Abstract
Background: A left ventricular (LV) thrombus is detected in approximately 5–10% of patients after myocardial infarction (MI). If left untreated, these LV thrombi carry a significant risk of complications including embolic stroke. According to current guidelines, anticoagulation with vitamin K antagonists (VKA) is recommended to treat a LV thrombus.
Case presentation: An 87 year old patient was referred to our department with non ST-elevation MI. Five months before, he had been diagnosed with a subacute ST elevation MI, which had been treated conservatively. Recently, a rectal neoplasia had been diagnosed, but not operated yet. The patient underwent coronary angiography with implantation of two drug eluting stents (Cre8) requiring dual antiplatelet therapy. During ventriculography an apical LV thrombus of 16 mm diameter was detected. Due to the high bleeding risk in this patient, VKA therapy with potentially fluctuating international normalized ratio (INR) values was considered unsuitable. Therefore, dabigatran at a dose of 110 mg bid was chosen as anticoagulation therapy. After 4 weeks, cardiac computed tomography was performed, which failed to detect the LV thrombus described previously. Notably, triple therapy with dabigatran, clopidogrel, and aspirin was well tolerated without evidence for bleeding. The surgical resection of the rectal neoplasm was performed 2 months later without bleeding complications.
Discussion: Anticoagulation is effective in patients with MI and a LV thrombus in reducing the risk of embolization and in dissolving the thrombus. Our case is complex due to the required triple therapy, very old age and significant bleeding risk of our patient due to the rectal neoplasia. Although only few reports are available for the use of non VKA oral anticoagulants (NOAC) in this indication, we chose dabigatran at a dose of 110 mg bid added to dual antiplatelet therapy for our patient. Besides the advantage of a predictable pharmacokinetic profile of NOAC in contrast to VKA, the effect of dabigatran can rapidly be reversed by idaruzicumab in the case of severe bleeding.
Conclusion remarks: Physicians should carefully weigh the risk of thromboembolic events versus the risk of bleeding when combining antiplatelet with anticoagulation therapy.
Introduction
An 87 year old patient was referred to our department with a non-ST-elevation myocardial infarction (MI). Five months before, he had been diagnosed with a subacute ST elevation MI, which had been treated conservatively. His medical history included a transient ischemic attack with subsequent endarterectomy in 2007, an infrarenal aortic aneurysm (max diameter 3, 6 cm) as well as arterial hypertension and diabetes mellitus type II. Shortly before this event, copidogrel, and aspirin had been interrupted due to a planned operation of a newly diagnosed rectal carcinoma.
Background
The formation of a left ventricular (LV) thrombus is not an unusual finding in patients with MI. In the literature, different frequencies of LV thrombi after MI have been reported. Solheim et al. described a frequency of 15% in the first 3 months after anterior wall MI (Solheim et al., 2010). Zielinska et al. demonstrated an incidence of 2.5% in patients with an acute MI (Zielinska et al., 2008). Recent reviews state the incidence of LV thrombus formation after ST-elevation MI to be approximately 5–10%. Due to more aggressive anticoagulation therapies in the acute phase and improved LV remodeling, the incidence of LV thrombi appears to be declining (Delewi et al., 2012). Presently, only a few case reports are available on the use of new oral anticoagulants (NOAC) in the literature.
Diagnosis
Due to the diagnosed non-ST-elevation MI coronary angiography was performed. The exam showed a proximal occlusion of the left anterior descending (LAD) artery and significant (80%) stenosis of the circumflex (CX) artery (Farooq et al., 2012), which were treated by implantation of two polymer-free drug eluting stents (DES) (Cre8 3 × 25 mm into the LAD, Cre8 3.6 × 16 mm into the CX) (Figure 1).
Figure 1
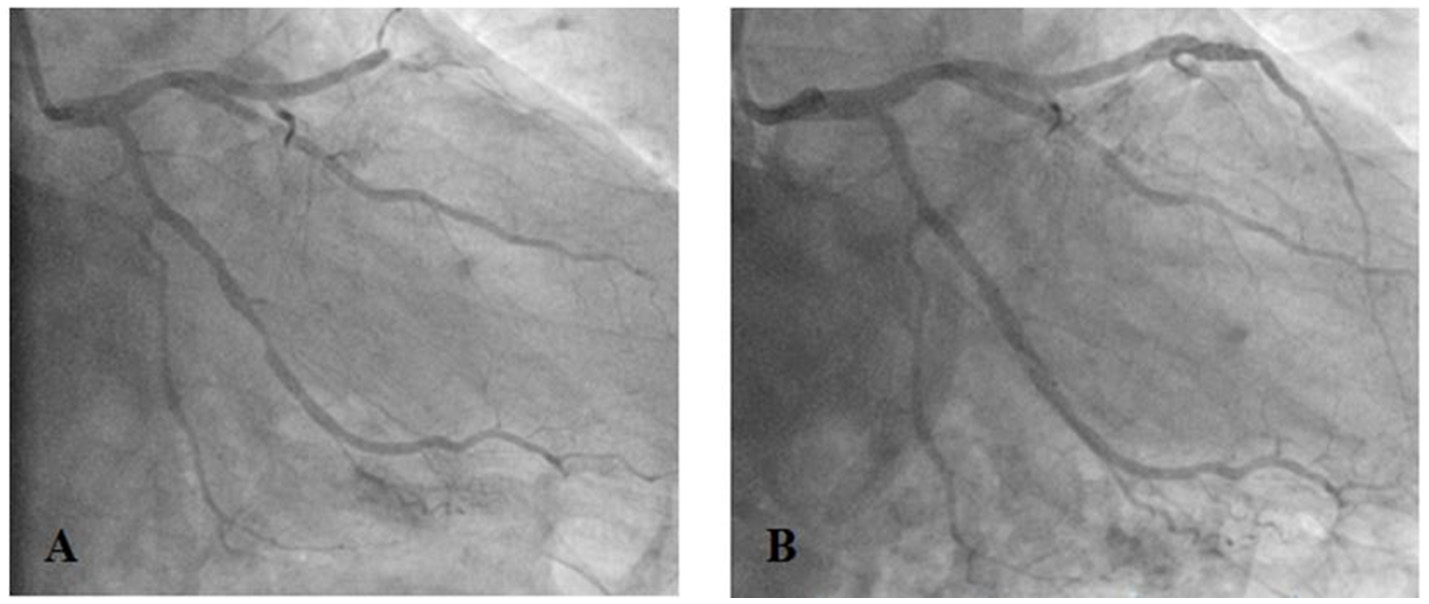
Proximal occlusion of the left anterior descending artery (LAD) and significant (80%) stenosis of the circumflex artery (CX) (A) treated by implantation of drug eluting stents (Cre8 3 × 25 mm into the LAD, Cre8 3.6 × 16 mm into the CX) (B).
Ventriculography showed a moderately reduced global LV function (ejection fraction of 40%) with apical and septal akinesia. In addition, a thrombus (16 mm diameter) was clearly visualized in the apical part of the left ventricle (Figure 2).
Figure 2
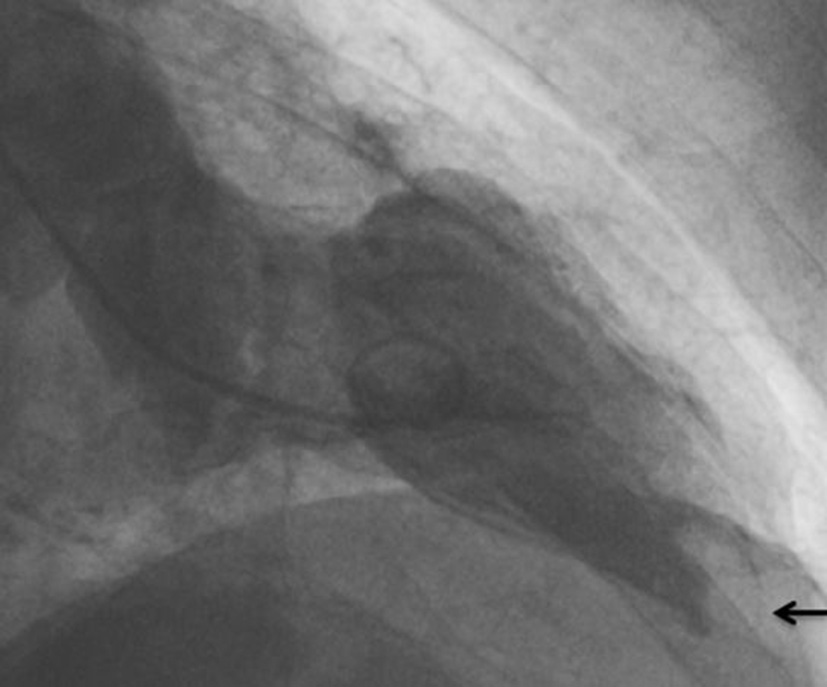
Thrombus (arrow) in the apical part of the left ventricle as demonstrated by ventriculography.
Treatment
Due to the acute coronary syndrome (ACS) with implantation of two DES, dual antiplatelet therapy (clopidogrel 75 mg and aspirin 100 mg) was started. In addition, oral anticoagulation therapy had to be initiated to treat the detected thrombus in the left ventricle. Because of the high bleeding risk in this patient with a newly diagnosed, not yet operated rectal neoplasia, vitamin K antagonist (VKA) therapy with potentially fluctuating international normalized ratio (INR) values was considered unsuitable. Therefore, dabigatran was chosen as anticoagulation therapy. Since the patient showed slightly reduced renal function parameters (creatinine clearance 58 ml/min/1.73 m2, creatinine 1.18 mg/dl) the reduced dose of dabigatran (of 110 mg bid) was used.
After 4 weeks, the patient was seen again in our outpatient clinic. Notably, triple therapy with dabigatran, clopidogrel, and aspirin had been well tolerated without evidence for significant bleeding. At this time, a cardiac computed tomography was performed, which failed to detect the LV thrombus described previously (Figure 3). Consequently, dabigatran therapy was stopped and dual antiplatelet therapy was continued for another 2 months. The patient was then switched to aspirin monotherapy and the surgical resection of the rectal neoplasm was performed in a peripheral hospital without any bleeding complications and stable hemoglobin values during and after the surgical resection.
Figure 3

Cardiac computed tomography of the left ventricle vertical view (A) and four chamber view (B) without any evidence for a left ventricular thrombus after 4 weeks.
Discussion
If left untreated, a LV thrombus may lead to devastating complications, most notably embolic stroke. The risk of embolization in patients who are not treated with anticoagulant therapy is between 10 and 15%. Most embolic events occur within the first 3–4 months (Stratton and Resnick, 1987). Patients with MI and LV thrombus treated with anticoagulation therapy have a better outcome due to the reduced risk of embolic events (Vaitkus and Barnathan, 1993).
Due to the lack of data from clinical studies for NOAC in the treatment of LV thrombi, VKA therapy is usually initiated in these patients. VKA have been used for atrial and ventricular thrombi (Nagamoto et al., 2014). Nieman et al. reported that anticoagulation with warfarin therapy can resolve fresh thrombi, but not chronic ventricular thrombi after MI (Niemann et al., 2012). However, several case reports have shown the feasibility of NOAC treatment of LV thrombi with dabigatran (Kaku, 2013; Nagamoto et al., 2014; Chung et al., 2015; Kolekar et al., 2015; Ohashi et al., 2015) or factor Xa inhibitors (Nakasuka et al., 2014; Padilla Pérez et al., 2014; Kaya et al., 2016; Makrides, 2016; Mano et al., 2016; Berry et al., 2017; Seecheran et al., 2017; Smetana et al., 2017). In the cases describing dabigatran to resolve LV thrombi, the doses varied between 110 and 150 mg bid and the resolution of the thrombi was confirmed after 3 weeks to 4 months (Hori et al., 2013).
The European Society of Cardiology—(ESC) Guidelines of 2014 recommend the use of new-generation DES over BMS (bare metal stents) (European Heart Rhythm et al., 2010), because of their lower rate of restenosis-and stent thrombosis (Lip et al., 2014). The risk for stent thrombosis is highest in the first months after stent implantation and dual antiplatelet therapy is recommended for at least 4 weeks (Levine et al., 2011).
Our case is particularly complex and unusual because of the required triple therapy, very old age and significant bleeding risk of our patient due to the newly diagnosed rectal carcinoma. Therefore, we considered VKA therapy for this patient with potentially fluctuating INR values unsuitable. We chose dabigatran due to the high bleeding risk of our patient and the availability of an efficient antidote (idarucizumab), which had shown rapid and complete reversion of the anticoagulant activity of dabigatran in the RE-VERSE AD study (Pollack et al., 2015). Only few cases have been reported in the literature where triple therapy was used to resolve a LV thrombus with Factor Xa inhibitors (Makrides, 2016; Mano et al., 2016; Berry et al., 2017; Seecheran et al., 2017; Smetana et al., 2017) or dabigatran (Chung et al., 2015; Ohashi et al., 2015). In contrast to these described cases, apparent development of a LV thrombus under dabigatran treatment has been published recently (Adar et al., 2018).
For patients requiring NOAC therapy in combination with clopidogrel and/ or low-dose aspirin, the ESC-Guidelines recommend the use of the lower dose of the NOAC, in the case of dabigatran 110 bid (Connolly et al., 2009). Therefore, and due to the considerable bleeding risk, we used dabigatran in the lower dose (110 mg bid) for our patient.
However, similar as VKA, combination of dabigatran with dual antiplatelet therapy carries an increased risk of major bleeding (Dans et al., 2013; Oldgren et al., 2013).
The RE-DEEM study showed a dose depending bleeding risk for dabigatran in combination with dual antiplatelet therapy. The addition of dabigatran to dual antiplatelet therapy in patients with recent ACS showed a reduction in major adverse cardiovascular events but an essential increase in bleeding compared to dual and single antiplatelet therapy alone (Oldgren et al., 2011).
The recently published RE-DUAL-PCI-Study represents an additional option in patients with risk of bleeding and thromboembolic events. This study showed a lower risk of bleeding and equal risk of thromboembolic events using dual therapy in patients with atrial fibrillation after percutaneous coronary intervention (PCI) with dabigatran (110 or 150 mg twice daily) and a P2Y12 inhibitor (clopidogrel or ticagrelor) compared to triple therapy with warfarin plus a P2Y12 inhibitor (clopidogrel or ticagrelor) and aspirin (for 1–3 months) (Cannon et al., 2017).
Concluding remarks
Physician should carefully weigh the risk of thromboembolic events versus the risk of bleeding when combining antiplatelet with antithrombotic therapy.
Statements
Ethics statement
The study is a case report describing routine treatment of a single patient and is therefore exempt from ethical approval procedures.
Author contributions
MN: Drafting the work, analysis and interpretation of data for the work, final approval of the version to be published, agreement to be accountable for all aspects of the work. NM: Performing the coronary angiography of the patient, final approval of the version to be published, agreement to be accountable for all aspects of the work, revising the work critically for important intellectual content. E-MG: Analysis and interpretation of the CT-Images, final approval of the version to be published, agreement to be accountable for all aspects of the work, revising the work critically for important intellectual content. PM: Analysis and interpretation of data for the work, final approval of the version to be published, agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work, revising the work critically for important intellectual content.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
- bid
bis in die, twice a day
- BMS
bare metal stent
- cm
centimeters
- CX
circumflex artery
- DES
drug eluting stent
- Dl
decilitres
- ESC
European Society of Cardiology
- et al.
and others
- Fig
figure
- INR
international normalized ratio
- LAD
left anterior descending
- LV
left ventricular
- m2
square meters
- mm
millimeters
- mg
milligrams
- MI
myocardial infarction
- min
minutes
- ml
milliliters
- NOAC
new oral anticoagulants
- VKA
vitamin K antagonist
- PCI
percutaneous coronary intervention.
Abbreviations
References
1
AdarA.OnalanO.CakanF. (2018). Newly developed left ventricular apical thrombus under dabigatran treatment. Blood Coagul. Fibrinolysis29, 126–128. 10.1097/MBC.0000000000000671
2
BerryA.BrancheauD.ZughaibM. (2017). Rapid resolution of left ventricular thrombus with apixaban therapy. SAGE Open Med. Case Rep.5:2050313X17745211. 10.1177/2050313X17745211
3
CannonC. P.BhattD. L.OldgrenJ.LipG. Y. H.EllisS. G.KimuraT.et al. (2017). Dual antithrombotic therapy with dabigatran after PCI in atrial fibrillation. New Engl. J. Med. 377, 1513–1524. 10.1056/NEJMoa1708454
4
ChungK.PaekY. M.LeeH. J.HongK. S. (2015). Dabigatran effect on left ventricular thrombus in a patient with acute ischemic stroke. J Stroke17, 366–368. 10.5853/jos.2015.17.3.366
5
ConnollyS. J.EzekowitzM. D.YusufS.EikelboomJ.OldgrenJ.ParekhA.et al. (2009). Dabigatran versus warfarin in patients with atrial fibrillation. N. Engl. J. Med.361, 1139–1151. 10.1056/NEJMoa0905561
6
DansA. L.ConnollyS. J.WallentinL.YangS.NakamyaJ.BrueckmannM.et al. (2013). Concomitant use of antiplatelet therapy with dabigatran or warfarin in the randomized evaluation of Long-Term Anticoagulation Therapy (RE-LY) trial. Circulation127, 634–640. 10.1161/CIRCULATIONAHA.112.115386
7
DelewiR.ZijlstraF.PiekJ. J. (2012). Left ventricular thrombus formation after acute myocardial infarction. Heart98, 1743–1749. 10.1136/heartjnl-2012-301962
8
European Heart RhythmA.European Association for Cardio-ThoracicS.CammA. J.KirchhofP.LipG. Y.SchottenU.et al. (2010). Guidelines for the management of atrial fibrillation: the task force for the management of atrial fibrillation of the European Society of Cardiology (ESC). Eur. Heart J.31, 2369–2429. 10.1093/eurheartj/ehq278
9
FarooqV.VergouweY.RäberL.VrancxP.GarciaH.BrugalettaS.et al. (2012). Combined anatomical and clinical factors for the risk stratification of patients undergoing percutaneous coronary intervention: the logistic clinical syntax score. J. Am. Coll. Cardiol.59, 3098–3104. 10.1016/S0735-1097(12)61375-8
10
HoriM.ConnollyS. J.ZhuJ.LiuL. S.LauC. P.PaisP.et al. (2013). Dabigatran versus warfarin effects on ischemic and hemorrhagic strokes and bleeding in Asians and non-Asians with atrial fibrillation. Stroke44:1891. 10.1161/STROKEAHA.113.000990
11
KakuB. (2013). Intra-cardiac thrombus resolution after anti-coagulation therapy with dabigatran in a patient with mid-ventricular obstructive hypertrophic cardiomyopathy: a case report. J. Med. Case Rep.7:238. 10.1186/1752-1947-7-238
12
KayaA.HayirogluM. I.KeskinM.TekkeşinA. I.AlperA. T. (2016). Resolution of left ventricular thrombus with apixaban in a patient with hypertrophic cardiomyopathy. Turk Kardiyol. Dern. Ars.44, 335–337. 10.5543/tkda.2015.68054
13
KolekarS.MunjewarC.SharmaS. (2015). Dabigatran for left ventricular thrombus. Indian Heart J.67, 495–496. 10.1016/j.ihj.2015.06.010
14
LevineG. N.BatesE. R.BlankenshipJ. C.BaileyS. R.BittlJ. A.CercekB.et al. (2011) ACCF/AHA/SCAI Guideline for percutaneous coronary intervention. a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines the society for cardiovascular angiography interventions. J. Am. College Cardiol. 58:e44–e122. 10.1161/CIR.0b013e31823ba622
15
LipG. Y.WindeckerS.HuberK.KirchhofP.MarinF.Ten BergJ. M.et al. (2014). Management of antithrombotic therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous coronary or valve interventions: a joint consensus document of the European Society of Cardiology Working Group on thrombosis, European Heart Rhythm Association (EHRA), European Association of Percutaneous Cardiovascular Interventions (EAPCI) and European Association of Acute Cardiac Care (ACCA) endorsed by the Heart Rhythm Society (HRS) and Asia-Pacific Heart Rhythm Society (APHRS). Eur. Heart J.35, 3155–3179. 10.1093/eurheartj/ehu298
16
MakridesC. A. (2016). Resolution of left ventricular postinfarction thrombi in patients undergoing percutaneous coronary intervention using rivaroxaban in addition to dual antiplatelet therapy. BMJ Case Rep.2016:bcr201621784. 10.1136/bcr-2016-217843
17
ManoY.KoideK.SukegawaH.KodairaM.OhkiT. (2016). Successful resolution of a left ventricular thrombus with apixaban treatment following acute myocardial infarction. Heart Vessels31, 118–123. 10.1007/s00380-014-0562-z
18
NagamotoY.ShiomiT.MatsuuraT.OkaharaA.TakegamiK.MineD.et al. (2014). Resolution of a left ventricular thrombus by the thrombolytic action of dabigatran. Heart Vessels9, 560–562. 10.1007/s00380-013-0403-5
19
NakasukaK.ItoS.NodaT.HasuoT.SekimotoS.OhmoriH.et al. (2014). Resolution of left ventricular thrombus secondary to tachycardia-induced heart failure with rivaroxaban. Case Rep. Med.2014:814524. 10.1155/2014/814524
20
NiemannM.GaudronP. D.BijnensB.StörkS.BeerM.HillenbrandH.et al. (2012). Differentiation between fresh and old left ventricular thrombi by deformation imaging. Circ-Cardiovasc. Imag.5, 667–675. 10.1161/CIRCIMAGING.112.974964
21
OhashiN.OkadaT.UchidaM.AmiokaM.FujiwaraM.KasedaS. (2015). Effects of dabigatran on the resolution of left ventricular thrombus after acute myocardial infarction. Intern. Med.54, 1761–1763. 10.2169/internalmedicine.54.4191
22
OldgrenJ.BudajA.GrangerC. B.KhderY.RobertsJ.SiegbahnA.et al. (2011). Dabigatran vs. placebo in patients with acute coronary syndromes on dual antiplatelet therapy: a randomized, double-blind, phase II trial. Eur.Heart J.32, 2781–2789. 10.1093/eurheartj/ehr113
23
OldgrenJ.WallentinL.AlexanderJ. H.JamesS.JönelidB.StegG.et al. (2013). New oral anticoagulants in addition to single or dual antiplatelet therapy after an acute coronary syndrome: a systematic review and meta-analysis. Eur. Heart J.4, 1670–1680. 10.1093/eurheartj/eht049
24
Padilla PérezM.Salas BravoD.Garcelán TrigoJ. A.Vazquez Ruiz de CastroviejoE.Torres LlergoJ.Lozano CabezasC.et al. (2014). Resolution of left ventricular thrombus by rivaroxaban. Future Cardiol.10, 333–336. 10.2217/fca.14.12
25
PollackC. V.Jr.ReillyP. A.EikelboomJ.GlundS.VerhammeP.BernsteinR. A.et al. (2015). Idarucizumab for dabigatran reversal. N. Engl. J. Med.373, 511–520. 10.1056/NEJMoa1502000
26
SeecheranR.SeecheranV.PersadS.SeecheranN. A. (2017). Rivaroxaban as an antithrombotic agent in a patient with ST-segment elevation myocardial infarction and left ventricular thrombus: a case report. J. Investig. Med. High Impact Case Rep.510.1177/2324709617697991
27
SmetanaK. S.DunneJ.ParrottK.DavisG. A.CollierA. C. S.CovellM.et al. (2017). Oral factor Xa inhibitors for the treatment of left ventricular thrombus: a case series. J. Thromb. Thrombolysis44, 519–524. 10.1007/s11239-017-1560-7
28
SolheimS.SeljeflotI.LundeK.BjørnerheimR.AakhusS.ForfangK.et al. (2010). Frequency of left ventricular thrombus in patients with anterior wall acute myocardial infarction treated with percutaneous coronary intervention and dual antiplatelet therapy. Am. J. Cardiol.106, 1197–1200. 10.1016/j.amjcard.2010.06.043
29
StrattonJ. R.ResnickA. D. (1987). Increased embolic risk in patients with left-ventricular thrombi. Circulation75, 1004–1011. 10.1161/01.CIR.75.5.1004
30
VaitkusP. T.BarnathanE. S. (1993). Embolic potential, prevention and management of mural thrombus complicating anterior myocardial-infarction - a metaanalysis. J. Am. Coll. Cardiol.22, 1004–1009. 10.1016/0735-1097(93)90409-T
31
ZielinskaM.KaczmarekK.TylkowskiM. (2008). Predictors of left ventricular thrombus formation in acute myocardial infarction treated with successful primary angioplasty with stenting. Am. J. Med. Sci.35, 171–176. 10.1097/MAJ.0b013e318142be20
Summary
Keywords
triple therapy, left ventricular thrombus, myocardial infarction, high bleeding risk, anticoagulation therapy, rectal neoplasms
Citation
Noflatscher M, Moes N, Gassner E-M and Marschang P (2018) Dabigatran Added to Dual Antiplatelet Therapy to Treat a Left Ventricular Thrombus in an 87 Year Old Patient With Myocardial Infarction and Very High Bleeding Risk. Front. Pharmacol. 9:217. doi: 10.3389/fphar.2018.00217
Received
17 October 2017
Accepted
27 February 2018
Published
04 April 2018
Volume
9 - 2018
Edited by
Pedro D'Orléans-Juste, Université de Sherbrooke, Canada
Reviewed by
Claudio de Lucia, Temple University, United States; Sang-Hyun Kim, Seoul Boramae Hospital, South Korea
Updates
Copyright
© 2018 Noflatscher, Moes, Gassner and Marschang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maria Noflatscher maria.noflatscher@i-med.ac.at
This article was submitted to Cardiovascular and Smooth Muscle Pharmacology, a section of the journal Frontiers in Pharmacology
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.