- 1Department of General Surgery (Hepatobiliary Surgery), The Affiliated Hospital of Southwest Medical University, Luzhou, Sichuan, China
- 2Department of Pathology, The Affiliated Hospital of Southwest Medical University, Luzhou, Sichuan, China
Xanthogranulomatous inflammation (XGI) is a rare, benign condition that can affect several organs, including the gallbladder, kidney, skin, gastrointestinal tract, lymph nodes, and soft tissues. It is often misdiagnosed as a malignancy. In this report, we present the case of a 79-year-old male who presented with persistent jaundice for 11 months. Computed tomography and magnetic resonance imaging revealed pancreatic head enlargement, gallbladder thickening, and common bile duct thickening, leading to a preoperative diagnosis of malignant neoplasm of the pancreatic head. During surgery, dense adhesions were found around the portal vein, suggestive of mass invasion. To relieve obstruction, choledochojejunostomy was performed. Postoperative pathological examination revealed xanthogranulomatous cholecystitis (XGCc), xanthogranulomatous cholangitis (XGCg), and xanthogranulomatous pancreatitis (XGP). XGI affecting the bile ducts and pancreas is extremely rare, and there are no reported cases of simultaneous involvement of the gallbladder, bile duct, and pancreas by XGI. This study provides valuable insight into the differential diagnosis of XGI by presenting the imaging features of XGI patients.
1 Introduction
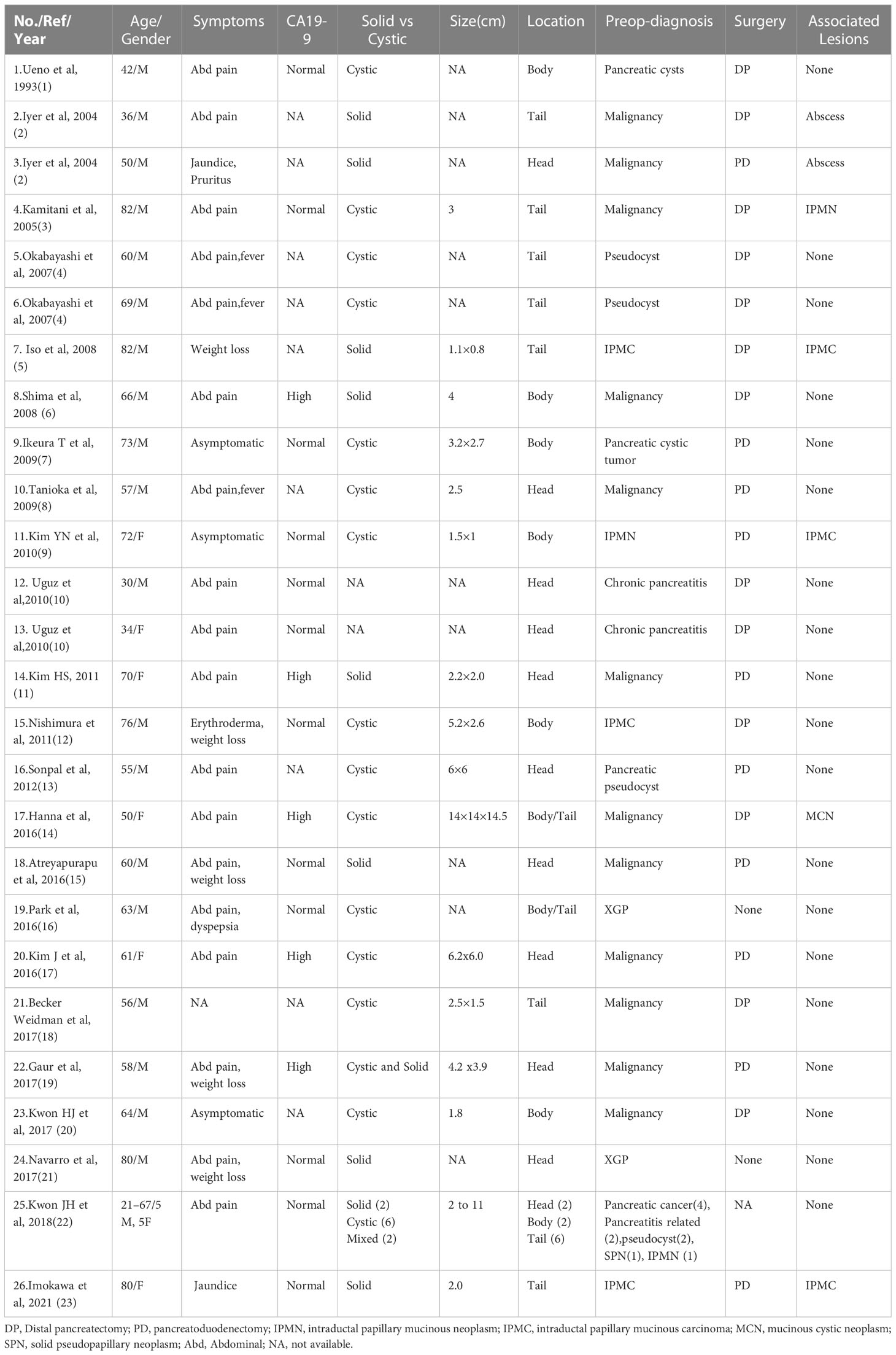
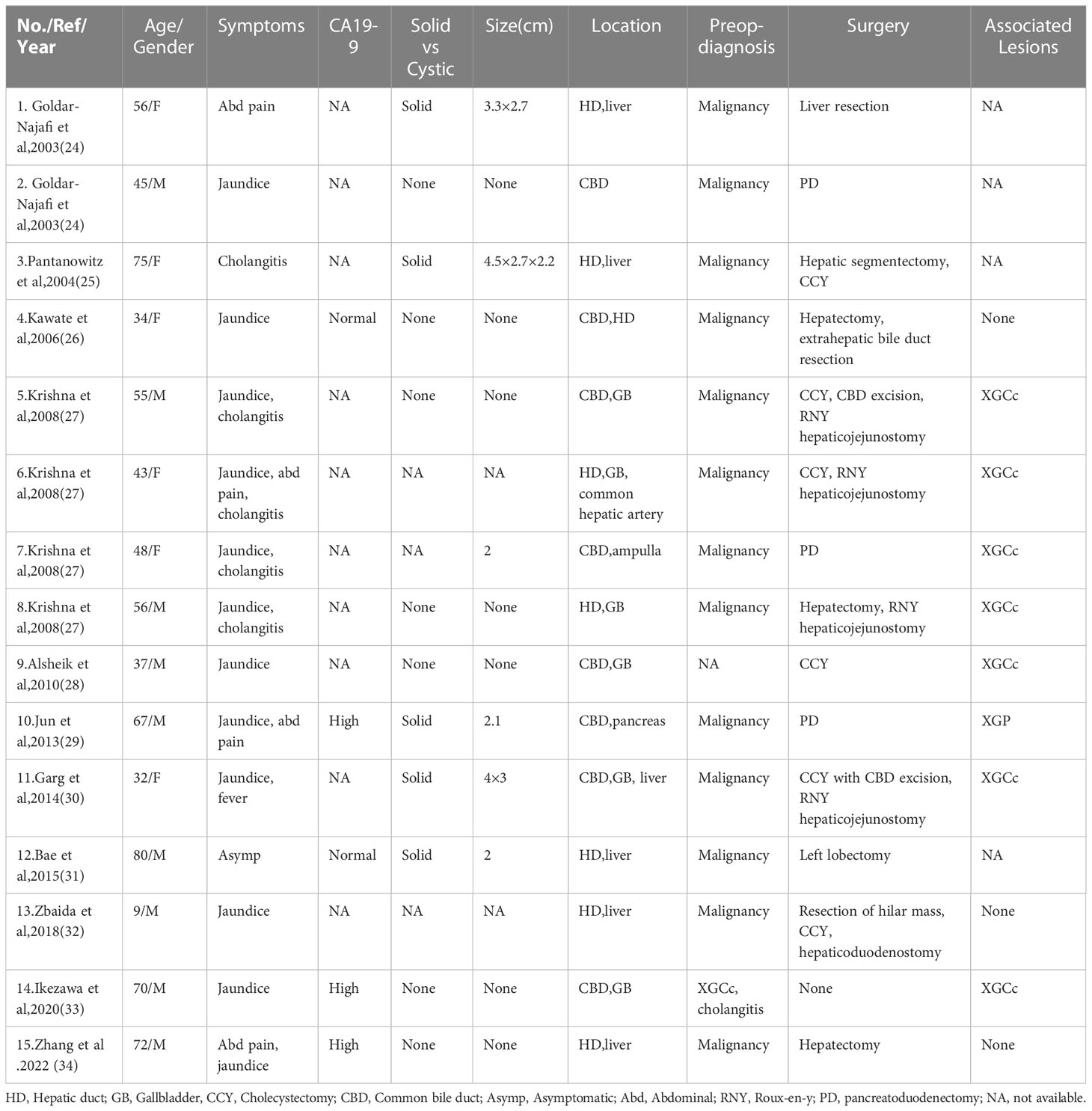
Xanthogranulomatous inflammation (XGI) is a rare but well-described disease characterized by the accumulation of foamy macrophages and inflammatory cells in different parts of the body, with infiltration and adhesion (1, 2). XGI can infiltrate any organ but most commonly appears in the gallbladder and kidneys (1), called xanthogranulomatous cholecystitis(XGCc) and xanthogranulomatous pyelonephritis. XGI rarely infiltrates the pancreas and bile ducts. Only 34 cases of xanthogranulomatous pancreatitis (XGP) (3) (Table 1) and 15 cases of xanthogranulomatous cholangitis (XGCg) (4) (Table 2) have been reported in the English language literature (supplementary). To our knowledge, we report the first case of XGI with the simultaneous involvement of the gallbladder, bile duct, and pancreas.
2 Case report
A 79-year-old male was admitted to our hospital with abdominal pain, jaundice and weight loss. No obvious abnormality was found in the physical examination of the patient. Laboratory results: carbohydrate antigen 19-9 (CA19-9)>400 U/ml(normal range <37 U/ml), total bilirubin (TBIL) 267.1 μmol/L (normal range <23 μmol/L). Other laboratory test results were within the normal range. Because the patient had severe jaundice, he first underwent percutaneous transhepatic cholangio drainage. One month later, he was hospitalized again. Laboratory results: CA19-9 125.2 U/ml, TBIL 96.3 μmol/L. Contrast-enhanced computed tomography (CT) showed that the common bile duct was thickened (Figure 1A) and the head of the pancreas was enlarged (Figure 1B), but no abnormal enhancing shadow was found. Magnetic resonance imaging (MRI) showed dilatation of the extrahepatic bile ducts (Figure 1C) and thickening of the gallbladder wall. The pancreatic head was enlarged — the maximum transverse diameter was about 3.7 cm, the pancreatic signal was uniform, and no exact abnormal enhancement shadow was found (Figure 1D). On contrast-enhanced ultrasound, an uneven low-intensity lesion with a size of about 2.8 × 2.7 cm was found in the pancreatic head, with an irregular shape and an unclear boundary. We planned to make a further diagnosis with endoscopic ultrasound fine-needle aspiration, but the patient refused. Based on the above findings, the possibility of a pancreatic head malignant tumor was very high. Therefore, a pancreaticoduodenectomy was planned to be performed. During surgery, dilated and completely obstructed common bile ducts were found, and dense adhesions were present around the portal veins, which could not be divided. It was surmised that the mass invaded the portal vein. To relieve the obstruction, a choledochojejunostomy was performed, and some masses were removed for biopsy.

Figure 1 CT (A) Arrows indicate thickened gallbladder wall and thickened common bile duct; (B) Arrows indicate enlarged pancreatic head; MRI (C) Arrows indicate dilated extrahepatic bile ducts; (D) Arrows indicate thickened gallbladder wall and enlarged pancreatic head; (E) Follow up CT at 4 months after surgery; (F) Subsequent CT performed at 9 months post-surgery revealed no significant abnormalities in the pancreas.
Numerous foam cell, lymphocyte, and plasma cell infiltrates were found in the resected mass and gallbladder (Figures 2A-C). Immunohistochemical findings showed CD68 (+) (Figure 2D), CK (-), VIM (+), CD19 (-), Ki-67 (<1%), ALK1 (-), and p53 (-). Immunohistochemical results supported the diagnosis of xanthogranuloma invading the pancreatic head, common bile duct, and gallbladder. After 10 months of close follow-up (Figures 1E, F), the patient had no symptoms and a good quality of life.

Figure 2 (A). Interstitial fibroplasia of the gallbladder is accompanied by infiltration of foam cells, lymphocytes, and plasma cells. Arrows indicate the location of foam cells and the muscularis layer of the gallbladder from left to right (100×); (B). Left-to-right pointing arrows denote the presence of pancreaticobiliary epithelial atrophy and foam cells, respectively (100×); (C). Nodular aggregates of foam cells are visible, and all foam cells are indicated by the arrows(100×); (D). Foam cell CD68+ (100×).
3 Discussion
XGI is a benign lesion, but it can be easily misdiagnosed as malignant and treated surgically. The pathogenesis underlying this condition remains unclear given the limited number of reported cases. The limited existing literature suggest that high intraluminal pressure and infection seem to be the etiology of the XGI series of disorders (3, 5). In the present case, it may be that XGCc occurred first because XGCc is more common and then inflammatory cells infiltrated into surrounding tissues along the biliary tract. This patient presented with progressive aggravation of jaundice for up to 11 months, which may account for such a wide range of infiltrates.
The diagnosis of most XGCg and XGP is achieved by the pathological evaluation of surgical or biopsy specimens. Therefore, we need to focus on the preoperative diagnosis of them. Although imaging findings and differential points of XGI have not been established, some features have been suggested to date. Zhao et al. (6) believe that diffuse gallbladder wall thickening, hypo-attenuated intramural nodules, continuous mucosal lines, lumen surface enhancement, and coexistence of gallstones highly suggest XGCc. In the present case, CT showed thickening of the gallbladder wall with continuous mucosal lines and the presence of an easily overlooked low-density image on the gallbladder wall. No gallstones were found, and parts of the CT features were the same as those reported by Zhao et al. (6). Krishna et al. (7) reported that a thick-walled gallbladder and bile duct stenosis might be indicators of XGCc with XGCg. In our CT features, a thick-walled gallbladder and thickened common bile duct were found. Therefore, the possibility of XGCc with XGCg should be considered when narrow or thickened bile ducts and thick-walled gallbladders occur together and simultaneously. XGP can develop from pancreatic pseudocyst or necrotizing pancreatitis. Early visible lobulated cystic masses can be misdiagnosed as solid pseudopapillary neoplasm, intraductal papillary mucinous neoplasm, and pseudocyst (8). Advanced imaging shows lobulated contours and heterogeneous masses, hypovascularity, and a progressive enhancement pattern with restricted diffusion, which are nearly identical to pancreatic cancer (9). Our case may be at an advanced stage.
Among treatment modalities, most previous cases were treated surgically, and only a few patients chose conservative treatment after diagnosis by one or more pathological examinations (10, 11). Currently, repeat pathological examination preoperatively is the only way to avoid surgical treatment. But repeat pathological examination preoperatively may also miss malignancy. Therefore, in the future, attention should be paid to the preoperative diagnostic methods for the XGI series of diseases.
4 Conclusion
In conclusion, although XGCg and XGP are rare diseases, they are often misdiagnosed as malignancies. Differential diagnosis should be emphasized. If CT simultaneously shows bile duct stenosis or thickening and gallbladder wall thickening, the possibility of XGI should be considered. Repeat pathological examination may be helpful in making the diagnosis.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JZ and HL are responsible for the writing of this article, and XL collected patient data. QG, PW, XY, and BL for help with reviewing previous articles. SS was responsible for the final review of the article. All authors contributed to the article and approved the submitted version.
Funding
This study is supported by the Key Research and Development Project of Science & Technology Department of Sichuan Province (20ZDYF1129).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Dhawan S, Jain D, Kalhan SK. Xanthogranulomatous inflammation of ascending colon with mucosal involvement: report of a first case. J Crohns Colitis (2011) 5(3):245–8. doi: 10.1016/j.crohns.2010.12.009
2. Kamitanim T, Nishimiya M, Takahashi N. Xanthogranulomatous pancreatitis associated with intraductal papillary mucinous tumor. AJR Am J Roentgenol (2005) 185(3):704–7. doi: 10.2214/ajr.185.3.01850704
3. Imokawa T, Ito K, Takemura N, Inagaki F, Mihara F, Kokudo N. Xanthogranulomatous pancreatitis accompanied by xanthogranulomatous cholecystitis: a case report and literature review. Pancreas (2021) 50(7):1037–41. doi: 10.1097/MPA.0000000000001875
4. Zhang JQ, Truong L, Pan J, Yakirevich E, Hyder SM, Beard RE. Xanthogranulomatous cholangitis mimicking cholangiocarcinoma: case report and review of literature. Int J Surg Case Rep (2022) 93:106921. doi: 10.1016/j.ijscr.2022.106921
5. Ueno T, Hamanaka Y, Nishihara K, Nishida M, Nishikawa M, Kawabata A, et al. Xanthogranulomatous change appearing in the pancreas cyst wall. Pancreas (1993) 8(5):647–57. doi: 10.1097/00006676-199309000-00020
6. Zhao F, Lu PX, Yan SX, Wang GF, Yuan J, Zhang SZ, et al. CT and MR features of xanthogranulomatous cholecystitis: an analysis of consecutive 49 cases. Eur J Radiol (2013) 82(9):1391–7. doi: 10.1016/j.ejrad.2013.04.026
7. Krishna RP, Kumar A, Singh RK, Sikora S, Saxena R, Kapoor VK, et al. Xanthogranulomatous inflammatory strictures of extrahepatic biliary tract: presentation and surgical management. J Gastrointest Surg (2008) 12(5):836–41. doi: 10.1007/s11605-008-0478-y
8. Park JM, Cho SH, Bae H-I, Seo NA, Kim HJ, Lee SM, et al. Xanthogranulomatous pancreatitis mimicking a pancreatic cancer on CT and MRI: a case report and literature review. Invest Magnetic Resonance Imaging (2016) 20(3). doi: 10.13104/imri.2016.20.3.185
9. Kwon JH, Kim JH, Kim SY, Byun JH, Kim HJ, Hong SM, et al. Imaging and clinical features of xanthogranulomatous pancreatitis: an analysis of 10 cases at a single institution. Abdom Radiol (NY) (2018) 43(12):3349–56. doi: 10.1007/s00261-018-1630-0
10. Ikezawa K, Wada H, Nakatsuka S, Takada R, Fukutake N, Ohkawa K. Gastrointestinal: xanthogranulomatous cholangitis diagnosed by endoscopic ultrasound-guided fine-needle aspiration. J Gastroenterol Hepatol (2020) 35(9):1464. doi: 10.1111/jgh.14953
Keywords: xanthogranulomatous cholangitis, xanthogranulomatous pancreatitis, xanthogranulomatous cholecystitis, XGI, XGP
Citation: Zhang J, Lin H, Li X, Wang P, Yang X, Li B, Guo Q and Su S (2023) Xanthogranulomatous inflammation involving the gallbladder, bile duct, and pancreas: a case report. Front. Oncol. 13:1191181. doi: 10.3389/fonc.2023.1191181
Received: 21 March 2023; Accepted: 10 April 2023;
Published: 16 May 2023.
Edited by:
Jose M. Ramia, Hospital General Universitario de Alicante, SpainReviewed by:
Rahul Gupta, Synergy Institute of Medical Sciences, IndiaRoberto de la Plaza Llamas, Head of the General Surgery and Digestive System Department, Spain
Copyright © 2023 Zhang, Lin, Li, Wang, Yang, Li, Guo and Su. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Song Su, MTM4ODI3Nzg1NTRAMTYzLmNvbQ==; Qinxi Guo, Z3F4Xzc3QDE2My5jb20=; Bo Li, bGlib2VyMjAwMkAxMjYuY29t
†These authors have contributed equally to this work and share first authorship
 Jinchang Zhang1†
Jinchang Zhang1† Xiaoli Yang
Xiaoli Yang Song Su
Song Su