- 1Department of Psychology, Harvard University, Cambridge, MA, United States
- 2Department of Psychology, University of Miami, Coral Gables, FL, United States
Background: Severe irritability is a common, impairing problem among youth referred for mental health services, but evidence to guide care is limited. Treatment research can be advanced by adopting a transdiagnostic perspective, leveraging existing evidence-based treatment (EBT) techniques, and situating irritability within the context of emotion dysregulation. Accordingly, this study examined treatment outcomes for youth with different levels of irritability and dysregulation who received cognitive-behavioral therapy (CBT) or behavioral parent training (BPT) in a modular EBT framework.
Method: We analyzed data from a community-based implementation trial of a transdiagnostic youth psychotherapy. Two-hundred treatment-referred youths (7-15 years; 47% female; 33% White, 28% Black, 24% Latinx, 14% multiracial, 2% other) and their caregivers completed measures of clinical problems and emotion dysregulation at baseline, with repeated outcomes assessments over 18 months. First, latent profile analysis was applied to baseline irritability and emotion dysregulation data; then, latent growth curve models were used to examine outcome trajectories, controlling for covariates.
Results: A two-class solution fit well, differentiating youth with high (n = 54) vs. low (n = 146) levels of dysregulation and irritability at baseline. Nearly all high-dysregulation youth received either BPT (n = 26) or CBT-Depression (n = 23). Across measures, both groups showed statistically and clinically significant improvements over time. High-dysregulation youth had greater baseline severity than low-dysregulation youth, but otherwise their longitudinal trajectories were mostly similar, with few between-group slope differences. There was virtually no evidence of differential effects for BPT vs. CBT on clinical outcomes.
Conclusions: Youth with severe irritability and dysregulation, treated with a transdiagnostic, modular, EBT approach, showed significant within-person improvements over time. Their outcome trajectories did not differ according to whether they received BPT or CBT. Findings extend the literature on modular, transdiagnostic, and EBT approaches for irritability and dysregulation, suggesting comparable benefits associated with BPT and CBT when treatment selection is guided by comprehensive assessment.
Clinical Trial Registration: www.ClinicalTrials.gov, identifier: NCT03153904.
Introduction
Severe irritability is a common treatment concern among children and adolescents (herein “youth”) referred for mental health services (1). Although some degree of irritability is normative across development, severe irritability is defined as a problem of emotion dysregulation characterized by a heightened proneness toward anger (2–4). A transdiagnostic symptom, irritability is an essential or associated feature of many different diagnostic categories (e.g., disruptive, depressive, anxiety, personality, and stress-related disorders). Despite recent advances in the developmental psychopathology of irritability (5–7), research to guide assessment and treatment remains limited. The best available evidence points to behavioral parent training (BPT) and cognitive-behavioral techniques (CBT) as being effective for irritability (2, 3, 8), and some research suggests these approaches may be more effective in a personalized, transdiagnostic format (9). However, CBT and BPT are seldom investigated together in the same study, making it hard to draw conclusions about relative effects. Further, it is challenging to interpret the evidence on treatment of irritability and related constructs [e.g., chronic irritability; severe mood dysregulation; Disruptive Mood Dysregulation Disorder (DMDD); symptoms of Oppositional Defiant Disorder (ODD)] because they have been inconsistently defined and measured in the literature (6), and available studies and treatments have most often focused on related problems like ADHD (10, 11). Responding to these challenges, researchers have emphasized the need to examine irritability from more established conceptual frameworks, including emotion regulation theory (4, 7, 12–14). The current study advances this literature by investigating clinical outcomes among youth with elevated irritability and emotion dysregulation, treated primarily with BPT or CBT in a transdiagnostic, personalized framework.
Broadly, emotion dysregulation refers to a maladaptive pattern of emotional management and expression (15, 16). Theorists have come to view emotion dysregulation as a common feature across many, if not most, forms of psychopathology (16, 17). It has been proposed that emotion dysregulation arises from dysfunctions in the processes that generate emotion and occurs due to problematic emotional arousal and reactivity—i.e., when the type, intensity, frequency, and duration of experienced emotions interfere with appropriate goal-directed behavior (18–20). Others have focused on emotion dysregulation that arises from dysfunctions in the processes that regulate emotions—i.e., from dysfunctions in individuals' emotional awareness and understanding, emotion regulation goals, and ability to implement different emotion regulation strategies (21–23). These views are not mutually exclusive, and various attempts at synthesis have been made [e.g., (24)]. In the context of youth psychopathology, emotion dysregulation has been characterized (17) by the occurrence emotions that (a) endure, despite attempts at regulation; (b) interfere with appropriate behavior; (c) are context-inappropriate; and (d) change atypically, that is, too abruptly or too slowly. These parameters align with current thinking about youth irritability, defined as an “increased proneness to anger compared with peers at same development level,” situated beneath the supraordinate construct of emotion dysregulation (p. 722) (2). Diagnostically, these terms algin with DMDD in DSM-5 (25) and with ODD with Chronic Irritability/Anger in ICD-11 (6), as well as across internalizing and externalizing psychopathology more broadly.
Indeed, the two components of emotion dysregulation—generation and regulation—are involved in the development and maintenance of youth internalizing and externalizing problems. Among youth with anxiety disorders/symptoms, researchers have documented greater intensity and frequency of negative emotional experiences (26); difficulties using cognitive reappraisal effectively (26, 27); and deficits in understanding and managing emotions (28). Youth with internalizing symptoms are also more likely to use emotion regulation strategies that increase negative emotion and functional impairment. Adolescents with anxiety and depressive symptoms show less frequent use of more adaptive strategies like cognitive reappraisal, problem-solving, and acceptance, and more frequent use of maladaptive strategies like avoidance, suppression, and rumination (29). Patterns of emotion regulation strategy use have also been implicated in youth externalizing problems and disorders, with anger rumination predicting aggressive behavior (30–32). High emotional reactivity, deficits in emotional understanding, and difficulty in managing negative emotions have been linked to aggressive behavior among youth both concurrently (33–35) and prospectively (36). And youth with ADHD are more likely to experience intense negative and positive emotions and show deficits in emotion regulation (37, 38). Importantly, emotion regulation strategies are not only a feature or correlate of psychopathology; they also predict increasing psychopathology over time (e.g., rumination and internalizing problems) (39, 40). Given these findings, it seems reasonable that research might be advanced through transdiagnostic approaches that collectively considers these multiple dimensions of emotion (dys)regulation and broad and narrow forms of psychopathology.
Severe irritability represents one form of emotion dysregulation that is implicated across the spectrum of psychopathology (2, 4). Like emotion dysregulation more broadly, youth irritability shows robust associations with anxiety, depressive, and externalizing disorders (41). Nosologically, the chronic form of severe irritability (i.e., not limited to mood episodes) has been situated as a disorder of depressive mood and disruptive behavior (6). Emotion dysregulation and irritability are both viewed as transdiagnostic phenomena (2). Many of the emotion-regulatory deficits that are maladaptive in other areas of psychopathology also play a role in irritability (4, 13). Indeed, the very term “dysregulation” is often used to name dimensions and categories of youth irritability, such as DMDD and SMD (3). The overlap among relevant diagnostic categories and absence of nosological consensus around irritability and dysregulation underscores the need for researchers to use empirical methods—and to evaluate these methods—for identifying severely irritable, dysregulated youth in clinical research. Accordingly, the present study seeks to advance the literature by considering multi-informant indicators of irritability and emotion dysregulation in forming subgroups, empirically derived through latent profile analysis.
One critical gap in the literature concerns the psychosocial treatment of youth irritability and dysregulation. The last half-century of psychotherapy research has seen considerable growth in the number of treatment protocols for psychopathology, most of which target rather specific problems or diagnostic categories (e.g., depression, ADHD) (42). Among existing evidence-based therapies, two have been highlighted as first-line interventions for youth irritability: CBT and BPT. A broad intervention framework, CBT has substantial empirical support for improving symptoms across a variety of youth mental health concerns including anxiety, depression, and aggression—all of which can include irritability. Youth CBT is primarily child-directed and often considered a first-line treatment for youth with emotional disorders. Treatment focuses on teaching youth specific skills for regulating and expressing their emotions. Targeting a different set of mechanisms related to youth psychopathology, BPT is considered the first-line and most effective treatment for children presenting with aggressive or disruptive behavior. Focusing mainly on the youth's caregiver(s) and social environment, BPT seeks to alter parenting practices and reverse the negative parent-youth interactions that reinforce youth disruptive behavior. Core BPT components include labeled praise for appropriate behavior, giving effective directives, ignoring attention-seeking behaviors, and consistent implementation of consequences.
Recent developments in intervention science have increasingly moved away from problem- or disorder-specific protocols and in a more transdiagnostic direction (43, 44). This has partly reflected the growing recognition that patient presentations do not usually fit cleanly within a single category like the ones around which manualized therapies have been designed. Presentations of severe irritability and emotion dysregulation have therefore been identified as strong candidates for transdiagnostic youth psychotherapies (45, 46). One approach, the Modular Approach to Therapy for Children with Anxiety, Depression, Traumatic Stress, or Conduct Problems (MATCH), is a modular, transdiagnostic intervention targeting multiple forms of psychopathology by bringing together common therapeutic procedures shown to be effective (47). Specifically, MATCH includes behavioral/cognitive-behavioral strategies organized within protocols targeting specific psychological problems, including CBT for anxiety, depression, and trauma, and BPT for conduct problems.
We recently re-analyzed data from a randomized effectiveness trial (48) of MATCH to investigate its effectiveness for youth with severe irritability. Overall, results showed that youth with severe irritability who had been randomly assigned to received MATCH tended to show greater improvements compared to those who had received treatment with standard manualized therapies or usual care (9). Yet, this study was primarily a trial of intervention format (i.e., modular/transdiagnostic vs. standard/diagnostic vs. usual care), rendering it challenging to draw conclusions about important questions of intervention content—i.e., what techniques work best for irritable, dysregulated youth? The modular transdiagnostic guidance and clinical judgment provides some insight into how MATCH could be used clinically (45), but such guidance must be interpreted with caution in the absence of empirical evidence. More generally, there is a paucity of interventions targeting severe irritability directly (2, 8). More research is needed to understand which approaches and content (parent-focused BPT, youth-focused CBT) might be most effective for this subset of youth.
The present study seeks to help fill these gaps regarding the treatment of severe irritability and emotion dysregulation. Specifically, we use data from a community-based implementation trial of MATCH among 200 youth referred for various emotional and behavioral problems (49). In this sample, the number of youth who received MATCH was more than 3× larger than that analyzed in our previous study (9), allowing for a closer and more sophisticated analysis of outcomes. Thus, in this paper we (a) investigate treatment outcomes for empirically derived classes of youth based on their transdiagnostic profiles of irritability and dysregulation, and (b) test whether clinical outcomes differed according to whether they had received BPT for disruptive behavior or CBT for depressed mood.
Materials and Methods
Participants and Procedures
This study was part of a randomized effectiveness trial of MATCH (47), a transdiagnostic, modular, cognitive-behavioral psychotherapy protocol for youth with anxiety, depression, traumatic stress, and/or disruptive behavior [see Weisz et al. (49) for primary study details]. All participating youth received community-based empirically supported psychotherapy via MATCH. Youth and therapists were randomly allocated to either the Low-Cost condition (consisting of therapist training in MATCH, plus inexpensive elements like access to online therapist resources) or the Consultation + Low-Cost Condition (consisting of everything in the Low-Cost Condition plus weekly consultation with MATCH clinical experts). Because there were essentially no differences in clinical outcomes between the two conditions (49), we analyzed the full sample together while accounting for condition as a covariate.
Two-hundred children and adolescents (46% female; Mage = 10.73 years, SD = 2.42, range = 7-15) representing diverse racial/ethnic backgrounds (33% White, 28% Black, 24% Hispanic/Latinx, 14% multiracial, 2% other) and their caregivers were referred for youth therapy at four community outpatient mental health clinics in the Northeastern United States. Study inclusion criteria included ages 6-15 on the day of the initial study telephone screen and scoring in the borderline or clinical range on at least one relevant scale (e.g., Withdrawn/Depressed, Aggressive Behavior, Anxiety Problems, Conduct Problems, Internalizing, and Externalizing) of the Youth Self Report (YSR) or Child Behavior Checklist (CBCL). Youth were excluded if they had a recent (past-year) history of suicide attempts or hospitalization for psychiatric concerns, or if they had been diagnosed with schizophrenia, autism spectrum disorder, or an eating disorder. Families were contacted at 0, 3, 6, 9, 12, and 18 months post-baseline to participate in caregiver-report and youth-report outcomes assessments administered by masked research staff. Informed consent and assent were collected from caregivers and youths, respectively. All study procedures were approved by review boards of Harvard University and the Department of Children and Families for the State of Connecticut.
Measures
Internalizing and Externalizing Problems
Youth internalizing and externalizing problems were assessed using the CBCL and YSR (50). These are widely used, comprehensive rating scales with parallel caregiver-report (CBCL) and youth-report (YSR) forms. Items are rated on a 3-point scale: 0 (not true), 1 (somewhat or sometimes true), and 2 (very true or often true). The CBCL and YSR both generate a Total Problems scale, two broadband syndrome scales (Internalizing Problems and Externalizing Problems), and eight narrowband syndrome scales (e.g., Aggressive Behavior, Anxious/Depressed). These scales have shown strong evidence for internal consistency, reliability, validity, and utility across multiple samples (50). Both measures were administered approximately quarterly from 0 to 18 months. To promote clinical relevance in interpreting our findings, t-scores were used for outcomes analyses models using Internalizing, Externalizing, and Total Problem scale data.
CBCL/YSR Irritability
Brief parent- and youth-report irritability scales were derived from three items on the CBCL and YSR. These items tap problems with temper loss, mood lability, and stubbornness, rated on the same 0-1-2 scale as described above. The CBCL/YSR irritability scales have been used in several prior studies (51–54). Between the two informants, CBCL irritability has been used more extensively and shows better psychometric properties than YSR irritability, although both were acceptably valid and reliable in a large sample of clinically referred youth (55). In the present investigation, we use these scales as multi-informant dimensional measures of irritability (range: 0-6), administered at all occasions. Baseline irritability data showed that Cronbach's alpha was 0.64 for caregiver-report and 0.63 for youth-report.
Top Problems
The Top Problems (TP) scale (56) is an idiographic measure designed for youth and caregivers to separately identify up to three “top problems” of greatest concern to be addressed in treatment. Once youth and caregivers identified their top problems in a pre-treatment interview, they completed weekly and quarterly assessments of the current severity of each problem on a 5-point scale from 0 (not a problem) to 4 (a very big problem). Given that this is an idiographic measure where top problem content varies across participants, Cronbach's alpha is not an appropriate indicator of reliability. Prior research has shown that the TP has shown strong test-retest reliability, convergent and discriminant validity, and sensitivity to change during treatment (48, 56–58).
Irritability Top Problems
One benefit of the TP measure is that the responses given by caregivers and youth can be reliably recoded into their nearest-matching item on the CBCL/YSR using a well-established coding protocol (59, 60). Applying this protocol, we coded which TPs represented at least one of the CBCL/YSR irritability items—that is, whether or not they identified irritability was one of their TPs for treatment at baseline. Youth and caregivers who reported a TP related to temper loss, mood lability, and so on, were identified by this variable as having an irritability TP (1 = present, 0 = absent). This approach has previously demonstrated evidence of validity and reliability (1). Based on double-coding of a randomly selected 49 cases, reliability was excellent for identifying irritability TPs identified by caregiver-report (κ = 0.95) and youth-report (κ = 0.98).
Emotion Regulation and Dysregulation
The Emotion Regulation Checklist (ERC) (61) is a 24-item parent-report questionnaire used to assess youth's ability to manage emotions. Caregivers were asked to rate items on a 4-point Likert scale from 1 (never) to 4 (always) across two scales: Emotion Regulation (e.g., happiness, recovering from negative mood, positive responses to adults and peers) and Lability/Negativity (e.g., outbursts of anger, intrusive enthusiasm, frustration, mood swings). Evidence supports the reliability and validity of the ERC (61). In this sample, reliabilities were 0.83 for negative lability and 0.55 for regulation.
The Children's Emotion Management Scale (CEMS) (62–64) was used to examine how youth managed their sadness (12 items), anger (11 items), and worry (13 items). The CEMS subscales assess youths' inhibition, dysregulation, and coping patterns with respect to each particular emotion (i.e., 3 subscales, 3-5 items each, within each emotion). Dysregulation measures inappropriate emotional expression (e.g., “I do things like slam doors when I'm mad,” “I cry and carry on when I'm sad.”) and coping measures adaptive methods of emotion regulation (e.g., “When I am mad, I can control my temper,” “I keep myself from losing control of my worried feelings”). Youth and their caregivers were asked to rate items on a 3-point Likert scale from 1 (hardly ever) to 3 (often). The present analyses used composite scores for emotion coping (calculated as the mean of sadness coping, anger coping, and worry coping scores) and emotion dysregulation (calculated as the mean of sadness dysregulation, anger dysregulation, and worry dysregulation scores). The CEMS has shown good reliability and validity (2–6), with alpha of 0.71 for coping and 0.64 for dysregulation.
Analytic Approach
Analyses were conducted within a latent multivariate framework, in two phases.
Phase 1: Latent Profile Analysis (LPA)
First, we used latent profile analysis (LPA) to differentiate high- vs. low-dysregulation classes of youth based on 10 indicators: (a) irritability levels, as rated on the CBCL and YSR three-item scales; (b) caregiver and youth identification of irritability as a treatment concern on the TP measure; (c) emotion regulation, as indicated by the CEMS Coping scale and ERC Regulation scale; (d) emotion dysregulation, as indicated by the CEMS Dysregulation scale and the ERC Lability/Negativity scale; and (e) overall psychopathology on the CBCL and YSR Total Problem raw scores, minus the three irritability items. Irritability TPs were binary variables, treated as probability estimates. Continuous variables were standardized. The emotion regulation variables (CEMS Coping and ERC Regulation) were the only measures where higher scores are considered more favorable; the other measures follow the reverse pattern, where higher scores are considered more severe. As shown in the results, LPA can accommodate these different types and directionality in the data. These 10 variables were selected to collectively capture the key facets of the relevant phenomena—including severe irritability specifically as well as the generation, regulation, and dysregulation of negative emotions broadly—per two informants, multiple methods, and in multiple directions.
Considering the overall complexity of our analytic plan and our a priori goal of investigating treatment outcomes for youth with high vs. low levels of multivariate dysregulation/ irritability, we decided to simply estimate a two-class LPA solution and then evaluate its fit overall and relative to a one-class solution. This focused two-class strategy follows in the tradition of some of the earliest applications of latent class/profile modeling (65). More recently, it has been used by Young (66) and Youngstrom (67) to delineate impulsive/reactive aggression constructs in clinical samples. In other LCA/LPA applications, investigators may enumerate many more classes to identify the best-fitting solution—e.g., going up to 6, 7, or more classes, or until convergence problems or fit decrements are encountered. We have adopted this type of thorough k-class enumeration approach in our own work, as appropriate to the research question and the data (68). But this practice requires very large samples and some rather subjective-decision-making on the part of the analyst, leading quantitative experts to recommend that it is almost always advisable to specify a focused a priori hypothesis, especially in smaller samples (66). It is possible that our data would reveal that a 3- or 4- or 5-class solution might also fit these baseline data, but such a solution would be inconsistent with the literature and our research question, adding greater complexity to our models while also limiting the utility and generalizability of our findings. Indeed, to continue with class enumeration risks the possibility of spuriously over-extracting classes that do not really exist (69), with the size classes getting smaller, chipping away at the major classes, and threatening the generalizability of the findings. Thus, for this analysis, the two-class solution of high and low dysregulation was well-justified and offered the greatest power for exploring treatment outcomes.
After estimating and evaluating our LPA, all 200 youths were assigned to their most likely class membership: high dysregulation and irritability (hereafter “HIDYS”) or low dysregulation and irritability (“LODYS”). These class assignments and their uncertainty (i.e., posterior probability of class assignment) were exported for subsequent analysis. Characteristics of youth within each latent profile were explored to assess the groups' validity and clinical, demographic, and study characteristics.
Phase 2: Latent Growth Curve (LGC) Models
Next, the two LPA-derived classes were specified as predictors of clinical outcome trajectories via latent growth curve (LGC) models. Our overall approach to these analyses draws from the log-transformed modeling strategy used in several prior randomized trial studies (9, 48, 57), including the primary outcomes of the present study (49). That is, we estimated outcome trajectories as longitudinal models wherein our metric of time was the natural logarithm of the number of days since baseline +1. This approach produces a single log-linear slope coefficient useful for interpretation of clinical outcomes. It is also more parsimonious than alternative approaches such as polynomial strategies to achieve a similar result with more terms (linear + quadratic) or estimating different outcome occasions separately (3-month, 6-month, etc., producing 5× more outcomes to interpret). Results confirmed that log-linear slopes fit the data well.
Substantively, our first question in these models was whether HIDYS and LODYS youth differed in their trajectories of improvement over time. It was expected that youth in the HIDYS group would show greater severity at baseline, but it was not clear whether they would improve faster or slower than the LODYS group over time. If the HIDYS group improved faster, this might suggest they are showing a greater response to intervention and/or a pattern of regression to the mean (i.e., higher scores have more room to decline simply as a function of chance and time). If the HIDYS group improved more slowly (or showed no change, or even deteriorated), this would indicate that highly dysregulated and irritable youth are not responding as well to MATCH in the same way that the majority of the sample is. And if the two groups showed parallel trajectories of improvement over time, this would suggest MATCH was similarly beneficial for all youth in this sample, irrespective of whether they are HIDYS or LODYS.
Our second question in these LGC models was about the relative effects of MATCH primary problem/protocol area, DEP or CON. That is, based on results of the baseline clinical assessment, youths were classified into their most appropriate treatment track, including (a) those who were viewed as having a primary depression problem and treated with the MATCH Depression CBT protocol (“DEP”); and (b) those who were viewed as having a primary disruptive behavior problem, and treated with the MATCH Conduct Problems BPT protocol (“CON”). If assignment to DEP vs. CON showed significantly different effects on slopes, this would indicate a differential treatment response favoring either CON or DEP. If they were not different, this would suggest that CON and DEP are similarly effective in for treating youth with HIDYS and LODYS profiles.
These questions were investigated in a series of multigroup LGC models for each outcome variable. Within each model, results were simultaneously estimated separately for two groups (HIDYS, LODYS) with major protocols—the MATCH Depression and Conduct protocols (DEP, CON)—modeled as fixed effect predictors of intercepts and slopes within group. The parameters of interest were the coefficients for latent intercepts and slopes within the HIDYS and LODYS groups, as well as the coefficients for the effects of CON and DEP on those slopes. Study questions were examined through individual model χ2 Wald tests of the equality of these coefficients. A statistically significant χ2 contrast for the latent intercepts of HIDYS and LODYS would mean one group had higher baseline problem levels than the other group; and a slope difference would mean that one group showed faster problem reduction than the other. Regarding treatment type, if the effect of DEP on slope was different from the effect for CON on slope, this would indicate differential effectiveness such that membership in one protocol/problem group (DEP vs. CON) predicted faster improvement than the other. Significant differences were investigated by examining other model terms to help contextualize the differential effect on slopes, and by probing the differences within each group.
LGC models controlled for covariates representing demographics (age, gender, race), study and treatment variables (clinic, RCT condition, medications, number of sessions), and uncertainty of class assignment. Covariates were specified as predictors of latent slopes and intercepts and were constrained to be equal across groups. Therapist nesting was not included in group-specific models due to the complex patterns of cross-nesting of therapists often treating patients in both LPA groups. Models were estimated in Mplus Version 8 with robust maximum likelihood estimation. Variables were mean-centered within dysregulation groups, such that the latent intercept and slope terms can be interpreted as representing the trajectories for hypothetical average HIDYS and LODYS youth. Baseline indicators of LGC slopes and intercepts were held to variance at 0 for model convergence.
Results
Class Differentiation
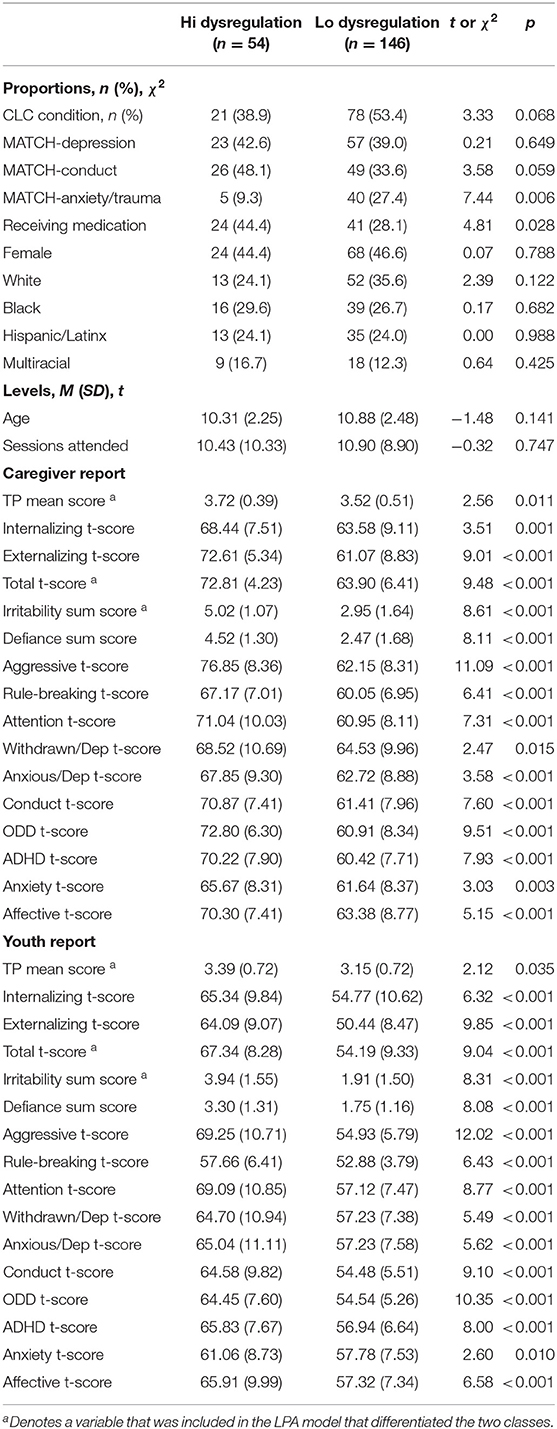
The two-class solution converged successfully and fit the data well. Entropy was 0.839, indicating a high degree of “cleanness” in the separation between the two classes. Average latent class probabilities for most likely class membership was 0.931 for Class 1 (HIDYS) and 0.966 for Class 2 (LODYS). The Lo-Mendell-Rubin (LMR; p = 0.0137), Vuong-LMR (VLMR; p = 0.0128), and bootstrapped (p < 0.0001) likelihood ratio tests all showed that the two-class solution fit the data better than a one-class solution, and the pattern of AIC/BIC results between the one- and two-class models supported this conclusion as well. Figure 1 presents the two profiles that characterized youth with high (n = 54; 27%) and low (n = 146; 73%) levels of dysregulation and irritability. As shown, the highly dysregulated group was nearly 1 SD above the sample mean on measures of irritability, dysregulation, and total problems. They also had below-average levels of coping/regulation skills and were considerably more likely to have a TP defined by irritability, especially by youth report.
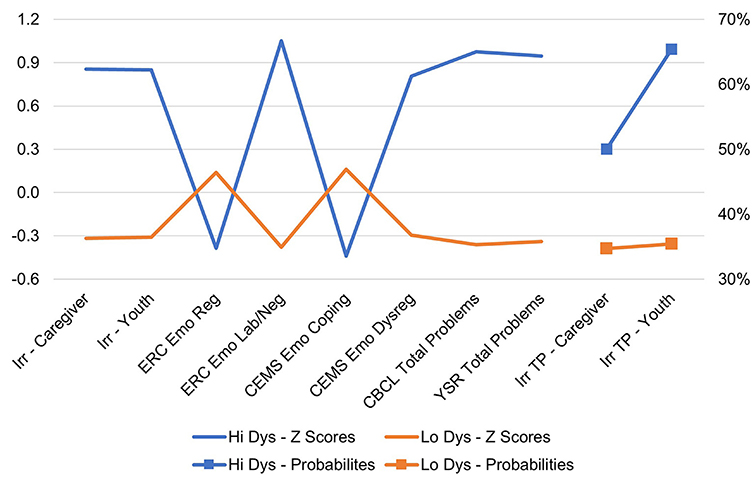
Figure 1. Two latent profiles: high dysregulation (n = 54) and low dysregulation (n = 146). Irr, irritability; ERC, Emotion Regulation Checklist; CEMS, Children's Emotion Management Scales; CBCL, Child Behavior Checklist; YSR, Youth Self-Report; TP, top problems.
Table 1 presents further results showing the clinical and demographic characteristics of the two groups. The HIDYS group showed significantly greater severity on the TP and all CBCL/YSR symptom scales and were significantly more likely to be receiving medication and less likely to be receiving the anxiety protocol. However, there were no differences in terms of study condition, gender, race/ethnicity, age, or number of sessions attended. Table 1 also reveals that youth in the HIDYS class tended to be most often assigned to Conduct (48%) and Depression (43%) MATCH protocols, with only five (9%) falling into the Anxiety or Trauma protocols. Youth in the LODYS Class were somewhat evenly distributed across the protocols for Conduct (34%), Depression (39%), and Anxiety/Trauma (27%). In other words, proportions were sufficient to allow us to compare the effects of Conduct (CON) vs. Depression (DEP) protocols within both the LODYS group (n = 49 vs. n = 57, respectively) and within the HIDYS group (n = 26 vs. n = 23, respectively). Given the smaller size of those in the Anxiety/Trauma group, an examination of treatment outcomes for this group was not possible. Instead, analyses focused on the effects of CON group membership and DEP group membership as binary predictor variables, with specific implications for results interpretation noted below where applicable.
Clinical Outcomes for Youth With High and Low Dysregulation
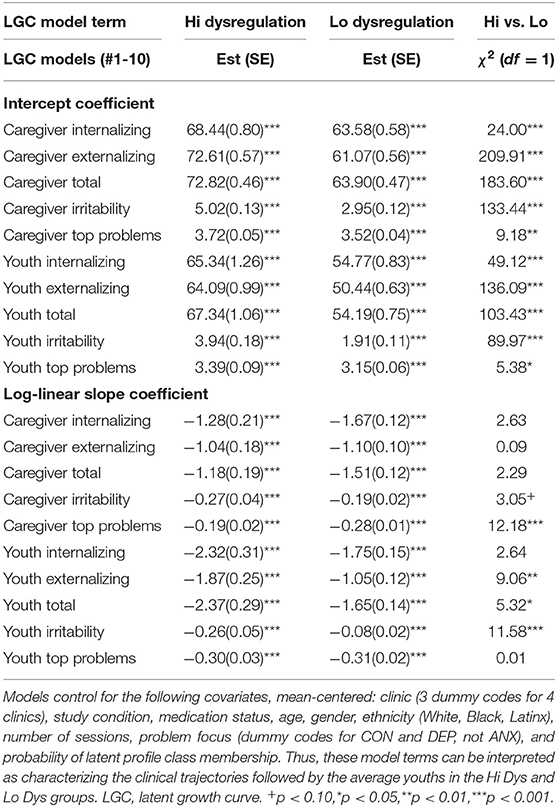
Outcome trajectories for these the HIDYS and LODYS groups were examined in a series of ten LGC models—five for youth-report variables and five for caregiver-report variables. For brevity and clarity, these results are presented in Tables 2, 3 and Figures 2A,B organized by coefficient and model number. That is, across all table sections and figure panels, results labeled with the same model number (#1-10) were generated from the same LGC model. The model-implied and observed outcome trajectories followed by youths in the HIDYS and LODYS groups are presented in Figures 2A,B, with the corresponding intercept and log-linear growth coefficients reported in Table 2. Generally, the degree to which group intercepts (i.e., baseline levels) and log-linear slopes (i.e., change over time) appear visually similar in these charts is a reasonable indicator of whether they are statistically different, with the exact χ2 (df = 1) difference tests reported in the far right column of Table 2.
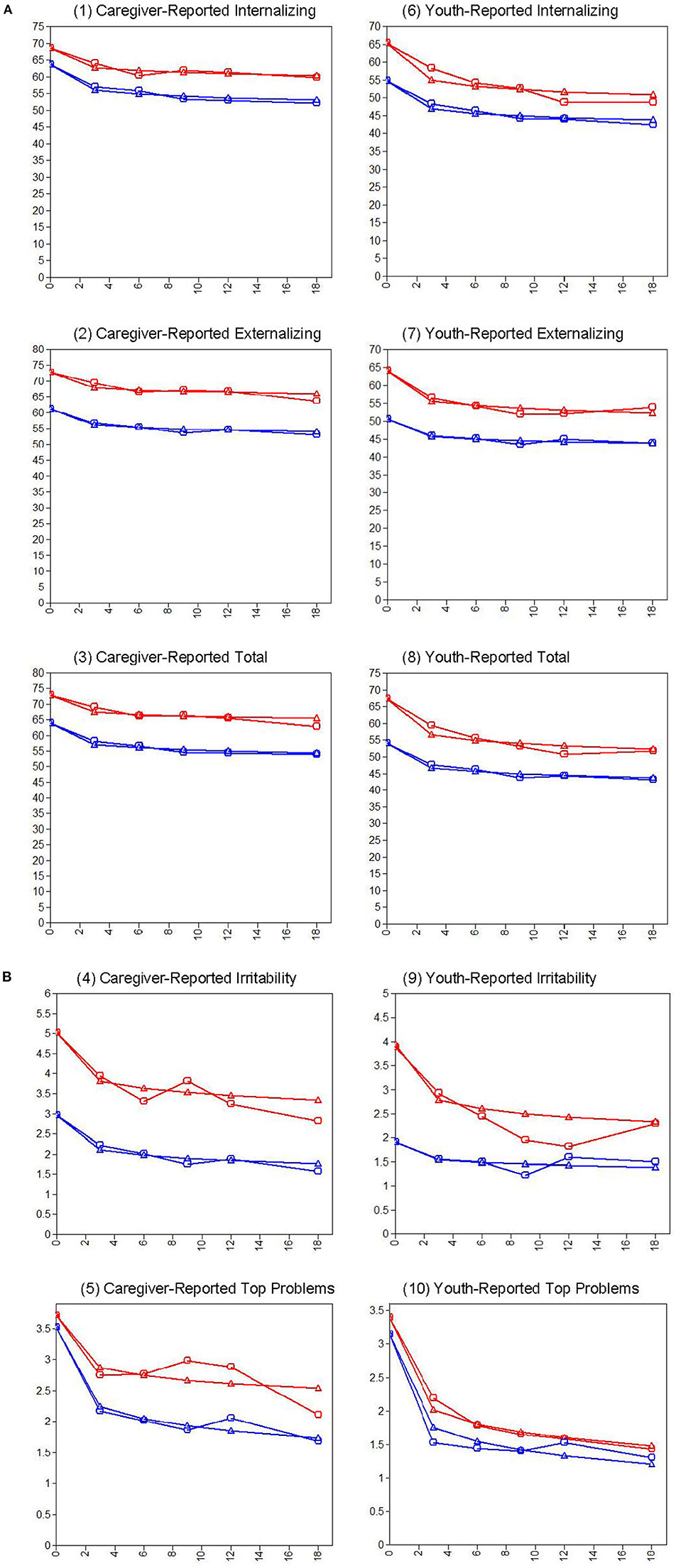
Figure 2. (A) CBCL and YSR problem trajectories for youth in the high dysregulation (Red) and low dysregulation (Blue) groups over time (0 to 18 months). Models control for the covariates noted previously (Table 2). (B) Irritability and top problem trajectories for youth in the high dysregulation (Red) and low dysregulation (Blue) groups over time (0 to 18 Months). Models control for the covariates noted previously (Table 2).
On all outcome measures, the HIDYS group showed significantly higher problem scores at baseline compared to the LODYS group (top portion of Table 2). This is as expected given how the classes were formed, but the consistency of this result across internalizing and externalizing problems is notable because classes were not formed based on those scales. In terms of outcomes, caregiver- and youth-rated internalizing, externalizing, total problems, and irritability all showed statistically significant log-linear declines over time, and this effect was largely similar between the high and low dysregulation groups (bottom portion of Table 2). On caregiver-rated internalizing problems, for example (see Table 2), youth in the HIDYS group started at 68.44 and improved over time at a rate of −1.28 points per log-day, whereas the LODYS group started at 63.58 and improved at a rate of −1.67 points per log-day. These trajectories differed in their baseline scores (χ2 = 24.00, p < 0.001) but not in their rates of change over time (χ2 = 2.63, p = 0.105).
This same pattern for HIDYS vs. LODYS results held across 6 of the 10 outcome variables. That is, the two groups differed at baseline but showed statistically similar slopes of improvement over time on CBCL irritability, internalizing, externalizing, total problems, and on youth-reported top problems and internalizing problems. The other 4 outcome measures, where slopes differed, can be interpreted as follows. On youth-rated irritability, externalizing, and total problems, the HIDYS group was more severe at baseline and improved faster over time than the LODYS group. The values on the scale metrics suggest that, despite these statically significant slope differences, trajectories of improvement were clinically significant for both groups. For example, in both groups youth-reported Total Problems dropped several points below the cutoffs for the “Borderline” (t-score ≥ 60) and “Clinical” (t-score ≥ 63) ranges, per Achenbach and Rescorla's interpretive guidelines (50). In fact, this was the case for the outcome trajectories for both groups, per both informants, on all normed outcome measures. Lastly, on caregiver-rated TP severity, the groups showed somewhat more similar ratings at baseline (though still statistically different), and over time the LODYS group improved faster than the HIDYS group. These diverging trajectories are potentially meaningful, result in a ~1-point score gap at 18-months, with the HIDYS falling closer to the 4 (very big problem) end of the severity scale and the LODYS group winding up closer to 0 (not a problem).
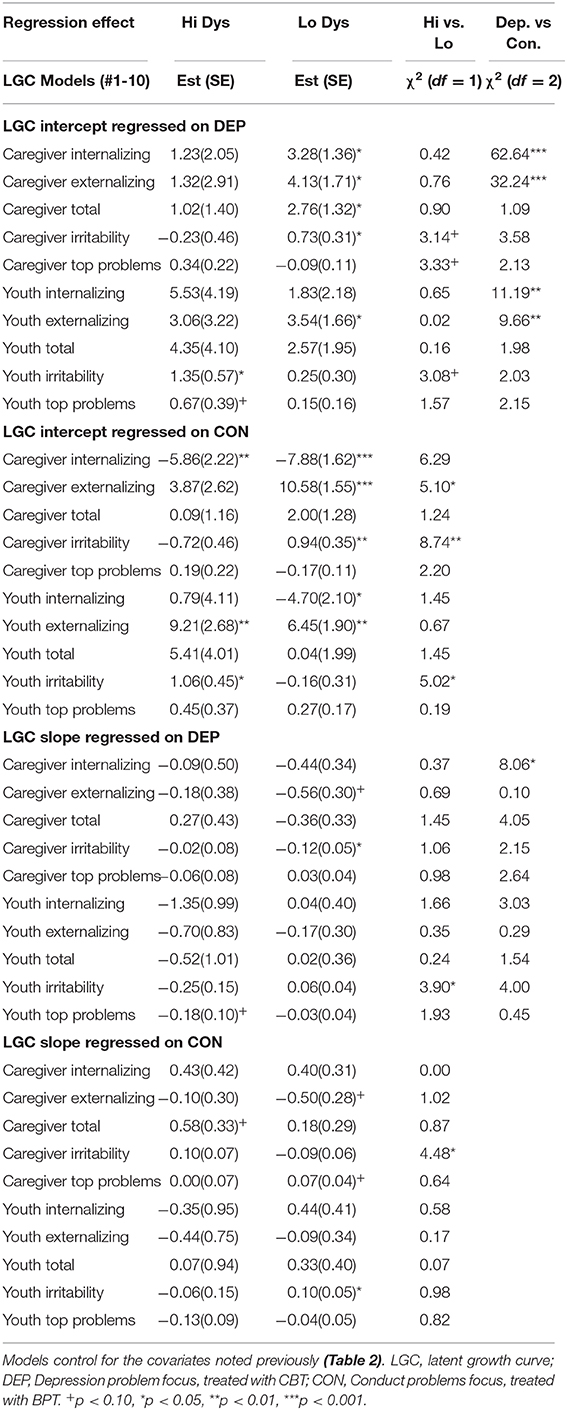
Effects of BPT-Conduct and CBT-Depression Protocols on Outcome Trajectories
The effects of LGC intercepts and slopes regressed on DEP and CON are presented in Table 3. Again, these DEP and CON variables represent binary dummy codes for 2 of the 3 possible MATCH primary problem/protocol areas; thus, the values presented in Table 3 can be interpreted as regression coefficients summarizing the effects that membership in the DEP or CON group had on “nudging” the LGC intercepts and slopes, relative to an ANX reference group (for which estimates are not presented). The benefit of this approach is that it yields results for the absolute effects that DEP and CON have on LGC slopes and intercepts (i.e., whether the effect is different from zero, reported in the HIDYS and LODYS columns) as well as a method for comparing the relative size of those effects in the rightmost two columns. Specifically, the model Wald χ2-tests in this table show whether the coefficients for those effects (a) differ from one another (“Dep vs. Con” column) and (b) whether they differ between the dysregulation groups (“Hi vs. Lo” column).
Of highest interest are the effects of DEP and CON on latent slopes (see Table 3, far right), where significant slope contrast values served as a gateway for further inspection of the other terms in the table. Here, there was only one outcome out of 10—caregiver-rated internalizing problems—that showed a significant differential effect for DEP vs. CON, χ2 (2) = 8.06, p = 0.018. When probed, the DEP vs. CON effect on slope was evident in the LODYS group (χ2 (1) = 7.37, p = 0.007) but not the HIDYS group (χ2 (1) = 1.18, p = 0.278), and was also accompanied by a differential effect on intercept (χ2 (1) = 17.40, p < 0.001). These results (see Figure 3) suggest that these effects within the LODYS group might be accounted for by regression to the mean, where those treated with DEP had much higher internalizing t-scores at baseline compared to those treated with CON in that same group. It makes sense that youth with higher internalizing scores should be treated with DEP, and that they would decline faster, for reasons of treatment appropriateness and perhaps regression to the mean. Further, the LODYS-CON youth had little room to improve, as they were already below the threshold for clinical significance (t < 60) on caregiver-rated internalizing problems at baseline.
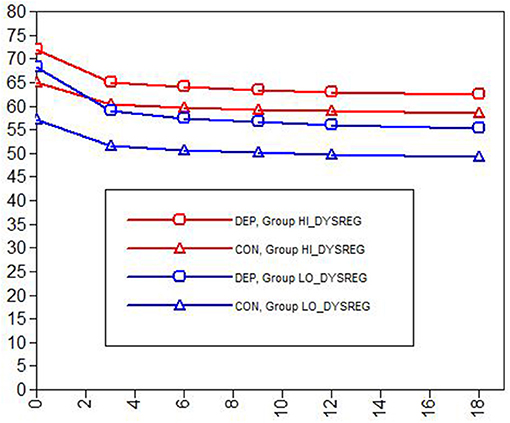
Figure 3. Caregiver-rated internalizing problems by dysregulation group (HI vs. LO) and problem/protocol (CON vs. DEP). DEP, Depression problem focus, treated with CBT; CON, Conduct problems focus, treated with BPT.
Discussion
We investigated multi-informant clinical outcome trajectories for two latent classes of treatment-referred youth—those characterized by high vs. low profiles of irritability and emotion dysregulation—and we tested whether these trajectories differed for those treated with BPT for conduct problems vs. CBT for depression. Overall, two findings emerged. First, high- vs. low-dysregulation youth were mostly similar in their trajectories, showing statistically and clinically significant improvement over time. Although a few significant differences in slopes emerged (caregiver top problems and some YSR scales), the overall pattern (Table 2, Figures 2A,B) was one in which both groups showed clear improvements across all measures. Second, we found virtually no evidence of different treatment outcomes based on one's primary problem/protocol area. That is, in treating clinically referred youth with (or without) severe dysregulation, a modular transdiagnostic approach involving BPT for externalizing problems and/or CBT for depression appears to be helpful. Importantly, the highly dysregulated youths (27% of the sample) showed significant and comparable improvements in all outcomes regardless of whether they received BPT (n = 26) or CBT (n = 23) as a primary approach.
One important caveat should be highlighted here to inform further interpretation of our findings: There was not random assignment to problem/protocol (CBT-Depression vs. BPT-Conduct), so causal explanations cannot be drawn as if this were a randomized trial comparing these two approaches. But while random treatment allocation is appropriate for causal inference regarding effectiveness, the world of routine youth mental health care is one of non-randomized allocation. That is, community clinicians do not randomly select one of two protocols to administer to patients referred to them who meet eligibility criteria. Instead, best practices involve conducting a comprehensive baseline assessment and developing a treatment plan involving EBTs based on the best available evidence, clinician judgment, and family preference. In this regard, our non-randomized comparison of CBT vs. BPT for youths with high and low dysregulation represents more of a real-world comparison and a useful contribution to the literature, highlighting the potential value of prospective randomized trials in the future.
In regard to the four variables where the groups' slopes differed, the pattern of this difference varied by informant and appeared to be largely related to baseline differences. For instance, on youth-rated externalizing, total, and irritability, the HIDYS group improved faster than the LODYS group. This pattern may suggest greater clinical benefits for the HIDYS group; however, it is a small difference with unclear practical significance and likely related to regression to the mean (i.e., youth in the HIDYS group started treatment with higher scores, and therefore had more room to improve even if only due to random chance with the passage of time). More importantly, both groups improved to such an extent that they fell well below the borderline and clinical cutoffs on these measures, consistent with the overall pattern described above. However, a unique pattern was observed for caregiver-rated TP severity, where the groups were equivalent at baseline and the LODYS group improved faster than the HIDYS group. Importantly, this suggests that greater levels of dysregulation/irritability predicted slowed improvement and greater treatment needs in these personalized domains of functional problems, at least per caregiver report. Alternatively, this pattern might be explained by the unique properties of the TP measure, which is designed to pull for high scores from all participants at baseline, regardless of clinical severity. That is, although the HIDYS and LODYS groups appeared similarly severe on TPs in a subjective, idiographic sense (see intercepts in Figure 2A, Panel 5), we know that the HIDYS group was more severe at baseline in an objective, nomothetic sense (see Figure 1, Table 2). Thus, caregiver TP scores for the LODYS group should be interpreted in light of these properties—i.e., there might be some degree of inflation in the LODYS baseline TP scores, and one might expect their scores to drop faster simply as a function of the group's lower overall severity (as seen across all other measures and informants).
Implications and Limitations
One important aspect of this study's design was that a thorough clinical assessment was conducted at baseline in order to guide treatment according to how each case was conceptualized. Youth whose assessment data indicated a primary mood problem received CBT, whereas those whose primary problem was disruptive behavior received BPT (2, 45). Although assessment is sometimes given limited attention in intervention research, accurate identification of the problem is an essential precondition for effective treatment. Perhaps especially in youth mental health, careful measurement is important and challenging, requiring multi-informant, evidence-based assessment approaches (60, 70, 71). Challenges with assessment and diagnosis of severe irritability are what prompted a groundswell of controversy and research in this area to begin with, and which continue presently (3, 6). Differential diagnosis for youth irritability can involve over a dozen different diagnostic categories—cutting across internalizing, externalizing, neurodevelopmental, and other domains—of which irritability is a core symptom or associated feature. Interventions such as MATCH rely heavily on assessment data for (a) the initial routing of the treatment plan to target a core problem area, and (b) ongoing progress-monitoring for treatment personalization and outcomes evaluation (48, 49). Thus, effective intervention for severe irritability begins with an effective assessment to clarify the presentation and focus of treatment (9, 45).
Treatments like MATCH might be considered part of a “first-generation” of transdiagnostic protocols—what some have begun calling “multi-diagnostic” rather than truly transdiagnostic. Research is emerging on promising new transdiagnostic approaches. One example is FIRST (72–74), which includes cross-cutting evidence-based principles that have been shown to be effective for disruptive behavior, mood, and anxiety problems; thus, a therapist could employ one or more principles tailored to address irritability and dysregulation as it manifests across these different dimensions of psychopathology. Another example is the Unified Protocol for Children and Adolescents (UP) (75), which was originally developed for emotional disorders (i.e., anxiety, depression) and has recently been adapted for irritability/anger as well (46, 76). Rather than compiling a large, complicated menu of treatment elements as MATCH does, these newer interventions focus more on transdiagnostic principles that have evidence supporting their effectives across major swaths of youth psychopathology (e.g., emotional disorders, or internalizing and externalizing disorders). It is possible that interventions like FIRST and UP, which do not require the clinician to classify each patient into this or that category, would be more efficient and effective. These are important questions for future research.
Some limitations and strengths should be noted. Limitations include the lack of certain instrumentation that could have shed further light on study questions. Namely, diagnostic data were not collected; nor were there multi-informant or multi-modal assessments of irritability, mood, or emotion dysregulation beyond the caregiver and self-report versions included here. More objective interviewer, behavioral, and physiological data could be helpful in future studies, especially to appropriately measure the emotion generation vs. regulation components of emotion regulation phenomena. However, the present study did help overcome these challenges by using carefully selected indicators in line with an irritability and emotion dysregulation framework, to tease apart empirically derived profiles of high vs. low dysregulation. This represents a methodological improvement over prior secondary analyses of trial data, which have employed observed variables with greater measurement error (9, 10). One additional strength of the present study is the diversity reflected in the participant sample, and the implementation of procedures in routine care settings with community clinicians. By nature, LGC models are exploratory, so generalizability and replicability may be limited. Alternative “manual” approaches to sample splitting are sometimes used, such as using a median split or applying cutoffs on one or more measures. This approach has been used in previous analyses attempting to simulate an randomized trial comparing different therapies among a subsample with irritability and impairment (9). However, these approaches are only as strong as the chosen instruments, informants, and cutoffs, which all have their own limitations. In the present study, such concerns were mitigated by our multivariate two-class LPA, our four community outpatient clinics, and the diverse clinical and demographic characteristics of our sample—all of which help promote generalizability and replicability. Lastly, our data cannot speak to specific treatment elements that might be responsible for the observed clinical gains, or the mechanisms of change underlying those gains. It is likely that well-established therapeutic principles in these EBTs (e.g., behavioral activation, changing environmental contingencies, increasing positive attention, restructuring negative cognitions, exposure, and rehearsal of adaptive behaviors) are likely to play important roles [for a practitioner-oriented discussion, see (45)]. It is important for future research to disentangle therapeutic components and mechanisms, to support the development of more personalized and effective approaches.
Conclusions
The present findings lend support to the notion of applying “old” treatments (CBT, BPT) to “new” problems (irritability/dysregulation), at least when doing so is guided by assessment data and clinician judgment. Well-established cognitive-behavioral treatments and principles provide large toolbox of potentially effective tools. These tools seem to remain effective for practitioners who continue to treat common presentations of emotional and behavioral disturbance in youth, even as researchers work to shed light on new questions about irritability and dysregulation within the context of those presentations. Indeed, evidence-based practice requires using strategies that are known to be effective in general, applying them with a particular youth, a particular clinician, and a feedback loop involving treatment guided by assessment guided by treatment—and so on (77). In this regard, the present study advances the literature while also highlighting important directions for future research. Specifically, there is a need to learn how to make new and old interventions even more effective for a variety of clinically referred youth populations—including the most irritable and dysregulated among them.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by The Committee on the Use of Human Subjects at Harvard University; and the State of Connecticut, Department of Children and Families' Institutional Review Board (IRB). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
SE was responsible for the initial conceptualization, data curation, analysis, writing, and editing of this paper. MW and SH contributed to the literature review and initial drafting. JW was principal investigator on the study and made contributions including data, resources, and editing/revising. All authors contributed to conceptualization, reviewing, approved, and agreed to the submission of this manuscript in its current form.
Funding
This study was directly funded by the Child Health and Development Institute of Connecticut (contract number 14DCF6673AA), with additional support from the Norlien Foundation. SE gratefully acknowledges research support from AIM for Mental Health (Clinical Science Fellowship), National Institute of Mental Health (Clinical Loan Repayment Program), American Psychological Foundation, and Harvard University during the preparation of this manuscript.
Conflict of Interest
JW is a co-author of the treatment protocol (MATCH; Chorpita & Weisz, 2009) used in this study and receives some income from its sales.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank the youth and families who participated in this study. We are grateful to all research staff who participated in the collection and validation of these data. Portions of this research were presented at the 2020 Meeting of the Association for Behavioral and Cognitive Therapies (ABCT).
References
1. Evans SC, Corteselli KA, Edelman A, Scott H, Weisz JR. Is irritability a top problem in youth mental health care? A multi-informant, multi-method investigation. Manuscr Submitt Publ. (2021).
2. Stringaris A, Vidal-Ribas P, Brotman MA, Leibenluft E. Practitioner review: definition, recognition, and treatment challenges of irritability in young people. J Child Psychol Psychiatry. (2018) 59:721–39. doi: 10.1111/jcpp.12823
3. Brotman MA, Kircanski K, Leibenluft E. Irritability in children and adolescents. Annu Rev Clin Psychol. (2017) 13:317–41. doi: 10.1146/annurev-clinpsy-032816-044941
4. Kircanski K, Leibenluft E, Brotman MA. Emotion regulation in severe irritability and disruptive mood dysregulation disorder. In: Essau CA, LeBlanc SS, Ollendick TH, editors. Emotion Regulation and Psychopathology in Children and Adolescents. Oxford: Oxford University Press (2017). doi: 10.1093/med:psych/9780198765844.003.0014
5. Leibenluft E, Stoddard J. The developmental psychopathology of irritability. Dev Psychopathol. (2013) 25:1473–87. doi: 10.1017/S0954579413000722
6. Evans SC, Burke JD, Roberts MC, Fite PJ, Lochman JE, Francisco R, et al. Irritability in child and adolescent psychopathology: an integrative review for ICD-11. Clin Psychol Rev. (2017). doi: 10.1016/j.cpr.2017.01.004
7. Brotman MA, Kircanski K, Stringaris A, Pine DS, Leibenluft E. irritability in youths: a translational model. Am J Psychiatry. (2017) 174:520–32. doi: 10.1176/appi.ajp.2016.16070839
8. Kircanski K, Clayton ME, Leibenluft E, Brotman MA. Psychosocial treatment of irritability in youth. Curr Treat Options Psychiatry. (2018) 5:129–40. doi: 10.1007/s40501-018-0141-5
9. Evans SC, Weisz JR, Carvalho AC, Garibaldi PM, Bearman SK, Chorpita BF. Effects of standard and modular psychotherapies in the treatment of youth with severe irritability. J Consult Clin Psychol. (2020) 88:255–68. doi: 10.1037/ccp0000456
10. Fernández de la Cruz L, Simonoff E, McGough JJ, Halperin JM, Arnold LE, Stringaris A. Treatment of children with attention-deficit/hyperactivity disorder (ADHD) and irritability: results from the multimodal treatment study of children With ADHD (MTA). J Am Acad Child Adolesc Psychiatry. (2015) 54:62–70.e3. doi: 10.1016/j.jaac.2014.10.006
11. Waxmonsky JG, Waschbusch DA, Belin P, Li T, Babocsai L, Humphery H, et al. A randomized clinical trial of an integrative group therapy for children with severe mood dysregulation. J Am Acad Child Adolesc Psychiatry. (2016) 55:196–207. doi: 10.1016/j.jaac.2015.12.011
12. Beauchaine TP, Tackett JL. Irritability as a transdiagnostic vulnerability trait: current issues and future directions. Behav Ther. (2020) 51:350–64. doi: 10.1016/j.beth.2019.10.009
13. Evans SC, Blossom JB, Fite PJ. Exploring longitudinal mechanisms of irritability in children: implications for cognitive-behavioral intervention. Behav Ther. (2020) 51:238–52. doi: 10.1016/j.beth.2019.05.006
14. Zachary C, Jones DJ. The role of irritability in the treatment of behavior disorders: a review of theory, research, and a proposed framework. Clin Child Fam Psychol Rev. (2019) 22:197–207. doi: 10.1007/s10567-018-00272-y
15. Gross JJ, Jazaieri H. Emotion, emotion regulation, and psychopathology: an affective science perspective. Clin Psychol Sci. (2014) 2:387–401. doi: 10.1177/2167702614536164
16. Sheppes G, Suri G, Gross JJ. Emotion regulation and psychopathology. Annu Rev Clin Psychol. (2015) 11:379–405. doi: 10.1146/annurev-clinpsy-032814-112739
17. Cole PM, Hall SE, Hajal NJ, Beauchaine TP, Hinshaw SP. Emotion dysregulation as a vulnerability to psychopathology. Child Adolesc Psychopathol. (2017) 11:346–86.
18. Beauchaine TP, Gatzke-Kopp L, Mead HK. Polyvagal theory and developmental psychopathology: emotion dysregulation and conduct problems from preschool to adolescence. Biol Psychol. (2007) 74:174–84. doi: 10.1016/j.biopsycho.2005.08.008
19. Beauchaine TP, Gatzke-Kopp LM. Instantiating the multiple levels of analysis perspective in a program of study on externalizing behavior. Dev Psychopathol. (2012) 24:1003–18. doi: 10.1017/S0954579412000508
20. Linehan MM, Bohus M, Lynch TR. Dialectical behavior therapy for pervasive emotion dysregulation. Handb Emot Regul. (2007) 1:581–605.
21. Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev. (2010) 30:217–37. doi: 10.1016/j.cpr.2009.11.004
22. Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. (2004) 26:41–54. doi: 10.1023/B:JOBA.0000007455.08539.94
23. Southam-Gerow MA. Emotion Regulation in Children and Adolescents: A Practitioner's Guide. Guilford Press (2013).
24. Beauchaine TP, Cicchetti D. Emotion dysregulation and emerging psychopathology: a transdiagnostic, transdisciplinary perspective. Dev Psychopathol. (2019) 31:799–804. doi: 10.1017/S0954579419000671
25. Roy AK, Lopes V, Klein RG. Disruptive mood dysregulation disorder: a new diagnostic approach to chronic irritability in youth. Am J Psychiatry. (2014) 171:918–24. doi: 10.1176/appi.ajp.2014.13101301
26. Carthy T, Horesh N, Apter A, Gross JJ. Patterns of emotional reactivity and regulation in children with anxiety disorders. J Psychopathol Behav Assess. (2010) 32:23–36. doi: 10.1007/s10862-009-9167-8
27. Carthy T, Horesh N, Apter A, Edge MD, Gross JJ. Emotional reactivity and cognitive regulation in anxious children. Behav Res Ther. (2010) 48:384–93. doi: 10.1016/j.brat.2009.12.013
28. Southam-Gerow MA, Kendall PC. A preliminary study of the emotion understanding of youths referred for treatment of anxiety disorders. J Clin Child Psychol. (2000) 29:319–27. doi: 10.1207/S15374424JCCP2903_3
29. Schäfer JÖ, Naumann E, Holmes EA, Tuschen-Caffier B, Samson AC. Emotion regulation strategies in depressive and anxiety symptoms in youth: a meta-analytic review. J Youth Adolesc. (2017) 46:261–76. doi: 10.1007/s10964-016-0585-0
30. Harmon SL, Stephens HF, Repper KK, Driscoll KA, Kistner JA. Children's rumination to sadness and anger: implications for the development of depression and aggression. J Clin Child Adolesc Psychol. (2019) 48:622–32. doi: 10.1080/15374416.2017.1359788
31. Peled M, Moretti MM. Rumination on anger and sadness in adolescence: fueling of fury and deepening of despair. J Clin Child Adolesc Psychol. (2007) 36:66–75. doi: 10.1080/15374410709336569
32. Smith SD, Stephens HF, Repper K, Kistner JA. The relationship between anger rumination and aggression in typically developing children and high-risk adolescents. J Psychopathol Behav Assess. (2016) 38:515–27. doi: 10.1007/s10862-016-9542-1
33. Bohnert AM, Crnic KA, Lim KG. Emotional competence and aggressive behavior in school-age children. J Abnorm Child Psychol. (2003) 31:79–91. doi: 10.1023/A:1021725400321
34. Factor PI, Rosen PJ, Reyes RA. The relation of poor emotional awareness and externalizing behavior among children with ADHD. J Atten Disord. (2016) 20:168–77. doi: 10.1177/1087054713494005
35. Shields A, Cicchetti D. Reactive aggression among maltreated children: the contributions of attention and emotion dysregulation. J Clin Child Psychol. (1998) 27:381–95. doi: 10.1207/s15374424jccp2704_2
36. McLaughlin KA, Hatzenbuehler ML, Mennin DS, Nolen-Hoeksema S. Emotion dysregulation and adolescent psychopathology: a prospective study. Behav Res Ther. (2011) 49:544–54. doi: 10.1016/j.brat.2011.06.003
37. Graziano PA, Garcia A. Attention-deficit hyperactivity disorder and children's emotion dysregulation: a meta-analysis. Clin Psychol Rev. (2016) 46:106–23. doi: 10.1016/j.cpr.2016.04.011
38. Lugo-Candelas C, Flegenheimer C, McDermott JM, Harvey E. Emotional understanding, reactivity, and regulation in young children with ADHD symptoms. J Abnorm Child Psychol. (2017) 45:1297–310. doi: 10.1007/s10802-016-0244-7
39. Abela JR, Hankin BL. Rumination as a vulnerability factor to depression during the transition from early to middle adolescence: a multiwave longitudinal study. J Abnorm Psychol. (2011) 120:259. doi: 10.1037/a0022796
40. Hankin BL. Rumination and depression in adolescence: Investigating symptom specificity in a multiwave prospective study. J Clin Child Adolesc Psychol. (2008) 37:701–13. doi: 10.1080/15374410802359627
41. Vidal-Ribas P, Brotman MA, Valdivieso I, Leibenluft E, Stringaris A. The status of irritability in psychiatry: a conceptual and quantitative review. J Am Acad Child Adolesc Psychiatry. (2016) 55:556–70. doi: 10.1016/j.jaac.2016.04.014
42. Weisz JR, Kuppens S, Ng MY, Eckshtain D, Ugueto AM, Vaughn-Coaxum R, et al. What five decades of research tells us about the effects of youth psychological therapy: a multilevel meta-analysis and implications for science and practice. Am Psychol. (2017) 72:79–117. doi: 10.1037/a0040360
43. Sauer-Zavala S, Gutner CA, Farchione TJ, Boettcher HT, Bullis JR, Barlow DH. Current definitions of “transdiagnostic” in treatment development: a search for consensus. Behav Ther. (2017) 48:128–38. doi: 10.1016/j.beth.2016.09.004
44. Marchette LK, Weisz JR. Practitioner review: empirical evolution of youth psychotherapy toward transdiagnostic approaches. J Child Psychol Psychiatry. (2017) 58:970–84. doi: 10.1111/jcpp.12747
45. Evans SC, Santucci L. A modular, transdiagnostic approach to treating severe irritability in children and adolescents. Child Adolesc Psychiatr Clin N Am Spec Ed Dev Treat Issues Emot Dysregulation. (2020). invited manuscript (G. A. Carlson, M. Singh, Eds.).
46. Grossman RA, Ehrenreich-May J. Using the unified protocol for transdiagnostic treatment of emotional disorders with youth exhibiting anger and irritability. Cogn Behav Pract. (2020) 27:184–201. doi: 10.1016/j.cbpra.2019.05.004
47. Chorpita BF, Weisz JR. MATCH-ADTC: Modular approach to therapy for children with anxiety, depression, trauma, or conduct problems. PracticeWise. (2009).
48. Weisz JR, Chorpita BF, Palinkas LA, Schoenwald SK, Miranda J, Bearman SK, et al. Testing standard and modular designs for psychotherapy treating depression, anxiety, and conduct problems in youth: a randomized effectiveness trial. Arch Gen Psychiatry. (2012) 69:274–82. doi: 10.1001/archgenpsychiatry.2011.147
49. Weisz JR, Thomassin K, Hersh J, Santucci LC, MacPherson HA, Rodriguez GM, et al. Clinician training, then what? A randomized controlled effectiveness trial of low-cost Child STEPs implementation support with vs. without expert consultation. J Consult Clin Psychol. (2020) 88:1065–78. doi: 10.1037/ccp0000536
51. Aebi M, Plattner B, Metzke CW, Bessler C, Steinhausen H-C. Parent- and self-reported dimensions of oppositionality in youth: construct validity, concurrent validity, and the prediction of criminal outcomes in adulthood. J Child Psychol Psychiatry. (2013) 54:941–9. doi: 10.1111/jcpp.12039
52. Althoff RR, Kuny-Slock AV, Verhulst FC, Hudziak JJ, van der Ende J. Classes of oppositional-defiant behavior: concurrent and predictive validity. J Child Psychol Psychiatry. (2014) 55:1162–71. doi: 10.1111/jcpp.12233
53. Tseng W-L, Moroney E, Machlin L, Roberson-Nay R, Hettema JM, Carney D, et al. Test-retest reliability and validity of a frustration paradigm and irritability measures. J Affect Disord. (2017) 212:38–45. doi: 10.1016/j.jad.2017.01.024
54. Stringaris A, Zavos H, Leibenluft E, Maughan B, Eley TC. Adolescent irritability: phenotypic associations and genetic links with depressed mood. Am J Psychiatry. (2012) 169:47–54. doi: 10.1176/appi.ajp.2011.10101549
55. Evans SC, Bonadio FT, Bearman SK, Ugueto AM, Chorpita BF, Weisz JR. Assessing the irritable and defiant dimensions of youth oppositional behavior using CBCL and YSR items. J Clin Child Adolesc Psychol. (2020) 49:804–19. doi: 10.1080/15374416.2019.1622119
56. Weisz JR, Chorpita BF, Frye A, Ng MY, Lau N, Bearman SK, et al. Youth Top Problems: using idiographic, consumer-guided assessment to identify treatment needs and to track change during psychotherapy. J Consult Clin Psychol. (2011) 79:369–80. doi: 10.1037/a0023307
57. Weisz JR, Bearman SK, Ugueto AM, Herren JA, Evans SC, Cheron DM, et al. Testing robustness of child STEPs effects with children and adolescents: a randomized controlled effectiveness Trial. J Clin Child Adolesc Psychol Off J Soc Clin Child Adolesc Psychol Am Psychol Assoc Div. (2019) 53:1–14.
58. Weisz JR, Vaughn-Coaxum RA, Evans SC, Thomassin K, Hersh J, Ng MY, et al. Efficient monitoring of treatment response during youth psychotherapy: the Behavior And Feelings Survey. J Clin Child Adolesc Psychol. (2019) 49:737–51. doi: 10.1080/15374416.2018.1547973
59. Hawley KM, Weisz JR. Child, parent and therapist (dis) agreement on target problems in outpatient therapy: the therapist's dilemma and its implications. J Consult Clin Psychol. (2003) 71:62. doi: 10.1037/0022-006X.71.1.62
60. Yeh M, Weisz JR. Why are we here at the clinic? Parent-child (dis)agreement on referral problems at outpatient treatment entry. J Consult Clin Psychol. (2001) 69:1018–25. doi: 10.1037/0022-006X.69.6.1018
61. Shields A, Cicchetti D. Emotion regulation among school-age children: the development and validation of a new criterion Q-sort scale. Dev Psychol. (1997) 33:906. doi: 10.1037/0012-1649.33.6.906
62. Zeman J, Shipman K, Suveg C. Anger and sadness regulation: Predictions to internalizing and externalizing symptoms in children. J Clin Child Adolesc Psychol. (2002) 31:393–8. doi: 10.1207/S15374424JCCP3103_11
63. Zeman J, Cassano M, Suveg C, Shipman K. Initial validation of the children's worry management scale. J Child Fam Stud. (2010) 19:381–92. doi: 10.1007/s10826-009-9308-4
64. Zeman J, Shipman K, Penza-Clyve S. Development and initial validation of the children's sadness management scale. J Nonverbal Behav. (2001) 25:187–205. doi: 10.1023/A:1010623226626
65. McCutcheon AL. Basic concepts and procedures in single-and multiple-group latent class analysis. In: McCutcheon AL, editor. Applied Latent Class Analysis. Cambridge: Cambridge University Press (2002). p. 56–88. doi: 10.1017/CBO9780511499531.003
66. Young AS, Youngstrom EA, Findling RL, Eck KV, Kaplin D, Youngstrom JK, et al. Developing and validating a definition of impulsive/reactive aggression in Youth. J Clin Child Adolesc Psychol. (2020) 49:787–803. doi: 10.1080/15374416.2019.1622121
67. Youngstrom E, Young AS, Langfus J, Findling R, Stapp EK, Williams SC, et al. 22.3 developing an empirical definition of impulsive aggression and mood latent profiles in children and adolescents. J Am Acad Child Adolesc Psychiatry. (2020) 59:S195. doi: 10.1016/j.jaac.2020.08.220
68. Evans SC, Diaz KI, Callahan KP, Wolock ER, Fite PJ. Parallel trajectories of proactive and reactive aggression in middle childhood and their outcomes in early adolescence. Res Child Adolesc Psychopathol. (2021) 49:211–26. doi: 10.1007/s10802-020-00709-5
69. Bauer DJ, Curran PJ. Distributional assumptions of growth mixture models: implications for overextraction of latent trajectory classes. Psychol Methods. (2003) 8:338. doi: 10.1037/1082-989X.8.3.338
70. De Los Reyes A, Augenstein TM, Wang M, Thomas SA, Drabick DAG, Burgers DE, et al. The validity of the multi-informant approach to assessing child and adolescent mental health. Psychol Bull. (2015) 141:858–900. doi: 10.1037/a0038498
71. Youngstrom EA. Future directions in psychological assessment: combining evidence-based medicine innovations with psychology's historical strengths to enhance utility. J Clin Child Adolesc Psychol. (2013) 42:139–59. doi: 10.1080/15374416.2012.736358
72. Cho E, Bearman SK, Woo R, Weisz JR, Hawley KM. A second and third look at FIRST: do adaptations impact the integrity, acceptability, and effectiveness of a brief intervention for youth anxiety, depression, and conduct problems? (2019). Forthcoming;
73. Weisz JR, Bearman SK. Principle-Guided Psychotherapy for Children and Adolescents: The FIRST Treatment Program for Behavioral and Emotional Problems. New York, NY: Guilford Press. (2019).
74. Weisz J, Bearman SK, Santucci LC, Jensen-Doss A. Initial test of a principle-guided approach to transdiagnostic psychotherapy with children and adolescents. J Clin Child Adolesc Psychol. (2017) 46:44–58. doi: 10.1080/15374416.2016.1163708
75. Ehrenreich-May J, Kennedy SM, Sherman JA, Bilek EL, Buzzella BA, Bennett SM, et al. Unified Protocols for Transdiagnostic Treatment of Emotional Disorders in Children and Adolescents: Therapist Guide. Oxford University Press. (2017). doi: 10.1093/med-psych/9780199340989.001.0001
76. Hawks JL, Kennedy SM, Holzman JBW, Ehrenreich–May J. Development and application of an innovative transdiagnostic treatment approach for pediatric irritability. Behav Ther. (2020) 51:334–49. doi: 10.1016/j.beth.2019.07.004
Keywords: irritability, cognitive-behavior therapy, dysregulation, behavioral parent training, emotion regulation, youth psychotherapy, transdiagnostic, modular
Citation: Evans SC, Wei MA, Harmon SL and Weisz JR (2021) Modular Psychotherapy Outcomes for Youth With Different Latent Profiles of Irritability and Emotion Dysregulation. Front. Psychiatry 12:618455. doi: 10.3389/fpsyt.2021.618455
Received: 17 October 2020; Accepted: 12 March 2021;
Published: 16 April 2021.
Edited by:
Carla Sharp, University of Houston, United StatesReviewed by:
Katherine Dixon-Gordon, University of Massachusetts Amherst, United StatesAndres Viana, University of Houston, United States
Copyright © 2021 Evans, Wei, Harmon and Weisz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Spencer C. Evans, c2V2YW5zQG1pYW1pLmVkdQ==
orcid.org/0000-0001-8644-817X
 Spencer C. Evans
Spencer C. Evans Melissa A. Wei1
Melissa A. Wei1 Sherelle L. Harmon
Sherelle L. Harmon