- Department of Internal Medicine II, Division of Gastroenterology and Hepatology, Klinikum Hanau, Academic Teaching Hospital of the Medical Faculty, Goethe University Frankfurt, Germany
One of the most difficult challenges in clinical hepatology is the diagnosis of a drug-induced liver injury (DILI). The timing of the events, exclusion of alternative causes, and taking into account the clinical context should be systematically assessed and scored in a transparent manner. RUCAM (Roussel Uclaf Causality Assessment Method) is a well-established diagnostic algorithm and scale to assess causality in patients with suspected DILI. First published in 1993 and updated in 2016, RUCAM is now the worldwide most commonly used causality assessment method (CAM) for DILI. The following manuscript highlights the recent implementation of RUCAM around the world, by reviewing the literature for publications that utilized RUCAM, and provides a review of “best practices” for the use of RUCAM in cases of suspected DILI. The worldwide appreciation of RUCAM is substantiated by the current analysis of 46,266 DILI cases, all tested for causality using RUCAM. These cases derived from 31 reports published from 2014 to early 2019. Their first authors came from 10 countries, with China on top, followed by the US, and Germany on the third rank. Importantly, all RUCAM-based DILI reports were published in high profile journals. Many other reports were published earlier from 1993 up to 2013 in support of RUCAM. Although most of the studies were of high quality, the current case analysis revealed shortcomings in few studies, not at the level of RUCAM itself but rather associated with the work of the users. To ensure in future DILI cases a better performance by the users, a list of essential elements is proposed. As an example, all suspected DILI cases should be evaluated 1) by the updated RUCAM to facilitate result comparisons, 2) according to a prospective study protocol to ensure complete data sets, 3) after exclusion of cases with herb induced liver injury (HILI) from a DILI cohort to prevent confounding variables, and 4) according to inclusion of DILI cases with RUCAM-based causality gradings of highly probable or probable, in order to increase the specificity of the results. In conclusion, RUCAM benefits from its high appreciation and performs well provided the users adhere to published recommendations to prevent confounding variability.
Introduction
Consensus exists that patients with suspected DILI (drug-induced liver injury) require a valid diagnosis, which is emphasized also in conclusions summarized after careful analysis of the DILI case highlights published in the last years and discussed in original publications or editorials (Teschke and Andrade, 2015; Danan and Teschke, 2016; Sarges et al., 2016; Shahbaz et al., 2017; Teschke and Danan, 2017a; Real et al., 2019; Teschke, 2018a; Danan and Teschke, 2019). The first publication of the Roussel Uclaf Causality Assessment Method (RUCAM) in 1993 and its implementation in clinical routine substantially improved the causality assessment in cases of suspected DILI. This improvement and success were essentially achieved by switching from the previously used, not transparent, and vague global introspection approach to a robust, transparent, and quantitative tool providing well-defined causality gradings, which were based on the sum of individually scoring key elements. The details were recently summarized in the presentation of the updated RUCAM version (Danan and Teschke, 2016). The numerous advantages of RUCAM over alternative attempts of causality assessment methods (CAMs) explain why RUCAM is still in use for the last 25 years with continuously increased international acceptance, applicable in suspected cases of DILI and HILI (herb induced liver injury) (Danan and Teschke, 2016; Danan and Teschke, 2018; Teschke and Danan, 2018b, Teschke and Danan, 2019).
With respect to liver injury by drugs, RUCAM can help verify or dismiss causality in cases of suspected DILI and facilitates and characterizes the multiple facets of DILI. RUCAM-based DILI cases are also required to establish and validate diagnostic biomarkers (Teschke et al., 2017b), considering that the liver injury as claimed to be DILI often is not DILI but caused by diseases not related to any drug treatment (Björnsson, 2016a; Björnsson and Hoofnagle, 2016b; Teschke and Danan, 2018c; Teschke, 2018d). DILI has to be differentiated from various other liver diseases. For this differentiation, experienced physicians including hepatologists are essential, who are devoted to solve this clinical issue through individual alertness and use of a validated CAM like RUCAM in its updated version. Missing the correct DILI diagnosis may harm the patient or, in worst-case scenario, cause legal discussions.
The focus of this review is on published DILI cases, assessed for causality using RUCAM. More specifically, a list of publications containing recent 46,266 DILI cases with RUCAM-based causality assessment and a list of the top drugs implicated in DILI are presented, along with a survey of alternative causes wrongly considered as DILI. The current analysis was limited to DILI cases published within the last 5 years: from January 2014 to February 2019.
Literature Search and Data Source
Aiming to identify publications relevant to the topic of the current review article, the database of PubMed was used for these search terms: drug-induced liver injury and DILI; both terms were used alone or in combination with RUCAM or Roussel Uclaf Causality Assessment Method. As a result, for drug-induced liver injury combined with RUCAM or Roussel Uclaf Causality Assessment Method, each provided around 33,200 hits; for DILI combined with RUCAM, around 7,070 hits were obtained, and for drug-induced liver injury together with Roussel Uclaf Causality Assessment Method, another 13,700 hits. The online search was completed on 22 February 2019.
Relevant publications of interest focusing on the topic of the article were included in the reference list. Reports in English language were preferred. The primary aim was to use original publications including case reports and case series, consensus reports, and review articles.
Definitions
In the analysis of this large case series, definitions of terms have been used in order to ensure homogeneity of the approach.
Liver Adaptation and Liver Injury
Provided contraindications are respected and the daily dose is within the recommended range, regulatory approved drugs are normally well-tolerated chemicals that are metabolized in the liver without harming the organ despite possible metabolic interactions. However, under certain circumstances, drugs may cause liver adaptation, also described as liver tolerance, or initiate even liver injury. Prerequisite for defining these conditions is the exclusion of alternative causes.
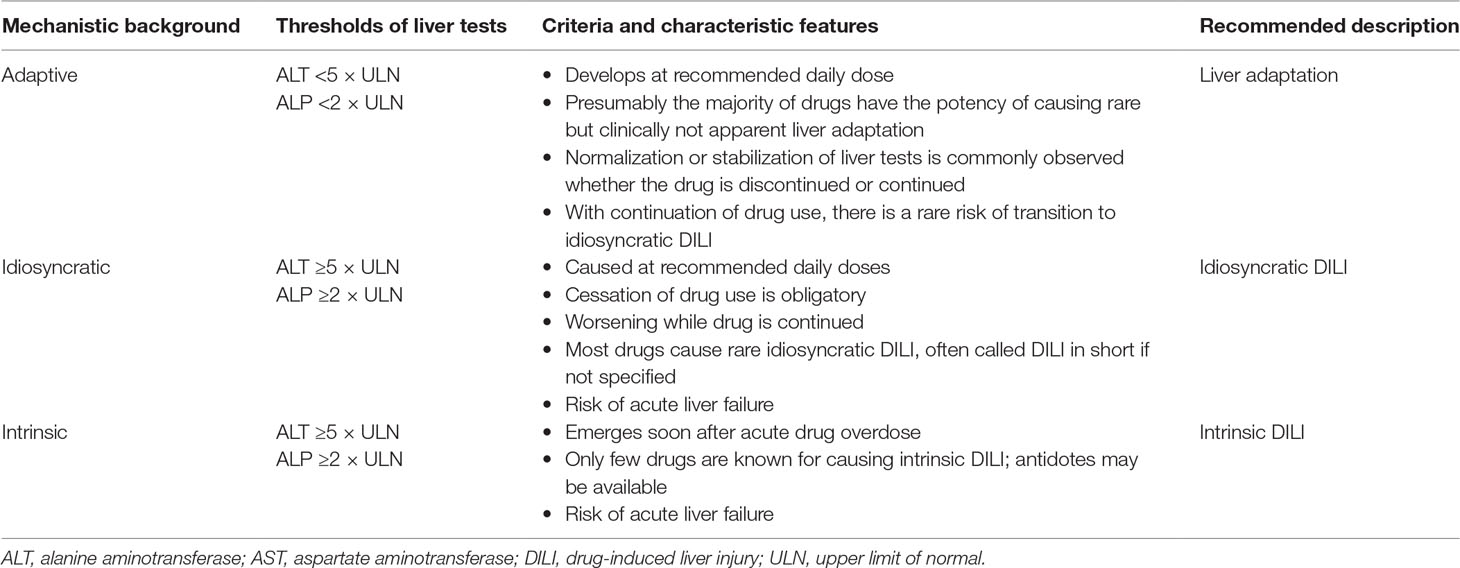
Liver Adaptation
Liver adaptation in connection with a drug therapy represents a mild modification of liver integrity, as evidenced by small increases of liver tests (LTs) that return to normal with continued drug treatment, referring to aminotransferases and/or alkaline phosphatase. Most of the commonly used drugs can presumably cause liver adaptation, although this question has rarely been extensively investigated in detail except in small samples within clinical trials. Examples for drugs causing liver adaptation include statins and isonicotinic acid hydrazine (INH; both are also known for causing also rare idiosyncratic DILI) (Björnsson, 2014; Teschke and Danan, 2016a, Teschke and Danan, 2017c; Teschke, 2018d), as well as paracetamol, which may cause liver adaptation, but mostly induces intrinsic DILI and extremely rare idiosyncratic DILI (Teschke and Zhu, 2018e). Some general features of drug-induced liver adaptation are known and listed (Table 1).
Idiosyncratic and Intrinsic DILI
Liver injury associated with a drug treatment can be ascribed to the interaction between the drug and patient factors (idiosyncrasy) or to the drug itself (intrinsic toxicity). In practice, DILI commonly stands for the idiosyncratic DILI, the basically preferred and more specific term to avoid confusion (Table 1), which develops among a few individuals under the treatment with drugs used at recommended doses and is caused by unpredictable events due to immunologic or metabolic drug reactions (Figure 1) (Teschke and Danan, 2018b). Conditions are different for the intrinsic DILI (Table 1), which shows a clear dependency on the drug dose and represents therefore a predictable reaction caused by overdose of the used drugs like paracetamol, also called acetaminophen (Teschke and Zhu, 2018e). The mechanistic background differs substantially between these two DILI types (Figure 2) (Teschke and Danan, 2018c). In a clinical setting, the offending drug(s) often cannot be identified, problems best ascribed to vague principles of diagnosis related to undetermined DILI typology and application of CAMs, which do not follow a quantitative and transparent scoring system such as RUCAM. Problematic are reports of liver injury case cohorts in which no group differentiation was made between patients who experienced idiosyncratic DILI and those with intrinsic DILI because results obtained from these mixed patient groups are vague and disputable.
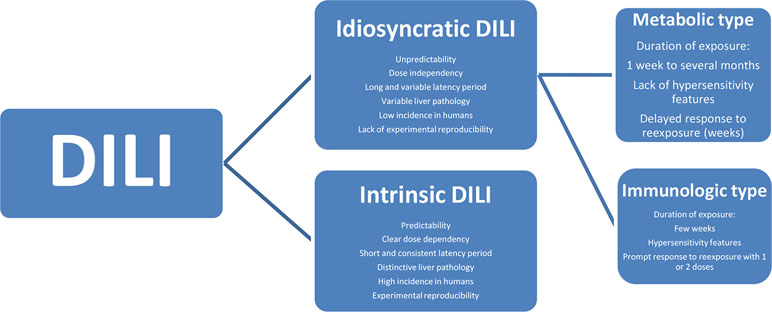
Figure 1 Characteristics of idiosyncratic DILI and intrinsic DILI. Reproduced from a previous report (Teschke and Danan, 2018b) with permission of the publisher Wiley-Blackwell Corporation. Abbreviation: DILI, drug-induced liver injury.
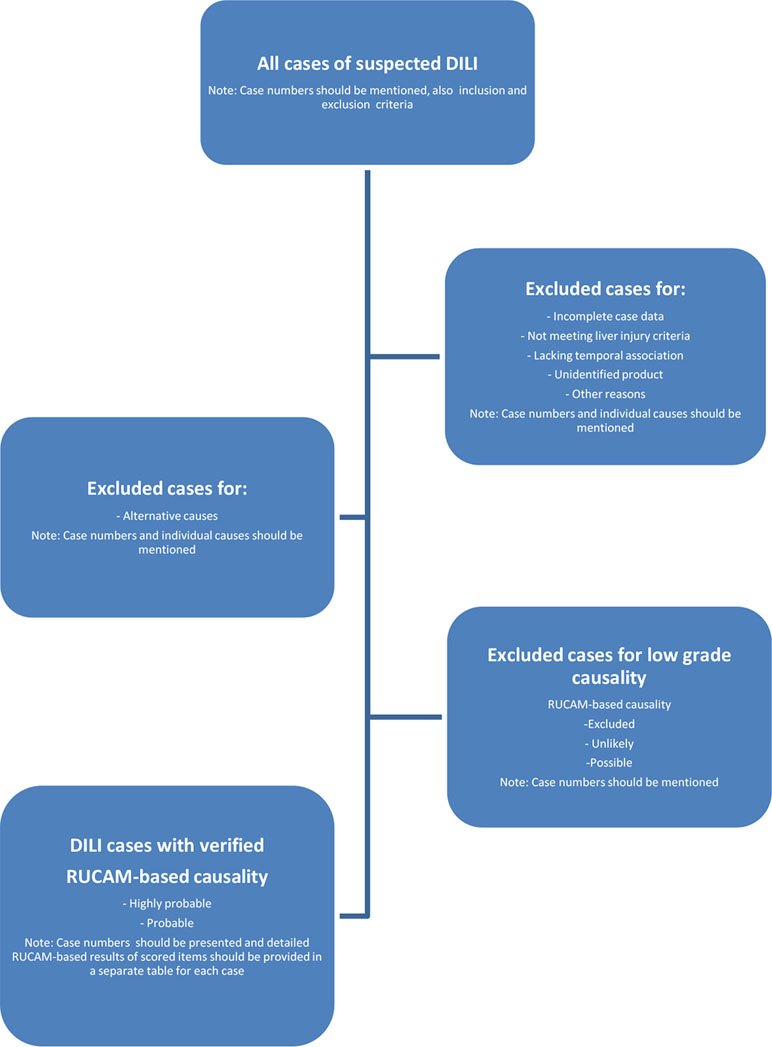
Figure 2 Suggestion for a diagnostic flow chart of a prospective case series DILI, in preparation of a publication. In this flow chart, DILI stand for idiosyncratic DILI. Abbreviations: DILI, drug-induced liver injury; RUCAM, Roussel Uclaf Causality Assessment Method. Modified and reproduced from a previous publication (Teschke and Danan, 2018b) with permission of the Publisher Wiley-Blackwell Corporation.
Thresholds
Assessing the causality in suspected DILI cases begins with defining the type of liver injury (Table 1). Currently used criteria of a major liver injury include serum activities of LTs, namely alanine aminotransferase (ALT) of at least 5 × ULN (upper limit of normal) and/or alkaline phosphatase (ALP) of hepatic origin and at least 2 × ULN (Danan and Teschke, 2016). This ALT threshold is important to recognize early and remove all cases with minor and usually reversible liver injury from the evaluation. Diseases to be excluded are, for instance, those occurring in patients who are overweight, who are obese or morbidly obese, or who have an increased body mass index (BMI). Patients with a high BMI are at risk of developing a metabolic syndrome, nonalcoholic fatty liver disease (NAFLD), or nonalcoholic steatohepatitis (NASH). It is therefore prudent to clear these cases away from the DILI cohorts and focus on actual DILI cases, efforts that also avoid costly diagnostic procedures.
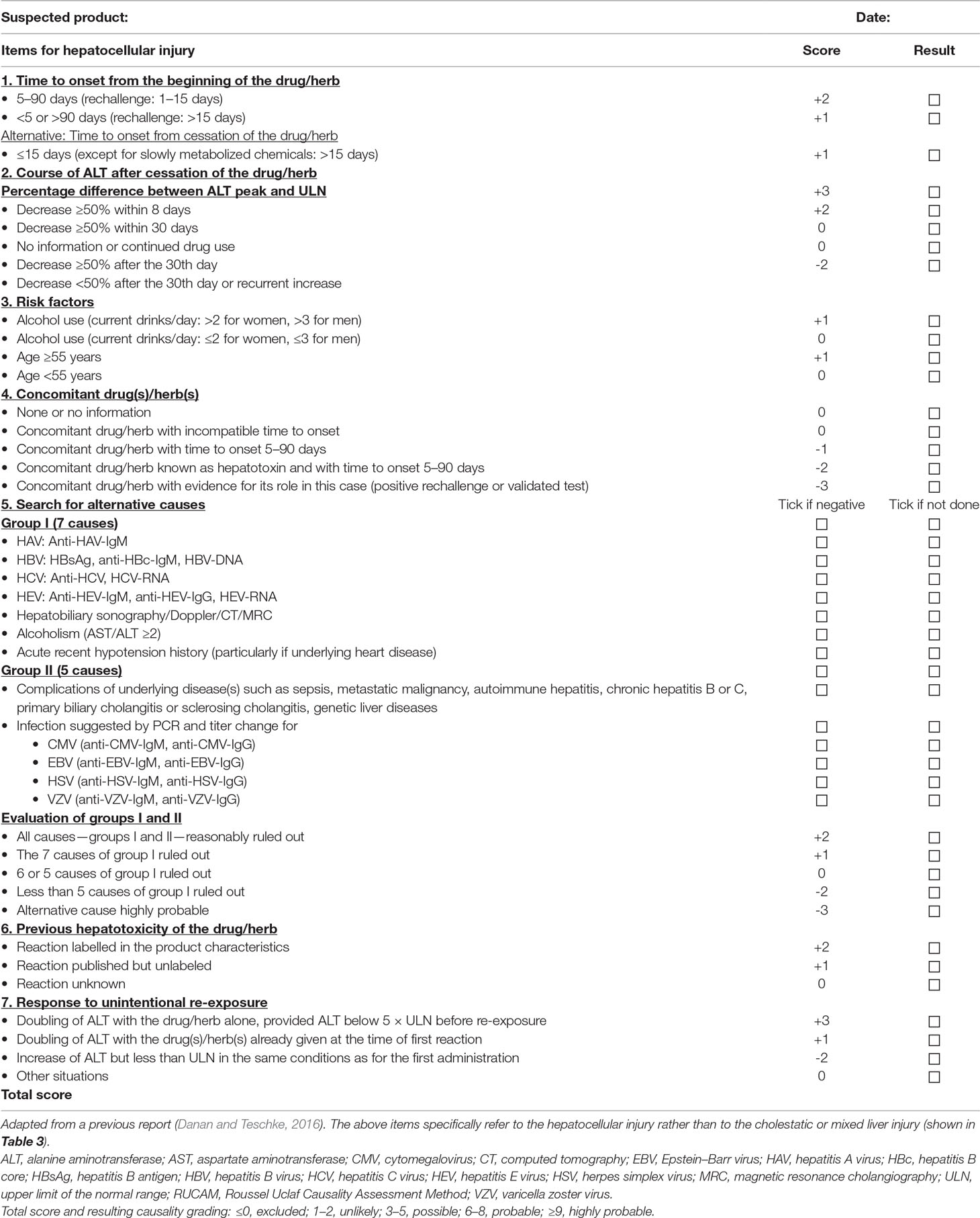
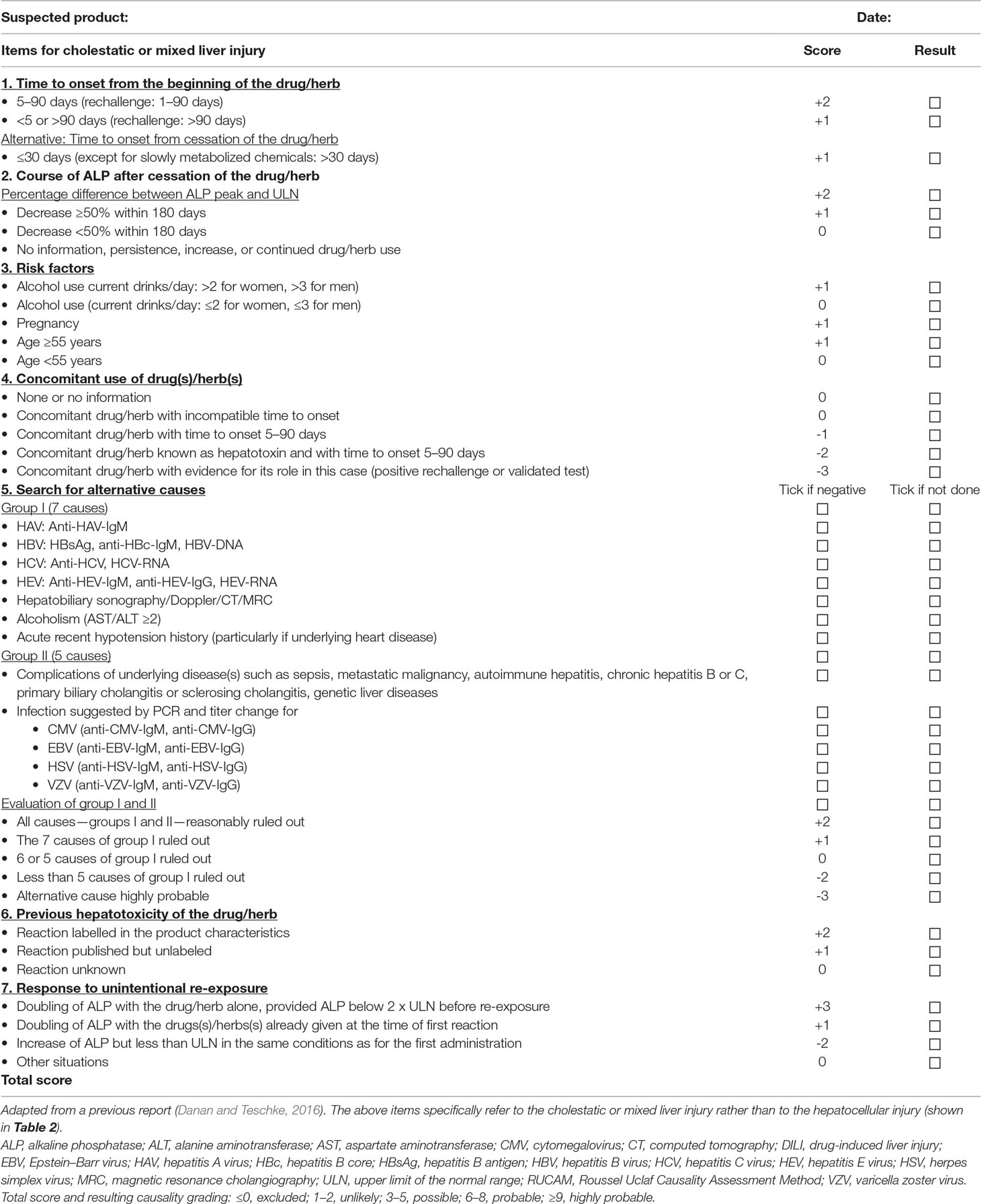
Laboratory-Defined Liver Injury Pattern
There is also a need to determine the liver injury pattern. This can be achieved by assessing the ratio R, to be calculated through the multiple of the ULN of serum ALT divided by the multiple of the ULN of serum ALP, provided the ALP increase is of hepatic origin. The R value allows differentiation of the hepatocellular injury from the cholestatic/mixed liver injury. For each injury type, a specific RUCAM subscale is available and must be used for causality assessment. The best time assessing the ratio R is at the start of the liver injury because the initial type could evolve in the further course towards another type that would change the criteria for the causality assessment (Danan and Teschke, 2016, Danan and Teschke, 2018, Danan and Teschke, 2019). For evaluation in a normal setting, two types of liver injury are to be considered: first a hepatocellular injury with R > 5, and second, a cholestatic/mixed liver injury with R ≤ 5. This differentiation is essential because risk factors and time courses of ALT and ALP are different, and it also explains why the RUCAM scale needs two subtypes (Danan and Teschke, 2016), one for the hepatocellular injury (Table 2) and the other one for the cholestatic/mixed liver injury (Table 3).
RUCAM
RUCAM with its two subscales (Tables 2 and 3) has received overwhelming international support, as evidenced by the large number of DILI and HILI case evaluations with causality assessment by RUCAM, which were reported from 1993 until 2016 in over 100 publications (Danan and Teschke, 2016). Since 2014, RUCAM has additionally been supported by DILI experts of several countries including the US, China, and Germany. For instance, in a large US study using RUCAM in search for DILI cases in electronic medical records, 11,109 patients overall with 14,925 DILI events were found (Cheetham et al., 2014). In addition, in the US, 493 DILI cases were assessed for causality by RUCAM (Hayashi and Björnsson, 2018). It looks like that other members of the US DILIN now become more familiar with RUCAM, as helpful comments on a recent manuscript have been acknowledged in the context of the Chinese guidelines for the diagnosis and treatment of drug-induced liver injury, which recommended the use of the original RUCAM of 1993 (Yu et al., 2017) but unfortunately not the actual updated RUCAM version of 2016 (Danan and Teschke, 2016). What’s even more and substantially better, a DILIN member co-authored a large Chinese DILI paper of 18,956 DILI patients, all assessed using the original RUCAM of 1993 (Shen et al., 2019). Another member of the US DILIN group served as a senior author of a publication with focus on a critical assessment of published DILI case reports, presenting in at least 318 cases an unlikely causality grading based on the original RUCAM of 1993 (Björnsson and Hoofnagle, 2016b). Support from China came from another publication with 870 RUCAM-based DILI cases and the recommendation for general use of RUCAM in DILI case assessment (Zhu et al., 2016). Substantial support for thorough analysis of DILI cases and promotion for causality assessment by the updated RUCAM was provided by US experts of DILI from the group of James H. Lewis and his associates (Sarges et al., 2016; Shahbaz et al., 2017; Real et al., 2018).
RUCAM is appreciated as a validated, liver-specific, structured, and quantitative CAM with a clear scoring system of well-defined key elements that provide a transparent final causality grading after summing up of the individual element scores (Danan and Teschke, 2016). Compared to RUCAM at the prime position, other CAMs are poorly positioned. In particular, there is no evidence in the global DILI setting that any other CAM can presently outperform RUCAM, which represents a learning system with a biological diagnostic background that represents a limitation of RUCAM use. Out of these reasons, RUCAM is not necessarily perfect in covering all tentative diagnostic aspects related to the variability of DILI features and covering all of the more than 1,000 different drugs implicated in causing liver injury (Teschke and Danan, 2018b). Certainly, a variety of other CAMs are on the market with their major shortcomings, which have been outlined recently (Danan and Teschke, 2016; Teschke and Danan, 2018b). In brief, some CAMs are not specific for the liver and liver injury; others are poor plagiates of the original RUCAM, confounded by deleting and modifying its original elements or adding new elements with not validated criteria and scoring. Other CAMs claimed having incorporated RUCAM elements, but by checking the conditions, it turned out that element criteria were insufficiently transferred from the RUCAM system, or the RUCAM specific scoring system was evidently omitted. Despite these deletions, new global causality gradings were offered as percentage ranges that may erroneously be misinterpreted as the result of obtained individual element scoring, which in fact was not done. Finally, CAMs based on global introspection are an additional problem because assessment is subjective and not transparent, not based on valid element criteria, and devoid of a validated scoring system. In essence, only RUCAM is seemingly in the comfortable situation to assist establishing causality in assumed DILI cases. No other CAM has a similar successful clinical and scientific run, and the lack of such a background and accuracy prevents any attempt of overriding and outperforming the successful RUCAM.
In line with other CAMs, RUCAM shares the problem of DILI diagnosis in patients with hepatitis B or C, which requires assistance by an experienced virologist to assess the viral infection and importance of the viral load as contributory or sole factor of the disease. In general, cases with preexisting liver disease require special clinical attention because for these an individual RUCAM scoring system is not available, but general recommendations have been published (Danan and Teschke, 2016). Previously, the issue of diagnosis and management of acute idiosyncratic DILI in patients with preexisting liver disease has thoroughly been analyzed and discussed (Teschke and Danan, 2016a). Regarding clinical trials using patients with preexisting liver disease, a pragmatic approach suggests subtracting baseline reference LT values before start of the trial from actual LT values obtained during the trial, because this would bring evidence whether the thresholds of ALT >5 × ULN or ALP >2 × ULN are fulfilled for the suspected DILI (Teschke and Danan, 2016a), and the available data can then undergo causality assessment based on the updated RUCAM (Danan and Teschke, 2016; Teschke and Danan, 2016a). Of note, RUCAM has no problem assessing drugs with unknown previous liver events (drugs in clinical trials) or newly marketed drugs like immune modulating agents and more specifically immune checkpoint inhibitors because it considers these drug-related limitations appropriately by not providing high causality gradings due to few missing elements and their individual scores.
Global DILI Cases Assessed by RUCAM
Large Case Series
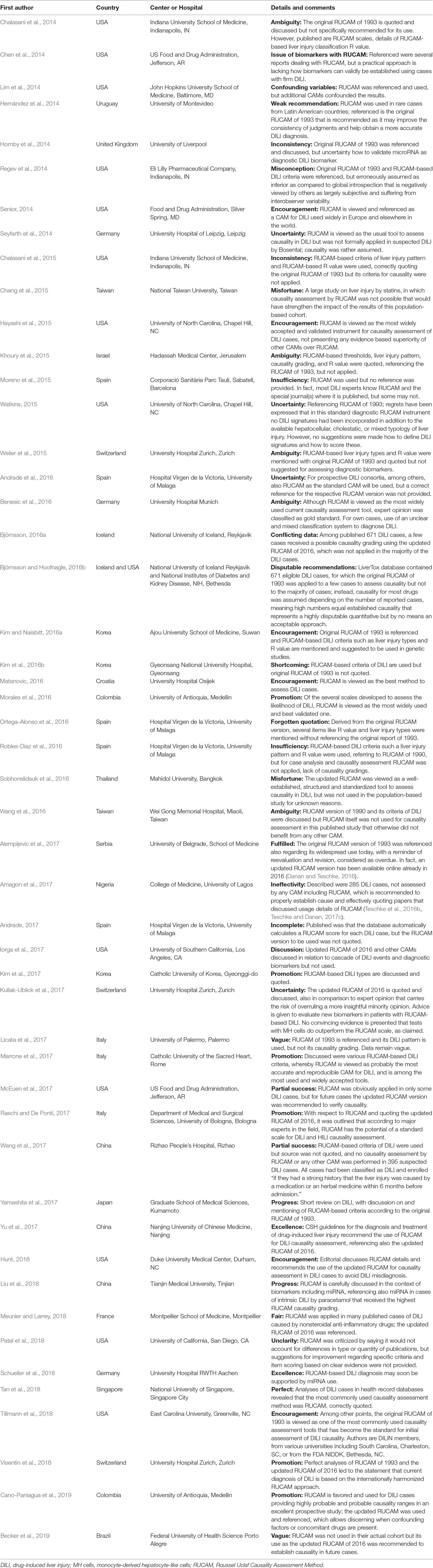
The present analysis of selected 36 reports provided by authors originating from 10 countries published from 2014 until end of February 2019 revealed that 46,266 DILI cases had been evaluated for causality by one of the two latest RUCAM versions of 1993 and 2016 (Table 4). This allows a good overview on the quality and shortcomings of DILI case assessment using RUCAM and merits some comments on the published reports (Table 4):
1. The current listing of RUCAM-based DILI cases is large (Table 4) and confirms previous impressions that RUCAM is well accepted in the scientific community of DILI experts (Danan and Teschke, 2016). The updated RUCAM of 2016 has increasingly been used in the last few years (Table 4) and should be the preferred RUCAM version in future DILI case assessments.
2. With few exceptions, drug groups or individual drugs were specified; this applies preferentially to cohorts of small or intermediate size, which often present detailed information on characteristic features of DILI caused by specific drugs, while large cohorts commonly failed to differentiate between individual drugs but provide a broader overview.
3. In most reports, final RUCAM scores with corresponding RUCAM-based causality gradings were carefully listed, allowing thereby some conclusions on case data quality. In general, high numbers of DILI cases with a possible causality grading commonly reflect incomplete case data sets because RUCAM includes this condition by providing low scores for missing key elements.
4. High causality gradings of probable or highly probable likelihood are commonly achieved with prospective studies that facilitate collection of complete data in time while the patient is under medical care. Consequently, prospective studies are preferred over retrospective ones because their results may be a matter of discussion.
5. Most reports present clear and precise data on DILI related to synthetic chemical drugs, allowing valid description of DILI features and discussion about other points of interest like aspects of epidemiology. Such data may differ from country to country, but conclusions should be valid as all studies were based only on RUCAM.
6. Publications with cohorts consisting of both DILI and HILI cases create confusion unless groups are separately considered prior to final analysis.
7. In the majority of reports, the RUCAM version used was specified with preference of the original RUCAM of 1993 and the now preferred updated RUCAM of 2016, whereas initial versions of 1990 or before are clearly incomplete.
8. Occasionally, reports came along without specifying the RUCAM version used or even without referencing the respective publication, to be viewed as a major deficiency. Some authors even misquote or fail to reference the correct original or updated RUCAM version or quote instead a secondary literature source that has nothing to do with the original one. Although DILI researchers and clinicians are likely familiar with RUCAM and its correct reference source, others may not and would appreciate a correct quotation.
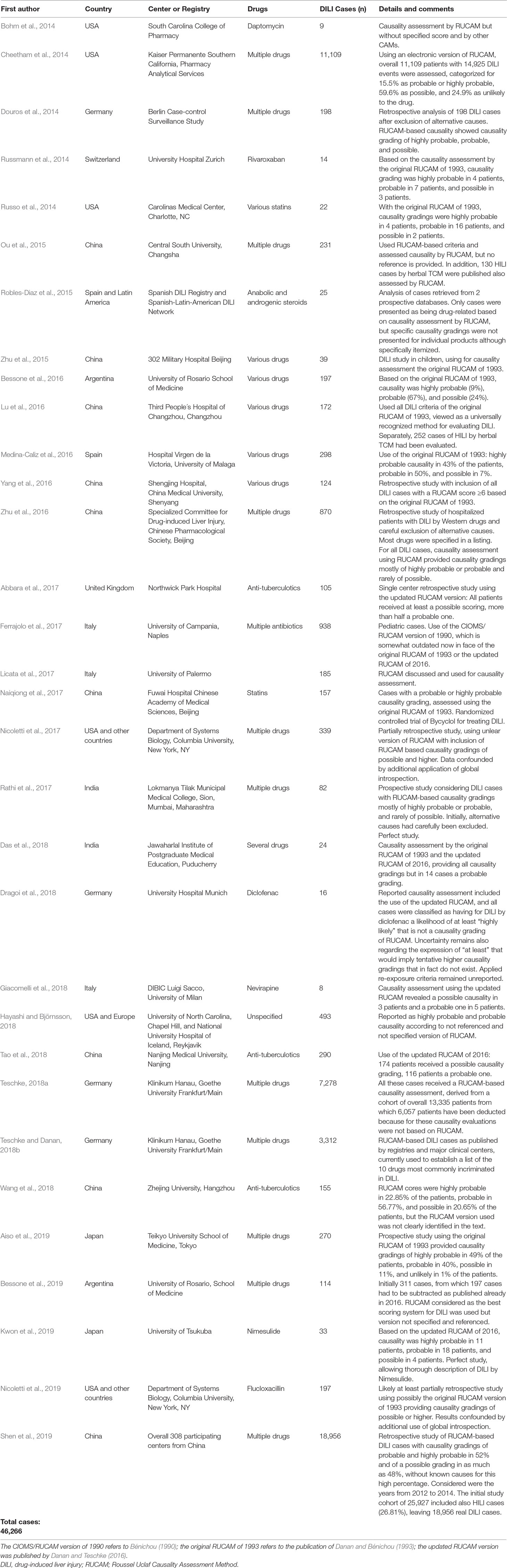
Table 4 List of selected publications and analyses from national registries and medical centers that applied RUCAM in suspected DILI cases included in major case series and published from 2014 to early 2019.
No question, many RUCAM reports of DILI are of high quality, especially those of national DILI registries in Europe, which assessed cases prospectively and provided excellent results with high causality gradings and details as referenced previously (Danan and Teschke, 2016; Teschke, 2018d). In addition, authors from India published another prospective study on DILI with high causality gradings (Rathi et al., 2017), classified as a report of excellence (Teschke and Danan, 2017a). Applying RUCAM prospectively in the Indian cohort study facilitated early detection of non-drug causes in eight patients. Among the alternative diagnoses were acute hepatitis E virus (HEV) in three patients, autoimmune hepatitis in two patients, and hepatitis A, B, and sarcoidosis in one patient each (Rathi et al., 2017). In all patients of the Indian study, infections by HEV were systematically excluded, not only because HEV is endemic in India but also because consensus exists among experts in the field that HEV infections must be excluded in any suspected DILI or HILI case. This study from India confirmed that alternative causes can be excluded only if the patients are correctly investigated at the early phase of the liver injury.
The analysis of the 10 countries, in which the authors of the 31 reports had their working place, showed China on top, followed by the US and Germany (Table 5). In some reports, authors came from different countries but this is not separately listed in the table. A listing with authors of RUCAM-based DILI and HILI cases from many more countries has previously been provided (Danan and Teschke, 2016). Importantly, RUCAM-based DILI reports have been published in journals considered as one of the most relevant ones (Table 5), suggesting that their editors perhaps appreciate RUCAM or are at least familiar with it.
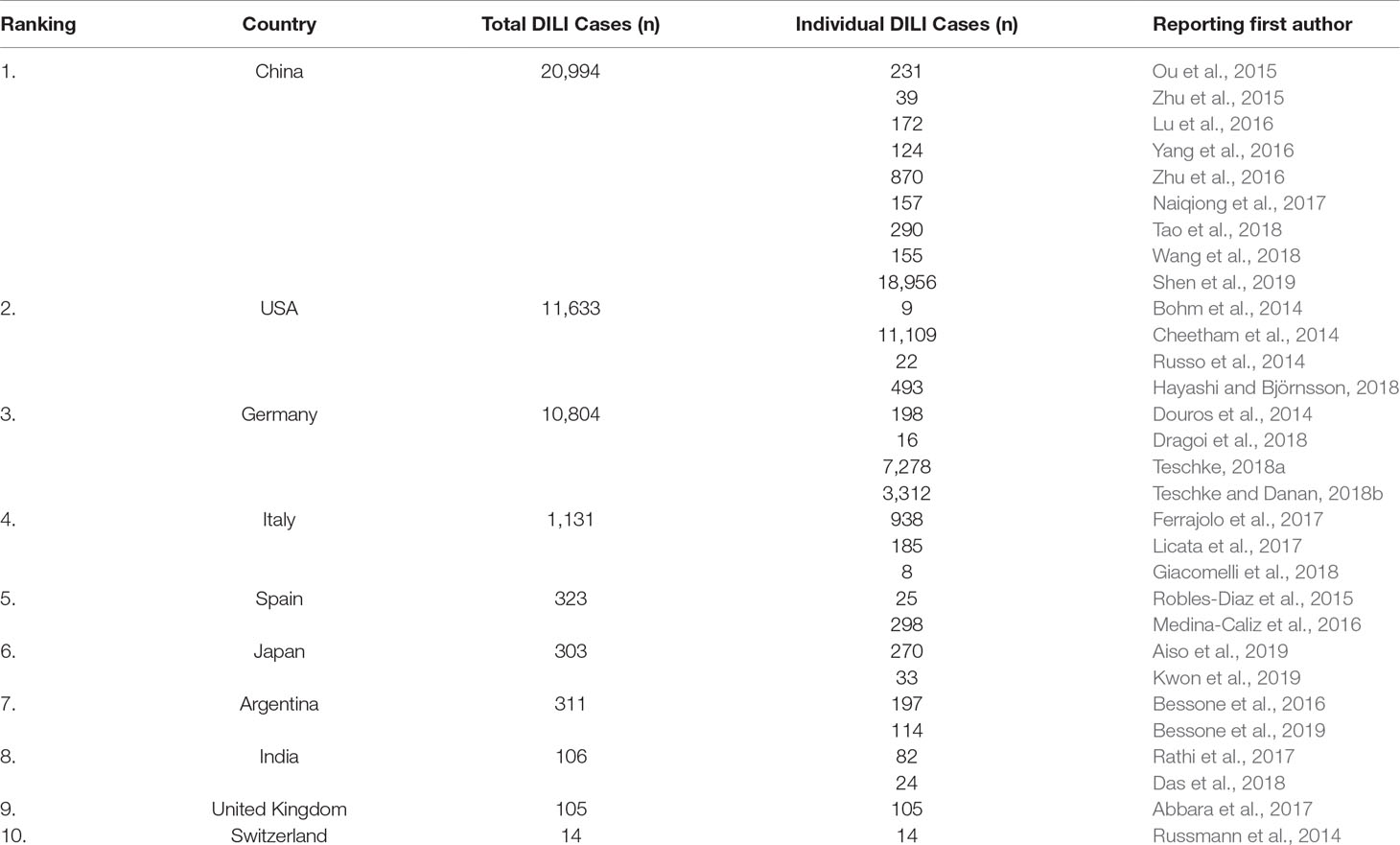
Table 5 Ranking of countries from which first authors reported DILI cases assessed by RUCAM as published from 2014 to early 2019 with specification of the publishing journal.
Single Case Reports and Small Case Series
As compared to large DILI case series, the clinical value of RUCAM-based DILI cases published as single case report or as small case series should not be underestimated; some of these had been selected as examples (Table 6). They usually provide a broad narrative of the DILI cases and often include for the cases a separate list with RUCAM elements and the respective scores. Using this approach, the case description itself benefits from transparency that cannot be provided for DILI cases from large case series. Therefore, short case series or single case reports are of particular value for physicians in search for details. Such informative reports of DILI cases with affirmed diagnosis should have a chance being included for instance in the LiverTox database, provided the case had been evaluated by RUCAM and qualified for a high causality grading. The impression prevails that within the last few years, the updated RUCAM is more often used (Table 6), good news not only for the updated RUCAM but also for the scientific community of individuals involved in DILI case assessment and management.
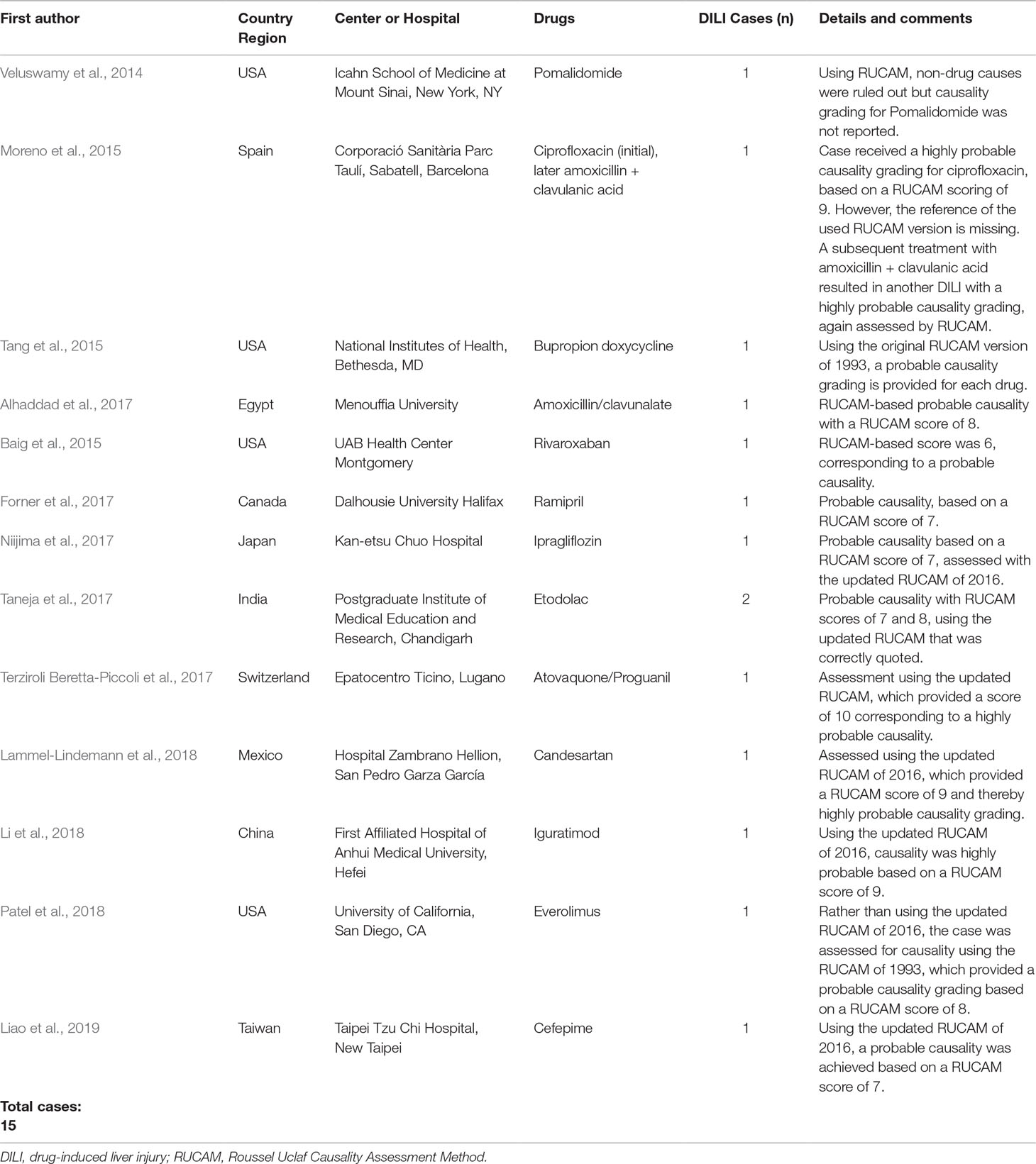
Table 6 List of offending drugs in selected case reports or small case series that applied RUCAM in suspected DILI cases, published from 2014 to early 2019.
Comments and Encouragements
The worldwide success of RUCAM is overwhelming, as evidenced by the large number of DILI cases assessed by RUCAM (Table 4). Analyzing the listed reports in detail, it seems that the use of RUCAM goes smoothly, more or less without major difficulties. Nevertheless, a few reports show shortcomings in case presentations and provide critical comments, which merit attention and are presented in condensed form, drawn from selected publications to provide an unbiased overview (Table 7). Included in the list are also encouraging statements that are refreshing. Overall, the impression prevails that RUCAM including its updated version is on the winning avenue.
RUCAM-DILI Case Quality (RDCQ)
The yield of highly qualified DILI reports of RUCAM-based cases could substantially be higher if some essentials would have been considered. In particular, the quality of present studies with RUCAM-based DILI cases is obviously variable regarding listed details of published cases (Tables 4 and 5). For instance, some reports had a retrospective study protocol instead of a preferred prospective one, and details occasionally were not reported such as the RUCAM version used, or results were incompletely provided. These shortcomings are, in principle, avoidable if studies are carefully planned prospectively. In an attempt to improve the quality of future DILI case publications, a list of essential items has been developed (Table 8). These items received a number of stars measuring the case or the study quality: the more stars the better the case or the study (Table 8). This tool may be called, in short, RDCQ (RUCAM-DILI Case Quality). Highly qualified reports may receive appreciation by 3 stars, whereas publications with an insufficient quality receive 2 or fewer stars. RDCQ provides a list of the most important elements required for planning studies on cases of suspected DILI and possible publication (Table 8). The first category comprises six essential elements, each awarded with 3 stars, while the second group consists of five elements, each of which may receive 2 stars, and the third category considers four elements, for each 1 star can be assigned. Accordingly, a quality ranking of intended DILI publications is achieved by summing up of the respective star numbers listed in front of each element of interest (Table 8). As a result, an excellent quality would be achieved with >28 stars, an acceptable one with 18–28 stars, and a disputable quality with <18 stars. Potential authors and editors are encouraged to use this qualifying scoring system.
Alternative Causes and RUCAM
RUCAM plays also an investigative role to critically screen for potential alternative causes in cases of assumed DILI, as outlined in a recent analysis of a large case study published in 2018. Frequency and type of alternative causes were evaluated in cohorts of case series provided by 22 publications (Table 9) (Teschke and Danan, 2018c). Presented primarily as DILI in these publications, only part of the cases turned out to be real DILI cases after investigations including the use of a CAM such as RUCAM in search for verification or exclusion of nondrug causes (Teschke and Danan, 2018c). In all referenced publications, many cases with initially assumed DILI were reported that were not DILI.
Frequency
The 22 publications reported on overall 13,336 cases. In 4,556/13,336 cases corresponding to 34.2%, alternative causes unrelated to DILI were presented; in other words, in more than one third of the cases, there was a potential alternative explanation for the hepatic disease, conditions not acceptable for the involved patients (Teschke and Danan, 2018c). The data on the 13,336 cases have been published by authors from different areas and countries, while reports were mostly from Asia, some came from the US, and less reports were published on cases from Europe. Overall, alternative diagnoses in the case series ranged from 4% up to 47%.
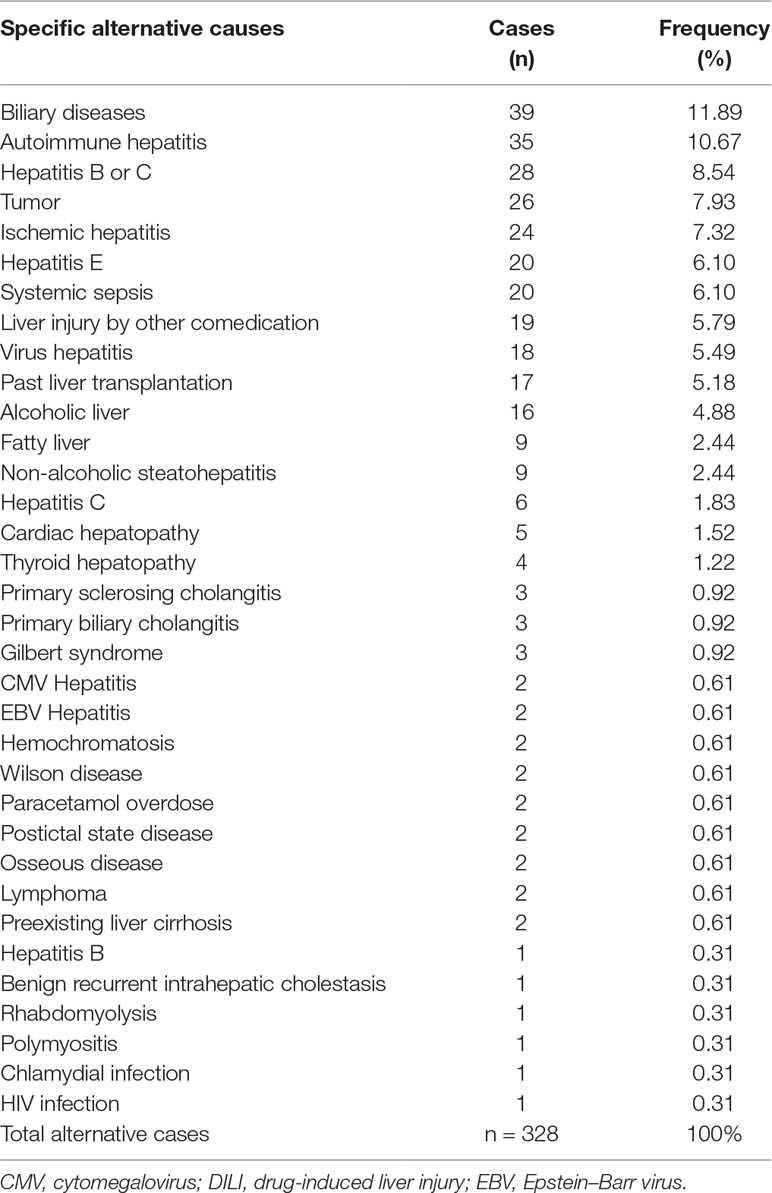
Types of Alternative, Not Drug-Related Causes
Although most reports presented their alternative drug unrelated causes with specific diagnoses, many of the remaining publications provided only case numbers with alternative causes lacking diagnostic specifications. The 328 cases with specified non-drug causes are provided (Table 9) and had been submitted to further analysis (Teschke and Danan, 2018c).
Bile Tract and Intrahepatic Biliary Diseases
Biliary diseases were among the most alternative diagnoses, accounting for almost 12% (Table 9). These included, for instance, bile tract disorders causing biliary obstruction such as choledocholithiasis or infections clinically described as cholangitis. With these bile tract diseases, patients are at a high risk if the appropriate surgical intervention, endoscopic therapy, or treatment with antibiotics was withheld or delayed. Among other unrecognized hepato-biliary diseases were primary biliary cholangitis, a disease affecting the liver, and primary sclerosing cholangitis, with possible localization in the extrahepatic biliary tract system and intrahepatic localization (Table 9). Patients with these forms of hepato-biliary diseases commonly respond well upon initiation of specific drug therapies.
Liver Diseases
A variety of liver diseases unrelated to the use of drugs escaped the diagnostic efforts of the treating physicians (Table 9) (Teschke and Danan, 2018c). Among the not recognized alternatives diseases of the liver were mostly virus infections like hepatitis B, C, and E, while virus hepatitis by cytomegalovirus (CMV) and Epstein–Barr virus (EBV) were rarely described (Table 9). With hepatitis A virus (HAV) infection as another form of virus hepatitis, this diagnosis was not described as a missed cause in any of the published cases, but this is typical text book diagnosis nor requiring much expertise (Teschke and Danan, 2018c). Higher risks exist for patients suffering from ischemic hepatitis and cardiac hepatopathy, because these diseases would have better been treated under the care of cardiologists, as these liver diseases were the consequence of cardiopulmonary disorders and have therefore their origin outside the liver. Missing the diagnosis of an autoimmune hepatitis is another problem because for this liver disease, a specific corticosteroid therapy is strongly indicated provided the diagnosis has validly been established (Table 9). Hemochromatosis or Wilson’s disease is a typical genetic liver disease and was rarely described as missed diagnosis in the study cohort, unlike the more frequent non-alcoholic fatty liver disease (NAFLD), non-alcoholic steatohepatitis (NASH), and alcoholic liver disease (ALD), which all together amount to 10.4% of the alternative causes (Table 9). Clinical differentiation from DILI is usually not a problem on the basis of careful analysis, the clinical context, and if RUCAM is used for DILI verification or exclusion.
Other Drug Unrelated Causes as Alternative Diagnoses
Reports have been published on cases with serum bilirubin values above the normal range together with normal LTs, conditions suggestive of Gilbert syndrome, but in some instances, these laboratory alterations have erroneously been ascribed to DILI while the diagnosis of Gilbert syndrome was missed and therefore not published (Table 9) (Teschke and Danan, 2018c). Additionally, increased LTs were wrongly attributed to DILI in patients who experienced hypothyroidism, thyrotoxicosis, rhabdomyolysis, polymyositis, and postictal state (Table 6). Difficult to reconcile in other patients, enhanced ALP activities in the serum were wrongly attributed to DILI of the cholestatic type instead of underlying osseous diseases with fractures or metastases (Table 9). Again as a reminder for RUCAM users, in patients with increased serum ALP values, a non-hepatobiliary disease as cause has to be excluded using additional laboratory test as outlined above and previously (Danan and Teschke, 2016). DILI was also not correctly diagnosed in patients with malignant disorders like lymphoma that were responsible for almost 9% of the alternative, nondrug causes, or in patients with sepsis accounting for around 6% (Teschke and Danan, 2018c). It is clear from these data that in patients with increased LTs many alternative causes were insufficiently looked for. Although RUCAM helps exclude other causes that are defined as a special key element, it is recommended to work up an additional list of differential diagnosis, which has been published with the updated RUCAM (Danan and Teschke, 2016).
Diagnostic Flow Chart
Diagnostic flow charts facilitate the quick catching of the presented data, for which respective references were provided earlier (Teschke and Danan, 2018c). The diagram helps the investigator at planning a prospective DILI study, and at its termination, it allows for a clear presentation of details obtained during the course of the study. This diagram should be submitted along with the manuscript to the journal as it enables the reader to gain a quick overview on the various steps during the course of the study. The suggested proposal should be viewed as a guidance allowing for modifications if necessary (Figure 2).
On top of the diagram, all cases of suspected idiosyncratic DILI have to be presented, with details of case numbers and criteria for exclusion and inclusion (Figure 2). Only cases with idiosyncratic DILI should be considered, excluding a priori all patients with intrinsic DILI and those with liver injury due to herbs or dietary supplements. Clearly, in analogy with conventional drugs as culprits of idiosyncratic DILI, herbs and dietary supplements can cause liver injury commonly viewed as HILI (herb-induced live injury). Characteristics of the two cohorts DILI and HILI differ substantially from each other and have to be evaluated separately in order to avoid results that are mixed up and thereby confounded. During the study, cases that do not meet the basic requirements for a good causality assessment should be excluded. Alternative causes and low causality gradings also should lead to case exclusion. At the end, a series of idiosyncratic DILI cases remains with uniform characteristics, which can easily be evaluated.
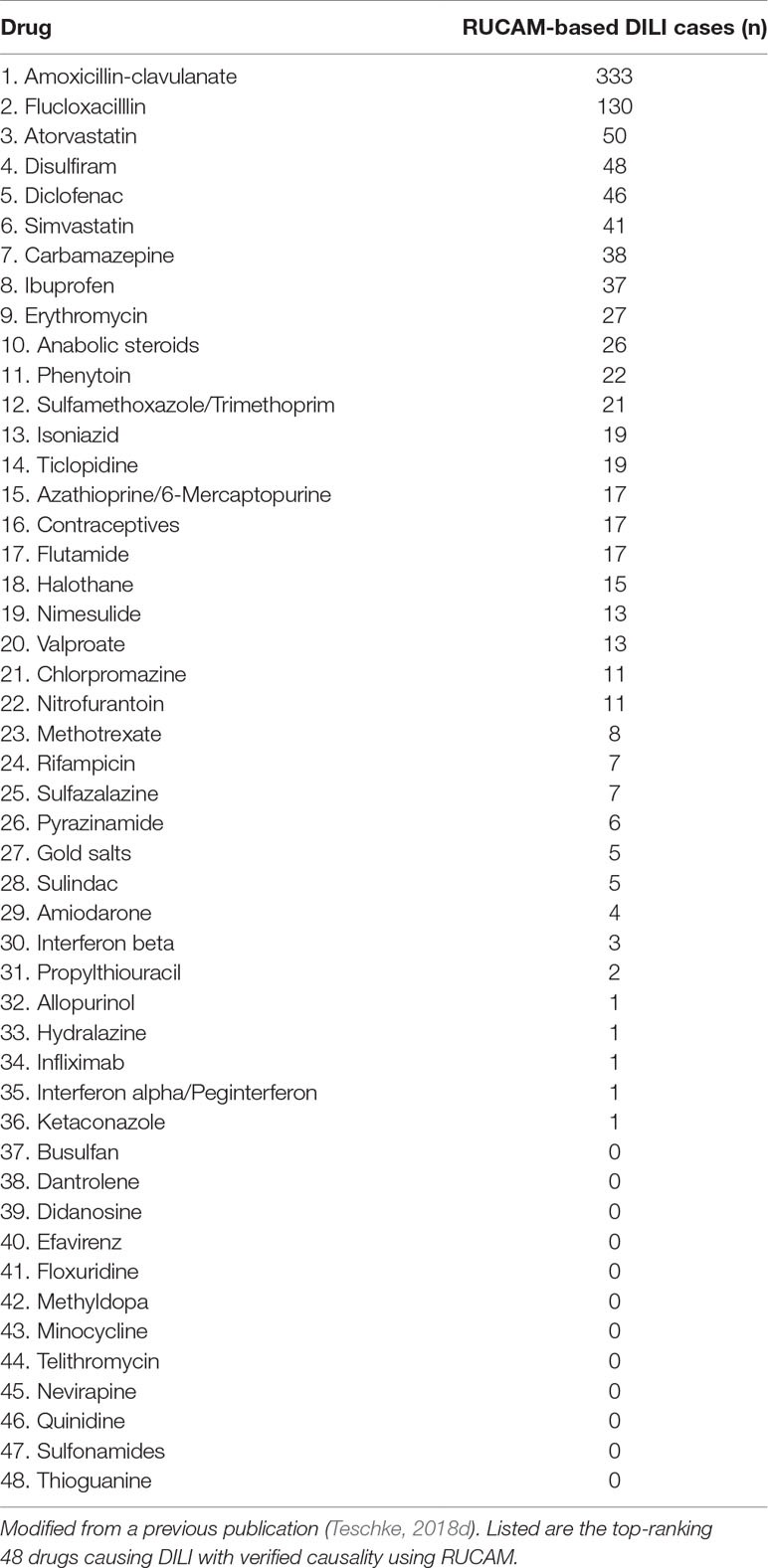
Top Drugs Implicated in Causing DILI Assessed by RUCAM
Among the list of DILI case series (Table 4), there was also a study on 3,312 RUCAM-based DILI cases, assessed for drugs most commonly implicated in causing DILI (Teschke and Danan, 2018c). This study was triggered by previous publications describing poor quality of DILI case data, the inability to find enough DILI cases with established causality, and the associated problem of listing the most common drugs implicated in causing DILI (Björnsson, 2016a; Björnsson and Hoofnagle, 2016b). These problems started with expert analyses of DILI cases originating from the US LiverTox database, whereby part of the cases had been reassessed by retrospective use of the updated RUCAM (Björnsson, 2016a) or the original RUCAM (Björnsson and Hoofnagle, 2016b). Their expertise showed that many of the LiverTox cases of DILI could not be verified as real DILI, a difficult outcome for the LiverTox database, and also frustrating for the scientific DILI community. The results of these investigations suggest a more cautious interpretation of the DILI cases online available at the LiverTox database. Presently, there is no public statement whether and when this shortcoming will be addressed and what kind of causality assessment approaches will be undertaken to solve these problems. The use of the updated RUCAM might be a good idea.
Closely associated with these database issues was the problem to establish a top ranking of potentially hepatotoxic drugs. To solve this issue, an attempt was undertaken using 48 LiverTox database drugs with more than 50 case reports, for which a firm diagnosis of DILI by high-ranking hepatotoxic drugs has arbitrarily been assumed (Björnsson, 2016a). Using merely these numbers of case reports as the sole criterion for a drug ranking could result in data lacking accuracy. Perhaps a better approach was the use of DILI cases that had been evaluated for causality using RUCAM, available in the DILI databases of several registries and medical centers (Teschke, 2018d). These well-organized databases provided 3,312 drugs overall suitable for establishing a new top ranking that differed substantially from the previous LiverTox-based analysis (Teschke, 2018d). The new ranking of the 10 leading drugs involved in DILI is as follows, from top to bottom: Amoxicillin-clavulanate, Flucloxacillin, Atorvastatin, Disulfiram, Diclofenac, Simvastatin, Carbamazepine, Ibuprofen, Erythromycin, and anabolic steroids (Table 10).
In agreement with the results of older DILI studies, Amoxicillin-clavulanate is the leading drug combination in DILI (Table 8) (Teschke, 2018d). Liver injury is likely more related to the Clavulanate part than to Amoxicillin. Assessing the individual hepatotoxic risk of this drug combination, other details of drug use are essential such as daily dose and duration of treatment. In order to reach at a final conclusion on risk assessment and risk management, assessments in various countries with the drug specificities are needed, as well as a comparison with other potentially hepatotoxic antibiotics. Nevertheless, this example shows that such top rankings may have pragmatic consequences. Compiled from results included in various databases of many countries (Table 10), this new drug ranking provides only a global overview but does not replace considerations on specificities of individual countries with a different disease spectrum, including or excluding, for instance, tuberculosis, causing variabilities of drug use and associated DILI (Teschke, 2018d). A good example is Germany with a special ranking of drugs implicated in DILI, starting on top with Flupirtine, Clarithromycin, Fluoroquinolones, Estrogen + Diogenoest, Irbesartan, Terbinafine, and Metamizole. Conditions are different in China, where DILI is most frequently reported following therapy with antibiotics, antituberculosis drugs, antithyroid drugs, antineoplastic drugs, hypolipidemic drugs, antipyretic analgesics, antiepileptics, hypoglycemic drugs, antivirals, glucocorticoids, antithrombotics, and antihypertensive drugs. India is of special interest, where the top drugs are antituberculosis medications, more so than antiepileptic drugs, complementary and alternative medicine, antiretroviral drugs, and non-steroidal anti-inflammatory drugs. Experienced clinicians in a specific region usually know the most likely cases of liver injury caused by the drugs used in the same region. National regulatory agencies or specialized DILI registries usually can provide additional information on DILI specificities in a certain region or country.
Good data quality can be assumed for the currently listed drugs derived from DILI cases because most of these were provided by registry and clinical studies with a prospective study protocol using RUCAM early in the assessment approach (Table 10) (Teschke, 2018d). This is an important point to be reiterated because the prospective use of RUCAM facilitates early collection of complete data that allow for desired high-causality gradings of highly probable or probable. Apart from these advantages, prospective studies using RUCAM allow for homogeneity of study cohorts, in which real DILI cases are included not confounded by cases with alternative diagnosis that have nothing to do with drugs and related liver injury (Danan and Teschke, 2016; Teschke and Danan, 2018c).
Biomarkers, DILI, and RUCAM
For confirming the diagnosis of idiosyncratic DILI in future suspected cases, a new and valid biomarker would be highly appreciated by the DILI community. For this purpose, there is an urgent need having case series at hands with DILI cases that have a valid diagnosis based on the use of a validated CAM (Teschke et al., 2017b), best achieved by using RUCAM (Danan and Teschke, 2016) and putting aside disputed subjective global introspection or opinion-based unstructured vague approaches lacking defined elements and respective scores (Teschke and Danan, 2018b).
In collaboration with IMI (Innovative Medicines Initiative) projects and more precisely the SAFE-T (Safer and Faster Evidence-based Translation) consortium, EMA (European Medicines Agency) presented a letter for support of DILI biomarker, addressing again various clinical and regulatory issues related to biomarkers in the setting of DILI (EMA, 2016). The focus was on the unavailability of clinical tests, sensitive and specific enough to validly establish the diagnosis of idiosyncratic DILI, and also to predict and monitor its clinical course. It was mentioned that current tools were limited and considered as a major hurdle in drug development if questions of liver injury are to be answered. Consensus exists among DILI experts that for clinical trials, specific DILI biomarkers have to be developed, with desired characteristics as outlined by EMA: 1) early or earlier detection of DILI as compared to current methods, 2) usability to predict DILI outcome and risk of severe DILI including acute liver failure, 3) monitoring of progression and regression of DILI, 4) assessment of liver adaptation as opposed to liver injury, and 5) searching for early intrinsic liver injury in clinical trials. It is of note that several heavily promoted biomarkers received critical comments in the past (Fontana, 2014), which is discussed in detail previously (Teschke et al., 2017b). A recent report on biomarkers focused on GLDH (Glutamate dehydrogenase) and provided an update of current knowledge in the DILI field (Church et al., 2019).
The EMA letter also called for biomarkers that could be used for early diagnosis of idiosyncratic DILI (EMA, 2016; Teschke et al., 2017b), with focus on CK-18 (Cytokeratin-18), microRNA-122 (microarray RNA-122), total HMGB-1 (High Mobility Group Box protein-1), GLDH, SDH (Sorbitol dehydrogenase), which is proposed as a marker for hepatocyte necrosis, and ccCK-18 (caspase-cleaved CytoKeratin-18), which is proposed as a marker for apoptosis (Table 9). Hyperacetylated HMGB-1 and MCSFR-1 (Macrophage colony-stimulating factor receptor-1) were proposed as markers for immune activation (Table 9) (EMA, 2016). Additional considerations focused on critically viewed M-30 (apoptosis), M-65 (apoptosis/necrosis), and microRNA-192 (unspecified liver damage) (Fontana, 2014). A recent report on proteomics analysis of monocyte-derived hepatocyte-like cells is of potential interest as it identified integrin beta 3 as a specific biomarker for DILI by diclofenac (Dragoi et al., 2018), but some basic questions are awaiting clarification as briefly mentioned (Table 4). However, a major problem emerged on 15 April 2019 that has only partially reached the DILI community, requiring new considerations of the above points on diagnostic biomarkers and partial retractions of previous claims in a variety of publications. Indeed, there is scientific misconduction of the lead investigator who characterized the marker hyperacetylated HMGB-1 (EMA, 2019). Further clarifications are needed for final conclusions, which is certainly outside the scope of the current article.
Considering the number of potential biomarkers and the variability of clinical and mechanistic targets (Teschke et al., 2017b; Church et al., 2019), it will be difficult to find at least one biomarker meeting all the essential requirements such as specificities for liver injury and among the around 1,000 drugs, which are potentially dangerous to the liver. As it presently stands, the situation remains unclear if, on the one hand, the suspected idiosyncratic DILI case is not validated and, on the other hand, the so-called established diagnostic serum marker is far from being validated. So the current solution of this dilemma is the use of RUCAM, which is the only element among the three items that is well established and enables an individual causality assessment of the suspected DILI case (Figure 3). Therefore, the medical problem is certainly not solved presently through a biomarker but via a diagnostic algorithm if RUCAM is used.
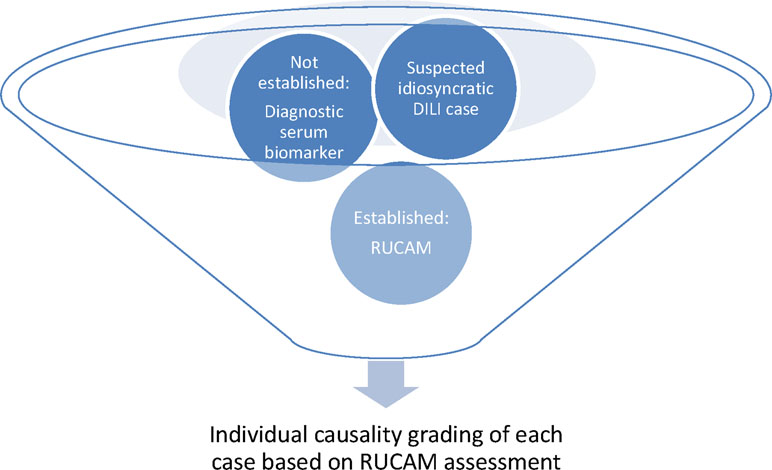
Figure 3 Valid causality assessment of idiosyncratic DILI using the established approach of RUCAM in the absence of a validated diagnostic serum biomarker. DILI, Drug induced liver injury; RUCAM, Roussel Uclaf Causality Assessment Method.
Occasionally, claims have been made that results obtained from genetic studies like those of HLA (human leucocyte antigen) genomes would represent diagnostic biomarkers of idiosyncratic DILI. This is certainly not correct because genetic data may represent risk factors but not diagnostic biomarkers. Prerequisite for both diagnostic biomarkers and risk factors is the need that is being derived from case series of RUCAM-based idiosyncratic DILI with high causality gradings like probable or highly probable.
Conclusions
Idiosyncratic DILI is a fascinating but challenging disease if it comes to clearly establishing its diagnosis. This requires intuition, expertise, and the use of a robust CAM such as RUCAM available in the updated version published in 2016. Even non-supporters of RUCAM from the US reportedly acknowledge that RUCAM is the most widely used CAM for assessing causality in suspected DILI cases. Alone within a short period from 2014 until early 2019, DILI and RUCAM experts published more than 46,266 DILI cases that had been evaluated by using RUCAM. A substantial number of DILI experts including DILIN members initially not known for their RUCAM enthusiasm are now authors of publications on RUCAM-based DILI cases, thereby promoting the idea of the universal use of RUCAM. There is presently no other CAM with such success story based on a rigorous clinical approach of the suspected case, and no other CAM has evidently outperformed RUCAM. Problems are rarely reported in connection with the use of RUCAM in DILI, and if present, the problems were not found at the level of RUCAM itself but rather were related to the users. Indeed, the current analysis of the publications reporting on these 46,266 cases shows that RUCAM performs well provided that the RUCAM users do a good job.
Best RUCAM-based results on DILI cases can be achieved if users take care of the following points:
1. The study protocol should be prospective to ensure completeness of case data;
2. Complete data are necessary to achieve highly probable and probable causality gradings obtained using RUCAM, essential conditions for describing correct DILI features and risk factors, and increasing the likelihood to find biomarkers that are liver specific and could be drug specific;
3. Careful presentation and use of the R value, type of liver injury, and selection of the correct RUCAM subscale;
4. Uniformity of the study cohort consisting of patients with idiosyncratic DILI, excluding all patients with intrinsic DILI, HILI, liver injury by dietary supplements, and nondrug alternative causes;
5. Transparent data presentation, including final RUCAM causality gradings and scores;
6. Short narratives and list of scored RUCAM elements in single case reports and small case series ≤10 cases;
7. Presentation of a diagnostic flow chart diagram including alternative causes;
8. Quantitative evaluation of the study case quality using scores or stars of the RDCQ system;
9. Analysis and discussion of results derived from DILI cases with RUCAM causality gradings of highly probable or probable, eliminating cases with a possible or lower causality grading and all cases with alternative causes. In essence, RUCAM benefits from its wide use and performs well provided that the users adhere at established rules to prevent confounding variability.
Author Contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of Interest Statement
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Abbara, A., Roe, J. K., Ghani, R., Collin, S. M., Ritchie, A., Kon, O. M., et al. (2017). Drug-induced liver injury from antituberculous treatment: a retrospective study from a large TB centre in the UK. BMC Infect. Dis. 17, 231. doi: 10.1186/s12879-017-2330-z
Aiso, M., Takikawa, H., Tsuji, K., Kagawa, T., Watanabe, M., Tanaka, A., et al. (2019). Analysis of 307 cases with drug-induced liver injury between 2010 and 2018 in Japan. Hepatol. Res. 49, 105–110. doi: 10.1111/hepr.13288
Alempijevic, T., Zec, S., Milosavljevic, T. (2017). Drug-induced liver injury: do we know everything? World J. Hepatol. 9, 491–502. doi: 10.4254/wjh.v9.i10.491
Alhaddad, O. M., Elsabaawy, M. M., Essa, M. S., Shaaban, A., Elsaharraawy, O., Rewisha, E., et al. (2017). Chronic drug-induced liver injury by Amoxicillin-Clavulanate. J. Hepatol. 3, 2. doi: 10.21767/2471-9706.100018
Amagon, K. I., Owodele, O., Akinsdele, A. J. (2017). Methionine and vitamin B-complex ameliorate antitubercular drugs-induced toxicity in exposed patients. Pharma. Res. Per. 5, e00360. doi: 10.1002/prp2.360
Andrade, R. J. (2017). Prospective European Drug-Induced Liver Injury Registry, PRO-EURO-DILI REGISTRY, 2017. Available at: ProEuroDILI Registry progress report year 1.pdf, referenced by: Teschke R, Danan G. Editorial. Drug-induced liver injury, mortality, and liver transplantation: is it reasonable to use a global introspection causality assessment? AME Med. J. 2, 144. doi: 10.21037/amj.2017.09.05
Andrade, R. J., Ortega-Alons, A., Lucena, M. (2016). Drug-induced liver injury clinical consortia: a global research response for a worldwide health challenge. Exp. Opin. Drug Metab. Toxicol. 12, 589–593. doi: 10.1517/17425255.2016.1141896
Baig, M., Wool, K. J., Halanych, J. H., Sarmad, R. A. (2015). Acute liver failure after initiation of Rivaroxaban: a case report and review of the literature. North Am. J. Med. Sci. 21, 407–410. doi: 10.4103/1947-2714.166221
Becker, M. W., Muller Lunardelli, M. J., Valle Tovo, C., Blatt, C. R. (2019). Drug and herb-induced liver injury: a critical review of Brasilian cases with proposals for the improvement of causality assessment using RUCAM. Ann. Hepatol. doi: 10.1016/j.aohep.2019.03.010
Benesic, A., Leitl, A., Gerbes, A. L. (2016). Monocyte-derived hepatocyte-like cells for causality assessment of idiosyncratic drug-induced liver injury. Gut 65, 1555–1563. doi: 10.1136/gutjnl-2015-309528
Bénichou, C. (1990). Criteria of drug-induced liver disorders. Report of an international consensus meeting. J. Hepatol. 11, 272–276. doi: 10.1016/0168-8278(90)90124-A
Bessone, F., Hermandez, N., Lucena, M. I., Andrade, R. J. (2016). The Latin American DILI registry experience: a successful ongoing collaborative strategic initiative. Int. J. Mol. Sci. 17, 313. doi: 10.3390/ijms17030313
Bessone, F., Hernandez, N., Mendizabal, M., Sanchez, A., Paraná, R., Arrese, M., et al. (2019). When the creation of a consortium provides useful answers: experience of The Latin American DILI Network (LATINDILIN). Clin. Liv. Dis., 13 (2), 51–57. doi: 10.1002/cld.778
Björnsson, E. S. (2014). Epidemiology and risk factors for idiosyncratic drug-induced liver injury. Semin Liver Dis. 34, 115–122. doi: 10.1055/s-0034-1375953
Björnsson, E. S. (2016a). Hepatotoxicity by drugs: the most common implicated agents. Int. J. Mol. Sci. 17, 224. doi: 10.3390/ijms17020224
Björnsson, E. S., Hoofnagle, J. H. (2016b). Categorization of drugs implicated in causing liver injury: critical assessment based on published case reports. Hepatology 63, 590–603. doi: 10.1002/hep.28323
Bohm, N., Makowski, C., Machado, M., Davie, A., Seabrook, N., Wheless, L., et al. (2014). Case report and cohort analysis of drug-induced liver injury associated with Daptomycin. Antimicrob. Agents Chemother. 58, 4902–4903. doi: 10.1128/AAC.03157-14
Cano-Paniagua, A., Amariles, P., Angulo, N., Restrepo-Garay, M. (2019). Epidemiology of drug-induced liver injury in a University Hospital from Colombia: updated RUCAM being used for prospective causality assessment. Ann. Hepatol. 18, 501–507.
Chalasani, N. P., Hayashi, P. H., Bonkovsky, H. L., Navarro, V. J., Lee, W. M., Fontana, R. J. (2014). Practice Parameters Committee of the American College of Gastroenterology. ACG Clinical Guideline: the diagnosis and management of idiosyncratic drug-induced liver injury. Am. J. Gastroenterol. 109, 950–966. doi: 10.1038/ajg.2014.131
Chalasani, N., Bonkovsky, H. L., Fontana, R., Lee, W., Stolz, A., Talwalkar, J., et al. (2015). Features and outcomes of 899 patients with drug-induced liver injury: the DILIN prospective study. Gastroenterology 148, 1340–1352. doi: 10.1053/j.gastro.2015.03.006
Chang, C. H., Chang, Y. C., Lee, Y. C., Liu, Y. C., Chuang, L. M., Lin, J. W. (2015). Severe hepatic injury associated with different statins in patients with chronic liver disease: a nationwide population-based cohort study. J. Gastroenterol. Hepatol. 30, 155–162. doi: 10.1111/jgh.12657
Chen, G. L., Hsiao, F. Y., Dong, Y. H., Shen, L. J., Wu, F. L. (2014). Statins and the risk of liver injury: a population-based case-control study. Pharmacoepidemiol. Drug Saf. 23, 719–725. doi: 10.1002/pds.3646
Cheetham, T. C., Lee, J., Hunt, C. M., Niu, F., Reisinger, S., Murray, R., et al. (2014). An automated causality assessment algorithm to detect drug-induced liver injury in electronic medical record data. Pharmacoepidemiol. Drug Saf. 23, 601–608. doi: 10.1002/pds.3531
Church, R. J., Kullack-Ublick, G. A., Aubrecht, J., Bonkovsky, H. L., Chalasani, N., Fontana, R. J., et al. (2019). Candidate biomarker for the diagnosis and prognosis of drug-induced liver injury: an international collaborator effort. Hepatology 69, 760–773. doi: 10.1002/hep.29802
Danan, G., Bénichou, C. (1993). Causality assessment of adverse reactions to drugs – I. A novel method based on the conclusions of international consensus meetings: application to drug-induced liver injuries. J. Clin. Epidemiol. 46, 1323–1330. doi: 10.1016/0895-4356(93)90101-6
Danan, G., Teschke, R. (2016). RUCAM in drug and herb induced liver injury: the update. Int. J. Mol. Sci. 17 (1). doi: 10.3390/ijms17010014
Danan, G., Teschke, R. (2018). Drug-induced liver injury: why is the Roussel Uclaf Causality Assessment Method (RUCAM) still used 25 years after its launch? Drug Saf. 41, 735–743. doi: 10.1007/s40264-018-0654-2
Danan, G., Teschke, R. (2019). Roussel Uclaf Causality Assessment Method for drug-induced liver injury: present and future. In: Special issue: Clinical drug induced liver injury: current diagnostic and mechanistic challenges, guest editors: Rolf Teschke, Gaby Danan, James H. Lewis. Front. Pharmacol. 10, 853. doi: 10.3389/fphar2019.00853
Das, S., Behera, S. K., Xavier, A. S., Velupula, S., Dkhar, S. A., Selvarajan, S. (2018). Agreement among different scales for causality assessment in drug-induced liver injury. Clin. Drug Invest. 38, 211–218. doi: 10.1007/s40261-017-0601-5
Dragoi, D., Benesic, A., Pichler, G., Kulak, N. A., Bartsch, H. S., Gerbes, A. L. (2018). Proteomics analysis of monocyte-derived hepatocyte-like cells identifies integrin beta 3 as a specific biomarker for drug-induced liver injury by diclofenac. Front. Pharmacol. 9, 699. doi: 10.3389/fphar.2018.00699
Douros, A., Bronder, E., Andersohn, F., Klimpel, A., Thomae, M., Sarganas, G., et al. (2014). Drug-induced liver injury: results from the hospital-based Berlin Case-Control Surveillance Study. Br. J. Clin. Pharmacol. 79, 988–999. doi: 10.1111/bcp.12565
EMA (2016). Letter of support for drug-induced liver injury (DILI) biomarker. EMA/423870/2016, edited Rassi, G.. Last updated: 30 September 2016. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/Other/2016/09/WC0021379.pdf Accessed 15 February 2019.
EMA (2019). Retraction of the Letter of support for drug-induced liver injury (DILI) biomarker (EMA/423870/2016) EMA website on 15 April 2019. Available at: https://www.europa.eu.documents/other/retraction-letter-support-drug-induced-liver-injury-dili-biomarker-ema/423870/2016_en.pdf. Accessed 15 April 2019.
Ferrajolo, C., Verhamme, K. M. C., Trifirò, G., Jong, G. W., Picelli, G., Giaquinto, C., et al. (2017). Antibiotic-induced liver injury in paediatric outpatients: a case-control study in primary care databases. Drug Saf. 40, 305–315. doi: 10.1007/s40264-016-0493-y
Fontana, R. J. (2014). Pathogenesis of idiosyncratic drug-induced liver injury and clinical perspectives. Gastroenterology 146, 914–928. doi: 10.1053/j.gastro.2013.12.032
Forner, D., Kulai, T., Arnason, T., Gruyhy, S. E., MacLeod, M. (2017). Ramipril-associated cholestasis in the setting of a recurrent drug-induced liver injury. Gastroenterol. Hepatol. Bed. Bench. 1, 143–146.
Giacomelli, A., Riva, A., Falvella, F. S., Oreni, M. L., Cattaneo, D., Stefania Cheli, S., et al. (2018). Clinical and genetic factors associated with increased risk of severe liver toxicity in a monocentric cohort of HIV positive patients receiving nevirapine-based antiretroviral therapy. BMC Inf. Dis. 18, 556. doi: 10.1186/s12879-018-3462-5
Hayashi, P. H., Barnhart, H. X., Fontana, R. J., Chalasani, N., Davern, T. J., Talwalkar, J. A., et al. (2015). Reliability of causality assessment for drug, herbal and dietary supplement hepatotoxicity in the Drug-Induced Liver Injury Network (DILIN). Liver Int. 35, 1623–1632. doi: 10.1111/liv.12540
Hayashi, P. H., Björnsson, E. S. (2018). Long-term outcomes after drug-induced liver injury. Curr. Hepatol. Rep. 17, 292–299. doi: 10.1007/s11901-018-0411-0
Hernández, N., Bessone, F., Sánchez, A., di Pace, M., Brahm, J., Zapata, R., et al. (2014). Profile of idiosyncratic drug induced liver injury in Latin America: an analysis of published reports. Ann. Hepatol. 13, 231–239. doi: 10.1016/S1665-2681(19)30886-5
Hornby, R. J., Lewis, P. S., Dear, J., Goldring, C., Park, B. K. (2014). MicroRNAs as potential circulating biomarkers of drug-induced liver injury: key current and future issues for translation to humans. Exp. Rev. Clin. Pharmacol. 7, 349–362. doi: 10.1586/17512433.2014.904201
Hunt, C. M. (2018). Editorial. Expanding our toolkit to better identify drug-induced liver injury in electronic medical records. Liver Int. 38, 585–587. doi: 10.1111/liv.13710
Khoury, T., Abu Rmeileh, A., Yosha, L., Benson, A. A., Daher, S., Mizrahi, M. (2015). Drug induced liver injury: review with a focus on genetic factors, tissue diagnosis, and treatment options. J. Clin. Transl. Hepatol. 3, 99–108. doi: 10.14218/JCTH.2015.00007
Kim, J. H., Choi, W. G., Lee, S., Lee, H. S. (2017). Revisiting the metabolism and bioactivation of ketoconazole in human and mouse using liquid chromatography-mass spectrometry-based metabolomics. Int. J. Mol. Sci. 18, 621. doi: 10.3390/ijms18030621
Kim, S. H., Naisbitt, D. J. (2016a). Update on advances in research on idiosyncratic drug-induced liver injury. Allergy Asthm. Immunol. Res. 8, 3–11. doi: 10.4168/aair.2015.8.1.3
Kim, W. S., Lee, S. S., Lee, C. M., Kim, H. J., Ha, C. Y., Kim, H. J., et al. (2016b). Hepatitis C and not hepatitis B virus is a risk factor for anti-tuberculosis drug induced liver injury. BMC Infect. Dis. 16, 50. doi: 10.1186/s12879-016-1344-2
Iorga, A., Dara, L., Kaplowitz, N. (2017). Drug-induced liver injury: cascade of events leading to cell death, apoptosis or necrosis. In: Special Issue. Molecular Research on Drug Induced Liver Injury, guest editors R. Teschke, and G. Danan. Int. J. Mol. Sci. 18, 1018. doi: 10.3390/ijms18051018
Kullak-Ublick, G. A., Andrade, R. J., Merz, M., End, P., Gerbes, A. L., Aithal, G. P. (2017). Drug-induced liver injury: recent advances in diagnosis and risk assessment. Gut 66, 1154–1164. doi: 10.1136/gutjnl-2016-313369
Kwon, J., Kim, S., Yoo, H., Lee, E. (2019). Nimesulide-induced hepatotoxicity: a systemic review and meta-analysis. PLoS One 14 (1), e0209264. doi: 10.1371/journal.pone.0209264
Lammel-Lindemann, J. A., Flores-Villalba, E., Martagón, A. J., Obeso-Gonzalez, E., Puente-Gallegos, F. (2018). Noncholestatic acute hepatocellular injury following candesartan administration. Br. J. Clin. Pharmacol. 84, 204–207. doi: 10.1111/bcp.13406
Li, X. L., Liu, X. C., Song, Y. L., Hong, R. T., Shi, H. (2018). Suspected drug-induced liver injury associated with iguratimod: a case report and review of the literature. BMC Gastroenterol. 18, 130. doi: 10.1186/s12876-018-0858-z
Liao, P. F., Wu, Y. K., Huang, K. L., Chen, H. Y. (2019). A rare case of cefepime-induced cholestatic liver injury. Tzu Chi. Med. J. 31, 124–128. doi: 10.4103/tcmj.tcmj_151_18
Licata, A., Minissale, M. G., Calvaruso, V., Craxi, A. (2017). A focus on epidemiology of drug-induced liver injury: analysis of a prospective study. Eur. Rev. Med. Pharmacol. Sci. 21 (1 Suppl), 112–121.
Lim, R., Choundry, H., Conner, K., Karnsakul, W. (2014). A challenge for diagnosing acute liver injury with concomitant/sequential exposure to multiple drugs: can causality assessment scales be utilized to identify the offending drug? Case Rep. Pediat. Article ID 156389. doi: 10.1155/2014/156389
Liu, Y., Li, P., Liu, L., Zhang, Y. (2018). The diagnostic role of miR-122 in drug-induced liver injury. A systematic review and meta-analysis. Medicine 97, 49. doi: 10.1097/MD.0000000000013478
Lu, R. J., Zhang, Y., Tang, F. L., Zheng, Z. W., Fan, Z. D., Zhu, S. M., et al. (2016). Clinical characteristics of drug-induced liver injury and related risk factors. Exp. Ther. Med. 12, 2606–2616. doi: 10.3892/etm.2016.3627
Marrone, G., Vaccaro, F. G., Biolata, M., Miele, L., Liguori, A., Araneo, C., et al. (2017). Drug-induced liver injury 2017: the diagnosis is not easy but always to keep in mind. Eur. Rev. Med. Pharmacol. Sci. 21 (1 Suppl), 122–134.
Matanovic, S. M. (2016). Changes to protocol in the regulation of adverse drug reactions –historical and current European view. Clin Res. Reg. Affairs 33, 49–58. doi: 10.3109/10601333.2016.1151610
McEuen, K., Borlak, J., Tong, W., Chen, M. (2017). Associations of drug lipophilicity and extent of metabolism with drug-induced liver injury. Int. J. Mol. Sci. 18, 1335. doi: 10.3390/ijms18071335
Medina-Caliz, I., Robles-Diaz, M., Garcia-Muñoz, B., Stephens, C., Ortega-Alonso, A., Garcia-Cortes, M., et al, Spanish DILI registry. (2016). Definition and risk factors for chronicity following acute idiosyncratic drug-induced liver injury. J. Hepatol. 65, 532–542. doi: 10.1016/j.jhep.2016.05.003
Meunier, L., Larrey, D. (2018). Viewpoint: recent advances in hepatotoxicity on non steroidal anti-inflammatory drugs. Ann. Hepatol. 17, 187–191. doi: 10.5604/01.3001.0010.8633
Morales, L., Vélez, N., Germán Munoz, O. (2016). Hepatoxicity: a drug-induced cholestatic pattern. Rev. Col. Gastroenterol. 31, 34–45.
Moreno, L., Sánchez-Delgado, J., Vergara, M., Casas, M., Miquel, M., Dalmau, B. (2015). Recurrent drug-induced liver injury (DILI) with ciprofloxacin and amoxillin/clavunate. Rev. Esp. Enferm. Dig. 107, 767–768. doi: 10.17235/reed.2015.3810/2015
Naiqiong, W., Liansheng, W., Zhanying, H., Yuanlin, G., Chenggang, Z., Ying, G., et al. (2017). A multicenter and randomized controlled trial of Bicyclol in the treatment of statin-induced liver injury. Med. Sci. Monit. 23, 5760–5766. doi: 10.12659/MSM.904090
Nicoletti, P., Aithal, G. P., Björnsson, E. S., Andrade, R. J., Sawle, A., Arrese, M., et al. (2017). International Drug-Induced Liver Injury Consortium (iDILIC). Association of liver injury from specific drugs or group of drugs with polymorphisms in HLA and other genes in a Genome-wide Association Study. Gastroenterology 152, 1078–1089. doi: 10.1053/j.gastro.2016.12.016
Nicoletti, P., Aithal, G. P., Chamberlain, T. C., Coulthard, S., Alshabeeb, M., Grove, J. I., et al. (2019). International Drug-Induced Liver Injury Consortium (iDILIC). Drug-induced liver injury due to Flucloxacillin: Relevance of multiple human leukocyte antigen alleles. Clin. Pharmacol. Ther. doi: 10.1002/cpt.1375
Niijima, K., Niijima, Y., Okada, S., Yamada, M. (2017). Drug-induced liver injury caused by Ipragliflozin administration with causality established by a positive lymphocyte transformation test (LTT) and the Roussel Uclaf Causality Assessment Method (RUCAM): a case report. Ann. Hepatol. 16, 308–311. doi: 10.5604/16652681.1231594
Ou, P., Chen, Y., Li, B., Zhang, M., Liu, X., Li, F., et al. (2015). Causes, clinical features and outcomes of drug-induced liver injury in hospitalized patients in a Chinese tertiary care hospital. SpringerPlus 4, 802. doi: 10.1186/s40064-015-1600-8
Ortega-Alonso, A., Stephens, C., Lucena, M. I., Andrade, R. J. (2016). Case characterization, clinical features and risk factors in drug-induced liver injury. Int. J. Mol. Sci. 17, 714. doi: 10.3390/ijms17050714
Patel, S., Mendler, M. H., Valasek, M. A., Tsunoda, S. M. (2018). Drug-induced liver injury associated with the use of Everolimus in a liver transplantant patient. Case Rep. Transpl. Article ID 7410508. doi: 10.1155/2018/7410508
Raschi, E., De Ponti, F. (2017). Drug-induced liver injury: towards early prediction and risk stratification. World J. Hepatol. 9, 30–37. doi: 10.4254/wjh.v9.i1.30
Rathi, C., Pipaliya, N., Patel, R., Ingle, M., Phadke, A., Sawant, P. (2017). Drug induced liver injury at a tertiary hospital in India: etiology, clinical features and predictors of mortality. Ann. Hepatol. 16, 442–450. doi: 10.5604/01.3001.0009.8600
Real, M., Barnhill, M. S., Higley, C., Rosenberg, J., Lewis, J. H. (2019). Drug-induced liver injury: highlights of the recent literature. Drug Saf. 42, 365–387. doi: 10.1007/s40264-018-0743-2
Regev, A., Seef, L. B., Merz, M., Ormardottir, S., Aithal, G. P., Gallivan, J., et al. (2014). Causality assessment for suspected DILI during clinical phases of drug development. Drug Saf. 37 (Suppl 1), S47–S56. doi: 10.1007/s40264-014-0185-4
Robles-Diaz, M., Gonzalez-Jimenez, A., Medina-Caliz, I., Stephens, C., Andrade, R. J., Lucena, M. I. (2016). Biomarker in DILI: one step forward. Front. Pharmacol. 7, 267. doi: 10.3389/fphar.2016.00267
Robles-Diaz, M., Gonzalez-Jimenez, A., Medina-Caliz, I., Stephens, C., García-Cortes, M., García-Muñoz, B., et al, Spanish DILI Registry, SLatinDILI Network (2015). Distinct phenotype of hepatotoxicity associated with illicit use of anabolic androgenic steroids. Aliment Pharmacol. Ther. 41, 116–125. doi: 10.1111/apt.13023
Russmann, S., Niedrig, D. F., Budmiger, M., Schmidt, C., Stieger, B., Hürlimann, S., et al. (2014). Rivaroxaban postmarketing risk of liver injury. J. Hepatol. 61, 293–300. doi: 10.1016/j.jhep.2014.03.026
Russo, M. W., Hoofnagle, J. H., Gu, J., Fontana, R. J., Barnhart, H., Kleiner, D., et al. (2014). Spectrum of statin hepatotoxicity: experience of the drug-induced liver injury network. Hepatology 60, 679–686. doi: 10.1002/hep.27157
Sarges, P., Steinberg, J. M., Lewis, J. H. (2016). Drug-induced liver injury: highlights from a review of the 2015 literature. Drug Saf. 39, 561–75. doi: 10.1007/s40264-016-0427-8
Schueller, F., Roy, S., Vucur, M., Trautwein, C., Luedde, T., Roderburg, C. (2018). The role of miRNAs in the pathophysiology of liver diseases and toxicity. Int. J. Mol. Sci. 19, 261. doi: 10.3390/ijms19010261
Senior, J. R. (2014). Evolution of the Food and Drug Administration approach to liver safety assessment for new drugs: current status and challenges. Drug Saf. 37 (Suppl 1), S9–S17. doi: 10.1007/s40264-014-0182-7
Seyfarth, H. J., Favreau, N., Tennert, C., Ruffert, C., Halank, M., Wirtz, H., et al. (2014). Genetic susceptibility to hepatoxicity due to bosentan treatment in pulmonary hypertension. Ann. Hepatol. 13, 803–809. doi: 10.1016/S1665-2681(19)30983-4
Shahbaz, O., Mahajan, S., Lewis, J. H. (2017). Highlights of drug- and herb-induced liver injury in the literature from 2016: how best to translate new information into clinical practice? Exp. Opin. Drug Metab. Toxicol. 13, 935–951. doi: 10.1080/17425255.2017.1362391
Shen, T., Liu, Y., Shang, J., Xie, Q., Li, J., Yan, M., et al. (2019). Incidence and etiology of drug-induced liver injury in Mainland China. Gastroenterology. 156, 2230–2241. doi: 10.1053/j.gastro.2019.02.002
Sobhonslidsuk, A., Poovorawan, K., Soonthornworasiri, N., Pan-Ngum, W., Phaosawasdi, K. (2016). The incidence, presentation, outcomes, risk of mortality and economic data of drug-induced liver injury from a national database in Thailand: a population-base study. BMC Gastroenterol. 16, 135. doi: 10.1186/s12876-016-0550-0
Tan, E. H., Low, E. X. S., Dan, Y. Y., Tai, B. C. (2018). Systematic review and meta-analysis of algorithms used to identify drug-induced liver injury (DILI) in health record databases. Liver Int. 38, 742–753. doi: 10.1111/liv.13646
Taneja, S., Kumar, P., Rathi, S., Duseja, A., Singh, V., Dhiman, R. K., et al. (2017). Acute liver failure due to Etodolac, a selective cyclogenase-2 (COX-2) inhibitor Non-steroidal anti-inflammatory drug established by RUCAM-based causality assessment. Ann. Hepatol. 16, 818–821. doi: 10.5604/01.3001.0010.2829
Tang, D. M., Koh, C., Twaddell, W. S., von Rosenvinge, E. C., Han, H. (2015). Acute hepatocellular drug-induced liver injury from Bupropion and Doxycycline. ACG Case Rep. J. 3, 66–68. doi: 10.14309/crj.2015.103
Tao, B., Chen, S., Lin, G., Yang, M., Lu, L., He, X., et al. (2018). Genetic polymorphisms of UGT 1A1 and susceptibility to anti-tuberculosis drug-induced liver: a RUCAM-based case-control study. Int. J. Immunopathol. Pharmacol. 32, 1–6. doi: 10.1177/2058738418816288
Terziroli Beretta-Piccoli, B., Mieli-Vergani, G., Bertoli, R., Mazzuccheli, L., Nofziger, C., Paulmichl, M., et al. (2017). Atovaquone/Proguanil-induced autoimmune-like hepatitis. Hepatol. Commun. 1, 293–298. doi: 10.1002/hep4.1039
Teschke, R., Andrade, R. (2015). Editorial. Drug-induced liver injury: expanding our knowledge by enlarging population analysis with prospective and scoring causality assessment. Gastroenterology 148, 1271–1273. doi: 10.1053/j.gastro.2015.04.027
Teschke, R., Danan, G. (2016a). Diagnosis and management of drug-induced liver injury (DILI) in patients with pre-existing liver disease. Drug Saf. 39, 729–744. doi: 10.1007/s40264-016-0423-z
Teschke, R., Larrey, D., Melchart, D., Danan, G. (2016b). Traditional Chinese Medicine (TCM) and herbal hepatotoxicity: RUCAM and the role of novel diagnostic biomarkers such as microRNAs. Medicines 3, 18. doi: 10.3390/medicines3030018
Teschke, R., Danan, G. (2017a). Editorial. Prospective Indian study of DILI with confirmed causality using the Roussel Uclaf Causality Assessment Method (RUCAM): a report of excellence. Ann. Hepatol. 16, 324–325. doi: 10.5604/16652681.1235471
Teschke, R., Schulze, J., Eickhoff, A., Danan, G. (2017b). Drug induced liver injury: can biomarkers assist RUCAM in causality assessment? Special issue: molecular research on drug induced liver injury. Int. J. Mol. Sci. 18, 803. doi: 10.3390/ijms18040803
Teschke, R., Danan, G. (2017c). Drug-induced liver injury: is chronic liver disease a risk factor and a clinical issue? Exp. Opin. Drug Metab. Toxicol. 13 (4), 425–438. doi: 10.1080/17425255.2017.1252749
Teschke, R. (2018a). Commentary. Drug- and herb-induced liver injury in 2016 with highly appreciated critical comments: related or not, that is the question! Clin. Diagn. Pathol. 2, 1–2. doi: 10.15761/CDP.1000122
Teschke, R., Danan, G. (2018b). “Causality assessment methods in drug-induced liver injury. In: Drug-induced Liver Toxicity (Chapter 27),” in Series: Methods in Pharmacology and Toxicology/Y. James Kang & David C. Casey. Eds. Chen, M., Will, Y. (Berlin Germany: Springer Protocols, Springer Nature), 555–594. In: Chen M and Will Y (ed), Drug-Induced Liver Toxicity, 1st ed. SpingerPlus, New York. doi: 10.1007/978-1-4939-7677-5_27
Teschke, R., Danan, G. (2018c). Review: drug induced liver injury with analysis of alternative causes as confounding variables. Br. J. Clin. Pharmacol. 84, 1467–1477. doi: 10.1111/bcp.13593
Teschke, R. (2018d). Review. Top-ranking drugs out of 3312 drug-induced liver injury cases evaluated by the Roussel Uclaf Causality Assessment Method. Exp. Opin. Drug Metab. Toxicol. 14, 1169–1187. doi: 10.1080/17425255.2018.1539077
Teschke, R., Zhu, Y. (2018e). Paracetamol (acetaminophen), alcohol, and liver injury: biomarkers, clinical issues, and experimental aspects. SL Pharmacol. Toxicol. 1, 113.
Teschke, R., Danan, G. (2019). “Drug induced liver injury,” in New Approach of Liver Diseases: Mechanism and Management. Eds. Radu-Ionita, F., Pyrsopoulos, N. T., Jinga, M., Tintoiu, I. C., Sun, Z., Bontas, E. (London: Springer Nature London Ltd.).
Tillmann, H. L., Barnhart, H. X., Serrano, J., Rockey, D. C. (2018). Novel approaches to causality adjudication in drug-induced liver disease. Curr. Hepatol. Rep. 17, 276–282. doi: 10.1007/s11901-018-0416-8
Veluswamy, R. R., Ward, S. C., Yum, K., Abramovitz, R. B., Isola, L. M., Jagannath, S., et al. (2014). Adverse drug reaction: pomalidomide-induced liver injury. Lancet 383, 2125–2126. doi: 10.1016/S0140-6736(14)61030-8
Visentin, M., Lenggenhager, D., Gai, Z., Kullak-Ublick, G. A. (2018). Drug-induced bile duct injury. Biochim. Biophys. Acta. 1864, 1498–1506. doi: 10.1016/j.bbadis.2017.08.033
Wang, H., Fu, J., Liu, G., Wang, L., Yan, A., Wang, G. (2017). Drug induced autoimmune hepatitis (DIAIH): pathological and clinical study. Biomed Res. 28, 6028–6034.
Wang, N. T., Huang, Y. S., Lin, M. H., Huang, B., Perng, C. L., Lin, H. C. (2016). Chronic hepatitis B infection and risk of antituberculosis drug-induced liver injury: systematic review and meta-analysis. J. Chin. Med. Assoc. 79, 368–374. doi: 10.1016/j.jcma.2015.12.006
Wang, S., Shangguan, Y., Ding, C., Li, P., Ji, Z., Shao, J., et al. (2018). Risk factors for acute liver failure among inpatients with anti-tuberculosis drug-induced liver injury. J. Int. Med. Res. 26, 300060518811512. doi: 10.1177/0300060518811512
Watkins, P. B. (2015). How to diagnose and exclude drug-induced liver injury. Dig. Dis. 33, 472–476. doi: 10.1159/000374091
Weiler, S., Merz, M., Kullak-Ublick, G. A. (2015). Drug-induced liver injury: the dawn of biomarkers? F1000Prime Rep. 7, 34. doi: 10.12703/P7-34
Yamashita, Y. I., Imai, K., Mima, K., Nakagawa, S., Hashimoto, D. (2017). Idiosyncratic drug-induced liver injury: a short review. Hepatol. Commun. 1, 494–500. doi: 10.1002/hep4.1064
Yang, J., Yu, Y. L., Jin, Y., Zhang, Y., Zheng, C. Q. (2016). Clinical characteristics of drug-induced liver injury and primary biliary cirrhosis. World J. Gastroenterol. 22, 7579–7586. doi: 10.3748/wjg.v22.i33.7579
Yu, Y. C., Mao, Y. M., Chen, C. W., Chen, J. J., Chen, J., Cong, W. M., et al. (2017). CSH guidelines for the diagnosis and treatment of drug-induced liver injury. Hepatol. Int. 11, 221–241. doi: 10.1007/s12072-017-9793-2
Zhu, Y., Niu, M., Chen, J., Zou, Z. S., Ma, Z. J., Liu, S. H., et al. (2016). Comparison between Chinese herbal medicine and Western medicine-induced liver injury of 1985 patients. J. Gastroenterol. Hepatol. 31, 1476–1482. doi: 10.1111/jgh.13323
Keywords: drug-induced liver injury (DILI), pharmacovigilance, Roussel Uclaf Causality Assessment Method (RUCAM), idiosyncratic DILI, intrinsic DILI, liver adaption
Citation: Teschke R (2019) Idiosyncratic DILI: Analysis of 46,266 Cases Assessed for Causality by RUCAM and Published From 2014 to Early 2019. Front. Pharmacol. 10:730. doi: 10.3389/fphar.2019.00730
Received: 02 April 2019; Accepted: 05 June 2019;
Published: 23 July 2019.
Edited by:
Ralf Weiskirchen, RWTH Aachen Universität, GermanyReviewed by:
Robert A. Roth, Michigan State University, United StatesGerd A. Kullak-Ublick, University of Zurich, Switzerland
Laura James, University of Arkansas for Medical Sciences, United States
Copyright © 2019 Teschke. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rolf Teschke, cm9sZi50ZXNjaGtlQGdteC5kZQ==
 Rolf Teschke
Rolf Teschke