- 1Department of Periodical Press, West China Hospital, Sichuan University, Chengdu, China
- 2West China School of Medicine, Sichuan University, Chengdu, China
- 3Department of Neurology, The Second Affiliated Hospital of Harbin Medical University, Harbin, China
- 4Department of General Surgery, Chengdu Integrated Traditional Chinese Medicine and Western Medicine Hospital, Chengdu, China
Objectives: Amidst rising global burden of depression and the associated challenges with conventional antidepressant therapies, there is a growing interest in exploring the efficacy and safety of alternative treatments. This study uses a Bayesian network meta-analysis to rigorously evaluate the therapeutic potential of Chinese herbal medicines in the treatment of depression, focusing on their comparative efficacy and safety against standard pharmacological interventions.
Methods: Five databases (PubMed, Wanfang Data, EMBASE, CNKI, and the Cochrane Library) and grey literature were searched from inception to end of July 2023 to identify studies that assessed the efficacy and safety of Chinese herbal medicines in treating depression. The response rate, Hamilton Depression Scale (HAMD) scores, and rates of adverse events were assessed through both direct and indirect comparisons. Data extraction and risk of bias assessment were meticulously performed. Statistical analysis used Markov chain Monte Carlo methods, with effect size estimates provided as odd ratios and their 95% confidence intervals.
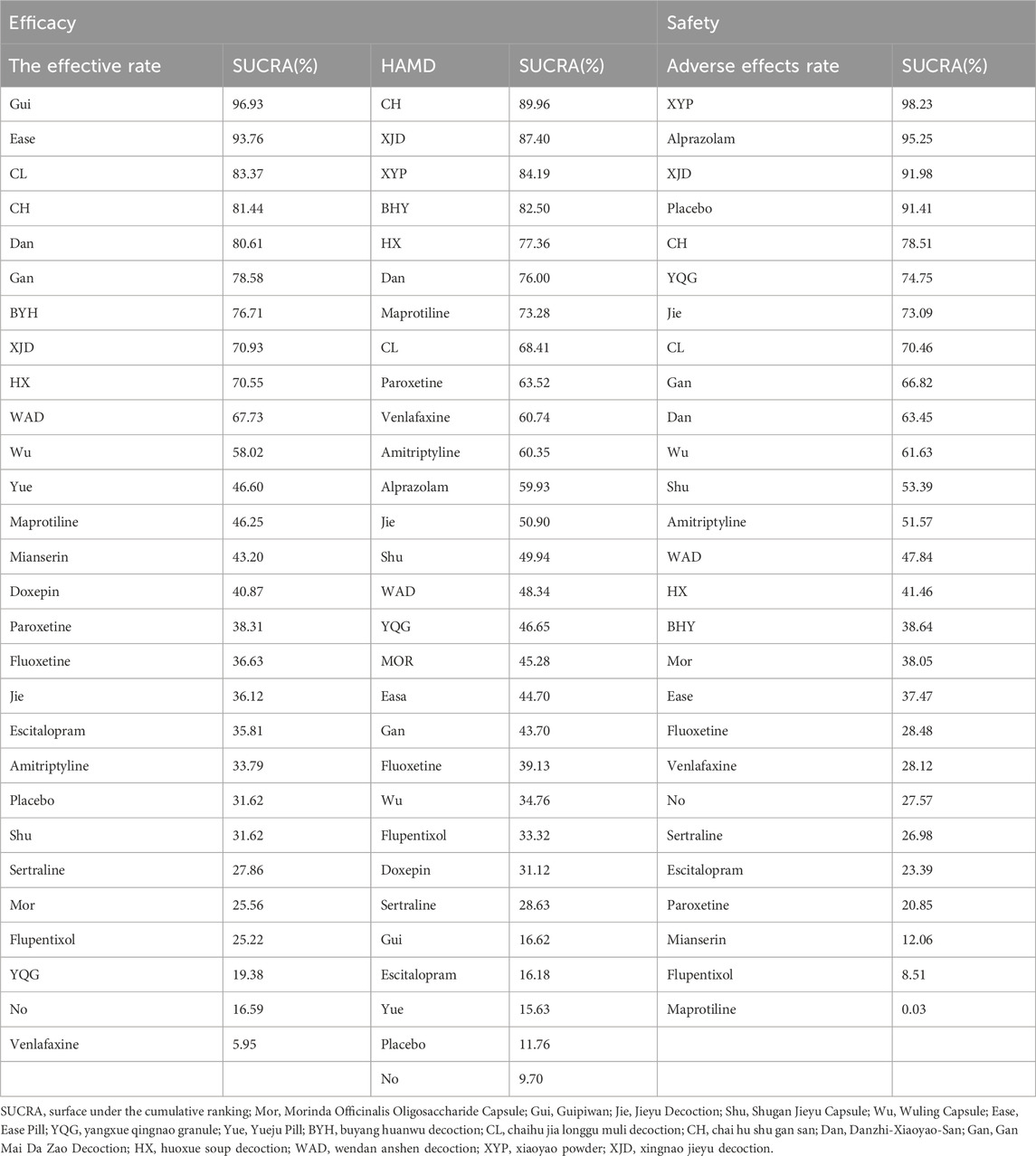
Results: A total of 198 RCTs involving 8,923 patients were analyzed, assessing 17 Chinese herbal medicines. Surface Under the Cumulative Ranking results indicated that the top three treatments with the best response rate were possibly Guipiwan, Ease Pill, and Chaihu Jia Longgu Muli Decoction; the top three treatments on the reduction of HAMD scores were Chai Hu Shu Gan San, Xingnao Jieyu Decoction, and Xiaoyao Powder; and the top three treatments with the lowest adverse effects rates were Xiaoyao Powder, Alprazolam, and Xingnao Jieyu Decoction. Interestingly, commonly used synthetic drugs such as Fluoxetine, Escitalopram, Amitriptyline, Sertraline, Flupentixol and Melitracen, and Venlafaxine, not only appeared to be less effective than specific Chinese herbal medicines (Gan Mai Da Zao Decoction, Chaihu Jia Longgu Muli Decoction, Chai Hu Shu Gan San, Danzhi-Xiaoyao-San, and Xingnao Jieyu Decoction), but they were also related to substantially higher risk of adverse events.
Conclusion: Our findings elucidate the promising therapeutic potential of Chinese herbal medicines as viable alternatives in the treatment of depression, with certain herbs demonstrating enhanced efficacy and safety profiles. The outcomes of this study advocate for the integration of these alternative modalities into contemporary depression management paradigms. However, it underscores the necessity for larger, methodologically robust trials to further validate and refine these preliminary findings.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/, identifier CRD42023452109.
Introduction
Depression is a pervasive mental disorder that causes people to experience anhedonia (Monroe and Harkness, 2022). Depression symptoms include sadness, cognitive difficulties, which reduce patients’ quality of life and social functioning (Bosc, 2000). Depression impacts approximately 3.8% of the global population. Its prevalence is notably higher in the adult demographic, affecting about 5% of this group. According to the World Health Organization, an estimated 280 million adults across the globe are afflicted with this condition (Freitas et al., 2023).
In the pharmacotherapeutic management of depressive disorders, a diverse array of antidepressant classes is employed. These include Tricyclic Antidepressants, Selective Serotonin Reuptake Inhibitors (SSRIs), Monoamine Oxidase Inhibitors, Serotonin and Noradrenaline Reuptake Inhibitors (SNRIs), Noradrenaline Reuptake Inhibitors, and Noradrenaline and Dopamine Reuptake Inhibitors. These pharmacological agents primarily function by inhibiting the transporters implicated in the reuptake of monoamines, a mechanism crucial in the modulation of mood and affective states (Dobrek and Głowacka, 2023). Additionally, several other compounds exhibit antidepressant properties. For instance, agomelatine acts as an MT1 and MT2 melatonin receptor agonist and a serotonin 5HT2 receptor antagonist, while mirtazapine is known to antagonize adrenergic alpha2-autoreceptors, alpha2-heteroreceptors, as well as 5-HT2 and 5-HT3 receptors. More recent developments in antidepressant pharmacotherapy include agents such as desvenlafaxine, vortioxetine, and vilazodone (Fournier et al., 2010; Faquih et al., 2019).
The therapeutic efficacy of antidepressants demonstrates considerable variability across the patient population. SSRIs and SNRIs are frequently prioritized as first-line treatments, owing to their favorable safety profiles and high tolerability. Empirical studies indicate that approximately 60%–70% of individuals diagnosed with depression experience a notable improvement in symptoms following their initial course of antidepressant therapy. Symptom amelioration can often be observed within a span of several weeks. However, there remains a substantial proportion, estimated at 30%–40%, who may not exhibit an adequate response to their first prescribed medication. This subset of patients may necessitate alterations in their pharmacological regimen or the incorporation of adjunctive therapeutic approaches (Irfan, 2024).
In addition, there are numerous adverse effects are caused by modern pharmacological drugs. The adverse effects of selective SSRIs include QT prolongation, serotonin syndrome, insomnia, rashes, and hyponatremia, whereas long-term use may lead to sexual dysfunction and weight gain (Goethe et al., 2007; Nachimuthu et al., 2012). Additionally, Monoamine Oxidase Inhibitors and Serotonin Reuptake Inhibitors are associated with potentially serious reactions such as hypertensive crisis, and increased risk of suicidal ideation (Sathyanarayana Rao and Yeragani, 2009; Nobile et al., 2019; Mrozek et al., 2023). Furthermore, overdoses of tricyclic antidepressants can precipitate severe cardiac complications, including sudden heart attack, tachycardia, and ventricular fibrillation (Scala et al., 2023; Yildiz et al., 2023).
In recent years, herbal medicines are gaining interests and recognitions (Saxena et al., 2023). Numerous Chinese herbal medicines have been investigated for their potential antidepressant effects (Garg et al., 2023). Various Chinese herbal medicines have been reported to have excellent antidepressant effects compared with current synthetic pharmaceuticals, such as Morinda Officinalis Oligosaccharide Capsule, Guipiwan, Jieyu Decoction, Shugan Jieyu Capsule, Wuling Capsule, Ease Pill, Yangxue Qingnao Granule, Yueju Pill, Buyang Huanwu Decoction, Chaihu Jia Longgu Muli Decoction, Chai Hu Shu Gan San, Danzhi-Xiaoyao-San, Gan Mai Da Zao Decoction, Huoxue Soup Decoction, Wendan Anshen Decoction, Xiaoyao Powder, and Xingnao Jieyu Decoction (Holden, 1987; Yeung et al., 2014a; Peng et al., 2014; Zhang et al., 2014; Feng et al., 2016; Kwon et al., 2018; Zhen et al., 2022).
The pharmacodynamic mechanisms on herbal medicines in treatment of psychiatric disorders are multifaceted. Primarily, these mechanisms encompass the modulation of neuronal communication. This is achieved through the binding of specific plant-derived metabolites to neurotransmitter and neuromodulator receptors (Sarris et al., 2011). Additionally, these herbal compounds can influence neurotransmitter synthesis and overall neurological function (Sarris, 2007). Beyond these neural interactions, herbal medicines may exert their therapeutic effects by either stimulating or sedating central nervous system activity. They also play a role in regulating and supporting the healthy functioning of the endocrine system (Kumar, 2006).
Previous published studies have only compared single Chinese herb medicine, without comparisons of multiple Chinese herb medicines. Therefore, the efficacy, tolerability, or safety is not possible to ascertain on various Chinese herb medicines. In this study, we chose common Chinese herbal medicines for depression treatment. This study rigorously evaluates specific aspects on efficacy (as measured by Hamilton Rating Scale for Depression (HAMD) score and response rate) and safety (adverse effects rate) in the context of therapeutic approaches for depression. The HAMD score is the foremost clinician-rated scale used for assessing depression severity in patients diagnosed with depressive disorders (Carrozzino et al., 2020). The response rate, defined as a reduction of ≥50% in HAMD scores at the study endpoint, is a validated and commonly employed measure of depression severity (McIntyre et al., 2005). Adverse effects rate, quantifying the proportion of patients experiencing at least one adverse event relative to the total number of patients in the intervention or control group, is a widely accepted metric for evaluating safety (Weibel et al., 2020; Dean et al., 2021; De Crescenzo et al., 2022).
Thus, this Bayesian network meta-analysis aims to synthesize and assess the existing available evidence for the efficacy and safety of various Chinese herbal medicines for the treatment of depression.
Methods
This network meta-analysis was registered in PROSPERO with accession number CRD42023452109. The protocol followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses Protocol (Moher et al., 2015). The time of registration occurred was 17 May 2023. There are not any modifications about the Preferred Reporting Items for Systematic Reviews and Meta-analyses Protocol during the study. The researchable question was performed using the PICOS (Population, Intervention, Comparison, Outcome, Study design) format. Population: patients with depression. Intervention: participants received Chinese herbal medicines. Comparison: participants received modern pharmacological antidepressants, placebo, or no-treatment. Outcome: HAMD scores, the response rate, and the incidence of drug-related adverse reactions. Study design: randomized controlled trials (RCTs).
Data searches
A systematic literature search for articles was performed in PubMed, Wanfang Data, EMBASE, CNKI, and the Cochrane Library. Grey literature was also searched. Articles were searched in English or Chinese from inception through the end of July 2023 for studies that assessed the efficacy and safety of Chinese medicines with depression. The detailed search strategy and search terms are shown in Supplementary Appendix S1.
Study selection
Two review authors (Chun Dang and Yaoheng Lu) independently screened the titles and abstracts, and differences were resolved through discussion and consensus agreement. Studies which potentially fulfilled the inclusion and exclusion criteria were identified, then full-text reviews were performed.
Inclusion criteria
The inclusion criteria were as follows: (1) Adult patients (≥18 years) with depressive symptoms were eligible. Depression was defined by the standardized diagnostic manuals (Blatch Armon, et al., 2023), such as the Diagnosis and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) or later versions (Hasin et al., 2006), the International Classification of Diseases, 10th Edition (ICD-10) (Herrmann et al., 1998), the Chinese Classification of Mental Disorders, Third Edition (CCMD-Ⅲ) or later versions. (2) The intervention group received common Chinese herbal medicines, while the control group received current synthetic pharmaceuticals, placebo, or no-treatment. All forms of Chinese herbal medicines (i.e., decoctions, formula, capsules, pills, and powders) were included. Current synthetic pharmaceuticals (i.e., Fluoxetine, Escitalopram, Amitriptyline, Maprotiline, Venlafaxine, Paroxetine, Venlafaxine) were included. Participants who were only assigned one drug without the combination of different antidepressants or non-pharmacology treatments (i.e., cognitive-behavioral therapy, psychotherapy). (3) Outcome included HAMD scores, the clinical response rate, and the incidence of drug-related adverse reactions. (4) Only RCTs were included.
Exclusion criteria
The exclusion criteria were as follows: (1) Treatment groups using combinations of other depression drugs; (2) Studies with missing data about HAMD scores, or the total clinical response rate. (3) Studies that were not RCTs.
Data extraction
Two review authors (Chun Dang and Yaoheng Lu) independently extracted the data from the included studies, resolving disagreements through consensus agreement or with third-party reviewers (Qian Li). We extracted data on patients’ characteristics (age, gender, numbers, comorbidity), interventions and control group (trial groups, duration, administration), outcomes (HAMD scores, the total clinical response rate in baseline and post-treatment), and adverse events. Due to the lengthy nature of the drug names, they have been abbreviated for enhanced readability and improved visual presentation in the figures and tables.
When discrepancies were identified, the primary reviewers discussed them to reach a consensus. If the primary reviewers cannot resolve a discrepancy, a third-party reviewer is consulted. The third-party reviewer provided an independent assessment of the disputed data points. Blinding was used during the data extraction process.
Study quality assessment
Due to the inclusion of RCTs in this study, we have used the Cochrane Collaboration’s recommended bias assessment tool, ROB 2.0, specifically designed for RCTs. ROB is widely recognized and extensively used as the predominant tool for assessing bias risk in RCTs (Higgins et al., 2011). The risk of bias was assessed in terms of the five domains: (1) Risk of bias arising from the randomization process; (2) Missing outcome data; (3) Risk of bias due to deviations from the intended interventions; (4) Risk of bias in the selection of the reported result; (4) Risk of bias in the measurement of the outcome. The risk of bias was graded as “low risk of bias”, “some concerns” and “high risk of bias”. All stages were independently performed by two authors (Chun Dang and Yaoheng Lu).
Statistical analysis
In this study, which involves the comparison of multiple different interventions and includes a significant number of indirect comparisons, we have adopted the commonly used Markov chain Monte Carlo method (MCMC). This approach utilizes a random effects generalized linear model for Bayesian network meta-analysis (Jansen et al., 2008). The nma. fit () function is adept at performing model fitting and identifying potential outliers. The lever plots and Deviance Information Criterion (DIC) values generated by this function are instrumental in determining the most suitable effect model. The lever diagram illustrates the comparison between leverage_ik (leverage for test i in arm k) and Bayesian deviation residuals for all I tests across each of the K arms. This diagram is particularly useful for highlighting potential outliers in model fitting. Specifically, if a data point falls outside the purple arc, it may indicate poor model fitting. We used odd ratios or their logarithms as the effect index of counting data and their 95% confidence intervals (CI) as limits. We use mean difference as the statistical effect size for continuous variables, and OR for binary variables, based on the type of outcome data. When the odds ratio (OR) value did not contain 1 at the 95% CI, the difference was considered statistically significant. Statistical heterogeneity was assessed using the I2 statistic (Chen and Benedetti, 2017). The I2 statistic for assessing statistical heterogeneity, serves as a method to measure the degree of variance among multiple study effects. It specifically quantifies the percentage of total variation that is attributable to differences between studies, rather than to sampling error. The categorization of heterogeneity via the I2 statistic is as follows: I2 of 0 indicates that the variation among studies is solely due to sampling error; I2 between 0.25 and 0.5 suggests moderate heterogeneity; and I2 greater than 0.5 is indicative of high heterogeneity. Some scholars argue that the I2 statistic, by applying a degrees-of-freedom adjustment, mitigates the impact of the number of included studies on the Q value, ensuring that its magnitude does not fluctuate with the number of studies and thus making the heterogeneity test results more robust and reliable (Higgins et al., 2003). The magnitude of publication bias is assessed by examining the distribution of individual study points within a funnel plot. If the points are symmetrically distributed on either side of the plot, it suggests a lower likelihood of publication bias. The convergence of the model was performed using the Gelman-Rubin method combined with a density plot and tractory plot (Brooks and AJJCGS, 1998). A network meta-analysis was performed for each collected outcome of studies. For different outcomes, we summarized the current evidence by drawing three network graphs. The effectiveness, and safety of different drugs in the treatment of depression were ranked based on the Surface Under the Cumulative Ranking (SUCRA) curve (Salanti et al., 2011). Pairwise meta-analysis will be conducted using Stata, version 17, and network meta-analysis within the Bayesian framework will be conducted by using R software, version 4.3.1 (R Foundation for Statistical Computing, Shanghai, Asia), with the package calling “gemtc 0.8–2” and “JAGS” (version 3.5.3) (Neupane et al., 2014; Shim et al., 2019). p < 0.05 was considered to indicate statistical significance.
Results
Screening results
After database retrieval, 8,923 citations were identified in five databases and 538 studies in the grey literature. Ultimately, 198 randomized control trials fulfilled the inclusion and exclusion criteria after reading the full text (Figure 1).
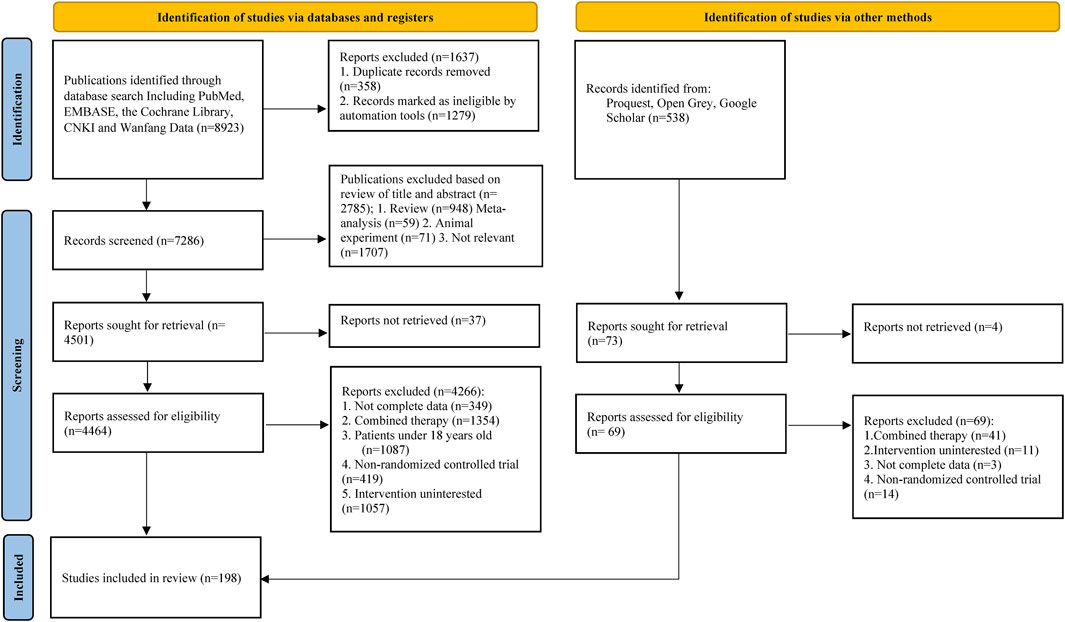
Figure 1. Supplementary Figure S1 Search results and study selection. This flow diagram adapted from PRISMA depicts the search results retrieved from databases and illustrates the process of literature screening.
Study and participant characteristics
The analysis incorporated 198 RCTs, which collectively enrolled 8,923 patients. These patients were treated with 17 Chinese herbal medicines for depression treatment. This study included six trials (646 patients) on Morinda Officinalis Oligosaccharide Capsule, two trials (92 patients) on Guipiwan, 18 trials (690 patients) on Jieyu Decoction, 35 trials (1,469 patients) on Shugan Jieyu Capsule, 15 trials (697 patients) on Wuling Capsule, five trials (187 patients) on Ease Pill, two trials (152 participants) on Yangxue Qingnao Granule, three trials (98 patients) on Yueju Pill, eight trials (326 patients) on Buyang Huanwu Decoction, 34 trials (1,601 patients) on Chaihu Jia Longgu Muli Decoction, 11 trials (391 patients) on Chai Hu Shu Gan San, 19 trials (834 patients) on Danzhi-Xiaoyao-San, 12 trials (382 patients) on Gan Mai Da Zao Decoction, 12 trials (644 patients) on Huoxue Soup Decoction, five trials (227 patients) on Wendan Anshen Decoction, seven trials (248 patients) on Xiaoyao Powder, and four trials (239 patients) on Xingnao Jieyu Decoction. The median follow-up period for these trials ranged from 4 weeks to 6 months. All studies were conducted in China. A detailed description of the participants is presented in Supplementary Table S1 (Cao and Zhong, 2008; Cao, 2009; Chang and Wang, 2010; Chen and Bai, 2011; Chen and Wang, 2012; Qu et al., 2012; Cao and Chi, 2017; An and Wang, 2019; Chen GXFN. and Li T., 2009; Chen KZC. and Li XX., 2009; Chen and He, 2009; Chen and Wang, 2009; Deng and Sun, 2012; Du and Yu, 2012; Chen and Dou, 2014; Chen and Wang, 2015; Ding, 2015; Chen and Ma, 2016; Cheng and Yang, 2016; Chen and Li, 2017; Chen and Zhang, 2018; Cheng and Li, 2020; Deng et al., 2022; Gong, 2010; He, 2011; Gao et al., 2012; Guo et al., 2012; Feng, 2013; Guan and Wu, 2014; Guo and Hu, 2014; Huang and Ting, 2014; Guo and Zhang, 2015; Guan et al., 2017; He et al., 2017; Guo et al., 2018; He and Wang, 2018; Hou and Wang, 2019; Guo and Li, 2020; Li and Zhang, 2004; Huang et al., 2007; Li and Li, 2008; Jing et al., 2009; Li et al., 2009; Li and Zhang, 2010; Li and Zhao, 2011; Li RGZT. and Li S., 2012; Li SHLY. and Li SS., 2012; Huang and Zhou, 2014; Li and Li, 2014; Jiao et al., 2015; Li and Gao, 2015; Li QLLJ. et al., 2016; Li SSYM. et al., 2016; Jin et al., 2017; Lai and Yi, 2017; Li and Guo, 2017; Jia et al., 2019; Li and Wang, 2019; Li et al., 2003; Li and Wang, 2004; Li, 2007; Li and Qian, 2007; Liu et al., 2007; Li and Tian, 2008; Li and Dong, 2009; Li et al., 2010; Liu and Tan, 2010; Lin et al., 2011; Liu and Zhang, 2012; Li and Luo, 2013; Li et al., 2014; Li and Wang, 2015; Liu and Wang, 2015; Liu and Wang, 2017; Li et al., 2018; Lin and Han, 2019; Liu and Wang, 2019; Li et al., 2020; Luo and Zhao, 2006; Meng et al., 2008; Mao and Li, 2010; Ran et al., 2010; Meng and Li, 2011; Qiu and Zhu, 2011; Qu et al., 2011; Mao and Li, 2016; Meng et al., 2016; Nie et al., 2016; Qin and Tang, 2016; Ma and Ye, 2017; Qi et al., 2017; Ren, 2017; Min CX and Li, 2018; Lu and Li, 2019; Luo et al., 2019; Lu and Xin, 2020; Luo and Wu, 2021; Lu and Sun, 2022; Shen and Zhao, 2004; Tao and Li, 2006; Shi and Zeng, 2008; Ta et al., 2008; Tang and Wang, 2009; Shao and Zhao, 2011; Wang and Wang, 2011; Sun and Li, 2012; Sun and Zhou, 2012; Tao and Yin, 2012; Ren and Li, 2015; Tan et al., 2015; Tao and Wang, 2015; Shao and li, 2016; Tu and Wang, 2016; Wang et al., 2016; Wang and Wang, 2018; Song and Li, 2019; Wang and Li, 2019; Wang and Shao, 2019; Wang and Ma, 2006; Wang and Luo, 2007; Wang and Wu, 2008; Wang and Shu, 2009; Wang and Ban, 2010; Wang et al., 2012; Wang et al., 2014; Wei and Huang, 2014; Wei and Lu, 2014; Wang and Liu, 2016; Wang and Yang, 2016; Wu and Zhu, 2016; Wang and Li, 2017; Wang and Liu, 2017; Wang and Dou, 2018; Wang and Zhang, 2018; Wang and Zhang, 2019; Wang and Guo, 2020; Wang and Wan, 2020; Wang and Jiang, 2021; Wu et al., 2002; Yan and Wang, 2003; Xiao and Huang, 2004; Xiao, 2006; Xu and Li, 2006; Xu et al., 2007; Xu and Wang, 2007; Yan and Li, 2008; Xun and Bai, 2010; Xu TWS. et al., 2011; Xu TSWQ. et al., 2011; Xie and Li, 2011; Wu et al., 2012; Xu and Li, 2012; Xu and Yang, 2014; Yan and Bo, 2014; Wu and Wan, 2015; Xu and Wang, 2015; Wu and Tian, 2018; Xu and Wu, 2019; Zhang and Tian, 2008; Yu and Zhao, 2010; Zhan and Wang, 2010; Zhang and Gu, 2010; Yang, 2012; Yu and Wang, 2012; Zhang and Tian, 2012; Ye and Xia, 2014; Yang and Rui, 2015; Zhang and Li, 2015; Zhang and Zhang, 2016; Yu and Zhang, 2017; Yin and Zhang, 2018; Yu and Tang, 2018; Zhang and Zhou, 2018; Yin et al., 2019; Zhang and Bai, 2019; Zhang and Gan, 2020; Zhang and Yan, 2020; Zhang and Ji, 2021; Zhou and Wang, 2005; Zhang and Zhang, 2009; Zhou and Geng, 2009; Zhou and Bao, 2010; Zhao and Hu, 2011; Zhao and Wang, 2011; Zhang and Tang, 2012; Zhao and Zhao, 2012; Zhou and Xiao, 2015; Zhao and Zhang, 2021; Du and Cai, 2005; Zhu and Yang, 2005; Dang and Chu, 2009; Liu and Ku, 2012; Zhu and Li, 2014; Guan and Wang, 2017; Liu et al., 2017; Deng and Li, 2019; Shao and Feng, 2019; Gou and Wu, 2023).
Risk-of-bias assessment
We comprehensively conducted a methodological quality assessment on 198 included RCTs. Based on the summary of the risk of bias, 135 studies (68.2%) were assessed as “some concerns”, 28 studies (14.1%) were rated as “low risk bias”, and 35 studies (17.7%) were classified as “high risk bias”. Overall, these factors result in an overall low-to-moderate risk of bias. The bias risk assessment results were presented in Figure 2.
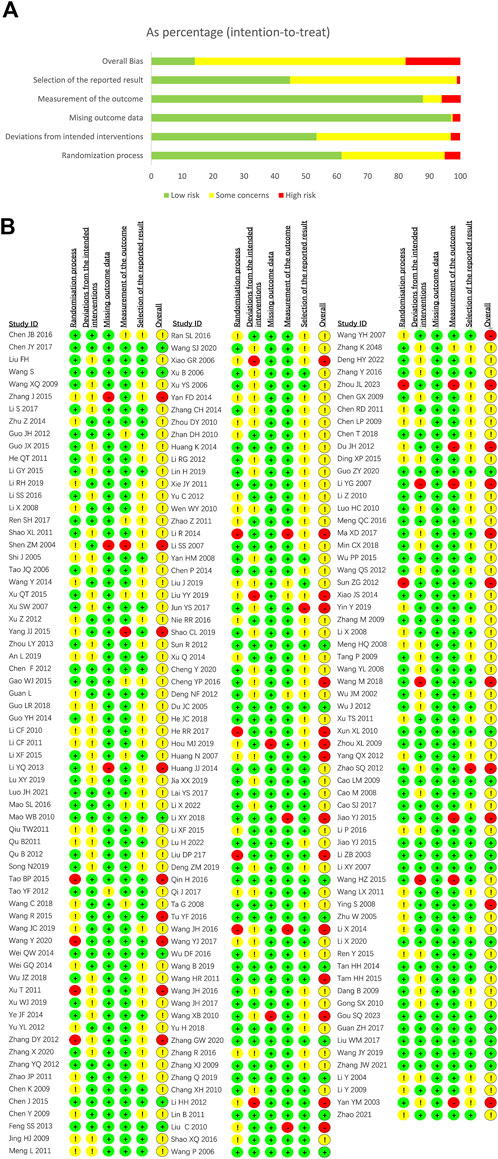
Figure 2. Risk assessment results for depression. (A) Risk of bias summary for depression; (B) Risk of bias graph for depression.
Network diagram
The network diagram provides a visual representation of all the studies included in the meta-analysis and their interconnections. It illustrates how each treatment is compared within the network of studies. The network diagram was outputted to describe the research network graphically. The node size is proportional to the total number of participants in each group. The line width is proportional to the number of clinical trials. When a closed loop is formed between nodes, these studies could be simultaneously compared. Among them, Fluoxetine, Shugan Jieyu Capsule, and Chaihu Jia Longgu Muli Decoction were more extensively studied, followed by Paroxetine, Danzhi-Xiaoyao-San, and Jieyu Decoction. The two groups most frequently compared were Shugan Jieyu Capsule and Fluoxetine, and Chaihu Jia Longgu Muli Decotion and Fluoxetine, respectively (Figure 3).
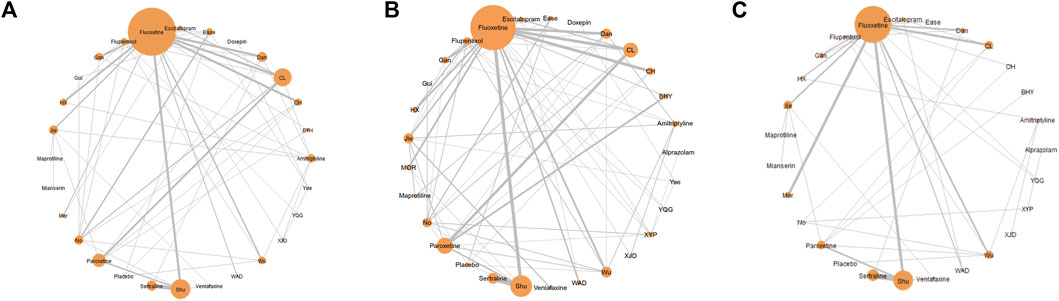
Figure 3. Network meta-analysis diagrams of eligible comparisons. (A) The response rate; (B) HAMD scores; (C) adverse effects rate. The size of nodes is proportional to the total number of participants for each group in the network. The edges represent direct comparisons of the drugs in trials. The line width is proportional to the number of trials directly compared at both ends of the nodes. Mor:Morinda Officinalis Oligosaccharide Capsule, Gui: Guipiwan, Jie: Jieyu Decoction, Shu: Shugan Jieyu Capsule, Wu: Wuling Capsule, Ease: Ease Pill, YQG: Yangxue Qingnao Granule, Yue: Yueju Pill, BYH; Buyang Huanwu Decoction, CL: Chaihu Jia Longgu Muli Decoction, CH: Chai Hu Shu Gan San, Dan: Danzhi-Xiaoyao-San, Gan: Gan Mai Da Zao Decoction, HX: Huoxue Soup Decoction, WAD: Wendan Anshen Decoction, XYP: Xiaoyao Powder, XJD: Xingnao Jieyu Decoction.
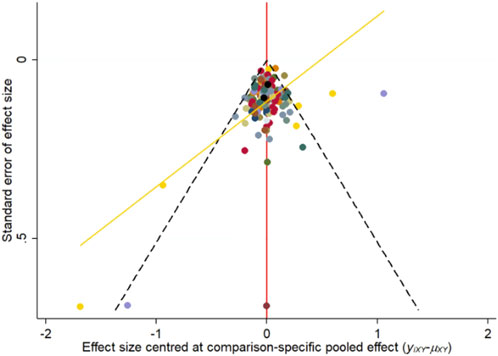
Publication bias and consistency assessment
The nma. fit () function was employed for model fitting and identification of potential outliers. The lever plots and DIC values were utilized to determine the optimal effect model (Watt and Del Giovane, 2022). Figures 4, 5 displayed the lever diagram and consistency test, respectively. Funnel plots presented a symmetrical distribution, thereby indicating limited publication bias (Figure 6).
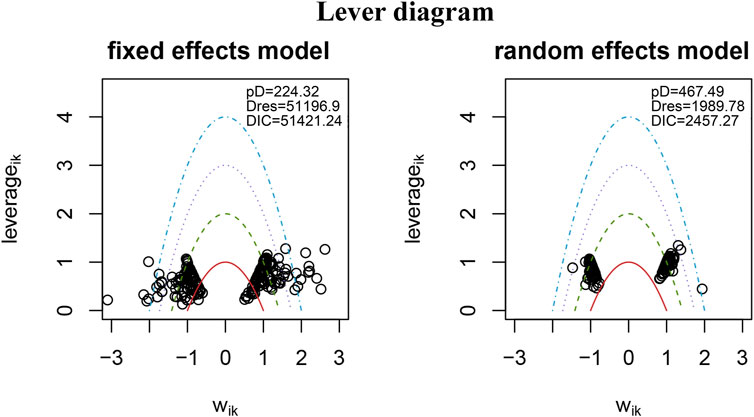
Figure 4. Lever diagram for depression. The lever diagram shows the comparison between leverageik and Bayesian deviation residuals of all I tests and each of the K arms.
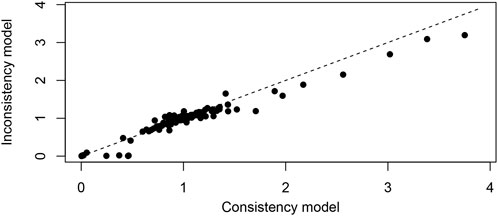
Figure 5. Conformance test for depression. The conformance test compares the posterior mean deviation of each data group between consistency and the ume m (b) Bias risk evaluation results displayed by including studies to judge the consistency among the included research results.
Trajectory plots (Supplementary Figure S1A) and density plots (Supplementary Figure S1B) were used to assess the degree of convergence. The trajectory plots showed that the MCMC chain stably fluctuates and present good overlap. The density plots indicated excellent model convergence. When the curve tends to 1 and remains stable, it indicates good convergence on the Brooks-Gelman-Rubin diagnostic diagram (Supplementary Figure S2).
Forest map
Forest map focus on these comparisons allows for a direct assessment of how alternative treatments like Chinese herbal medicines stack up against commonly used synthetic antidepressants in terms of both efficacy and safety. Forest maps compare the results of drugs, placebo, or no-treatment in various studies. The treatment efficacy of some Chinese herbal medicines was demonstrated to be generally superior to that of traditional antidepressants. Compared with those in Fluoxetine, Buyang Huanwu Decoction, Chai Hu Shu Gan San, Chaihu Jia Longgu Muli Decotion, Danzhi-Xiaoyao-San, Gan Mai Da Zao Decoction, Huoxue Soup Decoction, and Ease Pill groups exhibited higher response rates. In addition, interventions of Buyang Huanwu Decoction showed a higher response rate compared to Paroxetine groups. Moreover, Amitriptyline and Escitalopram were inferior to Chaihu Jia Longgu Muli Decoction. Additionally, Sertraline had a lower response rate compared to Danzhi-Xiaoyao-San group. Moreover, Yueju Pill and Flupentixol and Melitracen, Venlafaxine, with lower response rates, were comparable to the Ease Pill groups. Jieyu Decoction was demonstrated to significantly improve depressive symptoms compared to Venlafaxine (Figure 7A).
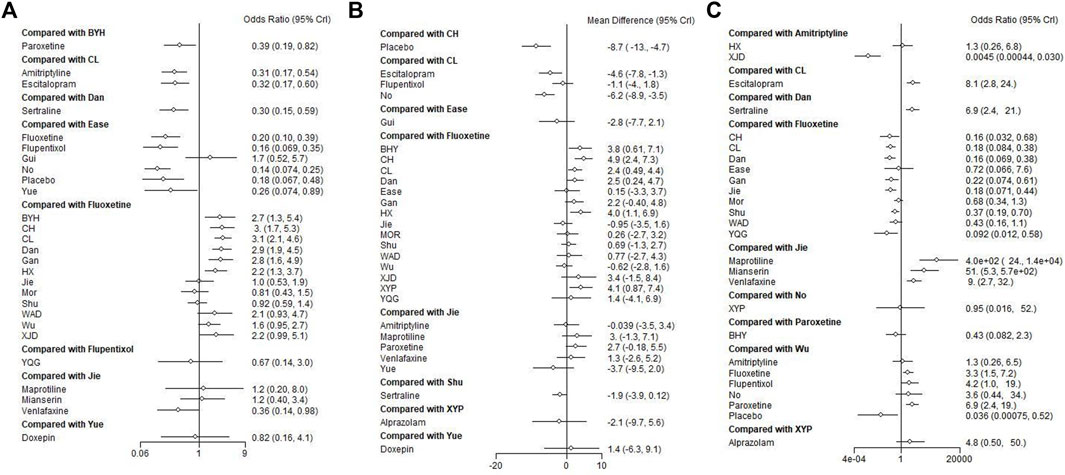
Figure 7. Forest plot of the network meta-analysis of all trials for efficacy and adverse effects in patients with depression. (A) Direct comparison of the response rate; (B) direct comparison of HAMD scores; (C) direct comparison of the adverse effects rate. Mor:Morinda Officinalis Oligosaccharide Capsule, Gui: Guipiwan, Jie: Jieyu Decoction, Shu: Shugan Jieyu Capsule, Wu: Wuling Capsule, Ease: Ease Pill, YQG: Yangxue Qingnao Granule, Yue: Yueju Pill, BYH: Buyang Huanwu Decoction, CL: Chaihu Jia Longgu Muli Decoction, CH: Chai Hu Shu Gan San, Dan: Danzhi-Xiaoyao-San, Gan: Gan Mai Da Zao Decoction, HX: Huoxue Soup Decoction, WAD: Wendan Anshen Decoction, XYP: Xiaoyao Powder, XJD: Xingnao Jieyu Decoction.
Compared to Fluoxetine, patients receiving Chinese herbal medicines, including Buyang Huanwu Decoction, Chai Hu Shu Gan San, Chaihu Jia Longgu Muli Decoction, Danzhi-Xiaoyao-San, Huoxue Soup Decoction, and Xiaoyao Powder, exhibited better efficacy in terms of HAMD scores. In particular, Chaihu Jia Longgu Muli Decoction presented a more promising antidepressant effect than Escitalopram on HAMD scores (Figure 7B).
In terms of adverse events, Xingnao Jieyu Decoction had a significantly lower safety risk than Amitriptyline. Compared with Fluoxetine, Chai Hu Shu Gan San, Chaihu Jia Longgu Muli Decoction, Danzhi-Xiaoyao-San, Gan Mai Da Zao Decoction, Jieyu Decoction, Shugan Jieyu Capsule, and Yangxue Qingnao Granule exhibited lower safety risks of adverse outcomes. Furthermore, compared with Maprotiline, Jieyu Decotion had lower safety risk. Jieyu Decoction had lower safety risk than Maprotiline, Mianserin, and Venlafaxine. Wuling Capsule had lower safety risk than Fluoxetine, Flupentixol and Melitracen, Paroxetine (Figure 7C).
The heatmap of the ranking table
The results are presented in a heatmap format, with colors representing the magnitude of effect or ranking probability. The rows of the heatmap typically represent different treatments, while columns represent different outcome measures. Each cell in the heatmap corresponds to the intersection of the categories on the x and y-axes. The colors in a heatmap are often used to represent a gradient in continuous data. Deep red may indicate higher values, * represents statistically significant data (p < 0.05). For instance, in the diagram where the horizontal axis represents Chai Hu Shu Gan San and the vertical axis represents Paroxetine (**3.11***), there is a statistically significant improvement in the HAMD score for Chai Hu Shu Gan San compared to Paroxetine (p < 0.05).
The heatmap of each outcome index ranking table included the 95% CI and OR of each outcome index across all groups. Interventions involving Buyang Huanwu Decoction, Chai Hu Shu Gan San, Chaihu Jia Longgu Muli Decoction, Danzhi-Xiaoyao-San, and Ease Pill presented more encouraging point estimates than Escitalopram, Fluoxetine, Flupentixol and Melitracen, Jieyu Decoction, Morinda Officinalis Oligosaccharide Capsule, Paroxetine, Sertraline, Venlafaxine, and Shugan Jieyu Capsule. Moreover, Gan Mai Da Zao Decoction and Guipiwan were statistically superior in evaluations compared to Jieyu Decoction, Morinda Officinalis Oligosaccharide Capsule, Paroxetine, Sertraline, Venlafaxine, and Shugan Jieyu Capsule (Figure 8A).
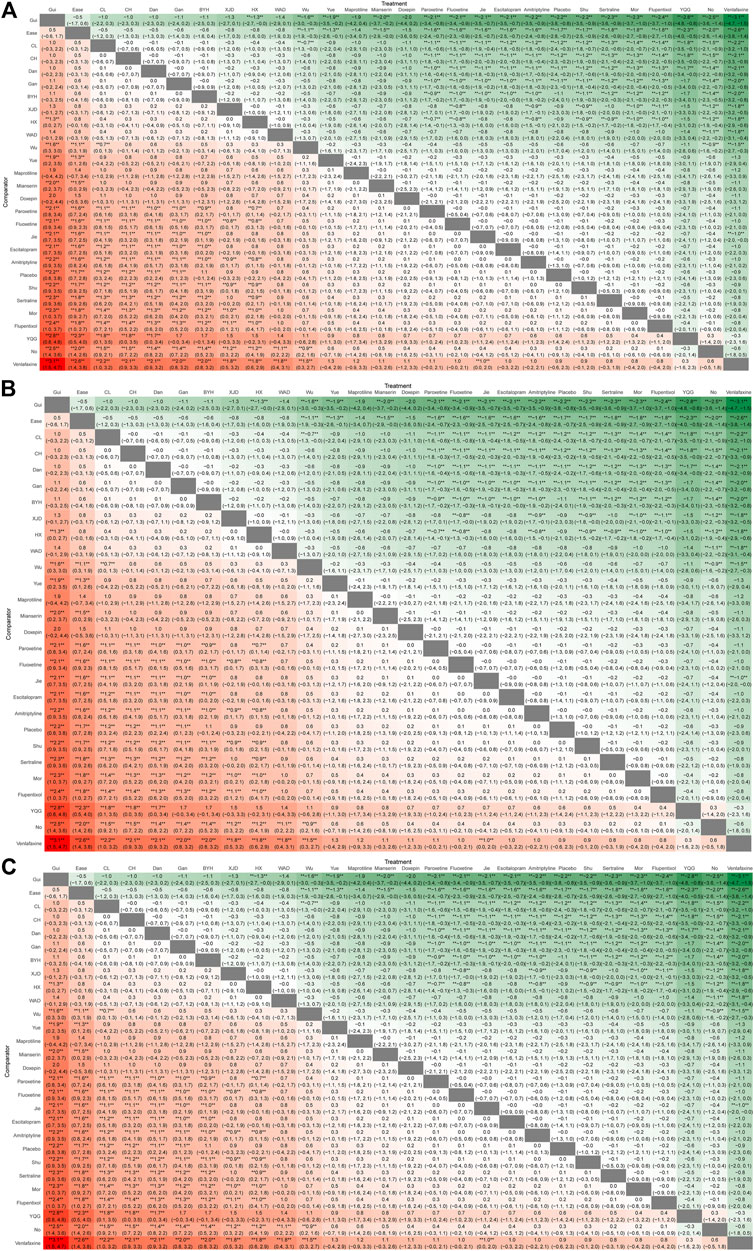
Figure 8. Ranking chart heatmap for depression. The heatmap of each outcome index ranking table shows comparisons of the relative effects between any pair of interventions, including the OR and 95% CI of each outcome index in all groups. (A) The response rate ranking chart heatmap; (B) HAMD scores ranking chart heatmap; (C) adverse effects rate ranking chart heatmap. Mor:Morinda Officinalis Oligosaccharide Capsule, Gui: Guipiwan, Jie: Jieyu Decoction, Shu: Shugan Jieyu Capsule, Wu: Wuling Capsule, Ease: Ease Pill, YQG: Yangxue Qingnao Granule, Yue: Yueju Pill, BYH: Buyang Huanwu Decoction, CL: Chaihu Jia Longgu Muli Decoction, CH: Chai Hu Shu Gan San, Dan: Danzhi-Xiaoyao-San, Gan: Gan Mai Da Zao Decoction, HX: Huoxue Soup Decoction, WAD: Wendan Anshen Decoction, XYP: Xiaoyao Powder, XJD: Xingnao Jieyu Decoction.
Chai Hu Shu Gan San, Huoxue Soup Decoction displayed significant effectiveness as active drugs with statistical certainty compared with Shugan Jieyu Capsule, Morinda Officinalis Oligosaccharide Capsule, Fluoxetine, Wuling Capsule, Jieyu Decoction, Amitriptyline, Sertraline, Escitalopram, Guipiwan, and Yueju Pill in terms of HAMD scores. Buyang Huanwu Decoction and Xingnao Jieyu Decoction exhibited greater efficacy than Fluoxetine, Wuling Capsule, Jieyu Decoction, Amitriptyline, Sertraline, Escitalopram, Guipiwan, and Yueju Pill in terms of HAMD scores. The efficacy of Danzhi-Xiaoyao-San and Chaihu Jia Longgu Muli Decoction was significantly greater than that of Fluoxetine, Wuling Capsule, Sertraline, Escitalopram, and Yueju Pill when assessed by HAMD scores (Figure 8B).
Regarding safety outcomes, treatments with a lower risk of depression-related adverse effects were Xingnao Jieyu Decoction and Chai Hu Shu Gan San (Figure 8C).
SUCRA rankings
After preparing the data with the data. prep () function, we utilized the net. plot () function to graphically depict the research network. The net. plot () function is capable of generating a network diagram for the outcome indicators as needed. SUCRA is a numerical representation method, often presents as a percentage, which is used to summarize the comprehensive ranking of each treatment across multiple outcome indicators. This value is derived from the cumulative ranking probabilities of each treatment, that is consistent with the area under the curve. The SUCRA value is higher, the ranking of the treatment in terms of effectiveness, or safety are higher. The ranking table provides a straightforward way to compare the performance of different interventions or treatments, offers quantitative insights that are more digestible than raw statistical data. The ranking table allows for a direct comparison of the effectiveness and safety of these treatments, making it easier to understand which treatments stand out.
Treatments were ranked for the response rate, HAMD score based on SUCRA values, as illustrated in Table 1. The ranking probability histogram and cumulative probability ranking chart intuitively displayed the sorting probability of each group in Figure 8, consistent with the SUCRA rankings (Table 1).
The results of SUCRA showed that Guipiwan may be the most efficacious Chinese herbal medicine to alleviate depressive symptoms but had only a small sample size. Meanwhile, the Guipiwan curve was higher than that of other treatments. Significantly, the total response rate of most Chinese herbal medicines was approximately superior to that of traditional antidepressants in this study. Chai Hu Shu Gan San was ranked best for the decrease in HAMD scores. Xingnao Jieyu Decoction was ranked second for reduction in HAMD scores. Moreover, Xiaoyao Powder was ranked best for safety in all treatments. Maprotiline was ranked worst for adverse effects rate with poor safety. Importantly, the safety of most Chinese herbal medicines was superior to that of traditional antidepressants in this study (Figure 9).
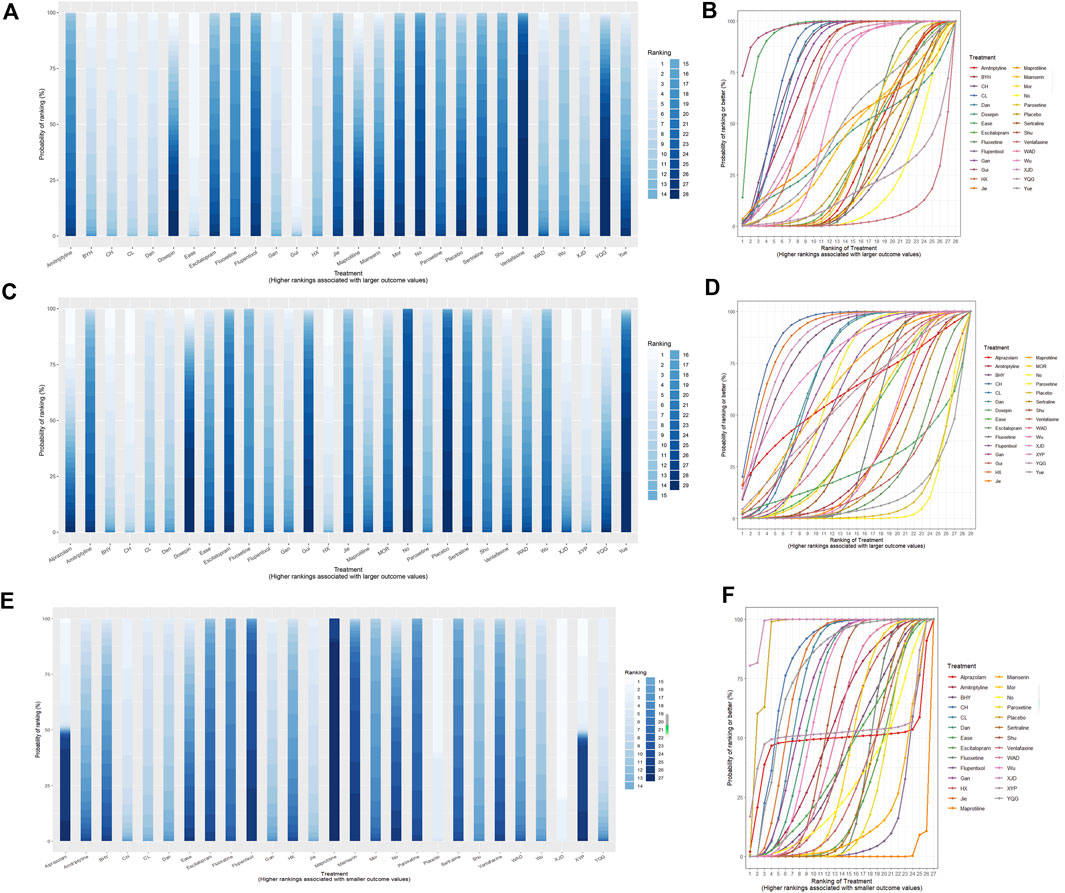
Figure 9. Ranking probability histogram and cumulative probability ranking chart for depression. The histogram and SUCRA charts intuitively display the sorting probability of each group in the form of histograms and curves. (A) Rankogram chart of response rate; (B) SUCRA chart of the response rate; (C) rankogram chart of HAMD scores; (D) SUCRA chart of HAMD scores; (E) rankogram chart of adverse effects rate; (F) SUCRA chart of adverse effects rate. Mor:Morinda Officinalis Oligosaccharide Capsule, Gui: Guipiwan, Jie: Jieyu Decoction, Shu: Shugan Jieyu Capsule, Wu: Wuling Capsule, Ease: Ease Pill, YQG: Yangxue Qingnao Granule, Yue: Yueju Pill, BYH: Buyang Huanwu Decoction, CL: Chaihu Jia Longgu Muli Decoction, CH: Chai Hu Shu Gan San, Dan: Danzhi-Xiaoyao-San, Gan: Gan Mai Da Zao Decoction, HX: Huoxue Soup Decoction, WAD: Wendan Anshen Decoction, XYP: Xiaoyao Powder, XJD: Xingnao Jieyu Decoction.
Summary
This study found that specific Chinese herbal medicines, including Guipiwan, Ease Pill, Chaihu Jia Longgu Muli decotion, Chai Hu Shu Gan San, Danzhi-Xiaoyao-San, Gan Mai Da Zao Decoction, Buyang Huanwu Decoction and Xingnao Jieyu Decoction, were not only more effective than commonly used synthetic drugs (such as Fluoxetine, Escitalopram, Amitriptyline, Sertraline, Flupentixol, and Venlafaxine) but also associated with a substantially lower risk of adverse events. The findings suggest that Chinese herbal medicines could be considered as viable alternatives to synthetic antidepressants for the treatment of depression, particularly for patients who might be looking for natural remedies or those who are intolerant to the side effects of synthetic drugs. These results could inform clinical practice by expanding the range of treatment options available for depression, potentially leading to more personalized and effective treatment strategies.
Discussion
In summary, this is the first study to systematically evaluate the safety and efficacy of 17 different Chinese herbal medicines attenuating depressive symptoms in depression patients. A Bayesian network meta-analysis was performed to explore the efficacy of single Chinese herbal medicines. The RoB2 was used to assess the methodological quality.
Principal findings
In network diagram, Fluoxetine, Shugan Jieyu Capsule, and Chaihu Jia Longgu Muli Decoction were more extensively studied, followed by Paroxetine, Danzhi-Xiaoyao-San, and Jieyu Decoction. In heatmap, the interventions of Buyang Huanwu Decoction, Chai Hu Shu Gan San, Chaihu Jia Longgu Muli Decoction, Danzhi-Xiaoyao-San, and Ease Pill, Gan Mai Da Zao Decoction and Guipiwan presented more encouraging point estimates. Through direct comparison of forest map, the treatment efficacy of some Chinese herbal medicines was shown to be broadly greater than that of traditional antidepressants. According to SUCRA ranking, Guipiwan (SUCRA value: 96.93%) had the highest efficacy, closely followed by Ease Pill (SUCRA value: 93.76%), Chaihu Jia Longgu Muli Decoction (SUCRA value: 83.37%), Chai Hu Shu Gan San (SUCRA value: 81.44%), and Danzhi-Xiaoyao-San (SUCRA value: 80.61%). Notably, Xiaoyao Powder exhibited the lowest incidence of adverse events (SUCRA value: 98.23%). Moreover, commonly used synthetic drugs such as Amitriptyline (SUCRA value: 51.57%), Fluoxetine (SUCRA value: 28.48%), Venlafaxine (SUCRA value: 28.12%), Escitalopram (SUCRA value: 23.39%), Sertraline (SUCRA value: 26.98%), Flupentixol (SUCRA value: 8.51%) and Maprotiline (SUCRA value: 0.03%), appeared to be less effective and carried higher risks of adverse events compared to most Chinese herbal medicines. Moreover, commonly used synthetic drugs such as Fluoxetine, Escitalopram, Amitriptyline, Sertraline, Flupentixol and Melitracen, and Venlafaxine, appeared to be less effective and carried higher risks of adverse events compared to most Chinese herbal medicines.
The mechanism of Chinese herbal medicines on depression
After thousands of years of exploration, Chinese herbal medicine has been shown advantages in the treatment of depression, such as multiple components, multitarget and strong safety, which plays a critical role in treating depression (Yeung et al., 2014b; Wang et al., 2017). The mechanisms of Chinese herbal medicines on treatment of depression are still largely unknown. The underlying pathophysiology of depression is associated with the damage of monoamine transmission systems (LeMoult and Gotlib, 2019). In fact, clinical studies have found that Chaihu Jia Longgu Muli Decoction, Gan Mai Da Zao Decoction, Xiao Yao San has a good antidepressant effect by preventing dopaminergic transmission in rats (Ding et al., 2021; Wan et al., 2021; Wang YT. et al., 2023). This core active ingredients of Chaihu Jia Longgu Muli Decoction consists of Chaihu (Bupleurum), Muli (Ostrea gigas), which are pivotal in treating depression (Wang Y. et al., 2023). The key active compounds in the Gan Mai Da Zao Decoction were identified as Quercetin, Luteolin, Kaempferol, Naringenin, and Isorhamnetin, contributing significantly to its antidepressant effect (Ding et al., 2021). Quercetin, Apigeni and Luteolin, key components of the Xiao Yao San, effectively mitigate the progression of depression (Chen, 2023).
Inflammation and mitochondrial dysfunction are also associated with the pathogenesis of depression (Bansal and Kuhad, 2016; Kohler et al., 2016). In addition, Morinda Officinalis Oligosaccharide Capsule mitigate depression by regulating Mitofusin two protein-mediated mitophagy in rats (Yang et al., 2023). Morinda Officinalis Oligosaccharide Capsule mainly contains inulin-type oligosaccharides extracted from the roots of M. officinalis, which is effective in ameliorating symptoms of depressive disorder (Zhang et al., 2018). Furthermore, Wuling Capsule mitigate depression by regulating translocator protein-mediated mitophagy, exhibit antioxidant and anti-inflammatory effects in rats (Zheng et al., 2016). Wuling Capsule is mainly formulated with Wulingshen powder, which is a kind of fungal sclerotia of a ginseng. Wulingshen contains flavonoids, triterpenoids, saponins and polysaccharides, which are beneficial in improving depression (Feng et al., 2016). Chai Hu Shu Gan San is composed of Chaihu (Bupleuri radix), Xiangfu (Cyperus rhizome), and Chuanxiong (Ligusticum chuanxiong rhizome), which have anti-inflammatory actions and neuroprotective effects (Sun et al., 2018).
Expectation and actual findings
The expectation of this study was Chinese herbal medicines exhibit better efficacy, and fewer side effects compared with synthetic antidepressants for the treatment of depression. It was expected to provide insights into the potential of Traditional Chinese Medicines as promising alternatives to conventional antidepressants.
The actual findings from this study are significant as they suggest that Chinese herbal medicines might be viable alternative therapies for depression, potentially offering benefits in terms of effectiveness and safety. In terms of clinical practice, these findings can inform healthcare professionals about alternative treatment options, especially for patients who may seek or prefer herbal remedies or for whom traditional antidepressants are not suitable. However, the generalizability of these results may be influenced by the study’s methodology and the specific patient populations included in the analyzed trials. Further research is needed to explore these findings in varied clinical settings and among diverse patient populations to fully ascertain the generalizability and practical application of the study’s conclusions.
Potential confounding factors or biases
The variation in risk of bias across different studies may impact outcomes, potentially affecting the reliability of comparisons between Chinese herbal medicines and synthetic drugs. Chinese herbal medicines and synthetic drugs often differ in their mechanisms of action, side effects, and patient adherence rates. These differences could introduce confounding factors in comparative analyses. The acceptance and use of Chinese herbal medicines might be influenced by cultural beliefs and practices, which could affect patient outcomes. Geographic locations of these studies could also introduce biases, as herbal medicine practices may vary significantly across regions. Specific characteristics of patient populations in the studies, such as severity of depression, age, gender, and comorbidities, can influence the effectiveness and safety of the treatments.
Strengths and limitations
We performed a comprehensive literature search focused on depression, addressed crucial outcomes, and rigorously assessed risk of bias at the level of evidence. The acceptability of various interventions was assessed based on criteria such as response rate, HAMD scores, and rate of adverse events on versus direct and indirect comparisons, thereby enhancing the persuasiveness of the evidence.
Traditional Chinese medicines are emerging as promising new drug candidates for depression treatment (Huhn, et al., 2020). This study aims to aims to determine the effectiveness, acceptability, and safety of Chinese herbal medicines in comparison with synthetic antidepressants. In addition, this study provides reference information suggesting that Chinese herbal medicines could serve as viable alternative therapies as natural remedies.
However, there are some limitations in this study. HAMD scores were used as the efficacy outcomes. Nevertheless, the data from other depression scales, such as Self-rating Depression Scale scores and Hamilton Anxiety Scale scores, were excluded due to a lack of sufficient clinical trials. These findings may lead to more complete conclusions about Chinese herbal medicines on depression. Remarkably, this study did not compare the multiple Chinese herbal medicine treatments according to the severity of depression. This review included numerous studies with small sample sizes, which limited the certainty of current evidence for the clinical use of Chinese medicines (Bian et al., 2020). Therefore, larger, more rigorous trials are necessary in the future.
Conclusion
The study is the first to systematically assess the efficacy and safety of traditional Chinese medicines for treating depression patients using Bayesian network meta-analysis. We conclude that Guipiwan, Ease Pill, Chaihu Jia Longgu Muli Decoction, Chai Hu Shu Gan San, Danzhi-Xiaoyao-San, Buyang Huanwu Decoction, Xiaoyao Powder, Huoxue Soup Decoction, Wendan Anshen Decoction, Wuling Capsule, and Yueju Pill have great promise for treating depression. Further research is necessary in larger sample sizes, diverse patient populations, long-term efficacy and safety investigations comparing multiple Chinese herbal medicine treatments based on depression severity.
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Author contributions
CD: Writing–original draft, Investigation. QW: Data curation, Software, Writing–original draft, Methodology. QL: Funding acquisition, Writing–review and editing, Investigation. YX: Writing–review and editing, Methodology. YL: Data curation, Investigation, Writing–original draft.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. National Natural Science Foundation of China (82001240), Natural Science Foundation of Heilongjiang Province (YQ 2021H011), China Postdoctoral Science Foundation (2020M670925, 2022T150172), and Postdoctoral Foundation of Heilongjiang Province (LBH-Z19027, LBH-TZ2019).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2024.1295564/full#supplementary-material
References
An, L. W. Z., and Wang, L. H. (2019). Clinical observation on shugan jieyu capsule on depression after cerebral infarction. Guangming J. Chin. Med. 34 (15), 2289–2291. doi:10.3969/j.issn.1003-8914.2019.15.006
Bansal, Y., and Kuhad, A. (2016). Mitochondrial dysfunction in depression. Curr. Neuropharmacol. 14 (6), 610–618. eng. Epub 2016/03/01. Cited in: Pubmed; PMID 26923778. doi:10.2174/1570159x14666160229114755
Bian, T., Corral, P., Wang, Y., Botello, J., Kingston, R., Daniels, T., et al. (2020). Kava as a clinical nutrient: promises and challenges. Nutrients 12 (10), 3044. eng. Epub 2020/10/09. Cited in: Pubmed; PMID 33027883. doi:10.3390/nu12103044
Bosc, M. (2000). Assessment of social functioning in depression. Compr. psychiatry 41 (1), 63–69. eng. Epub 2000/01/26, Cited in: Pubmed; PMID 10646621. doi:10.1016/s0010-440x(00)90133-0
Brooks, S., and Ajjcgs, G. (1998). General methods for monitoring convergence of iterative simulations. General methods Monit. convergence iterative simulations 7, 434–455. doi:10.1080/10618600.1998.10474787
Cao, L. M. HZLT (2009). Treatment of 45 cases of depression after cerebral infarction by Huoxue Huatan Jieyu decoction. Jiangxi J. Traditional Chin. Med. (4), 20–21. doi:10.3969/j.issn.0411-9584.2009.04.010
Cao, M. Q. H., and Zhong, Z. L. (2008). Clinical study on jieyuhuoxue decoction in treating 70 cases of depression after stroke. Zhejiang J. Traditional Chin. Med. 43 (10), 562–563. doi:10.3969/j.issn.0411-8421.2008.10.002
Cao, S. J. H. G., and Chi, Z. (2017). Clinical effect of yiqi Huoxue jieyu decoction in treatment of post-stroke depression. J. Anhui Univ. Chin. Med. 36 (3), 12–15. doi:10.3969/j.issn.2095-7246.2017.03.005
Carrozzino, D., Patierno, C., Fava, G. A., and Guidi, J. (2020). The Hamilton rating scales for depression: a critical review of clinimetric properties of different versions. Psychotherapy psychosomatics 89 (3), 133–150. eng. Epub 2020/04/15. Cited in: Pubmed; PMID 32289809. doi:10.1159/000506879
Chang, X. H. Z. L., and Wang, S. (2010). Treating 50 cases of post-stroke depression with Bupleurum Shugan powder. Liaoning J. Traditional Chin. Med. 37 (10), 1973–1974. CNKI:SUN:LNZY.0.2010-10-056.
Chen, B., and Benedetti, A. (2017). Quantifying heterogeneity in individual participant data meta-analysis with binary outcomes. Syst. Rev. 6 (1), 243. eng. Epub 2017/12/07. Cited in: Pubmed; PMID 29208048. doi:10.1186/s13643-017-0630-4
Chen, F. Z. W., and Wang, P. (2012). Clinical efficacy and security of shugan jieyu capsules in treatment of mild and moderate depression. Med. Pharm. J. Chin. People's Liberation Army 24 (12), 7–9. doi:10.3969/j.issn.2095-140X.2012.12.00
Chen, G. (2023). Molecular basis of breast cancer with comorbid depression and the mechanistic insights of Xiaoyaosan in treating breast cancer-associated depression. Medicine 102 (38), e35157. eng. Epub 2023/09/25. Cited in: Pubmed; PMID 37747031. doi:10.1097/md.0000000000035157
Chen, G. X. F. N., and Li, T. (2009a). Danzhi Xiaoyao Powder added flavor treatment of 45 cases of post-stroke depression. Guangming J. Chin. Med. 24 (10), 1901–1902. doi:10.3969/j.issn.1003-8914.2009.10.038
Chen, J. B. X. F., and Ma, X. (2016). Therapeutic effect of Morinda oligosaccharide capsule on mild and moderate depression. Shaanxi J. Traditional Chin. Med. (8), 1029–1031. doi:10.3969/j.issn.1000-7369.2016.08.043
Chen, J. C. S., and Wang, M. (2015). Efficacy and safety of Wuling capsule on patients with post-stroke depression. Chin. J. Biochem. Pharm. 35 (10), 29–31. CNKI:SUN:SHYW.0.2015-10-008.
Chen, J. Y. Z. T., and Li, Y. (2017). A control study on the efficacy and safety of Morinda officinalis oligose capsules ersus Escitalopram in patients with depression. J. Clin. Res. 34 (9), 1717–1719. doi:10.3969/j.issn.1671-7171.2017.09.016
Chen, K. Z. C., and Li, X. X. (2009b). Clinical observation of Wuling capsule in treating mild and moderate depression. Guide China Med. 7 (14), 51–52. doi:10.3969/j.issn.1671-8194.2009.14.026
Chen, L. P. W. Z., and Wang, F. W. (2009). The clinical study of suyusan in treatment of depression. J. Emerg. Traditional Chin. Med. 18 (10), 1583–1584. doi:10.3969/j.issn.1004-745X.2009.10.009
Chen, P. L. P., and Dou, H. Y. (2014). Observation on the curative effect of Buyang Huanwu Decoction in the treatment of depression after ischemic stroke. Guide China Med. 12 (21), 258–259. CNKI:SUN:YYXK.0.2014-21-192.
Chen, R. D. A. L., and Bai, L. (2011). Observation of Danzhi Xiaoyao powder in the treatment of 28 cases of post-stroke depression journal of practical traditional. Chin. Med. 27 (9), 591–592. doi:10.3969/j.issn.1004-2814.2011.09.006
Chen, T. C. F., and Zhang, X. (2018). Clinical observation on 40 cases of qi depression and fire depression treated by Ease powder of moutan bark and cape jasmine fruit. China Contin. Med. Educ. 10 (33), 149–151. doi:10.3969/j.issn.1674-9308.2018.33.064
Chen, Y. G. L., and He, W. Y. (2009). Effect of Wuling capsule on post-stroke depression. Chin. Tradit. Pat. Med. 31 (4), 503–504. doi:10.3969/j.issn.1001-1528.2009.04.005
Cheng, Y. P. W. Z., and Yang, T. T. (2016). Effect of Chaihu plus Keel Oyster decoction on depression and neurological impairment in patients with post-stroke depression. Electron. J. Clin. Med. Literature 3 (24), 4871–4872.
Cheng, Y. W. Z., and Li, A. A. (2020). Clinical observation on Chaihu Longgu Muli decoction in treating post-stroke depression patients. Guangming J. Chin. Med. 35 (9), 1351–1352. doi:10.3969/j.issn.1003-8914.2020.09.028
Dang, B. Z. X., and Chu, D. F. (2009). The effect of Prosperity powder on the psychological status of patients with depression. Psychol. Mag. 16 (4), 75–76.
Dean, R. L., Hurducas, C., Hawton, K., Spyridi, S., Cowen, P. J., Hollingsworth, S., et al. (2021). Ketamine and other glutamate receptor modulators for depression in adults with unipolar major depressive disorder. Cochrane database Syst. Rev. 9 (9), Cd011612. eng. Epub 2021/09/13. Cited in: Pubmed; PMID 34510411. doi:10.1002/14651858.CD011612.pub3
De Crescenzo, F., D'Alò, G. L., Ostinelli, E. G., Ciabattini, M., Di Franco, V., Watanabe, N., et al. (2022). Comparative effects of pharmacological interventions for the acute and long-term management of insomnia disorder in adults: a systematic review and network meta-analysis. Lancet 400 (10347), 170–184. eng. Epub 2022/07/18. Cited in: Pubmed; PMID 35843245. doi:10.1016/s0140-6736(22)00878-9
Deng, H. Y. S. Y., Tang, L., and Cai, C. (2022). Clinical study of Bupleurum Shugan Powder in treating tumor-related depression syndrome of liver-stagnation and spleen-deficiency. Int. J. traditional Chin. Med. 44 (2), 4. doi:10.3760/cma.j.cn115398-20210114-00138
Deng, N. F. Y. T., and Sun, Q. (2012). Chaihujialonggumuli decoction treating depression patients of cancer after chemotherapy and clinical observation. Guangming J. Chin. Med. 27 (1), 76–78. doi:10.3969/j.issn.1003-8914.2012.01.044
Deng, Z. M. D. Q., and Li, C. (2019). Clinical observation on the treatment of clinical depression by adding and Chaihu Jia Longgu Muli decoction. J. Emerg. Traditional Chin. Med. 24 (5), 894–896.
Ding, X. P. Z. X. (2015). Observation of clinical efficacy and adverse reactions of Danzhi Xiaoyao Powder in the treatment of depression. Med. Inf. 1 (38), 397. doi:10.3969/j.issn.1006-1959.2015.38.606
Ding, Z., Xu, F., Sun, Q., Li, B., Liang, N., Chen, J., et al. (2021). Exploring the mechanism of action of herbal medicine (Gan-Mai-Da-Zao decoction) for poststroke depression based on network pharmacology and molecular docking. Evidence-based complementary Altern. Med. eCAM. 2021, 2126967. eng. Epub 2021/09/03. Cited in: Pubmed; PMID 34471414. doi:10.1155/2021/2126967
Dobrek, L., and Głowacka, K. (2023). Depression and its phytopharmacotherapy-A narrative review. Int. J. Mol. Sci. 24 (5), 4772. eng. Epub 2023/03/12. Cited in: Pubmed; PMID 36902200. doi:10.3390/ijms24054772
Du, J. C. H. X., and Cai, L. (2005). Study of Chaihu Jia Longgu Muli decoction on myocardial infarction combined with depression. Chin. J. Traditional Med. Sci. Technol. 26 (1), 4–5.
Du, J. H. Y. W., and Yu, F. Y. (2012). On effectiveness of shengmai drink on top of Danzhi Xiaoyao powder on post diabetes depression in forty-four patients. World Chin. Med. 7 (1), 14–15. doi:10.3969/j.issn.1673-7202.2012.01.008
Faquih, A. E., Memon, R. I., Hafeez, H., Zeshan, M., and Naveed, S. (2019). A review of novel antidepressants: a guide for clinicians. Cureus 11 (3), e4185. eng. Epub 2019/05/21. Cited in: Pubmed; PMID 31106085. doi:10.7759/cureus.4185
Feng, D. D., Tang, T., Lin, X. P., Yang, Z. Y., Yang, S., Xia, Z. A., et al. (2016). Nine traditional Chinese herbal formulas for the treatment of depression: an ethnopharmacology, phytochemistry, and pharmacology review. Neuropsychiatric Dis. Treat. 12, 2387–2402. eng. Epub 2016/10/06. Cited in: Pubmed; PMID 27703356. doi:10.2147/ndt.S114560
Feng, S. S. Y. C. (2013). Wuling Capsule treating 35 cases of mild to moderate depression after cerebral infarction. China Pharm. 22 (20), 105. doi:10.3969/j.issn.1006-4931.2013.20.058
Fournier, J. C., DeRubeis, R. J., Hollon, S. D., Dimidjian, S., Amsterdam, J. D., Shelton, R. C., et al. (2010). Antidepressant drug effects and depression severity: a patient-level meta-analysis. Jama 303 (1), 47–53. eng. Epub 2010/01/07. Cited in: Pubmed; PMID 20051569. doi:10.1001/jama.2009.1943
Freitas, P. H. B., Meireles, A. L., Ribeiro, I., Abreu, M. N. S., Paula, W., and Cardoso, C. S. (2023). Symptoms of depression, anxiety and stress in health students and impact on quality of life. Rev. latino-americana Enferm. 31, e3884. Síntomas de depresión, ansiedad y estrés en estudiantes del área de la salud e impacto en la calidad de vida. spa eng por. Epub 2023/04/19. Cited in: Pubmed; PMID 37075384. doi:10.1590/1518-8345.6315.3884
Gao, W. J. H. Y., Wang, Z. Z., and Wang, H. (2012). A control study of Shuganjieyu capsules in treatment of depression of hepatic stagnation and spleen deficiency type. Med. J. Chin. People's Health 24 (5), 605–606. doi:10.3969/j.issn.1672-0369.2012.05.041
Garg, P., Alambayan, J., and Garg, V. (2023). Herbal approaches in the management of mental depression. CNS neurological Disord. drug targets 22 (1), 98–124. eng. Epub 2022/01/29. Cited in: Pubmed; PMID 35088681. doi:10.2174/1871527321666220128091408
Goethe, J. W., Woolley, S. B., Cardoni, A. A., Woznicki, B. A., and Piez, D. A. (2007). Selective serotonin reuptake inhibitor discontinuation: side effects and other factors that influence medication adherence. J. Clin. Psychopharmacol. 27 (5), 451–458. eng. Epub 2007/09/18, Cited in: Pubmed; PMID 17873676. doi:10.1097/jcp.0b013e31815152a5
Gong, S. X. Y. L. (2010). Efficacy observation of 30 cases of depression of breast cancer patients treated with Xiaoyaosan. Shandong J. Traditional Chin. Med. 29 (10), 674–675. CNKI:SUN:SDZY.0.2010-10-010.
Gou, S. Q. X. Z., and Wu, L. L. (2023). Study on the antidepressant effect of Xiaoyao powder. Acta Chin. Med. Pharmacol. 1 (2), 33–34.
Guan, H. Z. B., Zheng, L. Q., and Zhagn, L. (2017). Effect of modified Xiaoyao Powder on type 2 diabetes mellitus complicated with depression. Chin. J. Rural Med. Pharmac 24 (9), 37–38. doi:10.3969/j.issn.1006-5180.2017.09.022
Guan, L. L. X., and Wu, Z. M. (2014). Comparative study on shugan-jieyu capsule and sertraline in treatment of mild to moderate senile depression. Chin. J. Med. Guide 1 (6), 1034–1035. doi:10.3969/j.issn.1009-0959.2014.06.063
Guan, Z. H. W. M., and Wang, B. (2017). Observations on the clinical study of the antidepressant effect of Xiaoyao Powder. Liaoning J. Traditional Chin. Med. 38 (1), 38–39.
Guo, J. T. B. Z., Li, B., and Bai, B. (2012). Clinical observation of Jieyu pills in treating mild and moderate depression Chinese Community Doctors. Chin. J. Med. Guide 14 (13), 223–224. doi:10.3969/j.issn.1007-614x.2012.13.216
Guo, J. X. L. L., and Zhang, W. (2015). Treating 52 cases of depression with jieyu pills yiyao qianyan. Chin. J. Med. Guide 1 (17), 207–208. doi:10.3969/j.issn.2095-1752.2015.17.187
Guo, L. R. Z. M., An, L. L., and Li, C. (2018). Clinical effect of Shugan Jieyu capsule on mild to moderate depression. Chin J Clin. Ration. Drug Use 3 (11), 63–64. CNKI:SUN:PLHY.0.2018-09-032.
Guo, Y. H. L. B., and Hu, T. L. (2014). Comparative analysis of Shugan Jieyu Capsule and Sertraline in the treatment of mild to moderate depression. Guangming J. Chin. Med. 29 (3), 572–573. doi:10.3969/j.issn.1003-8914.2014.03.073
Guo, Z. Y. L. Q., and Li, X. B. (2020). Investigate the clinical effect of Danzhi Xiaoyao powder in the treatment of depression of qiyu huahuo type. World Latest Med. Inf. 20 (3), 208–209. doi:10.3969/j.issn.1671-3141.2020.103.113
Hasin, D., Hatzenbuehler, M. L., Keyes, K., and Ogburn, E. (2006). Substance use disorders: diagnostic and statistical manual of mental disorders, fourth edition (DSM-IV) and international classification of Diseases, tenth edition (ICD-10). Addict 101 (Suppl. 1), 59–75. eng. Epub 2006/08/26. Cited in: Pubmed; PMID 16930162. doi:10.1111/j.1360-0443.2006.01584.x
He, J. C. Z. Y., and Wang, H. X. (2018). Treatment of 41 cases of depression after tumor with Chaihu and Keel Oyster decoction. Guangdong Med. J. 33 (3), 386–388. doi:10.3969/j.issn.1003-8914.2018.03.040
He, Q. T. Z. K. (2011). The clinical observation of 45 cases liver stagnation impair mind depression by jieyu decoction. Chin. J. Ethnomedicine Ethnopharmacy 20 (4), 80–81. doi:10.3969/j.issn.1007-8517.2011.04.056
He, R. R. X. B., Liu, J., and Zhao, M. (2017). Clinical observation of 30 cases of postpartum depression treated by Chaihujia Kegu Oyster Decoction. Hunan J. Traditional Chin. Med. 33 (8), 79–81. doi:10.16808/j.cnki.issn1003-7705.2017.08.034
Herrmann, N., Black, S. E., Lawrence, J., Szekely, C., and Szalai, J. P. (1998). The Sunnybrook Stroke Study: a prospective study of depressive symptoms and functional outcome. Stroke 29 (3), 618–624. eng. Epub 1998/03/20. Cited in: Pubmed; PMID 9506602. doi:10.1161/01.str.29.3.618
Higgins, J. P., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., et al. (2011). The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ Clin. Res. ed 343, d5928. eng. Epub 2011/10/20. Cited in: Pubmed; PMID 22008217. doi:10.1136/bmj.d5928
Higgins, J. P., Thompson, S. G., Deeks, J. J., and Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ Clin. Res. ed 327 (7414), 557–560. eng. Epub 2003/09/06. Cited in: Pubmed; PMID 12958120. doi:10.1136/bmj.327.7414.557
Holden, C. (1987). Stanford psychiatrist resigns under a cloud. Sci. (New York, NY) 237 (4814), 479–480. eng. Epub 1987/07/31. Cited in: Pubmed; PMID 3299707. doi:10.1126/science.3299707
Hou, M. J. L. X., and Wang, Y. L. (2019). Treatment of AIDS with depression by combination of traditional Chinese and Western medicine. China J. Chin. Med. 34 (6), 1275–1278. doi:10.16368/j.issn.1674-8999.2019.06.303
Huang, J. J. Y. Z., and Ting, F. (2014). Clinical study of psychological intervention and Chaihu plus Keel oyster Decoction in the treatment of post-stroke depression: jiangsu. Nanjing, China, Nanjing University of Traditional Chinese Medicine.
Huang, K. Z. T., and Zhou, C. (2014). Clinical study of Xiaoyao Pill in treatment of type 2 diabetes mellitus complicated with depression. Asia-Pacific Tradit. Med. 10 (13), 124–125.
Huang, N. Z. N., Yao, X. N., and Chen, X. (2007). Treatment of 38 cases of post-stroke depression with Chaihu and keel oyster decoction. Hunan J. Traditional Chin. Med. 21 (9), 79–81. doi:10.16808/j.cnki.issn1003-7705.2017.08.034
Irfan, M. (2024). Sleep terrors. Sleep. Med. Clin. 19 (1), 63–70. eng. Epub 2024/02/18. Cited in: Pubmed; PMID 38368070. doi:10.1016/j.jsmc.2023.12.004
Jansen, J. P., Crawford, B., Bergman, G., and Stam, W. (2008). Bayesian meta-analysis of multiple treatment comparisons: an introduction to mixed treatment comparisons. Value health J. Int. Soc. Pharmacoeconomics Outcomes Res. 11 (5), 956–964. eng. Epub 2008/05/21. Cited in: Pubmed; PMID 18489499. doi:10.1111/j.1524-4733.2008.00347.x
Jia, X. X. J. S., Wang, L., and Zhang, B. (2019). Clinical value analysis of Chaihu and Kegu Oyster decoction in the treatment of depression after tumor. Yiyao Qianyan 9 (12), 204.
Jiao, Y. J. H. C., Li, Q., and Jiang, L. (2015). Clinical effect of Huoxue tongqiao jieyu decoction on post-stroke depression. J. Front. Med. 5 (26), 311–312. doi:10.3969/j.issn.2095-1752.2015.26.275
Jin, Y. S. L. A., Wang, Y. J., and Chen, L. (2017). Clinical study of modified Buyang Huanwu Decoction in the treatment of post-ischemic stroke depression. China Health Care and Nutr. 27 (36), 437.
Jing, H. J. S. Y., Zhou, C., and Ju, G. (2009). A comparative study of Wuling Capsule and Delisin in the treatment of post-stroke depression. China Pharm. 31 (7), 1154–1155. doi:10.3969/j.issn.1001-1528.2009.07.061
Kohler, O., Krogh, J., Mors, O., and Benros, M. E. (2016). Inflammation in depression and the potential for anti-inflammatory treatment. Curr. Neuropharmacol. 14 (7), 732–742. eng. Epub 2016/09/20. Cited in: Pubmed; PMID 27640518. doi:10.2174/1570159x14666151208113700
Kumar, V. (2006). Potential medicinal plants for CNS disorders: an overview. Phytotherapy Res. PTR 20 (12), 1023–1035. eng. Epub 2006/08/16. Cited in: Pubmed; PMID 16909441. doi:10.1002/ptr.1970
Kwon, C. Y., Lee, B., Chung, S. Y., Kim, J. W., Shin, A., Choi, Y. Y., et al. (2018). Herbal medicine Sihogayonggolmoryeo-tang or Chai-Hu-Jia-Long-Gu-Mu-Li-Tang for the treatment of post-stroke depression: a protocol for a systematic review and meta-analysis. Medicine 97 (38), e12384. eng. Epub 2018/09/22. Cited in: Pubmed; PMID 30235703. doi:10.1097/md.0000000000012384
Lai, Y. S. W. L., and Yi, C. (2017). Clinical observation on the treatment of 68 cases of post-stroke depression with Chaihujia Kegu Oyster Decoction. Hebei J. Traditional Chin. Med. 39 (4), 535–538. doi:10.3969/j.issn.1002-2619.2017.04.013
LeMoult, J., and Gotlib, I. H. (2019). Depression: a cognitive perspective. Clin. Psychol. Rev. 69, 51–66. eng. Epub 2018/07/03. Cited in: Pubmed; PMID 29961601. doi:10.1016/j.cpr.2018.06.008
Li, C. F. W. J., and Zhang, F. (2010). Comparative study of Shugan Jieyu capsule and fluoxetine capsule in treatment of tubular depression. China J. Health Psychol. 18 (12), 1413–1414. CNKI:SUN:JKXL.0.2010-12-005.
Li, C. F. W. J., and Zhao, Z. X. (2011). Shugan Jieyu capsule treating 40 cases of senile depression. Shaanxi J. Traditional Chin. Med. 32 (10), 1315–1316. doi:10.3969/j.issn.1000-7369.2011.10.029
Li, G. Y. F. T., and Gao, H. (2015). Clinical observation of Jieyu pills in treating depression. Guide China Med. 13 (6), 205–206.
Li, P. D. H., and Zhang, T. (2004). Clinical analysis on Huoxue jieyu decoction in the treatment of post-stroke depression. Guangming J. Chin. Med. 12 (5), 1410–1411. doi:10.3969/j.issn.1003-8914.2016.10.028
Li, Q. L. L. J., Li, L. T., and Cai, T. (2016a). A clinical study of self-prepared Jieyu Huoxue decoction in the treatment of post-stroke depression Clinical. J. Traditional Chin. Med. 28 (10), 1464–1466. doi:10.16448/j.cjtcm.2016.0515
Li, R. G. Z. T., and Li, S. (2012a). Clinical observation on 78 cases of cirrhosis complicated with depression treated with Xiaoyao pills. J. Math. Med. 25 (3), 313–314. doi:10.3969/j.issn.1004-4337.2012.03.022
Li, R. H. W. X., Li, X. M., and Si, M. (2009). Observation of curative effect of Jieyu pills on post-stroke depression. Chin. J. Integr. Med. Cardio/Cerebrovascular Dis. 7 (9), 1132–1133. doi:10.3969/j.issn.1672-1349.2009.09.069
Li, R. Z. C., and Li, C. H. (2014). Modified Yueju Pill for treating 36 cases of depression. Henan Tradit. Chin. Med. 34 (5), 974–975.
Li, S. H. L. Y., and Li, S. S. (2012b). Clinical study of Chaihu Shugan Powder in treating depression of lung cancer. J. Pract. Traditional Chin. Med. 28 (5), 366–367. doi:10.3969/j.issn.1004-2814.2012.05.007
Li, S. S. Y. M., Zhang, B. Y., and Gu, D. (2016b). Observation on the curative effect of Jieyu Pill in treating post-stroke depression of liver-qi stagnation type. Electron. J. Clin. Med. Literature 3 (30), 6083–6084. CNKI:SUN:LCWX.0.2016-30-123.
Li, S. X. X., and Guo, X. Z. (2017). Clinical observation on the efficacy of xiaoyaowan and guipiwan in treating sub-threshold depression of older people. World Chin. Med. 12 (3), 566–569. doi:10.3969/j.issn.1673-7202.2017.03.022
Li, X. F. Z. J., and Wang, Y. (2015). Shugan Jieyu capsule and Seculin in the treatment of moderate depression control study. World Latest Med. Inf. 1 (86), 160–161. doi:10.3969/j.issn.1671-3141.2015.86.088
Li, X. J. L., and Wang, C. (2019). Observation on the efficacy of modified Chaihu plus Longgu Muli Decoction in the treatment of depression. China Pract. Med. 17 (12), 22–25. doi:10.14163/j.cnki.11-5547/r.2022.12.005
Li, X. T. H., and Li, L. (2008). Clinical study of Jieyu Pill and maprotiline in the treatment of senile depression. J. Liaoning Univ. Traditional Chin. Med. 10 (3), 80–81. doi:10.3969/j.issn.1673-842X.2008.03.048
Li, X. T. H., Zhang, M. Z., and You, Y. (2014). Treatment of 43 cases of post-stroke depression by wendan anshen decoction. Shaanxi J. Traditional Chin. Med. 1 (2), 152–153. doi:10.3969/j.issn.1000-7369.2014.02.016
Li, X. T. H., Zhao, X., and Cang, T. (2020). Effect of wendan anshen decoction on depression with insomnia symptoms. J. Hebei North Univ. Nat. Sci. Ed. 36 (6), 27–29. doi:10.3969/j.issn.1673-1492.2020.06.009
Li, X. T. L., and Tian, L. (2008). Clinical observation on jiawei ganmai dazao injection in treating 32 cases of depression after interventional therapy for CHD. Zhejiang J. Traditional Chin. Med. 43 (2), 88–89. doi:10.3969/j.issn.0411-8421.2008.02.012
Li, X. Y. C. J., Chen, C. S., and Zhang, L. Y. (2018). Therapeutic effect of Chaihu plus Keel Oyster Decoction on depression and neurological impairment in patients with post-stroke depression. Spec. Health 1 (20), 267. doi:10.3969/j.issn.2095-6851.2018.20.426
Li, Y. J. L. H., and Qian, R. Q. (2007). Effect of Danzhi Xiaoyao powder on neuro-immuno-endocrine system in patients with depression. Chin. J. Integr. Traditional West. Med. 27 (3), 197–200. doi:10.3321/j.issn:1003-5370.2007.03.001
Li, Y. Q. C. P., and Luo, H. C. (2013). Comparative study of shugan jieyu capsule and paroxetine in the treatment of depression. Chinese journal of trauma and disability. Medicine 21 (8), 71–72. doi:10.3969/j.issn.1673-6567.2013.08.044
Li, Y. W. B., and Dong, R. F. (2009). Post stroke depression treated by Xingnao jieyu decoction. China's Naturop. 17 (5), 19–20. doi:10.3969/j.issn.1007-5798.2009.05.018
Li, Y. W. B., and Wang, A. (2004). Clinical observation of self-formulated Xingnaojieyu Decoction in the treatment of post-stroke depression. Beijing J. Traditional Chin. Med. 23 (5), 282–284. doi:10.3969/j.issn.1674-1307.2004.05.009
Li, Z. B. Z. Y., Zhang, J. J., and Qian, Q. (2003). Observation of curative effect of self-prepared huo xue Jie Yu decoction on stroke depression. Guangxi J. Traditional Chin. Med. 26 (6), 13–14. doi:10.3969/j.issn.1003-0719.2003.06.006
Li, Z. S. T. J. (2007). Clinical observation of Jieyou Decoction in treating 40 cases of liver-stagnation phlegm-blocking depression. J. Traditional Chin. Med. Univ. Hunan 27 (2), 58–59. doi:10.3969/j.issn.1674-070X.2007.02.022
Li, Z. Z. Y., Hu, J. J., and Hong, T. (2010). Danzhi Xiaoyao Powder in the treatment of 30 cases of depression after ischemic stroke. Henan Tradit. Chin. Med. 30 (4), 376–377. CNKI:SUN:HNZY.0.2010-04-033.
Lin, B. X. J., Tan, J., and Eng, J. X. (2011). Clinical study of supplemented Bupleurum Shugan Powder in the treatment of depression. J. New Chin. Med. 43 (8), 36–37. CNKI:SUN:REND.0.2011-08-021.
Lin, H. H. B., and Han, Zc (2019). Clinical observation of Jieyu Granules in treatment of mild depression. Chin. J. Integr. Med. Cardio/Cerebrovascular Dis. 17 (17), 2693–2696. doi:10.12102/j.issn.1672-1349.2019.17.041
Liu, C. H. M., and Tan, J. (2010). Treating 30 cases of post-stroke depression with added flavor of Chaihu Shugan powder. Shaanxi J. Traditional Chin. Med. 31 (10), 1315–1316. doi:10.3969/j.issn.1000-7369.2010.10.028
Liu, D. P. L. D., and Wang, X. F. (2017). Clinical efficacy of Chaihu Kegu Oyster Decoction plus decoction in the treatment of depression disorder. Health Guide 1 (17), 23. doi:10.3969/j.issn.1006-6845.2017.17.020
Liu, F. H. S. J., and Zhang, X. H. (2012). Morinda oligosaccharide capsule treating 42 cases of mild to moderate depression Shaanxi. J. Traditional Chin. Med. 33 (2), 165–167. doi:10.3969/j.issn.1000-7369.2012.02.021
Liu, F. S. G., and Ku, B. S. (2012). A preliminary study on the antidepressant effect of Morinda Officinalis Oligosaccharide Capsule Chinese. J. Integr. Traditional West. Med. 32 (15), 40–44.
Liu, J. W. B., and Wang, X. (2019). Clinical observation of 40 cases of post-ischemic stroke depression treated with modified Buyang Huanwu Decoction. Xinjiang J. Traditional Chin. Med. 37 (2), 10–12. CNKI:SUN:XJZY.0.2019-02-004.
Liu, W. M. L. S., Hou, X. C., et al. (2017). Study on the mechanism of action of Xiaoyao Powder in the treatment of depression. Chin. Tradit. Pat. Med. 2 (2), 3–8.
Liu, X. F. L. G., and Wang, S. Y. (2015). The influence of bupleurum decoction plus dragon bone and oyster shell on the expression of serum cytokines IL-1βand TNF-αin patients with post-stroke depression. Chin. Manip. Rehabilitation Med. 6 (13), 12–14.
Liu, X. Y. M. Y., Li, L. L., and Xi, X. (2007). Clinical observation of "Huoxue jieyu decoction" in treating 134 cases of post-stroke depression. Shanghai J. Traditional Chin. Med. 41 (5), 30–32. doi:10.3969/j.issn.1007-1334.2007.05.013
Lu, H. T. D., and Sun, A. J. (2022). Application effect of modified Chaihu Longgu Muli decoction on post-stroke depression. China Mod. Med. 29 (34), 164–167. doi:10.3969/j.issn.1674-4721.2022.34.042
Lu, X. Y. Y. Y., and Xin, M. (2020). Effect of Shugan Jieyu capsule on mild and moderate depression. Spec. Health 1 (36), 136.
Lu, Y. Y. L. Z., and Li, H. (2019). Effect of supplemented Buyang Huanwu decoction on depression patients after ischemic stroke. Pract. Clin. J. Integr. Traditional Chin. West. Med. 19 (9), 99–101. doi:10.13638/j.issn.1671-4040.2019.09.050
Luo, H. C. Q. R., and Zhao, X. Y. (2006). Clinical observation on effect of Danzhi Xiaoyao powder in treating depression. Chin. J. Integr. Traditional West. Med. 26 (3), 212–214. doi:10.3321/j.issn:1003-5370.2006.03.005
Luo, J. H. X. D., and Wu, T. (2021). Clinical effect of Shugan Jieyu Capsule and Sertraline on patients with mild to moderate depression. Strait Pharm. J. 33 (8), 143–145. doi:10.3969/j.issn.1006-3765.2021.08.064
Luo, Z. M. L. X., Xie, W. C., and Fu, C. (2019). Clinical observation of 42 cases of depressive disorder treated by Chaihu Kegu Oyster Decoction combined with Western medicine. Chin. J. Ethnomedicine Ethnopharmacy (3), 104–105. doi:10.3969/j.issn.1007-8517.2019.3.zgmzmjyyzz201903031
Ma, X. D. Y. L., and Ye, W. D. (2017). Discussion on the clinical effect of Danzhi Xiaoyao pill in the treatment of puerperal depression. Guangming J. Chin. Med. 32 (15), 2149–2151. doi:10.3969/j.issn.1003-8914.2017.15.005
Mao, S. L. L. S., and Li, S. (2016). Efficacy of Shuganjieyu capsule for the treatment of post-stroke depression. Clin. Medicat. J. 1 (1), 54–56. doi:10.3969/j.issn.1672-3384.2016.01.012
Mao, W. B. Z. H., and Li, S. S. (2010). Clinical observation of Shugan Jieyu capsule in treatment of senile depression. Chin. J. Clin. Ration. Drug Use 3 (21), 45–46. doi:10.3969/j.issn.1674-3296.2010.21.039
McIntyre, R. S., Konarski, J. Z., Mancini, D. A., Fulton, K. A., Parikh, S. V., Grigoriadis, S., et al. (2005). Measuring the severity of depression and remission in primary care: validation of the HAMD-7 scale. CMAJ Can. Med. Assoc. J. = J. de l'Association medicale Can. 173 (11), 1327–1334. eng. Epub 2005/11/23. Cited in: Pubmed; PMID 16301700. doi:10.1503/cmaj.050786
Meng, H. Q. S. J., Quan, Y. Q., and Ni, D. (2008). A clinical study of the efficacy ganmaidazaotang in treatment of post-stroke depression. Liaoning J. Traditional Chin. Med. 35 (3), 384–385. doi:10.3969/j.issn.1000-1719.2008.03.032
Meng, L. L. M., and Li, X. X. (2011). Clinical observation of Wuling capsule in the treatment of post-stroke depression. Chin. J. Pract. Nerv. Dis. 14 (9), 72–73. doi:10.3969/j.issn.1673-5110.2011.09.043
Meng, Q. C. W. J., Cao, L., and Nan, N. (2016). Clinical analysis of Danzhi Xiaoyao Powder in the treatment of post-stroke depression. World Latest Med. Inf. 16 (89), 107. doi:10.3969/j.issn.1671-3141.2016.89.098
Min Cx, W. T., and Li, X. P. (2018). Study on Xiaoyao pills in the treatment of depression disorder after cerebral infarction. Shandong, China: Qingdao University.
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., et al. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 4 (1), 1. eng. Epub 2015/01/03. Cited in: Pubmed; PMID 25554246. doi:10.1186/2046-4053-4-1
Monroe, S. M., and Harkness, K. L. (2022). Major depression and its recurrences: life course matters. Annu. Rev. Clin. Psychol. 18, 329–357. eng. Epub 2022/02/27 Cited in: Pubmed; PMID 35216520. doi:10.1146/annurev-clinpsy-072220-021440
Mrozek, W., Socha, J., Sidorowicz, K., Skrok, A., Syrytczyk, A., Piątkowska-Chmiel, I., et al. (2023). Pathogenesis and treatment of depression: role of diet in prevention and therapy. Nutr. Burbank, Los Angel. Cty. Calif. 115, 112143. eng. Epub 2023/08/10. Cited in: Pubmed; PMID 37562078. doi:10.1016/j.nut.2023.112143
Nachimuthu, S., Assar, M. D., and Schussler, J. M. (2012). Drug-induced QT interval prolongation: mechanisms and clinical management. Ther. Adv. drug Saf. 3 (5), 241–253. eng. Epub 2012/10/01. Cited in: Pubmed; PMID 25083239. doi:10.1177/2042098612454283
Neupane, B., Richer, D., Bonner, A. J., Kibret, T., and Beyene, J. (2014). Network meta-analysis using R: a review of currently available automated packages. PloS one 9 (12), e115065. eng. Epub 2014/12/30. Cited in: Pubmed; PMID 25541687. doi:10.1371/journal.pone.0115065
Nie, R. R. J. W., Lu, F. P., and Da, D. (2016). Clinical study of Jiawei Buyang Huanwu Decoction in the treatment of depression after ischemic stroke. Chin. Tradit. Pat. Med. 38 (4), 958–960. doi:10.3969/j.issn.1001-1528.2016.04.056
Nobile, B., Ramoz, N., Jaussent, I., Gorwood, P., Olié, E., Castroman, J. L., et al. (2019). Polymorphism A118G of opioid receptor mu 1 (OPRM1) is associated with emergence of suicidal ideation at antidepressant onset in a large naturalistic cohort of depressed outpatients. Sci. Rep. 9 (1), 2569. eng. Epub 2019/02/24. Cited in: Pubmed; PMID 30796320. doi:10.1038/s41598-019-39622-3
Peng, L., Zhang, X., Kang, D. Y., Liu, X. T., and Hong, Q. (2014). Effectiveness and safety of Wuling capsule for post stroke depression: a systematic review. Complementary Ther. Med. 22 (3), 549–566. eng. Epub 2014/06/08. Cited in: Pubmed; PMID 24906594. doi:10.1016/j.ctim.2014.04.005
Qi, J. G. G., Cao, L., and Yi, N. (2017). Application evaluation of Chaihu and Keel Oyster Decoction in patients with depression after chemotherapy for malignant tumor Guangming. J. Chin. Med. 32 (3), 382–384. doi:10.3969/j.issn.1003-8914.2017.03.035
Qin, H. S. Y., and Tang, D. P. (2016). Observation of clinical efficacy of Chaihu and Kegu Oyster Decoction in the treatment of depression after chemotherapy. Med. Inf. 29 (5), 371. doi:10.3969/j.issn.1006-1959.2016.05.314
Qiu, T. W. L. X., and Zhu, H. X. (2011). A comparative study of shugan-jieyu capsule and sertraline in treatment of depression. J. Traditional Chin. Med. Univ. Hunan 31 (8), 60–61. doi:10.3969/j.issn.1674-070X.2011.08.025
Qu, B. Z. S., Wang, Y., and Kai, X. (2011). A comparative study of Shugan Jieyu Capsule and Sertraline hydrochloride in the treatment of adolescent depression. Nei Mongol J. Traditional Chin. Med. 30 (19), 67–68. doi:10.3969/j.issn.1006-0979.2011.19.084
Qu, B. Z. Y., Zhu, M., and Wu, Q. (2012). Clinical observation on efficacy of shugan jieyu capsule in treatment of diabetes associated with depression in 64 cases. Asia-Pacific Tradit. Med. 8 (2), 56–57. doi:10.3969/j.issn.1673-2197.2012.02.027
Ran, S. L. Y. K., Lin, T., and Liu, Q. (2010). Clinical study of Wuling capsule in the treatment of post-stroke depression. China Pharm. 32 (7), 1271–1272. doi:10.3969/j.issn.1001-1528.2010.07.059
Ren, S. H. YCWW (2017). Observation on clinical therapeutic effect of jieyu pills in the treatment of mild and moderate postpartum depression. Guangming J. Chin. Med. (2), 225–226. doi:10.3969/j.issn.1003-8914.2017.02.031
Ren, Y. W. Z., and Li, X. X. (2015). Clinical value of Wendan Anshen Decoction in the treatment of post-stroke depression in elderly patients. Med. Aesthet. Cosmetol. 24 (2), 209–210.
Salanti, G., Ades, A. E., and Ioannidis, J. P. (2011). Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J. Clin. Epidemiol. 64 (2), 163–171. eng. Epub 2010/08/07. Cited in: Pubmed; PMID 20688472. doi:10.1016/j.jclinepi.2010.03.016
Sarris, J. (2007). Herbal medicines in the treatment of psychiatric disorders: a systematic review. Phytotherapy Res. PTR 21 (8), 703–716. eng. Epub 2007/06/15. Cited in: Pubmed; PMID 17562566. doi:10.1002/ptr.2187
Sarris, J., Panossian, A., Schweitzer, I., Stough, C., and Scholey, A. (2011). Herbal medicine for depression, anxiety and insomnia: a review of psychopharmacology and clinical evidence. Eur. Neuropsychopharmacol. J. Eur. Coll. Neuropsychopharmacol. 21 (12), 841–860. eng. Epub 2011/05/24. Cited in: Pubmed; PMID 21601431. doi:10.1016/j.euroneuro.2011.04.002
Sathyanarayana Rao, T. S., and Yeragani, V. K. (2009). Hypertensive crisis and cheese. Indian J. psychiatry 51 (1), 65–66. eng. Epub 2009/09/11. Cited in: Pubmed; PMID 19742203. doi:10.4103/0019-5545.44910
Saxena, K., Kurian, S., Kumar, R., Arnold, L. E., and Simkin, D. R. (2023). Mood disorders in youth: complementary and integrative medicine. Child Adolesc. psychiatric Clin. N. Am. 32 (2), 367–394. eng. Epub 2023/05/06. Cited in: Pubmed; PMID 37147043. doi:10.1016/j.chc.2022.08.012
Scala, M., Fanelli, G., De Ronchi, D., Serretti, A., and Fabbri, C. (2023). Clinical specificity profile for novel rapid acting antidepressant drugs. Int. Clin. Psychopharmacol. 38 (5), 297–328. eng. Epub 2023/06/29. Cited in: Pubmed; PMID 37381161. doi:10.1097/yic.0000000000000488
Shao, C. L. X. C., and Feng, X. X. (2019). A randomised, double-blind, placebo-controlled study of Buyang Huanwu Decoction in the treatment of mild-to-moderate depression. Chongqing Med. 40 (21), 2–3.
Shao, X. L. Z. S., and Zhao, S. Y. (2011). Clinical observation of Jieyu pills and Mianserin in treating climacteric depression. Med. J. Chin. People's Health 23 (9), 1107–1109. doi:10.3969/j.issn.1672-0369.2011.09.030
Shao, X. Q. Z. J., and li, X. S. (2016). Clinical experience of addition and reduction of Bupleurum Shugan Powder in treatment of 28 cases of depressio. World Latest Med. Inf. 16 (53), 181. doi:10.3969/j.issn.1671-3141.2016.53.138
Shen, Z. M. Z. M., and Zhao, A. Q. (2004). Comparative observation on efficacy of jieyu pill and maprotiline in treating depression. Chin. J. Integr. Traditional West. Med. 24 (5), 415–417. doi:10.3321/j.issn:1003-5370.2004.05.008
Shi, J. T. J., and Zeng, Q. (2008). Jieyu pills treated 68 cases of mild to moderate depression. Shaanxi J. Traditional Chin. Med. 29 (11), 1486–1488. doi:10.3969/j.issn.1000-7369.2008.11.041
Shim, S. R., Kim, S. J., Lee, J., and Rücker, G. (2019). Network meta-analysis: application and practice using R software. Epidemiol. health 41, e2019013. e2019013. eng. Epub 2019/04/20. Cited in: Pubmed; PMID 30999733. doi:10.4178/epih.e2019013
Song, N. Y. J., and Li, T. T. (2019). Comparison of the efficacy and safety of Shugan Jieyu Capsule and Sertraline hydrochloride tablets in the treatment of menopausal depression. Contemp. Med. Forum 17 (17), 152–153. CNKI:SUN:QYWA.0.2019-17-116.
Sun, R. W. C., and Zhou, T. (2012). Buyang Huanwu tang jiawei He fluoxetine treatment of 26 cases of post-stroke depression. Hunan J. Chin. Med. 28 (4), 2. CNKI:SUN:HNZO.0.2012-04-020.
Sun, Y., Xu, X., Zhang, J., and Chen, Y. (2018). Treatment of depression with Chai Hu Shu Gan San: a systematic review and meta-analysis of 42 randomized controlled trials. BMC complementary Altern. Med. 18 (1), 66. eng. Epub 2018/02/20. Cited in: Pubmed; PMID 29454341. doi:10.1186/s12906-018-2130-z
Sun, Z. G. W. X., and Li, S. (2012). Clinical and experimental study of shuyu powder in the treatment of depression: PLA general hospital. Springer, Berlin, Germany.
Ta, G. W. J., Du, X., and Hua, Q. (2008). Treating 24 cases of post-stroke depression with Chaihu and keel oyster decoction. Jilin J. Traditional Chin. Med. 28 (3), 179–180. doi:10.3969/j.issn.1003-5699.2008.03.014
Tan, H. H. L. X., Wang, J., and Xiao, H. (2015). Treatment of 48 cases of senile depression with wendan anshen decoction. Chin. J. Gerontology 1 (20), 5935–5936. doi:10.3969/j.issn.1005-9202.2015.20.126
Tang, P. L. J., and Wang, W. J. (2009). Clinical observation of Ganmai Dazao Decoction in treating 38 cases of post-stroke depression. Sichuan Med. J. 30 (5), 709–710. doi:10.3969/j.issn.1004-0501.2009.05.044
Tao, B. P. G. S., and Wang, Y. H. (2015). Effect of Shugan Jieyu capsule on adolescent depression. Zhejiang J. Integr. Traditional Chin. West. Med. 25 (5), 464–465. doi:10.3969/j.issn.1005-4561.2015.05.021
Tao, J. Q. Z. Y., and Li, T. R. (2006). Comparison of Chinese medicine Jieyu Pill and Venlafaxine sustained-release in the treatment of different degrees of depression. Chin. J. Tissue Eng. Res. 10 (39), 1–3. doi:10.3321/j.issn:1673-8225.2006.39.001
Tao, Y. F. Z. H., and Yin, L. (2012). A comparative study of Shugan-jieyu capsule and Paroxetine in the treatment of depression. Med. J. Chin. People's Health 24 (19), 2347–2348. doi:10.3969/j.issn.1672-0369.2012.19.012
Tu, Y. F. H. T., and Wang, M. (2016). Observation of therapeutic effect and mechanism of Chaihu plus Kegu Oyster Decoction in the treatment of depression associated with liver-qi depression Parkinson's disease. Chin. J. Tissue Eng. Res. 4, 4. doi:10.3969/j.issn.1003-8914.2017.04.027
Wan, R., Song, R., Fan, Y., Li, L., Zhang, J., Zhang, B., et al. (2021). Efficacy and safety of Chaihu Jia Longgu Muli decoction in the treatment of poststroke depression: a systematic review and meta-analysis. Evidence-based complementary Altern. Med. eCAM 2021, 7604537. eng. Epub 2021/08/31. Cited in: Pubmed; PMID 34457030. doi:10.1155/2021/7604537
Wang, B. X. Y., and Li, R. (2019). Effect of Chaihujia Keel oyster decoction on depression. Shandong Med. J. 59 (20), 62–64. doi:10.3969/j.issn.1002-266X.2019.20.017
Wang, C. L. C., and Wang, X. (2018). To explore the clinical effect of Shugan Jieyu capsule on depression. Health perspect. 4 (8), 253. doi:10.3969/j.issn.1005-0019.2018.08.323
Wang, H. R. S. L., and Wang, J. (2011). Clinical observation of Chaihu and Keel oyster decoction in the treatment of post-stroke depression. China Pract. Med. 6 (7), 175–176. doi:10.3969/j.issn.1673-7555.2011.07.146
Wang, H. Z. T. S., Wang, Y. G., and Re, N. (2016). Observation of therapeutic effect of Shugan Huoxue Jieyu Decoction on 70 cases of post-stroke depression. Shaanxi J. Traditional Chin. Med. 1 (2), 218–219. doi:10.3969/j.issn.1000-7369.2016.02.035
Wang, J. C. L. Q., and Shao, Z. Y. (2019). Clinical control study of Shugan Jieyu capsule and Morinda oligosaccharide capsule in the treatment of depression. Strait Pharm. J. 31 (1), 187–188. doi:10.3969/j.issn.1006-3765.2019.01.100
Wang, J. H. W. J., and Liu, H. W. (2016). Treatment of depression after tumor with Chaihu and Kegu decoction in 50 cases. Shaanxi Tradit. Chin. Med. 37 (9), 2. doi:10.3969/j.issn.1000-7369.2016.09.047
Wang, J. H. W. J., and Liu, H. W. (2017). Clinical observation of Chaihu and Kegu Oyster decoction in the treatment of depression after tumor. Acta Chin. Med. Pharmacol. 45 (1), 120–122. doi:10.3969/j.issn.1002-2392.2017.01.036
Wang, J. H. W. J., and Yang, J. Q. (2016). Clinical study on the treatment of breast cancer complicated with depression with Chaihu Keel Oyster Decoction. Shaanxi Tradit. Chin. Med. 19 (5), 732–736. doi:10.11723/mtgyyx1007-9564201605021
Wang, J. Y. L. Q., and Zhang, H. (2019). Effect of Xiaoyao Powder on 68 patients with post-stroke depression. Contemp. Med. Symp. 17 (10), 206–208. CNKI:SUN:QYWA.0.2019-10-152.
Wang, M. L. P., and Dou, H. Y. (2018). Study on the clinical effect of Ganmai Dazao Decoction in the treatment of post-stroke depression. Guide China Med. 16 (23), 180. CNKI:SUN:YYXK.0.2018-23-137.
Wang, P. W. H., and Ma, X. (2006). Clinical observation of 42 cases of post-stroke depression treated from liver Journal of Practical Traditional Chinese. Intern. Med. 20 (4), 381–382. doi:10.3969/j.issn.1671-7813.2006.04.022
Wang, Q. S. J. X., Shi, F., and Shou, F. (2012). Clinical observation of Danzhi Xiaoyao Powder in the treatment of mild to moderate depression. Proc. 12th Natl. Conf. Ment. Dis. Integr. Traditional Chin. West. Med. 2013, 77–79.
Wang, R. Z. J., and Zhang, Y. (2018). Clinical observation of Shuganjieyu capsules in treatment of depression of liver stagnation and spleen deficiency type. Med. J. Chin. People's Health. 1 (16), 75–77. doi:10.3969/j.issn.1672-0369.2015.16.042
Wang, S. D. X., and Jiang, T. (2021). Clinical observation and safety evaluation of Bajitian oligosaccharide capsules in the treatment of 60 cases with depressive disorder. Anhui Med. Pharm. J. 25 (6), 1232–1235. doi:10.3969/j.issn.1009-6469.2021.06.042
Wang, S. J. L. S., and Wan, H. Q. (2020). Effect of wuling capsule on clinical efficacy and negative emotion in patients with post-stroke depression. Hebei Med. 26 (1), 162–165. doi:10.3969/j.issn.1006-6233.2020.01.039
Wang, X. B. S. S., and Ban, Y. H. (2010). Clinical observation of Chaihu and Keel oyster decoction in the treatment of perimenopausal depression. Inf. Traditional Chin. Med. 27 (3), 98–99. doi:10.3969/j.issn.1002-2406.2010.03.038
Wang, X. Q. Z. H., and Shu, L. (2009). Efficacy and safety of morinda officinalis oligose capsule in the treatment of mild or moderate depression Chinese. J. New Drugs 18 (9), 802–843. doi:10.3321/j.issn:1003-3734.2009.09.010
Wang, Y., Guan, R., Zhong, J., Shi, Q., Ye, Z., and Pan, L. (2023b). Research progress on the treatment of perimenopausal insomnia with Chaihu Jia Longgu Muli decoction based on brain-intestine-bacteria axis: a review. Medicine 102 (51), e36537. eng. Epub 2023/12/22. Cited in: Pubmed; PMID 38134054. doi:10.1097/md.0000000000036537
Wang, Y., Li, M., Liang, Y., Yang, Y., Liu, Z., Yao, K., et al. (2017). Chinese herbal medicine for the treatment of depression: applications, efficacies and mechanisms. Curr. Pharm. Des. 23 (34), 5180–5190. eng. Epub 2017/09/20. Cited in: Pubmed; PMID 28925891. doi:10.2174/1381612823666170918120018
Wang, Y. H. X. X., and Luo, Y. (2007). Treatment of depression after cerebrovascular disease with Chaihu shugan decoction. Jilin J. Traditional Chin. Med. 27 (8), 2. doi:10.3969/j.issn.1003-5699.2007.08.012
Wang, Y. J. L. G., and Li, B. (2017). Treatment of depression after stroke by Chaihu kegu decoction. Jilin J. Traditional Chin. Med. 37 (5), 466–468. doi:10.13463/j.cnki.jlzyy.2017.05.011
Wang, Y. T., Wang, X. L., Wang, Z. Z., Lei, L., Hu, D., and Zhang, Y. (2023a). Antidepressant effects of the traditional Chinese herbal formula Xiao-Yao-San and its bioactive ingredients. Phytomedicine Int. J. phytotherapy Phytopharm. 109, 154558. eng. Epub 2023/01/08. Cited in: Pubmed; PMID 36610123. doi:10.1016/j.phymed.2022.154558
Wang, Y. Z. R., and Guo, A. (2020). Value of Shugan Jieyu capsule in the treatment of mild to moderate depression. Psychol. Mag. 15 (15), 106. doi:10.19738/j.cnki.psy.2020.15.075
Wang, Y. Z. R., Guo, S. Q., and Shou, F. (2014). Comparison of efficacy and safety between Jieyu pills and Venlafaxin in treatment of depression. Med. J. Chin. People's Health 26 (6), 10–12. doi:10.3969/j.issn.1672-0369.2014.06.004
Wang, Z. L. G. Y., and Wu, L. Z. (2008). Treatment of 30 cases of malignant tumor complicated with depression with Ganmai Dazao decoction. Jiangsu J. Traditional Chin. Med. 40 (12), 44–45. doi:10.3969/j.issn.1672-397X.2008.12.025
Watt, J., and Del Giovane, C. (2022). Network meta-analysis. Methods Mol. Biol. Clift. NJ 2345, 187–201. eng. Epub 2021/09/23. Cited in: Pubmed; PMID 34550592. doi:10.1007/978-1-0716-1566-9_12
Wei, G. Q. D. L., and Lu, Z. (2014). Efficacy and safety of shugan jieyu capsule in the treatment of depression in college students strait pharmaceutical. Journal 26 (11), 128–129. doi:10.3969/j.issn.1006-3765.2014.11.052
Wei, Q. W. M. X., and Huang, S. (2014). Shugan jieyu capsule of mild and moderate depression with fluoxetine in treatment of equivalent random parallel controlled study. J. Pract. Traditional Chin. Intern. Med. 28 (10), 32–34. doi:10.13729/j.issn.1671-7813.2014.10.17
Weibel, S., Rücker, G., Eberhart, L. H., Pace, N. L., Hartl, H. M., Jordan, O. L., et al. (2020). Drugs for preventing postoperative nausea and vomiting in adults after general anaesthesia: a network meta-analysis. Cochrane database Syst. Rev. 10 (10), Cd012859. eng. Epub 2020/10/20. Cited in: Pubmed; PMID 33075160. doi:10.1002/14651858.CD012859.pub2
Wu, D. F. W. M., and Zhu, M. (2016). Clinical study of Chaihu and Keel oyster decoction in the treatment of post-stroke depression. Med. Inf. 29 (5), 371–372. doi:10.3969/j.issn.1006-1959.2016.05.314
Wu, J. M. Z. M., Li, M., and Chi, K. (2002). A comparative study on the antidepressant effect of modified Ganmai Dazao Decoction. Chin. J. Clin. 30 (11), 18–19. doi:10.3969/j.issn.1008-1089.2002.11.01
Wu, J. W. H., Wang, C. C., and Ti, Z. (2012). Clinical observation of 60 cases of post-stroke depression treated by integrated Chinese and Western medicine. J. Sichuan Traditional Chin. Med. 30 (9), 71–72. CNKI:SUN:SCZY.0.2012-09-036.
Wu, J. Z. W. M., and Tian, L. P. (2018). Effect of Shugan Jieyu capsule on mild and moderate depression. Chin. Archives Traditional Chin. Med. 36 (6), 1482–1484. doi:10.13193/j.issn.1673-7717.2018.06.052
Wu, P. P. X. T., and Wan, Q. (2015). Effect of jiaweidanzhi Xiaoyao powder on post-stroke depression. Contemp. Med. Forum 13 (21), 11–12. CNKI:SUN:QYWA.0.2015-21-010.
Xiao, G. R. S. X. (2006). Effect of Wuling capsule on anxiety and depression after stroke. Beijing Med. J. 28 (2), 125. doi:10.3969/j.issn.0253-9713.2006.02.034
Xiao, J. S. Z. J., and Huang, C. Y. (2004). Treatment of 68 cases of post-stroke depression with Xiaoyao SAN. J. Math. Med. 017 (004), 333–334. doi:10.3969/j.issn.1004-4337.2004.04.023
Xie, J. Y. Z. X., and Li, C. H. (2011). Clinical observation on treatment of Ease pill in 58 cases coronary heart disease with depressive disorder. Mod. Hosp. 11 (4), 44–45. doi:10.3969/j.issn.1671-332X.2011.04.019
Xu, B. Z. M., Ying, S. J., and Zhang, S. j. (2007). Observation on effect of wuling capsule in treating poststroke depression. Chin. J. Integr. Traditional West. Med. 27 (7), 640–642. doi:10.3321/j.issn:1003-5370.2007.07.021
Xu, Q. C. W., and Yang, W. F. (2014). Therapeutic effect of Buyang Huanwu decoction on post-stroke depression. Shanghai J. Traditional Chin. Med. 48 (5), 2. CNKI:SUN:SHZZ.0.2014-05-018.
Xu, Q. T. Y. H., and Wang, F. (2015). Effects of Jieyu pills on depression and quality of life after stroke. Jilin Med. J. 36 (7), 1374–1375. doi:10.3969/j.issn.1004-0412.2015.07.062
Xu, S. W. G. H., and Wang, K. Q. (2007). Comparative study on the efficacy of Jieyu Pill and Venlafaxine in the treatment of first episode depression. China Pract. Med. 2 (24), 28–29. doi:10.3969/j.issn.1673-7555.2007.24.012
Xu, T. S. W. Q., Fang, Y., and Xue, Q. F. (2011b). Clinical study on treatment of 32 cases of depression with "modified ganmai dazao decoction. Jiangsu J. Traditional Chin. Med. 43 (9), 24–25. doi:10.3969/j.issn.1672-397X.2011.09.015
Xu, T. W. S., Wu, C. Y., and Xiao, X. (2011a). Clinical comparative study of shugan jieyu capsule and sertraline in the treatment of depression. Chin. J. Med. Guide 13 (9), 1654–1655. doi:10.3969/j.issn.1009-0959.2011.09.114
Xu, W. J. Z. Y., and Wu, L. (2019). Clinical study of Shugan Jieyu capsule in treating depression. J. New Chin. Med. 51 (5), 141–143. doi:10.13457/j.cnki.jncm.2019.05.042
Xu, Y. S. L. S., and Li, X. L. (2006). A paralleled compartive study of wuling capsule and amitriptylinein in the treatment of mild depression. J. Shandong Med. Coll. 28 (4), 281–282. doi:10.3969/j.issn.1674-0947.2006.04.011
Xu, Z. Z. M., and Li, L. J. (2012). Observation on therapeutic effect of Jieyu pills on depression. J. Community Med. 10 (16), 10–11. CNKI:SUN:SQYX.0.2012-16-006.
Xun, X. L. H. Q., and Bai, T. (2010). Clinical observation on the treatment of 30 cases of post stroke depression with combination of TCM and Western Medicin. China Med. Her. 07 (18), 90–91. doi:10.3969/j.issn.1673-7210.2010.18.04
Yan, F. D. C. S., and Bo, B. B. (2014). Analysis of the clinical effect of Wuling capsule in treating patients with moderate depression after cerebral infarction. World Health Dig. 1 (16), 282–283. doi:10.3969/j.issn.1672-5085.2014.16.359
Yan, H. M. C. Y., and Li, W. (2008). Clinical observation of 54 cases of depression treated by remote powder. Chin. Med. Mod. Distance Educ. China 9 (6), 1039–1040.
Yan, Y. M. H. W., and Wang, T. (2003). Clinical effect of removing phlegm and removing stasis, resolving depression and awakening brain in the treatment of 38 cases of post-stroke depression. Mod. Tradit. Chin. Med. 1 (4), 6–7. doi:10.3969/j.issn.1672-0571.2003.04.003
Yang, J. J. W. S., and Rui, Ao (2015). Clinical study of Jieyu pill in treating depression. China's Naturop. 23 (7), 53–54.
Yang, L., Ao, Y., Li, Y., Dai, B., Li, J., Duan, W., et al. (2023). Morinda officinalis oligosaccharides mitigate depression-like behaviors in hypertension rats by regulating Mfn2-mediated mitophagy. J. neuroinflammation 20 (1), 31. eng. Epub 2023/02/12. Cited in: Pubmed; PMID 36765376. doi:10.1186/s12974-023-02715-y
Yang, Q. X. F. H. (2012). Clinical observation of Ganmai Dazao Jieyu Decoction in treating 32 cases of senile depression. Henan Tradit. Chin. Med. 32 (6), 734–735.
Ye, J. F. L. Y., and Xia, J. M. (2014). Comparative study of shugan jieyu capsule and sertraline in the treatment of senile depression. Chin. Tradit. Pat. Med. 36 (5), 1104–1105. doi:10.3969/j.issn.1001-1528.2014.05.054
Yeung, W. F., Chung, K. F., Ng, K. Y., Yu, Y. M., Ziea, E. T., and Ng, B. F. (2014a). A meta-analysis of the efficacy and safety of traditional Chinese medicine formula Ganmai Dazao decoction for depression. J. Ethnopharmacol. 153 (2), 309–317. eng. Epub 2014/03/19. Cited in: Pubmed; PMID 24632021. doi:10.1016/j.jep.2014.02.046
Yeung, W. F., Chung, K. F., Ng, K. Y., Yu, Y. M., Ziea, E. T., and Ng, B. F. (2014b). A systematic review on the efficacy, safety and types of Chinese herbal medicine for depression. J. psychiatric Res. 57, 165–175. eng. Epub 2014/06/30. Cited in: Pubmed; PMID 24974002. doi:10.1016/j.jpsychires.2014.05.016
Yildiz, A., Siafis, S., Mavridis, D., Vieta, E., and Leucht, S. (2023). Comparative efficacy and tolerability of pharmacological interventions for acute bipolar depression in adults: a systematic review and network meta-analysis. lancet Psychiatry 10 (9), 693–705. eng. Epub 2023/08/19. Cited in: Pubmed; PMID 37595997. doi:10.1016/s2215-0366(23)00199-2
Yin, S. W. L., and Zhang, S. (2018). Observation on the effect of Shugan Huoxue Jieyu Decoction in the treatment of post-stroke depression liver-qi stagnation type. J. Pract. Traditional Chin. Med. 34 (6), 647–648. doi:10.3969/j.issn.1004-2814.2018.06.017
Yin, Y. Y. S., Wang, J., and Wang, Y. (2019). Herapeutic effect of Jiadanzhi Xiaoyao Powder on post-stroke depression. Heilongjiang J. Traditional Chin. Med. 48 (6), 132–133. CNKI:SUN:HLZY.0.2019-06-097.
Yu, C. Y. M., and Wang, S. (2012). Clinical observation of Xiaoyao Pill in treating 80 cases of diabetes mellitus complicated with depression. Strait Pharm. J. 24 (7), 120–121. doi:10.3969/j.issn.1006-3765.2012.07.059
Yu, H. S. B., and Tang, X. Y. (2018). Clinical analysis on Chaihu Longgu Muli decoction in the treatment of depression after tumor chemotherapy. Chin. Med. Mod. Distance Educ. China 16 (3), 55–56. doi:10.3969/j.issn.1672-2779.2018.03.026
Yu, W. Y. W. H., and Zhao, L. X. (2010). Clinical study of Yangxuenao Granule and Delisin in the treatment of post-stroke depression. Shaanxi J. Traditional Chin. Med. 31 (10), 1316–1317. doi:10.3969/j.issn.1000-7369.2010.10.029
Yu, Y. L. Y. G., and Zhang, Y. Q. (2017). Clinical study of Shugan Jieyu Capsule in treating mild and moderate senile depression. Clin. Educ. General Pract. 15 (1), 77–79. doi:10.13558/j.cnki.issn1672-3686.2017.01.024
Zhan, D. H. Z. S., and Wang, T. (2010). Treatment of 40 cases of mild depression with Wuling capsule. Her. Med. 29 (8), 1032–1033. doi:10.3870/yydb.2010.08.020
Zhang, D. Y. X. Y., and Tian, X. (2012). Comparative study of Shugan Jieyu Capsule and paroxetine in the treatment of mild and moderate depression patients. J. Clin. Psychiatry 22 (4), 288.
Zhang, G. W. D. X., and Gan, S. Y. (2020). Effect of Chaihu and Keel oyster decoction on post-stroke depression and its influence on neurological function. Clin. Res. 28 (6), 129–132. CNKI:SUN:LCYN.0.2020-06-070.
Zhang, H. C. L. W., and Gu, F. (2010). Observation on curative effect of Wuling capsule to treat post-stroke depression. J. Clin. Neurology 27 (8), 61–63.
Zhang, J. H., Xin, H. L., Xu, Y. M., Shen, Y., He, Y. Q., Hsien, Y., et al. (2018). Morinda officinalis How. - a comprehensive review of traditional uses, phytochemistry and pharmacology. J. Ethnopharmacol. 213, 230–255. eng. Epub 2017/11/12. Cited in: Pubmed; PMID 29126988. doi:10.1016/j.jep.2017.10.028
Zhang, J. W. J., and Li, P. (2015). Clinical study of morinda officinalis oligose capsule in the treatment of depression: shanxi taiyuan. Shanxi, China, Shanxi Medical University, 1–15.
Zhang, J. W. L. J., and Ji, B. (2021). Clinical observation of Xiaoyao Powder for type 2 diabetes with comorbid depression of liver spleen deficiency type. Hebei J. Traditional Chin. Med. 43 (12), 1979–1983. doi:10.3969/j.issn.1002-2619.2021.12.010
Zhang, K. L. T., and Zhou, L. (2018). To explore the clinical effect of Chaihu Shugan Decoction in treating depression caused by cerebrovascular disease. China Health Care and Nutr. 28 (29), 127. doi:10.3969/j.issn.1004-7484.2018.29.170
Zhang, M. X. W., and Tian, X. (2008). Clinical observation of Danzhi Xiaoyao Powder in treating diabetes mellitus with depression. J. Liaoning Univ. Traditional Chin. Med. 10 (2), 108–109. doi:10.3969/j.issn.1673-842X.2008.02.063
Zhang, Q. C. Z., and Bai, X. (2019). Effect of Chaihu and Keel oyster soup on patients with depression after chemotherapy for malignant tumor. Clin. Res. 27 (4), 133–134. doi:10.3969/j.issn.1004-8650.2019.04.074
Zhang, R. Z. S., and Zhang, T. (2016). Clinical observation of radix bupleuri add keel oyster granules in treating post-stroke depression. Clin. J. Traditional Chin. Med. 28 (11), 1606–1610. doi:10.16448/j.cjtcm.2016.0565
Zhang, X., Kang, D., Zhang, L., and Peng, L. (2014). Shuganjieyu capsule for major depressive disorder (MDD) in adults: a systematic review. Aging and Ment. health 18 (8), 941–953. eng. Epub 2014/04/05Cited in: Pubmed; PMID 24697344. doi:10.1080/13607863.2014.899975
Zhang, X. J. W. J., and Zhang, X. (2009). Effect of Chaihu and keel oyster decoction on depression after stroke. Chin. J. Inf. Traditional Chin. Med. 16 (4), 72. doi:10.3969/j.issn.1005-5304.2009.04.036
Zhang, X. L. Y., and Yan, Z. (2020). Comparative study of Shugan Jieyu Capsules and Sertraline in treatment of mild and moderate depression in the elderly. China Med. Her. 17 (32), 116–119.
Zhang, Y. Q. G. J., and Tang, L. (2012). “Clinical comparative study of Shugan Jieyu capsule in treating mild and moderate senile depression,” in Proceedings of the 11th Annual Conference of Mental Diseases Professional Committee of Chinese Association of Integrated Traditional and Western Medicine, Beijing, china, August 2012, 271–275.
Zhao, D. W. F., and Hu, J. B. (2011). Effect of yangxuenao Granule on post-stroke depression. Chin. J. Pract. Nerv. Dis. 14 (13), 71–72. doi:10.3969/j.issn.1673-5110.2011.13.044
Zhao, H. C. Y., and Zhang, H. (2021). Effect of XingnaoJieyu Decoction on post-stroke depression and its influence on serum NE and 5-HT levels. Chin. Archives Traditional Chin. Med. 39 (11), 202–205. doi:10.13193/j.issn.1673-7717.2021.11.047
Zhao, J. P. L. H., and Wang, J. J. (2011). A comparative study of Ganjieyu Capsule and fluoxetine in the treatment of depression. J. Chengde Med. Coll. 28 (1), 94–95. doi:10.3969/j.issn.1004-6879.2011.01.057
Zhao, S. Q. J. L., and Zhao, P. (2012). Clinical observation of modified Ganmai Dazao Decoction in treating depression. Clin. J. Traditional Chin. Med. 24 (8), 731–733. CNKI:SUN:AHLC.0.2012-08-022.
Zhen, K., Shi, H., Zhang, X., Liu, X., Li, W., Si, G., et al. (2022). Efficacy and safety of Buyang Huanwu Decoction in the treatment of post-stroke depression: a systematic review and meta-analysis of 15 randomized controlled trials. Front. neurology 13, 981476. eng. Epub 2022/11/22. Cited in: Pubmed; PMID 36408491. doi:10.3389/fneur.2022.981476
Zheng, W., Zhang, Y. F., Zhong, H. Q., Mai, S. M., Yang, X. H., and Xiang, Y. T. (2016). Wuling capsule for major depressive disorder: a meta-analysis of randomised controlled trials. East Asian archives psychiatry official J. 26 (3), 87–97. eng. Epub 2016/10/06. Cited in: Pubmed; PMID 27703096.
Zhou, D. Y. C. J., and Bao, L. (2010). A comparative study of Wuling Capsule and paroxetine in the treatment of mild to moderate depression after cerebral apoplexy. Chin. Tradit. Pat. Med. 32 (1), 186–188. doi:10.3969/j.issn.1001-1528.2010.02.006
Zhou, J. L. Y. Y., and Wang, J. M. (2005). Effect of bupleurum shugan powder on post-stroke depression. Clin. J. Chin. Med. 17 (4), 2. doi:10.3969/j.issn.1672-7134.2005.04.010
Zhou, L. Y. Z. W., and Xiao, T. (2015). Therapeutic effect of Jieyu pills on 100 patients with type 2 diabetes mellitus complicated with depression. Chin. J. Traditional Med. Sci. Technol. 22 (1), 85–87.
Zhou, X. Y. Q. X., and Geng, X. F. (2009). Clinical observation of Ganmai Dazao Decoction in treating 30 cases of post-stroke depression. J. Sichuan Traditional Chin. Med. (10), 75–76. CNKI:SUN:SCZY.0.2009-10-043.
Zhu, W. J. M., and Yang, T. (2005). Clinical observation of Jieyu Huoxue Decoction in treatment of post-stroke depression. Chin. J. Basic Med. Traditional Chin. Med. 11 (3), 230–231. doi:10.3969/j.issn.1006-3250.2005.03.029
Keywords: bayesian network meta-analysis, Chinese herbal medicine, depression, treatment, antidepressant
Citation: Dang C, Wang Q, Li Q, Xiong Y and Lu Y (2024) Chinese herbal medicines for the treatment of depression: a systematic review and network meta-analysis. Front. Pharmacol. 15:1295564. doi: 10.3389/fphar.2024.1295564
Received: 16 September 2023; Accepted: 11 March 2024;
Published: 03 April 2024.
Edited by:
Anna Tabęcka-Łonczynska, University of Information Technology and Management in Rzeszow, PolandReviewed by:
Kamila Rybczyńska-Tkaczyk, University of Life Sciences of Lublin, PolandPrzemyslaw Solek, Medical University of Lublin, Poland
Copyright © 2024 Dang, Wang, Li, Xiong and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yaoheng Lu, bHloOTNAY2R1dGNtLmVkdS5jbg==; Ying Xiong, NjE3MTE0NDVAcXEuY29t
 Chun Dang
Chun Dang Qinxuan Wang
Qinxuan Wang Qian Li
Qian Li Ying Xiong
Ying Xiong Yaoheng Lu
Yaoheng Lu