- 1Department of Psychiatry, The Second Xiangya Hospital, Central South University, The China National Clinical Research Center for Mental Health Disorders, Chinese National Technology Institute of Psychiatry, Key Laboratory of Psychiatry and Mental Health of Hunan Province, Changsha, China
- 2Female Psychiatric Ward, The First Psychiatric Hospital of Hengyang City, Hengyang, China
- 3Zhejiang Provincial People's Hospital, Hangzhou, China
- 4Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 5Brain Hospital of Hunan Province, Changsha, China
- 6Department of Psychiatry, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Hangzhou, China
Background: The high numbers of patients with mental illness, especially those who are misdiagnosed or delayed in treatment in China, have imposed a huge burden on the country and the society. This study was designed to investigate the mental health literacy (MHL) of non-mental health nurses.
Method: A cross-sectional survey was designed, and a convenient cluster sampling method was applied. We presented evidence on 601 nurses from the non-mental health department in four hospitals in Hengyang city, China. One-third of the vignettes were diagnosed with schizophrenia, depression, or generalized anxiety disorder (GAD).
Result: The correct identification rates for schizophrenia, depression, and GAD vignettes reached 38.9, 56.2, and 17.5%, respectively. The majority of the participants deemed that the person in each vignette needed professional help, and most of them preferred professional medical help and lifestyle interventions. As for the likely outcome for the persons described in each vignette, more than half of the participants thought that with professional help, the patients would make a full recovery, but problems would probably recur.
Conclusion: The MHL of non-mental health nurses is insufficient in China. This condition is particularly applicable in the case of GAD. Thus, the country must implement more mental health education programs to improve the MHL of non-mental health nurses.
Introduction
Mental disorders are common around the whole world and burdensome for individuals and the society (1). Mental disorders have become more common across China in the past 30 years. China has a population of about 1.4 billion, and the lifetime prevalence of mental disorders (excluding dementia) accounts for 16.6% (2). Globally, 17% of the burden caused by mental, neurological, and substance use disorder was suffered by Chinese people in 2013 and accounted for 36 million global disability-adjusted life years (10% for all disease burden) (3). Mental disorders are associated with enormous economic burden, including the high cost of treatment and regression of the society. In China, the total costs of mental disorders accounted for more than 15% of total health expenditure in 2013 and 1.1% of China's gross domestic products (4). Although continuous efforts have been made by the Chinese government, the mental health resources available in China remain limited. In 2015, the numbers of mental health institutes and psychiatric beds reached 1,650 and 228,000, respectively. A total of 1.49 psychiatrists are available per 100,000 people in China, whereas 2.03 psychiatrists are accessible in middle- and high-income countries worldwide (5). Given that specific mental disorders are mainly manifested as physical discomfort [such as anxiety disorder which is often accompanied by autonomic symptoms, including headache, palpitations, tightness in the chest, and mild stomach (6)], many patients seek help in internal medicine departments, such as those for neurology, gastroenterology, and cardiology. A total of 44.7, 25.7, and 7.9% of people with anxiety, substance, and mood disorders, respectively, had/have made psychotherapy contact (7). Long waiting time before treatment contact might cause the delayed treatment of diseases. Previous studies have demonstrated that delay time ranges from 6 to 8 years for mood disorders and 9 to 23 years for anxiety disorders without normal treatment contact (8). The long duration of untreated mental illness also results in poor treatment outcomes (9).
Mental health literacy (MHL) was first put forward by Jorm et al. in 1997 (10). This concept was defined as the knowledge and beliefs about mental disorders, aiding in the recognition, management, and prevention of such conditions. MHL includes the following components: the ability to recognize specific disorders; knowing how to seek mental health information; knowledge of risk factors and causes; knowledge of self-treatments; knowledge of professional help available; attitudes that promote recognition and appropriate help-seeking. Theoretically, improving MHL could improve the rates of early identification and help-seeking for mental illness, increase early intervention and successful treatment, and reduce the chances of increasing severity of disorders.
In the Chinese mental healthcare system, doctors and nurses usually work collaboratively to build a patient-centered care environment. Nurses are medical staff members who are in direct contact with patients and their families. Being in direct and long contact with patients, nurses have more opportunities to observe them. The initial identification of mental disorders from nurses helps doctors to further understand and deal with patients' conditions and improve the early identification and referral rates. Although a series of studies for MHL has been conducted among the public and professionals (11–15), a limited number of research used vignettes as a tool for studying non-mental health nurses. This study aimed to evaluate the identification and beliefs of Chinese non-mental health nurses about the interventions and outcomes regarding three common mental disorders, namely, schizophrenia, generalized anxiety disorder (GAD), and depression.
Methods
Sample
We used a cross-sectional survey and followed a cluster convenience sampling method. The survey was conducted between 2014 and 2015 in four general hospitals located in Hengyang, which is one of the prefecture-level cities in Hunan province, China. These hospitals are the First Affiliated Hospital of the University of South China, the First People's Hospital of Hengyang, the Fifth People's Hospital of Hengyang, and the People's Hospital of Hengyang County, which are tertiary or secondary hospitals. All these hospitals are teaching hospitals. In addition to mental health nurses, each hospital has nearly 400 nurses for the other departments. Thus, the total sample size was 1,600. We recruited nurses who are working in non-mental health departments to complete the questionnaire anonymously. We distributed 610 questionnaires, with 601 non-mental health nurses successfully completing the questionnaires. The response rate was 98.5%. The numbers of responses for each of the three vignettes types were as follows: schizophrenia, n = 198; depression, n = 203; GAD, n = 200.
The research program was approved by the ethics committee of the Second Xiangya Hospital of Central South University. Before completing the questionnaires, we stated the aim of the study and requested consent from the participants to participate by filling in the questionnaire.
Survey Questionnaires
The instrument used for data collection was adapted from that used by Jorm et al. (10) to investigate MHL among Australian samples. After obtaining the permission of the original author, Dr. Liu Wei translated and modified the questionnaires to conform to Chinese conditions. Dr. Liu removed several interventions which were used in the Australian samples but are inapplicable for Chinese mental services and included additional resources and treatment options, such as having a massage, Qigong/Tai Chi therapy, and acupuncture, to fit with the Chinese medical practices and beliefs (11). Dr. Liu Wei also examined the validity and reliability of the questionnaire (11).
First, demographic information (including age, gender, marital status, education level, work duration, and hospital level) of the participants were collected. Second, the participants were randomly assigned to one of the three vignettes describing GAD, depression, or schizophrenia. Each vignette was designed to satisfy the diagnostic criteria for schizophrenia, depression, or GAD in accordance with the Diagnostic and Statistical Manual of Mental Disorders (4th edition) and International Statistical Classification of Diseases and Related Health Problems (10th revision). Following the vignettes, the participants were asked to select one “most likely” diagnosis from a series of diagnostic options. Only one choice should be given to all questions. The participants were also requested to answer how the person in the vignette would be best helped, and they were allowed to select three answers. Afterward, the participants were asked to rate the likely effect of a range of interventions (rated as “helpful,” “harmful,” or “neither”) to assess their beliefs about the treatments. Choices about the possible results with or without professional help in the vignettes were also collected. Details of the questionnaire and the vignettes are presented below.
Statistical Analysis
The data were entered by double-entry strategy in EpiData version 3.1 (EpiData Association, Odense, Funen, Denmark). All statistical analyses were conducted with IBM-SPSS 25.0 software (IBM Corp., Armonk, NY, USA). In this survey, descriptive analyses using median (interquartile range) for skewed variables and frequency (percentage) for categorical variables were performed. Then, we computed the percentage and 95% confidence interval (CI) for helpful interventions and the best method of help. We use the Chi-square test to investigate whether any significant difference exists in each vignette in terms of the identification rate and calculated odd rate (OR) and 95% CI. In each vignette, general demographic data were compared between those who had been correctly identified and those who had not. For each item in helpful intervention and best method of help, we also used Chi-square test to study the differences between different vignettes in the proportion of helpfulness.
Results
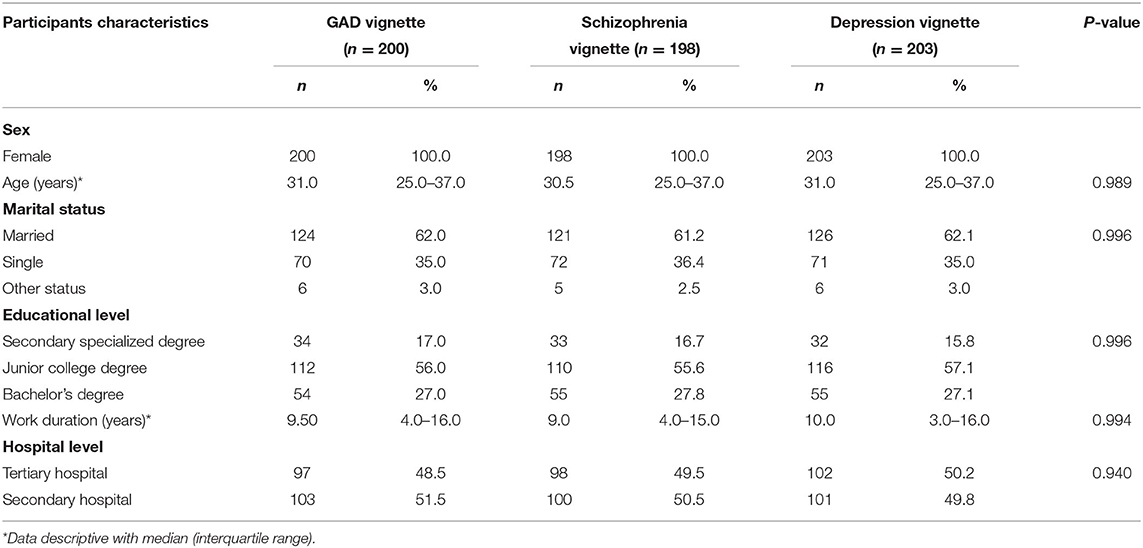
No significant difference was observed among the participants for the three vignettes in terms of sex, age, marital status, educational level, and work duration. All participants were female nurses from comprehensive departments. As shown in Table 1, the median age of all participants was 31 years old. About 61.7% of the participants are married. About 27.3% of the participants finished a bachelor's degree, and the others completed a junior college degree or secondary specialized degree. Medium work duration was 9.5 years, and about half of the participants worked in a tertiary hospital.
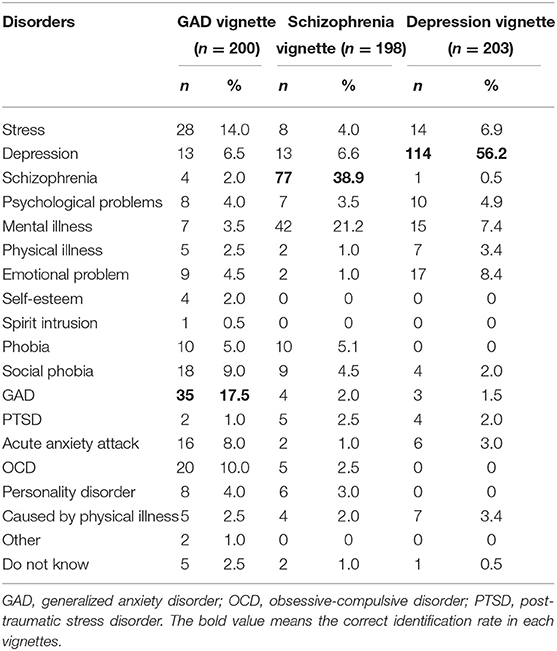
As for the diagnosis, Table 2 shows the frequency of participants who labeled all problems in each vignette. In the depression vignette, 56.2% (n = 114) of the non-mental health registered nurses provided correct answers. The correct identification rate for the schizophrenia vignette was 38.9% (n = 77), which was lower than the rate for the depression vignette. A total of 17.5% (n = 35) of the participants correctly identified the problems for the GAD vignette. We compared the correct identification rate among these three vignettes. The result shows that compared with GAD, schizophrenia was more likely to be identified correctly (OR: 3.00; CI: [1.89, 4.77]; P < 0.001). Depression was also considerably easier to properly identify than GAD (OR: 6.040; CI: [3.82, 9.55]; P < 0.001). Depression was more likely to gain better recognition than schizophrenia (OR: 2.01; CI: [1.35, 3.00]; P < 0.001).
In the GAD vignette, a significant difference (P < 0.05) in the work duration was observed between those who recognized correctly the condition and those who did not. A significant difference was observed in the education level between those who recognized depression in the vignette correctly and those who did not (P < 0.05). No significant difference was found among the participants who recognized correctly or not schizophrenia.
Tables 3, 4 show the non-mental health nurses' attitudes toward treatment for all the vignettes. Most of the participants thought they needed professional help in diagnosing GAD (85.5%), depression (89.2%), and schizophrenia (94.9%).
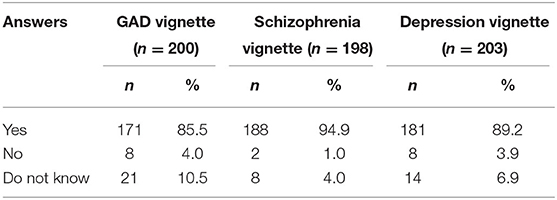
Table 3. Frequency of participants who answered whether professional help is needed in diagnosing the vignettes.
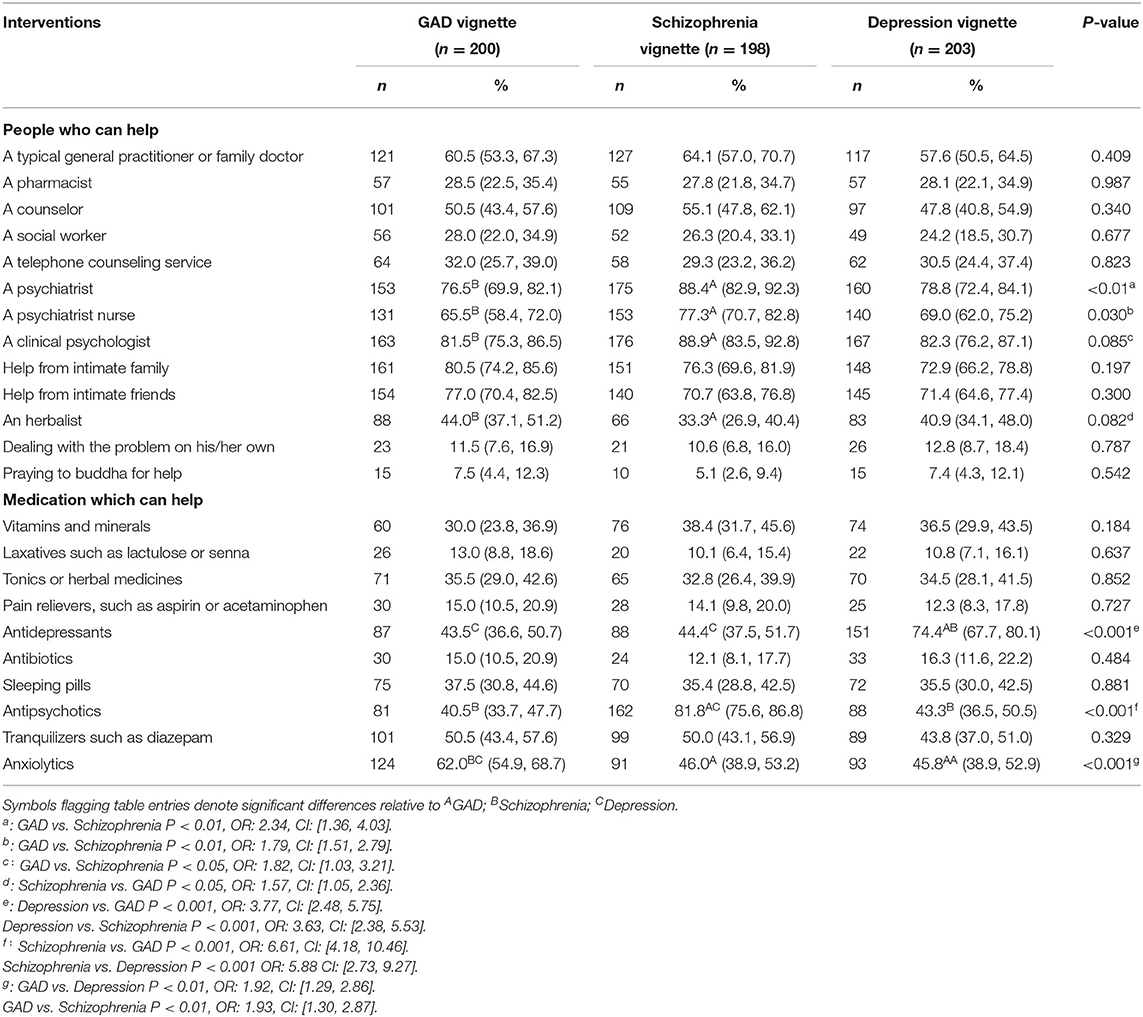
The participants were given a list of intervention treatments which they rated depending on helpfulness. For all the vignettes, a clinical psychologist, a psychiatrist, and helping intimate family were considered the most helpful (>70%). Praying to Buddha, dealing with the problem on their own, and seeking help from a counselor were the least helpful interventions (<30%). Anxiolytics (62.0%), followed by tranquilizers (50.5%) and antidepressants (43.5%), were recognized as the most helpful by the participants for the GAD vignettes. Antipsychotics were recognized as helpful by 81.8% of the participants for the schizophrenia vignette, followed by tranquilizers (50%) and anxiolytics (46.0%). Antidepressants were recognized as helpful by 74.4% of the participants for the depression vignette, followed by anxiolytics (45.8%) and tranquilizers (43.8%).
Compared with the GAD vignette, most participants believed that psychiatrists (P < 0.01; OR: 2.34; CI: [1.36, 4.03]), psychiatric nurses (P < 0.01; OR: 1.79; CI: [1.51, 2.79]), and clinical psychologists (P < 0.05; OR: 1.82; CI: [1.03, 3.21]) were more helpful in the schizophrenia vignette. Dealing with problem on his/her own was thought to be more helpful in GAD vignette than in schizophrenia (P < 0.05; OR: 1.57; CI: [1.05, 2.36]).
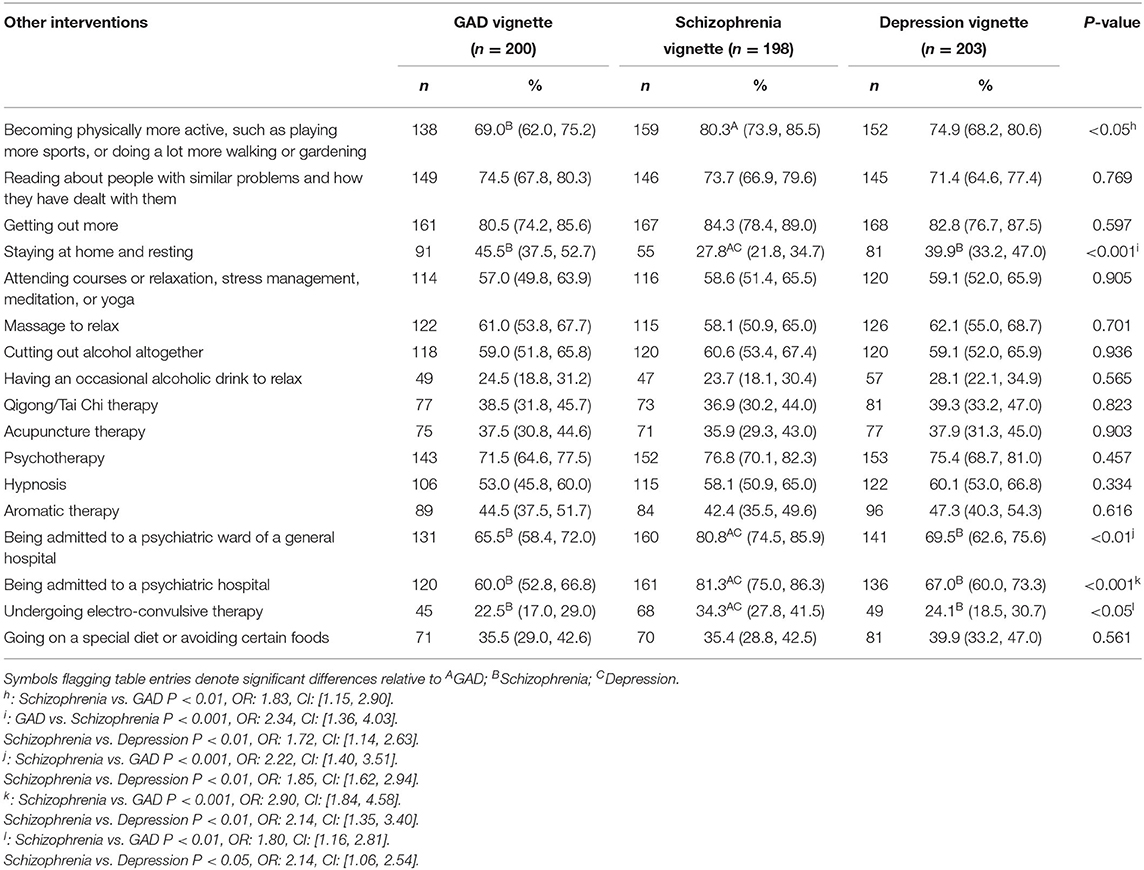
As shown in Table 5, going out was thought to be helpful by a majority of the participants for the GAD (80.5%), schizophrenia (84.3%), and depression vignettes (82.8%). For the GAD and depression vignettes, electro-convulsive therapy was considered the least helpful intervention. However, occasionally consuming alcoholic drink to relax was rated as the least helpful intervention in the schizophrenia vignette. Over 80% of the participants for the schizophrenia vignette thought that being admitted to a psychiatric ward of a general hospital or a psychiatric hospital was helpful, whereas the ratios in the GAD and depression vignettes were below 70%. The rate of participants who rated “being admitted to a psychiatric ward of a general hospital” as helpful was higher for the schizophrenia vignette than the depression vignette (P < 0.01; OR: 1.85; CI: [1.62, 2.94]) and GAD (P < 0.01; OR: 2.22; CI: [1.40, 3.51]) vignettes. More participants believed that “becoming physically more active” was more helpful in schizophrenia vignette than in GAD vignette (P < 0.05; OR: 1.83; CI: [1.15, 2.90]). The helpful rate of “being admitted to a psychiatric hospital” was significantly higher for the schizophrenia vignette than that of depression (P < 0.01; OR: 2.14; CI: [1.35, 3.40]) and GAD (P < 0.01; OR: 2.90; CI: [1.84, 4.58]). “Undergoing electro-convulsive therapy” was also thought to be more helpful in schizophrenia than depression (P < 0.05; OR: 1.64; CI: [1.06, 2.54]) and GAD (P < 0.01; OR: 1.80; CI: [1.16, 2.81]).
We asked the participants about how they would help the person in the vignettes if they were one of their families or friends. They were allowed to select 3 answers from 23 options (Table 6). Listening/talking with a person was thought to be the most helpful in the GAD (47.0%) and depression (40.9%) vignettes. In the schizophrenia vignette, encouraging the person to seek help from a psychologist was thought to be the most helpful choice, followed by listening/talking with the person and encouraging them to consult a counselor. “Encourage the person to go to a mental health hospital” was considered more helpful in schizophrenia than in depression (P < 0.05; OR: 1.64; CI: [1.00, 2.67]) and GAD (P < 0.01; OR: 2.41; CI: [1.41, 4.12]).
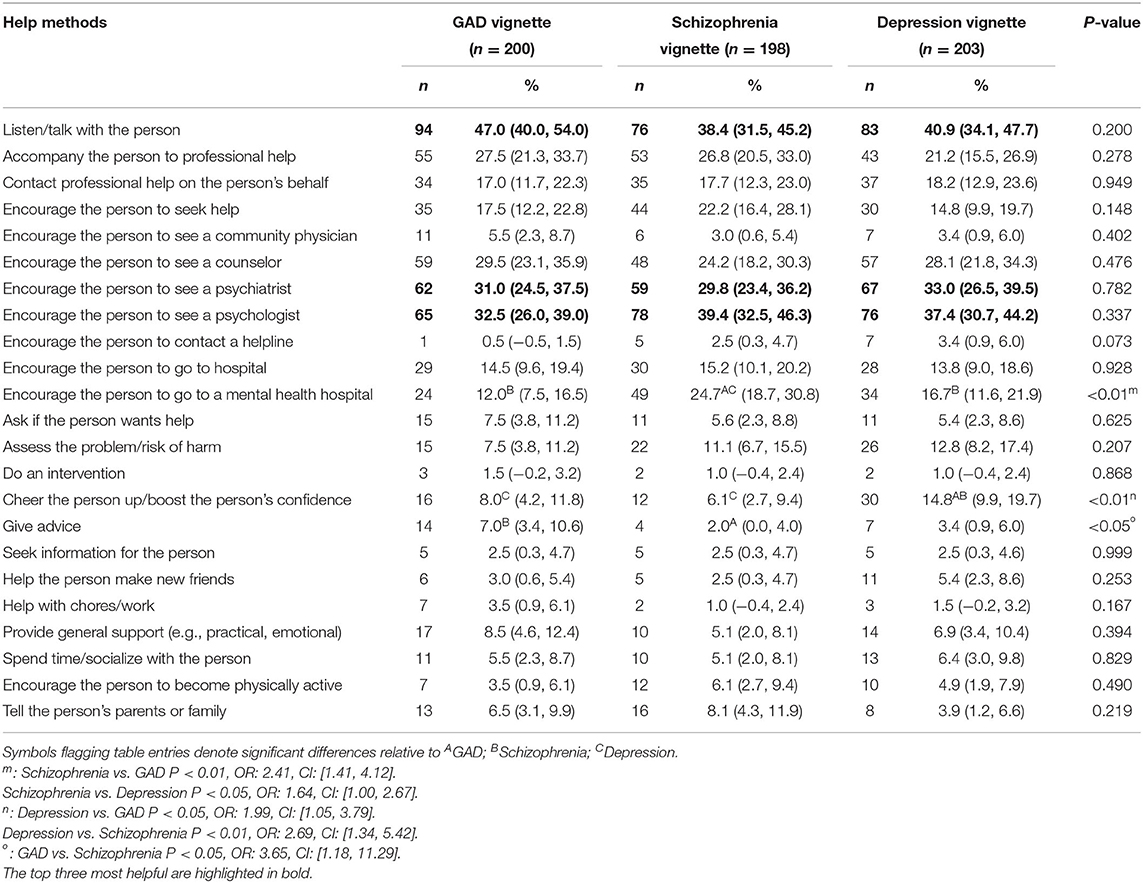
Table 6. Frequency of participants selecting each category to answer how the person in the vignettes could be best helped.
Table 7 shows the frequency of participants selecting each outcome as possible scenario for the person described in the vignettes. A majority of the participants endorsed that full recovery would be achieved, but problems would probably recur. A total of 70.7% of the participants for the schizophrenia vignette believed that the person's condition would worsen without professional help, whereas 66.0 and 56.5% held the same belief for the depression and GAD vignettes, respectively.
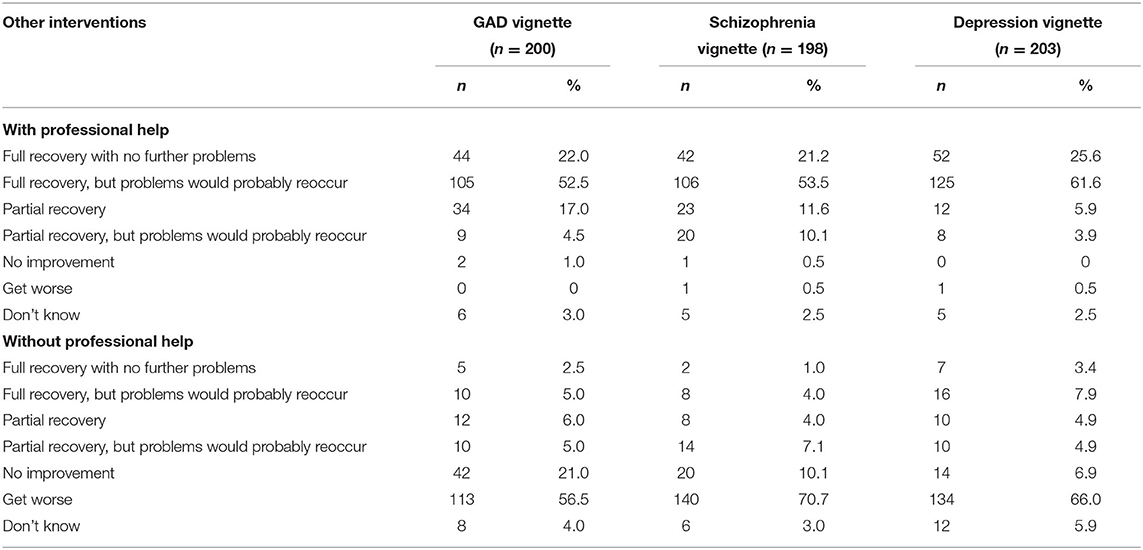
Table 7. Frequency of participants selecting each outcome as a likely scenario for the person described in the vignettes.
Discussions
This study was the first to use vignettes to investigate the MHL of non-mental health nurses in China. Preliminary data on their identification, attitudes toward treatments, and prognosis for common mental illnesses were presented. Our research has shown that the correct identification rate for the depression vignette was the highest among the three vignettes, and the value was significantly higher than those for the schizophrenia and GAD vignettes. A majority of the participants deemed that the person in each vignette needed professional help, and most of them preferred seeking professional medical help and implementing lifestyle interventions. As for the likely outcomes for the person described in each vignette, more than half of the participants thought that with professional help, the person with the disease would make a full recovery, but problems would probably recur.
Identification of Disorders in the Vignettes
The correct identification rates for depression and schizophrenia vignettes reached 56.2 and 38.9%, respectively. Less than 20% of the participants correctly labeled the GAD vignette, despite having a list of potential response options. For all the three vignettes, the correct recognition ratios were below 60%, and the correct ratio in each vignette was lower than the corresponding value in our investigation on non-mental health professionals (13). These outcomes are likely due to the role of nurses in the care process; they perform more work on observation, implementing medical orders, and rehabilitation guidance rather than diagnosis. The strong recognition rate for the depression vignette is expected, given the possibility of the high-frequency coverage of the disorder on television and in movies. In the schizophrenia vignette, the secondary diagnosis was “mental illness,” which accounted for 21.2% of the recognition rate. In this vignette, the person acknowledges their mental illness problem but cannot diagnosis it specifically. Although anxiety disorder has become the most prevalent lifetime mental disorder in China (2), the recognition rate in this study was <20%. The low value was due to the people's assumption about anxiety not being a disease, although they consider it as a stress or compulsive disorder. In our research, 15 and 10% of the participants misdiagnosed GAD as stress and obsessive-compulsive disorder, respectively. Therefore, patients with GAD utilize primary care resources frequently, and most of them visit various physicians before they are correctly diagnosed and treated (15). A high level of MHL would increase the possibility of the early identification of these disorders and referral to mental health specialists (13). As one of the important roles in physical treatment, nurses' identification of mental disorders is as important as that of physicians. Serious consequences might be engendered for individuals with mental disorders. Studies have shown that the longer a mental illness is left untreated, the poorer treatment outcomes would be (9, 16, 17). We observed that the longer the nurses work duration was, the higher the recognition rate was for the GAD vignette. This condition may due to the accumulation of experiences with the number of hours worked. In the depression vignette, education level influenced the rate of identification. This finding suggests the importance of enhancing the education level of nurses.
Helpfulness of Interventions
Most non-mental health nurses deemed that people in the vignettes need professional help. However, several nurses thought that no help was needed, or they were unfamiliar with the correct answer, especially for the GAD vignette. The potential reasons might include the following: the nurses do not consider GAD a disease (18); the disease has not reached the point of requiring treatment. In the schizophrenia vignette, most people thought that the patients needed professional help, probably because psychotic symptoms are perceived as more violent and unpredictable in contrast with those of people suffering from other mental disorders.
As for the people who can help, the results revealed a high rating of perceived helpfulness for treating mental illness by professionals, such as clinical psychologists and psychiatrists, in all the vignettes. The nurses would likely seek professional help. The participants also gave high remarks on seeking help from intimate families and friends. This result accords with the findings by Liu et al. (11) in China and Parker et al. (19) in Singapore. The potential reasons might be the social stigma and perceived discrimination felt by the participants; such conditions and symptoms may be shameful but are considered a private matter in China. Patients prefer handling their mental problems by themselves, and many patients with mental illness opt to conceal their condition. In a previous study carried out in four provinces of China, less than one-fifth of the individuals who met the diagnostic criteria for a mental disorder sought any type of professional help for their condition (20).
At least 60% of the participants in the three vignettes selected correctly the medications that could help. The rate was higher than the identification rate, possibly because in this question, participants can select more than one option and would opt for all the possible right answers. This finding may reflect the participants' ability to identify the disease. Such belief can positively affect treatment outcomes. However, more than 30% of the participants thought that vitamins, minerals, and herbal medicines were helpful in all the vignettes, and more than 10% endorsed laxatives and antibiotics as effective medications. Affected by Chinese traditional culture, many people believe that Chinese medicine is better than Western medicine and features less side effects.
Our results showed that 80.5, 82.8, and 84.3% of participants labeled “getting out more” as helpful for the GAD, depression, and schizophrenia vignettes, respectively. The results show that the participants lack knowledge about mental illness and understanding of the importance of early treatment. For the schizophrenia vignette, the other common helpful choices were being admitted to a psychiatric ward of a general or a psychiatric hospital, followed by being physically more active. Views on electroconvulsive therapy (ECT) were negative for the three vignettes, especially those with GAD and depression. However, ECT is a safe and efficacious treatment for specific mental illnesses. The medical staffs' negative views on ECT may prompt patients and their families to refuse this procedure when necessary. Therefore, the necessary efforts for educating these professionals and exploring the possibility of brief interventions must be considered in future studies.
Best Methods of Help
The rate for listening/talking with the person was the highest among all the help methods for the GAD and depression vignettes. Although this option was not the first for the schizophrenia vignette, it was followed by encouraging the person to consult a psychologist. This result was consistent with the above questions about interventions, suggesting that the participants believed that help from families or friends should be considered first, especially for the GAD and depression vignettes. Such result is expected given the low identification rates for the three vignettes, that is, people failed to recognize these conditions as diseases. People's identification of disease influences their choices of treatment. Thus, seeking help from professionals is not consequently considered necessary. Turning to family and friends for help causes no problems if they provide appropriate support, or if professional help is also sought (21).
Beliefs About Outcomes
Most participants expressed the same opinion on the prognosis of the three vignettes with or without professional treatment. The results show promise because more than half of the participants believed that the person with the diseases will fully recover with professional help, but problems would probably recur and worsen without professional help. However, the correct choice was the lowest for the GAD vignette, consistent with the identification rate. Numerous mental illnesses are chronic and persistent, with several exhibiting spontaneous remissions. This result may reflect that certain people, particularly GAD patients, would seek other non-professional interventions.
Our research showed the inadequate MHL of non-mental health nurses in China, especially the MHL for GAD. First, the identification rate was low, and the highest recognition rate was observed for the depression vignette. Although most participants for the GAD vignette thought that people with mental disorders need professional help, several deemed that help is unnecessary. In terms of specific interventions, more than 60% of the participants selected the correct drug, but several preferred giving higher evaluation scores to vitamins, minerals, and herbal medicines. Most participants thought that intervention from professional medical staff was helpful, and they also gave high ratings on lifestyle interventions. Notably, the ECT was rated with relatively low scores. More than 50% of the participants provided the right choice in the prognosis of mental disorders. These results could partially explain why many individuals with mental disorders never access services in their whole life (20). Given that the participants in our research completed a secondary specialized degree or above, and a series of research showed that increased health literacy is associated with better recognition of health problem, that is, the public may possess lower MHL (22–24). People with mental illness experience increased medical comorbidities and feature higher mortality rates than the general population (25). They may first seek treatment for somatic problems in non-mental health settings, or they may be transferred to non-mental health settings. Such condition should alert nurses and other healthcare professionals to better understand and improve mental health care for this group. Efforts should be taken to increase the medical personnel's MHL.
To close the gap in access to mental health services worldwide, the World Health Organization highlighted in its Comprehensive Mental Health Action Plan 2013–2020 an objective for all countries to achieve by 2020 (26): “to provide comprehensive, integrated and responsive mental health and social care services in community-based settings.” China has exerted efforts to achieve this goal. However, several proposals have yet to be fully activated, particularly those that focus on integrated care, thus leaving the country with serious challenges. For common mental disorders, the rates of contact (i.e., patients having contact with any general or mental healthcare providers) and provision of mental health services (i.e., delivery of evidence-based interventions, patient adherence to treatment, and retention of care and clinical and social outcomes) are low (27). As we mentioned before, mental health services and professionals are scarce in China. In addition to cultivating qualified people as soon as possible, we must find other possible ways to fill the lack of resources in this area. Increasing knowledge and positive attitudes about mental illness among the general population may improve the extent to which individuals seek help for and disclose a mental illness (28). Given that nurses are the persons who are in close contact with patients and their families, their beliefs about mental illnesses are crucial not only in providing appropriate and prompt referrals but also in influencing their attitudes toward people with mental illness. Improving the MHL of nurses can improve effective nursing interventions which may be critical to address the special needs of people with mental illness. In the absence of specialized education programs, nurses cannot provide adequate help for patients. Supplementing the education and training about mental health among nurses in China may be helpful. Actions should be taken to provide training programs to improve knowledge about mental health, awareness of how to seek help and treatment, and reduce the stigma against mental illness at the individual, community, and institutional levels. Such actions may promote the early identification of mental disorders, improve mental health outcomes, and increase the use of health services.
Conclusions
In conclusion, the MHL of non-mental health3 nurses in China is insufficient. This condition is particularly true for the case for GAD. Their ability to identify common mental diseases and their beliefs in helpful intervention and outcome need to be enhanced to reduce the disease burden caused by mental illness. More programs are needed to improve the MHL of non-mental health nurses.
Limitation
This study features major limitations that must be acknowledged. First, we only investigated four hospitals from one region, which might lead to a risk of bias in a relatively homogeneous sample. Second, the sample size was relatively small and may not represent the average MHL level of all non-mental health nurses in China. The current preliminary study must be extended to use a new and larger sample in the future research. Third, our research is a cross-sectional study that excluded determining an exact causal relationship. We have no way to assess how the nurses' MHL affects referrals or treatments of patients. Moreover, we listed multiple options for diagnosis and interventions, which might restrict the participants' choice and thoughts. We also only assessed their beliefs about interventions and not their practice in actual work. Furthermore, the professionals' behavior might be affected by local contextual factors such as accessibility to resources.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The research program was approved by the ethics committee of the Second Xiangya Hospital of Central South University. Before completing the questionnaires, we stated the aim of the study and requested consent from the participants to participate by filling in the questionnaire.
Author Contributions
TL was responsible for the study design, manuscript preparation, and revision. YH performed statistical analysis and wrote the first draft of the manuscript. QW wrote the protocol and revised the manuscript drafts. QW, XL, SC, CQ, and YX were responsible for data collection. All authors have contributed to and have approved the final manuscript.
Funding
This work was supported by grants from the National Key R&D Program of China (2017YFC1310400) and the National Natural Science Foundation of China (81371465 and 81671324). This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We gratefully thank all those have contributed to this article. We would also like to thank the nurses who volunteered their time to participate in the survey.
Abbreviations
ECT, electronic therapy; GAD, generalized anxiety disorder; MHL, mental health literacy; PTSD, post-traumatic stress disorder.
References
1. Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the world health organization world mental health surveys. JAMA. (2004) 291:2581–90. doi: 10.1001/jama.291.21.2581
2. Huang Y, Wang Y, Wang H. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiat. (2019) 6:211–24. doi: 10.1016/S2215-0366(18)30511-X
3. Charlson FJ, Baxter AJ, Cheng HG, Shidhaye R, Whiteford HA. The burden of mental, neurological, and substance use disorders in China and India: a systematic analysis of community representative epidemiological studies. Lancet. (2016) 388:376–89. doi: 10.1016/S0140-6736(16)30590-6
4. Xu J, Wang J, Wimo A, Qiu C. The economic burden of mental disorders in China, 2005–2013: implications for health policy. BMC Psychiatr. (2016) 16:137. doi: 10.1186/s12888-016-0839-0
5. General office of the state council. Guiding Opinions of the General Office of the State Councilon Propelling the Building of a Hierarchical Diagnosis and Treatment System (2016). Available online at: http://www.gov.cn/zhengce/content/2015-06/18/content_9860.htm
6. Benjamin James Sadock VAS. Kaplan And Sadocks Synopsis Of Psychiatry, 11th ed. Philadelphia, PA: Wolters Kluwer Health (2015). p. 89.
7. Lee S, Fung SC, Tsang A, Zhang MY, Huang YQ, He YL, et al. Delay in initial treatment contact after first onset of mental disorders in metropolitan China. Acta Psychiat Scand. (2007) 116:10–6. doi: 10.1111/j.1600-0447.2006.00933.x
8. Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in initial treatment contact after first onset of mental disorders in the National comorbidity survey replication. Arch Gen Psychiatr. (2005) 62:603–13. doi: 10.1001/archpsyc.62.6.603
9. Altamura AC, Dell'Osso B, Berlin HA, Buoli M, Bassetti R, Mundo E. Duration of untreated illness and suicide in bipolar disorder: a naturalistic study. Eur Arch Psychiatr Clin Neurosci. (2010) 260:385–91. doi: 10.1007/s00406-009-0085-2
10. Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P. “Mental health literacy”: a survey of the public's ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med Aust. (1997) 166:182. doi: 10.5694/j.1326-5377.1997.tb140071.x
11. Liu W, Gerdtz MF, Liu TQ. A survey of psychiatrists' and registered nurses' levels of mental health literacy in a Chinese general hospital. Int Nurs Rev. (2011) 58:361–9. doi: 10.1111/j.1466-7657.2011.00883.x
12. Chen S, Wu Q, Qi C, Deng H, Wang X, He H, et al. Mental health literacy about schizophrenia and depression: a survey among Chinese caregivers of patients with mental disorder. BMC Psychiatr. (2017) 17:89. doi: 10.1186/s12888-017-1245-y
13. Wu Q, Luo X, Chen S, Qi C, Long J, Xiong Y, et al. Mental health literacy survey of non-mental health professionals in six general hospitals in hunan province of China. PLoS ONE. (2017) 12:e180327. doi: 10.1371/journal.pone.0180327
14. Reavley NJ, Mackinnon AJ, Morgan AJ, Jorm AF. Stigmatising attitudes towards people with mental disorders: a comparison of Australian health professionals with the general community. Aust N Z J Psychiatr. (2014) 48:433–41. doi: 10.1177/0004867413500351
15. Reavley NJ, Jorm AF. Young people's recognition of mental disorders and beliefs about treatment and outcome: findings from an Australian national survey. Aust Nz J Psychiat. (2011) 45:890–8. doi: 10.3109/00048674.2011.614215
16. de Diego-Adelino J, Portella MJ, Puigdemont D, Perez-Egea R, Alvarez E, Perez V. A short duration of untreated illness (DUI) improves response outcomes in first-depressive episodes. J Affect Disord. (2010) 120:221–5. doi: 10.1016/j.jad.2009.03.012
17. Dell'Osso B, Buoli M, Hollander E, Altamura AC. Duration of untreated illness as a predictor of treatment response and remission in obsessive-compulsive disorder. World J Biol Psychiatr. (2010) 11:59–65. doi: 10.3109/15622970903418544
18. Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatr. (2010) 10:113. doi: 10.1186/1471-244X-10-113
19. Parker G, Mahendran R, Yeo SG, Loh MI, Jorm AF. Diagnosis and treatment of mental disorders: a survey of Singapore mental health professionals. Soc Psychiatry Psychiatr Epidemiol. (1999) 34:555–63. doi: 10.1007/s001270050175
20. Phillips MR, Zhang J, Shi Q, Song Z, Ding Z, Pang S, et al. Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001–001 during treatment, and assoLancet. (2009) 373:2041–53. doi: 10.1016/S0140-6736(09)60660-7
21. Morgan AJ, Reavley NJ, Jorm AF. Beliefs about mental disorder treatment and prognosis: comparison of health professionals with the Australian public. Aust N Z J Psychiatr. (2014) 48:442–51. doi: 10.1177/0004867413512686
22. Bennett CL, Ferreira MR, Davis TC, Kaplan J, Weinberger M, Kuzel T, et al. Relation between literacy, race, and stage of presentation among low-income patients with prostate cancer. J Clin Oncol. (1998) 16:3101–4. doi: 10.1200/JCO.1998.16.9.3101
23. Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients' knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med. (1998) 158:166–72. doi: 10.1001/archinte.158.2.166
24. Lindau ST, Tomori C, Lyons T, Langseth L, Bennett CL, Garcia P. The association of health literacy with cervical cancer prevention knowledge and health behaviors in a multiethnic cohort of women. Am J Obstet Gynecol. (2002) 186:938–43. doi: 10.1067/mob.2002.122091
25. Zolnierek CD. Non-psychiatric hospitalization of people with mental illness: systematic review. J Adv Nurs. (2009) 65:1570–83. doi: 10.1111/j.1365-2648.2009.05044.x
26. World Health Organization. Comprehensive Mental Health Action Plan 2013-2020 (2013). Available online at: http://apps.who.int/gb/ebwha/pdf_files/WHA66/A66_R8-en.pdf?ua1
27. Liang D, Mays VM, Hwang W. Integrated mental health services in China: challenges and planning for the future. Health Policy Plann. (2018) 33:107–22. doi: 10.1093/heapol/czx137
Keywords: mental health literacy, acknowledgment, non-mental health nurse, China, mental disorder
Citation: Hao Y, Wu Q, Luo X, Chen S, Qi C, Long J, Xiong Y, Liao Y and Liu T (2020) Mental Health Literacy of Non-mental Health Nurses: A Mental Health Survey in Four General Hospitals in Hunan Province, China. Front. Psychiatry 11:507969. doi: 10.3389/fpsyt.2020.507969
Received: 28 October 2019; Accepted: 18 September 2020;
Published: 27 October 2020.
Edited by:
Wulf Rössler, Charité – Universitätsmedizin Berlin, GermanyReviewed by:
Georgios D. Floros, Aristotle University of Thessaloniki, GreeceMythily Subramaniam, Institute of Mental Health, Singapore
Copyright © 2020 Hao, Wu, Luo, Chen, Qi, Long, Xiong, Liao and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tieqiao Liu, bGl1dGllcWlhbzEyM0Bjc3UuZWR1LmNu
 Yuzhu Hao1
Yuzhu Hao1 Qiuxia Wu
Qiuxia Wu Shubao Chen
Shubao Chen Yanhui Liao
Yanhui Liao Tieqiao Liu
Tieqiao Liu