- 1Post-Graduate Program in Medical Psychology and Psychiatry, Department of Psychiatry, Federal University of São Paulo, São Paulo, Brazil
- 2Program for Research and Care on Violence (PROVE) and Post Traumatic Stress Disorder, Federal University of São Paulo, São Paulo, Brazil
- 3Psychological Trauma Research and Treatment Program, Post Traumatic Stress Disorder, Clinical Hospital of Porto Alegre, Porto Alegre, Brazil
- 4Post-Graduate Program in Psychiatry and Behavioral Sciences, Federal University at Rio Grande Do Sul, Porto Alegre, Brazil
Objectives: The aim of this study was to validate CAPS-5 for the Brazilian-Portuguese language on a sample of 128 individuals from two centers (from the cities of São Paulo and Porto Alegre) who have been recently exposed to a traumatic event.
Methods: We performed a reliability analysis between interviewers (with a subset of 32 individuals), an internal consistency analysis, and a confirmatory factorial analysis for the validation study.
Results: The inter-rater reliability of the total PTSD symptom severity score was high [intraclass correlation coefficient =0.994, 95% CI (0.987–0.997), p < 0.001]. Cohen's Kappa for individual items ranged between 0.759 and 1. Cronbach's alpha coefficients indicated high internal consistency for the CAPS-5 full scale (α = 0.826) and an acceptable level of internal consistency for the four symptom clusters. The confirmatory factorial analysis for the 20-item original CAPS-5 did not fit the data well. A 15-item model with better results was then established by excluding the following CAPS-5 items: dissociative amnesia, recklessness, distorted cognitions, irritability, and hypervigilance.
Conclusion: Despite the limitation of the predominance of female victims, and the high number of sexually assaulted women in our sample, the model with only 15 items provided a good fit to the data with high internal consistency (α = 0.835).
Introduction
Post-traumatic stress disorder (PTSD) is a severe psychiatric condition developed after exposure to a traumatic event (1). Since 1980, when PTSD was first included in the third version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III), the definition has been changed and updated in the versions that followed (2). A traumatic event is required for the diagnosis of PTSD, and this has been highlighted in DSM-5, as PTSD is no longer classified among Anxiety Disorders, but in a specific category of Trauma and Stressor-Related Disorders (3). Other changes to the classification of PTSD have restricted what qualifies as a traumatic event and have split the symptoms into four clusters: reexperience, avoidance, negative thoughts and cognitions, and hyperarousal.
Due to the burden of traumatic events, the World Health Survey Consortium conducted a study, which demonstrated that 70.4% of the respondents of all countries had experienced at least one traumatic event in their lifetime (4). In Brazil, this number is even higher: ~80% of the Brazilian population has experienced a traumatic event, especially related to urban violence (5). This estimate raises great concern to the Brazilian public health system; an epidemiological study demonstrated that 10.2% of the trauma-exposed population in São Paulo and 8.7% in Rio de Janeiro develop PTSD (2). PTSD can cause a poorer quality of life, which consequently burdens health and social public services (3).
Due to the high prevalence of PTSD in Brazil, its proper assessment and diagnosis is crucial. Currently, the instrument recognized as the gold standard for evaluating PTSD is the clinician-administered PTSD scale (CAPS-5), a structured diagnostic interview to be applied by clinicians. In Brazil, although ICD-10 is the most used classification system regarding general medical diagnosis, concerning psychiatric diagnosis and research purposes DSM-5 is more used than ICD-10. The original scale (6), developed in English, has been last updated to match the DSM-5 PTSD diagnostic criteria (7). The scale has demonstrated high internal consistency, inter-rater reliability, and test-retest reliability. CAPS-5 also demonstrated good diagnostic correspondence with CAPS-IV (7) and has already been validated in other languages, such as Dutch and German (8, 9).
Adapting an instrument to a specific language has great significance, not only because of the language itself, but also because of the impact that differences in culture, beliefs, and behaviors have on understanding mental health (10). CAPS-5 was validated in the United States on predominantly male veterans (7), a very specific population that greatly differs from the PTSD population in the public health system of Brazil (11).
Brazilian epidemiological studies have revealed that women tend to be more often diagnosed with PTSD than men (12, 13). Ribeiro et al. (2) evaluated the conditional risk of developing PTSD following a traumatic event and found a three-fold increased risk of developing the disorder in females compared to that in males [15.9% in females (95% CI 14.2–17.6) vs. 5.1% in males (95% CI 4.0–6.2)]. These findings highlight the importance of adapting the original version of CAPS-5 to the Brazilian-Portuguese language and validating the instrument to better conduct research in Brazil.
The aim of this study was to validate CAPS-5 for the Brazilian-Portuguese language. Previously, our research team performed a cross-cultural adaptation process with a formal and structured methodology to ensure conceptual, semantic, and operational equivalence (14). In order to complete the validation process, we performed a reliability analysis between interviewers, evaluated internal consistency, and conducted a confirmatory factorial analysis (CFA). We hypothesized that the instrument would exhibit good inter-rater reliability and internal consistency, based on psychometric measurements obtained in previous studies performed in other countries (7–9).
Methods
The CAPS-5 Instrument
The scale assesses the diagnostic criteria based on DSM-5 and the intensity of the PTSD symptoms; CAPS-5 is considered the gold standard in the diagnosis of PTSD. It has 30 questions, 20 of which correspond to each DSM-5 diagnostic criterion. The first question refers to the existence of a traumatic experience (Criteria A); the original scale recommends another instrument to evaluate the occurrence of traumatic events, usually the Life Events Checklist (LEC-5) (15). The LEC-5 is a self-report measure designed to recognize potentially traumatic events in a respondent's lifetime. We also used LEC-5 to evaluate Criteria A, adapted to Brazilian-Portuguese in a previous study (16).
The 20 symptom-related questions were divided into four groups: intrusion symptoms (five items, Criterion B), avoidance questions (two items, Criterion C), negative alterations in cognition and mood (seven items, Criterion D), and hyperarousal (six items, Criterion E). Concerning other DSM-5 criteria, one question refers to how long the identified traumatic event lasted (Criteria F) and three questions to the impact of the disturbance on functionality (Criteria G). Three final questions regarding the interviewer's impression on the patient are presented, along with two questions regarding the presence of dissociative symptoms.
To evaluate frequency and intensity, which is separately assessed, the scale rated intensity as minimal, clearly present, pronounced, and extreme, and frequency is recorded as reported by the respondent as the number of times the symptom is present. After that, severity can be rated: 0 = absent, 1 = mild/subthreshold, 2 = moderate/threshold, 3 = severe/markedly elevated, and 4 = extreme/incapacitating. The symptom is consider present if its severity rating is 2 or higher (7).
Cross-Cultural Adaptation
The cross-cultural adaptation process was performed within the Program for Research and Care on Violence and PTSD (PROVE) at the Department of Psychiatry of The Federal University of São Paulo (UNIFESP) according to the model proposed by Reichenheim and Moraes (10). This process included the following steps: translation from English to Portuguese, a back-translation to the original language, a revision by an expert team, a pilot study using the adapted version, and an equivalence evaluation with the original version. This adaptation was published previously (14).
Participants
This study was conducted in two centers: at UNIFESP and at the Clinical Hospital of Porto Alegre (HCPA), which belongs to the Federal University of Rio Grande do Sul (UFRGS). The participants spontaneously sought psychiatric assistance after experiencing a traumatic event and were enrolled from the screening process of both centers, except for sample 1 described below, whose patients were addressed to UNIFESP after the first evaluation at a gynecological center, specialized to attend sexual abuse. In order to establish PTSD diagnosis, an experienced psychiatrist in attending PTSD patients performed a clinical evaluation in every patient during triage. All the participants who fulfilled the PTSD diagnostic criteria by DSM 5 after clinical assessment were invited to and agreed to participate in the study. Other inclusion criteria were to be able to understand the informed consent term (ICT), to be able to read and sign the ICT and being older than 18 years-old. Exclusion criteria were having other diagnosis besides PTSD (comorbid depression and anxiety were not excluded), and significant intellectual deficit.
The complete sample was composed of three groups of patients:
The first group (Sample 1) consisted of sexually assaulted women included in a randomized clinical trial, which is part of a thematic project sponsored by Fundação de Amparo a Pesquisa do Estado de São Paulo (FAPESP), conducted at PROVE-UNIFESP (17). The patients were enrolled between January 2016 and March 2019. The adapted CAPS-5 was applied during the screening process to select the participants for the study, together with other instruments concerning the thematic project. The scale was administrated by two trained professionals (one psychiatrist and one psychologist). All patients experienced the trauma up to 6 months before the assessment.
The second group (Sample 2) was enrolled from the screening process of PROVE outpatient's service. The participants spontaneously sought for psychiatric assistance after experiencing a traumatic event. The screening process was conducted by two professionals (one psychiatrist and one psychologist), who also applied the adapted version of CAPS-5. The patients were enrolled between March 2018 and February 2019.
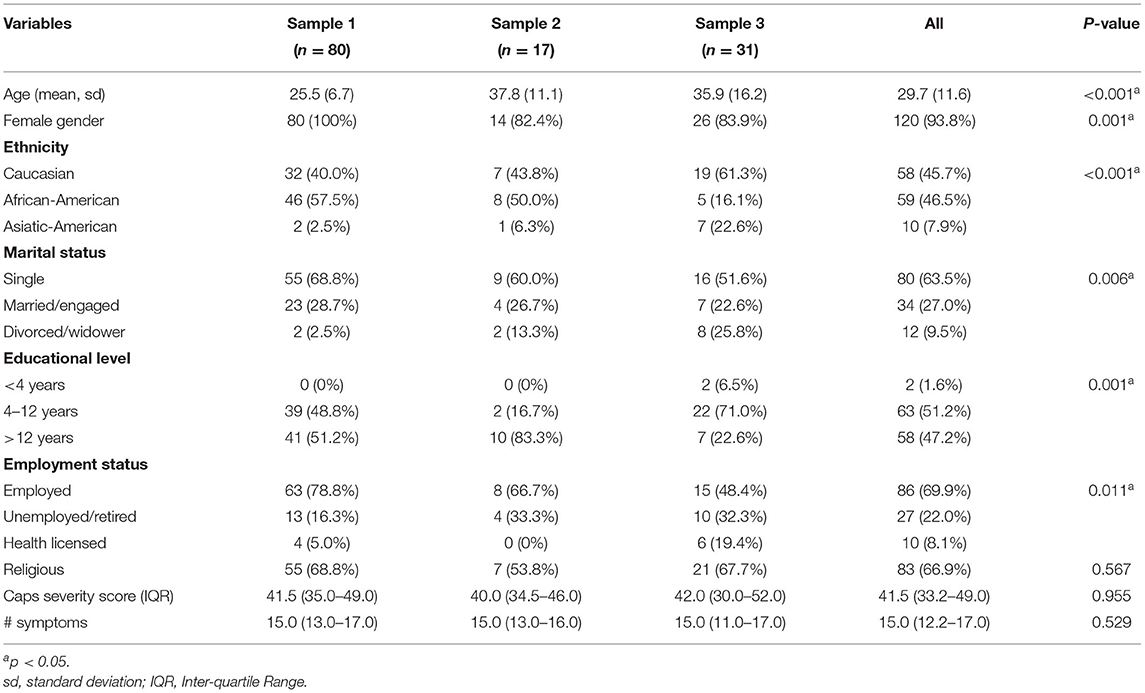
The third group (Sample 3) was enrolled at the Psychological Trauma Research and Treatment Program (NET-Trauma) outpatient service from HCPA-UFRGS. The screening process was similar to the PROVE outpatient center; patients suffering different types of trauma agreed to participate in the study. They were assessed between August 2018 and February 2019. A summary of the three samples is presented in Table 1.
All the professionals who applied the instrument were trained for CAPS-5 use. In every case, the LEC-5 scale was applied to ensure that the DSM-5 Criteria A for PTSD was fulfilled. This study was conducted with approval from the Ethics Committees of both UNIFESP and HCPA-UFRGS. All participants signed the informed consent form.
Data Analysis
Reliability Between Interviewers
We compared the results of two independent interviewers (one psychiatrist and one psychologist), who had administered CAPS-5 to the same participants. All ratings were performed by the same two raters between different groups. For the reliability evaluation between interviewers, 32 participants were selected from Sample 1 (n = 15 participants) and 2 (n = 17 participants). We calculated the Cohen's kappa coefficient, considering a confidence interval of 95% and the 20 items of the scale as ordinal variables. The kappa coefficient varies between 1 and −1, which indicates complete agreement or complete disagreement, and a value of 0 indicates a random result (18). This coefficient was applied to all of the 20 items of the scale corresponding to DSM-5 symptoms. We also used the intraclass correlation coefficient to evaluate the total PTSD severity score (19).
Internal Consistency
We combined the three samples in order to obtain the minimal number of participants acceptable for a good psychometric analysis; the final sample comprised 128 participants. The Cronbach's alpha coefficient was used to determine internal consistency, which is considered good when the value is > 0.80 and most inter-item correlations are in the recommended range of moderate magnitude (0.15–0.50) (20).
CFA
We used the final sample (with 128 participants) to elucidate whether the CAPS-5 in the Brazilian context should have the same structure as the original CAPS-5, validated in the American context. The factor structure of the adapted CAPS-5 was examined using CFA. Items were treated as ordinal variables, and parameters were estimated using the maximum-likelihood estimator method, which provides good performance for small samples and a robust chi-square. The model fit was evaluated using chi-square under the degree of freedom ratio (X2/df): values < 3 are considered acceptable for the model; Goodness of Fit Index (GFI), Tucker-Lewis Index, Comparative Fit Index (CFI): values < 0.90 indicate a lack of fit, values between 0.90 and 0.95 indicate a reasonable fit, and values between 0.95 and 1.00 indicate a good fit; Root Mean Square Error of Approximation (RMSEA): values ≤ 0.06 indicate a close fit; and Standardized Root Mean Square Residual (SRMR): values < 0.08 indicate a well-fitting model (21, 22).
For comparative analysis, we performed the chi-square, One-Way ANOVA and Kruskal-Wallis for categorical and continuous variables. Demographic information was missing for up to six patients, depending on the variable, in Sample 2. Otherwise, no other missing data were detected. The significance level of the tests was fixed at 0.05. All statistical analysis were performed using SPSS version 21 (IBM Corporation, Armonk, NY, USA). The SPSS AMOS was used to perform CFA.
Results
The sample included 128 patients: 97 patients from PROVE (Sample 1 and Sample 2) and 31 patients from HCPA-UFRGS (Sample 3). Most of the patients were female (93.8%), single (63.5%), employed (69.9%), and religious (66.9%). CAPS-5 total severity score and total amount of symptoms did not differ among samples (Table 1).
Inter-rater Reliability
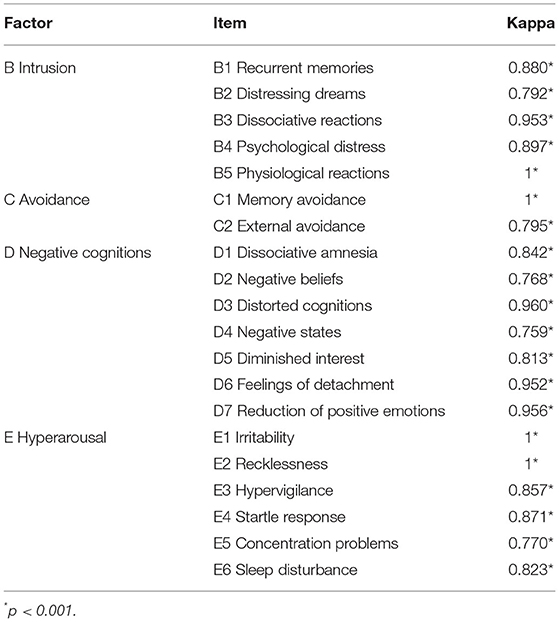
To estimate the inter-rater reliability, we considered the 32 individuals from Samples 1 and 2 who had CAPS-5 performed by two interviewers. The inter-rater reliability of the total PTSD symptom severity score was high [intraclass correlation coefficient = 0.994, 95% CI (0.987–0.997), p < 0.001]. Cohen's kappa for each item was evaluated to determine if there was agreement between the two raters. Among the 20 items from the CAPS-5 scale, we found total agreement in four (B5/Physiological distress; C1/Memory avoidance; E1/Irritability; E2/Recklessness). We found Kappa between 0.759 and 0.8 in five items (D2/Distressing dreams, k = 0.792; C2/External avoidance, k = 0.795; D2/Negative beliefs, k = 0.768; D4/Negative states, k = 0.759; E5/Concentration problems, k = 0.770). The remaining 15 symptoms resulted in a kappa value > 0.8, indicating an “almost perfect” agreement between raters (Table 2).
Internal Consistency
Cronbach's alpha coefficients indicated high internal consistency for the CAPS-5 full scale (α = 0.826) and an acceptable level of internal consistency (23) for the four symptom clusters: B/Intrusion (α = 0.631), C/Avoidance (α = 0.404), D/Negative cognitions (α = 0.701), and E/Hyperarousal (α = 0.537). Two symptoms, D1/Dissociative amnesia and E2/Recklessness, had low item-total correlations (0.025 and 0.095, respectively). The range of item-total correlations for the remaining 18 symptoms was 0.317–0.613, with a mean of 0.438. By excluding these two items, the Cronbach's alpha coefficient for the full scale increased to 0.842.
Most inter-item correlations were in the recommended range of 0.15–0.50 (20), with a mean of 0.193 across all 20 symptoms. The symptoms D1/Dissociative amnesia and E2/Recklessness exhibited low inter-item correlations, with values of 0.152 and 0.189, respectively. The mean inter-item correlation for the remaining 18 symptoms was 0.233.
CFA
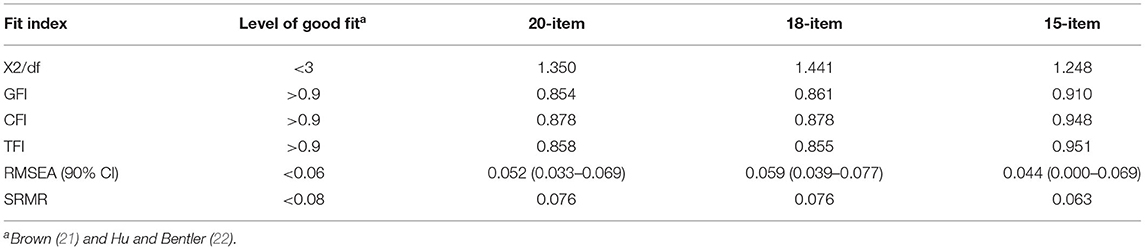
CFA with the maximum-likelihood estimation method was conducted to determine whether the factor structure indicated by the original scale could be confirmed. We performed CFA for the 20-item original CAPS-5 scale and for the 18-item model with the exclusion of two items (D1 and E2), suggested by the internal consistency analysis. The fit indices for the 18-item model were X2/gl = 1.441, GFI = 0.861, CFI = 0.878, TFI = 0.855, RMSEA = 0.059, and SRMR = 0.076, supporting a reasonable fit to the data. We concluded that the 20-item and 18-item CAPS-5 models did not fit the data adequately well.
In order to improve the performance of the instrument, we analyzed all factor loads from each item from the 18-item model. We found three items with low factor loads: D3/Distorted cognitions (0.388), E1/Irritability (0.305), and E3/Hypervigilance (0.400). All other items had factor loads > 0.40. We then performed a third CFA of the 15 remaining items. The 15-item model exhibited a good fit to the data (X2/gl = 1.248, GFI = 0.910, CFI = 0.948, TFI = 0.951, RMSEA = 0.044, and SRMR = 0.063) (Table 3).
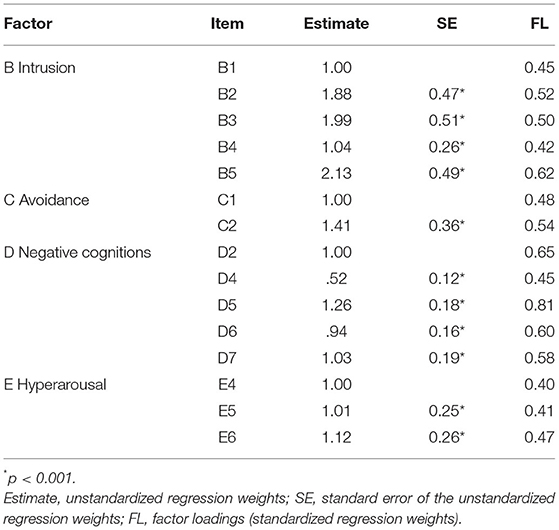
On observing the final 15-item model, all items were found to have significant loadings onto their respective latent constructs. The standardized regression weights (factor loadings) for all items were >0.3, corresponding to good-magnitude loadings (21). The occurrence of factors with item reduction (two items in factor D/Negative cognitions and three items in factor E/Hyperarousal) may explain the relatively poor loadings. The item D5/Diminished interest exhibited a high factor load: 81% of the factor variance was accounted by this item, suggesting that D5/Diminished interest is a strong indicator of negative cognition. All other factor loadings ranged between 0.40 and 0.65 (Table 4).
We calculated the new Cronbach's alpha coefficients for the 15-item model and found improvement compared with the full scale. The 15-item model exhibited high internal consistency (α = 0.835), and the two factors with item reduction maintained acceptable levels of internal consistency: D/Negative cognitions (α = 0.747) and E/Hyperarousal (α = 0.403).
Discussion
The present study describes the development of the Brazilian-Portuguese version of the CAPS-5 scale, a unique instrument for clinicians to evaluate PTSD in a structured manner in Brazil. Our research team has already translated the original English scale using a structured method published elsewhere (14). The present study now demonstrates a high inter-rater reliability for all 20 items and the total severity score. It is important to emphasize that the raters were experienced professionals in attending PTSD patients. Further studies with less experienced health-care professionals are necessary to determine the consistency of our results.
The present study has demonstrated an adequate internal consistency for the four clusters of symptoms and high internal consistency for the full scale. These findings are in line with previous scale validations for other languages (8, 9) as well as the validation of the original CAPS-5 version (7). Lower Cronbach's alpha coefficients for the cluster C/Avoidance have been reported before and can be explained by the existence of only two items in this cluster; similar results were found in the original English version and in the Dutch translated version (7, 9). On observing the items separately, we found that two items had a low item-total correlation (D1/Dissociative amnesia and E2/Recklessness), consistent with the findings of the original English version. According to the original CAPS-5 validation process (7), these findings may be attributable to a very infrequent endorsement of these two symptoms, corroborating the hypothesis that these items may be important but relatively rare symptoms of PTSD, or it may be that they are simply not representative of the PTSD construct.
A CFA was conducted to verify adequate fit to the data. Due to the similar validation process of CAPS-5 in previous studies and the existence of consolidated constructs (clusters) that explain PTSD, we decided to perform only a CFA instead of evaluating constructs from the entire scale (with exploratory factor analysis). Previous results from internal consistency analysis were used to suggest items for exclusion; the 15-item model provided the best fit to the data, compared to the full scale and 18-item model. We postulated that a 15-item model for CAPS-5 could maintain adequate results without compromising diagnostic capacity.
The use of heterogeneous data from different sources is a strength of the present study and is in contrast to the validation of the original scale, which was based on symptoms observed in only war veterans. It would be of interest for future studies to perform a more complete evaluation of the scale construct. A challenge observed in this study was the maintenance of the original structure and constructs/factors in the CFA: the occurrence of factors composed of few items can explain the relatively low factor loads. Other strong points are the well-trained professionals that were able to diagnose PTSD properly, only one research team undertaking the entire adaptation process of the scale, and strong inclusion criteria for the participants.
This study presents a limitation regarding the validation process. The main objective of this study was to adapt the scale for the Portuguese language and test its reliability and consistent validity. During the validation process, this study considered maintaining the original scale and its content validity; we did not intend to construct a different scale structure for the Brazilian context with the present results and to perform a complete validation study.
Another important limitation must be considered: although we were able to evaluate individuals from different institutions and sources, a significant number of participants were women who experienced a traumatic event related to sexual violence. To minimize the impact of using a convenience sample, we included participants from two different trauma centers and also 3 different samples, two of them with spontaneous demand, but it was observed that even in centers that receive all types of trauma in a naturalistic setting, a large number of patients are female who seek treatment for sexual assault. This is very common in a low- to middle-income country such as Brazil, where this type of trauma has a high prevalence due to the social context (24). However, this limitation compromises the generalization capacity of the study results. It is also important to mention that the original validation study for the English version had presented the same limitation, using a convenience sample composed only by war veterans, majoritarian male participants. Therefore, future studies should assess the consistency of results by comparing the 15-item scale with the 20-item scale for different types of traumatic events.
Conclusion
In developing countries, PTSD is mostly related to urban violence that has a high frequency of traumatic events, such as robbery, kidnapping, sexual assault, rape, witnessing shootings, and other life-threatening situations. This is frequently related to complex PTSD diagnoses; thus, we must ensure that the CAPS-5 is an efficient instrument to detect this reality. Establishing a validated version of a Brazilian-Portuguese diagnostic instrument to evaluate PTSD symptomatology is extremely important for researchers to better understand these issues in this socio-cultural context.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethical Committee of UNIFESP and UFRGS. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
CZ and BC were involved with the data collection. VC had data analyzed. MMa reviewed the article and helped with the discussion and the data collection. LF, MMe, and AM guided all the research process and reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by Fundação de Apoio à Pesquisa do Estado de São Paulo (FAPESP) Thematic Project number 2014/12559-5. Additional grant support came from CNPq 303389/2016-8. This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors wish to thank all the researchers involved in the Thematic Project that participated in data collection (Cecilia R. Proença, Bruna S. Nicoletta; Fernando R. Grecco; Ana Teresa D. D'Elia, Mary S. L. Yeh; Flavia F. Strumpf; Nina L. M. Valente) and the patients that contributed for increasing our knowledge on how to deal with sexual violence consequences on mental health.
References
1. American Psychiatric Association. DSM-5 Task Force. Diagnostic and Statistical Manual of Mental Disorders : DSM-5. Washington, DC: American Psychiatric Pub (2013).
2. Ribeiro WS, de Mari JJ, Quintana MI, Dewey ME, Evans-Lacko S, Vilete LMP, et al. The impact of epidemic violence on the prevalence of psychiatric disorders in Sáo Paulo and Rio de Janeiro, Brazil. PLoS ONE. (2013) 8:e63545. doi: 10.1371/journal.pone.0063545
3. Atwoli L, Stein DJ, Koenen KC, McLaughlin KA. Epidemiology of posttraumatic stress disorder: prevalence, correlates and consequences. Curr Opin Psychiatry. (2015) 28:307–11. doi: 10.1097/YCO.0000000000000167
4. Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, et al. The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychol Med. (2016) 46:327–43. doi: 10.1017/S0033291715001981
5. Teche SP, Barros AJS, Rosa RG, Guimarães LP, Cordini KL, Goi JD, et al. Association between resilience and posttraumatic stress disorder among Brazilian victims of urban violence: a cross-sectional case-control study. Trends Psychiatry Psychother. (2017) 39:116–23. doi: 10.1590/2237-6089-2016-0070
6. Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a clinician-administered PTSD scale. J Traum Stress. (1995) 8:75–90. doi: 10.1002/jts.2490080106
7. Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, et al. The clinician-administered PTSD scale for DSM−5 (CAPS-5): development and initial psychometric evaluation in military veterans. Psychol Assess. (2018) 30:383–95. doi: 10.1037/pas0000486
8. Boeschoten MA, Van der Aa N, Bakker A, Ter Heide FJJ, Hoofwijk MC, Jongedijk RA, et al. Development and evaluation of the Dutch clinician-administered PTSD scale for DSM-5 (CAPS-5). Eur J Psychotraumatol. (2018) 9:1546085. doi: 10.1080/20008198.2018.1546085
9. Müller-Engelmann M, Schnyder U, Dittmann C, Priebe K, Bohus M, Thome J, et al. Psychometric properties and factor structure of the German version of the clinician-administered PTSD scale for DSM-5. Assessment. (2018) 27. doi: 10.1177/1073191118774840
10. Reichenheim ME, Moraes CL. Operacionalização de adaptação transcultural de instrumentos de aferição usados em epidemiologia. Revista de Saude Publica. (2007) 41. doi: 10.1590/S0034-89102006005000035
11. Ramos-Lima LF, de Souza PRA, Teche SP, Freitas LHM. Trauma-related disorders in a low- to middle-income country: a four-year follow-up of outpatient trauma in Brazil. Psychiatry Res. (2019) 280:112525. doi: 10.1016/j.psychres.2019.112525
12. Andrade LH, Wang YP, Andreoni S, Silveira CM, Alexandrino-Silva C, Siu ER, et al. Mental disorders in megacities: findings from the São Paulo megacity mental health survey, Brazil. PLoS ONE. (2012) 7:e31879. doi: 10.1371/journal.pone.0031879
13. Seedat S, Scott KM, Angermeyer MC, Berglund P, Bromet EJ, Brugha TS, et al. Cross-national associations between gender and mental disorders in the World Health Organization world mental health surveys. Arch Gen Psychiatry. (2009) 66:785–95. doi: 10.1001/archgenpsychiatry.2009.36
14. Oliveira-Watanabe TT, Ramos-Lima LF, Santos RC, Mello MF, Mello AF. The clinician-administered PTSD scale (CAPS-5): adaptation to Brazilian Portuguese. Revista Brasileira de Psiquiatria. (2019) 41:92–3. doi: 10.1590/1516-4446-2018-0136
15. Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. (2004) 11:330–41. doi: 10.1177/1073191104269954
16. de Lima EP, Vasconcelos AG, Berger W, Kristensen CH, do Nascimento E, Figueira I, et al. Cross-cultural adaptation of the posttraumatic stress disorder checklist 5 (PCL-5) and life events checklist 5 (LEC-5) for the Brazilian context. Trends Psychiatry Psychother. (2016) 38:207–15. doi: 10.1590/2237-6089-2015-0074
17. Coimbra BM, Yeh M, D'Elia AT, Maciel MR, Carvalho CM, Milani AC, et al. Posttraumatic stress disorder and neuroprogression in women following sexual assault: protocol for a randomized clinical trial evaluating allostatic load and aging process acceleration. JMIR Res Protoc. (2020) 9:e19162. doi: 10.2196/19162
18. Andreoli S, Blay SL, de Almeida Filho N, de Jesus Mari J, Torres de Miranda CT, da Silva Freire Coutinho E, et al. Reliability of diagnostic instruments: investigating the psychiatric DSM-III checklist applied to community samples. Cadernos de Saúde Pública. (2001) 17:1393–402. doi: 10.1590/S0102-311X2001000600010
19. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. (1979) 86:420–8. doi: 10.1037/0033-2909.86.2.420
20. Clark LA, Watson D. Constructing validity: basic issues in objective scale development. Psychol Assess. (1995) 7:309–19. doi: 10.1037/1040-3590.7.3.309
21. Brown T. Confirmatory factor analysis for applied research. New York, NY: Guilford Publications (2015).
22. Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equation Model. (1999) 6:1–55. doi: 10.1080/10705519909540118
23. Gorenstein C, Wang YP, Hungerbühler I. Fundamentos de mensuração em saúde mental; Instrumentos de avaliação em saúde mental. Artmed Ed. Porto Alegre (2016).
Keywords: post-traumatic stress disorder, assessment, instrument validation, clinician-administered PTSD scale, psychometric evaluation validity/reliability
Citation: Oliveira-Watanabe TT, Ramos-Lima LF, Zylberstajn C, Calsavara V, Coimbra BM, Maciel MR, Freitas LHM, Mello MF and Mello AF (2021) Validation of the Brazilian-Portuguese Version of the Clinician Administered Post Traumatic Stress Disorder Scale-5. Front. Psychiatry 12:614735. doi: 10.3389/fpsyt.2021.614735
Received: 07 October 2020; Accepted: 24 May 2021;
Published: 22 June 2021.
Edited by:
Haim Y. Knobler, Hebrew University of Jerusalem, IsraelReviewed by:
Leonardo Baldaçara, Federal University of Tocantins, BrazilAndres Ricardo Schneeberger, Albert Einstein College of Medicine, United States
Copyright © 2021 Oliveira-Watanabe, Ramos-Lima, Zylberstajn, Calsavara, Coimbra, Maciel, Freitas, Mello and Mello. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thauana Torres Oliveira-Watanabe, dGhhdWFuYWVwbTc3QGhvdG1haWwuY29t
†These authors have contributed equally to this work and share first authorship
 Thauana Torres Oliveira-Watanabe
Thauana Torres Oliveira-Watanabe Luis Francisco Ramos-Lima
Luis Francisco Ramos-Lima Cecilia Zylberstajn
Cecilia Zylberstajn Vinicius Calsavara
Vinicius Calsavara Bruno Messina Coimbra
Bruno Messina Coimbra Mariana Rangel Maciel
Mariana Rangel Maciel Lucia Helena Machado Freitas3,4
Lucia Helena Machado Freitas3,4 Marcelo Feijo Mello
Marcelo Feijo Mello Andrea Feijo Mello
Andrea Feijo Mello