- 1Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 2Department of Public Health, Laboratory for Mother and Child Health, Mario Negri Institute for Pharmacological Research, Milan, Italy
- 3Institute of Mental Health, Suzhou Psychiatric Hospital, The Affiliated Guangji Hospital of Soochow University, Suzhou, Chinaz
- 4 Shanghai Mental Health Center, Shanghai Jiaotong University School of Medicine, Shanghai Key Laboratory of Psychotic Disorders, Shanghai, China
Introduction: It is common that personality disorder (PD) co-occurs with major depressive disorder (MDD). In the current literature, there is a dearth of information on the co-occurrence of PD and MDD among Chinese population.
Materials and Methods: 609 individuals were randomly sampled from outpatients diagnosed as MDD in Shanghai Mental Health Center. Co-morbidity of PDs was assessed using the Personality Diagnostic Questionnaire Fourth Edition Plus (PDQ-4+) and eligible subjects were interviewed with the Structured Clinical Interview for DSM-IV Axis II (SCID-II). The score of PDQ-4+ and the rate of SCID-II PD between subjects diagnosed with MDD and those with anxiety disorders (AD) were compared.
Results: Two hundred fifty-eight outpatients (42.36%) with MDD were recognized to possess at least one criterion of diagnosis for PD, according to the DSM-IV. The most prevalent PD was depressive PD (14.61%), followed by avoidant (11.49%) and borderline (11.49%) PD. Cluster C PDs (anxious and panic PD) were the most common PD types (12.12%) when compared to other clusters. Compared to patients with AD, individuals with MDD were significantly more likely to have paranoid PD (6.6% vs. 3.3%, p = 0.011), borderline PD (11.5% vs. 3.7%, p = 0.000), passive-aggressive PD (5.6% vs. 2.4%, p = 0.007), and depressive PD (14.6% vs. 7.8%, p = 0.000).
Discussion: The finding indicates that there is a high prevalence of PD among patients with MDD. More significant co-morbidity rates of PDs in MDD have been found when compared with AD. Further studies for the longitudinal impact of the PD-MDD co-morbidity are in need.
Introduction
Personality disorder (PD) with major depressive disorder (MDD) has been one of the most common co-morbidities in mental health disorders (1, 2). According to former studies, up to 3/4 of patients with PD have suffered from at least one episode of MDD (3, 4). Understanding the relation between PD and MDD has clinical importance in prognostic accuracy and individualized interventions of depression, with the fact that the co-morbidity would complicate the treatment and worsen the prognosis of this disorder (5, 6). It has been generally recognized that the chronicity of depression is related with a longer duration of untreated illness (DUI) (7), which might be influenced by many indicators (8). This underlines the necessity of considering the impact of the influential factors with poorer prognosis and incorporate specific interventions toward PD, including pharmacological (9–11), psychological (12–16), and social interventions (17).
Till now, many former studies have collected epidemiological data on the co-morbidity of PD and MDD (18–22). The reported prevalence of PD in MDD vary among previous studies, with the average rate of co-morbidity being approximately 50% (18, 21–23). The most frequently co-occurred PD subtypes were in turn: avoidant, borderline, dependent, obsessive-compulsive (24), and self-defeating PDs (1).
Although previous studies have been discussing the relationship between personality and depressive disorders in the past—with contributions ranging from the fields of epidemiology, epigenetics, and clinical treatments—the results have shown variations across countries, possibly due to the influence of different socio-cultural contexts (3, 4, 25–27). Moreover, there is a relative dearth of information in the current literature of Chinese patients with MDD. The only piece of Chinese literature accounting for pathological personality in MDD was published a decade ago, with a small sample of 102 patients with depressive disorders diagnosed by structured clinical interview for DSM-IV (SCID-II) (28). Considering the substantial difference between Eastern and Western culture, as well as the rapid changes in Chinese society (including the influence of westernization and modernization in the latest decades), the study in Chinese samples could not only guide contextually grounded clinical work with MDD patients with PDs but would also provide a comparable data to further understanding the interaction of the two disorders.
Research focusing on PDs among Chinese samples started in the 1980s (29, 30). Nevertheless, with the limitation of the Chinese diagnostic system, the prevalence rates of PD in the general Chinese population were underestimated (0.1‰–0.13‰). In 2000, Yang et al. has reported the prevalence of DSM-IV PDs in a sample of Chinese psychiatric patients, supporting the high clinical prevalence rates in Chinese population (31). In our former studies, a large-scale survey has been carried out and results led to the conclusions that the co-morbidity rate of PD with mood disorder was 42%, which is the highest among all the conditions (schizophrenia, mood disorder, and anxiety disorder [AD]) (32, 33). However, the demographic and clinical profile of the co-morbidity between PD and MDD is still unclear to the present date. The primary objective of this study is to examine the distribution of PDs in Chinese patients with MDD, using both DSM-IV (clinical interview) and the PDQ-4+ (self- report questionnaire) to assess personality traits. Anxiety-related disorders were settled as a comparative group to examine the difference in disturbance of PD subtypes. The possible intervention strategies of recognizing or treating specific pathological personality subtype in China would also be discussed in this study.
Materials and Methods
Sample Characteristics
The epidemiologic survey was conducted in one of the largest medical health service settings in China, the Shanghai Mental Health Center, in 2006 (32–37). As what has been comprehensively described in former studies (32, 33, 35), the participants were randomly sampled from the psycho-counseling and psychiatric clinics at the same hospital. To be briefly reviewed, a total of 3,402 individuals were randomly sampled between May and October 2006. Invitation letters were sent to them with a self-report questionnaire to collect information about PD.
The exclusion criteria were as follows: (a) presence of serious or acute psychotic symptoms; (b) a documented organic mental disorder; and (c) mental retardation. According to the exclusion criteria, subjects with serious or acute psychotic symptoms were excluded, ensuring that the participants included were in a stable state and with a degree of insight. Three hundred twenty-seven (9.6%) ineligible individuals were excluded. The overall response rate was 90.4%. More description of the inclusion and exclusion criteria could be found in our previous publications (32–34).
Out of the 3,075 patients included for PD assessment, 609 outpatients (19.8%) were diagnosed with MDD. Amongst the 609 patients (214 men, 395 women), with a mean age of 33.19 years (SD = 10.4, ranged 18–60 years), 359 of them (58.9%) were sampled from the psycho-counseling clinic and 250 individuals (41.1%) were recruited from the psychiatric clinic.
Three hundred seventy-five patients (61.6%) came to the clinic for the first time, whereas 111 patients (18.2%) showed at the location repeatedly (more than five times before the study). Eighty-seven patients (14.3%) have received pharmacological treatments, including antidepressant drug (n = 73), antipsychotic drug (n = 7), hypnotic drug (n = 4), and anxiolytics drug (n = 3). Seventy-seven patients (12.4%) had medical comorbidity, including cardiovascular disease (n = 15), digestive disease (n = 20), endocrinology disease (n = 8), immunology disease (n = 5), body pain (n = 8), tumor (n = 5), insomnia (n = 3), other diseases (n = 11), and multiple diseases (n = 2). The length of disorder varied from 0 to 372 months, with a mean course of 43 months. When taking marital status into consideration, 248 participants (40.7%) were single, 303 (49.8%) were married, 36 (5.9%) were divorced, 22 (3.6%) were widowed. As for the educational level, 316 (51.9%) participants were graduates, while only 73 (12.0%) participants earned more than 5,000 Yuan a month. Ninety (14.8%) participants had not been raised by both parents.
To make a comparison with MDD patients, 574 participants who were diagnosed with anxiety and related disorders were selected from the sample of 3,075 outpatients according to their medical records. Among these patients, more than a half of them were diagnosed with a general AD and panic disorder (n = 343), 153 with obsessive-compulsive disorder, 78 of them with phobia. The average age of the 574 patients (278 men, 296 women) was 32.52 years (SD = 10.0, ranged 18–60 years). ANOVA and Chi-squared tests were used to compare the results of PD assessment by using PDQ-4+ and SCID-II separately among different ADs (see Supplement). The results of most of PD subtypes, except schizotypal, avoidant, and obsessive-compulsive PD, did not present significant differences among these ADs.
Measures
General Questionnaire
The general questionnaire collected data that includes: (a) demographics; (b) family and social background; and (c) physical and mental health conditions.
Assessment of Personality Disorders
The Personality Diagnostic Questionnaire Fourth Edition Plus (PDQ-4+): as detailed in our previous studies (32–35), the PDQ4+ is a concise structured self-report questionnaire that contains 107 true-false items and screens for 12 Axis II DSM-IV Personality Disorders. The PDQ-4+ seeks to discriminate between individuals with and without characteristics that can be associated with PD (38–40). Although the specificity is medium (.65), the PDQ-4+ is a highly sensitive test (.89). It has been used to screen for DSM-IV PD in the Chinese psychiatric patients (31, 32) and college student populations (41). The test-retest reliability value amongst the Chinese populations was of .92.
The Structured Clinical Interview for DSM-IV Axis II (SCID-II): Is a Semi-Structured Clinical Interview for PD Diagnosis. the Pds Classification Is Made in Accordance With the DSM-IV Criteria, Which Includes Cluster a PD (Paranoid, Schizoid, Schizotypal PD), Cluster B PD (Histrionic, Narcissistic, Borderline, Antisocial PD), Cluster C PD (Avoidant, Dependent, Obsessive-Compulsive PD), Passive-Aggressive PD and Depressive PD (In the Appendix of DSM-IV). the SCID-II Is Consistent (.90) With the Clinical Diagnosis and Has a Relatively High Test-Retest Reliability (.70), With a Median of Coefficient for Internal Consistency Of.70 (42, 43).
Diagnosis of Major Depressive Disorder and Other Axis I Disorder
Patients' clinical diagnoses were assessed with the Chinese Classification and Diagnostic Criteria of Mental Disorders version 3, CCMD-3 (Chinese Society of Psychiatry, 2001) by psychiatrists at outpatient appointments. The CCMD-3 represents a classification of mental health disorders substantially influenced by ICD-10 and DSM-IV representations. Most of the diagnostic criteria of MDD and AD (including phobia, panic disorder, general AD, obsession) are identical to the international classifications.
Procedures
The Research Ethics Committee at the Shanghai Mental Health Centre approved the study in 2006. The sample was selected within a two-stage procedure. Firstly, 3,402 individuals were randomly sampled from the psycho-counseling and psychiatric clinics internal to the Shanghai Mental Health Center and invited to participate in the study. The participants were asked to complete the general questionnaire and PDQ-4+, under the guidance of three senior executive nurses. The data were checked by the trained nurses, to ensure that each questionnaire was completed. Then the PDQ-4+ was administered by a trained psychiatrist to screen for the presence of PD. Amongst the 3,075 eligible individuals, 2,706 patients met the criteria for DSM-IV PD and were recruited into the second stage of the study, the SCID-II interview.
In order to reduce the effect that subjective deviation had on the results of the SCID-II clinical interview, the interviewers, two senior psychiatrists who were trained for 2 weeks by the research team members (ZP, Xiao; YF, Dai et al.), were not aware of the PDQ-4+ test results and clinical diagnoses of the patients. The inter-rater reliability of the SCID interview was determined after training. Thirty inpatient interviews were scored by two raters independently. The kappa value of reliability for any PD was 0.82.
All participants were diagnosed according to CCMD-3 by the attending psychiatrists, who were unaware of the results of the personality evaluation of the patients. The clinical diagnoses of participants reported in this paper were made by two attending psychiatrists separately and written down in their outpatients' medical records, which was double-checked by researchers. In this study, 609 medical records of patients with MDD were selected from the large sample of outpatients. Among them, 536 were PDQ-4+ positive and interviewed with SCID-II. The interviewer reliability for PDQ4+ and SCID-II was satisfactory. The reliability of raters, according to the kappa value for the diagnosis of PD, fell between.78 and.98.
Statistical Analysis
SPSS 20.0 (SPSS Inc., Chicago, IL, USA) was used to analyze participants' demographic and clinical data. Frequencies and 95% confidence interval (95% CI) of PDs in patients with MDD, evaluated by PDQ-4+ and SCID-II, were calculated separately by cluster and specific PD. Odds ratios (OR) were generated to assess associations of PDs with demographic and clinical profiles such as age, gender, education and marriage state, parents' marriage state, type of outpatient service (psycho-counseling or psychiatric clinic), and self-reported characteristics. Two tailed t-tests were used to compare the average score of PDQ-4+ by cluster and specific PD between MDD and AD, while Chi-squared tests were used to compare the prevalence of PD detected by SCID-II. Stepwise regression was performed using clinical diagnosis (MDD vs. anxiety and related disorders) as dependent variables, with social-demographic characteristics (age, gender, marital status, parental divorce, normal trait, caregiver) and each cluster of PD as independent variables. All statistical differences were considered significant at p < .05.
Results
Prevalence of PDs
Table 1 reflects the prevalence of PDs among patients with MDD. According to the results of PDQ-4+, the rate of self-reported PDs in the depression sample was relatively high: 88.01% of the patients presented at least one self-reported PDs. The most frequent PD in this sample was avoidant PD (62.4%), followed by obsessive-compulsive (61.1%) and borderline PD (BPD) (54.02%). In addition, the structured interviewing tool of SCID-II was used to investigate clinical diagnosed PDs. The results significantly showed the prevalence of PD among patients with MDD with lower occurrence rates than the PDQ-4+ results. Among individuals 42.36% met at least one criterion for DSM-IV PD. The most prevalent PD was depressive (14.61%), followed by avoidant (11.49%) and BPD (11.49%). Cluster C PDs (12.12%) were the most common PD types compared to other clusters.
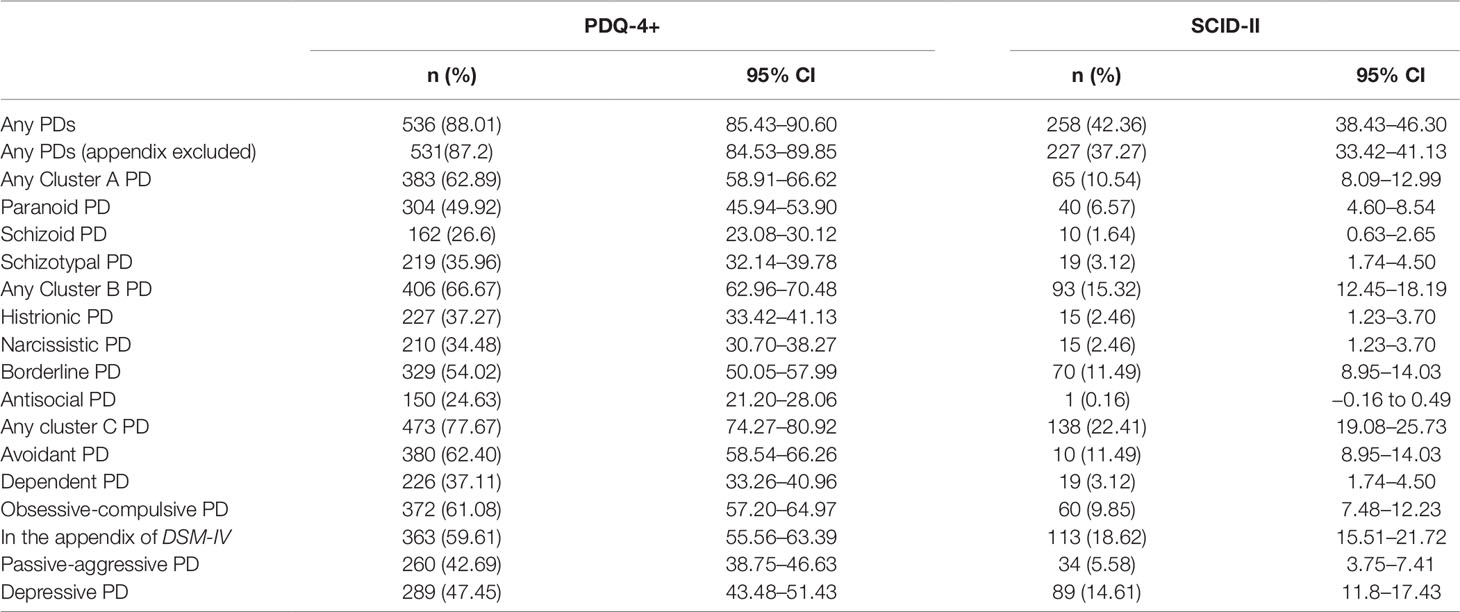
Table 1 Frequency of DSM-IV personality disorders (PDs) among patients with depression using Personality Diagnostic Questionnaire Fourth Edition Plus (PDQ-4+) and Structured Clinical Interview for DSM-IV Axis II (SCID-II).
Impact of Clinical and Socio-Demographic Characteristics
The overall prevalence of PDs among young people was significantly greater than the prevalence in older people (OR = 1.343) (Table 2). Compared with the group of married individuals, patients who were single (OR = 1.352) had a higher prevalence of PD. The prevalence of PD was greater in the psycho-counseling clinic (OR = 1.144) than in psychiatric clinic. Patients whose parents were divorced (OR = 1.663) were more likely to be diagnosed with PD. On the other hand, patients who were raised by their parents (OR = 0.627) were less likely to get diagnosed with PD. The prevalence of PD was higher in individuals with Introversion characteristics (OR = 1.348) than those with other types of characteristics (middle type, extraversion).
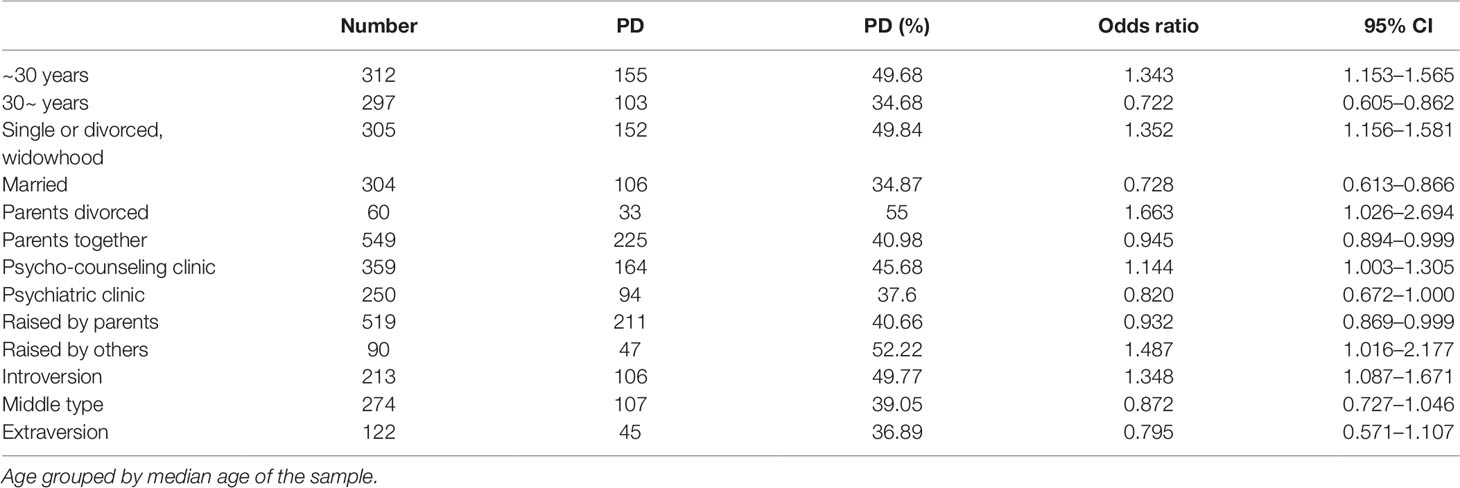
Table 2 Odds ratios (and 95% CI) of having Structured Clinical Interview for DSM-IV Axis II personality disorders (PDs) among patients with depression, by clinical and socio-demographic characteristics.
Comparative Analyses of Personality Disturbance
Table 3 has shown the personality disturbance between MDD and AD, evaluated by PDQ-4+ and SCID-II. According to the results in the first set of analyses, individuals with MDD reported significantly more symptoms of all PDs compared to individuals with AD, except for paranoid and schizotypal PD. In the second set of analyses, which was conducted to investigate the difference of PD prevalence between the MDD and AD group, individuals with MDD were significantly more likely to have paranoid PD (6.6% vs. 3.3%, p = 0.011), BPD (11.5% vs. 3.7%, p = 0.000), passive-aggressive PD (5.6% vs. 2.4%, p = 0.007), and depressive PD (14.6% vs. 7.8%, p = 0.000).
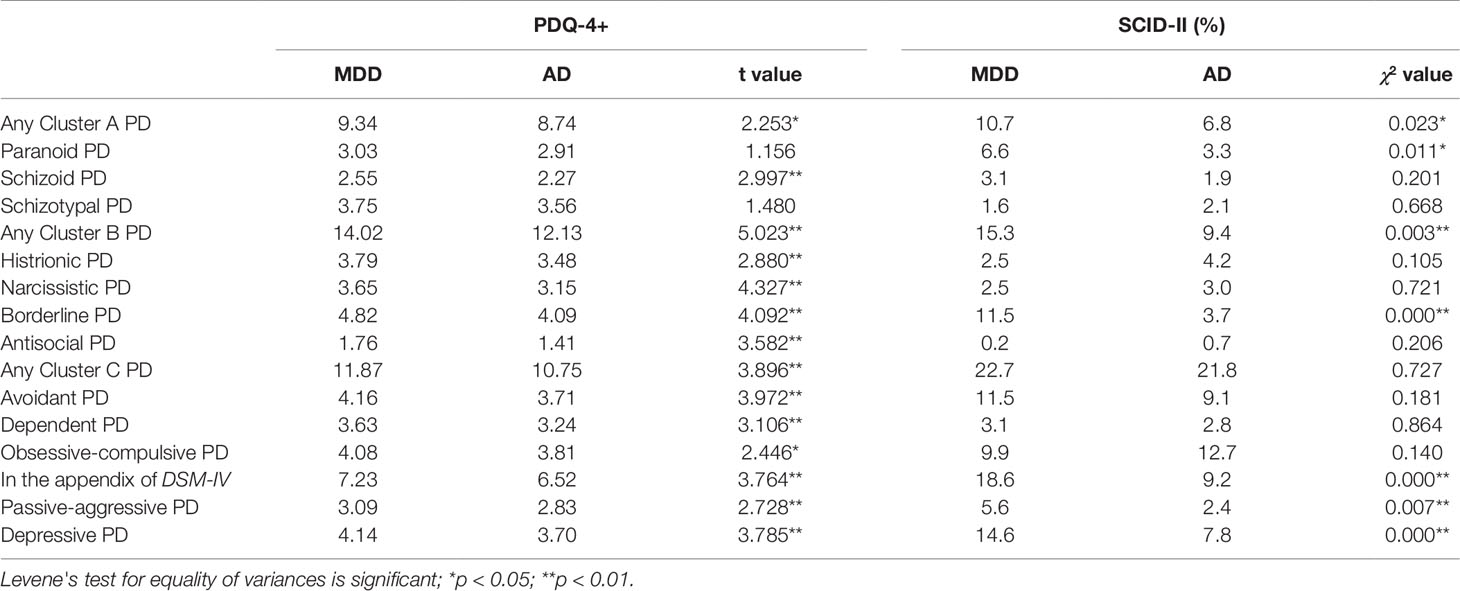
Table 3 Comparison of difference between major depressive disorder (MDD) and anxiety disorders for Personality Diagnostic Questionnaire Fourth Edition Plus (PDQ-4+) personality disorders (PDs) scores and Structured Clinical Interview for DSM-IV Axis II (SCID-II) PDs frequency.
Stepwise Regression Analyses
Stepwise regression was employed in an attempt to identify the risk factors of PDs related to MDD or AD, evaluated with PDQ-4+ and SCID-II. Logistic regression (forward stepwise) analyses were performed with clinical diagnosis (MDD vs. AD) as the dependent variable while social-demographic characteristics (age, gender, marital status, parental divorce, normal trait, caregiver) and different type of PDs acted as independent variables (Table 4). The results from self-report questionnaire (Table 4) indicated that borderline and narcissist PDs were significant predictors of MDD, while paranoid PD was a significant predictor of AD. The results evaluated by interviews showed that borderline and depressive PDs were significant predictors of MDD.
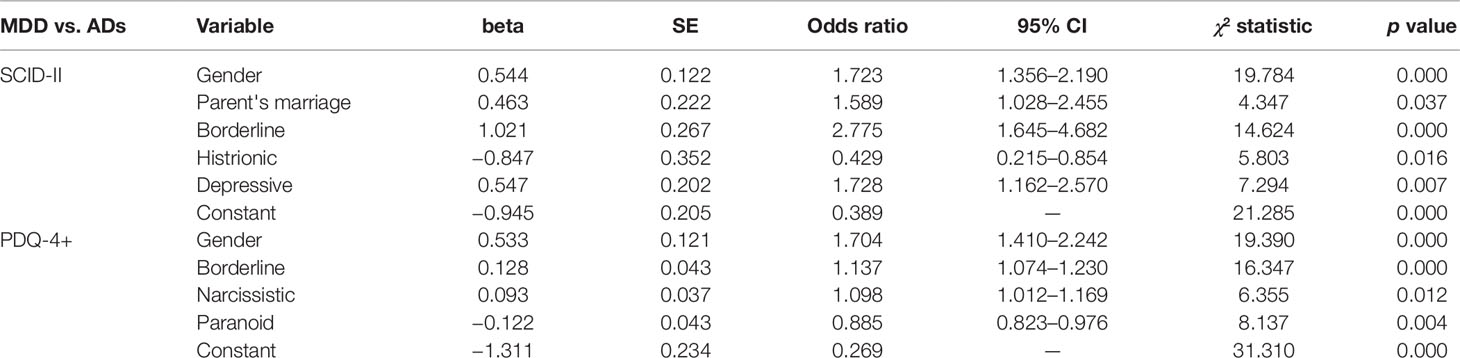
Table 4 Forward stepwise logistic regression for risk factors predicting the clinical diagnoses based on Structured Clinical Interview for DSM-IV Axis II (SCID-II) and Personality Diagnostic Questionnaire Fourth Edition Plus (PDQ-4+).
Discussion
The data gathered from this study has filled the existing gap in literature about the co-morbidity of PD-MDD in Chinese population. The primary aim of this study was to examine the distribution of PDs in Chinese patients with MDD. The result of this study indicates that the co-morbidity of PD was indeed common among Chinese patients with MDD: 88.01% of participants were presenting at least one self-reported PD, and 42.36% patients with MDD were meeting the clinical criteria of PD. According to former epidemiological studies, the number of rate of co-morbidity came within the average being approximately 50% (18). However, considering that the varied prevalence in previous surveys may have been influenced by different sample characteristics and research methods, comparing the rates with foreign studies without proper adaptive measures would represent a problem. Particularly, careful consideration is needed when taking timing of assessment, source of information, and diagnostic instruments into account (44).
Among three clusters of PDs in MDD patients, Cluster C PDs were the most common types, while Cluster A PDs were the least frequent. The possible explanation might be that Cluster C PDs are predominantly treatment-seeking unlike the other two types (45). Moreover, the help-seeking behaviors declined in Cluster A PDs as the results of stigma and social disability, which might in turn be caused by the lower prevalence of this cluster among the other three clusters. The distribution of different PD subtypes in MDD patients was mostly in accordance with the results in previous studies (24, 27), suggesting that avoidant and BPDs were two most common PD subtypes in patients with MDD.
The socio-demographic characteristics of MDD patients with PD have also been investigated in this study. The factors associated with increased odds of PD were shown to include a younger age, non-marriage status (single, divorced, or widowhood), not being raised by both parents, belonging to a family with divorce history, being in psycho-counseling clinic, and scoring higher as introverted in self-reported measures. This has replicated the finding in previous studies such as the Australian National Survey of Mental Health and Wellbeing, which led to the conclusion that youths and not married individuals were also more likely to have PD (46–49). The effect of age on PD prevalence has been supported by some studies (36, 50) but rejected by others (46, 51, 52). Detailed discussion could be found in our former study (36).The other result of these factors calls for needs to build a stronger supporting system as a protective measure.
The result of the comparison of PDs between MDD and AD was unexpected. When compared with Previous literature reported that PD patients were five times more likely to have an AD and four times more likely to have a mood disorder (46). However, in our studies, the prevalence of PD among patients with AD (84.8% with PDQ-4+ and 34.3% with SCID-II) turned out to be lower than the prevalence among patients with MDD. The comparably greater rates of PD among MDD patients was also supported by the distinct high co-morbidity of "eccentric" and "emotional" group PDs when compared to the patients with AD, while there was no significant difference in the "fearful" group of PDs. The higher rate of PD occurrence reflected by the self-report questionnaire, compared to the result of the clinical interview, possibly indicated the negative cognition of MDD patients to their own situation (53). Zimmerman et al. argued that diagnoses based on self-reported questionnaires might be more sensitive to clinical state than clinical interviews are (54). These different results were caused by variation in participant responses across measures. Shannon et al. found that participants with lower severity of disorder may show greater disclosure on anonymous inventories relative to interview formats (55). It might be because of lower defensiveness and fuller reporting of symptoms in the more anonymous paper and pencil setting of a self-report inventory (31). The difference in diagnoses of PD by using self-report questionnaires and clinical interviews requires further studies.
Based on the results of predictive factors, borderline and depressive PDs seemed to be strongly associated with MDD, while Histrionic PD was predictive of AD. Conceptualized as diagnostically distinct disorders, MDD and AD have high co-morbidity (56, 57), thus, more understanding about these two disorders are in need. This result of this study might provide specific clinical clues in understanding the personality characteristic between depression and ADs. The possible reasons for the inter-relationship of PDs and Axis I disorders has been discussed in our former studies (37), including the pre-morbid model and the post-morbid model. Meanwhile, Johnson et al. proposed that some PDs and mood disorders might be at different points on a common affective spectrum (58). The co-occurrence could also be partly attributable to overlapping diagnostic criteria between the two disorders.
The result of the stepwise logistic regression is consistent with previous studies (3, 59, 60), confirming that the BPD is the most significant predictor of MDD. Specifically, Gunderson et al. have found that among different types of PDs, BPD patients were most likely to have MDD and 85% of the patients with co-morbidity had more than one recurrence of a depressive episode (3, 59) Reichborn-Kjennerud et al. have paralleled this result with a twin study of 2,801 patients, which indicates that borderline, avoidant, and paranoid PDs could increase the risk of MDD and that, once again BPD was the strongest predictor of MDD (60).
The result of high prevalence and correlation with MDD of depressive PD, a PD subtype in DSM-IV appendix and now removed from the DSM-5 category, was parallel to previous studies, supporting that depressive PD is one of the most commonly diagnosed personality subtypes (61) and highly overlaps with MDD (62). Although this diagnoses was no longer included in current classification systems of mental disorders, partly because it overlaps with other diagnoses (63), there're still some arguments that depressive PD should be included as a diagnostic type (64, 65). Considered of these reasons, the result of depressive PD was retained in the analysis and might provide further evidence to future studies.
It is important to note that there are several methodological limitations in this study. Firstly, as a cross-sectional survey, it is unable to investigate the order of occurrence between PD and MDD. Meanwhile, some patients with a first depressive episode might subsequently change their diagnosis in bipolar disorder (66), the number of which was unclear under such limitation. To evaluate the longitudinal relationship of PD and MDD, as well as to minimize the influence of misdiagnosis, prospective follow-up studies of PD and MDD are in need. Secondly, the sample of this study was made up from outpatients from psycho-counseling and psychiatric clinics in one hospital in Shanghai. Hence, the results might not be generalized to a broader population with MDD in China. Thirdly, the prevalence of PDs based on SCID-II might be underestimated by using the PDQ-4+ as a screen. In this study, only patients with positive results on the PDQ-4+ entered the clinical interview with SCID-II. Although this self-report questionnaire has a high sensitivity (0.89), some participants with false negative results might be excluded. Moreover, the sensitivity of the PDQ-4+ varies by diagnosis (31, 32), which could also impact the diagnoses on different levels. Lastly, only one major diagnosis of the patients was collected (when some may have had two or more), which might not take the influence of other co-morbidity into consideration. Such influence could be bidirectional. The overlaps between some of PD symptoms and other Axis I disorders, such as schizophrenia and obsessive-compulsive disorder, may affect the accuracy of personality assessment and lead to an overestimation of PD prevalence. Meanwhile, the exclusion of some Axis I disorders, such as substance use disorders, which have high co-morbidity rate with PD (67, 68), might lead to an underestimation of the PD rates among the participants.
Conclusion
In summary, this study has provided important clues to understanding the relationship between MDD and PD and has highlighted the assessments and interventions of PD in patients with MDD. The results suggested that indicators, such as specific PD subtypes, might be helpful in further understanding how PD correlates to the difference between MDD and ADs. Further studies for longitudinal impact of the co-morbidity, including the psychopathology, progression, and outcome, could further reveal useful information on this topic.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
This study was carried out in accordance with the recommendations of the Research Ethics Committee at the Shanghai Mental Health Centre with written informed consent from all subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the Research Ethics Committee at the Shanghai Mental Health Centre.
Author Contributions
YZ designed and conducted this study, including data analysis and writing the article. FS revised the article. LH was responsible for collecting and entering data. HW and JW were responsible for recruiting, diagnosing, and classifying the patients. TZ revised the study design and the article.
Funding
This work was supported by the Ministry of Science and Technology of China, National Key R&D Program of China (2016YFC1306803), National Natural Science Foundation of China (81671329, 81671332), Clinical Research Plan of SHDC (16CR2015A, 16CR3016A), Shanghai Mental Health Center Foundation (2016-FX-01, 2017-TSXK-03), Shanghai Science and Technology Committee grants (16JC1420200).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank all the patients who participated in the research.
References
1. Hirschfeld RM. Personality disorders and depression: comorbidity. Depress Anxiety (1999) 10(4):142–6. doi: 10.1002/(sici)1520-6394(1999)10:4<142::aid-da2>3.0.co;2-q
2. Oldham JM, Skodol AE, Kellman HD, Hyler SE, Doidge N, Rosnick L, et al. Comorbidity of axis I and axis II disorders. Am J Psychiatry (1995) 152(4):571–8. doi: 10.1176/ajp.152.4.571
3. Gunderson JG, Stout RL, Sanislow CA, Shea MT, McGlashan TH, Zanarini MC, et al. New episodes and new onsets of major depression in borderline and other personality disorders. J Affect Disord (2008) 111(1):40–5. doi: 10.1016/j.jad.2008.01.026
4. Morey LC, Shea MT, Markowitz JC, Stout RL, Hopwood CJ, Gunderson JG, et al. State effects of major depression on the assessment of personality and personality disorder. Am J Psychiatry (2010) 167(5):528–35. doi: 10.1176/appi.ajp.2009.09071023
5. Zimmerman M, Rothschild L, Chelminski I. The prevalence of DSM-IV personality disorders in psychiatric outpatients. Am J Psychiatry (2005) 162(10):1911–8. doi: 10.1176/appi.ajp.162.10.1911
6. Marleen DB, Filip DF, Quilty LC, Jean-Pierre R, Mieke D, Michael B. Does personality disorder co-morbidity impact treatment outcome for patients with major depression? A multi-level analysis. J Pers Disord (2011) 25(1):1–15. doi: 10.1521/pedi.2011.25.1.1
7. Altamura AC, Buoli M, Albano A, Dell'Osso B. Age at onset and latency to treatment (duration of untreated illness) in patients with mood and anxiety disorders: a naturalistic study. Int Clin Psychopharmacol (2010) 25(3):172–9. doi: 10.1097/YIC.0b013e3283384c74
8. Eaton WW, Shao H, Nestadt G, Lee HB, Bienvenu OJ, Zandi P. Population-based study of first onset and chronicity in major depressive disorder. Arch Gen Psychiatry (2008) 65(5):513–20. doi: 10.1001/archpsyc.65.5.513
9. Coccaro EF, Kavoussi RJ. Fluoxetine and impulsive aggressive behavior in personality-disordered subjects. Arch Gen Psychiatry (1997) 54(12):1081–8. doi: 10.1001/archpsyc.1997.01830240035005
10. Fava M, Bouffides E, Pava JA, Mccarthy MK, Steingard RJ, Rosenbaum JF. Personality Disorder comorbidity with major depression and response to fluoxetine treatment. Psychother Psychosomatics (2010) 62(3-4):160–7. doi: 10.1159/000288918
11. Duggan C, Huband N, Smailagic N, Ferriter M, Adams C. The use of pharmacological treatments for people with personality disorder: a systematic review of randomized controlled trials. Pers Ment Health (2008) 2(3):119–70. doi: 10.1002/pmh.41
12. Bateman A, Fonagy P. Comorbid antisocial and borderline personality disorders: mentalization-based treatment. J Clin Psychol (2008) 64(2):181–94. doi: 10.1002/jclp.20451
13. Blum N, St John D, Pfohl B, Stuart S, McCormick B, Allen J, et al. Systems training for emotional predictability and problem solving (STEPPS) for outpatients with borderline personality disorder: a randomized controlled trial and 1-year follow-up. Am J Psychiatry (2008) 165(4):468–78. doi: 10.1176/appi.ajp.2007.07071079
14. Giesen-Bloo J, van Dyck R, Spinhoven P, van Tilburg W, Dirksen C, van Asselt T, et al. Outpatient psychotherapy for borderline personality disorder: randomized trial of schema-focused therapy vs transference-focused psychotherapy. Arch Gen Psychiatry (2006) 63(6):649–58. doi: 10.1001/archpsyc.63.6.649
15. Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch Genpsychiatry (2006) 63(7):757–66. doi: 10.1001/archpsyc.63.7.757
16. McMain SF, Links PS, Gnam WH, Guimond T, Cardish RJ, Korman L, et al. A randomized trial of dialectical behavior therapy versus general psychiatric management for borderline personality disorder. Am J Psychiatry (2009) 166(12):1365–74. doi: 10.1176/appi.ajp.2009.09010039
17. Tyrer P. Nidotherapy in the treatment of personality disorder. Psychiatry (2008) 7(3):121–3. doi: 10.1016/j.mppsy.2008.01.008
18. Grant BF, Hasin DS, Stinson FS, Dawson DA, Patricia Chou S, June Ruan W, et al. Co-occurrence of 12-month mood and anxiety disorders and personality disorders in the US: results from the national epidemiologic survey on alcohol and related conditions. J Psychiatr Res (2005) 39(1):1–9. doi: 10.1016/j.jpsychires.2004.05.004
19. Charney DS, Nelson JC, Quinlan DM. Personality traits and disorder in depression. Am J Psychiatry (1981) 138(12):1601–4. doi: 10.1176/ajp.138.12.1601
20. Pfohl B, Stangl D, Zimmerman M. The implications of DSM-III personality disorders for patients with major depression. J Affect Disord (1984) 7(3):309–18. doi: 10.1016/0165-0327(84)90052-1
21. Melartin TK, RytsäLä HJ, Leskelä US, Lestelä-Mielonen PS, Petteri S, Isometsä ET. Current comorbidity of psychiatric disorders among DSM-IV major depressive disorder patients in psychiatric care in the Vantaa Depression Study. J Clin Psychiatry (2002) 63(2):126. doi: 10.4088/JCP.v63n0207
22. Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry (2005) 62(10):1097. doi: 10.1001/archpsyc.62.10.1097
23. Lenzenweger MF, Lane MC, Loranger AW, Kessler RC. DSM-IV Personality disorders in the national comorbidity survey replication. Biol Psychiatry (2007) 62(6):553–64. doi: 10.1016/j.biopsych.2006.09.019
24. Skodol AE, Stout RL, McGlashan TH, Grilo CM, Gunderson JG, Shea MT, et al. Co-occurrence of mood and personality disorders: a report from the Collaborative Longitudinal Personality Disorders Study (CLPS). Depress Anxiety (1999) 10(4):175–82. doi: 10.1002/(sici)1520-6394(1999)10:4<175::aid-da6>3.0.co;2-2
25. Newton-Howes G, Tyrer P, Johnson T, Mulder R, Kool S, Dekker J, et al. Influence of personality on the outcome of treatment in depression: systematic review and meta-analysis. J Pers Disord (2014) 28(4):577–93. doi: 10.1521/pedi_2013_27_070
26. Weber K, Giannakopoulos P, Canuto A. Exploring the impact of personality dimensions in late-life depression: from group comparisons to individual trajectories. Curr Opin Psychiatry (2011) 24(6):478–83. doi: 10.1097/YCO.0b013e32834a349f
27. Bagby RM, Psych C, Quilty LC, Ryder AC. Personality and depression. Can J Psychiatry Rev Can Psychiatr (2008) 53(1):14–25. doi: 10.1177/070674370805300104
28. Zhou YP, Gao XC, Liu HX, Xie XY, Xie CG. Comorbidity of depressive disorders and personality disorders. Shandong Arch Psychiatry (2005) 18(1):17–20.
29. Chen CH. Data analysis of an epidemiological study of mental disorders, drug and alcoholic dependence and personality disorders. Zhonghua shen jing jing shen ke za zhi (1986) 19(2):70–2.
30. Zhang W, Shen Y, Li S. Epidemiological investigation on mental disorders in 7 areas of China. Chin J Psychiatry (1998) 31(2):69–71.
31. Yang J, Mccrae RR, Costa PT Jr., Yao S, Dai X, Cai T, et al. The cross-cultural generalizability of axis-ii constructs: an evaluation of two personality disorder assessment instruments in the people's republic of China. J Pers Disord (2000) 4(3):249–63. doi: 10.1521/pedi.2000.14.3.249
32. Zhang TH, Xiao ZP, Wang LL, Dai YF, Zhang HY, Qiu JY, et al. cross-sectional survey on personality disorder in mental disorder outpatients in Shanghai. Chin J Epidemiol (2010) 31(08):933–7. doi: 10.3760/cma.j.issn.0254-6450.2010.08.023
33. Zhang T, Wang L, Good MJ, Good BJ, Chow A, Dai Y, et al. Prevalence of personality disorders using two diagnostic systems in psychiatric outpatients in Shanghai, China: a comparison of uni-axial and multi-axial formulation. Soc Psychiatry Psychiatr Epidemiol (2012) 47(9):1409–17. doi: 10.1007/s00127-011-0445-x
34. Zhang T, Chow A, Wang L, Dai Y, Xiao Z. Role of childhood traumatic experience in personality disorders in China. Compr Psychiatry (2012) 53(6):829–36. doi: 10.1016/j.comppsych.2011.10.004
35. Zhang TH, Chow A, Wang LL, Yu JH, Dai YF, Lu X, et al. Childhood maltreatment profile in a clinical population in China: a further analysis with existing data of an epidemiologic survey. Compr Psychiatry (2013) 54(7):856–64. doi: 10.1016/j.comppsych.2013.03.014
36. Zhang T, Good MJ, Good BJ, Chow A, Wang L, Dai Y, et al. Age and remission of personality pathology in the psychotic disorders compared to mood and/or anxiety disorders. Int J Psychiatry Med (2012) 44(3):241–55. doi: 10.2190/PM.44.3.e
37. Wei Y, Zhang T, Chow A, Tang Y, Xu L, Dai Y, et al. Co-morbidity of personality disorder in schizophrenia among psychiatric outpatients in China: data from epidemiologic survey in a clinical population. BMC Psychiatry (2016) 16:224. doi: 10.1186/s12888-016-0920-8
38. Hurt SW, Hyler SE, Frances A, Clarkin JF, Brent R. Assessing borderline personality disorder with self-report, clinical interview, or semistructured interview. Am J Psychiatry (1984) 141(10):1228–31. doi: 10.1176/ajp.141.10.1228
39. Hyler SE, Skodol AE, Oldham JM, Kellman HD, Doidge N. Validity of the personality diagnostic questionnaire-revised: a replication in an outpatient sample. Compr Psychiatry (1992) 33(2):73–7. doi: 10.1016/0010-440x(92)90001-7
40. Hyler SE, Skodol AE, Kellman HD, Oldham JM, Rosnick L. Validity of the personality diagnostic questionnaire–revised: comparison with two structured interviews. Am J Psychiatry (1990) 147(8):1043–8. doi: 10.1176/ajp.147.8.1043
41. Huang X, Ling H, Yang B, Dou G. Screening of personality disorders among chinese college students by personality diagnostic questionnaire-4+. J Pers Disord (2007) 21(4):448–54. doi: 10.1521/pedi.2007.21.4.448
42. Dai YF. A survey on the comorbidity of personality disorders in patients counseling in a mental hospital. Chin Ment Heath J (2006) 18:5–7. doi: 10.1016/S1872-2075(08)60026-6
43. Dai YF, Xiao ZP, Wang Z, Zhang HY, Chen J. The reliability and validity of a Chinese version of the Structured Clinical Interview for DSM-IV personality disorders. Shanghai Arch Psychiatry (2006) 18:1–4. doi: 10.3969/j.issn.1002-0829.2006.01.001
44. Beckwith H, Moran PF, Reilly J. Personality disorder prevalence in psychiatric outpatients: A systematic literature review. Personal Ment Health 8(2):91–101.
45. Ranger M, Methuen C, Rutter D, Rao B, Tyrer P. Prevalence of personality disorder in the case-load of an inner-city assertive outreach team. Psychiatr Bull (2004) 28(12):441. doi: 10.1192/pb.28.12.441
46. Jackson HJ, Burgess PM. Personality disorders in the community: a report from the Australian national survey of mental health and wellbeing. Soc Psychiatry Psychiatr Epidemiol (2000) 35(12):531–8. doi: 10.1007/s001270050276
47. Ames A, Molinari V. Prevalence of personality disorders in community-living elderly. J geriatric Psychiatry Neurol (1994) 7(3):189–94. doi: 10.1177/089198879400700311
48. Bernstein DP, Cohen P, Velez CN, Schwab-Stone M, Siever LJ, Shinsato L. Prevalence and stability of the DSM-III-R personality disorders in a community-based survey of adolescents. Am J Psychiatry (1993) 150(8):1237–43. doi: 10.1176/ajp.150.8.1237
49. Johnson JG, Cohen P, Kasen S, Skodol AE, Hamagami F, Brook JS. Age-related change in personality disorder trait levels between early adolescence and adulthood: a community-based longitudinal investigation. Acta Psychiatr Scand (2000) 102(4):265–75. doi: info:doi/10.1034/j.1600-0447.2000.102004265.x
50. Engels GI, Duijsens IJ, Haringsma R, van Putten CM. Personality disorders in the elderly compared to four younger age groups: a cross-sectional study of community residents and mental health patients. J Pers Disord (2003) 17(5):447–59. doi: 10.1521/pedi.17.5.447.22971
51. Enfoux A, Courtois R, Duijsens I, Reveillere C, Senon JL, Magnin G, et al. Comorbidity between personality disorders and depressive symptomatology in women: A cross-sectional study of three different transitional life stages. Pers Ment Health (2013) 7(3):233–41. doi: 10.1002/pmh.1228
52. Stevenson J, Datyner A, Boyce P, Brodaty H. The effect of age on prevalence, type and diagnosis of personality disorder in psychiatric inpatients. Int J geriatric Psychiatry (2011) 26(9):981–7. doi: 10.1002/gps.2645
53. Farabaugh A, Mischoulon D, Fava M, Guyker W, Alpert J. The overlap between personality disorders and major depressive disorder (MDD). Ann Clin Psychiatry (2011) 16(4):217–24. doi: 10.1080/10401230490522043
54. Zimmerman M, Pfohl B, Coryell WH, Corenthal C, Stangl D. Major depression and personality disorder. J Affect Disord (1991) 22(4):199–210. doi: 10.1016/0165-0327(91)90066-2
55. Kelley SE, Balsis S, Smith ST, Edens JF, Douglas KS, Poythress NG Jr. A dimensional comparison of a self-report and a structured interview measure of conduct disorder. J Pers Disord (2015) 30(2):1–10. doi: 10.1521/pedi_2015_29_191
56. Kessler RC, Chiu W, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month dsm-iv disorders in the national comorbidity survey replication. Arch Gen Psychiatry (2005) 62(6):617–27. doi: 10.1001/archpsyc.62.6.617
57. Mineka S, Watson D, Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annu Rev Psychol (1998) 49:377–412. doi: 10.1146/annurev.psych.49.1.377
58. Johnson JG, Cohen P, Kasen S, Brook JS. Personality disorder traits associated with risk for unipolar depression during middle adulthood. Psychiatry Res (2005) 136(2-3):113–21. doi: 10.1016/j.psychres.2005.02.007
59. Gunderson JG, Stout RL, McGlashan TH, Shea MT, Morey LC, Grilo CM, et al. Ten-year course of borderline personality disorder: psychopathology and function from the collaborative longitudinal personality disorders study. Arch Gen Psychiatry (2011) 68(8):827–37. doi: 10.1001/archgenpsychiatry.2011.37
60. Reichborn-Kjennerud T, Czajkowski N, Roysamb E, Orstavik RE, Neale MC, Torgersen S, et al. Major depression and dimensional representations of DSM-IV personality disorders: a population-based twin study. Psychol Med (2010) 40(9):1475–84. doi: 10.1017/s0033291709991954
61. Shedler J, Westen D. Refining personality disorder diagnosis: integrating science and practice. Am J Psychiatry (2004) 161(8):1350–65. doi: 10.1176/appi.ajp.161.8.1350
62. Orstavik RE, Kendler KS, Czajkowski N, Tambs K, Reichborn-Kjennerud T. The relationship between depressive personality disorder and major depressive disorder: a population-based twin study. Am J Psychiatry (2007) 164(12):1866–72. doi: 10.1176/appi.ajp.2007.07010045
63. Ryder AG, Schuller DR, Bagby RM. Depressive personality and dysthymia: evaluating symptom and syndrome overlap. J Affect Disord (2006) 91(2-3):217–27. doi: 10.1016/j.jad.2006.01.008
64. Huprich SK. Considering the evidence and making the most empirically informed decision about depressive personality disorder in DSM-5. Pers Disord (2012) 3(4):470–82. doi: 10.1037/a0027765
65. Huprich S. New directions for an old construct: Depressive personality research in the DSM-5 era. Pers Ment Health (2013) 7(3):213–22. doi: 10.1002/pmh.1217
66. Altamura AC, Buoli M, Caldiroli A, Caron L, Cumerlato Melter C, Dobrea C, et al. Misdiagnosis, duration of untreated illness (DUI) and outcome in bipolar patients with psychotic symptoms: A naturalistic study. J Affect Disord (2015) 182:70–5. doi: 10.1016/j.jad.2015.04.024
67. Sher KJ, Trull TJ. Substance use disorder and personality disorder. Curr Psychiatry Rep (2002) 4(1):25–9. doi: 10.1007/s11920-002-0008-7
Keywords: personality disorder, major depressive disorder, anxiety disorders, co-morbidity, China
Citation: Zheng Y, Severino F, Hui L, Wu H, Wang J and Zhang T (2019) Co-Morbidity of DSM-IV Personality Disorder in Major Depressive Disorder Among Psychiatric Outpatients in China: A Further Analysis of an Epidemiologic Survey in a Clinical Population. Front. Psychiatry 10:833. doi: 10.3389/fpsyt.2019.00833
Received: 23 April 2019; Accepted: 21 October 2019;
Published: 12 November 2019.
Edited by:
Yuan-Pang Wang, University of São Paulo, BrazilCopyright © 2019 Zheng, Severino, Hui, Wu, Wang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jijun Wang, amlqdW53YW5nMjdAMTYzLmNvbQ==; Tianhong Zhang, emhhbmdfdGlhbmhvbmdAMTI2LmNvbQ==
 Yuchen Zheng
Yuchen Zheng Francesca Severino
Francesca Severino Li Hui3
Li Hui3 Jijun Wang
Jijun Wang Tianhong Zhang
Tianhong Zhang