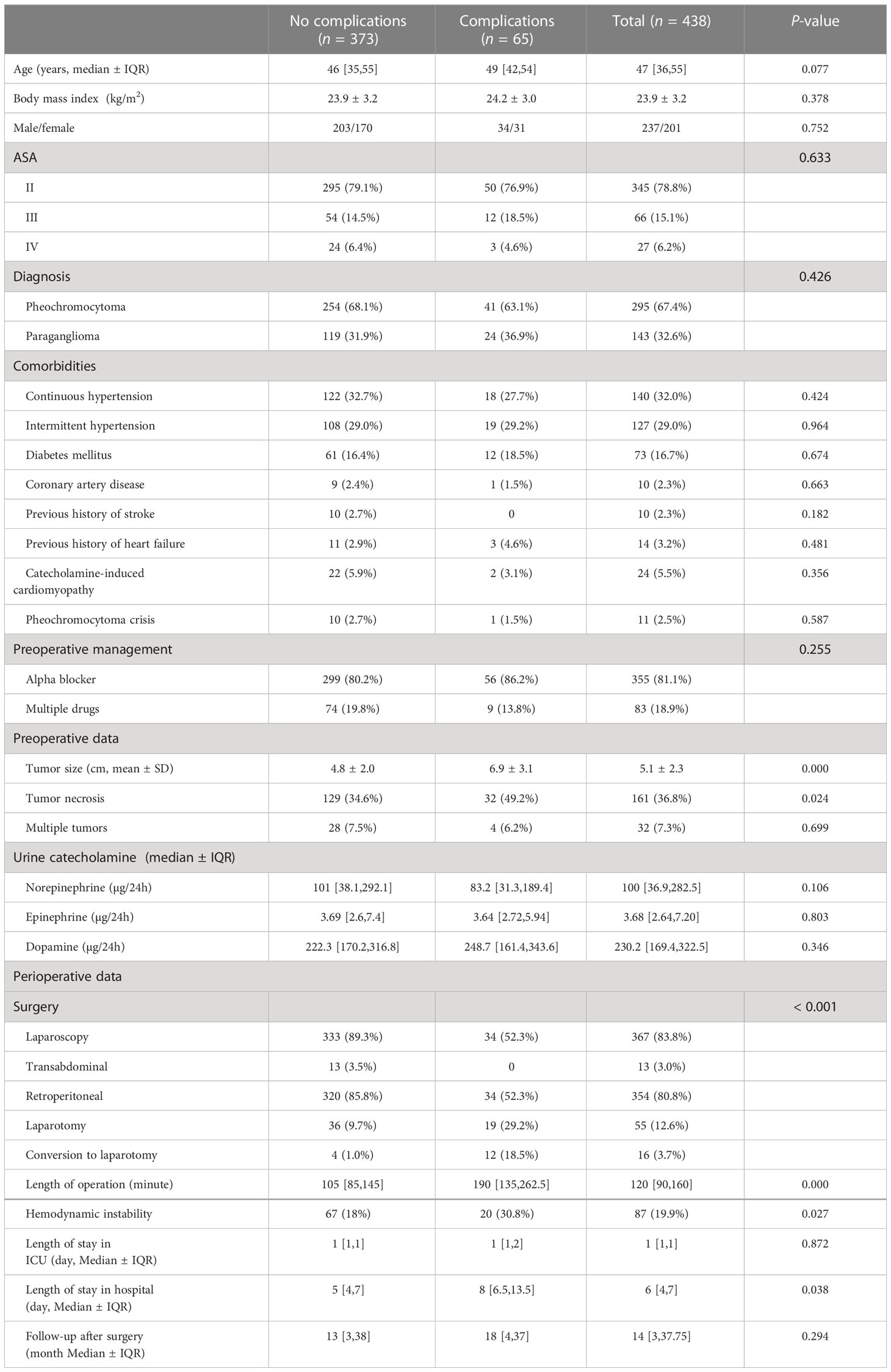
Table 1 Demographic characteristics and perioperative data of patients after resection of pheochromocytoma and/or paraganglioma.
The prevalence of continuous hypertension and intermittent hypertension was 140 (32.0%) and 127 (29.0%), respectively. Twenty-four (5.5%) patients were diagnosed as catecholamine cardiomyopathy, and 11 patients (2.5%) experienced pheochromocytoma crisis before the operations. Alpha blocker was the primary antihypertension drug preoperatively. Eighty-three patients (18.9%) had multiple drugs for preoperative preparation.
The mean diameter of the tumor was 5.1 ± 2.3 cm, and 161 patients (36.8%) had tumor necrosis presented in CT. Three hundred sixty-seven (87.8%) patients had laparoscopic operation, and 55 (12.6%) patients had laparotomy; the conversion rate from laparoscopy to laparotomy was 3.7%. Eighty-seven (19.9%) patients experienced intraoperative hemodynamic instability.
Of 438 patients, 65(14.8%) patients had 87 postoperative complications with a Dindo–Clavien grade of 2 or greater. Sixty-three patients (14.4%) and 15 patients (3.4%) had postoperative complications of grade II and grade III, respectively. Moreover, nine patients (2.1%) suffered complications of grade IV. The details of complications were presented in Table 2. Transfusion (36, 8.2%) was the most common complications. Eight patients (1.8%) developed postoperative hypotension. Eight (1.8%) patients had reoperation, and no death occurred in our study.
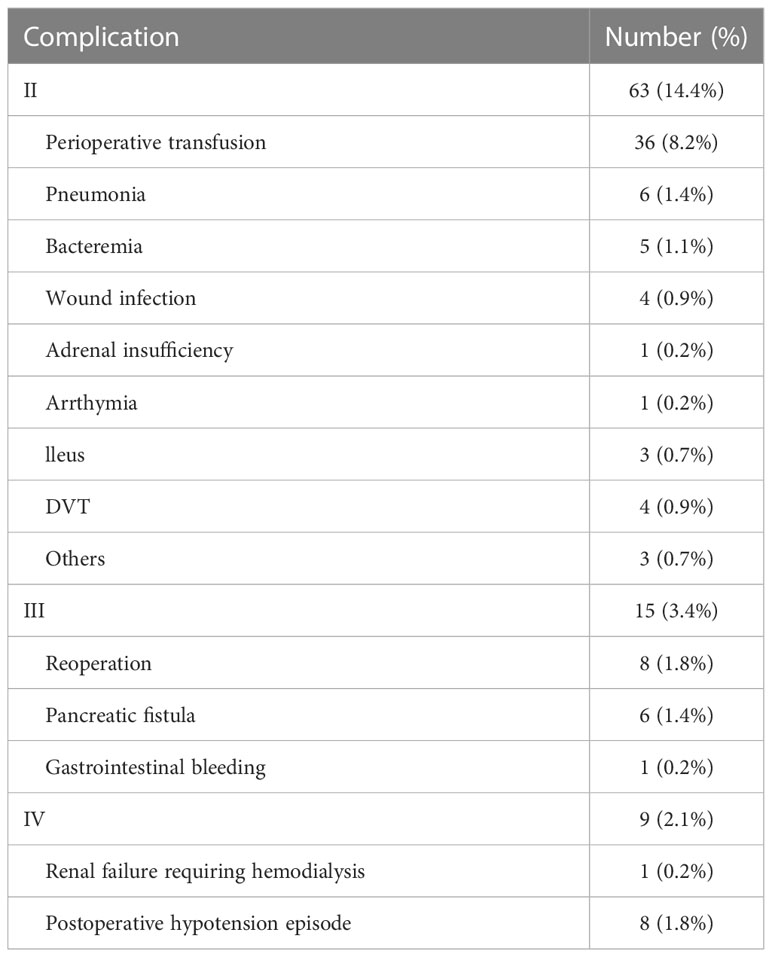
Table 2 Postoperative complications after surgery in patients with pheochromocytoma and paraganglioma.
In order to explore whether there was any difference between patients with pheochromocytoma and paraganglioma, demographic characteristics and perioperative data were compared and presented in Table 3. There was no significant difference in age (P = 0.532), BMI (P = 0.050), sex distribution (P = 0.592), ASA status (P = 0.986). Comorbidities were similar in both groups, except that a higher incidence of previous history of heart failure (P = 0.010) in patients with paraganglioma. Tumor size (P = 0.325) and the proportion of multiple tumors (P = 0.318) were similar. Patients in paraganglioma were more likely to have operation in laparotomy, and the conversion rate from laparoscopy to laparotomy was higher (P < 0.001). Moreover, for laparoscopic approach, patients with paraganglioma were more likely to have transabdominal approach. Patients with paragangliomas had longer operation time (P < 0.001) and higher incidence of postoperative complications (16.8% vs. 13.9%, P = 0.426).
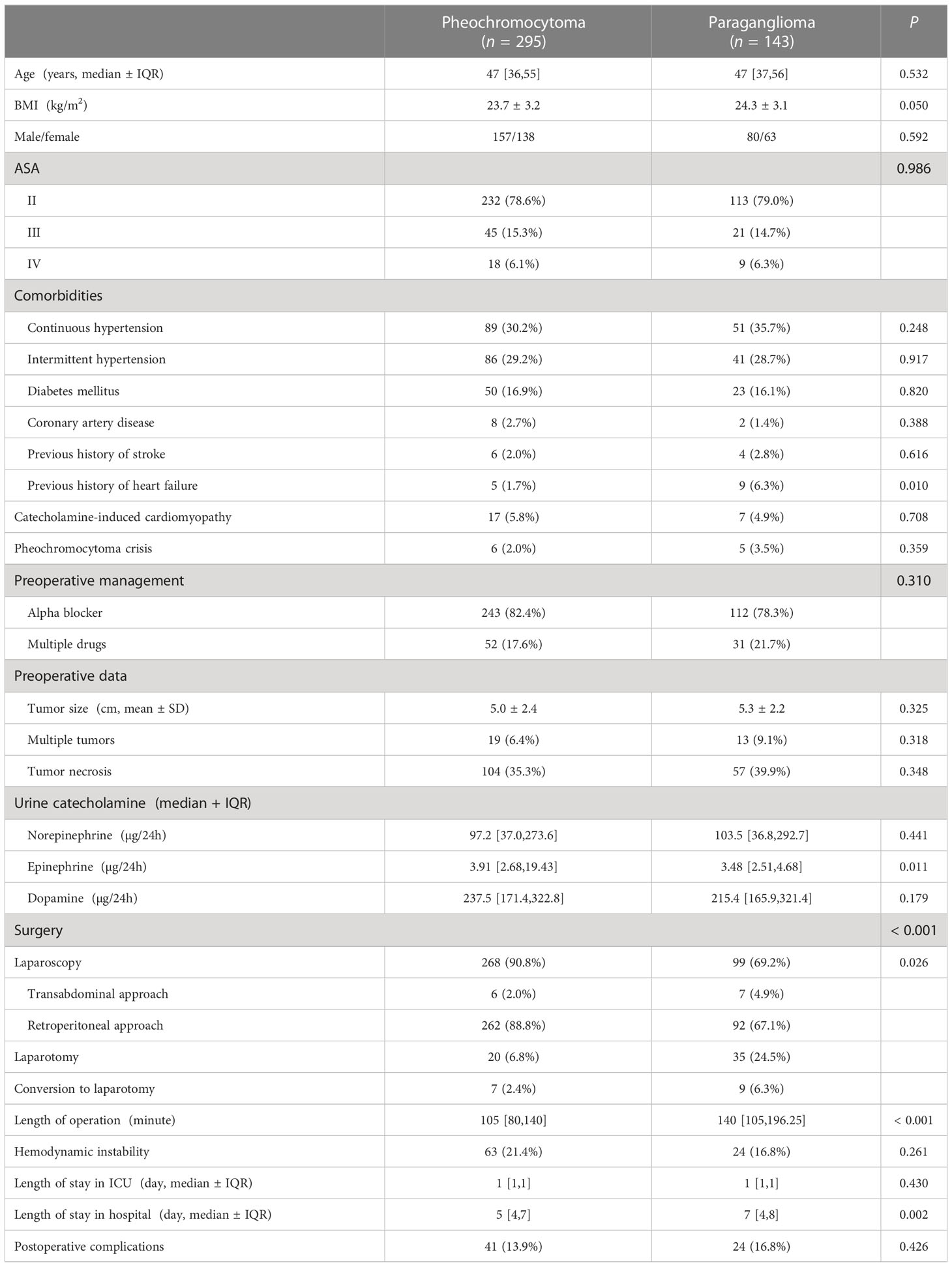
Table 3 Comparisons of demographic characteristics and perioperative data between pheochromocytoma and paraganglioma.
There was no significant difference in age (P = 0.077), gender distribution (P = 0.752), BMI (P = 0.378), and preoperative comorbidities between patients with and without complications. Patients with complications had larger tumor (P < 0.001), and they were more likely to have laparotomy or convert to laparotomy intraoperatively (P < 0.001) (see Table 1). Longer operation time (P < 0.001), higher prevalence of intraoperative hemodynamic instability (P = 0.027), and longer stay in hospital (P = 0.038) were also observed in patients with complications (see Table 1).
Binary logistical regression showed tumor larger than 5.6 cm (OR = 2.427, 95% CI 1.284–4.587, P = 0.006), laparotomy (OR = 2.590, 95% CI 1.230–5.453, P = 0.012), conversion to laparotomy (OR = 8.384, 95% CI 2.247–31.285, P = 0.002), and the operation time longer than 188 min (OR = 3.709, 95% CI 1.847–7.450, P < 0.001) were risk factors of postoperative complications after resection of pheochromocytoma and paraganglioma (see Table 4).
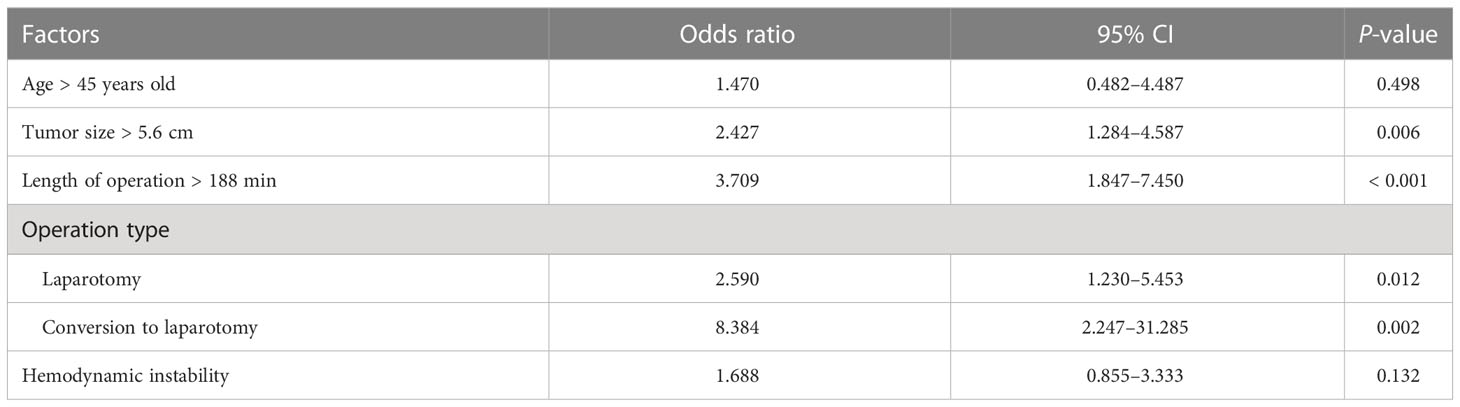
Table 4 Multivariable analysis of risk factor associated with postoperative complications in patients with pheochromocytoma and or paraganglioma.
Discussion
The incidence of postoperative complication in this high-volume, single-institution analysis was 14.8%, which was similar to that described in previous reports (5, 6). No death occurred in our analysis, and our results suggested the overall safety of perioperative management of patients with pheochromocytoma and or paraganglioma in our center.
Transfusion was the most common postoperative complication in our cohort, which was in accordance with reported series from other single-center study (7). Patients with pheochromocytoma and paraganglioma were at high risk of intraoperative blood loss due the dense vascular network (10). Cardiovascular morbidity, which included prolonged hypotension had been reported as the most common postoperative complication in other series (11–14). In our study, cardiovascular complications were lower than previously reported. The incidence of postoperative hypotension episode was 1.8% in our series. Moreover, Lan reported that only one patient was diagnosed with cardiac infarction in 350 patients in our center (15). The possible reasons were as followings: first, the mean age of our study was younger than previous reports. Second, our center was the high-volume referral center for pheochromocytoma and/or paraganglioma. Timely diagnosis and effective preoperative medical preparation all contribute to better outcome. Third, different definitions of complications, and the decades of the studies performed might lead to the different incidences of complications.
Tumor size had been confirmed as the risk factor for postoperative complications after laparoscopic adrenalectomy (7) and pheochromocytoma surgery. Tumor size was also demonstrated as the risk factor for intraoperative complications (8, 16, 17). Larger tumor is associated with more intraoperative blood loss (11) and higher level of catecholamine. Operation duration had also been confirmed as the risk factor of postoperative outcome in different types of surgery (18–21). Longer operation time is associated with more tissue damage and more blood loss; it also indicates the extent and complexity of the operation. Preoperative surgical plan and intraoperative cooperation between surgeons and anesthesiologists are essential to improve patients’ outcome.
Surgical type was the risk factors of postoperative complications for patients with pheochromocytoma and/or paraganglioma. Conversion to open laparotomy was reported in 16 patients. Open surgery or conversion to open surgery increased the incidence of complications by 2.590- and 8.384-folds, respectively. Open surgery or conversion to open surgery usually suggests the difficulty of tumor resection, longer operation time, more tissue injury, and more intraoperative blood loss. Although laparoscopic approach had been confirmed as the safety procedure for adrenalectomy, even for large tumors (22), the decision of surgical type should be determined based on surgeons’ experience, the comorbidities of patients, tumor size, and vicinity to blood vessels (23). Moreover, intraoperative conversion to open approach should not be hesitating when life-threatening bleeding occurs or malignancy was suspected. Although patients with paraganglioma were more likely to have open or conversion to open surgery, and the operation time was longer for paraganglioma resection, paraganglioma was not the risk factor of postoperative complications. Thus, the limited number of patients with paraganglioma and the impossibility of including all factors related to postoperative complications may contribute to this result.
This is a large study to evaluate postoperative outcome in patients with pheochromocytoma and/or paraganglioma; however, there are several limitations. First, this is a single-center analysis and selection bias could not be avoided. Second, postoperative complications were difficult to qualified due to the variety of definition, incomplete data, and lack of audit system. The incidence of postoperative complications may be underestimated due to the nature of retrospective study and incomplete date. Third, we did not include all potential parameters (e.g., dosage and duration of preoperative medication, the duration of hypertension), which may influence postoperative complications. Furthermore, we only analyzed the in-hospital complications, and long-term morbidity (e.g., 30-day readmission) was not performed.
In conclusion, postoperative complications after pheochromocytoma or paraganglioma were not uncommon. Tumor size, the type of surgery, and the duration of operation were risk factors for postoperative complications.
Data availability statement
The raw data supporting the conclusions of this article will be made available on reasonable request and with the permission of institution where the data were generated.
Ethics statement
The studies involving human participants were reviewed and approved by Peking Union Medical College Hospital. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
LM collected the data and wrote the manuscript. XY designed the study, performed the statistical analysis and revised the manuscript. YH supervised the study. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by National High Level Hospital Clinical Research Funding 2022-PUMCH-A-062.
Acknowledgments
We acknowledge Dr. Yuelun Zhang for his help in statistics.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Conzo G, Pasquali D, Colantuoni V, Circelli L, Tartaglia E, Gambardella C, et al. Current concepts of pheochromocytoma. Int J Surg (2014) 12:469–74. doi: 10.1016/j.ijsu.2014.04.001
2. Vorselaars WMCM, Postma EL, Mirallie E, Thiery J, Lustgarten M, Pasternak JD, et al. Hemodynamic instability during surgery for pheochromocytoma: comparing the transperitoneal and retroperitoneal approach in a multicenter analysis of 341 patients. Surgery (2018) 163(1):176–82. doi: 10.1016/j.surg.2017.05.029
3. Brunaud L, Nguyen-Thi PL, Mirallie E, Raffaelli M, Vriens M, Theveniaud PE, et al. Predictive factors for postoperative morbidity after laparoscopic adrenalectomy for pheochromocytoma: a multicenter retrospective analysis in 225 patients. Surg Endosc (2016) 30(3):1051–9. doi: 10.1007/s00464-015-4294-7
4. Bai S, Yao Z, Zhu X, Li Z, Jiang Y, Wang R, et al. Risk factors for postoperative severe morbidity after pheochromocytoma surgery: a single center retrospective analysis of 262 patients. Int J Surg (2018) 60:188–93. doi: 10.1016/j.ijsu.2018.11.019
5. Araujo-Castro M, García Centero R, López-García MC, Álvarez Escolá C, Calatayud Gutiérrez M, Blanco Carrera C, et al. Surgical outcomes in the pheochromocytoma surgery. Results from the PHEO-RISK STUDY. Endocr (2021) 74:676–84. doi: 10.1007/s12020-021-02843-6
6. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg (2004) 240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae
7. Chen Y, Scholten A, Chomsky-Higgins K, Nwaogu I, Gosnell JE, Seib C, et al. Risk factors associated with perioperative complications and prolonged length of stay after laparoscopic adrenalectomy. JAMA Surg (2018) 153:1036–41. doi: 10.1001/jamasurg.2018.2648
8. Ma L, Shen L, Zhang X, Huang Y. Predictors of hemodynamic instability in patients with pheochromocytoma and paraganglioma. J Surg Oncol (2020) 122:803–8. doi: 10.1002/jso.26079
9. Livingstone M, Duttchen K, Thompson J, Sunderani Z, Hawboldt G, Sarah Rose M, et al. Hemodynamic stability during pheochromocytoma resection: lessons learned over the last two decades. Ann Surg Oncol (2015) 22:4175–80. doi: 10.1245/s10434-015-4519-y
10. Dickson PV, Alex GC, Grubbs EG, Ayala-Ramirez M, Jimenez C, Evans DB, et al. Posterior retroperitoneoscopic adrenalectomy is a safe and effective alternative to transabdominal laparoscopic adrenalectomy for pheochromocytoma. Surgery (2011) 150:452–8. doi: 10.1016/j.surg.2011.07.004
11. Gao X, Yamazaki Y, Pecori A, Tezuka Y, Ono Y, Omata K, et al. Histopathological analysis of tumor microenvironment and angiogenesis in pheochromocytoma. Front Endocrinol (2020) 11:587779. doi: 10.3389/fendo.2020.587779
12. Kong H, Li N, Tian J, Li XY. Risk predictors of prolonged hypotension after open surgery for pheochromocytomas and paragangliomas. World J Surg (2020) 44:3786–94. doi: 10.1007/s00268-020-05706-9
13. Namekawa T, Utsumi T, Kawamura K, Kamiya N, Imamoto T, Takiguchi T, et al. Clinical predictors of prolonged postresection hypotension after laparoscopic adrenalectomy for pheochromocytoma. Surgery (2016) 159:763–70. doi: 10.1016/j.surg.2015.09.016
14. Shen WT, Grogan R, Vriens M, Clark OH, Duh QY. One hundred two patients with pheochromocytoma treated at a single institution since the introduction of laparoscopic adrenalectomy. Arch Surg (2010) 145:893–7. doi: 10.1001/archsurg.2010.159
15. Stolk RF, Bakx C, Mulder J, Timmers HJ, Lenders JW. Is the excess cardiovascular morbidity in pheochromocytoma related to blood pressure or to catecholamines? J Clin Endocrinol Metab (2013) 98:1100–6. doi: 10.1210/jc.2012-3669
16. Lan L, Shu Q, Yu C, Pei L, Zhang Y, Xu L, et al. Incidence and risk factors for myocardial injury after laparoscopic adrenalectomy for pheochromocytoma: a retrospective cohort study. Front Oncol (2022) 12:979994. doi: 10.3389/fonc.2022.979994
17. Pisarska-Adamczyk M, Zawadzka K, Więckowski K, Przęczek K, Major P, Wysocki M, et al. Risk factors for hemodynamic instability during laparoscopic pheochromocytoma resection: a retrospective cohort study. Gland Surg (2021) 10:892–900. doi: 10.21037/gs-20-783
18. Bai S, Yao Z, Zhu X, Li Z, Jiang Y, Wang R, et al. Risk factors for postoperative cardiovascular morbidity after pheochromocytoma surgery: a large single center retrospective analysis. Endocr J (2019) 66:165–73. doi: 10.1507/endocrj.EJ18-0402
19. Surace P, Sultan AA, George J, Samuel LT, Khlopas A, Molloy RM, et al. The association between operative time and short-term complications in total hip arthroplasty: an analysis of 89,802 surgeries. J Arthroplasty (2019) 34:426–32. doi: 10.1016/j.arth.2018.11.015
20. Kim BD, Hsu WK, De Oliveira GS Jr, Saha S, Kim JY. Operative duration as an independent risk factor for postoperative complications in single-level lumbar fusion: an analysis of 4588 surgical cases. Spine (2014) 39:510–20. doi: 10.1097/BRS.0000000000000163
21. Krishnan NK, Zappia J, Calaway AC, Nagle RT, Sundaram CP, Boris RS. Identifying preoperative predictors of operative time and their impact on outcomes in robot-assisted partial nephrectomy. J Endourol (2022) 36:71–6. doi: 10.1089/end.2021.0075
22. Amri R, Dinaux AM, Kunitake H, Bordeianou LG, Berger DL. Risk stratification for surgical site infections in colon cancer. JAMA Surg (2017) 152:686–90. doi: 10.1001/jamasurg.2017.0505
23. Feo CV, Portinari M, Maestroni U, Del Rio P, Severi S, Viani L, et al. Applicability of laparoscopic approach to the resection of large adrenal tumors: a retrospective cohort study on 200 patients. Surg Endosc (2016) 30:3532–40. doi: 10.1007/s00464-015-4643-6
Keywords: pheochromocytoma, paraganglioma, postoperative complication, laparoscopy, laparotomy
Citation: Ma L, Yu X and Huang Y (2023) Risk factors for postoperative complications after pheochromocytoma and/or paraganglioma: a single-center retrospective study. Front. Oncol. 13:1174836. doi: 10.3389/fonc.2023.1174836
Received: 27 February 2023; Accepted: 20 April 2023;
Published: 05 May 2023.
Edited by:
Sergei Tevosian, University of Florida, United StatesReviewed by:
Roberto de la Plaza Llamas, Head of the General Surgery and Digestive System Department, SpainAditya Shirali, University of Florida, United States
Copyright © 2023 Ma, Yu and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xuerong Yu, MTc0Nzg2NDUxNUBxcS5jb20=
 Lulu Ma
Lulu Ma Xuerong Yu
Xuerong Yu Yuguang Huang
Yuguang Huang