- 1Department of Radiation Oncology, University of Tsukuba, Tsukuba, Japan
- 2Department of Pediatric Radiation Therapy Center/Pediatric Proton Beam Therapy Center, Hebei Yizhou Cancer Hospital, Zhuozhou, China
- 3Department of Radiation Oncology, Tsukuba Medical Center Hospital, Tsukuba, Japan
- 4Department of Pediatrics, University of Tsukuba Hospital, Tsukuba, Japan
- 5Department of Child Health, Institute of Medicine, University of Tsukuba, Tsukuba, Japan
- 6Department of Biostatistics, Institute of Medicine, University of Tsukuba, Tsukuba, Japan
Introduction: Chondrosarcoma is a rare malignant bone tumor. Particle beam therapy (PT) can concentrate doses to targets while reducing adverse events. A meta-analysis based on a literature review was performed to examine the efficacy of PT and photon radiotherapy for skull base chondrosarcoma.
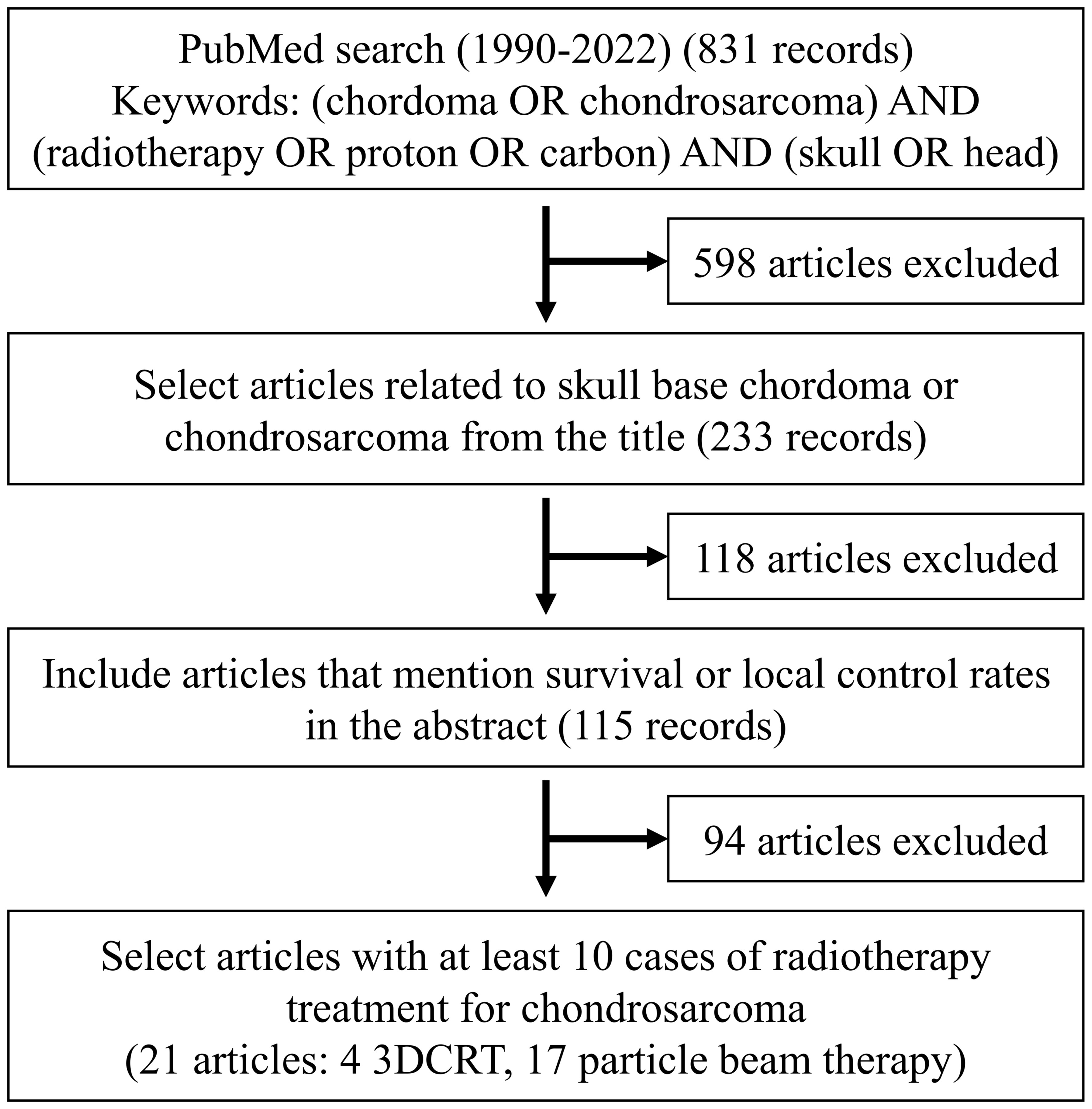
Methods: The meta-analysis was conducted using 21 articles published from 1990 to 2022.
Results: After PT, the 3- and 5-year overall survival (OS) rates were 94.1% (95% confidence interval [CI]: 91.0-96.2%) and 93.9% (95% CI: 90.6-96.1%), respectively, and the 3- and 5-year local control rates were 95.4% (95% CI: 92.0-97.4%) and 90.1% (95% CI: 76.8-96.0%), respectively. Meta-regression analysis revealed a significant association of PT with a superior 5-year OS rate compared to three-dimensional conformal radiotherapy (p < 0.001). In the studies used in the meta-analysis, the major adverse event of grade 2 or higher was temporal lobe necrosis (incidence 1-18%, median 7%).
Conclusion: PT for skull base chondrosarcoma had a good outcome and may be a valuable option among radiotherapy modalities. However, high-dose postoperative irradiation of skull base chondrosarcoma can cause adverse events such as temporal lobe necrosis.
1 Introduction
Chondrosarcoma is a rare malignant bone tumor that originates from cells that produce cartilage (1). It is the second most prevalent sarcoma of the bone, after osteosarcoma (1). Chondrosarcomas can develop anywhere in the body. The most common type found in the skull base is mesenchymal chondrosarcoma, which is typically a malignant tumor with slow growth and a low rate of metastasis (2). However, skull base chondrosarcomas are locally invasive tumors that often pose challenges in achieving complete removal through surgical resection (3). There is also a high incidence of local recurrence, and this has been suggested to be significantly associated with an elevated risk of metastasis and death due to the tumor (3). Therefore, postoperative radiotherapy is generally recommended following as extensive surgical resection as possible (4).
Advances in technology have permitted the use of stereotactic radiotherapy and intensity-modulated radiotherapy for the administration of high doses of radiation to lesions (5). Proton beam therapy (PBT) and carbon-ion radiotherapy (CIRT) are types of particle beam therapy (PT) that offer physical advantages enabling the delivery of a high dose to the target area while minimizing exposure to healthy surrounding organs (6, 7). Good survival and local control rates have also been reported for CIRT in comparison to PBT and definitive irradiation of unresectable cases (7). Since skull base chondrosarcoma is a rare disease, there is a scarcity of randomized controlled trials of treatment. Consequently, there is a need for meta-analyses and systematic reviews to examine different treatment modalities. Here, we conducted such a meta-analysis based on a literature review.
2 Methods
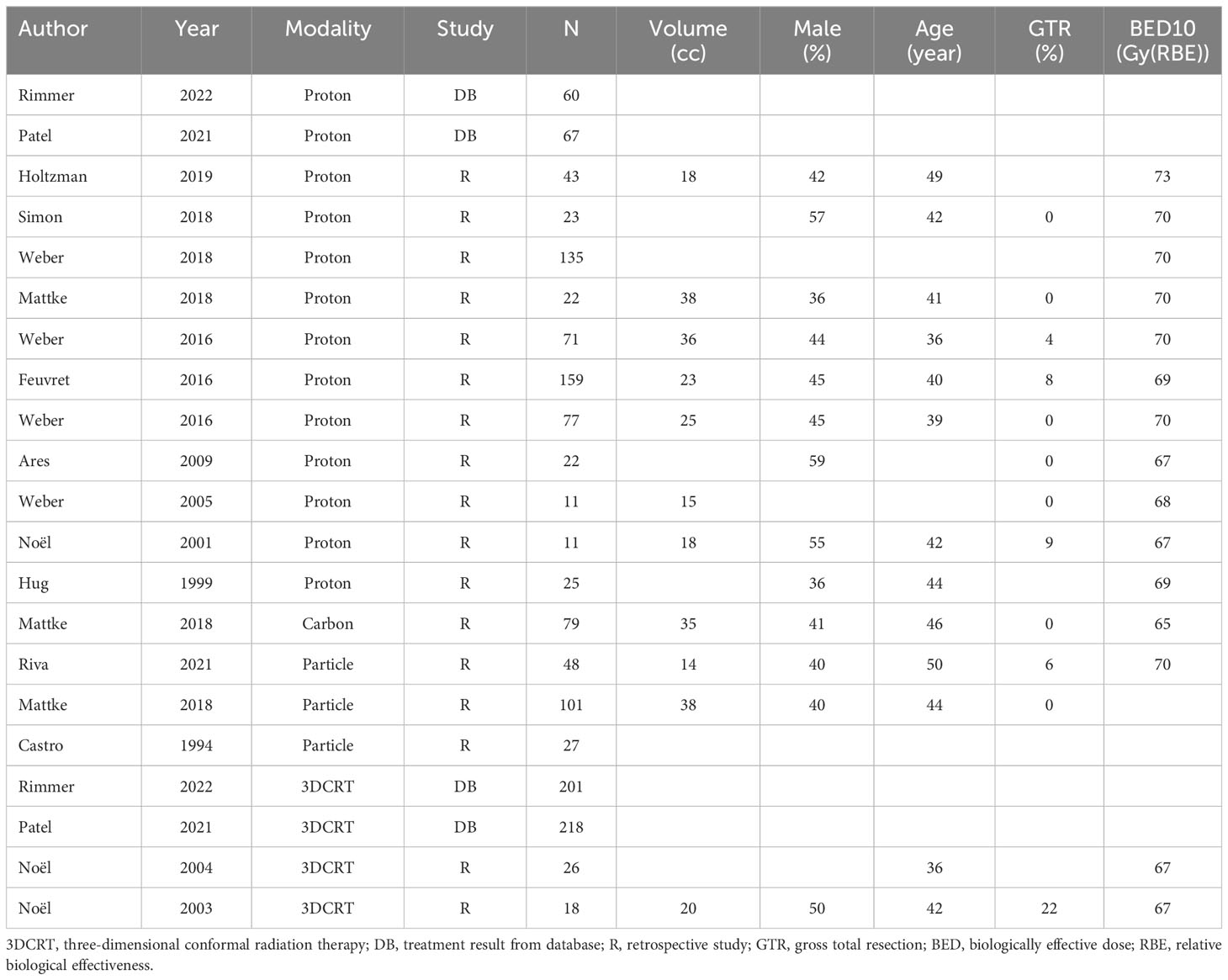
This review and meta-analysis were conducted following the guidelines and recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (8, 9). A search was performed for relevant articles published in English between 1990 and 2022. The selection criteria are shown in Figure 1. The search was conducted in PubMed using the terms (chordoma OR chondrosarcoma) AND (radiotherapy OR proton OR carbon) AND (skull OR head). Among the 831 articles identified, two reviewers screened the titles to extract articles pertaining to skull base chordoma or skull base chondrosarcoma. In cases of uncertainty, a third reviewer was consulted for further evaluation. The reviewers examined the abstracts to identify those that specified survival or local control rates, resulting in the selection of 115 out of 233 abstracts. The full text of the selected abstracts was then read to extract information on variables such as the number of cases, survival rate, local control rate, gender, resection, resection rate, tumor size, tumor volume, prescription dose, number of fractions, and treatment modality. This process yielded a final selection of articles (4, 6, 10–24) with at least 10 cases per treatment modality, including 38 cases of chordoma and 21 cases of chondrosarcoma (Table 1). The extracted data comprised the author, year, sample size, country, article type, age, gender, tumor diameter, tumor volume, resection rate, and tissue type. Radiotherapy data, including the modality and prescribed dose, are shown in Table 2.
Random effects meta-analyses of 3- and 5-year overall survival (OS) and local control (LC) rates for each treatment modality were performed to generate forest plots. For studies with missing accuracy data, missing values were imputed using information on the number of cases, size of the risk set each year, and mean dropout rate. Heterogeneity in each meta-analysis was assessed by I-square statistics. Random-effects meta-regressions with modality as the explanatory variable were performed for each outcome to compare across modalities. All analyses were performed using R software (R Core Team, Vienna, Austria) and its meta package (25).
3 Results
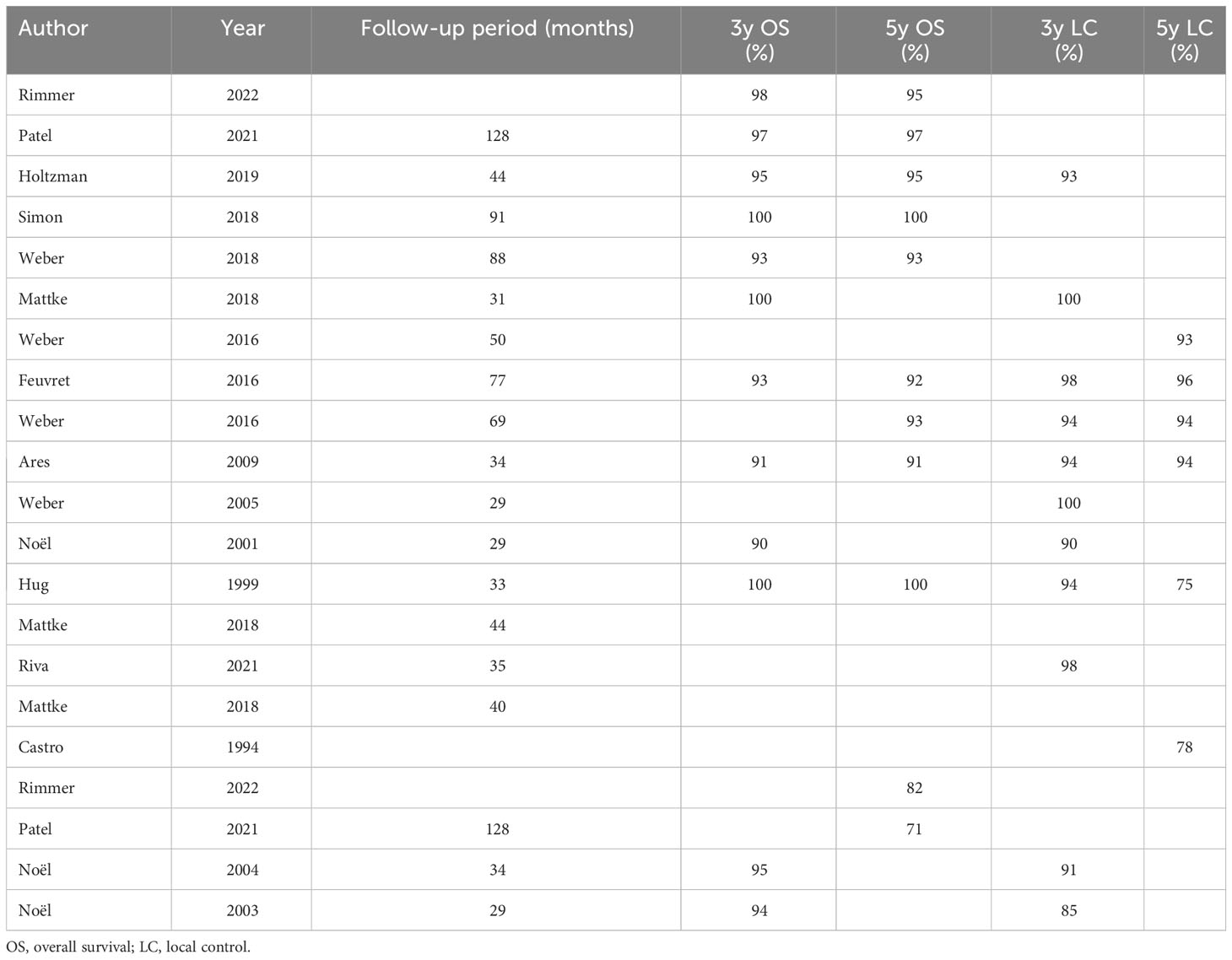
Initially, a meta-analysis was conducted using all the selected literature. Due to the limited number of articles, it was challenging to generate forest plots for three-dimensional conformal radiotherapy (3DCRT). Therefore, forest plots for OS and LC rates are only presented for PT (Figures 2, 3). After PT, the 3- and 5-year OS rates were 94.1% (95% confidence interval [CI]: 91.0-96.2%) and 93.9% (95% CI: 90.6-96.1%), respectively, and the 3- and 5-year LC rates were 95.4% (95% CI: 92.0-97.4%) and 90.1% (95% CI: 76.8-96.0%), respectively. Meta-regression analysis revealed a significant association between PT and a superior 5-year OS rate compared to 3DCRT (p < 0.001). Comparison of the 5-year LC rate for PT and 3DCRT could not be made due to insufficient data. The doses used in PT in the selected articles were 60 Gy (relative biological effectiveness [RBE]) in 20 fraction, 68 Gy (RBE) in 34 fraction, 70 Gy (RBE) in 35 fraction, 70.2 Gy (RBE) in 39 fraction, and 73.8 Gy (RBE) in 41 fraction. The major adverse events (AEs) of grade 2 or higher were temporal lobe necrosis (incidence 1-18%, median 7%) (6, 11, 13, 15, 21) and pituitary hypofunction (incidence 9-27%, median 16%) (6, 11, 15, 18).
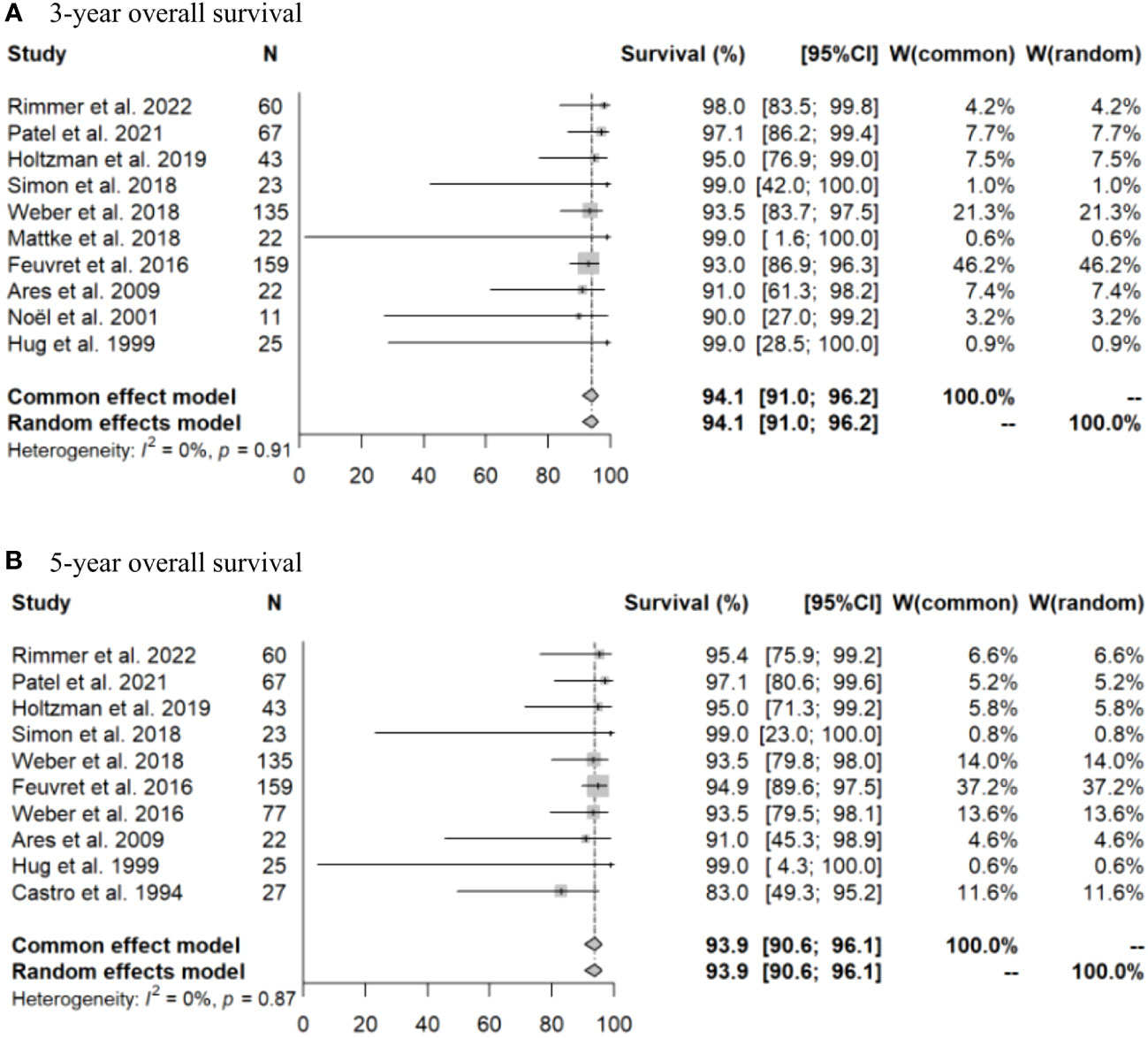
Figure 2 Forest plots for (A) 3-year and (B) 5-year overall survival rates after particle beam therapy.
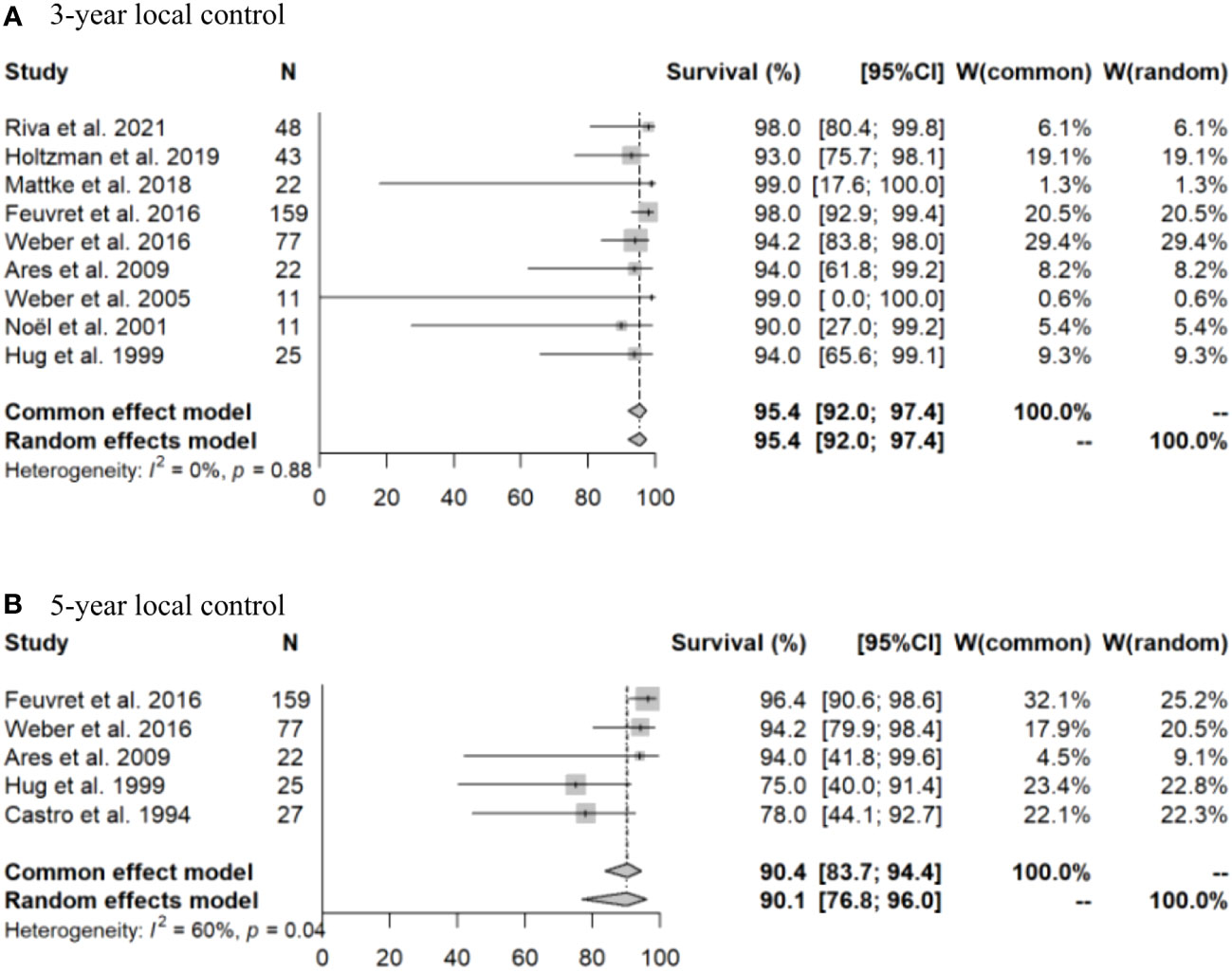
Figure 3 Forest plots for (A) 3-year and (B) 5-year local control rates after particle beam therapy.
4 Discussion
Chondrosarcoma of the skull base is a rare disease and is often reported together with chordoma of the skull base; however, several studies have suggested that chondrosarcoma has a better prognosis (26–29). Since these are locally invasive tumors, the best way to improve the local progression-free period is to remove as much tumor as possible while preserving function, with postoperative radiotherapy for cases of chondrosarcoma without complete resection (30, 31). The effects of different radiotherapy modalities have not been examined in this context, although the higher dose concentration as an advantage of PT over conventional 3DCRT has been noted (32, 33). This study was designed to examine this issue, but it was difficult to collect sufficient cases in the literature, and only a summary of the results of postoperative irradiation with PT was ultimately possible.
In this study, the 5-year OS was better after PT (93.9%) than after 3DCRT (71.0-82.3%) (p<0.001), which may reflect the value of postoperative PT. At our center, the 5-year LC rate after PBT for 18 cases of chondrosarcoma was 100%, and the prognosis for skull base chondrosarcoma was favorable (34). However, AEs from postoperative irradiation can be problematic. Advances in radiotherapy techniques have allowed delivery of higher doses to the target, but radiation brain necrosis, especially of the temporal lobe, is a major AE in irradiation of the skull base (6, 34, 35). Radiation brain necrosis is generally shown that the risk is significantly related to the dose and volume of irradiated normal brain (36, 37). In a report on stereotactic radiotherapy, the incidence of radiation brain necrosis was significantly higher when the volume of normal brain irradiated with >25 Gy exceeded 16cc or with >30 Gy exceeded 10 cc, when metastatic brain tumors were irradiated in 5 fractions (36). For conventional fractionation to partial brain, a 5% and 10% risk of symptomatic radiation necrosis is predicted to occur at 72 Gy [range, 60–84] and 90 Gy [range, 84–102], and the brain is especially sensitive to fraction sizes >2 Gy (37). In PBT, risk factors for temporal lobe brain necrosis include a volume of 5.5 cc irradiated at ≥60 Gy and a volume of 1.7 cc irradiated at ≥70 Gy (35). Our PBT facility has reported an incidence of brain necrosis of grade 2 or higher of 3.9% over 5 years, with the total dose at treatment associated with the development of brain necrosis (34). The incidence of temporal lobe necrosis of grade 2 or higher in the studies in the current analysis was 1-18% (median 7%), which is slightly higher than that at our center. The dose-volume-histogram for the temporal lobes in each study was a concern.
It was difficult to compare PBT vs, X-ray radiotherapy because of the small number of articles on X-ray. However, there are many references on PBT, and the results of a meta-analysis showed a good 5-year overall survival rate of 93.9% and a 5-year local control rate of 90.1%, so we think it was meaningful to show that PT is appropriate as postoperative irradiation for skull base chondrosarcoma. On the other hand, temporal lobe necrosis also occurred in 1-18% of patients, although the number of severe cases was small. The future challenge is to select an irradiation strategy that minimizes the probability of adverse events such as temporal lobe necrosis while maintaining this treatment outcome.
The limitation of this study is that it could not be performed in detail because of the lack of information on how to determine the margin to the target and the setting of the prophylactic irradiation range, and because of the different treatment policies at each center. The differences in PT due to different irradiation techniques (fixed beam or gantry-based beam and passive-scattering or scanning) were not discussed due to the lack of detailed information. Since the resection rate varies with time for surgery as well as radiotherapy, and the resection rate may affect the outcome of treatment, we tried to incorporate the resection rate as a risk factor, but the limitation is that we could not analyze it well because there are few articles specifying the resection rate. Moreover, it is not very accurate due to the small number of articles on X-ray radiotherapy, so the data will need to be updated in the future when more stereotactic radiotherapy and stereotactic radiosurgery articles are published.
5 Conclusion
Comparison of X-ray therapy with PT for skull base chondrosarcoma is challenging, but PT has a good outcome and may be a useful option among radiotherapy modalities. A good survival rate is likely after high-dose postoperative irradiation of skull base chondrosarcoma, but AEs such as temporal lobe necrosis may occur and there is room for improvement in both the choice of the radiotherapy modality and setting of the irradiation field.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
MN: Visualization, Writing – original draft, Writing – review & editing, Data curation. MM: Conceptualization, Data curation, Validation, Writing – original draft, Writing – review & editing. TS: Data curation, Writing – review & editing. SS: Data curation, Investigation, Writing – review & editing. YL: Data curation, Investigation, Writing – review & editing. YO: Data curation, Writing – review & editing. MI: Data curation, Writing – review & editing. SH: Conceptualization, Data curation, Writing – review & editing. HF: Conceptualization, Data curation, Writing – review & editing. RS: Conceptualization, Data curation, Writing – review & editing. TI: Conceptualization, Methodology, Writing – review & editing. KN: Conceptualization, Data curation, Writing – review & editing. KM: Formal analysis, Validation, Writing – review & editing. HS: Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by institutional funds only.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Gazendam A, Popovic S, Parasu N, Ghert M. Chondrosarcoma: a clinical review. J Clin Med. (2023) 12:2506. doi: 10.3390/jcm12072506
2. Awad M, Gogos AJ, Kaye AH. Skull base chondrosarcoma. J Clin Neurosci. (2016) 24:1–5. doi: 10.1016/j.jocn.2015.10.029
3. Kremenevski N, Schlaffer SM, Coras R, Kinfe TM, Graillon T, Buchfelder M. Skull base chordomas and chondrosarcomas. Neuroendocrinology. (2020) 110:836–47. doi: 10.1159/000509386
4. Patel S, Nunna RS, Ryoo JS, Ansari D, Chaudhry NS, Mehta AI. Outcomes and patterns of care in adult skull base chondrosarcoma patients in the United States. World Neurosurg. (2021) 150:71–83. doi: 10.1016/j.wneu.2021.03.097
5. Combs SE, Baumert BG, Bendszus M, Bozzao A, Brada M, Fariselli L, et al. ESTRO ACROP guideline for target volume delineation of skull base tumors. Radiother Oncol. (2021) 156:80–94. doi: 10.1016/j.radonc.2020.11.014
6. Holtzman AL, Rotondo RL, Rutenberg MS, Indelicato DJ, Mercado CE, Rao D, et al. Proton therapy for skull-base chondrosarcoma, a single-institution outcomes study. J Neurooncol. (2019) 142:557–63. doi: 10.1007/s11060-019-03129-8
7. Cuccia F, Fiore MR, Barcellini A, lannalfi A, Vischoni B, Ronchi S, et al. Outcome and toxicity of carbon ion radiotherapy for axial bone soft tissue sarcomas. Anticancer Res. (2020) 40:2853–9. doi: 10.21873/anticanres.14260
8. Knobloch K, Yoon U, Vogt PM. Preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement and publication bias. J Craniomaxillofac Surg. (2011) 39:91–2. doi: 10.1016/j.jcms.2010.11.001
9. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PloS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
10. Rimmer RA, Mace JC, Andersen PE, Cetas JS, Ciporen JN, Dogan A, et al. Determinants of survival in sinonasal and skull base chondrosarcoma: An analysis of the National Cancer Database. Int Forum Allergy Rhinol. (2022) 12:699–713. doi: 10.1002/alr.22909
11. Simon F, Feuvret L, Bresson D, Guichard JP, EI Zein S, Bernat AL, et al. Surgery and protontherapy in Grade I and II skull base chondrosarcoma: A comparative retrospective study. PloS One. (2018) 13:e0208786. doi: 10.1371/journal.pone.0208786
12. Weber DC, Murray F, Combescure C, Calugaru V, Alapetite C, Albertini F, et al. Long term outcome of skull-base chondrosarcoma patients treated with high-dose proton therapy with or without conventional radiation therapy. Radiother Oncol. (2018) 129:520–6. doi: 10.1016/j.radonc.2018.06.040
13. Mattke M, Vogt K, Bougatf N, Welzel T, Oelmann-Avendano J, Hauswald H, et al. High control rates of proton- and carbon-ion-beam treatment with intensity-modulated active raster scanning in 101 patients with skull base chondrosarcoma at the Heidelberg Ion Beam Therapy Center. Cancer. (2018) 124:2036–44. doi: 10.1002/cncr.31298
14. Weber DC, Malyapa R, Albertini F, Bolsi A, Kliebsch U, Walser M, et al. Long term outcomes of patients with skull-base low-grade chondrosarcoma and chordoma patients treated with pencil beam scanning proton therapy. Radiother Oncol. (2016) 120:169–74. doi: 10.1016/j.radonc.2016.05.011
15. Feuvret L, Bracci S, Calugaru V, Bolle S, Mammar H, De Marzi L, et al. Efficacy and safety of adjuvant proton therapy combined with surgery for chondrosarcoma of the skull base: A retrospective, population-based study. Int J Radiat Oncol Biol Phys. (2016) 95:312–21. doi: 10.1016/j.ijrobp.2015.12.016
16. Weber DC, Badiyan S, Malyapa R, Albertini F, Bolsi A, Lomax AJ, et al. Long-term outcomes and prognostic factors of skull-base chondrosarcoma patients treated with pencil-beam scanning proton therapy at the Paul Scherrer Institute. Neuro Oncol. (2016) 18:236–43. doi: 10.1093/neuonc/nov154
17. Ares C, Hug EB, Lomax AJ, Bolsi A, Timmermann B, Rutz HP, et al. Effectiveness and safety of spot scanning proton radiation therapy for chordomas and chondrosarcomas of the skull base: first long-term report. Int J Radiat Oncol Biol Phys. (2009) 75:1111–8. doi: 10.1016/j.ijrobp.2008.12.055
18. Weber DC, Rutz HP, Pedroni ES, Bolsi A, Timmermann B, Verwey J, et al. Results of spot-scanning proton radiation therapy for chordoma and chondrosarcoma of the skull base: the Paul Scherrer Institut experience. Int J Radiat Oncol Biol Phys. (2005) 63:401–9. doi: 10.1016/j.ijrobp.2005.02.023
19. Noël G, Habrand JL, Mammar H, Pontvert D, Haie-Méder C, Hasboun D, et al. Combination of photon and proton radiation therapy for chordomas and chondrosarcomas of the skull base: the Centre de Protonthérapie D’Orsay experience. Int J Radiat Oncol Biol Phys. (2001) 51:392–8. doi: 10.1016/s0360-3016(01)01634-0
20. Hug EB, Loredo LN, Slater JD, DeVries A, Grove RI, Schaefer RA, et al. Proton radiation therapy for chordomas and chondrosarcomas of the skull base. J Neurosurg. (1999) 91:432–9. doi: 10.3171/jns.1999.91.3.0432
21. Riva G, Cavallo I, Gandini S, Ingargiola R, Pecorilla M, Imparato S, et al. Particle radiotherapy for skull base chondrosarcoma: A clinical series from Italian national center for oncological hadrontherapy. Cancers (Basel). (2021) 13:4423. doi: 10.3390/cancers13174423
22. Castro JR, Linstadt DE, Bahary JP, Petti PL, Daftari I, Collier JM, et al. Experience in charged particle irradiation of tumors of the skull base: 1977-1992. Int J Radiat Oncol Biol Phys. (1994) 29:647–55. doi: 10.1016/0360-3016(94)90550-9
23. Noël G, Feuvret L, Ferrand R, Boisserie G, Mazeron JJ, Habrand JL. Radiotherapeutic factors in the management of cervical-basal chordomas and chondrosarcomas. Neurosurgery. (2004) 55:1252–60. doi: 10.1227/01.NEU.0000143330.30405.AA
24. Noël G, Habrand JL, Jauffret E, de Crevoisier R, Dederke S, Mammar H, et al. Radiation therapy for chordoma and chondrosarcoma of the skull base and the cervical spine. Prognostic factors and patterns of failure. Strahlenther Onkol. (2003) 179:241–8. doi: 10.1007/s00066-003-1065-5
25. Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. (2019) 22:153–60. doi: 10.1136/ebmental-2019-300117
26. Rosenberg AE, Nielsen GP, Keel SB, Renard LG, Fitzek MM, Munzenrider JE, et al. Chondrosarcoma of the base of the skull: a clinicopathologic study of 200 cases with emphasis on its distinction from chordoma. Am J Surg Pathol. (1999) 23:1370–8. doi: 10.1097/00000478-199911000-00007
27. Almefty K, Pravdenkova S, Colli BO, AI-Mefty O, Gokden M. Chordoma and chondrosarcoma: similar, but quite different, skull base tumors. Cancer. (2007) 110:2457–67. doi: 10.1002/cncr.23073
28. Bloch OG, Jian BJ, Yang I, Han SJ, Aranda D, Ahn BJ, et al. A systematic review of intracranial Chondrosarcoma and survival. J Clin Neurosci. (2009) 16:1547–51. doi: 10.1016/j.jocn.2009.05.003
29. Bohman LE, Koch M, Bailey RL, Alonso-Basanta M, Lee JY. Skull base chordoma and chondrosarcoma: influence of clinical and demographic factors on prognosis: a SEER analysis. World Neurosurg. (2014) 82:806–14. doi: 10.1016/j.wneu.2014.07.005
30. Brackmann DE, Teufert KB. Chondrosarcoma of the skull base: long-term follow-up. Otol Neurotol. (2006) 27:981–91. doi: 10.1097/01.mao.0000233812.48800.b4
31. Bloch O, Parsa AT. Skull base chondrosarcoma: evidence-based treatment paradigms. Neurosurg. (2013) 24:89–96. doi: 10.1016/j.nec.2012.08.002
32. Nguyen QN, Chang EL. Emerging role of proton beam radiotherapy for chordoma and chondrosarcoma of the skull base. Curr Oncol Rep. (2008) 10:338–43. doi: 10.1007/s11912-008-0052-5
33. Amichetti M, Cisnchetti M, Amelio D, Enrici RM, Minniti G. Proton therapy in Chordoma of the base of the skull: a systematic review. Neurosurg Rev. (2009) 32:403–16. doi: 10.1007/s10143-009-0194-4
34. Takahashi M, Mizumoto M, Oshiro Y, Kino H, Akutsu H, Nakai K, et al. Risk factors for radiation necrosis and local recurrence after proton beam therapy for skull base chordoma or chondrosarcoma. Cancers (Basel). (2023) 15:5687. doi: 10.3390/cancers15235687
35. McDonald MW, Linton OR, Calley CS. Dose-volume relationships associated with temporal lobe radiation necrosis after skull base proton beam therapy. Int J Radiat Oncol Biol Phys. (2015) 91:261–7. doi: 10.1016/j.ijrobp.2014.10.011
36. Andruska N, Kennedy WR, Bonestroo L, Anderson R, Huang Y, Robinson CG, et al. Dosimetric predictors of symptomatic radiation necrosis after five-fraction radiosurgery for brain metastases. Radiother Oncol. (2021) 156:181–7. doi: 10.1016/j.radonc.2020.12.011
Keywords: chondrosarcoma, skull base, proton, meta-analysis, systematic review, temporal lobe necrosis, TRP
Citation: Nakamura M, Mizumoto M, Saito T, Shimizu S, Li Y, Oshiro Y, Inaba M, Hosaka S, Fukushima H, Suzuki R, Iizumi T, Nakai K, Maruo K and Sakurai H (2024) A systematic review and meta-analysis of radiotherapy and particle beam therapy for skull base chondrosarcoma: TRP-chondrosarcoma 2024. Front. Oncol. 14:1380716. doi: 10.3389/fonc.2024.1380716
Received: 02 February 2024; Accepted: 06 March 2024;
Published: 19 March 2024.
Edited by:
François Chevalier, UMR6252 Centre de Recherche sur les Ions, les Matériaux et la Photonique (CIMAP), FranceReviewed by:
Frederic Jungbauer, Heidelberg University, GermanyFrancesco Cuccia, ARNAS Ospedali Civico Di Cristina Benfratelli, Italy
Copyright © 2024 Nakamura, Mizumoto, Saito, Shimizu, Li, Oshiro, Inaba, Hosaka, Fukushima, Suzuki, Iizumi, Nakai, Maruo and Sakurai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Masashi Mizumoto, bWl6dW1vdG9AcG1yYy50c3VrdWJhLmFjLmpw
 Masatoshi Nakamura
Masatoshi Nakamura Masashi Mizumoto
Masashi Mizumoto Takashi Saito1
Takashi Saito1 Shosei Shimizu
Shosei Shimizu Yinuo Li
Yinuo Li Yoshiko Oshiro
Yoshiko Oshiro Kazushi Maruo
Kazushi Maruo