- The Affiliated Brain Hospital of Guangzhou Medical University, Guangzhou, China
Background: Electroconvulsive therapy (ECT) is a safe and effective therapy for individuals suffering from major psychiatric disorders, but attitudes towards ECT among patients and caregivers have not been well studied. This study was conducted to elucidate patient and caregiver knowledge and attitudes concerning ECT in South China.
Methods: The sample comprised 92 patients diagnosed with major psychiatric disorders and their caregivers (n = 92). Participants completed questionnaire measures of knowledge and attitudes related to ECT.
Results: Information before ECT was inadequately provided to both caregivers and patients (55.4% versus 37.0%, p < 0.05). Caregivers reported receiving more adequate information about the therapeutic effects (50.0% versus 44.6%), side effects (67.4% versus 41.3%), and risks (55.4% versus 20.7%) of ECT when compared to patients (all p < 0.05). However, less than half of patients and caregivers believed that ECT was effective (43.5% versus 46.7%, p > 0.05), while more than half of them believed that ECT was beneficial (53.3% versus 71.7%, p < 0.05), and approximately half of them believed that ECT was safe (50.0% versus 51.1%, p > 0.05). A total of 32.6% of patients and 55.4% of caregivers (p < 0.05) reported that ECT was used only for critically ill patients. A total of 62.0% of patients experienced side effects, with memory impairment being the most commonly reported.
Conclusion: Clinicians should develop a systematic health education program before ECT treatment and ensure that patients and caregivers have an accurate understanding of ECT, particularly the treatment process, its therapeutic effects and potential side effects prior to administering this treatment.
1. Introduction
Electroconvulsive therapy (ECT), as a non-invasive brain stimulation technique (1), is effective in treating severe psychiatric disorders such as bipolar disorder (BD), schizophrenia, and major depressive disorder (MDD) in clinical practice (2–5). Since its introduction as a non-invasive brain stimulation technique in 1938, ECT has been widely used in many countries, including the United States (5, 6) and China (7, 8). Apart from ECT, other non-invasive brain stimulation techniques, such as repetitive transcranial magnetic stimulation (rTMS), transcranial direct current stimulation (tDCS), and transcranial alternating current stimulation (tACS) have been widely used in treating major mental disorders (6). ECT has been shown to be more effective than rTMS, tACS, or tDCS for treatment-resistant depression (TRD) (5, 9).
In general, ECT is a highly effective treatment for severe psychiatric disorders, and the gold-standard therapy for patients suffering from TRD (10). While ECT is a therapeutically effective alternative in older patients and adolescents with major psychiatric disorders (11, 12), some studies have discouraged the use of ECT because of its potential adverse effects, such as short-term confusion and memory impairment (13). For example, a meta-analysis of randomized controlled studies (RCTs) found that ECT combined with antipsychotics led to significantly greater transient memory impairment in patients with schizophrenia (13).
The number of patients who have received a course of ECT is vast in China. For example, a cross-sectional survey (n = 1,364) focusing on adult patients (≥18 years old) found that 52.1% received ECT, with 53.4% receiving ECT for MDD, 57.8% for BD, 57.0% for schizophrenia, and 32.4% for other diagnoses (14). In a retrospective study, 28.1% of 2,339 hospitalized older Chinese psychiatric patients (aged 60 years and older) received ECT, including 21.2% for schizophrenia, 43.6% for MDD, 37.9% for BD, and 10.7% for other diagnoses (15). Another retrospective study focusing on Chinese adolescent psychiatric patients aged between 13 and 17 years found that 42.6% of the total sample received ECT, including 57.8% for BD, 41.8% for MDD, 46.5% for schizophrenia, and 23.9% for other diagnoses (16). However, there is an ongoing debate about the use of ECT for major psychiatric disorders in China. Some advocate its use because of rapid improvements in psychiatric symptoms (17), while others argue that the utility of ECT is limited given its adverse effects (18).
To understand the acceptance of ECT as a treatment among patients with psychiatric disorders who had ECT, it is important to investigate patient and caregiver attitudes and knowledge regarding the intervention (19). Relatively few studies have examined this issue (19), and related findings have been inconsistent (7, 19–21). For example, a previous study found that caregivers (75.0%) reported receiving significantly more adequate information about the therapeutic effects of ECT than did older psychiatric patients (56.1%) (19). However, another study found that more adolescents with psychiatric disorders (55.7%) reported receiving adequate information about the therapeutic effects of ECT than their caregivers (50.6%) (20). Given that ECT practice is influenced by cultural, social, and legal factors, findings from previous studies on ECT attitudes and knowledge from other countries or regions may not be applicable to samples in different regions of China (22–24).
Thus, the purpose of this study was to investigate the knowledge and attitudes towards ECT among patients and caregivers as well as patients’ subjective experiences regarding ECT in South China.
2. Methods
2.1. Study design and participants
This cross-sectional survey was conducted from 5 February 2021 to 31 May 2022 at the Affiliated Brain Hospital of Guangzhou Medical University, a setting that has 1800 psychiatric beds and performs approximately 1,500 ECT sessions monthly. The study protocol was approved by the Research Ethics Panel of the Affiliated Brain Hospital of Guangzhou Medical University (No. 2021001). Both patients receiving a course of ECT sessions and caregivers who provided informed consent in writing were invited to join the study.
The following were inclusion criteria for patients in this study: (1) understanding the questionnaire content focusing on knowledge and attitudes towards ECT; (2) a diagnosis of schizophrenia, BD, or MDD; (3) aged 18 years or older; (4) treated with a course of ECT in the past 6 months; and (5) completion of the last ECT session more than 1 month before this questionnaire. Similarly, caregivers had to fulfill the following inclusion criteria: (1) understanding of the questionnaire content; (2) aged 18 years or older; and (3) a friend or family member (e.g., spouse, sister, and brother) who has provided primary personal care and handled medical-related issues for the patient during the past 6 months.
2.2. ECT parameters
ECT is available only as an inpatient procedure at the Affiliated Brain Hospital of Guangzhou Medical University. ECT (Spectrum 5000Q ECT machine, MECTA Inc., Lake Oswego, OR, USA) generally consists of 6–12 sessions per course, performed 2–3 times per week from 8:00 a.m. to noon on weekdays. During each ECT session, the patient’s blood oxygen, heart rate, and blood pressure are monitored with a cardiac monitor.
2.3. Measures
Face-to-face interviews were performed by one interviewer for all assessments. According to the methodology of previous studies (7, 19, 21), patients completed a three-part self-report questionnaire that included subjective experience, knowledge, and attitudes towards ECT. Another knowledge and attitudes questionnaire about ECT was given to caregivers. Each question on the questionnaire offered three options: “I do not know,”"disagree/no,” and “agree/yes.”
2.4. Statistical analysis
All statistical analyses in the present study were performed using SPSS version 24.0 (SPSS Inc., Chicago, IL, USA). For descriptive analyses, continuous and categorical variables were expressed as the means ± standard deviations (SD) and percentages (%) with regard to the demographic and clinical data of patients. Chi-square tests were utilized to determine the differences in ECT knowledge and attitudes between patients with major psychiatric disorders and their caregivers. p values less than 0.05 (two-tailed) were deemed statistically significant.
3. Results
3.1. Basic demographic and clinical data
Of the 96 patients and 96 caregivers invited to participate in the study, 92 (95.8%) patients with major psychiatric disorders who received ECT and 92 (95.8%) caregivers fulfilled the inclusion criteria and completed the assessment. Demographic and clinical data of subjects undergoing ECT are summarized in Table 1. Among the patients, 16.3%, 52.2%, and 31.5% were diagnosed with schizophrenia, BD, and MDD, respectively; 57.6% of patients were female, and 32.6% were married. The mean age, age of onset, and body mass index (kg/m2) of patients were 27.9 ± 10.7 years, 20.9 ± 7.5 years, and 22.3 ± 2.6 kg/m2, respectively.
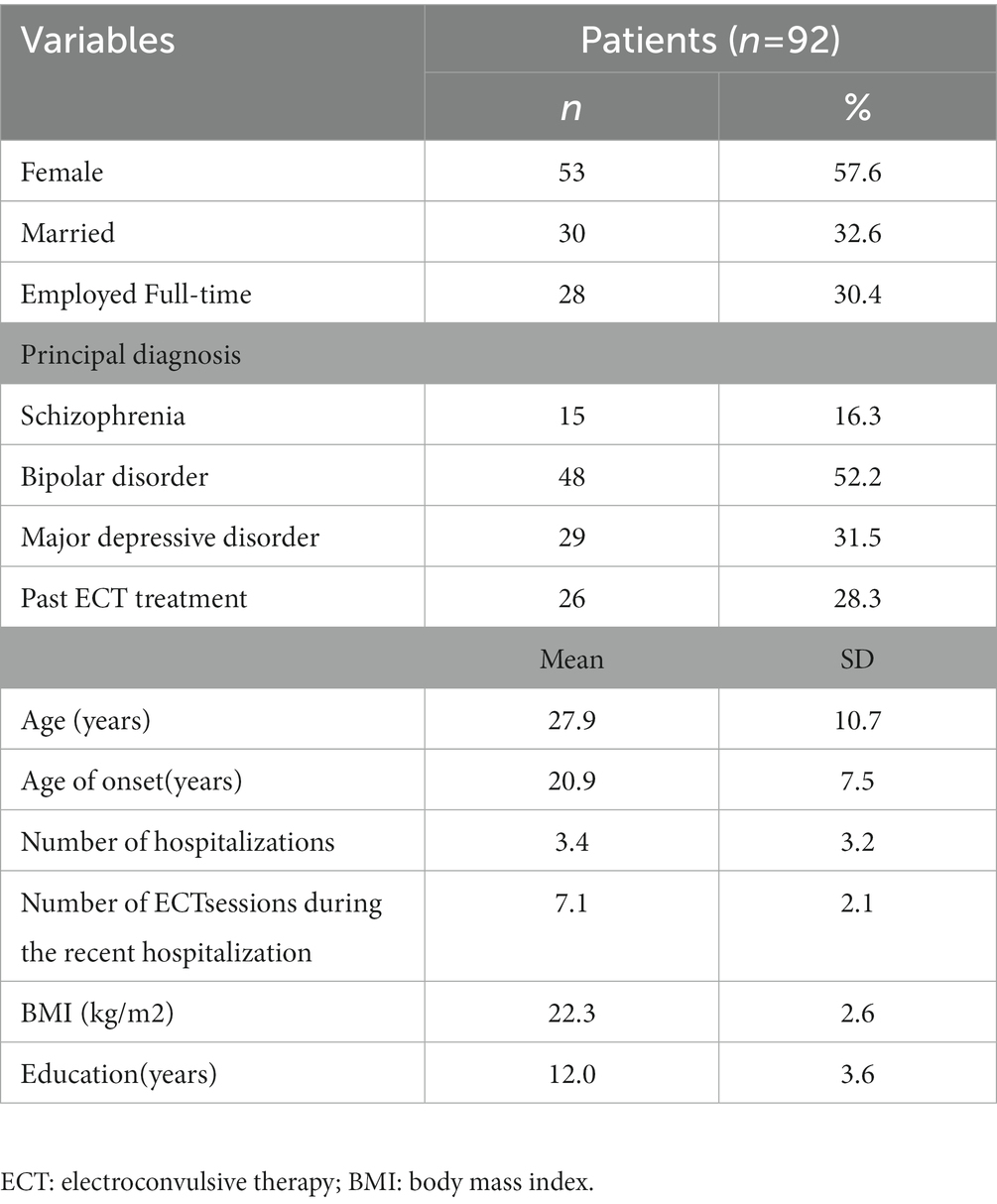
Table 1. Basic demographic and clinical characteristics of patients receiving electroconvulsive therapy.
3.2. ECT knowledge of patients and caregivers
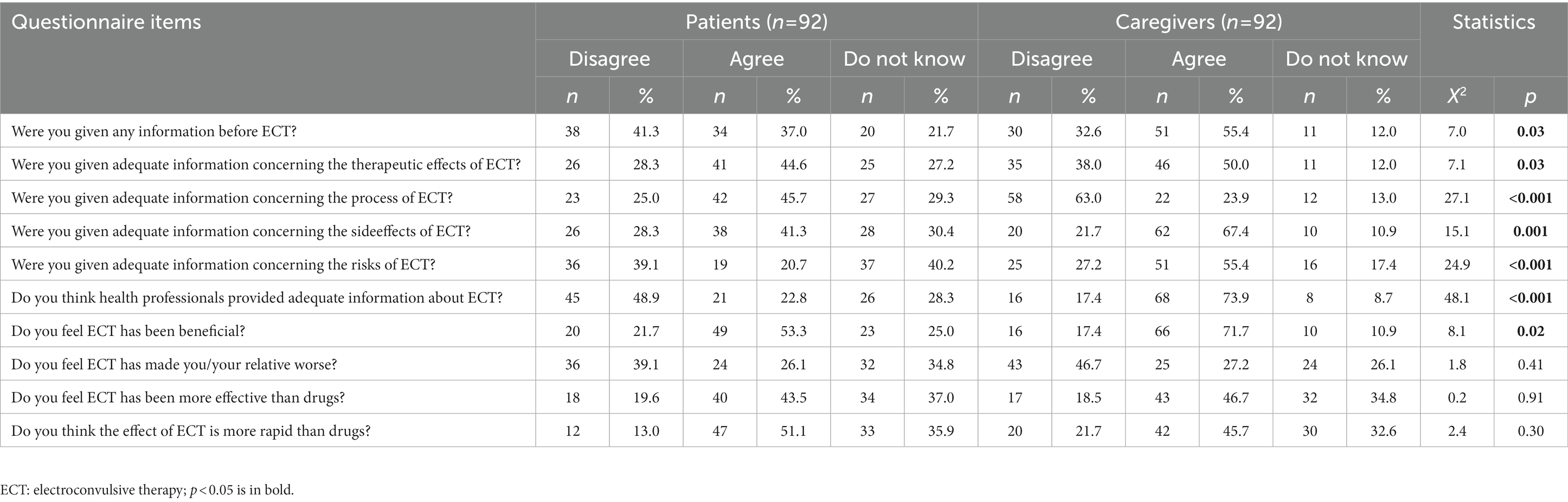
As shown in Table 2, 55.4% of caregivers and 37.0% of patients reported that they received any information before ECT (p < 0.05). Caregivers (versus patients) reported receiving relatively more adequate information regarding therapeutic effects (50.0% versus 44.6%), side effects (67.4% versus 41.3%), and risks (55.4% versus 20.7%) of ECT (all p < 0.05). However, patients (versus caregivers) reported receiving more adequate information on the process of ECT (45.7% versus 23.9%) (p < 0.05). A significantly larger percentage of caregivers (71.7%) versus patients (53.3%) believed that ECT was beneficial (p < 0.05). Approximately half of patients (versus caregivers) thought that ECT was more effective (43.5% versus 46.7%) and more rapid than drugs (51.1% versus 45.7%) (all p > 0.05).
3.3. ECT attitudes of patients and caregivers
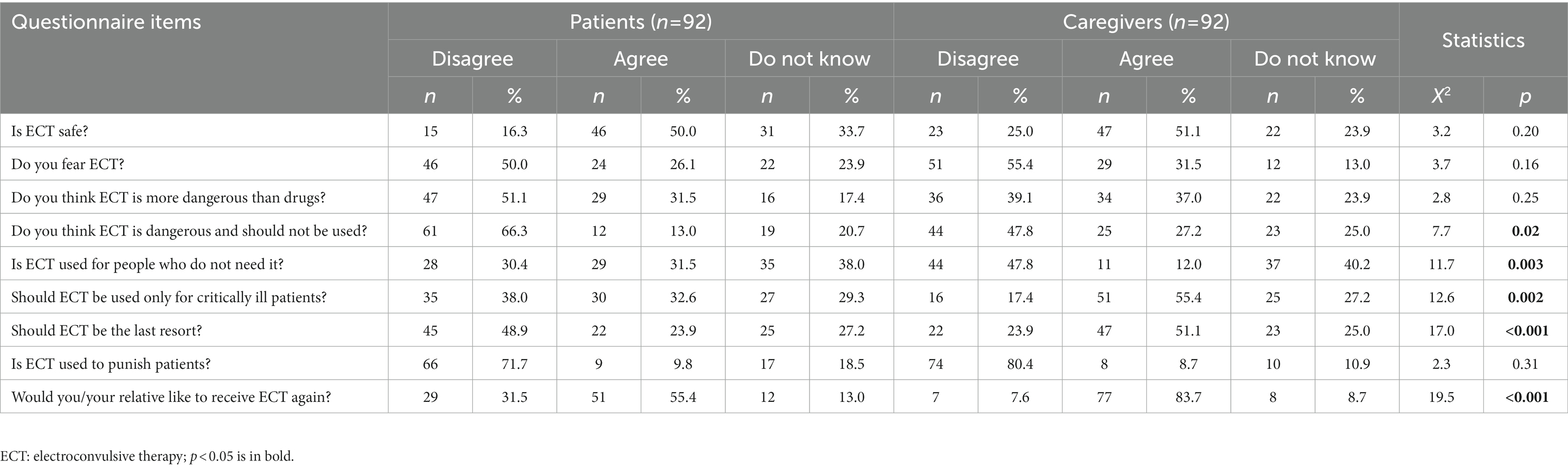
As depicted in Table 3, 50.0% of patients and 51.1% of caregivers reported positive attitudes towards ECT (p > 0.05). More patients than caregivers disagreed with the statement, “Do you think ECT is dangerous and should not be used?” (66.3% versus 47.8%), and a significantly higher proportion of caregivers than patients endorsed the following queries: “Should ECT be used only for critically ill patients?” (55.4% versus 32.6%), “Should ECT be the last resort?” (51.1% versus 23.9%), and “Would you/your relative like to receive ECT again?” (83.7% versus 55.4%) (all p < 0.05). Alternatively, a significantly higher proportion of patients (31.5%)versus caregivers (12.0%) responded affirmatively to the question, “Is ECT used for people who do not need it?” (p < 0.05).
3.4. Patient experiences of ECT and associated side effects
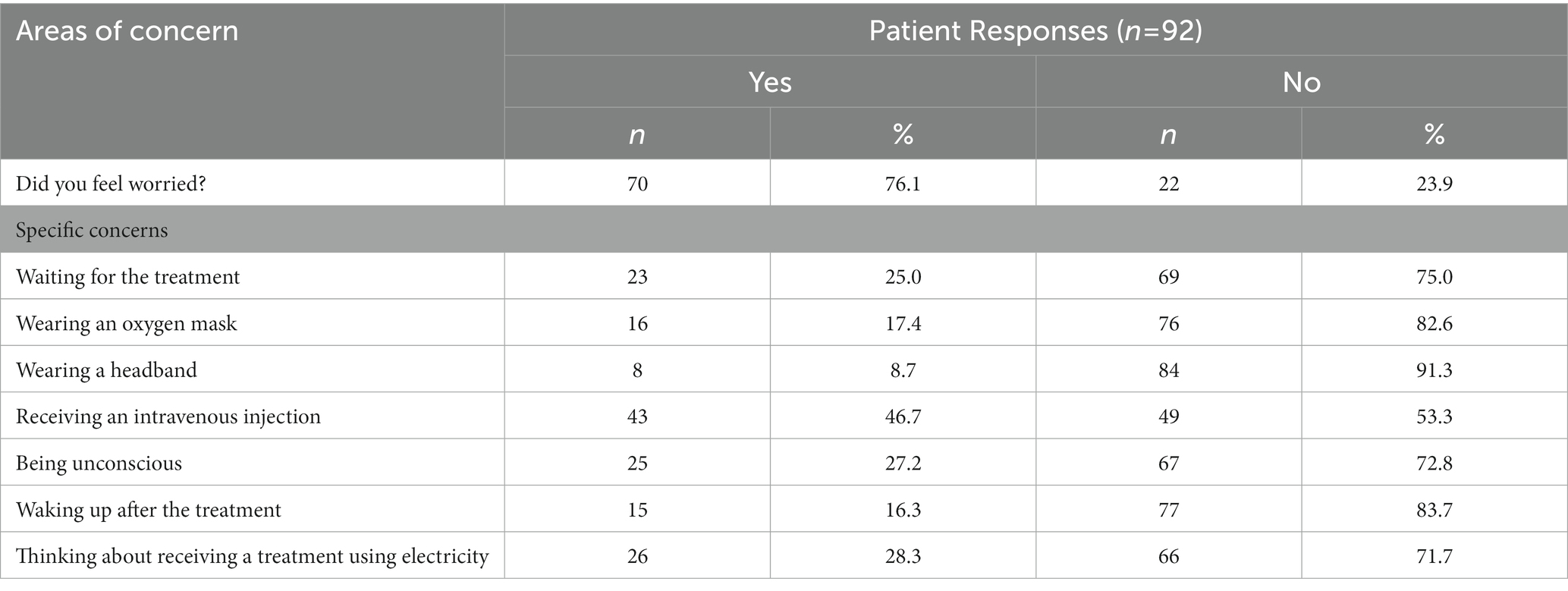
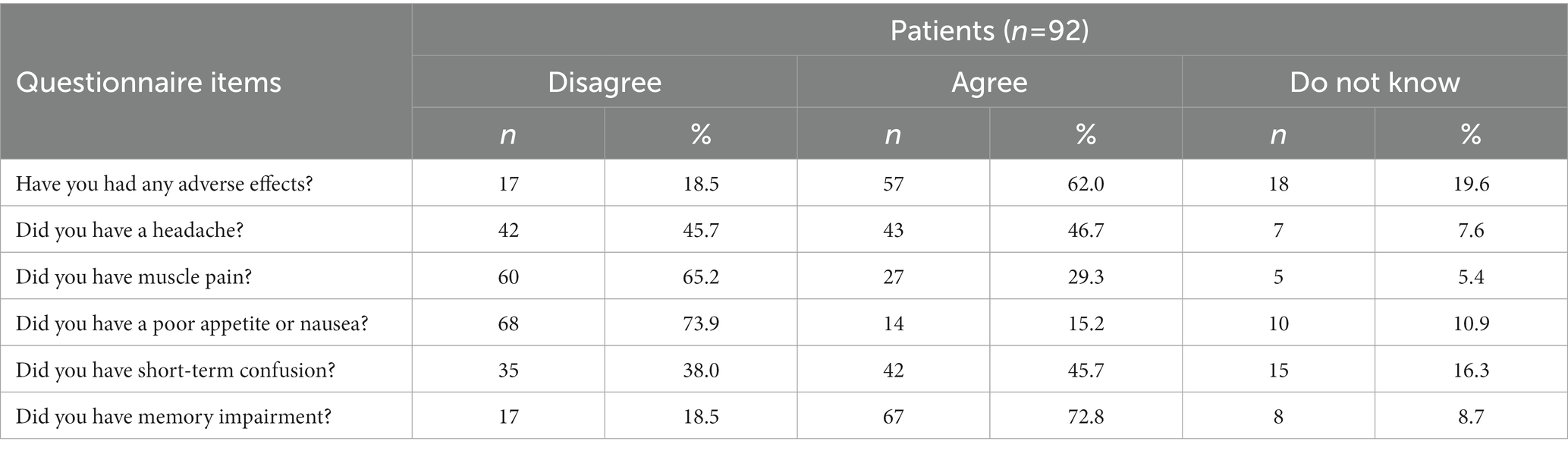
Patient experiences of having ECT are summarized in Table 4. During ECT, up to 76.1% of patients felt worried, particularly when receiving an intravenous injection (46.7%) or when thinking about receiving a treatment that used electricity (28.3%). As shown in Table 5, 62.0% of patients reported side effects caused by ECT; within this group, memory impairment (72.8%) was the most common side effect, followed by headache (46.7%) and short-term confusion (45.7%).
4. Discussion
As reported by Tang et al. (8), China has the largest patient population receiving ECT in the world. The main findings of this study were: (1) patients and caregivers were not adequately provided with comprehensive information about ECT yet generally had positive attitudes towards ECT; (2) patients reported receiving an intravenous injection as their most pressing worry during ECT; and (3) patients who had side effects endorsed memory impairment as the most common side effect of ECT.
In this study, only 37.0% of patients and 55.4% of caregivers reported receiving any information about ECT before ECT was conducted. Similar findings from samples in Hong Kong, China (19.8% in patients and 58.6% in caregivers) (21), Beijing, China (42.4% in patients and 59.5% in caregivers) (7), and Turkey (32.9% in patients and 51.4% in caregivers) (25) have been reported previously. Furthermore, substantial percentages of patients and caregivers reported not being informed about the process of ECT, therapeutic effects, and risks of ECT, consistent with low rates reported by previous studies (7, 19). Patients have generally positive attitudes toward rTMS (6), while no studies that examine the knowledge and attitudes of other non-invasive brain stimulation techniques including tACS, tDCS or magnetic seizure therapy (MST) among patients and caregivers have been published. To improve the knowledge of patients and caregivers toward ECT or other non-invasive brain stimulation techniques, systematic health education methods, such as video, brochures and video-assisted educational programs, need to be developed (26–28), and follow-ups are needed to ensure that patients and caregivers have an accurate understanding of the information they have received. Patients reported lower ECT knowledge levels than their caregivers (7, 19, 21), which may be partly attributed to illness factors, such as ECT-induced memory impairment and inadequate or lack of insight about their condition (7, 29, 30). However, the cognition functions and insight recovery of patients were unclear because they were not assessed in this study.
In the past, ECT was often misrepresented in the mass media as a punitive measure for aggressive behaviour; such portrayals contributed to negative public attitudes towards ECT (31, 32). Encouragingly, our study showed that approximately half of patients and their caregivers had positive attitudes towards ECT, viewing it as a beneficial and more effective and rapid treatment than drugs. Furthermore, approximately half of patients and caregivers believed that ECT is safe (50.0% versus 51.1%) and does not induce fear (50.0% versus 55.4%). Approximately three-quarters of patients (71.7%) and caregivers (80.4%) believed that ECT is not a punishment. Up to 83.7% of caregivers and 55.4% of patients might have received ECT again if necessary. Taken together, these findings in the current study do not support the negative attitudes regarding ECT in China (8, 21). Unlike in many Western countries, ECT is widely accepted by clinicians and patients in China, and it has been frequently prescribed in clinical practice (33). For example, a recent study found that both older Chinese patients with severe psychiatric disorders and their caregivers mostly reported positive attitudes towards ECT (19). The possible reasons for the above inconsistent findings were mainly attributed to the fact that the use of ECT is associated with cultural, social, and legal factors (22–24).
A majority of patients (76.1%) reported feeling worried during ECT, which is similar to findings of previous studies (7, 19). However, the incidence of worry has varied widely across studies, ranging from 14% to 75% (34, 35). The most commonly reported worry in our study was receiving intravenous injections, in contrast to other studies that have reported memory impairment or brain damage as the most pressing worries (36). Higher levels of ECT knowledge are related to lower levels of fear and more positive attitudes towards ECT (37). Consequently, psychiatric clinicians should educate patients and caregivers about ECT, including its nature and side effects. As part of the process, patient understanding of information should also be assessed.
Approximately two-thirds of the patients experienced side effects of ECT, including memory impairment (72.8%), short-term confusion (45.7%), and headache (46.7%). Memory impairment was the most commonly reported side effect, while associated rates have varied in the literature from 29% to 79% (38–40). More severe side effects may be associated with higher doses of ECT, existing brain disease, and older age (16, 41). A recent systematic review found that nonconvulsive electrotherapy (NET) appeared to be a safe and effective treatment option for patients diagnosed with depression without serious cognitive impairments (30). Furthermore, a recent meta-analysis found that MST showed shorter recovery time and reorientation time when compared to ECT (42). However, no head-to-head studies have compared the effectiveness and cognitive effects of NET and MST in severe psychiatric disorders, especially MDD.
The main strength of this study is the first to assess ECT knowledge and attitudes among patients who had undergone the intervention and their caregivers in South China. However, this study has several limitations that should be acknowledged. First, there is no standardized preexisting, interviewer-rated tool to assess ECT knowledge and attitudes. Second, this study with a single-center design was conducted in a psychiatric hospital in southern China. Therefore, the findings of this study cannot be generalized to other countries. Third, the sample size of this study was relatively small, limiting our capacity to detect the differences in attitudes or experiences of ECT among patients with different diagnoses. Fourth, key factors influencing participants’ attitudes towards ECT, such as disease severity and the nature/use of psychiatric medications, were not evaluated. Finally, this cross-sectional study has not been registered.
In conclusion, clinicians should develop a systematic health education program before ECT treatment and ensure that patients and their caregivers have an accurate understanding of ECT, particularly the treatment process, its therapeutic effects and potential side effects prior to administering this treatment.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Research Ethics Panel of the Affiliated Brain Hospital of Guangzhou Medical University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
WZ was responsible for study design, process supervision, data interpretation, and critical revision of the article. SN and C-JD were responsible for organizing and analyzing the data, data interpretation, and drafting the manuscript. J-XM, XH, and X-BH were responsible for implementing the study, data collection, and data interpretation. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by Guangzhou Liwan District Science and Technology Plan Project (202201012), Guangzhou Science and Technology Project of Traditional Chinese Medicine and integrated traditional Chinese and Western medicine (20211A011045), China International Medical Exchange Foundation (Z-2018-35-2002), Guangzhou Clinical Characteristic Technology Project (2019TS67), and Science and Technology Program Project of Guangzhou (202102020658). The funders had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rosson, S, de Filippis, R, Croatto, G, Collantoni, E, Pallottino, S, Guinart, D, et al. Brain stimulation and other biological non-pharmacological interventions in mental disorders: an umbrella review. Neurosci Biobehav Rev. (2022) 139:104743. doi: 10.1016/j.neubiorev.2022.104743
2. AlHadi, AN, AlShahrani, FM, Alshaqrawi, AA, Sharefi, MA, and Almousa, SM. Knowledge of and attitudes towards electroconvulsive therapy (ECT) among psychiatrists and family physicians in Saudi Arabia. Ann General Psychiatry. (2017) 16:16. doi: 10.1186/s12991-017-0139-1
3. Wang, G, Zheng, W, Li, XB, Wang, SB, Cai, DB, Yang, XH, et al. ECT augmentation of clozapine for clozapine-resistant schizophrenia: a meta-analysis of randomized controlled trials. J Psychiatr Res. (2018) 105:23–32. doi: 10.1016/j.jpsychires.2018.08.002
4. Zheng, W, He, M, Gu, LM, Lao, GH, Wang, DF, Mai, JX, et al. Early improvement as a predictor of final remission in patients with treatment-resistant depression receiving electroconvulsive therapy with ketofol anesthesia. J Affect Disord. (2022) 310:223–7. doi: 10.1016/j.jad.2022.05.027
5. Mutz, J, Vipulananthan, V, Carter, B, Hurlemann, R, Fu, CHY, and Young, AH. Comparative efficacy and acceptability of non-surgical brain stimulation for the acute treatment of major depressive episodes in adults: systematic review and network meta-analysis. BMJ. (2019) 364:l1079. doi: 10.1136/bmj.l1079
6. Stillianesis, G, Cavaleri, R, Tang, CY, and Summers, SJ. Exploring patient perceptions of noninvasive brain stimulation: a systematic review. Neuromodultion. (2022) 25:487–93. doi: 10.1111/ner.13461
7. Li, Y, An, FR, Zhu, H, Chiu, HF, and Ungvari, GS. C HN, et al. knowledge and attitudes of patients and their relatives toward electroconvulsive therapy in China. Perspect Psychiatr Care. (2016) 52:248–53. doi: 10.1111/ppc.12124
8. Tang, YL, Jiang, W, Ren, YP, Ma, X, Cotes, RO, and McDonald, WM. Electroconvulsive therapy in China: clinical practice and research on efficacy. J ECT. (2012) 28:206–12. doi: 10.1097/YCT.0b013e31825957b1
9. Ravindran, AV, Balneaves, LG, Faulkner, G, Ortiz, A, McIntosh, D, Morehouse, RL, et al. Canadian network for mood and anxiety treatments (canmat) 2016 clinical guidelines for the management of adults with major depressive disorder: section 5. Complementary and alternative medicine treatments. Focus. (2018) 16:85–94. doi: 10.1176/appi.focus.16106
10. Jelovac, A, Kolshus, E, and McLoughlin, DM. Relapse following successful electroconvulsive therapy for major depression: a meta-analysis. Neuropsychopharmacology. (2013) 38:2467–74. doi: 10.1038/npp.2013.149
11. Karayağmurlu, A, Coşkun, M, Elboğa, G, Ghaziuddin, N, Karayağmurlu, E, Gökçen, C, et al. Efficacy and safety of electroconvulsive therapy in adolescents: a retrospective chart review study from Turkey. J ECT. (2020) 36:54–9. doi: 10.1097/yct.0000000000000602
12. Jiang, X, and Xie, Q. Efficacy and safety of modified electroconvulsive therapy for the refractory depression in older patients. Asia-Pac Psychiatry. (2020) 12:e12411. doi: 10.1111/appy.12411
13. Zheng, W, Tong, G, Ungvari, GS, Ng, CH, Chiu, HFK, Xiang, YQ, et al. Memory impairment following electroconvulsive therapy in Chinese patients with schizophrenia: meta-analysis of randomized controlled trials. Perspect Psychiatr Care. (2018) 54:107–14. doi: 10.1111/ppc.12206
14. An, FR, Zhang, L, Zhang, QE, Ungvari, GS, Ng, CH, Chiu, HFK, et al. Electroconvulsive therapy and its relationships with clinical characteristics and quality of life in Chinese psychiatric patients. Psychiatry Res. (2016) 246:246–9. doi: 10.1016/j.psychres.2016.09.046
15. Zhang, XQ, Wang, ZM, Pan, YL, Chiu, HF, Ng, CH, Ungvari, GS, et al. Use of electroconvulsive therapy in older Chinese psychiatric patients. Int J Geriatr Psychiatry. (2015) 30:851–6. doi: 10.1002/gps.4227
16. Zhang, QE, Wang, ZM, Sha, S, Ng, CH, Seiner, SJ, Welch, CA, et al. Common use of electroconvulsive therapy for Chinese adolescent psychiatric patients. J ECT. (2016) 32:251–5. doi: 10.1097/yct.0000000000000327
17. Huang, J, Gao, Y, and Liu, D. Modified electroconvulsive therapy for bipolar disorders (in Chinese). J Clin Psychol Med. (2010) 20:57.
18. Chung, KF. Electroconvulsive therapy in Hong Kong: rates of use, indications, and outcome. J ECT. (2003) 19:98–102. doi: 10.1097/00124509-200306000-00008
19. Zhang, QE, Zhou, FC, Zhang, L, Ng, CH, Ungvari, GS, Wang, G, et al. Knowledge and attitudes of older psychiatric patients and their caregivers towards electroconvulsive therapy. Psychogeriatrics. (2018) 18:343–50. doi: 10.1111/psyg.12326
20. Zong, QQ, Qi, H, Wang, YY, Zhang, C, Balbuena, L, Ungvari, GS, et al. Knowledge and attitudes of adolescents with psychiatric disorders and their caregivers towards electroconvulsive therapy in China. Asian J Psychiatr. (2020) 49:101968. doi: 10.1016/j.ajp.2020.101968
21. Tang, WK, Ungvari, GS, and Chan, GW. Patients' and their relatives' knowledge of, experience with, attitude toward, and satisfaction with electroconvulsive therapy in Hong Kong. China J ECT. (2002) 18:207–12. doi: 10.1097/00124509-200212000-00008
22. Bustin, J, Rapoport, MJ, Krishna, M, Matusevich, D, Finkelsztein, C, Strejilevich, S, et al. Are patients' attitudes towards and knowledge of electroconvulsive therapy transcultural? A multi-national pilot study. Int J Geriatr Psychiatry. (2008) 23:497–503. doi: 10.1002/gps.1926
23. Papakosta, VM, Zervas, IM, Pehlivanidis, A, Papadimitriou, GN, and Papakostas, YG. A survey of the attitudes of Greek medical students toward electroconvulsive therapy. J ECT. (2005) 21:162–4. doi: 10.1097/01.yct.0000170036.13610.a9
24. Tsai, J, Huang, M, He, H, Selek, S, and Rosenheck, RA. Cross-cultural comparison of perceptions and knowledge about electroconvulsive therapy among adults who screened positive for depression in the United States, India, and China. J ECT. (2021) 37:274–80. doi: 10.1097/yct.0000000000000775
25. Virit, O, Ayar, D, Savas, HA, Yumru, M, and Selek, S. Patients' and their relatives' attitudes toward electroconvulsive therapy in bipolar disorder. J ECT. (2007) 23:255–9. doi: 10.1097/yct.0b013e318156b77f
26. Tsai, J, Huang, M, Rosenheck, RA, and Wilkinson, S. A randomized controlled trial of video psychoeducation for electroconvulsive therapy in the United States. Psychiatr Serv. (2020) 71:562–9. doi: 10.1176/appi.ps.201900448
27. Nagarajan, P, Balachandar, G, Menon, V, and Saravanan, B. Effect of a video-assisted teaching program about ECT on knowledge and attitude of caregivers of patients with major mental illness. Indian J Psychol Med. (2021) 43:45–50. doi: 10.1177/0253717620938038
28. Cheung, O, and Baker, M. Improving attitudes toward electroconvulsive therapy. BJPsych Bull. (2022) 46:4–10. doi: 10.1192/bjb.2021.5
29. Rose, DS, Wykes, TH, Bindman, JP, and Fleischmann, PS. Information, consent and perceived coercion: patients' perspectives on electroconvulsive therapy. Br J Psychiatry. (2005) 186:54–9. doi: 10.1192/bjp.186.1.54
30. Chakrabarti, S, Grover, S, and Rajagopal, R. Electroconvulsive therapy: a review of knowledge, experience and attitudes of patients concerning the treatment. World J Biol Psychiatry. (2010) 11:525–37. doi: 10.3109/15622970903559925
31. Fink, M. Impact of the antipsychiatry movement on the revival of electroconvulsive therapy in the United States. Psychiatr Clin North Am. (1991) 14:793–801.
32. Goodman, JA, Krahn, LE, Smith, GE, Rummans, TA, and Pileggi, TS. Patient satisfaction with electroconvulsive therapy. Mayo Clin Proc. (1999) 74:967–71. doi: 10.4065/74.10.967
33. Leung, CM, Xiang, YT, He, JL, Xu, HL, Ma, L, Fok, ML, et al. Modified and unmodified electroconvulsive therapy: a comparison of attitudes between psychiatrists in Beijing and Hong Kong. J ECT. (2009) 25:80–4. doi: 10.1097/YCT.0b013e31817b8135
34. Obbels, J, Verwijk, E, Bouckaert, F, and Sienaert, P. ECT-related anxiety: a systematic review. J ECT. (2017) 33:229–36. doi: 10.1097/yct.0000000000000383
35. Koopowitz, LF, Chur-Hansen, A, Reid, S, and Blashki, M. The subjective experience of patients who received electroconvulsive therapy. Aust N Z J Psychiatry. (2003) 37:49–54. doi: 10.1046/j.1440-1614.2003.01108.x
36. Walter, G, Koster, K, and Rey, JM. Electroconvulsive therapy in adolescents: experience, knowledge, and attitudes of recipients. J Am Acad Child Adolesc Psychiatry. (1999) 38:594–9. doi: 10.1097/00004583-199905000-00022
37. Sharma, N, Ghai, S, and Grover, S. Knowledge and attitude of nursing students toward electroconvulsive therapy. J Neurosci Rural Pract. (2017) 8:S7–s12. doi: 10.4103/jnrp.jnrp_441_16
38. Tielkes, CE, Comijs, HC, Verwijk, E, and Stek, ML. The effects of ECT on cognitive functioning in the elderly: a review. Int J Geriatr Psychiatry. (2008) 23:789–95. doi: 10.1002/gps.1989
39. Myers, DH. A questionnaire study of patients' experience of electroconvulsive therapy. J ECT. (2007) 23:169–74. doi: 10.1097/yct.0b013e318093eecb0
40. Rose, D, Fleischmann, P, Wykes, T, Leese, M, and Bindman, J. Patients' perspectives on electroconvulsive therapy: systematic review. BMJ. (2003) 326:1363. doi: 10.1136/bmj.326.7403.1363
41. Andrade, C, Arumugham, SS, and Thirthalli, J. Adverse effects of electroconvulsive therapy. Psychiatr Clin North Am. (2016) 39:513–30. doi: 10.1016/j.psc.2016.04.004
Keywords: electroconvulsive therapy, attitudes, knowledge, caregivers, major psychiatric disorders
Citation: Deng C-J, Nie S, Mai J-X, Huang X, Huang X-B and Zheng W (2023) Electroconvulsive therapy knowledge and attitudes among patients and caregivers in South China: A preliminary study. Front. Psychiatry 14:1145301. doi: 10.3389/fpsyt.2023.1145301
Edited by:
Chaomeng Liu, Capital Medical University, ChinaReviewed by:
Shen Li, Tianjin Medical University, ChinaShi-Bin Wang, Guangdong Mental Health Center, China
Copyright © 2023 Deng, Nie, Mai, Huang, Huang and Zheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Zheng, emhlbmd3ZWkwNzAyQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
 Can-Jin Deng
Can-Jin Deng Sha Nie†
Sha Nie† Xing-Bing Huang
Xing-Bing Huang Wei Zheng
Wei Zheng