Abstract
Background and Objectives: Phenibut (4-amino-3-phenyl-butyric acid), acting as a GABA-B receptor agonist, has a beneficial effect on anxiety. Although its medical use is not approved in western countries, it can be easily obtained worldwide via the Internet, so it spread as a substance of abuse. In recent years, some case reports have, therefore, highlighted episodes of acute toxicity or withdrawal, but it is still a largely unknown phenomenon.
Methods: In this case report, a 50-year-old woman was admitted to the emergency room with psychomotor agitation, psychotic symptoms, and insomnia, and was non-responsive to treatment. She was hospitalized at the psychiatry ward for 25 days and gave her consent for the publication of the present case report.
Results: The suspicion of phenibut withdrawal allowed to establish the appropriate management, leading to the restitutio ad integrum of the psychopathological case.
Conclusions: In the face of an incoercible psychomotor agitation case, the knowledge of the so-called novel psychoactive substances allows for more appropriate clinical management of intoxication and withdrawal syndromes. This is a scientifically significant report as it provides therapeutic and outcome data concerning a syndrome that is still quite unfamiliar.
Introduction
Phenibut (4-amino-3-phenyl-butyric acid) is a glutamic acid derivative compound synthesized in Russia in the early 1960s and available nowadays in ex-Soviet countries as a cognitive enhancer, food supplement, adjuvant for anxiety and insomnia, and alcohol withdrawal symptoms (1). This substance seems to primarily act as a γ-aminobutyric acid (GABA) B receptor agonist, consequently closing voltage-dependent calcium channels and inhibiting neurotransmission, similar to other drugs, such as pregabalin, gabapentin, and baclofen (2). Moreover, phenibut seems also to boost both dopaminergic and serotoninergic neurotransmission (3). The pharmacological characteristics of phenibut can be viewed in Table 1. However, even though its medical use is not approved in western and European countries, since it was classified as a novel psychoactive substance (NPS) by the United Nations Office of Drug and Crime (UNODC), phenibut can be easily obtained worldwide via the Internet as a dietary supplement in the form of powder, pills, or crystals with an increasing risk of potential misuse (4). In this regard, both acute intoxication and withdrawal syndromes related to phenibut consumption have been reported in literature (5). Specifically, intoxication mainly induces the risk of respiratory failure, paradoxical agitation, seizures, and delirium, while withdrawal is a condition that can last for a significant period and is characterized by psychomotor agitation, psychosis, autonomic instability, seizures, nausea, and vomiting (6, 7). These clinical conditions must be timely recognized and treated in order to avoid serious complications, such as respiratory or acute renal failures due to rhabdomyolisis (5). However, the clinical manifestation characterized by non-specific signs and symptoms together with the lack of a specific protocol for the treatment of both phenibut intoxication and withdrawal symptoms could delay the recognition of these syndromes and their effective management. Therefore, the description of case reports related to phenibut misuse is crucial in order to make clinicians aware of this emerging NPS misuse.
Table 1
| Phenibut, Anvifen, Fenibut, Noofen | |
|---|---|
| 4-Amino-3-phenyl-butyric acid Chemical structure: C10H13NO2 |  |
| Pharmacological characteristics: -GABA-mimetic, primarily at GABA(B) and, to some extent, at GABA(A) receptors -Stimulator of dopamine receptors and antagonizes beta-phenethylamine, a putative endogenous anxiogenic -Blocker of α2δ subunit-containing voltage-dependent calcium channels | |
Phenibut: chemical and pharmacological characteristics.
Case Report
A 50-year-old woman with previously unknown psychiatric history was admitted to the emergency department at night in a state of confusion and psychomotor agitation. Her partner declared that during the morning, the patient suddenly developed motor stereotypies, hyperactivity, and fluctuations of both attention and consciousness. Although her partner denied that the patient had used any psychoactive drugs or alcohol previously, he reported an occasional consumption of diazepam oral solution for anxiety. The patient was not taking any drug therapy with medical prescription. Since psychomotor agitation was becoming more severe with the patient's risk of self-injurious conduct, intramuscular medication with delorazepam up to 6 mg was administered without any substantial modification of the symptomatology. Meanwhile, a CT scan without contrast, performed at the emergency room, was negative for acute neurological events, while toxicological screening of urine (research for opioids, cocaine, methamphetamine, cannabinoids, and benzodiazepines) was positive only for benzodiazepines. The patient's blood tests showed no significant alterations except for creatine phosphokinase (CPK), while the electrocardiogram detected no significant alterations except for a tachycardia (120 beats for a minute). After 2 h of intramuscular therapy with benzodiazepines, haloperidol, and promazine, the patient had no clinical improvement showing abnormal motor behaviors, disorganized thinking, echolalia, visual hallucinations, and total insomnia. Her partner was able to recover a series of tablets at home, of which phenibut, in its various commercial formulations (Fenibut, Anvifen, and Noofen) was the main ingredient (Figure 1). Upon contacting the Poison Control Center, the clinical symptomatology presented by the patient was suspected to be related to phenibut withdrawal since the patient had started consuming phenibut in the previous months. It was subsequently possible to reconstruct that the interval between the last dose of phenibut and the onset of symptoms was about 3 days. The patient was, therefore, hospitalized in the psychiatric ward. Meanwhile, intravenous diazepam up to 30 mg and intramuscular haloperidol up to 5-mg therapy was administered. Following the recommendations for phenibut withdrawal syndrome from previous case reports (5), a baclofen medication of up to 20 mg/day was started. This is because previous literature reported baclofen as a GABA-B agonist, which allows an alternative binding of GABA-B receptors and, therefore, an improvement on withdrawal (8). A time course regarding the drug treatment and the dosages used is shown in Table 2.
Figure 1
Table 2
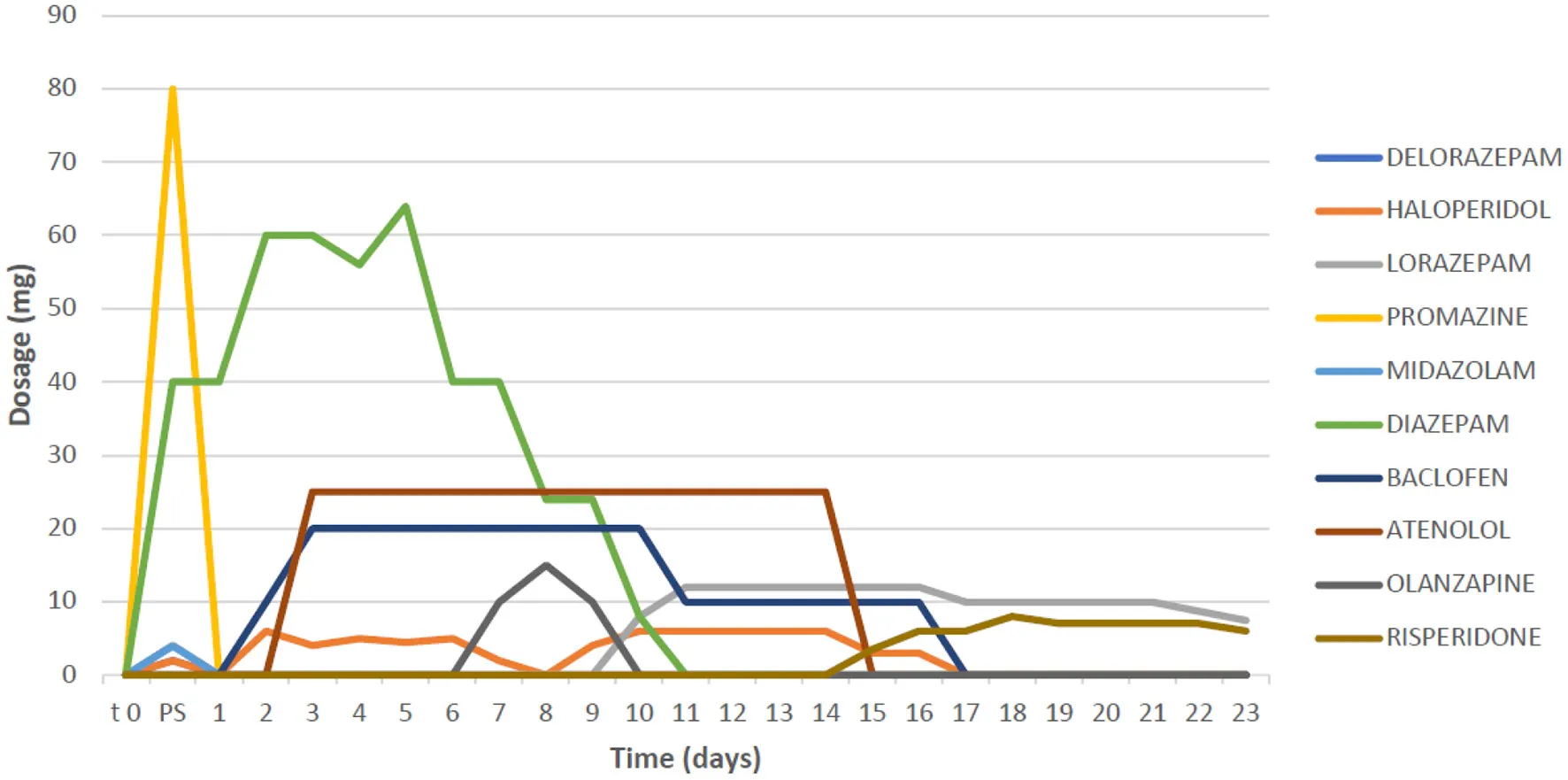 |
Timeline regarding drug treatment and dosages.
Despite the therapy, the patient still spent two completely sleepless nights, experiencing visual hallucinatory disturbances, disorganized behavior, and thinking, with no clearly structured delusions. Psychometric rating scales were performed, with evidence of significant alteration of the mental state [Brief Psychiatric Rating Scale (BPRS) = 75, Hamilton Rating Scale for Depression (HAM-D) = 24, Mania Rating Scale (MRS) = 22, Positive and Negative Syndrome Scale (PANSS) = 102, and Global Assessment of Functioning (GAF) = 25]. Afterward, her mental status began to change from agitation, self-directed aggressiveness, and persecutory delusions to episodes of catatonia, during which she did not react to stimuli and appeared hostile and opposed to any therapeutic contact. Electroencephalogram (EEG) and magnetic resonance imaging (MRI) were performed, with the former showing rapid rhythms compatible with benzodiazepine therapy, and the latter exhibiting rare punctiform hyperintense signal alterations in T2-FLAIR affecting the bihemispheric subcortical white matter of non-specific gliotic significance. In the context of catatonia, the patient developed bladder globe and urinary tract infection with the consequent need for antibiotic treatment (ceftriaxone 2 g for 6 days). She never showed signs of kidney damage, and there was a progressive decrease in CPK (from 1,504 to 195 U/L). Instead, a picture of autonomic instability emerged, characterized by pressure peaks and tachycardia; therefore, atenolol treatment up to 10 mg/day was started, and this had positive effects on symptoms.
Meanwhile, it was possible to view previous health records, and the patient's medical history was reconstructed. She did not suffer from any major medical diseases, but she had been previously treated by private psychiatrists at the age of 36, for depressive episodes in the context of bipolar disorder with psychotic features. She had not been working for 20 years, and she had been living with her partner, living a mainly solitary life with few social interactions. Complete intercritical resolution of the depressive episodes was reported, with a return to the previous functioning. However, for cultural reasons, the patient continued to have magical thoughts. Amitriptyline and benzodiazepines were the last pharmacological therapy administered, prescribed 3 years before the current episode by a private psychiatrist and consumed by the patient without any medical supervision, which, due to her history of poor pharmacological compliance and her tendency to prefer natural remedies, may have not been taken correctly. She had no history of substance abuse, although a trend of excessive consumption of benzodiazepines was also reconstructed for anxiolytic and hypno-inductive purposes.
In light of the catatonic state, the therapy was changed from diazepam to intravenous lorazepam up to 12 mg/day (9). Furthermore, since occasional lengthening of the QT interval was detected through ECG, haloperidol was replaced first with olanzapine, then with risperidone up to 6 mg in order to facilitate the management of psychomotor agitation with a daily QT monitoring. Gradually, the patient progressively showed a reduction in both disorganized thinking and agitation. In addition, psychotic symptoms, such as persecutory delusions and both visual and auditory hallucinations, slowly diminished until finally ending after 4 weeks. Atenolol therapy was stopped after 15 days, and the patient did not experience any further symptoms of autonomic instability.
After resolving the psychotic symptomatology, the patient showed positive recovery in regard to delusional thinking and hallucinatory phenomena, but she also experienced a few days of moderate expansive mood, which resolved after a few days. The patient revealed that she had been consuming phenibut in high dosage (up to 5 g/day) in the previous months in order to treat anxiety and insomnia that began during the COVID-19 pandemic quarantine. Therefore, the diagnosis of phenibut withdrawal was confirmed. Finally, psychometric rating scales were performed at the end of the hospitalization showing the following results: BPRS = 25, HAM-D = 5, MRS = 2, PANSS = 37, GAF = 80. We concluded on a diagnosis of withdrawal psychosis and mixed psychotic episode in the context of bipolar disorder. The patient was, therefore, discharged after 25 days of hospitalization, with a diagnosis of withdrawal psychosis and mixed psychotic episode in bipolar disorder, and with the following treatment: risperidone 6 mg and lorazepam 10 mg/day.
Although it was impossible to have a detailed view of her perspective during the entire hospitalization, at the time of discharge, the patient expressed feelings of relief and amazement concerning her well-being. She also said that she had lived “a nightmare” and that she not only had fear but also, in some moments, the certainty that it would never end. The patient gave her informed consent for the publication of the present case report.
Conclusions
This case report aims to underline the disruptive action that NPS can have in the psyche of a subject, especially due to intoxication and abstinence. In this case, surely the duration of the episode is not to be attributed only to the severity of the condition of abuse but also to the presence of the patient's previous psychiatric disorder. In fact, the previous diagnosis of bipolar disorder may have affected both the emotional instability, which pushed the patient toward the abuse of phenibut, and the severity of the consequent psychopathological picture (10). Moreover, in this patient, it seems that the abuse was not determined by a sensation-seeking modality but by the inability to manage feelings of emptiness and fear due to the COVID-19 pandemic emergency that recently occurred in northern Italy (11, 12). The observation of the exotoxic origin of the very serious episode of psychosis described in this case report creates an interesting field of investigation with respect to the so-called synthetic psychosis. This has led to a great diffusion in recent years and, thus, has made it important for knowledge to be acquired on the phenomenon to enable its differentiation from non-exotoxic psychiatric disorders (13, 14).
The emerging worldwide misuse of phenibut (an NPS inaccurately marketed as a dietary supplement) requires major attention from clinicians in order to recognize both its intoxication and abstinence syndromes, which are two clinical conditions that can be characterized by initial slow response to multiple treatments and several serious life complications. Finally, given its various pharmacological actions with potential for tolerance and withdrawal, phenibut should be considered a substance requiring close medical supervision, and its prescription should be regulated by competent medical authorities.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
AF and PB conceived the presented idea. CE and GM wrote the manuscript in consultation with GD. PB supervised the project. All authors contributed to the article and approved the submitted version.
Funding
This study was partially supported by funds from ERANET NEURON JTC2018 Mental Disorders UNMET project (Neuron-051).
Acknowledgments
We thank Dr. R. Aronica for the contribution to create the figure and Dr. M. Ariyo to revise the English language.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
OwenDRWoodDMArcherJRDarganPI. Phenibut (4-amino-3-phenyl-butyric acid): availability, prevalence of use, desired effects and acute toxicity. Drug Alcohol Rev. (2016) 35:591–6. 10.1111/dar.12356
2.
ZvejnieceLVaversESvalbeBVeinbergGRizhanovaKLiepinsVet al. R-phenibut binds to the α2-δ subunit of voltage-dependent calcium channels and exerts gabapentin-like anti-nociceptive effects. Pharmacol Biochem Behav. (2015) 137:23–9. 10.1016/j.pbb.2015.07.014
3.
SchifanoFOrsoliniLDuccio PapantiGCorkeryJM. Novel psychoactive substances of interest for psychiatry. World Psychiatry. (2015) 14:15–26. 10.1002/wps.20174
4.
JourneyEA. Phenibut (β-Phenyl-γ-Aminobutyric Acid): an easily obtainable “dietary supplement” with propensities for physical dependence and addiction. Curr Psychiatry Rep. (2019) 21:23. 10.1007/s11920-019-1009-0
5.
HardmanMISprungJWeingartenTN. Acute phenibut withdrawal: a comprehensive literature review and illustrative case report. Bosnian J Basic Med Sci. (2019) 19:125. 10.17305/bjbms.2018.4008
6.
MagsalinRMMKhanAY. Withdrawal symptoms after internet purchase of phenibut (β-phenyl-γ-aminobutyric acid HCl). J Clin Psychopharmacol. (2010) 30:648–9. 10.1097/JCP.0b013e3181f057c8
7.
McCabeDJBanghSAArensAMColeJB. Phenibut exposures and clinical effects reported to a regional poison center. Am J Emerg Med. (2019) 37:2066–71. 10.1016/j.ajem.2019.02.044
8.
CoenenNCDijkstraBABatallaASchellekensAF. Detoxification of a patient with comorbid dependence on phenibut and benzodiazepines by tapering with Baclofen: case report. J Clin Psychopharmacol. (2019) 39:511–4. 10.1097/JCP.0000000000001104
9.
PelzerACvan der HeijdenFMden BoerE. Systematic review of catatonia treatment. Neuropsychiatr Dis Treat. (2018) 14:317. 10.2147/NDT.S147897
10.
MesserTLammersGMüller-SiechenederFSchmidtRFLatifiS. Substance abuse in patients with bipolar disorder: a systematic review and meta-analysis. Psychiatry Res. (2017) 253:338–50. 10.1016/j.psychres.2017.02.067
11.
FornaroMVentriglioADe PasqualeCPistorioMLDe BerardisDCattaneoCIet al. Sensation seeking in major depressive patients: relationship to sub-threshold bipolarity and cyclothymic temperament. J Affect Disord. (2013) 148:375–83. 10.1016/j.jad.2013.01.002
12.
EspositoCMD'AgostinoADell OssoBFiorentiniAPrunasCCallariAet al. Impact of the first Covid-19 pandemic wave on first episode psychosis in Milan, Italy. Psychiatry Res. (2021) 298:113802. 10.1016/j.psychres.2021.113802
13.
OrsoliniLPapantiGDDe BerardisDGuirguisACorkeryJMSchifanoF. The “endless trip” among the NPS users: psychopathology and psychopharmacology in the hallucinogen-persisting perception disorder. A systematic review. Front Psychiatry. (2017) 20:8:240. 10.3389/fpsyt.2017.00240
14.
OrsoliniLChiappiniSPapantiDDe BerardisDCorkeryJMSchifanoF. The bridge between classical and “synthetic”/chemical psychoses: towards a clinical, psychopathological, therapeutic, and perspective. Front Psychiatry. (2019) 20:851. 10.3389/fpsyt.2019.00851
Summary
Keywords
withdrawal, psychiatric aspects, psychopharmacology, phenibut, psychomotor agitation
Citation
Esposito CM, Mandolini GM, Delvecchio G, Fiorentini A and Brambilla P (2021) Psychomotor Agitation Non-responsive to Treatment: A Case Report of Phenibut Withdrawal Syndrome. Front. Psychiatry 12:688147. doi: 10.3389/fpsyt.2021.688147
Received
30 March 2021
Accepted
14 May 2021
Published
28 June 2021
Volume
12 - 2021
Edited by
Giuseppe Bersani, Sapienza University of Rome, Italy
Reviewed by
Domenico De Berardis, Azienda Usl Teramo, Italy; Fabrizio Schifano, University of Hertfordshire, United Kingdom; Jolanta B. Zawilska, Medical University of Lodz, Poland
Updates
Copyright
© 2021 Esposito, Mandolini, Delvecchio, Fiorentini and Brambilla.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alessio Fiorentini alessio.fiorentini@gmail.com
This article was submitted to Addictive Disorders, a section of the journal Frontiers in Psychiatry
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.