- 1Affiliated Mental Health Center and Hangzhou Seventh People’s Hospital, Zhejiang University School of Medicine, Hangzhou, China
- 2Fuyang Third People’s Hospital, Hangzhou, China
- 3The Fifth Hospital of Ruian, Wenzhou, China
- 4Zhejiang Provincial Institute of Drug Abuse Research, Hangzhou, China
Background: Social cognition and interaction training (SCIT) is a psychosocial intervention program for patients with psychosis, designed to improve their social functioning by improving social cognition. Although the feasibility and efficacy of SCIT have been verified, patients with schizophrenia tend to suffer from motivational deficits and low treatment adherence. It has been suggested that using virtual reality (VR) technology might be effective in addressing these issues. In this study, we aimed to develop a VR-based SCIT and compare its efficacy with that of traditional SCIT.
Materials and methods: We developed a novel VR-based social cognition and interaction training (VR-SCIT) that combines traditional SCIT (TR-SCIT) intervention with VR technology. Participants were randomly assigned in a 1:1:1 ratio to the VR-SCIT (n = 28), TR-SCIT (n = 30), or waiting-list groups (n = 29). All treatments were combined with treatment-as-usual. Assessments of social cognition (i.e., Chinese version of Face-Affective Identification Task, Chinese version of Social Cognition Screening Questionnaire) and social functioning (i.e., Chinese version of Personal and Social Performance Scale) were administered from baseline to post-intervention.
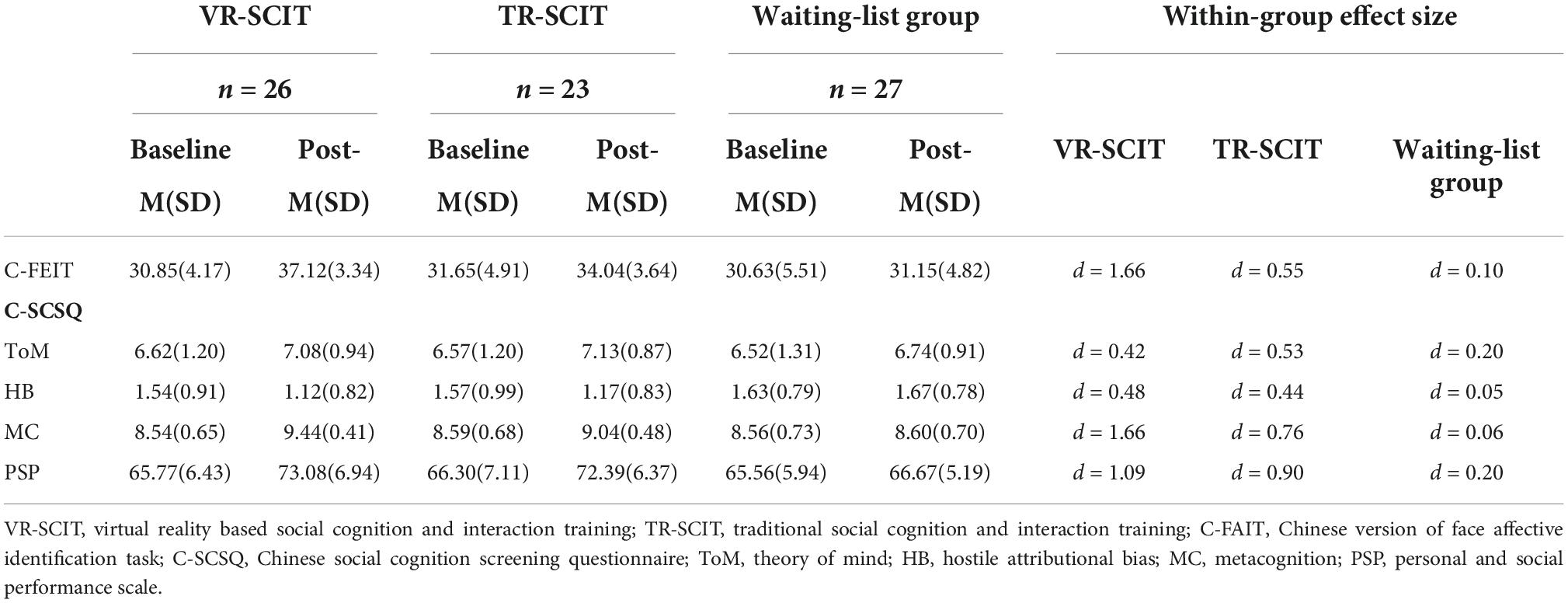
Results: Patients receiving VR-SCIT and TR-SCIT showed a significantly greater improvement on the assessments of emotion perception (Cohen’s d was 1.66, 0.55, and 0.10 for VR-SCIT, TR-SCIT, and Waiting-list, respectively), hostile attributional bias (Cohen’s d was 0.48, 0.44, and 0.05 for VR-SCIT, TR-SCIT, and Waiting-list, respectively), metacognition (Cohen’s d was 1.66, 0.76, and 0.06 for VR-SCIT, TR-SCIT, and waiting-list, respectively), and social functioning (Cohen’s d was 1.09, 0.90, and 0.20 for VR-SCIT, TR-SCIT, and waiting-list, respectively) from baseline to post-intervention, compared to those in waiting-list group. Additionally, VR-SCIT showed an advantage over TR-SCIT in improving emotion perception and metacognition with higher treatment compliance.
Conclusion: These preliminary findings indicate that VR-SCIT is a feasible and promising method for improving social cognition and social functioning in patients with schizophrenia.
Introduction
Schizophrenia is a chronic, severe, and crippling mental illness, with a lifetime prevalence of 0.6% in China, which results in a substantial societal burden (1). Social dysfunction is a core clinical feature of schizophrenia and is associated with poor quality of life (2). Reportedly, social dysfunction in patients with schizophrenia is mostly due to an impairment of social cognition (3).
Social cognition refers to understanding the self and others’ mental states and applying this social knowledge to build social behavior (4). Social cognition plays a critical role in daily social interactions and contributes to social success (5). Social cognition is severely impaired in patients with schizophrenia across a variety of domains, such as emotion processing, social perception, theory of mind, and attributional bias (6). Various interventions have been developed over the last few decades to ameliorate social cognition deficits in schizophrenia (7). Among these, social cognition and interaction training (SCIT) has become one of the most widely accepted clinical practices in patients with schizophrenia (8). The feasibility and efficacy of SCIT in schizophrenia have been verified in different clinical settings and cultural backgrounds (9–18).
Motivation deficits and a lack of ecological validity are the main challenges for the implementation of conventional social interventions (19–22). The lack of motivation is a critical factor that contributes to functional disability in schizophrenia, as it discourages an individual from engaging in and adhering to an effective treatment program (23). Meanwhile, as a result of training approaches that may not adequately reflect the complex, interactive, and dynamic nature of real-life social settings, the effects of conventional social interventions on higher-order social cognitive processes and social functioning may be restricted (24). Furthermore, low session adherence has been reported in previous studies on SCIT (25, 26). For example, Dark et al. (25) reported that session adherence was only around 50% on average in their study, which was close to the minimum threshold needed to ensure treatment effectivity (10, 13).
The use of virtual reality (VR) for psychological interventions with gamification-oriented design has been proposed as a possible way to address these issues (27). VR is immersive, interactive, and dynamic, and it elicits psychological reactions that are similar to those occurring in everyday life. Therefore, it is suitable for simulating a range of social situations and accurately portraying their complexity (28). Simultaneously, due to the controllability of VR, situations may be scripted, repeated, modified, and customized, facilitating systematic practice (29). More importantly, gamification has the potential to compensate for motivational impairments using game design elements (30, 31).
Virtual reality interventions have already been utilized successfully in a variety of settings aimed at evaluating and improving symptoms and functional outcomes in schizophrenia (32–36). These studies show that VR can be tolerated by patients with schizophrenia and other psychotic diseases, and it may be useful as a stand-alone or adjunct treatment for a range of medical and psychological therapies (37, 38).
In this study, we aimed to develop an SCIT based on VR and check its efficacy compared to traditional SCIT. It is expected that gamification of VR-SCIT would be associated with a higher feasibility, which may in turn result in a higher adherence to intervention. We also hypothesized that a well-designed VR-SCIT would show an improved efficacy compared with traditional SCIT.
Materials and methods
Participants
Eighty-seven participants were diagnosed with schizophrenia based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition criteria (39). Eligibility requirements included the following: (1) 18–50 years old, right-handed, with normal vision and hearing; (2) meeting the diagnostic principles for Andreasen’s remission criteria (40); and (3) only treated with atypical antipsychotics during the study period. Individuals were excluded if they met the criteria for substance use disorder, intellectual disability, head injury, or disease of the central nervous system. Those who had received previous psychological therapy were also excluded. All participants were recruited from the Seventh Hospital of Hangzhou. All participants in this study gave written, informed consent. Written informed consent was also obtained from the individuals for the publication of any potentially identifiable images or data included in this article. This study was approved by the local ethics committee of the Seventh Hospital of Hangzhou (identifier 2019-004).
Participants were randomly distributed using a computer-generated list of random numbers and assigned in a 1:1:1 ratio to the following groups: VR-SCIT group (n = 28), TR-SCIT group (n = 30), or waiting-list group (n = 29). These groups received the corresponding treatments (VR-SCIT, TR-SCIT, or no treatment) along with the usual medical treatment. During the study, two patients dropped out for symptom aggravation in the VR-SCIT group, one patient dropped out for symptom aggravation and five for voluntary withdrawal in the TR-SCIT group, and two patients dropped out for symptom aggravation in the waiting list group at week-3 time-point. In addition, one patient dropped out for voluntary withdrawal in the TR-SCIT group at week-5 time-point. Therefore, 26 VR-SCIT, 23 TR-SCIT, and 27 waiting-list participants completed the post-intervention assessments. A flowchart of the study is shown in Figure 1.
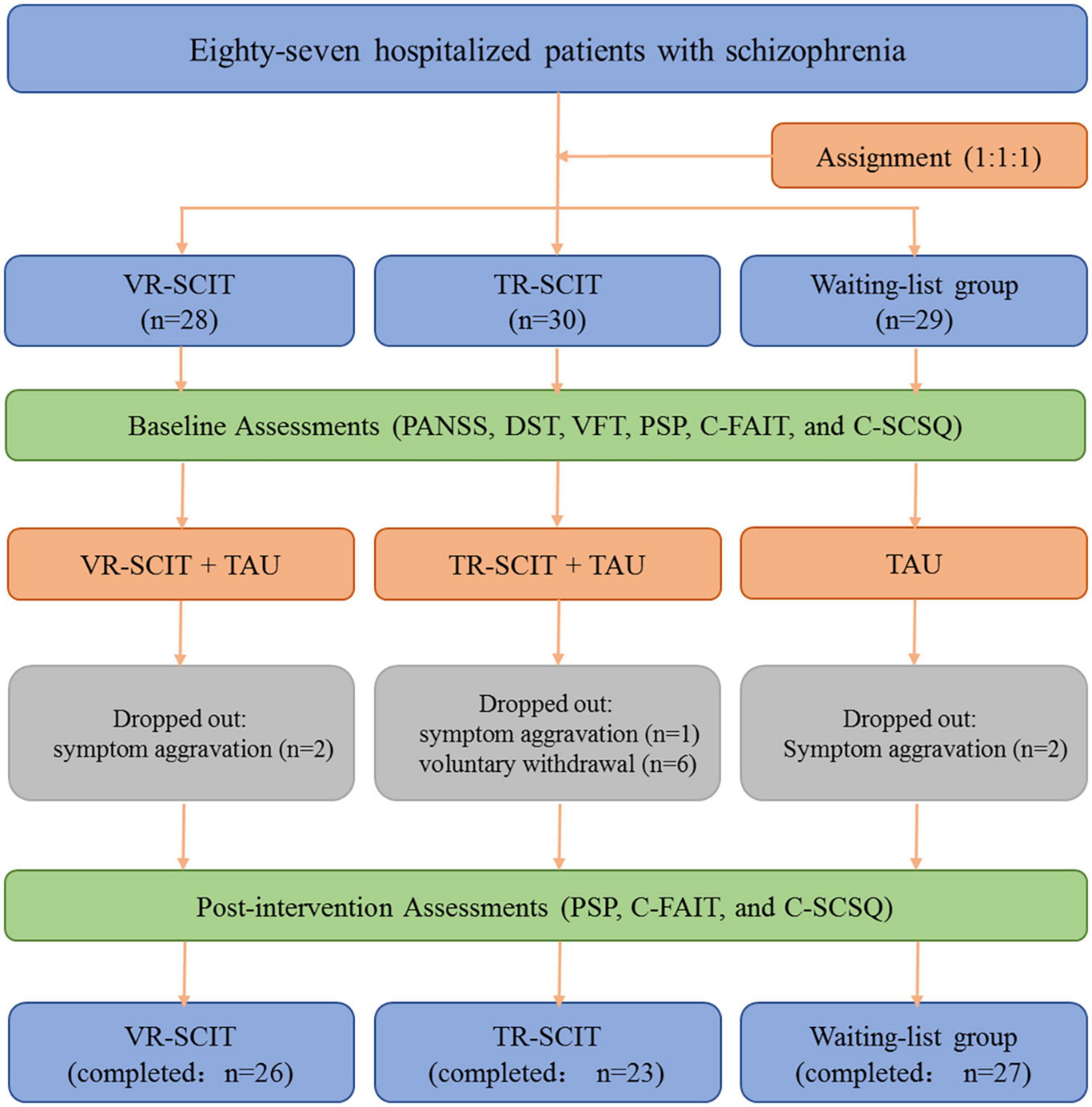
Figure 1. Flowchart of the present work. VR-SCIT, virtual reality based social cognition and interaction training; TR-SCIT, traditional social cognition and interaction training; PANSS, positive and negative syndrome scale; PSP, personal and social performance scale; DST, digit span test; VFT, verbal fluency test; C-FAIT, Chinese version of face affective identification task; C-SCSQ, Chinese social cognition screening questionnaire.
Interventions and procedure
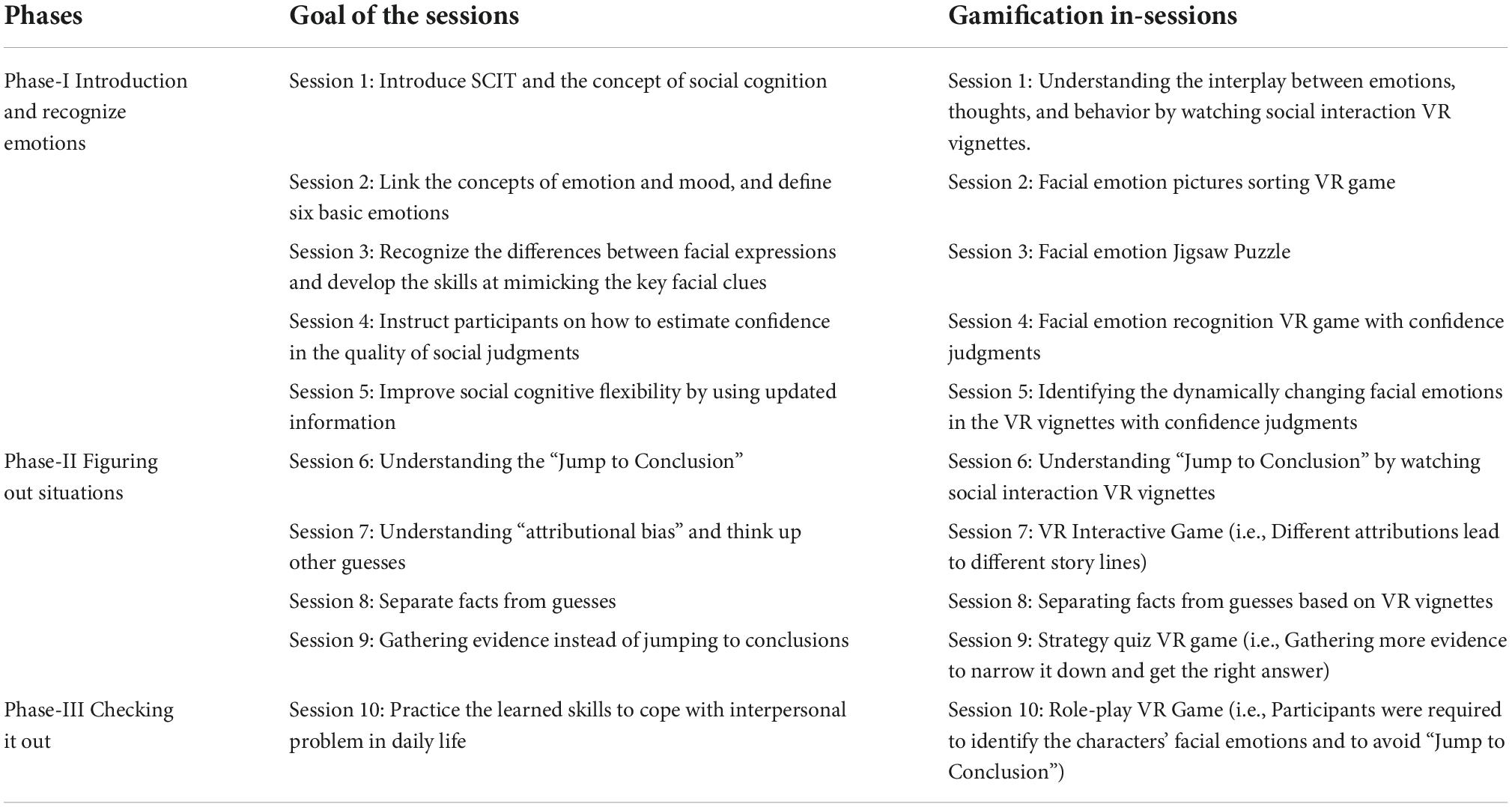
Virtual reality-based social cognition and interaction training was a 3-phase, 10-sessions individual intervention. Each phase took place once a week over a period of 3 weeks. VR-SCIT was delivered to the inpatient department, which was completed by the participants according to the instructions. This involves mass practice and compensatory strategy training (Table 1).
Phase I consisted of five sessions focused on emotion-perception training. Participants learned about six basic emotions through a picture-sorting game and identified facial cues associated with different emotions through a jigsaw puzzle in VR. Participants practiced several strategies (e.g., mimicking emotions) to aid in emotion recognition, which they were encouraged to try at home. Phase II, with four sessions, addressed theory of mind deficits and attributional bias, in which participants were trained to avoid the pitfalls associated with jumping to conclusions. Participants recognized the harm of jumping to conclusions by viewing scripted social scenarios in the VR environment. Three social strategies can be learned to understand situations: generating perspective-taking, distinguishing social facts from guesses, and gathering additional evidence. Phase III with one session, focused on the integration of learned skills to cope with real-life interpersonal and emotional problems. Participants applied social cognitive skills in a VR role-play game, in which they could consider different possible ways to react to a situation. The game continued until the most appropriate answer was chosen. Participants continued to practice identifying emotions, thoughts, and behaviors, and understanding their interrelatedness (Figure 2).

Figure 2. Example of virtual reality based social cognition and interaction training (VR-SCIT) scenarios. (A) VR screen shot of phase-I (recognize emotions): A person was answering a phone (voice shielding) with an angry expression on his face, and participants were asked to judge the emotion by recognizing facial cues. (B) VR screen shot of phase-II (figuring out situations): After the girl left, another person came in looking for something and messed up her desk. When the girl came back, she blamed the boy for messing up her desk without knowing the facts. (C) VR screen shot of phase-III (checking it out): This was a Role-Play Game about office stories, participants needed to make the right choices about identifying emotions, thoughts and behaviors. (D) The scene of VR-SCIT intervention.
The TR-SCIT was exactly the same as the previous work we conducted in the community setting [Wang et al. (15)], but with an interval of 2–3 days between sessions. Five SCIT interventions were conducted, each with six inpatient participants. The TR-SCIT took 5 weeks to complete and included three phases: (1) introduction and emotions (seven sessions), (2) figuring out situations (eight sessions), and (3) checking it out (five sessions).
For all participants, antipsychotic medication type and dose were not controlled and instead left to the discretion of the participants’ treating psychiatrists. The psychiatrists who were blinded to the interventional conditions administered all assessments measures to the subjects at both baseline and the endpoint.
Virtual reality application and virtual reality devices
A Visual Studio code editor was used to write and debug the code. Unity3D software was used to create the UI. Finally, the application runs on the Pico Goblin2 All-In-One (Featuring the Qualcomm® Snapdragon 835 CPU with 4G high-speed LPDDR4-1866 RAM) with the Android 8.1 operating system.
Assessments
Psychopathology and neuropsychological tests
Psychopathology was assessed using the Positive and Negative Syndrome Scale (PANSS) by experienced clinicians (41, 42). The Digit Span Test (DST) and Verbal Fluency Test (VFT) were administered to all participants as neuropsychological background tests (43, 44). The total score on the VFT was the number of animals named correctly in a minute. The total score on the DST was the sum of correctly recalled digits across the digits-forward and digits-backward sub-tests.
Social functioning
Social functioning was evaluated using the Chinese version of the Personal and Social Performance Scale (PSP) by psychiatrists who had received training in the use of this method. The PSP total ratings had adequate inter-rater reliability in this study (inter-class correlation coefficient was 0.81) (45).
Social cognition
Emotion perception
Emotion perception (EP) was assessed using the Chinese version of the Face-Affective Identification Task (C-FAIT) (46). Participants were required to indicate the emotion conveyed in each photograph. The set of C-FAIT test photos used in the current study consisted of 56 photos in total: 48 photos showing six basic emotions (happiness, anger, disgust, sadness, surprise, and fear) and eight photos conveying neutral emotions. The total score for the C-FAIT ranged from 0 to 48, with higher scores indicating better emotion perception.
Chinese version of social cognition screening questionnaire
The Chinese version of social cognition screening questionnaire (C-SCSQ) was used to probe the participants’ social cognition, including theory of mind, metacognition, and hostile attributional bias (47). In the C-SCSQ, participants were presented orally with 10 interpersonal vignettes that describe ambiguous interpersonal situations and were required to answer three yes/no questions. In the present work, the scores of theory of mind (ranging from 0–10 to, with higher scores indicating better performance), metacognition (ranging from 7–10 to, higher scores indicate better metacognitive ability), and hostile attributional bias (ranging from 0–5 to, higher scores indicate greater bias) were calculated for each participant.
Statistical analysis
Pearson’s chi-square test was performed for the female/male ratio and persistence rate of intervention between the groups. One-way analysis of variance (ANOVA) was performed for group comparisons of the demographic and clinical characteristics. A repeated measures ANOVA was conducted for the C-FAIT, C-SCSQ, and PSP scores, with time (baseline vs. post-intervention) as the within-group factor and group (VR-SCIT vs. TR-SCIT vs. waiting-list) as a between-group factor. Within-group effect size estimates were computed using Cohen’s d (d). Post-hoc multiple comparisons were conducted using Bonferroni correction.
Results
Demographic and clinical characteristics
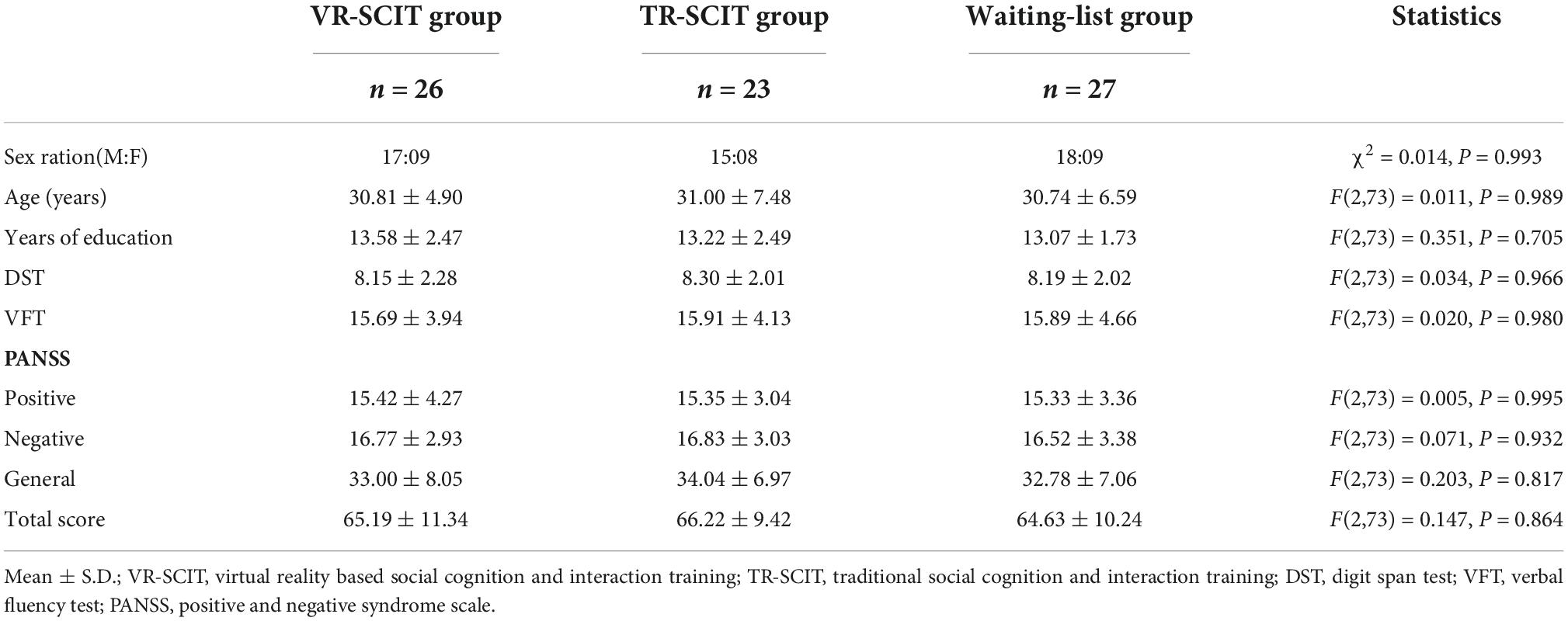
Chi-square tests showed no significant difference in sex between the three groups (χ2 = 0.014, P = 0.993). No significant difference was found between groups for age (F(2,73) = 0.011, P = 0.989), education levels (F(2,73) = 0.351, P = 0.705), DST (F(2,73) = 0.034, P = 0.966), VFT (F(2,73) = 0.020, P = 0.980), PANSS-P (F(2,73) = 0.005, P = 0.995), PANSS-N (F(2,73) = 0.071, P = 0.932), PANSS-G (F(2,73) = 0.203, P = 0.817) and PANSS-T (F(2,73) = 0.147, P = 0.864), respectively. The details are summarized in Table 2.
Feasibility
Although there was no significant difference in the overall dropout rate between the VR-SCIT and the TR-SCIT groups (week-3 time-point: 2/28 and 6/30, respectively, χ2 = 1.077, P = 0.299; week-5 time-point: 2/28 and 7/30, respectively, χ2 = 1.793, P = 0.181), the TR-SCIT group had a significantly higher voluntary withdrawal rate than the VR-SCIT group (week-3 time-point: 5/30 and 0/28, respectively, Fisher’s exact test, P = 0.053; week-5 time-point: 6/30 and 0/28, respectively, Fisher’s exact test, P = 0.024).
Social cognition and social functioning
Details of social cognition and social functioning outcomes are summarized in Table 3.
Emotion perception
For C-FAIT, there was a significant main effect of time (F(1,73) = 110.619, P < 0.001, partialη2 = 0.602), indicating that participants had a higher C-FAIT score at post-intervention than at baseline. There was a significant main effect of group (F(2,73) = 3.513, P = 0.035, partialη2 = 0.088) and a significant interaction between group and time (F(2,73) = 35.338, P < 0.001, partialη2 = 0.492). Further analyses revealed that both VR-SCIT (P < 0.001) and TR-SCIT (P = 0.039) groups had a significantly higher score than the waiting-list group post-intervention, although there was no significant difference among groups at baseline (all P≈1.000). In addition, the VR-SCIT group had a significantly higher post-intervention score than the TR-SCIT group (P = 0.027).
Theory of mind
For theory of mind, there was a significant main effect of time (F(1,73) = 11.849, P = 0.001, partialη2 = 0.140), reflecting that participants had a higher theory of mind score post-intervention than at baseline. There was no significant main effect of group (F(2,73) = 0.455, P = 0.636, partialη2 = 0.012) and no significant interaction between group and time (F(2,73) = 0.712, P = 0.494, partialη2 = 0.019).
Hostile attributional bias
For hostile attributional bias, there was a significant main effect of time (F(1,73) = 14.957, P < 0.001, partialη2 = 0.170), reflecting that participants had a lower hostile attributional bias post-intervention than at baseline. There was no significant main effect of group (F(1,73) = 1.244, P = 0.294, partialη2 = 0.033). There was a significant interaction between group and time (F(2,73) = 5.099, P = 0.008, partialη2 = 0.123). Further analyses revealed that the VR-SCIT group had a significantly lower score than the waiting-list group at post-intervention (P = 0.047), while no other significant differences were found in the rest of pairwise comparisons at post-intervention or at baseline (P ≥ 0.106).
Metacognition
For metacognition, there was a significant main effect of time (F(1,73) = 82.545, P < 0.001, partialη2 = 0.531), reflecting that participants had a higher metacognition score post-intervention than at baseline. There was a significant main effect of group (F(2,73) = 3.269, P = 0.044, partialη2 = 0.082) and a significant interaction between group and time (F(2,73) = 25.491, P < 0.001, partialη2 = 0.411). Further analyses revealed that both VR-SCIT (P < 0.001) and TR-SCIT (P = 0.019) groups had a significantly higher score than the waiting-list group at post-intervention, although there was no significant difference between the groups at baseline (all P≈1.000). In addition, the VR-SCIT group had a significantly higher post-intervention score than the TR-SCIT group (P = 0.036).
Social functioning
For PSP, there was a significant main effect of time (F(1,73) = 68.818, P < 0.001, partialη2 = 0.485), but the analysis did not reveal an effect of group (F(2,73) = 2.773, P = 0.069, partialη2 = 0.071). The participants had a higher PSP score post-intervention than at baseline. There was a significant interaction between group and time (F(2,73) = 11.065, P < 0.001, partialη2 = 0.233). Further analyses revealed that both VR-SCIT (P = 0.001) and TR-SCIT (P = 0.005) groups had a significantly higher score than the waiting-list group post-intervention, but there was no significant difference between groups at baseline (all P≈1.000).
Discussion
In the present study, we developed a VR-SCIT with a gamification-oriented design according to the principles of TR-SCIT. Our primary findings indicate that VR-SCIT had a higher treatment adherence than TR-SCIT and a comparable efficacy.
Patients in the VR-SCIT group had a lower dropout rate than those in the TR-SCIT group at both week-3 and week-5 time-point. Notably, none of the participants voluntarily withdrew from the VR-SCIT sessions. These findings, as expected, indicate that VR-SCIT has a high acceptability among patients with schizophrenia. We cautiously speculate that the high compliance in VR-SCIT could be partly explained by its gamification-oriented design. Recently, gamification has been widely used in the research realm of psychosocial interventions for psychosis (31, 48). In gamification, the introduction of game elements can significantly compensate for patients’ lack of motivation toward the treatment (30, 31). However, our results revealed that six patients voluntarily withdrew from TR-SCIT. These findings are contrary to those from our previous work in community settings [Wang et al. (15)], in which we found that no participants withdrew from the intervention. We speculate that this inconsistency could be accounted for by the type of sample enrolled in these studies. In the study by Wang et al. (15), patients were recruited from Chinese community settings and received regular follow-up in accordance with the local mental health policy. However, in the present study, all the included patients were inpatients. The average length of hospital stay was approximately 30 days. In this sense, it was difficult to ensure the participants’ retention under the TR-SCIT program, which lasted for 5 weeks. Taken together, we could expect that the 3-week VR-SCIT program with a gamification-oriented design would be more feasible in different clinical settings.
Regarding efficacy, both the VR-SCIT and TR-SCIT demonstrated statistically significant improvements in the domains of emotion perception, metacognition, hostile attributional bias, and social functioning. These findings are mostly consistent with those of previous studies and support the efficacy of SCIT for the improvement of social cognition and social functioning in patients with schizophrenia. However, neither SCIT format showed an advantage over the waiting list group in improving the theory of mind. The lack of an effect on theory of mind is inconsistent with our previous work but consistent with other studies (10, 13). One explanation, as Roberts pointed out, may be that SCIT has less impact on higher-functioning patients (13). In the present study, the patients were hospitalized with acute episodes, many of which were first episodes. In contrast, in our previous study (15), participants were patients with chronic schizophrenia. In addition, we found that VR-SCIT showed an advantage over TR-SCIT in improving emotion perception and metacognition. We speculate that this may be associated with the more intense and immersive training in VR-SCIT than in TR-SCIT. In addition, the gamification design offered participants the opportunity to practice these skills.
In general, the present study was preliminary and had a few limitations. First, the sample size was small, which limits the generalizability of our findings. Second, the assessments of psychopathology and neuropsychological were only administered at baseline; thus, no conclusions can be drawn regarding whether VR-SCIT may be also effective for the improvement of psychotic symptoms or neurocognitive. Third, follow-up was not conducted after the intervention. Therefore, it is uncertain whether the observed efficacy was stable over time. Further multi-center, large-sample, long-term follow-up randomized controlled studies are needed in the future. In addition, our team is developing a VR-based social cognitive assessment tool to improve the ecological validity of the assessment.
In summary, despite several limitations, the present study provides the first evidence that VR-SCIT has the potential to improve social cognition in patients with schizophrenia. Although preliminary, it is suggested that the SCIT program, including the VR-based format, should become part of routine clinical interventions for patients with schizophrenia.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the local ethics committee of the Seventh Hospital of Hangzhou. The patients/participants provided their written informed consent to participate in this study. Written informed consent was also obtained from the individuals for the publication of any potentially identifiable images or data included in this article.
Author contributions
Z-HS contributed to data collection, data analyses, writing—original draft, and manuscript redaction and revisions. M-HL, YW, and Q-QL contributed to data collection and data analyses. Y-GW contributed to study design and manuscript redaction and revisions. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Science and Technology Bureau of Hangzhou (Grant Nos. 20180533B82, 20190101A11, and 20201203B190), the Zhejiang Provincial Natural Science Foundation of China (Grant Nos. LGF18H090023 and LGF22H090036), and the Project for Hangzhou Medical Disciplines of Excellence and Key Project for Hangzhou Medical Disciplines.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. (2019) 6:211–24. doi: 10.1016/S2215-0366(18)30511-X
2. Tan XW, Seow E, Abdin E, Verma S, Sim K, Chong SA, et al. Subjective quality of life among patients with schizophrenia spectrum disorder and patients with major depressive disorder. BMC Psychiatry. (2019) 19:267. doi: 10.1186/s12888-019-2248-7
3. Green MF, Horan WP, Lee J. Nonsocial and social cognition in schizophrenia: current evidence and future directions. World Psychiatry. (2019) 18:146–61. doi: 10.1002/wps.20624
4. Adolphs R. The neurobiology of social cognition. Curr Opin Neurobiol. (2001) 11:231–9. doi: 10.1016/s0959-4388(00)00202-6
5. Harvey PD, Penn D. Social cognition: the key factor predicting social outcome in people with schizophrenia? Psychiatry. (2010) 7:41–4.
6. Portillo C. The Significance of Social Cognition and Neurocognition on Functional Capacity in Schizophrenia Spectrum Disorders. Dissertations, Hofstra University, Hempstead, NY (2020).
7. Nijman SA, Veling W, van der Stouwe ECD, Pijnenborg GHM. Social cognition training for people with a psychotic disorder: a network meta-analysis. Schizophr Bull. (2020) 46:1086–103. doi: 10.1093/schbul/sbaa023
8. Vass E, Fekete Z, Simon V, Simon L. Interventions for the treatment of theory of mind deficits in schizophrenia: systematic literature review. Psychiatry Res. (2018) 267:37–47. doi: 10.1016/j.psychres.2018.05.001
9. Combs DR, Adams SD, Penn DL, Roberts D, Tiegreen J, Stem P. Social cognition and interaction training (SCIT) for inpatients with schizophrenia spectrum disorders: preliminary findings. Schizophr Res. (2007) 91:112–6. doi: 10.1016/j.schres.2006.12.010
10. Roberts DL, Penn DL. Social cognition and interaction training (SCIT) for outpatients with schizophrenia: a preliminary study. Psychiatry Res. (2009) 166:141–7. doi: 10.1016/j.psychres.2008.02.007
11. Combs DR, Elerson K, Penn DL, Tiegreen JA, Nelson A, Ledet SN, et al. Stability and generalization of Social cognition and interaction training (SCIT) for schizophrenia: six-month follow-up results. Schizophr Res. (2009) 112:196–7. doi: 10.1016/j.schres.2009.04.010
12. Roberts DL, Penn DL, Labate D, Margolis SA, Sterne A. Transportability and feasibility of social cognition and interaction training (SCIT) in community settings. Behav Cogn Psychother. (2010) 38:35–47. doi: 10.1017/S1352465809990464
13. Roberts DL, Combs DR, Willoughby M, Mintz J, Gibson C, Rupp B, et al. A randomized, controlled trial of social cognition and interaction training (SCIT) for outpatients with schizophrenia spectrum disorders. Br J Clin Psychol. (2014) 53:281–98. doi: 10.1111/bjc.12044
14. Zhu S, Zhu K, Jiang D, Shi J. Social cognition and interaction training for major depression: a preliminary study. Psychiatry Res. (2018) 270:890–4. doi: 10.1016/j.psychres.2018.11.008
15. Wang Y, Roberts DL, Xu B, Cao R, Yan M, Jiang Q. Social cognition and interaction training for patients with stable schizophrenia in Chinese community settings. Psychiatry Res. (2013) 210:751–5. doi: 10.1016/j.psychres.2013.08.038
16. Gordon A, Davis PJ, Patterson S, Pepping CA, Scott JG, Salter K, et al. A randomized waitlist control community study of social cognition and interaction training for people with schizophrenia. Br J Clin Psychol. (2018) 57:116–30. doi: 10.1111/bjc.12161
17. Kanie A, Kikuchi A, Haga D, Tanaka Y, Ishida A, Yorozuya Y, et al. The feasibility and efficacy of social cognition and interaction training for outpatients with schizophrenia in Japan: a multicenter randomized clinical trial. Front Psychiatry. (2019) 10:589. doi: 10.3389/fpsyt.2019.00589
18. Voutilainen G, Kouhia T, Roberts DL, Oksanen J. Social cognition and interaction training (SCIT) for adults with psychotic disorders: a feasibility study in Finland. Behav Cogn Psychother. (2016) 44:711–6. doi: 10.1017/S1352465816000151
19. Hermans K, Achterhof R, Myin-Germeys I, Kasanova Z, Kirtley O, Schneider M. Improving ecological validity in research on social cognition. Soc Cogn Psychosis. (2019) 2019:249–68. doi: 10.1016/B978-0-12-815315-4.00010-0
20. Gard DE, Sanchez AH, Starr J, Cooper S, Fisher M, Rowlands A, et al. Using self-determination theory to understand motivation deficits in schizophrenia: the ‘why’ of motivated behavior. Schizophr Res. (2014) 156:217–22. doi: 10.1016/j.schres.2014.04.027
21. Fervaha G, Zakzanis KK, Foussias G, Graff-Guerrero A, Agid O, Remington G. Motivational deficits and cognitive test performance in schizophrenia. JAMA Psychiatry. (2014) 71:1058–65. doi: 10.1001/jamapsychiatry.2014.1105
22. Osborne-Crowley K. Social cognition in the real world: reconnecting the study of social cognition with social reality. Rev Gen Psychol. (2020) 24:144–58. doi: 10.1177/1089268020906483
23. Schlosser DA, Fisher M, Gard D, Fulford D, Loewy RL, Vinogradov S. Motivational deficits in individuals at-risk for psychosis and across the course of schizophrenia. Schizophr Res. (2014) 158:52–7. doi: 10.1016/j.schres.2014.06.024
24. Peyroux E, Franck N. RC2S: a cognitive remediation program to improve social cognition in schizophrenia and related disorders. Front Hum Neurosci. (2014) 8:400. doi: 10.3389/fnhum.2014.00400
25. Dark F, Scott JG, Baker A, Parker S, Gordon A, Newman E, et al. Randomized controlled trial of social cognition and interaction training compared to befriending group. Br J Clin Psychol. (2020) 59:384–402. doi: 10.1111/bjc.12252
26. Parker S, Foley S, Walker P, Dark F. Improving the social cognitive deficits of schizophrenia: a community trial of social cognition and interaction training (SCIT). Australas Psychiatry. (2013) 21:346–51. doi: 10.1177/1039856213486305
27. Kim S, Kim E. The use of virtual reality in psychiatry: a review. Soa Chongsonyon Chongsin Uihak. (2020) 31:26–32. doi: 10.5765/jkacap.190037
28. Nijman SA, Veling W, Greaves-Lord K, Vermeer RR, Vos M, Zandee CER, et al. Dynamic interactive social cognition training in virtual reality (DiSCoVR) for social cognition and social functioning in people with a psychotic disorder: study protocol for a multicenter randomized controlled trial. BMC Psychiatry. (2019) 19:272. doi: 10.1186/s12888-019-2250-0
29. Maskey M, Rodgers J, Ingham B, Freeston M, Evans G, Labus M, et al. Using virtual reality environments to augment cognitive behavioral therapy for fears and phobias in autistic adults. Autism Adulthood. (2019) 1:134–45. doi: 10.1089/aut.2018.0019
30. Sardi L, Idri A, Fernández-Alemán JL. A systematic review of gamification in e-Health. J Biomed Inform. (2017) 71:31–48. doi: 10.1016/j.jbi.2017.05.011
31. Vajawat B, Varshney P, Banerjee D. Digital gaming interventions in psychiatry: evidence, applications and challenges. Psychiatry Res. (2021) 295:113585. doi: 10.1016/j.psychres.2020.113585
32. Rus-Calafell M, Garety P, Sason E, Craig TJK, Valmaggia LR. Virtual reality in the assessment and treatment of psychosis: a systematic review of its utility, acceptability and effectiveness. Psychol Med. (2018) 48:362–91. doi: 10.1017/S0033291717001945
33. Park KM, Ku J, Choi SH, Jang HJ, Park JY, Kim SI, et al. A virtual reality application in role-plays of social skills training for schizophrenia: a randomized, controlled trial. Psychiatry Res. (2011) 189:166–72. doi: 10.1016/j.psychres.2011.04.003
34. Pot-Kolder RMCA, Geraets CNW, Veling W, van Beilen M, Staring ABP, Gijsman HJ, et al. Virtual-reality-based cognitive behavioural therapy versus waiting list control for paranoid ideation and social avoidance in patients with psychotic disorders: a single-blind randomised controlled trial. Lancet Psychiatry. (2018) 5:217–26. doi: 10.1016/S2215-0366(18)30053-1
35. Horan B, Heckenberg R, Maruff P, Wright B. Development of a new virtual reality test of cognition: assessing the test-retest reliability, convergent and ecological validity of CONVIRT. BMC Psychol. (2020) 8:61. doi: 10.1186/s40359-020-00429-x
36. Nijman SA, Veling W, Greaves-Lord K, Vos M, Zandee CER, Aan Het Rot M, et al. Dynamic interactive social cognition training in virtual reality (DiSCoVR) for people with a psychotic disorder: single-group feasibility and acceptability study. JMIR Ment Health. (2020) 7:e17808. doi: 10.2196/17808
37. Adery LH, Ichinose M, Torregrossa LJ, Wade J, Nichols H, Bekele E, et al. The acceptability and feasibility of a novel virtual reality based social skills training game for schizophrenia: preliminary findings. Psychiatry Res. (2018) 270:496–502. doi: 10.1016/j.psychres.2018.10.014
38. Freeman D, Reeve S, Robinson A, Ehlers A, Clark D, Spanlang B, et al. Virtual reality in the assessment, understanding, and treatment of mental health disorders. Psychol Med. (2017) 47:2393–400. doi: 10.1017/S003329171700040X
39. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Virginia, VA: American Psychiatric Association (2013)
40. Andreasen NC, Carpenter WT Jr, Kane JM, Lasser RA, Marder SR, Weinberger DR. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry. (2005) 162:441–9. doi: 10.1176/appi.ajp.162.3.441
41. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. (1987) 13:261–76. doi: 10.1093/schbul/13.2.261
42. Si TM, Yang JZ, Shu L, Wang XL, Zhou M, Li XN, et al. The reliability, validity of PANSS and its implication. Chin Ment Health J. (2004) 1:45–7.
43. Leung JL, Lee GT, Lam YH, Chan RC, Wu JY. The use of the Digit Span Test in screening for cognitive impairment in acute medical inpatients. Int Psychogeriatr. (2011) 23:1569–74. doi: 10.1017/S1041610211000792
44. Ghemulet M, Baskini M, Messinis L, Mouza E, Proios H. Taste perception analysis using a semantic verbal fluency task. Psychol Res Behav Manag. (2014) 7:261–72. doi: 10.2147/PRBM.S66428
45. Tianmei S, Liang S, Yun’ai S, Chenghua T, Jun Y, Jia C, et al. The Chinese version of the personal and social performance scale (PSP): validity and reliability. Psychiatry Res. (2011) 185:275–9. doi: 10.1016/j.psychres.2010.05.001
46. Wang K, Hoosain R, Lee TMC, Meng Y, Fu J, Yang R. Perception of six basic emotional facial expressions by the Chinese. J Cross Cult Psychol. (2006) 37:623–9. doi: 10.1177/0022022106290481
47. Lo PMT, Siu AMH. Assessing social cognition of persons with schizophrenia in a Chinese population: a pilot study. Front Psychiatry. (2018) 8:302. doi: 10.3389/fpsyt.2017.00302
Keywords: virtual reality, social cognition and interaction training, schizophrenia, social cognition, social functioning, psychosis
Citation: Monaco M, Floridia M, Giuliano M, Palmieri L, Lo Noce C, Pantosti A, Palamara AT, Brusaferro S, Onder G and The Italian National Institute of Health COVID-19 Mortality Group (2022) Virtual-reality-based social cognition and interaction training for patients with schizophrenia: A preliminary efficacy study. Front. Psychiatry 13:1022278. doi: 10.3389/fpsyt.2022.1022278
Received: 18 August 2022; Accepted: 02 November 2022;
Published: 17 November 2022.
Edited by:
Jung-Seok Choi, Samsung Medical Center, South KoreaReviewed by:
Sung Nyun Kim, Seoul National University, South KoreaYanghua Tian, First Affiliated Hospital of Anhui Medical University, China
Copyright © 2022 Shen, Liu, Wu, Lin and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yong-Guang Wang, d2FuZ3lvbmdndWFuZzc4QDE2My5jb20=
 Zhi-Hua Shen
Zhi-Hua Shen Meng-Hui Liu2
Meng-Hui Liu2 Qian-Qian Lin
Qian-Qian Lin Yong-Guang Wang
Yong-Guang Wang