- 1Department of Psychiatric Rehabilitation and Counseling Professions, Rutgers University, Scotch Plains, NJ, United States
- 2Center for Psychiatric Rehabilitation, Sargent College of Health and Rehabilitation Sciences, Boston University, Boston, MA, United States
- 3Department of Psychiatry, Dartmouth Medical School, Hanover, NH, United States
- 4Dartmouth Trauma Intervention Research Center, Lebanon, NH, United States
- 5Department of Psychology, John Jay College of Criminal Justice, CUNY, New York, NY, United States
The current study aimed to evaluate the potentially traumatic aspects of psychotic symptoms and psychiatric treatment of psychosis using qualitative methods. Participants included 63 people with first episode psychosis or multiple psychotic episodes recruited from an inpatient psychiatric unit and an urban state psychiatric hospital in the North East region of the United States. Quasi-structured interviews were used to explore those aspects of symptoms and treatment that were perceived as traumatic Emotional reactions to the most traumatic aspect of symptoms and treatment, during and after the event, were also examined. Participants described a number of traumatogenic aspects of psychotic symptoms, including frightening hallucinations; suicidal thought/attempts, thoughts/attempts to hurt others; paranoia/delusions and bizarre/disorganized behavior or catatonia. Traumatic aspects of psychosis elicited emotions including anger, sadness and confusion, anxiety, and numbness at the time of event. Furthermore, many participants found aspects of treatment to be traumatic, including: being forced to stay in the hospital for a long time; experiencing upsetting side-effects; coercive treatments, including involuntary hospitalization, use of restraints, and forced medication; being exposed to aggressive patients; and mistreatment by professionals. These experiences elicited emotions of anger, sadness, distrust, and a sense of helplessness. Study findings suggest that the experiences both of psychotic symptoms and psychiatric treatment, potentially traumatic, can be a powerful barrier to engaging people in mental health services and facilitating recovery. Clinical implications were discussed.
Introduction
The emergence of a psychotic disorder can be a devastating event for an individual, with major impact on perception of self, self-esteem, and ability to function adequately (1). Psychotic symptoms and treatment experiences can lead to posttraumatic stress disorder (PTSD) symptoms similar to those observed in individuals who have experienced traumatic events such as disasters and rape (2–4). Psychotic symptoms such as command hallucinations to hurt self or others, persecutory delusions, or disorganized behavior can be frightening (2, 4–6). Coercive interventions, such as involuntary hospitalization, seclusion/restraint, and being forced to take medication can be further traumatizing (7–10). These aspects of psychotic episodes are often perceived as threatening and can lead to feelings of fear, helplessness, or horror (4, 11).
The literature regarding psychological reactions to psychosis and its treatment has emphasized both post-psychotic depression and post-psychotic, PTSD symptoms (2, 12, 13). In fact, PTSD is now considered by some as a secondary psychiatric morbidity following psychosis (2). Over 20 years ago, Shaner and Eth (14) reported a case study of a person who developed symptoms, following a schizophrenic episode, that were consistent with PTSD. These symptoms included re-experiencing the traumatic event(s), avoidance of trauma-related stimuli, and over-arousal. Since then, over 17 studies have reported high rates of post-psychotic PTSD symptoms related to these experiences. These 17 studies have included 760 participants, primarily composed of non-affective psychotic disorders (2, 6, 10, 11, 15–27). Using a variety of assessment methods among inpatients and outpatients with psychosis, participants have been asked to respond to the questions based on their reactions toward potentially frightening psychotic symptoms and/or treatment experiences (i.e., negative aspects of treatment). When excluding consideration of whether psychotic or treatment experiences met criterion A for PTSD as defined by DSM-IV, symptoms consistent with a diagnosis of PTSD have been found in 11–67% of the samples, with an average rate of 46%. In addition to traumatic reactions similar to PTSD, depression, suicidality, and low self-esteem are common negative emotional reactions after a psychotic episode.
Post-psychotic depression has been well documented in studies conducted in England (12, 22, 28, 29). It has been found that 36% of patients develop depression following a psychotic episode (12). Depression is common in patients with a first episode psychosis (FEP). Reported prevalence rates varied from 17 to 83% in the different studies (30–33, 34). Relevant studies have generally found that, as treatment progressed, rates of depression decreased. For example, in a sample of 198 Norwegian clients with FEP, 50% of the participants were depressed at the start of treatment, while 35% exhibited depression at one year follow-up after treatment (34). Upon becoming depressed, patients with post-psychotic depression developed lower self-esteem and a worsening of their appraisals of psychosis (35). Additionally, the lifetime risk of suicide in psychotic illness remains high at approximately 7% (29, 36). Suicide risk is highest in the early phases of psychosis (31, 36–39). Upthegrove et al. (36) conducted a study among persons with a first episode of psychosis and found frequent suicidal acts such as overdosing and attempted hanging in this group. Reactions toward psychosis and its treatment are further compounded by the effects of being labeled with a mental illness, rejection and the internalization, acceptance, and resignation to societal stigma toward mental illness (40, 41). Individuals early in the course of psychosis frequently avoid professional help because of concerns about stigma (42), and the negative effects of the internalization of stigma on functioning and well-being have been well-documented [e.g., Ref. (43)].
In the study of psychosis and trauma, there has been significant evidence documenting increased trauma exposure in psychosis and schizophrenia (44–46). Trauma exposure is common among patients with psychosis ranging from 49 to 100% [see, Ref. (46) for a review]: childhood sexual abuse reported by 13 to 64%, childhood physical abuse by 22 to 66%, adulthood sexual assault by 13 to 79%, and adulthood physical assault by 30 to 87% of persons with serious mental illness. Multiple traumatization is common with 75 to 98% of participants report multiple trauma [see, Ref. (46) for a review]. Among 962 participants with psychosis, 17.9% of their sample reported criminal victimization in the past year (47). PTSD is common as a result of trauma exposure among people with psychosis. The current rate of PTSD has been reported as between 25 and 48% in this population in various studies [see, Ref. (46) for a review], nearly ten times higher than that of the general population (48). These traumatic life events, along with the traumatic experience of psychotic episodes and psychiatric treatment, have drawn attention to the need for treatments to reduce the consequences of trauma in this population (49).
Although quantitative literature has documented psychological reactions toward psychosis and its treatment, research is less clear about how psychotic symptoms or coercive treatment experiences are perceived by persons with psychosis. Qualitative research methods are a promising strategy for understanding subjective experience and offering suggestions for potentially useful treatment approaches (42, 50, 51). However, few qualitative inquiries have investigated the subjective experiences of reactions toward psychosis and its treatment.
The current study aimed to evaluate subjective experiences related to psychotic symptoms and treatment in clients with multiple psychotic episodes using qualitative methods. Aspects of symptoms and treatment that were perceived as traumatic, as well as emotional reactions to the most traumatic aspect of symptoms and treatment, were explored.
Materials and Methods
The current investigation is part of a study evaluating prevalence of PTSD symptoms in FEP or multi-episode participants with psychosis (6, 10). The study was conducted at an inpatient psychiatric unit at a general hospital affiliated with a medical school in North East region as well as an urban state hospital which included both acute inpatient care, as well as intermediate and longer-term treatment. Treatment team members (attending psychiatrists, psychologists, and nurses) were informed about the study and eligibility criteria and then identified potentially eligible participants and referred them to the study team. An important question addressed in the study was the importance of the A1/A2 criteria for traumatic event in diagnosing PTSD related to a psychotic episode. For this reason, we chose to assess participants as soon as possible after the symptoms of their episode had been stabilized to enhance the accuracy of their perceptions and emotional reactions during the index events. Participants were referred to the study after they were judged to be symptomatically stable by their treatment team, and able to provide consent. All of the study procedures were approved of by the appropriate university and hospital Institutional Review Boards.
Participants
Inclusion criteria for participation in the study were:
(a) age 18 and above;
(b) chart or clinician diagnosis of schizophrenia, schizoaffective disorder, schizophreniform disorder, bipolar disorder with psychotic features, major depression with psychotic features, brief reactive psychosis, or unspecified psychosis;
(c) presentation for treatment of a psychotic episode within the past 6 weeks;
(d) psychotic symptoms of moderate severity or greater on any item on the Brief Psychiatric Rating Scale (52) thought disturbance subscale which includes hallucinatory behavior, unusual thought content, grandiosity, and suspiciousness persisting for at least 2 days in the absence of substance use (53).
(e) history of treatment for at least one psychotic episode including the current episode. A psychotic episode was defined as an episode in which there was the presence of one (or more) of the following symptoms: delusions, hallucinations, disorganized speech, or grossly disorganized or catatonic behavior for at least one week; and
(f) voluntary signed informed consent to participate in the study.
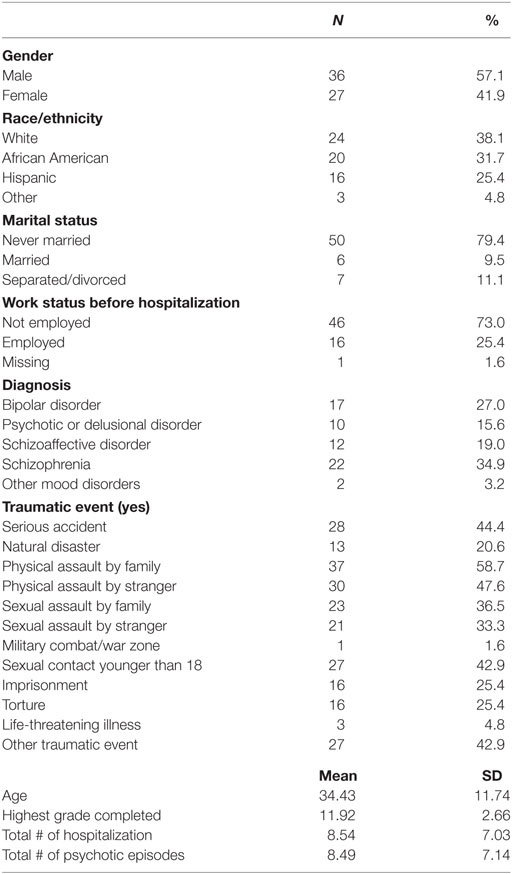
A total of 63 individuals met eligibility criteria and agreed to participate in the study. The characteristics of the study sample are summarized in Table 1. Participants tended to be in their 30s, with an average of over eight past hospitalizations, with 54% of participants were diagnosed with schizophrenia or schizoaffective disorders. A large proportion of the participants in this study were never married (76.9%), and the majority of the participants were African–American or Latino/a.
Measures
Trauma and PTSD Symptoms
Lifetime exposure to trauma (e.g., sexual assault, serious accident) was evaluated with an abbreviated version of the Traumatic Life Events Questionnaire (54) that included 12 items, each rated on a no/yes basis. After completion of the questionnaire, the participant was oriented to the assessment of psychologically traumatic events related to psychotic symptoms or treatment experiences with the following statement: “I would now like to spend a few minutes finding out about your experiences with psychiatric symptoms.” Interviewers were instructed to adopt the participant’s language when referring to psychiatric symptoms and psychiatric illnesses, such as using terms like “nervous breakdown,” “mental illness,” “stress reaction,” or “emotional upset.” A modified version of the PTSD Assessment Tool for Schizophrenia (PATS), a semi-structured interview designed to elicit posttraumatic reactions to psychosis and treatment experiences (55), was used to guide the discussion. The modified PATS was divided into two sections: reactions to psychotic symptoms; and reactions to treatment experiences. For the first section, reactions to psychotic symptoms were assessed by initially asking a series of 15 questions (e.g., “Have the symptoms of your psychiatric illness ever caused you to feel extremely anxious or terrified?” “Did you believe that groups of people wanted to hurt you?”). An affirmative response to any item was followed up by probes to elicit specific examples. After these questions, participants were asked to identify which experience across all their episodes was most distressing when they looked back on it. Additional questions were then directed at eliciting further details of the event (e.g., when and where it happened, other people who were involved) and how the person reacted to it at the time. Respondents were asked directly: “How did you respond emotionally,” and “What was that like?” Participants were also asked about their immediate and subsequent emotional reactions after the event by inquiring: “What about after the event, how did you respond emotionally?”
Reactions to treatment experiences were assessed in a similar fashion, by initially asking a series of questions (nine in total; e.g., “Have you ever been given a treatment that frightened you?” “Have you ever been forcibly taken to the hospital or to jail?”). Any affirmative response was followed up by questions to elicit specific examples. After these questions, participants were asked to identify the most distressing treatment experience, followed by asking questions aimed at understanding what happened and the person’s reactions to the event both at the time of the event and after the event.
Following the end of the qualitative-portion of the interview, standardized assessments were completed to evaluate PTSD and other symptoms, which have been previously reported (6). The qualitative portion of the interview ranged in length from 15 to 35 min. Field notes by the interviews were used to maintain a record of responses.
Procedures
Study participants were identified by the clinical treatment team. When potentially eligible patients were identified and were symptomatically stable, permission was obtained from the client for a research team member to discuss the study with them. If permission was granted, a meeting was set up between a research team member and the client, the study was explained, and if the client was interested he or she provided signed informed consent. An interview was then arranged to conduct the assessment, and a chart review was performed. Patients were paid for their participation in the study.
Analysis
The data analysis for this study was informed by grounded theory, which seeks to generate theory from a data set and is utilized to generate hypotheses (56, 57). The data analysis process in this investigation consisted of an initial open coding of the participant’s responses from the field notes into initial categories by two graduate students. Three raters reviewed the data and the initial categories. They performed axial coding and deleted or combined several of the original codes. After several iterations, a final selective coding process among reviewers which determined the core themes and concepts was implemented (56, 57). Two raters rated the responses independently using the coding theme. The differences and discrepancies were discussed and reconciled after clarifying the original coding scheme.
Results
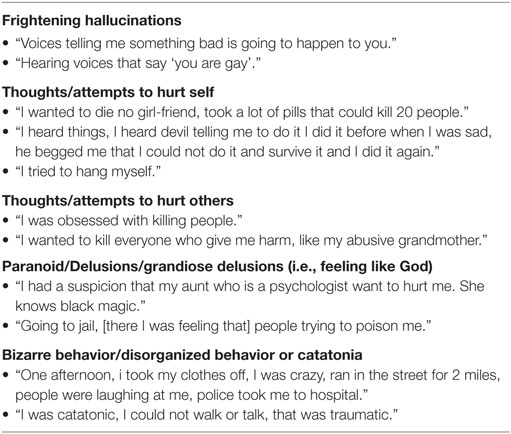
Themes specifically regarding one’s perception and emotional reactions toward psychosis and one’s encounters with the mental health system are presented here. Participants described a number of traumatogenic aspects of psychotic symptoms. Five themes concerning traumatogenic aspects of psychosis emerged (see Table 2): (1) frightening hallucinations, reported by 23.8% of the participants; (2) paranoia/delusions, reported by 20.6% of the participants; (3) suicidal thoughts/attempts, reported by 15.9% of the participants; (4) thoughts/attempts to hurt others, reported by 9.5% of the participants; (5) bizarre/disorganized behavior or catatonia; reported by 7.9% of the participants. Other categories included various themes such as flashbacks of past abuse, panic attacks, mania, loss of child custody, etc., were reported by 22.2% of the participants. The most commonly reported theme of traumatogenic aspects of psychosis was that of frightening hallucinations including command hallucinations or persistent hallucinations that last for years, followed by thought/attempts to hurt self, and next by thought/attempts to hurt others. A patient reporting a frightening hallucination (the most commonly identified trauma) is quoted below:
[The most traumatic part is] hearing voices telling me where to move. Three years ago I started to hear voices on TV and radio, telling me to move. I moved non-stop in the past two years, not finding a place to live. People on radio and TV suggest places for me to go.
Another participant described how hearing critical voices led to thoughts which led to self-harm:
I was just feeling very guilty about not being a good mother and a good wife. I just felt very bad, and did not think I should be allowed to live, so that’s when I decided that I should hurt myself.
In terms of having experienced thoughts/attempts to hurt self as the most traumatic aspect of symptoms, one participant reported, “I don’t think about killing myself but killing comes to me.” Another reported, “I tried to hang myself.” Another reported, “During [my] first breakdown, when I thought of running into traffic, [that was most traumatic.]” In terms of having experienced thoughts/attempts to hurt others as the most traumatic aspect of symptoms, one participant reported: “I was obsessed with idea of killing people.” One participant reported experiencing homicidal ideas toward her mother and found it traumatic. Participants also found paranoia/delusions the most disturbing. One reported having experienced people spying on him: “[I felt] people spying on me. It happened gradually, everybody saw signs except me.” Another reported, “I feel like I was going to die. Because my other friends will do anything for money there is a possible thing that I may die. People may set things up to get me before my birthday.” A few participants found their bizarre/disorganized behavior most traumatic. One reported great humiliation at having run through the streets naked. He stated, “One afternoon, I took my clothes off, and ran in the street for two miles. People were laughing at me. The police took me to hospital.” Another reported, “I was catatonic, I could not walk or talk, that was traumatic.”
Emotions Associated With Traumatic Aspects of Psychosis
Emotions associated with traumatic aspects of psychosis involved anger; sadness; mixed feelings such as confusion, sadness, and anger; numbness; sense of shock and anxiety (Table 3). The most commonly experienced emotion in relation to symptoms was anger (reported by 22.0% of participants), followed by shock/anxiety (reported by 18.6% of participants); mixture of the above feelings, or a mixture of sadness and anger (reported by 16.9%); sadness (reported by 15.3%); and numbness (reported by 11.9%). Other categories were reported by 15.3% of the participants. With regard to anger, one participant reported, “I felt angry, clumsy, and confused. I can’t break the spell.” One reported confusion, “I could not understand why I was doing that.” A few participants reported feeling shocked/nervous about their psychotic symptoms. One stated being horrified. Another reported feeling nervous and out of control. One participant specifically reported feeling sad at hearing voices, stating “[After hearing the voices], I was falling apart, crying, always sleeping, never wanted to go out of the house.” Not all participants reported experiencing emotions, but rather reported feeling numb toward what happened during psychosis. One stated, “I felt emotionless” after slashing wrists. Two participants reported they did not know how they felt.
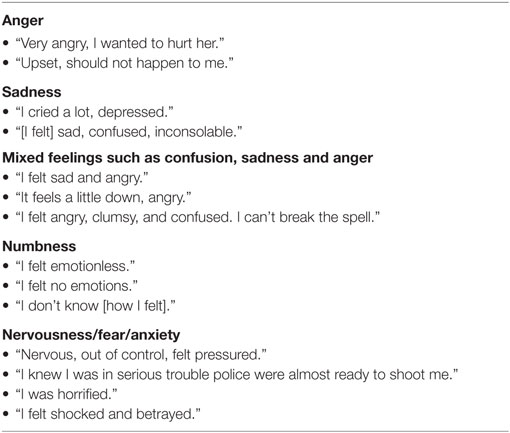
Table 3. Themes and illustrative quotations of emotional reaction to symptoms at the time of psychosis.
Descriptions of emotion looking back after the episode of psychosis involved a wider range of reactions. These involved sadness (14.5%); relief that symptoms went away (14.5% of participants reported); anxiety (12.9%); neutral feelings (11.2%); mixed emotions such as relief mixed with anxiety (9.7%); anger (9.7%); numbness (9.7%); shame (8.1%) and distrust/helplessness (8.1%). Looking back at the most traumatic aspect of psychosis, participants most commonly expressed experiencing sadness about what had happened. It was interesting that equal number of people reported feeling relieved that symptoms were lessened compared to the number of people who expressed sadness about what had happened. Some participants reported feeling neutral about what happened when looking back. Anxiety, mixed emotions, anger, numbness, shame, distrust, and helplessness were also reported by approximately 8–13% of people for each category.
Traumatogenic Aspects of Psychiatric Treatment
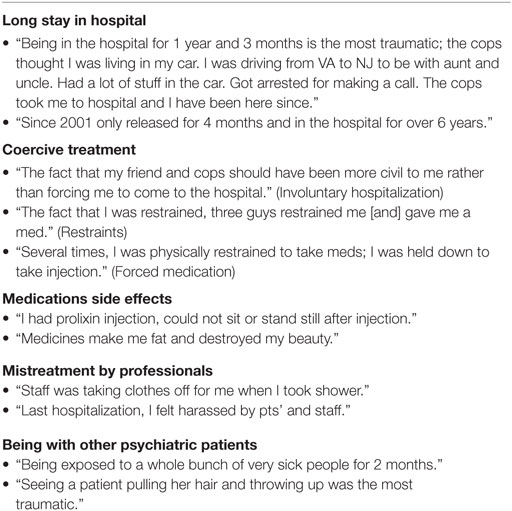
Participants described a number of traumatogenic aspects of psychiatric treatment (Table 4). Amongst the participants who experienced at least one episode of psychosis, five major themes concerning traumatogenic aspects of treatment emerged: (1) long stay in the hospital; (2) medication side effects; (3)coercive treatments, including involuntary hospitalization, use of restraints, and forced medication, and (4) being with other patients; and (5) mistreatment by professionals, not including the use of coercive treatments. The mostly commonly reported theme of traumatogenic aspects of psychiatric treatment was long stay in the hospital, reported by 25 participants (25.8%). One participant in his early 20s was in the hospital for more than 1 year for his first psychotic episode. Another reported, “Staying here for 9 months; I don’t have an apartment, my mom and I don’t get along; [I don’t have a place to go], it feels ridiculous.” Participants also indicated feeling confused about a long stay in the hospital. One person said, “I don’t understand why I am here; they say I should be here for at least 21 days, but I’ve been here for 12 years; the psychologists say I’ll be here permanently.” Another reported, “Since 2001, [I was] only released for 4 months and [I have been] in the hospital for over 6 years.”
The next most commonly reported traumatic event related to treatment was coercive treatments, reported by 14 patients (22.6%), including involuntary hospitalization, use of restraints, and forced medication. In the category of restraints, one reported, “The fact that I was restrained by three guys was the most traumatic.” In the category of involuntary hospitalization, one reported, “The fact that my friend and cops should have been more civil to me rather than forcing me. My friend called cops who hand-cuffed me, and brought me to the ER. Then they shifted me to psych ward.” In the category of forced medication, participants reported that being forced to take medication could be traumatogenic. One reported, “Having them give me Risperdal every two weeks; When I was in the quiet room, they told me if I don’t take it, then they will force me to take it—restrain me to the bed.”
Side effects of psychotropic medication were the third most commonly reported traumatic aspect of treatment (reported by 12 participants; 19.3%). One participant said, “I had Prolixin injections, [and] could not sit or stand still after injection.” Another said she passed out after taking medication. One stated, “Taking bad medications with side effects [was really traumatic]. The psychiatrist gave me a lot of milligrams of medications. After taking them, I could not walk. I felt like I was drunk. It felt like I was being poisoned by the medications.” Others reported medication side effects of weight gain, sleepiness, and fatigue as the most disturbing aspect of treatment.
Mistreatment by professionals, not including the use of coercive treatments, was reported by 14.5% of participants. One stated, “Verbal abuse by staff [was the most traumatic aspect of treatment]. They make fun of our feelings, make me behave the way I don’t want to. If I don’t keep staff happy they will drop my level like a punishment.”
Last, participants also found being exposed to other patients in the hospital, particularly aggressive patients, was traumatic. This was reported by seven participants (11.2%). One reported, “Seeing a patient pulling her hair and throwing up [was the most traumatic aspect of treatment].” Another reported, “I miss my family, I was physically assaulted by two patients, one punched me and the other squeezed my breast.” One reported, “Being exposed to a whole bunch of very sick people for two months was traumatic. At admission, they would scream, cry really loud, there were fights among the patients.”
Emotions Associated With Traumatic Aspects of Psychiatric Treatment
Participants described a wide range of emotions related to traumatic treatment experiences (Table 5). Participants frequently expressed feeling angry about their psychiatric treatment (reported by 19.0% of participants). One reported, “I got angry. [I felt] violated.” Some participants reported a mixture of feelings such as feeling upset, sad, and angry at the same time: “I got upset,” or “[I was] mad and depressed.” This was reported by 14.3% of participants. Participants commonly dealt with feelings of sadness related to psychiatric treatment (11.1% reported so). One reported, “I felt frustrated, sad, depressed.” Themes of shock, frustration, and helplessness were described by 14.3% of participants. Fear and anxiety were also experienced by 7.9% of participants. One reported, “I was scared.” Another reported, “[I was] terrified.” Feelings of distrust were reported by 6.3% of participants: “I feel paranoid, feel like things are not going to happen in my way.” Lastly, a sense of numbness was reported by 6.3% of participants.
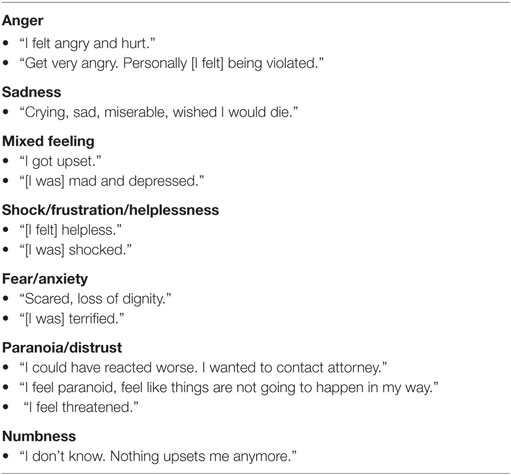
Table 5. Themes and illustrative quotations of emotional reaction to treatment at the time of event.
When asked to how they responded emotionally subsequently to the most traumatic aspect of the treatment, participants described a wider range of emotions related to traumatic treatment experiences. 10% of participants reported feeling neutral about the most traumatic aspect of treatment, when looking back; 8% reported developing a distrust of the system, while another 8% reported numbness or having no emotions after the event. 8% of participants reported feeling relieved that the worst part of treatment was over, while 7% remained sad at what happened. Another 7% of people reported feeling angry or frustrated with the treatment, while 6% of participants reported helplessness or feeling threatened. Mixed emotions or other emotions were reported by four percent of the participants. In total, approximately one-third of the participants continued to experience negative emotions such as sadness, hurt, anger, feeling violated, distrust, dislike, helplessness, or anxiety regarding treatment received.
Discussion
This study examined traumatic reactions to the experience of psychosis and associated treatment for people with FEP or multiple episodes of psychosis. It supports the conclusion of previous studies that psychosis itself, and related treatment, can both be traumatic for many people. Most of the participants reported traumatic responses related to both their psychotic symptoms and their treatment experiences, consistent with previous reports [i.e., Ref. (11, 18, 20, 21)]. Participants described a number of traumatogenic aspects of psychotic symptoms, corresponding to five themes: (1) frightening hallucinations, (2) suicidal thought/attempts, (3) thoughts/attempts to hurt others, (4) paranoia/delusions, and (5) bizarre/disorganized behavior or catatonia. Traumatic aspects of psychosis elicited emotions including anger, sadness and confusion, anxiety, and numbness. Furthermore, many participants found aspects of treatment to be traumatic, including being forced to stay in the hospital for a long time, experiencing upsetting side-effects, coercive treatments, including involuntary hospitalization, use of restraints, and forced medication, being exposed to aggressive patients, and mistreatment by professionals, and that these experiences elicited emotions such as anger, sadness, distrust, and a sense of helplessness. These findings suggest that the experiences of both symptoms and treatment as traumatic can be a powerful barrier to engaging people in mental health services and facilitating recovery.
Results document the need to address the issues related to posttraumatic reactions to psychosis in people with multiple psychotic episodes. Our findings can inform the development of treatment that is sensitive to these issues. Specifically, findings suggest the need to validate the intense and negative emotional reactions people frequently experience during a psychotic episode and during treatment episodes. Reactions following the acute psychotic episode were more varied, with a small percentage of people reported relief that the worst part was over, while others remained traumatized about what happened. Psychotherapy can be offered to clients who show evidence of posttraumatic reactions and should address these reactions through validation to alleviate traumatic reactions to psychosis. Findings on aspects of symptoms that can cause traumatogenic reactions among clients could also inform the development of treatment protocols so that patients can know what to expect when going to a psychotic episode. Clients commonly reported negative, often traumatizing treatment experiences. The damaging effects of such experiences on client’s trust of mental health professionals were evident in client interviews. Effective treatment of posttraumatic reactions to psychosis can potentially improve clients’ ability to form more collaborative relationships with treatment providers and to play a more active role in the management of their psychiatric disorder (8, 58). Emerging research addressing post-psychotic depression indicates promising results for cognitive behavior therapy (CBT) as a treatment for traumatic reactions toward psychosis (59). Jackson et al. (59) evaluated a form of CBT in reducing trauma, depression, and low self esteem following a first episode of psychosis, in a randomized controlled trial among 66 patients who had recently experienced a first episode of psychosis. CBT has also been found to be effective in reducing hopelessness, when compared to treatment as usual, among a total of 66 participants recovering from FEP (28). In a third study (60), among 22 people recovering from psychosis, those who wrote about the most stressful aspects of their illness showed fewer traumatic symptoms than those who wrote about emotionally neutral topics. Findings suggest that narrative statements disclosing the most stressful aspects of psychosis may lessen the traumatic impact of psychosis (60). Future research on focused intervention for posttraumatic reactions toward psychosis is needed.
Findings from this study underline some of the complicated issues facing the mental health service system. On one hand, participants reported being traumatized by symptoms of mental illness such as distressing auditory hallucinations, bizarre behavior, and persecutory delusions. Simultaneously participants reported being traumatized by interventions (such as involuntary hospitalization, restraints, and forced medication) designed to alleviate these symptoms. However, in many cases, participants experienced these interventions as humiliating or violations of self. Trauma informed care (61) may offer alternatives to restraints and seclusion. Newer models of treatment that place an emphasis on “shared-decision making,” such as the Open Dialog Model (62), have been recommended for people experiencing a first psychotic episode, but our findings suggest that these approaches may need to be offered for persons experiencing multiple psychotic episodes as well. Shared-decision making in medication management, which emphasizes “partnership between two experts: the client and the practitioner,” provides a model for the client to “assess a treatment’s advantages and disadvantages” in medication management [Ref. (63), p. 1636]. Commonground, a web-based application of shared decision making model, encourages the use of resilient self-care strategy in addition to the use of psychotropic medication. It has been found that when CommonGround is implemented, the use of self-management strategies among clients correlated with less concerns about medication side effect, increased perception that medicines were helping, and improved recovery (64). CommonGround has been implemented successfully in community mental health centers (65) while its implementation in psychiatric hospitals has not been reported in the literature. The adoption of shared decision model may reduce traumatic reactions during treatment and foster better trust between providers and clients.
The limitations of this study include sampling issues and the retrospective nature of the data collected. The inpatient participants in the present study were significantly younger (mean age was 33.78) than studies of multi-episode patients with severe mental illness [e.g., Ref. (44, 66–68)]. The participants also had a higher number of hospitalizations (8.55) upon the time of assessments compared to the participants in other studies of persons with severe mental illness. Participants also were more likely to be diagnosed with schizophrenia or schizoaffective disorders (54%), and to be non-white compared to other studies of persons with severe mental illness. These divergences with previous studies suggest that our findings may not be generalizable to a wider range of persons with psychotic disorders. Additionally, experiences of psychosis and contact with psychiatric services were reported retrospectively, recall bias may have affected the accuracy of people’s recollections about their reactions to psychotic experiences and treatment. Finally, during a psychotic episode such as during the height of hallucinations or delusions, the patient may be unable to distinguish reality from non-reality, or even self from other. Therefore, technically, the experience of delusions or hallucinations may not be considered as a traumatic life event, to the same extent as events such as criminal victimization. For some patients with chronic schizophrenia, there is a possibility that these patients never experienced traumatic life events such as abuse or criminal victimization. While we would caution the distinction between a traumatic life event and a traumatic experience of psychosis, treatment however could be similar. Clinical experience has indicated that PTSD-like symptoms induced by delusions can be similarly treated using CBT. For example, a client experienced the delusion of police “shooting” and “killing” his best friend who “stalked” him. Client held onto this fixed delusion and blamed himself for causing the “death” of his best friend. He in turn suffered PTSD-like symptoms including avoidance, hypervigilance, and re-experiencing symptoms. He was successfully treated with CBT by treating his delusion as though the event was real. Once his beliefs in causing the “death” of his best friend were challenged, his PTSD-like symptoms went away. The fixed delusion no longer significantly impacted his life as his guilt for causing his friend’s “death” went away (Lu, unpublished manuscript). Further research is needed in this regard for trauma informed care for persons with psychosis.
In summary, this qualitative study describes the experiences of people during the episodes of psychosis. We found multiple factors contributing to traumatic dimensions of the experience, including actual or perceived coercive aspects of psychiatric treatment. Further research is needed to determine how mental health services can be improved to reduce illness related trauma and facilitate recovery.
Ethics Statement
This study was carried out in accordance with the recommendations of Rutgers RBHS Institutional Review Board (previously UMDNJ-Newark IRB) and Dartmouth College Institutional Review Board with written informed consent from all subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the Rutgers RBHS Institutional Review Board (previously UMDNJ-Newark IRB) and Dartmouth College Institutional Review Board.
Author Contributions
WL was the site PI for this project. She supervised the operation the project, collected some of the data herself, supervised the data entry and data analysis. She contributed to the conception and the writing of the manuscript. KM obtained the grant. Was the PI of the grant. He supervised WL in the conduction of the research activities in this grant. He provided the research instruments, research ideas, and supervision for the original project. He also contributed to the writing of the manuscript. SR was the co-PI of the project. He provided the research instruments, research ideas, and supervision for the original project. He also contributed to the writing of the manuscript. PY contributed to the writing of the manuscript. NM contributed to the data analysis of the manuscript, composition of the tables, and the editorial assistance of the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding
This research was partially supported by a Distinguished Investigator Award to the second author from the National Alliance for Research on Schizophrenia and Depression (NARSAD) and by departmental funding to the first author from the Department of Psychiatric Rehabilitation at Rutgers University.
References
1. Davidson L. Living Outside Mental Illness: Qualitative Studies of Recovery in Schizophrenia. New York, NY: New York University Press (2003).
2. Shaw K, McFarlane A, Bookless C. The phenomenology of traumatic reactions to psychotic illness. J Nerv Ment Dis (1997) 185(7):434–41. doi:10.1097/00005053-199707000-00003
3. Birchwood M. Pathways to emotional dysfunction in first-episode psychosis. Br J Psychiatry (2003) 182(5):373–5. doi:10.1192/bjp.02.153
4. Boevink WA. From being a disorder to dealing with life: an experiential exploration of the association between trauma and psychosis. Schizophr Bull (2006) 32(1):17–9. doi:10.1093/schbul/sbi068
5. Cohen LJ. Psychiatric hospitalization as an experience of trauma. Arch Psychiatr Nurs (1994) 8(2):78–81. doi:10.1016/0883-9417(94)90037-X
6. Lu W, Mueser KT, Shami A, Siglag M, Petrides G, Schoepp E, et al. Post-traumatic reactions to psychosis in people with multiple psychotic episodes. Schizophr Res (2011) 127(1):66–75. doi:10.1016/j.schres.2011.01.006
7. Frueh BC, Knapp RG, Cusack KJ, Grubaugh AL, Sauvageot JA, Cousins VC, et al. Patients’ reports of traumatic or harmful experiences within the psychiatric setting. Psychiatr Serv (2005) 56(9):1123–33. doi:10.1176/appi.ps.56.9.1123
8. Gallop R, McCay E, Guha M, Khan P. The experience of hospitalization and restraint of women who have a history of childhood sexual abuse. Health Care Women Int (1999) 20(4):401–16. doi:10.1080/073993399245683
9. Ray NK, Myers KJ, Rappaport ME. Patient perspectives on restraint and seclusion experiences: a survey of former patients of New York State psychiatric facilities. Psychiatr Rehabil J (1996) 20(1):11–8. doi:10.1037/h0095407
10. Mueser KT, Lu W, Rosenberg SD, Wolfe R. The trauma of psychosis: posttraumatic stress disorder and recent onset psychosis. Schizophr Res (2010) 116(2):217–27. doi:10.1016/j.schres.2009.10.025
11. Chisholm B, Freeman D, Cooke A. Identifying potential predictors of traumatic reactions to psychotic episodes. Br J Clin Psychol (2006) 45(4):545–59. doi:10.1348/014466505X90136
12. Birchwood M, Iqbal Z, Chadwick P, Trower P. Cognitive approach to depression and suicidal thinking in psychosis. Br J Psychiatry (2000) 177(6):516–28. doi:10.1192/bjp.177.6.516
13. Barrett LF, Mesquita B, Gendron M. Context in emotion perception. Curr Direct Psychol Sci (2011) 20(5):286–90. doi:10.1177/0963721411422522
14. Shaner A, Eth S. Can schizophrenia cause posttraumatic stress disorder. Am J Psychother (1989) 4:588–97.
15. McGorry PD, Chanen A, McCarthy E, Van Riel R, McKenzie D, Singh BS. Posttraumatic stress disorder following recent-onset psychosis an unrecognized postpsychotic syndrome. J Nerv Ment Dis (1991) 179(5):253–8. doi:10.1097/00005053-199105000-00002
16. Priebe S, Bröker M, Gunkel S. Involuntary admission and posttraumatic stress disorder symptoms in schizophrenia patients. Compr Psychiatry (1998) 39(4):220–4. doi:10.1016/S0010-440X(98)90064-5
17. Meyer H, Taiminen T, Vuori T, Äijälä A, Helenius H. Posttraumatic stress disorder symptoms related to psychosis and acute involuntary hospitalization in schizophrenic and delusional patients. J Nerv Ment Dis (1999) 187(6):343–52. doi:10.1097/00005053-199906000-00003
18. Morrison AP, Bowe S, Larkin W, Nothard S. The psychological impact of psychiatric admission: some preliminary findings. J Nerv Ment Dis (1999) 187(4):250–3. doi:10.1097/00005053-199904000-00011
19. Frame L, Morrison AP. Causes of posttraumatic stress disorder in psychotic patients. Arch Gen Psychiatry (2001) 58(3):305–6. doi:10.1001/archpsyc.58.3.305
20. Shaw K, McFarlane AC, Bookless C, Air T. The aetiology of postpsychotic posttraumatic stress disorder following a psychotic episode. J Trauma Stress (2002) 15(1):39–47. doi:10.1023/A:1014331211311
21. Jackson C, Knott C, Skeate A, Birchwood M. The trauma of first episode psychosis: the role of cognitive mediation. Aust N Z J Psychiatry (2004) 38(5):327–33. doi:10.1080/j.1440-1614.2004.01359.x
22. Tarrier N, Khan S, Cater J, Picken A. The subjective consequences of suffering a first episode psychosis: trauma and suicide behaviour. Soc Psychiatry Psychiatr Epidemiol (2007) 42(1):29–35. doi:10.1007/s00127-006-0127-2
23. White RG, Gumley AI. Postpsychotic posttraumatic stress disorder: associations with fear of recurrence and intolerance of uncertainty. J Nerv Ment Dis (2009) 197(11):841–9. doi:10.1097/NMD.0b013e3181bea625
24. Beattie N, Shannon C, Kavanagh M, Mulholland C. Predictors of PTSD symptoms in response to psychosis and psychiatric admission. J Nerv Ment Dis (2009) 197(1):56–60. doi:10.1097/NMD.0b013e31819273a8
25. Sin GL, Abdin E, Lee J, Poon L-Y, Verma S, Chong S-A. Prevalence of post-traumatic stress disorder in first-episode psychosis. Early Interv Psychiatry (2010) 4:299–304. doi:10.1111/j.1751-7893.2010.00199.x
26. van den Berg DP, van der Gaag M. Treating trauma in psychosis with EMDR: a pilot study. J Behav Ther Exp Psychiatry (2012) 43(1):664–71. doi:10.1016/j.jbtep.2011.09.011
27. Bendall S, Alvarez-Jimenez M, Hulbert CA, McGorry PD, Jackson HJ. Childhood trauma increases the risk of post-traumatic stress disorder in response to first-episode psychosis. Aust N Z J Psychiatry (2012) 46(1):35–9. doi:10.1177/0004867411430877
28. Power PJR, Bell RJ, Mills R, Herrman-Doig T, Davern M, Henry L, et al. Suicide prevention in first episode psychosis: the development of a randomized controlled trial of cognitive therapy for acutely suicidal patients with early psychosis. Aust N Z J Psychiatry (2003) 37(4):414–20. doi:10.1046/j.1440-1614.2003.01209.x
29. Pompili M, Serafini G, Innamorati M, Lester D, Shrivastava A, Girardi P, et al. Suicide risk in first episode psychosis: a selective review of the current literature. Schizophr Res (2011) 129(1):1–11. doi:10.1016/j.schres.2011.03.008
30. Sim K, Mahendran R, Siris SG, Heckers S, Chong SA. Subjective quality of life in first episode schizophrenia spectrum disorders with comorbid depression. Psychiatry Res (2004) 129(2):141–7. doi:10.1016/j.psychres.2004.07.007
31. Addington D, Addington J, Patten S. Depression in people with first-episode schizophrenia. Br J Psychiatry (1998) 172(33):90–2.
32. Bottlender R, Strauss A, Möller HJ. Prevalence and background factors of depression in first admitted schizophrenic patients. Acta Psychiatr Scand (2000) 101(2):153–60. doi:10.1034/j.1600-0447.2000.90063.x
33. Romm KL, Rossberg JI, Berg AO, Barrett EA, Faerden A, Agartz I, et al. Depression and depressive symptoms in first episode psychosis. J Nerv Ment Dis (2010) 198(1):67–71. doi:10.1097/NMD.0b013e3181c81fc0
34. Sönmez N, Romm KL, Andreasssen OA, Melle I, Røssberg JI. Depressive symptoms in first episode psychosis: a one-year follow-up study. BMC Psychiatry (2013) 13:106. doi:10.1186/1471-244X-13-106
35. Iqbal Z, Birchwood M, Chadwick P, Trower P. Cognitive approach to depression and suicidal thinking in psychosis. 2. Testing the validity of a social ranking model. Br J Psychiatry (2000) 177:522–8. doi:10.1192/bjp.177.6.522
36. Upthegrove R, Birchwood M, Ross K, Brunett K, McCollum R, Jones L. The evolution of depression and suicidality in first episode psychosis. Acta Psychiatr Scand (2010) 122(3):211–8. doi:10.1111/j.1600-0447.2009.01506.x
37. González-Pinto A, Aldama A, González C, Mosquera F, Arrasate M, Vieta E. Predictors of suicide in first-episode affective and nonaffective psychotic inpatients: five-year follow-up of patients from a catchment area in Vitoria, Spain. J Clin Psychiatry (2007) 68(2):242–7. doi:10.4088/JCP.v68n0209
38. Mortensen PB, Juel K. Mortality and causes of death in first admitted schizophrenic patients. Br J Psychiatry (1993) 163(2):183–9. doi:10.1192/bjp.163.2.183
39. Verdoux H, Liraud F, Gonzales B, Assens F, Abalan F, Van Os J. Predictors and outcome characteristics associated with suicidal behaviour in early psychosis: a two-year follow-up of first-admitted subjects. Acta Psychiatr Scand (2001) 103(5):347–54. doi:10.1034/j.1600-0447.2001.00202.x
40. Deegan PE. Recovering our sense of value after being labeled: mentally Ill. J Psychosoc Nurs Ment Health Serv (1993) 31(4):7–9.
41. Estroff SE. Making It Crazy: An Ethnography of Psychiatric Clients in an American Community. Berkeley, CA: University of California Press (1985).
42. Judge AM, Estroff SE, Perkins DO, Penn DL. Recognizing and responding to early psychosis: a qualitative analysis of individual narratives. Psychiatr Serv (2008) 59(1):96–9. doi:10.1176/appi.ps.59.1.96
43. Yanos PT, Roe D, Markus K, Lysaker PH. Pathways between internalized stigma and outcomes related to recovery in schizophrenia-spectrum disorders. Psychiatr Serv (2008) 59:1437–42. doi:10.1176/ps.2008.59.12.1437
44. Mueser KT, Goodman LA, Trumbetta SL, Rosenberg SD, Osher FC, Vidaver R, et al. Trauma and posttraumatic stress disorder in severe mental illness. J Consult Clin Psychol (1998) 66:493–9. doi:10.1037/0022-006X.66.3.493
45. Neria Y, Bromet EJ, Sievers S, Lavelle J, Fochtmann LJ. Trauma exposure and posttraumatic stress disorder in psychosis: findings from a first-admission cohort. J Consult Clin Psychol (2002) 70:246–51. doi:10.1037/0022-006X.70.1.246
46. Grubaugh AL, Zinzow HM, Paul L, Egede LE, Frueh BC. Trauma exposure and posttraumatic stress disorder in adults with severe mental illness: a critical review. Clin Psychol Rev (2011) 31:883–99. doi:10.1016/j.cpr.2011.04.003
47. Chapple B, Chant D, Nolan P, Cardy S, Whiteford H, McGrath J. Correlates of victimisation amongst people with psychosis. Soc Psychiatry Psychiatr Epidemiol (2004) 39:836–40. doi:10.1007/s00127-004-0819-4
48. Kessler RC, Bergland P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry (2005) 62:593–602. doi:10.1001/archpsyc.62.6.617
49. Mueser KT, Gottlieb JD, Xie H, Lu W, Yanos PT, Rosenberg SD, et al. Evaluation of cognitive restructuring for post-traumatic stress disorder in people with severe mental illness. Br J Psychiatry (2015) 201(6):501–8. doi:10.1192/bjp.bp.114.147926
50. Davidson L, Ridgway P, Kidd S, Topor A, Borg M. Using qualitative research to inform mental health policy. Can J Psychiatry (2008) 53(3):137–44. doi:10.1177/070674370805300303
51. Tanskanen S, Morant N, Hinton M, Lloyd-Evans B, Crosby M, Killaspy H, et al. Service user and carer experiences of seeking help for a first episode of psychosis: a UK qualitative study. BMC Psychiatry (2011) 11(1):157. doi:10.1186/1471-244X-11-157
52. Lukoff D, Nuechterlein KH, Ventura J. Manual for the expanded Brief Psychiatric Rating Scale (BPRS). Schizophr Bull (1986) 12:594–602.
53. Mueser KT, Curran PJ, McHugo GJ. Factor structure of the Brief Psychiatric Rating Scale in schizophrenia. Psychol Assess (1997) 9:196–204. doi:10.1037/1040-3590.9.3.196
54. Kubany E, Haynes S, Leisen M, Owens J, Kaplan A, Watson S, et al. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: the Traumatic Life Events Questionnaire. Psychol Assess (2000) 12(2):210–24. doi:10.1037/1040-3590.12.2.210
56. Creswell JW. Qualitative Inquiry and Research Design: Choosing among Five Approaches. Thousand Oaks, CA: SAGE (2013).
57. Krathwohl DR. Methods of Educational and Social Science Research: An Integrated Approach. New York, NY: Longman/Addison Wesley Longman (1993).
58. Hughes R, Hayward M, Finlay WML. Patients’ perceptions of the impact of involuntary inpatient care on self, relationships and recovery. J Ment Health (2009) 18(2):152–60. doi:10.1080/09638230802053326
59. Jackson C, Trower P, Reid I, Smith J, Hall M, Townend M, et al. Improving psychological adjustment following a first episode of psychosis: a randomized controlled trial of cognitive therapy to reduce post psychotic trauma symptoms. Behav Res Ther (2009) 47(6):454–62. doi:10.1016/j.brat.2009.02.009
60. Bernard M, Jackson C, Jones C. Written emotional disclosure following first-episode psychosis: effects on symptoms of post-traumatic stress disorder. Br J Clin Psychol (2006) 45:403–15. doi:10.1348/014466505X68933
61. Fallot RD, Harris M. Trauma-informed services. In: Reyes G, Elhai JD, Ford JD, editors. The Encyclopedia of Psychological Trauma. Hoboken, NJ: John Wiley (2008). p. 660–2.
62. Seikkula J, Alakare B. Open dialogues with patients with psychosis and their families. In: Romme M, Escher S, editors. Psychosis as a Personal Crisis: An Experience-Based Approach. New York: Routledge (2012). p. 116–28.
63. Deegan PE, Drake RE. Shared decision making and medication management in the recovery process. Psychiatr Serv (2006) 57(11):1636–9. doi:10.1176/ps.2006.57.11.1636
64. MacDonald-Wilson KL, Deegan PE, Hutchison SL, Parrotta N, Schuster JM. Integrating personal medicine into service delivery: empowering people in recovery. Psychiatr Rehabil J (2013) 36(4):258–63. doi:10.1037/prj0000027
65. MacDonald-Wilson KL, Hutchison SL, Karpov I, Wittman P, Deegan PE. A successful implementation strategy to support adoption of decision making in mental health services. Community Ment Health J (2017) 53(3):251–6. doi:10.1007/s10597-016-0027-1
66. Rosenberg SD, Goodman LA, Osher FC, Swartz M, Essock SM, Butterfield MI, et al. Prevalence of HIV, hepatitis B and hepatitis C in people with severe mental illness. Am J Public Health (2001) 91:31–7. doi:10.2105/AJPH.91.1.31
67. Lommen MJ, Restifo K. Trauma and posttraumatic stress disorder (PTSD) in patients with schizophrenia or schizoaffective disorder. Community Ment Health J (2009) 45:485–96. doi:10.1007/s10597-009-9248-x
Keywords: trauma, psychosis, posttraumatic stress disorder, treatment, qualitative analysis
Citation: Lu W, Mueser KT, Rosenberg SD, Yanos PT and Mahmoud N (2017) Posttraumatic Reactions to Psychosis: A Qualitative Analysis. Front. Psychiatry 8:129. doi: 10.3389/fpsyt.2017.00129
Received: 16 December 2016; Accepted: 04 July 2017;
Published: 19 July 2017
Edited by:
Gretchen Hermes, Yale University, United StatesReviewed by:
Bernhard J. Mitterauer, Volitronics-Institute for Basic Research Psychopathology and Brain Philosophy, AustriaWissam El-Hage, François Rabelais University, France
Copyright: © 2017 Lu, Mueser, Rosenberg, Yanos and Mahmoud. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weili Lu, bHV3ZTFAc2hwLnJ1dGdlcnMuZWR1
 Weili Lu
Weili Lu Kim T. Mueser
Kim T. Mueser Stanley D. Rosenberg3,4
Stanley D. Rosenberg3,4