- 1Department of Psychiatry and Psychotherapy, Carl Gustav Carus University Hospital, Technische Universität Dresden, Dresden, Germany
- 2Department of Addiction Medicine and Psychotherapy, Kbo-Isar-Amper-Klinikum München-Ost, Haar, Germany
- 3Department of Psychiatry and Psychotherapy, Elblandklinikum Radebeul, Radebeul, Germany
Background: Integrated care is a promising model for pregnant and parenting women with problems related to methamphetamine use. Yet more research is imperative to guide services for this vulnerable population as methamphetamine use contributes to housing instability, which is associated with heavier use and overdose death.
Method: This prospective observational study analyzed how housing at discharge from psychiatric care was related to patient characteristics, program participation, and aftercare in 102 pregnant and/or parenting women.
Results: Twelve of 23 women who were unstably housed at admission (three of six homeless) achieved stable housing by discharge from integrated care. Women were more likely unstably housed at discharge when unstably housed at admission, single, living apart from at least one minor, or when the other parent had a substance use disorder (p < 0.05). Unstably housed women at discharge were also more likely to have used social and inpatient services, and to transition to inpatient rehabilitation (p < 0.05). Among baseline characteristics, logistic regression identified unstable housing at admission (OR = 6.07) and being single (OR = 4.01) as the strongest unique contributors to unstable housing at discharge (p < 0.05).
Conclusion: Unstably housed women and single women seem particularly at risk of remaining in precarious living conditions despite accessing integrated care for problems associated with methamphetamine use. Future work should investigate whether stronger partnerships with government and community agencies could be a way forward to help these women attain and maintain stable housing.
Introduction
Global methamphetamine markets continue expanding while methamphetamine use has reached epidemic proportions in many parts of the world (1–3). This escalation threatens public health due to the related morbidity, mortality, and criminality (1–3). Methamphetamine use and unintended pregnancies can have detrimental consequences for women and their offspring, such as eclampsia and death (4–8). Newborns with prenatal methamphetamine exposure are at risk for withdrawal symptoms and developmental deficits, which include reduced weight, size, and head circumference (5–8). These children also exhibit more problems in later life, such as signs of attention-deficit hyperactivity disorder at school age (5–7). Pregnant and parenting women who use methamphetamine often struggle with polysubstance use, mental illness, socioeconomic deprivation, and single parenting (8–11). Compared with parents using other substances, parents using methamphetamine are more likely female, unemployed, not in a committed relationship, and without custody of their children (12). Moreover, parenting stress is even higher in methamphetamine-using mothers than fathers (13, 14). Despite the need for prevention and intervention, methamphetamine-using women experience limited pregnancy, pediatric, and mental healthcare (6, 8, 10, 11, 15). Barriers concern the awareness of services and care needs, availability, affordability, logistics, and legal implications regarding substance use and childcare (16, 17). Access is additionally hampered by stigmatizing attitudes toward methamphetamine use, substance use in pregnancy, socioeconomic adversity, and legal system involvement (16, 17). This accumulation of biopsychosocial stressors can fuel a vicious cycle of poor maternal and child health, substance use, adversity, and marginalization (6, 9, 18).
The concept “Mama denk an mich” (Mamadam, “Mommy think of me”) was developed to break this cycle by providing low-barrier care across disciplines and settings. Case management and coordination meetings integrate the Psychiatric, Obstetric, and Pediatric Departments at the Dresden University Hospital with child welfare and community substance use services. Care is mainly provided on an outpatient basis to promote psychosocial functioning and well-being in daily life.
Psychiatric care draws on the available evidence and best practice for the management of methamphetamine-related disorders (19). Patients consult with a psychiatrist and/or psychotherapist from several times a week to once a month as needed. Mamadam provides women-only group psychotherapy based on a manual that combines methamphetamine-specific psychoeducation, motivational interviewing, and cognitive behavior therapy (20–23). Hospital social workers partner with community and government agencies to aid patients in finances, work, and housing. Childcare is supported by establishing a crisis plan in case of relapse and by in-home assistance if needed. Supervised random substance screening is employed to promote treatment engagement. Inpatient care is also available, which provides additional group therapies, such as exercise classes, progressive muscle relaxation, occupational therapy, social skills training, and specific therapies for psychiatric comorbidities.
Previous studies described the Mamadam concept in detail and added to the evidence that pregnancy and parenthood provide opportunities to motivate change (13, 19, 24), thereby decreasing substance use and child removal (15, 25–27). Patients could be engaged in outpatient psychiatric treatment over months, but more research is imperative to evaluate and optimize care strategies. Studying housing instability is insightful as it may not only be a consequence (28, 29) but also a cause of substance use and even overdose death (30, 31). Moreover, meeting the basic need for stable housing is essential for effective social and professional reintegration. We thus investigated how housing at discharge from Mamadam was related to health and life circumstances at admission as well as healthcare utilization before, during, and after Mamadam. The goal was to gather information on what interventions may be beneficial and how best to integrate them to prevent and mitigate harms related to methamphetamine and other substance use during pregnancy and parenthood. These findings should inform care initiatives that are urgently needed to counter the impact of the global methamphetamine crisis on women and children.
Methods
This prospective observational study aimed to identify baseline and treatment correlates of housing in pregnant and parenting women with methamphetamine use disorder according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. We studied all 102 women who accessed psychiatric care within Mamadam since its start in 2016 and left or completed treatment before July 30, 2020. This naturalistic sample included the 73 women whose treatment adherence was previously analyzed (27). Adherence was categorized as early discontinuation (before implementing a care plan), partial completion of the program (late discontinuation), or successful completion (requiring stable abstinence).
Statistics were performed in SPSS 27 (IBM, Armonk, NY, USA), using two-sided tests, a significance level of 0.05, and data on all patients unless stated otherwise. We categorized women depending on whether they had control over their living arrangements at discharge as stably (own apartment, condominium, house) or unstably housed (supported transitional accommodation with children, living in others' homes, homeless). They were compared on baseline characteristics, Mamadam participation, and aftercare. Pearson's chi-square test (or Fisher's exact test when cell sizes were too small) and Bonferroni-adjusted pairwise comparisons were applied for categorical variables. We used Mann-Whitney U tests as histograms, normal quantile-quantile plots, and tests of normality demonstrated that continuous data were not normally distributed.
We quantified associations between variables that differed significantly between groups with the phi coefficient. To identify the variables with the strongest unique contributions to housing at discharge, we built one model with baseline and another with treatment variables. All variables that had complete data and met the assumptions of logistic regression were considered for forward stepwise selection using the likelihood ratio. Significant variables from these models were entered in a third model to discriminate how much variability of housing stability at discharge was explained by each variable when controlling for the others.
Results
Study Sample and Care Utilization
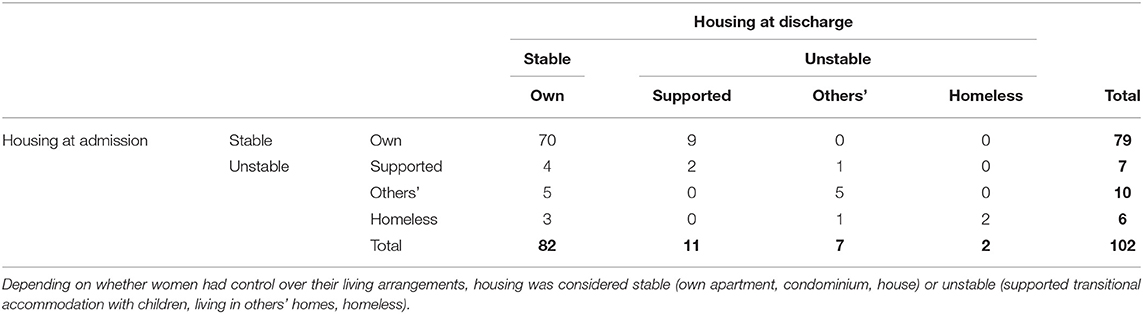
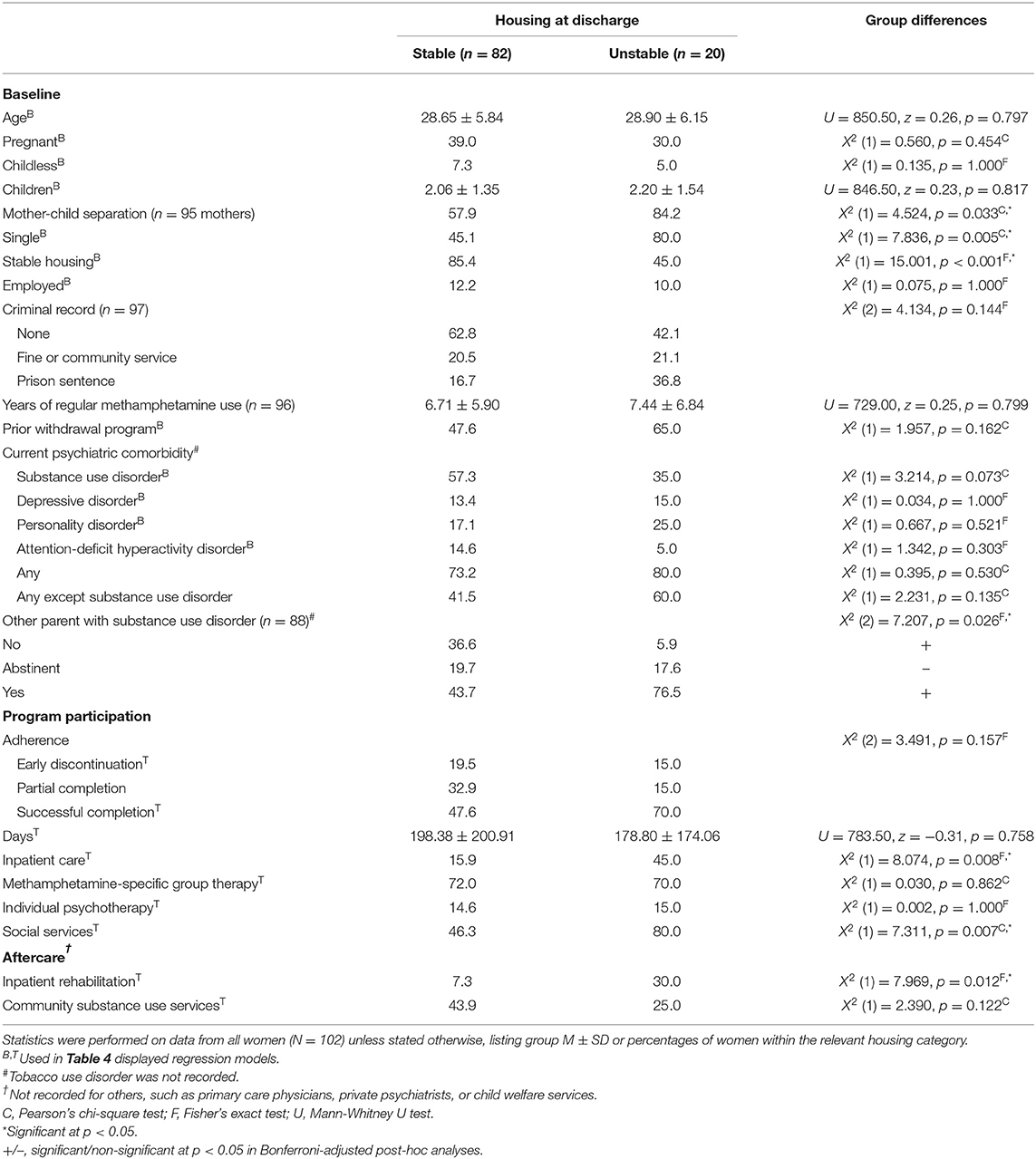
The naturalistic sample consisted of pregnant (n = 38) and/or parenting (n = 95) women with problems related to methamphetamine use. Of the 102 women, 79 were stably housed at admission to psychiatric care and 82 at discharge. Living arrangements and changes therein are detailed in Table 1. Table 2 displays baseline characteristics, program participation, and aftercare, stratified by housing at discharge.
Baseline Correlates of Housing at Discharge
Women were more likely unstably housed at discharge when single, unstably housed at admission, living apart from at least one minor, or when the other parent had a substance use disorder (p < 0.05). The majority of unstably housed women at discharge had a criminal record (prison sentence in over one-third), whereas almost two-thirds of stably housed patients had no record (prison sentence in one-sixth), yet there was no overall significant difference in criminal system involvement between groups. About 10% of women across groups were employed and about three-fourths had a current psychiatric comorbidity. Groups were also similar in age, being pregnant, being childless, number of minors, years of methamphetamine use, and prior withdrawal program participation (p > 0.05).
Treatment Correlates of Housing at Discharge
Unstably housed women at discharge were more likely to have used social and inpatient services, and to transfer to inpatient rehabilitation (p < 0.05). Groups were comparable in attendance at individual and methamphetamine-specific group psychotherapies as well as in program adherence and duration (p > 0.05).
Associations Between Correlates of Housing at Discharge
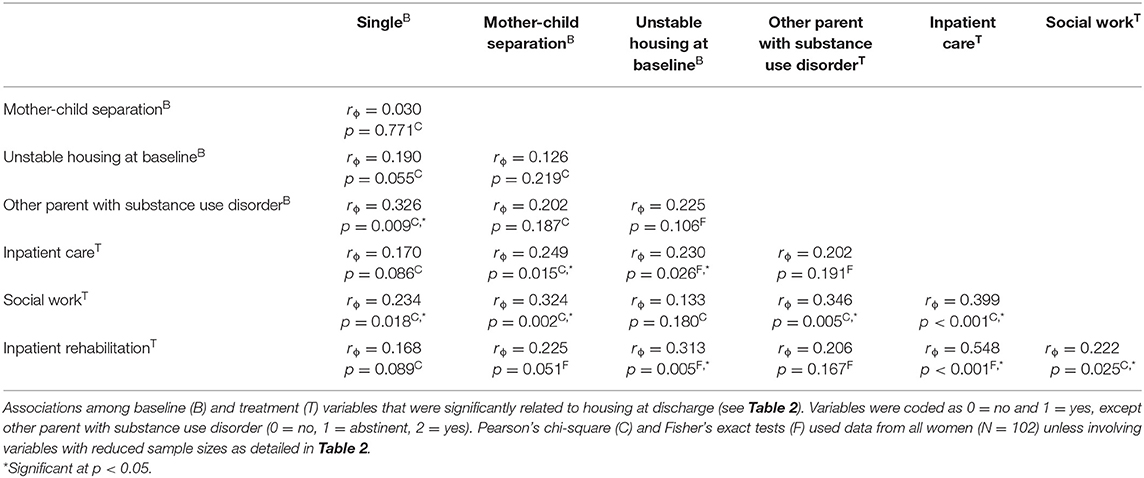
Table 3 presents associations among all baseline and treatment variables that differed significantly between stably and unstably housed women at discharge. Being single was significantly related to the other parent having a substance use disorder and trend-level related to unstable housing at baseline. These three baseline characteristics and living apart from at least one minor were each related to one or more variables of higher treatment intensity (accessing social services, inpatient care, inpatient rehabilitation), which in turn were positively intercorrelated (p < 0.05).
Predictors of Housing at Discharge
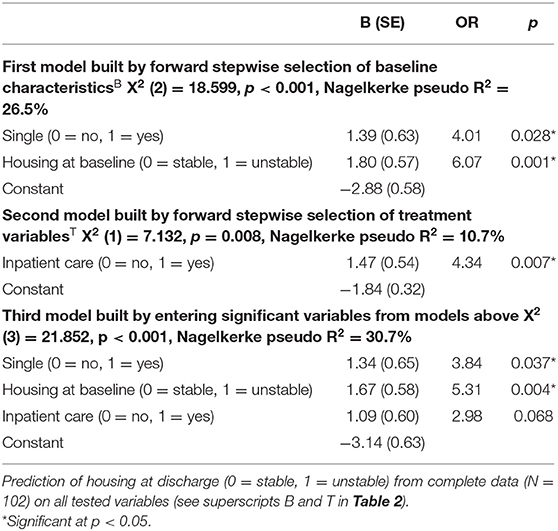
Table 4 lists the unique (net) contributions of selected baseline and treatment variables to housing at discharge (controlled for the other variables in the respective model). Among baseline characteristics (first model), being single and unstably housed predicted unstable housing at discharge (p < 0.05). Among treatment variables (second model), entering inpatient care predicted unstable housing at discharge (p < 0.05). When these three variables were tested together (third model), being single and unstably housed at baseline retained significance, whereas inpatient care reached trend-level significance.
Discussion
This prospective observational study documents the importance of housing in the complex dynamics between social stressors and treatment response in pregnant and parenting women with problems related to methamphetamine use. Our real-world data have direct implications for clinical practice as we continue developing integrated care for this underserved population.
Baseline Correlates of Housing
Psychiatric comorbidities and social complexities were frequent in our naturalistic sample of pregnant and parenting women, echoing the multiple burdens reported in association with methamphetamine use (19, 24). We previously found that comorbid attention-deficit hyperactivity disorder and depression jeopardized treatment engagement in integrated care (27). Yet in contrast to social challenges, psychiatric comorbidities were not significantly related to housing at discharge. As both treatment discontinuation and unstable housing predict substance use (30–32), our studies indicate that psychiatric comorbidities and social challenges are differentially associated with important determinants of treatment success.
Being single may be a key stressor as it predicted unstable housing at discharge even when adjusting for housing at admission. This aligns with a study in people injecting substances where a partnered relationship seemed conducive to attaining stable housing (28). Yet substance-using partners are influential in the use of methamphetamine (9, 13), and being single was significantly related to the other parent having a substance use disorder, which predicted unstable housing at discharge as did living apart from children. These data combined with the stresses of single parenting (10, 12–14) indicate that women could greatly benefit from interventions targeted at building relationships. Couple counseling should be offered and cover substance use, family planning, and parenting skills (19).
The majority of unstably housed women at discharge had a criminal record (prison sentence in over one-third), whereas almost two-thirds of stably housed patients had no record (prison sentence in one-sixth). Although there was no overall significant difference in criminal system involvement between these groups, incarceration history was previously associated with an increased likelihood of unstable housing and methamphetamine use (33). Thus, housing may be lost while imprisoned and prison sentences may hamper attaining stable housing. As employment rates were similarly low across stably and unstably housed women at discharge, prison sentences may thwart stable housing by factors other than lost income, such as lost community or additional stigma. Nonetheless, the low levels of employment highlight the general need for vocational education, training, and reintegration.
Treatment Correlates of Housing
Twelve of 23 women who were unstably housed at admission (three of six homeless) achieved stable housing by discharge. Nine women transitioned from their own to supported transitional accommodation with children as they required intensive care that could not otherwise be provided after discharge from Mamadam.
The relations among housing at admission and discharge, being single, the other parent having a substance use disorder, mother-child separation, social work involvement, and inpatient care and rehabilitation show that women in difficult circumstances were more likely to access social and inpatient services, and to transition to inpatient rehabilitation. Stable housing would facilitate the use of outpatient social work to build community relationships, receive home support for childcare, and pursue employment. To deliver on this prospect, stronger partnerships with government and community agencies are needed to provide faster access to public housing and support for independent housing.
Housing at discharge was not significantly associated with adherence to or duration of Mamadam, or with prior withdrawal program participation. Yet less than one-third of unstably housed women at discharge had discontinued Mamadam and almost two-thirds had accessed a withdrawal program, whereas adherence and withdrawal program participation were below 50% in stably housed women at discharge. In mothers with substance use and/or other psychiatric disorders, accessing treatment was related to being single and having a low socioeconomic status (11). However, substance use treatment was inversely associated with attaining stable housing, even after adjustment for relationship status, employment status, and substance use (28). Completion of addiction treatment is associated with abstinence, less crime, and greater employment (32), whereas the relation to housing is mixed (30). These findings collectively suggest that current programs engage socially disadvantaged patients in care but are often not sufficient to improve housing conditions.
Limitations
We used a dichotomous measure of housing stability as more women in supported transitional accommodation with children, living in others' homes, and without housing would have been required to gain insight into potential differences between these living arrangements. The lack of post-discharge data precludes claims regarding potential benefits of transitioning from own to supported transitional housing for some women. Moreover, our care concept and some of our findings (e.g., employment unrelated to housing at discharge) may not be readily transferable to other healthcare systems and communities in different social, financial, or legal contexts.
Conclusion
Integrated services promise better care for pregnant and parenting women with problems related to methamphetamine use, yet challenges remain given the complex needs of this population. Single women and unstably housed women are particularly at risk of remaining in precarious living conditions, which threaten to drive them into heavier substance use and socioeconomic deprivation. Future work should consider developing and studying housing and relationship interventions, which may break this downward spiral.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee at the Carl Gustav Carus Faculty of Medicine at the Technische Universität Dresden, Germany. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
UZ, MP, and MS contributed to the development of the care concept. UZ, MP, MS, and BW were members of the care team. MP, UZ, LR, MK, and JP designed the study. UZ, MP, and JP obtained funding. LR, MK, MS, BW, MP, and UZ collected the data. JP analyzed and interpreted the data and wrote the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The German Research Foundation (Project Number 402170461, TRR 265) (34) supported this research and paid the article processing charge but was not involved in the conceptualization or conduct of the study, the collection, analysis, interpretation of data, the preparation of the manuscript, or the decision to submit it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank the staff at the psychiatric outpatient department for assistance with data collection and Matthew Belanger for diligent proofreading.
References
1. Paulus MP, Stewart JL. Neurobiology, clinical presentation, and treatment of methamphetamine use disorder: a review. JAMA Psychiatry. (2020) 77:959–66. doi: 10.1001/Jamapsychiatry.2020.0246
2. Stoneberg DM, Shukla RK, Magness MB. Global methamphetamine trends: an evolving problem. Int Crim Justice Rev. (2018) 28:136–61. doi: 10.1177/1057567717730104
3. UNODC. World Drug Report 2021, Booklet 4 Drug Market Trends: Cocaine Amphetamine-Type Stimulants. Vienna: United Nations Publication(2021).
4. Admon LK, Bart G, Kozhimannil KB, Richardson CR, Dalton VK, Winkelman TNA. Amphetamine- and opioid-affected births: incidence, outcomes, and costs, United States, 2004–2015. Am J Public Health. (2019) 109:148–54. doi: 10.2105/Ajph.2018.304771
5. Dinger J, Hinner P, Reichert J, Rüdiger M. Methamphetamine consumption during pregnancy—effects on child health. Pharmacopsychiatry. (2017) 50:107–13. doi: 10.1055/s-0042-122711
6. Perez FA, Blythe S, Wouldes T, McNamara K, Black KI, Oei JL. Prenatal methamphetamine- impact on the mother and child—a review. Addiction. (2021). doi: 10.1111/add.15509
7. Harst L, Deckert S, Haarig F, Reichert J, Dinger J, Hellmund P, et al. Prenatal methamphetamine exposure: effects on child development–a systematic review. Dtsch Arztebl Int. (2021) 118:313–9. doi: 10.3238/Arztebl.M2021.0128
8. Schmidt U, Capek C, Birdir C, Erfurt C, Nitzsche K. Crystal und schwangerschaft – erste ergebnisse einer retrospektiven studie zum schwangerschafts- und geburtsverlauf methamphetamin-konsumierender frauen in sachsen. Z Geburtshilfe Neonatol. (2019) 223:221–9. doi: 10.1055/a-0831-3642
9. O'Connor A, Harris E, Hamilton D, Fisher C, Sachmann M. The experiences of pregnant women attending a specialist service and using methamphetamine. Women Birth. (2021) 34:170–9. doi: 10.1016/j.Wombi.2020.01.011
10. Wouldes TA, LaGasse LL, Derauf C, Newman E, Shah R, Smith LM, et al. Co-morbidity of substance use disorder and psychopathology in women who use methamphetamine during pregnancy in the US and New Zealand. Drug Alcohol Depend. (2013) 127:101–7. doi: 10.1016/j.Drugalcdep.2012.06.016
11. Stevens S, Rogers J, Dansereau L, DellaGrotta S, Lester BM, Wouldes TA, et al. Prospective study of service use in the year after birth by women at high risk for antenatal substance use and mental health disorders. Int J Ment Health Addict. (2019) 19:1005–18. doi: 10.1007/S11469-019-00207-W
12. Carlson BE, Williams LR, Shafer MS. Methamphetamine-involved parents in the child welfare system: are they more challenging than other substance-involved parents? J Public Child Welf. (2012) 6:280–95. doi: 10.1080/15548732.2012.683361
13. Dyba J, Moesgen D, Klein M, Leyendecker B. Methamphetamine use in German families: parental substance use, parent-child interaction and risks for children involved. Subst Use Misuse. (2019) 54:583–91. doi: 10.1080/10826084.2018.1528459
14. Semple SJ, Strathdee SA, Zians J, Patterson TL. Methamphetamine-using parents: the relationship between parental role strain and depressive symptoms. J Stud Alcohol Drugs. (2011) 72:954–64. doi: 10.15288/Jsad.2011.72.954
15. Dinger J, Näther N, Wimberger P, Zimmermann US, Schmitt J, Reichert J, et al. Increasing consumption of crystal meth in saxony and its risks for mother and child - experiences at a level I perinatal center from a pediatric viewpoint. Z Geburtshilfe Neonatol. (2017) 221:73–80. doi: 10.1055/s-0043-102953
16. Cumming C, Troeung L, Young JT, Kelty E, Preen DB. Barriers to accessing methamphetamine treatment: a systematic review and meta-analysis. Drug Alcohol Depend. (2016) 168:263–73. doi: 10.1016/j.Drugalcdep.2016.10.001
17. Holt K, French G. Exploring the motherhood experiences of active methamphetamine users. Crime, Law and Social Change. (2020) 73:297–314. doi: 10.1007/S10611-019-09862-5
18. Wakeman B, Kremer M, Schulkin J. The application of harm reduction to methamphetamine use during pregnancy: a call to arms. Am J Obstet Gynecol MFM. (2021) 3:100418. doi: 10.1016/j.Ajogmf.2021.100418
19. Braunwarth W-D, Christ M, Dirks H, Dyba J, Härtel-Petri R, Harfst T, et al. S3 Practice Guideline Methamphetamine-Related Disorders. 1st ed. Berlin: Agency for Quality in Medicine (2016).
20. Groß C, Schützwohl M, Mayer-Pelinski R, Hasler H, Kirchner T, Scheck A, et al. “CrystalClean”—a German-language manual for qualified detoxification and motivation treatment in cases of “crystal meth” dependency—feasibility and acceptance. Psychiatr Prax. (2020) 47:22–8. doi: 10.1055/a-1003-5148
21. Petzold J, Weber B, Bassett TR, Bauer M, Bernhardt N, Gross C, et al. Effectiveness of the first German-language group psychotherapy manual to accompany short-term treatment in methamphetamine dependence. Front Psychiatry. (2020) 11:130. doi: 10.3389/Fpsyt.2020.00130
22. Bernhardt N, Petzold J, Groß C, Scheck A, Pooseh S, Mayer-Pelinski R, et al. Neurocognitive dysfunctions and their therapeutic modulation in patients with methamphetamine dependence: a pilot study. Front Psychiatry. (2020) 11:581. doi: 10.3389/Fpsyt.2020.00581
23. Pilhatsch M, Pooseh S, Junke A, Kohno M, Petzold J, Sauer C, et al. Probabilistic reversal learning deficits in patients with methamphetamine use disorder-a longitudinal pilot study. Front Psychiatry. (2020) 11:588768. doi: 10.3389/Fpsyt.2020.588768
24. Grigg J, Manning V, Arunogiri S, Volpe I, Frei M, Phan V, et al. Methamphetamine Treatment Guidelines: Practice Guidelines for Health Professionals. 2nd ed. Richmond, Victoria: Turning Point (2018).
25. Dinger J, Reichert J. “Mama Denk' an Mich” (MAMADAM) - ein interdisziplinäres und multiprofessionales hilfsangebot für mutter und kind mit methamphetamin-konsum während der schwangerschaft. Ärzteblatt Sachsen. (2018) 8:331–7.
26. Groß C, Hahn S, Spreer M, Behrendt S, Dinger J, Reichert J, et al. Mama Denk' an Mich (MAMADAM)—ein multimodales therapieprogramm für suchtkranke schwangere, mütter und väter im rahmen der psychiatrischen institutsambulanz. SUCHT. (2018) 64:97–108. doi: 10.1024/0939-5911/A000533
27. Petzold J, Spreer M, Krüger M, Sauer C, Kirchner T, Hahn S, et al. Integrated care for pregnant women and parents with methamphetamine-related mental disorders. Front Psychiatry. (2021) 12:762041. doi: 10.3389/Fpsyt.2021.762041
28. Palepu A, Marshall BD, Lai C, Wood E, Kerr T. Addiction treatment and stable housing among a cohort of injection drug users. PLoS ONE. (2010) 5:E11697. doi: 10.1371/Journal.Pone.0011697
29. Shearer RD, Howell BA, Bart G, Winkelman TNA. Substance use patterns and health profiles among US adults who use opioids, methamphetamine, or both, 2015-2018. Drug Alcohol Depend. (2020) 214:108162. doi: 10.1016/j.Drugalcdep.2020.108162
30. Austin AE, Shiue KY, Naumann RB, Figgatt MC, Gest C, Shanahan ME. Associations of housing stress with later substance use outcomes: a systematic review. Addict Behav. (2021) 123:107076. doi: 10.1016/j.Addbeh.2021.107076
31. Shokoohi M, Karamouzian M, Sharifi H, Rahimi-Movaghar A, Carrico AW, Hosseini Hooshyar S, et al. Crystal methamphetamine use and its correlates in women engaged in sex work in a developing country setting. Drug Alcohol Depend. (2018) 185:260–5. doi: 10.1016/j.Drugalcdep.2017.12.025
32. Brorson HH, Ajo Arnevik E, Rand-Hendriksen K, Duckert F. Drop-out from addiction treatment: a systematic review of risk factors. Clin Psychol Rev. (2013) 33:1010–24. doi: 10.1016/j.cpr.2013.07.007
33. Anderson-Carpenter KD, Fletcher JB, Reback CJ. Associations between methamphetamine use, housing status, and incarceration rates among men who have sex with men and transgender women. J Drug Issues. (2017) 47:383–95. doi: 10.1177/0022042617696917
Keywords: perinatal substance use, maternal drug use, pregnancy, socioeconomic deprivation, unstable housing, multimodal therapy, methamphetamine use disorder, drug addiction
Citation: Petzold J, Rehmet L, Weber B, Spreer M, Krüger M, Zimmermann US and Pilhatsch M (2022) Housing Correlates in Pregnant and Parenting Women Using Methamphetamine and Accessing Psychiatric Care. Front. Psychiatry 13:890635. doi: 10.3389/fpsyt.2022.890635
Received: 06 March 2022; Accepted: 05 May 2022;
Published: 27 May 2022.
Edited by:
Anette Skårner, University of Gothenburg, SwedenReviewed by:
Peter Higgs, Burnet Institute, AustraliaMei Yang, Shenzhen Mental Health Centre, China
Jonas Stålheim, University of Gothenburg, Sweden
Copyright © 2022 Petzold, Rehmet, Weber, Spreer, Krüger, Zimmermann and Pilhatsch. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Johannes Petzold, am9oYW5uZXMucGV0em9sZEB1bmlrbGluaWt1bS1kcmVzZGVuLmRl
†ORCID: Johannes Petzold orcid.org/0000-0003-4163-9014
Benjamin Weber orcid.org/0000-0002-4941-1332
Ulrich S. Zimmermann orcid.org/0000-0001-7900-4992
Maximilian Pilhatsch orcid.org/0000-0003-4323-3309
 Johannes Petzold
Johannes Petzold Laura Rehmet
Laura Rehmet Benjamin Weber1†
Benjamin Weber1† Maria Krüger
Maria Krüger Ulrich S. Zimmermann
Ulrich S. Zimmermann Maximilian Pilhatsch
Maximilian Pilhatsch