- 1College of Medicine, Tzu Chi University, Hualien, Taiwan
- 2Department of Internal Medicine, Taichung Tzu Chi General Hospital, Taichung, Taiwan
- 3College of Medicine, China Medical University, Taichung, Taiwan
- 4Department of Family Medicine, China Medical University Hospital, Taichung, Taiwan
Objective: Few studies are available on the association between gallstones and metformin use. The objective of the study was to determine whether metformin use is associated with gallstones.
Methods: A population-based retrospective cohort study was conducted using the database of the Taiwan National Health Insurance Program. Subjects of newly diagnosed diabetes mellitus were included from 2002 to 2013. The metformin-exposure group was defined as ≥29 cumulative defined daily dose (DDD) of metformin use. The un-exposure group was defined as <29 cumulative DDD of metformin use. The major endpoint was a new diagnosis of gallstones during the follow-up period. A multivariable Cox proportional hazards regression model was used to evaluate the hazard ratio (HR) and 95% confidence interval (CI) of gallstones associated with metformin use.
Results: After controlling for potential confounders, the adjusted HRs of gallstones were 1.11 (95%CI: 0.84–1.46) for subjects with metformin dosage of 29–180 cumulative DDD, and 0.57 (95%CI: 0.42–0.78) for subjects with metformin dosage >180 cumulative DDD, compared with the un-exposure group.
Conclusion: Long-term use of metformin is associated with reduced risk of gallstones.
Introduction
Diabetes mellitus remains a public health problem in Taiwan due to its high incidence and prevalence, and significant mortality (Liao and Tsai, 2014; Jao et al., 2015; Yang et al., 2017). One epidemiological study using the database of Taiwan National Health Insurance Program has shown that the incidence and the prevalence of diabetes mellitus gradually increased in Taiwan from 2000 to 2008 (Jiang et al., 2012). Overall, the increase of the incidence was 14.6% for women and 29.6% for men from 2000 to 2008 (Jiang et al., 2012). The increase of the prevalence was 56% for women and 74% for men from 2000 to 2008 (Jiang et al., 2012). Diabetes mellitus was the fifth leading cause of death in Taiwan in 2015 (crude mortality rate 40.6/per 100000 persons) (Ministry of Health and Welfare, Taiwan, 2015). Diabetes mellitus has been associated with increased risk of some comorbidities including microvascular and macrovascular complications, and cancer (Bailes, 2002; Pandey et al., 2011; Shikata et al., 2013; Forouhi and Wareham, 2014). One meta-analysis has shown that diabetes mellitus is associated with increased risk of gallbladder disease including gallstones, cholecystectomy, and cholecystitis (relative risk 1.56, 95% CI: 1.26–1.93) (Aune and Vatten, 2016).
Metformin is the first-line medication to treat diabetes mellitus. To date, no large scale study explores the association between gallstones and metformin use. Therefore, a population-based retrospective cohort study was conducted using the database of the Taiwan National Health Insurance Program to explore the association between gallstones and metformin use.
Materials and Methods
Ethics Statement
The Institutional Review Board of Taichung Tzu Chi General Hospital in Taiwan approved the study protocol (REC104-30). Because the identification numbers and personal information of the individuals in the study were not included in the secondary files, the review board waived the need for written consent.
Data Source, Study Design, and Subject Selection
Taiwan is an independent country with more than 23 million people (Li et al., 2015; Lin C.H. et al., 2015; Lin C.J. et al., 2015; Lin T.Y. et al., 2015; Lin Y.J. et al., 2015; Liu J.C. et al., 2015; Liu S.P. et al., 2015; Liu W.H. et al., 2015; Su, 2015; Tien et al., 2015; Wu C.Y. et al., 2015; Wu I.C. et al., 2015; Yao et al., 2015; Yin, 2015; Lai et al., 2017b; Liao et al., 2017b). A population-based retrospective cohort study was conducted using the database from the Taiwan National Health Insurance Program. The database is available to researchers (National Health Insurance Research Database, 2017).
Subjects of newly diagnosed diabetes mellitus (International Classification of Diseases, Ninth Revision, Clinical Modification, ICD-9 code 250) were included from 2002 to 2013. The date for subjects being diagnosed with diabetes mellitus was defined as the index date. Subjects who had a diagnosis of gallstones, or had at least a prescription for metformin before the index date were excluded from the study.
Major Endpoint
It was a new diagnosis of gallstones during the follow-up period.
Comorbid Conditions and Socioeconomic Status
Comorbid conditions and socioeconomic status were included as follows: atrial fibrillation, chronic kidney disease, coronary artery disease, heart failure, hypertension, lipid disorders, socioeconomic status, urbanization, and geographic region of residence. All comorbid conditions were diagnosed based on ICD-9 codes, which have been discussed in previous studies (Hung et al., 2011; Shen et al., 2016; Lai et al., 2017a; Liao et al., 2017a; Lin et al., 2017a,b).
Assessment of Metformin Exposure
The definition of defined daily dose (DDD) was adapted from previous studies as follows (Lu et al., 2005; Yang et al., 2014; Lee et al., 2016). The DDD is regarded as a unit for estimating a prescribed amount of a medication. It is the assumed average daily maintenance dose of a medication prescribed for its major indication in adults. The cumulative DDD, which indicates the exposure duration of a medication, was estimated as the sum of dispensed DDD of metformin to compare its use with the risk of gallstones. The metformin-exposure group was defined as ≥29 cumulative DDD of metformin. The un-exposure group was defined as <29 cumulative DDD of metformin.
Other anti-diabetic medications were included as follows: dipeptidyl peptidase-4 inhibitor, insulin, sulfonylurea, and thiazolidinedione.
Statistical Analysis
SPSS version 19 (SPSS Inc., Chicago, IL, United States) was used for all data analyses. Pearson’s chi-square test was used for categorical variables such as sex, other anti-diabetic medications use, comorbid conditions, socioeconomic status, urbanization, and geographic region of residence. Continuous variables were analyzed using one-way analysis of variance (ANOVA). A multivariable Cox proportional hazards regression model was used to evaluate the hazard ratio (HR) and 95% confidence interval (CI) of gallstones associated with metformin use after adjustment for subject characteristics (including age, sex, other anti-diabetic medications, comorbid conditions, socioeconomic status, urbanization, and geographic region of residence). Statistical significance was set at a two-sided P < 0.05.
Results
Characteristics of the Study Population
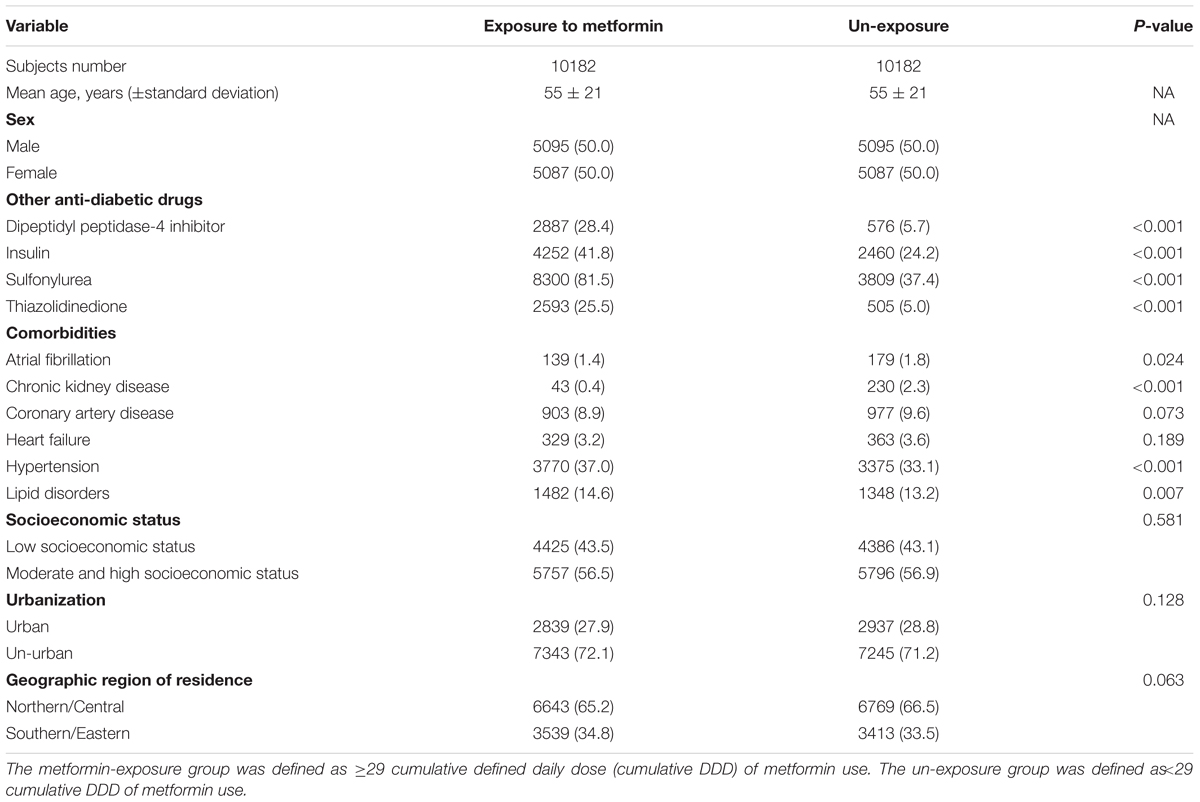
Table 1 reveals the baseline characteristics between the metformin-exposure group and the un-exposure group. The study included 10182 subjects in the metformin-exposure group and 10182 subjects in the un-exposure group, with similar distributions of age and sex. The proportions of other anti-diabetic medications use, hypertension, and lipid disorders were statistically higher in the metformin-exposure group than the un-exposure group (Pearson’s chi-square test, P < 0.05).
Association of Gallstones with Metformin Use
After adjustment for subject characteristics (including age, sex, other anti-diabetic medications, comorbid conditions, socioeconomic status, urbanization, and geographic region of residence), a multivariable Cox proportional hazards regression model revealed that the adjusted HRs of gallstones were 1.11 (95%CI: 0.84–1.46) for subjects with metformin dosage of 29–180 cumulative DDD, and 0.57 (95%CI: 0.42–0.78) for subjects with metformin dosage >180 cumulative DDD, compared with the un-exposure group (Table 2).
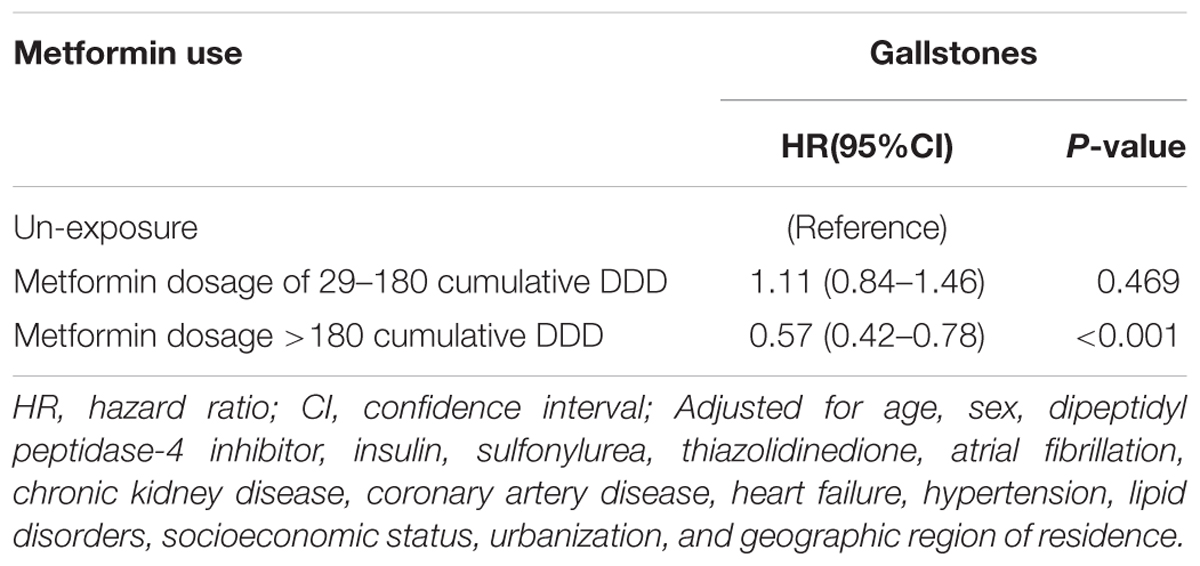
TABLE 2. Hazard ratio (HR) and 95% confidence interval (CI) of gallstones associated with metformin use in a multivariable Cox proportional hazard model.
Discussion
We found that metformin use was associated with reduced risk of gallstones for subjects with metformin dosage >180 cumulative DDD (adjusted HR 0.57, Table 2). However, the HR was 1.11 for subjects with metformin dosage of 29–180 cumulative DDD, without statistic significance. These findings indicate that there is a duration-response relationship between the risk of gallstones and metformin use. That is, the protective effect on gallstones is greater for longer duration of metformin use.
The mechanisms underlying the protective effect of metformin use cannot be fully determined in our observational study. Moreover, De Santis et al.’s (1997) study has shown that the fasting glucose levels and 2-h glucose levels of oral glucose tolerance test were significantly higher in patients with gallstones than those without gallstones. As well known, hemoglobin A1c is an important measure of glycemic control. It has been a better indicator of long-term glycemic control. Al-Bayati and Kodayer’s (2012) study has shown that the prevalence of gallstones was higher among patients with high level of hemoglobin A1c. That is, high glycemic status is associated with a high prevalence of gallstones (De Santis et al., 1997; Al-Bayati and Kodayer, 2012). Therefore, we make a rational explanation that patients with long-term use of metformin could have a good glycemic control, which further reduce the risk of gallstones development. The present study cannot prove this issue because hemoglobin A1c was not recorded due to the inherent limitation of the database. However, it indicates a further research direction on the association between gallstones and hemoglobin A1c levels.
Some limitations should be discussed. Theoretically, we need to test the association between gallstones and medications for comorbidities. It is difficult to conduct such a cohort study which needs to include all concomitant medications for adjustments. The rational step is to test the relative risk of gallstones associated with one potential drug. According to the recommendation of American Diabetes Association (2017) metformin is the first-line medication for patients with type 2 diabetes mellitus. That is why we only included metformin for statistical analysis. However, it indicates a further research direction on the association between gallstones and other concomitant medications.
Some strength should be discussed. To the best of our knowledge, this is the first epidemiological study to explore the association between gallstones and metformin use. This is a unique finding supported by a large database.
Conclusion
We conclude that long-term use of metformin is associated with reduced risk of gallstones. A further research is needed to clarify the association between gallstones and hemoglobin A1c levels.
Author Contributions
K-FL contributed to the conception of the article, participated in the data interpretation, and revised the article. H-YC conducted the data analysis and revised the article. S-WL initiated the draft of the article and revised the article.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This study was supported in part by Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW106-TDU-B-212-113004), China Medical University Hospital, Academia Sinica Taiwan Biobank Stroke Biosignature Project (BM10601010036), Taiwan Clinical Trial Consortium for Stroke (MOST 106-2321-B-039-005), Tseng-Lien Lin Foundation, Taichung, Taiwan, Taiwan Brain Disease Foundation, Taipei, Taiwan, and Katsuzo and Kiyo Aoshima Memorial Funds, Japan. These funding agencies did not influence the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
Al-Bayati, S., and Kodayer, S. (2012). Gallstones in a group of Iraqi patients with type 2 diabetes mellitus. Saudi Med. J. 33, 412–417.
American Diabetes Association (2017). Pharmacologic approaches to glycemic treatment. Diabetes Care 40, S64–S74. doi: 10.2337/dc17-S011
Aune, D., and Vatten, L. J. (2016). Diabetes mellitus and the risk of gallbladder disease: a systematic review and meta-analysis of prospective studies. J. Diabetes Complications 30, 368–373. doi: 10.1016/j.jdiacomp.2015.11.012
Bailes, B. K. (2002). Diabetes mellitus and its chronic complications. AORN J. 76, 266–276. doi: 10.1016/S0001-2092(06)61065-X
De Santis, A., Attili, A. F., Ginanni Corradini, S., Scafato, E., Cantagalli, A., De Luca, C., et al. (1997). Gallstones and diabetes: a case-control study in a free-living population sample. Hepatology 25, 787–790. doi: 10.1002/hep.510250401
Forouhi, N. G., and Wareham, N. J. (2014). Epidemiology of diabetes. Medicine 42, 698–702. doi: 10.1016/j.mpmed.2014.09.007
Hung, S. C., Liao, K. F., Lai, S. W., Li, C. I., and Chen, W. C. (2011). Risk factors associated with symptomatic cholelithiasis in Taiwan: a population-based study. BMC Gastroenterol. 11:111. doi: 10.1186/1471-230X-11-111
Jao, C. L., Hung, C. C., Tung, Y. S., Lin, P. Y., Chen, M. C., and Hsu, K. C. (2015). The development of bioactive peptides from dietary proteins as a dipeptidyl peptidase IV inhibitor for the management of type 2 diabetes. Biomedicine 5, 14. doi: 10.7603/s40681-015-0014-9
Jiang, Y. D., Chang, C. H., Tai, T. Y., Chen, J. F., and Chuang, L. M. (2012). Incidence and prevalence rates of diabetes mellitus in Taiwan: analysis of the 2000-2009 Nationwide Health Insurance database. J. Formos. Med. Assoc. 111, 599–604. doi: 10.1016/j.jfma.2012.09.014
Lai, S. W., Lin, C. L., and Liao, K. F. (2017a). Population-based cohort study investigating the correlation of diabetes mellitus with pleural empyema in adults in Taiwan. Medicine 96:e7763. doi: 10.1097/MD.0000000000007763
Lai, S. W., Lin, C. L., and Liao, K. F. (2017b). Risk of contracting pneumonia among patients with predialysis chronic kidney disease: a population-based cohort study in Taiwan. Biomedicine 7:20. doi: 10.1051/bmdcn/2017070320
Lee, S. S., Yang, Y. W., Tsai, T. H., Kuo, Y. H., Chuang, H. Y., Lee, C. C., et al. (2016). 5-alpha-reductase inhibitors and the risk of diabetes mellitus: a nationwide population-based study. Prostate 76, 41–47. doi: 10.1002/pros.23097
Li, T. C., Li, C. I., Liao, L. N., Liu, C. S., Yang, C. W., Lin, C. H., et al. (2015). Associations of EDNRA and EDN1 polymorphisms with carotid intima media thickness through interactions with gender, regular exercise, and obesity in subjects in Taiwan: Taichung Community Health Study (TCHS). Biomedicine 5:8. doi: 10.7603/s40681-015-0008-7
Liao, K. F., Cheng, K. C., Lin, C. L., and Lai, S. W. (2017a). Etodolac and the risk of acute pancreatitis. Biomedicine 7:4. doi: 10.1051/bmdcn/2017070104
Liao, K. F., Huang, P. T., Lin, C. C., Lin, C. L., and Lai, S. W. (2017b). Fluvastatin use and risk of acute pancreatitis: a population-based case-control study in Taiwan. Biomedicine 7:17. doi: 10.1051/bmdcn/2017070317
Liao, W. L., and Tsai, F. J. (2014). Personalized medicine in Type 2 Diabetes. Biomedicine 4:8. doi: 10.7603/s40681-014-0008-z
Lin, C. H., Li, T. C., Tsai, P. P., and Lin, W. C. (2015). The relationships of the pulmonary arteries to lung lesions aid in differential diagnosis using computed tomography. Biomedicine 5:11. doi: 10.7603/s40681-015-0011-z
Lin, C. J., Lai, C. K., Kao, M. C., Wu, L. T., Lo, U. G., Lin, L. C., et al. (2015). Impact of cholesterol on disease progression. Biomedicine 5, 7. doi: 10.7603/s40681-015-0007-8
Lin, T. Y., Fan, C. W., Maa, M. C., and Leu, T. H. (2015). Lipopolysaccharide-promoted proliferation of Caco-2 cells is mediated by c-Src induction and ERK activation. Biomedicine 5, 5. doi: 10.7603/s40681-015-0005-x
Lin, Y. J., Ho, T. J., Lin, T. H., Hsu, W. Y., Huang, S. M., Liao, C. C., et al. (2015). P-coumaric acid regulates exon 12 splicing of the ATP7B gene by modulating hnRNP A1 protein expressions. Biomedicine 5, 10. doi: 10.7603/s40681-015-0010-0
Lin, H. F., Liao, K.-F., Chang, C.-M., Lin, C.-L., and Lai, S.-W. (2017a). Population-based cohort study examining the association between splenectomy and empyema in adults in Taiwan. BMJ Open 7:e015101. doi: 10.1136/bmjopen-2016-015101
Lin, H. F., Liao, K. F., Chang, C. M., Lin, C. L., and Lai, S. W. (2017b). Correlation between proton pump inhibitors and risk of pyogenic liver abscess. Eur. J. Clin. Pharmacol. 73, 1019–1025. doi: 10.1007/s00228-017-2256-9
Liu, J. C., Shen, W. C., Shih, T. C., Tsai, C. W., Chang, W. S., Cho, D. Y., et al. (2015). The current progress and future prospects of personalized radiogenomic cancer study. Biomedicine 5:2. doi: 10.7603/s40681-015-0002-0
Liu, S. P., Hsu, C. Y., Fu, R. H., Huang, Y. C., Chen, S. Y., Lin, S. Z., et al. (2015). Sambucus williamsii induced embryonic stem cells differentiated into neurons. Biomedicine 5, 3. doi: 10.7603/s40681-015-0003-z
Liu, W. H., Liu, T. C., and Mong, M. C. (2015). Antibacterial effects and action modes of asiatic acid. Biomedicine 5, 16. doi: 10.7603/s40681-015-0016-7
Lu, C. L., Lang, H. C., Chang, F. Y., Chen, T. J., Chen, C. Y., Luo, J. C., et al. (2005). Social and medical impact, sleep quality and the pharmaceutical costs of heartburn in Taiwan. Aliment. Pharmacol. Ther. 22, 739–747. doi: 10.1111/j.1365-2036.2005.02664.x
Ministry of Health and Welfare, Taiwan (2015). Statistics of Causes of Death. Available at: http://www.mohw.gov.tw/EN/Ministry/Index.aspx [accessed August 1, 2017].
National Health Insurance Research Database (2017). Taiwan. Available at: http://nhird.nhri.org.tw/en/index.html [August 1, 2017].
Pandey, A., Forte, V., Abdallah, M., Alickaj, A., Mahmud, S., Asad, S., et al. (2011). Diabetes mellitus and the risk of cancer. Minerva Endocrinol. 36, 187–209.
Shen, M. L., Liao, K. F., Tsai, S. M., Lin, C. L., and Lai, S. W. (2016). Herpes zoster correlates with pyogenic liver abscesses in Taiwan. Biomedicine 6, 22.
Shikata, K., Ninomiya, T., and Kiyohara, Y. (2013). Diabetes mellitus and cancer risk: review of the epidemiological evidence. Cancer Sci. 104, 9–14. doi: 10.1111/cas.12043
Su, K. P. (2015). Nutrition, psychoneuroimmunology and depression: the therapeutic implications of omega-3 fatty acids in interferon-alpha-induced depression. Biomedicine 5:21. doi: 10.7603/s40681-015-0021-x
Tien, N., Sung, Y. J., Chang, Y. C., You, B. J., Liang, M., Lim, Y. P., et al. (2015). The medical diagnostic approaches with phylogenetic analysis for rare Brucella spp. diagnosis in Taiwan. Biomedicine 5:9. doi: 10.7603/s40681-015-0009-6
Wu, C. Y., Huang, H. M., and Cho, D. Y. (2015). An acute bleeding metastatic spinal tumor from HCC causes an acute onset of cauda equina syndrome. Biomedicine 5:18. doi: 10.7603/s40681-015-0018-5
Wu, I. C., Lin, C. C., and Hsiung, C. A. (2015). Emerging roles of frailty and inflammaging in risk assessment of age-related chronic diseases in older adults: the intersection between aging biology and personalized medicine. Biomedicine 5:1. doi: 10.7603/s40681-015-0001-1
Yang, J. S., Lu, C. C., Kuo, S. C., Hsu, Y. M., Tsai, S. C., Chen, S. Y., et al. (2017). Autophagy and its link to type II diabetes mellitus. Biomedicine 7:8. doi: 10.1051/bmdcn/2017070201
Yang, Y. W., Hsieh, T. F., Yu, C. H., Huang, Y. S., Lee, C. C., and Tsai, T. H. (2014). Zolpidem and the risk of Parkinson’s disease: a nationwide population-based study. J. Psychiatr. Res. 58, 84–88. doi: 10.1016/j.jpsychires.2014.07.003
Yao, H. T., Yang, Y. C., Chang, C. H., Yang, H. T., and Yin, M. C. (2015). Protective effects of (-)-epigallocatechin-3-gallate against acetaminophen-induced liver injury in rats. Biomedicine 5:15. doi: 10.7603/s40681-015-0015-8
Keywords: diabetes mellitus, gallstones, metformin, Taiwan, National Health Insurance Program
Citation: Liao K-F, Chuang H-Y and Lai S-W (2017) Metformin Use Correlates with Reduced Risk of Gallstones in Diabetic Patients: A 12-Year Follow-up Study. Front. Pharmacol. 8:765. doi: 10.3389/fphar.2017.00765
Received: 30 August 2017; Accepted: 11 October 2017;
Published: 24 October 2017.
Edited by:
Jean-Paul Deslypere, Besins Healthcare, ThailandCopyright © 2017 Liao, Chuang and Lai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shih-Wei Lai, d2VpQG1haWwuY211aC5vcmcudHc=
 Kuan-Fu Liao
Kuan-Fu Liao Hsun-Yang Chuang
Hsun-Yang Chuang Shih-Wei Lai
Shih-Wei Lai