- 1Department of Educational Sciences, University of Catania, Catania, Italy
- 2Vascular Surgery and Organ Transplant Unit, University Hospital of Catania, Catania, Italy
- 3SIPsiTO, Italian Society of Psychology and Psychiatry of Organ Transplants, Catania, Italy
- 4Department of General Surgery and Medical-Surgical Specialties, University of Catania, Catania, Italy
- 5Department of Surgery, Transplantation and Advanced Technologies GF Ingrassia, University of Catania, Catania, Italy
- 6Clinical Psychology and Psychotherapy Unit, San Martino Hospital—Genoa, Genoa, Italy
- 7University Hospital, City of Health and Science, Turin, Italy
- 8Department of Mental Health, Bergamo Local Health Authority, Bergamo, Italy
- 9Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy
Kidney transplantation is a serious event that involves profound psychological, relational and social changes both for the patient and his family context. Assessment of personality profile, awareness of disease, family and social support of the patient candidate for kidney transplantation are necessary because factors not adequately considered, can influence the success of the transplant and alter the psychological stability of the patient. The present study aims to provide a systematic review of the literature of the last twelve years (2006–2018), focusing in particular on patient’s readiness level and illness management and on possible psychopathology. Sixty-two studies were examined. Based on the Downs and Black checklist, most studies (n = 32) were of high quality; 15 of which related to lifestyle, health education, and therapeutic adherence in post-renal transplantation, 17 studies concerned the possible existence of psychopathology and cognitive impairment of renal deceased transplanted subjects. The literature used has shown that the population of kidney transplant patients is exposed to a high risk of psychiatric disorders with repercussions on the quality of life and the risk of rejection. Therefore, an adequate pre-transplant psychosocial assessment is necessary, which allows a more in-depth knowledge of the candidate to plan coping strategies and possible post-transplant psychotherapy.
Introduction
Kidney transplantation is a valid treatment option for end-stage renal disease, the only one capable of correcting, in addition to the emuntory function, also metabolic, hematological and endocrine abnormalities, allowing most patients to obtain a better quality of life (1–6).
Despite the progress of medical science and technology in this field, remain problems that affect the amount of transplants implemented as well as their success. In addition to the insufficient number of organs donated by deceased or living donors, one of the main difficulties is the management of the pre- and post-transplant pathways, often exclusively medical-surgical, which excludes the importance of integrity between mind and body. Transplantation is a very demanding and particularly stressful event that requires the patient to implement his bio-psycho-social skills in order to accept and integrate the new organ physically and mentally. This surgery, therefore, involves numerous psychological, existential, affective, relational, and social changes both for the patient candidate and for his family context. (7–9).
In transplantation, surgery allows rapid functioning from the anatomical and physiological point of view, but cognitive and emotional integration is also necessary (“psychological transplant”) (10–12).
Surgery such as transplantation is a time of great stress that threatens the sense of continuity and personal integrity, causing strong emotions and can alter one's personal identity, with the possible onset of psychopathology and psychosocial problems (10, 13–15).
The psychopathology or insufficient internal and external resources of the subject can lead to a poor adherence to post-transplant pharmacological treatment, greater probability of rejection, and greater probability of beginning of organic pathology (16, 17).
The term adherence refers to the concept of continuity to medical prescription (drugs, diet, lifestyle) and patient satisfaction. In this perspective, adherence is understood as a sharing based on the therapeutic “alliance” between doctor and patient respecting the needs of both. The term compliance, on the other hand, represents the patient's obligation to follow drug therapy and therefore assumes a negative connotation (18).
In this context, it is necessary to evaluate the psychological profile and the personality of the patient who is a candidate for kidney transplantation in order to prevent factors that are not adequately monitored from influencing the positive outcome of the surgery or causing emotional disorders for the subject himself (15–21). At the same time, the evaluation of the family and the social context, of which the patient is a part, play a fundamental role. This allows us to investigate whether the family environment is favorable in terms of social, material and emotional support for the candidate, and through the analysis of communication between the various family members, it allows us to understand the fears of the path undertaken both in the pre that in the post intervention (22, 23).
Recent literature shows that patients who receive psychotherapy support in the pre- and post-transplant areas improve treatment compliance and limit possible anxiety and depression. Patients seem to recover a significant quality of life with changes in physical aspects but to an even greater extent in emotional and psychological ones (4, 22).
Regarding the close relationship between psychopathology and therapeutic adherence, De Pasquale et al. (24), examining the literature, analyzed the psychopathological aspects in kidney transplantation, affirming that the presence of a multidisciplinary team allows the transplanted patient greater adherence to therapy, the use of new coping strategies and the adoption of more appropriate lifestyles.
The aim of the present paper is to offer a systematic review of the literature of the last twelve years (2006-2018), on the psychopathological and psychological aspects and on awareness disease of adult kidney transplant subjects. Since the psychopathological complications, if present in the kidney transplanted subject, represent a risk factor for non-adherence to the treatment, the authors intend to analyze whether a correct psychological, psychiatric evaluation in pre and post transplantation and patient support interventions for the disease management, can improve long-term transplantation results, avoiding non-adherent behaviors and negative outcomes such as rejection. A well-structured assessment which includes information regarding the personality, possible psychopathology, the experience of illness and the motivation to transplant, could thus be used as a basis to guide experts in the sector towards a homogeneous clinical activity, and identifying most appropriate treatment for a “best practice” (25).
Methods
Data Source and Selection Criteria
A literature search has been performed following the main research items reported in literature during last 12 years. The literature was examined using the preferred reporting items for systematic reviews and meta-analysis (PRISMA), a checklist of 27 items based on the Cochrane Consumers and Communication Review model (26).
The following keywords have been selected for research: “(self-efficacy, coping, health education, anxiety, depression, psychopathology, awareness diseases, social support, family support, quality of life, body image, adherence, compliance, psychosis, personality disorders, sleep disorders, neuropsychological disease) and (kidney transplant).”
For the research we used databases such as: MEDLINE, Scopus, Embase, PsycINFO and Cochrane Library which combine free terms and controlled terms (MeSH: Medical Subject Headings).
The topics chosen to deepen the study referred to the 4 domains of the Stanford Integrated Psychosocial Assessment for Transplantation (SIPAT) (27) that is: 1. “Patient’s readiness level and illness management;” 2. “Social support system level of readiness;” 3. “Psychological stability and psychopathology;” 4. “Lifestyle and effect of substance use.” SIPAT is a reliable tool that allows us to predict the psychosocial outcome of transplantation (positive or negative), its strength is the standardization of its evaluation process (27).
Only full/text manuscript concerning clinical studies on adult (>18 years) deceased donor kidney transplantation published in peer-reviewed journals in English between January 2006 and December 2018, were included in the selection.
The reference lists of the articles included in the review have been checked manually by several independent authors (CDP, MLP, LI, MV) for the selection of the most relevant studies. Moreover, members of the Board of Directors of the Italian Society on the psychological and psychiatric aspects of organ transplants (SIPSITO) were also contacted as experts in the field (PZ, LB, GB).
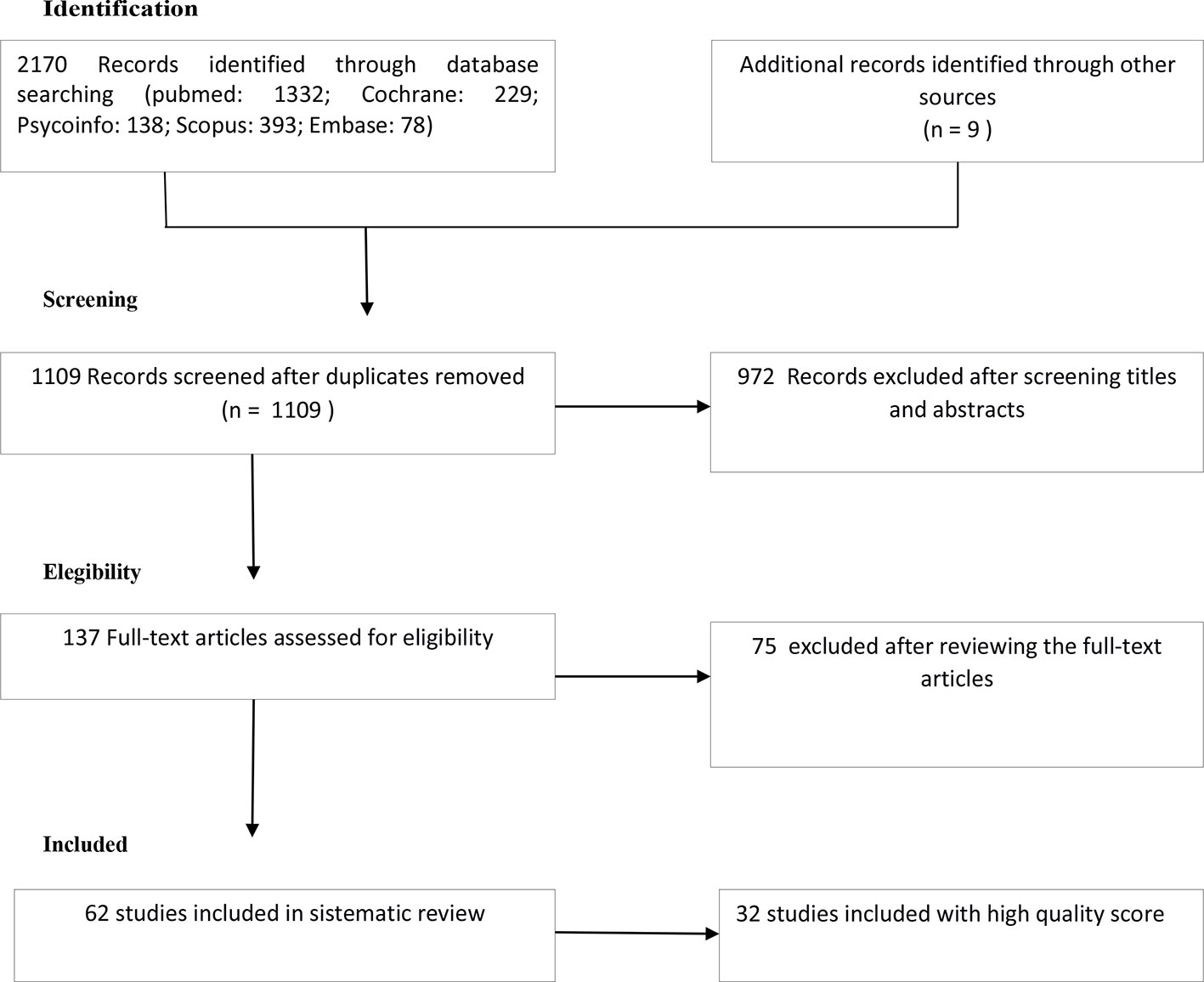
Exclusion criteria included non-English documents, studies that included adolescents or children (age < 18 years) and articles with no abstract or incomplete results. Figure 1 summarizes the research strategy used to select the studies (identification, screening, eligibility, inclusion process) in the critical review.
Recorded Variables
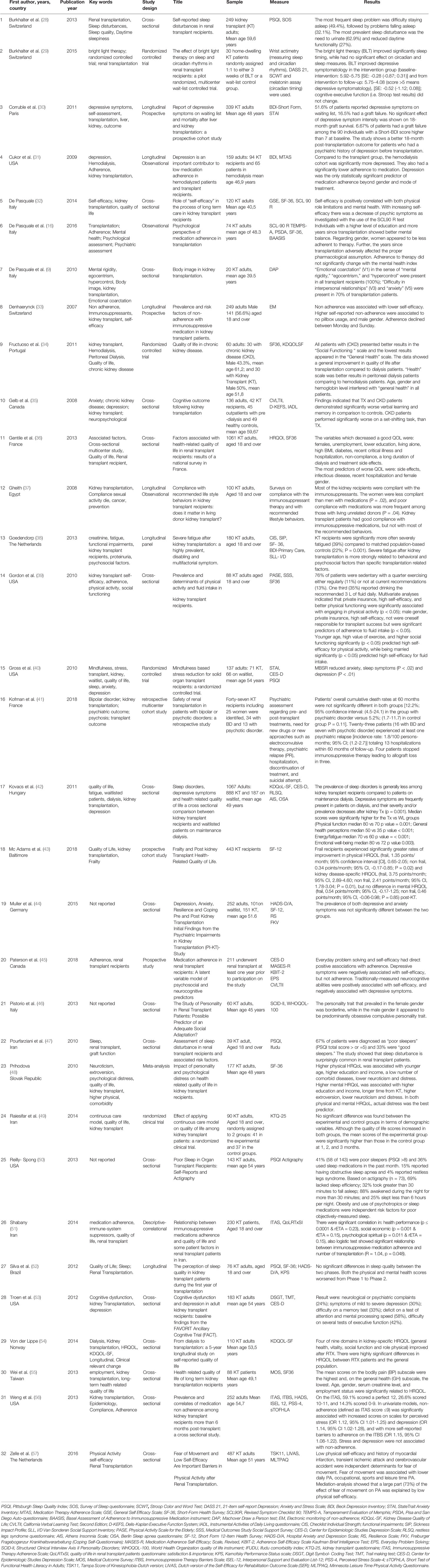
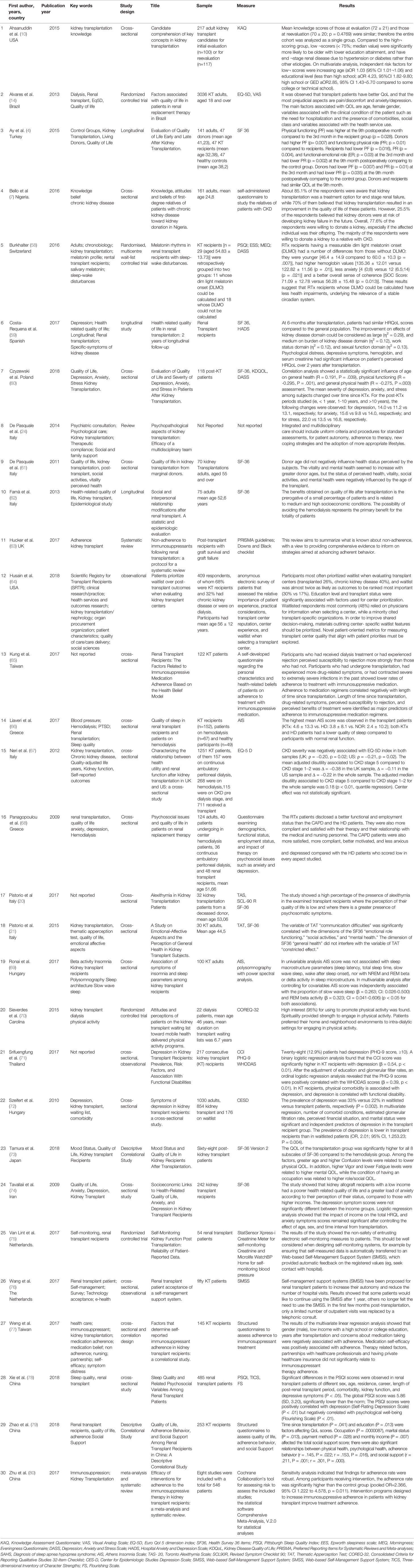
The variables recorded for each article included in the review were: author (s), year of publication, country, keywords, study design, title, sample (age, gender), measurements, results (Tables 1 and 2), quality score (Table 3).
Quality Score and Quality Differentiation
Performing a meta-analysis seemed inappropriate due to the heterogeneity of the included studies, the authors decided pragmatically to categorize the outcome measures in outcome domains on the basis of consensus among study authors (CDP, MLP, MV, AG, PV) and they sorted two domains according to the criteria of the SIPAT (Stanford Integrated Psychosocial Assessment for Transplantation): “patients’ readiness level and illness management;” “psychological stability and psychopathology” (SIPAT domains 1 and 3) (27). These two domains represent the most important aspects of recent literature on deceased donor kidney transplantation, psychosocial factors and patient’s therapeutic adherence.
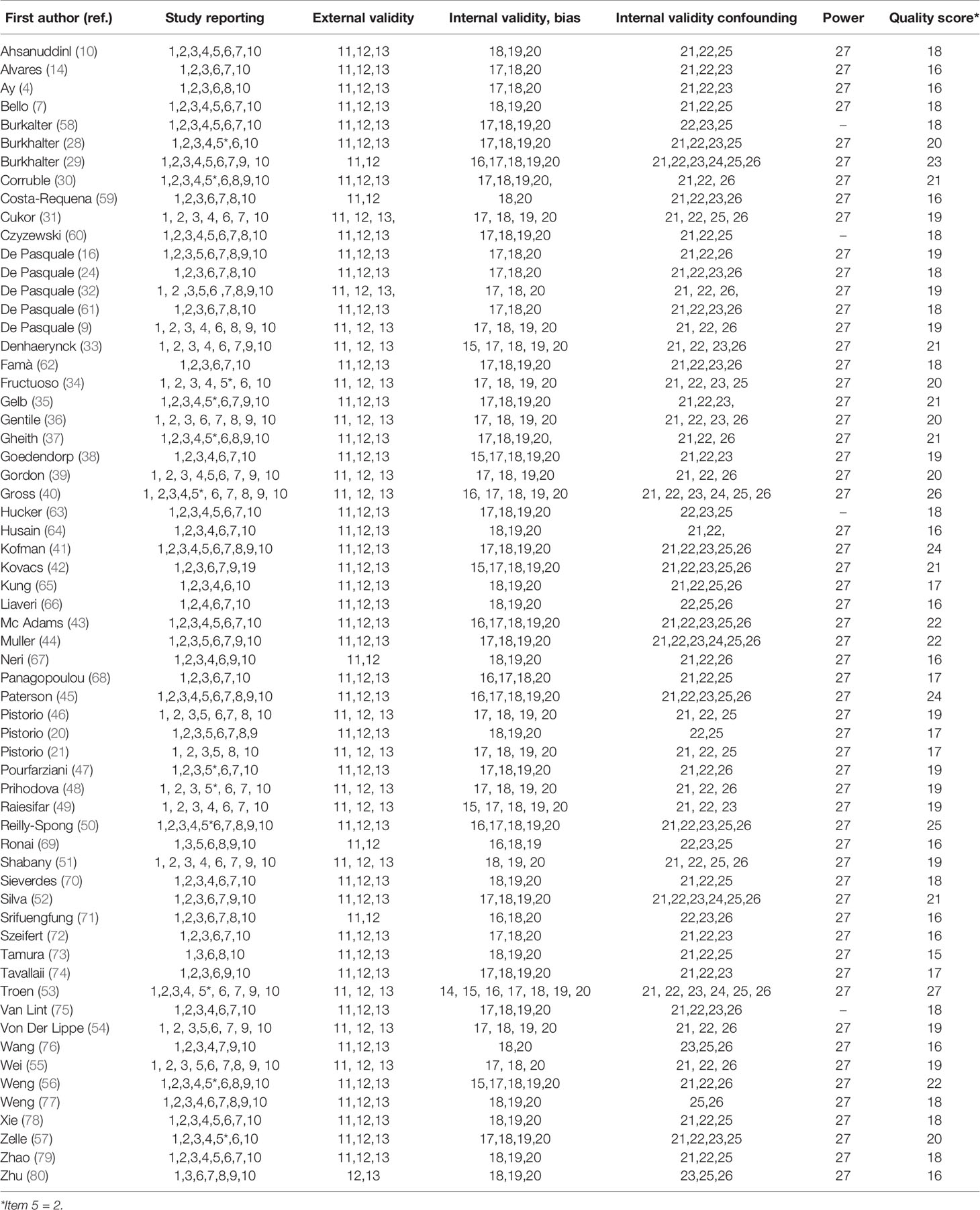
The quality of the studies was assessed independently by the CDP, MLP, LI reviewers using the “Downs and Black checklist for non-randomized studies” (81). The Downs and Black checklist is composed of 27 items distributed over five sub-scales: “reporting” (10 items), which verifies that the data in the document comes from an impartial evaluation of the results of the study; “external validity” (3 items), which measures the possibilities of generalization of the study to the reference population; “bias” (7 items), which measures the possibility of “bias” in the results of the study; “confounding” (6 items), which dealt with the “bias” in selecting the study participants; “power” (1 item), which allows to evaluate possible study errors due to chance. Responses are assigned 0 or 1, with the exception of item 5, which can get a score from 0 to 2. The maximum total score was therefore 28 (81). Since the checklist is not a classification to distinguish between low and high quality studies, consequently we defined a study with a score ≥ 19 a priori as being considered of high quality, reflecting two-thirds of the maximum score, such as reported in the literature (82).
Results
Number of Studies Found in the Selection of Studies
The PUBMED search generated 1,332 articles and 838 additional articles were found through the Cochrane, Psychoinfo, Scopus, Embase databases. The combined search strategy collected a total of 1,109 articles after removing duplicates. 137 full-text articles were evaluated for suitability with respect to inclusion and exclusion criteria after the exclusion of 972 registrations after the revision of titles and abstracts. Of these, 75 were removed after reviewing the full-text articles, as they did not contain primary quantitative data, contained duplicate data or otherwise fulfilled the exclusion criteria (Figure 1). Therefore, 62 articles were admitted in the systematic review. In Table 1 we reported the high quality studies (score ≥ 19), presented in detail in the text. Table 2 shows the low quality studies (score ≤ 19).
Quality Score Results
The results of the quality assessment using Downs and Black checklists are shown in Table 3. Thirty-two articles were classified as high quality with an average score of 20.91; fifteen concerned patients’ readiness level and illness management with an average total score of 19.67; seventeen studies concerned psychological stability and psychopathology with an average total score of 22.
Patient’s Readiness Level and Disease Management
A total of 30 studies investigated patient’s readiness level and illness management, 15 of them were high-quality studies and will be described.
Personality Factors and Therapeutic Adherence
Adherence to post transplant immunosuppressive therapy is of fundamental importance for the long-term survival of the graft. Personality factors can diversify the emotional response to transplantation and the clinical course of post-transplant patients. A wider perception of the personality of these patients is essential for favorable outcomes for kidney transplantation.
The study of Pistorio et al. (46) shows that personality traits, such as borderline (BP) and obsessive-compulsive (OCP), are predictors of low social adaptation in transplanted patients. The authors explored personality traits in 60 deceased donor kidney transplant recipients, with the “Structured Clinical Interview Axis II Personality Disorders” (SCID-II) for “Diagnostic and Statistical Manual of Mental Disorders fourth edition” (DSM-IV R). The OC personality trait and quality of life correlate negatively (Pearson r correlation) (r = -0.401; p < 0.05). The obsessive personality trait was more present in the male subjects, while the borderline personality trait was found more in the female subjects. These subjects showed a low level of general health (r = -0.188; p < 0.05) and difficulties in interpersonal relationships (r = -0.147; p < 0.05). The study suggests that personality traits are a good indicator of quality of life. In this study, early identification, with adequate assessment, of subjects transplanted with behavioral problems is required to provide them with adequate psychological-psychiatric support during follow-up.
Prihodova et al. (48) studied the impact of some personality factors (neuroticism, extroversion and psychological stress) on the “health-related quality of life” (HRQOL) of 177 patients with renal transplantation. “Short Form Health Survey” (SF-36) was used to study quality of life. Personality factors were studied using the Eysenck Personality Questionnaire Revised-Abbreviated (EPQR-A) and to identify psychological stress, the General Health Questionnaire-12 (GHQ-12) was used. Data analysis showed that high scores in the physical component of quality of life are associated with young age (p value ≤ 0.001), higher education level (p value ≤ 0.05) and low scores on the “neuroticism” factor (p value ≤ 0.005) and psychophysical stress (p value ≤ 0.001). High scores on the SF-36 mental health index were associated with a greater presence of extraversion (p value ≤ 0.05) and a low presence of neuroticism (p value ≤ 0.001) and psychological stress (p value ≤ 0.001). In summary, the study shows, with reference to the literature data, that high psychological stress can cause low quality long-term life in transplanted subjects and contributes considerably to the presence of somatic symptoms in these patients.
The study of Cukor et al. (31) compared patients with end-stage renal disease (ESRD) including both kidney transplant recipients and subjects undergoing hemodialysis (HD) treatment on psychological-emotional evaluations and adherence to therapeutic treatments. Ninety-four patients undergoing functional renal transplantation and 65 hemodialysis patients completed the evaluation (total participants 159). The questionnaires used were: Beck Depression Inventory-II (BDI) to measure possible depression; Immunosuppressive therapy adherence scale-medication (ITAS-M) to assess adherence to immunosuppressive therapy.
The results showed that a greater presence of depressive symptoms corresponded to a lower therapeutic adherence in the sample of hemodialysis subjects (r = -0.47, p value = 0.001), in the sample of transplanted subjects (r = -0.38, p value = 0.001) and in the whole sample (r = -0.47, p value = 0.001).
In a prospective study, Denhaerynck et al. (33) assessed and comprehensively tested the possible risk factors for nonadherence in 249 kidney transplant patients using cutting-edge measures. This study included patients who had undergone kidney transplantation for at least one year, over the age of 18 years. Non-adherence to immunosuppressive therapy was assessed using an electronic measuring instrument: MEMS®-V Track-Cap (Aardex Group, Switzerland).
Some significant variables were examined, potentially related to a good therapeutic adherence: self-efficacy with the use of drugs, using the Long-term Medication Behaviour Self-Efficacy Scale; representations of the disease, according to the Siegal scale of 10 elements; The coping was evaluated by the Utrecht Coping List (UCL); The authors also measured depressive symptoms using the Beck Depression Inventory. The results of the study showed that the most significant risk factors are: young age [odds ratio (OR) = 0.96; q-value (q) = 0.02], male gender (OR = 0.37; q value = 0.02), low self-efficacy (OR = 0.24; q value = 0.02), high self-reported non-adherence (OR = 4.34; q value < 0.001), hectic lifestyle (OR = 2.3; q value = 0.03). To conclude, the authors underline how important it is to analyze the variables useful for detecting non-compliance or to improve adherence.
De Pasquale et al. (16) evaluated the possible psychopathological variables responsible for non-adherence behaviors in 74 kidney transplant patients. For the psychological-psychiatric evaluation the following tests were used: Symptom checklist 90—revised (SCL-90 R) to evaluate the psychological symptomatology, Temperament Evaluation of Memphis, Pisa and San Diego Questionnaire (TEMPS-A) for the study of the personality and temperament, the Short Form Health Survey (SF-36) to assess mental health score (MIS), Basel Assessment of Adherence to Immunosuppressive Medication instrument (BAASIS) for assessing adherence to the immunosuppressive drug. Analysis of the data showed that the subjects most educated and transplanted the longest had good level of mental health “(Education, E/MIS r = 0.61; Years from transplantation, YT/MIS r = 0.48).” The female gender was less adherent to therapy, while the perceived state of mental health did not affect adherence “(MIS/BAASIS total score, BT r = -0.01).” The cyclothymic (CT), irritable (IT), and depressive (DT) temperament was negatively correlated with therapeutic adherence “(BT/CT r = 0.39; BT/IT r = 0.44; BT/DT r = 0.21).” Significant associations (p value < 0.05) emerged among some predictors (gender, post-transplant years, anxiety and cyclothymic temperament) and the outcome variable (BT). Through this study, the authors proposed cognitive pathways and psychotherapy for a better adaptation of transplanted subjects and to guarantee a good post-transplant quality of life. In this context, the study of post-transplant quality of life becomes essential.
Self-Perceived Health and Post-Transplant Lifestyles
In kidney transplanted subjects it is important to deepen the perception of one's health. The subject in the immediate post transplant must be helped to plan self-efficacy and resilience skills, necessary to achieve a correct lifestyle for the maintenance of the transplanted organ.
Fructuoso et al. (34) examined the concept of quality of life, subjectively perceived, in 4 groups of patients: thirty of the 821 patients with chronic kidney disease (CKD) in stage 1–4, 30 of 117 kidney transplanted patients (KT), 37/43 in hemodialysis patients (HD) and 14/17 in peritoneal dialysis (PD). Two tests were administered to the subjects: short Form-36 (SF-36) and “kidney disease and quality of life—short form” (KDQOL-SF). The four groups achieved better results on the “social functioning” scale “(77.68 ± 18.46 in PD; 74.17 ± 29.53 in KT; 66.81 ± 31.39 in CKD 1 -4; 62.16 ± 32.84 in HD; p value = 0.192).” Non-significant scores were found in the “General Health” scale of the physical health component “(39.92 ± 19.12 in CKD; 45.95 ± 21.56 in HD; 47.13 ± 23.15 in KT; 51, 79 ± 18.89 in PD; p value = 0.321).” Specifically, this study confirms the importance of assessing post-transplant quality of life as it allows physicians to monitor the patient's self-perceived health and improve their adherence to treatment.
Gentile et al. (36) emphasized which variables may be needed to improve adherence to treatment such as: providing more detailed medical examinations, explaining immunosuppressive therapy and highlighting side effects, maintaining an adequate lifestyle, a healthy diet. The authors conducted a cross-sectional multicenter study with 1061 kidney transplant patients in France. For the evaluation of health-related quality of life (HRQOL), the “Short Form-36 health survey” (SF-36) and a questionnaire for “Recipient transplant quality of life” (RTQOL) were administered. The variance explained in the SF-36 regression models varies from 20 to 40% and from 9 to 33% for RTQOL. The study highlights how a careful evaluation of the socio-demographic variables (women, unemployment, lower education, life alone, high body mass index) and clinical aspects (diabetes, hypertension and hospitalization, a long duration of dialysis and side effects of treatment) are essential to optimize HRQOL.
Gheith et al. (37) focus on necessity of a good therapeutic adherence for the maintenance of the graft in the post-transplant. In particular, a questionnaire was administered, identified as a reliable method for the assessment of non-compliance, divided into two parts: the first part relating to demographic data and patient history, the second part relating to knowledge and awareness of the behavioral lifestyle recommended for subjects with kidney transplantation. Specifically, the second part included questions about: immunosuppressive therapy (dosages, regular intake, forgetfulness, side effects); nutrition (number of daily meals, presence of refined foods, etc., monitoring of body weight, control visits, infection prevention, physical activity, smoking, sun exposure, and sexual activity). From 22 to 48%, higher rates of non-compliance with immunosuppressive drugs have been reported. Any differences in compliance can be attributed to the length of the post-transplant time, age, gender and nature of the donor. A better adherence was found in subjects receiving the organ from a family donor (p value = 0.04). Analysis of the data showed that men were significantly more complier with drugs (p value = 0.02), while women were more compliant with recommended diets (p value = .03). In the case of infection prevention, the adhesion of the subjects to the measures to be adopted was partial (57%). Only 9% of patients avoid exposure to the sun. Regarding smoking, only 29.4% quit smoking after the transplant. Concerning sexual activity, 30% of subjects consulted the nephrologist for sexual problems. As far as physical activity are concerned, only 23% of the patients examined regularly practiced physical activity. In summary, kidney transplant patients examined in this study observe better adherence to drug therapy and less adherence to the suggested healthy lifestyle. Therefore the authors point out the need of a psychoeducational course of preparation for transplantation. Fundamental is the role assumed by the nurse who must provide patients undergoing a renal transplant the right knowledge of recommended lifestyle with the family support.
The study of Zelle et al. (57) analyzed the “fear of movement” related to daily “physical activity” (PA) in 487 renal transplant patients (RTR). The “Tampa Score of Kinesiophobia—Dutch Version” (TSK-11) was administered to evaluate the “fear of movement.” The Dutch translation of the “perceived physical activity scale” (LIVAS scale) was used to assess the perceived physical activity. Analysis of the data showed that subjects with a lower perception of their state of mental health had a greater “fear of movement” (p value = < 0.001), while the levels of physical self-efficacy were much lower (p value = < 0.001). The higher the scores on “fear of movement” in kidney transplanted subjects, the less physical activity was present daily (r = -0.22; p value < 0.001). The fear of movement was also associated with employment (r = -0.16; p value = 0.001), with sport (r = -0.12; p value = 0.01) and with free time PA (r = -0.12; p value = 0.02). This study demonstrates the importance of planning strategies to reduce fear of movement and optimize post-transplant physical activity for long-term maintenance of the graft.
Gordon et al. (39) observed the physical activity of kidney transplant patients, adherence to fluid intake recommendations and subjective behaviors related to psychophysical well-being. Semi-structured interviews on kidney transplant patients were carried out by telephone or in person within 2 months of transplantation. 90 out of 158 (57%) patients participated. The “Physical activity scale for the elderly” (PASE) questionnaire was used to assess physical activity. The PASE is a 21-element tool that evaluates physical activity in some areas: leisure sports, home activities, such as vacuum cleaners or lawn work and other activities, such as walking or using machinery in the last 7 days. Through the short form health survey (SF-36) the relationship between physical and mental health was assessed while the social support received, through the Medical Outcomes Study “Social Support Survey” (SSS). Analysis of the data showed that the majority of subjects (83%) were adherents regarding fluid intake, while half of the subjects (49%) reported high adherence to physical activity. It was shown that subjects of younger age and those with adequate social activities had greater self-efficacy with respect to physical exercise (r = 0.42; r = 0.30 p value < 0.01). The authors suggest that educational strategies should also focus on strengthening the sense of self-efficacy, thus stressing the importance of new information practices. This is particularly relevant as recent legislation states that “educational services” for subjects suffering from a renal disease are an indicator of improved quality of life.
Post-transplant Quality of Life Indicators
The in-depth analysis of various aspects of quality of life is necessary for monitoring transplanted patients and predicting results. The evaluation of the quality of life as an outcome measure of a solid organ transplant is an important tool, since it allows to highlight indicators of the general state of health useful for implementing any suitable treatments (medical, rehabilitation, psychological support) and getting the best from transplant surgery.
Kovacs et al. (42), through the cross-sectional observational study, state that kidney transplant patients (Tx) have a much better quality of life than patients on waited list (WL). Eight hundred eighty-eight transplant subjects and 187 subjects on the waiting list were studied. Quality of life studied with the Kidney Disease Quality of Life-Short Form (KDQoL-SF). The sub-scales evaluated were: “Physical functioning,” “General health perceptions,” “Energy/fatigue,” and “Emotional well-being.” Median scores were significantly higher for the Tx vs WL groups “(median physical function 80 vs 70 p value = 0.001; general perceptions on median health 50 vs 35 p value < 0.001; median energy/fatigue 70 vs 60 p value = < 0.001; emotional well-being median 80 versus 72, p value 0.003).” The symptoms of depression and the possible presence of sleep disorders were studied through the “Center for Epidemiologic Studies Depression” questionnaire (CES-D) and the “Athens Insomnia Scale” (AIS). Sleep disorders are less present in transplanted subjects compared to those on dialysis. Depressive symptoms are quite frequent in the subjects studied, but this symptomatology decreases after the kidney transplant (p value = 0.001). The authors suggest the importance of assessing quality of life after kidney transplantation.
Raiesifar et al. (49) conducted a three-month randomized clinical trial involving 90 kidney transplant patients divided into two groups: the treatment group included sessions to make the patient aware of the disease, even with the presence of family members, through lessons, informative and educational material on the transplant pathway, creating a need for follow-up. Instead, no specific intervention was performed in the control group. The “kidney transplant questionnaire” (KTQ-25), a designated tool for assessing quality of life in kidney transplant patients, was administered. The dimensions analyzed were: physical symptoms, fatigue, appearance, fear, and emotional insecurity. The scores on the questionnaire were high in the two groups of subjects, but the scores of the subjects belonging to the experimental group were considerably higher than those of the control group at 3 months. The mean total scores of KTQ-25 were 87.0 ± 6.2 (treatment group) and 88.0 ± 5.5 (control group) (p value < .001). This study underscores the importance of the continuing care model's effect on routine quality of life care among kidney transplant patients.
In a longitudinal study, von der Lippe et al. (54) evaluated changes in “health-related quality of life” (HRQOL) of subjects on dialysis compared to kidney transplant recipients in a cohort of 110 patients. HRQOL was observed through the “Kidney disease and quality of life-short form” (KDQOL-SF). General health improved after kidney transplantation (RTX), respectively from 58 ± 20 to 68 ± 21, p value < 0.001. In particular, it was found that with transplantation, younger subjects had better social relationships than older subjects (p value = 0.035). In general, the authors of the study showed an improvement in the quality of life in transplanted subjects compared to subjects on dialysis.
In a cross-sectional study of correlational design, Wei et al. (55) evaluated the “health-related quality of life” (HRQOL) of 88 kidney transplant (KT) subjects using the eighth SF-36 subscales: “Physical functioning” (PF), “physical role” (RP), “body pain” (BP), “vitality” (VT), “general perception of health” (GH), “social functioning” (SF), “emotional role” (RE), and “mental health” (MH). The results showed that with increasing age the scores in the subscales PF, RE, and BP decreased (r = -0.25, p value = 0.021; r = -0.21, p value = 0.047; r = -0.22, p value = 0.04, respectively). Scores on the PF subscale were lower in women than in men (76.2 versus 85.1, p value = 0.038). The subjects employed showed better scores at many subscales of the questionnaire compared to subjects not employed: PF (83.7 versus 73.8, p value = 0.034), RP (76.3 versus 52.4, p value = 0.013), GH (63.6 versus 51, 6, p value = 0.012), RE (78.3 versus 54.8, p value = 0.016), and MH (71.6 versus 63.3, p value = 0.039). The study reaffirms the importance of “health-related quality of life” (HRQOL) for a long-term compliance in kidney transplant subjects.
Shabany Hamedan and Mohamad Aliha (51) measured the relationship between adherence to immunosuppressive therapy and “quality of life” in 230 kidney transplant subjects. The “Immunosuppressant Therapy Adherence Scale” (ITAS) was used to assess adherence to immunosuppressive drugs. The questionnaire related to the study of quality of life has measured four dimensions: health/performance, socioeconomic, psychological/spiritual, family. The two questionnaires were completed by the patients. Evaluating adherence to immunosuppressive drug therapy, it was noted that adherence improved with older patients compared to younger ones [p value = 0.049, Chi-squared test (X²) = 8.873]; furthermore, it is negatively correlated with the time elapsed since transplantation (p value = 0.041, X² = 9.948) and with the amount of transplants performed (p value = 0.036, X² = 4.376). Data analysis pointed out that patients who adhered had a desirable quality of life: “health performance” [p value ≤0.0001 and correlation ratio eta (rETA) = 0.23], “socio-economic” (p value = 0.001 and rETA = 0.15), “psychological-spiritual” (p value = 0.011 and rETA = 0.15). Through this study the authors stressed that a good therapeutic adherence, should be an essential objective in the care of kidney transplant patients.
Psychological Stability and Psychopathology
A total of 32 studies investigated psychological stability and psychopathology, 17 of them were high-quality studies and will be described.
Mental Distress and Psychological Symptoms
Kidney transplantation is an established treatment for end-stage kidney disease. However, it is a complex psychological experience that can generate mental distress and psychopathology. The affective profile in transplant patients should be examined in depth to highlight all the facets in their mental and emotional evaluation, which can represent easy barriers to treatment in post-transplantation.
De Pasquale et al. (9) explored behavioral and adaptation difficulties in kidney transplant patients through a graphical test: “Machover Draw-a-person test,” as the transplanted patient communicates with difficulty his deeper psychological contents. The variables emerging from the Machover Test regarded: “emotional coarctation” in 100% of the sample, “difficulty in interpersonal relationships and “anxiety” in 70% of the sample. The study showed that the design of the human figure (projective method) was useful for identifying and studying possible mental distress in post-transplant follow-up.
De Pasquale et al. (32) studied psychopathology, self-efficacy and quality of life in 120 kidney transplant subjects. The “Symptom Checklist 90 Revised” (SCL-90 R) was used to assess psychopathology. Self-efficacy has been studied with the “General self-efficacy scale,” quality of life with the “Short Form Health Survey” (SF-36). High self-efficacy was associated with a reduction in psychological symptoms “(self-efficacy/somatization, r = 0.145; self-efficacy/obsession, r = 0.557; self-efficacy/depression, r = 0.547; self-efficacy/Anxiety, r = 0.445; Self-efficacy/hostility, r = 0.528; self-efficacy/paranoia, r = 0.646; self-efficacy/psychosis, r = 0.264).” Self-efficacy is also positively correlated with a good quality of life on SF-36 “(Self-efficacy/Limitations of the physical role, r = 0.376; Self-efficacy/mental health, r = 0.493).” The authors pointed out that mental health and psychophysical well-being of these subjects was correlated with a good personal self-efficacy.
Mc Adams et al. (43) studied fragility and the quality of life subjectively perceived in 443 kidney transplant patients (2014–2017) using the “Kidney Disease Quality Of Life short form” (KDQOL-SF) instrument. Fragility was assessed through five components: “weight loss;” “weakness,” “exhaustion,” “low physical activity,” and “slowed walking speed.” Three months after transplantation, despite the reduced physiological reserve, frail subjects experienced an improvement in physical component of health related quality of life (HRQOL) (p value < 0.001) compared to non-fragile subjects. The study showed that even a high-risk group such as fragile kidney transplant (KT) recipients could experience the benefit of better HRQOL with KT.
Kofman et al. (41) in a retrospective multicenter study analyzed the presence of bipolar disorder (BD) and psychotic disorder in pre-transplantation and their evolution in 5 years post-transplantation. Forty-seven patients were identified including 34 with BD and 13 with psychotic disorder. During post-transplant follow-up half of the patients underwent various hospitalizations, within 60 months of the follow-up, due to psychiatric relapse [(incidence rate: 1.8/100 people-months; 95% confidence interval (CI); (1.2–2.7)] with poor therapeutic adherence to immunosuppressive drugs. This study suggested the need for psychiatric follow-up after transplantation in patients with pre-transplant psychiatric diagnosis.
Cognitive Impairments and Depressive Symptoms
The study of cognitive functions in kidney transplant patients has shown cognitive deficits, in particular impairments in verbal memory and executive functions, often associated with mood disorders. These adverse effects can persist and have a negative impact on all aspects of life. Post-transplant cognitive assessment can therefore be used to develop cognitive rehabilitation programs and other interventions in compromised transplant subjects.
Gelb et al. (35) compared the cognitive functions of42 kidney transplant patients with those of 49 healthy controls and 45 patients with chronic renalfailure. Verbal memory was studied through the “California Verbal Learning Test—SecondEdition (CVLT-II);” Executive functions were studied with the “Delis-Kaplan ExecutiveFunction System (D-KEFS).” Data analysis showed that subjects with chronic renal failure havecompromised cognitive functions than healthy controls [Color-word interference: Cohen’s d (d) = -0.68; learning and memory: d = -0.95]. The data is similar in transplant patients that have showed more compromised cognitive functions than healthy controls with low scores on Color-word interference (d = -0.56) and on the task of learning and memory (d = -0.74).
Goedendorp et al. (38) analyzed “severe fatigue” in 278 kidney transplant subjects, and the relationship between fatigue (concentration problems, reduced motivation and activity) and psychopathology related to kidney transplantation, such as depressive symptoms and sleep disturbances. “Severe fatigue” was studied using the “Checklist Individual Strength (CIS)—Subscale Fatigue.” Depressive symptoms were studied with “Beck Depression Inventory—Primary Care (BDI-PC).” Sleep disorders have been studied with the “Sickness Impact Profile 8 (SIP) —Sleep-Rest Subscale.” The study showed that 151 subjects showed a positive correlation between “depression, sleep disorders and fatigue (odd ratio = 9.70 and 1.02; p value = 0.013 and ≤0.001).”
Paterson et al. (45) analyzed the relationships between cognitive functions, depression, and adherence in 211 participants through a multivariate statistical analysis. Adherence was measured using the “Medication adherence self-efficacy scale-revised” (MASES-R); the measurement of cognitive functions included the use of an assessment comprising: the “Kaufman Brief Intelligence Test” (KBIT-2), the “California Verbal Learning Test” (CVLT-II) and the “Delis-Kaplan executive function system” (D-KEFS). Depression was assessed through the “Center for Epidemiological Studies Depression Scale” (CES-D); The authors suggested the influence of depressive symptoms and neurocognitive abilities in modifying therapeutic adherence [χ² (degree of freedom df = 313) = 376.24, p value=.009].
Troen et al. (53) evaluated the prevalence of cognitive dysfunctions and depression in transplant patients. The cognitive dysfunctions were evaluated with a battery of tests to measure: attention, memory, mental processing speed, and executive function. Depressive symptoms were studied through the “Center for Epidemiological Depression Scale” (CES-D) questionnaire. 30% of 183 participants had symptoms of mild to severe depression (score from 16 to 22 or higher). In the case of cognitive dysfunction, it was found that 33% had difficulty with memory tests, 58% showed deficits in attention tests and mental processing speed and 42% showed difficulties in executive tests. The study confirms the possible co-presence of mood and cognitive disorders in kidney transplant patients and reiterates the importance of monitoring cognitive and emotional aspects in the care of these patients.
The cross-sectional study by Weng et al. (56) analyzed clinical factors (anxiety and depression) and non-adherence variables in 252 subjects with renal transplantation for more than six months. The “Immunosuppressant Therapy Adherence Scale” (ITAS) was used to observe the adhesion variables. The evaluation of the symptoms of anxiety and depression was studied by the “Hospital Anxiety and Depression Scale” (HADS), while the “Interpersonal Support and Evaluation List-12” (ISEL-12) and the “Perceived stress scale—4” (PSS- 4) for the assessment of perceived interpersonal support and stress. The results of the study showed a significant correlation between non-adherence, depression (HADS p value= 0.02), perceived stress (PSS-4 p value = 0.04), lower family income (p value = 0.004), and lack of employment (p value = 0.03). The study suggests the need to plan interventions for the treatment of perceived stress, depressive symptoms and anxiety in order to increase adherence among kidney transplant recipients.
The study by Corruble et al. (30) showed a significant association between depressive symptoms reporting on the waiting list and post-transplant outcome. The “Short Form of Beck Depression Inventory” (Short-BDI) was used to assess depression. At baseline 51.6% of the evaluated subjects (n = 339) had depression “(Short-BDI score of 4 or more).” After 18 months from transplantation only 6.67% of patients (n = 6) had a graft failure among the 90 individuals (Short-BDI score higher than 7 at baseline). The study showed that depressive symptoms are not significantly associated with a negative transplant outcome.
Muller et al. (44) in a cross-sectional study studied the presence of anxiety and depression using the “Hospital anxiety and depression scale” (HADS-D/A) in kidney transplant patients. Regarding depression, the mean HADS-D scores were 4.48 ± 2.96; regarding anxiety the mean HADS-A scores were 5.01 ± 4.04. In particular, the authors pointed out that the prevalence of depression and anxiety remains surprisingly constant in patients after kidney transplantation.
Sleep Disorders, Anxiety, and Depression
Poor sleep quality is common after kidney transplantation and is one of the factors that adversely affects patients' quality of life after transplantation. This problem is associated with greater medical comorbidity and also with a state of emotional fragility. Therefore it is necessary to monitor changes in sleep quality and analyze the variables (anxiety, depression, fatigue, pain) that affect sleep quality in the first years after kidney transplantation, as these disorders represent important risk factors for non-adherence to treatments.
The study of Gross et al. (40) showed the presence of depressive symptoms (38%), anxiety (39%) and sleep disturbances (42%) in 138 transplant patients.
sThe “State-Trait Anxiety Inventory (STAI)” was used to assess anxiety, the “Center for Epidemiological Studies—Depression Scale (CES-D)” to assess depression and the “Pittsburgh Sleep Quality Index (PSQI)” for sleep disorders. Recipients of kidney, kidney/pancreas (n = 72) were included in a program based on stress reduction techniques, a training program for mindfulness meditation (awareness-based stress reduction—MBSR). The remaining patients (n = 66) were included in a health education program. After 8 weeks, in subjects who had undergone the “MBSR” program, anxiety, depression, and sleep disorders had declined, while quality of life had improved “(p value < 0.01, all)” and the benefits were maintained at 1 year “(p value < 0.05, all).” Instead, the results relating to the health education program were modest and not lasting. The study highlighted the importance and effectiveness of a non-pharmacological intervention for the treatment of post-transplant psychiatric symptoms.
Burkhalter et al. (28) studied sleep disorders in 249 kidney transplant subjects (RTx) transplanted into three Swiss transplant centers, through self-report questionnaires (Survey of Sleep—SOS) and more structured interviews. This study showed the high incidence of insomnia in kidney transplant patients (49.4% of the evaluated subjects). In 62.9% of the subjects sleep disorders were associated with the need to urinate. The authors of the study underline how important is the research in this field and the treatment of sleep disorders in subjects undergoing kidney transplantation.
Burkhalter et al. (29) evaluated the effect of “bright light therapy” (BLT) on sleep disorders and depression in adult patients with kidney transplantation (RTx) more than 1 year and diagnosed with sleep—waking disorders (SWD). This study included 30 subjects with RTx randomly assigned: BLT group or control group. Research has shown the presence of “chronic insomnia” in 42.5% of the examined sample. The “Depression, Anxiety and Self-reported Stress—21 elements” (DASS 21) was used to evaluate depression. The results showed that BLT improved significantly sleep timing. Moreover, depressive symptoms improved in BLT group “(basic intervention: 5.92–5.75 [standard error (SE): -0.28 (-0.87; 0.31)]” with progressive improvement up to follow-up: “5.75–4.08 (score > 5 means depressive symptomatology),” “[SE: -0.52 (-1.12; 0.08)].”
Pourfarziani et al. (47) evaluated sleep disorders in 39 kidney transplant patients using the “Pittsburg Sleep Quality Index” (PSQI) to evaluate the quality of sleep. The results of the study showed that 67% of patients were diagnosed as “poor sleepers” (PSQI total score > 5). The study confirms that sleep disorders are surprisingly common in renal transplant patients.
Reilly-Spong et al. (50) studied the prevalence, characteristics and correlates of sleep difficulties in 143 subjects who underwent solid organ transplantation; the recipients of the kidneys included about half of the sample (77 out of 143). Sleep quality was expected to have moderate to strong correlations with symptoms of depression, anxiety, fatigue and pain. Sleep disorders were measured with the “Pittsburgh Sleep Quality Index” (PSQI), Anxiety with the “State-Trait Anxiety Inventory—State Version” (STAI); depression was measured by the “Center for Epidemiological Studies—Depression Scale” (CES-D), fatigue (vitality) and pain with the “Subscale Short-Form 36 version 2” (SF-36). All transplanted subjects studied had sleep disturbances correlated (Pearson r) with depression (r = 0.61), anxiety (r = 0.58), fatigue (r = -0.58) and pain (r = -0.49) (p value < 0.001, all). The authors concluded that sleep disturbances are present in transplanted subjects and they are not adequately treated, therefore it is necessary to deepen them adequately and provide, for these subjects, educational strategies for a good quality of sleep.
The prospective study by Silva et al. (52) showed a high incidence of sleep disorders, with anxiety and depressive symptoms in 76 patients who underwent kidney transplantation, without significant changes in the two evaluation times (phase 1: 3-6 months; phase 2: 12 -15 months, after transplantation). Poor sleep prevalence, assessed with the “Pittsburg Sleep Quality Index” (PSQI) was slightly increased in the second evaluation time (36.7% in phase 1 and 38.3% in phase 2). The presence of anxiety (p value = 0.113) and symptoms of depression (p value = 0. 432), measured with the “Hospital Anxiety and Depression Scale” (HADS), were not significantly different at the two phases. The study confirms the presence of sleep disorders, anxiety and depression in the short and long term post-transplant period.
Discussion
The data available to date suggest that pre and post- transplant screening process must include both a medical evaluation and a thorough psychological and psychiatric assessment for a better therapeutic adherence. Adherence is a very important issue in the medical care of kidney transplant patients (51). The life style and quality of life of a transplanted subject represent a key point, and it is essential to adhere to the therapy and prescribed behaviors (34, 79).
In the field of kidney transplantation, it is important to understand and be aware of the “seriousness” of the disease that caused the specific organ failure. However, it is necessary to realistically discuss what the transplantation means, to adequately inform the patient about transplant procedures and to support the willingness to face the surgery (10). Failure to adhere to immunosuppressive therapy may increase the risk of rejection of the transplanted organ and cause the loss of the latter. Non-adherence seems to be related to the complexity of medical prescriptions, the individual and clinical characteristics of the patient (personality traits, pre-transplant lifestyle including diet, physical activity, a long duration of dialysis) (36, 39, 46, 48). Moreover, it is important that the transplanted person accepts the support of their family and collaborates with the transplant team to adhere to the new lifestyle, such as the resumption of healthy exercise (37, 49, 57, 80). Also the return to work after a kidney transplant is an important indicator of psychophysical well-being (74, 83).
Organ transplantation is generally the last possible therapeutic act for chronic kidney disease and the process that precedes and follows its implementation subjects the patient to an important burden of psychological stress, with the possible appearance of psychopathology. The literature underline the need to evaluate, with adequate screening, the possible presence of psychopathology, such as anxiety, depression, cognitive impairment, sleep disorders in the kidney transplanted subjects, which can represent a negative factor for the good therapeutic adherence (42, 60, 72, 84).
Anxiety and depression are the most common disorders in kidney transplant recipients that may affect disease process and graft survival (12).
In the daily experience of transplanted patients, anxiety is a condition of alertness and apprehension that increases when infections occur, drug side effects and other conditions that expose the subject to a state of physical discomfort until the fear of rejection (44, 52).
Depressive episodes can manifest years after the transplant, when the subject has failed to plan adaptation coping strategies and he realizes that the transplant will not bring him back to the state of health that precedes kidney disease (38, 41, 71, 73).
In cases where depression reaches levels of clinical relevance, it would be good to treat it with antidepressant drugs and psychotherapeutic and supportive interventions and implement preventive education on patients and family members (40, 56).
Sleep disorders are very common in kidney transplant patients; the causes can regard demographic factors, lifestyles, disease-related factors, and social factors (28, 47, 52). If not adequately treated, they interfere with a good post-transplant quality of life and so they have recently stimulated interest of the researchers, with the need to investigate non-pharmacological interventions, such as “Bright light therapy” (BLT) (50, 58, 66, 69, 78).
Sleep disorders are less present in transplanted subjects compared to those on dialysis. Depressive symptoms are quite frequent both in transplanted and dialysis subjects, but this symptomatology decreases after the kidney transplant (42).
Often cognitive impairment is also found in kidney transplant patients. In particular those most analyzed in the reported studies concern: attention, visual spatial memory, working memory and problem solving (35, 53). It has been shown that cognitive disorders in kidney transplant recipients can influence therapeutic adherence (45, 85).
If the risk factors that could influence the correct approach to the therapeutic scheme are identified, it will be possible to optimize the patient's resources and at the same time establish a good therapeutic adherence (16, 33, 51, 56). In fact, following the transplantation, it is necessary that the patient actively participates in his own care pathway, through the regular intake of drugs, the correct maintenance of follow-up and the maintenance of a lifestyle in accordance with medical indications in order to allow him a satisfactory quality of life. It is essential that kidney transplanted subject be aware of the best quality of life (psychological well-being, general health, vitality) found after the transplant compared to the time of dialysis. It may happen that lack of awareness of the “change” and living a poorly recommended lifestyle endanger the survival of the graft (34, 54).
Psychiatric and psychological support is often necessary to favor the process of adaptation to transplant in the long term, since aspects of psychopathology have been analyzed by different authors in the post-transplantation, with results of lower levels of adherence (59, 61, 63, 65).
Future directions of research should focus on deepening all those factors (self-efficacy, awareness disease, social and family support, health education) that influence the transplant preparation pathway and post-transplant results (32, 80). Furthermore, the development of interdisciplinary interventions with the various specialists (surgeon, nephrologist, psychiatrist and psychologist) would be desirable to identify shared operational protocols for integrated care of the transplanted patient and also plan training and updating courses for the “health team” with particular attention to psychological, communicative and relational aspects (24, 62, 64, 67, 68, 70, 75–77).
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Author Contributions
CP, MP, VM, and MV contributed conception and design of the study. They participated in drafting the work. PZ, NB, GB, LI, AG, and PV have made substantial contributions to the conception of the work and interpretation of data. They participated in revising the work critically for important intellectual content. All authors contributed to manuscript revision, read and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank Italian Society on the psychological and psychiatric aspects of organ transplants (SIPSITO) for the comments and suggestions expressed.
References
1. Christensen AJ, Turner C., Smith TW, Holman J, Gregory MC. Health locus of control and depression in end-stage renal disease. J Consult Clin Psychol (1991) 59:419–24. doi: 10.1037/0022-006X.59.3.419
2. Witzke O, Heemann U, Thesing A, Wolfhard U, Erhard J, Philipp T, et al. A comparison of EMIT and FPIA methods for the detection of cyclosporin A blood levels: does impaired liver function make a difference? Eur J Clin Pharmacol (1997) 52:413–6. doi: 10.1007/s002280050311
3. Johnson DW, Herzig K, Purdie D, Brown AM, Rigby RJ, Nicol DL, et al. A comparison of the effects of dialysis and renal transplantation on the survival of older uremic patients. Transplantation (2000) 69:794–9. doi: 10.1097/00007890-200003150-00020
4. Ay N, Anıl M, Alp V, Sevük U, Dinç B, Çelik M, et al. Evaluation of Quality of Life Early and Late After Kidney Transplantation. Ann Transplant (2015) 20:493–9. doi: 10.12659/AOT.895139
5. van der Mei SF, Groothoff JW, van Sonderen EL, van den Heuvel WJ, de Jong PE, van Son WJ. Clinical factors influencing participation in society after successful kidney transplantation. Transplantation (2006) 82:80–5. doi: 10.1097/01.tp.0000225768.56981.aa
6. Bakewell AB, Higgins RM, Edmunds ME. Does ethnicity influence perceived quality of life of patients on dialysis and following renal transplant? Nephrol Dial Transplant (2001) 16:1395–401. doi: 10.1093/ndt/16.7.1395
7. Bello BT, Raji YR. Knowledge, attitudes and beliefs of first-degree relatives of patients with chronic kidney disease toward kidney donation in Nigeria. Saudi J Kidney Dis Transpl (2016) 27:118–24. doi: 10.4103/1319-2442.174141
8. Rupolo G, Poznanski C. Psicologia e psichiatria del trapianto d’organi. Masson: Elsevier (1999) p. 1–188.
9. De Pasquale C, Pistorio ML, Sorbello M, Parrinello L, Corona D, Gagliano M, et al. Body image in kidney transplantation. Transplant Proc (2010) 42:1123–6. doi: 10.1016/j.transproceed.2010.03.071]
10. Ahsanuddin S, Bento S, Swerdlow N, Cervera I., Kayler LK. Candidate comprehension of key concepts in kidney transplantation. Ann Transplant (2015) 20:124–31. doi: 10.12659/AOT.892596
11. Castelnuovo Tedesco P, Levy NB. Psychological implications of changes in body image. In: Levy NB, editor. Psychonefrology, vol. 1 . New York: New York Plenum (1981).
12. Fukunishi I, Aikawa A, Ohara T, Hasegawa A. Psychiatric problems among recipients of kidney transplants: a 10-year follow-up. Transplant Proc (2002) 34:2766. doi: 10.1016/S0041-1345(02)03401-2
13. Stukas A, Dew MA, Switzer GE, DiMartini A, Kormos RL, Griffith BP. PTSD in heart transplant recipients and their primary family caregivers. Psychosomatics (1999) 40:212–21. doi: 10.1016/S0033-3182(99)71237-5
14. Alvares J, Almeida AM, Szuster DA, Gomes IC, Andrade EI, Acurcio Fde A, et al. Factors associated with quality of life in patients in renal replacement therapy in Brazil. Cien Saude Colet (2013) 18:1903–10. doi: 10.1590/S1413-81232013000700005
15. House RM, Thompson TL. Psychiatric aspects of organ transplantation. JAMA (1988) 260:535–9. doi: 10.1001/jama.260.4.535
16. De Pasquale C, Veroux M, Fornaro M, Sinagra N, Basile G, Gozzo C, et al. Psychological perspective of medication adherence in transplantation. World J Transplant (2016) 6(4):736–42. doi: 10.5500/wjt.v6.i4.736
17. De Pasquale C, Conti D, Pistorio ML, Fatuzzo P, Veroux M, Di Nuovo S. Comparison of the CBA-H and SF-36 for the screening of the psychological and behavioural variables in chronic dialysis patients. PLoS One (2017) 12(6):e0180077. doi: 10.1371/journal.pone.0180077. eCollection 2017.
18. Denhaerynck K, Dobbels F, Cleemput I, Desmyttere A, Schäfer-Keller P, Schaub S, et al. Prevalence, consequences, and determinants of nonadherence in adult renal transplant patients: a literature review. Transpl Int (2005) 18:1121–33. doi: 10.1111/j.1432-2277.2005.00176.x
19. Dew MA, Jacobs CL, Jowsey SG, Hanto R, Miller C, Delmonico FL, et al. Guidelines for the psychosocial evaluation of living unrelated kidney donors in the United States. Am J Transplant (2007) 7:1047–54. doi: 10.1111/j.1600-6143.2007.01751.x
20. Pistorio ML, Veroux M, Sinagra N, Basile G, De Pasquale C. Alexithymia in kidney transplantation patients. Transplant Proc (2017) 49(4):642–5. doi: 10.1016/j.transproceed.2017.02.031
21. Pistorio ML, Veroux M, Giaquinta A, Sinagra N, Corona D, Veroux P, et al. Study on emotional-affective aspects and the perception of general health in kidney transplant subjects. Transplant Proc (2015) 47:2135–8. doi: 10.1016/j.transproceed.2015.01.034
22. Christensen AJ, Raichle K, Ehlers SL, Bertolatus AJ. Effect of family environment and donor source on patient quality of life following renal transplantation. Health Psychol (2002) 21:468–76. doi: 10.1037/0278-6133.21.5.468
23. Moran PJ, Christensen AJ, Ehlers SL, Bertolatus JA. Family environment, intrusive ideation, and adjustment among renal transplant candidates. Ann Behav Med (1999) 21:311–6. doi: 10.1007/BF02895963
24. De Pasquale C, Veroux M, Indelicato L, Sinagra N, Giaquinta A, Fornaro M, et al. Psychopathological aspects of kidney transplantation: Efficacy of a multidisciplinary team. World J Transplant (2014) 4(4):267–75. doi: 10.5500/wjt.v4.i4.267
25. OPTN/UNOS. OPTN/UNOS Ethics Committee General Considerations in Assessment for Transplant Candidacy. (2010) U.S. Department of Health and Human Services: Washington, U. S. (cited 2011 March 29, 2011); Available from: http://optn.transplant.hrsa.gov/resources/bioethics.asp?index_5.
26. Moher D, Liberati A, Tetzlaff J, Douglas G. Linee guida per il reporting di revisioni sistematiche e meta-analisi: il Prisma Statement. Evidence (2015) 7:e1000114.
27. Maldonado JR, Dubois HC, David EE, Sher Y, Lolak S, Dyal J, et al. The Stanford Integrated Psychosocial Assessment for Transplantation (SIPAT): a new tool for the psychosocial evaluation of pre-transplant candidates. Psychosomatics (2012) 53:123–32. doi: 10.1016/j.psym.2011.12.012
28. Burkhalter H, Brunner DP, Wirz-Justice A, Cajochen C, Weaver TE, Steiger J, et al. Self-reported sleep disturbances in renal transplant recipients. BMC Nephrol (2013) 14:220. doi: 10.1186/1471-2369-14-220
29. Burkhalter H, Wirz-Justice A, Denhaerynck K, Fehr T, Steiger J, Venzin RM, et al. The effect of bright light therapy on sleep and circadian rhythms in renal transplant recipients: a pilot randomized, multicentre wait-list controlled trial. Transpl Int (2015) 28:59–70. doi: 10.1111/tri.12443
30. Corruble E, Barry C, Varescon I, Durrbach A, Samuel D, Lang P, et al. Report of depressive symptoms on waiting list and mortality after liver and kidney transplantation: a prospective cohort study. BMC Psychiatry (2011) 11:182. doi: 10.1186/1471-244X-11-182
31. Cukor D, Rosenthal DS, Jindal RM, Brown CD, Kimmel PL. Depression is an important contributor to low medication adherence in hemodialyzed patients and transplant recipients. Kidney Int (2009) 75:1223–9. doi: 10.1038/ki.2009.51
32. De Pasquale C, Pistorio ML, Corona D, Sinagra N, Giaquinta A, Zerbo D, et al. Role of “self-efficacy” in the process of long-term care in kidney transplant recipients. Transplant Proc (2014) 46:2235–7. doi: 10.1016/j.transproceed.2014.07.035
33. Denhaerynck K, Steiger J, Bock A, Schäfer-Keller P, Köfer S, Thannberger N, et al. Prevalence and risk factors of non-adherence with immunosuppressive medication in kidney transplant patients. Am J Transplant (2007) 7:108–16. doi: 10.1111/j.1600-6143.2006.01611.x
34. Fructuoso M, Castro R, Oliveira L, Prata C, Morgado T. Quality of life in chronic kidney disease. Nefrologia (2011) 31:91–6. doi: 10.3265/Nefrologia.pre2010.Jul.10483
35. Gelb S, Shapiro RJ, Hill A, Thornton WL. Cognitive outcome following kidney transplantation. Nephrol Dial Transplant (2008) 23:1032–8. doi: 10.1093/ndt/gfm659
36. Gentile S, Beauger D, Speyer E, Jouve E, Dussol B, Jacquelinet C, et al. Factors associated with health-related quality of life in renal transplant recipients: results of a national survey in France. Health Qual Life Outcomes (2013) 11:88. doi: 10.1186/1477-7525-11-88
37. Gheith OA, El-Saadany SA, Abuo Donia SA, Salem YM. Compliance with recommended life style behaviors in kidney transplant recipients: does it matter in living donor kidney transplant? Iran J Kidney Dis (2008) 2:218–26.
38. Goedendorp MM, Hoitsma AJ, Bloot L, Bleijenberg G, Knoop H. Severe fatigue after kidney transplantation: a highly prevalent, disabling and multifactorial symptom. Transpl Int (2013) 26:1007–15. doi: 10.1111/tri.12166
39. Gordon EJ, Prohaska TR, Gallant MP, Sehgal AR, Strogatz D, Conti D, et al. Prevalence and determinants of physical activity and fluid intake in kidney transplant recipients. Clin Transplant (2010) 24:e69–81. doi: 10.1111/j.1399-0012.2009.01154.x
40. Gross CR, Kreitzer MJ, Thomas W, Reilly-Spong M, Cramer-Bornemann M, Nyman JA, et al. Mindfulness-based stress reduction for solid organ transplant recipients: a randomized controlled trial. Altern Ther Health Med (2010) 16:30–8.
41. Kofman T, Pourcine F, Canoui-Poitrine F, Kamar N, Malvezzi P, François H, et al. Safety of renal transplantation in patients with bipolar or psychotic disorders: a retrospective study. Transpl Int (2018) 31(4):377–85. doi: 10.1111/tri.13078
42. Kovacs AZ, Molnar MZ, Szeifert L, Ambrus C, Molnar-Varga M, Szentkiralyi A, et al. Sleep disorders, depressive symptoms and health-related quality of life–a cross-sectional comparison between kidney transplant recipients and waitlisted patients on maintenance dialysis. Nephrol Dial Transplant (2011) 26:1058–65. doi: 10.1093/ndt/gfq476
43. McAdams-DeMarco MA, Olorundare IO, Ying H, Warsame F, Haugen CE, Hall R, et al. Frailty and postkidney transplant health-related quality of life. Transplantation (2018) 102(2):291–9. doi: 10.1097/TP.0000000000001943
44. Müller HH, Englbrecht M, Wiesener MS, Titze S, Heller K, Groemer TW, et al. Depression, anxiety, resilience and coping pre and post kidney transplantation - initial findings from the psychiatric impairments in kidney transplantation (PI-KT)-Study. PLoS One (2015) 10:e0140706. doi: 10.1371/journal.pone.0140706
45. Paterson TSE, O'Rourke N, Shapiro RJ, Loken Thornton W.Medication adherence in renal transplant recipients: a latent variable model of psychosocialand neurocognitive predictors. PLoS One (2018) 13(9):e0204219. doi: 10.1371/journal.pone.0204219
46. Pistorio ML, Veroux M, Corona D, Sinagra N, Giaquinta A, Zerbo D, et al. The study of personality in renal transplant patients: possible predictor of an adequate social adaptation? Transplant Proc (2013) 45:2657–9. doi: 10.1016/j.transproceed.2013.07.003
47. Pourfarziani V, Taheri S, Sharifi-Bonab MM, Mohammadzadeh M. Assessment of sleep disturbance in renal transplant recipients and associated risk factors. Saudi J Kidney Dis Transpl (2010) 21:433–7.
48. Prihodova L, Nagyova I, Rosenberger J, Roland R, van Dijk JP, Groothoff JW. Impact of personality and psychological distress on health-related quality of life in kidney transplant recipients. Transpl Int (2010) 23:484–92. doi: 10.1111/j.1432-2277.2009.01003.x
49. Raiesifar A, Tayebi A, Najafi Mehrii S, Ebadi A, Einollahi B, Tabibi H, et al. Effect of applying continuous care model on quality of life among kidney transplant patients: a randomized clinical trial. Iran J Kidney Dis (2014) 8:139–44.
50. Reilly-Spong M, Park T, Gross CR. Poor sleep in organ transplant recipients: self-reports and actigraphy. Clin Transplant (2013) 27(6):901–13. doi: 10.1111/ctr.12255
51. Shabany Hamedan M, Mohamad Aliha J. Relationship between immunosuppressive medications adherence and quality of life and some patient factors in renal transplant patients in Iran. Glob J Health Sci (2014) 6:205–12. doi: 10.5539/gjhs.v6n4p205
52. Silva DS, Andrade Edos S, Elias RM, David-Neto E, Nahas WC, Castro MC, et al. The perception of sleep quality in kidney transplant patients during the first year of transplantation. Clinics (Sao Paulo) (2012) 67:1365–71. doi: 10.6061/clinics/2012(12)04
53. Troen AM, Scott TM, D’Anci KE, Moorthy D, Dobson B, Rogers G, et al. FACT study investigators. Cognitive dysfunction and depression in adult kidney transplant recipients: baseline findings from the FAVORIT Ancillary Cognitive Trial (FACT). J Ren Nutr (2012) 22:268–76. e1-3. doi: 10.1053/j.jrn.2011.07.009
54. Von der Lippe N, Waldum B, Brekke FB, Amro AA, Reisæter AV, Os I. From dialysis to transplantation: a 5-year longitudinal study on self-reported quality of life. BMC Nephrol (2014) 15:191. doi: 10.1186/1471-2369-15-191
55. Wei TY, Chiang YJ, Hsieh CY, Weng LC, Lin SC, Lin MH. Health related quality of life of long-term kidney transplantation recipients. BioMed J (2013) 36:243–51. doi: 10.4103/2319-4170.113186
56. Weng FL, Chandwani S, Kurtyka KM, Zacker C, Chisholm-Burns MA, Demissie K. Prevalence and correlates of medication non-adherence among kidney transplant recipients more than 6 months post-transplant: a cross-sectional study. BMC Nephrol (2013) 14:261. doi: 10.1186/1471-2369-14-261
57. Zelle DM, Corpeleijn E, Klaassen G, Schutte E, Navis G, Bakker SJ. Fear of movement and low self-efficacy are important barriers in physical activity after renal transplantation. PLoS One (2016) 11:e0147609. doi: 10.1371/journal.pone.0147609
58. Burkhalter H, De Geest S, Wirz-Justice A, Cajochen C. Melatonin rhythms in renal transplant recipients with sleep-wake disturbances. Chronobiol Int (2016) 33:810–20. doi: 10.3109/07420528.2016.1169192
59. Costa-Requena G, Cantarell MC, Moreso F, Parramon G, Seron D. Health related quality of life in renal transplantation: 2 years of longitudinal follow-up. Med Clin (Barc) (2017) 149(3):114–8. doi: 10.1016/j.medcli.2017.02.032
60. Czyżewski Ł, Frelik P, Wyzgał J, Szarpak Ł. Evaluation of quality of life and severity of depression, anxiety, and stress in patients afterkidney transplantation. Transplant Proc (2018) 50(6):1733–7. doi: 10.1016/j.transproceed.2018.04.026
61. De Pasquale C, Pistorio ML, Veroux P, Giuffrida G, Sinagra N, Ekser B, et al. Quality of life in kidney transplantation from marginal donors. Transplant Proc (2011) 43:1045–7. doi: 10.1016/j.transproceed.2011.01.156
62. Famà F, Micali E, Linard C, Venuti MD, Costantino G, Gioffrè-Florio M. Social and interpersonal relationship modifications after renal transplant. A statistic and epidemiologic evaluation. J Prev Med Hyg (2013) 54:208–11.
63. Hucker A, Bunn F, Carpenter L, Lawrence C, Farrington K, Sharma S. Non-adherence to immunosuppressants following renal transplantation: a protocol for a systematic review. BMJ Open (2017) 7(9):e015411. doi: 10.1136/bmjopen-2016-015411
64. Husain SA, Brennan C, Michelson A, Tsapepas D, Patzer RE, Schold JD, et al. Patients prioritize waitlist over posttransplant outcomes when evaluating kidney transplant centers. Am J Transplant (2018) 18(11):2781–90. doi: 10.1111/ajt.14985
65. Kung PC, Yeh MC, Lai MK. Renal transplant recipients: the factors related to immunosuppressive medication adherence based on the health belief model. J Nurs Res (2017) 25(5):392–7. doi: 10.1097/JNR.0000000000000181
66. Liaveri PG, Dikeos D, Ilias I, Lygkoni EP, Boletis IN, Skalioti C, et al. Quality of sleep in renal transplant recipients and patients on hemodialysis. J Psychosom Res (2017) 93:96–101. doi: 10.1016/j.jpsychores.2016.12.013
67. Neri L, McEwan P, Sennfält K, Baboolal K. Characterizing the relationship between health utility and renal function after kidney transplantation in UK and US: a cross-sectional study. Health Qual Life Outcomes (2012) 10:139. doi: 10.1186/1477-7525-10-139
68. Panagopoulou A, Hardalias A, Berati S, Fourtounas C. Psychosocial issues and quality of life in patients on renal replacement therapy. Saudi J Kidney Dis Transpl (2009) 20:212–8.
69. Ronai KZ, Szentkiralyi A, Lazar AS, Lazar ZI, Papp I, Gombos F, et al. Association of symptoms of insomnia and sleep parameters among kidney transplantrecipients. J Psychosom Res (2017) 99:95–104. doi: 10.1016/j.jpsychores.2017.05.019
70. Sieverdes JC, Raynor PA, Armstrong T, Jenkins CH, Sox LR, Treiber FA. Attitudes and perceptions of patients on the kidney transplant waiting list toward mobile health-delivered physical activity programs. Prog Transplant (2015) 25:26–34. doi: 10.7182/pit2015884
71. Srifuengfung M, Noppakun K, Srisurapanont M, Dis A. Depression in Kidney Transplant Recipients: Prevalence, Risk Factors, and Association With Functional Disabilities. J Nerv Ment Dis (2017) 205(10):788–92. doi: 10.1097/NMD.0000000000000722
72. Szeifert L, Molnar MZ, Ambrus C, Koczy AB, Kovacs AZ, Vamos EP, et al. Symptoms of depression in kidney transplant recipients: a cross-sectional study. Am J Kidney Dis (2010) 55:132–40. doi: 10.1053/j.ajkd.2009.09.022
73. Tamura Y, Urawa A, Watanabe S, Hasegawa T, Ogura T, Nishikawa K, et al. Mood Status and Quality of Life in Kidney Recipients After Transplantation. Transplant Proc (2018) 50(8):2521–5. doi: 10.1016/j.transproceed.2018.03.077
74. Tavallaii SA, Einollahi B, Azizabadi Farahani M, Namdari M. Socioeconomic links to health-related quality of life, anxiety, and depression in kidneytransplant recipients. Iran J Kidney Dis (2009) 3(1):40–4.
75. van Lint C, Wang W, van Dijk S, Brinkman WP, Rövekamp TJ, Neerincx MA, et al. Self-monitoring kidney function post transplantation: reliability of patient-reported data. J Med Internet Res (2017) 19(9):e316. doi: 10.2196/jmir.7542
76. Wang W, van Lint CL, Brinkman WP, Rövekamp TJM, van Dijk S, van der Boog PJM, et al. Renal transplant patient acceptance of a self-management support system. BMC Med Inform Decis Mak (2017) 17(1):58. doi: 10.1186/s12911-017-0456-y
77. Weng LC, Yang YC, Huang HL, Chiang YJ, Tsai YH. Factors that determine self-reported immunosuppressant adherence in kidney transplantrecipients: a correlational study. J Adv Nurs (2017) 73(1):228–39. doi: 10.1111/jan.13106
78. Xie J, Wang L, Tang X, Yi Y, Ding S, Yan J, et al. Sleep quality and related psychosocial variables among renal transplant patients. Transplant Proc (2018) 50(10):3426–33. doi: 10.1016/j.transproceed.2018.06.030
79. Zhao SM, Dong FF, Qiu HZ, Li D. Quality of life, adherence behavior, and social support among renal transplant recipientsin china: a descriptive correlational study. Transplant Proc (2018) 50(10):3329–37. doi: 10.1016/j.transproceed.2018.05.026
80. Zhu Y, Zhou Y, Zhang L, Zhang J, Lin J. Efficacy of interventions for adherence to the immunosuppressive therapy in kidney transplant recipients: a meta-analysis and systematic review. J Invest Med (2017) 65(7):1049–56. doi: 10.1136/jim-2016-000265
81. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health (1998) 52:377–84. doi: 10.1136/jech.52.6.377
82. Willems LM, Vriezekolk JE, Schouffoer AA, Poole JL, Stamm TA, Boström C, et al. Effectiveness of nonpharmacologic interventions in systemic sclerosis: a systematic review. Arthritis Care Res (Hoboken) (2015) 67:1426–39. doi: 10.1002/acr.22595
83. De Pasquale C, Veroux M, Pistorio ML, Papotto A, Basile G, Patanè M, et al. Return to work and quality of life: a psychosocial survey after kidney transplant. Transplant Proc (2019) 51(1):153–6. doi: 10.1016/j.transproceed.2018.04.083
84. Dew MA, Rosenberger EM, Myaskovsky L, DiMartini AF, DeVito Dabbs AJ, Posluszny DM, et al. Depression and anxiety as risk factors for morbility and mortality after organ transplantation: a systematic review and meta-analysis. Transplantation (2015) 100(5):988–1003. doi: 10.1097/TP.0000000000000901. Review. PMDI: 26492128.
Keywords: psychopathology, depression, anxiety, cognitive disorders, sleep disorders, adherence, social functioning, kidney transplantation
Citation: De Pasquale C, Pistorio ML, Veroux M, Indelicato L, Biffa G, Bennardi N, Zoncheddu P, Martinelli V, Giaquinta A and Veroux P (2020) Psychological and Psychopathological Aspects of Kidney Transplantation: A Systematic Review. Front. Psychiatry 11:106. doi: 10.3389/fpsyt.2020.00106
Received: 14 October 2019; Accepted: 07 February 2020;
Published: 05 March 2020.
Edited by:
Martina De Zwaan, Hannover Medical School, GermanyReviewed by:
Mariel Nöhre, Hannover Medical School, GermanySusanne Unverzagt, University Hospital in Halle, Germany
Copyright © 2020 De Pasquale, Pistorio, Veroux, Indelicato, Biffa, Bennardi, Zoncheddu, Martinelli, Giaquinta and Veroux. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Concetta De Pasquale, ZGVwYXNxdWFAdW5pY3QuaXQ=
 Concetta De Pasquale
Concetta De Pasquale Maria Luisa Pistorio2,3,4
Maria Luisa Pistorio2,3,4 Gabriella Biffa
Gabriella Biffa Valentina Martinelli
Valentina Martinelli