Abstract
Mood disorders, also often referred to as affective disorders, are a group of psychiatric illnesses that severely impact mood and its related functions. The high medical expenditures have placed a significant financial burden on patients and their families. Aromatherapy is an alternative and complementary treatment that utilizes essential oils (EOs) or volatile oils (VOs) to achieve major therapeutic goals. In general, EOs are volatile chemicals that enter the body primarily through skin absorption and/or nasal inhalation. In addition, they can work through oral administration. Inhalation aromatherapy has shown unique advantages for treating mood disorders, especially depression, anxiety and mental disorders such as sleep disorder, which have been validated over the last decade through clinical and animal studies. Accumulating evidence has shown that EOs or VOs can bypass the blood-brain barrier to target brain tissue through the nasal-brain pathway. Subsequently, they act on the cerebral cortex, thalamus, and limbic system in the brain to improve symptoms of anxiety, depression and improve sleep quality. Here, we review the natural aromatic plants’ volatiles or essential oils used commonly as adjuncts to manage mood disorders and illustrate the mechanisms of inhalation aromatherapy, and mainly summarized the application of transnasal inhalation aromatherapy in depression, anxiety, and sleep disorders. We conclude that aromatherapy does not cause side-effects, which is vastly different from commonly used psychotropic drugs. Inhalation aromatherapy via brain-targeted nasal delivery offers potentially efficacious treatment for mental disorders and merits further study.
Introduction
Mood disorders are affective mental disorders characterized by significant and persistent changes in emotion or state of mind (Marvel and Paradiso, 2004; Hasler, 2020). They can originate from psychological disorders, organic damage, nerve injury, side effects of medications used to treat physical or mental disorders, and chronic stress (Jorge and Arciniegas, 2014; Sanacora et al., 2022). The COVID-19 pandemic has severely aggravated the occurrence of mental illness and contributed significantly to the global increase in the prevalence of morbidity and disability (Vigo et al., 2016; COVID-19 Mental Disorders Collaborators, 2021). Studies on the global disease burden have revealed the severity of this ailment (Yun et al., 2016; Feigin et al., 2019). The pathogenesis of which are related to gene-environment interactions. In addition, they are multifactorial illnesses triggered by particular environmental variables in genetically vulnerable people, which can impact their capacity to relate to others and function (Cenit et al., 2017; Briguglio et al., 2020). Severe mood disorders could have serious negative consequences extending to family members (Fekadu et al., 2021). Moreover, the International Classification of Diseases (ICD-11) published by the World Health Organization (WHO) reveals that mental disorders include diseases of depression, bipolar illness, anxiety (e.g., panic attacks and phobias), mood-related sleep disorders, and other mood disorders (e.g., compulsive overeating) and conditions associated with post-traumatic stress disorder and more (Krawczyk and Święcicki, 2020). In most cases, mild symptoms can be relieved with a combination of medications and psychotherapy.
It has long been speculated that some essential oils derived from natural aromatic plants can help improve sleep quality and mood disorders by inhalation (Ko et al., 2021). In the early 20th century, aromatherapy was first defined as a medical treatment by a French chemist, René-Maurice Gattefossé (Koyama and Heinbockel, 2020). In 1975, Pierre Franchomme, a pharmacologist and aromatologist, proposed the concept of the “chemotype,” the true chemical identity of a plant, and listed the critical aromatic compounds that characterize each plant and their influence on its properties—made breakthroughs in aromatherapy. In recent years, use of natural aromatherapy as adjuvant therapy for mental disorders, especially anxiety and depression has increased steadily, and increasing research is being done on the treatment mechanism (Lizarraga-Valderrama, 2021). And furthermore, it has been proven to produce pharmacological effects via the use of high-quality essential oils entering the body by the nasal inhalation (through the respiratory system or olfactory nerves), through topical absorption (skin), or through oral administration (digestive system) (Martinec, 2012; Gnatta et al., 2016; Acimovic, 2021). It is important to note that systemic administration of essential oils via intraperitoneal injection is often used in animal studies. The results of an animal experiment showed that systemic administration of essential oils induced antioxidant, anti-inflammatory, and γ-aminobutyric acid (GABA) changes to alleviate anxiety-like behavior in rats (Cui et al., 2020). Essential oils used in aromatherapy are hydrophobic liquids containing volatile aromatic molecules extracted in concentrated form from herbs, flowers, and other plant parts (Wang and Heinbockel, 2018). Researchers have analyzed the physiological effects of volatile aromatic molecules from pharmacological and aromatherapy perspectives and suggested that aromatherapy be a natural therapy for patients suffering from anxiety or depression (Tsang and Ho, 2010; Saiyudthong and Marsden, 2011; Amsterdam et al., 2012). Specifically, a significant reason for aromatherapy’s effectiveness in treating mood disorders is the presence of desirable chemical components and biological activities in essential oils such as limonene, linalool, linalyl acetate, geraniol, citronellol, and more. These chemicals have been extensively studied and have shown anxiolytic and antidepressant properties (Setzer, 2009; Vieira et al., 2018; Zhang and Yao, 2019; Agatonovic-Kustrin et al., 2020; Soares et al., 2021).
Inhalation aromatherapy via brain-targeted nasal delivery is one of the most common methods of administration in trials of aromatherapy and has evolved from the inhalation of essential oils, in which simple inhalation benefits the emotional wellbeing, tranquility, relaxation, or renewal of the human body (Ali et al., 2015). In clinical applications, transnasal inhalation of essential oils can be used nasal inhaler, vapor diffuser, spraying into the air, vapor balms, or direct inhalation by evaporation using tissue or cotton round (Acimovic, 2021). Notably, inhalation of essential oils or aromatic plant volatile oils can send signals directly to the olfactory system and trigger the brain to produce neurotransmitters e.g., serotonin [5-hydroxytryptamine (5-HT) and dopamine], influence the neuroendocrinological system, neurophysiological brain activity, sympathetic and parasympathetic nervous system, biomarkers changes, psychological and behaviour effects, and to modulate mental disorders further (Masago et al., 2000; Hongratanaworakit, 2004; Lahlou, 2004; Watanuki and Kim, 2005; Strous and Shoenfeld, 2006; Tanida et al., 2008; MPham et al., 2012; Lv et al., 2013; Angelucci et al., 2014). From this, it can be seen that inhalation aromatherapy on mental disorders is due to the pharmacological effect caused by systemic absorption or act on the nervous system, but not only due to the psychological perception of the scent (Scuteri et al., 2019). A potential mechanism for the effects of inhalation aromatherapy on brain function is the activation of nasal olfactory chemoreceptors and subsequent olfactory signaling. Olfaction is not only the oldest and the most vital sense for survival, it is also the only one unaffected by psychological processes (Cook and Lynch, 2008; Schneider et al., 2018; Cha et al., 2021). In humans, ∼300 genes are dedicated to detecting thousands of distinct scent molecules through a vast family of olfactory receptors (Sowndhararajan and Kim, 2016). In recent years, the mechanism of inhaled essential oils delivered to brain targets is being intensively studied. According to neurobiological studies, the olfactory nerve links the olfactory system to the central nervous system, which allows odor information processing. Moreover, higher-order (prefrontal) processes mediate the “smell experience.” If odor molecules contact the nasal mucosa, first-order neurons transmit the odor-evoked response to the olfactory bulb (Schneider et al., 2018). The olfactory tract is a complex system comprising sensory axons and second-order dendrites (mitral and tufted cells) located in the olfactory sulcus of the basal forebrain, and conveys information to several locations within the frontal and dorsomedial lobes (Nagayama et al., 2014; Smith and Bhatnagar, 2019). Olfactory perception starts with the binding of odorant molecules with suitable receptor proteins, and terminates in higher cerebral cortex, making us consciously aware of an odor. Odorous compounds can elicit chemo-electrical transduction pathways to modulate the excitability of the sensory neurons through converting the chemical stimulus into electrical impulses (Buck and Axel, 1991; Breer, 2003). Following that, olfactory sensory neurons convey electrical impulses to the limbic and hypothalamic regions of the brain through the olfactory bulb and upper olfactory cortex. These projections together comprise the primary olfactory cortex. Then, these olfactory areas produce higher-order projections to the orbital prefrontal cortex, amygdala, hypothalamus, basal ganglia, and hippocampus (Figure 1) (Angelucci et al., 2014; Lie et al., 2021). Another potential mechanism is that the essential oil molecules inhaled via steam enter the blood circulation by the alveoli of the respiratory system, and subsequently small lipophilic molecules easily cross the blood-brain barrier (BBB) to affect the brain (Faturi et al., 2010; Selvaraj et al., 2017). However, whether this pathway of nasal/respiratory system/circulation system/brain produces pharmacological effects is highly dependent on the drug properties, dose and concentration of the administration (Illum, 2003). In recent years, based on the limitations of dosages and amount of activity in inhalation administration, researchers have focused on the use of nanocarrier technology for transnasal targeting of drugs to the brain to improve drug utilization.
FIGURE 1
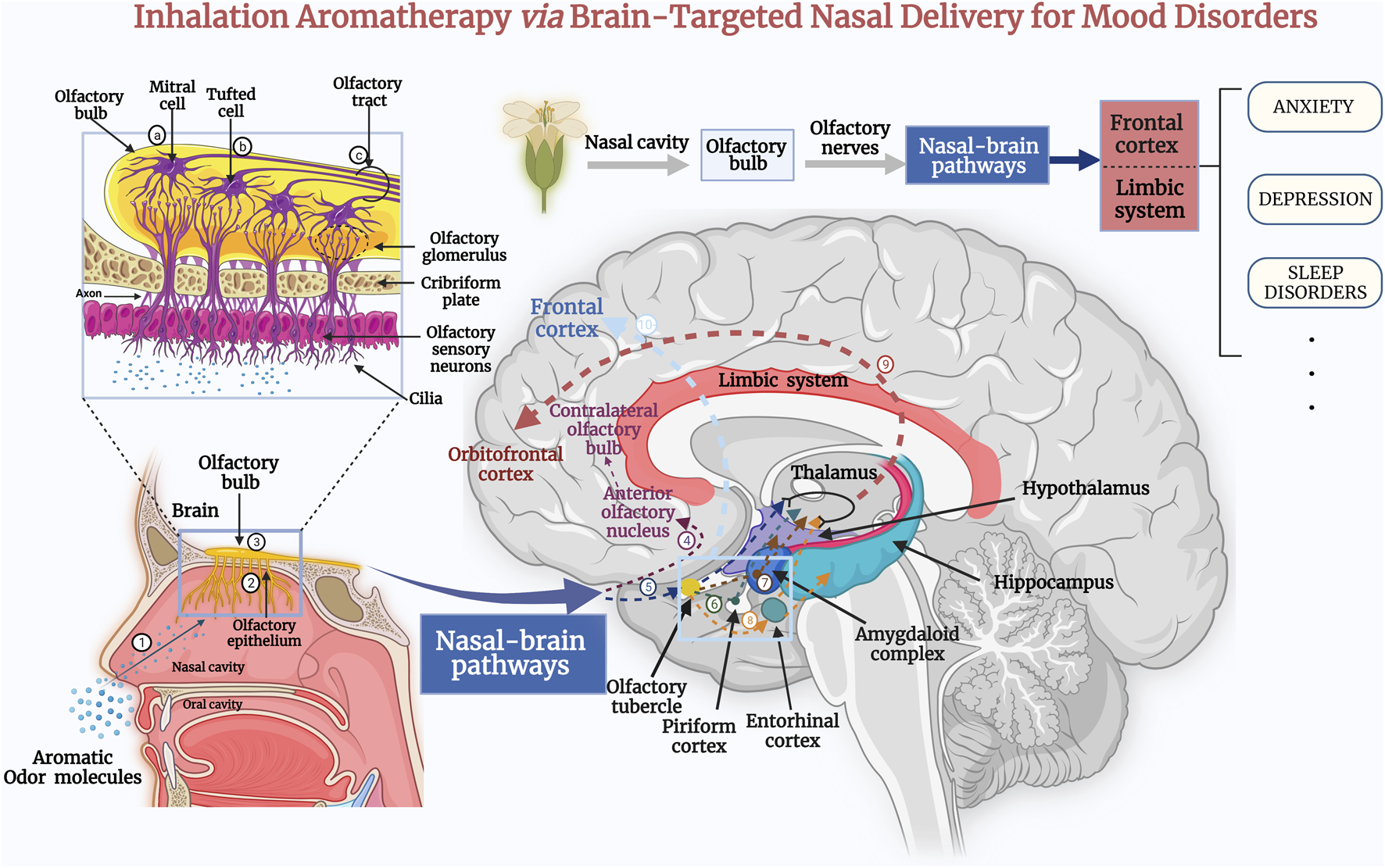
Inhalation of the extracts of aromatic plant via the nose sends signals directly to the olfactory system, where odor molecules target therapeutic drugs to brain tissue via nasal–brain channels. Subsequently, they act on the cerebral cortex, the thalamus, and the limbic system of the brain, and stimulate the brain to produce neurotransmitters to treat the symptoms of anxiety and depression, as well as improve sleep quality (Lv et al., 2013). The aromatic odor molecules are inhaled through the nasal cavity (1) to reach the olfactory epithelium (2) of the nasal mucosa (Schneider et al., 2018). First-order neurons transmit the odor-evoked response to the olfactory bulb (3). In the olfactory bulb, the axons of mitral cells (a) and some tufted cells (b) (secondary neurons) form the olfactory tract (c). The axons of some mitral cells or lateral branches enter the anterior olfactory nucleus (4) and pass to the contralateral olfactory bulb (Cha et al., 2021). Additional secondary neurons enter the olfactory striatum (medial, lateral, and medial) and then project to central olfactory areas, including the olfactory tubercle (5), piriform cortex (6), amygdala (7), and the entorhinal cortex (8). The entorhinal cortex partially transmits to the hippocampus. Eventually, the central olfactory-area signals are transmitted through the thalamus to the orbitofrontal cortex (9) (Lie et al., 2021). An additional olfactory signaling pathway passes directly from the central olfactory area to the prefrontal cortex (10). These impulses induce the release of neurotransmitters such as serotonin or endorphin, which act as a “bridge” between nerves and other bodily systems (Schneider et al., 2018; Smith and Bhatnagar, 2019).
This review summarizes the aromatic oils that may be used to treat mood disorders, assesses the efficacy of inhaled aromatherapy in treating anxiety, depression and sleep disorders (Table 1), and delves into their mechanism of action. In addition, we discuss recent data on the impact of inhalation aromatherapy on the brain and the pathways involved (Figure 1). Further, we summarized animal and clinical data and analyzed transnasal brain-targeted inhaled aromatherapy in anxiety, depression, and sleep disorders. Inhalation aromatherapy holds promise for preventing or treating mood disorders, but additional study is required to grasp the fundamental mechanisms involved. We argue for further clinical and scientific studies on inhalation aromatherapy to treat mental disorders, especially anxiety, depression, sleep disorders.
TABLE 1
| Scientific name | Main active ingredients | Main indications | Mechanism of action | References |
|---|---|---|---|---|
| Lavender (Lavandula angustifolia Mill.) Essential Oil | Linalyl acetate, linalool, (E)-β- stilbene, limonene | Anxiety Depression Sleep disorder | ↑: Parasympathetic nervous system | López et al. (2017); Ozkaraman et al. (2018) ; Mahdavikian et al. (2020); Kim M. et al. (2021) |
| ↑: Dopamine receptors subtype D3 | ||||
| ↑: Alpha waves in the brain | ||||
| ↓: NMDA receptors | ||||
| ↓: Serotonin transporter (SERT) | ||||
| Roman Chamomile (Chamaemelum nobile L.) Essential Oil | Angelic acid, tiglic acid, α-pinene, and 2-methyl butanoic acid | Anxiety Depression Sleep disorder | ↑: Mitochondrial function | Kong et al. (2017); Ebrahimi et al. (2021); Jia et al. (2021) |
| ↑: Expression of parvalbumin mRNA in hippocampus | ||||
| ↑: Neuroactive ligand- receptor interactions | ||||
| ↑: 5-hydroxytryptamine | ||||
| synapses | ||||
| Bergamot (Citrus bergamia Risso et Poiteau) Essential Oil | Monoterpenes limonene, monoterpene esters, linalyl acetate, and linalool | Anxiety Depression Sleep disorder | ↑: Synaptic transmission | Costa et al. (2010); Donato et al. (2014); Watanabe et al. (2015); Rombolà et al. (2017) |
| ↑: EEG activity | ||||
| ↑: Neuroprotective effects | ||||
| Lemon Balm (Melissa officinalis L.) Essential Oil | Citral, citronellal, linalool, geraniol and β-caryophyllene-oxide | Anxiety Depression Fatigue | ↑: Dopamine | Komiya et al. (2006) |
| ↑: Serotonin | ||||
| Saint John’s wort (Hypericum perforatum L.) extracts | Germacrene D, (E)-caryophyllene, 2-methyl octane, α-pinene, hypericin, proto-hypericin | Anxiety Depression Sleep disorder | ↑: Serotonergic system | Wong et al. (2004); Linde et al. (2008); Di Pierro et al. (2018) |
| ↓: Monoamine neurotransmitters | ||||
| Rhodiola rosea L. (R. rosea L.) extracts | Cinnamyl alcohol glycosides such as rosin, rosavin, and the phenylethanoid compound salidroside with its aglycone tyrosol | Anxiety Depression Sleep disorder Fatigue | ↑: Neurotransmitters | Panossian et al. (2010); Alperth et al. (2019); Panossian et al. (2021); Kim K. J. et al. (2021) |
| ↑: BDNF/TrkB signaling pathway | ||||
| ↓: Anti-inflammatory action | ||||
| ↓: Glucocorticoid receptor | ||||
| ↓: Activity of HPA axis | ||||
| Cang-ai volatile oil | Eugenol, 1,8-cineole, patchouli alcohol, acetyl eugenol, linalool, linalyl acetate | Depression | ↑: Dopamine | Chen et al. (2019) |
| ↑: 5-hydroxytryptamine |
Use of aromatic plants’ volatiles or essential oils to treat neuropsychiatric disorders.
↑, enhance, activate or increase; ↓, weaken, inactivate or decrease.
Aromatic Plants and Extracts for Mood Disorders
The essential oils used for aromatherapy have been extracted from aromatic plants and herbs to treat various ailments for centuries. About 17,500 plants have an aromatic scent (Tu et al., 2020). Because of their specific pharmacological functions, essential oils can be used in various ways to stimulate specific physiological responses for symptom relief. For instance, some scents (e.g., Mentha × piperita L. peppermint oil) can change the endogenous opioid pathways of the brain to alleviate pain and anxiety (Zarzo, 2007; Angelucci et al., 2014). Moreover, aromatic herbal preparations have long been a mainstay for treating anxiety and depression. Volatile oils are active chemicals derived from aromatic herbal remedies that often possess a broad spectrum of biological actions (Wang et al., 2014). Recent research indicates that the chemically active components in essential oils or volatile oils have neuroprotective effects, which may help alleviate depression and anxiety symptoms. Table 1 summarizes the properties of aromatic herbs or essential oils for the treatment of mood disorders.
Lavender (Lavandula angustifolia Mill.) Extract
Lavandula angustifolia Mill. is an aromatic plant that belongs to the Labiatae family. It contains high concentration of volatile oils from the aromatic parts of the plant, and is considered one of the most effective over-the-counter aromatic herbal extracts for the treatment of anxiety, depression, and stress (López et al., 2017). Many botanical species of lavender can be used medicinally, and most have a similar chemical composition, including Lavandula angustifolia (English lavender), L. stoechas (French lavender), L. latifolia (a Mediterranean grass-like lavender) (Cavanagh and Wilkinson, 2002; Sanna et al., 2019). The chemical compounds linalyl acetate (3,7-dimethyl-1,6-octadien-3yl acetate), linalool (3,7-dimethylocta-1,6-dien-3-ol), lavandulol, 1,8-cineole, lavandulyl acetate, and camphor are the primary constituents (Da Porto et al., 2009; Carson and Hammer, 2010; Ozkaraman et al., 2018). However, the main chemical composition of lavender oil varies from species to species. A study determined the composition of the essential oils of Lavandula angustifolia and Lavandula latifolia. Of these, linalool (37–54%), linalyl acetate (21–36%), and (E)-β-stilbene (1–3%) were the most abundant in Lavandula angustifolia. In contrast, the higher content of linalool (35–51%), eucalyptol (26–32%), camphor (10–18%), α-pinene (1–2%), α-terpineol (1–2%) and α-bisabolene (1–2%) were found in L. latifolia (Carrasco et al., 2015). Linalool and linalyl acetate are the most important constituents of lavender. Linalool contains sedative and narcotic properties, whereas linalyl acetate possesses narcotic properties. The scent of lavender has been studied, and linalool and linalyl acetate have been found to activate the parasympathetic nervous system (Fayazi et al., 2011; Mahdavikian et al., 2020).
An animal study demonstrated that inhalation of lavender oil improves anxiety-like behaviors in rats. After at least 30 min of inhalation, peripheral movements, and defecation in an open field were reduced in anxiety model rats (Shaw et al., 2007). Lavender essential oil improved depression-like behavior, neurogenesis, and synaptic plasticity, and depression-like and anxiety-like behaviors were alleviated significantly by corticosterone administration in animal models. Furthermore, L. angustifolia essential oil increases the number of bromodeoxyuridine-positive cells in the rat hippocampus and ameliorates corticosterone-induced neuro-regeneration disorders (Sánchez-Vidaña et al., 2019). Related animal studies have shown that lavender possesses significant receptor-binding affinities and activity on the N-methyl-D-aspartate (NMDA) receptor. Hence, the anxiolytic and antidepressant properties of lavender oil may be due (at least in part) to its regulation of glutamate NMDA receptors and suppression of the serotonin transporter (López et al., 2017).
Research has shown that high-stress levels or continuous exposure to stress can impair human social interaction and lead to social anxiety. A randomized controlled trial showed the effects of lavender oil aromatherapy on anxiety and sleep quality in chemotherapy patients. Lavender oils were administered to the respective intervention groups, and no aromatherapy was administered to the control group. The outcome evaluation indicators were the State-Trait Anxiety Inventory (STAI) and the Pittsburgh Sleep Quality Index (PSQI). This study determined that chemotherapy patients were inhaling three drops of lavender essential oil nightly before sleep can reduce trait anxiety levels and improve sleep quality (Ozkaraman et al., 2018). Kim and others conducted a systematic review and meta-analysis using PRISMA criteria to investigate the efficacy of lavender on anxiety, depression, or physiologic factors in humans. They found that lavender aromatherapy decreased anxiety and despair significantly, and that one administration session strengthened the anxiolytic effects of lavender aromatherapy (Kim M. et al., 2021). However, according to Kang and co-workers, lavender oil is effective in reducing anxiety, but there is some variation in the magnitude of the effect. When analyzing by route of administration, the effect of inhalation via intranasal administration is the most prominent (Donelli et al., 2019; Kang et al., 2019). Hence, animal research and clinical trials should be undertaken to gain deeper understanding of the effects of L. angustifolia essential oil administered through nasal–brain pathways.
Roman Chamomile (Chamaemelum nobile L.) Essential Oil
Chamomile is an aromatic medicinal plant in the Asteraceae family, widely used by ethnic and traditional medicine, represented by two common varieties viz. German Chamomile (Matricaria chamomilla) and Roman Chamomile (Chamaemelum nobile) (Hansen and Christensen, 2009). Due to its volatile, bioactive phytochemicals, it has been used to treat various diseases. However, there are differences in the main volatile substances of different species of chamomile, an analysis of terpenoid biosynthesis pathways based on co-expression networks showed that the main volatiles of German chamomile are monoterpenes and sesquiterpenes, while the main volatiles of Roman chamomile are esters (Mann and Staba, 1986; Tai et al., 2020). Roman Chamomile essential oils are often used as a mild sedative to calm nerves, decrease anxiety, and cure nightmares, insomnia, and other sleep difficulties (McKay and Blumberg, 2006; Singh et al., 2011). Researchers investigated the effect of inhalation of Roman chamomile essential oil on depressive-like behaviors in Wistar–Kyoto (WKY) rats for 2 weeks. After inhaling Roman chamomile essential oil or one of its main components, α-pinene, depression-like behavior in WKY rats was improved during the forced swimming test (FST). Furthermore, an increase in expression of the proteins involved in oxidative phosphorylation and parvalbumin mRNA expression in the hippocampus were documented. Those findings suggested that mitochondrial function and small parvalbumin-related signaling may be involved in the antidepressant effect of chamomile (Kong et al., 2017). Hashikawa-Hobara and others suggested a new role for Roman chamomile. They found that inhalation of Roman chamomile essential oil combined with chlorpromazine reduced drug-resistant depression-like behavior in mice, and had a crucial role in drug-resistant depression-like behavior. Their results may help people suffering from drug-resistant depression and provide a target for innovative antidepressant therapies (Hashikawa-Hobara et al., 2019). Future emphasis should be placed on animal studies with chamomile involving animal models of various psychiatric disorders, which will help develop chamomile as a promising therapeutic agent (Srivastava et al., 2010).
Matricaria chamomilla L. has multi-target and multi-pathway characteristics to treat anxiety disorders and depression. Jia and others undertook research based on network pharmacology and database mining. They revealed that the active components of Roman chamomile participate in neuroactive ligand-receptor interactions, 5-HT release into synapses, the cyclic adenosine monophosphate signaling pathway, and neurotransmitter-binding pathway, and that LRRK2 may be a critical gene in Roman chamomile for the treatment of anxiety disorders (Jia et al., 2021). In a recent three-arm parallel randomized controlled trial, 183 participants were included in the study and randomized into three groups (n = 61): lavender, chamomile, and control groups. Participants in the experimental group inhaled three drops of 1.5% lavender and chamomile essential oils for 30 nights. Participants in the control group inhaled only distilled water similarly. Compared to the control group, the lavender and chamomile groups showed statistically significant improvements in depression, anxiety, and stress levels immediately and 1 month after the intervention (p < 0.01). The trial found that inhalation aromatherapy with chamomile essential oils and lavender extract reduced depression, anxiety, and stress levels in older community-dwelling people (Ebrahimi et al., 2021). Effectiveness of using chamomile essential oil on stress symptoms and stress management in clinical practice is required. Further studies on the effectiveness of chamomile essential oil in clinical applications for psychiatric disorders are needed, and further search is more focused on antidepressant and anxiolytic pharmacological mechanisms.
Bergamot (Citrus bergamia Risso et Poiteau) Extracts
Citrus bergamia Risso et Poiteau is a species of plant in the Rutaceae family (subfamily Esperidea), also known as “Bergamot.” Bergamot essential oil (BEO) is a volatile oil preparation obtained by rasping and cold pressing the peel of the fruit (Mannucci et al., 2017). The main active ingredients of BEO are composed of 93–96% volatile and 4–7% non-volatile components. The volatile components mainly include monoterpene limonene accounts for 25–53% and a large number of oxygenated compounds, such as linalool, linalyl acetate, γ-terpinene, and β-pinene (Mondello et al., 1998; Moufida and Marzouk, 2003; Costa et al., 2010; Donato et al., 2014; Navarra et al., 2015). In addition, linalyl acetate is also a highly represented monoterpene in bergamot oil, sometimes almost as abundant as limonene (Poiana et al., 2003; Verzera et al., 2003; González-Mas et al., 2019). Its non-volatile component 5-MOP can cause phototoxicity, however, modern vacuum distillation of bergamot peel technology can obtain high-quality C. bergamia essential oil utterly free of 5-MOP, and chemical properties are comparable to those of cold-pressed oil (Belsito et al., 2007). Animal model studies have shown that the main components of bergamot can affect the synaptic transmission, regulate electroencephalography (EEG) activity, and have neuroprotective effects (Rombolà et al., 2009; Bagetta et al., 2010). One study in rats focused on the anxiolytic and sedative effects of bergamot essential oils. The behavioral effects were compared with benzodiazepine diazepam by subjecting rats to the forced swimming test (FST), open field test (OFT), and elevated maze test (EMT). The results indicated that bergamot alleviated anxiety-like behavior in rats, thereby adding to the understanding of the pharmacological profile of bergamot and bolstering its rational use in aromatherapy (Rombolà et al., 2017).
In 2015, Watanabe and others undertook a random crossover trial examining the effects of inhalation of the vapor of bergamot essential oil for 15 min on 41 healthy women. They measured the salivary level of cortisol and heart rate, as well as self-reported anxiety, fatigue, and emotional state. Volatile oils were inhaled into the lungs via the nose and transported into the bloodstream via the alveoli, and elicited significant psychoactive and physiological effects. The results showed that inhalation of bergamot oil helped slow-down anxiety-induced tachycardia, reduce salivary cortisol levels, and improve negative mood and fatigue scores significantly (Watanabe et al., 2015). In 2011, Hongratanaworakit showed that bergamot essential oil helped treat depression. The analyses were based on the blood pressure, pulse rate, respiration rate, and skin temperature. Compared with placebo, bergamot oil reduced the pulse rate and blood pressure significantly (Hongratanaworakit, 2011). The studies cited above provide evidence for clinical use of the volatile oils of C. bergamia essential oil for treating depression or anxiety, but additional high-quality evidence is required to support such use. Rigorous animal studies and high-quality clinical trials on treating mental disorders with Bergamot essential oil are highly needed, and this is a worthwhile direction for the future.
Essential Oil from Melissa officinalis L
Lemon Balm (Melissa officinalis L.) is an aromatic medicinal herbal plant from the Labiatae family (Mint family). The Melissa officinalis L. essential oils are widely used in traditional medicine to treat many mental disorders such as depression, anxiety, insomnia, anxiety-induced heart palpitations and stress (Shakeri et al., 2016). Not only does it boost mood, but it also helps alleviate depression-related symptoms such as “brain fog,” but the mechanism of action is incompletely understood. Although over 100 chemicals have been identified in M. officinalis, the main components of the essential oil are citral, citronellal, linalool, geraniol, and β-caryophyllene-oxide (Miraj et al., 2017). A systematic review and meta-analysis evaluated the effects of Melissa officinalis L. essential oil as an herbal remedy on anxiety and depression and its side effects in clinical trials. The abstracts of 68 clinical research studies and the full text of 27 articles were analyzed, 17 studies were excluded after evaluation because they were not randomized controlled trials or did not have a control group. Finally, only 10 articles were included in the qualitative synthesis and six in the quantitative synthesis (meta-analysis). According to the results of the meta-analysis, lemon balm essential oil significantly improved the symptoms of anxiety (standardized mean difference, SMD: 0.98; 95% CI: 1.63 to 0.33; p = 0.003) and depression (SMD: 0.47; 95% CI: 0.73 to 0.21; p = 0.0005), without serious side effects compared to placebo (Ghazizadeh et al., 2021). Although some animal and clinical studies about inhalation of lemon balm essential oil have been undertaken in recent years, limitations exist due to the high heterogeneity among clinical studies, the small sample size of clinical trials, differences in statistical methods, and the lack of in-depth research on pharmacological effects and mechanisms. In the future, further high-quality randomized controlled trials are needed to clarify the clinical efficacy of Melissa officinalis L. oils, and research on the mechanism of action and efficacy also should be increased.
Saint John’s Wort (Hypericum perforatum L.) Extracts
Saint John’s wort (SJW), also known as Hypericum perforatum L., the extracts can inhibit reuptake of monoamine neurotransmitters, and is often used as an antidepressant. The main active ingredients of Hypericum perforatum L. extracts are hypericin, proto-hypericin, pseudohy-pericin, proto-pseudohypericin. Its primary use is as an over-the-counter anti-depressive or anxiolytic (Hamid et al., 2017; Zirak et al., 2019). Numerous research has shown that a multi-fractionated SJW extracts improve therapeutic results in patients suffering from depression. Nevertheless, the exact mechanism of action of SJW (and most of the compounds involved) is not known (Di Pierro et al., 2018).
Yu and others discovered that the levels of 5-hydroxy indole acetic acid (5-HIAA) in the cerebral cortex, hypothalamus, hippocampus, and caudate nucleus of mice increased dramatically 3 h after treatment with SJW extracts at concentrations as low as 10 mg/kg body weight. The effects of SJW extract are compatible with the involvement of the serotonergic system (Yu, 2000). Yu and others studied the effects of SJW extracts and the influence of the tricyclic antidepressant (TCA) imipramine on the transcription of hypothalamic genes in rats. They discovered significant correlations between six genes that were regulated directly. Research into the mechanism of action of the purported therapeutic effect of SJW could reveal new processes, novel chemicals, and new biological targets for the development of antidepressant drugs (Wong et al., 2004). Linde and others examined 29 trials involving 5,489 individuals who had depression, and compared therapy with SJW extracts for 4–12 weeks with placebo treatment or conventional antidepressants. The SJW extracts outperformed a placebo in terms of efficacy and had fewer adverse effects than typical antidepressants. Furthermore, it was better tolerated than prescription medications (Linde et al., 2005; Linde et al., 2008). Therefore, the pharmacological effects and mechanisms of SJW extracts in the treatment of mood disorders need to be further investigated in the future.
Rhodiola Rosea L. (R. Rosea L.) Extracts
R. Rosea L. is considered a “universal” aromatic botanical, and extracts can be employed to treat fatigue, depression, cognitive dysfunction, and nerve disorders (Brinckmann et al., 2021). The main bioactive compounds of Rhodiola Rosea L. are phenylpropanoids such as cinnamyl alcohol glycosides rosin and rosavin. Furthermore, the phenylethanoid molecule salidroside contains the aglycone tyrosol (Ma et al., 2018; Alperth et al., 2019). Phenylpropane derivatives mediate the adaptogenic action of R. Rosea preparations (e.g., rosavin) and phenylethylene derivatives (e.g., tyrosol and salidroside), which have pleiotropic pharmacological effects on the neuroendocrine and immune systems (Panossian et al., 2021). The rhizome of R. Rosea L. (and the chemicals isolated from it) have been shown to protect neuronal PC-12 cells from oxidative stress and demonstrate mild acetylcholinesterase inhibition, respectively (Kim K. J. et al., 2021). Several clinical studies have demonstrated that using the R. Rosea extract SHR-5 regularly has an anti-fatigue effect and promotes cognitive function while decreasing “burnout” in individuals with chronic fatigue syndrome. Moreover, R. Rosea has shown promising benefits in treating mild-to-severe depression and generalized anxiety disorder (GAD) (Panossian et al., 2010). One randomized phase-III pilot trial was conducted to determine the efficacy and safety of a standardized extract SHR-5 of the rhizomes of R. Rosea L. in individuals experiencing a bout of mild-to-moderate depression. When the extract was taken at 340 mg every day for 6 weeks, a significant decrease in the total level of symptoms of depression (e.g., sleeplessness, mood instability, and somatization) was noted. At greater doses (four pills a day for 6 weeks), a considerable increase in self-esteem was observed (Darbinyan et al., 2007). Future studies may focus on the pharmacological mechanism of R. Rosea on mild-to-moderate depression.
Cang-ai Volatile Oil
Cang-ai Volatile oil (CAVO) is an inhalational preparation employed to treat depressive and emotional disorders, and extracted from the ethnic aromatic herbs such as Cyperus rotundus L, Mugwort (Artemisia vulgaris L.), patchouli (Pogostemon cablin (Blanco) Benth.), clove (Syzygium aromaticum (L.) Merr. & L.M.Perry) and Perrin (Pimpinella anisum L.). The top-10 volatile compounds in CAVO identified by gas chromatography-mass spectrometry (GC-MS) are eugenol, 1,8-cineole, patchouli alcohol, acetyl eugenol, linalool, linalyl acetate, caryophyllene, terpinene-4-ol, cineol, and terpineol. CAVO has been shown to ameliorate depression-like behavior in animal studies, and be better than the traditional oral route of antidepressants, the mechanism of action appears to be related to dopamine and 5-HT (Chen et al., 2019). This observation suggests a new aromatic volatile oil preparation for anti-depression medications. In this way, more meaningful pharmacological evidence for efficacious and safe treatments can be obtained. In addition, preliminary results for self-reported pre-and post-tests in patients with depressive tendencies on CAVO inhalation have been obtained. In the future, more clinical trials will be conducted to observe the safety and efficacy of CAVO.
Aromatherapy Inhalation for Anxiety
Anxiety disorders are the most frequent mental ailment, with a global prevalence ranging between 2.4 and 20% per nation. According to the WHO, 3.6% of the world’s population—around 264 million people—suffer from anxiety (Baxter et al., 2013; Bandelow and Michaelis, 2015; Munir and Takov, 2021). It is a type of dread that emerges in response to potentially dangerous or stressful events, and results from a complex interaction of biological factors, as well as psychological, temperamental, and environmental elements (Thibaut, 2017).
Anxiety disorders include (but are not limited to) panic disorder/agoraphobia (PDA), GAD, social anxiety disorder (SAD), and obsessive-compulsive disorder (OCD) (Giacobbe and Flint, 2018). Panic disorder (with or without agoraphobia) is the most common, accounting for 6.0% of all types, followed by social phobia (2.7%) and GAD as the most common phobias (2.2%) (Craske et al., 2017). Each subcategory of anxiety disorders has its own set of symptoms and diagnostic criteria, but ICD-11 identifies the common symptoms apprehension, motor overactivity, and autonomic overactivity (Reed et al., 2019). Several biological anomalies have been implicated in the pathophysiology of anxiety disorders. The gamma-aminobutyric acid (GABA), norepinephrine, and 5-HT systems have critical roles in modulating the emotional circuitry that underlies anxiety and depression, which are closely connected (Romana et al., 2020).
For anxiety disorders, various treatment options, such as medication and psychotherapy, are available. These treatments may exert their advantages by top-down or bottom-up regulation of abnormal brain activity, respectively (Bandelow et al., 2017; Giacobbe and Flint, 2018). Mild anxiety disorder, in general, does not require excessive treatment, but treatment is indicated if patients manifest significant discomfort or experience disorder-related consequences. For example, subsequent depression, suicidal thoughts, or alcohol misuse are possible outcomes (Bandelow et al., 2017). First-line therapies for anxiety include lifestyle modifications, cognitive behavioral therapy, selective serotonin reuptake inhibitors (SSRIs), or serotonin-norepinephrine reuptake inhibitors (SNRIs) (Bandelow et al., 2015; Mangolini et al., 2019; Garakani et al., 2020). Since the 1980s, researchers have conducted upwards of 10,000 animal studies of nearly 1,500 medications for anxiety, and the number of such studies has shown a marked increase in recent years. However, many studies have not yielded satisfactory results. In many cases, severe adverse drug reactions, dependence, and poor treatment outcomes have persisted (Griebel and Holmes, 2013). There is an immediate need for safe and efficacious treatments and medications for anxiety. The number of studies on inhalation aromatherapy for anxiety disorders has been increasing recently. In general, chamomile, lavender, bergamot, clary sage, rosemary, ylang-ylang, frankincense, and damask rose are used commonly as “anti-anxiety oils.” Essential oils to treat anxiety have been used throughout Europe for many years (Seol et al., 2010). Also, the chemical and biological properties of essential oils have resulted in the development of crucial treatment strategies for anxiety disorders (Fernandes et al., 2021). Essential oils have fewer side effects and more administration methods than traditional anti-anxiety medications. Among them, inhalation has been the most common method of administration in trials of aromatherapy, and the most efficacious (Zhang and Yao, 2019).
Among anxiety-related research items, the lavender essential oil has received the most attention. Franco and others evaluated the reduced anxiety effect of lavender aroma on women before breast surgery. Inhalation of lavender-fragrance aromatherapy treatments reduced anxiety before surgery (Franco et al., 2016). A randomized, double-blind, placebo-controlled clinical study by Farshbaf-Khalili and others focused on anxiety in postmenopausal women. They compared the effects of inhaling oils of lavender or bitter-orange, and found them to have a beneficial impact on anxiety in this population (Farshbaf-Khalili et al., 2018). A randomized controlled study investigating the effect of lavender-oil inhalation on vital signs and anxiety revealed that inhalation aromatherapy was favorable for anxious individuals about to undergo surgical procedures under local anesthesia (Karan, 2019). Guo and others analyzed the efficacy of inhalation aromatherapy on preoperative anxiety. They discovered evidence to support using aromatherapy to alleviate preoperative anxiety in adults. Their results suggested that aromatherapy inhalation was the most practical and feasible mode of administration, and had the advantage of a short duration of administration (20 min for each session). Hence, recent research suggests that lavender oil, preparations of citrus species, and rose oil are the most common and efficacious fragrance preparations for anxiety disorders (Guo et al., 2020). With regard to using essential oils to treat anxiety, initially researchers examined the direct effects of scent on the brain through EEG and functional imaging. They found that the essential oils of rose, lavender, lemon, and peppermint had anti-anxiety effects, and more in-depth research has been conducted in recent years (Lehrner et al., 2005; Bradley et al., 2007; Zhang et al., 2013). Inhaled aromatherapy could reduce preoperative anxiety, but data from primary studies are needed to improve evidence quality (Men et al., 2021).
Animal experiments have shown that inhalation of essential oils can prevent or relieve anxiety symptoms. These beneficial effects may result from modulation of monoamine levels, induction of neurotrophic factors expression, regulation of the endocrine system, and promotion of neurogenesis (Fung et al., 2021). However, an animal experiment has shown that olfactory deficit induced by zinc (zinc gluconate + zinc acetate) did not impair the anxiolytic effects of lavender essential oil inhalation in the marble-burying test. This study demonstrated that the active compounds of lavender oil might enter the systemic circulation and central nervous system through the respiratory system in the absence of olfaction, ultimately activating the relevant receptors to improve anxiety symptoms (Chioca et al., 2013). In future studies, researchers can evaluate the importance of the olfactory system through pharmacological and physiological alterations induced by inhaled essential oils in olfactory impairment animal models. In another animal study, the authors reported that the sedative effect of inhaling a lavender-Roman chamomile oil mixture was impaired by reduced olfactory function (Kagawa et al., 2003). It can be concluded that the olfactory system has an essential role in inhalation aromatherapy, and olfactory impairment on the effects of inhalation is also related to the different types and active ingredients of the essential oils. We can synthesize that the mechanism of transnasal inhalation of essential oils in psychiatric disorders is a function of multiple factors. Researchers should undertake more rigorous animal studies to gain more insight into the mechanisms of inhalation aromatherapy.
Aromatherapy Inhalation for Depression
Depression is a prevalent mental illness and “mood illness” that manifests via a mix of emotional (sadness and anhedonia), cognitive (thinking problems and inability to focus), and somatic symptoms (changes in appetite and insomnia). Approximately 280 million people worldwide suffer from depression. The incidence of depression varies significantly according to geographic location, and depression may increase dramatically in the next decade (Wang, 2021). It is characterized by the profound emotions of melancholy, hopelessness, despair, and an inability to find pleasure in routine activities, as well as changes in sleep and food habits, fatigue, and suicidal thoughts (Sánchez-Vidaña et al., 2019).
Mainstream interventions for depression have relied primarily on medication, such as antidepressants, which may have unacceptable side effects, such as headache, insomnia, nausea, potential drug interactions, or the danger of overdose (Bauer, 2007). Antidepressant medicines may be used as first-line therapy for depressive disorder and are classified into several types. The antidepressants used most often are SSRIs, SNRIs, TCAs, and monoamine oxidase inhibitors (Ramachandraih et al., 2011; Hillhouse and Porter, 2015; Kok and Reynolds, 2017; Zanos and Gould, 2018; InformedHealth.org, 2021). The American College of Physicians advises that practitioners treat individuals with major depressive disorder using cognitive behavioral therapy or second-generation antidepressants (Qaseem et al., 2016). However, ∼30% of persons who use SSRIs for depression experience no response. In addition, the first-line drugs used to treat depression (SSRIs) often have severe side-effects, which stops patients taking them or to lose confidence in treatment. As a result, many people suffering from depression do not achieve remission of symptoms and have to endure relapses and more functional impairment (Adell et al., 2005; Arroll et al., 2005). This phenomenon has pushed patients and researchers to seek more efficacious alternative medicines, particularly in the early phase of treatment. Due to the limitations of those traditional methods and antidepressants, there is a growing interest in using aromatic naturopathy as an alternative therapy. As a complementary approach, inhalation aromatherapy is used widely for treating depression (Koo, 2017; Liang et al., 2021). Numerous studies have indicated that some of the critical constituents of essential oils may reduce depressive symptoms markedly via nasal–brain pathways, including those in patients with severe depressive disorder, postpartum women, postmenopausal women, and cancer patients (Chan et al., 2015; Han et al., 2017). In addition, the researchers discovered that citrus scents containing 95% citral were often more appealing and pleasant to people who felt sad (Pause et al., 2001). Inhalation of aromatic molecules through the nose is mild and has few adverse effects, which makes it an attractive option for treating depression (Yim et al., 2009; Lv et al., 2013). And they work more quickly than other methods because the blood-brain barrier does not interfere with the effects. In this way, aromatherapy looks to be a straightforward, cost-effective, and low-risk adjuvant approach for treating depression (Sánchez-Vidaña et al., 2017).
The use of animal models has enabled elucidation of different molecular pathways for treating depression by essential oils, such as the hypothalamic-pituitary-adrenal axis, sympathetic nervous system, cyclic adenosine monophosphate response element-binding protein signaling pathway, and neurotransmitter systems (e.g., serotonergic, dopaminergic, and GABAergic pathways) (Guillemain et al., 1989; Tafet et al., 2001; Raison et al., 2006; Chung et al., 2011; Slavich and Irwin, 2014; Chen et al., 2016; Xiong et al., 2018). de Sousa and others used a rodent model of depression and demonstrated the antidepressant activity of the essential oils of several plants: Acorus tatarinowii Schott, Asarum heterotropoides F. Schmidt, Litsea glaucescens Kunth, Mentha × Piperita L, Citrus limon (L.) Osbeck, Eugenia uniflora L, Lavandula angustifolia Mill, Perilla frutescens (L.) Britton, Salvia sclarea L, Rosmarinus officinalis L, Schinus terebinthifolius Raddi, and Syzygium aromaticum (L.) (de Sousa et al., 2017). A behavioral experiment in a rat model of depression using the FST examined the antidepressant effects of the essential oils of chamomile (A. nobilis), clary (Salvia sclarea), rosemary (Rosmarinus officinalis), and lavender (L. angustifolia) in rats. They showed that these oils improved depressive-like behavioral effectively (Seol et al., 2010). In addition, Bagci and others investigated the positive effects of the scopolamine component of Anthriscus nemorosa essential oil on memory, anxiety, and depression in rats: their behavior improved (Bagci et al., 2016). Notably, one animal study revealed that lemon oil increased the metabolic turnover of 5-HT markedly in the prefrontal cortex and striatum to enhance 5-HT function, which demonstrated a mechanism of action comparable with that of SSRIs (Komiya et al., 2006; Cowen, 2008). Although various animal studies on the treatment of depression with inhaled essential oils, more sophisticated experiments should be designed to investigate the pharmacological effects.
Aromatherapy Inhalation for Sleep Disorders
Sleep is vital for sustaining physiological and psychological welfare (Karadag et al., 2017). Numerous mental disorders and sleep disorders show a bidirectional relationship. Patients suffering from anxiety, depression, and other mood disorders have persistent difficulties obtaining a decent night’s sleep. Sleep disturbances can contribute to the risk of mental-health illnesses (Santamaria and Iranzo, 2014; Freeman et al., 2020; Momen et al., 2020). In addition, many antipsychotic agents affect sleep and sleep architecture. Even though sedative-hypnotics may enhance sleep quality significantly, these medications have adverse effects, are addictive, and do not lead to sufficient sleep (Pagel and Parnes, 2001; Hajibagheri et al., 2014). Hence, the application of a less harmful relief method with fewer adverse effects is significant (Hajibagheri et al., 2014; Jodaki et al., 2021).
From ancient times, aromatherapy has been an effective natural therapy for sleep problems, through massage and inhalation using essential oils are the main strategies (Bikmoradi et al., 2015; Guadagna et al., 2020; Mahdavikian et al., 2020). Numerous essential oils have been used to treat sleep difficulties, including lavender oils and peppermint oils (Blackburn et al., 2017; Salamati et al., 2017; Mahdavikian et al., 2020; Malloggi et al., 2021). Research has shown that bergamot oil can reduce blood pressure and the heart rate and aid sleep. Moreover, jasmine and frankincense have been shown to aid restless sleep and improve sleep quality. Takeda and co-workers explored the benefits of inhalation aromatherapy on sleep disturbances in elderly dementia patients by placing essential oils on towels wrapped around their pillows each night. They measured sleep latency, total sleep time, sleep effectiveness, duration of the most extended sustained sleep phase, waking time after sleep onset, early-morning awakening, total daytime sleep, and assessed the Neuropsychiatric Inventory. Inhalation aromatherapy had a beneficial impact on sleep-disruption symptoms in that population (Takeda et al., 2017). Moreover, aromatherapy using the oils of sweet-orange and lavender have been suggested to improve sleep quality and reduce tiredness in hemodialysis patients (Muz and Taşcı, 2017). Another comprehensive study and meta-analysis determined that aromatherapy significantly improved sleep quality and was quick-acting, simple to apply, and did not require additional equipment (Hwang and Shin, 2015). Recently, Zhong and others investigated the compatibility of using the essential oils of Compound Anshen with those of lavender, sweet orange, and sandalwood with sedative and hypnotic properties. They demonstrated improved sleep quality by combining essential oils and blends. Overall, aromatherapy has improved sleep quality in healthy and unwell people, especially if used as inhalation rather than massage treatment (Hwang and Shin, 2015; Zhong et al., 2019). The molecules in essential oils entering the limbic system of the brain through the nasal passages simultaneously affect GABA receptors in the hypothalamus, which are crucial for maintaining sleep. Hence, aromatherapy is quite popular and used commonly to manage sleep quality (Tang et al., 2021).
Conclusion and Perspectives
In summary, inhalation aromatherapy via brain-targeted nasal delivery can be an effective option for improving depression, anxiety, and sleep disorders. When used in inhalation aromatherapy, the advantages of essential oils are high permeability, fast metabolism, non-retention, and low toxicity. Since essential oils are bioactive molecules and have a molecular weight of less than 300 Da (Dhifi et al., 2016), considered safe and biocompatible with a great range of therapeutic applications due to their heterogeneous composition of fatty acids, terpenes, triterpenes, and many other lipophilic components. In addition, a few minutes of inhalation of essential oils via the nose can affect the limbic system, and all leave the body by urination, excretion, breathing, and pores in 4–20 h after use (Barradas and de Holanda e Silva, 2021). Notably, the active chemical components of the essential oils or volatile oils used in aromatherapy have fewer side effects than traditional medications for treating mental disorders, but the safety and purity of oils must be considered. Under the supervision of a physician, essential oils of assured quality and demonstrated efficacy should be selected to improve depression or anxiety symptoms. Although the use of volatile essential oils for transnasal administration is common in aromatherapy, inhalation of concentrated forms of essential oils may pose a risk of eye and skin irritation, so direct inhalation of pure essential oils is not recommended. There is an urgent need to clarify the safe dose of inhaled essential oils in clinical applications. One research described a series of methods to assess the efficacy of inhaled essential oils, and clarified that EOs intake dose-relationships with the efficacy of brain function. In general, the inhalation of EOs indicated a dose-dependent relationship with efficacy (Aponso et al., 2020).
Taken together, those data suggest that inhalation aromatherapy may have a more excellent therapeutic range than thought previously, especially in the domain of mental diseases (Perry and Perry, 2006; Ayaz et al., 2017). In the future, more universities, research centers, and medical institutions should conduct qualitative and quantitative analyses of aromatic drugs and extract their components. Also, more multicenter, large-sample, high-quality randomized controlled trials on inhaled aromatherapy for mood disorders are needed. In particular, the use of doses and treatment protocols need to be optimized. We hope that transnasal aromatherapy will lead to further breakthroughs on research into mood disorders.
Statements
Author contributions
All authors contributed substantially to the scientific process and writing of the manuscript. DQ, JC, XM and ML designed the structure and wrote the first draft of the manuscript. HL, XH, YW, QY, ZW, ZL, QC and JD drew complied Table 1 and Figure 1, and they have compiled references. JC, GL, BC, XM, LX, and DQ supervised and revised the final version of the manuscript. All authors approved the final version of the manuscript submitted.
Funding
This work was supported by the National Natural Science Foundation of China (31960178, 82074421, 82160923, 82160924, 8207153176, 82160924), the Applied Basic Research Programs of Science and Technology Commission Foundation of Yunnan Province (2019FA007), the Joint Project of Applied Basic Research of Yunnan University of Chinese Medicine and Yunnan Provincial Science and Technology Department [2019FF002(-001)], Yunnan Provincial Department of Education Science Research Fund Project (2020Y0203, 2021Y456), the Key Realm R&D Program of Guangdong Province (2019B030335001), the China Postdoctoral Science Foundation (2018M631105), and the Yunnan Provincial Academician and Expert Workstation (202005AF150017, 202105AF150037, 2019IC051).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1
AcimovicM. (2021). Essential Oils: Inhalation Aromatherapy-A Comprehensive Review. J. Agron. Technol. Eng. Manag.4, 547–557.
2
AdellA.CastroE.CeladaP.BortolozziA.PazosA.ArtigasF. (2005). Strategies for Producing Faster Acting Antidepressants. Drug Discov. Today10, 578–585. 10.1016/S1359-6446(05)03398-2
3
Agatonovic-KustrinS.KustrinE.GegechkoriV.MortonD. W. (2020). Anxiolytic Terpenoids and Aromatherapy for Anxiety and Depression. Adv. Exp. Med. Biol.1260, 283–296. 10.1007/978-3-030-42667-5_11
4
AliB.Al-WabelN. A.ShamsS.AhamadA.KhanS. A.AnwarF. (2015). Essential Oils Used in Aromatherapy: a Systemic Review. Asian Pac. J. Trop. Biomed.5, 601–611. 10.1016/j.apjtb.2015.05.007
5
AlperthF.TurekI.WeissS.VogtD.BucarF. (2019). Qualitative and Quantitative Analysis of Different Rhodiola Rosea Rhizome Extracts by UHPLC-DAD-ESI-MSn. Sci. Pharm.87, 8. 10.3390/scipharm87020008
6
AmsterdamJ. D.ShultsJ.SoellerI.MaoJ. J.RockwellK.NewbergA. B. (2012). Chamomile (Matricaria Recutita) May Provide Antidepressant Activity in Anxious, Depressed Humans: an Exploratory Study. Altern. Ther. Health Med.18, 44–49. PMID: 22894890
7
AngelucciF. L.SilvaV. V.Dal PizzolC.SpirL. G.PraesC. E.MaibachH. (2014). Physiological Effect of Olfactory Stimuli Inhalation in Humans: an Overview. Int. J. Cosmet. Sci.36, 117–123. 10.1111/ics.12096
8
AponsoM.PattiA.BennettL. E. (2020). Dose-related Effects of Inhaled Essential Oils on Behavioural Measures of Anxiety and Depression and Biomarkers of Oxidative Stress. J. Ethnopharmacol250, 112469. 10.1016/j.jep.2019.112469
9
ArrollB.MacgillivrayS.OgstonS.ReidI.SullivanF.WilliamsB.et al (2005). Efficacy and Tolerability of Tricyclic Antidepressants and SSRIs Compared with Placebo for Treatment of Depression in Primary Care: a Meta-Analysis. Ann. Fam. Med.3, 449–456. 10.1370/afm.349
10
AyazM.SadiqA.JunaidM.UllahF.SubhanF.AhmedJ. (2017). Neuroprotective and Anti-aging Potentials of Essential Oils from Aromatic and Medicinal Plants. Front. Aging Neurosci.9, 168. 10.3389/fnagi.2017.00168
11
BagciE.AydinE.UngureanuE.HritcuL. (2016). Anthriscus Nemorosa Essential Oil Inhalation Prevents Memory Impairment, Anxiety and Depression in Scopolamine-Treated Rats. Biomed. Pharmacother.84, 1313–1320. 10.1016/j.biopha.2016.10.075
12
BagettaG.MorroneL. A.RombolàL.AmanteaD.RussoR.BerliocchiL.et al (2010). Neuropharmacology of the Essential Oil of Bergamot. Fitoterapia81, 453–461. 10.1016/j.fitote.2010.01.013
13
BandelowB.MichaelisS. (2015). Epidemiology of Anxiety Disorders in the 21st century. Dialogues Clin. Neurosci.17, 327–335. 10.31887/DCNS.2015.17.3/bbandelow
14
BandelowB.MichaelisS.WedekindD. (2017). Treatment of Anxiety Disorders. Dialogues Clin. Neurosci.19, 93–107. 10.31887/DCNS.2017.19.2/bbandelow
15
BandelowB.ReittM.RöverC.MichaelisS.GörlichY.WedekindD. (2015). Efficacy of Treatments for Anxiety Disorders: a Meta-Analysis. Int. Clin. Psychopharmacol.30, 183–192. 10.1097/YIC.0000000000000078
16
BarradasT. N.de Holanda e SilvaK. G. (2021). Nanoemulsions of Essential Oils to Improve Solubility, Stability and Permeability: a Review. Environ. Chem. Lett.19, 1153–1171. 10.1007/s10311-020-01142-2
17
BauerM. (2007). Updated WFSBP Guidelines for the Biological Treatment of Unipolar Depressive Disorders in Primary Care. World J. Biol. Psychiatry8, 66. 10.1080/15622970701308413
18
BaxterA. J.ScottK. M.VosT.WhitefordH. A. (2013). Global Prevalence of Anxiety Disorders: a Systematic Review and Meta-Regression. Psychol. Med.43, 897–910. 10.1017/S003329171200147X
19
BelsitoE. L.CarboneC.Di GioiaM. L.LeggioA.LiguoriA.PerriF.et al (2007). Comparison of the Volatile Constituents in Cold-Pressed Bergamot Oil and a Volatile Oil Isolated by Vacuum Distillation. J. Agric. Food Chem.55, 7847–7851. 10.1021/jf070997q
20
BikmoradiA.SeifiZ.PoorolajalJ.AraghchianM.SafiaryanR.OshvandiK. (2015). Effect of Inhalation Aromatherapy with Lavender Essential Oil on Stress and Vital Signs in Patients Undergoing Coronary Artery Bypass Surgery: A Single-Blinded Randomized Clinical Trial. Complement. Ther. Med.23, 331–338. 10.1016/j.ctim.2014.12.001
21
BlackburnL.AchorS.AllenB.BauchmireN.DunningtonD.KlisovicR. B.et al (2017). The Effect of Aromatherapy on Insomnia and Other Common Symptoms Among Patients with Acute Leukemia. Oncol. Nurs. Forum44, E185–E193. 10.1188/17.ONF.E185-E193
22
BradleyB. F.StarkeyN. J.BrownS. L.LeaR. W. (2007). The Effects of Prolonged Rose Odor Inhalation in Two Animal Models of Anxiety. Physiol. Behav.92, 931–938. 10.1016/j.physbeh.2007.06.023
23
BreerH. (2003). Sense of Smell: Recognition and Transduction of Olfactory Signals. Biochem. Soc. Trans.31, 113–116. 10.1042/bst0310113
24
BriguglioM.VitaleJ. A.GalentinoR.BanfiG.Zanaboni DinaC.BonaA.et al (2020). Healthy Eating, Physical Activity, and Sleep Hygiene (HEPAS) as the Winning Triad for Sustaining Physical and Mental Health in Patients at Risk for or with Neuropsychiatric Disorders: Considerations for Clinical Practice. Neuropsychiatr. Dis. Treat.16, 55–70. 10.2147/NDT.S229206
25
BrinckmannJ. A.CunninghamA. B.HarterD. E. V. (2021). Running Out of Time to Smell the Roseroots: Reviewing Threats and Trade in Wild Rhodiola Rosea L. J. Ethnopharmacol269, 113710. 10.1016/j.jep.2020.113710
26
BuckL.AxelR. (1991). A Novel Multigene Family May Encode Odorant Receptors: A Molecular Basis for Odor Recognition. Cell65, 175–187. 10.1016/0092-8674(91)90418-X
27
CarrascoA.Martinez-GutierrezR.TomasV.TudelaJ. (2015). Lavandula Angustifolia and Lavandula Latifolia Essential Oils from Spain: Aromatic Profile and Bioactivities. Planta Med.82, 163–170. 10.1055/s-0035-1558095
28
CarsonC. F.HammerK. A. (2010). “Chemistry and Bioactivity of Essential Oils,” in Lipids and Essential Oils as Antimicrobial Agents. Editor ThormarH. (Chichester, UK: John Wiley & Sons), 203–238. 10.1002/9780470976623.ch9
29
CavanaghH. M.WilkinsonJ. M. (2002). Biological Activities of Lavender Essential Oil. Phytother Res.16, 301–308. 10.1002/ptr.1103
30
CenitM. C.SanzY.Codoñer-FranchP. (2017). Influence of Gut Microbiota on Neuropsychiatric Disorders. World J. Gastroenterol.23, 5486–5498. 10.3748/wjg.v23.i30.5486
31
ChaH.KimS.SeoM. S.KimH. S. (2021). Effects of Olfactory Stimulation on Cognitive Function and Behavior Problems in Older Adults with Dementia: A Systematic Literature Review. Geriatr. Nurs.42, 1210–1217. 10.1016/j.gerinurse.2021.07.003
32
ChanY. Y.LoW. Y.YangS. N.ChenY. H.LinJ. G. (2015). The Benefit of Combined Acupuncture and Antidepressant Medication for Depression: A Systematic Review and Meta-Analysis. J. Affect Disord.176, 106–117. 10.1016/j.jad.2015.01.048
33
ChenB.LiJ.XieY.MingX.LiG.WangJ.et al (2019). Cang-ai Volatile Oil Improves Depressive-like Behaviors and Regulates DA and 5-HT Metabolism in the Brains of CUMS-Induced Rats. J. Ethnopharmacol244, 112088. 10.1016/j.jep.2019.112088
34
ChenY. F.WangY. W.HuangW. S.LeeM. M.WoodW. G.LeungY. M.et al (2016). Trans-Cinnamaldehyde, an Essential Oil in Cinnamon Powder, Ameliorates Cerebral Ischemia-Induced Brain Injury via Inhibition of Neuroinflammation through Attenuation of iNOS, COX-2 Expression and NFκ-B Signaling Pathway. Neuromolecular Med.18, 322–333. 10.1007/s12017-016-8395-9
35
ChiocaL. R.AntunesV. D.FerroM. M.LossoE. M.AndreatiniR. (2013). Anosmia Does Not Impair the Anxiolytic-like Effect of Lavender Essential Oil Inhalation in Mice. Life Sci.92, 971–975. 10.1016/j.lfs.2013.03.012
36
ChungS.SonG. H.KimK. (2011). Circadian Rhythm of Adrenal Glucocorticoid: its Regulation and Clinical Implications. Biochim. Biophys. Acta1812, 581–591. 10.1016/j.bbadis.2011.02.003
37
CookN.LynchJ. (2008). Aromatherapy: Reviewing Evidence for its Mechanisms of Action and CNS Effects. Br. J. Neurosci. Nurs.4, 595–601. 10.12968/bjnn.2008.4.12.31963
38
CostaR.DugoP.NavarraM.RaymoV.DugoG.MondelloL. (2010). Study on the Chemical Composition Variability of Some Processed Bergamot (Citrus Bergamia) Essential Oils. Flavour Fragr. J.25, 4–12. 10.1002/ffj.1949
39
COVID-19 Mental Disorders Collaborators (2021). Global Prevalence and burden of Depressive and Anxiety Disorders in 204 Countries and Territories in 2020 Due to the COVID-19 Pandemic. Lancet398, 1700–1712. 10.1016/S0140-6736(21)02143-7
40
CowenP. J. (2008). Serotonin and Depression: Pathophysiological Mechanism or Marketing Myth?Trends Pharmacol. Sci.29, 433–436. 10.1016/j.tips.2008.05.004
41
CraskeM. G.SteinM. B.EleyT. C.MiladM. R.HolmesA.RapeeR. M.et al (2017). Anxiety Disorders. Nat. Rev. Dis. Primers3, 17024. 10.1038/nrdp.2017.24
42
CuiY.CheY.WangH. (2020). Bergamot Essential Oil Attenuate Aluminum-Induced Anxiety-like Behavior through Antioxidation, Anti-inflammatory and GABA Regulation in Rats. Food Chem. Toxicol.145, 111766. 10.1016/j.fct.2020.111766
43
Da PortoC.DecortiD.KikicI. (2009). Flavour Compounds of Lavandula Angustifolia L. To Use in Food Manufacturing: Comparison of Three Different Extraction Methods. Food Chem.112, 1072–1078. 10.1016/j.foodchem.2008.07.015
44
DarbinyanV.AslanyanG.AmroyanE.GabrielyanE.MalmströmC.PanossianA. (2007). Clinical Trial of Rhodiola Rosea L. Extract SHR-5 in the Treatment of Mild to Moderate Depression. Nord J. Psychiatry61, 343–348. 10.1080/08039480701643290
45
de SousaD. P.SilvaR. H. N.SilvaE. F. D.GavioliE. C. (2017). Essential Oils and Their Constituents: An Alternative Source for Novel Antidepressants. Molecules22, E1290. 10.3390/molecules22081290
46
DhifiW.BelliliS.JaziS.BahloulN.MnifW. (2016). Essential Oils' Chemical Characterization and Investigation of Some Biological Activities: A Critical Review. Medicines (Basel)3, 25. 10.3390/medicines3040025
47
Di PierroF.RissoP.SettembreR. (2018). Role in Depression of a Multi-Fractionated versus a Conventional Hypericum perforatum Extract. Panminerva Med.60, 156–160. 10.23736/S0031-0808.18.03518-8
48
DonatoP.BonaccorsiI.RussoM.DugoP. (2014). Determination of New Bioflavonoids in Bergamot (Citrus Bergamia) Peel Oil by Liquid Chromatography Coupled to Tandem Ion Trap-Time-Of-Flight Mass Spectrometry. Flavour Fragr. J.29, 131–136. 10.1002/ffj.3188
49
DonelliD.AntonelliM.BellinazziC.GensiniG. F.FirenzuoliF. (2019). Effects of Lavender on Anxiety: A Systematic Review and Meta-Analysis. Phytomedicine65, 153099. 10.1016/j.phymed.2019.153099
50
EbrahimiH.MardaniA.BasirinezhadM. H.HamidzadehA.EskandariF. (2021). The Effects of Lavender and Chamomile Essential Oil Inhalation Aromatherapy on Depression, Anxiety and Stress in Older Community-Dwelling People: A Randomized Controlled Trial. Explore, S1550-8307(21)00001-X. 10.1016/j.explore.2020.12.012
51
Farshbaf-KhaliliA.KamalifardM.NamadianM. (2018). Comparison of the Effect of Lavender and Bitter orange on Anxiety in Postmenopausal Women: A Triple-Blind, Randomized, Controlled Clinical Trial. Complement. Ther. Clin. Pract.31, 132–138. 10.1016/j.ctcp.2018.02.004
52
FaturiC. B.LeiteJ. R.AlvesP. B.CantonA. C.Teixeira-SilvaF. (2010). Anxiolytic-like Effect of Sweet orange Aroma in Wistar Rats. Prog. Neuropsychopharmacol. Biol. Psychiatry34, 605–609. 10.1016/j.pnpbp.2010.02.020
53
FayaziS.BabashahiM.RezaeiM. (2011). The Effect of Inhalation Aromatherapy on Anxiety Level of the Patients in Preoperative Period. Iran J. Nurs. Midwifery Res.16, 278–283. PMID: 23449862
54
FeiginV. L.NicholsE.AlamT.BannickM. S.BeghiE.BlakeN.et al (2019). Global, Regional, and National burden of Neurological Disorders, 1990-2016: a Systematic Analysis for the Global Burden of Disease Study 2016. Lancet Neurol.18, 459–480. 10.1016/S1474-4422(18)30499-X
55
FekaduW.CraigT. K. J.KebedeD.MedhinG.FekaduA. (2021). Multidimensional and Intergenerational Impact of Severe Mental Disorders. EClinicalMedicine41, 101151. 10.1016/j.eclinm.2021.101151
56
FernandesL. C. B.CostaI. M.FreireM. A. M.LimaF. O. V.NetaF. I.de Souza LucenaE. E.et al (2021). Essential Oils in Experimental Models of Neuropsychiatric Disorders: A Systematic Review. Curr. Neuropharmacology19, 1738–1759. 10.2174/1570159X19666210421091734
57
FrancoL.BlanckT. J.DuganK.KlineR.ShanmugamG.GalottiA.et al (2016). Both lavender Fleur Oil and Unscented Oil Aromatherapy Reduce Preoperative Anxiety in Breast Surgery Patients: a Randomized Trial. J. Clin. Anesth.33, 243–249. 10.1016/j.jclinane.2016.02.032
58
FreemanD.SheavesB.WaiteF.HarveyA. G.HarrisonP. J. (2020). Sleep Disturbance and Psychiatric Disorders. Lancet Psychiatry7, 628–637. 10.1016/S2215-0366(20)30136-X
59
FungT. K. H.LauB. W. M.NgaiS. P. C.TsangH. W. H. (2021). Therapeutic Effect and Mechanisms of Essential Oils in Mood Disorders: Interaction between the Nervous and Respiratory Systems. Int. J. Mol. Sci.22, 4844. 10.3390/ijms22094844
60
GarakaniA.MurroughJ. W.FreireR. C.ThomR. P.LarkinK.BuonoF. D.et al (2020). Pharmacotherapy of Anxiety Disorders: Current and Emerging Treatment Options. Front. Psychiatry11, 595584. 10.3389/fpsyt.2020.595584
61
GhazizadehJ.Sadigh-EteghadS.MarxW.FakhariA.HamedeyazdanS.TorbatiM.et al (2021). The Effects of Lemon Balm (Melissa Officinalis L.) on Depression and Anxiety in Clinical Trials: A Systematic Review and Meta-Analysis. Phytother Res.35, 6690–6705. 10.1002/ptr.7252
62
GiacobbeP.FlintA. (2018). Diagnosis and Management of Anxiety Disorders. Continuum (Minneap Minn)24, 893–919. 10.1212/CON.0000000000000607
63
GnattaJ. R.KurebayashiL. F.TurriniR. N.SilvaM. J. (2016). Aromatherapy and Nursing: Historical and Theoretical conception. Rev. Esc. Enferm. USP50, 130–136. 10.1590/S0080-623420160000100017
64
González-MasM. C.RamblaJ. L.López-GresaM. P.BlázquezM. A.GranellA. (2019). Volatile Compounds in Citrus Essential Oils: A Comprehensive Review. Front. Plant Sci.10, 12. 10.3389/fpls.2019.00012
65
GriebelG.HolmesA. (2013). 50 Years of Hurdles and hope in Anxiolytic Drug Discovery. Nat. Rev. Drug Discov.12, 667–687. 10.1038/nrd4075
66
GuadagnaS.BarattiniD. F.RosuS.Ferini-StrambiL. (2020). Plant Extracts for Sleep Disturbances: A Systematic Review. Evid. Based Complement. Alternat Med.2020, 3792390. 10.1155/2020/3792390
67
GuillemainJ.RousseauA.DelaveauP. (1989). Neurodepressive Effects of the Essential Oil of Lavandula Angustifolia Mill. Ann. Pharm. Fr47, 337–343.
68
GuoP.LiP.ZhangX.LiuN.WangJ.YangS.et al (2020). The Effectiveness of Aromatherapy on Preoperative Anxiety in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. J. Nurs. Stud.111, 103747. 10.1016/j.ijnurstu.2020.103747
69
HajibagheriA.BabaiiA.Adib-HajbagheryM. (2014). Effect of Rosa Damascene Aromatherapy on Sleep Quality in Cardiac Patients: A Randomized Controlled Trial. Complement. Ther. Clin. Pract.20, 159–163. 10.1016/j.ctcp.2014.05.001
70
HamidH. A.RamliA. N.YusoffM. M. (2017). Indole Alkaloids from Plants as Potential Leads for Antidepressant Drugs: A Mini Review. Front. Pharmacol.8, 96. 10.3389/fphar.2017.00096
71
HanX.GibsonJ.EggettD. L.ParkerT. L. (2017). Bergamot (Citrus Bergamia) Essential Oil Inhalation Improves Positive Feelings in the Waiting Room of a Mental Health Treatment Center: A Pilot Study. Phytother Res.31, 812–816. 10.1002/ptr.5806
72
HansenH. V.ChristensenK. I. (2009). The Common Chamomile and the Scentless Mayweed Revisited. Taxon58, 261–264. 10.1002/tax.581024
73
Hashikawa-HobaraN.OtsukaA.IshikawaR.HashikawaN. (2019). Roman Chamomile Inhalation Combined with Clomipramine Treatment Improves Treatment-Resistant Depression-like Behavior in Mice. Biomed. Pharmacother.118, 109263. 10.1016/j.biopha.2019.109263
74
HaslerG. (2020). Understanding Mood in Mental Disorders. World Psychiatry19, 56–57. 10.1002/wps.20719
75
HillhouseT. M.PorterJ. H. (2015). A Brief History of the Development of Antidepressant Drugs: From Monoamines to Glutamate. Exp. Clin. Psychopharmacol.23, 1–21. 10.1037/a0038550
76
HongratanaworakitT. (2011). Aroma-therapeutic Effects of Massage Blended Essential Oils on Humans. Nat. Prod. Commun.6, 1199–1204. 10.1177/1934578x1100600838
77
HongratanaworakitT. (2004). Physiological Effects in Aromatherapy. Songklanakarin J. Sci. Techn.26, 9.
78
HwangE.ShinS. (2015). The Effects of Aromatherapy on Sleep Improvement: a Systematic Literature Review and Meta-Analysis. J. Altern. Complement. Med.21, 61–68. 10.1089/acm.2014.0113
79
IllumL. (2003). Nasal Drug Delivery-Ppossibilities, Problems and Solutions. J. Control. Release87, 187–198. 10.1016/S0168-3659(02)00363-2
80
InformedHealth.org. (2021). Depression: How Effective Are Antidepressants? - InformedHealth.Org - NCBI BookshelfAvailable at: https://www.ncbi.nlm.nih.gov/books/NBK361016/[Accessed October 7, 2021].
81
JiaY.ZouJ.WangY.ZhangX.ShiY.LiangY.et al (2021). Action Mechanism of Roman Chamomile in the Treatment of Anxiety Disorder Based on Network Pharmacology. J. Food Biochem.45, e13547. 10.1111/jfbc.13547
82
JodakiK.AbdiK.MousaviM. S.MokhtariR.AsayeshH.VandaliV.et al (2021). Effect of Rosa Damascene Aromatherapy on Anxiety and Sleep Quality in Cardiac Patients: A Randomized Controlled Trial. Complement. Ther. Clin. Pract.42, 101299. 10.1016/j.ctcp.2020.101299
83
JorgeR. E.ArciniegasD. B. (2014). Mood Disorders after TBI. Psychiatr. Clin. North. Am.37, 13–29. 10.1016/j.psc.2013.11.005
84
KagawaD.JokuraH.OchiaiR.TokimitsuI.TsuboneH. (2003). The Sedative Effects and Mechanism of Action of Cedrol Inhalation with Behavioral Pharmacological Evaluation. Planta Med.69, 637–641. 10.1055/s-2003-41114
85
KangH. J.NamE. S.LeeY.KimM. (2019). How Strong Is the Evidence for the Anxiolytic Efficacy of Lavender?: Systematic Review and Meta-Analysis of Randomized Controlled Trials. Asian Nurs. Res. (Korean Soc. Nurs. Sci.13, 295–305. 10.1016/j.anr.2019.11.003
86
KaradagE.SamanciogluS.OzdenD.BakirE. (2017). Effects of Aromatherapy on Sleep Quality and Anxiety of Patients. Nurs. Crit. Care22, 105–112. 10.1111/nicc.12198
87
KaranN. B. (2019). Influence of Lavender Oil Inhalation on Vital Signs and Anxiety: A Randomized Clinical Trial. Physiol. Behav.211, 112676. 10.1016/j.physbeh.2019.112676
88
KimK. J.JungY. S.YouD. M.LeeS. H.LeeG.KwonK. B.et al (2021). Neuroprotective Effects of Ethanolic Extract from Dry Rhodiola Rosea L. Rhizomes. Food Sci. Biotechnol.30, 287–297. 10.1007/s10068-020-00868-7
89
KimM.NamE. S.LeeY.KangH.-J. (2021). Effects of Lavender on Anxiety, Depression, and Physiological Parameters: Systematic Review and Meta-Analysis. Asian Nurs. Res.15, 279–290. S1976131721000773. 10.1016/j.anr.2021.11.001
90
KoL. W.SuC. H.YangM. H.LiuS. Y.SuT. P. (2021). A Pilot Study on Essential Oil Aroma Stimulation for Enhancing Slow-Wave EEG in Sleeping Brain. Sci. Rep.11, 1078. 10.1038/s41598-020-80171-x
91
KokR. M.ReynoldsC. F. (2017). Management of Depression in Older Adults: A Review. JAMA317, 2114–2122. 10.1001/jama.2017.5706
92
KomiyaM.TakeuchiT.HaradaE. (2006). Lemon Oil Vapor Causes an Anti-stress Effect via Modulating the 5-HT and DA Activities in Mice. Behav. Brain Res.172, 240–249. 10.1016/j.bbr.2006.05.006
93
KongY.WangT.WangR.MaY.SongS.LiuJ.et al (2017). Inhalation of Roman Chamomile Essential Oil Attenuates Depressive-like Behaviors in Wistar Kyoto Rats. Sci. China Life Sci.60, 647–655. 10.1007/s11427-016-9034-8
94
KooM. (2017). A Bibliometric Analysis of Two Decades of Aromatherapy Research. BMC Res. Notes10, 46. 10.1186/s13104-016-2371-1
95
KoyamaS.HeinbockelT. (2020). The Effects of Essential Oils and Terpenes in Relation to Their Routes of Intake and Application. Int. J. Mol. Sci.21, E1558. 10.3390/ijms21051558
96
KrawczykP.ŚwięcickiŁ. (2020). ICD-11 vs. ICD-10 - a Review of Updates and Novelties Introduced in the Latest Version of the WHO International Classification of Diseases. Psychiatr. Pol.54, 7–20. 10.12740/PP/103876
97
LahlouM. (2004). Essential Oils and Fragrance Compounds: Bioactivity and Mechanisms of Action. Flavour Fragr. J.19, 159–165. 10.1002/ffj.1288
98
LehrnerJ.MarwinskiG.LehrS.JohrenP.DeeckeL. (2005). Ambient Odors of orange and Lavender Reduce Anxiety and Improve Mood in a Dental Office. Physiol. Behav.86, 92–95. 10.1016/j.physbeh.2005.06.031
99
LiangX.WangX.ZhaoG.HuangX.XuX.DongW. (2021). Research Progress of Essential Oil as a New Complementary Therapy in the Treatment of Depression. Mini Rev. Med. Chem.21, 2276–2289. 10.2174/1389557521666210219161747
100
LieG.WilsonA.CampionT.AdamsA. (2021). What's that Smell? A Pictorial Review of the Olfactory Pathways and Imaging Assessment of the Myriad Pathologies that Can Affect Them. Insights Imaging12, 7. 10.1186/s13244-020-00951-x
101
LindeK.BernerM. M.KristonL. (2008). St John's Wort for Major Depression. Cochrane Database Syst. Rev.2008 (4), CD000448. 10.1002/14651858.CD000448.pub3
102
LindeK.MulrowC.BernerM.EggerM.The Cochrane Collaboration (2005). “St John's Wort for Depression,” in Cochrane Database of Systematic Reviews (Chichester, UK: John Wiley & Sons), CD000448. 10.1002/14651858.CD000448.pub2
103
Lizarraga‐ValderramaL. R. (2021). Effects of Essential Oils on central Nervous System: Focus on Mental Health. Phytotherapy Res.35, 657–679. 10.1002/ptr.6854
104
LópezV.NielsenB.SolasM.RamírezM. J.JägerA. K. (2017). Exploring Pharmacological Mechanisms of Lavender (Lavandula Angustifolia) Essential Oil on Central Nervous System Targets. Front. Pharmacol.8, 280. 10.3389/fphar.2017.00280
105
LvX. N.LiuZ. J.ZhangH. J.TzengC. M. (2013). Aromatherapy and the Central Nerve System (CNS): Therapeutic Mechanism and its Associated Genes. Curr. Drug Targets14, 872–879. 10.2174/1389450111314080007
106
MaG.ZhengQ.XuM.ZhouX.LuL.LiZ.et al (2018). Rhodiola Rosea L. Improves Learning and Memory Function: Preclinical Evidence and Possible Mechanisms. Front. Pharmacol.9, 1415. 10.3389/fphar.2018.01415
107
MahdavikianS.RezaeiM.ModarresiM.KhatonyA. (2020). Comparing the Effect of Aromatherapy with Peppermint and Lavender on the Sleep Quality of Cardiac Patients: a Randomized Controlled Trial. Sleep Sci. Pract.4, 10. 10.1186/s41606-020-00047-x
108
MalloggiE.MenicucciD.CesariV.FrumentoS.GemignaniA.BertoliA. (2021). Lavender Aromatherapy: A Systematic Review from Essential Oil Quality and Administration Methods to Cognitive Enhancing Effects. Appl. Psychol. Health Well‐being, 1–28. 10.1111/aphw.12310
109
MangoliniV. I.AndradeL. H.Lotufo-NetoF.WangY. P. (2019). Treatment of Anxiety Disorders in Clinical Practice: a Critical Overview of Recent Systematic Evidence. Clinics (Sao Paulo)74, e1316. 10.6061/clinics/2019/e1316
110
MannC.StabaE. J. (1986). The Chemistry, Pharmacology, and Commercial Formulations of Chamomile. Herbs, spices, Med. plants : Recent Adv. Bot. Hortic. Pharmacol. (Usa)1, 235–280. Available at: https://agris.fao.org/agris-search/search.do?recordID=US8700832 (Accessed March 8, 2022).
111
MannucciC.NavarraM.CalapaiF.SqueriR.GangemiS.CalapaiG. (2017). Clinical Pharmacology of Citrus Bergamia: A Systematic Review. Phytother. Res.31, 27–39. 10.1002/ptr.5734
112
MartinecR. (2012). Some Implications of Using Aromatherapy as Complementary Method in Oncology Setting. Arch. Oncol.20, 70–74. 10.2298/AOO1204070M
113
MarvelC. L.ParadisoS. (2004). Cognitive and Neurological Impairment in Mood Disorders. Psychiatr. Clin. North. Am.27, 19–viii. 10.1016/S0193-953X(03)00106-0
114
MasagoR.MatsudaT.KikuchiY.MiyazakiY.IwanagaK.HaradaH.et al (2000). Effects of Inhalation of Essential Oils on EEG Activity and Sensory Evaluation. J. Physiol. Anthropol. Appl. Hum. Sci19, 35–42. 10.2114/jpa.19.35
115
McKayD. L.BlumbergJ. B. (2006). A Review of the Bioactivity and Potential Health Benefits of Chamomile tea (Matricaria Recutita L.). Phytother Res.20, 519–530. 10.1002/ptr.1900
116
MenY.ChenJ.YangY.CaoY. (2021). The strength of evidence of aromatherapy alleviating preoperative anxiety in adults: Comment on Guo et al. 2020. Int. J. Nurs. Stud.115, 103829. 10.1016/j.ijnurstu.2020.103829
117
MirajS.KianiS.Rafieian-Kopaei (2017). Melissa Officinalis L: A Review Study with an Antioxidant Prospective. J. Evid. Based Complement. Altern Med22, 385–394. 10.1177/2156587216663433
118
MomenN. C.Plana-RipollO.AgerboE.BenrosM. E.BørglumA. D.ChristensenM. K.et al (2020). Association between Mental Disorders and Subsequent Medical Conditions. N. Engl. J. Med.382, 1721–1731. 10.1056/NEJMoa1915784
119
MondelloL.VerzeraA.PrevitiP.CrispoF.DugoG. (1998). Multidimensional Capillary GC−GC for the Analysis of Complex Samples. 5. Enantiomeric Distribution of Monoterpene Hydrocarbons, Monoterpene Alcohols, and Linalyl Acetate of Bergamot (Citrus bergamia Risso et Poiteau) Oils. J. Agric. Food Chem.46, 4275–4282. 10.1021/jf980228u
120
MoufidaS.MarzoukB. (2003). Biochemical Characterization of Blood orange, Sweet orange, Lemon, Bergamot and Bitter orange. Phytochemistry62, 1283–1289. 10.1016/S0031-9422(02)00631-3
121
MPhamW. S.SiripornpanichV.PiriyapunyapornT.KotchabhakdiN.RuangrungsiN. (2012). The Effects of Lavender Oil Inhalation on Emotional States, Autonomic Nervous System, and Brain Electrical Activity. J. Med. Assoc. Thai.95, 598606. PMID: 22612017
122
MunirS.TakovV. (2021). “Generalized Anxiety Disorder,” in StatPearls (Treasure Island (FL): StatPearls Publishing). Available at: http://www.ncbi.nlm.nih.gov/books/NBK441870/(Accessed October 6, 2021).
123
MuzG.TaşcıS. (2017). Effect of Aromatherapy via Inhalation on the Sleep Quality and Fatigue Level in People Undergoing Hemodialysis. Appl. Nurs. Res.37, 28–35. 10.1016/j.apnr.2017.07.004
124
NagayamaS.HommaR.ImamuraF. (2014). Neuronal Organization of Olfactory Bulb Circuits. Front. Neural Circuits.8, 98. 10.3389/fncir.2014.00098
125
NavarraM.MannucciC.DelbòM.CalapaiG. (2015). Citrus Bergamia Essential Oil: from Basic Research to Clinical Application. Front. Pharmacol.6, 36. 10.3389/fphar.2015.00036
126
OzkaramanA.DügümÖ.Özen YılmazH.Usta YesilbalkanÖ. (2018). Aromatherapy: The Effect of Lavender on Anxiety and Sleep Quality in Patients Treated with Chemotherapy. Clin. J. Oncol. Nurs.22, 203–210. 10.1188/18.CJON.203-210
127
PagelJ. F.ParnesB. L. (2001). Medications for the Treatment of Sleep Disorders: An Overview. Prim. Care Companion J. Clin. Psychiatry3, 118–125. 10.4088/pcc.v03n0303
128
PanossianA.WikmanG.SarrisJ. (2010). Rosenroot (Rhodiola Rosea): Traditional Use, Chemical Composition, Pharmacology and Clinical Efficacy. Phytomedicine17, 481–493. 10.1016/j.phymed.2010.02.002
129
PanossianA. G.EfferthT.ShikovA. N.PozharitskayaO. N.KuchtaK.MukherjeeP. K.et al (2021). Evolution of the Adaptogenic Concept from Traditional Use to Medical Systems: Pharmacology of Stress- and Aging-Related Diseases. Med. Res. Rev.41, 630–703. 10.1002/med.21743
130
PauseB. M.MirandaA.GöderR.AldenhoffJ. B.FerstlR. (2001). Reduced Olfactory Performance in Patients with Major Depression. J. Psychiatr. Res.35, 271–277. 10.1016/s0022-3956(01)00029-2
131
PerryN.PerryE. (2006). Aromatherapy in the Management of Psychiatric Disorders: Clinical and Neuropharmacological Perspectives. CNS Drugs20, 257–280. 10.2165/00023210-200620040-00001
132
PoianaM.MincioneA.GionfriddoF.CastaldoD. (2003). Supercritical Carbon Dioxide Separation of Bergamot Essential Oil by a Countercurrent Process. Flavour Fragr. J.18, 429–435. 10.1002/ffj.1245
133
QaseemA.BarryM. J.KansagaraD.Clinical Guidelines Committee of the American College of Physicians (2016). Nonpharmacologic versus Pharmacologic Treatment of Adult Patients with Major Depressive Disorder: A Clinical Practice Guideline from the American College of Physicians. Ann. Intern. Med.164, 350. doi:10.7326/M15-2570
134
RaisonC. L.CapuronL.MillerA. H. (2006). Cytokines Sing the Blues: Inflammation and the Pathogenesis of Depression. Trends Immunol.27, 24–31. 10.1016/j.it.2005.11.006
135
RamachandraihC. T.SubramanyamN.BarK. J.BakerG.YeraganiV. K. (2011). Antidepressants: From MAOIs to SSRIs and More. Indian J. Psychiatry53, 180–182. 10.4103/0019-5545.82567
136
ReedG. M.FirstM. B.KoganC. S.HymanS. E.GurejeO.GaebelW.et al (2019). Innovations and Changes in the ICD-11 Classification of Mental, Behavioural and Neurodevelopmental Disorders. World Psychiatry18, 3–19. 10.1002/wps.20611
137
RomanaR. K.SharmaA.GuptaV.KaurR.KumarS.BansalP. (2020). Was Hawan Designed to Fight Anxiety-Scientific Evidences?J. Relig Health59, 505–521. 10.1007/s10943-016-0345-1
138
RombolàL.CorasanitiM. T.RotirotiD.TassorelliC.SakuradaS.BagettaG.et al (2009). Effects of Systemic Administration of the Essential Oil of Bergamot (BEO) on Gross Behaviour and EEG Power Spectra Recorded from the Rat hippocampus and Cerebral Cortex. Funct. Neurol.24, 107–112. PMID:19775539
139
RombolàL.TridicoL.ScuteriD.SakuradaT.SakuradaS.MizoguchiH.et al (2017). Bergamot Essential Oil Attenuates Anxiety-like Behaviour in Rats. Molecules22, 614. 10.3390/molecules22040614
140
SaiyudthongS.MarsdenC. A. (2011). Acute Effects of Bergamot Oil on Anxiety-Related Behaviour and Corticosterone Level in Rats. Phytother Res.25, 858–862. 10.1002/ptr.3325
141
SalamatiA.MashoufS.MojabF. (2017). Effect of Inhalation of Lavender Essential Oil on Vital Signs in Open Heart Surgery ICU. Iran J. Pharm. Res.16, 404–409. PMCID: PMC5423266
142
SanacoraG.YanZ.PopoliM. (2022). The Stressed Synapse 2.0: Pathophysiological Mechanisms in Stress-Related Neuropsychiatric Disorders. Nat. Rev. Neurosci.23, 86–103. 10.1038/s41583-021-00540-x
143
Sánchez-VidañaD. I.NgaiS. P.HeW.ChowJ. K.LauB. W.TsangH. W. (2017). The Effectiveness of Aromatherapy for Depressive Symptoms: A Systematic Review. Evid. Based Complement. Alternat Med.2017, 5869315–5869321. 10.1155/2017/5869315
144
Sánchez-VidañaD. I.PoK. K.FungT. K.ChowJ. K.LauW. K.SoP. K.et al (2019). Lavender Essential Oil Ameliorates Depression-like Behavior and Increases Neurogenesis and Dendritic Complexity in Rats. Neurosci. Lett.701, 180–192. 10.1016/j.neulet.2019.02.042
145
SannaM. D.LesF.LopezV.GaleottiN. (2019). Lavender (Lavandula Angustifolia Mill.) Essential Oil Alleviates Neuropathic Pain in Mice with Spared Nerve Injury, Front. Pharmacol.10, 472. 10.3389/fphar.2019.00472
146
SantamariaJ.IranzoA. (2014). Sleep Disorders Matter in Neurology. Lancet Neurol.13, 18–20. 10.1016/S1474-4422(13)70273-4
147
SchneiderR.SingerN.SingerT. (2018). Medical Aromatherapy Revisited-Basic Mechanisms, Critique, and a New Development. Hum. Psychopharmacol. Clin. Exp.34 (2), e2683. 10.1002/hup.2683
148
ScuteriD.RombolàL.MorroneL. A.BagettaG.SakuradaS.SakuradaT.et al (2019). Neuropharmacology of the Neuropsychiatric Symptoms of Dementia and Role of Pain: Essential Oil of Bergamot as a Novel Therapeutic Approach. Int. J. Mol. Sci.20, 3327. 10.3390/ijms20133327
149
SelvarajK.GowthamarajanK.KarriV. V. S. R. (2017). Nose to Brain Transport Pathways an Overview: Potential of Nanostructured Lipid Carriers in Nose to Brain Targeting. Artif. Cell Nanomedicine, Biotechnol.46, 8. 10.1080/21691401.2017.1420073
150
SeolG. H.ShimH. S.KimP. J.MoonH. K.LeeK. H.ShimI.et al (2010). Antidepressant-like Effect of Salvia Sclarea Is Explained by Modulation of Dopamine Activities in Rats. J. Ethnopharmacol130, 187–190. 10.1016/j.jep.2010.04.035
151
SetzerW. N. (2009). Essential Oils and Anxiolytic Aromatherapy. Nat. Prod. Commun.4, 1305–1316. 10.1177/1934578x0900400928
152
ShakeriA.SahebkarA.JavadiB. (2016). Melissa Officinalis L. - A Review of its Traditional Uses, Phytochemistry and Pharmacology. J. Ethnopharmacol188, 204–228. 10.1016/j.jep.2016.05.010
153
ShawD.AnnettJ. M.DohertyB.LeslieJ. C. (2007). Anxiolytic Effects of Lavender Oil Inhalation on Open-Field Behaviour in Rats. Phytomedicine14, 613–620. 10.1016/j.phymed.2007.03.007
154
SinghO.KhanamZ.MisraN.SrivastavaM. K. (2011). Chamomile (Matricaria Chamomilla L.): An Overview. Pharmacogn Rev.5, 82–95. 10.4103/0973-7847.79103
155
SlavichG. M.IrwinM. R. (2014). From Stress to Inflammation and Major Depressive Disorder: a Social Signal Transduction Theory of Depression. Psychol. Bull.140, 774–815. 10.1037/a0035302
156
SmithT. D.BhatnagarK. P. (2019). “Anatomy of the Olfactory System,” in Handbook of Clinical Neurology164, 17–28. 10.1016/B978-0-444-63855-7.00002-2
157
SoaresG. A. B. E.BhattacharyaT.ChakrabartiT.TagdeP.CavaluS. (2021). Exploring Pharmacological Mechanisms of Essential Oils on the Central Nervous System. Plants11, 21. 10.3390/plants11010021
158
SowndhararajanK.KimS. (2016). Influence of Fragrances on Human Psychophysiological Activity: With Special Reference to Human Electroencephalographic Response. Sci. Pharm.84, 724–751. 10.3390/scipharm84040724
159
SrivastavaJ. K.ShankarE.GuptaS. (2010). Chamomile: A Herbal Medicine of the Past with a Bright Future (Review). Mol. Med. Rep.3 (6), 895–901. 10.3892/mmr.2010.377
160
StrousR. D.ShoenfeldY. (2006). To Smell the Immune System: Olfaction, Autoimmunity and Brain Involvement. Autoimmun. Rev.6, 54–60. 10.1016/j.autrev.2006.07.002
161
TafetG. E.Idoyaga-VargasV. P.AbulafiaD. P.CalandriaJ. M.RoffmanS. S.ChiovettaA.et al (2001). Correlation between Cortisol Level and Serotonin Uptake in Patients with Chronic Stress and Depression. Cogn. Affect Behav. Neurosci.1, 388–393. 10.3758/cabn.1.4.388
162
TaiY.LingC.WangC.WangH.SuL.YangL.et al (2020). Analysis of Terpenoid Biosynthesis Pathways in German Chamomile (Matricaria Recutita) and Roman Chamomile (Chamaemelum Nobile) Based on Co-expression Networks. Genomics112, 1055–1064. 10.1016/j.ygeno.2019.10.023
163
TakedaA.WatanukiE.KoyamaS. (2017). Effects of Inhalation Aromatherapy on Symptoms of Sleep Disturbance in the Elderly with Dementia. Evid. Based Complement. Alternat Med.2017, 1902807. 10.1155/2017/1902807
164
TangY.GongM.QinX.SuH.WangZ.DongH. (2021). The Therapeutic Effect of Aromatherapy on Insomnia: a Meta-Analysis. J. Affect Disord.288, 1–9. 10.1016/j.jad.2021.03.066
165
TanidaM.KatsuyamaM.SakataniK. (2008). Effects of Fragrance Administration on Stress-Induced Prefrontal Cortex Activity and Sebum Secretion in the Facial Skin. Neurosci. Lett.432, 157–161. 10.1016/j.neulet.2007.12.014
166
ThibautF. (2017). Anxiety Disorders: a Review of Current Literature. Dialogues Clin. Neurosci.19, 87–88. 10.31887/DCNS.2017.19.2/fthibaut
167
TsangH. W.HoT. Y. (2010). A Systematic Review on the Anxiolytic Effects of Aromatherapy on Rodents under Experimentally Induced Anxiety Models. Rev. Neurosci.21, 141–152. 10.1515/revneuro.2010.21.2.141
168
TuQ.-B.WangP.-Y.ShengS.XuY.WangJ.-Z.YouS.et al (2020). Microencapsulation and Antimicrobial Activity of Plant Essential Oil against Ralstonia Solanacearum. Waste Biomass Valor.11, 5273–5282. 10.1007/s12649-020-00987-6
169
VerzeraA.TrozziA.GazeaF.CicciarelloG.CotroneoA. (2003). Effects of rootstock on the composition of bergamot (Citrus bergamia Risso et Poiteau) essential oil. J. Agric. Food Chem.51, 206–210. 10.1021/jf0206872
170
VieiraA. J.BeserraF. P.SouzaM. C.TottiB. M.RozzaA. L. (2018). Limonene: Aroma of Innovation in Health and Disease. Chem. Biol. Interact283, 97–106. 10.1016/j.cbi.2018.02.007
171
VigoD.ThornicroftG.AtunR. (2016). Estimating the True Global burden of Mental Illness. Lancet Psychiatry3, 171–178. 10.1016/S2215-0366(15)00505-2
172
WangQ. (2021). The Social Determinants of Depressive Disorders in China. Lancet Psychiatry8 (11), 939–940. 10.1016/S2215-0366(21)00389-8
173
WangS. J.WuZ. F.YangM.WangY. Q.HuP. Y.JieX. L.et al (2014). Application Characteristics and Situation Analysis of Volatile Oils in Database of Chinese Patent Medicine. Zhongguo Zhong Yao Za Zhi39, 3379–3383. 10.4268/cjcmm20141735
174
WangZ. J.HeinbockelT. (2018). Essential Oils and Their Constituents Targeting the GABAergic System and Sodium Channels as Treatment of Neurological Diseases. Molecules23, 1061. 10.3390/molecules23051061
175
WatanabeE.KuchtaK.KimuraM.RauwaldH. W.KameiT.ImanishiJ. (2015). Effects of Bergamot (Citrus Bergamia (Risso) Wright & Arn.) Essential Oil Aromatherapy on Mood States, Parasympathetic Nervous System Activity, and Salivary Cortisol Levels in 41 Healthy Females. Complement. Med. Res.22, 43–49. 10.1159/000380989
176
WatanukiS.KimY. K. (2005). Physiological Responses Induced by Pleasant Stimuli. J. Physiol. Anthropol. Appl. Hum. Sci24, 135–138. 10.2114/jpa.24.135
177
WongM. L.O'KirwanF.HannestadJ. P.IrizarryK. J.ElashoffD.LicinioJ. (2004). St John's Wort and Imipramine-Induced Gene Expression Profiles Identify Cellular Functions Relevant to Antidepressant Action and Novel Pharmacogenetic Candidates for the Phenotype of Antidepressant Treatment Response. Mol. Psychiatry9, 237–251. 10.1038/sj.mp.4001470
178
XiongM.LiY.TangP.ZhangY.CaoM.NiJ.et al (2018). Effectiveness of Aromatherapy Massage and Inhalation on Symptoms of Depression in Chinese Community-Dwelling Older Adults. J. Altern. Complement. Med.24, 717–724. 10.1089/acm.2017.0320
179
YimV. W.NgA. K.TsangH. W.LeungA. Y. (2009). A Review on the Effects of Aromatherapy for Patients with Depressive Symptoms. J. Altern. Complement. Med.15, 187–195. 10.1089/acm.2008.0333
180
YuP. H. (2000). Effect of the Hypericum perforatum Extract on Serotonin Turnover in the Mouse Brain. Pharmacopsychiatry33, 60–65. 10.1055/s-2000-7970
181
YunS.ReynoldsR. P.MasiulisI.EischA. J. (2016). Re-evaluating the Link between Neuropsychiatric Disorders and Dysregulated Adult Neurogenesis. Nat. Med.22, 1239–1247. 10.1038/nm.4218
182
ZanosP.GouldT. D. (2018). Mechanisms of Ketamine Action as an Antidepressant. Mol. Psychiatry23, 801–811. 10.1038/mp.2017.255
183
ZarzoM. (2007). The Sense of Smell: Molecular Basis of Odorant Recognition. Biol. Rev. Camb Philos. Soc.82, 455–479. 10.1111/j.1469-185X.2007.00019.x
184
ZhangN.YaoL. (2019). Anxiolytic Effect of Essential Oils and Their Constituents: A Review. J. Agric. Food Chem.67, 13790–13808. 10.1021/acs.jafc.9b00433
185
ZhangY.WuY.ChenT.YaoL.LiuJ.PanX.et al (2013). Assessing the Metabolic Effects of Aromatherapy in Human Volunteers. Evid. Based Complement. Alternat Med.2013, 356381–356389. 10.1155/2013/356381
186
ZhongY.ZhengQ.HuP.HuangX.YangM.RenG.et al (2019). Sedative and Hypnotic Effects of Compound Anshen Essential Oil Inhalation for Insomnia. BMC Complement. Altern. Med.19, 306. 10.1186/s12906-019-2732-0
187
ZirakN.ShafieeM.SoltaniG.MirzaeiM.SahebkarA. (2019). Hypericum perforatum in the Treatment of Psychiatric and Neurodegenerative Disorders: Current Evidence and Potential Mechanisms of Action. J. Cel Physiol234, 8496–8508. 10.1002/jcp.27781
Summary
Keywords
inhalation aromatherapy, nasal-brain pathway, mood disorders, aromatic herbs, essential oils, anxiety, depression, sleep disorders
Citation
Cui J, Li M, Wei Y, Li H, He X, Yang Q, Li Z, Duan J, Wu Z, Chen Q, Chen B, Li G, Ming X, Xiong L and Qin D (2022) Inhalation Aromatherapy via Brain-Targeted Nasal Delivery: Natural Volatiles or Essential Oils on Mood Disorders. Front. Pharmacol. 13:860043. doi: 10.3389/fphar.2022.860043
Received
04 February 2022
Accepted
22 March 2022
Published
12 April 2022
Volume
13 - 2022
Edited by
Fabio Boylan, Trinity College Dublin, Ireland
Reviewed by
Astrid Sasse, Trinity College Dublin, Ireland
Laura Rombolà, University of Calabria, Italy
Updates
Copyright
© 2022 Cui, Li, Wei, Li, He, Yang, Li, Duan, Wu, Chen, Chen, Li, Ming, Xiong and Qin.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xi Ming, 863455756@qq.com; Lei Xiong, xlluck@sina.com; Dongdong Qin, qindong108@163.com
†These authors have contributed equally to this work
This article was submitted to Ethnopharmacology, a section of the journal Frontiers in Pharmacology
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.