- 1Department of Psychology, Bar-Ilan University, Ramat Gan, Israel
- 2School of Behavioral Sciences, The Academic College of Tel-Jaffa (MTA), Tel-Jaffa, Israel
- 3Shaare Zedek Medical Center, Hadassah-Hebrew University School of Medicine, Jerusalem, Israel
- 4Ministry of Health, Jerusalem, Israel
Objectives: There is limited data regarding the prevalence of suicidal risk among physicians during COVID-19, and the risk factors relating to it. Dominant risk factors for suicide among physicians are depression and burnout. Maladaptive perfectionism may also serve as a profound risk factor for suicidality among physicians and may aggravate symptoms of distress under the challenges of COVID-19. This study aims to evaluate current suicidal risk, suicidal ideation, depression, and burnout before and during COVID-19 among physicians in Israel, and to identify the best sets of correlates between perfectionism and burnout, depression and suicidal ideation, during these time periods.
Methods: A sample of 246 Israeli physicians (160 before COVID-19 and 86 during COVID-19) completed online surveys assessing lifetime suicidal risk, suicidal ideation during the last year and current suicidal ideation, depression, burnout symptoms and maladaptive perfectionism.
Results: More than one-fifth of the sample (21.9%) reported high suicidal risk (Lifetime suicidal behaviors). More than one-fourth (27.2%) reported suicidal ideation during the last 12 months; and 13.4% reported suicidal ideation during the last 3 months. In addition, more than one-third (34.6%) exhibited moderate–severe levels of depressive symptoms and more than a half of the sample reported burnout symptoms. Maladaptive perfectionism was positively correlated with current suicidal ideation, burnout, and depression. Moderated serial mediation analysis demonstrated indirect effect of perfectionism on suicidal ideation by its impact on burnout and depression only during COVID-19. Before COVID-19, physicians were more likely to experience depressive symptoms.
Conclusion: Physicians in Israel are at increased risk for depression and suicidal ideation, regardless of the COVID-19 pandemic. Maladaptive perfectionism was found to be a risk factor for burnout, depression, and suicidal ideation. During the first waves of the pandemic, physicians were less likely to experience depressive symptoms. However, among physicians who were characterized with high maladaptive perfectionism, depression served as a significant risk factor for suicidal ideation during the pandemic, which places these individuals at increased risk for suicidality. These results highlight the importance of implementing intervention programs among physicians to reduce suicidal risk and to better identify rigid perfectionism and depressive symptoms.
Introduction
Physicians are routinely exposed to environmental and professional stressors that may increase mental health problems. These include a heavy workload, workplace conflicts, functioning under life and death emergencies, and other stressors associated with depression and suicidal behaviors (1, 2). In addition to these ongoing challenges, the Coronavirus 2019 (COVID-19) outbreak destabilized physicians’ work conditions and sense of security (3, 4) and has led to unprecedented adversities among physicians, who, according to the literature, were an at-risk group for suicidal ideation and behaviors prior to the epidemic (5, 6). Amidst the growing public concern surrounding the impact of the COVID-19 epidemic on physicians’ mental health, it is important to highlight the existing dearth of information regarding the specific effect of COVID-19 on physicians’ suicidal risk (7). Moreover, studies conducted during COVID-19 report high levels of stress reaction symptoms among medical staff, including high frequencies of depression, anxiety (8–11) and burnout (11). However, studies that compare distress symptoms among physicians prior and during COVID-19 are scarce. These findings call for further exploration regarding the prevalence of physicians’ suicidal risk, and the factors relating to it, before and during COVID-19.
Perfectionism and other risk-factors for suicide among physicians, before and during COVID-19
Although there is abundance of research regarding risk factors for suicide among physicians, there are few studies which examine the effect of personality characteristics, which may be prevalent among physician population, on physicians’ suicidal risk. Specifically, there is a lack of research exploring the interrelationships between multiple risk factors for physician suicidality.
The literature has identified several risk factors that are consistently associated with physician suicidal behaviors. Among the multitude of factors examined in various studies, two have emerged as particularly dominant in their association with physician suicide.
Depression
Depressive symptoms were reported in high rates among medical trainees and attending physicians compared to the general population (5, 12). These symptoms tend to exacerbate, because physicians’ population usually avoid seeking help for their mental distress (13). Thus, untreated depression was found to be the most dominant risk factor in predicting deaths by suicide among physicians (14).
Burnout
The World Health Organization defines burnout as an occupational syndrome which is caused by an extreme mental and emotional reaction to work-related stress. Burnout is characterized by high emotional exhaustion, high depersonalization, and a low sense of personal accomplishment (15). Burnout is found in high rates among physicians (16, 17) and has been reported to play a dominant role in predicting depression and suicidal behaviors among this population (18, 19).
Perfectionism
Perfectionism is a personality trait that is considered as a positive quality (20), one that appears to be required to undertake the challenges of physicians’ training. However, research suggests that perfectionism is a multidimensional component which includes maladaptive dimensions that are strongly associated in the general population with depression, hopelessness, and suicidal ideation (21, 22). Frost (1990) defined two of these dimensions as Concern over Mistakes (CM) – the tendency to relate mistakes with personal failure, and Doubts about Action (DA) – tendency to self-doubt and uncertainty. Both were shown to represent aspects of excessive maladaptive perfectionism and were related to symptoms of psychopathology (22). This extreme or maladaptive perfectionism may be prevalent, especially among physicians and medical trainees, owing to their striving for excellence in training, leading them to feel vulnerable and overwhelmed (23). Accordingly, initial evidence demonstrates that maladaptive perfectionism is associated with depression and suicidal ideation among medical students (24). Therefore, expanding the knowledge regarding perfectionism and its contribution to suicidal behaviors is imperative to understand suicide among physicians. During the COVID-19 outbreak, maladaptive perfectionism may have constituted a more salient risk factor for depression and suicide, owing to the uncertainty and the sense of helplessness, which characterized a physicians’ work. The current study explored the effect of maladaptive perfectionism on physician burnout, depression, and suicidal ideation, and sought to identify pathways associated with physician suicidal ideation before and during COVID-19.
The present study
The study presented in this article was a part of comprehensive research initiated before the COVID-19 outbreak in Israel, which examined risk factors for suicidal risk among physicians. The study evaluates the effect of maladaptive perfectionism on suicidal ideation among physicians, and identifies trajectories from perfectionism to current suicidal ideation, prior and during COVID-19. Also, this article evaluates the frequencies of suicidal ideation and lifetime suicidal risk among physicians in Israel, and examines the prevalence of physicians’ current suicidal ideation, depressive and burnout symptoms before COVID-19 and during the subsequent outbreak. Three hypotheses were tested: (1) Physicians would report higher frequencies of current suicidal ideation, depressive symptoms, and burnout symptoms during COVID-19 than prior to COVID-19. (2) Maladaptive perfectionism would be positively associated with higher frequencies of depressive symptoms, burnout, and current suicidal ideation among physicians. (3) Study findings suggest a predictive model to identify the pathway between maladaptive perfectionism and suicidal ideation. COVID-19 would affect the association between burnout and depressive symptoms with current suicidal ideation among physicians characterized by high maladaptive perfectionism.
Methods
Procedures and ethical considerations
Following the receipt of Institutional Review Board (IRB) approval, we commenced the recruitment process by utilizing snowball sampling to gather participants from the pool of physicians. This involved initially approaching Israeli medical organizations and hospitals to access their mailing lists and social media platforms. Snowball sampling allowed us to extend our reach and engage with a wider network of physicians who may be interested in participating in our study. By employing this method, we aimed to ensure a diverse and representative sample of physicians for our research. All respondents participated in the study voluntarily and anonymously, after giving their consent, through computerized self-report questionnaires. All participants were given a referral sheet with the researchers’ contact information, as well as information for mental-health services, if needed.
All translated versions of the measurement tools have been validated in published articles for the Israeli language.
Materials
1. Suicidal risk was measured via the Suicide Behaviors Questionnaire revised (SBQ-R) (25). This instrument comprises four items, each covering a different dimension of suicidality: lifetime suicidal ideation and attempts; the frequency of suicidal ideation over the preceding 12 months; the threat of suicide attempts; self-reported probability of suicidal behavior in the future. Items scored on a Likert scale were summed for a final score, that ranged from 3 to 18. High scores represent greater risk for suicidal behaviors. A score of 7 or higher is considered as screening positive for “lifetime suicidal risk,” because it maximizes the rates of sensitivity and specificity for lifetime suicidal risk in non-clinical samples (25). In this study, the internal consistency of the SBQ-R was acceptable (α = 0.73).
To assess suicidal ideation during the last year, the second item in the SBQ-R “How often have you thought about killing yourself in the past year?” was used. The responses range from 1 (“never”) to 5 (“very often – five times or more”). In the current study, any response over 1 (at least once) was considered positive for suicidal ideation during the last 12 months.
2. Current suicidal ideations were estimated by the question: “During the last three months have you experienced thoughts about killing yourself / end your life? (Check: Yes/No).” Current suicidal ideation was calculated for any participants who checked “Yes” for experiencing suicidal ideation during the last 3 months.
3. Depression was assessed with the standardized and validated PHQ-8 (26). The total score is between 0 and 24 points. A total score of 0–4 represents no significant depressive symptoms. A total score of 5–9 represents mild depressive symptoms; 10–14, moderate; 15–19, moderately severe; and 20–24, current severe depression (27). In the study, a cut-off score of 10 or higher was used in order to screen positive for depressive symptoms, since it was useful in maximizing the sensitivity and specificity rates for measuring moderate–severe symptoms of depression (28). In this study, the internal consistency of PHQ-8 was good (α = 0.84).
4. Burnout symptoms were assessed via Maslach Burnout Inventory-Human Services Survey (MBI-HSS) (29). This 22-item questionnaire has three subscales evaluating three domains of burnout: emotional exhaustion (EE)- nine items (e.g., “I feel emotionally drained from my work”), depersonalization (DP) – five items (e.g., “I do not really care what happens to some patients”), and personal accomplishments (PA) – eight items (e.g., “I feel I’m positively influencing other people’s lives through my work”). All items are scored from 0 to 6 (“never” to “every day”). In this study, the added sum of EE and DP scales were used to measure burnout. The PA scale was not used in data analysis since it was considered in previous research to be less associated as a measure of burnout symptoms that are caused by work-related stress (30). In this study the cut-off scores of each scale, representing various aspects of burnout symptoms, were defined by norms for medical professionals used in previous research. Thus, screening positive for EE is defined as total score of 27 and above at this subscale, and screening positive for DP is defined as total score of 10 and above at this subscale (29). In this study, the internal consistency of MBI total score was excellent (α = 0.90), and the internal consistencies of each of the scales were good (EE α = 0.79, DP α = 0.88).
5. Maladaptive perfectionism was measured with The Frost Multidimensional Perfectionism Scale (FMPS), which is one of the most validated and widely used questionnaires for measuring perfectionism (31). It includes 35 items rated on a 5-point Likert-type scale, and measures six dimensions of perfectionism, which considered adaptive and maladaptive. In the current study the added sum of two maladaptive perfectionistic attitudinal scales were used: Concern over mistakes (CM) and Doubts about action (DA). In this study, the internal consistency of the two scales’ total score was good (α = 0.87), and the internal consistencies of each of the scales were acceptable (CM α = 0.87, DA α = 0.76).
6. Demographic data, including stage of professional training (internship, residency, or attending physicians), gender, age, and marital status were obtained from all participants. The study’s time of participation was divided into two groups: before COVID-19 (participation before March 2020—the beginning of the first quarantine in Israel) and during COVID-19 (participation after the beginning of the first quarantine).
Data analysis
Data were analyzed using IBM SPSS statistics version 26 (32), with an alpha level of 0.05 for all statistical tests. First, data were analyzed for missing data. Little’s Missing Completely at Random test (4MCAR test) (33) was non-significant, χ2 (19) = 19.76, p = 0.409, indicating that data were missing completely at random. Therefore, the maximum likelihood was used to manage the missing data, which was lower than 1.5% for all values. Differences of background variables by time (before and during COVID-19) were analyzed. An independent sample t-test was used for continuous variables and a Chi-square (χ2) test for independence or Fisher’s exact test [FIT] for categorical variables were used. In addition, Zero-order correlations were performed for associations among continuous variables. Lastly, moderated serial mediation analysis was conducted using the PROCESS macro for SPSS [model 92; (34)] in order to examine the best fitting moderated-mediation model for suicidal ideation during the last 3 months (No versus Yes). Percentile confidence intervals (CI) were estimated for the indirect effects based on 5,000 bootstrap samples of the study’s group, beyond time (before and during COVID-19). In the analysis, maladaptive perfectionism served as the independent variable, burnout and depression scores as the mediators (in serial), time (dummy coded: 0 = before COVID-19; 1 = During COVID-19) as the moderator and SI during the last 3 months as the dependent variable. Family status, stage of training (two dummy coded variables: resident and attending with intern as the reference group for both dummy variables), age and gender, served as covariates. Following Aiken and West (1991), maladaptive perfectionism, burnout and depression were mean-centered.
Results
Sample
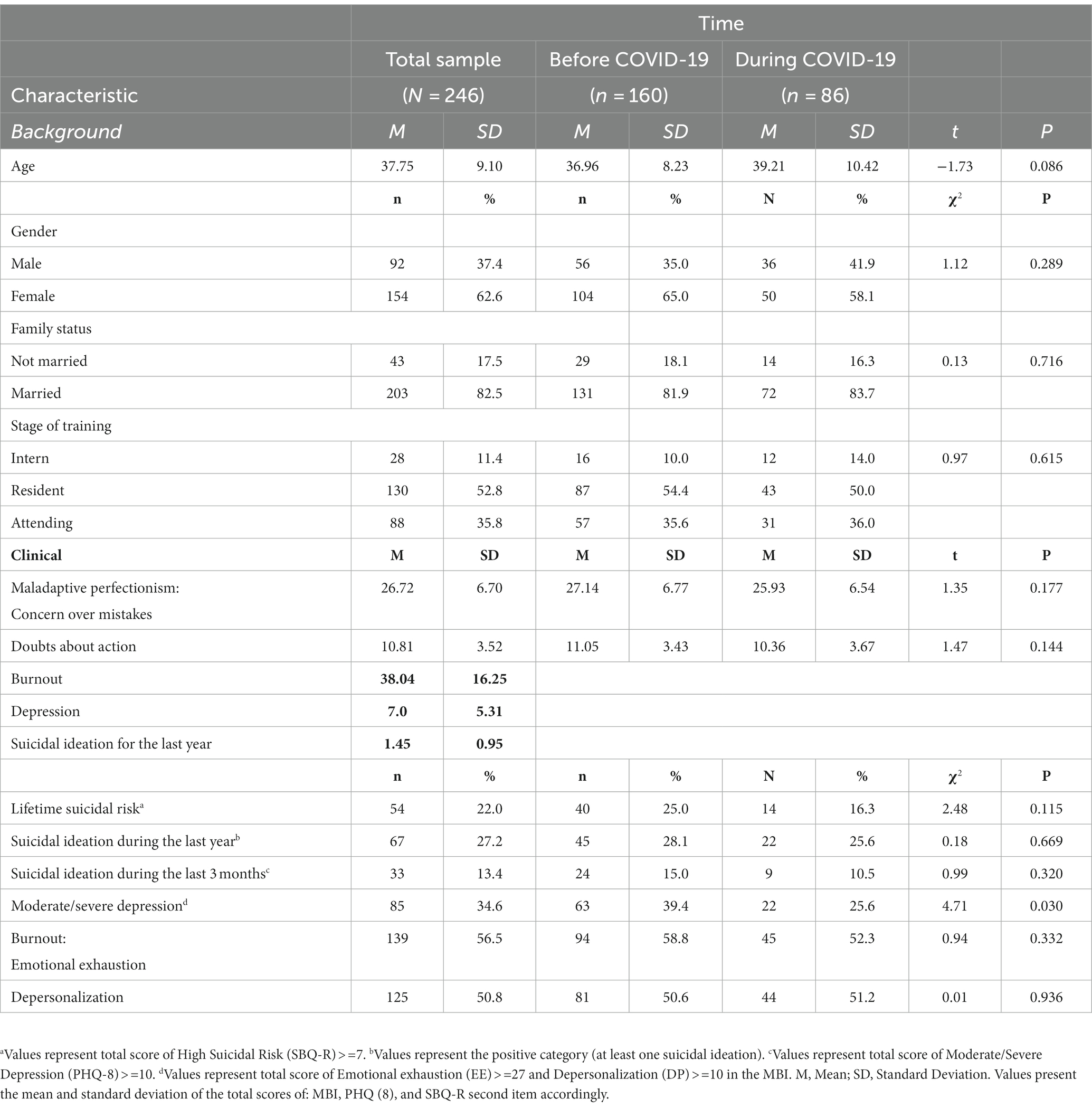
The sample included 246 physicians from various internships and hospitals in Israel who completed the survey (11.4% interns, 52.8% residents, and 35.8% attendings). Slightly above one-third (35%) of participants completed the survey after the initial COVID-19 outbreak in Israel on March 2020 (between the end of April 2020 and January 2021), while 65% of the participants completed the survey prior to the outbreak (between January and the beginning of March 2020). Most participants were married (82.5%), and their mean age was 37.75 (SD = 9.10). There were no significant differences in demographic data among the two groups (before and during COVID-19) (p > 0.05) (Table 1).
Participant clinical characteristics
Of all participants, 22.0% screened positive for lifetime suicidal risk, 27.2% had experienced suicidal ideation at least once during the previous year, and 13.4% had experienced suicidal ideation during the last 3 months. Moreover, 34.6% of all participants reported moderate to severe depressive symptoms, 56.5% had screened positive for emotional exhaustion, and 50.8% for depersonalization symptoms. Physicians were more likely to experience depressive symptoms before the outbreak than during COVID-19. No other significant differences were found before and during COVID-19 (all p’s > 0.05) (Table 1).
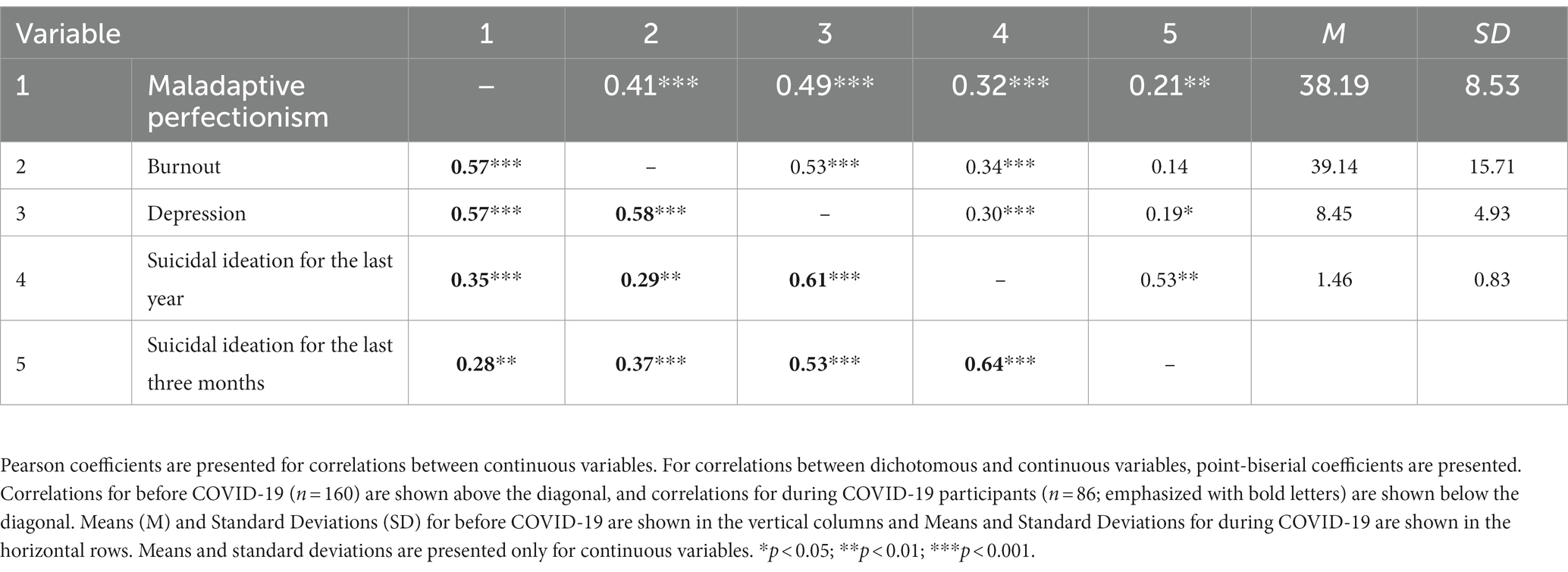
Correlations between study variables
Current suicidal ideation was positively correlated with maladaptive perfectionism, burnout, and depression before and during COVID-19. Moreover, burnout and depression were positively associated with maladaptive perfectionism and each other, before and during COVID-19. Correlations were found among perfectionism, burnout, depression, and suicidal ideation (during the last 12 and 3 months) before and during COVID-19 (Table 2).
Moderated serial mediation analysis model
As presented in the model (Figure 1), the interaction between depressive symptoms and time on current suicidal ideation was marginally significant (B = 0.24, SE = 0.12, p = 0.051), showing a positive and significant association during COVID-19 compared to non-significance before COVID-19 time period.
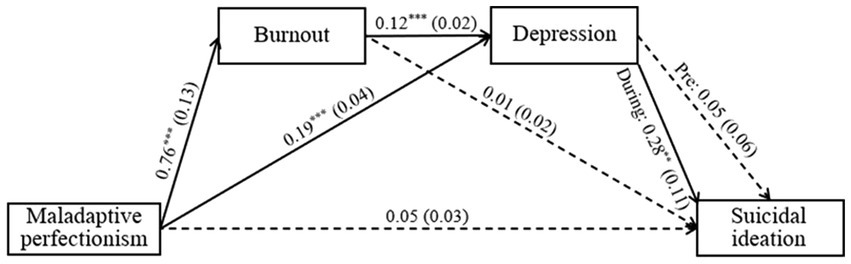
Figure 1. Moderated serial mediation model depicting the indirect effect of maladaptive perfectionism on suicidal ideations conditional to time (before and during COVID-19). N = 246. Values are unstandardised regression. In parentheses: standard errors. Solid lines indicate significant paths and dashed lines indicate nonsignificant paths. Pre, Before COVID-19; During, During COVID-19. **p < = 0.01. ***p < = 0.001.
The effect of maladaptive perfectionism on burnout and depression was positive and significant, and not statistically different between before and during COVID-19 (B = 0.24, SE = 0.21, p = 0.248 and B = 0.02, SE = 0.07, p = 0.828, respectively). The effect of maladaptive perfectionism on current suicidal ideation was non-significant and was not moderated by time (B = −0.10, SE = 0.07, p = 0.168).
In addition, the effect of burnout on depression was positive and significant, and not statistically different between before and during COVID-19 (B = 0.002, SE = 0.04, p = 0.966). The effect of burnout on suicidal ideation was non-significant and was not moderated by time (B = 0.04, SE = 0.04, p = 0.390).
As for the conditional indirect effects, the indirect effect of maladaptive perfectionism on suicidal ideation via burnout and depression was non-significant before COVID-19 (B = 0.004, SE = 0.01, bootstrapped 95% CI: −0.01, 0.02). As mentioned above, percentile confidence intervals (CI) were estimated for the indirect effects based on 5,000 bootstrap samples of the study’s group. In contrast, the serial indirect effect was positive and significant during COVID-19 (B = 0.04, SE = 0.17, bootstrapped 95% CI: 0.01, 0.58), meaning, that higher maladaptive perfectionism predicted higher burnout, which in turn predicted higher depression, which subsequently predicted higher likelihood of current suicidal ideation. Moreover, the index of moderated mediation was significant (B = 0.03, SE = 0.17, bootstrapped 95% CI: 0.003, 0.57), thus supporting the moderating role of time on the serial indirect effect. Controlling for demographic characteristics of age, gender, family status, and stage of training did not contribute to any statistically significant changes in the model, with one exception of the direct effect of maladaptive perfectionism on current suicidal ideation, which became marginally significant (B = 0.06, SE = 0.03, p = 0.080).
Discussion
This study forms part of a broader cross-sectional research endeavor aimed at investigating the relationships between personal and professional risk factors and their impact on physicians’ suicidal thoughts and behaviors. During the initial phase of participant recruitment, COVID-19 emerged in Israel, presenting physicians with unprecedented and challenging circumstances that had a profound effect on both them and their environment. It is reasonable to assume that individual characteristics would influence the stress response and distress experienced by physicians in the face of these adversities. Consequently, this article presents a unique opportunity to explore the association between maladaptive perfectionism and burnout, depression, and suicidal ideation among physicians, both before and during the COVID-19 pandemic. Additionally, this study seeks to estimate the prevalence of suicidal risk and suicidal ideation among physicians during these distinct time periods, offering valuable insights into the impact of the pandemic on their mental well-being.
Maladaptive perfectionism and its relation to burnout, depression and suicidal ideation
A main aim of the current study was to explore the effect of maladaptive perfectionism on physicians’ distress and suicidality. Our hypothesis posited that perfectionism would be a prominent risk-factor under the uncertainty and frustration that took place in physicians’ working environment during the initial outburst of COVID-19 (35). Hence, a model was suggested that would examine how maladaptive perfectionism effects physicians’ current suicidal ideation through its effect on burnout and depressive symptoms before and during COVID-19. Indeed, high maladaptive perfectionism is associated with higher rates of burnout, which in turn is associated with higher rates of depressive symptoms, before and during COVID-19. These results complement the literature discussing the risk that rigid and extreme forms of perfectionism poses for physicians’ mental health (23). While the correlation between maladaptive perfectionism and suicidal ideation was found to be highly significant, it is important to note that maladaptive perfectionism did not show a direct association with suicidal ideation, both before and during the COVID-19 period. This suggests that maladaptive perfectionism alone does not independently contribute to the prevalence of suicidal ideation. However, an intriguing finding emerged during the COVID-19 period, where burnout and depression mediated the relationship between maladaptive perfectionism and suicidal ideation. This indicates that, specifically during this challenging and stressful time, high levels of maladaptive perfectionism may lead to suicidal ideation through the pathway of increased depression. In essence, the interplay between maladaptive perfectionism, burnout, and depression becomes particularly salient during times of heightened stress, such as the COVID-19 pandemic. Considering the overall reduction in symptoms of depression among the sample during the initial waves of COVID-19, it was concluded that during these times it is imperative to identify physicians who are characterized with high maladaptive perfectionism, because they could be at an increased risk for depression and suicide. Interventions aimed at treating physicians who suffer from depression should consider perfectionism a central factor for change that will lessen suicidal risk.
Suicidal risk among physicians before and during COVID-19
Although research evidence and literature reviews over the years suggest that physicians are vulnerable to mental disorders and suicidal thoughts and behaviors, there is a lack of updated evidence-based data regarding physicians’ suicidal risk, especially during the COVID-19 outbreak (36). Moreover, recent publications that studied physician population prior to COVID-19 have reported contradictory findings regarding physician suicide rates, such as a decline in suicide over the last decades compared to the general population (26, 37, 38). Thus, there is a need to further investigate physician suicidal behaviors rates, as well as the prevalence rates of central risk-factors that contribute to suicidality among physicians. The current study’s results demonstrate high prevalence of lifetime suicidal risk among physicians in Israel, compared to other findings among the general population (39). These results are compatible with some evidence worldwide regarding physicians’ suicidal risk (40). The findings suggest prevalence rates of prolonged and current suicidal ideation among medical professionals in Israel, which are higher than other reported suicidal ideation rates among the general population (41–43) and among physicians worldwide, before as well as during the initial outbreak of COVID-19 (44). The high rates of suicidal ideation found in the current study among physicians highlight the importance of further investigation of the specific working conditions in the country’s medical system. A possible explanation for the elevation in suicidal ideation among the study’s population, could be related to several incidents of physician deaths by suicide that had occurred in Israel close in time during the year preceding the study, which had a shocking effect on physicians. Both the research and clinical literature suggest an emotional “contagion” in suicide (45, 46), which approximates the time-period of the current research that may have affected the results (47).
Contrary to the initial hypothesis of the reported study, there were no significant differences in suicidal ideation among physicians before and during the outbreak. There is a need to further explore possible explanations for these findings, perhaps through narrative studies and interviews with physicians. One explanation may be related to the fact that the study was conducted during the first waves of the COVID-19 outbreak in Israel, and that physicians may have felt a sense of meaning and importance in their work. These results resonate with Joiner’s “pulling together” phenomena that occurs during initial outbreaks and other times of crisis (48). Other explanations could be related to individual characteristics and predispositions that were not explored in this study, such as physicians’ years of professional experience (49), and history of military service, which is mandatory in Israel and may provide more resiliency in times of crisis (50). The results are compatible with other studies that found no changes concerning suicidality before and during the first waves of COVID-19 among the general population (51, 52). Some studies even found a reduction in suicidal behaviors during the initial outburst of the pandemic (53). However, studies that have been conducted during later stages of the epidemic among the general population reported an initial reduction of suicidality, followed by a rise of suicide cases during later waves (54, 55). Accordingly, medical staffs may have experienced a lapse in the sense of meaning and importance in later waves of the pandemic (56), while still facing its enduring challenges (57). That change may aggravate their distress and burnout, and eventually expose them to additional risk for suicide.
Depressive symptoms and burnout before and during COVID-19
High rates of depressive symptoms were found among the study participants, regardless of COVID-19. These rates are higher than those reported among the general population (58), which included the outbreak in Israel and worldwide (59). However, they are compatible with some recent studies among physicians and medical trainees (60, 61). About one-half of the total sample reported experiencing clinically significant burnout symptoms, that are associated with depression and suicidal ideation (62). The findings call for further investigation regarding the professional and individual reasons for which many physicians experience substantial mental distress.
The present findings suggest that physicians’ distress during the first months of the COVID-19 outbreak did not change significantly and, to some extent, might have improved, as shown by the reduction in rates of depressive symptoms among the sample. Although evidence suggest high rates of burnout, anxiety, and depression among physicians during the outbreak (11), these high frequencies of depression and other mental disorders may reflect physicians’ overall mental health beyond the impact of COVID-19. Few studies have reported that during the first waves of the pandemic, physicians who were treating COVID-19 patients experienced lower levels of burnout symptoms (63, 64). It can be postulated that physicians who worked during the initial waves of COVID-19 held a higher sense of purpose, as has been shown in studies regarding other outbursts (56). Moreover, during the beginning of the COVID-19 crisis, physicians in Israel were given a wider systematic and social support, as the public and the media applauded their work, aiding medical staffs to improve their working conditions. In addition, during COVID-19 initial outbreak, many hospitals made systematic changes in physicians’ schedules and shifts (65), which may have minimized sleep deprivation. Moreover, hospitals provided medical staffs with personal protective equipment that could have reduced anxiety symptoms (66). These changes may have had a positive impact on physicians’ mental state and well-being.
Conclusion
In the current study, high rates of suicidal ideation, depression and burnout symptoms were found among physicians in Israel, before and during COVID-19. These results reflect the vulnerability of physicians to mental distress, and the need to engage in systematic interventions to promote their overall well-being, beyond the specific challenges of COVID-19. These results highlight the importance of recognizing maladaptive perfectionism as a risk factor for poor mental health outcomes in physicians, especially during times of heightened stress and adversity. The identification and implementation of effective intervention programs should take into account the impact of maladaptive perfectionism and its potential role in exacerbating mental health challenges among physicians. By addressing maladaptive perfectionism within such programs, healthcare organizations and institutions can better support physicians’ well-being and mitigate the risk of suicidal ideation. Despite the adversities of the initial outbreak, physicians’ overall mental state during this time period had not changed and even improved in certain aspects. It can be assumed that the social support provided for physicians during the initial waves of the pandemic, had a central role in protecting their well-being. However, considering the provision of routine services needed during the prolonged battle against COVID-19, the public and systematic support physicians are receiving is thinning, while their workload continues to rise. This could place them in additional risk for mental illness and suicidality.
Limitations
The study has several limitations: First, is the use of self-reported measures. The self-reporting in the questionnaires might have affected the findings of high depression/suicidal ideation. We suggest that future research concerning physicians’ suicidal ideation should include standardized interviews to make psychiatric diagnoses. Second is the study’s cross-sectional design, which limits conclusions regarding causality. Longitudinal studies could overcome this prominent issue in future studies. Moreover, as the survey was distributed through e-mail and social media to hundreds of physicians, it was challenging to determine the study’s exact response rate. Still, it can be assumed it was substantially low, in accordance with other studies concerning physicians (67). While the recruitment method employed in our study is commonly accepted in research conducted among the physician population, it is important to acknowledge the limitations associated with the relatively small sample size and snowball sampling technique. These limitations restrict the generalizability of the findings and may introduce sampling bias, potentially impacting the accurate representation of symptoms of psychopathology among physicians. Additionally, it is worth noting that the questionnaire was distributed a few months prior to the onset of the COVID-19 outbreak in Israel, and during the initial waves of contagion. As the pandemic unfolded, there were significant changes in the work environment of physicians and the overall public response to the crisis, which could have influenced the results. Therefore, the findings of our study reflect the initial reaction of the physician population to the outbreak. Future research may provide a more comprehensive understanding of the mental state of physicians across different stages of the pandemic, allowing for a more nuanced assessment of the long-term impact of COVID-19 on physicians’ mental well-being. Finally, the relatively small sample size of physicians collected during the pandemic prevents further analysis of differences between subgroups of interest, such as first-year interns or intensive care unit physicians who were treating most cases of COVID-19 patients. However, findings from other studies in Israel that were conducted during the pandemic, suggest that emergency department physicians reported lower levels of burnout compared to physicians in internal departments, even though they were more exposed to COVID-19 patients (50).
Nonetheless, to the best of our knowledge, the current study is one of the first to address the contribution of maladaptive perfectionism to physicians’ mental distress and suicidal risk. Also, it is one of the first to provide updated information regarding suicidal risk among physicians in Israel, and to estimate the effects of COVID-19 on physicians’ suicidal ideation and depression, compared to their mental state prior the pandemic. The results demonstrate that the battle against COVID-19 was a part of a broader picture of physicians’ adversities and mental distress. Hence, there is a need for organization-directed interventions that will promote physicians’ supportive working environments during their routine work, as well as during crisis. The results also highlight the role of maladaptive perfectionism in the development and maintenance of burnout, depressive symptoms, and suicidal ideation among physicians. These findings are applicable to better identify physicians at risk and to promote intervention programs that will moderate rigid perfectionism.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board (IRB) of Bar-Ilan University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
DK-L and YG were responsible together with SH and JM for the ideas, formulation of overarching research goals and aims, design of methodology, and supervision of DK-L. DK-L conducted the research, analyzed the data, and wrote the first draft. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to thank Eran Druckman for his contribution to the study’s data analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Fink-Miller, EL, and Nestler, LM. Suicide in physicians and veterinarians: risk factors and theories. Curr Opin Psychol. (2018) 22:23–6. doi: 10.1016/j.copsyc.2017.07.019
2. Pereira-Lima, K, Mata, DA, Loureiro, SR, Crippa, JA, Bolsoni, LM, and Sen, S. Association between physician depressive symptoms and medical errors: a systematic review and meta-analysis. JAMA Netw Open. (2019) 2:e1916097. doi: 10.1001/jamanetworkopen.2019.16097
3. Abbasi, J. Prioritizing physician mental health as COVID-19 marches on. JAMA. (2020) 323:2235–6. doi: 10.1001/jama.2020.5205
4. Santarone, K, McKenney, M, and Elkbuli, A. Preserving mental health and resilience in frontline healthcare workers during COVID-19. Am J Emerg Med. (2020) 38:1530–1. doi: 10.1016/j.ajem.2020.04.030
5. Torre, DM, Wang, N-Y, Meoni, LA, Young, JH, Klag, MJ, and Ford, DE. Suicide compared to other causes of mortality in physicians. Suicide Life Threat Behav. (2005) 35:146–53. doi: 10.1521/suli.35.2.146.62878
6. Dong, M, Zhou, FC, Xu, SW, Zhang, Q, Ng, CH, Ungvari, GS, et al. Prevalence of suicide-related behaviors among physicians: a systematic review and meta-analysis. Suicide Life Threat Behav. (2020) 50:1264–75. doi: 10.1111/sltb.12690
7. Bruffaerts, R, Voorspoels, W, Jansen, L, Kessler, RC, Mortier, P, Vilagut, G, et al. Suicidality among healthcare professionals during the first COVID19 wave. J Affect Disord. (2021) 283:66–70. doi: 10.1016/j.jad.2021.01.013
8. Sun, P, Wang, M, Song, T, Wu, Y, Luo, J, Chen, L, et al. The psychological impact of COVID-19 pandemic on health care workers: a systematic review and meta-analysis. Front Psychol. (2021) 12:626547. doi: 10.3389/fpsyg.2021.626547
9. Khatun, MF, Parvin, MF, Rashid, MM-U, Alam, MS, Kamrunnahar, M, Talukder, A, et al. Mental health of physicians during COVID-19 outbreak in Bangladesh: a web-based cross-sectional survey. Front Public Health. (2021) 9:592058. doi: 10.3389/fpubh.2021.592058
10. Kang, L, Ma, S, Chen, M, Yang, J, Wang, Y, Li, R, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. (2020) 87:11–7. doi: 10.1016/j.bbi.2020.03.028
11. Barello, S, Palamenghi, L, and Graffigna, G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. (2020) 290:113129. doi: 10.1016/j.psychres.2020.113129
12. Mata, DA, Ramos, MA, Bansal, N, Khan, R, Guille, C, Di Angelantonio, E, et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA. (2015) 314:2373–83. doi: 10.1001/jama.2015.15845
13. Moutier, C. Physician mental health: an evidence-based approach to change. J Med Regulat. (2018) 104:7–13. doi: 10.30770/2572-1852-104.2.7
14. Gold, KJ, Sen, A, and Schwenk, TL. Details on suicide among US physicians: data from the national violent death reporting system. Gen Hosp Psychiatry. (2013) 35:45–9. doi: 10.1016/j.genhosppsych.2012.08.005
15. World Health Organization. Burn-Out an “Occupational Phenomenon”: International Classification of Diseases. Geneva, Switzerland: World Health Organization (2019). Available online: https://wwwwhoint/mental_health/evidence/burn-out/en/
16. Shanafelt, TD, West, CP, Dyrbye, LN, Trockel, M, Tutty, M, Wang, H, et al. Changes in burnout and satisfaction with work-life integration in physicians during the first 2 years of the COVID-19 pandemic. Mayo Clin Proc. (2022) 97:2248–58. doi: 10.1016/j.mayocp.2022.09.002
17. Kleiner, S, and Wallace, JE. Oncologist burnout and compassion fatigue: investigating time pressure at work as a predictor and the mediating role of work-family conflict. BMC Health Serv Res. (2017) 17:1–8. doi: 10.1186/s12913-017-2581-9
18. Becker, JL, Milad, MP, and Klock, SC. Burnout, depression, and career satisfaction: cross-sectional study of obstetrics and gynecology residents. Am J Obstet Gynecol. (2006) 195:1444–9. doi: 10.1016/j.ajog.2006.06.075
19. Stehman, CR, Testo, Z, Gershaw, RS, and Kellogg, AR. Burnout, drop out, suicide: physician loss in emergency medicine, part I. Western J Emerg Med. (2019) 20:485–94. doi: 10.5811/westjem.2019.4.40970
20. Flett, GL, and Hewitt, PL. Managing perfectionism and the excessive striving that undermines flourishing: implications for leading the perfect life. Flourishing in life, work and careers : Cheltenham, United Kingdom: Edward Elgar Publishing; (2015). p. 45–66.
21. Adkins, KK, and Parker, W. Perfectionism and suicidal preoccupation. J Pers. (1996) 64:529–43. doi: 10.1111/j.1467-6494.1996.tb00520.x
22. Smith, MM, Sherry, SB, Chen, S, Saklofske, DH, Mushquash, C, Flett, GL, et al. The perniciousness of perfectionism: a meta-analytic review of the perfectionism–suicide relationship. J Pers. (2018) 86:522–42. doi: 10.1111/jopy.12333
23. Myers, MF, and Gabbard, GO. The physician as patient: a clinical handbook for mental health professionals. Washington, DC, USA: American Psychiatric Publication (2008).
24. Enns, MW, Cox, BJ, Sareen, J, and Freeman, P. Adaptive and maladaptive perfectionism in medical students: a longitudinal investigation. Med Educ. (2001) 35:1034–42. doi: 10.1046/j.1365-2923.2001.01044.x
25. Osman, A, Bagge, CL, Gutierrez, PM, Konick, LC, Kopper, BA, and Barrios, FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment. (2001) 8:443–54. doi: 10.1177/107319110100800409
26. Dutheil, F, Aubert, C, Pereira, B, Dambrun, M, Moustafa, F, Mermillod, M, et al. Suicide among physicians and health-care workers: a systematic review and meta-analysis. PLoS One. (2019) 14:e0226361. doi: 10.1371/journal.pone.0226361
27. Kroenke, K, Spitzer, RL, and Williams, JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
28. Kroenke, K, Strine, TW, Spitzer, RL, Williams, JB, Berry, JT, and Mokdad, AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. (2009) 114:163–73. doi: 10.1016/j.jad.2008.06.026
29. Maslach, C. Maslach burnout inventory-human services survey (MBI-HSS). MBI Manual. (1996):192–8.
30. Schaufeli, WB, and Taris, TW. The conceptualization and measurement of burnout: common ground and worlds apart. Work Stress. (2005) 19:256–62. doi: 10.1080/02678370500385913
31. Frost, RO, Marten, P, Lahart, C, and Rosenblate, R. The dimensions of perfectionism. Cogn Ther Res. (1990) 14:449–68. doi: 10.1007/BF01172967
32. SPSS I. Statistics for Macintosh (Version 26.0)[Computer Software]. Armonk, NY: IBM Corp (2019).
33. Little, RJ. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc. (1988) 83:1198–202. doi: 10.1080/01621459.1988.10478722
34. Hayes, AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York, NY: Guilford Publications (2017).
35. Bashkin, O, Davidovitch, N, Asna, N, Schwartz, D, and Dopelt, K. The organizational atmosphere in Israeli hospital during COVID-19: concerns, perceptions, and burnout. Int J Environ Res Public Health. (2021) 18:5544. doi: 10.3390/ijerph18115544
36. Leung, TI, Kuhn, T, and Dumontier, M. Representing physician suicide claims as nanopublications: proof-of-concept study creating claim networks. JMIRx Med. (2022) 3:e34979. doi: 10.2196/34979
37. Duarte, D, El-Hagrassy, MM, TCE, C, Gurgel, W, Fregni, F, and Correa, H. Male and female physician suicidality: a systematic review and meta-analysis. JAMA Psychiatry. (2020) 77:587–97. doi: 10.1001/jamapsychiatry.2020.0011
38. Davis, MA, Cher, BA, Friese, CR, and Bynum, JP. Association of US nurse and physician occupation with risk of suicide. JAMA Psychiat. (2021) 78:651–8. doi: 10.1001/jamapsychiatry.2021.0154
39. Blüml, V, Kapusta, ND, Doering, S, Brähler, E, Wagner, B, and Kersting, A. Personality factors and suicide risk in a representative sample of the German general population. PLoS One. (2013) 8:e76646. doi: 10.1371/journal.pone.0076646
40. Hem, E, Grønvold, NT, Aasland, OG, and Ekeberg, Ø. The prevalence of suicidal ideation and suicidal attempts among Norwegian physicians. Results from a cross-sectional survey of a nationwide sample. Eur Psychiatry. (2000) 15:183–9. doi: 10.1016/S0924-9338(00)00227-3
41. Levinson, D, Haklai, Z, Stein, N, Polakiewicz, J, and Levav, I. Suicide ideation, planning and attempts: results from the Israel National Health Survey. Isr J Psychiatry Relat Sci. (2007) 44:136–43.
42. Wu, R, Zhu, H, Wang, Z-J, and Jiang, C-L. A large sample survey of suicide risk among university students in China. BMC Psychiatry. (2021) 21:1–9. doi: 10.1186/s12888-021-03480-z
43. Bryan, CJ, Bryan, AO, and Baker, JC. Associations among state-level physical distancing measures and suicidal thoughts and behaviors among US adults during the early COVID-19 pandemic. Suicide Life Threat Behav. (2020) 50:1223–9. doi: 10.1111/sltb.12653
44. Al-Humadi, S, Bronson, B, Muhlrad, S, Paulus, M, Hong, H, and Cáceda, R. Depression, suicidal thoughts, and burnout among physicians during the COVID-19 pandemic: a survey-based cross-sectional study. Acad Psychiatry. (2021) 45:557–65. doi: 10.1007/s40596-021-01490-3
45. Haw, C, Hawton, K, Niedzwiedz, C, and Platt, S. Suicide clusters: a review of risk factors and mechanisms. Suicide Life Threat Behav. (2013) 43:97–108. doi: 10.1111/j.1943-278X.2012.00130.x
46. Maple, M, Cerel, J, Sanford, R, Pearce, T, and Jordan, J. Is exposure to suicide beyond kin associated with risk for suicidal behavior? A systematic review of the evidence. Suicide Life Threat Behav. (2017) 47:461–74. doi: 10.1111/sltb.12308
47. Laramée, J, and Kuhl, D. Suicidal ideation among family practice residents at the University of British Columbia. Can Fam Physician. (2019) 65:730–5.
48. Joiner, TE Jr, Hollar, D, and Orden, KV. On Buckeyes, Gators, Super Bowl Sunday, and the Miracle on Ice:“Pulling together” is associated with lower suicide rates. J Soc Clin Psychol. (2006) 25:179–95. doi: 10.1521/jscp.2006.25.2.179
49. Gawrych, M, Cichoń, E, and Kiejna, A. Mental health predictors of medical staff in the early stage of COVID-19 pandemic in Poland. Arch Psychiatry Psychother. (2023) 25:42–53. doi: 10.12740/APP/156923
50. Trotzky, D, Aizik, U, Mosery, J, Carady, N, Tavori, G, Cohen, A, et al. Resilience of hospital staff facing COVID-19 pandemic: lessons from Israel. Front Public Health. (2023) 11:1050261. doi: 10.3389/fpubh.2023.1050261
51. John, A, Eyles, E, Webb, RT, Okolie, C, Schmidt, L, Arensman, E, et al. The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: update of living systematic review. F1000Res. (2021) 9:1097. doi: 10.12688/f1000research.25522.2
52. Killgore, WD, Cloonan, SA, Taylor, EC, Allbright, MC, and Dailey, NS. Trends in suicidal ideation over the first three months of COVID-19 lockdowns. Psychiatry Res. (2020) 293:113390. doi: 10.1016/j.psychres.2020.113390
53. Sueki, H, and Ueda, M. Short-term effect of the COVID-19 pandemic on suicidal ideation. Crisis. (2022) 43:315–322. doi: 10.1027/0227-5910/a000797
54. Tanaka, T, and Okamoto, S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat Hum Behav. (2021) 5:229–38. doi: 10.1038/s41562-020-01042-z
55. Ueda, M, Nordström, R, and Matsubayashi, T. Suicide and mental health during the COVID-19 pandemic in Japan. J Public Health. (2022) 44:541–8. doi: 10.1093/pubmed/fdab113
56. Sanghera, J, Pattani, N, Hashmi, Y, Varley, KF, Cheruvu, MS, Bradley, A, et al. The impact of SARS-CoV-2 on the mental health of healthcare workers in a hospital setting-A Systematic Review. J Occup Health. (2020) 62:e12175. doi: 10.1002/1348-9585.12175
57. Cox, CL. ‘Healthcare Heroes’: problems with media focus on heroism from healthcare workers during the COVID-19 pandemic. J Med Ethics. (2020) 46:510–3. doi: 10.1136/medethics-2020-106398
58. Cao, C, Hu, L, Xu, T, Liu, Q, Koyanagi, A, Yang, L, et al. Prevalence, correlates and misperception of depression symptoms in the United States, NHANES 2015–2018. J Affect Disord. (2020) 269:51–7. doi: 10.1016/j.jad.2020.03.031
59. Vindegaard, N, and Benros, ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. (2020) 89:531–42. doi: 10.1016/j.bbi.2020.05.048
60. Zhang, H, Ye, Z, Tang, L, Zou, P, Du, C, Shao, J, et al. Anxiety symptoms and burnout among Chinese medical staff of intensive care unit: the moderating effect of social support. BMC Psychiatry. (2020) 20:197. doi: 10.1186/s12888-020-02603-2
61. Ofei-Dodoo, S, Loo-Gross, C, and Kellerman, R. Burnout, depression, anxiety, and stress among family physicians in kansas responding to the COVID-19 pandemic. J Am Board Fam Med. (2021) 34:522–30. doi: 10.3122/jabfm.2021.03.200523
62. Rotenstein, LS, Torre, M, Ramos, MA, Rosales, RC, Guille, C, Sen, S, et al. Prevalence of burnout among physicians: a systematic review. JAMA. (2018) 320:1131–50. doi: 10.1001/jama.2018.12777
63. Dinibutun, SR. Factors associated with burnout among physicians: an evaluation during a period of COVID-19 pandemic. J Healthcare Leadership. (2020) 12:85–94. doi: 10.2147/JHL.S270440
64. Wu, Y, Wang, J, Luo, C, Hu, S, Lin, X, Anderson, AE, et al. A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in Wuhan, China. J Pain Symptom Manag. (2020) 60:e60–5. doi: 10.1016/j.jpainsymman.2020.04.008
65. Hu, X, and Dill, MJ. Changes in physician work hours and patterns during the COVID-19 pandemic. JAMA Netw Open. (2021) 4:e2114386. doi: 10.1001/jamanetworkopen.2021.14386
66. Aslanidis, V, Tsolaki, V, Papadonta, ME, Amanatidis, T, Parisi, K, Makris, D, et al. The impact of the COVID-19 pandemic on mental health and quality of life in COVID-19 department healthcare workers in Central Greece. J Pers Med. (2023) 13:250. doi: 10.3390/jpm13020250
Keywords: physicians, COVID-19, perfectionism, suicidal ideation, suicidal riskfactors, practitioner burnout
Citation: Kleinhendler-Lustig D, Hamdan S, Mendlovic J and Gvion Y (2023) Burnout, depression, and suicidal ideation among physicians before and during COVID-19 and the contribution of perfectionism to physicians’ suicidal risk. Front. Psychiatry. 14:1211180. doi: 10.3389/fpsyt.2023.1211180
Edited by:
Reza Lashgari, Shahid Beheshti University, IranReviewed by:
Keith V. Bletzer, Arizona State University, United StatesAgata Ewa Chudzicka-Czupała, SWPS University of Social Sciences and Humanities, Poland
Copyright © 2023 Kleinhendler-Lustig, Hamdan, Mendlovic and Gvion. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dafna Kleinhendler-Lustig, RGFmbmEubHVzdGlnQGdtYWlsLmNvbQ==
†ORCID: Joseph Mendlovic https://orcid.org/0000-0002-6319-141X
Yari Gvion https://orcid.org/0000-0003-1269-6415
 Dafna Kleinhendler-Lustig
Dafna Kleinhendler-Lustig Sami Hamdan
Sami Hamdan Joseph Mendlovic3,4†
Joseph Mendlovic3,4† Yari Gvion
Yari Gvion