- 1Department of Psychotherapy and Diagnostics, Technische Universität Braunschweig, Braunschweig, Germany
- 2Research Group Psychosomatic Rehabilitation, Department of Psychosomatic Medicine, Charité University Medicine Berlin, Berlin, Germany
Introduction: The most prevalent psychotherapy schools are psychodynamic (PDT) and cognitive behavior therapy (CBT). There are no scientific guidelines on which type of patient should be treated by which therapist, and how they can find the best one. Part of the answer can be derived from data on who is treated in which way.
Objective: Objective of this study was to compare patients in routine PDT and CBT to describe similarities and differences in regard to patient status and treatment.
Materials and Methods: A research psychotherapist visited 73 cognitive behavior therapists and 58 psychodynamic psychotherapists in their office and asked them to report about the last cases they had seen. There were 188 CBT and 134 PD case reports.
Results: There were no significant differences in socio-demographics between PDT and CBT patients. The average number of treatment session so far was significantly higher in PDT than CBT. There were longer duration of illness, more parallel medical treatments and higher rates of sick leave in CBT patients. While assessment of capacities with the Mini-ICF-APP showed no differences, more participation restrictions were found in CBT patients. Correspondingly there were more sociomedical interventions, especially in regard to work.
Conclusions: The differences between PDT and CBT may be explained by the fact that PDT requires analytical capabilities on the side of the patient, which may exclude patients with social problems, while CBT is coping oriented which allows the inclusion of all kinds of patients. Still, in both treatment modes, complex patients are treated with multidimensional interventions.
Introduction
There are different psychotherapy schools, following different theoretical models and using different techniques (1, 2). They similarly aim to reduce the symptoms of illness and suffering of the patient, though following different concepts, and using different approaches and techniques (3, 4). There have been changing tendencies for predominance of certain therapy forms during the development of psychotherapy until now (5). But, most known and used are psychodynamic therapy (PDT) and cognitive behavior therapy (CBT). Their similar efficacy has well been shown in many empirical studies across a wide spectrum of disorders (6–14).
Still, there is a lack of research on which patients should best be treated in CBT and PDT. Some suggestions are that phobias might preferably need behavioral exposure therapy, and some personality disorders preferably PDT (15), but both treatments are effective (16). It was found that PDT therapists valued a neutral relationship, CBT therapists emphasized a didactic interaction (2).
But, superiority effects of the one or other therapy are often small (12). Recommendations are rather vague and do not result in guidelines which could guide patients to find the best therapy. According to theoretical frames of reference, it may be that PDT is primarily focused on inner psychodynamic conflicts, whereas CBT rather aims at symptom management and improvement of coping. Qualitative differences are also described for inter-session processes (17), or dose effects in relation to lasting outcomes (15), or effects of specific resource-oriented interventions (10).
A survey in a naturalistic setting for patients with substance use disorders in Sweden (18) found that there are more often trauma problems in PDT (22% as compared to 6% in cognitive therapy), more often anxiety problems in CBT (52 vs. 24%), that personality disorders are diagnosed in 20% of PDT and 8–29% in CBT patients, while the global assessment of functioning (GAF) is similar with a score of 54 in PDT and 55 in CBT. When comparing patients between therapies, it is also of interest to study what is done therapeutically. In 29% of PDT treatments relational improvement was the primary goal, but only in 12–16% in CBT, whereas in CBT the focus was on symptom and affect management (28–39% in CBT vs. 18% in PDT), and behavior change (29–62% in CBT vs. 9% in PDT) (18).
Apart from school-specific and symptom oriented treatment goals and techniques, there is school-overlapping a second level of targets and interventions, regarding capacity limitations and participation restrictions in life, as defined by the International Classification of Functioning Disability and Health (19). Many patients have to struggle with problems at home, at work, and in leisure time, and show high rates of work incapacity and early retirement (20–28). This must therapeutically be addressed. Treatments in this regard can be called “sociomedical treatments.” Psychotherapists should initiate and guarantee interdisciplinary cooperative treatments. They should take care of disability assessments and work related measures, or procure help in daily life problems. A comparison of such interventions in PDT and CBT can also shed some light on the question of differential patient allocation and care.
There is a lack of empirical data on the indication of different psychotherapy schools. It is therefore of interest, whether in routine care PDT and CBT therapists see different or the same patients. It could be that PDT and CBT therapists have their ideas on which type of problem they can best deal with and therefore accept different patients for treatment. It could be that patients are informed by their physicians or other therapists to go here or there. Patients may also have thoughts of their own about what is done in PDT or CBT, and what they prefer. With this given, the objective of our study was to assess the severity and chronicity of illness, capacity limitations, participation restrictions, the prognosis of treatment, and resulting sociomedical interventions in PDT and CBT.
As can be seen from the empirical evidence until now, there is a lot of research on patients characteristics and psychotherapy in PDT and CBT. What has until now been missing (and is central part of this present study) are socio-medical problems and social-oriented / socio-medical treatments in PDT and CBT. Therefore our study is of high originality and novelty. It presents first data on socio-medical aspects in psychotherapy treatments (comparing PDT and CBT).
Materials and Methods
Health Care System in Germany
The study was done in Berlin, Germany. Health insurance covers all citizens and fully reimburses up to 80 sessions CBT or 120 sessions PDT. Psychotherapy is provided by physicians and psychologists in private practice, who either have a state licensed school specific education in PDT or CBT, and who are obliged to provide only the treatment of their expertise. We included psychologist-psychotherapists, who were doing psychotherapy only. In Berlin there is a total of 2.051 listed, so that there is about one per 2000 inhabitants. There are furthermore physician-psychotherapists, who were not contacted, as they can do additional medical treatments, so that patient selection may not only be due to psychotherapy.
Recruitment of Psychotherapists
Referring to official listings, psychotherapists were contacted with no special selection, but an equal number of PDT and CBT. Therapists were informed that the goal was to study which type of patients were finding their way into psychotherapy. Therapists reported on their gender, age, education, years of practice, number of patients, and predominant spectrum of disorders in their practice.
Interviews With Psychotherapists
Therapists were interviewed in their office by researchers who were themselves psychotherapists, following a semi standardized interview. The interviewers validated the answers of the therapists by clarifying what was meant. Based on 20 parallel interviews, the interrater reliability was κ = 0.803 (95% CI, p < 0.0005). Therapists were asked to refer anonymously to the last patients of working age whom they had seen, with a minimum of 10 therapy sessions. In accordance with the WHO International Classification of Functioning Disability and Health [ICF, (19)] patient assessment did not only ask for symptoms (disorders of functions) and course of illness, but also for capacities and participation.
“Disorders of functions (symptoms)” were assessed with a Visual Analog Mood Scale [VAS, (29)] with ratings from 0 = negative to 10 = good for depression, anxiety, nervousness, somatoform symptoms, tiredness, memory problems, delusional symptoms.
“Severity of illness” was rated on the Clinical Global Impression scale [CGI, (30)] from normal, not at all ill (1) to among the most extremely ill patients (7).
“Capacity limitations” were assessed following the Mini-ICF Assessment of Activities and Participation in Psychological Disorders [Mini-ICF-APP (31, 32)]. It lists in reference to the ICF (19) capacities which are typically impaired by mental disorders. These are: (1) adherence to regulations, (2) planning and structuring of tasks, (3) flexibility, (4) competency, (5) competence to judge and decide, (6) proactivity, (7) endurance, (8) assertiveness, (9) contact with others, (10) group integration, (11) dyadic relationships, (12) self-care, and (13) mobility. Each dimension was rated on a six-point Likert-scale (0: cannot be assessed; 1: no disability; 2: mild disability; 3: moderate disability; 4: severe disability; 5: total disability). The degree of impairment per capacity was rated in reference to the workplace, or in case of unemployment, to the general labor market. A sum score gives an idea of the overall impairment.
“Participation restrictions” were assessed with the Index for Measuring Participation Problems (IMEP) (31, 33), covering (1) activities of daily living, (2) recreational activities, (3) social activities, (4) close relationships, (5) special stressors in life, (6) work. A judgment is made on a visual analog scale from 0 = no impairment to 10 = full impairment, i.e., no activity is possible in this domain of life.
“Sociomedical interventions” were coded in reference to the TOPP Checklist [(Treatment Options for Persistent Psychological Problems; (34)], listing 38 items, like cooperation with other therapists, contacts with institutions, work-related interventions, social support. Therapist are asked to indicate, whether they have done, initiated or participated in these interventions.
Ethical Considerations
The project was approved by the ethical committee of the Charité University Medicine Berlin and by the data privacy department of the Pension Insurance Berlin-Brandenburg (EA4/027/18, 10-R-40.07.05.07.017). The therapists gave written informed consent. There was no direct involvement of patients and no interference with the ongoing treatment.
Statistical Analysis
Data have been analyzed with SPSS, version 26. Exploratory group comparisons have been calculated with T-test for continuous variables and Chi2-Test for frequencies. Significance levels are reported for single items to guide attendance to points of special interest.
Results
We invited 326 therapists. An interview could be done with 131 therapists. There were 74% female therapists, with an average age of 54 years (s.d. 10.97, range 32–74). They worked as psychotherapist for 16.8 years (s.d. 10.70, range 1–45). Of these, 43.5% were psychodynamic therapists, 55.7% cognitive behavior therapist, and one was trained in both. Therapists reported to treat on average 39 patients (SD ± 24; min. 5, max. 150). This includes short- and long-term treatments, as well as acute counseling sessions and sessions for relapse prevention.
Referring to the last seen patients in working age, therapists reported on 322 case vignettes (58.4% CBT, 41.6% PDT).
Sociodemographic Characteristic of Patients
There were no differences between PDT and CBT in regard to general patient characteristics like age, gender, migration background, family status, education, employment (see Table 1).
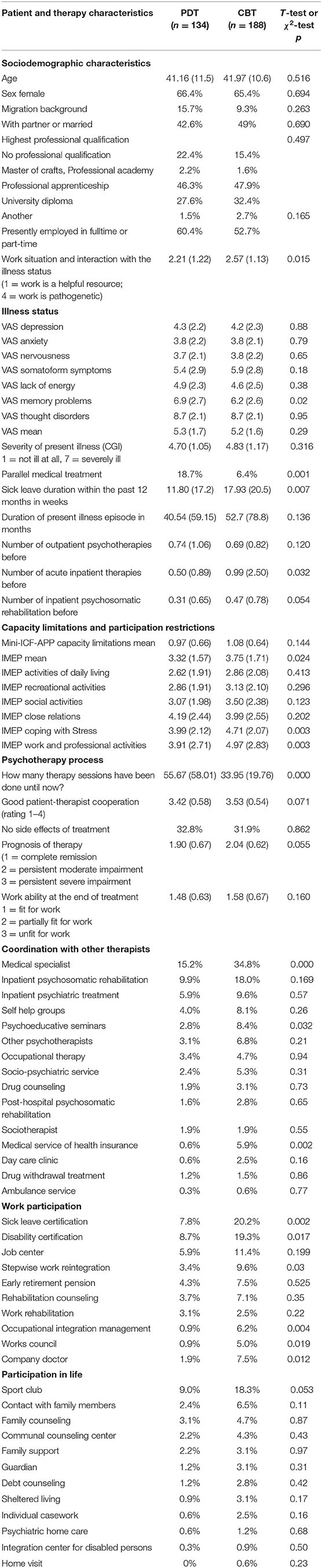
Table 1. Characteristics of patients and therapy methods in cognitive behavior therapy and psychodynamic psychotherapy.
Illness Status
Both therapist groups made similar diagnoses, mostly depression (F30: PDT 26.1%, CBT 35.1%), adjustment and traumatic disorder (F43: PDT 9.3%, CBT 15.5%), somatoform disorders (F45: PDT 4.3%, CBT 11.5%), and personality disorders (PDT 6.8%, CBT 9.3%). Therapists reported no significant differences in regard to the illness status, neither in the spectrum and severity of the symptoms, as measured with the VAS and CGI. Duration of illness was similar in PDT and CBT, though with a large variance. There was a trend for more inpatient stays in CBT patients, be it in acute or rehabilitation hospitals. CBT patients are also more often in parallel medical treatment.
Capacity Limitations
Therapists reported a similar degree of capacity limitations, be it in the global score or individual dimensions of the Mini-ICF-APP.
Participation Restrictions
The IMEP mean score suggests that CBT therapists see more participation problems than PDT therapists. This is especially so for coping with stress and work.
Psychotherapy Process
PDT patients are on average significantly longer in treatment than CBT patients. There is a trend that CBT therapist report a somewhat better patient therapist cooperation. There were no differences in regard to report on negative effects of treatment. CBT therapists expect a relatively poorer prognosis of therapy.
Sociomedical Interventions
Table 1 groups sociomedical interventions, which have been effected, in the sections (a) coordination and cooperation with other therapists, (b) interventions to improve work participation, and (c) interventions to improve participation in daily life. There by and large a similar global rank order for these interventions in both treatment groups. CBT therapists report higher rates for all items. Greatest differences are found for psychoeducation courses, which are a typical behavior therapy treatment method in itself. There are foremost relevant differences in regard to work related interventions, like inability and disability certification, occupational integration management, stepwise work reintegration, and contacts with work doctors or councils.
Discussion
A first result is that there are no major differences between CBT and PDT patients in regard to sociodemographic characteristics. Similar patients are seen in both treatments. While both therapist groups rate the severity of illness very similar, there are still indicators that in CBT more heterogeneous or complex cases may be treated. There is a longer duration of illness, a higher rate of parallel medical treatments, of sick leave, and more prior inpatient stays. CBT therapist report more participation problems as measured with the IMEP. Correspondingly, CBT therapists report more sociomedical interventions, like interdisciplinary treatment, work oriented interventions, and social support. Finally, CBT therapists expect a poorer outcome of treatment.
In summary, these findings suggest that PDT and CBT therapists attract or accept patients with different types of problems and execute different treatments. This corresponds with basic concepts of both treatment approaches. As described in the scientific literature, CBT is seen as more problem oriented which allows to treat more chronic illnesses and to apply more socio-medical interventions. CBT may highlight their client's wish to master demands in family and work. PDT is described to be more insight oriented and highlighting their patients wishes to be taken care of by their therapists. In CBT therapist are very active and the approach is rather structured while in PDT patients learn insight in their unconscious dynamics (10, 15, 17, 18, 35–37). Traditionally, PDT is also characterized by the requirement, that patients must show “analytic capability.” This may exclude to some part patients with a lack of psychological insight, with complex mental disorders, like dementia, or with severe social problems. CBT in contrast is rather focusing on coping, not only with internal psychological processes, but also with social and life problems. This allows to target a broad spectrum of mental and somatic disorders, but also problems in daily life or at work, as can be concluded from differences in sociomedical interventions. Our findings are in line with these different psychotherapy concepts.
Limitations
When discussing the results, one has to take into account as a limitation, that we did not assess patients directly, but asked therapists about their cases and treatments. The answers therefore reflect the views of the therapists. This results in some objective data, like the information on the duration of treatment. There is other information which is a mixture of patient characteristics and the perspective of the therapist, like the expectation of treatment outcome. For our research question it seems to be appropriate and an even advantage to interview therapists on their patients and treatment, when one wants to compare PDT and CBT.
The response rate of participating therapists was 40% in this present study. Compared with similarly scoped research in the same region done with primary physicians, which achieved a response rate of 13% (27), this present rate is a quite high response rate. The participating therapists must be expected to be prototypically representative psychotherapists, i.e., especially good colleagues with high interest in additional professional learning and activities beside their routine duties. The data must be interpreted against this background: from this sample of engaged therapists, is might be concluded what could be done (but not what is routinely done) in outpatient psychotherapy.
The reported differences represent trends. When one looks at the absolute data, it can be seen, that therapists in PDT and CBT alike treat patients of all sorts with a similarly broad spectrum of therapeutic interventions.
Conclusion
The data add information on differential indications and patient allocation and may help to further guide research on this subject. This should get more scientific attention.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The project was approved by the ethical committee of the Charité University Medicine Berlin and by the data privacy department of the Pension Insurance Berlin-Brandenburg (EA4/027/18, 10-R-40.07.05.07.017). The therapists gave written informed consent. There was no direct involvement of patients and no interference with the ongoing treatment. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
ML designed the study and research question and supervised the research process. BM analyzed the data and wrote the manuscript. MR and ML reviewed and contributed to the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This research has been supported by a research grant of the German Pension Fund Berlin-Brandenburg (10-R-40.07.05.07.017).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank the participating psychotherapists.
References
1. Roth AD. Are competence frameworks fit for practice? Examining the validity of competence frameworks for CBT, psychodynamic, humanistic psychotherapy. Psychother Res. (2015) 2015:460–72. doi: 10.1080/10503307.2014.906763
2. Boterhoven de Haan KL, Lee CW. Therapists' thoughts on therapy: clinicians' perceptions on the therapy process that distinguish schema, cognitive behavioural and psychodynamic approaches. Psychother Res. (2014) 24:538–49. doi: 10.1080/10503307.2013.861092
3. Pilecki B, Thoma N, McKay D. Cognitive behavioral and psychodynamic therapies: points of intersection and divergence. Psychodynamic Psychiat. (2015) 43:463–90. doi: 10.1521/pdps.2015.43.3.463
4. Warner LK, Herron WG, Javier RA, Patalano F, Sisenwein F, Primavera LH. A comparison of dose-response curves in cognitive-behavioral and psychodynamic psychotherapies. J Clin Psychol. (2001) 57:63–73. doi: 10.1002/1097-4679(200101)57:1<63::AID-JCLP8>3.0.CO;2-E
5. Overholser JC. 50 years of psychotherapy: erudition, evolution, and evaluation. J Contemp Psychother. (2019) 50:87–93. doi: 10.1007/s10879-019-09441-8
6. Steinert C, Munder T, Rabung S, Hoyer J, Leichsenring F. Psychodynamic therapy: as efficacious as other empirically supported treatments? A meta-analysis testing equivalence of outcomes. Am J Psychiatr. (2017) 174:943–53. doi: 10.1176/appi.ajp.2017.17010057
7. Stiles WB, Barkham M, Mellor-Clark J, Connell J. Effectiveness of cognitive-behavioural, person-centred, and psychodynamic therapies in UK primary-care routine practice: replication in a larger sample. Psychol Med. (2008) 38:677–88. doi: 10.1017/S0033291707001511
8. Cuijpers P, Karvotaki E, de Wit L, Ebert DD. The effects of fifteen evidence-supported therapies for adult depression: a meta-analytic review. Psychother Res. (2020) 30:279–93. doi: 10.1080/10503307.2019.1649732
9. Leichsenring F. Comparative effects of short-term psychodynamic psychotherapy and cognitive-behavioral therapy in depression: a meta-analytic approach. Clin Psychol Rev. (2001) 21:401–19. doi: 10.1016/S0272-7358(99)00057-4
10. Munder T, Karcher A, Yadikar Ö, Szeles T, Gumz A. Focusing on patients' existing resources and strengths in cognitive-Behavioral therapy and psychodynamic therapy: a Systematic review and meta-analysis. ZPMP. (2019) 65:144–61. doi: 10.13109/zptm.2019.65.2.144
11. Watzke B, Rüddel H, Koch U, Rudolph M, Schulz H. Comparison of therapeutic action, style and content in cognitive-behavioural and psychodynamic group therapy under clinically representative conditions. Clin Psychol Psychother. (2008) 15:404–17. doi: 10.1002/cpp.595
12. Pompoli A, Furukawa TA, Imai H, Tajika A, Efthimiou O, Salanti G. Psychological therapies for panic disorder with or without agoraphobia in adults: a network meta-analysis. Cochrane Database Syst Rev. (2016) 13:CD011004. doi: 10.1002/14651858.CD011004.pub2
13. Shinohara K, Honvashiki M, Imai H, Hunot V, Caldwell DM, Davies P, et al. Behavioural therapies versus other psychological therapies for depression. Cochrane Database Syst Rev. (2013) 16:CD008696. doi: 10.1002/14651858.CD008696
14. Wilson KCM, Mottram PG, Vassilas CA. Psychotherapeutic treatments for older depressed people. Cochrane Database Syst Rev. (2008) 23:CD004853. doi: 10.1002/14651858.CD004853.pub2
15. Huber D, Zimmermann J, Henrich G, Klug G. Comparison of cognitive-behaviour therapy with psychoanalytic and psychodynamic therapy for depressed patients - a three-year follow-up study. ZPMP. (2012) 58:299–316. doi: 10.13109/zptm.2012.58.3.299
16. Leichsenring F, Leibing E. The effectiveness of psychodynamic therapy and cognitive behavior therapy in the treatment of personality disorders: a meta-analysis. Am Psychiatry J. (2003) 160:1223–32. doi: 10.1176/appi.ajp.160.7.1223
17. Zeeck A, Hartmann A, Wild B, de Zwaan M, Herpertz S, Burgmer M, et al. How do patients with anorexia nervosa “process” psychotherapy between sessions? A comparison of cognitive-behavioral and psychodynamic interventions. Psychother Res. (2018) 28:873–86. doi: 10.1080/10503307.2016.1252866
18. Philips B. Comparing apples and oranges: how do patient characteristics and treatment goals vary between different forms of psychotherapy? Psychol Psychother. (2009) 82:323–36. doi: 10.1348/147608309X431491
19. World Health Organization (WHO). International Classification of Functioning, Disability and Health (ICF). Geneva: WHO Press (2001).
20. Kühn KU, Quednow BB, Barkow K, Heun R, Linden M, Maier W. Chronifizierung und psychosoziale behinderung durch depressive erkrankungen bei patienten in der allgemeinarztpraxis im einjahresverlauf. Ergebnisse aus einer studie der weltgesundheitsorganisation. Nervenarzt. (2002) 73:644–50. doi: 10.1007/s00115-002-1334-z
21. Gilbert P, Allan S, Nicholls W, Olsen K. The assessment of psychological symptoms of patients referred to community mental health teams: distress, chronicity and life interference. Clin Psychol Psychother. (2005) 12:10–27. doi: 10.1002/cpp.426
22. Torpey DC, Klein DN. Chronic depression: update on classification and treatment. Current Psychiatr Rep. (2008) 10:458–64. doi: 10.1007/s11920-008-0074-6
23. Eaton WW, Shao H, Nestadt G, Lee BH, Bienvenu OJ, Zandi P. Population-based study of first onset and chronicity in major depressive disorder. Arch Gen Psychiat. (2008) 65:513–20. doi: 10.1001/archpsyc.65.5.513
24. Muschalla B, Linden M. Workplace problems, workplace phobia and work ability in primary care patients with chronic mental disorders. J Am Board Fam Med. (2014) 27:486–94. doi: 10.3122/jabfm.2014.04.130308
25. Errichiello L, Iodice D, Bruzzese D, Gherghi M, Senatore I. Prognostic factors and outcome in anorexia nervosa: a follow-up study. Eat Weight Disord. (2016) 21:73–82. doi: 10.1007/s40519-015-0211-2
26. Linden M. Definition and assessment of disability in mental disorders under the perspective of the international classification of functioning disability and health (ICF). Behav Sci Law. (2017) 35:124–34. doi: 10.1002/bsl.2283
27. Linden M, Deck R, Muschalla B. Rate and spectrum of participation impairment in patients with chronic mental disorders: comparison of self- and expert ratings. Contemp Behav Health Care. (2018) 3:1–5. doi: 10.15761/CBHC.1000124
28. Linden M, Muschalla B. Type, severity and course of chronic mental disorders in general health care. Psychol Dis Res. (2018) 1:2–6. doi: 10.31487/j.PDR.2018.02.004
29. Hayes MH. Experimental development of the graphics rating method. Psychol Bull. (1921) 18:98–9. doi: 10.1177/003463732101800112
30. Guy W. The clinical global impression scale. The ECDEU assessment manual for psychopharmacology revised, vol. DHEW. Rockvillee, MD: US Department of Health, Education, and Welfare. Public Health Service, Alcohol, Drug Abuse, Mental Health Administration, NIMH Psychopharmacology Research Branch, Division of Extramural Research (1976).
31. Linden M, Baron S, Muschalla B. Mini-ICF-Rating für Psychische Störungen (Mini-ICF-APP). Ein Kurzinstrument zur Beurteilung von Fähigkeits- bzw. Kapazitätsstörungen bei Psychischen Störungen. Göttingen: Hans Huber (2009).
32. Molodynski A, Linden M, Juckel G, Yeeles K, Anderson C, Vazquez-Montes M, et al. The reliability, validity, and applicability of an english language version of the mini-ICF-APP. Soc Psy Psychiatr Epidemiol. (2013) 48:1347–54. doi: 10.1007/s00127-012-0604-8
33. Deck R, Mittag O, Hüppe A, Muche-Borowski C, Raspe H. Index zur messung von einschränkungen der teilhabe (IMET) - erste ergebnisse eines ICF-orientierten assessmentinstruments. Praxis Klinische Verhaltensmedizin und Rehabilitation. (2007) 20:113–20.
34. Linden M, Muschalla B, Noack N, Heintze C, Döpfmer S. Treatment changes in general practice patients with chronic mental disorders following a psychiatric-psychosomatic consultation. Health Serv Res Manag Epidemiol. (2018) 5:1–6. doi: 10.1177/2333392818758523
35. Jones EE, Pulos SM. Comparing the process in psychodynamic and cognitive-behavioral therapies. J Consult Clin Psychol. (1993) 61:306–16. doi: 10.1037/0022-006X.61.2.306
36. Wiser SL, Goldfried MR, Raue PJ, Vakoch DA. Cognitive-behavioral and psychodynamic therapies: a comparison of change processes. In: Dryden W, editor. Research in Counselling and Psychotherapy: Practical Applications. London: Sage (1196). p. 101–132. doi: 10.4135/9781446279786.n5
37. Haverkampf CJ. CBT and psychodynamic psychotherapy-A comparison. J Psychiatry Psychother Commun. (2017) 6:61–8. Available online at: https://zenodo.org/record/3529280#.YJDbwKFCQuU
Keywords: capacity, International Classification of Functioning Disability and Health (ICF), participation, biopsychosocial, Mini-ICF-APP, cognitive behavior counseling, psychodynamic, psychotherapy
Citation: Muschalla B, Linden M and Rose M (2021) Patients Characteristics and Psychosocial Treatment in Psychodynamic and Cognitive Behavior Therapy. Front. Psychiatry 12:664975. doi: 10.3389/fpsyt.2021.664975
Received: 06 February 2021; Accepted: 13 April 2021;
Published: 14 May 2021.
Edited by:
Hitesh Khurana, Pandit Bhagwat Dayal Sharma University of Health Sciences, IndiaReviewed by:
Soni Kewalramani, Amity University, Lucknow, IndiaSarita Sood, University of Jammu, India
Vikas Punia, Shree Guru Gobind Singh Tricentenary University, India
Copyright © 2021 Muschalla, Linden and Rose. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Beate Muschalla, Yi5tdXNjaGFsbGFAdHUtYnJhdW5zY2h3ZWlnLmRl; orcid.org/0000-0001-5285-6618
 Beate Muschalla
Beate Muschalla Michael Linden
Michael Linden Matthias Rose
Matthias Rose