- 1Department of Pharmacy, Children's Hospital of Fudan University, Shanghai, China
- 2Department of Nephrology, Children's Hospital of Fudan University, Shanghai, China
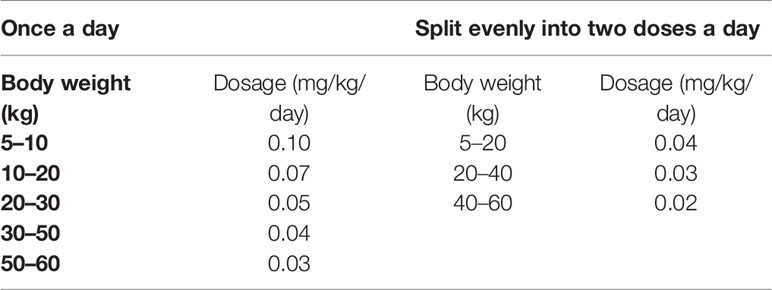
Sirolimus is already used in the treatment of tuberous sclerosis complex (TSC), however, with narrow therapeutic range and considerable inter- and intra-individual pharmacokinetic variability, making it hard to develop an appropriate sirolimus initial dosage regimen, especially in children with TSC. The aim of this study was to recommend the optimal sirolimus initial dosing regimen in pediatric patients with TSC. Underlying physiological and genetic factors were collected to explore the effects on clinical sirolimus concentrations by establishing a nonlinear mixed effect (NONMEM) model, and to further simulate the optimal sirolimus initial dosing regimen using Monte Carlo method in pediatric patients with TSC. The once-daily regimen and the twice-daily regimen were recommended, respectively. For once-daily regimen, the dosages of 0.10, 0.07, 0.05, 0.04, 0.03 mg/kg/day were recommended for children with weights of 5–10, 10–20, 20–30, 30–50, and 50–60 kg, respectively. For twice-daily regimen, the dosages of 0.04, 0.03, 0.02 mg/kg/day (the daily dose was divided evenly into two doses) were recommended for children with weights of 5–20, 20–40, 40–60 kg, respectively. The initial dosages of sirolimus in children with TSC were recommended for the first time.
Introduction
Tuberous sclerosis complex (TSC), a genetic autosomal dominant disorder, is caused by constitutive activation of mammalian target of rapamycin complex 1 (mTORC1) due to mutations in genes coding for hamartin (TSC1) or tuberin (TSC2) proteins, and its incidence is 0.10–0.17‰ (Osborne et al., 1991; Crino et al., 2006; Curatolo et al., 2008). The TSC1 or TSC2 genes pathogenic changes lead to upregulation of the mechanistic target of rapamycin (mTOR) signal pathway, in charge of synaptic plasticity, protein synthesis, cell growth, proliferation, differentiation, and migration, which has relationship with the formation of benign hamartomas in the brain, heart, liver, kidneys, lungs, skin and retina etc. (van der Poest Clement et al., 2020). Therefore, patients with TSC have constitutive activation of mTOR resulting in hamartomas in the above tissues (Ebrahimi-Fakhari et al., 2018).
Sirolimus, an mTOR inhibitor, has shown good effects on multiple manifestations of TSC, which has been approved for treating TSC (Franz and Capal, 2017). The biggest difference from other treatments for TSC is that sirolimus works directly on the potential pathogenesis of TSC, not its symptoms (Ebrahimi-Fakhari et al., 2019). However, with narrow therapeutic range and considerable inter- and intra-individual pharmacokinetic variabilities, making it hard to develop a sirolimus initial dosage regimen, especially in children with TSC. The aim of this study was to explore the effects of underlying physiological and genetic factors on clinical sirolimus concentrations by establishing a nonlinear mixed effect (NONMEM) model, and to further simulate the optimal sirolimus initial dosing regimen using Monte Carlo method in pediatric patients with TSC.
Methods
Patients
Pediatric patients from June 2016 to September 2019 at the Children's Hospital of Fudan University (Shanghai, China) were collected, retrospectively. Partial basic clinical dataset of some children were collected from a previous research (Wang et al., 2018). The criteria for inclusion were as follows: (i) aged <16 years old, (ii) diagnosed with TSC, (iii) treated by sirolimus, (iv) therapeutic drug monitoring (TDM) for sirolimus, (v) blood samples can be obtained for pharmacogenomics analysis. Exclusion criteria: patients with medications which effect sirolimus metabolism, mainly including CYP 3A4 inhibitors or inducers, and P-gp inhibitors or inducers. The study was approved by the Research Ethics Committee of Children's Hospital of Fudan University (Ethical code: [2019] 019). As for the study was retrospective and blood samples for pharmacogenomics analysis were leftover or discarded specimens from TDM, the analysis was approved by the ethics committee of our hospital without the need for written informed consent.
TDM and Pharmacogenomic Analysis
Sirolimus concentrations were tested with the Emit 2000 Sirolimus Assay (Siemens Healthcare Diagnostics Inc.) with range of linear response, 3.5–30 ng/ml, whose values of inter-assay variability [coefficient of variation (CV%)] <4.0%, and values of intra-assay CV (%) <6.2%.
The blood samples used for pharmacogenomic testing came from TDM residual samples, and the analysis was measured by Admera Health (Suzhou, China) with PGxOne®160 via the Illumina X10 Sequencing System. Hardy–Weinberg equilibrium was investigated with STATA computer software (version 12.0, Stata Corp LP, USA) and the value of P <0.05 was considered significant from a statistical point of view.
Population Pharmacokinetic Model
Dataset were used to build population pharmacokinetic model using the non-linear mixed-effects modeling software, NONMEM (edition 7, ICON Development Solutions, Ellicott City, MD, USA) and a first-order conditional estimation method with interaction (FOCE-I method). The pharmacokinetic parameters included apparent oral clearance (CL/F), volume of distribution (V/F), and absorption rate constant (Ka), whose value was fixed at 0.485/h (Wang et al., 2018; Wang et al., 2019a).
Random Effect Model
Equation (1) showed the inter-individual variability:
Pi was on behalf of the individual parameter value and TV(P) represented the typical individual parameter value. ηi was symmetrical distribution, which was random term with zero mean and variance omega2 (ω2).
Equation (2) showed the random residual variability:
OBSi was the observed concentration, PREi was the individual predicted concentration and ϵ1 and ϵ2 were symmetrical distribution, which was random term with zero mean and variance sigma2 (σ2).
Covariate Model
Equation (3) showed the relation of pharmacokinetic parameters with weight:
Pi represented the i-th individual parameter, Wi represented the i-th individual weight. Wstd was the standard weight of 70 kg. Pstd was the typical individual parameter, whose weight was Wstd. index was the allometric coefficient: 0.75 for the CL/F and 1 for the V/F (Anderson and Holford, 2008).
Equations (4) showed pharmacokinetic parameters and genotype:
Equations (5) and (6) showed pharmacokinetic parameters and the other continuous covariates or categorical covariates, respectively:
Pi was the individual parameter value, TV(P) was the typical individual parameter value. θ was the parameter to be estimated and Covi was the covariate of the i-th individual. Covmedian was the population median for the covariate.
Changes of objective function value (OFV) was calculated using covariate inclusions and a decrease in the OFV >3.84 (P < 0.05, degree of freedom = 1) was used as a criterion for inclusion of the covariate in the base model. When a full regression model was built, the model was further testified by dropping the covariate from each parameter one at a time to acquire the final model. An increase in the OFV >6.64 (P < 0.01, degree of freedom = 1) was used as a criterion for retaining significant covariate–parameter relationships in the model (Wang et al., 2020).
Model Evaluation
The final model was estimated by individual plots, distribution of weighted residuals for model (density vs. weighted residuals, and quantiles of weighted residuals vs. quantiles of normal), goodness-of-fit plots of model (observations vs. population predictions, observations vs. individual predictions, absolute value of weighted residuals of individual (│iWRES│) vs. individual predictions, weighted residuals vs. time), and visual predictive check (VPC) of model. In addition, bootstrap method was used to repeated random sampling with replacement from the raw data base with 1,000 repetitions with different random sampling. The medians and 2.5th–97.5th percentiles of the results from bootstrap were used for comparing with final model parameters.
Simulation
The influence of sirolimus initial doses on the probability to achieve the target concentration (5–15 ng/ml) (MacKeigan and Krueger, 2015; Nathan et al., 2015) were simulated by Monte Carlo method based on a once-daily regimen or a twice-daily regimen. In every case, 1,000 virtual patients were simulated in each of the seven weight groups (5, 10, 20, 30, 40, 50, and 60 kg) and for ten doses (0.01, 0.02, 0.03, 0.04, 0.05, 0.06, 0.07, 0.08, 0.09, and 0.10 mg/kg/day). The twice-daily regimen was split evenly into two doses a day.
Results
Patient Data
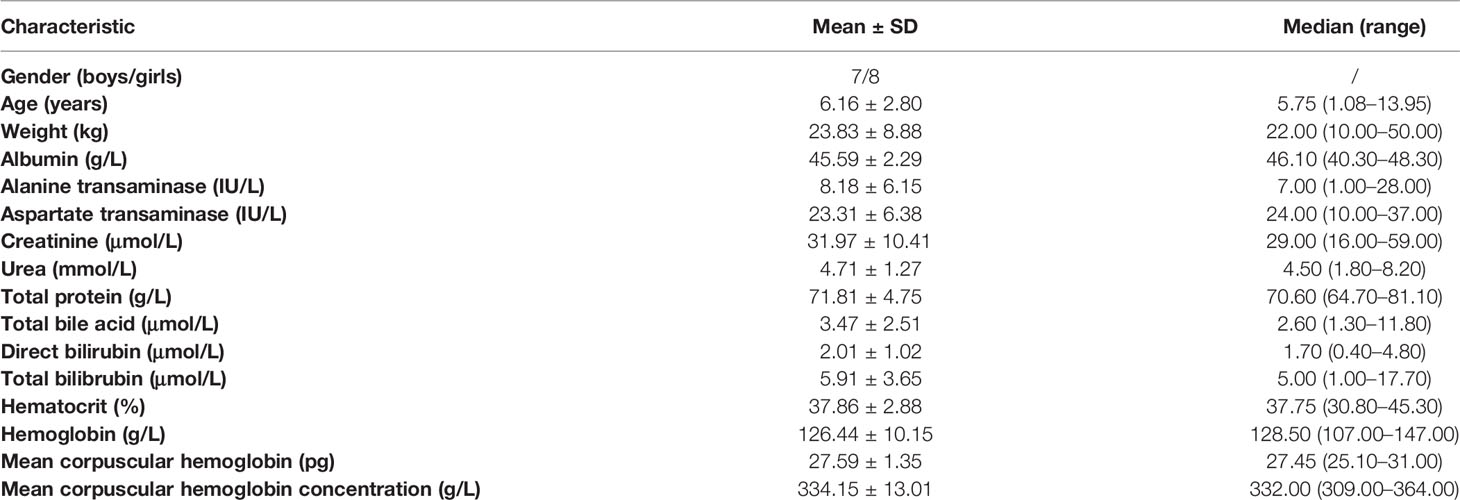
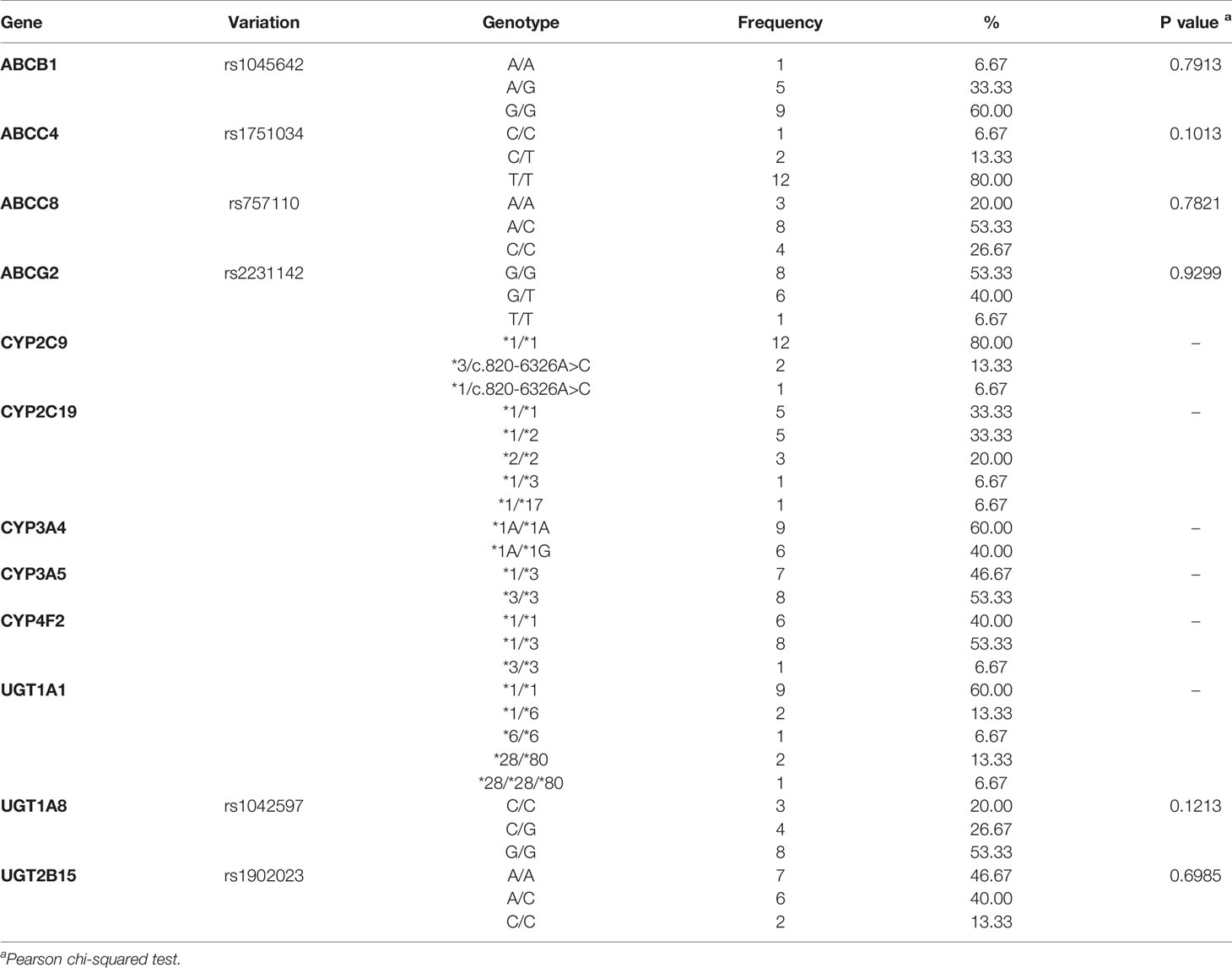
A total of 15 children with TSC, included seven boys and eight girls and whose ages were from 1.08 to 13.95 years old. The demographic data of patients was shown in Table 1. Partial basic clinical dataset of some children were collected from a previous research (Wang et al., 2018). Table 2 showed pharmacogenetics analysis and Hardy–Weinberg equilibrium. The P value of Pearson's Chi-squared test from every gene >0.05, showing Hardy–Weinberg equilibrium.
Modeling and Evaluation
The final population pharmacokinetics model was as follow:
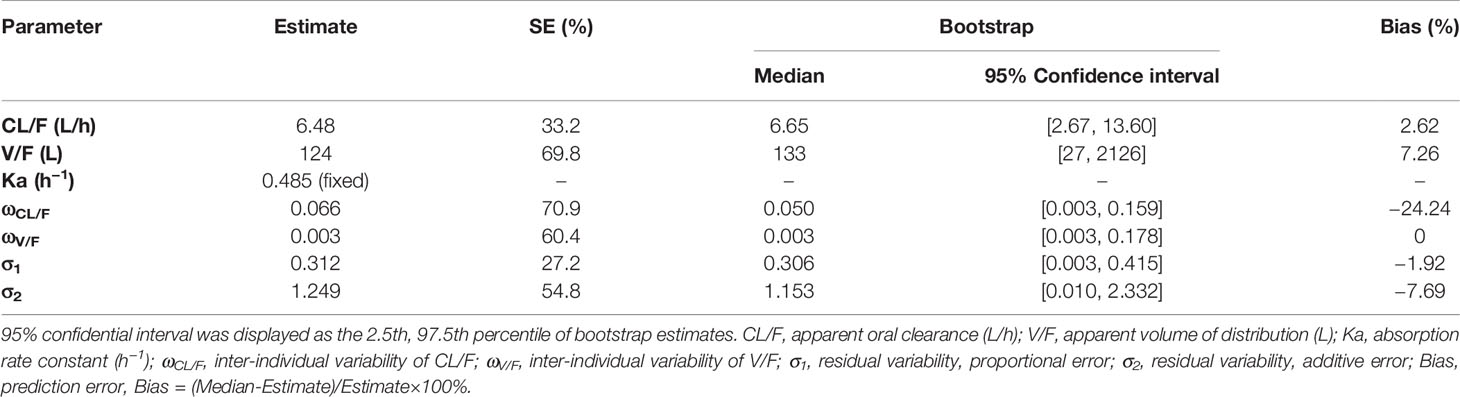
Figure 1A was individual plots of all 15 pediatric patients with TSC, demonstrating acceptable predictability from the perspective of clinical sparse data. Figure 1B was distribution of weighted residuals for final model and the distribution was normal. Figure 1C was goodness-of-fit plots of final model. Table 3 was parameter estimates of the final model and bootstrap validation. Figure 1D was VPC of final model and most of the observed sirolimus concentrations were within the 95% prediction intervals from the simulation data, indicating that the prediction-corrected concentrations were well predicted by the final model.
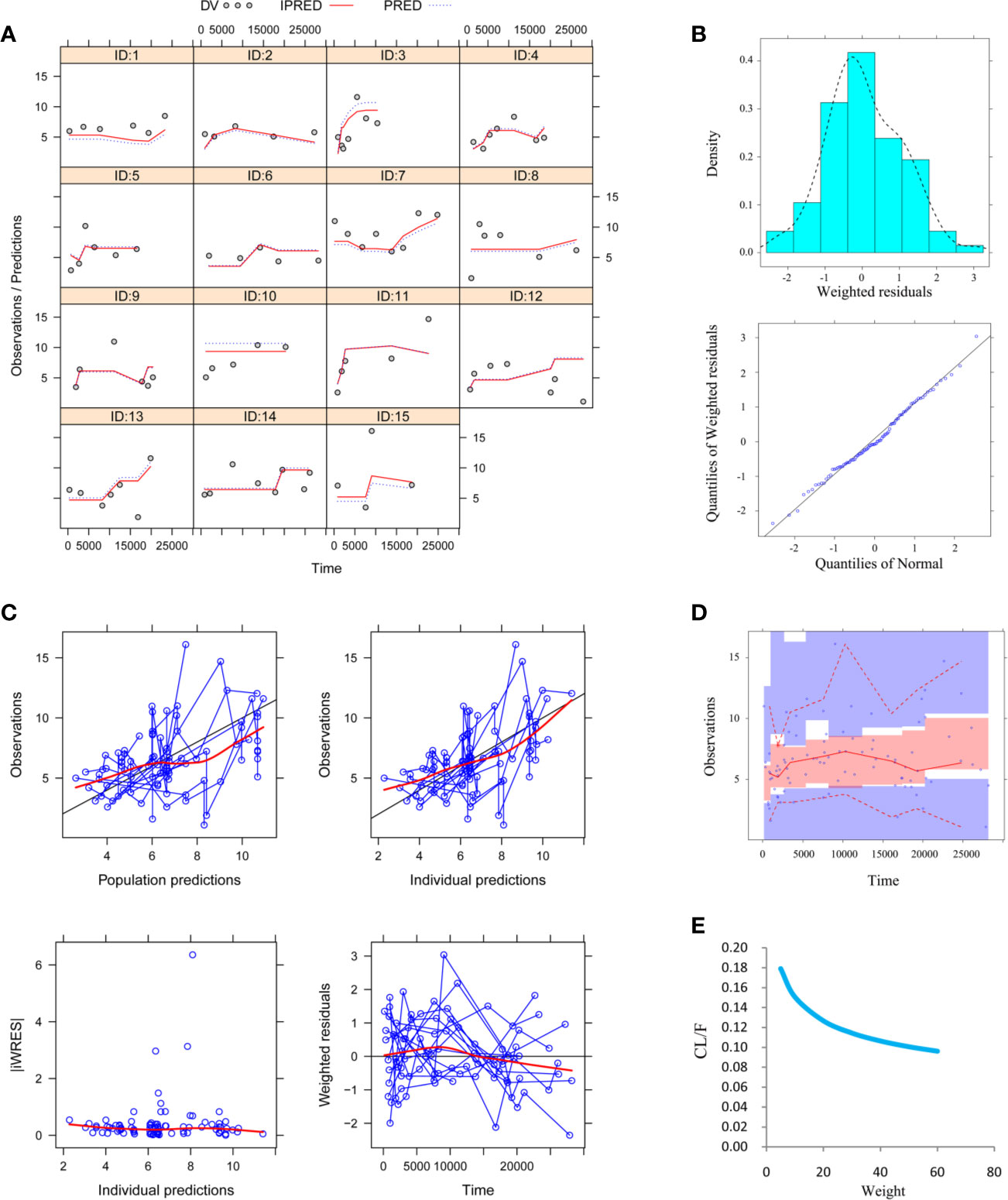
Figure 1 Model evaluation. (A) Individual plots. (B) Distribution of weighted residuals for model. Density vs. weighted residuals, and quantiles of weighted residuals vs. quantiles of normal. (C) Goodness-of-fit plots of model. Observations vs. population predictions, observations vs. individual predictions, absolute value of weighted residuals of individual (│iWRES│) vs. individual predictions, weighted residuals vs. time. (D) Visual predictive check (VPC) of model. The middle solid line represents the median of the prediction-corrected concentrations. The lower and upper dashed lines are the 2.5th and 97.5th percentiles of the prediction-corrected concentrations. (E) Sirolimus apparent clearance rate (CL/F, L/h/kg) of pediatric tuberous sclerosis complex patients with different weight. Partial concentration values were collected in a previous study (Wang et al., 2018).
Simulation
Figure 1E was the clearance rate of sirolimus in children with TSC of different weights and we found that clearance rate range was about 0.18–0.10 L/h/kg from children with weight of 5–60 kg. According to the final model, we carried out the simulation. Based on a once-daily regimen or a twice-daily regimen, we simulated two sirolimus initial dosing regimens, as shown in Figure 2 (a once-daily regimen) and Figure 3 (a twice-daily regimen). The probability of reaching the target concentrations (5–15 ng/ml)(MacKeigan and Krueger, 2015; Nathan et al., 2015) and the 95% confidence interval of sirolimus concentrations were both considered, in other words, it was necessary to consider both safety and effectiveness. Finally, as shown in Table 4, for once-daily regimen, the dosages of 0.10, 0.07, 0.05, 0.04, 0.03 mg/kg/day were recommended for children with weights of 5–10, 10–20, 20–30, 30–50, and 50–60 kg, respectively; for twice-daily regimen, the dosages of 0.04, 0.03, 0.02 mg/kg/day (the daily dose was divided evenly into two doses) were recommended for children with weights of 5–20, 20–40, 40–60 kg, respectively.
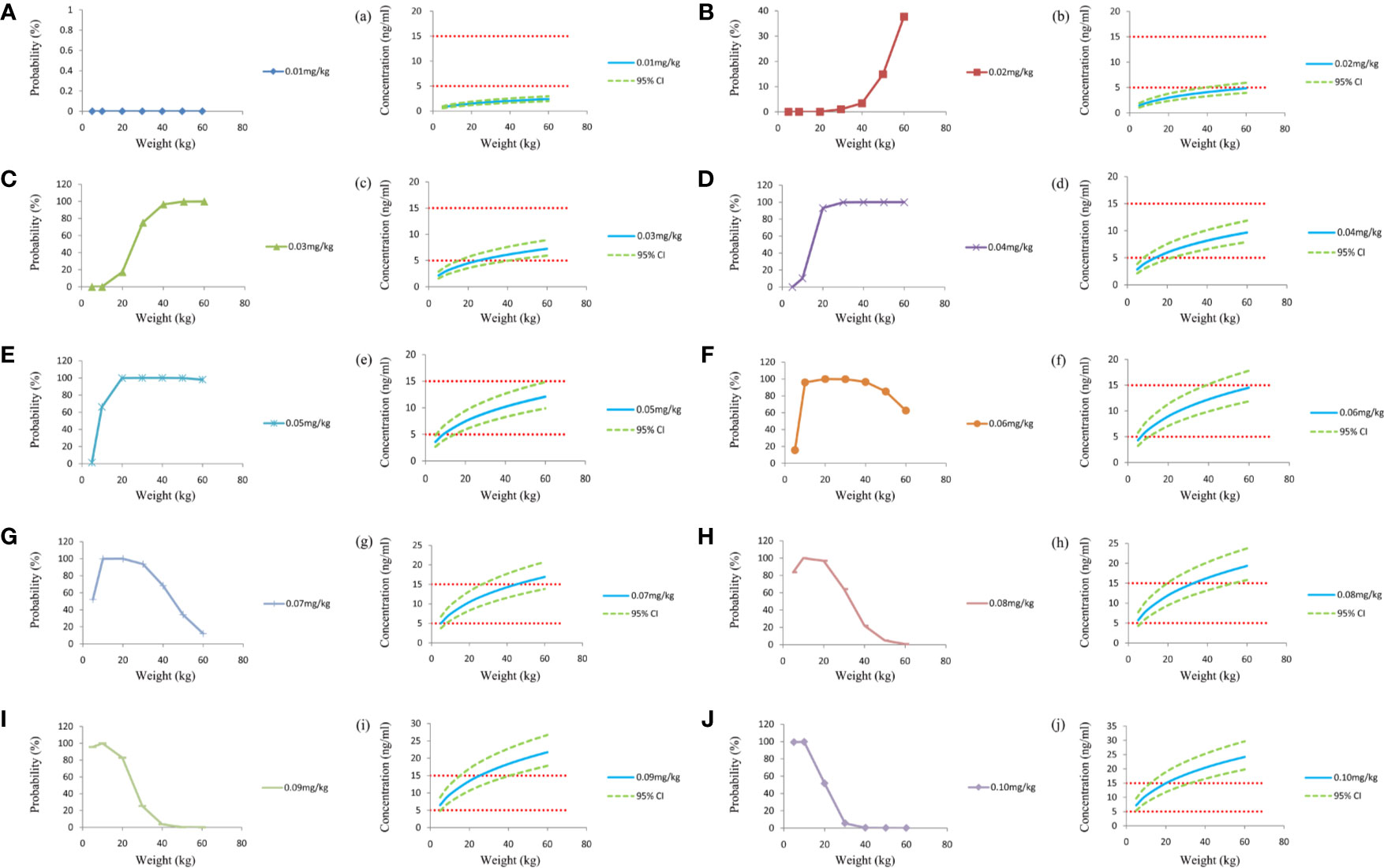
Figure 2 Simulation of sirolimus concentrations at different initial dosages once a day. (A–J) The probability to achieve the target concentration (5–15 ng/ml) at different initial dosages. a–j, sirolimus concentrations at different initial dosages. CI, confidence interval.
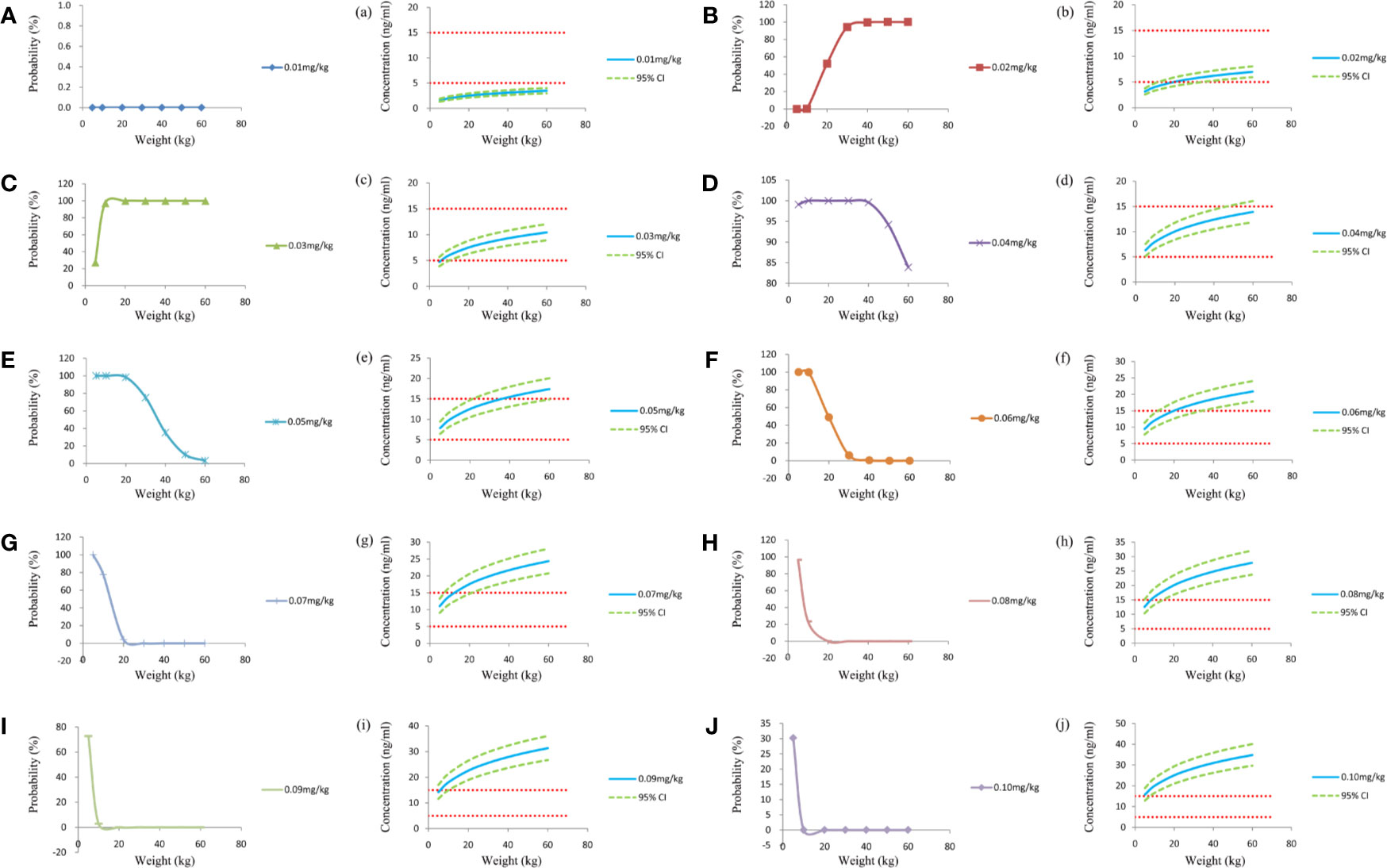
Figure 3 Simulation of sirolimus concentrations at different initial dosages which were split evenly into two doses a day. (A–J) The probability to achieve the target concentration (5–15 ng/ml) at different initial dosages. a–j, sirolimus concentrations at different initial dosages. CI, confidence interval.
Discussion
Sirolimus, also known as rapamycin, is a macrolide antibiotic immunosuppressant, which has been widely used for liver transplantation (Song et al., 2019; Zhang et al., 2019), kidney transplantation (Ferron et al., 1997; Jiao et al., 2009), kaposiform hemangioendothelioma (Wang et al., 2019a) etc. In addition, it was also been reported that sirolimus has been used for TSC (Franz and Capal, 2017). However, with narrow therapeutic range and considerable inter- and intra-individual pharmacokinetic variabilities, making it hard to develop a sirolimus initial dosage regimen, especially in children with TSC. In clinical practice, TDM was used to monitor sirolimus concentrations and further adjust the next dose according to the concentration results. However, the initial dose cannot be recommended by this method, traditional TDM.
Fortunately, the combination of population pharmacokinetics and Monte Carlo simulation can successfully predict and recommend the best initial dosing regimen, the method has been widely used in clinical practice (Niu et al., 2019; Ren et al., 2019; Tang et al., 2019; Wang et al., 2019b). For example, Ren et al. (2019) reported population pharmacokinetics of voriconazole and optimization of dosage regimens based on Monte Carlo simulation in patients with liver cirrhosis, Niu et al. (2019) reported that population pharmacokinetics and dosing regimen optimization of lopinavir in Chinese adults infected with HIV, Wang et al. (2019b) reported population pharmacokinetics and initial dosing regimen optimization of cyclosporin in pediatric hemophagocytic lymphohistiocytosis patients, Tang et al. (2019) reported population pharmacokinetics and dosing optimization of amoxicillin in neonates and young infants. Based on these studies, the present study was to establish a population pharmacokinetics model of sirolimus in pediatric patients with TSC, and to further simulate the optimal sirolimus initial dosing regimen using Monte Carlo method.
In our final model, body weight was included as a covariate in models that affected sirolimus clearance. As many studies have reported, there was a non-linear relationship between drug clearance and body weight in pediatric patients, and it may be well described with allometric scaling using a coefficient of 0.75 for clearance and 1 for volume (Anderson and Holford, 2008; Hao et al., 2018). It is well known that the polymorphism of CYP3A4 and CYP3A5 affect sirolimus metabolism among adults to some extent (Tamashiro et al., 2017; Zhang et al., 2017). However, interestingly, during our modeling process, the polymorphism of CYP3A4 and CYP3A5 were not successfully included as covariates based on our sirolimus concentrations in clinical practice from pediatric patients with TSC. The main reason may be that our population of children has a wide age span, and the gene expression in different age development process is developmentally dependent and the expression levels of CYP3A isoforms were highly variable after birth (Lacroix et al., 1997). In other words, the activity of drug metabolizing enzymes of the same CYP3A genotype may be different in different age groups and genotypes may not accurately explain the differences from sirolimus concentrations in present study. It's not independent, in Mizuno et al.'s (Mizuno et al., 2017a), population pharmacokinetics of temsirolimus and sirolimus in children with recurrent solid tumors: a report from the children's oncology group, genotypes were not included in the final model. Besides, in another study, developmental pharmacokinetics of sirolimus: implications for precision dosing in neonates and infants with complicated vascular anomalies, genotypes were also not included (Mizuno et al., 2017b). Most importantly, the pharmacogenomics of sirolimus is not routinely tested in clinical pediatric pharmacotherapy, and the weight-based dose recommendation in our final model is more appropriate and convenient and has better clinical practice value.
Based on a once-daily regimen or a twice-daily regimen, we simulated two initial dosing regimens. The probability of reaching the target concentrations (5–15 ng/ml) (MacKeigan and Krueger, 2015; Nathan et al., 2015) and the 95% confidence interval were both considered. For once-daily regimen, the dosages of 0.10, 0.07, 0.05, 0.04, 0.03 mg/kg/day were recommended for children with weights of 5–10, 10–20, 20–30, 30–50, and 50–60 kg, respectively; for twice-daily regimen, the dosages of 0.04, 0.03, 0.02 mg/kg/day (the daily dose was divided evenly into two doses) were recommended for children with weights of 5–20, 20–40, 40–60 kg, respectively. We found that the twice-daily regimen increased the frequency of use, but reduced the total use of sirolimus, which to some extent reduced the medical cost. Specific selection of one or two times a day for drug administration, the clinician or pharmacist can choose according to the actual clinical situation.
There were limitations in the present study, because of the low incidence of the TSC in children, the collection of patients was extremely difficult, which was also the objective reason for our small number of patients. In addition, the study is its retrospective nature and will be verified in future prospective studies.
Conclusion
We established a population pharmacokinetic model of sirolimus in pediatric patients with TSC and the initial dosages of sirolimus in children with TSC were recommended for the first time. Large-scale pediatric TSC population needs to be validated.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding authors.
Author Contributions
Z-PL and HX conceived and designed the study. D-DW, and XC collected the data. D-DW and XC built the model and evaluated the data. D-DW wrote the manuscript. XC reviewed and edited the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by Clinical Pharmacy Key Specialty Construction Project of Shanghai (No. YZ2017/5). Important Weak Subject Construction Project of Shanghai (No. 2016ZB0305). Scientific research project of Science and Technology Commission of Shanghai Municipality (No. 18DZ1910604). The China Scholarship Council (No. 201906100164).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Anderson, B. J., Holford, N. H. (2008). Mechanism-based concepts of size and maturity in pharmacokinetics. Annu. Rev. Pharmacol. Toxicol. 48, 303–332. doi: 10.1146/annurev.pharmtox.48.113006.094708
Crino, P. B., Nathanson, K. L., Henske, E. P. (2006). The tuberous sclerosis complex. N. Engl. J. Med. 355 (13), 1345–1356. doi: 10.1056/NEJMra055323
Curatolo, P., Bombardieri, R., Jozwiak, S. (2008). Tuberous sclerosis. Lancet 372 (9639), 657–668. doi: 10.1016/S0140-6736(08)61279-9
Ebrahimi-Fakhari, D., Mann, L. L., Poryo, M., Graf, N., von Kries, R., Heinrich, B., et al. (2018). Incidence of tuberous sclerosis and age at first diagnosis: new data and emerging trends from a national, prospective surveillance study. Orphanet. J. Rare Dis. 13 (1), 117. doi: 10.1186/s13023-018-0870-y
Ebrahimi-Fakhari, D., Agricola, K. D., Tudor, C., Krueger, D., Franz, D. N. (2019). Cannabidiol Elevates Mechanistic Target of Rapamycin Inhibitor Levels in Patients With Tuberous Sclerosis Complex. Pediatr. Neurol. 105, 597–561. doi: 10.1016/j.pediatrneurol.2019.11.017
Ferron, G. M., Mishina, E. V., Zimmerman, J. J., Jusko, W. J. (1997). Population pharmacokinetics of sirolimus in kidney transplant patients. Clin. Pharmacol. Ther. 61 (4), 416–428. doi: 10.1016/S0009-9236(97)90192-2
Franz, D. N., Capal, J. K. (2017). mTOR inhibitors in the pharmacologic management of tuberous sclerosis complex and their potential role in other rare neurodevelopmental disorders. Orphanet. J. Rare Dis. 12 (1), 51. doi: 10.1186/s13023-017-0596-2
Hao, G. X., Huang, X., Zhang, D. F., Zheng, Y., Shi, H. Y., Li, Y., et al. (2018). Population pharmacokinetics of tacrolimus in children with nephrotic syndrome. Br. J. Clin. Pharmacol. 84 (8), 1748–1756. doi: 10.1111/bcp.13605
Jiao, Z., Shi, X. J., Li, Z. D., Zhong, M. K. (2009). Population pharmacokinetics of sirolimus in de novo Chinese adult renal transplant patients. Br. J. Clin. Pharmacol. 68 (1), 47–60. doi: 10.1111/j.1365-2125.2009.03392.x
Lacroix, D., Sonnier, M., Moncion, A., Cheron, G., Cresteil, T. (1997). Expression of CYP3A in the human liver–evidence that the shift between CYP3A7 and CYP3A4 occurs immediately after birth. Eur. J. Biochem. 247 (2), 625–634. doi: 10.1111/j.1432-1033.1997.00625.x
MacKeigan, J. P., Krueger, D. A. (2015). Differentiating the mTOR inhibitors everolimus and sirolimus in the treatment of tuberous sclerosis complex. Neuro Oncol. 17 (12), 1550–1559. doi: 10.1093/neuonc/nov152
Mizuno, T., Fukuda, T., Christians, U., Perentesis, J. P., Fouladi, M., Vinks, A. A. (2017a). Population pharmacokinetics of temsirolimus and sirolimus in children with recurrent solid tumours: a report from the Children's Oncology Group. Br. J. Clin. Pharmacol. 83 (5), 1097–1107. doi: 10.1111/bcp.13181
Mizuno, T., Fukuda, T., Emoto, C., Mobberley-Schuman, P. S., Hammill, A. M., Adams, D. M., et al. (2017b). Developmental pharmacokinetics of sirolimus: Implications for precision dosing in neonates and infants with complicated vascular anomalies. Pediatr. Blood Cancer 64 (8) e26458. doi: 10.1002/pbc.26470
Nathan, N., Wang, J. A., Li, S., Cowen, E. W., Haughey, M., Moss, J., et al. (2015). Improvement of tuberous sclerosis complex (TSC) skin tumors during long-term treatment with oral sirolimus. J. Am. Acad. Dermatol. 73 (5), 802–808. doi: 10.1016/j.jaad.2015.07.018
Niu, W. J., Sun, T., Liu, L., Liu, X. Q., Zhang, R. F., Yin, L., et al. (2019). Population pharmacokinetics and dosing regimen optimisation of lopinavir in Chinese adults infected with HIV. Basic Clin. Pharmacol. Toxicol. 124 (4), 456–465. doi: 10.1111/bcpt.13154
Osborne, J. P., Fryer, A., Webb, D. (1991). Epidemiology of tuberous sclerosis. Ann. N. Y. Acad. Sci. 615, 125–127. doi: 10.1111/j.1749-6632.1991.tb37754.x
Ren, Q. X., Li, X. G., Mu, J. S., Bi, J. F., Du, C. H., Wang, Y. H., et al. (2019). Population Pharmacokinetics of Voriconazole and Optimization of Dosage Regimens Based on Monte Carlo Simulation in Patients With Liver Cirrhosis. J. Pharm. Sci. 108 (12), 3923–3931. doi: 10.1016/j.xphs.2019.09.019
Song, J., Du, G., Chen, W., Bao, P., Li, B., Lu, Q., et al. (2019). The advantage of Sirolimus in amplifying regulatory B cells and regulatory T cells in liver transplant patients. Eur. J. Pharmacol. 869, 172872. doi: 10.1016/j.ejphar.2019.172872
Tamashiro, E. Y., Felipe, C. R., Genvigir, F. D. V., Rodrigues, A. C., Campos, A. B., Hirata, R. D. C., et al. (2017). Influence of CYP3A4 and CYP3A5 polymorphisms on tacrolimus and sirolimus exposure in stable kidney transplant recipients. Drug Metab. Pers. Ther. 32 (2), 89–95. doi: 10.1515/dmpt-2016-0036
Tang, B. H., Wu, Y. E., Kou, C., Qi, Y. J., Qi, H., Xu, H. Y., et al. (2019). Population Pharmacokinetics and Dosing Optimization of Amoxicillin in Neonates and Young Infants. Antimicrob. Agents Chemother. 63 (2) e02336–18. doi: 10.1128/AAC.02336-18
van der Poest Clement, E., Jansen, F. E., Braun, K. P. J., Peters, J. M. (2020). Update on Drug Management of Refractory Epilepsy in Tuberous Sclerosis Complex. Paediatr. Drugs. 22 (1), 73–84. doi: 10.1007/s40272-019-00376-0
Wang, D. D., Lu, J. M., Li, Y. Z., Li, Q., Li, Z. P. (2018). Population pharmacokinetics of sirolimus in pediatric tuberous sclerosis complex: from Real World Study. Int. J. Clin. Exp. Med. 11 (11), 12302–12309.
Wang, D., Chen, X., Li, Z. (2019a). Population pharmacokinetics of sirolimus in pediatric patients with kaposiform hemangioendothelioma: A retrospective study. Oncol. Lett. 18 (3), 2412–2419. doi: 10.3892/ol.2019.10562
Wang, D. D., Ye, Q. F., Chen, X., Xu, H., Li, Z. P. (2019b). Population pharmacokinetics and initial dosing regimen optimization of cyclosporin in pediatric hemophagocytic lymphohistiocytosis patients. Xenobiotica, 50 (4), 435–441. doi: 10.1080/00498254.2019.1651419
Wang, D., Chen, X., Xu, H., Li, Z. (2020). Population pharmacokinetics and dosing regimen optimization of tacrolimus in Chinese pediatric hematopoietic stem cell transplantation patients. Xenobiotica 50 (2), 178–185. doi: 10.1080/00498254.2019.1601791
Zhang, J., Dai, Y., Liu, Z., Zhang, M., Li, C., Chen, D., et al. (2017). Effect of CYP3A4 and CYP3A5 Genetic Polymorphisms on the Pharmacokinetics of Sirolimus in Healthy Chinese Volunteers. Ther. Drug Monit. 39 (4), 406–411. doi: 10.1097/FTD.0000000000000415
Keywords: initial dosage, recommendation, sirolimus, children, tuberous sclerosis complex
Citation: Wang D-D, Chen X, Xu H and Li Z-P (2020) Initial Dosage Recommendation for Sirolimus in Children With Tuberous Sclerosis Complex. Front. Pharmacol. 11:890. doi: 10.3389/fphar.2020.00890
Received: 20 February 2020; Accepted: 29 May 2020;
Published: 11 June 2020.
Edited by:
Jeannine S. McCune, Beckman Research Institute, City of Hope, United StatesReviewed by:
Paolo Curatolo, University of Rome Tor Vergata, ItalyMichael Frost, Minnesota Epilepsy Group, United States
Copyright © 2020 Wang, Chen, Xu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hong Xu, aHh1QHNobXUuZWR1LmNu; Zhi-Ping Li, enBsaUBmdWRhbi5lZHUuY24=
†These authors have contributed equally to this work
 Dong-Dong Wang
Dong-Dong Wang Xiao Chen1†
Xiao Chen1† Zhi-Ping Li
Zhi-Ping Li