- 1Department of Pediatrics, Tangdu Hospital, Air Force Medical University, Xi’an, China
- 2Department of Neurosurgery, Tangdu Hospital, Air Force Medical University, Xi’an, China
Poisoning is a type of accidental injury and it is considered a major public health problem worldwide. Oral drug poisoning in children is an important cause of accidental injury and even death. It is a common critical emergency in the field of pediatrics. Once a child unintentionally takes an overdose, regardless of whether it caused poisoning or not, they should be admitted to the hospital for emergency treatment. Acute poisoning in children most frequently occurs through the digestive tract. Drug poisoning can happen in children of all ages. In children younger than 1 year, drug poisoning is mostly caused by the parents during feeding, while in children aged 1–3 years, it predominantly occurs as a result of an accident. A case of diagnosis and treatment of a child with diphenoxylate-atropine poisoning is reported herein. The early manifestation of this child was acute toxic encephalopathy with clinical manifestations of a coma, convulsions, and respiratory depression. A brain MRI showed extensive damage to the bilateral caudate nucleus, lenticular nucleus, parietal lobe, precuneus lobe, and occipital lobe. Accidental administration of a large dose of diphenoxylate results in severe clinical symptoms and can cause obvious diffuse brain damage.
Introduction
Diphenoxylate, also known as penehyclidine and cyanophenoxylate, is used in the treatment of acute and chronic functional diarrhea and chronic enteritis. The conventional therapeutic amount of this drug has no effect on the central nervous system (Murphy et al., 2009). However, diphenoxylate poisoning caused by improper dosage is relatively common, particularly in the population of children under 10-years-old. At doses significantly higher than the therapeutic amount, the occurrence of strong respiratory depression and coma is observed (Karim et al., 1972). Thus, diphenoxylate has been listed as one of the major harmful drugs in pediatrics (Shee and Pounder, 1980; Thomas et al., 2008). Even low doses of diphenoxylate can cause poisoning in children; therefore, it is not suitable for the treatment of diarrhea as a conventional drug. Nonetheless, some doctors may lack understanding of the side effects caused by the drug, which might lead to overdose and poisoning. Moreover, many families use diphenoxylate as a home remedy for diarrhea. The drug is available in the form of sugar-coated tablets; thus, improper storage often leads to serious symptoms of poisoning in infants and young children.
Case Presentation
A 3-year-old boy accidentally swallowed diphenoxylate-atropine on May 12, 2019. The quantity of the ingested drug was 35 tablets (each tablet contained diphenoxylate 2.5 mg and atropine 0.025 mg), which was confirmed by the parents. The patient experienced a respiratory arrest on the way to the hospital and recovered after cardiopulmonary resuscitation in the ambulance. In the pediatric emergency department, warm saline water was administered for gastric lavage until the liquid was clear, and the gastric tube was retained. Liquid paraffin was injected through the gastric tube for catharsis. Concurrently, warm saline solution and liquid paraffin enema were given to facilitate the discharge of diphenoxylate. Naloxone was administered to excite the respiratory center to fight against the respiratory depression caused by diphenoxylate overdose. On the second day of admission, the child was conscious and fluent in response to questions. However, on the third day of admission, the child suddenly experienced frequent generalized tonic-clonic seizures (GTCS) and subsequently developed status epilepticus. Midazolam was given as a continuous intravenous infusion of 10 μg/kg/min to control the seizures.
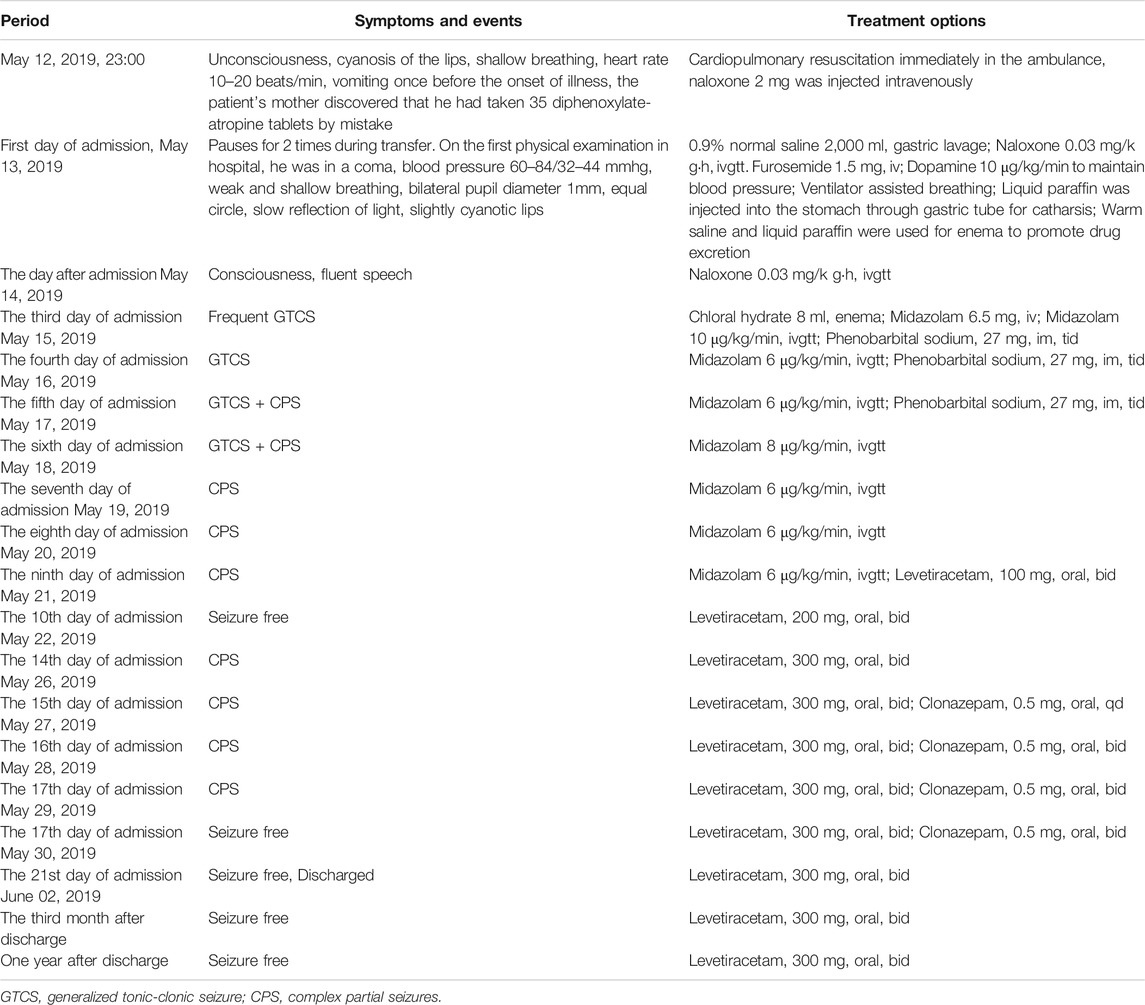
The body temperature was 37.7°C, and all blood results were within normal limits, except for the percentage of neutrophils (89.3% with the reference range of 31–40%). EEG showed numerous irregular high amplitude slow waves and sharp slow waves during the interictal period (Figure 1). No abnormalities were found in the head CT. The convulsions were difficult to manage; however, gradual control was achieved following combined use of a levetiracetam oral liquid. The diffusion-weighted imaging (DWI) of the head MRI revealed that the bilateral parietal lobe, precuneus, and occipital lobe exhibited brain-like hyperintensity, with apparent diffusion coefficient (ADC) values of 0.000644–0.000811 (Figures 2B,C).
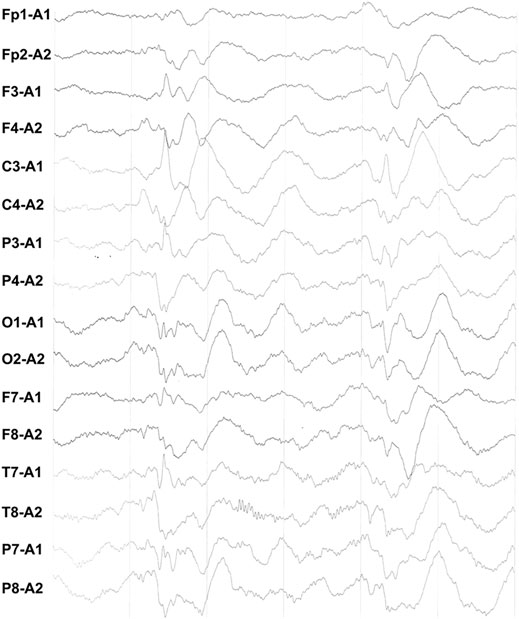
FIGURE 1. During interictal EEG, diffuse irregular high amplitude slow waves of bilateral symmetry were found.
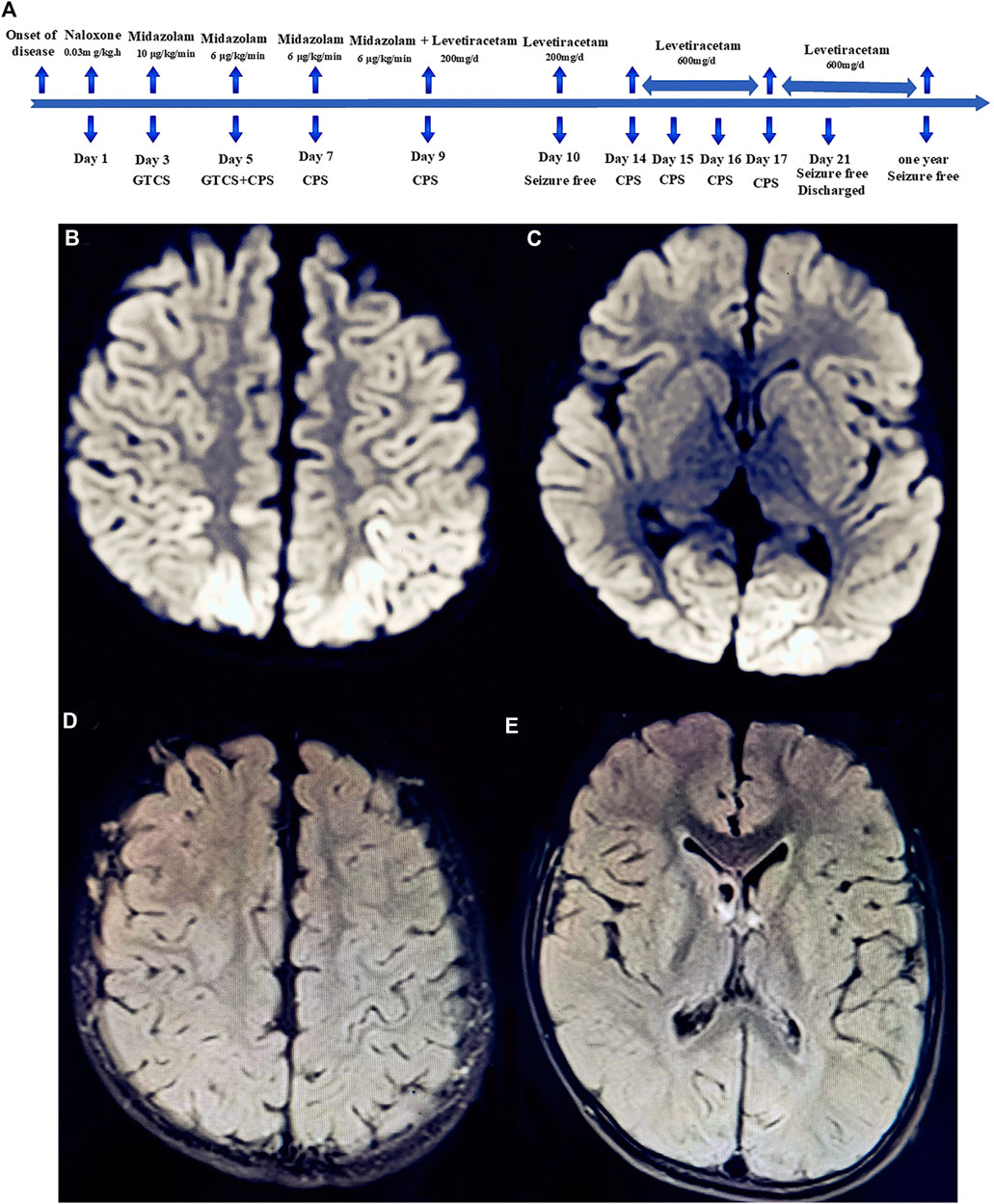
FIGURE 2. Timeline of the patient’s clinical course and outcome (A). Diffusion-weighted magnetic resonance imaging (DW-MRI) of the head showed abnormal high signal intensity in the bilateral parietal lobe (B), anterior wedge, and occipital lobe (C). Head MRI-DWI re-examined after 1 year of follow-up revealed that the abnormal signal intensity of brain gray matter disappeared completely (D,E).
On the fifth day of admission, the child developed complex partial seizures (CPS), with specific manifestations as follows: loss of consciousness, upward gaze, frequent blinking lasting for approximately 8–10 s, no limb tonic-clonic twitch, seizure frequency 2–4 times per day. Following the administration of a levetiracetam oral solution, the frequency of seizures was considerably reduced. CPS disappeared on the 10th day of admission, but reappeared on the 14th day. After 3 weeks of treatment, the child showed substantial clinical improvement. The boy was discharged from the hospital and took oral levetiracetam to prevent seizures. At a 12-months follow-up, the child felt good and experienced no seizures (Figure 2A). For the administration schedule, see Table 1. No abnormality was found in MRI-DWI (Figures 2D,E).
Discussion
A diphenoxylate-atropine overdose in children can lead to poisoning, which might be related to various physiological characteristics. On the one hand, the function of the blood-brain barrier in children is imperfect. Thus, the drug can easily produce an inhibitory effect on the central nervous system by passing through the blood-brain barrier. On the other hand, the liver function in children is immature; therefore, drug metabolism is slow and diphenoxylate can remain in the body for a long time.
Although the studied child underwent two gastric lavages, some of diphenoxylate-atropine was discharged into the intestines due to the excessive ingestion of the drug. Gastric lavage and catharsis did not lead to complete excretion. Consequently, diphenoxylate-atropine was absorbed in the intestines, which led to brain damage and seizures.
Anoxic-ischemic encephalopathy caused by diphenoxylate-atropine is the most likely diagnosis. There were some early discussions regarding the likely diagnosis. Due to multiple epileptic seizures and fever, the child was at first suspected to suffer from a central nervous system infection; however, this diagnosis was excluded following cerebrospinal fluid testing and continuous monitoring of the body temperature.
Diphenoxylate is one of the deadly single dose agents, which can cause accidental home poisoning in children (Euwema and Swanson, 2020). In the past, 10 children with acute diphenoxylate-atropine poisoning were admitted to our department. Nonetheless, the clinical manifestations of poisoning were predominantly mild and mainly included gastrointestinal symptoms. The degree of respiratory depression was minor. The clinical symptoms of this case were severe and could be related to the overdose ingestion of diphenoxylate-atropine. Diphenoxylate prolongs the transit time of the stomach and small intestine contents, and the drug absorption delay might cause secondary poisoning (Xiao et al., 2011). The characteristics of the MRI in the late stage were consistent with the manifestations of poisoning-induced hypoxic ischemic encephalopathy, and the degree of MRI lesions was highly correlated with clinical symptoms.
We have the following experience in the treatment of children with diphenoxylate poisoning. First, children suffering from diphenoxylate poisoning should be given regular gastric lavage because absorption might be delayed secondary to the inhibition of the gastrointestinal motility (Michael and Sztajnkrycer, 2004). A review by Thomas et al. demonstrated that diphenoxylate-atropine poisoning can cause serious complications, such as aspiration pneumonia, cerebral edema, and death (Thomas et al., 2008). In some cases, intact pill fragments were found 15–27 h after ingestion (Rumack and Temple, 1974; Wasserman et al., 1975; Thomas et al., 2008). Thus, once children accidentally swallow excessive amounts of diphenoxylate-atropine, gastric lavage and catharsis are required as soon as possible. In this case, after thorough gastric lavage, a gastric tube was inserted and liquid paraffin was used for catharsis. Second, timely administration of intravenous rehydration and diuretic drugs promotes the excretion of diphenoxylate. Third, the rescue drug for diphenoxylate poisoning is naloxone (McCarron et al., 1991). Early and appropriate continuous intravenous application of naloxone is the key to successful treatment of diphenoxylate poisoning. Children with severe poisoning were given naloxone 0.05–0.1 mg/kg. After the first injection, administration by intravenous drip infusion was performed at a rate of 10–20 μg/(kgh) for 2–3 days. The drug dosage was gradually reduced when the breathing was stable and the mind appeared clear. Administration of naloxone in children with severe poisoning should not be stopped too early. The drug should be administered repeatedly to avoid recurrence of respiratory depression. Finally, excessive intake of diphenoxylate might cause toxic encephalopathy; therefore, prophylactic administration of antiepileptic agents should be considered.
Conclusion
Overdose diphenoxylate-atropine ingestion often leads to secondary absorption in the intestines, which causes brain damage. Continuous intravenous administration of naloxone is necessary for severely poisoned children. Early gastric lavage and repeated catharsis are key to reducing impairment and disability. Naloxone should not be stopped early in the treatment of children with severe diphenoxylate-atropine poisoning. Safe storage of toxic drugs is an effective way to prevent accidental swallowing by children.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics Statement
The studies involving human participants were reviewed and approved by the Human Research Committee of Tangdu Hospital of the Fourth Military Medical University. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author Contributions
BL, LL, C-HW, YY, X-PQ, and L-JS participated in the whole process of patient diagnosis and treatment. BL and LL made the diagnosis and treatment plan. C-HW, YY, X-PQ, and L-JS participated in the whole follow-up process. BL, LL, C-HW, and L-JS contributed to writing of the manuscript.
Funding
This work was funded by National Natural Science Foundation of China (NSFC) (81971206).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank the patient's parents for providing permission to share the patient’s information.
References
Euwema, M. S., and Swanson, T. J. (2020). Deadly single dose agents. Treasure Island (FL): StatPearls Publishing.
Karim, A., Ranney, R. E., Evensen, K. L., and Clark, M. L. (1972). Pharmacokinetics and metabolism of diphenoxylate in man. Clin. Pharmacol. Ther. 13, 407–419. doi:10.1002/cpt1972133407
McCarron, M. M., Challoner, K. R., and Thompson, G. A. (1991). Diphenoxylate-atropine (Lomotil) overdose children: an update (report of eight cases and review of the literature). Pediatrics 87, 694–700.
Michael, J. B., and Sztajnkrycer, M. D. (2004). Deadly pediatric poisons: nine common agents that kill at low doses. Emerg. Med. Clin. North America. 22, 1019–1050. doi:10.1016/j.emc.2004.05.004
Murphy, R., Doerger, K. M., Nathan, M. A., and Lowe, V. J. (2009). Pretreatment with diphenoxylate hydrochloride/atropine sulfate (Lomotil) does not decrease physiologic bowel FDG activity on PET/CT scans of the abdomen and pelvis. Mol. Imaging Biol. 11, 114–117. doi:10.1007/s11307-008-0178-8
Shee, C. D., and Pounder, R. E. (1980). Loperamide, diphenoxylate, and codeine phosphate in chronic diarrhoea. Br Med J. 280, 524. doi:10.1136/bmj.280.6213.524
Thomas, T. J., Pauze, D., and Love, J. N. (2008). Are one or two dangerous? Diphenoxylate-atropine exposure in toddlers. J. Emerg. Med. 34, 71–75. doi:10.1016/j.jemermed.2007.03.051
Wasserman, G. S., Green, V. A., and Wise, G. W. (1975). Lomotil ingestions in children. Am. Fam. Physician. 11, 93–97.
Keywords: children, toxic encephalopathy, seizure, neuropharmacology, diphenoxylate-atropine
Citation: Wang C-H, Song L-J, Yang Y, Qu X-P, Lan L and Liu B (2021) Case Report: Multiple Seizures After a Diphenoxylate-Atropine Overdose in a Small Child. Front. Pharmacol. 12:646530. doi: 10.3389/fphar.2021.646530
Received: 27 December 2020; Accepted: 05 March 2021;
Published: 12 April 2021.
Edited by:
Kamil Musilek, University of Hradec Králové, CzechiaReviewed by:
Georg A. Petroianu, Khalifa University, United Arab EmiratesJosipa Vlainic, Rudjer Boskovic Institute, Croatia
Copyright © 2021 Wang, Song, Yang, Qu, Lan and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li Lan, NDE4ODkzODE5QHFxLmNvbQ==; Bei Liu, bGl1YmVpMjA2QDE2My5jb20=
†These authors have contributed equally to this work
 Chun-Hui Wang1†
Chun-Hui Wang1† Xiao-Peng Qu
Xiao-Peng Qu Bei Liu
Bei Liu