- 1Department of Psychiatry, National Health Insurance Service Ilsan Hospital, Goyang-si, South Korea
- 2Institute of Behavioral Sciences in Medicine, College of Medicine, Yonsei University, Seoul, South Korea
- 3Department of Psychiatry, Samsung Medical Center, Sungkyunkwan University, Seoul, South Korea
- 4Center for Clinical Research, Samsung Biomedical Research Institute (SBRI), Seoul, South Korea
- 5School of Medicine, Sungkyunkwan University, Suwon, South Korea
Introduction: Non-suicidal self-injury (NSSI) is frequently encountered in patients with mood disorders. Emotion dysregulation (ED), frequently observed in mood disorders, could be a major mediating factor in NSSI. The aim of this study was to explore differences in NSSI behavior and ED across mood disorder subtypes. The relationships between childhood trauma and NSSI and ED were also explored.
Methods: A total of 191 patients with mood disorders were included in this study. The patterns of NSSI behavior and ED across patients with bipolar I disorder (BD-I), bipolar II disorder (BD-II), and major depressive disorder (MDD) were compared.
Results: More than half (54%) of the subjects experienced NSSI. Patients with BD-II and MDD engaged in NSSI behavior more frequently than those diagnosed with BD-I. NSSI behaviors in patients with BD-II most commonly included cutting, whereas hitting behaviors were most common among other groups. Patients with BD-II and MDD reported more severe ED than those with BD-I. In the case of childhood trauma, those with BD-II and MDD reported greater emotional neglect than those with BD-I. Structural equation modeling revealed that ED mediated the association between childhood trauma and NSSI.
Conclusion: BD-I was associated with less frequent NSSI behavior and less severe ED than BD-II and MDD. ED mediated the association between childhood trauma and NSSI. Promoting emotion regulation strategies could prevent NSSI behavior in patients with mood disorders.
Introduction
Non-suicidal self-injury (NSSI) has been defined as the deliberate and self-inflicted destruction of body tissues without suicidal intent (1). The prevalence of NSSI among the clinical samples of adults ranged from 13 to 37% (2–4). Typical NSSI behaviors include cutting, scraping skin, skin-picking, self-hitting and biting, burning, and tying (5, 6). NSSI usually begins in adolescence. It has the highest prevalence during adolescence and early adulthood, but it can manifest at any age (4, 7, 8). Although by definition, NSSI occurs without an intent to commit suicide, it is strongly associated with suicidal thoughts and behaviors (8, 9).
NSSI has received increasing attention over the past several decades (10) with growing evidence suggesting that it is a transdiagnostic symptom commonly associated with psychiatric disorders including mood disorders (11–13). While self-harm is a diagnostic criterion of borderline personality disorder, studies have shown that mood disorders and NSSI frequently co-exist (14, 15). Individuals who engaged in NSSI exhibited elevated levels of anxiety and depression compared to those who did not engage (16, 17). A meta-analysis showed that individuals with mood disorders exhibited more than twice the odds (odds ratio = 2.09) of engaging in NSSI compared to those without such disorders (18).
Emotion dysregulation (ED) is a factor that could mediate the relationship between mood disorders and NSSI behavior (19). ED refers to “an individual's ability to modify an emotional state so as to promote adaptive, goal-oriented behaviors” (20). Therefore, ED refers to the failure to change the reactivity of emotions or the unacceptance and devaluing of emotions (21). ED has been proposed as a critical component in the development and maintenance of mood disorders (19). NSSI is often used to regulate affect to reduce or escape from an aversive or negative affective state (22, 23). It may provide relief from emotional distress (24). Thus, NSSI is often intended to avoid the negative emotional experiences associated with mood disorders.
Previous studies demonstrated the association of mood disorders with NSSI and ED (13, 19). However, little is known about whether the patterns of NSSI behavior and ED differ by mood disorder subtypes such as bipolar disorder (BD) and major depressive disorder (MDD). In addition, differences in NSSI behavior and ED between patients with bipolar I disorder (BD-I) and bipolar II disorder (BD-II) remain unclear. Considering that BD-I, BD-II, and MDD differ clinically in terms of long-term illness trajectory (25–27), they might show different patterns of ED and NSSI behavior.
Childhood trauma is generally accepted as a risk factor for NSSI (28, 29) and mood disorders (30). Some studies have suggested that depression (31) and ED (24, 32) might play a potential role in the association between NSSI and childhood trauma. However, previous studies investigating the relationship between NSSI and childhood trauma mainly targeted adolescents (29). Few studies involved adult clinical samples.
The aim of this study was to determine differences in NSSI patterns and association with ED according to mood disorder subtypes (i.e., BD-I, BD-II, and MDD). The relationship between childhood trauma and NSSI and the possible mediating effects of ED on the relationship were also explored.
Materials and Methods
Study Participants
Study participants were recruited from the psychiatry outpatient clinic of Samsung Medical Center from January 2019 to November 2020. Subjects aged between 18 and 60 years who were diagnosed with BD-I, II, or recurrent MDD were included. Board-certified psychiatrists who had at least one year of research experience evaluated the participants' psychiatric diagnoses using DSM-V criteria. These study participants were clinically stable, i.e., they scored 3 (mildly ill) or lower on the Clinical Global Impression of Severity scale (33) at the time of assessment. Clinical severity was evaluated by the same psychiatrists who made the clinical diagnosis. Based on comprehensive psychiatric evaluations, we only included individuals who could reliably report their symptoms and past histories. All participants were undergoing standard pharmacological treatment, which included mood stabilizers or antidepressants. The other inclusion criterion was the absence of evidence of schizophrenia, organic mental disorder, intellectual disability, and substance or medical illness-induced mood disorders. Patients who could not reliably report their lifetime history were excluded. Information was collected using a checklist of demographic data, as well as psychiatric and medical history. The participants completed self-reported questionnaires related to childhood trauma, emotion regulation, and the lifetime frequency of NSSI. Written informed consent was obtained from all subjects after a complete explanation of the study. This study was approved by the Institutional Review Board (IRB) of Samsung Medical Center (IRB no. 2018-11-019).
Measures
Non-suicidal Self-Injury
NSSI behaviors and functions were assessed using the Korean version of the Inventory of Statements about Self-Injury (ISAS) (5, 34). The first section of the ISAS measures the lifetime frequency of 12 NSSI behaviors including cutting, biting, carving, burning, pinching, pulling hair, severe scratching, banging or hitting self, interfering with wound healing, rubbing skin against a rough surface, sticking self with needles, and swallowing dangerous substances. In this section, the participants are also asked about the frequency of each behavior and the method they most commonly used.
Emotion Dysregulation
The Korean version of Difficulties in Emotion Regulation Scale (DERS) (35, 36) was used to measure ED. This 36-item scale asked the relevance of each item based on a 5-point scale. Difficulties in emotion regulation were assessed using six subscales: impulse control difficulties, lack of emotional awareness, non-acceptance of emotional response, lack of emotional clarity, limited access to emotion regulation strategies, and difficulties engaging in goal-directed behavior. The cumulative scores of the DERS subscales were also calculated.
Childhood Trauma
A childhood history of abuse was assessed retrospectively using the Korean version of the Child Trauma Questionnaire (CTQ) (37, 38). The CTQ is a 28-item self-reported assessment of the severity and frequency of childhood maltreatment, including physical, sexual, and emotional abuse, and physical and emotional neglect. The items were scored using a 5-point Likert scale ranging from 1 (never true) to 5 (very often true). The total score of the CTQ subscales was also calculated.
Statistical Analysis
All statistical analyses were executed using IBM SPSS statistics version 23 (IBM Corp., Armonk, NY, USA) and SAS version 9.4 (SAS Institute Inc, Cary, NC, USA). The Shapiro-Wilk test was used to determine the normality of parametric variables. Variables that were normally distributed with equal variance among groups were compared using the Student's t-test or one-way ANOVA followed by Fisher's LSD post-hoc comparison. Data that were neither normally distributed nor had equal variance were tested using Mann-Whitney's U-test. Categorical variables were compared using the χ2-test.
The relationship between childhood trauma and NSSI and the mediating effect of ED on such relationships were explored via structural equation modeling (SEM) analysis using Markov Chain Monte Carlo (MCMC) with 1000 bootstrap samples in SPSS AMOS. Age and sex variables were included in the model as covariates to control for their potential confounding effects. Model fit was examined using the Comparative Fit Index (CFI), the Root Mean Square Error of Approximation (RMSEA), and the Standardized Root Mean Square Residual (SRMR). The acceptable fit of SEM was defined as CFI values above 0.90, RMSEA values <0.08, and SRMR values less than 0.08 (39, 40).
Results
Patterns of NSSI Behaviors and Emotion Dysregulation in Patients With Mood Disorders
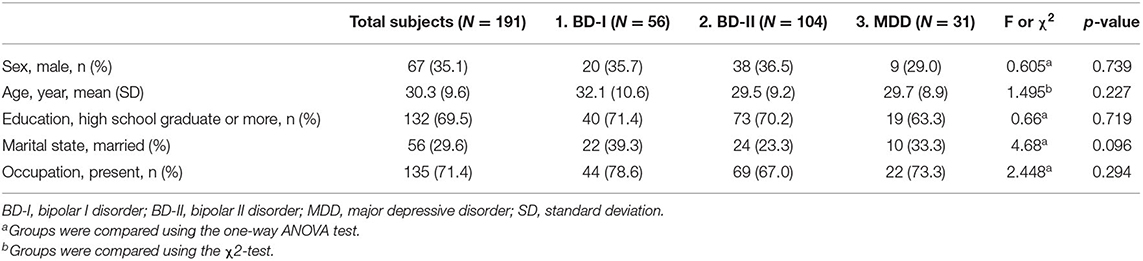
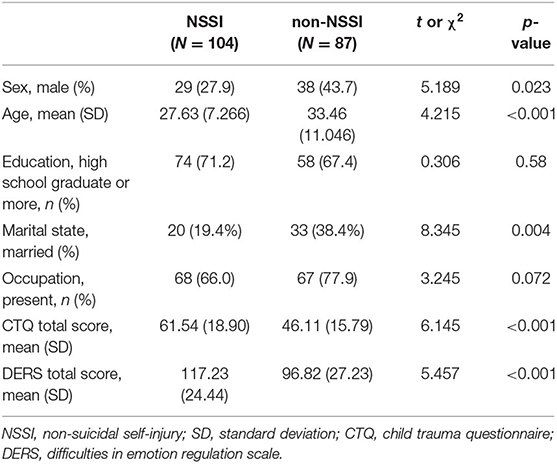
No significant differences in sociodemographic variables including sex and age were found between the diagnostic groups (Table 1). Of all participants, 54% had a lifetime NSSI history (Table 2). When statistically analyzing the proportion of patients who experienced NSSI by diagnosis, patients with BD-I were less likely to engage in NSSI compared to other diagnostic groups (BD-I: 33.9%, BD-II: 64.4%, MDD: 58.1%, χ2 = 13.843, p = 0.001) (Table 2).
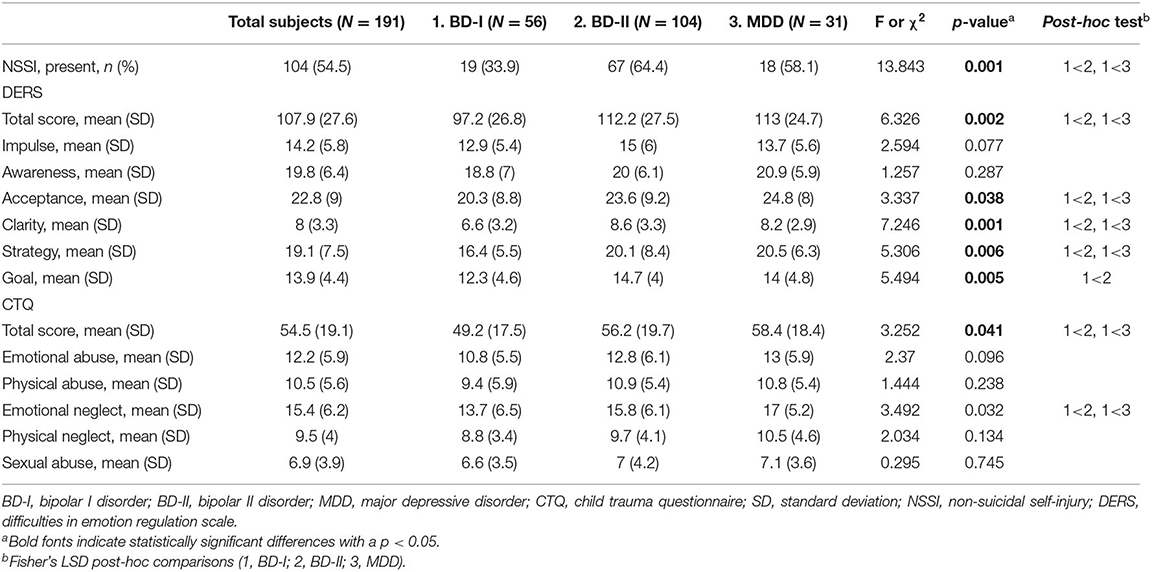
Table 2. Descriptive statistics and differences in NSSI and DERS and CTQ scores between diagnostic groups.
Figure 1 shows the different types of NSSI behavior (ISAS section 1) according to the diagnostic groups. When the methods ever used in their lifetime were queried (multiple responses allowed), “cutting” was the most common method, followed by “banging or hitting self” and “severe scratching” in patients with BD-II. In patients with BD-I or MDD, “banging or hitting self” was the most commonly used self-harm method, followed by “cutting,” “pinching,” and “severe scratching.” “Cutting” was the most commonly used method of self-harm, followed by “banging or hitting self,” “others,” and “interfering with wound healing” in patients with BD-II. However, “banging or hitting self” was the mainly used self-harm method in patients with BD-I and MDD (Supplementary Table 1).
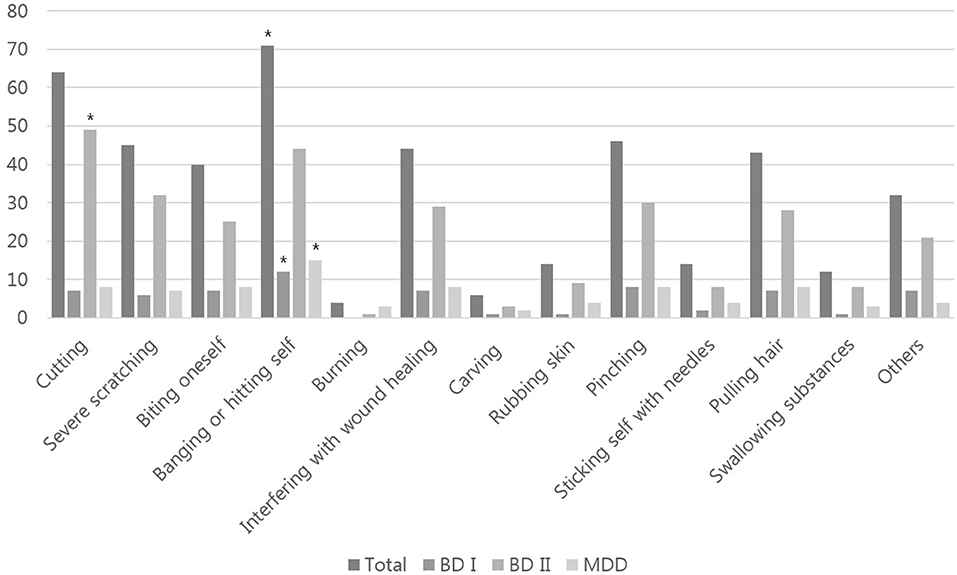
Figure 1. Types of NSSI behavior based on diagnostic group (multiple responses were allowed). BD-I, bipolar I disorder; BD-II, bipolar II disorder; MDD, major depressive disorder. Asterisk indicates the most commonly used self-injury method by the diagnostic group.
Statistically significant differences between the diagnostic groups were detected in total DERS scores. The BD-I group reported lower DERS total scores, indicating less severe ED compared to the other diagnostic groups (F = 6.326, p = 0.002) (Table 2). This overall pattern was repeated for the DERS subscales except for impulse control difficulties and the lack of emotional awareness subscales. Patients with BD-I also reported a lower CTQ total score, indicating less severe overall childhood trauma experience compared to the other groups (CTQ total score: F = 3.252, p = 0.041). In sub-score analyses, the BD-I group scored significantly lower on the emotional neglect subscale than the other groups (F = 3.492, p = 0.032).
Comparison Between Patients With and Without a Lifetime History of NSSI
Table 3 shows differences in the variables based on NSSI experience. A significantly greater proportion of females than males reported engaging in NSSI (χ2 = 5.189, p = 0.023). The NSSI group was younger (z = −3.659, p < 0.001) and more frequently unmarried (χ2 = 8.345, p = 0.004). Participants with and without NSSI did not differ in educational level or occupational status. As for the clinical variables, the NSSI group reported significantly higher levels of childhood traumatic experience (t = −6.145, p < 0.001) and difficulties in emotion regulation (t = −5.457, p < 0.001).
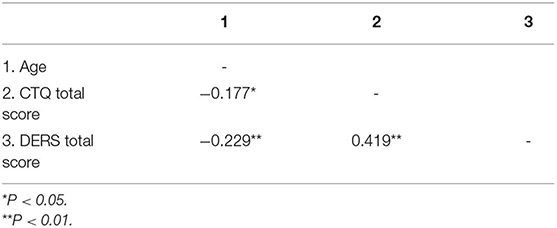
Structural Equation Modeling Analysis
Table 4 presents the correlation of age with the total CTQ and DERS scores. Since age is known to be related to DERS scores, it was included in the correlation analysis. The rate of childhood trauma and severity of emotion dysregulation showed a significant positive correlation (r2 = 0.419, p < 0.001). Age was negatively correlated with ED (r2 = −0.229, p = 0.001) and childhood trauma (r2 = −0.177, p = 0.014). Figure 2 presents a conceptual model of the relationship between childhood trauma and ED and NSSI. Age and sex were included in the model as covariates to control for its potential confounding effect. The results showed that all paths were statistically significant. The model explained 36.4% of the NSSI of patients with mood disorders (total effect coefficient = 0.437). An increased incidence of childhood trauma directly predicted increased levels of NSSI (coefficient = 0.3286, 95% confidence interval (CI): 0.1629–0.4832). Childhood trauma was related to ED (coefficient = 0.4204, 95% CI: 0.2959–0.5334), which in turn, was significantly predictive of NSSI (coefficient = 0.2582, 95% CI: 0.0829–0.4256). Mediation analysis revealed that ED mediated the relationship between childhood trauma and NSSI (standardized indirect effect coefficient = 0.1086, 95% CI: 0.0332–0.1919; standardized total effect coefficient = 0.4372, 95% CI: 0.2857–0.5742). The model fit including all diagnostic groups was as follows: CFI = 0.943, RMSAEA = 0.103 (90% CI:0.029–0.183), SRMR = 0.045. The SEM results and fitness in each diagnostic group are presented in Supplementary Figure 1.
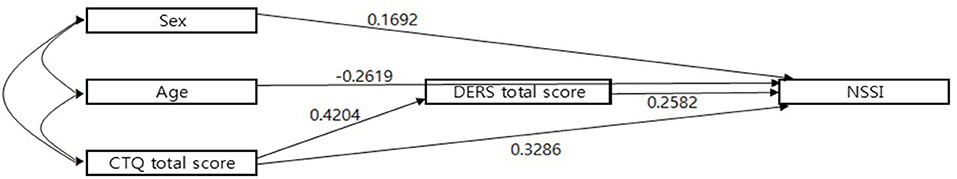
Figure 2. A conceptual model of the relationship between childhood trauma and emotion dysregulation (ED) and NSSI using standardized beta coefficients. Age and sex variables were included in the model as covariates. All paths were statistically significant. CTQ, child trauma questionnaire; DERS, Difficulties in Emotion regulation scale; NSSI, non-suicidal self-injury.
Discussion
NSSI is a widespread phenomenon without diagnostic boundaries. However, previous studies did not explore the differences across mood disorder subgroups. The current study investigated NSSI and ED patterns among patients with BD-I, BD-II, and MDD. We additionally analyzed the association of NSSI and ED with childhood trauma in patients with mood disorders.
Approximately 54% of the participants in our study reported a lifetime history of NSSI. The rate of NSSI in our study was comparable to that of a previous study (13). A previous study involving patients seeking treatment at a general practice clinic in the United States (U.S.) reported a higher prevalence of NSSI in patients with mood disorders than in those with other psychiatric disorders (43 vs. 20%, respectively) (13). The prevalence of NSSI was especially high in subjects with bipolar disorder (up to 52%) (13).
This was the first study that compared the rates and patterns of NSSI in patients with BD-I, BD-II, and MDD. Notably, patients with BD-I showed substantially lower rates of lifetime NSSI behavior than the other groups. The rate of lifetime NSSI behavior was the highest in the BD-II group. Previous studies evaluating the rate of NSSI behavior in patients with psychiatric diagnoses reported mixed results regarding NSSI rates in patients with BD (18, 41). The contrasting results of NSSI frequency between BD-I and BD-II patients might have contributed to the mixed results. The patterns of NSSI behavior also differed among the three groups. Patients diagnosed with BD-II manifested cutting as the most common method of NSSI, which is potentially associated with a high degree of tissue damage compared to the other methods.
Consistent with the higher rate of NSSI behavior in patients with BD-II and MDD, difficulties in ED were more severe in those groups. BD-II was associated with profound ED, similar to MDD, rather than BD-I. A meta-analysis revealed that ED was common in patients with BD, but the differences in ED between patients with BD-I and BD-II were not clear (42). A single study reported the absence of differences in DERS scores between patients with BD-I and BD-II (43). However, the small sample size affected the results. Previous studies reported significant ED in patients with mood disorders compared to the general population, which was pervasive across diverse mood states including manic, depressive, and euthymic conditions (44, 45). In particular, mood dysregulation is more severe in BD-II than in BD-I (46, 47), which corroborates our study findings. Decreased ED correlated with a decrease in depression and anxiety (42), suggesting an association between negative affect and persistent ED. Depressive episodes are known to be more frequent in patients with BD-II than BD-I (27). The more frequent depressive episodes and mood swings observed in patients with BD-II often resemble severe ED found in borderline personality disorder (48, 49). A neuroimaging study also suggested differences in mood regulation circuitry between patients with BD-I and BD-II (50).
Consistent with the significant differences in total DERS scores, patients with BD-I showed better emotion regulation than those manifesting BD-II and MDD on all subscales of the DERS, and the difference reached a significant level in four domains (non-acceptance of emotion response, lack of emotional clarity, limited access to emotion regulation strategies, and difficulties engaging in goal-directed behavior). In contrast to our study, no previous studies analyzed the differences in DERS subscales between mood disorder subtypes. In a previous meta-analysis, subjects with BD showed significantly higher DERS subscale scores except for the awareness subscale score compared to healthy controls (42). Compared to borderline personality disorder, BD was associated with significantly lower scores on all the DERS subscales. A previous study investigating the latency profiles of DERS reported that the awareness subscale did not correlate with other subscale scores (51). Understanding the ED profiles across mood disorder subtypes will facilitate treatment strategies for these populations. Further studies are needed to confirm the study findings.
Although NSSI implies non-suicidal intent, it is associated with an increased risk of suicidal attempts (8, 9). The higher the rate of NSSI behavior, the more frequent the use of methods with the potential for a high degree of tissue damage, and greater ED in patients with BD-II might contribute to the increased suicide risk in patients with BD-II. A recent clinical study with the largest-ever sample size (52) and a meta-analysis (53) confirmed the higher prevalence of suicide attempts in patients with BD-II. In a recent prospective study of patients diagnosed with BD and MDD (54, 55), suicide attempts were more frequently observed in patients with BD than in those with MDD mainly because of the higher duration of high-risk illness, i.e., more frequent depressive episodes. Subjects in the MDD group in our study showed NSSI rates comparable to those in the BD-II group, reinforcing the association between NSSI behavior and recurrent depression.
In our study, the CTQ scores were also higher in patients with BD-II and MDD than in patients with BD-I. However, in the sub-scale analyses, such differences were significant only for the emotional neglect subscale. Emotional neglect is arguably the most subjective and difficult to define among the forms of abuse (56). A prior study reported no differences in the rate of childhood traumatic experience of patients with BD-I and BD-II (57). Further studies are needed to confirm our findings.
In accordance with previous studies (8, 58), the NSSI group was younger and included proportionately higher numbers of females than the non-NSSI group. The CTQ and DERS scores differed depending upon the diagnosis, with NSSI being more prevalent in the group with higher CTQ and DERS scores. These results support the mediating role of ED on the association between childhood trauma and NSSI. As hypothesized, the SEM results revealed that ED mediated the relationship between childhood trauma and NSSI. When evaluating the model fit using total subjects including all diagnostic groups, a single indicator was not acceptable (RMSAEA), probably due to heterogeneity between the diagnostic groups. Subgroup analyses showed a better fit except for the BD-II group for unknown reasons. Diagnostic characteristics may also affect the model fit. The correlation between CT and NSSI has been confirmed in studies enrolling various subjects as well as clinical samples (29). A single study explored the mediating role of ED in the relationship between CT and NSSI, although it involved adolescent inpatients (59). A study of adult clinical samples has yet to be reported. The current study further emphasized the importance of ED as a mediating factor by limiting the patient group to those with mood disorders. ED is a major independent risk factor for NSSI (21, 60). The functional aspects of ED in NSSI have been studied, especially in terms of behavioral theory. Based on the behavioral model, the positive reinforcement function (e.g., to feel something) and negative reinforcement function (e.g., to relieve depression or uncomfortable internal experiences) of NSSI might be relevant to individuals with ED (22, 61). In this respect, individuals who experience negative emotions may use NSSI as a coping strategy. A group skills training program in dialectical behavior therapy is one possible treatment option that appears to be effective in decreasing emotional reactivity and improving psychological wellbeing in patients with bipolar disorder (62). A further study is needed to identify better strategies to decrease ED and NSSI in patients with mood disorders.
This study had several limitations. First, all measures were evaluated using self-reported questionnaires. In particular, the retrospective study may be associated with recall bias. However, a previous study showed that recall bias accounted for <1% of the reported variance in measures of childhood abuse (63). Second, since the data included patients with mood disorders only, it was not clear if the current study results apply only to mood disorders or the findings could be generalized to other clinical samples. Third, this study was performed as a cross-sectional and single-center study of patients who were treated in a single hospital. Therefore, prospective and multicenter studies are needed before the results can be generalized. Fourth, SEM showed that childhood trauma and ED only explained part of the mechanism of NSSI. Further studies that include diverse factors that contribute to the development of NSSI are needed.
Conclusions
In conclusion, NSSI is common across diverse mood disorders subtypes. Patients with BD-I had the lowest prevalence of NSSI and significantly less ED compared to those diagnosed with BD-II and MDD. The association between NSSI and childhood trauma was also mediated by ED. Thus, it could be beneficial to promote emotional coping skills in patients with mood disorders and a history of childhood trauma to prevent NSSI.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Review Board (IRB) of Samsung Medical Center. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JB designed the study and wrote the protocol. JB and KH obtained the funding. DL, YC, and JA collected and managed the data. SY managed the literature searches and analyses. SY, DL, and HJ performed the statistical analysis, and SY and JB wrote the first draft of the manuscript. All authors contributed to the final manuscript and have approved it.
Funding
This work was supported by the Korea Medical Device Development Fund grant funded by the Korean government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health & Welfare, and the Ministry of Food and Drug Safety) [Project Numbers NTIS 9991006915 and KMDF_PR_20200901_0250] and the Original Technology Research Program for Brain Science through the National Research Foundation of Korea (NRF) funded by the Ministry of Science and ICT [No. 2019M3C7A1030624].
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.757933/full#supplementary-material
Supplementary Figure 1. A conceptual model of the relationship between childhood trauma and emotion dysregulation and NSSI in each diagnostic group. Age and sex were included in the model as covariates. Statistically significant paths are indicated with an asterisk (*). The BD-I and MDD models showed acceptable fit (CFI = 1.000, RMSAEA = 0.000 (90% CI: 0.000–0.169), with SRMR = 0.024 and CFI = 1.000, RMSAEA 0.000 (90% CI: 0.000–0.329) and SRMR = 0.053, respectively). The BD-II model showed poor fit (CFI = 0.850, RMSAEA = 0.213 (90% CI: 0.105–0.340), SRMR = 0.079). CTQ, child trauma questionnaire; DERS, difficulties in emotion regulation scale; NSSI, non-suicidal self-injury; BD-I, bipolar I disorder; BD-II, bipolar II disorder; MDD, major depressive disorder; CFI, comparative fit index; RMSEA, root-mean-square error of approximation; SRMR, standardized root-mean-square residual.
Supplementary Table 1. Main form of individual's NSSI behaviors by diagnotic groups.
References
1. Klonsky ED, Muehlenkamp JJ. Self-injury: a research review for the practitioner. J Clin Psychol. (2007) 63:1045–56. doi: 10.1002/jclp.20412
2. Briere J, Gil E. Self-mutilation in clinical and general population samples: prevalence, correlates, and functions. Am J Orthopsychiatry. (1998) 68:609–20. doi: 10.1037/h0080369
3. Esposito-Smythers C, Goldstein T, Birmaher B, Goldstein B, Hunt J, Ryan N, et al. Clinical and psychosocial correlates of non-suicidal self-injury within a sample of children and adolescents with bipolar disorder. J Affect Disord. (2010) 125:89–97. doi: 10.1016/j.jad.2009.12.029
4. Bae Y, Seong Y, Kim SH, Kim S. Clinical characteristics of non-suicidal self-injury and suicide attempts among psychiatric patients in Korea: a retrospective chart review. Psychiatry Investig. (2020) 17:320. doi: 10.30773/pi.2019.0269
5. Klonsky ED, Glenn CR. Assessing the functions of non-suicidal self-injury: Psychometric properties of the Inventory of Statements About Self-injury (ISAS). J Psychopathol Behav Assess. (2009) 31:215–9. doi: 10.1007/s10862-008-9107-z
6. Andover MS, Primack JM, Gibb BE, Pepper CM. An examination of non-suicidal self-injury in men: do men differ from women in basic NSSI characteristics? Arch Suicide Res. (2010) 14:79–88. doi: 10.1080/13811110903479086
7. Klonsky ED. Non-suicidal self-injury in United States adults: prevalence, sociodemographics, topography and functions. Psychol Med. (2011) 41:1981. doi: 10.1017/S0033291710002497
8. Ose SO, Tveit T, Mehlum L. Non-suicidal self-injury (NSSI) in adult psychiatric outpatients–a nationwide study. J Psychiatr Res. (2021) 133:1–9. doi: 10.1016/j.jpsychires.2020.11.031
9. Ribeiro J, Franklin J, Fox KR, Bentley K, Kleiman EM, Chang B, et al. Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. Psychol Med. (2016) 46:225–36. doi: 10.1017/S0033291715001804
10. Nock MK. Self-injury. Ann Rev Clin Psychol. (2010) 6:339–63. doi: 10.1146/annurev.clinpsy.121208.131258
11. Jacobson CM, Gould M. The epidemiology and phenomenology of non-suicidal self-injurious behavior among adolescents: A critical review of the literature. Arch Suicide Res. (2007) 11:129–47. doi: 10.1080/13811110701247602
12. Wilkinson P, Goodyer I. Non-suicidal self-injury. Eur Child Adolesc Psychiatry. (2011) 20:103–8. doi: 10.1007/s00787-010-0156-y
13. Selby EA, Bender TW, Gordon KH, Nock MK, Joiner Jr TE. Non-suicidal self-injury (NSSI) disorder: a preliminary study. Personal Disord. (2012) 3:167. doi: 10.1037/a0024405
14. Klonsky ED, Oltmanns TF, Turkheimer E. Deliberate self-harm in a nonclinical population: prevalence and psychological correlates. Am J Psychiatry. (2003) 160:1501–8. doi: 10.1176/appi.ajp.160.8.1501
15. Jacobson CM, Muehlenkamp JJ, Miller AL, Turner JB. Psychiatric impairment among adolescents engaging in different types of deliberate self-harm. J Clin Child Adolesc Psychol. (2008) 37:363–75. doi: 10.1080/15374410801955771
16. Andover MS, Pepper CM, Ryabchenko KA, Orrico EG, Gibb BE. Self-mutilation and symptoms of depression, anxiety, and borderline personality disorder. Suicide Life Threat Behav. (2005) 35:581–91. doi: 10.1521/suli.2005.35.5.581
17. Prinstein MJ, Heilbron N, Guerry JD, Franklin JC, Rancourt D, Simon V, et al. Peer influence and nonsuicidal self injury: Longitudinal results in community and clinically-referred adolescent samples. J Abnorm Child Psychol. (2010) 38:669–82. doi: 10.1007/s10802-010-9423-0
18. Bentley KH, Cassiello-Robbins CF, Vittorio L, Sauer-Zavala S, Barlow DH. The association between nonsuicidal self-injury and the emotional disorders: a meta-analytic review. Clin Psychol Rev. (2015) 37:72–88. doi: 10.1016/j.cpr.2015.02.006
19. Hofmann SG, Sawyer AT, Fang A, Asnaani A. Emotion dysregulation model of mood and anxiety disorders. Depress Anxiety. (2012) 29:409–16. doi: 10.1002/da.21888
20. Thompson RA. Emotion regulation: a theme in search of definition. Monogr Soc Res Child Dev. (1994) 59:25–52. doi: 10.1111/j.1540-5834.1994.tb01276.x
21. You J, Ren Y, Zhang X, Wu Z, Xu S, Lin MP. Emotional dysregulation and nonsuicidal self-injury: a meta-analytic review. Neuropsychiatry. (2018) 8:733–48. doi: 10.4172/Neuropsychiatry.1000399
22. Nock MK, Prinstein MJ. A functional approach to the assessment of self-mutilative behavior. J Consult Clin Psychol. (2004) 72:885. doi: 10.1037/0022-006X.72.5.885
23. Klonsky ED. The functions of deliberate self-injury: a review of the evidence. Clin Psychol Rev. (2007) 27:226–39. doi: 10.1016/j.cpr.2006.08.002
24. Ford JD, Gómez JM. The relationship of psychological trauma and dissociative and posttraumatic stress disorders to nonsuicidal self-injury and suicidality: a review. J Trauma Dissociation. (2015) 16:232–71. doi: 10.1080/15299732.2015.989563
25. Judd LL. The clinical course of unipolar major depressive disorders. Arch Gen Psychiatry. (1997) 54:989–91. doi: 10.1001/archpsyc.1997.01830230015002
26. Judd LL, Akiskal HS, Schettler PJ, Coryell W, Maser J, Rice JA, et al. The comparative clinical phenotype and long term longitudinal episode course of bipolar I and II: a clinical spectrum or distinct disorders? J Affect Disord. (2003) 73:19–32. doi: 10.1016/S0165-0327(02)00324-5
27. Baek JH, Park DY, Choi J, Kim JS, Choi JS, Ha K, et al. Differences between bipolar I and bipolar II disorders in clinical features, comorbidity, and family history. J Affect Disord. (2011) 131:59–67. doi: 10.1016/j.jad.2010.11.020
28. Brodsky BS, Stanley B. Adverse childhood experiences and suicidal behavior. Psychiatr Clin North Am. (2008) 31:223–35. doi: 10.1016/j.psc.2008.02.002
29. Serafini G, Canepa G, Adavastro G, Nebbia J, Belvederi Murri M, Erbuto D, et al. The relationship between childhood maltreatment and non-suicidal self-injury: a systematic review. Front Psychiatry. (2017) 8:149. doi: 10.3389/fpsyt.2017.00149
30. Nelson J, Klumparendt A, Doebler P, Ehring T. Childhood maltreatment and characteristics of adult depression: meta-analysis. Br J Psychiatry. (2017) 210:96–104. doi: 10.1192/bjp.bp.115.180752
31. Cicchetti D, Toth SL. Child maltreatment. Annu Rev Clin Psychol. (2005) 1:409–38. doi: 10.1146/annurev.clinpsy.1.102803.144029
32. Shipman K, Zeman J, Penza S, Champion K. Emotion management skills in sexually maltreated and nonmaltreated girls: a developmental psychopathology perspective. Dev Psychopathol. (2000) 12:47–62. doi: 10.1017/S0954579400001036
33. Guy W. ECDEU Assessment Manual for Psychopharmacology. Rockville, MD: US Department of Health, Education, and Welfare Public Health Service Alcohol, Drug Abuse, and Mental Health Administration (1976).
34. Kim S, Kim Y, Hur JW. Nonsuicidal self-injury among Korean young adults: a validation of the Korean version of the inventory of statements about self-injury. Psychiatry investig. (2019) 16:270. doi: 10.30773/pi.2019.01.23
35. Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. (2004) 26:41–54. doi: 10.1023/B:JOBA.0000007455.08539.94
36. Cho, Y. r. Assessing emotion dysregulation: Psychometric properties of the Korean version of the difficulties in emotion regulation scale. Korean J Clin Psychol. (2007) 26:1015–38. doi: 10.15842/kjcp.2007.26.4.012
37. Bernstein DP, Fink L. Childhood Trauma Questionnaire: A Retrospective Self-Report Manual. San Antonio, TX: The Psychological Corporation (1998).
38. Yu J, Park J, Park D, Ryu S, Ha J. Validation of the Korean Childhood Trauma Questionnaire: the practical use in counselling and therapeutic intervention. Korean J Health Psychol. (2009) 14:563–78. doi: 10.17315/kjhp.2009.14.3.006
39. Mueller R, Hancock G. Best practices in structural equation modeling. In: Osborne J, editor. Best Practices in Quantitative Methods. SAGE Publications, Inc (2008). p. 488–508. doi: 10.4135/9781412995627
41. Kiekens G, Hasking P, Claes L, Mortier P, Auerbach RP, Boyes M, et al. The DSM-5 nonsuicidal self-injury disorder among incoming college students: prevalence and associations with 12-month mental disorders and suicidal thoughts and behaviors. Depress Anxiety. (2018) 35:629–37. doi: 10.1002/da.22754
42. Sloan E, Hall K, Moulding R, Bryce S, Mildred H, Staiger PK. Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders: a systematic review. Clin Psychol Rev. (2017) 57:141–63. doi: 10.1016/j.cpr.2017.09.002
43. Grant M, Salsman NL, Berking M. The assessment of successful emotion regulation skills use: development and validation of an english version of the emotion regulation skills questionnaire. PLoS ONE. (2018) 13:e0205095. doi: 10.1371/journal.pone.0205095
44. Becerra R, Cruise K, Murray G, Bassett D, Harms C, Allan A, et al. Emotion regulation in bipolar disorder: are emotion regulation abilities less compromised in euthymic bipolar disorder than unipolar depressive or anxiety disorders?. Open J Psychiatry. (2013) 3:1–7. doi: 10.4236/ojpsych.2013.34A001
45. Musket CW, Hansen NS, Welker KM, Gilbert KE, Gruber J. A pilot investigation of emotional regulation difficulties and mindfulness-based strategies in manic and remitted bipolar I disorder and major depressive disorder. Int J Bipolar Disorders. (2021) 9:1–8. doi: 10.1186/s40345-020-00206-0
46. Green E, Toma S, Collins J, Fiksenbaum L, Timmins V, Omrin D, et al. Similarities and differences across bipolar disorder subtypes among adolescents. J Child Adolesc Psychopharmacol. (2020) 30:215–21. doi: 10.1089/cap.2019.0031
47. Akiskal HS, Kilzieh N, Maser JD, Clayton PJ, Schettler PJ, Traci Shea M, et al. The distinct temperament profiles of bipolar I, bipolar II and unipolar patients. J Affect Disord. (2006) 92:19–33. doi: 10.1016/j.jad.2005.12.033
48. Parker G. Clinical differentiation of bipolar II disorder from personality-based “emotional dysregulation” conditions. J Affect Disord. (2011) 133:16–21. doi: 10.1016/j.jad.2010.10.015
49. Fletcher K, Parker G, Bayes A, Paterson A, McClure G. Emotion regulation strategies in bipolar II disorder and borderline personality disorder: differences and relationships with perceived parental style. J Affect Disord. (2014) 157:52–9. doi: 10.1016/j.jad.2014.01.001
50. Caseras X, Murphy K, Lawrence NS, Fuentes-Claramonte P, Watts J, Jones DK, et al. Emotion regulation deficits in euthymic bipolar I versus bipolar II disorder: a functional and diffusion-tensor imaging study. Bipolar Disord. (2015) 17:461–70. doi: 10.1111/bdi.12292
51. Rufino KA, Ellis TE, Clapp J, Pearte C, Fowler JC. Variations of emotion dysregulation in borderline personality disorder: a latent profile analysis approach with adult psychiatric inpatients. Borderline Personal Disord Emot Dysregul. (2017) 4:17. doi: 10.1186/s40479-017-0068-2
52. Karanti A, Kardell M, Joas E, Runeson B, Pålsson E, Landén M. Characteristics of bipolar I and II disorder: a study of 8766 individuals. Bipolar Disord. (2020) 22:392–400. doi: 10.1111/bdi.12867
53. Plans L, Barrot C, Nieto E, Rios J, Schulze T, Papiol S, et al. Association between completed suicide and bipolar disorder: a systematic review of the literature. J Affect Disord. (2019) 242:111–22. doi: 10.1016/j.jad.2018.08.054
54. Holma KM, Haukka J, Suominen K, Valtonen HM, Mantere O, Melartin TK, et al. Differences in incidence of suicide attempts between bipolar I and II disorders and major depressive disorder. Bipolar Disord. (2014) 16:652–61. doi: 10.1111/bdi.12195
55. Pallaskorpi S, Suominen K, Ketokivi M, Valtonen H, Arvilommi P, Mantere O, et al. Incidence and predictors of suicide attempts in bipolar I and II disorders: a 5-year follow-up study. Bipolar Disord. (2017) 19:13–22. doi: 10.1111/bdi.12464
56. Watson S, Gallagher P, Dougall D, Porter R, Moncrieff J, Ferrier IN, et al. Childhood trauma in bipolar disorder. Aust N Z J Psychiatry. (2014) 48:564–70. doi: 10.1177/0004867413516681
57. Janiri D, Sani G, Danese E, Simonetti A, Ambrosi E, Angeletti G, et al. Childhood traumatic experiences of patients with bipolar disorder type I and type II. J Affect Disorders. (2015) 175:92–7. doi: 10.1016/j.jad.2014.12.055
58. Weintraub MJ, Van de Loo MM, Gitlin MJ, Miklowitz DJ. Self-harm, affective traits, and psychosocial functioning in adults with depressive and bipolar disorders. J Nerv Ment Dis. (2017) 205:896. doi: 10.1097/NMD.0000000000000744
59. Titelius EN, Cook E, Spas J, Orchowski L, Kivisto K, O'Brien K, et al. Emotion dysregulation mediates the relationship between child maltreatment and non-suicidal self-injury. J Aggress Maltreat Trauma. (2018) 27:323–31. doi: 10.1080/10926771.2017.1338814
60. Messer JM, Fremouw WJ. A critical review of explanatory models for self-mutilating behaviors in adolescents. Clin Psychol Rev. (2008) 28:162–78. doi: 10.1016/j.cpr.2007.04.006
61. Chapman AL, Gratz KL, Brown MZ. Solving the puzzle of deliberate self-harm: The experiential avoidance model. Behav Res Ther. (2006) 44:371–94. doi: 10.1016/j.brat.2005.03.005
62. Eisner L, Eddie D, Harley R, Jacobo M, Nierenberg AA, Deckersbach T. Dialectical behavior therapy group skills training for bipolar disorder. Behav Ther. (2017) 48:557–66. doi: 10.1016/j.beth.2016.12.006
Keywords: mood disorders, non-suicidal self-injury (NSSI), emotional dysregulation, bipolar II disorder (BD-II), childhood trauma
Citation: Yang SY, Lee D, Jeong H, Cho Y, Ahn JE, Hong KS and Baek JH (2022) Comparison of Patterns of Non-suicidal Self-Injury and Emotion Dysregulation Across Mood Disorder Subtypes. Front. Psychiatry 13:757933. doi: 10.3389/fpsyt.2022.757933
Received: 13 August 2021; Accepted: 19 April 2022;
Published: 12 May 2022.
Edited by:
Marco Grados, Johns Hopkins Medicine, United StatesReviewed by:
Julieta Azevedo, University of Coimbra, PortugalJi Sun Kim, Soon Chun Hyang University Cheonan Hospital, South Korea
Copyright © 2022 Yang, Lee, Jeong, Cho, Ahn, Hong and Baek. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ji Hyun Baek, amloeXVuYmFla0Bza2t1LmVkdQ==
 So Yung Yang1,2
So Yung Yang1,2 Dongbin Lee
Dongbin Lee Ji Hyun Baek
Ji Hyun Baek