- 1Center of Innovation in Long Term Services and Supports, VA Providence Healthcare System, Providence, RI, United States
- 2Department of Psychiatry and Human Behavior, Alpert Medical School of Brown University, Providence, RI, United States
- 3Geriatric Research, Education and Clinical Center, Durham VA Health Care System, Durham, NC, United States
- 4Durham VA Health Care System, Durham, NC, United States
- 5Department of Psychiatry and Behavioral Sciences, Duke University School of Medicine, Durham, NC, United States
- 6Center for Psychiatric Rehabilitation and Departments of Occupational Therapy, Psychology, and Psychiatry, Boston University, Boston, MA, United States
- 7Department of Health Services, Policy & Practice, Brown University, Providence, RI, United States
- 8Medical Service, VA Providence Healthcare System, Providence, RI, United States
- 9VA RR&D Center for Neurorestoration and Neurotechnology, VA Providence Healthcare System, Providence, RI, United States
- 10Mental Illness Research, Education and Clinical Center, VA Greater Los Angeles, Los Angeles, CA, United States
- 11Department of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles, Los Angeles, CA, United States
- 12Center for the Study of Aging and Human Development, Duke University School of Medicine, Durham, NC, United States
Older adults with serious mental illness (SMI) have compromised physical function that could be improved with exercise; however, retention in exercise programs is a challenge. This study was a retrospective analysis of retention for the 150 older veterans with SMI that enrolled in Gerofit, a clinical exercise program offered in the Veterans Health Administration. Chi-square and t-tests were conducted to evaluate baseline differences between those that were and were not retained at six and 12 months. Retention was 33% and better health-related quality of life and endurance were related to retention. Future work is needed to improve exercise program retention in this population.
1. Introduction
Older people with serious mental illness (SMI) have mental and physical health challenges that reduce their functioning and quality of life (QOL) (1, 2). The physical functional decline in this group includes compromised endurance, strength, and mobility (3), which predict disability and mortality (4, 5). Exercise improves physical function in older adults (6) and in people with SMI (7); however, retention remains a major challenge for the SMI population (8).
Mental health symptoms, low motivation, medical concerns, medication side effects, and social isolation are obstacles to exercise engagement for people with SMI (9, 10). Disparities in access to quality care, which disproportionately affect Black adults (11), further exacerbate the health burden of SMI (12) and contribute to low participation in exercise and lifestyle programs (13–15). To address these barriers, many exercise and lifestyle programs for this group are offered at accessible locations (e.g., mental health clinics), include motivational components, and provide opportunities for social support (16, 17). Yet, most work has focused on young and middle-aged adults within research studies, and there is a lack of information on retention of older people with SMI in real-world exercise programs.
The purpose of this study was to examine retention of older veterans with SMI in Gerofit, an effective outpatient clinical exercise program available to eligible older veterans enrolled in the Veterans Health Administration (VHA) (18–20). The study aimed to evaluate differences in demographic and baseline health characteristics between older veterans with SMI that were and were not retained at six- and 12-months post-enrollment. We hypothesized that race (White), age (younger), SMI diagnosis (recurrent major depressive disorder), and baseline health status (fewer medical comorbidities, better physical function, and health-related QOL) would be associated with retention.
2. Method
2.1. Study design and participants
This study was a retrospective analysis approved by Institutional Review Boards at the Durham and Providence VA Healthcare Systems.
Veterans are eligible for Gerofit if they (a) are aged 65 or older, (b) are medically stable, and (c) have their own transportation. They are not eligible if they (a) are unable to independently perform activities of daily living, (b) experience cognitive impairment preventing safe exercise, (c) have any medical conditions for which exercise is contraindicated (e.g., unstable angina, active proliferative diabetic retinopathy, oxygen dependence, frank incontinence, active open wounds), (d) have an active substance use disorder, (e) are experiencing homelessness, (f) are unable to successfully participate in a group setting, and (g) are experiencing behavioral concerns that impact group participation (18, 21).
2.2. Gerofit program
Gerofit is a supervised, outpatient clinical exercise program offered in the VHA free of cost (21) except that veterans must have their own transportation to participate. Enrolled veterans complete an initial performance-based assessment of their functional capacity. Results of this initial assessment guide the creation of an individualized exercise prescription that include movements targeting endurance, strength, and mobility. Veterans are encouraged to complete their prescription multiple times per week in a group-based setting. Trained exercise staff provide supervision at gym facilities during specific hours.
2.3. Measures
2.3.1. Retention
Six- and 12-month retention was defined as completion of the Gerofit assessment at the specified timepoint. Assessment completion is an adequate indicator of retention because testing is a core component of the Gerofit program and guides the exercise prescription (22).
2.3.2. Baseline variables
Demographics (age, sex, race, ethnicity, marital status), SMI diagnosis (schizophrenia, schizoaffective disorder, bipolar disorder, recurrent major depressive disorder), psychiatric medication prescriptions (antipsychotics, mood stabilizers, antidepressants), and medical comorbidities (count of 26 possible medical conditions) (23) were obtained from the VHA electronic health record for the year prior to Gerofit enrollment.
Performance-based physical function measures included the six-minute walk test (endurance), 30-s arm curls and chair stands (strength), and the 8-foot-up-and-go and 10-meter walk tests (mobility) (24–26). Health-related QOL was assessed with the Patient-Reported Outcomes Measurement Information System Global Health Short Form (PROMIS) (27), which includes a single-item indicator of general health and three subscales (mental health, physical health, and satisfaction with social roles). These measures are completed at the Gerofit assessment.
2.4. Procedure
VHA clinical providers refer veterans to Gerofit. Gerofit staff assess eligibility through chart review followed by a phone screening. Interested and eligible veterans are then scheduled for a baseline assessment completed at the health facility.
2.5. Data analysis
Analyses were conducted with SAS (Version 9.4). Differences in baseline variables between older veterans with SMI that were and were not retained at six and 12 months were assessed with independent sample t-tests for continuous and chi-square tests for categorical variables.
3. Results
3.1. Participants
The sample included 150 older veterans with SMI (out of 1,414 total older veterans) that enrolled in Gerofit between 2010 and 2019 across eight VA sites (two northeast, two southeast, four west). The sample was, on average, 70 years old (SD = 5.4), predominately male (91%), White (53%) or Black (43%), not Hispanic or Latinx (95%), and not married (57%). Sixty-one percent had three or more medical comorbidities, 75% had a recurrent major depressive disorder diagnosis, and 77% had an antidepressant medication prescription. Retention was 33% at six and 12 months.
3.2. Baseline differences by retention status
Older veterans with SMI who were retained at 6 months had better health-related QOL on the PROMIS: general health [t (122) = −2.29, p = 0.02], physical health [t (43) = −2.12, p = 0.04], mental health [t (43) = −3.61, p = 0.001], and satisfaction with social roles [t (42) = −3.52, p = 0.001] than those who were not retained. None of the other measures were significantly related to six-month retention (all ps > 0.05) (Table 1).
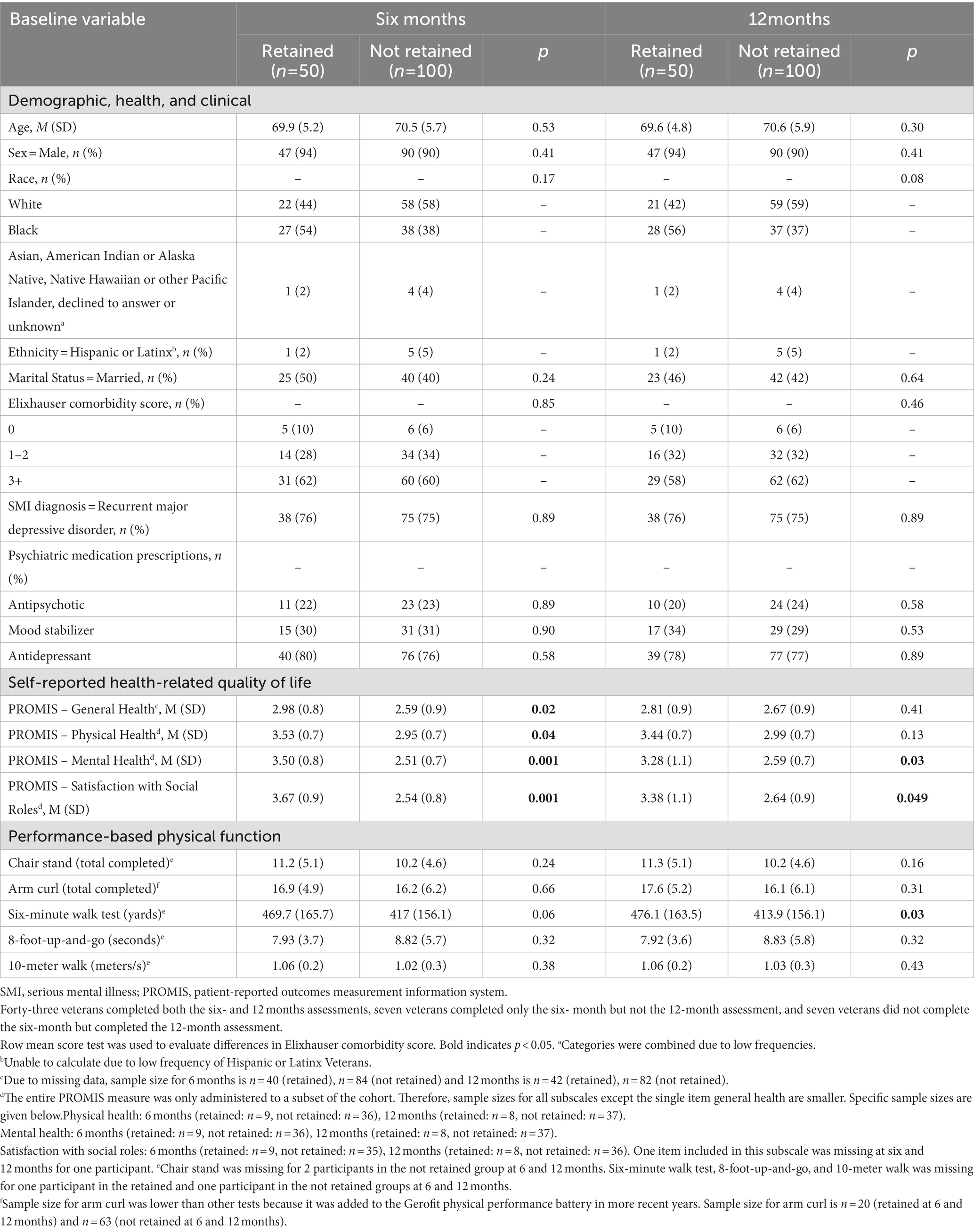
Table 1. Comparison of baseline characteristics between older Veterans with SMI that were retained versus not retained at six and 12 months in Gerofit.
Older veterans with SMI who were retained at 12 months had better health-related QOL on the PROMIS mental health [t (43) = −2.25, p = 0.03] and satisfaction with social roles [t (42) = −2.03, p = 0.049] subscales than those that were not retained. Those who were retained had better endurance on the six-minute walk test [t (146) = −2.25, p = 0.03] than those who were not retained. None of the other measures were significantly related to 12-month retention (all ps > 0.05) (Table 1).
4. Discussion
This study examined retention of older veterans with SMI in a supervised exercise program. Retention was 33%; but 86% percent of veterans with SMI that were retained at six months remained in the program to 12 months. Better baseline health-related QOL and endurance were the only variables associated with retention. These findings highlight the need for additional tailoring of clinical exercise programming to better retain the older veteran population with SMI, particularly during the first six months and for those with lower initial QOL and endurance.
Our retention rate of 33% is much lower than those reported in large SMI health promotion trials (≥68%) (28, 29, 30). The present analysis focused on retention in a free-of-cost clinical exercise program without any monetary incentives and was not conducted as a research trial where dedicated outreach and compensation for assessments are often standard. Further, Gerofit is designed broadly for older veterans and does not include specific tailoring for the SMI population. Nonetheless, the low retention rate is surprising given that Gerofit does address many established barriers to exercise for the SMI population (e.g., social support, access, cost, supervision) (8, 9). These findings suggest that there are SMI-specific barriers to exercise engagement that are not adequately addressed in Gerofit, which may include, among others, unreliable transportation and low motivation (31).
Better health-related QOL and endurance were the only baseline characteristics that distinguished retention status. Prior research has also shown that better self-reported physical health but not specific medical conditions were related to greater exercise in SMI (32, 33). None of the demographic or mental health variables were related to retention. Homogeneity of our sample with respect to age and SMI diagnosis may have obscured potential relationships. But, the non-significant relationship between race and retention is consistent with prior work showing reduced racial disparities between Black and White older veterans with SMI in a VHA clinical program compared to other programs (34). As such, Gerofit may reduce racial disparities in retention through its cost-free availability to older veterans.
The sample comprised mainly male veterans although the racial diversity of Gerofit is a strength. Further, we did not have data on exercise attendance or adherence. Finally, aside from the general health single item, the PROMIS scale was only administered to a subset of participants. Future exercise programs for this population should consider alternate strategies to enhance retention in the SMI population. For example, home-based models of exercise are effective for older adults and improve engagement by limiting the need for transportation (35, 36). In fact, home-based programs that include motivational strategies have shown initial promise for those with SMI in improving engagement and targeting the well-established motivational difficulties present for this group (37). Therefore, future exercise programs developed for the older population with SMI should consider home-based or hybrid (i.e., combination home-based and facility-based) modalities in tandem with activities targeting motivation to improve retention. Overall, this study highlights an opportunity to modify existing clinical exercise programming for older veterans to address the unmet needs of the older SMI population.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Boards at Durham and Providence VA Healthcare Systems. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
JB, EE, KM, and KH conceptualized the study. RS conducted the data analyses. JB wrote the first draft. JR, WCW, NP, WM, and AY provided the feedback and input on the analytical interpretation and manuscript writing. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by a VA Rehabilitation Research and Development Career Development Award (IK1RX003904) to JB. The Durham Gerofit program has been locally supported by the Durham VA Geriatric, Research, Education and Clinical Program, and KH is supported in part by VA RR&D (RX003120), and the Duke Claude D. Pepper Older Americans Independence Center (NIA P30 AG028716), and the Duke Roybal Center (NIA P30 AG064201).
Acknowledgments
We would like to thank all the Veterans who participated in Gerofit and the staff from Gerofit sites in Baltimore, Denver, Durham, Honolulu, Los Angeles, Canandaigua, Pittsburgh, and Puget Sound. We are grateful to the VA offices and centers that have supported the Gerofit dissemination efforts: Office of Geriatrics and Extended Care Mentored Partnerships Program; Geriatric Research, Education and Clinical Center; Office of Rural Health Enterprise-Wide Initiatives; and Whole Health. We would also like to acknowledge the Durham Implementation Team, in particular Stephen Jennings, for their data management assistance. We would also like to thank Orna Intrator and Jiejin Li at the Geriatrics and Extended Care Data Analysis Center for their valuable analytic support of this work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the United States Government or Department of Veterans Affairs.
References
1. Bartels, SJ, DiMilia, PR, Fortuna, KL, and Naslund, JA. Integrated care for older adults with serious mental illness and medical comorbidity: evidence-based models and future research directions. Psychiatr Clin North Am. (2018) 41:153–64. doi: 10.1016/j.psc.2017.10.012
2. Hendrie, HC, Hay, D, Lane, KA, Gao, S, Purnell, C, Munger, S, et al. Comorbidity profile and health care utilization in elderly patients with serious mental illnesses. Am J Geriatr Psychiatry. (2014) 21:1–14. doi: 10.1097/JGP.0b013e31826d6937
3. Browne, J, Elbogen, EB, Mueser, KT, Rudolph, JL, Wu, WC, Philip, NS, et al. Physical function assessment of older veterans with serious mental illness. Am. J. Geriatr Psychiatry. (2023) advance online publication. doi: 10.1016/j.jagp.2023.02.048
4. Groessl, EJ, Kaplan, RM, Rejeski, WJ, Katula, JA, Glynn, NW, King, AC, et al. Physical activity and performance impact long-term quality of life in older adults at risk for major mobility disability. Am J Prev Med. (2019) 56:141–6. doi: 10.1016/j.amepre.2018.09.006
5. Studenski, S, Perera, S, Patel, K, Rosano, C, Faulkner, K, and Inzitari, M. Gait speed and survival in older adults. J Am Med Assoc. (2011) 305:50–8. doi: 10.1001/jama.2010.1923
6. Giné-Garriga, M, Roqué-Fíguls, M, Coll-Planas, L, Sitjà-Rabert, M, and Salvà, A. Physical exercise interventions for improving performance-based measures of physical function in community-dwelling, frail older adults: a systematic review and meta-analysis. Arch Phys Med Rehabil. (2014) 95:753–769.e3. doi: 10.1016/j.apmr.2013.11.007
7. Vancampfort, D, Rosenbaum, S, Schuch, F, Ward, PB, Richards, J, Mugisha, J, et al. Cardiorespiratory fitness in severe mental illness: a systematic review and meta-analysis. Sport Med. (2017) 47:343–52. doi: 10.1007/s40279-016-0574-1
8. Vancampfort, D, Rosenbaum, S, Schuch, FB, Ward, PB, Probst, M, and Stubbs, B. Prevalence and predictors of treatment dropout from physical activity interventions in schizophrenia: a meta-analysis. Gen Hosp Psychiatry. (2016) 39:15–23. doi: 10.1016/j.genhosppsych.2015.11.008
9. Firth Rosenbaum, S, Stubbs, B, Gorczynski, P, Yung, AR, and Vancampfort, D. Motivating factors and barriers towards exercise in severe mental illness: a systematic review and meta-analysis. Psychol Med. (2016) 46:2869–81. doi: 10.1017/S0033291716001732
10. Soundy, A, Freeman, P, Stubbs, B, Probst, M, Coffee, P, and Vancampfort, D. The transcending benefits of physical activity for individuals with schizophrenia: a systematic review and meta-ethnography. Psychiatry Res. (2014) 220:11–9. doi: 10.1016/j.psychres.2014.07.083
11. Maura, J, and Weisman de Mamani, A. Mental health disparities, treatment engagement, and attrition among racial/ethnic minorities with severe mental illness: a review. J Clin Psychol Med Settings. (2017) 24:187–210. doi: 10.1007/s10880-017-9510-2
12. Sayer, J, Paniagua, D, Ballentine, S, Sheehan, L, Carson, M, Nieweglowski, K, et al. Perspectives on diet and physical activity among urban African Americans with serious mental illness. Soc Work Health Care. (2019) 58:509–25. doi: 10.1080/00981389.2019.1587662
13. Cabassa, LJ, Ezell, JM, and Lewis-Fernandez, R. Lifestyle interventions for adults with serious mental illness: a systematic literature review. Psychiatr Serv. (2010) 61:774–82. doi: 10.1176/ps.2010.61.8.774
14. Olmos-Ochoa, TT, Niv, N, Hellemann, G, Cohen, AN, Oberman, R, Goldberg, R, et al. Barriers to participation in web-based and in-person weight management interventions for serious mental illness. Psychiatr Rehabil J. (2019) 42:220–8. doi: 10.1037/prj0000363
15. Stefancic, A, Bochicchio, L, Tuda, D, Gurdak, K, and Cabassa, LJ. Participant experiences with a peer-led healthy lifestyle intervention for people with serious mental illness. Psychiatr Serv. (2021) 72:530–8. doi: 10.1176/appi.ps.202000311
16. Bartels, SJ. Can behavioral health organizations change health behaviors? The STRIDE study and lifestyle interventions for obesity in serious mental illness. Am J Psychiatry. (2015) 172:9–11. doi: 10.1176/appi.ajp.2014.14101246
17. Rosenbaum Tiedemann, A, Sherrington, C, Curtis, J, and Ward, PB. Physical activity interventions for people with mental illness: a systematic review and meta-analysis. J Clin Psychiatry. (2014) 75:964–74. doi: 10.4088/JCP.13r08765
18. Addison, O, Serra, MC, Katzel, L, Giffuni, J, Lee, CC, Castle, S, et al. Mobility improvements are found in older veterans after 6 months of gerofit regardless of body mass index classification. J Aging Phys Act. (2019) 27:848–54. doi: 10.1123/japa.2018-0317
19. Morey, MC, Cowper, PA, Feussner, JR, DiPasquale, RC, Crowley, GM, Samsa, GP, et al. Two-year trends in physical performance following supervised exercise among community-dwelling older veterans. J Am Geriatr Soc. (1991) 39:986–92. doi: 10.1111/j.1532-5415.1991.tb04045.x
20. Morey, MC, Robert, JS, Crowley, GM, Cowper, PA, and Robbins, MS. Five-year performance trends for older exercisers: a hierarchical model of endurance, strength, and flexibility. J Am Geriatr Soc. (1996) 44:1226–31. doi: 10.1111/j.1532-5415.1996.tb01374.x
21. Morey, MC, Lee, CC, Castle, S, Valencia, WM, Katzel, L, Giffuni, J, et al. Should structured exercise be promoted as a model of care? Dissemination of the Department of Veterans Affairs Gerofit Program. J Am Geriatr Soc. (2018) 66:1009–16. doi: 10.1111/jgs.15276
22. Brown, CS, Sloane, R, and Morey, MC. Developing predictors of long-term adherence to exercise among older veterans and spouses. J Appl Gerontol. (2020) 39:1159–62. doi: 10.1177/0733464819874954
23. Elixhauser, A, Steiner, C, Harris, DR, and Coffey, RM. Comorbidity measures for use with administrative data. Med Care. (1998) 36:8–27. doi: 10.1097/00005650-199801000-00004
24. Middleton, A, Fritz, SL, and Lusardi, M. Walking speed: the functional vital sign. J Aging Phys Act. (2015) 23:314–22. doi: 10.1123/japa.2013-0236
25. Peters, DM, Fritz, SL, and Krotish, DE. Assessing the reliability and validity of a shorter walk test compared with the 10-meter walk test for measurements of gait speed in healthy, older adults. J Geriatr Phys Ther. (2013) 36:24–30. doi: 10.1519/JPT.0b013e318248e20d
26. Rikli, RE, and Jones, CJ. Development and validation of a functional fitness test for community-residing older adults. J Aging Phys Act. (1999) 7:129–61. doi: 10.1123/japa.7.2.129
27. Hays, RD, Bjorner, JB, Revicki, DA, Spritzer, KL, and Cella, D. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual Life Res. (2009) 18:873–80. doi: 10.1007/s11136-009-9496-9
28. Bartels, SJ, Pratt, SI, Aschbrenner, KA, Barre, LK, Naslund, JA, Wolfe, R, et al. Pragmatic replication trial of health promotion coaching for obesity in serious mental illness and maintenance of outcomes. Am J Psychiatry. (2015) 172:344–52. doi: 10.1176/appi.ajp.2014.14030357
29. Daumit Dickerson, FB, Wang, NY, Dalcin, A, Jerome, GJ, Anderson, CA, et al. A behavioral weight-loss intervention in persons with serious mental illness. N Engl J Med. (2013) 368:1594–602. doi: 10.1056/NEJMoa1214530
30. Young, AS, Cohen, AN, and Goldberg, R. Improving weight in people with serious mental illness: the effectiveness of computerized services with peer coaches. J Gen Intern Med. (2017) 32:48–55.
31. Browne, J, Mihas, P, and Penn, DL. Focus on exercise: client and clinician perspectives on exercise in individuals with serious mental illness. Community Ment Health J. (2016) 52:387–94. doi: 10.1007/s10597-015-9896-y
32. Cabassa, LJ, Stefancic, A, Wang, X, Guo, S, Lu, NY, and Weatherly, C. Correlates of physical activity and cardiorespiratory fitness in racially and ethnically diverse people with serious mental illness in supportive housing. Community Ment Health J. (2020) 56:1139–52. doi: 10.1007/s10597-020-00610-x
33. Mishu, MP, Peckham, EJ, Heron, PN, Tew, GA, Stubbs, B, and Gilbody, S. Factors associated with regular physical activity participation among people with severe mental ill health. Soc Psychiatry Psychiatr Epidemiol. (2019) 54:887–95. doi: 10.1007/s00127-018-1639-2
34. Browne, J, and Mohamed, S. The impact of mental health intensive case management on functioning and clinical outcomes of older black and white veterans with serious mental illness. Am J Geriatr Psychiatry. (2022) 30:1183–94. doi: 10.1016/j.jagp.2022.02.009
35. Chaabene, H, Prieske, O, Herz, M, Moran, J, Höhne, J, Kliegl, R, et al. Home-based exercise programmes improve physical fitness of healthy older adults: a PRISMA-compliant systematic review and meta-analysis with relevance for COVID-19. Ageing Res Rev. (2021) 67:101265. doi: 10.1016/j.arr.2021.101265
36. Drwal, KR, Wakefield, BJ, Forman, DE, Wu, WC, Haraldsson, B, and El Accaoui, RN. Home-based cardiac rehabilitation: experience from the veterans affairs. J Cardiopulm Rehabil Prev. (2021) 41:93–9. doi: 10.1097/HCR.0000000000000594
Keywords: physical activity, dropout, engagement, schizophrenia, bipolar disorder, recurrent major depressive disorder
Citation: Browne J, Elbogen EB, Mueser KT, Rudolph JL, Wu WC, Philip NS, Mills WL, Young AS, Sloane R and Hall KS (2023) Retention of older veterans with serious mental illness in a clinical exercise program. Front. Psychiatry. 14:1221030. doi: 10.3389/fpsyt.2023.1221030
Edited by:
Rajesh Tampi, Creighton University, United StatesReviewed by:
Anil K. Bachu, Baptist Health Foundation, United StatesSenthil Vel Rajan Rajaram Manoharan, Huntsville Hospital, United States
Copyright © 2023 Browne, Elbogen, Mueser, Rudolph, Wu, Philip, Mills, Young, Sloane and Hall. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Julia Browne, SnVsaWEuYnJvd25lQHZhLmdvdg==
 Julia Browne
Julia Browne Eric B. Elbogen
Eric B. Elbogen Kim T. Mueser
Kim T. Mueser James L. Rudolph1,7
James L. Rudolph1,7 Wen Chih Wu
Wen Chih Wu Noah S. Philip
Noah S. Philip Richard Sloane
Richard Sloane