- 1 Université de Lyon, Lyon, France
- 2 Université Lyon 1, Lyon, France
- 3 EA4615, Centre Hospitalier Le Vinatier, Bron, France
Objectives: Repetitive transcranial magnetic stimulation (rTMS) seems to be effective as an antidepressant, however, some confusion remains about the best parameters to apply and the efficacy of its association with pharmacological antidepressant treatments. Method: In a single blind randomized study 14 patients with unipolar resistant depression to one antidepressant treatment were enrolled to receive, in combination with venlafaxine (150 mg), either 20 sessions of 10 Hz rTMS (2000 pulses per session) applied over the left dorsolateral prefrontal cortex (DLPFC) or 20 sessions of 1 Hz rTMS (120 stimulations per sessions) applied over the right DLPFC. Results: A similar antidepressant effect was observed in both groups with a comparable antidepressant delay of action (2 weeks) and a comparable number of responders (MADRS < 15) after 4 weeks of daily rTMS sessions (66 vs 50%). Conclusion: Low- and high- frequency rTMS seems to be effective as an add-on treatment to venlafaxine as monotherapy in pharmacological refractory major depression (stage 1). Due to its short duration (one session of 1 Hz rTMS lasts 4 min vs 16 for 10 Hz rTMS) and its safety, low frequency rTMS may be a useful alternative treatment for patients with refractory depression.
Introduction
Depression constitutes a major public health concern with a considerably high level of morbidity and mortality. Although antidepressant (AD) treatments have demonstrated their efficiency, a substantial number of depressed patients (50–60%) respond only partially or not at all to at least one trial of an antidepressant medication (Steffens et al., 1997) and close to 20% of these patients are refractory to any antidepressant medication (Fava, 2003). Moreover, the clinical utility of antidepressant drugs is impaired by the delay in onset of their therapeutic action.
Most of recent studies as well as meta-analysis support an antidepressant effect of high frequency (HF) repetitive transcranial magnetic stimulation (rTMS) applied to the left dorsolateral prefrontal cortex (LDLPFC; George et al., 2010; for review: Brunelin et al., 2007). However there remains some confusion about the best beneficial stimulation site to target as well as the best parameters to apply. While the impact of starting a combination between rTMS and an AD at the same time is still poorly studied, some authors support the hypothesis that this association could shorten the AD treatment delay of action (Poulet et al., 2004; Rumi et al., 2005). On the other hand, there is growing evidence that HF LDLPFC is as effective as low frequency (LF) rTMS applied to the right DLPFC (RDLPFC) in the treatment of depressive episode (Höppner et al., 2003; Isenberg et al., 2005; Stern et al., 2007; Fitzgerald et al., 2009; Pallanti et al., 2010; Rossini et al., 2010).
We report here results from a pilot single blind double arms controlled study investigating the antidepressant effect, in association with venlafaxine, of active HF (10 Hz) LDLPFC rTMS compared to active LF (1 Hz) LDLPFC rTMS (150 mg) in patient with refractory depressive symptoms.
Materials and Methods
Sixteen patients with unipolar major depression according to DSM IV were included through clinical and MINI evaluation (Mini version 4.4). All of them gave their written informed consent before entering the study which was approved by a regional ethical committee. They were aged between 18 and 65 and have not tried venlafaxine for the present depression episode. Patients were recruited at the “Le vinatier” Hospital. At inclusion, all of them present a Montgomery and Asberg (1979) Depression Rating Scale (MADRS) score >20 despite the prescription of an AD at efficient dose for at least 12 weeks. Patients respond to stage 1 of treatment-resistant depression as described in Fava (2003).
Prospective patients were screened for contraindications to rTMS, including a history of personal or family seizures, neurological or neurosurgical antecedent, inner ear prosthesis, pacemaker, and anticonvulsive medication. Electroencephalographic and clinical examination was made before the first rTMS sequence.
Participants were randomly allocated into two groups after 2 weeks of wash out period for all medications. Venlafaxine (75 mg/day) administration as monotherapy began 3 days before the start of rTMS treatment. The day of the first rTMS session, venlafaxine was increased to 150 mg on the morning. Then, one group was treated with venlafaxine and HF-rTMS applied over the LDLPFC and the second group was treated with venlafaxine and LF-rTMS applied over the RDLPFC.
Stimulations were carried out using a MagPro 100 (Medtronic–Boulogne–France) stimulator system using figure-eight 70-mm coils. Stimulation intensity was 100% of resting motor threshold. Motor threshold was identified as the minimum magnetic field strength required to produce left thenar muscle activation by single transcranial magnetic pulses delivered to the motor cortex for at least 5 of 10 trials. Coil placement was 5 cm anterior from motor cortex (international 10–20 system). Because two patients withdrew their consent before the start of the trial, the final groups were:
– High-frequency group (n = 6): Stimulation frequency was 10 Hz. Each patient received 10, 15, or 20 rTMS sessions depending on the response rate after 10 sessions, one session per day (2 or 4 weeks). Each daily session consisted in a total of 2000 pulses 40 trains of 5 s duration and 30 s intertrain intervals.
– Low frequency group (n = 8): Stimulation frequency was 1 Hz. Each patient received 10, 15, or 20 rTMS sessions depending on the response rate after 10 sessions, one session per day (2 or 4 weeks). Each daily session consisted in a total of 120 pulses of 2 trains of 60 s duration and 120 s intertrain intervals.
A psychiatrist blind to group assignment conducted all assessments of patients’ symptoms. To assess antidepressant effects, we used the 10-items MADRS. We measured MADRS scores at baseline, after 5, 10, 15, and 20 rTMS sessions. Patients who were responders after the first 10 or 15 rTMS sessions (defined as MADRS score <15) did not received more rTMS sessions.
Analysis
Comparisons between groups at baseline were assessed using student t-tests except for gender (Fischer’s chi-square). Statistical analysis was performed at a significant threshold of 0.05 using a repeated measures analysis of variance (ANOVA) on MADRS scores at each assessment times. Number of responders was compared between the groups using Fischer’s chi-square test. Statistics were done using the Statistica software.
Results
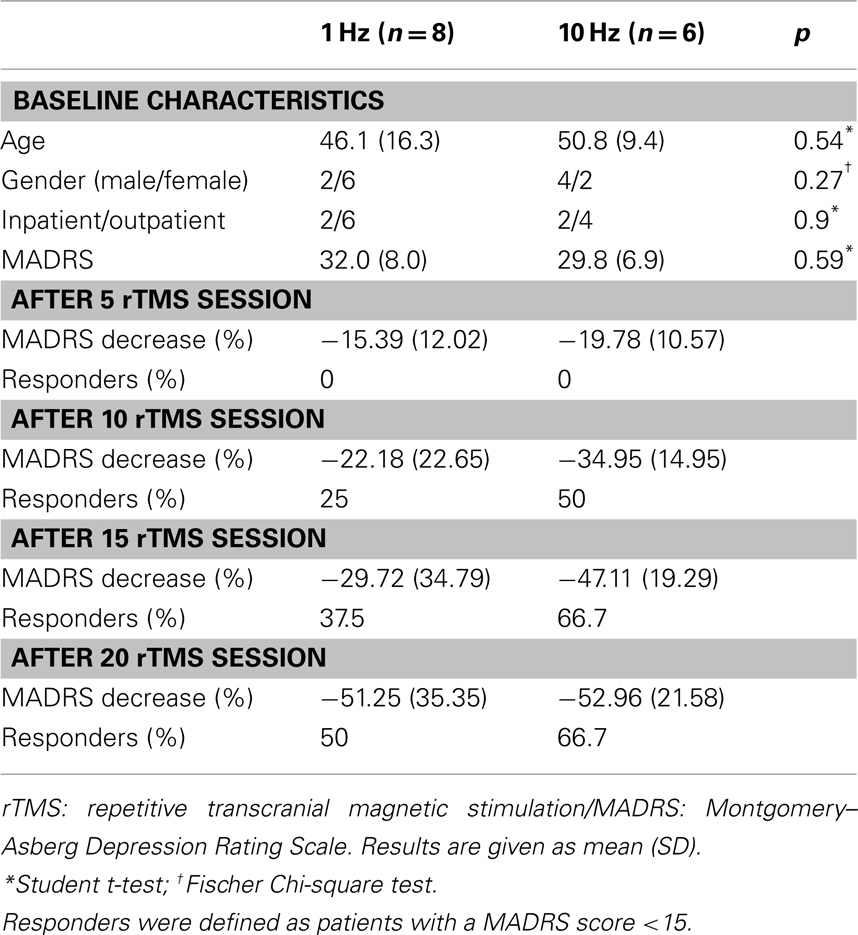
At baseline, the two groups did not significantly differ for age, sex ratio, and for MADRS scores (Table 1). No adverse event was observed in both groups.
Number of responders did not differ in each group at each assessment (χ2 = 0.4; dl = 1; p = 0.57). First responders (MADRS < 15) were observed after 10 rTMS session in both groups (Table 1). More than 50% of patients were responders at the end of the study period (4 weeks).
Effect of treatment (time) was significant in both group [F(4,44) = 15.42; p < 10−7]. No significant statistical difference was observed for MADRS scores between the two groups [F(1,11) = 0.32; p = 0.58]. We reported no interaction between group (HF or LF) and time [F(4,44) = 0.61; p = 0.66], suggesting that decreases of MADRS scores were comparable in both groups (Figure 1).
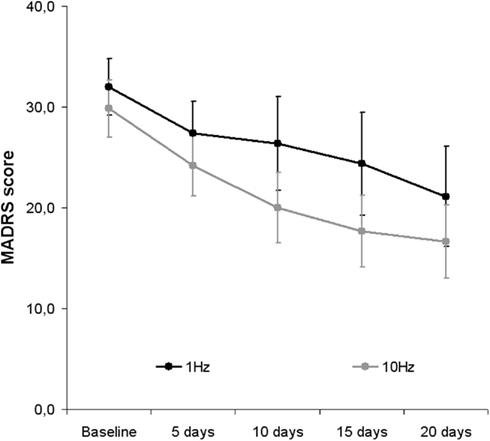
Figure 1. Changes in MADRS scores following rTMS sessions in combination with venlafaxine (150 mg) in both groups: 1 Hz applied over the right dorsolateral prefrontal cortex (DLPFC)/10 Hz applied over the left DLPFC. rTMS: repetitive transcranial magnetic stimulation/MADRS: Montgomery–Asberg Depression Rating Scale Results are given as mean and SE.
Discussion
Our results replicate and extend previous findings showing that DLPFC LF-rTMS administered on the right side results in a similar effect compared to left-sided DLPFC HF-rTMS (Höppner et al., 2003; Isenberg et al., 2005; Stern et al., 2007; Fitzgerald et al., 2009; Pallanti et al., 2010; Rossini et al., 2010). Despite a failure in response to one previous AD, we reported that some patients could be considered as responders only 2 weeks after the start of treatment and after 4 weeks, more than a half of group could be qualified as responders as defined by a MADRS score <15.
In combination with venlafaxine (150 mg/day), 120 pulses/session of LF-rTMS over the RDLPFC (delivered during 4 min) could be as effective as 2000 pulses/session of HF-rTMS over the left DLPFC (delivered during 16 min). As the most serious potential side effect of rTMS is seizure, and that LF-rTMS may be protective against it (Theodore et al., 2002), thus, more than saving the user and patient time, LF-rTMS should be a treatment of choice for patients.
We have observed no relapse during the study period (4 weeks) but a follow up period is required before any conclusion on this point. We reported no adverse events in the combination of medication.
The lack of an arm with placebo venlafaxine in association with active rTMS and of an arm with active venlafaxine and sham rTMS are some limitations of our study. However, it has been reported that 1 Hz rTMS is as effective as venlafaxine in the treatment of resistant depression (Bares et al., 2009). Moreover, it is important to note that in a large randomized controlled trial using venlafaxine alone (Rush et al., 2006), with a demographic comparable depressed group, among the patients who had a remission (24.8% of the sample), the mean time to remission was 5.5 ± 4.7 weeks (median, 4.2). We reported more than 50% decrease of MADRS score after 4 weeks of treatment while a 30% decrease of HDRS was reported in a large study investigating the impact of venlafaxine after previous AD failure (Baldomero et al., 2005). On the other hand, as it seems to be the case in our results, Rumi et al. (2005) have reported that in add-on therapy rTMS may be able to accelerate the delay efficacy of AD.
In conclusion, although limited by small sample size and lack of venlafaxine placebo arm, in a sample of patients who have not responded to one trial of antidepressant medication, in combination with venlafaxine 150 mg/day, right-sided LF-rTMS seems as effective as left-sided HF-rTMS. In order to investigate the real impact of LF-rTMS without any antidepressant treatment compared to rTMS in add-on therapy with venlafaxine and to venlafaxine alone, we have started a large multicentric study (clinicaltrials.gov; NCT00714090).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This work was supported by the Conseil Scientifique de la Recherche (CSR), CH le Vinatier. Mondino Marine held a doctoral fellowship from la Région Rhône-Alpes.
References
Baldomero, E. B., Ubago, J. G., Cercós, C. L., Ruiloba, J. V., Calvo, C. G., and López, R. P. (2005). Venlafaxine extended release versus conventional antidepressants in the remission of depressive disorders after previous antidepressant failure: ARGOS study. Depress. Anxiety 22, 68–76.
Bares, M., Kopecek, M., Novak, T., Stopkova, P., Sos, P., Kozeny, J., Brunovsky, M., and Höschl, C. (2009). Low frequency (1-Hz), right prefrontal repetitive transcranial magnetic stimulation (rTMS) compared with venlafaxine ER in the treatment of resistant depression: a double-blind, single-centre, randomized study. J. Affect. Disord. 118, 94–100.
Brunelin, J., Poulet, E., Boeuve, C., Zeroug-Vial, H., D’Amato, T., and Saoud, M. (2007). Efficacy of repetitive transcranial magnetic stimulation (rTMS) in major depression. Encephale 33, 126–134.
Fava, M. (2003). Diagnosis and definition of treatment-resistant depression. Biol. Psychiatry 53, 649–659.
Fitzgerald, P. B., Hoy, K., Daskalakis, Z. J., and Kulkarni, J. (2009). A randomized trial of the anti-depressant effects of low- and high-frequency transcranial magnetic stimulation in treatment-resistant depression. Depress. Anxiety 26, 229–234.
George, M. S., Lisanby, S. H., Avery, D., McDonald, W. M., Durkalski, V., Pavlicova, M., Anderson, B., Nahas, Z., Bulow, P., Zarkowski, P., Holtzheimer, P. E. III, Schwartz, T., and Sackeim, H. A. (2010). Daily left prefrontal transcranial magnetic stimulation therapy for major depressive disorder: a sham-controlled randomized trial. Arch. Gen. Psychiatry 67, 507–516.
Höppner, J., Schulz, M., Irmisch, G., Mau, R., Schläfke, D., and Richter, J. (2003). Antidepressant efficacy of two different rTMS procedures. High frequency over left versus low frequency over right prefrontal cortex compared with sham stimulation. Eur. Arch. Psychiatry Clin. Neurosci. 253, 103–109.
Isenberg, K., Downs, D., Pierce, K., Svarakic, D., Garcia, K., Jarvis, M., North, C., and Kormos, T. C. (2005). Low frequency rTMS stimulation of the right frontal cortex is as effective as high frequency rTMS stimulation of the left frontal cortex for antidepressant-free, treatment-resistant depressed patients. Ann. Clin. Psychiatry 17, 153–159.
Montgomery, S. A., and Asberg, M. (1979). A new depression scale designed to be sensitive to change. Br. J. Psychiatry 134, 383–389.
Pallanti, S., Bernardi, S., Di Rollo, A., Antonini, S., and Quercioli, L. (2010). Unilateral low frequency versus sequential bilateral repetitive transcranial magnetic stimulation: is simpler better for treatment of resistant depression? Neuroscience 167, 323–328.
Poulet, E., Brunelin, J., Boeuve, C., Lerond, J., D’Amato, T., Dalery, J., and Saoud, M. (2004). Repetitive transcranial magnetic stimulation does not potentiate antidepressant treatment. Eur. Psychiatry 19, 382–383.
Rossini, D., Lucca, A., Magri, L., Malaguti, A., Smeraldi, E., Colombo, C., and Zanardi, R. (2010). A symptom-specific analysis of the effect of high-frequency left or low-frequency right transcranial magnetic stimulation over the dorsolateral prefrontal cortex in major depression. Neuropsychobiology 62, 91–97.
Rumi, D. O., Gattaz, W. F., Rigonatti, S. P., Rosa, M. A., Fregni, F., Rosa, M. O., Mansur, C., Myczkowski, M. L., Moreno, R. A., and Marcolin, M. A. (2005). Transcranial magnetic stimulation accelerates the antidepressant effect of amitriptyline in severe depression: a double-blind placebo-controlled study. Biol. Psychiatry 57, 162–126.
Rush, A. J., Trivedi, M. H., Wisniewski, S. R., Stewart, J. W., Nierenberg, A. A., Thase, M. E., Ritz, L., Biggs, M. M., Warden, D., Luther, J. F., Shores-Wilson, K., Niederehe, G., and Fava, M., for the STAR*D Study Team. (2006). Bupropion-SR, sertraline, or venlafaxine-XR after failure of SSRIs for depression. N. Engl. J. Med. 354, 1231–1242.
Steffens, D. C., Krishnan, K. R., and Helms, M. J. (1997). Are SSRIs better than TCAs? Comparison of SSRIs and TCAs: a meta-analysis. Depress. Anxiety 6, 10–18.
Stern, W. M., Tormos, J. M., Press, D. Z., Pearlman, C., and Pascual-Leone, A. (2007). Antidepressant effects of high and low frequency repetitive transcranial magnetic stimulation to the dorsolateral prefrontal cortex: a double-blind, randomized, placebo-controlled trial. J. Neuropsychiatry Clin. Neurosci. 19, 179–186.
Keywords: transcranial magnetic stimulation, dorsolateral prefrontal cortex, rTMS, venlafaxine, depression
Citation: Eche J, Mondino M, Haesebaert F, Saoud M, Poulet E and Brunelin J (2012) Low- vs high-frequency repetitive transcranial magnetic stimulation as an add-on treatment for refractory depression. Front. Psychiatry 3:13. doi: 10.3389/fpsyt.2012.00013
Received: 31 October 2011; Accepted: 12 February 2012;
Published online: 07 March 2012.
Edited by:
William McDonald, Emory University School of Medicine, USAReviewed by:
Christopher A. Wall, Mayo Clinic, USAWonnei Caumo, Universidade Federal do Rio Grande do Sul, Brazil
Copyright: © 2012 Eche, Mondino, Haesebaert, Saoud, Poulet and Brunelin. This is an open-access article distributed under the terms of the Creative Commons Attribution Non Commercial License, which permits non-commercial use, distribution, and reproduction in other forums, provided the original authors and source are credited.
*Correspondence: Jerome Brunelin, EA 4615, Pôle EST, Centre Hospitalier Le Vinatier, 95 Boulevard Pinel, 69 677 Bron Cedex, France. e-mail:amVyb21lLmJydW5lbGluQGNoLWxlLXZpbmF0aWVyLmZy


 Frederic Haesebaert1,2,3
Frederic Haesebaert1,2,3